- 1Department of Psychology, Manchester Metropolitan University, Manchester, United Kingdom
- 2Faculty of Health Sciences, Mejiro University, Saitama, Japan
- 3Department of Psychology, University of Turin, Turin, Italy
- 4Laboratory of Research and Interventions in Psychoanalysis (psiA), Department of Clinical Psychology, Institute of Psychology, University of São Paulo, São Paulo, Brazil
by Granieri, A., Bonafede, M., Marinaccio, A., Iavarone, I., Marsili, D., and Franzoi, I. G. (2020). Front. Psychol. 11:584320. doi: 10.3389/fpsyg.2020.584320
Recently, Granieri et al. (2020) highlighted multiple similarities between COVID-19 and Malignant Mesothelioma (MM). Here, we argue that despite the relevant similarities between these two conditions, their differences—including aetiology, infection pattern, chronological course, physical symptoms, and prognosis—outweigh their similarities. Moreover, we suggest the need to move away from a mere symptom consideration, adopting an ecological perspective focused on the different levels on which trauma occurs and the intra- and inter-personal dynamics involved in these diseases.
Firstly, as the Authors suggested, there is an important difference between the causative processes in MM and COVID-19, which reflects on their mental representations and dynamics. As asbestos exposure is usually connected to industrial activity, MM can be characterised as an occupational disease (Noonan, 2017), for which responsibility and intentionality can be traced in companies, purposely exposing their workers to harmful pollutants and prioritising their profit instead of people's safety (Guglielmucci et al., 2014). MM patients often feel betrayed by their employers, with consequent anger and claims for compensation (Sherborne et al., 2020). These behaviours could be seen as an attempt to minimise feelings of guilt over one own's responsibility for negative health outcomes, to find an external scapegoat to blame and to increase the perceived control over a situation entailing feelings of danger and helplessness (Rothschild et al., 2012; Guglielmucci, 2016).
Conversely, COVID-19 is a pandemic of probable zoonotic origin (Ivers and Walton, 2020)—despite the controversies about its origins (Mallapaty et al., 2021)—and there is, therefore, no identifiable culprit. COVID-19 has represented a global mental health crisis [World Health Organization (WHO), 2020a for a large-scale meta-analysis of the evidence of COVID-19 impact on public mental health services, see Liu et al., 2021] leading to widespread negative consequences on the mental health and well-being of individuals, communities, and societies (Dong and Bouey, 2020; Kazlauskas and Quero, 2020; Shigemura et al., 2020) and financial and economic disruption (Pak et al., 2020; World Health Organization (WHO), 2020b). In other words, when considering COVID-19, we need to take into account a systemic dimension of trauma and the presence of a violation of social trust. The lack of clear information about the disease's transmission and the available treatments have contributed to promoting uncertainty, fear of dying and fear of others, perceived as a possible vehicle of infection (Presti et al., 2020; Schimmenti et al., 2020). Despite—as the Authors argue—similar dynamics related to the fear of an “aerial contagion” brought by an “invisible killer” and the fear to infect/to be infected by others have also been found to be related to MM (Guglielmucci et al., 2015, 2018), these dynamics are mainly found in people residing in contaminated sites, in which asbestos exposure assumes a wider resonance as it potentially applies to the whole community.
Additionally, the traumatic breadth of the COVID-19 situation was enhanced by the social restrictions imposed by authorities, which did not occur in MM and have often caused people to experience loss of social interactions and income, increasing the prevalence rates of psychological problems all over the world (see for example Ahrens et al., 2021; Evans et al., 2021).
In emergency and crisis situations, people often turn to authorities to receive guidance and support and the quality of their responses can influence how the public copes with hardship (Smith, 2006; Glik, 2007). Since the start of the pandemic, individuals have relied on governments, services, and institutions which have often failed to recognise these vulnerabilities in their citizens and to respond appropriately to their needs (Altman, 2020; Karlsson, 2020; Olivia et al., 2020; Ham, 2021), often worsening socio-economic inequalities (Dorn et al., 2020) and betraying people's needs for security, protection, and care (Klest et al., 2020). This responsiveness failure constitutes a type of traumatic experience known as “institutional betrayal,” which refers to wrongdoings perpetrated by institutions upon individuals relying on them and include failure to prevent and respond appropriately to individuals' needs (Smith and Freyd, 2013, 2014). All these dynamics put to test—consciously or unconsciously—the capability of the mind to deal with feelings of powerless and helplessness, exposing people to long-lasting detrimental psychological effects that may even influence future generations (Leuzinger-Bohleber and Montigny, 2021).
Therefore, whilst the traumatic sequelae of MM are mainly situated at an individual and community level, the ones related to COVID-19 can be best understood as occurring at a systemic level, as they led to a cumulative, collective/societal trauma affecting the relationships among individuals and between individuals and their “macrosystem” (Scalabrini et al., 2020).
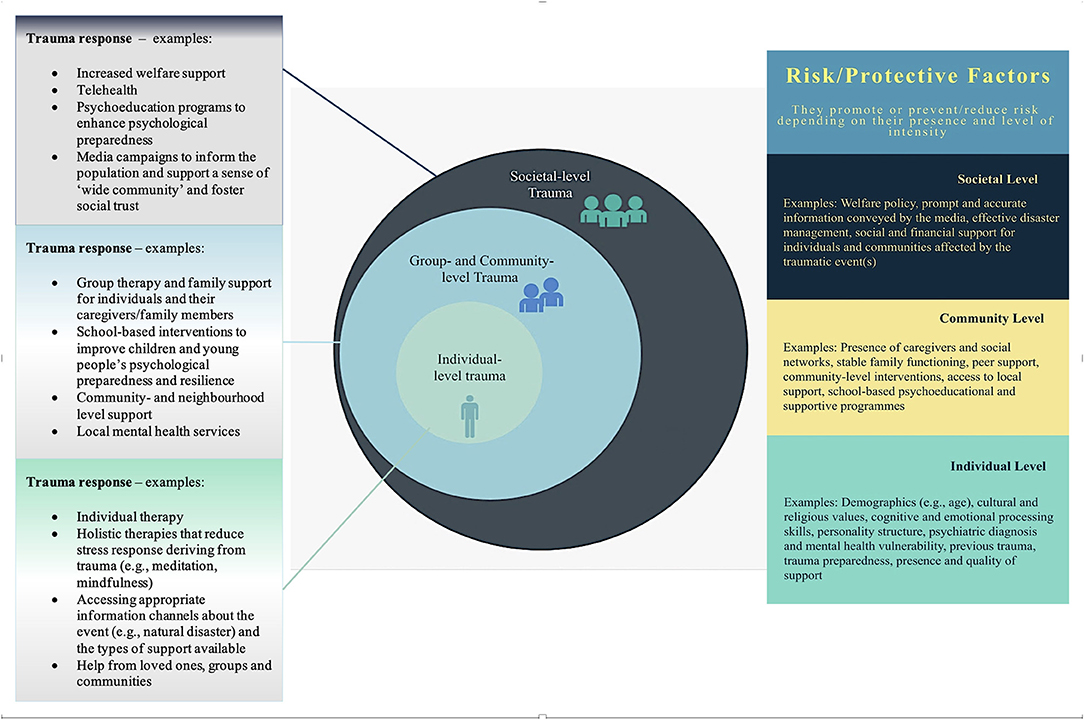
In Bronfenbrenner's 1979 ecological model, the “macrosystem” encompasses -among others- cultural influences, media messages, social policies, economic systems, government agencies, educational, and healthcare resources. This considered, to better understand the differences between the type of trauma (and its sequelae) in MM and COVID-19, we propose a model named “Ecological Response to Complex Trauma (ERCT) model (Figure 1).”
The ERCT model entails three concentric levels (individual, community, and societal) that trauma can occur on. For each level, there are specific mental representations of the traumatic situation and risk/protective factors, which are intertwined and create cross-pathways among levels. We also suggest some of the measures that should be present on each level to mitigate the impact of trauma. For example, some of the individual-level protective factors include emotional and cognitive preparedness to face a natural or man-made disaster (Gabriel et al., 2007; Roudini et al., 2017), absence of pre-existing trauma and psychiatric history (Alvarez and Hunt, 2005; Esterwood and Saeed, 2020), good emotional regulation skills (Restubog et al., 2020; Wang et al., 2021), and sense of control during and after the disaster (Reich, 2006). At collective and societal levels, examples of protective factors include social support (Ehring et al., 2011; Huang et al., 2013; Pietrzak et al., 2014), community-level preparedness training (Morrissey and Reser, 2003), receiving post-disaster professional support (Tak et al., 2007; Brooks et al., 2016) and using social media as a source of information and psychological “first aid” (Finch et al., 2016; Yang et al., 2019). Social media were also used to cope with social isolation and feelings of loneliness in COVID-19 lockdown phases (Boursier et al., 2020), providing an “online community” that improved people's collective resilience (Marzouki et al., 2021). Previous literature on collective/social traumatic events (e.g., Eriksson, 2015; Neubaum et al., 2014) showed that in disaster contexts, social media can be useful for social regulation and information sharing. Nonetheless, during COVID-19 social media also contributed to spreading panic (Ahmad and Murad, 2020), and in some cases, the fear of “missing out” and becoming “socially invisible” resulted in excessive use of online social interactions (Gioia et al., 2021), showing a dual-sided connotation of social media engagement as both able to foster relational closeness and alleviate social panic (Wiederhold, 2020; Cauberghe et al., 2021; Musetti et al., 2021) and as a maladaptive behaviour leading to increased levels of anxiety and negative affect contagion (Boursier et al., 2020; Shao et al., 2021).
Clinical implications of our model also are relevant for targeting psychological interventions. In our model, MM could be conceptualised as a two-level traumatic event affecting MM patients and families—in line with Granieri et al. (2020), group therapy could be beneficial to address the effects of MM-related trauma. Conversely, as COVID-19 is a social catastrophe, it would be best addressed with a combination of interventions encompassing the three trauma levels. In other words, when in presence of traumatic events affecting the individual, community and societal levels, the type of trauma response should also be complex and multi-level. This implies that social agents (e.g., governments, policymakers, social media) should acknowledge their responsibility in supporting trauma containment and trauma healing and show responsiveness particularly in two main domains: (1) Healthcare and (2) Informative communication to foster education and trauma preparedness. More specifically, a wider range of need-based, person-centred interventions for different target populations (e.g., COVID-19 survivors, their family members, healthcare professionals, and the general public) should be provided, with specific consideration for the socio-economic determinants of health that may increase risk or provide protection against mortality, morbidity, and trauma-related outcomes (Abrams and Szefler, 2020; Burström and Tao, 2020). These interventions should reach a large number of individuals in a relatively short time, with particular attention to the most vulnerable segments of society (e.g., immigrants, ethnic minorities, people with unstable and low-income jobs), to mitigate pre-existing socioeconomic disparities and the pandemic-related burden (Bambra et al., 2020; Dorn et al., 2020).
Digitally delivered care and telehealth (e.g., video calls or app-delivered support) have the potential to achieve these aims, fostering a considerable sense of control over one's health, and facilitating access to services (McGeary et al., 2012; Keshvardoost et al., 2020). Telehealth and digital interventions have proven to be beneficial to those experiencing mental health issues during human-caused and natural disasters (Ruzek et al., 2016) and recent evidence (Centers for Disease Control Prevention, 2020; Monaghesh and Hajizadeh, 2020) indicated that their use increased exponentially during COVID-19. Moreover, in societal-level and global crises, governments and institutions should pay particular attention to the communicative strategies adopted, to avoid the confusing messages and panic-eliciting communication that occurred during the COVID-19 pandemic (Garrett, 2020; Sauer et al., 2021).
On the contrary, trauma-informed communication should entail the use of media (including social media) to contain negative emotions, “buffer” the traumatic response and help to maintain a sense of social trust, which is likely to be deeply compromised in situations of systemic-level trauma (Bachem et al., 2020).
In conclusion, the ERCT model proposes that complex trauma such as the one characterising COVID-19 needs to be addressed with multi-level trauma-informed care. Governments and institutions should be more aware of the dynamics at play and of their role in them. A structural change in our society is needed, “transitioning from a primary disease-centred system to a balanced preventive and healthcare system” (Fontana et al., 2021, 4). Discussions should be held on how to engage current and future generations to allow for this “switch” to happen. In our opinion, health literacy rooted in the complex array of relations among physical, socio-economic, affective, and environmental dimensions that can worsen or mitigate trauma effects should be embedded in education pathways across the life span (and particularly in early stages) to shape health and well-being across people's lives and promote appropriate individual, community, and systemic responses to trauma.
Author Contributions
DD wrote the manuscript, led the literature research, conceived the clinical-conceptual model in collaboration with FG, and designed the figures with input from all authors. FG co-produced the clinical-conceptual model and critically revised the manuscript providing important theoretical and clinical contributions. JS contributed to the writing of the manuscript offering feedback and valuable advice throughout the writing process. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abrams, E. M., and Szefler, J. S. (2020). COVID-19 and the impact of social determinants of health. Lancet Respir. Med. 8, 659–661. doi: 10.1016/S2213-2600(20)30234-4
Ahmad, A. R., and Murad, H. R. (2020). The impact of social media on panic during the Covid-19 pandemic in Iraqi Kurdistan: online questionnaire study. J. Med. Internet Res. 22:e19556. doi: 10.2196/19556
Ahrens, K. F., Neumann, R. J., Kollmann, B., Plichta, M. M., Lieb, K., Tüscher, O., et al. (2021). Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry 20, 140–141. doi: 10.1002/wps.20830
Altman, D. (2020). Understanding the US failure on coronavirus—an essay by drew Altman. BMJ 1–3. doi: 10.1136/bmj.m3417
Alvarez, J., and Hunt, M. (2005). Risk and resilience in canine search and rescue handlers after 9/11. J. Traumatic Stress 18, 497–505. doi: 10.1002/jts.20058
Bachem, R., Tsur, N., Levin, Y., Abu-Raiya, H., and Maercker, A. (2020). Negative Affect, fatalism, and perceived institutional betrayal in times of the coronavirus pandemic: a cross-cultural investigation of control beliefs. Front. Psychiatry 11:589914. doi: 10.3389/fpsyt.2020.589914
Bambra, C., Riordan, R., Ford, J., and Matthews, F. (2020). The COVID-19 pandemic and health inequalities. J. Epidemiol. Commun. Health 74, 964–968. doi: 10.1136/jech-2020-214401
Boursier, V., Gioia, F., Musetti, A., and Schimmenti, A. (2020). Facing loneliness and anxiety during the COVID-19 isolation: the role of excessive social media use in a sample of Italian adults. Front. Psychiatry. 11:586222. doi: 10.3389/fpsyt.2020.586222
Bronfenbrenner, U. (1979). The Ecology of Human Development: Experiments in Nature and Design. Cambridge, MA: Harvard University Press.
Brooks, S. K., Dunn, R., Amlôt, R., Greenberg, N., and Rubin, J. G. (2016). Social and occupational factors associated with psychological distress and disorder among disaster responders: a systematic review. BMC Psychol. 4:18. doi: 10.1186/s40359-016-0120-9
Burström, B., and Tao, W. (2020). Social determinants of health and inequalities in COVID-19. Eur. J. Public Health 30, 617–618. doi: 10.1093/eurpub/ckaa095
Cauberghe, V., Wesenbeeck, I. V., De Jans, S., Hudders, L., and Ponnet, K. (2021). How adolescents use social media to cope with feelings of loneliness and anxiety during COVID-19 lockdown. Cyberpsychol. Behav. Soc. Netw. 24, 250–257. doi: 10.1089/cyber.2020.0478
Centers for Disease Control and Prevention (2020). Using Telehealth to Expand Access to Essential Health Services During the COVID-19 Pandemic. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html (accessed May 12, 2021).
Dong, L., and Bouey, J. (2020). Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 26, 1616–1618. doi: 10.3201/eid2607.200407
Dorn, A. V., Cooney, R. E., and Sabin, M. L. (2020). COVID-19 exacerbating inequalities in the US. Lancet 395, 1243–1244. doi: 10.1016/s0140-6736(20)30893-x
Ehring, T., Razik, S., and Emmelkamp, P. M. G. (2011). Prevalence and predictors of posttraumatic stress disorder, anxiety, depression, and burnout in Pakistani Earthquake recovery workers. Psychiatry Res. 185, 161–166. doi: 10.1016/j.psychres.2009.10.018
Eriksson, M. (2015). Managing collective trauma on social media: the role of Twitter after the 2011 Norway Attacks. Media Cult. Soc. 38, 365–380. doi: 10.1177/0163443715608259
Esterwood, E., and Saeed, S. A. (2020). Past epidemics, natural disasters, Covid19, and mental health: learning from history as we deal with the present and prepare for the future. Psychiatr. Q. 91, 1121–1133. doi: 10.1007/s11126-020-09808-4
Evans, S., Alkan, E., Bhangoo, J. K., Tenenbaum, H., and Ng-Knight, T. (2021). Effects of the COVID-19 lockdown on mental health, wellbeing, sleep, and alcohol use in a UK student sample. Psychiatry Res. 298:113819. doi: 10.1016/j.psychres.2021.113819
Finch, K. C., Snook, K. R., Duke, C. H., Fu, K.-W., Tse, Z. T. H., Adhikari, A., et al. (2016). Public health implications of social media use during natural disasters, environmental disasters, and other environmental concerns. Nat. Hazards 83, 729–760. doi: 10.1007/s11069-016-2327-8
Fontana, L., Fasano, A., Chong, Y. S., Vineis, P., and Willett, W. C. (2021). Transdisciplinary research and clinical priorities for better health. PLoS Med. 18:e1003699. doi: 10.1371/journal.pmed.1003699
Gabriel, R., Ferrando, L., Sainz Cortón, E., Mingote, C., García-Camba, E., Liria, A. F., et al. (2007). Psychopathological consequences after a terrorist attack: an epidemiological study among victims, the general population, and police officers. Euro. Psychiatry 22, 339–346. doi: 10.1016/j.eurpsy.2006.10.007
Garrett, L. (2020). COVID-19: the medium is the message. Lancet 395, 942–943. doi: 10.1016/s0140-6736(20)30600-0
Gioia, F., Fioravanti, G., Casale, S., and Boursier, V. (2021). The effects of the fear of missing out on people's social networking sites use during the COVID-19 pandemic: the mediating role of online relational closeness and individuals' online communication attitude. Front. Psychiatry 12:146. doi: 10.3389/fpsyt.2021.620442
Glik, D. C. (2007). Risk communication for public health emergencies. Annu. Rev. Public Health 28, 33–54. doi: 10.1146/annurev.publhealth.28.021406.144123
Granieri, A., Bonafede, M., Marinaccio, A., Iavarone, I., Marsili, D., and Franzoi, I. G. (2020). Sars-Cov-2 and asbestos exposure: can our experience with mesothelioma patients help us understand the psychological consequences of Covid-19 and develop interventions?. Front. Psychol. 11:584320. doi: 10.3389/fpsyg.2020.584320
Guglielmucci, F. (2016). Vita, Morte E Lotta Nel Sito Contaminato Di Casale Monferrato. Alcune Riflessioni Tra Clinica e Ricerca. Genoa: Fratelli Frilli.
Guglielmucci, F., Franzoi, I. G., Barbasio, C. P., Borgogno, F. V., and Granieri, A. (2014). Helping traumatized people survive: a psychoanalytic intervention in a contaminated site. Front. Psychol. 5:1419. doi: 10.3389/fpsyg.2014.01419
Guglielmucci, F., Franzoi, I. G., Bonafede, M., Borgogno, F. V., Grosso, F., and Granieri, A. (2018). The less I think about it, the better I feel: a thematic analysis of the subjective experience of malignant mesothelioma patients and their caregivers. Front. Psychol. 9:205. doi: 10.3389/fpsyg.2018.00205
Guglielmucci, F., Franzoi, I. G., Zuffranieri, M., and Granieri, A. (2015). Living in contaminated sites: which cost for psychic health?. Mediterranean J. Soc. Sci. 6:207.
Ham, C. (2021). The UK's poor record on Covid-19 is a failure of policy learning. BMJ 372, 1–2. doi: 10.1136/bmj.n284
Huang, J., Liu, Q., Li, J., Li, X., You, J., Zhang, L., et al. (2013). Post-traumatic stress disorder status in a rescue group after the Wenchuan Earthquake relief. Neural Regener. Res. 8, 1898–1906. doi: 10.3969/j.issn.1673-5374.2013.20.009
Ivers, L. C., and Walton, D. A. (2020). Covid-19: global health equity in pandemic response. Am. J. Trop. Med. Hyg. 102, 1149–1150. doi: 10.4269/ajtmh.20-0260
Karlsson, C.-J. (2020). Sweden's second wave is a failure of government—and guidance. Foreign Policy. Available online at: https://foreignpolicy.com/2020/12/18/sweden-second-covid-wave-failure-of-government-guidance/ (accessed December 18, 2020).
Kazlauskas, E., and Quero, S. (2020). Adjustment and coronavirus: how to prepare for COVID-19 pandemic-related adjustment disorder worldwide?. Psychol. Trauma Theory Res. Prac. Policy 12, S22–S24. doi: 10.1037/tra0000706
Keshvardoost, S., Bahaadinbeigy, K., and Fatehi, F. (2020). Role of telehealth in the management of Covid-19: lessons learned from previous Sars, Mers, and Ebola outbreaks. Telemed. e-Health 26, 850–852. doi: 10.1089/tmj.2020.0105
Klest, B., Smith, P. C., May, C., McCall-Hosenfeld, J., and Tamaian, A. (2020). COVID-19 has united patients and providers against institutional betrayal in health care: a battle to be heard, believed, and protected. Psychol. Trauma Theory Res. Prac. Policy 12, S159–S161. doi: 10.1037/tra0000855
Leuzinger-Bohleber, M., and Montigny, N. (2021). The pandemic as a developmental risk. Int. J. Appl. Psychoanalytic Stud. 18, 121–132. doi: 10.1002/aps.1706
Liu, X., Zhu, M., Zhang, R., Zhang, J., Zhang, C., Liu, P., et al. (2021). Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence. Transl. Psychiatry 11, 1–10. doi: 10.1038/s41398-021-01501-9
Mallapaty, S., Maxmen, A., and Callaway, E. (2021). ‘Major stones unturned’: COVID origin search must continue after WHO report, say Scientists. Nature 590, 371–372. Available online at: https://www.nature.com/articles/d41586-021-00375-7
Marzouki, Y., Aldossari, F. S., and Veltri, G. A. (2021). Understanding the buffering effect of social media use on anxiety during the Covid-19 pandemic lockdown. Humanities Soc. Sci. Commun. 47, 1–10. doi: 10.1057/s41599-021-00724-x
McGeary, D., McGeary, C., Gatchel, R. J., Allison, S., and Hersh, A. (2012). Assessment of research quality of telehealth trials in pain management: a meta-analysis. Pain Prac. 13, 422–431. doi: 10.1111/j.1533-2500.2012.00601.x
Monaghesh, E., and Hajizadeh, A. (2020). The role of telehealth during Covid-19 outbreak: a systematic review based on current evidence. BMC Public Health 20:1193. doi: 10.1186/s12889-020-09301-4
Morrissey, S., and Reser, J. P. (2003). Evaluating the effectiveness of psychological preparedness advice in community cyclone preparedness materials. Austral. J. Emerg. Manage. 18, 46–61. doi: 10.3316/ielapa.281780145360789
Musetti, A., Starcevic, V., Boursier, V., Corsano, P., Billieux, J., and Schimmenti, A. (2021). Childhood emotional abuse and problematic social networking sites use in a sample of italian adolescents: the mediating role of deficiencies in self-other differentiation and uncertain reflective functioning. J. Clin. Psychol. 77, 1666–1684. doi: 10.1002/jclp.23138
Neubaum, G., Rösner, L., Rosenthal-von der Pütten, A. M., and Krämer, N. (2014). Psychosocial functions of social media usage in a disaster situation: a multi-methodological approach. Comput. Human Behav. 34, 28–38. doi: 10.1016/j.chb.2014.01.021
Noonan, C. W. (2017). Environmental asbestos exposure and risk of mesothelioma. Ann. Transl. Med. 5, 234–234. doi: 10.21037/atm.2017.03.74
Olivia, S., Gibson, J., and Nasrudin, R. (2020). Indonesia in the time of Covid-19. Bull. Indones. Econ. Stud. 56, 143–174. doi: 10.1080/00074918.2020.1798581
Pak, A., Adegboye, O. A., Adekunle, A. I., Rahman, K. M., McBryde, E. S., and Eisen, D. P. (2020). Economic consequences of the COVID-19 outbreak: the need for epidemic preparedness. Front. Public Health 8:241. doi: 10.3389/fpubh.2020.00241
Pietrzak, R. H., Feder, A., Singh, R., Schechter, C. B., Bromet, E. J., Katz, C. L., et al. (2014). Trajectories of PTSD risk and resilience in world trade center responders: an 8-year prospective cohort study. Psychol. Med. 44, 205–219. doi: 10.1017/S0033291713000597
Presti, G., McHugh, L., Gloster, A., Karekla, M., and Haye, S. C. (2020). The dynamics of fear at the time of Covid-19: a contextual behavioral science perspective. Clin. Neuropsychiatry J. Treatment Eval. 17, 65–71. doi: 10.36131/CN20200206
Reich, J. (2006). Three psychological principles of resilience in natural disasters. Disaster Prev. Manag. 15, 793–798. doi: 10.1108/09653560610712739
Restubog, S. L. D., Ocampo, A. C. G., and Wang, L. (2020). Taking control amidst the chaos: emotion regulation during the COVID-19 pandemic. J. Vocat. Behav. 119:103440. doi: 10.1016/j.jvb.2020.103440
Rothschild, Z., Landau, M. J., Sullivan, D., and Keefer, L. A. (2012). A dual-motive model of scapegoating: displacing blame to reduce guilt or increase control. J. Pers. Soc. Psychol. 102, 1148–1163. doi: 10.1037/a0027413
Roudini, J., Khankeh, H. R., and Witruk, E. (2017). Disaster mental health preparedness in the community: a systematic review study. Health Psychol. Open 4, 1–12. doi: 10.1177/2055102917711307
Ruzek, J., Kuhn, E., Jaworski, B. K., Owen, J. E., and Ramsey, K. M. (2016). Mobile mental health interventions following war and disaster. Mhealth 2, 1–12. doi: 10.21037/mhealth.2016.08.06
Sauer, M. A., Truelove, S., Gerste, A. K., and Limaye, R. J. (2021). A failure to communicate? How public messaging has strained the COVID-19 response in the United States. Health Secur. 19, 65–74. doi: 10.1089/hs.2020.0190
Scalabrini, A., Mucci, C., Lucherini Angeletti, L., and Northoff, G. (2020). The self and its world: a neuro-ecological and temporo-spatial account of existential fear. Clin. Neuropsychiatry 17, 46–58. doi: 10.36131/CN20200203
Schimmenti, A., Starcevic, V., Giardina, A., Khazaal, Y., and Billieux, J. (2020). Multidimensional assessment of Covid-19-related fears (Mac-Rf): a theory-based instrument for the assessment of clinically relevant fears during pandemics. Front. Psychiatry 11:748. doi: 10.3389/fpsyt.2020.00748
Shao, R., Shi, Z., and Zhang, D. (2021). Social media and emotional burnout regulation during the COVID-19 pandemic: multilevel approach. J. Med. Internet Res. 23:e27015. doi: 10.2196/27015
Sherborne, V., Seymour, J., Taylor, B., and Tod, A. (2020). What are the psychological effects of mesothelioma on patients and their carers? A scoping review. Psycho Oncol. 29, 1464–1473. doi: 10.1002/pon.5454
Shigemura, J., Ursano, R. J., Morganstein, J. C., Kurosawa, M., and Benedek, D. M. (2020). Public responses to the novel 2019 coronavirus (2019-ncov) in Japan: mental health consequences and target populations. Psychiatry Clin. Neurosci. 74, 281–282. doi: 10.1111/pcn.12988
Smith, C. P., and Freyd, J. J. (2013). Dangerous safe havens: institutional betrayal exacerbates sexual trauma. J. Trauma. Stress 26, 119–124. doi: 10.1002/jts.21778
Smith, C. P., and Freyd, J. J. (2014). Institutional betrayal. Am. Psychol. 69, 575–587. doi: 10.1037/a0037564
Smith, R. D. (2006). Responding to global infectious disease outbreaks: lessons from SARS on the role of risk perception, communication and management. Soc. Sci. Med. 63, 3113–3123.
Tak, S. W., Driscoll, R., Bernard, B., and West, C. (2007). Depressive symptoms among firefighters and related factors after the response to Hurricane Katrina. J. Urban Health 84, 153–161. doi: 10.1007/s11524-006-9155-1
Wang, Q.-Q., Fang, Y.-Y., Huang, H.-L., Lv, W.-J., Wang, X.-X., Yang, T.-T., et al. (2021). Anxiety, depression and cognitive emotion regulation strategies in chinese nurses during the COVID-19 outbreak. J. Nurs. Manage. 29, 1263–1274. doi: 10.1111/jonm.13265
Wiederhold, B. K. (2020). Using social media to our advantage: alleviating anxiety during a pandemic. Cyberpsychol. Behav. Soc. Netw. 23, 197–198. doi: 10.1089/cyber.2020.29180.bkw
World Health Organization (WHO). (2020a). Coronavirus Disease 2019 (COVID-19): Situation Report 85. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed July 29, 2021).
World Health Organization (WHO). (2020b). Impact of COVID-19 on People's Livelihoods, Their Health and Our Food Systems. Available online at: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people's-livelihoods-their-health-and-our-food-systems (accessed July 31, 2021).
Keywords: COVID-19, asbestos, ecological trauma, trauma interventions, risk prevention, post-disaster trauma, public health
Citation: Di Basilio D, Shigemura J and Guglielmucci F (2021) Commentary: SARS-CoV-2 and Asbestos Exposure: Can Our Experience With Mesothelioma Patients Help Us Understand the Psychological Consequences of COVID-19 and Develop Interventions? Front. Psychol. 12:720160. doi: 10.3389/fpsyg.2021.720160
Received: 03 June 2021; Accepted: 04 August 2021;
Published: 09 September 2021.
Edited by:
Alessandro Musetti, University of Parma, ItalyReviewed by:
Valentina Boursier, University of Naples Federico II, ItalyLucia Sideli, Libera Università Maria SS. Assunta, Italy
Copyright © 2021 Di Basilio, Shigemura and Guglielmucci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniela Di Basilio, ZC5kaS1iYXNpbGlvQG1tdS5hYy51aw==
 Daniela Di Basilio
Daniela Di Basilio Jun Shigemura
Jun Shigemura Fanny Guglielmucci
Fanny Guglielmucci