- 1School of Health Services Management, Anhui Medical University, Hefei, China
- 2Office of Science and Education, Suzhou Hospital Affiliated to Anhui Medical University, Suzhou, China
Background: Depression is a prevalent health condition among hypertension patients in elderly caring social organizations (SOs). Patients with hypertension and depression symptoms have worse health outcomes than those without depression. As the population ages, chronic and mental health issues such as depression of hypertension patients in elderly caring SOs have become prominent. However, the combined effects of social support, institutional satisfaction, and anxiety on depression among hypertension individuals in elderly caring SOs remain unclear. This study aimed to explore the mediating effects of institutional satisfaction and anxiety on the relationship between social support and depression among hypertension patients in elderly caring SOs in Anhui Province, China.
Methods: A cross-sectional study was conducted using a multi-stage stratified random sampling method. A questionnaire was used to collect data on demographic characteristics, the satisfaction of elderly caring SOs, social support, anxiety, and depression. A multiple linear regression model was utilized to investigate depression-related factors, and structural equation modeling (SEM) was employed to examine the relationships between social support, institutional satisfaction, anxiety, and depression among patients with hypertension in elderly caring SOs.
Results: Our results indicated that the mean scores of social support were 20.19 ± 6.98 and 1.92 ± 3.18 for anxiety, and 6.24 ± 5.03 for depression; besides, 33.3% of participants were very satisfied with elderly caring SOs, 48.5% were satisfied, and only 6.0% were dissatisfied or very dissatisfied. Comorbid chronic diseases were significantly associated with depression. Institutional satisfaction was directly negatively related to depression, whereas anxiety was directly positively correlated with depression. Social support had an indirect negative association with depression by the mediating effects of institutional satisfaction and anxiety.
Conclusions: The study highlights the importance of social support in maintaining mental health among hypertension patients residing in elderly caring SOs. To alleviate depression among hypertension patients in elderly caring SOs, strategies that target enhancing social support, institutional satisfaction, and anxiety reduction should be prioritized. More importantly, more attention should be paid to patients with comorbid chronic diseases.
Introduction
Hypertension is one of the most common chronic diseases worldwide, accounting for two-thirds of all strokes and half of all coronary disease, and thus representing a major risk factor for cardiovascular morbidity and mortality (Chobanian et al., 2003; Perkovic et al., 2007; Prince et al., 2015). Numerous surveys conducted in China have revealed an increased prevalence of hypertension, affecting 18.8% of the population in 2002 and 27.8% in 2014 (Wu et al., 2008; Li et al., 2017). By 2025, this disease is anticipated to affect 29% of the world's population (Mittal and Singh, 2010). Due to the rapidly increasing prevalence of hypertension and disease burden, its effective and timely management and control have become a basic public health service priority in China.
Depression is the major cause of disability among patients with chronic diseases, impacting 350 million people worldwide (Davidson et al., 2000; Long et al., 2015). Hypertension patients are more likely to develop depression, and depression has been recognized as an independent risk factor for hypertension (Davidson et al., 2000; Meurs et al., 2015). Patients with hypertension and depression have worse health status, poorer quality of life, impaired well-being, higher health care expenditure, and increased mortality than those without depression (Oganov et al., 2011; Scuteri et al., 2011; Tsartsalis et al., 2016; Shao et al., 2017). Furthermore, patients with depression display lower adherence to hypertension treatment (Krousel-Wood and Frohlich, 2010), resulting in a 50% failure rate (Stephenson, 1999; Naderi et al., 2012). These studies highlight the importance of addressing depression in hypertension patients.
Social support is defined as “the social resources that persons perceive to be available or that are provided to them” (Gottlieb and Bergen, 2010). It is one of the most well-documented psychosocial factors associated with physical health outcomes (Cohen et al., 2000; Pinquart and Duberstein, 2010; Compare et al., 2013), including hypertension (Strogatz and James, 1986). Prior studies have demonstrated the association between social support and depression among patients with hypertension (Dennis et al., 2008; Ma, 2018). Poor social support has also been linked to poor adherence to anti-hypertension treatment and poor blood pressure control (Berkman et al., 2000; Taher et al., 2014; Ojo et al., 2016) and may thus cause poor prognosis and eventually influence the mental state of hypertension patients.
According to a previous report, anxiety was one of the most prevalent classes of problems in China and abroad, with ~5.3% of the population suffering from anxiety (Yu et al., 2018; Shi et al., 2020). Moreover, hypertension patients are at greater risk of exhibiting anxious symptoms (Cheung et al., 2005; Wei and Wang, 2006). Additionally, 39% of individuals with a generalized anxiety disorder have been demonstrated to meet depression criteria (Hunt et al., 2002).
Institutional satisfaction refers to the elderly's subjective evaluation of their overall satisfaction level, including quality of life, quality of care, and quality of service in elderly caring social organizations (SOs). Satisfaction with primary healthcare services appears to affect depression (Kavalniene et al., 2018). Numerous research has demonstrated a negative correlation between life satisfaction and depression (Gómez-Restrepo et al., 2013; Atienza-González et al., 2020; Köttl et al., 2021). However, the relationship between institutional satisfaction and depression among hypertension patients in elderly caring SOs remains unknown.
Hypertension is prevalent among nursing home residents, with prevalence ranging from 72 to 90% worldwide (Simonson et al., 2011; Könner et al., 2014; Benetos et al., 2015; Harris-Kojetin et al., 2016). The ineffective control of hypertension patients may increase their difficulty in coping with depressive symptoms and the possibility of developing anxiety and a low level of institutional satisfaction. In China, nursing homes and elderly apartments are classified into three major types, which can be operated by government organizations, SOs, or private investors (Chu and Chi, 2008). Commonly, the government-sponsored or -owned nursing homes are mainly served older people who have been disabled in financial resources. On the other hand, older people who are affordable are often covered by nursing homes that are operated by private investors. While the others have dwelled in nursing homes operated by SOs, which can play a major role in planning and developing relevant services for the elderly (Brick and Clarfield, 2007; Yang, 2018). Yet, little attention has been paid to the potential of SOs to participate in China's elderly care services.
Furthermore, previous studies had investigated associations between social support, institutional satisfaction, anxiety, and depression (Seabrook et al., 2016; Alipour et al., 2019; Barnett et al., 2019); however, the combined effects of these factors on depression and the underlying mechanisms of those relationships remain unclear. Besides, lacking social support has been positively associated with anxiety in type 2 diabetic patients (Wu et al., 2013) and hospitalized cardiac patients (Hughes et al., 2004). Given recent findings indicating that anxiety predicts depression (Gay et al., 2010, 2017) and the acknowledged role of social support in mental health (Yasin and Dzulkifli, 2010), we speculated that anxiety mediates the relationship between social support and depression in hypertension patients in elderly caring SOs. In addition, a prior study demonstrated the relationship between social support and life satisfaction, as well as their interactions in explaining depression among the elderly (Moon, 2010; Nam and Bok, 2013; Matud et al., 2019; Fang et al., 2021). Thus, we hypothesized the mediation effect of institutional satisfaction on the association between social support and depression among hypertension patients in elderly caring SOs. Moreover, researchers suggest that a high level of anxiety is associated with lower levels of life satisfaction (Rogowska et al., 2020). A low level of institutional satisfaction may cause hypertension patients to have feelings of distrust and disgust of elderly caring SOs, resulting in anxiety symptoms.
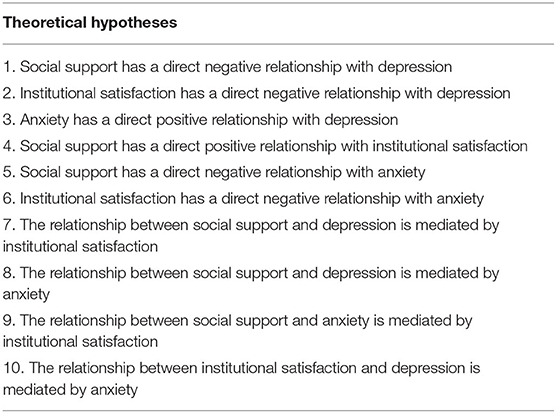
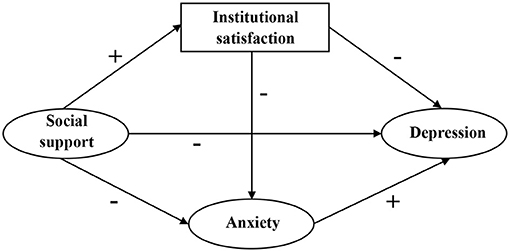
Thereby, to testify above mentioned research gaps and hypotheses, we employed structural equation modeling (SEM) to explore interrelationships between latent variables, which cannot be directly measured. According to the theoretical framework mentioned above, we developed the hypotheses shown in Table 1, corresponding to the structural equation model displayed in Figure 1. Eventually, we aimed to provide a reference for interventions targeting mental health improvement of hypertension patients in elderly caring social organizations.
Materials and Methods
Study Design and Data Collection
We conducted this cross-sectional survey in Anhui province, eastern China, between November and December 2019. Moreover, we used a multi-stage stratified random sampling method to ensure a representative sample considering socioeconomic levels and geographic location. As a result, we selected 15 elderly caring SOs from six cities in Anhui province: Fuyang, Anqing, Chizhou, Huainan, Luan, and Suzhou.
Following that, we identified potential participants, individuals diagnosed with hypertension in secondary hospitals and above, using chronic disease-related information from health records of residents in elderly caring SOs. With assistance from elderly caring SOs managers, skilled or trained graduate students personally conducted structured face-to-face interviews with participants. First, students verbally explained the study's purposes and procedures to interviewees, who were then requested to complete voluntary consent forms before the interviews. Those who could not fully understand verbal explanations due to severe deafness and limited communication skills were excluded. The analysis included 518 hypertension patients who agreed to be interviewed.
Measures
Demographic Data
Demographic data comprised age, gender, education level, visited frequency of relatives, marital status, self-perceived health level, and comorbid chronic diseases. Age was categorized as <70, 70–79, and ≥80 years. The educational level was divided into middle school and above, primary school, and no formal education. The visited frequency of relatives was classified into three categories: <2, 2–4, and ≥5 (times per month). Marital status was defined as a binary variable: married with spouse and divorced, unmarried, or widowed. Self-perceived health level was divided into low, medium, and high. We asked participants whether they were diagnosed with heart disease, malignant tumors, chronic obstructive pulmonary disease, diabetes (type 1 or 2), neurological disorders, hyperlipidemia, chronic hepatitis, or other chronic diseases. Finally, hypertension patients were categorized into a comorbid chronic diseases group if they had at least one of the above-mentioned diseases (Yan et al., 2019).
Social Support
Social support was assessed using Multidimensional Scale of Perceived Social Support (MSPSS) assessment scores. Gregory developed MSPSS scale to identify the participants' perceived social support elements (Zimet et al., 1988). This measure includes three subscales assessing perceived support quality from family, friends, and special persons. Participants rated on a seven-point Likert response format (1 = “very strongly disagree” to 7 = “very strongly agree”). As a result, higher scores indicate high social support (Zimet et al., 1988). Scores from 12 to 48 indicate low social support, scores from 49 to 68 indicate moderate social support, and scores from 69 to 84 indicate high social support. In this study, Cronbach's α was found to be 0.98 for the family support subfield, 0.98 for the friend support subfield, 0.97 for the special person support subfield, and 0.96 for the scale in total, respectively, suggesting an adequate psychometric property in this sample.
Anxiety
Anxiety was measured using Generalized Anxiety Disorder 7-item Scale (GAD-7) (Spitzer et al., 2006). Participants indicate how frequently they have been bothered by each symptom over the last 2 weeks on a four-point Likert scale (0 = not at all, to 3 = nearly every day). Possible scores range from 0 to 21, with higher scores indicating higher levels of generalized anxiety. According to the scoring standard, the GAD-7 score is divided into 4 groups: 0–5, 6–10, 10–15, 16–21, corresponding to no, mild, moderate, and severe anxiety, respectively (Spitzer et al., 2006; Yang et al., 2020). GAD-7 has been shown to produce reliable and valid scores in community studies (Hinz et al., 2017), and the reliability in the current sample was acceptable (Cronbach's α = 0.88).
Institutional Satisfaction
A single item, “What is your overall satisfaction with the elderly caring social organizations?” was used to measure the institutional satisfaction of hypertension patients in elderly caring SOs. Many studies use a single item to measure overall satisfaction in large-scale satisfaction surveys with good reliability (Labarbera and Mazursky, 1983; Yi, 1990; Mittal et al., 1998). In this study, we employed a single item with a Likert 5-point option to measure the overall satisfaction of elderly caring SOs, where 1 represents very dissatisfied, and 5 represents very satisfied.
Depression
To assess depression, the Center for Epidemiologic Studies Depression Scale 10-item version (CESD-10) was employed, which has been demonstrated to appropriately reflect depressive symptoms experienced in the previous week (Andresen et al., 1994). CESD-10 includes ten items addressing depressed affect, somatic symptoms, and positive affect. The options for each item range from “rarely or none of the time” (score of 0) to “all of the time” (score of 3). The scoring is reversed for items 5 and 8, which are positive effect statements. Total scores can range from 0 to 30. Scores of 10 or over indicate clinically relevant depression (Andresen et al., 1994). The scale has excellent internal reliability (Cronbach's α = 0.80) and good validity (Roberts and Vernon, 1983). In the present study, Cronbach's α coefficient was acceptable (Cronbach α =0.81).
Statistical Analysis
Statistical analyses were conducted using SPSS 23.0 and MPLUS 8.3. First, descriptive statistics were calculated to describe the sample, and continuous variables are presented as mean ± standard deviation, while categorical variables are presented as percentages (%). Second, Pearson correlations were employed to explore the relationships between social support, institutional satisfaction, anxiety, and depression. A multiple linear regression model was used to estimate associations between independent variables and depression. Finally, SEM was used to test the hypotheses about four study variables. We used subscale scores of social support, scale scores of anxiety and depression as measurement variables, then used the total scores of these measures as latent variables. Institutional satisfaction was included as a measurement variable. Statistical significance was set at P < 0.05.
Results
Descriptive Analysis
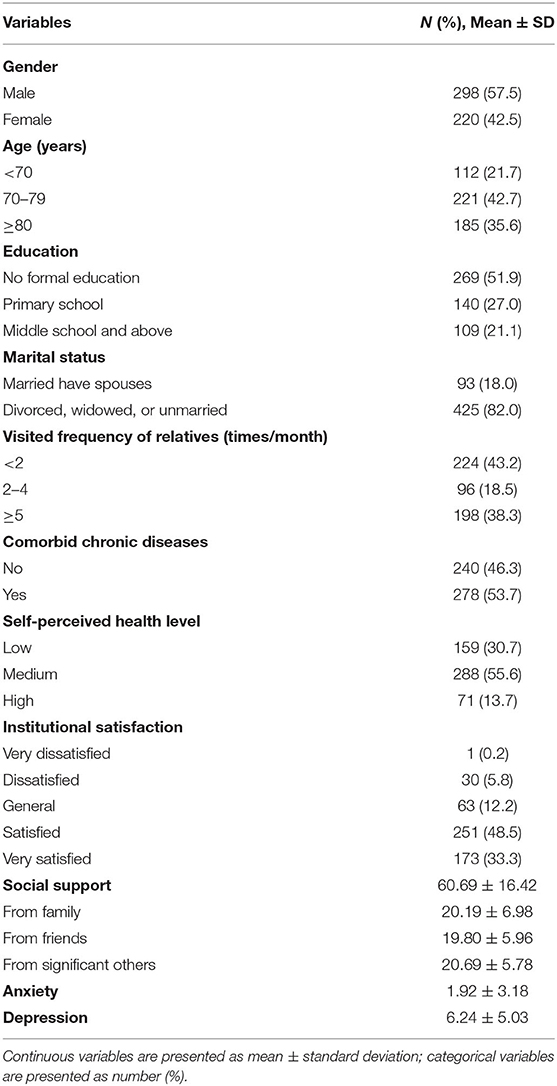
Descriptive statistics of the sample are displayed in Table 2. The participants contained 298 men (57.5%) and 220 women (42.5%). The highest proportion was 70–79 years old (42.7%), with no formal education (51.9%). Most participants were divorced, widowed, or unmarried (82.0%) and had comorbid chronic diseases (53.7%). A large proportion of hypertension patients in elderly caring SOs are visited by relatives less than twice a month (43.2%), and low levels of self-perceived health (30.7%) are more than those high levels of self-perceived health (13.7%).
The mean scores for social support, anxiety and depression were 60.69 ± 16.42, 1.92 ± 3.18, and 6.24 ± 5.03, respectively. The proportion of individuals with a high level of social support was 38.0%, and 86.7% of subjects had no anxiety symptoms. In addition, 21.4% of hypertension patients in elderly caring SOs exhibited depressive symptoms. Furthermore, 81.8% of participants were satisfied or very satisfied with their elderly caring SOs.
Correlations Between Study Variables
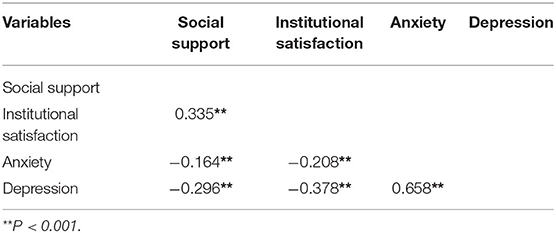
Correlations between social support, institutional satisfaction, anxiety, and depression are presented in Table 3. Social support was negatively correlated with anxiety and depression but positively correlated with the satisfaction of elderly caring SOs. Additionally, there was a significant negative correlation between institutional satisfaction and anxiety and depression. Anxiety was significantly positively correlated with depression.
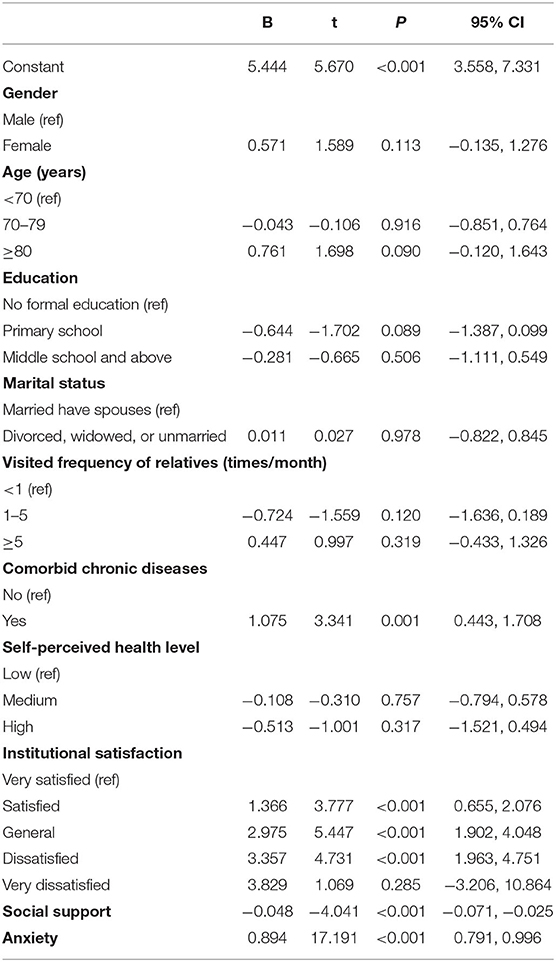
Linear Regression Analysis of Study Variables
Table 4 reveals that depression among hypertension patients in elderly caring SOs was associated with the factor of comorbid chronic diseases, in addition to social support, institutional satisfaction, and anxiety. The depressive symptoms of hypertension patients who had comorbid chronic diseases were more serious than those who did not have (β = 0.105, P = 0.001).
Test of Study Model
SEM was used to test the model depicted in Figure 1. The path coefficient of the link between social support and depression was not statistically significant. As a result, we revised our model by removing this path. After setting socio-demographic characteristics as covariates, the direction of influence among key variables remained unchanged, and corresponding coefficients remained unchanged. Thus, the socio-demographic characteristics were not confounding factors and were excluded from the final model. To improve model fitness, the covariance between measurement errors was set based on modification indices. Figure 2 displays the final modified model that examined the associations between depression and social support, institutional satisfaction, and anxiety. Standardized coefficients representing direct associations between variables are displayed over the arrows. The model demonstrated good fit: χ2 = 631.57 (p < 0.001), χ2/df = 3.53, CFI = 0.93, TLI = 0.92, SRMR = 0.06, RMSEA = 0.07.
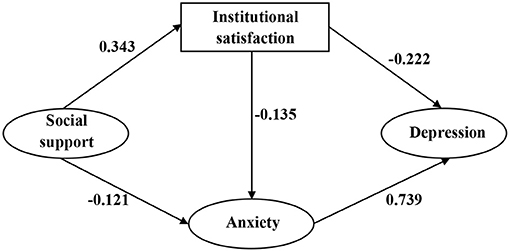
Figure 2. Structural analysis of social support, institutional satisfaction, anxiety and depression. All coefficients are significant (P < 0.05).
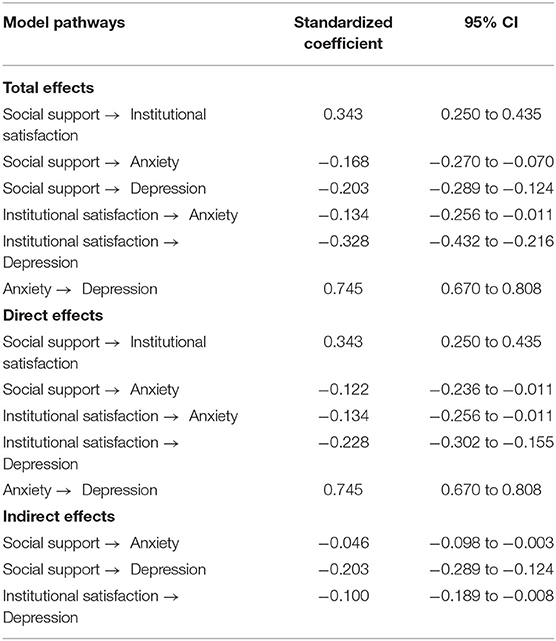
The total, direct, and indirect effects between social support, institutional satisfaction, anxiety, and depression are displayed in Table 5. Institutional satisfaction directly affected the depression (β = −0.228, 95% CI: −0.302 to −0.155) of hypertension patients in elderly caring SOs, thus supporting Hypothesis 2. Anxiety was directly associated with depression (β = 0.745, 95% CI: 0.670–0.808), corroborating Hypothesis 3. However, social support was only indirectly associated with depression (β = −0.203, 95% CI: −0.289 to −0.124), rather than directly associated, leading us to reject Hypothesis 1. Greater social support was linked to an enhanced likelihood of having higher institutional satisfaction (β = 0.343, 95% CI: 0.250–0.435) and a lower level of anxiety (β = −0.122, 95% CI: −0.236 to −0.011), corroborating Hypotheses 4 and 5. Institutional satisfaction exhibited a direct association with the anxiety of hypertension patients (β = −0.134, 95% CI:−0.256 to−0.011), corroborating Hypothesis 6.
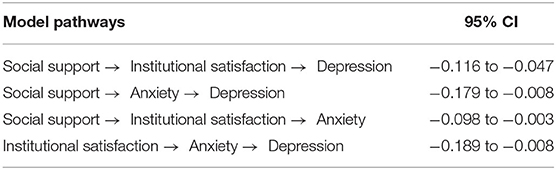
Table 6 displays significance testing results of mediating pathways. A mediating effect was considered statistically significant if 95% confidence interval did not include zero. The results illustrated that institutional satisfaction and anxiety mediated the relationship between social support and depression (95% CI: −0.116 to −0.047 and −0.179 to −0.008, respectively), supporting Hypotheses 7 and 8. Besides, institutional satisfaction mediated the relationship between social support and anxiety (95% CI: −0.098 to −0.003), corroborating Hypothesis 9. Anxiety mediated the relationship between institutional satisfaction and depression (95% CI: −0.189 to −0.008), thus supporting Hypothesis 10.
Discussion
To the best of our knowledge, this research is the first to explore the relationships between social support, institutional satisfaction, anxiety, and depression in hypertension patients in elderly caring SOs in China.
In the current study, lower institutional satisfaction was linked to an increased risk of depression in hypertension patients in elderly caring SOs. Lower institutional satisfaction may result in lower quality of life and trust, a weaker sense of happiness, and easy to produce negative emotions, which is similar to a study indicating a significant negative correlation between depression and life satisfaction in nursing home residents (Kim and Hwang, 2017). Additionally, high-level institutional satisfaction may be conducive to hypertension control and prognosis. A study found that the correlation between patient satisfaction and compliance to treatment is well documented (Calabro et al., 2018).
The present study found that anxiety was positively linked to depressive symptoms in study samples, consistent with previous research showing that anxiety was an independent predictor of depressive symptoms (Gay et al., 2017). Individuals with high anxiety levels often exhibit symptoms such as fear, worry, insomnia, and fatigue, leading to accumulation of negative emotions that cannot be resolved for a long time (Gay et al., 2017), which may contribute to depressive symptoms in this group. Interestingly, our study evidenced the mediating effect of anxiety on the relationship between institutional satisfaction and depression. Hypertension patients in elderly caring SOs with a high level of institutional satisfaction may have more trust in elderly caring SOs, promoting communication with others and improving interpersonal relationships, and ultimately reducing their risk of depression. In other words, anxiety not only has a direct positive relationship with depression but has also been shown to weaken the possible beneficial effects of institutional satisfaction on depression.
According to previous research, subjects with a lower level of social support are more likely to develop cardiovascular disease due to a history of hypertension. They are at increased risk of experiencing higher blood pressure, less nocturnal blood pressure decrease, and a worse prognosis after a cardiovascular event (Blumenthal et al., 1987; Rosengren et al., 2004; Barth et al., 2010). One study reported a threefold increase in the risk of all-cause mortality in hypertension patients with poor social support (Menéndez-Villalva et al., 2015). Consequently, insufficient social support offered to hypertension patients calls for more attention. In this study, participants received relatively little support from family and friends. Therefore, special attention needs to be given to hypertension patients in elderly caring SOs who lack the care of friends and family members and improve their social support to reduce negative emotions.
Multiple literature documented that lack of social support is a strong predictor of depression in hypertension patients (Dennis et al., 2008; Ma, 2018). However, different from other studies, our study indicated that the direct relationship between social support and depression was not significant in the study samples. Through the mediating effects of institutional satisfaction and anxiety, social support had an indirect effect on depression. A lack of social support was associated with a higher likelihood of having a low level of institutional satisfaction, suggesting that social support can increase the trust and sense of belonging in hypertension patients in elderly caring SOs, thereby enhancing institutional satisfaction should be emphasized. The mediating pathways revealed that lack of social support might impact the risk of institutional dissatisfaction and cause anxiety, thus potentially contributing to a higher prevalence of depression. This study contributes to our understanding of how social support affects depression and offers strategies that may benefit the mental health of hypertension patients.
Furthermore, linear regression revealed that comorbid chronic diseases were associated with depression among hypertension patients in elderly caring SOs. Participants with comorbid chronic diseases had a higher degree of depression than those without, which is consistent with previous studies (Findley et al., 2011; Ma, 2018). Higher physical comorbidities were associated with an increased risk of depression in hypertension patients in elderly caring SOs, resulting from persistent limitations in daily functioning associated with coexisting diseases.
Overall, relieving depressive symptoms in hypertension individuals in elderly caring SOs requires social support enhancement, institutional satisfaction, and anxiety reduction. In particular, more attention should be directed toward hypertension patients with comorbid chronic diseases in elderly caring SOs. More institution-based collective activities and social opportunities should be provided for hypertension individuals in elderly caring SOs to address the lack of social support caused by conditions. Moreover, care providers are an important social support resource whose activities in this regard should be encouraged (Chen et al., 2018). To enhance the institutional satisfaction of hypertension patients within elderly caring SOs, we suggest that elderly caring SOs should improve their environment and service quality while also expanding social capital into the elderly care sector to provide targeted elderly care services. The findings of previous study indicated that nursing home residents are more satisfied in smaller nursing homes and nursing homes with frequent opportunities for physical and social activity (Spangler et al., 2019). In addition, as artificial intelligence advances, applying data-driven intelligent platforms has huge potential in health management and health decision-making (Gu et al., 2019), effectively improving organizational performance and internal and external satisfaction. Elderly caring SOs should also pay attention to the anxiety of hypertension patients and take steps to reduce their anxiety levels.
This study has several limitations. First, the cross-sectional design of this study describes the relationships between depression and social support, anxiety, and institutional satisfaction; it does not enable one to infer causality of the three determinants on depression in hypertension individuals in elderly caring SOs. Further studies using a longitudinal or randomized control trial design are proposed. Second, since we conducted this study in Anhui Province, the generalizability of our findings is limited. Future studies that include expanded areas and larger sample size are required.
Despite the above limitations, our findings are reliable because the sample was representative and had high response rates. Furthermore, our study adds important findings regarding the factors that influence depression and mechanisms underlying these factors' relationships in hypertension patients in elderly caring SOs and provide insights into designing focused and effective measures for depression prevention in hypertension patients in elderly caring SOs and control work.
Conclusion
Our findings indicated that social support, institutional satisfaction, anxiety, and comorbid chronic diseases were significantly associated with depression in hypertension patients in elderly caring SOs and elucidated possible mechanisms behind these variables. Institutional satisfaction had a direct negative correlation with depression, whereas anxiety was directly positively associated with depression. Social support was indirectly negatively associated with depression, mediated by anxiety and institutional satisfaction. Institutional satisfaction also had an indirect negative effect on depression via anxiety. In addition, hypertension patients with comorbid chronic diseases in elderly caring SOs exhibited more depressive symptoms.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics Statement
This study was approved and ethical approval was obtained from the Biomedical Ethics Committee, Anhui Medical University (No. 20180181). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KJ and ZB: conceptualization. HY and GC: methodology. YZ and LT: investigation. KJ: writing—original draft preparation. KJ, ZB, and RC: writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the National Nature Science Foundation of China (Nos. 71874002 and 72174001) and Research fund of Anhui Medical University (No. 2021xkj255).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors sincerely thank the provincial and local Civil Affairs Department in Anhui Province, Anhui elderly caring social organizations, and all participants for their collaboration.
References
Alipour, Z., Kazemi, A., Kheirabadi, G., and Eslami, A. A. (2019). Relationship between marital quality, social support and mental health during pregnancy. Commun. Ment. Health J. 55, 1064–1070. doi: 10.1007/s10597-019-00387-8
Andresen, E. M., Malmgren, J. A., Carter, W. B., and Patrick, D. L. (1994). Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med. 10, 77–84.
Atienza-González, F. L., Martínez, N., and Silva, C. (2020). Life satisfaction and self-rated health in adolescents: the relationships between them and the role of gender and age. Span. J. Psychol. 23:e4. doi: 10.1017/sjp.2020.10
Barnett, M. D., Martin, K. J., and Garza, C. J. (2019). Satisfaction with work-family balance mediates the relationship between workplace social support and depression among hospice nurses. J. Nurs. Scholarsh. 51, 187–194. doi: 10.1111/jnu.12451
Barth, J., Schneider, S., and von Känel, R. (2010). Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom. Med. 72, 229–238. doi: 10.1097/PSY.0b013e3181d01611
Benetos, A., Labat, C., Rossignol, P., Fay, R., Rolland, Y., Valbusa, F., et al. (2015). Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE study. JAMA Intern. Med. 175, 989–995. doi: 10.1001/jamainternmed.2014.8012
Berkman, L. F., Kawachi, I., and Glymour, M. (2000). Social Epidemiology. Oxford: Oxford University Press, 200–203.
Blumenthal, J. A., Burg, M. M., Barefoot, J., Williams, R. B., Haney, T., and Zimet, G. (1987). Social support, type A behavior, and coronary artery disease. Psychosom. Med. 49, 331–340. doi: 10.1097/00006842-198707000-00002
Brick, Y., and Clarfield, A. M. (2007). “JDC-ESHEL,” a unique non-governmental organization dedicated to the elderly in Israel. Arch. Gerontol. Geriatr. 44, 225–234. doi: 10.1016/j.archger.2006.05.002
Calabro, K. A., Raval, M. V., and Rothstein, D. H. (2018). Importance of patient and family satisfaction in perioperative care. Semin. Pediatr. Surg. 27, 114–120. doi: 10.1053/j.sempedsurg.2018.02.009
Chen, Y. C., Chang, L. C., Liu, C. Y., Ho, Y. F., Weng, S. C., and Tsai, T. I. (2018). The roles of social support and health literacy in self-management among patients with chronic kidney disease. J. Nurs. Scholarsh. 50, 265–275. doi: 10.1111/jnu.12377
Cheung, B., Au, T., Chan, S., Lam, C., Lau, S., Lee, R., et al. (2005). The relationship between hypertension and anxiety or depression in Hong Kong Chinese. Exp. Clin. Cardiol. 10, 21–24. Available online at: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2716224/pdf/ecc10021.pdf
Chobanian, A. V., Bakris, G. L., Black, H. R., Cushman, W. C., Green, L. A., Izzo, J. L. Jr., et al. (2003). Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42, 1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2
Chu, L. W., and Chi, I. (2008). Nursing homes in China. J. Am. Med. Dir. Assoc. 9, 237–243. doi: 10.1016/j.jamda.2008.01.008
Cohen, S., Underwood, L. G., and Gottlieb, L. (2000). Social Support Measurement and Intervention. Oxford: Oxford University Press
Compare, A., Zarbo, C., Manzoni, G. M., Castelnuovo, G., Baldassari, E., Bonardi, A., et al. (2013). Social support, depression, and heart disease: a ten year literature review. Front. Psychol. 4:384. doi: 10.3389/fpsyg.2013.00384
Davidson, K., Jonas, B. S., Dixon, K. E., and Markovitz, J. H. (2000). Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary artery risk development in young adults. Arch. Intern. Med. 160, 1495–1500. doi: 10.1001/archinte.160.10.1495
Dennis, J. P., Markey, M. A., Johnston, K. A., Vander Wal, J. S., and Artinian, N. T. (2008). The role of stress and social support in predicting depression among a hypertensive African American sample. Heart Lung 37, 105–112. doi: 10.1016/j.hrtlng.2007.03.003
Fang, Y., Niu, Y., and Dong, Y. (2021). Exploring the relationship between narcissism and depression: the mediating roles of perceived social support and life satisfaction. Personal. Indiv. Differ. 173:110604. doi: 10.1016/j.paid.2020.110604
Findley, P., Shen, C., and Sambamoorthi, U. (2011). Multimorbidity and persistent depression among veterans with diabetes, heart disease, and hypertension. Health Soc. Work 36, 109–119. doi: 10.1093/hsw/36.2.109
Gay, M. C., Bungener, C., Thomas, S., Vrignaud, P., Thomas, P. W., Baker, R., et al. (2017). Anxiety, emotional processing and depression in people with multiple sclerosis. BMC Neurol. 17:43. doi: 10.1186/s12883-017-0803-8
Gay, M. C., Vrignaud, P., Garitte, C., and Meunier, C. (2010). Predictors of depression in multiple sclerosis patients. Acta Neurol. Scand. 121, 161–170. doi: 10.1111/j.1600-0404.2009.01232.x
Gómez-Restrepo, C., Rodríguez, M. N., Díaz, N., Cano, C., and Tamayo, N. (2013). Depression and life satisfaction in people over 60 years old in the City of Bogotá: Survey of health, wellbeing and aging (SABE). Rev. Colomb. Psiquiatr. 43(Suppl 1), 65–70. doi: 10.1016/j.rcp.2013.11.008
Gottlieb, B. H., and Bergen, A. E. (2010). Social support concepts and measures. J. Psychosom. Res. 69, 511–520. doi: 10.1016/j.jpsychores.2009.10.001
Gu, D., Deng, S., Zheng, Q., Liang, C., and Wu, J. (2019). Impacts of case-based health knowledge system in hospital management: the mediating role of group effectiveness. Inform. Manag. 56:103162. doi: 10.1016/j.im.2019.04.005
Harris-Kojetin, L., Sengupta, M., Park-Lee, E., Valverde, R., Caffrey, C., Rome, V., et al. (2016). Long-term care providers and services users in the United States: data from the National Study of Long-Term Care Providers, 2013–2014. Vital Health Stat. 3, 1–105. doi: 10.13140/RG.2.1.1207.6407
Hinz, A., Klein, A. M., Brähler, E., Glaesmer, H., Luck, T., Riedel-Heller, S. G., et al. (2017). Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J. Affect. Disord. 210, 338–344. doi: 10.1016/j.jad.2016.12.012
Hughes, J. W., Tomlinson, A., Blumenthal, J. A., Davidson, J., Sketch, M. H., and Watkins, L. L. (2004). Social support and religiosity as coping strategies for anxiety in hospitalized cardiac patients. Ann. Behav. Med. 28, 179–185. doi: 10.1207/s15324796abm2803_6
Hunt, C., Issakidis, C., and Andrews, G. (2002). DSM-IV generalized anxiety disorder in the Australian National Survey of Mental Health and Well-Being. Psychol. Med. 32, 649–659. doi: 10.1017/s0033291702005512
Kavalniene, R., Deksnyte, A., Kasiulevičius, V., Šapoka, V., Aranauskas, R., and Aranauskas, L. (2018). Patient satisfaction with primary healthcare services: are there any links with patients' symptoms of anxiety and depression? BMC Fam. Pract. 19:90. doi: 10.1186/s12875-018-0780-z
Kim, K. H., and Hwang, E. H. (2017). Comparison of quality of sleep, depression, and life satisfaction between older adults in nursing homes and long-term care hospitals in Korea. Geriatr. Gerontol. Int. 17, 142–149. doi: 10.1111/ggi.12651
Könner, F., Kuhnert, R., Budnick, A., Kolloch, R., Scholze, J., Dräger, D., et al. (2014). Arterial hypertension, antihypertensive therapy, and visit-to-visit blood pressure variability of elderly nursing home residents. Dtsch Med. Wochenschr. 139, 2441–2447. doi: 10.1055/s-0034-1387422
Köttl, H., Fallahpour, M., Hedman, A., Nygård, L., and Kottorp, A. (2021). Depression, everyday technology use and life satisfaction in older adults with cognitive impairments: a cross-sectional exploratory study. Scand. J. Caring Sci. 35, 233–243. doi: 10.1111/scs.12838
Krousel-Wood, M. A., and Frohlich, E. D. (2010). Hypertension and depression: coexisting barriers to medication adherence. J. Clin. Hypertens. 12, 481–486. doi: 10.1111/j.1751-7176.2010.00302.x
Labarbera, P. A., and Mazursky, D. (1983). A longitudinal assessment of consumer satisfaction/dissatisfaction: the dynamic aspect of the cognitive process. J. Market. Res. 20, 393–404.
Li, Y., Yang, L., Wang, L., Zhang, M., Huang, Z., Deng, Q., et al. (2017). Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int. J. Cardiol. 227, 516–523. doi: 10.1016/j.ijcard.2016.10.110
Long, J., Duan, G., Tian, W., Wang, L., Su, P., Zhang, W., et al. (2015). Hypertension and risk of depression in the elderly: a meta-analysis of prospective cohort studies. J. Hum. Hypertens. 29, 478–482. doi: 10.1038/jhh.2014.112
Ma, C. (2018). The prevalence of depressive symptoms and associated factors in countryside-dwelling older Chinese patients with hypertension. J. Clin. Nurs. 27, 2933–2941. doi: 10.1111/jocn.14349
Matud, M. P., García, M. C., and Fortes, D. (2019). Relevance of gender and social support in self-rated health and life satisfaction in elderly Spanish people. Int. J. Environ. Res. Public Health 16:2725. doi: 10.3390/ijerph16152725
Menéndez-Villalva, C., Gamarra-Mondelo, M. T., Alonso-Fachado, A., Naveira-Castelo, A., and Montes-Martínez, A. (2015). Social network, presence of cardiovascular events and mortality in hypertensive patients. J. Hum. Hypertens. 29, 417–423. doi: 10.1038/jhh.2014.116
Meurs, M., Groenewold, N. A., Roest, A. M., van der Wee, N. J., Veltman, D. J., van Tol, M. J., et al. (2015). The associations of depression and hypertension with brain volumes: independent or interactive? Neuroimage Clin. 8, 79–86. doi: 10.1016/j.nicl.2015.03.020
Mittal, B. V., and Singh, A. K. (2010). Hypertension in the developing world: challenges and opportunities. Am. J. Kidney Dis. 55, 590–598. doi: 10.1053/j.ajkd.2009.06.044
Mittal, V., Ross, W. T., and Baldasare, P. M. (1998). The asymmetric impact of negative and positive attribute-level performance on overall satisfaction and repurchase intentions. J. Market. 62, 33–47. doi: 10.1177/002224299806200104
Moon, M. J. (2010). Factors influencing depression in elderly people living at home. J. Korean Acad. Nurs. 40, 542–550. doi: 10.4040/jkan.2010.40.4.542
Naderi, S. H., Bestwick, J. P., and Wald, D. S. (2012). Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am. J. Med. 125, 882–887.e881. doi: 10.1016/j.amjmed.2011.12.013
Nam, K. S., and Bok, L. S. (2013). Spiritual well-being, social support, life satisfaction and depression in the community dwelling elderly. J. East-West Nurs. Res. 19, 186–194. doi: 10.14370/jewnr.2013.19.2.186
Oganov, R. G., Pogosova, G. V., Koltunov, I. E., Romasenko, L. V., Deev, A. D., and Iufereva Iu, M. (2011). Depressive symptoms worsen cardiovascular prognosis and shorten length of life in patients with arterial hypertension and ischemic heart disease. Kardiologiia 51, 59–66. Available online at: https://europepmc.org/article/med/21627600
Ojo, O. S., Malomo, S. O., and Sogunle, P. T. (2016). Blood pressure (BP) control and perceived family support in patients with essential hypertension seen at a primary care clinic in Western Nigeria. J. Family Med. Prim. Care 5, 569–575. doi: 10.4103/2249-4863.197284
Perkovic, V., Huxley, R., Wu, Y., Prabhakaran, D., and MacMahon, S. (2007). The burden of blood pressure-related disease: a neglected priority for global health. Hypertension 50, 991–997. doi: 10.1161/HYPERTENSIONAHA.107.095497
Pinquart, M., and Duberstein, P. R. (2010). Associations of social networks with cancer mortality: a meta-analysis. Crit. Rev. Oncol. Hematol. 75, 122–137. doi: 10.1016/j.critrevonc.2009.06.003
Prince, M. J., Wu, F., Guo, Y., Gutierrez Robledo, L. M., O'Donnell, M., Sullivan, R., et al. (2015). The burden of disease in older people and implications for health policy and practice. Lancet 385, 549–562. doi: 10.1016/s0140-6736(14)61347-7
Roberts, R. E., and Vernon, S. W. (1983). The center for epidemiologic studies depression scale: its use in a community sample. Am. J. Psychiatry 140, 41–46. doi: 10.1176/ajp.140.1.41
Rogowska, A. M., Kuśnierz, C., and Bokszczanin, A. (2020). Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in Polish sample of University students. Psychol. Res. Behav. Manag. 13, 797–811. doi: 10.2147/prbm.S266511
Rosengren, A., Hawken, S., Ounpuu, S., Sliwa, K., Zubaid, M., Almahmeed, W. A., et al. (2004). Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 364, 953–962. doi: 10.1016/s0140-6736(04)17019-0
Scuteri, A., Spazzafumo, L., Cipriani, L., Gianni, W., Corsonello, A., Cravello, L., et al. (2011). Depression, hypertension, and comorbidity: disentangling their specific effect on disability and cognitive impairment in older subjects. Arch. Gerontol. Geriatr. 52, 253–257. doi: 10.1016/j.archger.2010.04.002
Seabrook, E. M., Kern, M. L., and Rickard, N. S. (2016). Social networking sites, depression, and anxiety: a systematic review. JMIR Ment. Health 3:e50. doi: 10.2196/mental.5842
Shao, H., Mohammed, M. U., Thomas, N., Babazadeh, S., Yang, S., Shi, Q., et al. (2017). Evaluating excessive burden of depression on health status and health care utilization among patients with hypertension in a nationally representative sample from the medial expenditure panel survey (MEPS 2012). J. Nerv. Ment. Dis. 205, 397–404. doi: 10.1097/nmd.0000000000000618
Shi, L., Lu, Z. A., Que, J. Y., Huang, X. L., Liu, L., Ran, M. S., et al. (2020). Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
Simonson, W., Han, L. F., and Davidson, H. E. (2011). Hypertension treatment and outcomes in US nursing homes: results from the US National Nursing Home Survey. J. Am. Med. Dir. Assoc. 12, 44–49. doi: 10.1016/j.jamda.2010.02.009
Spangler, D., Blomqvist, P., Lindberg, Y., and Winblad, U. (2019). Small is beautiful? Explaining resident satisfaction in Swedish nursing home care. BMC Health Serv. Res. 19:886. doi: 10.1186/s12913-019-4694-9
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Stephenson, J. (1999). Noncompliance may cause half of antihypertensive drug “failures”. JAMA 282, 313–314. doi: 10.1001/jama.282.4.313
Strogatz, D. S., and James, S. A. (1986). Social support and hypertension among blacks and whites in a rural, southern community. Am. J. Epidemiol. 124, 949–956. doi: 10.1093/oxfordjournals.aje.a114484
Taher, M., Abredari, H., Karimy, M., Abedi, A., and Shamsizadeh, M. (2014). The relation between social support and adherence to the treatment of hypertension. J. Educ. Commun. Health 1, 59–67. doi: 10.20286/jech-010348
Tsartsalis, D., Dragioti, E., Kontoangelos, K., Pitsavos, C., Sakkas, P., Papadimitriou, G. N., et al. (2016). The impact of depression and cardiophobia on quality of life in patients with essential hypertension. Psychiatriki 27, 192–203. doi: 10.22365/jpsych.2016.273.192
Wei, T. M., and Wang, L. (2006). Anxiety symptoms in patients with hypertension: a community-based study. Int. J. Psychiatry Med. 36, 315–322. doi: 10.2190/5lx9-d3bh-fua3-pqf0
Wu, S. F., Young, L. S., Yeh, F. C., Jian, Y. M., Cheng, K. C., and Lee, M. C. (2013). Correlations among social support, depression, and anxiety in patients with type-2 diabetes. J. Nurs. Res. 21, 129–138. doi: 10.1097/jnr.0b013e3182921fe1
Wu, Y., Huxley, R., Li, L., Anna, V., Xie, G., Yao, C., et al. (2008). Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 118, 2679–2686. doi: 10.1161/circulationaha.108.788166
Yan, R., Xia, J., Yang, R., Lv, B., Wu, P., Chen, W., et al. (2019). Association between anxiety, depression, and comorbid chronic diseases among cancer survivors. Psychooncology 28, 1269–1277. doi: 10.1002/pon.5078
Yang, X., You, L., Jin, D., Zou, X., Yang, H., and Liu, T. (2020). A community-based cross-sectional study of sleep quality among internal migrant workers in the service industry. Comprehen. Psychiatry 97:152154. doi: 10.1016/j.comppsych.2019.152154
Yang, Y. (2018). The role of NGOs in enabling elderly activity and care in the Community: a case study of silver wings in South Korea. J. Cross-Cult. Gerontol. 33, 217–228. doi: 10.1007/s10823-017-9323-7
Yasin, A. S., and Dzulkifli, M. A. (2010). The relationship between social support and psychological problems among students. Int. J. Bus. Soc. Sci. 1, 110–117. Available online at: http://ijbssnet.com/journals/Vol._1_No._3_December_2010/11.pdf
Yu, W., Singh, S. S., Calhoun, S., Zhang, H., Zhao, X., and Yang, F. (2018). Generalized anxiety disorder in urban China: Prevalence, awareness, and disease burden. J. Affect. Disord. 234, 89–96. doi: 10.1016/j.jad.2018.02.012
Keywords: social support, satisfaction, anxiety, depression, hypertension, elderly caring, social organizations, China
Citation: Ji K, Bai Z, Tang L, Yan H, Zhu Y, Chen G and Chen R (2021) Institutional Satisfaction and Anxiety Mediate the Relationship Between Social Support and Depression in Hypertension Patients in Elderly Caring Social Organizations: A Cross-Sectional Study. Front. Psychol. 12:772092. doi: 10.3389/fpsyg.2021.772092
Received: 07 September 2021; Accepted: 27 September 2021;
Published: 25 October 2021.
Edited by:
Feng Jiang, Shanghai Jiao Tong University, ChinaReviewed by:
Enhong Dong, Shanghai University of Medicine and Health Sciences, ChinaXin Li, East China University of Science and Technology, China
Copyright © 2021 Ji, Bai, Tang, Yan, Zhu, Chen and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ren Chen, Y2hlbnJlbjIwMDZAaG90bWFpbC5jb20=
†These authors have contributed equally to this work
 Kai Ji1†
Kai Ji1† Huosheng Yan
Huosheng Yan Ren Chen
Ren Chen