- 1Kinesiology Department, State University of New York at Cortland, Cortland, NY, United States
- 2Kinesiology Department, Centenary College of Louisiana, Shreveport, LA, United States
- 3Kinesiology Department, University of Texas at Arlington, Arlington, TX, United States
Fundamental motor skills (FMS) and cognitive function are important indicators of development in early childhood. Using a cross-sectional design, the purpose of this study was to investigate obesity (healthy weight vs. overweight/obese) and socio-demographic (i.e., gender, SES) disparities in FMS (locomotor and ball skills) and cognitive function (reaction time [RT] and movement time [MT]), in preschoolers. There were 74 preschoolers (girl = 38; Mage = 4.02 ± 0.73) recruited from two childcare centers and were categorized into healthy weight (n = 58, BMI percentile < 85%) and overweight/obese (n = 16, BMI percentile ≥ 85%) categories. Children’s FMS were assessed using the TGMD-3; cognitive function was assessed by the iPad-based CANTAB™ software using the Reaction Time Task (RTI), including reaction time (RT; Simple RT [SRT], choice RT [CRT]) and movement time (MT; simple MT [SMT], choice MT [CMT]). Children presented less FMS proficiency compared to recent data. Both weight groups performed comparably in FMS (ps > 0.05; ball skill Cohen’s d = 0.40; locomotor Cohen’s d = 0.02). Children in the overweight/obese group performed significantly worse on all cognitive tests compared to healthy weight peers (ps < 0.05; Cohen’s d range from −0.93 to −1.43). No significant gender or SES disparities were observed. Maintaining healthy weight status is critical for cognitive development among preschoolers, which may influence their developmental trajectory and school readiness.
1. Introduction
According to the recent report from the Center for Disease Control and Prevention, over 45 million children aged 2–5 years old are categorized as overweight/obese in the U.S. which has increased by almost 4 million children over the last 6 years (CDC Division of Nutrition, 2021). Children categorized as overweight/obese pose themselves at a higher risk for developmental delays and poorer fundamental school readiness skills compared to their healthy weight counterparts (Kelsey et al., 2014; Pearce et al., 2016). A recent meta-analysis included 52 studies and noted that children and adolescents (5–18 years old) that were obese were 1.4–26.1 times more likely to have metabolic comorbidities and/or psychological issues than healthy weight peers (Sharma et al., 2019). This evidence widens the need for more research in the early childhood stage (3–5 years old) in order to establish a clearer consensus on the effects of weight status on other developmental and health-related outcomes. Research has consistently reported how obesity contributes to health and educational disparities and its association with poorer academic performance in childhood, especially in children with a disadvantaged and low socioeconomic status (Winter and Sass, 2011). The evidence suggests that obesity may have detrimental effects on development trajectory and related indicators such as fundamental motor skills (FMS) and cognitive functioning, especially during early childhood (Khalaj and Amri, 2013; Chang and Gu, 2018; Eichen et al., 2018).
Early childhood is a crucial time for assessing and augmenting specific developmental skills and potential social determinants, especially given how health disparities have been further enlarged during the COVID-19 pandemic (Krombholz, 2013; Martin et al., 2016; López-Bueno et al., 2020). FMS are goal-derived basic gross motor skills that form specific skilled movements and functioning for daily activities (Kipling Webster and Ulrich, 2017). Proficiency in FMS can be used as an indicator to gauge children’s cognitive, social, and emotional development (McClelland and Cameron, 2019; Viegas et al., 2021). FMS including locomotor skills (e.g., running, galloping, jumping, hopping, and sliding) and ball skills (e.g., catching, throwing, kicking, and dribbling) are introduced and learned in early childhood years (Lloyd et al., 2014; Kipling Webster and Ulrich, 2017). Mastery of these movements through learning, practice, and reinforcement is essential for a child’s independence and positive developmental trajectory in physical, motor, and cognitive health as they mature (Logan et al., 2012). Children that demonstrate motor delays are also likely to incur cognitive and academic struggles (Cameron et al., 2012). A previous literature review synthesized research in preschoolers, children, adolescents, and adults infered underperformance in academics are ingrained from attention deficit hyperactivity disorder (ADHD) symptoms and underlying cognitive deficits (Daley and Birchwood, 2010). Daley and Birchwood also suggested that enhancing children’s cognitive function and providing tools for motor enhancement (fidget spinner, stress ball) could be helpful strategies to indirectly improve academic performance. Ultimately, it’s important to assess children’s motor competency and cognitive function in early childhood so potential developmental delays are monitored and appropriate actions are taken early on.
Obesity/overweight has also been investigated as a potential indicator for developmental delays in children. From a socio-ecological perspective, Hulteen et al. (2018) proposed a conceptual model supporting the notion that skill development may be impacted (hindered or enhanced) by weight status along with other physical and psychological attributes from infant to adult. From this model, it would be of importance to investigate influences of weight status on FMS and cognitive function in a young childhood sample. Evidence of cognitive differences based on weight status has been noted in the literature, but mostly in elementary-aged children (6–11 years old), so weight status and cognition have not been adequately investigated in a young preschool population (Hjorth et al., 2016; Groppe and Elsner, 2017; Raine et al., 2018). For instance, Raine et al. (2018) showed that children with obesity significantly underperformed compared to their healthy weight peers in various cognitive functions such as ability, reading, and math skills. Notably, two earlier studies have found significantly slower computer-based reaction times among elementary-aged children with greater body mass index (Gentier et al., 2013; Frazier-Wood et al., 2014). Recent evidence also indicated that over one-third of studied preschoolers were classified as overweight/obese and were more likely to demonstrate motor and cognitive delays (Cataldo et al., 2016; Hamilton et al., 2017). Similarly, another study by Musalek et al. (2017) indicated children (3–6 years old) that were overweight/obese were three times more likely to have severe motor deficits than their non-obese peers. However, observed obesity disparities in motor and cognitive development are still in its infancy and most previous studies implemented paper-and-pencil surveys to subjectively assess cognitive function (Hjorth et al., 2016; Quan et al., 2018), which has been claimed to be lacking process-purity and often paired with outdated principles (Kessels, 2019). More evidence is needed to further investigate the dynamic effects of overweight/obesity may yield on both FMS and cognitive functioning in early childhood to minimize the potential disparities identified in the literature.
Socio-demographic (gender, SES) disparities among FMS have been well documented in the literature; preschool-aged boys have been shown to surpass girls, specifically in ball skills (Goodway et al., 2010; Vameghi et al., 2013; Kokštejn et al., 2017). In one longitudinal study, it was suggested that the magnitude of the gender disparities in FMS (specifically ball skills) could be accelerated from childhood into adolescence (Barnett et al., 2010). Preschoolers living in low SES conditions may also present delayed motor proficiency compared to normative values and/or high SES counterparts (Goodway et al., 2010; Liu et al., 2015). Consequently, these motor delays may transpire into physical inactivity, cognitive dysfunction, and lack of school readiness in later stages of childhood and adolescence (Piek et al., 2008; Stodden et al., 2014; Hamilton et al., 2017). For example, Piek and colleagues found that SES was a significant predictor of motor performance and cognitive function (i.e., intellect) among their sample of 6–11 year old children (Piek et al., 2008). Gender disparities also exist among cognitive function variables, although methodologies have not been consistent which has created inconclusive findings in the early childhood populations. It has been shown in previous studies that preschool and elementary-aged girls produced better cognitive and executive functions than boys (Berlin and Bohlin, 2002; Vuontela, 2003; Mileva-Seitz et al., 2015). Alternatively, in one study, researchers used a manual assessment to measure reaction time (ruler drop test) in children (Mage = 5 years old) and found boys had a quicker reaction time than girls (Latorre-Roman et al., 2018). Further investigation of these gender differences in an objective manner among a preschool sample is essential to further develop gender-inclusive intervention strategies for early development and school readiness.
Given the strong prevalence of childhood obesity and its negative impact on children’s overall health and early success, it is critical to use a comprehensive approach to assess developmental status (i.e., motor and cognitive skills) within early childhood and any potential socio-demographic disparities. Obtaining objectively assessed cognitive measures can be challenging in a young population due to the lack of appropriate measures for specific assessments (Blair et al., 2005). It’s also important to note that cognitive function is an umbrella term that houses many different variables that can be used to represent cognitive function. Reaction time is a longstanding method used to examine cognitive function, providing the interpretation of motor and mental response speeds, as well as measures of movement time, reaction time, response accuracy, and impulsivity (Moradi and Esmaeilzadeh, 2017). This can be measured by evaluating individual’s responses with one (simple RT; SRT) or multiple (choice RT; CRT) stimuli (Moradi and Esmaeilzadeh, 2017). The sensitivity of neuropsychological assessments via computerized tests have been explored (Sahakian and Owen, 1992; Fisher et al., 2011; Syväoja et al., 2015). The Cambridge Neuropsychological Test Battery (CANTAB™) has been deemed age-appropriate for young populations (Fisher et al., 2011). Thus, by measuring FMS (Test of Gross Motor Development—3rd edition; TGMD-3) and cognitive function (CANTAB™), the present study aimed to investigate obesity (healthy weight vs. overweight/obese) and socio-demographic (gender, SES) disparities in FMS (locomotor and ball skills) and cognitive function (reaction time [RT] and movement time [MT]), in a sample of preschoolers.
2. Materials and methods
2.1. Participants
Using a cross-sectional research design, a total of 74 preschoolers (boys = 36; girls = 38; Mage = 4.02 years ranging from 3 to 5 years old) were recruited from two childcare centers located in North Texas. There were 49 children (boys = 26; girls = 23; Mage = 4.32 years) recruited from Center A, in which the majority of children were identified as African American (42.9%) while others identified as White (33.3%), Hispanic (14.3%), and Asian (9.5%). Children in Center A were enrolled in the Head Start Program and are identified as low-SES. In Center B, there were 25 children (Mage = 3.37 years), in which the majority were identified as White (72.7%), while others identified as African American (4.5%), Hispanic (18.2%), and Native American (4.5%). Center B is a private childcare center and children in this center identify with families in middle or upper class. Geographically, both centers shared the same zip code and were in a suburban area. The study protocol was approved by the University’s Institutional Review Board and the directors of both childcare centers. Before the data collection, parent consent forms were obtained.
2.2. Measurements
2.2.1. Body mass index
Body mass index (BMI) was calculated using children’s height (inches) and weight (lbs) and then categorized into a BMI percentile established from the Centers of Disease Control and Prevention (CDC, 2020). According to the CDC chart, children were then categorized into healthy weight (n = 58, BMI percentile 5%–85%) and overweight/obese (n = 16, BMI percentile ≥ 85%) groups, respectively.
2.2.2. Fundamental motor skills
Children’s fundamental motor skills (FMS) were assessed using the Test of Gross Motor Development—3rd edition (TGMD-3; Kipling Webster and Ulrich, 2017). The TGMD-3 assesses 13 FMS: six locomotor skills and seven ball skills in children 3–10 years of age. Locomotor skills include running, skipping, galloping, hopping, horizontal jumping, and sliding. Ball skills included two-hand striking, one hand striking, overhand throwing, underhand throwing, kicking, dribbling, and catching. The researcher verbally explained how to perform each skill and demonstrated the skill to each child. Children then performed 2 trials of each skill and were assessed based on each skills’ component criteria (0 = component was unsuccessful; 1 = component was successful). The total score for the locomotor and ball skills subtests are 48 and 54, respectively. Guided by the TGMD-3 gender and age-specified scoring system, children’s raw score for locomotor and ball skills were converted to a standard score (Mean = 10, SD = 3). Psychometric properties have been established in children from the United States (Webster et al., 2015).
2.2.3. Cognitive function
The cognitive domain of attention can measure continuous performance and visual sustained attention. Reaction Time (RTI) from the Cambridge Assessment of Neuropsychological Test Automated Battery (CANTAB™) provides assessments of the psychomotor speed by looking at an individual’s ability to detect and respond to rapid changes in the environment, such as the presence of a stimulus. With this the reaction time and movement time were measured in this study. It is recommended the CANTAB cognitive assessments shall be applied to participants ≥4 years of age, so a subgroup of children aged over 4 were assessed. Eligible children were instructed to hold down the response button with their dominant forefinger on a 10 × 10 inch iPad until the target stimulus was presented (flashed yellow). Once the stimulus was presented, participants would lift their finger, touch the stimulus, then return their forefinger to the response button as quickly and accurately as possible. Reaction time (RT; time taken to release the response button after the presentation of the target stimulus) and movement time (MT; time taken from release of the response button and selection of the target stimulus after flashing yellow on the screen) were calculated for this study. Specifically, single reaction time (SRT) and single movement time (SMT) were calculated in a simple reaction time situation while the child was required to respond to one possible stimulus and then returning to the response button. Choice reaction time (CRT) and choice movement time (CMT) were captured in a choice reaction time situation where the child was required to respond to one of the five possible stimuli and then returning to the response button. The accuracy scores (time in milliseconds) were calculated based on the total correct and assessed trials per child. The average RT and MT (time in milliseconds) in both single and choice reaction time situations were generated through the CANTAB™ software and used in the analyses. Internal consistency and stability have been established in a childhood population using the RTI task (Syväoja et al., 2015).
2.3. Data collection and procedures
The researchers performed the data collection during recess and free times in each childcare center. During children’s recess time, research staff went to each childcare center to measure children’s height (inches) and weight (lbs). For assessing FMS, a trained research assistant provided a verbal and kinesthetic demonstration to each child, and then the trained raters (one for locomotor and one for ball skills) graded each child’s performance of each skill after one practice trial. The assessment was conducted outside on the playground or inside the gym (depending on weather). On a separate day (2–4 days apart), the research team assessed children’s cognitive function (i.e., reaction and movement time) via CANTAB™. One member of the research team administered the CANTAB™ test via a 10 × 10 inch iPad individually (~15 min per child) as recommended by the manufacturer.1 One trained research member and one child relocated to a private, quiet area where there would be little to no distractions while the CANTAB™ test was administered. A subgroup of children who were 4–5 years old (n = 21; 8 boys and 13 girls) performed the CANTAB™ test.
2.3.1. Statistical analyses
Descriptive analyses (minimum, maximum, mean, standard deviation) of BMI percentile, FMS, and cognitive function were conducted. The power analysis (G*Power 3.1.9.4) was conducted for group comparisons in fundamental motor skills. The results indicated the sample size for a group size ratio as low as 0.28 (i.e., overweight/obese group vs. healthy weight group) met the minimum requirements to achieve 80% power for detecting a large effect (effect size d = 0.80) at an alpha level of 0.05 in two-tailed independent t-test. Data was only retained for analyses if children completed all components for the RTI and TGMD-3. An independent t-test was used to test the gender, SES, and obesity disparities in FMS and cognitive function variables. Cohen’s d was reported for effect size and an alpha level of 0.05 using a two-tail test was incorporated in all analyses. All data analyses were completed using SPSS version 26.
3. Results
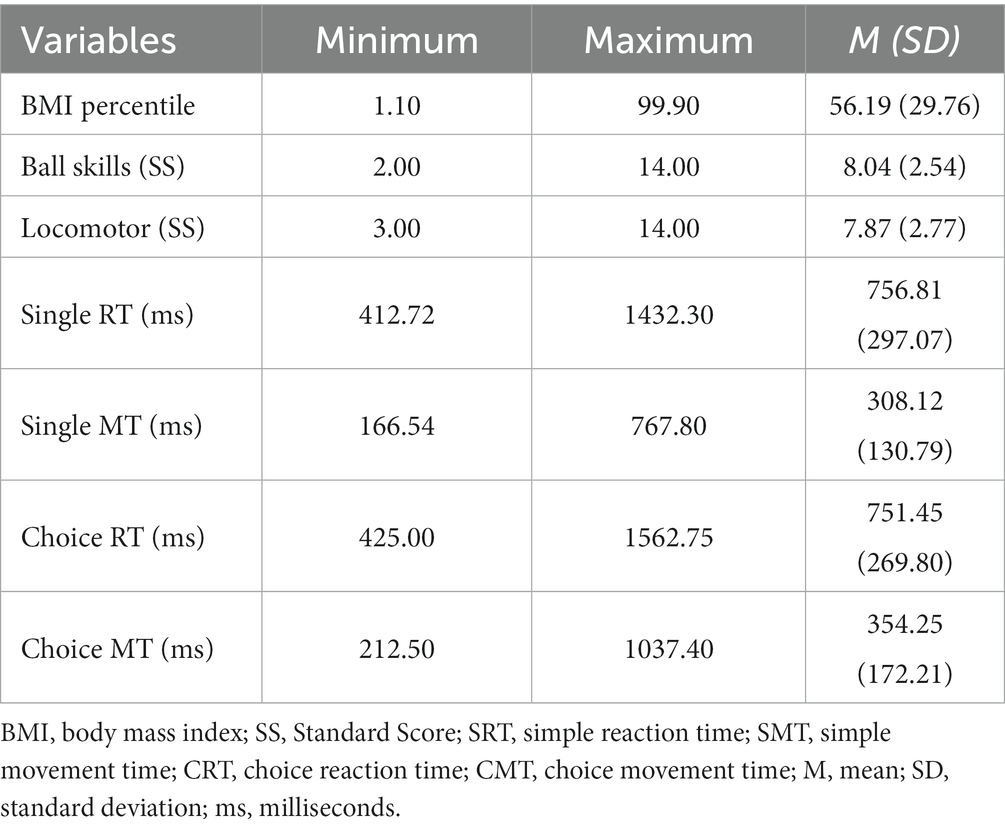
Descriptive characteristics for BMI percentile, FMS and cognitive function among studied children are shown in Table 1. In total, there were 38 girls and 36 boys between both centers with an average age of 4.02 years (±0.73). There were 58 children classified as healthy weight and 16 classified as overweight/obese. Among the 74 children, 21 were classified as high SES and the remaining were classified as low SES based on their respected preschool. The studied children had a BMI-for-age percentile average of 56.19 (SD = 29.76; ranging from 1.11 to 99.9 percentile). Overall, children showed lower locomotor standard scores (M = 7.87 ± 3.77) and ball skill standard scores (M = 8.04 ± 2.54) compared to a recent paper examining FMS in 339 preschool aged children (locomotor: M = 10.0 ± 0.2; ball skills: M = 8.5 ± 0.1) (Kit et al., 2017). Regarding cognitive function (n = 21), all preschoolers in this study demonstrated fairly similar responses between single and choice reaction and movement times: SRT (756.81 ± 297.07), SMT (308.12 ± 130.79), CRT (751.45 ± 269.80), and CMT (354.25 ± 172.21). To our knowledge, there were no previous studies that have used this objective measurement among 3- to 5-year-old children, thus, comparisons with other datasets was not applicable.
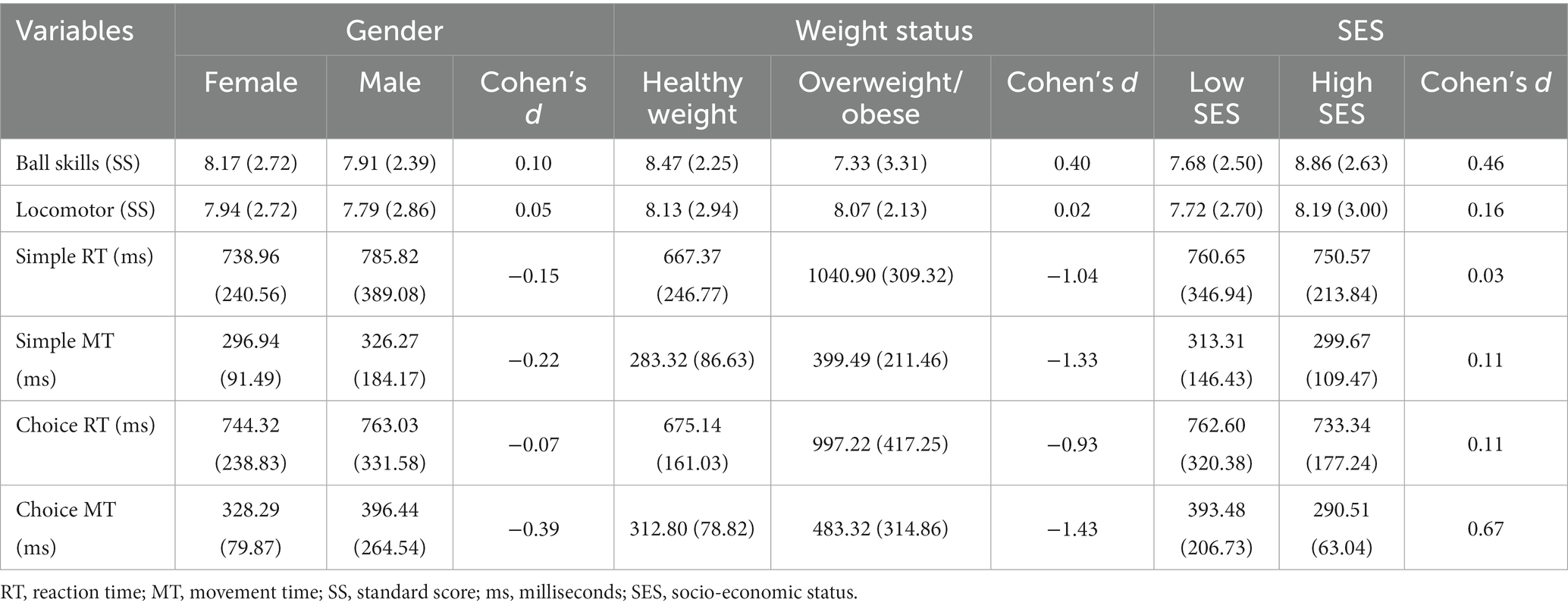
Overall, there were no significant gender differences within BMI percentile (p > 0.05), but girls were in a slightly higher percentile compared to boys (M = 60.56 vs. M = 53.12; Cohen’s d = 0.31). Boys and girls also had similar FMS scores in both ball and locomotor categories. The group differences between children in the healthy weight and overweight/obese groups were insignificant in terms of FMS (ps > 0.05) even though the healthy weight group marginally outperformed the overweight/obese group in ball skills (8.47 vs. 7.33, respectively). As for SES, there were no significant differences in FMS, however differences in ball skills approached significance, favoring children classified as higher SES, with a moderate effect size (high SES M = 8.86 vs. low SES M = 7.68; Cohen’s d = 0.46). These results are presented in Table 2 and Figure 1.
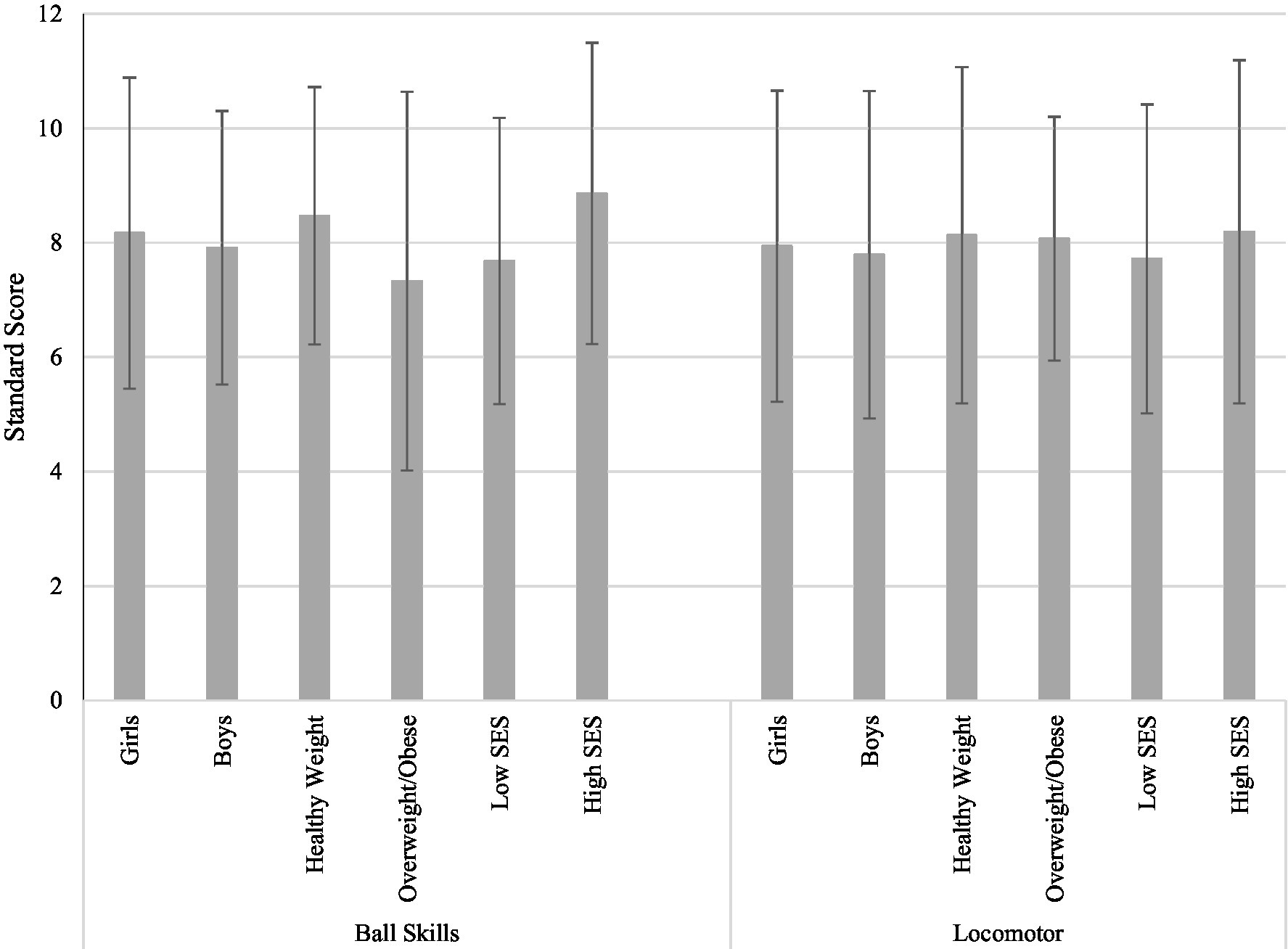
Figure 1. Disparities in fundamental motor skills (n = 74). Averages of each demographic group is graphed with standard deviations as error bars. SES, socio-economic status; ps > 0.05.
Girls (n = 13) outperformed boys (n = 8) in all four reaction and movement time measures but significantly in CMT (M = 328.29 vs. M = 396.44; Cohen’s d = −0.39). Other cognitive variables (SMT, CRT, and SRT) did not reach significant gender differences (ps > 0.05). There were statistically significant differences in SRT, SMT, CRT, and CMT based on children’s weight status (ps < 0.05). Children categorized into the healthy weight group had faster SMT (M = 283.32 vs. M = 399.49, Cohen’s d = −1.33) and CMT (M = 312.80 vs. M = 483.32, Cohen’s d = −1.43), compared to children in the overweight/obese group. Also, healthy weight children had faster SRT (M = 667.37 vs. M = 1040.90, Cohen’s d = 1.04) and CRT (M = 675.14 vs. 997.22, Cohen’s d = −0.93) compared to children in the overweight/obese group. It was found that SES showed effects with a moderate effect size on the CMT but not on other tests (high SES M = 290.51 vs. low SES M = 393.48; Cohen’s d = 0.67). These results are visualized in Figure 2 by each measured cognitive variable.

Figure 2. Disparities in cognitive function (n = 21). Averages of each demographic group is graphed with standard deviations as error bars. SRT, single reaction time; SMT, single movement time; CRT, choice reaction time; CMT, choice movement time; ms, milliseconds; SES, socio-economic status; *p < 0.05.
4. Discussion
The purpose of this study was to investigate obesity (healthy weight vs. overweight/obese) and socio-demographic (gender, SES) disparities in FMS (locomotor and ball skills) and cognitive function (single and choice reaction time and single and choice movement time) in a sample of preschoolers. Objectively measured cognitive function using the CANTAB™ is an innovative strategy, and to the best of our knowledge, this is one of the first attempts to be implemented in a young preschool sample in conjunction with a process-oriented motor skill assessment. The results of this study provide insight of the potential detrimental effects of unhealthy BMI on cognitive function in preschoolers and highlights the likelihood of socio-demographic disparities in developmental outcomes.
4.1. Obesity disparities
The investigation for weight-related effects on cognitive function in early childhood is still in its infancy, however, the current study brings a pioneering measurement to further guide future research. As the most important finding of this study, the obesity disparity in cognitive function was significant in this age group. That is, children with healthy weight had a significantly faster reaction and movement time in a single and choice exhibition compared to their overweight/obese peers. It was noted that obesity can be detrimental to cognitive functioning, however, specific mechanisms are still being uncovered in youth populations (Eichen et al., 2018). Obesity-related biomarkers have been seen to be associated with different areas of cognitive function (i.e., learning, memory, and general ability), but have mainly been observed in animal models and adult populations; identifying the presence of potential biomarkers in an early childhood may be necessary to effectively deter the negative effects on cognitive function in a more proactive and timely manner (Miller et al., 2015). Furthermore, there is limited evidence using neuropsychological assessment of cognitive function, specifically regarding reaction time measurements, so more research with longitudinal designs are suggested to further dissect this relationship in early childhood. Children with healthy weight may have more cognitive advancements and greater academic achievements than children categorized as overweight/obese possibly due to their higher activity/fitness levels (Hillman et al., 2005; Castelli et al., 2007; Davis et al., 2011; Palmer et al., 2013; Crova et al., 2014). Due to obesity potentially positing lower physical activity/exercise levels in children compared to children in a healthy weight category, children that are overweight/obese may not sufficiently activate neurophysiological components in their brain essential for cognitive function (Hillman et al., 2008), which could inevitably hinder their school readiness and success entering elementary/grade school. Two recent reviews examining cognitive functions with physical activity and motor skill performance in a preschool sample underscore the lack of sound methodology in retained studies and encourage future studies to adopt a clinical trial design that emphasizes different components of cognitive function (Jylänki et al., 2022; Malambo et al., 2022). It’s important to mention that the relationship between obesity and physical activity is not linear, so other factors would also need to be accounted for in future studies for a comprehensive understanding. Maintaining healthy weight status in early childhood is essential to promote cognitive function, which ultimately may benefit school readiness when entering elementary/grade school. It is of great benefit for future studies to objectively measure physical activity/fitness levels in conjunction with objective cognitive measures, to understand this relationship more thoroughly in a preschool population.
These results suggest that providing more opportunities for preschoolers to participate in physical activity in and out of the school settings are highly recommended to eliminate the obesity disparity in early childhood. If children are playing organized sports/activities that require timing execution (baseball/softball, dance), it’s possible these activities are not only promoting a healthier BMI, but also improving their cognitive skills (i.e., reaction and movement timing). A recent study found that using an intervention containing motor games (motor stories, learning environments, and motor circuits) can be used to facilitate learning new skills, such as swimming (Simón-Piqueras et al., 2022). Although assessing physical activity and/or fitness was outside the scope of this study, research has shown in school-aged children, more physical activity/greater fitness was related to greater cognitive gains (Castelli et al., 2007; Hillman et al., 2008). The overweight/obese group in our sample may not have participated in organized sports/activities compared to their healthy weight peers, which could deter important physiological and metabolic responses conducive for healthy cognitive function (Hillman et al., 2008). Assessing cognition objectively (i.e., reaction and movement time via CANTAB™; investigating brain activity) in a young preschool sample may be needed in future work to identify delays or signs of dysfunction earlier so appropriate interventions could be implemented sooner (i.e., structured physical activity or FMS-based recess). Previous research also indicates that different types of physical activities for obesity prevention could influence (hinder or improve) children’s cognitive functioning from a young age. For example, activities such as playing outside, playing strategy-based sports/games, and active classroom breaks may instantly activate the brain and promote reaction time capability, whereas passive sedentary activities (i.e., only watching TV/video, using internet on mobile or computer device) may hinder or delay cognitive development (Esteban-Cornejo et al., 2015). Since these children are only 3–5 years old, it’s unlikely that they have developed autonomy over their free time, so their activities may be determined from their parents/family’s interests and values. Early childhood obesity prevention strategies may also be required to be individually tailored towards community and home environmental specific structures to fully capture a child’s developmental profile (Moss and Gu, 2022).
The current findings are consistent with two previous studies among preschoolers; however, methods of cognitive assessments differed (Krombholz, 2013; Martin et al., 2016). For instance, Krombholz (2013) assessed intelligence, verbal ability, and concentration to represent cognition and found children in the overweight group demonstrated lower intelligence. Martin et al. (2016) assessed vocabulary, picture similarity, and pattern construction to represent cognition and reported that obesity at 3 years old was associated with some significant adverse cognitive outcomes at 5 years old, robustly in boys’ pattern construction. Even though a similar trend favoring healthy weight was reached among these studies, assessing cognition utilizing various methodology may make generalizing results difficult, especially in a young sample. There is a need for more standardized, objective measurements in younger samples’ cognitive function to produce more comparable data. Nonetheless, the current study augments the established evidence that weight status (favoring healthy weight) influences children’s cognitive function in early childhood. The obesity disparity revealed here should encourage schools and parents to monitor children’s weight status to pave opportunities for cognitive growth.
Although, no significant overweight/obese disparities were observed in FMS, children in the healthy weight group demonstrated better locomotor and ball skills than their counterparts, especially in ball skills. Consistent with a recent systematic review, the relationship between weight status and FMS is inconsistent across age groups and many studies utilized various methods of obesity measures (BMI, Waist circumferences, DXA) (Slotte et al., 2017). Emerging research acknowledges the important role FMS posits toward obesity trajectory during childhood (Stodden et al., 2008; Robinson et al., 2015). The current study provides the preliminary evidence on an emerging obesity disparity trend in ball skills regardless of gender and SES status. It is critical to implement intervention programs that focus on promoting movement opportunities (regularly scheduled FMS-based play time or structured recess) in early childcare settings to ensure sufficient practice and developmental opportunities are provided for this vulnerable population.
4.2. Gender disparities
Regarding cognitive function, gender differences were not found through our measures. Girls did, however, show to be faster in reaction and movement time (significantly in CMT) which contradicts the work from Latorre-Roman et al. (2018), exhibiting 4 year old girls demonstrating slower reaction times than boys in the ruler drop test. Within this young population, it’s important to emphasize activities to facilitate healthy cognitive development for both boys and girls. Typically, boys are more involved in organized sports than girls (Marques et al., 2016) which could enhance aspects of cognitive function (i.e., reaction and movement time) due to practicing the skills necessary to complete the action needed in the sport (i.e., timing in throwing, striking). In the current sample, however, girls showed to be faster than boys in both reaction and movement time; specifically, girls presented higher scores on the ball skills involving eye-hand coordination capability. These girls could be involved in extracurricular activities promoting these skills, which could be the potential explanation of the inconsistency with Marques et al.’s findings.
Gender-inclusive FMS interventions have been shown to improve ball skills in girls, which can aid in eliminating the gender disparity at a young age (Veldman et al., 2017). Incorporating more gender-inclusive FMS-based interventions in childcare and home settings can help develop FMS, and consequently, facilitate academic and cognitive success (Chang and Gu, 2018). As a whole, the sample in the current study acquired lower locomotor and ball skills compared to a nationally representative sample (Kit et al., 2017). Childcare center professionals and parents should facilitate gender inclusive opportunities throughout early childhood to further develop FMS and avoid potential motor delays that may enlarge the disparity in later childhood and adolescence.
4.3. Socio-economic status disparities
Encompassing the environmental role that is used to shape children’s cognitive function and motor acquisition is essential to fully understand the impact of affordances throughout development (Zoghi et al., 2019). Although SES was not seen to bear significant differences in cognitive function, it’s important to note there were observed slower reaction and movement times throughout the low SES group as well as the overweight/obese group. Families that are identified as low income may struggle to support the fundamental needs of their children and may not have available funds to invest in cognitive stimulating activities/opportunities as wealthier families would (Poh et al., 2019). It has been shown cognitive function is linearly associated with parental education (Noble et al., 2015), which is a correlate of SES. Low SES preschoolers in the current study may not have the same affordances for cognitive growth at home or school settings as their high SES peers may have, which could explain the emerging disparity in cognitive function.
It was found that children identified as low SES demonstrated poorer locomotor and ball skills compared to children identified as high SES, even though disparities did not reach significance. The SES and gender disparities in preschoolers’ FMS and cognitive development may even widen or become statistically significant due to the COVID-19 pandemic by exacerbating the already known health-related disparities in low SES populations (López-Bueno et al., 2020). Pairing that with childcare/school closures throughout 2020 and 2021 might lead detrimental effects on low SES children’s motor development due to the lack of motor affordances they may have in their home environment. Future research should investigate the implications of the COVID-19 pandemic on preschoolers’ developmental outcomes, especially in vulnerable populations such as children in low SES and/or overweight/obese children. It’s important for childcare professionals to provide opportunities fairly and adequately for motor and cognitive growth, such as incorporating different toys and equipment in their curriculum and provide more opportunities to promote equality of affordances, especially in the low-SES population. Public policy and government funding strategies may need to be reevaluated to ensure these needs can be met.
5. Conclusion
The strength of this study was assessing cognitive function objectively using CANTAB™ in a preschool-aged sample and identifying potential obesity and socio-demographic disparities in motor and cognitive outcomes. The CANTAB™ assessment of reaction and movement time provides solid, preliminary evidence of the status of children’s cognitive function and also generates insights of how socio-demographic factors may influence FMS and cognitive function. Some limitations should be acknowledged, however. First, all children lived a similar geographic region, which can make it difficult for generalizability of the findings. Second, given the strength of the objective measures for cognitive function, we were only able to assess a small subgroup of children in this study due to its monetary and timely costs as well as the guideline from CANTAB™. The current findings highlight the importance of healthy weight status in young children’s development, especially regarding cognitive function. It’s important for parents and childcare stakeholders to actively monitor weight status and encourage cognitively-stimulating activities that will promote motor skill development and also cognitive functions such as reaction and movement time. In conclusion, this study provides preliminary evidence identifying the potential obesity and socio-demographic disparities in preschoolers’ motor and cognitive skill development using objective measurements during early childhood.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Texas at Arlington IRB. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
The authors received financial support for this research from the University of Texas at Arlington Research Enhancement Program (REP).
Acknowledgments
The authors would like to thank the children, faculty, staff, and parents involved with this project and the research team who participated.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Barnett, L. M., van Beurden, E., Morgan, P. J., Brooks, L. O., and Beard, J. R. (2010). Gender differences in motor skill proficiency from childhood to adolescence: a longitudinal study. Res. Q. Exerc. Sport 81, 162–170. doi: 10.1080/02701367.2010.10599663
Berlin, L., and Bohlin, G. (2002). Response inhibition, hyperactivity, and conduct problems among preschool children. J. Clin. Child Adolesc. Psychol. 31, 242–251. doi: 10.1207/s15374424jccp3102_09
Blair, C., David Zelazo, P., and Greenberg, M. T. (2005). The measurement of executive function in early childhood. Dev. Neuropsychol. 28, 561–571. doi: 10.1207/s15326942dn2802_1
Cameron, C. E., Brock, L. L., Murrah, W. M., Bell, L. H., Worzalla, S. L., Grissmer, D., et al. (2012). Fine motor skills and executive function both contribute to kindergarten achievement. Child Dev. 83, 1229–1244. doi: 10.1111/j.1467-8624.2012.01768.x
Castelli, D., Hillman, C. H., Buck, S. M., and Erwin, H. (2007). Physcal fitness and academic achievement in 3rd & 5th grade students. J. Sport Exerc. Psychol. 29, 239–252. doi: 10.1123/jsep.29.2.239
Cataldo, R., Huang, J., Calixte, R., Wong, A. T., Bianchi-Hayes, J., and Pati, S. (2016). Effects of overweight and obesity on motor and mental development in infants and toddlers. Pediatr. Obes. 11, 389–396. doi: 10.1111/ijpo.12077
CDC Division of Nutrition, P.A., and Obesity, National Center for Chronic Disease Prevention and Health Promotion (2021). Childhood obesity facts: prevalence of childhood obesity in the United States [Online]. Available: https://www.cdc.gov/obesity/data/childhood.html#Prevalence (Accessed April 4, 2020).
Chang, M., and Gu, X. (2018). The role of executive function in linking fundamental motor skills and reading proficiency in socioeconomically disadvantaged kindergarteners. Learn. Individ. Differ. 61, 250–255. doi: 10.1016/j.lindif.2018.01.002
Crova, C., Struzzolino, I., Marchetti, R., Masci, I., Vannozzi, G., Forte, R., et al. (2014). Cognitively challenging physical activity benefits executive function in overweight children. J. Sports Sci. 32, 201–211. doi: 10.1080/02640414.2013.828849
Daley, D., and Birchwood, J. (2010). ADHD and academic performance: why does ADHD impact on academic performance and what can be done to support ADHD children in the classroom? Child: care. Health Dev. 36, 455–464. doi: 10.1111/j.1365-2214.2009.01046.x
Davis, C. L., Tomporowski, P., McDowell, M., Austin, B. P., Miller, P. H., Yanasak, N. E., et al. (2011). Exercise improves executive function and achievement and alters brain activiation in overweight children: a randomized, controlled trial. Health Psychol. 30, 91–98. doi: 10.1037/a0021766
Eichen, D. M., Appleton-Knapp, S., and Boutelle, K. N. (2018). “Childhood obesity and cognitive function.” Pediatric obesity: Etiology, Pathogenesis and Treatmen), 539–551.
Esteban-Cornejo, I., Martinez-Gomez, D., Sallis, J. F., Cabanas-Sánchez, V., Fernández-Santos, J., Castro-Piñero, J., et al. (2015). Objectively measured and self-reported leisure-time sedentary behavior and academic performance in youth: the UP&DOWN study. Prev. Med. 77, 106–111. doi: 10.1016/j.ypmed.2015.05.013
Fisher, A., Boyle, J. M. E., Paton, J. Y., Tomporowski, P., Watson, C., McColl, J. H., et al. (2011). Effects of a physical education intervention on cognitive function in young children: randomized controlled pilot study. BMC Pediatr. 11, 1–9. doi: 10.1186/1471-2431-11-97
Frazier-Wood, A. C., Carnell, S., Pena, O., Hughes, S. O., O'Connor, T. M., Asherson, P., et al. (2014). Cognitive performance and BMI in childhood: shared genetic influences between reaction time but not response inhibition. Obesity 22, 2312–2318. doi: 10.1002/oby.20862
Gentier, I., Augustijn, M., Deforche, B., Tanghe, A., De Bourdeaudhuij, I., Lenoir, M., et al. (2013). A comparative study of performance in simple and choice reaction time tasks between obese and healthy-weight children. Res. Dev. Disabil. 34, 2635–2641. doi: 10.1016/j.ridd.2013.04.016
Goodway, J. D., Robinson, L. E., and Crowe, H. (2010). Gender differences in fundamental motor skill development in disadvantaged preschoolers from two geographical regions. Res. Q. Exerc. Sport 81, 17–24. doi: 10.1080/02701367.2010.10599624
Groppe, K., and Elsner, B. (2017). Executive function and weight status in children: a one-year longitudinal perspective. Child Neuropsychol. 23, 129–147. doi: 10.1080/09297049.2015.1089981
Hamilton, M., Liu, T., and ElGarhy, S. (2017). The relationship between body weight and motor skill competence in hispanic low-ses preschool children. Early Childhood Educ. J. 45, 529–535. doi: 10.1007/s10643-016-0785-y
Hillman, C. H., Castelli, D. M., and Buck, S. M. (2005). Aerobic fitness and neurocognitive function in healthy preadolescent children. Med. Sci. Sports Exerc. 37, 1967–1974. doi: 10.1249/01.mss.0000176680.79702.ce
Hillman, C. H., Erickson, K. I., and Kramer, A. F. (2008). Be smart, exercise your heart: exercise effects on brain and cognition. Nat. Rev. Neurosci. 9, 58–65. doi: 10.1038/nrn2298
Hjorth, M. F., Sørensen, L. B., Andersen, R., Dyssegaard, C. B., Ritz, C., Tetens, I., et al. (2016). Normal weight children have higher cognitive performance – independent of physical activity, sleep, and diet. Physiol. Behav. 165, 398–404. doi: 10.1016/j.physbeh.2016.08.021
Hulteen, R. M., Morgan, P. J., Barnett, L. M., Stodden, D. F., and Lubans, D. R. (2018). Development of foundational movement skills: a conceptual model for physical activity across the lifespan. Sports Med. 48, 1533–1540. doi: 10.1007/s40279-018-0892-6
Jylänki, P., Mbay, T., Hakkarainen, A., Sääkslahti, A., and Aunio, P. (2022). The effects of motor skill and physical activity interventions on preschoolers' cognitive and academic skills: a systematic review. Prev. Med. 155:106948. doi: 10.1016/j.ypmed.2021.106948
Kelsey, M. M., Zaepfel, A., Bjornstad, P., and Nadeau, K. J. (2014). Age-related consequences of childhood obesity. Gerontology 60, 222–228. doi: 10.1159/000356023
Kessels, R. P. C. (2019). Improving precision in neuropsychological assessment: bridging the gap between classic paper-and-pencil tests and paradigms from cognitive neuroscience. Clin. Neuropsychol. 33, 357–368. doi: 10.1080/13854046.2018.1518489
Khalaj, N., and Amri, S. (2013). Mastery of gross motor skills among preschool obese children. Ovidius Univ. Ann. Ser. Phys. Educ. Sport. Sci. Mov. Health 184, 795–802.
Kipling Webster, E., and Ulrich, D. (2017). Evaluation of the psychometric properties of the test of gross motor development-3rd edition. J. Mot. Learn. Dev. 5, 45–58. doi: 10.1123/jmld.2016-0003
Kit, B. K., Akinbami, L. J., Isfahani, N. S., and Ulrich, D. A. (2017). Gross motor development in children aged 3–5 years, United States 2012. Matern. Child Health J. 21, 1573–1580. doi: 10.1007/s10995-017-2289-9
Kokštejn, J., Musálek, M., and Tufano, J. J. (2017). Are sex differences in fundamental motor skills uniform throughout the entire preschool period? PLoS One 12:e0176556. doi: 10.1371/journal.pone.0176556
Krombholz, H. (2013). Motor and cognitive performance of overweight preschool children. Percept. Mot. Skills Learn. Mem. 116, 40–57. doi: 10.2466/22.25.PMS.116.1.40-57
Latorre-Roman, P. A., Robles-Fuentes, A., García-Pinillos, F., Salas-Sánchez, J. S., and Salas-Sánchez, J. (2018). Reaction times of preschool children on the ruler drop test: a cross-sectional study with reference values. Percept. Mot. Skills 125, 866–878. doi: 10.1177/0031512518789563
Liu, T., Hamilton, M., and Smith, S. (2015). Motor proficiency of the head start and typically developing children on MABC-2. J. Child Adolesc. Behav. 03, 1–4. doi: 10.4172/2375-4494.1000198
Lloyd, M., Saunders, T. J., Bremer, E., and Tremblay, M. S. (2014). Long-term importance of fundamental motor skills: a 20-year follow-up study. Adapt. Phys. Act. Q. 31, 67–78. doi: 10.1123/apaq:2013-0048
Logan, S. W., Robinson, L. E., Wilson, A. E., and Lucas, W. A. (2012). Getting the fundamentals of movement: a meta-analysis of the effectiveness of motor skill interventions in children. Child Care Health Dev. 38, 305–315. doi: 10.1111/j.1365-2214.2011.01307.x
López-Bueno, R., López-Sánchez, G. F., Casajús, J. A., Calatayud, J., Tully, M. A., and Smith, L. (2020). Potential health-related behaviors for pre-school and school-aged children during COVID-19 lockdown: a narrative review. Prev. Med. 143:106349. doi: 10.1016/j.ypmed.2020.106349
Malambo, C., Nová, A., Clark, C., and Musálek, M. (2022). Associations between fundamental movement skills, physical fitness, motor competency, physical activity, and executive functions in pre-school age children: a systematic review. Children 9:1059. doi: 10.3390/children9071059
Marques, A., Ekelund, U., and Sardinha, L. B. (2016). Associations between organized sports participation and objectively measured physical activity, sedentary time and weight status in youth. J. Sci. Med. Sport 19, 154–157. doi: 10.1016/j.jsams.2015.02.007
Martin, A., Booth, J. N., Young, D., Revie, M., Boyter, A. C., Johnston, B., et al. (2016). Associations between obesity and cognition in the pre-school years. Obesity 24, 207–214. doi: 10.1002/oby.21329
McClelland, M. M., and Cameron, C. E. (2019). Developing together: the role of executive function and motor skills in children’s early academic lives. Early Child. Res. Q. 46, 142–151. doi: 10.1016/j.ecresq.2018.03.014
Mileva-Seitz, V. R., Ghassabian, A., Bakermans-Kranenburg, M. J., Van Den Brink, J. D., Linting, M., Jaddoe, V. W. V., et al. (2015). Are boys more sensitive to sensitivity? Parenting and executive function in preschoolers. J. Exp. Child Psychol. 130, 193–208. doi: 10.1016/j.jecp.2014.08.008
Miller, A. L., Lee, H. J., and Lumeng, J. C. (2015). Obesity-associated biomarkers and executive function in children. Pediatr. Res. 77, 143–147. doi: 10.1038/pr.2014.158
Moradi, A., and Esmaeilzadeh, S. (2017). Simple reaction time and obesity in children: whether there is a relationship? Environ. Health Prev. Med. 22:2. doi: 10.1186/s12199-017-0612-0
Moss, S., and Gu, X. (2022). Home-and community-based interventions for physical activity and early child development: a systematic review of effective strategies. Int. J. Environ. Res. Public Health 19:11968. doi: 10.3390/ijerph191911968
Musalek, M., Kokstejn, J., Papez, P., Scheffler, C., Mumm, R., Czernitzki, A.-F., et al. (2017). Impact of normal weight obesity on fundamental motor skills in pre-school children aged 3 to 6 years. Anthropol. Anz. 74, 203–212. doi: 10.1127/anthranz/2017/0752
Noble, K. G., Houston, S. M., Brito, N. H., Bartsch, H., Kan, E., Kuperman, J. M., et al. (2015). Family income, parental education and brain structure in children and adolescents. Nat. Neurosci. 18, 773–778. doi: 10.1038/nn.3983
Palmer, K. K., Miller, M. W., and Robinson, L. E. (2013). Acute exercise enhances preschoolers’ ability to sustain attention. J. Sport Exerc. Psychol. 35, 433–437. doi: 10.1123/jsep.35.4.433
Pearce, A., Scalzi, D., Lynch, J., and Smithers, L. G. (2016). Do thin, overweight and obese children have poorer development than their healthy-weight peers at the start of school? Findings from a south Australian data linkage study. Early Child. Res. Q. 35, 85–94. doi: 10.1016/j.ecresq.2015.10.007
Piek, J. P., Dawson, L., Smith, L. M., and Gasson, N. (2008). The role of early fine and gross motor development on later motor and cognitive ability. Hum. Mov. Sci. 27, 668–681. doi: 10.1016/j.humov.2007.11.002
Poh, B. K., Lee, S. T., Yeo, G. S., Tang, K. C., Noor Afifah, A. R., Siti Hanisa, A., et al. (2019). Low socioeconomic status and severe obesity are linked to poor cognitive performance in Malaysian children. BMC Public Health 19:541. doi: 10.1186/s12889-019-6856-4
Quan, M., Zhang, H., Zhang, J., Zhou, T., Zhang, J., Zhao, G., et al. (2018). Preschoolers’ technology-assessed physical activity and cognitive function: a cross-sectional study. J. Clin. Med. 7:108. doi: 10.3390/jcm7050108
Raine, L., Drollette, E., Kao, S. C., Westfall, D., Chaddock-Heyman, L., Kramer, A. F., et al. (2018). The associations between adiposity, cognitive function, and achievement in children. Med. Sci. Sports Exerc. 50, 1868–1874. doi: 10.1249/MSS.0000000000001650
Robinson, L. E., Stodden, D. F., Barnett, L. M., Lopes, V. P., Logan, S. W., Rodrigues, L. P., et al. (2015). Motor competence and its effect on positive developmental trajectories of health. Sports Med. 45, 1273–1284. doi: 10.1007/s40279-015-0351-6
Sahakian, B. J., and Owen, A. M. (1992). Computerized assessment in neuropsychiatry using CANTAB: discussion paper. J. R. Soc. Med. 85, 399–402.
Sharma, V., Coleman, S., Nixon, J., Sharples, L., Hamilton-Shield, J., Rutter, H., et al. (2019). A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes. Rev. 20, 1341–1349. doi: 10.1111/obr.12904
Simón-Piqueras, J. Á., Prieto-Ayuso, A., Gómez-Moreno, E., Martínez-López, M., and Gil-Madrona, P. (2022). Evaluation of a program of aquatic motor games in the improvement of motor competence in children from 4 to 5 years old. Children 9:1141. doi: 10.3390/children9081141
Slotte, S., Sääkslahti, A., Kukkonen-Harjula, K., and Rintala, P. (2017). Fundamental movement skills and weight status in children: a systematic review. Balt. J. Health Phys. Act. 9, 115–127. doi: 10.29359/BJHPA.09.2.11
Stodden, D., Gao, Z., Goodway, J. D., and Langendorfer, S. J. (2014). Dynamic relationships between motor skill competence and health-related fitness in youth. Pediatr. Exerc. Sci. 26, 231–241. doi: 10.1123/pes.2013-0027
Stodden, D. F., Goodway, J. D., Langendorfer, S. J., Roberton, M. A., Rudisill, M. E., Garcia, C., et al. (2008). A developmental perspective on the role of motor skill competence in physical activity: an emergent relationship. Quest 60, 290–306. doi: 10.1080/00336297.2008.10483582
Syväoja, H. J., Tammelin, T. H., Ahonen, T., Räsänen, P., Tolvanen, A., Kankaanpää, A., et al. (2015). Internal consistency and stability of the CANTAB neuropsychological test battery in children. Psychol. Assess. 27, 698–709. doi: 10.1037/a0038485
Vameghi, R., Shams, A., and Dehkordi, P. (2013). Relationship between age, sex and body mass index with fundamental motor skills among 3 to 6 years-old children. Medicinski glasnik Specijalna bolnica za bolesti stitaste zlezde i bolesti metabolizma Zlatibor 18, 7–15. doi: 10.5937/medgla1347007v
Veldman, S. L., Palmer, K. K., Okely, A. D., and Robinson, L. (2017). Promoting ball skills in preschool-age girls. J. Sci. Med. Sport 20, 50–54. doi: 10.1016/j.jsams.2016.04.009
Viegas, Â. A., Mendonça, V. A., Pontes Nobre, J. N., Souza Morais, R. L. D., Fernandes, A. C., Oliveira Ferreira, F. D., et al. (2021). Associations of physical activity and cognitive function with gross motor skills in preschoolers: cross-sectional study. J. Mot. Behav., 1–16. doi: 10.1080/00222895.2021.1897508
Vuontela, V. (2003). Audiospatial and visuospatial working memory in 6-13 year old school children. Learn. Mem. 10, 74–81. doi: 10.1101/lm.53503
Webster, E. K., Pitchford, E. A., and Ulrich, D. A. (2015). Psychometric properties for a United States cohort for the test of gross motor development -3rd edition. J. Sport Exerc. Psychol. 37:S17.
Winter, S. M., and Sass, D. A. (2011). Healthy & ready to learn: examining the efficacy of an early approach to obesity prevention and school readiness. J. Res. Child. Educ. 25, 304–325. doi: 10.1080/02568543.2011.580211
Keywords: obesity, cognitive function, fundamental motor skills, socio-economic status, preschoolers, reaction time, movement time
Citation: Moss S, Zhang X, Tamplain P and Gu X (2023) Overweight/obesity and socio-demographic disparities in children’s motor and cognitive function. Front. Psychol. 14:1134647. doi: 10.3389/fpsyg.2023.1134647
Edited by:
Boris Schmitz, Witten/Herdecke University, GermanyReviewed by:
Josie Booth, University of Edinburgh, United KingdomPedro Gil-Madrona, University of Castilla-La Mancha, Spain
Copyright © 2023 Moss, Zhang, Tamplain and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangli Gu, eGlhbmdsaS5ndUB1dGEuZWR1
 Samantha Moss
Samantha Moss Xiaoxia Zhang
Xiaoxia Zhang Priscila Tamplain3
Priscila Tamplain3 Xiangli Gu
Xiangli Gu