- 1Department of Psychology, Shahid Beheshti University, Tehran, Iran
- 2Centre of Precision Rehabilitation for Spinal Pain (CPR Spine), School of Sport, Exercise and Rehabilitation Sciences, College of Life and Environmental Sciences, University of Birmingham, Birmingham, United Kingdom
- 3Institute for Mental Health (IMH), School of Psychology, University of Birmingham, Birmingham, United Kingdom
- 4The Centre for Human Brain Health (CHBH), School of Psychology, University of Birmingham, Birmingham, United Kingdom
Fear of cancer recurrence is fear or worry about cancer recurrence or progress. Fear of recurrence can impact patients’ quality of life and wellbeing. Cancer survivors’ families support them practically and emotionally, making them a vital supplement for official healthcare. Given the well-established important role of the family in dealing with cancer, we compiled the studies that examined the relationship between family-related factors and fear of cancer recurrence (FCR) among cancer survivors (CSs). One of the foremost studies in this field is the FCR model presented by Mellon and colleagues, which included concurrent family stressors and family-caregiver FCR as factors linked to survivor FCR. Our goal was to prepare the ground for a family-based model of FCR that is more comprehensive than the one proposed by Mellon et al. sixteen years ago. The studies included those with samples of adult cancer survivors from different regions of the world. Most of the studies we reviewed are cross-sectional studies. We categorized family-related factors associated with survivor FCR into partner-related factors, including subgroups of disclosure to partner, cognitions of partner, and partner’s sources of support; parenthood-related factors, including having children and parenting stress; family-related factors, including living situation, family history of cancer, family’s perception of the illness, and family characteristics; and social interactions including social support, disclosure, social constraints, and attitudes of others. This review sheds light on how significant others of cancer survivors can affect and be affected by cancer-related concerns of survivors and emphasizes the necessity of further investigation of family-related factors associated with FCR.
1 Introduction
Cancer has become one of the most prevalent conditions that impact people worldwide, but the number of survivors is increasing with improvements in treatments and care (Cancer Today, 2020). For instance, nearly 20 million new cancer cases were diagnosed worldwide in 2020 (Sung et al., 2021). However, for some types of cancer, a significant percentage of patients are expected to survive. For example, global 5-year survival rates for breast and prostate cancer, two of the most common cancers, exceed 90% (Nardin et al., 2020; Subudhi, 2023). While it is great news that many people are now surviving a once-deadly disease, research shows that Cancer survivors (CS) experience a wide range of problems caused by cancer and its treatments, including physical, psychosocial, spiritual, and existential issues, some of which persist for years (Institute of Medicine and National Research Council, 2006). Future uncertainty and fear of cancer recurrence are among the most common difficulties that CSs and their caregivers experience (Institute of Medicine and National Research Council, 2006; Jefford et al., 2008).
Fear of cancer recurrence (FCR) is defined as fear or worry about cancer recurrence or progress (Lebel et al., 2016) and is experienced at moderate to high levels by 59% of CSs (Luigjes-Huizer et al., 2022). FCR can motivate survivors to promote healthy behaviors to adapt to their new situation (Park and Gaffey, 2007). On the other hand, lower quality of life, more psychological distress, increased use of healthcare, and increased healthcare costs are downsides to FCR (Thewes et al., 2012; Simard et al., 2013; Lebel et al., 2014, 2016; Jimenez et al., 2017; Champagne et al., 2018; Hall et al., 2018).
Family support is one of the sources that help the survivors deal with their challenges to such a degree that it has been known as a vital supplement for official healthcare (Nijboer et al., 1998; Haley, 2003; Koltai et al., 2018). The family becomes a part of the caregiving team for patients. They get involved in a wide range of issues, from symptom management to problems related to hospitalization and dealing with financial, autonomy, psychological, and social issues (Effendy et al., 2015). Families of CSs support them emotionally by reassuring and consoling, expressing love and affection, being present, distracting the patient from cancer, and practically by accompanying them to the hospital for examinations, treatments, support with household chores, etc. (Vrontaras, 2018). The impact of the family on patients’ adaptation to their new situation and how they cope with the condition goes beyond simply being a support network. For example, spouse-caregivers with higher emotional distress early after diagnosis significantly decrease patient adaptation to cancer a year later (Park et al., 2010). Many studies tried to model the family’s contribution to cancer survivorship, hoping that the model can help design interventions to improve patient’s quality of life and adaptation.
Exploring familial aspects of fear of cancer recurrence needs to be a priority in psycho-oncology because this form of health anxiety is increasing due to the increasing number of survivors. Moreover, research has shown that multiple dimensions of both caregiver and patient well-being, including role adjustment, mental health, quality of life, and psychological distress are interrelated (Northouse et al., 2000; Chen et al., 2004; Bambauer et al., 2006; Kim and Given, 2008). Following the lead of these studies, fear of cancer recurrence should be seen as a factor influenced by caregivers, which usually means family members. As a result of our deepened understanding of how family members influence survivor FCR, we can educate families on how to alleviate FCR in survivors. Further, we would be able to design psychological interventions that could involve family members in the therapy for those with elevated FCR. It should arguably be so because family members are as involved as the survivors with the emotional impacts of cancer.
Mellon et al. (2007) suggested a family-based model of FCR, which was influenced by the resilience model (McCubbin and McCubbin (1996). This intricate family resilience model describes the link between stressors and increased demands for family adaptation. In short, according to this model, stressor events and the pile-up of demands affect family meaning and schema, situational appraisal, family resources, and social support, either through family type or directly, which in turn influence family problem-solving and coping skills. Finally, family problem-solving and coping skills are directly linked to family adaptation (McCubbin and McCubbin, 1996). Inspired by this model, Mellon et al. (2007) proposed their model of FCR in which several individual factors (including age, education, sex, and race), stressors (including concurrent family stressors and illness-related stressors), and family resources (including family hardiness and social support) affected fear of recurrence in survivors and family members through their illness representation. In this model, there is a bidirectional relationship between CS and family members’ fears. Testing their model on a sample of CSs and their family members, they presented a revised model (Mellon et al., 2007): individual factors, stressors, and illness representation affect the CS and family members’ FCR directly, and the relationship between the CS and family member’s fear is bidirectional, as it was in the initial model. Mellon et al. (2007) have acknowledged that many other factors can be added to their model. Since Mellon et al. (2007) model was proposed, several studies have looked into family-related factors, such as the type of relationship and social context, associated with survivors’ FCR that may suggest alterations to the original model.
This narrative review aims to examine the studies investigating the link between fear of recurrence in patients and family members and how their relationship and social context impacted patients’ fear of recurrence. We have categorized family-related factors into partner-related, parenthood-related, family-related, and social interactions.
2 Study selection
The search was conducted on PubMed and Google Scholar. Relevant keywords in the search included fear of cancer recurrence, FCR, fear of cancer progression AND family, caregiver, spouse, partner, parent, mother, father, child. During reviewing papers, if a new keyword was discovered (e.g., disclosure), it was searched to include potentially relevant articles. References and citations have been explored for relevant publications. Among the articles, those that assessed FCR in adult survivors and contained variables or themes that involved the social circle of cancer survivors were selected for the review. The search was conducted in April 2023 and included peer-reviewed articles published in English between 2001 and 2023. A total number of 38 publications met these criteria and were included in this review. Table 1 presents an overview of these studies.
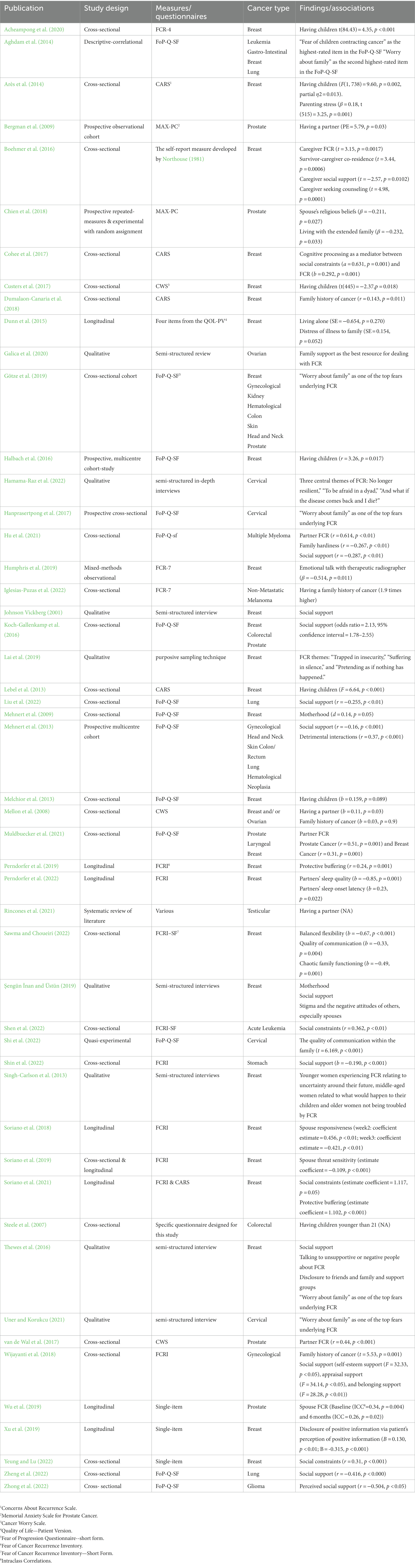
Table 1. Studies included in the current review examining family-related factors related to FCR and summary of their findings.
3 Synthesis of findings
3.1 Partner-related factors associated with fear of cancer recurrence
To begin with, having a partner or not is one of the factors that may impact the level of FCR in CSs. Partnered men diagnosed with prostate or testicular cancer have shown significantly less FCR than single ones (Bergman et al., 2009; Rincones et al., 2021). In contrast, married women had more cancer worries than non-married women in a sample of women with breast or ovarian cancer (Mellon et al., 2008). These studies may not be comparable due to differences in design, scales used, different definitions of relationship and the different nature of prostate, testicular, breast, and ovarian cancers. Also, the mentioned studies are exceptions in the relationship between FCR and marital status since most studies have found no significant relationship between the two variables (Northouse, 1981; Leake et al., 2001; Llewellyn et al., 2008; Simard et al., 2010; Custers et al., 2017; Dumalaon-Canaria et al., 2018; Lebel et al., 2018; Starreveld et al., 2018; Thewes et al., 2018). However, a plausible explanation for the contrasting results could be that women are traditional caregivers in most cultures, and this makes them a relieving caregiver when their partner is ill. In these circumstances, they become care receivers, and the same fact makes them feel like a burden on their partners. A study finds gender role conditioning to be an underlying factor for women assuming the role of caregiver for themselves (Guberman et al., 1992). In addition to gender differences, it would be beneficial to analyse the data controlling for age since it is possible that age would be a moderator in the relationship between marital status and FCR.
In a qualitative study investigating the meaning of FCR for cervical cancer survivors, one of the main themes that emerged was “to be afraid in a dyad,” which refers to FCR being the sort of challenge that is discussed with a partner and dealt with by getting help from partner’s resources (Hamama-Raz et al., 2022). In this study, communication with partners seems to be the main distinction between women who feel alone in their survivorship experience and those who do not (Hamama-Raz et al., 2022). Several quantitative studies confirm the significant relationship between open communication with a partner and survivor FCR. Protective buffering, which is defined as “efforts to protect one’s partner from upset and burden by concealing worries, hiding concerns, and yielding to the partner to avoid disagreements” (Manne et al., 2007), is a construct measured by the extent to which CSs or their partners engage in specific behaviors to deal with cancer-related issues. Likewise, the social constraints are constructs reflecting the perception that one cannot share cancer-related thoughts, concerns, or worries with one’s spouse on account of his/her disinterest, unavailability, or disapproval (Lepore and Revenson, 2007). Higher protective buffering and social constraints of CSs have been shown to predict their increased FCR in longitudinal studies, although one’s protective buffering or social constraints do not affect his/her partner’s FCR (Perndorfer et al., 2019; Soriano et al., 2021). Cognitive processing is suggested to mediate the relationship between social constraints and FCR, according to Cohee et al. (2017).
Capitalisation, which describes the process of disclosing positive events to a close other (attempt), whose response is perceived as genuine and enthusiastic (perceived partner responsiveness, hereafter termed responsiveness) (Langston, 1994; Gable and Reis, 2010), is another way of looking into couple communication. A study by Soriano et al. (2018) has examined the relationship between capitalisation and FCR around the first mammogram post-diagnosis, from which inconsistent results have emerged: although they had hypothesized that both attempts and responsiveness would buffer FCR, attempts never significantly predicted lower FCR and responsiveness only predicted lower FCR after the mammogram. Disclosure of positive information by spouse is also another factor influencing FCR according to a longitudinal study: spouses’ disclosure of information that was communicated in a positive manner (i.e., supportive, inclusive, and concerned manner) has shown to be linked to breast cancer survivors’ decreased FCR via breast cancer survivors’ perceptions of positive information (Xu et al., 2019). The results of the studies that emphasize the effect of within-couple communication on FCR can be justified by the social-cognitive processing model, which suggests that sharing concerns with a close other is an adaptive response to adversity since it facilitates cognitive processing (Lepore, 2001; Lepore and Revenson, 2007). So, any variable that refers to openness to communication may be related to FCR, while withholding worries hinders cognitive processing, thus impends adjustment and maintains FCR (Lepore, 2001; Lepore and Revenson, 2007). Within-couple communication relationship with survivor FCR has been supported by several studies, most of which are longitudinal ones, making the data more reliable and the suggested relationship more likely to be a cause-and-effect relationship. However, all quantitative studies that suggest this link have been conducted on women diagnosed with breast cancer, which hinders the generalizability of the results. Women diagnosed with breast cancer are more concerned with some cancer-related problems than women diagnosed with other cancer types, which probably makes the nature of their fears about recurrence different from other CSs. For example, women with breast cancer experience higher sexual dysfunction [including abnormalities in sexual desire, arousal, lubrication, satisfaction, orgasm, and dyspareunia (Boquiren et al., 2016)] in comparison with women with other cancer types (Jing et al., 2019), which probably causes more worries concerning sexuality. Worries about the sexual consequences of cancer and its treatment is a topic to discuss with a partner, so couples’ communication may be quite beneficial for women with breast cancer but not as helpful for women with other cancer types. Future research is needed to investigate the content of discussions about FCR with partners (e.g., surrounding which items of CARS) and compare the effect of discussing each specific concern on FCR. Furthermore, no study has been conducted on men regarding the relationship between couples’ communication and FCR.
Some cognitions of CSs’ partners are also associated with survivor FCR. In a qualitative study on Turkish breast cancer survivors, an identified trigger of FCR was stigma and negative attitude of spouses (Şengün İnan and Üstün, 2019). Threat sensitivity, which reflects individual differences in the general tendency to attend to, behaviourally and emotionally respond to, and avoid threatening negative stimuli (Carver and White, 1994), is also characteristic in partners that can influence survivor FCR. When FCR peaks in the first mammogram post-diagnosis in breast cancer survivors and their spouses, spouse threat sensitivity, not CS’s, predicts longer recovery from FCR peak in both CS and spouse (Soriano et al., 2019). However, spouse threat sensitivity could not predict reactivity or patient FCR on mammogram day (Soriano et al., 2019). Like attitudes toward cancer and threat sensitivity, having religious beliefs or not as the partner of a CS is linked to survivor FCR. In a sample of Taiwanese prostate cancer survivors and their partners, CSs whose partners had religious beliefs reported less FCR than those with partners without religious beliefs (Chien et al., 2018). Of course, we are unsure which element or function of religion causes this link. The most studied construct concerning survivor FCR in a relationship context is partner FCR. Several studies have shown a positive association between survivor FCR and partner FCR among different sexes, cancer types, countries, and FCR scales (Boehmer et al., 2016; van de Wal et al., 2017; Hu et al., 2021; Muldbuecker et al., 2021). Not much is known about the causality that may lay under this association. However, in the study by Boehmer et al. (2016), partners’ FCR directly affected survivors’ FCR, while survivors’ FCR did not affect partners’ FCR. Likewise, spouse FCR 6 months after treatment showed a significant association with patient FCR a year after treatment, but no trends toward patient FCR being correlated with later spouse FCR emerged, which indicates that it may be spouse FCR, that influences patient FCR, not vice versa (Wu et al., 2019). The effect of partner cognitions on survivor FCR seems only natural since FCR is coped with in a dyad (Hamama-Raz et al., 2022), and partners are frequently cited as the most important confidants (Figueiredo et al., 2004); when a CS counts on someone as her companion in adversity, the companion’s thoughts on the matter gains importance and affects the way the CS thinks and feels about her experience.
Another category of partner-related factors associated with survivor FCR is the partner’s source of support. CSs whose partners have higher social support seem to have lower FCR, while those who seek counseling have higher FCR (Boehmer et al., 2016). A possible explanation could be that seeing a partner receiving support from more conventional sources (e.g., family and friends) is a sign of them handling the situation well, whereas seeking help from a professional signifies a crisis or an overwhelming situation. According to this potential explanation, CSs are less fearful about cancer relapse or progression when their partner is handling the situation well.
Not many studies have worked on factors associated with FCR in the relationship context that are potential consequences of survivor FCR. But, survivor FCR is associated with a partner’s reduced sleep quality and greater sleep onset latency in a sample of American couples coping with early-stage breast cancer (Perndorfer et al., 2022). Speculation about why this association exists can be that partners are emotionally and physiologically sensitive to CSs’ worries to a high degree.
3.2 Parenthood-related factors associated with fear of cancer recurrence
Not much research has been done on how being a parent affects FCR. But several studies suggest that motherhood is a trigger of FCR, a factor affecting the nature of FCR, and associated with higher FCR (Mellon et al., 2008; Mehnert et al., 2009; Lebel et al., 2013; Melchior et al., 2013; Arès et al., 2014; Halbach et al., 2016; Custers et al., 2017; Şengün İnan and Üstün, 2019; Acheampong et al., 2020). Further, Steele et al. (2007) found that women younger than 21 with children experience higher levels of FCR. Similarly, Singh-Carlson et al. (2013) found that younger women commonly experienced FCR relating to uncertainty around their future, whereas, for middle-aged women, the FCR centred around what would happen to their children and older women were not troubled by FCR. A more specific construct concerning parenting and how it might interact with FCR is investigated by Arès et al. (2014), who found that parenting stress increases FCR. In the study by Arès et al. (2014), young breast cancer survivors who had children Arès et al. (2014) also reported that breast cancer interfered more with their intimate lives than childless CSs. These findings pieced together imply that the heightening effect of motherhood on FCR comes from women’s responsibility for their children. Cancer recurrence means having to go through intense treatment, having less time to spend with their children; an increase in the possibility of their death, leaving their children motherless; and an increase in the responsibilities expected from their adolescent due to his/her mother being hospitalized or debilitated. Consequently, women worry about cancer recurrence more if they have children they should care for.
A study by Aghdam et al. (2014) on Iranian CSs (male and female) showed that fear of children contracting cancer is the highest-rated item in the Fear of Progression Questionnaire. To our knowledge, no study has specifically examined the relationship between fatherhood and FCR.
3.3 Family-related factors associated with fear of cancer recurrence
Some quantitative and qualitative studies on samples from various cultures, cancer types, and ages have identified “worry about family” as one of the top fears underlying FCR (Aghdam et al., 2014; Thewes et al., 2016; Hanprasertpong et al., 2017; Götze et al., 2019; Uner and Korukcu, 2021). Further, Uner and Korukcu (2021) have found the basis for fear of death to be fear of leaving their loved ones alone among young Turkish CSs suspected of new cancer. Considering this finding, it could be estimated that some CSs’ worry for their families is manifested in items or themes other than “fear of family being affected by cancer,” and family has even greater importance in their mind than the results that research shows.
The living situation of CSs seems to influence their FCR levels. Survivors who do not live alone experience higher FCR (Dunn et al., 2015) and survivor-caregiver co-residence seem to increase survivors’ FCR (Boehmer et al., 2016). Although these results have come solely from female breast cancer survivors from the USA, a population probably not representative of all CSs, and they used unconventional measurements for FCR, they give us a cue for further investigation of how CSs perceive the influence cancer has on their relationships with people around them. Another study concerning the living situation of cancer survivors and FCR was carried out on an entirely different population. Chien et al. (2018) found Taiwanese prostate cancer survivors with their partners, children, and grandchildren to have lower FCR than those with only their partners. The contrasting results of these studies emphasize sex and cultural differences. For example, it may be the case that CSs in American culture, an individualistic society that emphasizes autonomy, feel like a burden on the people they live with, while CSs in Taiwanese culture, a collectivist society that counts taking care of elderly family members as a duty, feel quite comfortable with getting as much help as they need from their extended families. Alternatively, the reason for the difference between the studies of Boehmer et al. (2016) and Dunn et al. (2015) and the study of Chien et al. (2018) may be partially again due to women being traditional caregivers, who feel like they should not be care receivers.
Another family-related factor associated with FCR is a family history of cancer. Having a family history of cancer seems to increase FCR, as seen in American women with breast/ovarian cancer, Australian women with breast cancer, Spanish melanoma patients and Indonesian women with gynaecological cancer (Mellon et al., 2008; Dumalaon-Canaria et al., 2018; Wijayanti et al., 2018; Iglesias-Puzas et al., 2022). More research is needed to make clear how a family history of cancer may affect a CS’s perception of cancer, recurrence, and caregiving. However, a plausible explanation is that maybe CSs with a family history of cancer are more cognizant of the difficulties accompanied by cancer, or they think that their family resources are drained after dealing with cancer once.
Similar to the study by Mellon et al. (2007), which relates the meaning of illness to family members to FCR, Dunn et al. (2015) showed that distress of illness in the family is associated with FCR. This data means there may be a cause-and-effect relationship or a bidirectional interaction between how family members perceive and feel about cancer and survivor FCR. This is very likely since there is evidence of CSs mentioning the attitude of people around them, especially their partners, as affecting their FCR (Thewes et al., 2016; Şengün İnan and Üstün, 2019).
Some family characteristics have been linked to FCR, expected concerning how families communicate and handle difficulties. Family hardiness, balanced flexibility and the quality of communication within the family are associated with decreased FCR (Hu et al., 2021; Sawma and Choueiri, 2022; Shi et al., 2022). On the other hand, chaotic family functioning increases FCR levels, while cohesion, disengagement, enmeshment, and family satisfaction does not seem to impact the severity of FCR (Sawma and Choueiri, 2022). These studies only include Chinese and Lebanese CSs, with the majority of them being women. So, with regard to differences in the role of the family in Eastern cultures and Western ones, it seems necessary to compare the relationship of these constructs with FCR in various cultures. But according to what we know until now, it could be said that FCR is more effectively curbed in families that are more flexible in their roles, more resilient to stress, better in problem-solving, cooperation, and open communication, and feel more in control of difficulties.
Family support is the best resource for dealing with FCR for some CSs (Galica et al., 2020). However, not all people feel comfortable to discuss their worries about cancer with their family members. In a Taiwanese qualitative study on women who have been diagnosed with breast cancer in the last 2 years, three themes emerged for FCR: “Trapped in insecurity,” “Suffering in silence,” and “Pretending as if nothing happened” (Lai et al., 2019). These women did not mention their feelings surrounding cancer to their families to maintain family balance and continued to perform their roles in the family as before the cancer (Lai et al., 2019).
3.4 Social interactions’ relationship with FCR
Some researchers prefer not to limit social interactions that relate to FCR to partners and family members. They, thus, explore the social support construct in their studies, which refers to the support that an individual gets from family, friends, and other people she may feel close to, such as colleagues, neighbors, and her medical team. This expansion makes sense since many people feel closest to their significant others who are not family members or partners. In this case, these significant others probably play a bigger role in supporting the CS. Also, this type of research’s findings apply to a family context. Therefore they are included in the current review.
Many studies from different countries and various cancer types have shown that CSs with higher social support experience lower FCR (Mehnert et al., 2013; Koch-Gallenkamp et al., 2016; Şengün İnan and Üstün, 2019; Hu et al., 2021; Liu et al., 2022; Shin et al., 2022; Zheng et al., 2022; Zhong et al., 2022). Likewise, a significant negative relationship has been observed between the number of significant others and FCR, along with a strong link between the number of significant others CSs identify as understanding her health concerns and FCR (Northouse, 1981). Fear of loneliness and fear of relying on strangers for daily activities in case of cancer recurrence has also been mentioned as an important part of FCR, which confirms the idea that social support is a determining factor in FCR (Götze et al., 2019; Şengün İnan and Üstün, 2019). How social support may link to lower FCR can have multiple answers, one of which is extracted from qualitative studies showing that CSs find social support an effective coping strategy in the face of FCR, using it more than any other coping strategy (Johnson Vickberg, 2001; Thewes et al., 2016). Another way of social support influencing FCR can be through resilience, as suggested by Zhong et al. (2022).
An important part of social support, which researchers address, is communication. Failure to disclose is reported to be inversely correlated to social support and positively associated with receiving unsupportive responses (Figueiredo et al., 2004). There seem to be two sides to disclosing FCR-related thoughts and emotions: In a study by Thewes et al. (2016), some participants from all levels of FCR reported that disclosure to friends, family, and support groups provided opportunities for emotional ventilation and mutual support, while some others found it anxiety-producing because of the perceived impact of these discussions on others. Due to the adverse effect that talking about cancer-related worries may have on others, some CSs withhold these worries in order to protect family and friends (Şengün İnan and Üstün, 2019). Taking into account worries about the effect of cancer talk on family and friends, some patients opt to disclose their worries to professionals, which seems to reduce FCR: emotional talk of breast cancer patients during their second review appointment with their therapeutic radiographers is negatively associated with follow-up FCR, which is measured 6–8 weeks after the end of treatment (Humphris et al., 2019). We can again interpret these associations in the social-cognitive processing model framework, which suggests that sharing concerns with a close other is an adaptive response to adversity since it facilitates cognitive processing (Lepore, 2001; Lepore and Revenson, 2007).
In its broad sense, social constraints not limited to spouses discussed previously can increase FCR (Shen et al., 2022; Yeung and Lu, 2022). Mediating factors between social constraints and FCR for which evidence has emerged are illness perception, self-stigma, bodily pain, and ambivalence over emotional expression (Shen et al., 2022; Yeung and Lu, 2022). Both studies that link social constraints and FCR have been done on Chinese samples, which may limit the generalizability of these findings. For instance, the Chinese tend to translate their inhibited emotions into somatic symptoms (e.g., pain), which means that the mediating effect of bodily pain in the link between social constraints and FCR could be limited to the Chinese culture (Mak and Zane, 2004). So, in order to generalize these findings, more research has to be done in other cultures, along with a quest for other possible mediating factors in the relationship between social constraints and FCR, such as cognitive processing, coping behaviors, optimism, self-efficacy, and threat appraisal.
Although getting help from their support circle can assist CSs in reducing their FCR, sometimes, this support circle triggers FCR. Women from a study by Thewes et al. (2016) identified talking to unsupportive or negative people as an ineffective coping strategy for FCR, and women from a study by Şengün İnan and Üstün (2019) think that behaving as if they were still ill after treatment by people around them was a trigger for FCR. Moreover, detrimental interactions (including over-protective behavior, dismissive, conflictual behavior patterns, and pessimism) have been identified to predict higher FCR (Mehnert et al., 2013). Hence, disclosing cancer-related thoughts and feelings to others does not decrease FCR unconditionally, and potential harm underlies some social interactions.
4 Discussion
This narrative review paper aimed to categorize family-related factors associated with survivors’ FCR under partner-related factors, including subgroups of disclosure to partner, cognitions of partner, and partner’s sources of support; parenthood-related factors, including having children and parenting stress; family-related factors, including living situation, family history of cancer, family’s perception of the illness, and family characteristics; and social interactions including social support, disclosure, social constraints, and attitudes of others.
The results of this narrative review of quantitative and qualitative literature signify a variety of family-related factors greatly affecting survivors’ fear of recurrence. Although relatively few studies account for familial aspects of FCR, the results promise at least some family-related factors to account for FCR variations. This means that in the near future, we may be able to have a family-based model of FCR and base a family-oriented intervention on it.
We chose narrative review over systematic review because the inclusion and exclusion criteria required by systematic review limit the breadth of the papers included. Some reviewed papers that offer insightful contributions to the field have used unconventional scales, do not have a rigorous methodology, or are unsuitable for quantitative synthesis. We aimed to bring attention to all the family-related constructs correlated with FCR to lay the grounds for original research that models potential contributing factors. So, we refrained from a methodology that would dismiss a paper with relevant findings that could inspire us to find other constructs in the same category. Moreover, not many papers explore the familial aspect of FCR; therefore, excluding a few papers affects the take-home message of this review more than it usually does.
The most prominent feature of this literature review is that it gathers together studies from different countries, various cancer types, and various methodologies that have one thing in common, which is the key to looking at FCR in a new way: accounting for family resources. This review intends to lead researchers to look for resources for improving the mental health of survivors in the family and even community instead of looking for what resources an individual has. No single person can bear the burden of dealing with cancer and its consequences alone since this disease makes them physically and mentally vulnerable.
The obvious limitation of this study is that it has yet to use rigorous methodologies. Thus, regardless of the authors’ attempts to stay impartial, it is inclined to bias.
Researchers in the FCR field have addressed many family-related variables that have proved to be linked to FCR. However, most of them cannot be generalized to all CSs due to the dominance of research on women and cultural gulfs that are very important in family matters. Also, our knowledge of how parenthood, especially fatherhood, can affect the nature and intensity of FCR is extremely limited, which calls for further investigation. The current literature review attempted to critically analyse the most significant results of the previous studies on family-related factors associated with FCR and categorize them in a way that reveals the strengths and limitations of the current models and sets the stage to elaborate on them (please see Figure 1 for an overview).
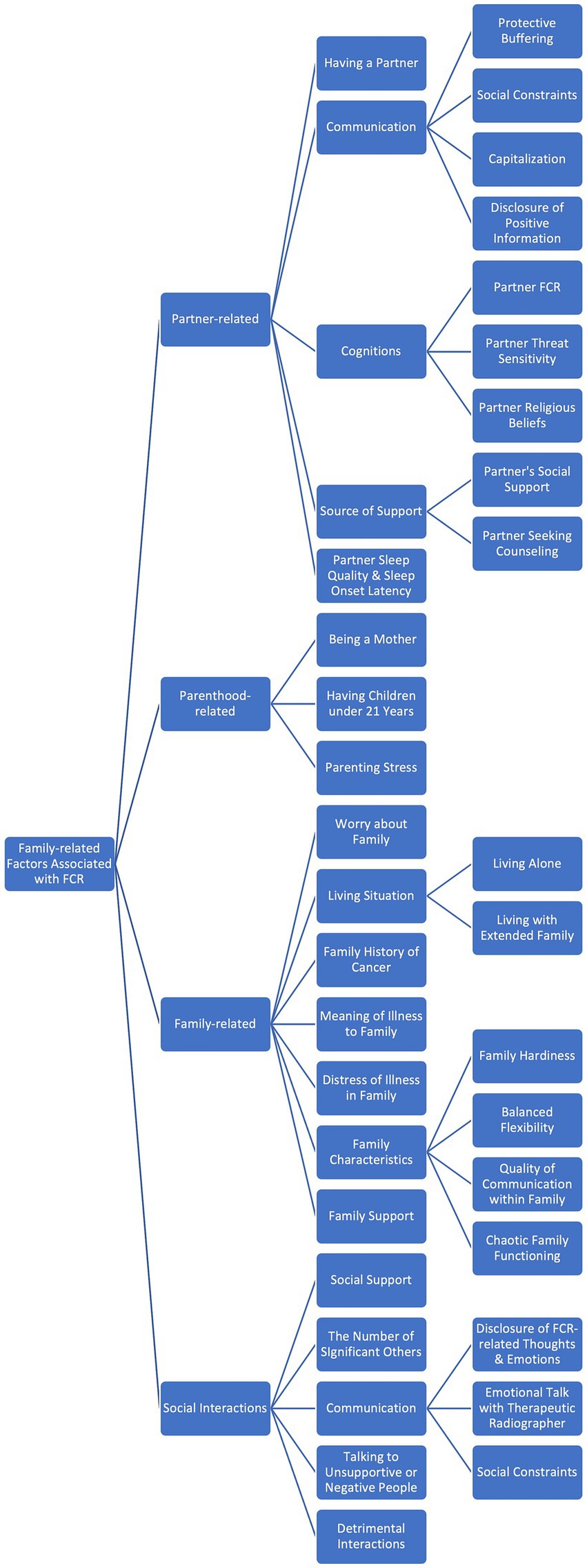
Figure 1. The Categorisation of family-related factors associated with FCR (Fear of Cancer Recurrence).
5 Conclusion
In brief, we categorized family-related factors associated with survivor FCR into partner-related factors, including subgroups of disclosure to partner, cognitions of partner, and partner’s sources of support; parenthood-related factors, including having children and parenting stress; family-related factors, including living situation, family history of cancer, family’s perception of the illness, and family characteristics; and social interactions including social support, disclosure, social constraints, and attitudes of others. Knowing how and why each factor relates to survivor FCR helps us to construct a more comprehensive family-based model in completion of Mellon et al.’s (2007) model, which can, in turn, assist clinicians in designing family interventions for managing FCR. Researchers in the FCR field have addressed many family-related variables that have proved to be linked to FCR. However, most of them cannot be generalized to all CSs due to the dominance of research on women and cultural gulfs that are very important in family matters. Also, our knowledge of how parenthood, especially fatherhood, can affect the nature and intensity of FCR is extremely limited, which calls for further investigation. The current literature review attempted to critically analyse the most significant results of the studies on family-related factors associated with FCR and categorize them in a way that reveals the strengths and limitations of the current literature.
Author contributions
AF: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. MD: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. AK: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Acheampong, R., Bergman, K., Sweeny, K., and Wilson, M. (2020). Fear of cancer recurrence among black and white mothers. UC Riverside Undergrad. Res. J. Submit 14, 17–22. doi: 10.5070/RJ5141049261
Aghdam, A. M., Rahmani, A., Nejad, Z. K., Ferguson, C., Mohammadpoorasl, A., and Sanaat, Z. (2014). Fear of cancer recurrence and its predictive factors among Iranian cancer patients. Indian J. Palliat. Care 20, 128–133. doi: 10.4103/0973-1075.132632
Arès, I., Lebel, S., and Bielajew, C. (2014). The impact of motherhood on perceived stress, illness intrusiveness and fear of cancer recurrence in young breast cancer survivors over time. Psychol. Health 29, 651–670. doi: 10.1080/08870446.2014.881998
Bambauer, K. Z., Zhang, B., Maciejewski, P. K., Sahay, N., Pirl, W. F., Block, S. D., et al. (2006). Mutuality and specificity of mental disorders in advanced cancer patients and caregivers. Soc. Psychiatry Psychiatr. Epidemiol. 41, 819–824. doi: 10.1007/s00127-006-0103-x
Bergman, J., Gore, J. L., Saigal, C. S., Kwan, L., and Litwin, M. S. (2009). Partnership and outcomes in men with prostate cancer. Cancer 115, 4688–4694. doi: 10.1002/cncr.24544
Boehmer, U., Tripodis, Y., Bazzi, A. R., Winter, M., and Clark, M. A. (2016). Fear of cancer recurrence in survivor and caregiver dyads: differences by sexual orientation and how dyad members influence each other. J. Cancer Surviv. 10, 802–813. doi: 10.1007/s11764-016-0526-7
Boquiren, V. M., Esplen, M. J., Wong, J., Toner, B., Warner, E., and Malik, N. (2016). Sexual functioning in breast cancer survivors experiencing body image disturbance. Psycho-Oncology 25, 66–76. doi: 10.1002/pon.3819
Cancer Today (2020) Estimated number of new cases in 2020, world, both sexes, all ages. Lyon: International Agency for Research on Cancer. Available at: https://gco.iarc.fr/today/online-analysis-table
Carver, C. S., and White, T. L. (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J. Pers. Soc. Psychol. 67, 319–333. doi: 10.1037/0022-3514.67.2.319
Champagne, A., Ivers, H., and Savard, J. (2018). Utilization of health care services in cancer patients with elevated fear of cancer recurrence. Psycho-Oncology 27, 1958–1964. doi: 10.1002/pon.4748
Chen, M.-L., Chu, L., and Chen, H.-C. (2004). Impact of cancer patients’ quality of life on that of spouse caregivers. Support. Care Cancer 12, 469–475. doi: 10.1007/s00520-004-0636-z
Chien, C.-H., Chuang, C.-K., Liu, K.-L., Wu, C.-T., Pang, S.-T., and Chang, Y.-H. (2018). Positive and negative affect and prostate cancer-specific anxiety in Taiwanese patients and their partners. Eur. J. Oncol. Nurs. 37, 1–11. doi: 10.1016/j.ejon.2018.09.004
Cohee, A. A., Adams, R. N., Johns, S. A., Von Ah, D., Zoppi, K., Fife, B., et al. (2017). Long-term fear of recurrence in young breast cancer survivors and partners. Psycho-Oncology 26, 22–28. doi: 10.1002/pon.4008
Custers, J. A. E., Gielissen, M. F. M., de Wilt, J. H. W., Honkoop, A., Smilde, T. J., van Spronsen, D.-J., et al. (2017). Towards an evidence-based model of fear of cancer recurrence for breast cancer survivors. J. Cancer Surviv. 11, 41–47. doi: 10.1007/s11764-016-0558-z
Dumalaon-Canaria, J. A., Prichard, I., Hutchinson, A. D., and Wilson, C. (2018). Fear of cancer recurrence and psychological well-being in women with breast cancer: the role of causal cancer attributions and optimism. Eur. J. Cancer Care 27:e12579. doi: 10.1111/ecc.12579
Dunn, L. B., Langford, D. J., Paul, S. M., Berman, M. B., Shumay, D. M., Kober, K., et al. (2015). Trajectories of fear of recurrence in women with breast cancer. Support. Care Cancer 23, 2033–2043. doi: 10.1007/s00520-014-2513-8
Effendy, C., Vernooij-Dassen, M., Setiyarini, S., Kristanti, M. S., Tejawinata, S., Vissers, K., et al. (2015). Family caregivers' involvement in caring for a hospitalized patient with cancer and their quality of life in a country with strong family bonds. Psycho-Oncology 24, 585–591. doi: 10.1002/pon.3701
Figueiredo, M. I., Fries, E., and Ingram, K. M. (2004). The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psychooncology 13, 96–105. doi: 10.1002/pon.717
Gable, S. L., and Reis, H. T. (2010). Good news! Capitalizing on positive events in an interpersonal context. Adv. Exp. Soc. Psychol. 42, 195–257. doi: 10.1016/S0065-2601(10)42004-3
Galica, J., Giroux, J., Francis, J.-A., and Maheu, C. (2020). Coping with fear of cancer recurrence among ovarian cancer survivors living in small urban and rural settings: a qualitative descriptive study. Eur. J. Oncol. Nurs. 44:101705. doi: 10.1016/j.ejon.2019.101705
Götze, H., Taubenheim, S., Dietz, A., Lordick, F., and Mehnert-Theuerkauf, A. (2019). Fear of cancer recurrence across the survivorship trajectory: results from a survey of adult long-term cancer survivors. Psycho-Oncology 28, 2033–2041. doi: 10.1002/pon.5188
Guberman, N., Maheu, P., and Maille, C. (1992). Women as family caregivers: why do they care? The Gerontologist 32, 607–617. doi: 10.1093/geront/32.5.607
Halbach, S. M., Enders, A., Kowalski, C., Pförtner, T. K., Pfaff, H., Wesselmann, S., et al. (2016). Health literacy and fear of cancer progression in elderly women newly diagnosed with breast cancer—a longitudinal analysis. Patient Educ. Couns. 99, 855–862. doi: 10.1016/j.pec.2015.12.012
Haley, W. E. (2003). Family caregivers of elderly patients with cancer: understanding and minimizing the burden of care. J. Support. Oncol. 1, 25–29.
Hall, D. L., Luberto, C. M., Philpotts, L. L., Song, R., Park, E. R., and Yeh, G. Y. (2018). Mind-body interventions for fear of cancer recurrence: a systematic review and meta-analysis. Psycho-Oncology 27, 2546–2558. doi: 10.1002/pon.4757
Hamama-Raz, Y., Shinan-Altman, S., and Levkovich, I. (2022). The intrapersonal and interpersonal processes of fear of recurrence among cervical cancer survivors: a qualitative study. Support. Care Cancer 30, 2671–2678. doi: 10.1007/s00520-021-06695-8
Hanprasertpong, J., Geater, A., Jiamset, I., Padungkul, L., Hirunkajonpan, P., and Songhong, N. (2017). Fear of cancer recurrence and its predictors among cervical cancer survivors. J. Gynecol. Oncol. 28:e72. doi: 10.3802/jgo.2017.28.e72
Hu, X., Wang, W., Wang, Y., and Liu, K. (2021). Fear of cancer recurrence in patients with multiple myeloma: prevalence and predictors based on a family model analysis. Psycho-Oncology 30, 176–184. doi: 10.1002/pon.5546
Humphris, G., Yang, Y., Barracliffe, L., Cameron, J., and Bedi, C. (2019). Emotional talk of patients with breast cancer during review appointments with therapeutic radiographers: effects on fears of cancer recurrence. Support. Care Cancer 27, 2143–2151. doi: 10.1007/s00520-018-4484-7
Iglesias-Puzas, Á., García-González, V., Conde-Taboada, A., and López-Bran, E. (2022). Fear of cancer recurrence in patients with non-metastatic melanoma: Spanish validation and disease-related factors. Australas. J. Dermatol. 63, e312–e319. doi: 10.1111/ajd.13907
Institute of Medicine and National Research Council (2006) From Cancer patient to Cancer survivor: lost in transition. Washington, DC: The National Academies Press.
Jefford, M., Karahalios, E., Pollard, A., Baravelli, C., Carey, M., Franklin, J., et al. (2008). Survivorship issues following treatment completion—results from focus groups with Australian cancer survivors and health professionals. J. Cancer Surviv. 2, 20–32. doi: 10.1007/s11764-008-0043-4
Jimenez, R. B., Perez, G. K., Rabin, J., Hall, D., Quain, K., Park, E., et al. (2017). Fear of recurrence among cancer survivors. vol. 35. Alexandria, Virginia, USA: American Society of Clinical Oncology, 10053.
Jing, L., Zhang, C., Li, W., Jin, F., and Wang, A. (2019). Incidence and severity of sexual dysfunction among women with breast cancer: a meta-analysis based on female sexual function index. Support. Care Cancer 27, 1171–1180. doi: 10.1007/s00520-019-04667-7
Johnson Vickberg, S. M. (2001). Fears about breast cancer recurrence: interviews with a diverse sample. Cancer Pract. 9, 237–243. doi: 10.1046/j.1523-5394.2001.009005237.x
Kim, Y., and Given, B. A. (2008). Quality of life of family caregivers of cancer survivors: across the trajectory of the illness. Cancer 112, 2556–2568. doi: 10.1002/cncr.23449
Koch-Gallenkamp, L., Bertram, H., Eberle, A., Holleczek, B., Schmid-Höpfner, S., Waldmann, A., et al. (2016). Fear of recurrence in long-term cancer survivors—do cancer type, sex, time since diagnosis, and social support matter? Health Psychol. 35, 1329–1333. doi: 10.1037/hea0000374
Koltai, K., Walsh, C., Jones, B., and Berkelaar, B. L. (2018). Applying social network analysis to identify the social support needs of adolescent and young adult cancer patients and survivors. J. Adolesc. Young Adult Oncol. 7, 181–186. doi: 10.1089/jayao.2017.0058
Lai, W. S., Shu, B. C., and Hou, W. L. (2019). A qualitative exploration of the fear of recurrence among Taiwanese breast cancer survivors. Eur. J. Cancer Care 28:e13113. doi: 10.1111/ecc.13113
Langston, C. A. (1994). Capitalizing on and coping with daily-life events: expressive responses to positive events. J. Pers. Soc. Psychol. 67, 1112–1125. doi: 10.1037/0022-3514.67.6.1112
Leake, R. L., Gurrin, L. C., and Hammond, I. G. (2001). Quality of life in patients attending a low-risk gynaecological oncology follow-up clinic. Psycho-Oncology 10, 428–435. doi: 10.1002/pon.539
Lebel, S., Beattie, S., Arès, I., and Bielajew, C. (2013). Young and worried: age and fear of recurrence in breast cancer survivors. Health Psychol. 32, 695–705. doi: 10.1037/a0030186
Lebel, S., Maheu, C., Lefebvre, M., Secord, S., Courbasson, C., Singh, M., et al. (2014). Addressing fear of cancer recurrence among women with cancer: a feasibility and preliminary outcome study. J. Cancer Surviv. 8, 485–496. doi: 10.1007/s11764-014-0357-3
Lebel, S., Maheu, C., Tomei, C., Bernstein, L. J., Courbasson, C., Ferguson, S., et al. (2018). Towards the validation of a new, blended theoretical model of fear of cancer recurrence. Psycho-Oncology 27, 2594–2601. doi: 10.1002/pon.4880
Lebel, S., Ozakinci, G., Humphris, G., Mutsaers, B., Thewes, B., Prins, J., et al. (2016). From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support. Care Cancer 24, 3265–3268. doi: 10.1007/s00520-016-3272-5
Lepore, S. J. (2001). “A social–cognitive processing model of emotional adjustment to cancer” in Psychosocial interventions for cancer. eds. A. Baum and B. L. Andersen (Washington, D.C., USA: American Psychological Association), 99–116.
Lepore, S. J., and Revenson, T. A. (2007). Social constraints on disclosure and adjustment to cancer. Soc. Personal. Psychol. Compass 1, 313–333. doi: 10.1111/j.1751-9004.2007.00013.x
Liu, M., Liu, L., Zhang, S., Li, T., Ma, F., and Liu, Y. (2022). Fear of cancer recurrence and hope level in patients receiving surgery for non-small cell lung cancer: a study on the mediating role of social support. Support. Care Cancer 30, 9453–9460. doi: 10.1007/s00520-022-07318-6
Llewellyn, C. D., Weinman, J., McGurk, M., and Humphris, G. (2008). Can we predict which head and neck cancer survivors develop fears of recurrence? J. Psychosom. Res. 65, 525–532. doi: 10.1016/j.jpsychores.2008.03.014
Luigjes-Huizer, Y. L., Tauber, N. M., Humphris, G., Kasparian, N. A., Lam, W. W., Lebel, S., et al. (2022). What is the prevalence of fear of cancer recurrence in cancer survivors and patients? A systematic review and individual participant data meta-analysis. Psycho-Oncology 31, 879–892. doi: 10.1002/pon.5921
Mak, W. W., and Zane, N. W. (2004). The phenomenon of somatization among community Chinese Americans. Soc. Psychiatry Psychiatr. Epidemiol. 39, 967–974. doi: 10.1007/s00127-004-0827-4
Manne, S. L., Norton, T. R., Ostroff, J. S., Winkel, G., Fox, K., and Grana, G. (2007). Protective buffering and psychological distress among couples coping with breast cancer: the moderating role of relationship satisfaction. J. Fam. Psychol. 21, 380–388. doi: 10.1037/0893-3200.21.3.380
McCubbin, M., and McCubbin, H. (1996). “Resiliency in families: a conceptual model of family adjustment and adaptation in response to stress and crises” in Family assessment: Resiliency, coping and adaptation: Inventories for research and practice. eds. M. C. HI, A. I. Thompson, and M. C. MA (Madison, WI: University of Wisconsin), 1–64.
Mehnert, A., Berg, P., Henrich, G., and Herschbach, P. (2009). 'Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology 18, 1273–1280. doi: 10.1002/pon.1481
Mehnert, A., Koch, U., Sundermann, C., and Dinkel, A. (2013). Predictors of fear of recurrence in patients one year after cancer rehabilitation: a prospective study. Acta Oncol. 52, 1102–1109. doi: 10.3109/0284186X.2013.765063
Melchior, H., Büscher, C., Thorenz, A., Grochocka, A., Koch, U., and Watzke, B. (2013). Self-efficacy and fear of cancer progression during the year following diagnosis of breast cancer. Psycho-Oncology 22, 39–45. doi: 10.1002/pon.2054
Mellon, S., Gold, R., Janisse, J., Cichon, M., Tainsky, M. A., Simon, M. S., et al. (2008). Risk perception and cancer worries in families at increased risk of familial breast/ovarian cancer. Psycho-Oncology 17, 756–766. doi: 10.1002/pon.1370
Mellon, S., Kershaw, T. S., Northouse, L. L., and Freeman-Gibb, L. (2007). A family-based model to predict fear of recurrence for cancer survivors and their caregivers. Psychooncology 16, 214–223. doi: 10.1002/pon.1074
Muldbuecker, P., Steinmann, D., Christiansen, H., de Zwaan, M., and Zimmermann, T. (2021). Are women more afraid than men? Fear of recurrence in couples with cancer–predictors and sex-role-specific differences. J. Psychosoc. Oncol. 39, 89–104. doi: 10.1080/07347332.2020.1762823
Nardin, S., Mora, E., Varughese, F. M., D'Avanzo, F., Vachanaram, A. R., Rossi, V., et al. (2020). Breast Cancer survivorship, quality of life, and late toxicities. Front. Oncol. 10:864. doi: 10.3389/fonc.2020.00864
Nijboer, C., Tempelaar, R., Sanderman, R., Triemstra, M., Spruijt, R. J., and Van Den Bos, G. A. (1998). Cancer and caregiving: the impact on the caregiver's health. Psychooncology 7, 3–13. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<3::AID-PON320>3.0.CO;2-5
Northouse, L. L. (1981). Mastectomy patients and the fear of cancer recurrence. Cancer Nurs. 4, 213–220. doi: 10.1097/00002820-198106000-00004
Northouse, L. L., Mood, D., Templin, T., Mellon, S., and George, T. (2000). Couples' patterns of adjustment to colon cancer. Soc. Sci. Med. 50, 271–284. doi: 10.1016/S0277-9536(99)00281-6
Park, C. L., and Gaffey, A. E. (2007). Relationships between psychosocial factors and health behavior change in cancer survivors: an integrative review. Ann. Behav. Med. 34, 115–134. doi: 10.1007/BF02872667
Park, S. M., Kim, Y. J., Kim, S., Choi, J. S., Lim, H.-Y., Choi, Y. S., et al. (2010). Impact of caregivers’ unmet needs for supportive care on quality of terminal cancer care delivered and caregiver’s workforce performance. Support. Care Cancer 18, 699–706. doi: 10.1007/s00520-009-0668-5
Perndorfer, C., Soriano, E. C., Siegel, S. D., and Laurenceau, J. P. (2019). Everyday protective buffering predicts intimacy and fear of cancer recurrence in couples coping with early-stage breast cancer. Psycho-Oncology 28, 317–323. doi: 10.1002/pon.4942
Perndorfer, C., Soriano, E. C., Siegel, S. D., Spencer, R. M., Otto, A. K., and Laurenceau, J.-P. (2022). Fear of cancer recurrence and sleep in couples coping with early-stage breast cancer. Ann. Behav. Med. 56, 1131–1143. doi: 10.1093/abm/kaac018
Rincones, O., Smith, A. B., Naher, S., Mercieca-Bebber, R., and Stockler, M. (2021). An updated systematic review of quantitative studies assessing anxiety, Depression, Fear of Cancer Recurrence or Psychological Distress in Testicular Cancer Survivors. Cancer Manag. Res. 13, 3803–3816. doi: 10.2147/CMAR.S198039
Sawma, T., and Choueiri, P. (2022). The influence of family functioning on the severity of fear of cancer recurrence: a cross-sectional study in a sample of breast cancer survivors of Lebanese women. Eur. J. Oncol. Nurs. 60:102169. doi: 10.1016/j.ejon.2022.102169
Şengün İnan, F., and Üstün, B. (2019). Fear of recurrence in Turkish breast cancer survivors: a qualitative study. J. Transcult. Nurs. 30, 146–153. doi: 10.1177/1043659618771142
Shen, Z., Xie, J., Ruan, C., and Li, C. (2022). Mediating effect of ill perception on the relationship between social constraints and fear of cancer recurrence among adolescent and young adult survivors who underwent hematopoietic stem cell transplantation. Asia Pac. J. Oncol. Nurs. 9:100060. doi: 10.1016/j.apjon.2022.03.012
Shi, Y., Wu, Z., Wang, H., Kong, W., and Zhuansun, X. (2022). The influence of family-oriented enabling psychological nursing on posttraumatic stress and fear of recurrence in patients with cervical Cancer. Evid. Based Complement. Alternat. Med. 2022, 1–6. doi: 10.1155/2022/6720287
Shin, J., Shin, D. W., Lee, J., Hwang, J., Lee, J. E., Cho, B., et al. (2022). Exploring socio-demographic, physical, psychological, and quality of life-related factors related with fear of cancer recurrence in stomach cancer survivors: a cross-sectional study. BMC Cancer 22, 1–10. doi: 10.1186/s12885-022-09507-2
Simard, S., Savard, J., and Ivers, H. (2010). Fear of cancer recurrence: specific profiles and nature of intrusive thoughts. J. Cancer Surviv. 4, 361–371. doi: 10.1007/s11764-010-0136-8
Simard, S., Thewes, B., Humphris, G., Dixon, M., Hayden, C., Mireskandari, S., et al. (2013). Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J. Cancer Surviv. 7, 300–322. doi: 10.1007/s11764-013-0272-z
Singh-Carlson, S., Wong, F., Martin, L., and Nguyen, S. (2013). Breast cancer survivorship and south Asian women: understanding about the follow-up care plan and perspectives and preferences for information post treatment. Curr. Oncol. 20, 63–79. doi: 10.3747/co.20.1066
Soriano, E. C., Otto, A. K., LoSavio, S. T., Perndorfer, C., Siegel, S. D., and Laurenceau, J.-P. (2021). Fear of cancer recurrence and inhibited disclosure: testing the social-cognitive processing model in couples coping with breast cancer. Ann. Behav. Med. 55, 192–202. doi: 10.1093/abm/kaaa043
Soriano, E. C., Perndorfer, C., Otto, A. K., Siegel, S. D., and Laurenceau, J. P. (2018). Does sharing good news buffer fear of bad news? A daily diary study of fear of cancer recurrence in couples approaching the first mammogram post-diagnosis. Psycho-Oncology 27, 2581–2586. doi: 10.1002/pon.4813
Soriano, E. C., Perndorfer, C., Siegel, S. D., and Laurenceau, J.-P. (2019). Threat sensitivity and fear of cancer recurrence: a daily diary study of reactivity and recovery as patients and spouses face the first mammogram post-diagnosis. J. Psychosoc. Oncol. 37, 131–144. doi: 10.1080/07347332.2018.1535532
Starreveld, D. E., Markovitz, S. E., van Breukelen, G., and Peters, M. L. (2018). The course of fear of cancer recurrence: different patterns by age in breast cancer survivors. Psycho-Oncology 27, 295–301. doi: 10.1002/pon.4505
Steele, N., Haigh, R., Knowles, G., and Mackean, M. (2007). Carcinoembryonic antigen (CEA) testing in colorectal cancer follow up: what do patients think? Postgrad. Med. J. 83, 612–614. doi: 10.1136/pgmj.2007.059634
Subudhi, S. K. (2023) “What makes immunotherapy for prostate Cancer a promising treatment?”. Cancer Research Institute. Available at: cancerresearch.org/cancer-types/prostate-cancer Accessed: October 19, 2023.
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Thewes, B., Butow, P., Zachariae, R., Christensen, S., Simard, S., and Gotay, C. (2012). Fear of cancer recurrence: a systematic literature review of self-report measures. Psycho-Oncology 21, 571–587. doi: 10.1002/pon.2070
Thewes, B., Kaal, S. E. J., Custers, J. A. E., Manten-Horst, E., Jansen, R., Servaes, P., et al. (2018). Prevalence and correlates of high fear of cancer recurrence in late adolescents and young adults consulting a specialist adolescent and young adult (AYA) cancer service. Support. Care Cancer 26, 1479–1487. doi: 10.1007/s00520-017-3975-2
Thewes, B., Lebel, S., Seguin Leclair, C., and Butow, P. (2016). A qualitative exploration of fear of cancer recurrence (FCR) amongst Australian and Canadian breast cancer survivors. Support. Care Cancer 24, 2269–2276. doi: 10.1007/s00520-015-3025-x
Uner, F. O., and Korukcu, O. (2021). A qualitative exploration of fear of cancer recurrence in Turkish cancer survivors who were referred for colposcopy. Health Soc. Care Community 29, 729–737. doi: 10.1111/hsc.13326
van de Wal, M., Langenberg, S., Gielissen, M., Thewes, B., van Oort, I., and Prins, J. (2017). Fear of cancer recurrence: a significant concern among partners of prostate cancer survivors. Psycho-Oncology 26, 2079–2085. doi: 10.1002/pon.4423
Vrontaras, N. (2018). Cancer patients’ views on the family changes and the family social support. J. Eur. Psychol. Stud. 9:16. doi: 10.5334/jeps.403
Wijayanti, T., Afiyanti, Y., Rahmah, H., and Milanti, A. (2018). Fear of cancer recurrence and social support among Indonesian gynecological cancer survivors. Arch. Oncol. 24, 12–19. doi: 10.2298/AOO180201004W
Wu, L. M., McGinty, H., Amidi, A., Bovbjerg, K., and Diefenbach, M. A. (2019). Longitudinal dyadic associations of fear of cancer recurrence and the impact of treatment in prostate cancer patients and their spouses. Acta Oncol. 58, 708–714. doi: 10.1080/0284186X.2018.1563714
Xu, W., Wang, J., and Schoebi, D. (2019). The role of daily couple communication in the relationship between illness representation and fear of cancer recurrence in breast cancer survivors and their spouses. Psycho-Oncology 28, 1301–1307. doi: 10.1002/pon.5082
Yeung, N. C., and Lu, Q. (2022). Social constraints and fear of recurrence among Chinese American breast cancer survivors: an exploration of psychosocial mediators. Psycho-Oncology 31, 98–106. doi: 10.1002/pon.5784
Zheng, W., Hu, M., and Liu, Y. (2022). Social support can alleviate the fear of cancer recurrence in postoperative patients with lung carcinoma. Am. J. Transl. Res. 14, 4804–4811.
Keywords: fear of cancer recurrence, family caregiver, close relationships, communication, cancer survivors, cancer-related concerns
Citation: Faraji A, Dehghani M and Khatibi A (2023) Familial aspects of fear of cancer recurrence: current insights and knowledge gaps. Front. Psychol. 14:1279098. doi: 10.3389/fpsyg.2023.1279098
Edited by:
Rubén González-Rodríguez, University of Vigo, SpainReviewed by:
Spela Mirosevic, University of Ljubljana, SloveniaAna-María Rodriguez-Gonzalez, International University of La Rioja, Spain
Copyright © 2023 Faraji, Dehghani and Khatibi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Khatibi, bS5raGF0aWJpdGFiYXRhYmFlaUBiaGFtLmFjLnVr; YWxpLmtoYXRpYmlAZ21haWwuY29t
 Aida Faraji
Aida Faraji Mohsen Dehghani
Mohsen Dehghani Ali Khatibi
Ali Khatibi