- 1Department of Sociology, Changchun University of Science and Technology, Changchun, China
- 2School of Psychology, Northeast Normal University, Changchun, China
Introduction: Depression is primarily characterized by persistent low mood and cognitive dysfunction, whereas whereas alexithymia refers to difficulties in cognitively processing emotions. Although alexithymia being recognized as a risk factor for depression, there is no clear scholarly consensus on its exact role.
Methods: This investigation employs a meta-analytic random effects model to examine the relationship between alexithymia and depression. The analysis draws on data from 35 studies involving 23,085 individuals.
Results: Several key findings are revealed: Firstly, the total alexithymia score shows a positive correlation with depression severity, possibly influenced by cultural differences between Eastern and Western populations. Secondly, Difficulty in Describing Feelings (DDF) and Difficulty in Identifying Feelings (DIF) are significantly associated with depression, while Externally Oriented Thinking (EOT) has a weaker link. Thirdly, the relationship varies across different demographic groups and depends on the depression assessment tool used.
Discussion: These results emphasize the importance of examining not only the overall relationship between alexithymia and depression but also its specific dimensions. Additionally, the study explores the rational explanation of the interplay between alexithymia and depression within a Chinese cultural context and within the framework of the interpersonal theory of depression.
1 Introduction
Depression, from a medical standpoint, is a debilitating mental and physical condition characterized by persistent low mood and cognitive dysfunction. It profoundly affects an individual’s social functioning and ranks among the most common mental disorders (Rock et al., 2014). The recurrence rate of depressive disorders is notably high, ranging from 50 to 85%, with relapses occurring within 2 years of initial onset. The lifetime prevalence rate of depressive disorders among adults is approximately 6.8%. In addition to severe social impairments, depression imposes a significant economic burden (Trautmann and Wittchen, 2016; Tran et al., 2018). Global estimates suggest that treatment costs could reach nearly US$16 trillion by 2030, positioning depression as the fourth highest global burden of disease, as recognized by the World Health Organization (Bloom et al., 2011; Patel et al., 2018).
Alexithymia, often described as “inability to express emotions” or “affective dysphoria” (Sifneos, 1973), refers to an individual’s difficulty in recognizing and expressing their own or others’ emotions. It reflects deficiencies in the cognitive processing of emotions, impairing social–emotional communication, such as empathy, and leading to impaired social functioning (Wingbermühle et al., 2012). The Toronto Alexithymia Scale (TAS Scale), a widely used self-reported assessment tool, is commonly employed for its evaluation (Fujiwara, 2018). Alexithymia, considered a stable personality trait, is characterized by difficulty in identifying personal emotions (Difficulty in Identifying Feelings - DIF), differentiating emotions from somatic sensations (Difficulty in Describing Feelings - DDF), and displaying limited emotional imagination alongside an externally oriented cognitive style (Externally Oriented Thinking - EOT) (Taylor et al., 1999; Kooiman et al., 2002). Research shows that individuals from Eastern collectivist cultures may experience greater challenges with alexithymia. Unlike Western individualistic cultures (IDV), Eastern collectivist cultures (COL;see Gelfand et al., 2004; Hofstede, 2011) are rooted in Confucian values, which place a strong emphasis on emotional regulation (Butler et al., 2007; Dere et al., 2013). Deficits in emotional regulation play a key role in this issue (Marroquín, 2011).
Scholars have emphasized the need to investigate risk factors or determinants influencing depression, as this can inform preventive strategies aimed at reducing the likelihood of developing such mental disorders, thereby enhancing public mental health (Guan et al., 2022). One high-risk factor receiving increased attention is alexithymia (Hou et al., 2024); however, the current understanding of the relationship between them remains subject to debate.
1.1 The relationship between alexithymia and depression
Some scholars advocate that alexithymia influences depression, positing it as susceptible to and potentially influential in the development of depression (Van Der Cruijsen et al., 2019). Numerous studies have highlighted a potential correlation between total alexithymia scores and depression (Kenangil et al., 2020; Farhoumandi et al., 2022; Shi et al., 2022; Koppelberg et al., 2023), suggesting alexithymia as a predisposing factor for psychiatric disorders, particularly depression (Kinnaird et al., 2019). Meta-analytic evidence from Li et al. (2015) further supports this assertion, revealing a moderate correlation (r = 0.459) between total alexithymia scores and depression severity across a sample of 3,572 subjects from 19 Western studies.
Conversely, some scholars contest the association between alexithymia and depression. Some studies find that the two failed to establish a significant correlation in smokers and extremely obese individuals (Grabowska et al., 2005; Da Ros et al., 2011), while others report correlation coefficients below Cohen’s (1988) threshold for meaningfulness (Reker et al., 2010; Luca et al., 2013). Despite efforts to elucidate the relationship, dissenting views persist. Barbasio et al. (2015) found no significant correlation between alexithymia, depression, and illness perception among 100 patients with Systemic Lupus Erythematosus (SLE). Recent research in the autism community also indicates no impact of alexithymia on depression (Oakley et al., 2022).
Given the notable challenges associated with alexithymia in East Asian cultures, the present study examines both Western and Eastern cultural contexts. Numerous theorists have argued that the two cultures exhibit distinct differences in cultural beliefs, norms, and values, which may influence individuals’ abilities to identify and communicate emotions (e.g., Markus and Kitayama, 1994). Building on this foundational research, the current study proposes H1: There is a significant correlation between total alexithymia scores and depression, with potential differences in the correlation between Eastern and Western cultural settings.
1.2 There are differences in the effects of alexithymia factors on depression
While scholars recognize alexithymia as a risk factor for depression, considerable debate persists regarding the specific effects of its constituent factors. Difficulty Identifying Feelings (DIF) Factor: Empirical evidence, including a follow-up study involving 4,431 individuals from Northern Finland, highlights DIF as notably associated with depression (Ramzi et al., 2023). De Berardis et al. (2008) asserted DIF as the primary predictor of depression based on a study of medication-naive patients with Major Depression (MD). Similarly, in Korean depressed patients, measures of alexithymia and stress response patterns corroborated the significant correlation between DIF and depression (Kim et al., 2009). Nonetheless, conflicting findings emerge, as some studies fail to establish a significant correlation between DIF and depression (He et al., 2022).
Difficulty Describing Feelings (DDF) Factor: In contrast to De Berardis et al. (2008) and Leweke et al. (2011) found a significant correlation between the DDF factor and depression. Intriguingly, while DIF and Externally Oriented Thinking (EOT) were not correlated with depression, DDF emerged as a potential discriminatory feature of depression. Externally Oriented Thinking (EOT) Factor: Although several studies report no correlation between EOT and depression severity (Marchesi et al., 2008; Bamonti et al., 2010; Son et al., 2012), Saarijärvi et al. (2006) observed unaltered EOT scores during a longitudinal study of outpatients with Major Depressive Disorder. However, recent evidence suggests a significant positive association between EOT and depression in cancer patients (Ozonder Unal and Ordu, 2023).
In light of these findings, this study proposes H2: alexithymia and depression may exhibit inconsistencies, with weakly correlated or uncorrelated alexithymia factors potentially existing.
1.3 Impact of additional variables on the alexithymia-depression relationship
Furthermore, demographic variables such as subject group, gender, depression measurement tools, and publication age of literature may influence the correlation between alexithymia and depression.
1.3.1 Subject group
The prevalence of alexithymia varies across community and clinical samples, highlighting the role of subject group in its association with depression. Populations with psychological or somatic disorders, such as autism, Parkinson’s disease, and sleep disorders, show particularly high rates of alexithymia. Notably, the incidence of alexithymia may reach up to 55% among autistic adolescents (Milosavljevic et al., 2016). This suggests that the elevated prevalence of alexithymia in these groups may impact the extent to which alexithymia predicts depression. Hence, this study posits H3: Different subject groups affect the conclusion regarding the correlation between alexithymia and depression.
1.3.2 Gender factors
Gender plays a complex role in alexithymia and its association with depression. While some studies suggest higher mean scores of alexithymia in males, others dispute gender differences. Nonetheless, the female gender is prominently associated with depression due to various biological, psychological, and social factors. Therefore, this study proposes H4: Gender factors influence the association between alexithymia and depression.
1.3.3 Depression measurement tools
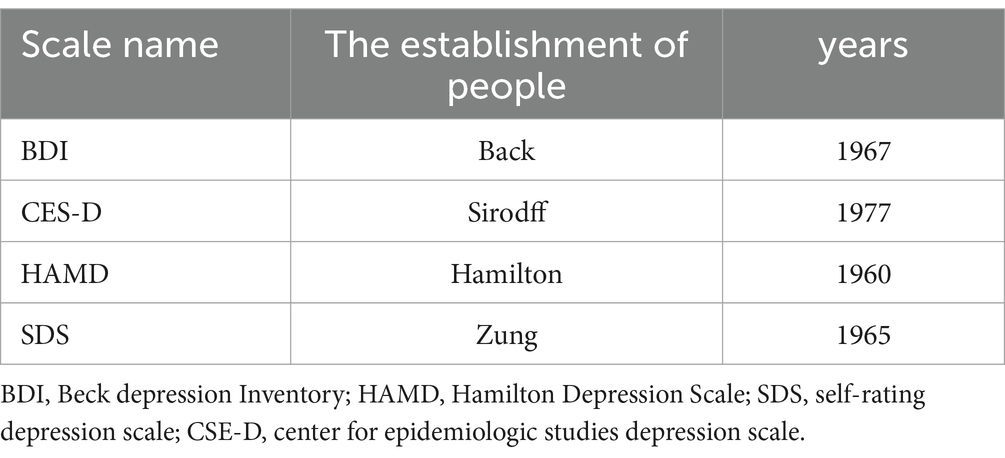
Inconsistencies in the alexithymia-depression relationship may stem from differences in depression measurement tools. Given the variety of tools employed in academia, including self-report measures and clinician-administered scales, the choice of tool may affect the observed correlation (see Table 1).
Although all these scales have passed the measurement methodology test, there are differences in the applicable groups, assessment methods, and scoring methods, which may impact the study results. Firstly, the Hamilton Depression Rating Scale (HAMD) was utilized in patients with depression to evaluate illness severity, while the remaining instruments were commonly employed in the general population to screen for symptoms. Secondly, the Beck Depression Inventory (BDI), Center for Epidemiologic Studies Depression Scale (CES-D), and Self-Rating Depression Scale (SDS) are self-report measures, whereas the HAMD is an observer-rated measure administered by trained personnel. Thirdly, regarding the scoring method: the HAMD employs a 3- or 5-point scale based on severity, while the other scales use 4-point scales, albeit with subtle variations. For instance, the BDI assesses severity, while the SDS and CES-D measure time-frequency. Additionally, considering that the literature in the meta-analysis encompasses both Chinese and foreign languages, equivalence across five systematic assessment aspects—content, semantics, methodology, norms, and constructs—must be considered in cross-cultural research, as recommended by Flaherty et al. (1988).
Consequently, this study posits H5: Different depression measurement tools may influence the correlation between alexithymia and depression.
1.3.4 Publication year
It may also potentially affect the correlation between depression and alexithymia. Prior studies have affirmed the increasing prevalence of depression in the general population, partly attributed to evolving societal dynamics that exacerbate stressors leading to depression. Conversely, heightened societal awareness of mental illnesses, including depression, has fostered open discussions in recent years, thereby enhancing recognition and acknowledgment of depression. However, it is noteworthy that literature also indicates stable depression trends, underscoring relevant changes in depression over time.
Thus, this measure of publication year tests the hypothesis that the correlation between alexithymia and depression has changed over time, with the expectation of H6 that more recent studies would find a stronger correlation.
2 Methods
2.1 Literature search and selection
Sterne et al. (2011) emphasized the pivotal role of a systematic and exhaustive literature search preceding meta-analysis in mitigating publication bias, advocating for proactive measures over post hoc analyses. In line with this principle, our study meticulously scrutinized both Chinese and English literature spanning the East and West over a continuous period of 22 years (2001–2023). For English sources, we utilized Web of Science, PubMed, and Google Scholar, employing the search terms “Alexithymia” and “depression.” Additionally, to enhance our understanding of the evolving relationship between alexithymia and depression, we incorporated longitudinal studies specifically focusing on “follow-up duration,” “longitudinal.” Chinese databases such as China National Knowledge Infrastructure, China Science and Technology Journal Database, and Wan-fang database were queried using equivalent Chinese terms.
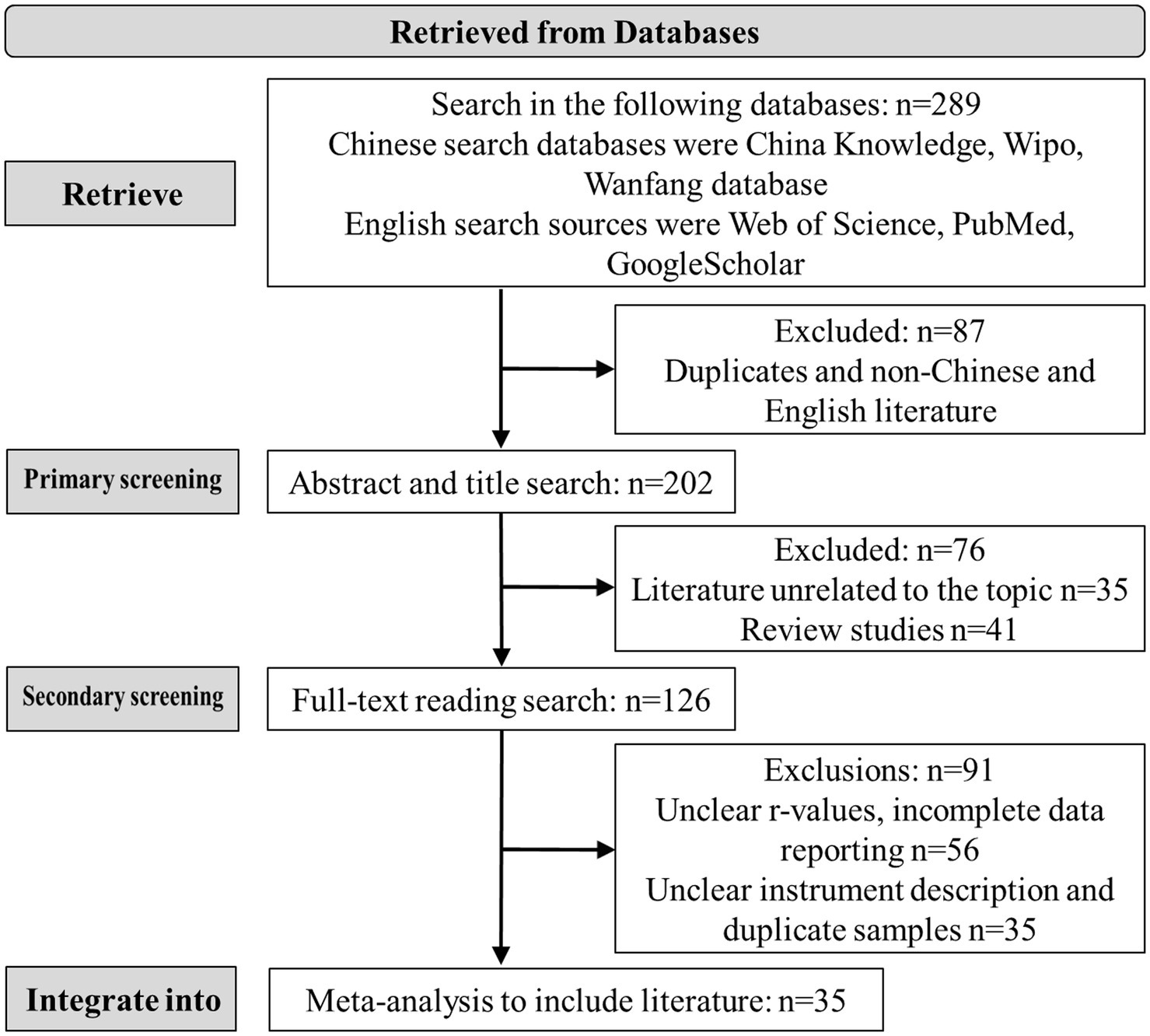
Following the PRISMA statement guidelines (Moher et al., 2009), we meticulously screened the identified literature based on the following criteria: (1) inclusion of quantitative empirical studies elucidating the correlation between alexithymia and depression, (2) provision of descriptions regarding the instruments employed to assess alexithymia and depression, (3) independence of studies, excluding those with overlapping samples or duplications, (4) exclusion of studies deemed low quality (scoring 0–3 points), and (5) clarity on sample sizes. To ensure comprehensiveness, we conducted a secondary search within the references of retrieved articles (see Figure.1).
2.2 Literature quality assessment and coding
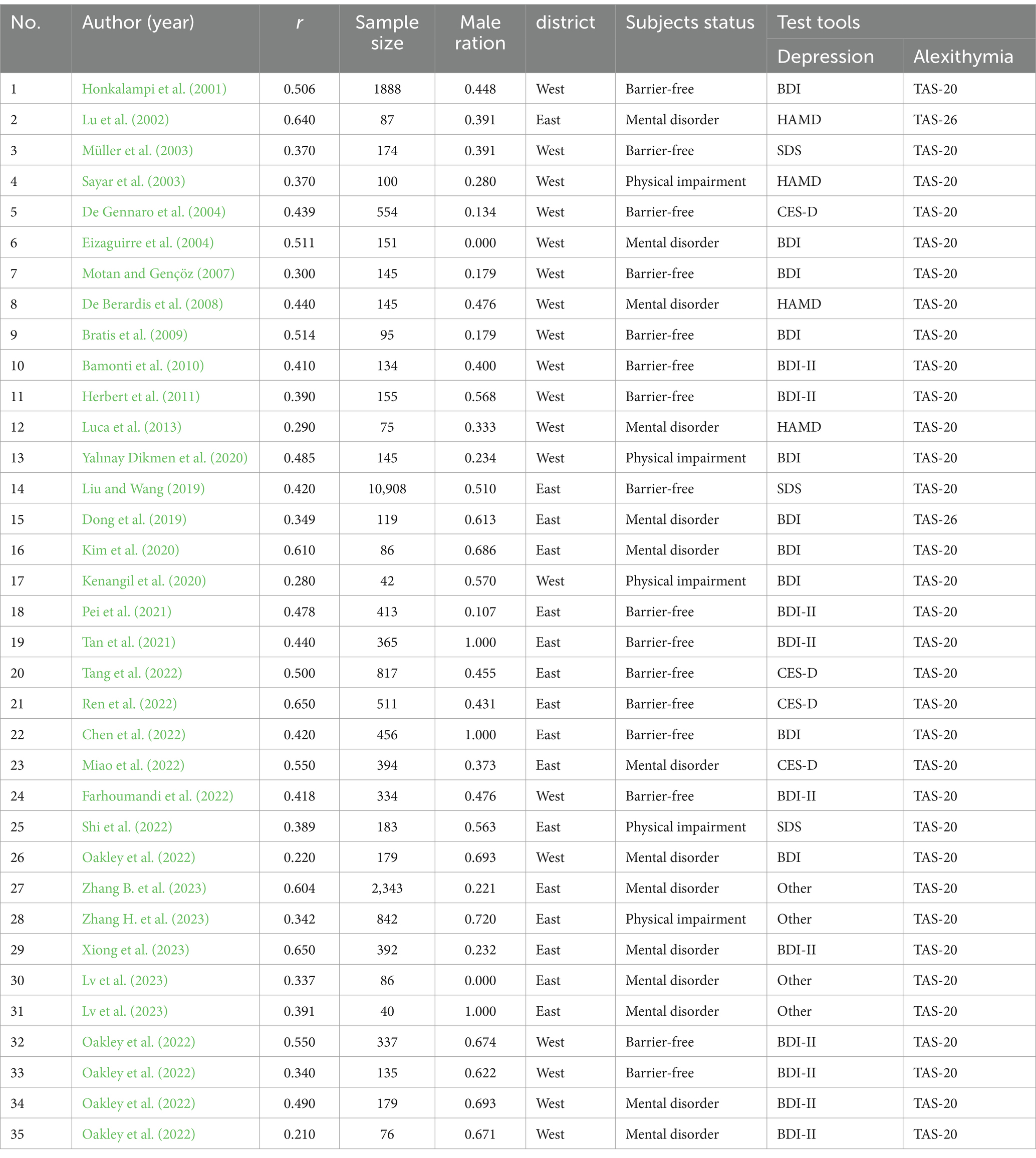
The Meta-Analysis Assessment Scale, as devised by Boyle (1998), was employed for systematic evaluation, encompassing sample representativeness, measurement tool validity, and analytical results across eight criteria. Each assessor independently conducted the assessment, assigning scores ranging from 0 to 8, wherein scores falling within 0 to 3 denoted low quality, 4 to 6 indicated moderate quality, and a score of 7 or higher signified high quality. The inter-rater agreement, measured by the Kappa coefficient, yielded a value of 0.84, suggesting substantial concordance between assessors, as per Orwin and Vevea’s (2009) classification, where values exceeding 0.75 denote very good agreement (specifically: 0.40 to 0.59 for fair, 0.60 to 0.74 for fairly good, and 0.75 and above for very good agreement). This study encompasses 35 investigations, with sample sizes ranging from 40 to 10,908, totaling 23,085 participants, of whom female representation exceeds 53.2%. The descriptive information for each study is shown in Table 2.
2.3 Data processing
This study utilized Pearson’s product-difference correlation coefficient (r) between alexithymia and depression as the effect size indicator, favored for its advantages over alternative measures (Rosenthal and DiMatteo, 2001). Potential publication bias was evaluated using funnel plots in CMA 3.3 (Comprehensive Meta-Analysis Version 3.3) and the Egger regression test. Specifically, a symmetrical funnel plot suggests an absence of publication bias, while non-significant results from the Egger regression imply negligible bias (Egger and Smith, 1998; Viechtbauer, 2007).
Furthermore, Cochran’s Q test with the I2 statistic was employed to gauge heterogeneity among studies, where I2 = 100% × (Q-df)/Q (df representing degrees of freedom). As per Higgins et al. (2003), an I2 value exceeding 75% indicates substantial heterogeneity, justifying the use of a random effects model for meta-analysis. Given the inclusion of diverse subject groups from both Eastern and Western contexts, and in line with Quintana’s (2015) recommendation, the random effects model was adopted.
Additionally, this study conducted subgroup analyses and meta-regression to explore potential moderators influencing heterogeneity. These analytical methods, deemed indispensable for meta-analyses, were employed to investigate factors contributing to variation (Lee et al., 2022).
Following Card’s (2012) criteria, each moderator variable required a minimum of five representative effect sizes for analysis. Finally, sensitivity analyses were performed to ensure the robustness of the meta-analytic findings, mitigating the influence of small sample size studies or literature not entirely meeting the screening criteria (Li et al., 2018).
3 Results
3.1 Publication Bias and heterogeneity test
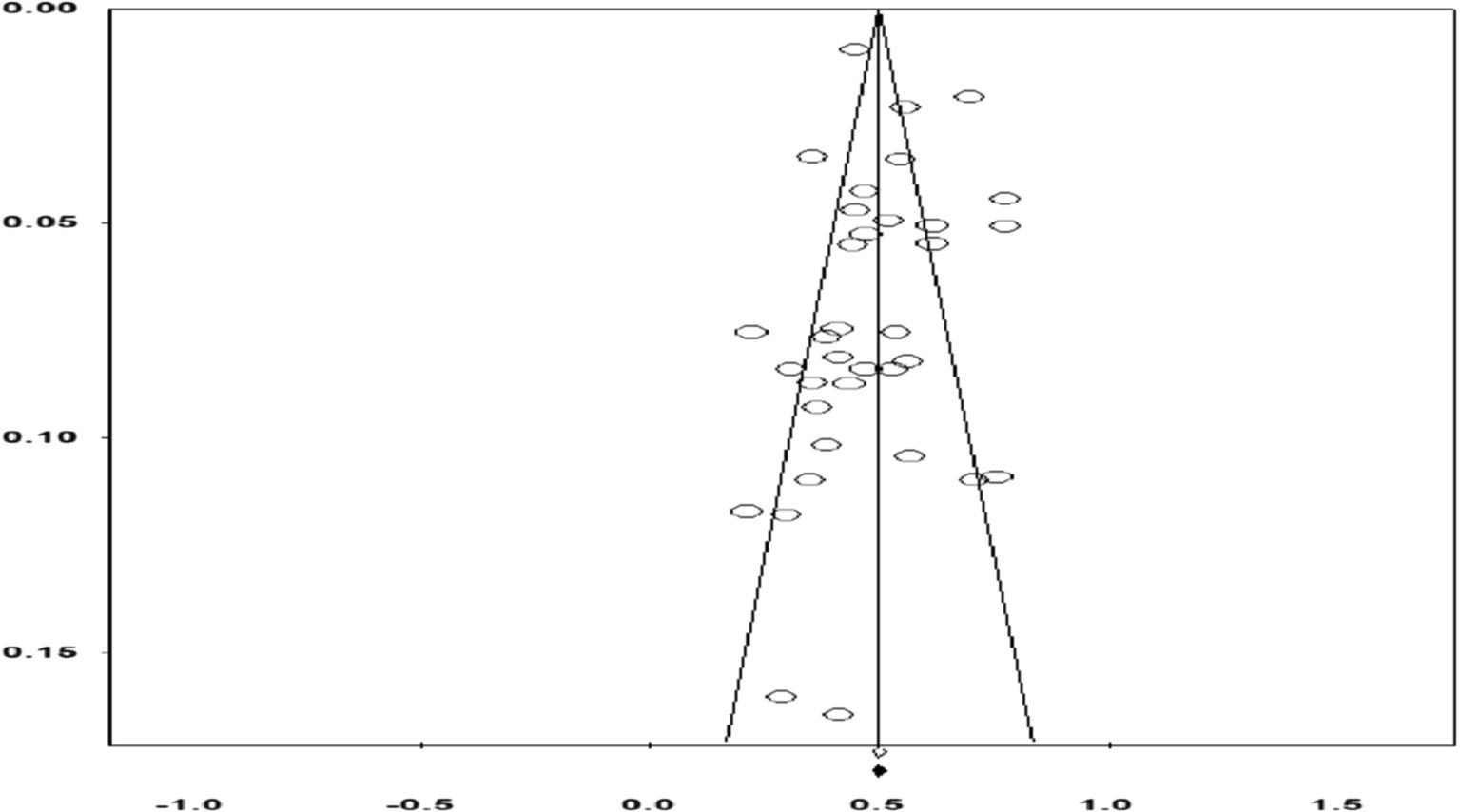
Firstly, examination of the funnel plot revealed a concentration of effect sizes in the upper-middle section, evenly distributed on either side of the overall effect, forming a symmetrical funnel shape (Figure 2). Subsequently, Egger’s test indicated no statistically significant publication bias, yielding β = 0.045, p = 0.951, with a 95% CI = [−1.441, 1.532]. Following guidelines by Higgins et al. (2019), no evidence of publication bias was observed.
Secondly, to assess heterogeneity among included effect sizes and validate the selection of the random effects model, this study conducted a comprehensive analysis. The results demonstrated a significant departure from the null hypothesis (Z = 75.933, p < 0.001), alongside Cochrane’s Q statistic of 283.226 with 34 degrees of freedom, yielding p < 0.001, and an I2 value of 87.995%, exceeding the threshold of 75% proposed by Higgins et al. (2003). This substantial level of heterogeneity indicates that variations in effect sizes concerning the relationship between alexithymia and depression across the literature are not merely attributed to chance but likely reflect genuine underlying factors. Consequently, employing a random effects model is deemed appropriate, necessitating subsequent meta-regression and subgroup analyses to delve deeper into potential contributors to study heterogeneity.
3.2 Correlation test between alexithymia TAS Total score and depression
The Project 35 study revealed a significant association between total TAS scores for alexithymia and depression, encompassing 23,085 participants. Employing a random-effects model, the overall effect size was r = 0.455, with a 95% CI = [0.417, 0.491], across 35 studies. Individual study effect sizes ranged from 0.313 to 0.462, all indicating positive correlations. Sensitivity analyses, excluding the smallest sample size studies (n = 40), resulted in an adjusted overall effect size of r = 0.456, 95% CI = [0.417, 0.492], across 34 studies, indicating a stable association. Cohen’s (1988) conventions classify correlations of r = 0.10, r = 0.30, and r = 0.50 as weak, moderate, and high, respectively. In this study, the association between alexithymia TAS total scores and depression ranged from moderate to high correlations. Notably, Gignac and Szodorai (2016) suggested that an r = 0.30 could be considered highly correlated in meta-analytic contexts, thereby characterizing the present study’s findings as demonstrating a highly positive correlation between total TAS score of alexithymia and depression. Additionally, sensitivity analyses excluding either sample yielded consistent results, suggesting a stable association.
Furthermore, the study investigated the influence of cultural background factors through subgroup analyses. Firstly, employing a random effects model for Eastern cultural background revealed an overall effect size of r = 0.498, 95% CI = [0.438, 0.553], across 16 studies, with significant heterogeneity observed (Q = 231.949, df = 15, p < 0.001; I2 = 93.533%). Sensitivity analyses, excluding studies with the smallest sample size, yielded an adjusted overall effect size of r = 0.501, 95% CI = [0.440, 0.557], across 15 studies, indicating a slight increase in association. Secondly, the random effects model for Western cultural background yielded an overall effect size of r = 0.416, 95% CI = [0.371, 0.460], across 19 studies, with indications of substantial heterogeneity (Q = 50.384, df = 18, p = 0.001; I2 = 64.274%). Sensitivity analyses, excluding the smallest sample size study, yielded a consistent overall effect size of r = 0.406, 95% CI = [0.359, 0.450], across 18 studies. Notably, confidence intervals for overall effect sizes varied considerably between cultural contexts, suggesting differing correlations between alexithymia and depression in Eastern and Western cultures, with a potentially higher correlation observed in Eastern cultures.
3.3 Correlation test between alexithymia sub-dimensions and depression
To investigate whether TAS subscales contribute to heterogeneity in the alexithymia-depression association, subgroup analyses of TAS subscales were conducted involving 7,885 participants across 30 studies (see Supplementary material). Visual inspection of funnel plots revealed symmetrical distributions, and Egger’s test indicated non-significant publication bias [β = 1.617, p = 0.117, 95% CI = (−0.430, 3.665)]. Firstly, random effects model results for DDF subscale subgroup analysis exhibited a moderate correlation, with a mean effect size of r = 0.331, 95% CI = [0.268, 0.391], across 30 studies. Significant inter-study heterogeneity was observed (Q = 232.862, df = 29, p < 0.001; I2 = 87.546%). Secondly, subgroup analysis focusing on DIF subscales showed a mean effect size of r = 0.411, 95% CI = [0.357, 0.463], across 30 studies, indicating a moderate correlation. However, substantial and significant inter-study heterogeneity was noted (Q = 194.679, df = 29, p < 0.001; I2 = 85.104%).
Conversely, EOT subscale analysis revealed a weak correlation with depression, with a mean effect size of r = 0.120, 95% CI = [0.080, 0.159], across 30 studies. Heterogeneity between studies was evident (Q = 69.015, df = 29, p < 0.001; I2 = 57.980%). Thus, differences were observed in the associations between TAS subscales and depression. While DDF and DIF showed moderate correlations, EOT exhibited a weak correlation, suggesting a minimal contribution. This finding supports H2.
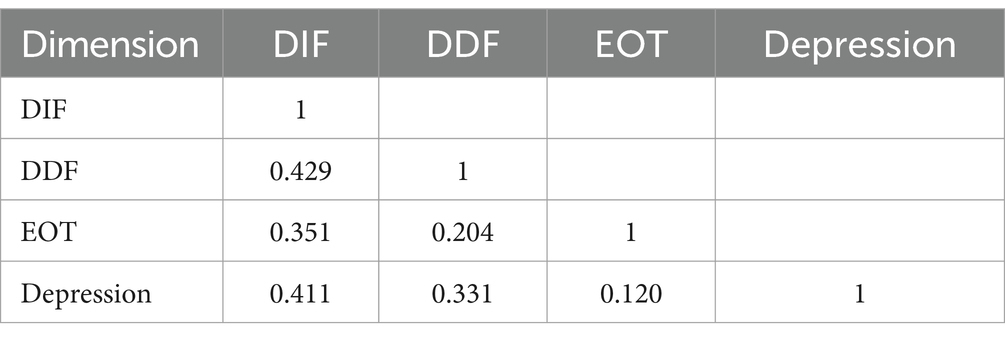
Moreover, this study employed meta-analytic structural equation modeling to explore TAS subscales’ role in the alexithymia-depression association. A correlation matrix for structural equation modeling was derived from 14 studies providing correlation coefficients between DDF, DIF, EOT, and depression. A reconciled mean was utilized to obtain observations for the structural variance model (N = 245.388) (see Table 3).
The results of the model fit showed a moderate fit with χ2 = 3.820, df = 2, CFI = 0.982, TLI = 0.946, RMSEA = 0.069 [90% CI = 0.000, 0.186], SRMR = 0.033. The results indicated a significant association between the alexithymia latent variable and depression (ρ = 0.504, p < 0.001), providing supporting evidence for the association between alexithymia and depression. The factor loadings for DIF, DDF, and EOT were all significant (ps < 0.001), but EOT explained the least amount of variance (R2 = 0.158), less than 20%, compared to DIF (R2 = 0.670) and DDF (R2 = 0.293), which explained more than 25% of the variance. This result once again highlights the relatively weak contribution of EOT (see Figure 3).
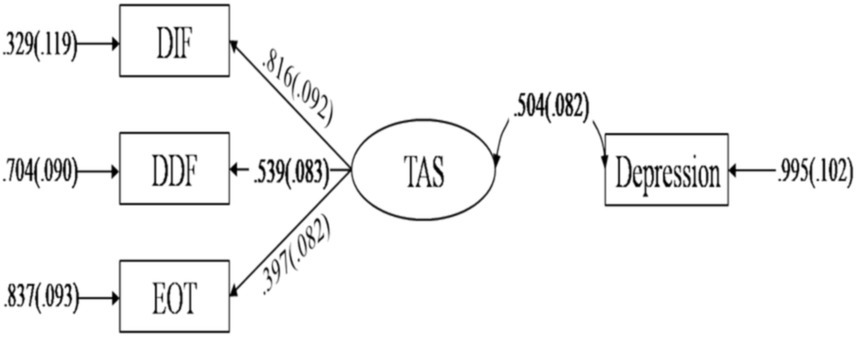
Figure 3. Meta-analytical structural equation model for the relationship between TAS subscales and depression.
3.4 Moderating effects test
To explore potential moderator variables affecting the relationship between alexithymia and depression, subgroup analyses and meta-regression were conducted. Subgroup analyses investigated the influence of group type and heterogeneity of measurement instruments. Notably, significant between-study heterogeneity by group type was observed (Q = 9.999, df = 2, p = 0.007), supporting Hypothesis 3. For the mental disorders group, an overall effect size of r = 0.470, 95% CI = [0.393, 0.540], across 15 studies, exhibited substantial heterogeneity (Q = 95.533, df = 14, p < 0.001; I2 = 85.345%). Similarly, the no-impairment group showed an overall effect size of r = 0.461, 95% CI = [0.419, 0.501], across 15 studies, with significant heterogeneity (Q = 87.892, df = 14, p < 0.001; I2 = 84.071%). Conversely, the physically impaired group displayed no heterogeneity in the overall effect size, r = 0.366, 95% CI = [0.315, 0.414], across 5 studies (Q = 4.171, df = 4, p = 0.383; I2 = 4.098%). Notably, confidence intervals for the no-impairment and physical-impairment groups did not overlap, suggesting greater relevance of the former.
Additionally, confidence intervals for the mental-impairment and physical-impairment groups had a noticeable gap with slight overlap, implying the former’s likely greater relevance. Furthermore, neither the depression measurement tool (Q = 6.892, df = 5, p = 0.229) nor the alexithymia measurement tool (Q = 0.031, df = 1, p = 0.861) appeared to significantly contribute to heterogeneity between studies, thus Hypothesis 5 was not supported. Therefore, different measurement instruments for depression and alexithymia did not significantly influence the relationship. Information of subgroup comparisons is shown in Table 4.
In addition, publication year and sex ratio were treated as continuous predictor variables in a meta-regression analysis to explore their potential impact on the heterogeneity of results. The results indicated a non-significant regression for sex ratio [β = −0.139, SE = 0.086, Z = −1.61, p = 0.107, 95% CI (−0.307, 0.030)], thus failing to support Hypothesis 4. Similarly, publication year did not explain a significant portion of the variability in effect size [β = 0.001, SE = 0.003, Z = 0.26, p = 0.792, 95% CI (−0.006, 0.007)], indicating that the association between alexithymia and depression has remained stable over time and thereby failing to support Hypothesis 6.
4 Discussion
4.1 Effects of alexithymia on depression
Alexithymia, recognized as a vulnerability for depression, is notably shaped by cross-cultural dynamics. Individuals from Eastern cultures tend to exhibit higher levels of alexithymia compared to those from Western cultures (Dion, 1996; Le et al., 2002). This discrepancy likely arises from cultural variations in attitudes towards individualism and the expression of inner feelings, rather than biological factors or differences in cognitive abilities. Rooted in Confucian principles, Chinese culture places emphasis on virtues and social obligations (Yao, 2000). Unlike Western societies, East Asian cultures prioritize emotional restraint over the exploration and outward expression of emotions (Butler et al., 2007; Dere et al., 2013). Therefore, understanding the relationship between alexithymia and depression requires careful consideration of cross-cultural factors. While previous meta-analyses have primarily focused on Western literature, our study aims to incorporate a broader range of literature from Eastern cultural backgrounds to provide a more comprehensive perspective on this relationship.
Furthermore, culture itself may act as a potential risk factor for certain mental health conditions, including depression, which can be influenced by environmental factors. Confucian societies tend to exhibit higher levels of depression indicators and lower resilience scores among adolescents compared to European societies, with significant disparities noted. These societies often uphold stricter standards, potentially contributing to heightened levels of anxiety and self-doubt among Asian students (Stankov, 2010). Existing research highlights a connection between Confucian personality traits, particularly moderate thinking, and emotional relationships in Chinese culture. The doctrine of the mean, central to Confucian ideal personality, promotes a balanced approach in behavior and interpersonal interactions, restricting emotional expression and potentially exacerbating negative emotions, thus increasing the risk of depression (Ma et al., 2015). Additionally, individuals with alexithymia experience difficulties in processing and regulating emotions, which can predispose them to psychological issues such as depression (Preece et al., 2022), as supported by numerous studies (Kenangil et al., 2020; Farhoumandi et al., 2022; Shi et al., 2022).
In the extended process theory of emotion regulation, Gross (2015) highlights that emotion identification is pivotal for adaptive emotion regulation. Individuals with alexithymia often face challenges in recognizing and articulating their feelings. Previous studies have demonstrated their struggle in regulating negative emotions or their correlation with negative emotions (De Gucht et al., 2004; Yelsma, 2007). This difficulty may consequently exacerbate depression or lead to heightened levels of depression as negative emotions accumulate.
Our study revealed varying correlations between Toronto Alexithymia Scale (TAS) sub-dimensions and depression. Difficulty Identifying Feelings (DIF) showed the strongest correlation, followed by Difficulty Describing Feelings (DDF), while Externally Oriented Thinking (EOT) exhibited the lowest correlation. This aligns with findings by De Gucht et al. (2004), who emphasized DIF as a significant predictor of depression levels. Despite EOT showing a weaker correlation, it remains relevant in understanding depression and alexithymia. Cohen (1988) warned against dismissing small effects, as they can still be meaningful. Previous research indicated that high EOT scores in depressed patients are linked to concrete thinking and poor introspection, associated with cognitive deficits and psychomotor retardation (De Berardis et al., 2008; Tominaga et al., 2014). Moreover, the reliability issue of EOT intersects with cultural differences, underscoring the need to consider linguistic and cultural contexts in assessment tools.
Our findings indicate a significant moderating effect of the tested group on the relationship between depression and alexithymia, particularly within the mental disorders group. This supports previous studies emphasizing the role of psychological factors in alexithymia (Obeid et al., 2020). Theory of Mind (ToM), or mentalizing, involves understanding one’s own and others’ mental states to predict and explain behaviors (Moriguchi et al., 2006). Individuals with high alexithymia levels often struggle with ToM, leading to difficulties in social interactions and relationships (Demers and Koven, 2015). Moreover, evidence indicates that individuals with alexithymia exhibit a limited response to psychotherapy (Ogrodniczuk et al., 2005). For instance, individuals with high levels of alexithymia on the autism spectrum often face challenges in recognizing emotions conveyed through facial expressions, vocal intonations, and musical cues (Allen and Heaton, 2010). Consequently, these individuals may have unique needs that necessitate specific interventions and could benefit from tailored therapeutic approaches (Kinnaird et al., 2019).
The study highlighted the potential interference of depression measurement tools with the effect of alexithymia on depression. This interference may arise from differences in scoring methods, target groups, assessment approaches, and scale items across various scales, leading to potential inaccuracies in information and resulting in varied final correlations. Notably, variations in total scores and prevalence of depressive symptoms among different scales may be due to their distinct focuses in assessing depressive symptoms. For example, the CES-D primarily measures depressive symptom levels within the general population over the current week, emphasizing affective components and depressive states (Radloff, 1977). In contrast, the BDI-II-C assesses the severity of depressive symptoms concerning clinical diagnosis. Additionally, depression scales often originate from foreign sources, raising concerns about equivalence across dimensions such as content, semantics, methodology, norms, and conceptualization, as noted by Flaherty et al. (1998) in cross-cultural research contexts.
Regarding gender and publication year, the study did not find significant differences in the current effect of alexithymia on depression. Previous findings on gender differences in alexithymia have varied. Levant et al. (2006) observed higher alexithymia scores among males in some studies, while others reported higher scores among females or no significant differences. Our study aligns with the latter trend. Levant et al. (2006) reviewed multiple studies and noted that while gender differences in alexithymia were generally insignificant in clinical samples, males tended to score higher in non-clinical samples. The absence of gender differences in clinical samples might be attributed to emotion recognition and expression processes in men seeking psychotherapy. Additionally, it has been suggested that the etiology or pathogenesis of alexithymia differs between genders and may be influenced by traumatic experiences, leading to variations in neuroendocrine functioning, which itself differs between males and females (Spitzer et al., 2005). Consequently, future research on gender differences in alexithymia warrants a more comprehensive approach. Conversely, the non-significance of publication year suggests that alexithymia may not only serve as a risk factor for depression but also persist as a stable personality trait (Hemming et al., 2019), resistant to change over shorter periods.
4.2 Limitations and implications
This study delves into the correlation between narrative affective disorder and depression, alongside its influencing factors. However, it also highlights some limitations. Firstly, the reviewed literature mainly employed the TAS scale to measure narrative affective disorder. While efficient, the TAS-20 may not accurately capture the extent of dysphoria within a sample. Individuals with heightened narrative dysphoria may struggle to reliably assess their deficits using self-report scales (Taylor and Bagby, 2013). To address this limitation, some scholars have suggested using clinician-rated instruments like the Toronto Structured Interview for Narrative Disorders (Bagby et al., 2005). However, these tools have their own constraints, including high costs, the need for interviewer training, reliance on interviewer quality, and uncertainties surrounding interview outcomes (Cameron et al., 2014). Individuals with elevated levels of dysarthria and those with Autism Spectrum Conditions (ASC) may encounter difficulties in self-awareness and articulating aspects of themselves (Griffin et al., 2016), potentially leading to underestimation of dysgraphia (and ASC). It has been proposed that the efficacy of the BVAQ-40 could be enhanced. The BVAQ-40, an alternative instrument to the TAS-20, is commonly used to evaluate the cognitive and affective dimensions of affective disorders (Goerlich and Aleman, 2018). However, the assertion regarding an affective component within narrative affective disorders remains subject to scholarly debate (Bagby et al., 2007; Preece et al., 2017; Goerlich, 2018). Therefore, future research should acknowledge this debate and explore methodologies for measuring dysarthria that do not solely rely on self-insight (Bird and Cook, 2013).
Secondly, regarding the subject group, this study noted that individuals with mental disorders exhibited the highest effect sizes. However, it overlooked the extent of dysphoria within this subgroup, potentially underestimating the significance of co-occurring dysphoria as a critical risk factor. This conclusion requires further validation through a comprehensive integration of subgroups based on their individual levels of dysphoria. Moreover, prior research indicates that socio-demographic variables such as gender, age, and education level may independently or jointly influence the association between dysphoria and depression severity (Mattila et al., 2006; Kim et al., 2009; Luca et al., 2013). These relationships warrant further exploration.
Lastly, considering that this study collected data from multiple countries within the North America-East Asia dichotomy, we employed the Individualism–Collectivism (IDV-COL) cultural dimension to examine the cultural impact on the correlations between alexithymia and depression. The IDV-COL dimensions demonstrate robust reliability and validity (Minkov et al., 2018). However, this research has limitations. While the IDV-COL framework provides valuable insights into overarching cultural influences, it does not fully capture the complexities of intra-cultural variations that can significantly shape emotional perception and expression. Specifically, cultural groups may exhibit diversity in emotional processes based on factors such as regional traditions and collective experiences (Mesquita, 2001; Mesquita and Walker, 2003; Tsai and Levenson, 1997). Consequently, the failure to account for these intra-cultural nuances may limit the generalisability of our findings.
5 Conclusion
Using a meta-analytic approach, this study established significant correlations between total scores of affective disorders and depression. Specifically, Difficulty Identifying Feelings (DIF) and Difficulty Describing Feelings (DDF) showed strong correlations with depression, while Externally Oriented Thinking (EOT) exhibited a weaker correlation.
The correlation between depression and dysphoria was notably influenced by the characteristics of the group under investigation and the depression measurement tool, with no apparent impact from gender or publication age. These findings contribute to the theoretical understanding of trait inference in depression and may have implications for social cognitive research in clinical disorders.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ZL: Formal analysis, Methodology, Software, Writing – original draft. SH: Data curation, Investigation, Writing – original draft. CH: Funding acquisition, Project administration, Supervision, Writing – review & editing, Conceptualization, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by “Humanity and Social Science Research Project of Ministry of Education of China (22YJA190002)”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1465286/full#supplementary-material
References
Allen, R., and Heaton, P. (2010). Autism, music, and the therapeutic potential of music in alexithymia. Music. Percept. 27, 251–261. doi: 10.1525/mp.2010.27.4.251
Bagby, R. M., Taylor, G. J., Parker, J. D., and Dickens, S. E. (2005). The development of the Toronto structured interview for alexithymia: item selection, factor structure, reliability and concurrent validity. Psychother. Psychosom. 75, 25–39. doi: 10.1159/000089224
Bagby, R. M., Taylor, G. J., Quilty, L. C., and Parker, J. D. (2007). Reexamining the factor structure of the 20-item Toronto alexithymia scale: commentary on Gignac, palmer, and Stough. J. Pers. Assess. 89, 258–264. doi: 10.1080/00223890701629771
Bamonti, P. M., Heisel, M. J., Topciu, R. A., Franus, N., Talbot, N. L., and Duberstein, P. R. (2010). Association of alexithymia and depression symptom severity in adults aged 50 years and older. Am. J. Geriatr. Psychiatry 18, 51–56. doi: 10.1097/JGP.0b013e3181bd1bfe
Barbasio, C., Vagelli, R., Marengo, D., Querci, F., Settanni, M., Tani, C., et al. (2015). Illness perception in systemic lupus erythematosus patients: the roles of alexithymia and depression. Compr. Psychiatry 63, 88–95. doi: 10.1016/j.comppsych.2015.09.004
Bird, G., and Cook, R. (2013). Mixed emotions: the contribution of alexithymia to the emotional symptoms of autism. Transl. Psychiatry 3, 1–8. doi: 10.1038/tp.2013.61
Bloom, D. E., Cafiero, E., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L. R., Fathima, S., et al. (2011). The global economic burden of noncommunicable diseases. Geneva: World Economic Forum.
Boyle, M. H. (1998). Guidelines for evaluating prevalence studies. Evid. Based Ment. Health 1, 37–39. doi: 10.1136/ebmh.1.2.37
Bratis, D., Tselebis, A., Sikaras, C., Moulou, A., Giotakis, K., Zoumakis, E., et al. (2009). Alexithymia and its association with burnout, depression and family support among Greek nursing staff. Hum. Resour. Health 7, 1–6. doi: 10.1186/1478-4491-7-72
Butler, E. A., Lee, T. L., and Gross, J. J. (2007). Emotion regulation and culture: are the social consequences of emotion suppression culture-specific? Emotion 7, 30–48. doi: 10.1037/1528-3542.7.1.30
Cameron, K., Ogrodniczuk, J., and Hadjipavlou, G. (2014). Changes in alexithymia following psychological intervention: a review. Harv. Rev. Psychiatry 22, 162–178. doi: 10.1097/HRP.0000000000000036
Chen, P., Sun, X., Zhang, Q., Yang, C., Ye, X., Wang, Y., et al. (2022). Alexithymia and depressive symptoms mediated the relationship between childhood trauma and suicidal risk in Chinese male prisoners. Curr. Psychol. 42, 1–12. doi: 10.1007/s12144-022-03975-2
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. 2nd Edn. Hillsdale: Erlbaum.
Da Ros, A., Vinai, P., Gentile, N., Forza, G., and Cardetti, S. (2011). Evaluation of alexithymia and depression in severe obese patients not affected by eating disorders. Eat. Weight Disord. 16, 24–29. doi: 10.1007/BF03327517
De Berardis, D., Serroni, N., Campanella, D., Carano, A., Gambi, F., Valchera, A., et al. (2008). Alexithymia and its relationships with C-reactive protein and serum lipid levels among drug naïve adult outpatients with major depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 32, 1982–1986. doi: 10.1016/j.pnpbp.2008.09.022
De Gennaro, L., Martina, M., Curcio, G., and Ferrara, M. (2004). The relationship between alexithymia, depression, and sleep complaints. Psychiatry Res. 128, 253–258. doi: 10.1016/j.psychres.2004.05.023
De Gucht, V., Fischler, B., and Heiser, W. (2004). Neuroticism, alexithymia, negative affect, and positive affect as determinants of medically unexplained symptoms. Pers. Individ. Differ. 36, 1655–1667. doi: 10.1016/j.paid.2003.06.012
Demers, L. A., and Koven, N. S. (2015). The relation of alexithymic traits to affective theory of mind. Am. J. Psychol. 128, 31–42. doi: 10.5406/amerjpsyc.128.1.0031
Dere, J., Sun, J., Zhao, Y., Persson, T. J., Zhu, X., Yao, S., et al. (2013). Beyond “somatization” and “psychologization”: symptom-level variation in depressed Han Chinese and euro-Canadian outpatients. Front. Psychol. 4:377. doi: 10.3389/fpsyg.2013.00377
Dion, S. (1996). Why is secession difficult in well-established democracies? Lessons from Quebec. Br. J. Polit. Sci. 26, 269–283. doi: 10.1017/S0007123400000466
Dong, Z., Zhao, W., and Sun, J. (2019). The influence analysis of depression level and social support on narrative affective disorders in patients with Crohn’s disease. Shanghai Med. J. 42, 257–262.
Egger, M., and Smith, G. D. (1998). Bias in location and selection of studies. BMJ 316, 61–66. doi: 10.1136/bmj.316.7124.61
Eizaguirre, A. E., de Cabezón, A. O. S., de Alda, I. O., Olariaga, L. J., and Juaniz, M. (2004). Alexithymia and its relationships with anxiety and depression in eating disorders. Personal. Individ. Differ. 36, 321–331. doi: 10.1016/S0191-8869(03)00099-0
Farhoumandi, N., Zarean, M., Nasiri, M., and Jega, M. (2022). Somatization mediates the structural relationship of alexithymia with anxiety and depression. Iran. J. Psychiatry 17, 144–153. doi: 10.18502/ijps.v17i2.8904
Flaherty, J. A., Gaviria, F. M., Pathak, D., Mitchell, T., Wintrob, R., Richman, J. A., et al. (1988). Developing instruments for cross-cultural psychiatric research. J. Nerv. Ment. Dis. 176, 257–263. doi: 10.1097/00005053-198805000-00001
Flaherty, J. H., McBride, M., Marzouk, S., Miller, D. K., Chien, N., Hanchett, M., et al. (1998). Decreasing hospitalization rates for older home care patients with symptoms of depression. Journal of the American Geriatrics society, 46, 31–38.
Fujiwara, E. (2018). Looking at the eyes interferes with facial emotion recognition in alexithymia. J. Abnorm. Psychol. 127, 571–577. doi: 10.1037/abn0000361
Gelfand, M., Bhawuk, D., Nishii, L. H., and Bechtold, D. (2004). “Individualism and collectivism” in Culture, leadership, and organizations: The GLOBE study of 62 societies. eds. R. J. House, P. J. Hanges, M. Javidan, P. W. Dorfman, and V. Gupta (Thousand Oaks, CA: SAGE), 437–512.
Gignac, G. E., and Szodorai, E. T. (2016). Effect size guidelines for individual differences researchers. Personal. Individ. Differ. 102, 74–78. doi: 10.1016/j.paid.2016.06.069
Goerlich, K. S. (2018). The multifaceted nature of alexithymia–a neuroscientific perspective. Front. Psychol. 9:1614. doi: 10.3389/fpsyg.2018.01614
Goerlich, K. S., and Aleman, A. (2018). “Neuroimaging studies of alexithymia” in Alexithymia: Advances in research, theory, and clinical practice, eds. O. Luminet, G. J. Taylor, and R. M. Bagby. Cambridge University Press. 207–249.
Grabowska, P., Targowski, T., Rozyńska, R., Mierzejewska, J., and From, S. (2005). Alexithymia and depression: relationship to cigarette smoking, nicotine dependence and motivation to quit smoking. Przegl. Lek. 62, 1004–1006.
Griffin, C., Lombardo, M. V., and Auyeung, B. (2016). Alexithymia in children with and without autism spectrum disorders. Autism Res. 9, 773–780. doi: 10.1002/aur.1569
Gross, J. J. (2015). Emotion regulation: current status and future prospects. Psychol. Inq. 26, 1–26. doi: 10.1080/1047840X.2014.940781
Guan, N., Guariglia, A., Moore, P., Xu, F., and Al-Janabi, H. (2022). Financial stress and depression in adults: a systematic review. PLoS One 17:e0264041. doi: 10.1371/journal.pone.0264041
He, C., Zhang, X., Xia, Q., Gao, H., Yan, J., Chen, X., et al. (2022). Exploring the link between cognitive deficit, self-esteem, alexithymia, and depressive symptom of schizophrenia. Brain Behav. 12:e2648. doi: 10.1002/brb3.2648
Hemming, L., Haddock, G., Shaw, J., and Pratt, D. (2019). Alexithymia and its associations with depression, suicidality, and aggression: an overview of the literature. Front. Psych. 10:203. doi: 10.3389/fpsyt.2019.00203
Herbert, B. M., Herbert, C., and Pollatos, O. (2011). On the relationship between interoceptive awareness and alexithymia: is interoceptive awareness related to emotional awareness? J. Pers. 79, 1149–1175. doi: 10.1111/j.1467-6494.2011.00717.x
Higgins, J. P., Savović, J., Page, M. J., Elbers, R. G., and Sterne, J. A. (2019). “Assessing risk of bias in a randomized trial” in Cochrane handbook for systematic reviews of interventions, Cochrane Handbook for Systematic Reviews of Interventions version 6.0. Eds. J. P. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, and M. J. Page. Chichester, UK: John Wiley and Sons. pp. 205–228.
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327, 557–560. doi: 10.1136/bmj.327.7414.557
Hofstede, G. (2011). Dimensionalizing cultures: the Hofstede model in context. Online Read. Psychol. Cult. 2, 1–26. doi: 10.9707/2307-0919.1014
Honkalampi, K., Hintikka, J., Laukkanen, E., and Viinamäki, J. L. H. (2001). Alexithymia and depression: a prospective study of patients with major depressive disorder. Psychosomatics 42, 229–234. doi: 10.1176/appi.psy.42.3.229
Hou, C., Shi, H., Ma, Y., and Chou, J. (2024). Heterogeneity of alexithymia subgroups: a factor mixture modelling approach. Eur. J. Psychol. Assess. doi: 10.1027/1015-5759/a000828
Kenangil, G., Demir, M., Tur, E. K., and Domac, F. M. (2020). Alexithymia, depression, and cognition in patients with Parkinson’s disease. Parkinsonism Relat. Disord. 79, e17–e18. doi: 10.1007/s13760-020-01581-2
Kim, H. J., Kim, S. J., and Lee, S. A. (2020). Severity of idiopathic rapid eye movement sleep behavior disorder correlates with depression and alexithymia. Sleep Med. 74, 25–30. doi: 10.1016/j.sleep.2020.05.039
Kim, H. W., Rim, H. D., Kim, J. H., and Lee, S. J. (2009). Alexithymia and stress response patterns among patients with depressive disorders in Korea. Psychiatry Investig. 6, 13–18. doi: 10.4306/pi.2009.6.1.13
Kinnaird, E., Stewart, C., and Tchanturia, K. (2019). Investigating alexithymia in autism: a systematic review and meta-analysis. Eur. Psychiatry 55, 80–89. doi: 10.1016/j.eurpsy.2018.09.004
Kooiman, C. G., Spinhoven, P., and Trijsburg, R. W. (2002). The assessment of alexithymia: a critical review of the literature and a psychometric study of the Toronto alexithymia Scale-20. J. Psychosom. Res. 53, 1083–1090. doi: 10.1016/S0022-3999(02)00348-3
Koppelberg, P., Kersting, A., and Suslow, T. (2023). Alexithymia and interpersonal problems in healthy young individuals. BMC Psychiatry 23:688. doi: 10.1186/s12888-023-05191-z
Le, H.-N., Berenbaum, H., and Raghavan, C. (2002). Culture and alexithymia: mean levels, correlates and the role of parental socialization of emotions. Emotion 2, 341–360. doi: 10.1037/1528-3542.2.4.341
Lee, K. S., Zhang, J. J., Nga, V. D. W., Ng, C. H., Tai, B. C., Higgins, J. P., et al. (2022). Tenets for the proper conduct and use of meta-analyses: a practical guide for neurosurgeons. World Neurosurg. 161, 291–302. doi: 10.1016/j.wneu.2021.09.034
Levant, R. F., Good, G. E., Cook, S. W., O’Neil, J. M., Smalley, K. B., Owen, K., et al. (2006). The normative male alexithymia scale: measurement of a gender-linked syndrome. Psychol. Men Masculin. 7:212. doi: 10.1037/1524-9220.7.4.212
Leweke, F., Leichsenring, F., Kruse, J., and Hermes, S. (2011). Is alexithymia associated with specific mental disorders. Psychopathology 45, 22–28. doi: 10.1159/000325170
Li, L., Xu, D. D., Chai, J. X., Wang, D., Li, L., Zhang, L., et al. (2018). Prevalence of internet addiction disorder in Chinese university students: a comprehensive meta-analysis of observational studies. J. Behav. Addict. 7, 610–623. doi: 10.1556/2006.7.2018.53
Li, S., Zhang, B., Guo, Y., and Zhang, J. (2015). The association between alexithymia as assessed by the 20-item Toronto alexithymia scale and depression: a meta-analysis. Psychiatry Res. 227, 1–9. doi: 10.1016/j.psychres.2015.02.006
Liu, H., and Wang, W. (2019). The relationship between autism traits and suicidal ideation: the mediating role of narrative affective disorders and depression. Chin. J. Clin. Psychol. 27, 889–893. doi: 10.16128/j.cnki.1005-3611.2019.05.007
Lu, Y., Wang, F., Tian, M., and Si, D. (2002). Suicide attempt and narrative affective disorders. Chin. J. Neurol. Psychiatr. 28, 102–103.
Luca, M., Luca, A., and Calandra, C. (2013). Psychomotor retardation and externally oriented thinking in major depression. Neuropsychiatr. Dis. Treat. 9, 759–766. doi: 10.2147/NDT.S44650
Lv, Q., Li, X., Zhang, Y., Lu, D., Lu, J., Xie, Q., et al. (2023). Sex differences in subjective cognitive impairment and clinical correlates in Chinese patients with subthreshold depression. Biol. Sex Differ. 14:6. doi: 10.1186/s13293-023-00488-w
Ma, Z., Dong, W., Wu, J., Liang, D., and Yin, X. (2015). Confucian ideal personality and Chinese business negotiation styles: an indigenous perspective. Group Decis. Negot. 24, 383–400. doi: 10.1007/s10726-014-9394-6
Marchesi, C., Bertoni, S., Cantoni, A., and Maggini, C. (2008). Is alexithymia a personality trait increasing the risk of depression? A prospective study evaluating alexithymia before, during and after a depressive episode. Psychol. Med. 38, 1717–1722. doi: 10.1017/S0033291708003073
Markus, H. R., and Kitayama, S. (1994). “The cultural construction of self and emotion: implications for social behavior” in Emotion and culture. eds. S. Kitayama and H. R. Markus (Washington, DC: American Psychological Association), 89–130.
Marroquín, B. (2011). Interpersonal emotion regulation as a mechanism of social support in depression. Clin. Psychol. Rev. 31, 1276–1290. doi: 10.1016/j.cpr.2011.09.005
Mattila, A. K., Salminen, J. K., Nummi, T., and Joukamaa, M. (2006). Age is strongly associated with alexithymia in the general population. J. Psychosom. Res. 61, 629–635. doi: 10.1016/j.jpsychores.2006.04.013
Mesquita, B. (2001). Emotions in collectivist and individualist contexts. J. Pers. Soc. Psychol. 80, 68–74. doi: 10.1037/0022-3514.80.1.68
Mesquita, B., and Walker, R. (2003). Cultural differences in emotions: a context for interpreting emotional experiences. Behav. Res. Ther. 41, 777–793. doi: 10.1016/S0005-7967(02)00189-4
Miao, Z., Cheng, M., Ding, Z., Song, Q., Cao, W., Ye, H., et al. (2022). The relationship between narrative affective disorders and depression: the mediating role of maladaptive cognitive emotion regulation strategies and family environment. Chin. J. Clin. Psychol. 30, 1270–1281. doi: 10.16128/j.cnki.1005-3611.2022.06.0022022
Milosavljevic, B., Leno, V. C., Simonoff, E., Baird, G., Pickles, A., Jones, C. R., et al. (2016). Alexithymia in adolescents with autism spectrum disorder: its relationship to internalising difficulties, sensory modulation and social cognition. J. Autism Dev. Disord. 46, 1354–1367. doi: 10.1007/s10803-015-2670-8
Minkov, M., Bond, M. H., Dutt, P., Schachner, M., Morales, O., Sanchez, C., et al. (2018). A reconsideration of Hofstede’s fifth dimension: new flexibility versus monumentalism data from 54 countries. Cross-Cult. Res. 52, 309–333. doi: 10.1177/1069397117727488
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. The PRISMA Group (2009). Methods of systematic reviews and meta-analysis preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 62, 1006–1012. doi: 10.7326/0003-4819-151-4-200908180-00135
Moriguchi, Y., Ohnishi, T., Lane, R. D., Maeda, M., Mori, T., Nemoto, K., et al. (2006). Impaired self-awareness and theory of mind: an fMRI study of mentalizing in alexithymia. NeuroImage 32, 1472–1482. doi: 10.1016/j.neuroimage.2006.04.186
Motan, I., and Gençöz, T. (2007). The relationship between the dimensions of alexithymia and the intensity of depression and anxiety. Turk. J. Psychiatry 18, 333–343.
Müller, J., Bühner, M., and Ellgring, H. (2003). Relationship and differential validity of alexithymia and depression: a comparison of the Toronto alexithymia and self-rating depression scales. Psychopathology 36, 71–77. doi: 10.1159/000070361
Oakley, B. F., Jones, E. J., Crawley, D., Charman, T., Buitelaar, J., Tillmann, J., et al. (2022). Alexithymia in autism: cross-sectional and longitudinal associations with social-communication difficulties, anxiety and depression symptoms. Psychol. Med. 52, 1458–1470. doi: 10.1017/S0033291720003244
Obeid, S., Akel, M., Haddad, C., Fares, K., Sacre, H., Salameh, P., et al. (2020). Factors associated with alcohol use disorder: the role of depression, anxiety, stress, alexithymia and work fatigue-a population study in Lebanon. BMC Public Health 20, 1–11. doi: 10.1186/s12889-020-8345-1
Ogrodniczuk, J. S., Joyce, A. S., and Piper, W. E. (2005). Strategies for reducing patient-initiated premature termination of psychotherapy. Harv. Rev. Psychiatry 13, 57–70. doi: 10.1080/10673220590956429
Orwin, R. G., and Vevea, J. L. (2009). “Evaluating coding decisions” in The handbook of research synthesis and meta-analysis. eds. H. Cooper, L. Hedges, and J. Valentine (New York: Russell Sage Foundation Publications), 177–203.
Ozonder Unal, I., and Ordu, C. (2023). Alexithymia, self-compassion, emotional resilience, and cognitive emotion regulation: charting the emotional journey of Cancer patients. Curr. Oncol. 30, 8872–8887. doi: 10.3390/curroncol30100641
Patel, V., Saxena, S., Lund, C., Thornicroft, G., Baingana, F., Bolton, P., et al. (2018). The lancet commission on global mental health and sustainable development. Lancet 392, 1553–1598. doi: 10.1016/S0140-6736(18)31612-X
Pei, J., Wang, X., Chen, H., Zhang, H., Nan, R., Zhang, J., et al. (2021). Alexithymia, social support, depression, and burnout among emergency nurses in China: a structural equation model analysis. BMC Nurs. 20, 1–10. doi: 10.1186/s12912-021-00702-3
Preece, D., Becerra, R., Allan, A., Robinson, K., and Dandy, J. (2017). Establishing the theoretical components of alexithymia via factor analysis: introduction and validation of the attention-appraisal model of alexithymia. Pers. Individ. Differ. 119, 341–352. doi: 10.1016/j.paid.2017.08.003
Preece, D. A., Mehta, A., Becerra, R., Chen, W., Allan, A., Robinson, K., et al. (2022). Why is alexithymia a risk factor for affective disorder symptoms? The role of emotion regulation. J. Affect. Disord. 296, 337–341. doi: 10.1016/j.jad.2021.09.085
Quintana, D. S. (2015). From pre-registration to publication: a non-technical primer for conducting a meta-analysis to synthesize correlational data. Front. Psychol. 6:1549. doi: 10.3389/fpsyg.2015.01549
Radloff, L. S. (1977). A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401. doi: 10.1177/014662167700100306
Ramzi, N. H., Auvinen, J., Veijola, J., Miettunen, J., Ala-Mursula, L., Sebert, S., et al. (2023). Depression mediates the relationship between alexithymia and obesity in the northern Finland birth cohort 1966 (NFBC1966). J. Affect. Disord. 331, 1–7. doi: 10.1016/j.jad.2023.03.026
Reker, M., Ohrmann, P., Rauch, A. V., Kugel, H., Bauer, J., Dannlowski, U., et al. (2010). Individual differences in alexithymia and brain response to masked emotion faces. Cortex 46, 658–667. doi: 10.1016/j.cortex.2009.05.008
Ren, L., Yang, Y., Zhang, S., and Fu, W. (2022). The relationship between childhood abuse and depression in junior high school students: the chain mediating role of narrative affective disorders and self-pity. Chin. J. Health Psychol. 30, 1734–1740. doi: 10.13342/j.cnki.cjhp.2022.11.024
Rock, P. L., Roiser, J. P., Riedel, W. J., and Blackwell, A. (2014). Cognitive impairment in depression: a systematic review and meta-analysis. Psychol. Med. 44, 2029–2040. doi: 10.1017/S0033291713002535
Rosenthal, R., and DiMatteo, M. R. (2001). Meta-analysis: recent developments in quantitative methods for literature reviews. Annu. Rev. Psychol. 52, 59–82. doi: 10.1146/annurev.psych.52.1.59
Saarijärvi, S., Salminen, J. K., and Toikka, T. (2006). Temporal stability of alexithymia over a five-year period in outpatients with major depression. Psychother. Psychosom. 75, 107–112. doi: 10.1159/000090895
Sayar, K., Kirmayer, L. J., and Taillefer, S. S. (2003). Predictors of somatic symptoms in depressive disorder. Gen. Hosp. Psychiatry 25, 108–114. doi: 10.1016/S0163-8343(02)00277-3
Shi, H., Wang, L., Zeng, T., Li, Y., Xu, H., Sui, X., et al. (2022). The mediating role of alexithymia: social support and depression among colorectal Cancer patients. Comput. Math. Methods Med. 2022, 1–7. doi: 10.1155/2022/6771005
Sifneos, P. E. (1973). The prevalence of ‘alexithymic’characteristics in psychosomatic patients. Psychother. Psychosom. 22, 255–262. doi: 10.1159/000286529
Son, S. H., Jo, H., Rim, H. D., Kim, J. H., Kim, H. W., Bae, G. Y., et al. (2012). A comparative study on alexithymia in depressive, somatoform, anxiety, and psychotic disorders among Koreans. Psychiatry Investig. 9, 325–331. doi: 10.4306/pi.2012.9.4.325
Spitzer, C., Brandl, S., Rose, H. J., Nauck, M., and Freyberger, H. J. (2005). Gender-specific association of alexithymia and norepinephrine/cortisol ratios. A preliminary report. Journal of psychosomatic research, 59, 73–76. doi: 10.1016/j.jpsychores.2004.07.006
Stankov, L. (2010). Unforgiving Confucian culture: a breeding ground for high academic achievement, test anxiety and self-doubt? Learn. Individ. Differ. 20, 555–563. doi: 10.1016/j.lindif.2010.05.003
Sterne, J. A., Sutton, A. J., Ioannidis, J. P., Terrin, N., Jones, D. R., Lau, J., et al. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. doi: 10.1136/bmj.d4002
Tan, Y., Yang, C., Ou, Y., Hu, M., Wu, S., Lai, X., et al. (2021). The relationship between narrative affective disorders and suicide risk among prisoners: the mediating role of depression and anxiety. Chin. J. Health Psychol. 6, 810–815. doi: 10.13342/j.cnki.cjhp.2021.06.003
Tang, W. C., Lin, M. P., Wu, J. Y. W., Lee, Y. T., and You, J. (2022). Mediating role of depression in the association between alexithymia and nonsuicidal self-injury in a representative sample of adolescents in Taiwan. Child Adolesc. Psychiatry Ment. Health 16:43. doi: 10.1186/s13034-022-00477-8
Taylor, G. J., and Bagby, R. M. (2013). Psychoanalysis and empirical research: the example of alexithymia. J. Am. Psychoanal. Assoc. 61, 99–133. doi: 10.1177/0003065112474066
Taylor, G. J., Bagby, R. M., and Parker, J. D. (1999). Disorders of affect regulation: Alexithymia in medical and psychiatric illness. Cambridge, UK: Cambridge University Press.
Tominaga, T., Choi, H., Nagoshi, Y., Wada, Y., and Fukui, K. (2014). Relationship between alexithymia and coping strategies in patients with somatoform disorder. Neuropsychiatr. Dis. Treat. 10, 55–62. doi: 10.2147/ndt.s55956
Tran, A. G., Mintert, J. S., Llamas, J. D., and Lam, C. K. (2018). At what costs? Student loan debt, debt stress, and racially/ethnically diverse college students’ perceived health. Cult. Divers. Ethn. Minor. Psychol. 24, 459–469. doi: 10.1037/cdp0000207
Trautmann, S., and Wittchen, H. U. (2016). Do our societies react appropriately to the burden of mental disorders. EMBO Rep. 17, 1245–1249. doi: 10.15252/embr.201642951
Tsai, J. L., and Levenson, R. W. (1997). Cultural influences on emotional responding: Chinese American and European American dating couples during interpersonal conflict. J. Cross-Cult. Psychol. 28, 600–625. doi: 10.1177/0022022197285006
Van Der Cruijsen, R., Murphy, J., and Bird, G. (2019). Alexithymic traits can explain the association between puberty and symptoms of depression and anxiety in adolescent females. PloS one, 14:e0210519. doi: 10.1371/journal.pone.0210519
Viechtbauer, W. (2007). Publication bias in meta-analysis: prevention, assessment and adjustments. Psychometrika 72, 269–271. doi: 10.1007/s11336-006-1450-y
Wingbermühle, E., Theunissen, H., Verhoeven, W. M., Kessels, R. P., and Egger, J. I. (2012). The neurocognition of alexithymia: evidence from neuropsychological and neuroimaging studies. Acta Neuropsychiatr. 24, 67–80. doi: 10.1111/j.1601-5215.2011.00613.x
Xiong, Q., Shen, X., Yang, H., Wang, X., Yi, J., and Zhu, X. (2023). Alexithymia and non-suicidal self-injury in adolescents: the chain mediating role of maladaptive emotion regulation and depression. Chin. J. Clin. Psychol. 31, 574–577. doi: 10.16128/j.cnki.1005-3611.2023.03.013
Yalınay Dikmen, P., Onur Aysevener, E., Kosak, S., Ilgaz Aydınlar, E., and Sağduyu Kocaman, A. (2020). Relationship between MIDAS, depression, anxiety and alexithymia in migraine patients. Acta Neurol. Belg. 120, 837–844. doi: 10.1007/s13760-017-0856-x
Yelsma, P. (2007). Associations among alexithymia, positive and negative emotions, and self-defeating personality. Psychol. Rep. 100, 575–584.
Zhang, H., Wang, Y., Lou, H., Zhu, Y., Dong, Z., Dong, D., et al. (2023). Prevalence of and factors associated with alexithymia among patients with chronic obstructive pulmonary disease in China: a cross-sectional study. BMC Pulm. Med. 23, 1–9. doi: 10.1186/s12890-023-02335-5
Keywords: alexithymia, depression, meta-analysis, difficulty in describing feelings, difficulty in identifying feelings, externally oriented thinking
Citation: Liu Z, He S and Hou C (2025) The effect of alexithymia on depression: evidence from meta-analysis. Front. Psychol. 16:1465286. doi: 10.3389/fpsyg.2025.1465286
Edited by:
Ivan Cherrez-Ojeda, Espiritu Santo University, EcuadorReviewed by:
Rory Allen, Goldsmiths University of London, United KingdomClaudia Henschel de Lima, Fluminense Federal University, Brazil
Copyright © 2025 Liu, He and Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunna Hou, aG91Y2h1bm5hQDEyNi5jb20=
 Zhijun Liu
Zhijun Liu Shiwei He1
Shiwei He1 Chunna Hou
Chunna Hou