- 1University of Ottawa Heart Institute, Ottawa, ON, Canada
- 2Department of Medicine and School of Psychology, University of Ottawa, Ottawa, ON, Canada
- 3Département de Psychoéducation et de Psychologie, Université du Québec en Outaouais, Gatineau, QC, Canada
- 4Mayo Clinic, Rochester, MN, United States
- 5Stanford University School of Medicine, Stanford, CA, United States
- 6International Centre for Excellence in Emotionally Focused Therapy, Ottawa, ON, Canada
Introduction: Couple relationships are important for health. Relationship distress is associated with increased incident and prognostic cardiovascular risk, while positive support is linked to heart-healthy behaviors and improved outcomes. This paper describes the study rationale, objectives, design, and methods of the Healing Hearts Together (HHT) randomized controlled trial (RCT).
Objectives: The primary objective is to examine the difference in relationship quality between the 8-week HHT intervention group and usual care (UC) at program completion. Secondary objectives include evaluating the impact of HHT on relationship quality at 6 months, and mental health, quality of life, and cardiovascular risk factors measured at 8 weeks and 6 months post-intervention, as compared to usual care.
Methods: Patients and their partners are recruited within 6 months of a cardiac event, procedure, or hospitalization and randomized 1:1 to HHT or UC. Assessments occur at baseline, 8 weeks, and 6 months follow-up. Analyses are planned as intention-to-treat, with multi-level analyses of covariance (ANCOVA) for the primary outcome: 8-week relationship quality as measured by the Dyadic Adjustment Scale. Secondary objectives will be evaluated using multi-level modeling for repeated measures.
Anticipated results: It is expected that participants randomized to HHT will report higher relationship quality and improved secondary outcomes than will participants in UC.
Conclusion: As the first study to evaluate a relationship-enhancement program for couples with cardiac disease, findings will have important clinical implications regarding the effect of relationship interventions on heart health.
Background
The quality of couple relationships significantly affects both psychological and physical health, particularly in the context of cardiovascular disease (CVD) (Azizi et al., 2024). High-quality relationships, characterized by satisfaction and minimal hostility, are linked to better health outcomes, whereas strained relationships or a sense of disconnection from close others can lead to adverse outcomes. To illustrate, a meta-analysis involving 35,925 participants reported that loneliness and social isolation increased the risk of coronary artery disease (CAD) by 29% (Valtorta et al., 2016). In contrast, positive support provided by a partner can protect against cardiac-related health issues, including metabolic syndrome and post-operative complications. For example, patients reporting satisfying relationships are 3 times more likely to be alive at 15 years post-bypass surgery (King and Reis, 2012).
Couples’ relationship quality (RQ) may influence heart health both directly and indirectly. Direct pathways include the impact of psychological and physical challenges on the cardiovascular, neuroendocrine, and immune systems. Psychological stress from relationship strain or hostility can activate the sympathetic nervous system, leading to increased blood pressure, heart rate, and cardiac output (Valtorta et al., 2016; Kelli et al., 2019). Supportive relationships, on the other hand, are linked to improved heart rate variability (HRV), a measure of the heart’s ability to respond to stress. Higher HRV is associated with better cardiovascular health (Goodyke et al., 2024) and lower stress hormone levels, reducing the risk of CAD and mortality (Pourmand et al., 2023). Further, couples in which one partner criticizes while the other shuts down emotionally secrete higher levels of cortisol during conflict. Elevated cortisol levels are strong predictors of CAD and cardiac mortality (Shrout et al., 2020).
Indirect pathways in which RQ influences heart health involve health behaviors driven by RQ (Azizi et al., 2024; Khaing et al., 2017; Rapelli et al., 2022; Bertoni et al., 2023). Relationship problems can lead to engagement in risky health behaviors such as smoking and alcohol use (Roberson et al., 2018), whereas better marital adjustment and positive dyadic coping is associated with enhanced medication compliance (Rapelli et al., 2022) and cardiac rehabilitation (CR) (Trevino et al., 1990). Spouses can exert social influence over health behaviors, such as preparing low-sodium meals, modeling healthy behavior (e.g., exercise), or assisting in the management of disease (e.g., medication management) (Ford et al., 2009). However, if this support is in the form of overprotection, for example, it may cause more harm than good (Bertoni et al., 2023). Satisfying relationships are associated with lower rates of mental health problems and better quality of life in cardiac patients, whereas discord can exacerbate anxiety and depression (Bouchard et al., 2021; Bouchard et al., 2023), increasing the risk of cardiac complications and death (Civieri et al., 2024).
Current cardiac interventions often overlook the importance of RQ. Consequently, few studies exist that measure the effect of couples-based interventions in patients with heart disease and their partners. Existing research has focused on traditional approaches such as diet, exercise, and stress management, producing inconsistent results. A recent scoping review (Rapelli et al., 2023) of couple-based psychological interventions for cardiac patients and their partners identified 11 studies (6 RCTs). Many interventions were classified as “partner-assisted” (i.e., partners complete tasks to help the patient), with the remaining studies being “couple-interaction” interventions in which couple adjustment and coping were addressed (Gartner et al., 1988; Lenz and Perkins, 2000; Sher et al., 2014; Stewart et al., 2001). Of the latter studies (3 RCTs), the interventions showed little improvement over control conditions. Gartner et al. (1988) reported increased patient tolerance for emotional distress at 3 months post surgery, but no differences were found at 6 months, and no partner effects were observed. An enhanced version of this intervention did not produce differences between intervention and control groups (Lenz and Perkins, 2000). Lastly, compared to a patient-only education program for cardiac risk reduction, couples receiving education plus counseling on communication skills and relationship issues reported higher levels of physical activity, but no differences were detected on any of the other variables of interest (e.g., body mass index, nutrition, medication compliance) (Sher et al., 2014). As such, there has been a call in the literature for high-quality, contemporary studies of couples facing heart disease that includes enhanced relationship-focused interventions and measures of RQ for the patient and partner to enhance intervention success (Rapelli et al., 2023; Pietromonaco and Collins, 2017; Pietromonaco et al., 2013; Smith, 2022). The inclusion of partners in the care of patients with CVD has the potential to not only enhance patient outcomes, but also to help partners who often share similar cardiovascular risk factors.
With its solid foundation of evidence (Mikulincer and Shaver, 2016; Cassidy and Shaver, 2016) relationship scientists have applied attachment theory to understand the link between RQ and health, as well as to address the role of relationship distress in the health context. Attachment theory specifies that all human beings have an innate need for emotional connections with significant others and, when these ties are threatened (e.g., during a cardiac event), immense distress is triggered and attachment behaviors (e.g., seeking closeness) as well as caregiving behaviors (e.g., protection) are activated in an attempt to gain reassurance and/or emotional homeostasis. Emotionally focused, attachment-based interventions have been applied to help couples solidify a sense of security and connection by articulating and reaching out when feeling vulnerable (e.g., “what would I do if you died?”). These interventions have produced improved relationship satisfaction and health outcomes (e.g., reduce heart rate and cortisol levels) during stressful situations (Greenberg and Watson, 2006; Johnson, 2019; Johnson and Denton, 2002).
In the cardiac context, members of our team created the Healing Hearts Together (HHT) program, adapted from the Hold Me Tight: Conversations for Connection program (Johnson, 2010). Rooted in attachment theory, HHT emphasizes the need for close emotional bonds between partners and introduces strategies to address the emotional challenges of heart disease to promote healthy coping (Tulloch et al., 2021). Our proof-of-concept data demonstrated clinically significant improvements from pre- to post-intervention on relationship distress, depression, anxiety and quality of life (Tulloch et al., 2021) among patients with heart disease and their partners. However, no lifestyle, physiological (e.g., inflammatory makers, cortisol reactivity), or cardiovascular risk factors or outcomes were measured, and a comparison group was not included. Further study is needed to definitively determine the clinical impact and underlying mechanisms of HHT.
Study aims and objectives
The primary aim of this RCT is to examine the efficacy of the 8-week HHT program on the relationship quality of patients with CVD and their romantic partners at 8 weeks, in comparison to UC. We expect that those assigned to the HHT condition will have greater improvements in RQ scores (as measured by the dyadic adjustment scale) than will those in UC. Secondary aims include measuring the impact of the program on relationship quality at 6 months and secondary outcomes, including cardiovascular and cortisol reactivity, inflammatory markers, mental health, quality of life, health behaviors, and cardiovascular risk factors, at 8 weeks and 6 months. We expect greater improvements in all secondary outcomes among HHT participants than in UC participants. This paper describes the study design, objectives and method.
Method
Design
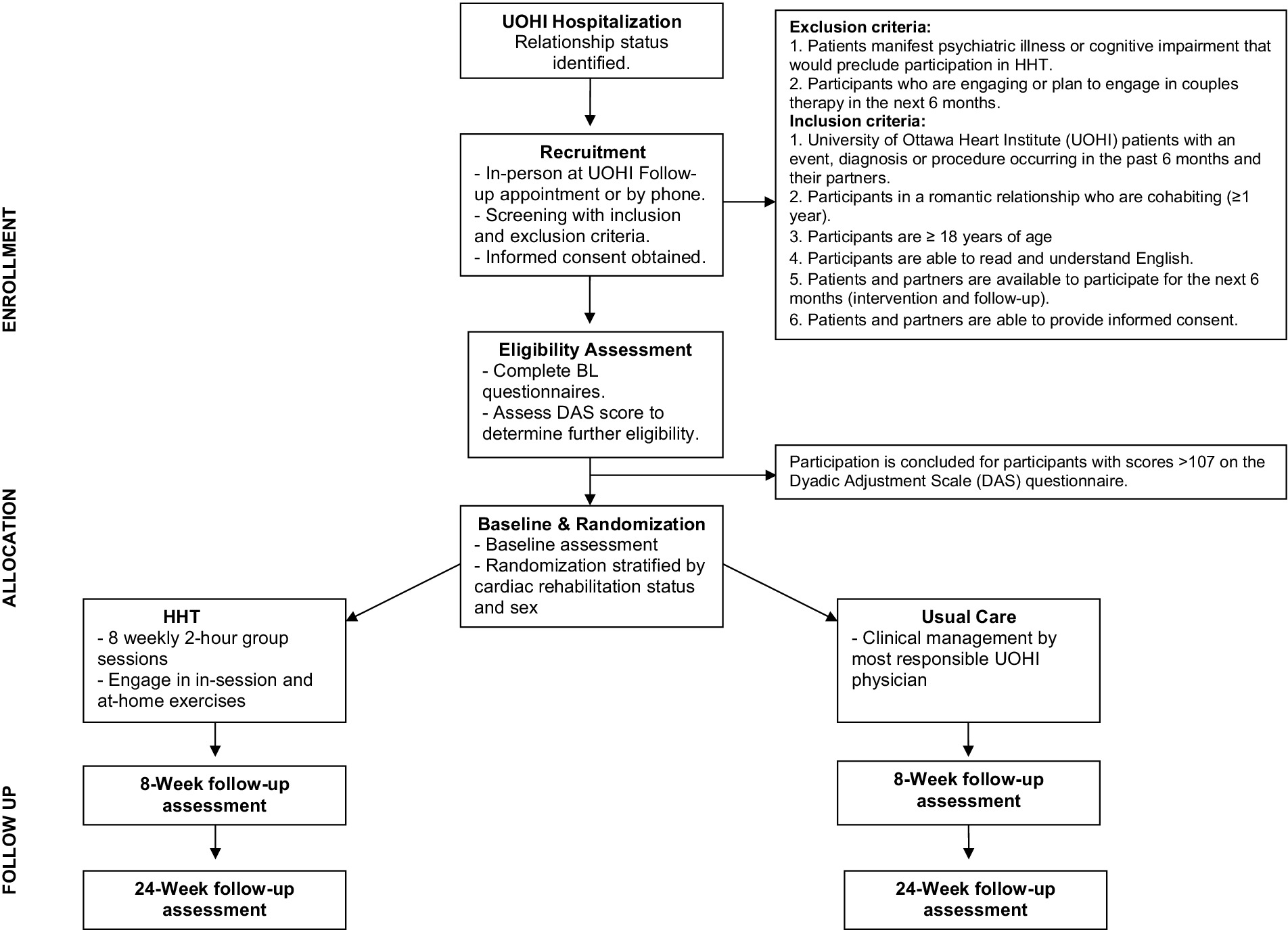
The study is a single-centre, RCT with parallel group design. After a baseline assessment, participants are randomized in a 1:1 fashion, using a computer-generated sequence utilizing permuted blocks of 4, 8 and 10 initiated by the institutional methods centre, to the HHT program or to UC. Since sex and participation in CR can have an impact on the study outcomes, randomization is stratified by patient sex (male/female) and participation in the University of Ottawa Heart Institute (UOHI) CR program (yes/no). The trial began in October 2019 and data collection is ongoing. The protocol was approved by our institutional research ethics board (OHSN-REB# 20190101-01H) and all participants provide informed consent. Figure 1 depicts the study design and cohort flow.
Participants
Patients at a large cardiac care hospital in Canada and their partners are approached to participate if they meet the study eligibility criteria, including: (1) being in a romantic relationship of any sexual orientation for at least 1 year; (2) living together for one or more years; (3) the patient having a cardiac event, procedure, or hospitalization in the past 6 months; (4) being 18 years or older; and, (5) being available to participate for 6 months. As a substantial number of participating couples reported high relationship satisfaction and, thereby, likely experience limited benefit from the HHT intervention, in July 2023, another inclusion criterion – one or both partners must score below the satisfied range on relationship quality (i.e., score of <107 on the Dyadic Adjustment Scale (DAS) questionnaire) (Spanier, 1976) - was added as advised by the study biostatistician. Exclusion criteria include: (1) those with any psychiatric or cognitive problems that would impair participation in the HHT program. Staff screen for impairment via chart review. If nothing is documented but a potential participant appears to have these impairments, the study psychologist would determine (either through further chart review or discussion with the research coordinator, referring clinician, or patient) whether participation is appropriate, or (2) planned or active participation in couples’ therapy. Since the HHT program materials were available in English only at the study outset, participants are required to read and understand English. However, the option to complete questionnaires in French or English or speak in their first language during some tasks is possible.
Recruitment and data collection
Following their discharge, patients in a romantic relationship who provided institutional consent to be approached for research are directly contacted in-person or by phone by a research coordinator (RC). For those who do not provide such consent, a member of their circle of care initiates contact and obtains permission for the RC to contact the patient to provide information about the study. Recruitment strategies are adopted to achieve adequate participant enrolment, such as approaching patients at scheduled follow-up appointments and emailing additional information to those who indicate initial interest and confirm email consent. If patients express interest in participating following initial contact, the RC then explains the study procedures and obtains informed consent from the patient and partner. Participants are then invited to fill out an online questionnaire package via Research Electronic Data Capture (REDCap), a secure web-based application designed to support data capture for research studies. Those who prefer may complete the questionnaires on paper; these data are entered into REDCap by the RC. If DAS scores are above the established cut off, participation is concluded. Those in the eligible range are invited to complete the full study and scheduled for a baseline appointment at the UOHI.
Baseline assessment
Prior to the baseline assessment, participants fast, abstain from exercise for 12 h, and avoid caffeine and non-prescription diuretics for 4 h. At the assessment, they review and sign two copies of the study consent form. After obtaining signed consent, participants provide a blood sample (10 mL) and rinse their mouth in preparation for the saliva samples. Staff then attach pre-gelled electrodes under the participant’s right clavicle and below the left ribcage for HRV recordings. Saliva samples are collected 10 min after arrival. Then, participants complete the spousal disagreement form, followed by a 15-min rest period during which participants sit quietly but avoid sleeping. The conflict resolution task is completed next. Immediately before and after the conflict resolution task, blood pressure (BP) and heart rate readings are recorded, and additional saliva samples are taken. Participants are asked to rest for another 15 min upon completion of the second set of BP readings. Two final saliva samples are collected at 20 and 40 min after the conflict resolution task (Birkett, 2011). Finally, height, weight, waist circumference, and carbon monoxide levels are recorded, and patients are given an accelerometer to wear for a 7-day period. Bloodwork is collected by staff phlebotomist, and assessments are carried out by research staff with backgrounds in nursing, psychology, and health sciences. Study staff are trained on assessment procedures, including the reading of BP results and protocols for abnormal values or adverse events during the appointments. At the end of the baseline assessment, the RC randomizes participants to the HHT or UC and informs them of group assignment. Randomly generated intervention allocations are contained within sealed opaque envelopes. Research staff who assist with assessments are not present during randomization. Couples in the intervention arm receive information about HHT group logistics.
Follow-up assessments
The same procedures are conducted at each follow-up assessment (8 weeks and 6 months). A REDCap link is sent to participants via email or, if preferred, printed questionnaires are sent by post to be completed before the assessment. Patients also report if they enrolled in CR and, if so, in which program options they participated (e.g., exercise, nutrition, stress management class). They also indicate if they partook in any individual or couples-based psychological services. Research staff conducting follow up data collection, intervention infidelity checks, and behavioral coding are blind to the randomized condition. To maximize participant retention, assessments are scheduled to coincide with regular follow-up appointments or rehabilitation sessions at the UOHI whenever possible. Appointment reminders and parking passes are provided at each assessment, and gift cards are distributed after their final assessment. Efforts are made to collect primary outcome data despite potential deviation from study protocols. For example, the completion of online questionnaires will still be offered to those who might withdraw from in-person study activities.
Data management
Following study assessments, research assistants enter data into SPSS. Other staff members periodically carry out quality checks, and discrepancies are recorded and reported to the staff leading data entry. After assessment completion and data entry, files with participant information are stored in locked cabinets on site. To maintain confidentiality, all data entered is coded with study ID numbers instead of personal identifying information.
Interventions
Healing hearts together intervention
Couples are invited to attend 8 weekly 2-h sessions facilitated by clinical psychologists with EFT training. Before providing the intervention, facilitators review information on CVD and its treatments, theory and practice of group interventions, and familiarize themselves with the HHT facilitator materials. An HHT facilitators manual was developed to standardize intervention delivery (Tulloch et al., 2017). Planned group size is 3–8 couples, with sessions available in the day or evening to accommodate participants’ work schedules. Since the onset of the COVID-19 pandemic (March 2020), however, groups have been conducted online using the secure platform Zoom; only one group was held in-person before the pandemic. During the program, participants are guided through seven conversations in which they learn to identify and improve communication patterns for positive interactions in relationships (Tulloch et al., 2021). EFT interventions allow couples to acknowledge their fears and vulnerabilities and solidify their sense of security and emotional connection by guiding partners to respond to these feelings in comforting ways (Johnson, 2004; Johnson, 2008). The intervention maintains principles from the Hold Me Tight program (Johnson, 2010) but, as alluded to above, centres on identifying the impact of CVD on relationship dynamics, including the recognition and processing of worries and emotions following a cardiac diagnosis or event, healing interactions, and discussing sexuality in a health context (Tulloch et al., 2021). Materials, such as in-class and take-home worksheets, didactic presentations, and videos, are incorporated to facilitate these conversations (Johnson, 2010; Tulloch et al., 2021). The session-by-session overview has been previously described (Tulloch et al., 2021). In brief, each session begins with a review of the previous session and its homework, followed by a didactic presentation, a video clip of a couple discussing EFT principles, a private dyadic conversation, a final group discussion, and a homework assignment. In addition, each couple receives a copy of the book, Hold Me Tight, in print or audio version (Johnson, 2008) to be read in-between sessions. Attendance is noted at each session. Participants are asked to inform research staff if they must miss a session, and if this is the case, they are sent presentation slides from the respective session for review. Participant feedback surveys are sent via email after each session. All sessions incorporate group discussions and private conversations between patients and partners. Group discussion allows couples to share experiences related to CVD with their partners and peers. Session two allows for participants to discuss their experiences as patients in a patient-only group and as partners of someone with CVD in a partner-only group discussion, both of which are guided by a facilitator. Zoom break-out rooms are used for dyadic-specific exercises; facilitators assist during these discussions. HHT intervention materials may be found here: https://iceeft.com/healing-hearts-together-relationship-education-program/.
Usual care
All patients at the study hospital are scheduled for a follow-up visit 4–8 weeks after hospitalization. At this appointment, a physician conducts a clinical assessment and determines appropriate medical management. Patients are automatically referred to the centre’s CR program, which includes exercise training and potential referrals to medical and allied health services, including dietetics, social work, psychology, and vocational rehabilitation; patients may choose whether they wish to receive these services or not. Optional attendance at nursing-led patient/caregiver support groups (e.g., heart failure support) and peer-support groups (e.g., Women at Heart) is also available. While the control group is potentially extensive, it represents evidence-based care for patients with CVD and, as such, preventing participants from enrollment would be unethical.
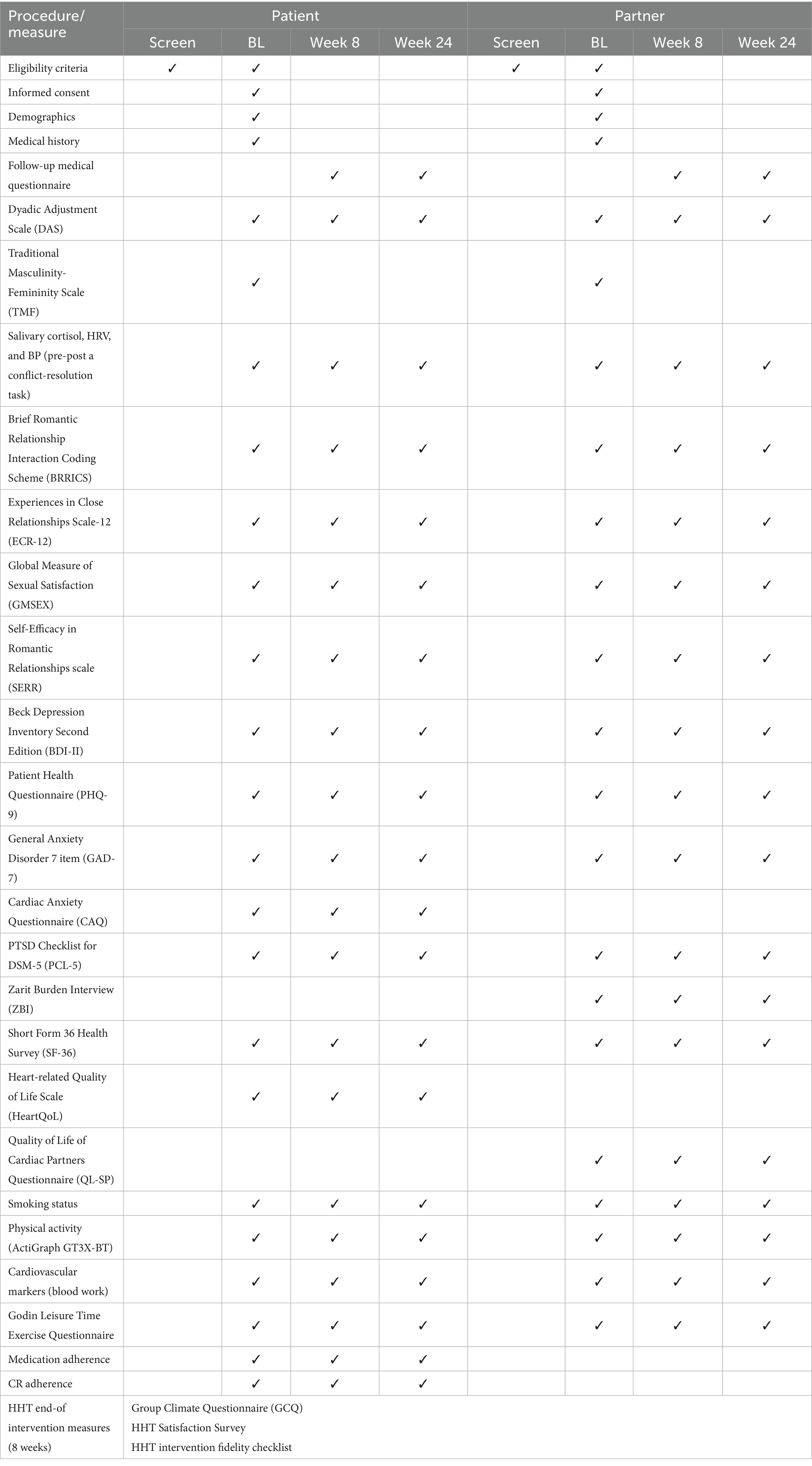
Measures
Assessments are conducted at baseline before randomization, and at 8 weeks and 6 months; the timeline for all measures is presented in Table 1. As previous couples-based research often failed to include partners in their measurements, all participants complete measures assessing relationship variables, mental health, general Quality of Life (QoL), and health behaviors; are monitored for HRV, heart rate, and BP; and provide salivary and plasma samples. Disease-specific QoL, medication compliance, and CR adherence (if enrolled) is collected for patients only.
Demographic and clinical information
Participants report their demographic (e.g., age, education, ethnicity) and clinical information (e.g., medical history, comorbidities, medications). Staff also extract patients’ medial history from their hospital chart. To explore how gender-related self-perceptions influence health outcomes and relational dynamics, participants complete the Traditional Masculinity-Femininity (TMF) Scale, a 6-item measure of self-ascribed masculinity and femininity. Psychometric properties have been established (Cronbach’s alpha = 0.94) (Kachel et al., 2016).
Relationship quality is assessed in 2 ways: (1) The primary outcome, participants’ perceived RQ, is evaluated using the Dyadic adjustment scale (DAS), a 32-item questionnaire with well-established psychometric properties (e.g., Cronbach’s alpha = 0.96) (Spanier, 1976; Prouty et al., 2000; Spanier and Thompson, 1982). The DAS has been employed in research and clinical settings among various populations, including patients with heart disease (Spanier, 1976; Prouty et al., 2000; Spanier and Thompson, 1982). Scores range from 0 to 151, with higher scores indicating higher RQ. Scores ≥108 indicate high couple satisfaction; scores ≤70 indicate extreme couple distress (divorcing couples) (Spanier, 1976). The four subscales measure couple satisfaction, cohesion, consensus and affectionate expression (Spanier, 1976). (2) Couple dynamics are recorded during a 15-min conflict-resolution task, during which couples are instructed to discuss their top 3 topics that regularly cause disagreement in their relationship such as health, money, sex, or in-laws, with the intention of coming to a resolution. These recordings are then coded by 2 blinded independent reviewers (psychology staff and graduate students) using the Brief Romantic Relationship Interaction Coding Scheme (BRRICS) (Humbad et al., 2011), a standard procedural guideline for coding behaviors in romantic relationships. Routine spot checks are conducted by co-PI Greenman (blinded) to ensure reliability among the coders. The BRRICS evaluates both individual and dyadic aspects of interactions between partners, including positive and negative affect, positive and negative reciprocity, demand-withdraw patterns, and overall relationship satisfaction (Wildey and Burt, 2018).
Other relationship-related variables include attachment style, sexual satisfaction, and relationship self-efficacy. Participants complete the Experiences in Close Relationships Scale-12 (ECR-12) (Lafontaine et al., 2015) assessing attachment orientations using the dimensions of attachment anxiety and attachment avoidance with two subscales of six items each (rating from strongly disagree = 1 to strongly agree = 7). Low scores on both subscales indicate higher levels of secure attachment (Lafontaine et al., 2015; Wei et al., 2007; Brennan et al., 1998). Validity and reliability (Cronbach’s alpha = 0.74–87) of the scale has been established (Lafontaine et al., 2015). The adapted version of the Global Measure of Sexual Satisfaction (GMSEX), a 6-item measure, was used to assess overall satisfaction with the sexual relationship. Each item is rated on a 7-point bipolar scale (e.g., good-bad, valuable-worthless), with total scores ranging from 6 to 42, where higher scores indicate greater satisfaction (Lawrance and Byers, 1998). The psychometric performance of the scale is strong (e.g., Cronbach’s alpha = 0.96) (Quinn-Nilas, 2023). The Self-Efficacy in Romantic Relationships scale (SERR) is a 12-item questionnaire measuring confidence in romantic relationships. Participants indicate on a 9-point scale (1 = do not agree at all; 9 = completely agree) how much they agree with statements such as “I am just one of those people who is not good at being a romantic relationship partner” or “I feel insecure about my ability to be a good romantic partner.” (Riggio et al., 2013) Scores are totaled in a positive direction (i.e., higher scores indicate higher self-efficacy in a romantic partnership). The measure has been deemed valid and reliable (e.g., Cronbach alphas >0.79) (Riggio et al., 2013).
Mental health
Participants symptoms of depression over the past week are measured with the 21-item Beck Depression Inventory Second Edition (BDI-II) (Beck et al., 1996). Total scores range from 0 to 63; <13 = minimal, 14–19 = mild, 20–28 = moderate, and ≥29 = severe. The BDI-II demonstrated strong high internal consistency (Cronbach’s alpha = 0.90–0.93) and test–retest reliability (García-Batista et al., 2018). The Patient Health Questionnaire (PHQ-9), a 9-item, 4-point Likert scale (0 = not at all; 3 = nearly every day) assessing depressive symptoms over the past 2 weeks is also completed by participants. Scores range from 0 to 27; cut-off scores for moderate, moderately severe and severe depressive symptoms are 10, 15, and 20, respectively (Kroenke and Spitzer, 2002). The tool shows strong psychometric properties, including good internal consistency (Cronbach’s alpha = 0.89) and robust validity (Kroenke et al., 2001). Two measures of depression were used because they provide complementary information. The PHQ-9 coincides with DSM-IV criteria for major depressive disorder. The BDI-II is more detailed measure that assesses the severity of cognitive, behavioral, and physiological symptoms of depression. Participants’ generalized anxiety is evaluated with the General Anxiety Disorder 7 item (GAD-7) questionnaire, a 4-point Likert scale with a total score of 0–21, where 10–14 and 15–21 indicate moderate and severe anxiety, respectively (Spitzer et al., 2006). The GAD-7 demonstrated strong reliability, with a Cronbach’s alpha of 0.89 and a composite reliability index of 0.90. It also exhibited robust validity across procedural, criterion, construct, and factorial measures (Bolgeo et al., 2023). Patient participants’ cardiac specific anxiety was assessed with the 18-item Cardiac Anxiety Questionnaire (CAQ). The CAQ yields 3 subscales reflecting fear, heart-focused attention, and related avoidance. Patients rate, on a 5-point Likert scale (0 = never, 4 = always), how frequent a behavior occurs (e.g., “I avoid activities that make my heartbeat faster”). Responses are summed for a total score; scores >26 are considered elevated (Eifert et al., 2000). The CAQ has shown good internal consistency (Cronbach’s alpha = 0.083) and construct validity (Eifert et al., 2000; Leissner et al., 2022).
The PTSD Checklist for DSM-5 (PCL-5) is a 20-item questionnaire used to assess post-traumatic stress symptoms. Responses to trauma-related statements are rated on a 5-point scale (0 = not at all, 4 = extremely); scores ≥33 are indicative of probable PTSD diagnosis (Weathers et al., 2013). Participants are directed to focus on the cardiac event when responding. The PCL-5 demonstrates strong reliability and validity in assessing PTSD symptoms across diverse populations (Cronbach’s alpha>0.91) (Blevins et al., 2015). One partner-specific questionnaire, the 22-item Zarit Burden Interview (ZBI), assesses how partners feel when taking care of another person and indicates the degree of caregiver burden. Responses are indicated on a 5-point Likert scale (0 = never; 4 = nearly always). Total scores ≥17 are considered high burden (Al-Rawashdeh et al., 2016). Psychometric properties of the ZBI have been established (e.g., Cronbach alphas>0.80) (Bachner and O’Rourke, 2007). As noted, all the mental health scales have been validated and used with patients with cardiovascular disease (Al-Rawashdeh et al., 2016; Van Beek et al., 2012; Seng et al., 2010; Blanchard et al., 1996; Hammash et al., 2013; Moullec et al., 2015; Löwe et al., 2008).
Quality of life
General and disease-specific QoL is assessed with 3 questionnaires. All participants complete the Rand 36-item Short Form Health Survey (Ware et al., 1993) to assess QoL across eight domains: physical functioning, role limitations due to physical health, role limitations due to emotional problems, energy/fatigue, emotional well-being, social functioning, pain, and general health. The SF-36 is widely used and validated across various patient populations, including those with cardiovascular disease (Brazier et al., 1992; Ware and Gandek, 1998). Patients also complete the Heart-related Quality of Life Scale (HeartQoL) (Oldridge et al., 2014), a 14-item validated questionnaire designed to evaluate how heart disease impacts daily functioning. The HeartQoL includes a global health-related QoL score and separate physical and emotional subscales (Oldridge et al., 2014). Similarly, partners complete the Quality of Life of Cardiac Spouses Questionnaire (QL-SP), a validated 26-item measure with two subscales: emotional functioning (14 items) and physical and social functional dimensions (12 items) (Ebbesen et al., 1990). Psychometric properties have been established for all scales with Cronbach alphas exceeding 0.70 (Brazier et al., 1992; Oldridge et al., 2014; Thomson et al., 2013; Zangger et al., 2018).
Health behaviors
Smoking status is reported by participants and confirmed with CO concentration (<10 ppm) in an expired breath sample, using the Russell standard (West et al., 2005). Participants wear an ActiGraph GT3X-BT accelerometer on their non-dominant hand for 7 days to assess physical activity and sedentary behaviors. Self-reported frequency and duration of mild, moderate and vigorous physical activity is also measured using a modified and validated version of the Godin Leisure Time Exercise Questionnaire (GLTEQ) (Godin and Shephard, 1985). Two adherence measures are used: (1) Medication adherence is measured with 3-items (e.g., how often do you forget to take your medication?) and (2) CR adherence is calculated by the percentage of exercise sessions attended relative to those prescribed.
Physical/cardiovascular markers
Blood samples taken by a staff phlebotomist are analyzed for total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), C-reactive protein (CRP), and hemoglobin A1C (A1C). Saliva samples are collected using Salimetrics Oral Swab (Salimetrics, State College, PA) to assess cortisol and inflammatory marker IL-6. Following the Trier Social Stress Test Protocol (Birkett, 2011), 5 samples are taken: upon arrival, before and after the conflict resolution task and 20 and 40 min later. Samples are stored at −80°C and shipped frozen to Salimetrics for analysis. Heart Rate Variability (HRV) is measured by continuous heart period recordings of R-R intervals sampled at the rate of 1,000 Hz using First Bodyguard 2 (Firstbeat Technologies, OyJyvaskyla, Finland) connected to 2 leads by pre-gelled (Ag/AgCl) disposable electrocardiograph electrodes attached beneath the right clavicle and left ribcage (Firstbeat Technologies, 2025). BP is measured with the BpTru using standardized procedures (Myers et al., 2008). Finally, weight, height and waist circumference are recorded.
HHT intervention participant evaluation
HHT group participants complete the Group Climate Questionnaire (GCQ) (MacKenzie, 1983), a 12-item instrument designed to assess group engagement, conflict and avoidance. Responses are recorded on a 7-point Likert scale, from 0 (not at all) to 7 (extremely). The treatment specific HHT Satisfaction Survey, a 22-item survey assessing participants’ experience and satisfaction with the HHT sessions and the online delivery of the intervention, is given to HHT participants after program completion.
HHT intervention attendance and fidelity
Participation in the HHT intervention is recorded by class attendance (% attended). To ensure that the HHT intervention is delivered as intended, two sessions of every 8-session group are randomly pre-selected, recorded and scored on study-specific HHT intervention fidelity checklist by two independent raters (psychology trainees). Points are given, and percentage calculated, for each key point that is outlined in the session-by-session HHT manual (Tulloch et al., 2017).
Data monitoring
Adverse events are recorded and reported to the principal investigator for review. Endorsement of the suicide item of the PHQ-9 or BDI are reported immediately to one of the study psychologists for risk assessment and care. The Healing Hearts Together study was initially granted ethics approval without a Data Safety Monitoring Board (DSMB); it was not recommended nor inquired by ethics. Nonetheless, the PIs convened a DSMB committee in 2024, consisting of a psychiatrist, cardiologist and consulting statistician, to discuss data management for the study.
Auditing
The study has undergone 2 routine internal audits: one divisional, investigator-initiated audit in February 2022 and an institutionally led audit in February 2023. No major infractions were noted.
Statistical analyses
Sample-size calculation
An a priori calculation was performed using RQ as measured by the DAS at 8 weeks as the primary outcome. Sample size was derived in 3 steps. First, we examined the standard deviation (SD) of the DAS scores pre-post intervention (SDchange) of pilot patients and partners separately (i.e., HHT pilot data); all SDchange values were close to 10. The consensus of the study investigators and other clinical content experts was to identify a minimum clinically important difference (MCID) based on a small (0.20) to moderate (0.50) Cohen’s effect size. The difference between the HHT and UC groups in the mean change was 3.9 for a small to moderate effect size. This value is close to the commonly used minimum mean change score for the DAS (3.16) (Jacobson and Truax, 1991). Then, we used these values (SDchange = 10; MCID = 3.9) to calculate the sample size with PASS15 sample size software. With 210 couples assigned in a 1:1 fashion to the two groups, we will have 80% power to detect a difference of 3.9 in the change in the DAS between the HHT and UC groups (α = 0.05). Nonetheless, we aim to inflate our sample size to account for the design effect of clustering (design effect = 1 + (m-1)*ICC = 1.21 = 254 couples), assuming that our average group size (m) will be 8 couples and our ICC is 0.030. We further increased our sample size target to 304 couples to account for an expected 20% loss to follow-up. As such, we aim to recruit 304 couples but will have sufficient power to detect differences in the primary outcome with 210 couples.
Planned statistical analyses
SPSS and HLM statistical software will be used to analyze the study data. Demographic and clinical variables reported by participants who complete assessments will be compared to those lost to follow-up to verify the representativeness of the cohort. Analyses will be with the intent to treat sample. Research staff record all cases of missing data, including non-retention of participants or withdrawal of consent. Where data are missing, the frequency and reasons for missing data will be recorded. Missing data will be statistically examined for patterns of systematic missingness, and an appropriate missing data strategy will be employed. In situations where data are missing, the data collected up to that point will be used, provided the participant has not withdrawn their consent or requested that the information be removed. For the primary outcome, a multilevel analysis of covariance with individuals’ DAS values at 8 weeks as the dependent variable and DAS baseline scores as the covariate at level 1 of the model. The study conditions (HHT vs. UC) to which couples were assigned will be dummy-coded and entered at level 2. To evaluate secondary outcomes, a three-level multi-level model for repeated measurements will be utilized. The analysis will include repeated measurements within individuals in Level 1, between-individual variability in Level 2, and couples in Level 3. Within-couple slope variances will be fixed at Level 2 but allowed to vary at Level 3 (Atkins, 2005). A linear parameter will model changes in outcomes from baseline to 8 weeks to 24 weeks. The study condition (HHT vs. UC) will be dummy-coded and modeled as a fixed effect at Level 3. Baseline patient control variables will be entered at Level 2. Binary outcomes will be modeled utilizing a logit link. Improved model fit between nested models will be evaluated using deviance statistics and a chi-square distribution. Effect sizes will be assessed with the pseudo-R squared statistic or Cohen’s d when appropriate. Full maximum likelihood estimation method will be applied for all analyses. For both primary and secondary analyses, we will also conduct stratified analyses for all outcomes by sex (male/female), CR participation (yes/no), and relationship quality (distressed/not distressed on the DAS).
Anticipated outcomes
It is expected that participants randomized to HHT intervention will report higher RQ (≥3.9 points on the DAS) and improved secondary outcomes as compared to those in UC.
Dissemination plans
Trial results will be shared through published manuscripts to participants, healthcare professionals, and the public. To enhance the accessibility of the research findings, results will also be disseminated in interactive formats. For example, findings will be presented during hospital rounds and in-services to inform clinical staff of the importance of relationship quality and encourage the inclusion of the partner in the care team. Results will be disseminated to research participants and the lay public in formats such as community presentations, in-person research dissemination events, and media releases.
Discussion
To our knowledge, the HHT randomized trial is one of few studies evaluating a relationship-enhancement intervention specifically designed for couples facing the challenges of CVD. The HHT intervention is rooted in an evidence-based theoretical framework, expert recommendations (Johnson, 2004; Johnson, 2008), and direct input from couples managing CVD (Tulloch et al., 2020). Further, the intervention and trial design address many methodological limitations in the couples-based literature in the cardiac domain, including small sample sizes; samples restricted to specific cardiac populations limiting generalizability; data collection limited to patients only; limited and solely subjective measures of RQ, and, few relevant and cardiac-specific health outcomes. Indeed, the current trial has several strengths, including the RCT design, comprehensive assessments using validated, objective and self-report measures, partner-specific data collection, and aims to recruit a large sample. Our proof-of-concept data showed pre-post improvements in RQ, mental health and quality of life (Tulloch et al., 2021). The present RCT now tests if the HHT intervention is better than usual care on many relationship and health outcomes. With significant findings, the finalized intervention will signal if effectiveness testing is required and may indicate that the intervention should be systematically implemented at other cardiac care sites, as well as pave the way for future intervention research for other chronic conditions (e.g., cancer). If positive, this research may also contribute to a shift from medical and physical indicators alone to a more holistic approach which comprises the promotion of enhanced social support through improved couple relationships, thereby enhancing cardiovascular outcomes. Considering that partners often share similar age and lifestyle factors as patients, they too may be vulnerable to poor mental or physical health outcomes, and programs such as HHT enhancing RQ may improve partners’ health along with improving the CVD recovery process for patients (Bouchard et al., 2019).
Data availability statement
The datasets presented in this article are not readily available because the study is ongoing. Requests to access the datasets should be directed to Heather Tulloch, aGV0dWxsb2NoQG90dGF3YWhlYXJ0LmNh.
Ethics statement
The studies involving humans were approved by Ottawa Health Science Network Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HT: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. PG: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing. JR: Methodology, Resources, Writing – review & editing. SS: Data curation, Project administration, Writing – review & editing. EK: Writing – original draft, Writing – review & editing. GT: Methodology, Writing – review & editing. LM: Methodology, Supervision, Writing – review & editing. GW: Methodology, Writing – review & editing. LS: Methodology, Writing – review & editing. SJ: Conceptualization, Funding acquisition, Methodology, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by a Canadian Institutes of Health Research (CIHR) project grants (400694, 508648).
Acknowledgments
We are grateful to the participants and research staff who assisted with program facilitation and RCT data collection to date. Our heartful thanks goes to Sue Johnson (deceased), who kindly shared her time, expertise, and friendship, and helped us to adapt her previously established Hold Me Tight program to a cardiac context.
Conflict of interest
HT and PG are co-authors of the Healing Hearts Together Program and receive royalties from its sales.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Al-Rawashdeh, S. Y., Lennie, T. A., and Chung, M. L. (2016). Psychometrics of the Zarit burden interview in caregivers of patients with heart failure. J. Cardiovasc. Nurs. 31, E21–E28. doi: 10.1097/JCN.0000000000000348
Atkins, D. C. (2005). Using multilevel models to analyze couple and family treatment data: basic and advanced issues. J. Fam. Psychol. 19, 98–110. doi: 10.1037/0893-3200.19.1.98
Azizi, B., Soltani, D., Arero, A. G., Karimi, A. S., Ramezani, A., Vasheghani-Farahani, A., et al. (2024). Marital quality-a neglected player in the prevention of cardiovascular diseases: a systematic review of longitudinal studies. Curr. Cardiol. Rep. 26, 821–831. doi: 10.1007/s11886-024-02082-x
Bachner, Y. G., and O’Rourke, N. (2007). Reliability generalization of responses by care providers to the Zarit burden interview. Aging Ment. Health 11, 678–685. doi: 10.1080/13607860701529965
Beck, A. T., Steer, R. A., and Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
Bertoni, A., Rapelli, G., Parise, M., Pagani, A. F., and Donato, S. (2023). “Cardiotoxic” and “cardioprotective” partner support for patient activation and distress: are two better than one? Fam. Relat. 72, 1335–1350. doi: 10.1111/fare.12694
Birkett, M. A. (2011). The Trier social stress test protocol for inducing psychological stress. J. Vis. Exp. 56:3238. doi: 10.3791/3238
Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., and Forneris, C. A. (1996). Psychometric properties of the PTSD checklist (PCL). Behav. Res. Ther. 34, 669–673. doi: 10.1016/0005-7967(96)00033-2
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., and Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J. Trauma. Stress. 28, 489–498. doi: 10.1002/jts.22059
Bolgeo, T., Di Matteo, R., Simonelli, N., Molin, A. D., Lusignani, M., Bassola, B., et al. (2023). Psychometric properties and measurement invariance of the 7-item general anxiety disorder scale (GAD-7) in an Italian coronary heart disease population. J. Affect. Disord. 334, 213–219. doi: 10.1016/j.jad.2023.04.140
Bouchard, K., Gareau, A., Gallant, N. L., Lalande, K., Greenman, P. S., Sztajerowska, K., et al. (2021). Dyadic effects of anxiety and depression on quality of life among couples facing cardiovascular disease. J. Psychosom. Res. 149:110601. doi: 10.1016/J.JPSYCHORES.2021.110601
Bouchard, K., Gareau, A., Greenman, P. S., Lalande, K., Sztajerowska, K., and Tulloch, H. (2023). What’s love got to do with it? Relationship quality appraisals and quality of life in couples facing cardiovascular disease. Health Psychol. Behav. Med. 11:2237564. doi: 10.1080/21642850.2023.2237564
Bouchard, K., Greenman, P. S., Pipe, A., Johnson, S. M., and Tulloch, H. (2019). Reducing caregiver distress and cardiovascular risk: a focus on caregiver-patient relationship quality. Can. J. Cardiol. 35, 1409–1411. doi: 10.1016/j.cjca.2019.05.007
Brazier, J. E., Harper, R., Jones, N. M. B., Jones, N. M., O'Cathain, A., Thomas, K. J., et al. (1992). Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Br. Med. J. 305:6846. doi: 10.1136/bmj.305.6846.160
Brennan, K. A., Clark, C. L., and Shaver, P. R. (1998). “Self-report measurement of adult attachment: An integrative overview,” in Attachment theory and close relationships. eds. J. A. Simpson and S. W. Rholes (New York: Guilford Press).
Cassidy, J., and Shaver, P. R. (eds.). (2016). Handbook of attachment: theory, research, and clinical applications. 3rd ed. eds. J. Cassidy and P. R. Shaver (New York: Guilford Press).
Civieri, G., Abohashem, S., Grewal, S. S., Aldosoky, W., Qamar, I., Hanlon, E., et al. (2024). Anxiety and depression associated with increased cardiovascular disease risk through accelerated development of risk factors. JACC Adv. 3:101208. doi: 10.1016/j.jacadv.2024.101208
Ebbesen, L. S., Guyatt, G. H., McCartney, N., and Oldridge, N. B. (1990). Measuring quality of life in cardiac spouses. J. Clin. Epidemiol. 43, 481–487. doi: 10.1016/0895-4356(90)90137-E
Eifert, G. H., Thompson, R. N., Zvolensky, M. J., Edwards, K., Frazer, N. L., Haddad, J. W., et al. (2000). The cardiac anxiety questionnaire: development and preliminary validity. Behav. Res. Ther. 38, 1039–1053. doi: 10.1016/S0005-7967(99)00132-1
Firstbeat Technologies O. (2025). Firstbeat bodyguard 2. Available at: https://support.firstbeat.com/hc/en-us/categories/360001268694-Firstbeat-Bodyguard-2 (Accessed January 13, 2025).
Ford, E. S., Bergmann, M. M., Kröger, J., Schienkiewitz, A., Weikert, C., and Boeing, H. (2009). Healthy living is the best revenge: findings from the European prospective investigation into cancer and nutrition-Potsdam study. Arch. Intern. Med. 169, 1355–1362. doi: 10.1001/archinternmed.2009.237
García-Batista, Z. E., Guerra-Peña, K., Cano-Vindel, A., Herrera-Martínez, S. X., and Medrano, L. A. (2018). Validity and reliability of the beck depression inventory (BDI-II) in general and hospital population of Dominican Republic. PLoS One 13:e0199750. doi: 10.1371/journal.pone.0199750
Gartner, S. R., Gilliss, C. L., Shinn, J. A., Sparacino, P. A., Rankin, S., Leavitt, M., et al. (1988). Improving recovery following cardiac surgery: a randomized clinical trial. J. Adv. Nurs. 13, 649–661. doi: 10.1111/j.1365-2648.1988.tb01459.x
Godin, G., and Shephard, R. J. (1985). A simple method to assess exercise behavior in the community. Can. J. Appl. Sport Sci. 10, 141–164.
Goodyke, M. P., Bronas, U. G., Baynard, T., Tintle, N., DeVon, H. A., Collins, E., et al. (2024). Relationships among heart rate variability, perceived social support, and hopelessness in adults with ischemic heart disease. J. Am. Heart Assoc. 13:e032759. doi: 10.1161/JAHA.123.032759
Greenberg, L. S., and Watson, J. C. (2006). Emotion-focused therapy for depression. 1st ed. Washington, DC: American Psychological Association.
Hammash, M. H., Hall, L. A., Lennie, T. A., Heo, S., Chung, M. L., Lee, K. S., et al. (2013). Psychometrics of the PHQ-9 as a measure of depressive symptoms in patients with heart failure. Eur. J. Cardiovasc. Nurs. 12, 446–453. doi: 10.1177/1474515112468068
Humbad, M. N., Donnellan, M. B., Klump, K. L., and Burt, S. A. (2011). Development of the brief romantic relationship interaction coding scheme (BRRICS). J. Fam. Psychol. 25, 759–769. doi: 10.1037/A0025216
Jacobson, N. S., and Truax, P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 59, 12–19. doi: 10.1037/0022-006X.59.1.12
Johnson, S. M. (2004). The practice of emotionally focused couple therapy: Creating connections. New York: Brunner-Routledge.
Johnson, S. M. Hold me tight: Seven conversations for a lifetime of love. Little, Brown Spark; (2008). Accessed December 29, 2024. Available online at:https://www.amazon.com/Hold-Me-Tight-Conversations-Lifetime/dp/031611300X
Johnson, S. M. (2010). The facilitator’s guide for the hold me tight program: Conversations for connection. 2nd ed. Available at: https://iceeft.com/product/the-facilitators-guide-for-the-hold-me-tight-program-conversations-for-connection/ (Accessed December 29, 2024).
Johnson, S. M. (2019). Attachment theory in practice: emotionally focused therapy (EFT) with individuals, couples, and families. New York: The Guilford Press.
Johnson, S. M., and Denton, W. (2002). “Emotionally focused couple therapy: creating secure connections,” in Clinical handbook of couple therapy. 3rd ed. eds. A. S. Gurman and N. S. Jacobson (New York: Guilford Press), p. 221–50.
Kachel, S., Steffens, M. C., and Niedlich, C. (2016). Traditional masculinity and femininity: validation of a new scale assessing gender roles. Front. Psychol. 7:164027. doi: 10.3389/fpsyg.2016.00956
Kelli, H. M., Mehta, A., Tahhan, A. S., Liu, C., Kim, J. H., Dong, T. A., et al. (2019). Low educational attainment is a predictor of adverse outcomes in patients with coronary artery disease. J. Am. Heart Assoc. 8:s013165. doi: 10.1161/JAHA.119.013165/SUPPL_FILE/JAH34349-SUP-0001-SUPINFO.PDF
Khaing, W., Vallibhakara, S. A., Attia, J., McEvoy, M., and Thakkinstian, A. (2017). Effects of education and income on cardiovascular outcomes: a systematic review and meta-analysis. Eur. J. Prev. Cardiol. 24:1032. doi: 10.1177/2047487317705916
King, K. B., and Reis, H. T. (2012). Marriage and long-term survival after coronary artery bypass grafting. Health Psychol. 31, 55–62. doi: 10.1037/a0025061
Kroenke, K., and Spitzer, R. L. (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 32, 509–515. doi: 10.3928/0048-5713-20020901-06
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2001). The PHQ-9 validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Lafontaine, M. F., Brassard, A., Lussier, Y., Valois, P., Shaver, P. R., and Johnson, S. M. (2015). Selecting the best items for a short-form of the experiences in close relationships questionnaire. Eur. J. Psychol. Assess. 32, 140–154. doi: 10.1027/1015-5759/a000243
Lawrance, K., and Byers, E. S. (1998). “Interpersonal exchange model of sexual satisfaction questionnaire,” in Sexuality related measures: A compendium. 2nd ed. eds. C. M. Davis, W. L. Yarber, R. Bauserman, G. Schreer, and S. L. Davis (Thousand Oaks: Sage Publication Inc.), p. 525–30.
Leissner, P., Held, C., Rondung, E., and Olsson, E. M. G. (2022). The factor structure of the cardiac anxiety questionnaire, and validation in a post-MI population. BMC Med. Res. Methodol. 22:338. doi: 10.1186/s12874-022-01820-5
Lenz, E. R., and Perkins, S. (2000). Coronary artery bypass graft surgery patients and their family member caregivers: outcomes of a family-focused staged psychoeducational intervention. Appl. Nurs. Res. 13, 142–150. doi: 10.1053/apnr.2000.7655
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., et al. (2008). Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care 46, 266–274. doi: 10.1097/MLR.0b013e318160d093
MacKenzie, K. R. (1983). “The clinical application of a group climate measure,” in Advances in group psychotherapy: integrating research and practice. eds. R. R. Dies and K. R. MacKenzie (New York, N.Y.: International Universities Press, Inc.), p. 159–70.
Mikulincer, M., and Shaver, P. R. (2016). Attachment in adulthood: Structure, dynamics, and change. 2nd Edn: The Guilford Press.
Moullec, G., Plourde, A., Lavoie, K. L., Suarthana, E., and Bacon, S. L. (2015). Beck depression inventory II: determination and comparison of its diagnostic accuracy in cardiac outpatients. Eur. J. Prev. Cardiol. 22, 665–672. doi: 10.1177/2047487314527851
Myers, M. G., McInnis, N. H., Fodor, G. J., and Leenen, F. H. H. (2008). Comparison between an automated and manual sphygmomanometer in a population survey. Am. J. Hypertens. 21, 280–283. doi: 10.1038/ajh.2007.54
Oldridge, N., Höfer, S., McGee, H., Conroy, R., Doyle, F., and Saner, H. (2014). The HeartQoL: part I. Development of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur. J. Prev. Cardiol. 21, 90–97. doi: 10.1177/2047487312450544
Pietromonaco, P. R., and Collins, N. L. (2017). Interpersonal mechanisms linking close relationships to health. Am. Psychol. 72, 531–542. doi: 10.1037/amp0000129
Pietromonaco, P. R., Uchino, B., and Schetter, C. D. (2013). Close relationship processes and health: implications of attachment theory for health and disease. Health Psychol. 32, 499–513. doi: 10.1037/a0029349
Pourmand, V., Froidevaux, N. M., Williams, D. W. P., Yim, I. S., and Campos, B. (2023). Attachment insecurity, heart rate variability, and perceived social support in a diverse sample of young adults. Front. Psychol. 14:1208924. doi: 10.3389/fpsyg.2023.1208924
Prouty, A. M., Johnson, S., and Protinsky, H. O. (2000). Recruiting the next generation of marriage and family therapists through undergraduate internships. J. Marital. Fam. Ther. 26, 47–50. doi: 10.1111/j.1752-0606.2000.tb00275.x
Quinn-Nilas, C. (2023). Time for a measurement check-up: testing the couple’s satisfaction index and the global measure of sexual satisfaction using structural equation modeling and item response theory. J. Soc. Pers. Relat. 40, 2252–2276. doi: 10.1177/02654075221143360
Rapelli, G., Donato, S., Parise, M., Pagani, A. F., Castelnuovo, G., Pietrabissa, G., et al. (2022). Yes, I can (with you)! Dyadic coping and self-management outcomes in cardiovascular disease: the mediating role of health self-efficacy. Health Soc. Care Community 30, e2604–e2617. doi: 10.1111/hsc.13704
Rapelli, G., Giusti, E. M., Tarquinio, C., Varallo, G., Franceschini, C., Musetti, A., et al. (2023). Psychological couple-oriented interventions for patients with heart disease and their partners: a scoping review and guidelines for future interventions. Front. Psychol. 14:1194767. doi: 10.3389/fpsyg.2023.1194767
Riggio, H. R., Weiser, D. A., Valenzuela, A. M., Lui, P. P., Montes, R., and Heuer, J. (2013). Self-efficacy in romantic relationships: prediction of relationship attitudes and outcomes. J. Soc. Psychol. 153:629. doi: 10.1080/00224545.2013.801826
Roberson, P. N. E., Shorter, R. L., Woods, S., and Priest, J. (2018). How health behaviors link romantic relationship dysfunction and physical health across 20 years for middle-aged and older adults. Soc. Sci. Med. 201, 18–26. doi: 10.1016/j.socscimed.2018.01.037
Seng, B. K., Luo, N., Ng, W. Y., Lim, J., Chionh, H. L., Goh, J., et al. (2010). Validity and reliability of the Zarit burden interview in assessing caregiving burden. Ann. Acad. Med. Singap. 39, 758–763. doi: 10.47102/annals-acadmedsg.V39N10p758
Sher, T., Braun, L., Domas, A., Bellg, A., Baucom, D. H., and Houle, T. T. (2014). The Partners for Life Program: a couples approach to cardiac risk reduction. Fam. Process 53, 131–149. doi: 10.1111/famp.12061
Shrout, M. R., Renna, M. E., Madison, A. A., Jaremka, L. M., Fagundes, C. P., Malarkey, W. B., et al. (2020). Cortisol slopes and conflict: a spouse’s perceived stress matters. Psychoneuroendocrinology 121:104839. doi: 10.1016/j.psyneuen.2020.104839
Smith, T. W. (2022). Intimate relationships and coronary heart disease: implications for risk, prevention, and patient management. Curr. Cardiol. Rep. 24, 761–774. doi: 10.1007/s11886-022-01695-4
Spanier, G. B. (1976). Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J. Marriage Fam. 38:15. doi: 10.2307/350547
Spanier, G. B., and Thompson, L. (1982). A confirmatory analysis of the dyadic adjustment scale. J. Marriage Fam. 44, 731–738. doi: 10.2307/351593
Spitzer, R. L., Kroenke, K., Williams, J. B. W., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166:1092. doi: 10.1001/archinte.166.10.1092
Stewart, M., Davidson, K., Meade, D., Hirth, A., and Weld-Viscount, P. (2001). Group support for couples coping with a cardiac condition. J. Adv. Nurs. 33, 190–9. doi: 10.1111/j.1365-2648.2001.01652.x
Thomson, P., Niven, C. A., Peck, D. F., and Eaves, J. (2013). Patients’ and partners’ health-related quality of life before and 4 months after coronary artery bypass grafting surgery. BMC Nurs. 12:16. doi: 10.1186/1472-6955-12-16
Trevino, D. B., Young, E. H., Groff, J., and Jono, R. T. (1990). The association between marital adjustment and compliance with antihypertension regimens. J. Am. Board Fam. Pract. 3, 17–25. doi: 10.3122/JABFM.3.1.17
Tulloch, H., Bouchard, K., Clyde, M. J., Madrazo, L., Demidenko, N., Johnson, S. M., et al. (2020). Learning a new way of living together: A qualitative study exploring the relationship changes and intervention needs of patients with cardiovascular disease and their partners. BMJ Open. 10:e032948. doi: 10.1136/bmjopen-2019-032948
Tulloch, H., Greenman, P., Demidenko, N., and Johnson, S. M. (2017). Healing hearts together relationship education program: Facilitator’s guide for small groups.
Tulloch, H., Johnson, S., Demidenko, N., Clyde, M., Bouchard, K., and Greenman, P. S. (2021). An attachment-based intervention for patients with cardiovascular disease and their partners: a proof-of-concept study. Health Psychol. 40, 909–919. doi: 10.1037/hea0001034
Valtorta, N. K., Kanaan, M., Gilbody, S., Ronzi, S., and Hanratty, B. (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 102, 1009–1016. doi: 10.1136/heartjnl-2015-308790
Van Beek, M., Voshaar, R., Van Deelen, F., Van Balkom, A., Pop, G., and Speckens, A. (2012). The cardiac anxiety questionnaire: cross-validation among cardiac inpatients. Int. J. Psychiatry Med. 43, 349–364. doi: 10.2190/PM.43.4.e
Ware, J. E., and Gandek, B. (1998). Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J. Clin. Epidemiol. 51, 903–912. doi: 10.1016/S0895-4356(98)00081-X
Ware, J. E., Snow, K. K., Kosinski, M., and Gandek, B. (1993). SF-36 health survey manual and interpretation guide. Boston: New England Medical Centre.
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., and Schnurr, P. P. (2013). PTSD Checklist for DSM-5 (PCL-5) - Standard [Measurement instrument]. Scale available from the National Center for PTSD at www.ptsdvagov.
Wei, M., Russell, D. W., Mallinckrodt, B., and Vogel, D. L. (2007). The experiences in close relationship scale (ECR)-short form: reliability, validity, and factor structure. J. Pers. Assess. 88, 187–204. doi: 10.1080/00223890701268041
West, R., Hajek, P., Stead, L., and Stapleton, J. (2005). Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction 100, –303. doi: 10.1111/j.1360-0443.2004.00995.x
Wildey, M. N., and Burt, S. A. (2018). “BRRICS: Brief Romantic Relationship Interaction Coding Scheme,” in The Cambridge handbook of group interaction analysis. eds. E. Brauner, M. Boos, and M. Kolbe (Cambridge University Press), p. 613–21.
Zangger, G., Zwisler, A. D., Kikkenborg Berg, S., Kristensen, M. S., Grønset, C. N., Uddin, J., et al. (2018). Psychometric properties of HeartQoL, a core heart disease-specific health-related quality of life questionnaire, in Danish implantable cardioverter defibrillator recipients. Eur. J. Prev. Cardiol. 25, 142–149. doi: 10.1177/2047487317733074
Keywords: cardiovascular disease, couples, relationship quality, intervention, emotionally focused therapy (EFT), attachment
Citation: Tulloch HE, Greenman PS, Reed J, Susinski S, Kasos E, Tasca GA, Mielniczuk L, Wells G, Sun LY and Johnson SM (2025) Healing Hearts Together — an emotionally focused intervention for couples after a cardiac event: a randomized controlled trial protocol. Front. Psychol. 16:1564666. doi: 10.3389/fpsyg.2025.1564666
Edited by:
Changiz Mohiyeddini, Oakland University William Beaumont School of Medicine, United StatesReviewed by:
Amanda Marin-Chollom, Central Connecticut State University, United StatesGiada Rapelli, University of Bologna, Italy
Copyright © 2025 Tulloch, Greenman, Reed, Susinski, Kasos, Tasca, Mielniczuk, Wells, Sun and Johnson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heather E. Tulloch, aGV0dWxsb2NoQG90dGF3YWhlYXJ0LmNh
†Author deceased as of April 2024
 Heather E. Tulloch
Heather E. Tulloch Paul S. Greenman
Paul S. Greenman Jennifer Reed
Jennifer Reed Stephanie Susinski1
Stephanie Susinski1 Louise Y. Sun
Louise Y. Sun