- 1Department of Prosthetic Dental Sciences, College of Dentistry, King Saud University, Riyadh, Saudi Arabia
- 2Dental Internship Training Program, College of dentistry, King Saud University, Riyadh, Saudi Arabia
Aim: The bond strength between resin composite and ceramics is critical for the success of fractured ceramics repaired with resin composites. The aim of the present study was to investigate and compare the shear bond strength (SBS) between resin composites and lithium disilicate (LD) ceramics using three different surface treatments of the LD.
Methodology: One hundred twenty samples of lithium disilicate were fabricated, out of which 60 were layered with fluoroapatite. Three surface treatment protocols were used: Sandblasting, phosphoric acid and clearfil ceramic prime plus (PA+CFCP); Sandblasting, hydrofluoric acid and clearfil ceramic prime plus (HA+CFCP); Hydrofluoric acid with Monobond N. All specimens were repaired with resin composite, aged using 5,000 cycles of thermocycling (5 °C–55 °C), followed by SBS testing. Specimens were examined under scanning electron and digital microscopes for type of failure. Two-way, one-way ANOVA and t-tests were used for statistical analysis (P < 0.05).
Results: A two-way ANOVA revealed that both ceramic type and the interaction with surface treatment significantly influenced SBS (p < 0.05). While no significant differences in SBS were found among protocols for lithium disilicate, porcelain showed significantly higher SBS when treated with hydrofluoric acid followed by Clearfil Ceramic Primer Plus (HF + CFCP) compared to hydrofluoric acid with Monobond N (HF + MB). Failure mode analysis showed consistent patterns in lithium disilicate across treatments, while porcelain exhibited more mixed failures—indicative of stronger bonds—in the HF + CFCP group. These findings underscore the importance of tailoring surface treatments to the specific ceramic to achieve optimal bond strength and durability.
Conclusion: Clearfil Ceramic Primer Plus demonstrated shear bond strength (SBS) comparable to hydrofluoric acid-based protocols when used with lithium disilicate, even in the absence of hydrofluoric acid. Moreover, in porcelain repair, it achieved superior SBS compared to the conventional hydrofluoric acid and silane combination, highlighting its potential as a safer and more effective surface treatment option for both ceramic types.
Introduction
For dental restorations, ceramics are growing in popularity (Shi et al., 2022). Lithium disilicate, a ceramic composed of glass particles, is one of the materials utilized (Zarone et al., 2019). According to Zarone et al. (2019), it can be used for single crowns, fixed partial dentures, anterior veneers, posterior inlays, onlays, and overlays. Because lithium disilicate lacks metallic elements in its microstructure and has a low refractive index, it offers a high translucency that resembles natural teeth and good aesthetics. When compared to zirconia or cobalt-chromium alloy, it is thought to be the most biocompatible (Forster et al., 2014).
Glass is the main component of another type of dental ceramic that mimics real teeth. Whereby triaxial porcelain compositions of feldspar, quartz, and kaolin are usually the source (Zhang and Kelly, 2017). Despite being the most artistically amazing; they are thought to be the weakest. In terms of applications, it works well with veneering metal coping and bi-layered ceramic (Warreth and Elkareimi, 2020). Because of its similar coefficient of thermal expansion to dental alloys, it helps to avoid thermal stress when cooling after firing (Zhang and Kelly, 2017). An established method for microscopically roughening the fitting surface is hydrofluoric acid (HF) etching. The cement-ceramic bond will also be strengthened by aluminum oxide sandblasting. Furthermore, silane promotes the link between the inorganic substrate (porcelain) and the organic polymers (resin cement) (El-Mowafy et al., 2018).
Lithium disilicate is bonded chemically and mechanically, with the latter resulting in defects on the internal surface (Moreno et al., 2019). The dissolution of a portion of the glassy phase during the etching process with HF reveals the material’s crystal structure and creates a layer suitable for micromechanical retention, allowing the application of a silane-containing solution (Torres et al., 2009). Silane is an efficient adhesion promoter that promotes chemical interaction between inorganic ceramic crystals and resin (Lima et al., 2024). Although dentists adopted HF because it was inexpensive and effective, it is considered harmful (Prado et al., 2018).
According to the manufacturer, clearfil ceramic primer plus (Kuraray Noritake Dental Inc., Sakazu, Kurashiki, Okayama, Japan) is another material that does not require HF and may be used with phosphoric acid. It is an adhesive primer made specifically for indirect restorative bonding. According to the manufacturer, the product is composed of ethanol, 10-Methacryloyloxydecyl dihydrogen phosphate (MDP), and 3-Methacryloxypropyl trimethoxysilane (MPTS). While the addition of MDP enables the material to attach to zirconia, MPTS creates the siloxane bond to ceramic (Moreno et al., 2019). According to Uğur et al. (2023), combining MPTS with MDP strengthens the interaction with ceramics.
The bond strength between resin composites and lithium disilicate ceramics after various surface treatments has been examined in the literature, however the results are contentious (Shoorgashti et al., 2024; AbuHaimed et al., 2022). The present study aimed to compare the effect of various surface treatments that does not necessitate the use of HF acid as an etchant in repairing silica-based ceramics on the shear bond strength (SBS) between resin composites and silica-based ceramics. The null hypothesis was that there would be no significant difference in SBS obtained between the resin composite and feldspathic ceramic/lithium disilicate materials with the three types of surface treatments.
Methodology
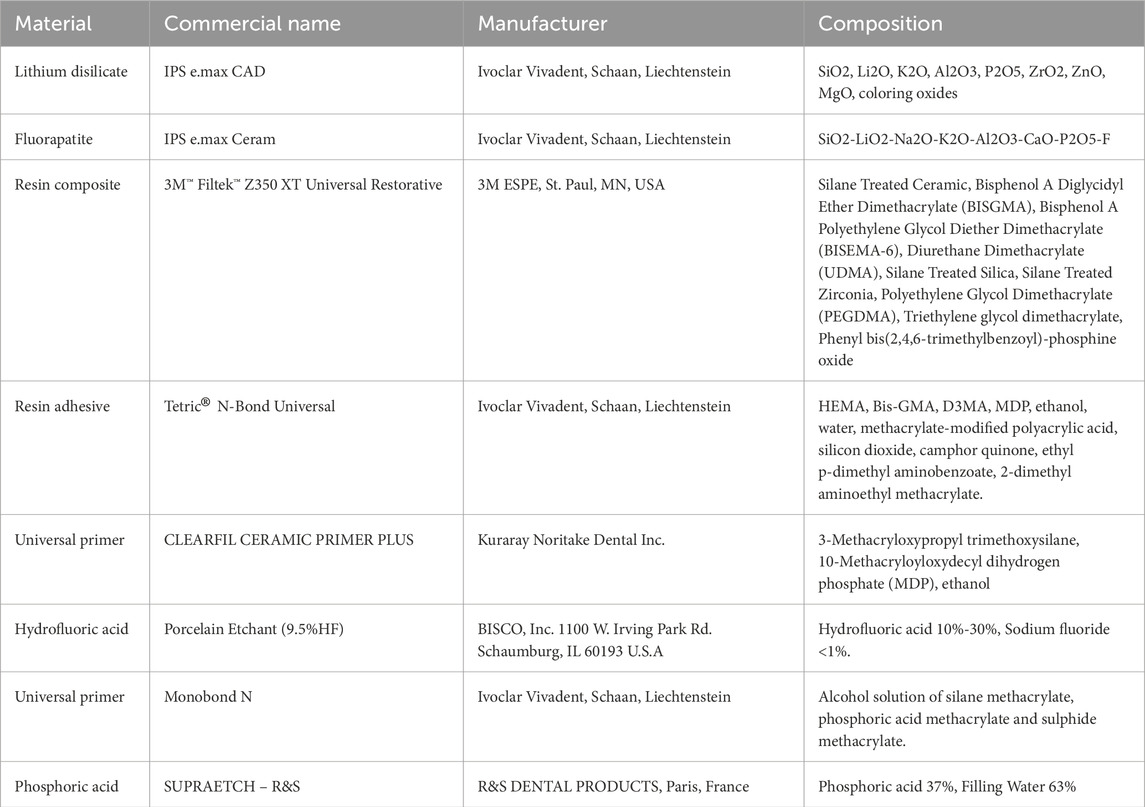
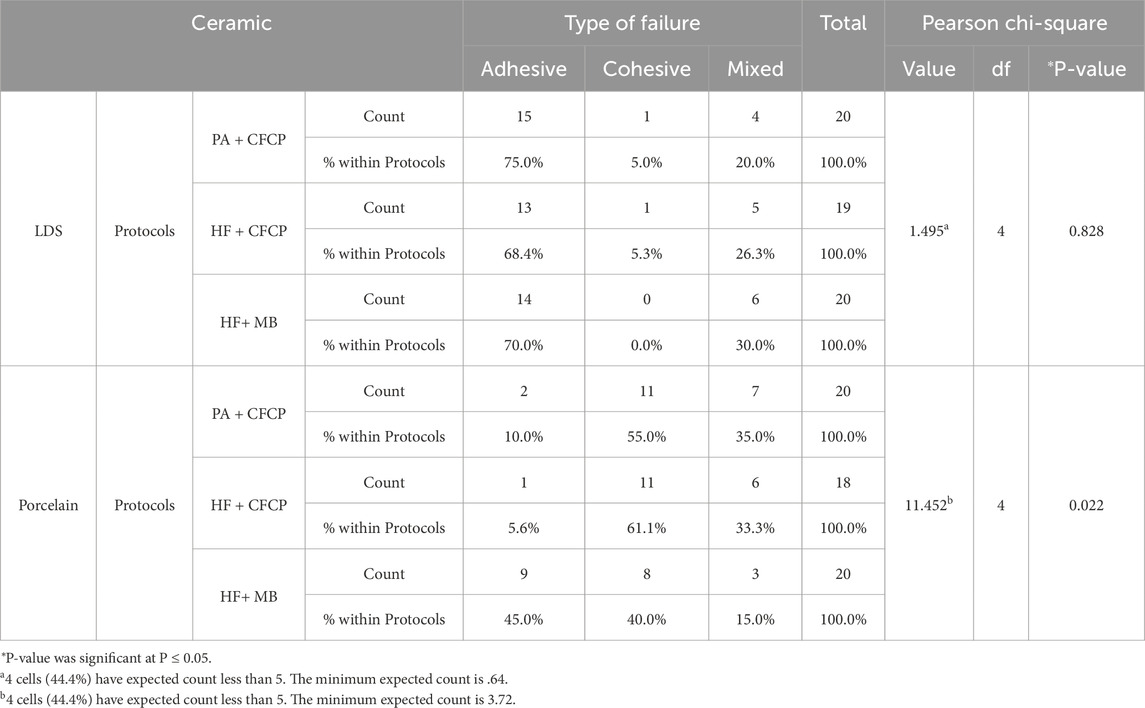
The materials that were used in this study are stated in Table 1 and the process summarized in Figure 1.
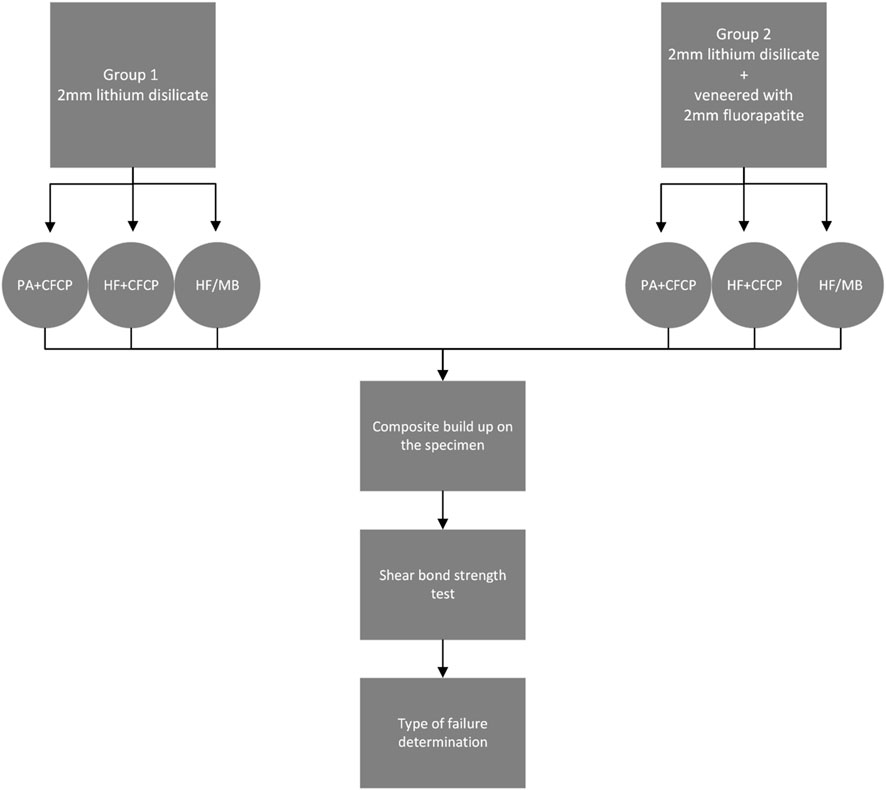
Figure 1. Flowchart of the specimen’s distribution and test groups. PA, phosphoric acid; CFCP, Clearfil ceramic prime plus; HF, Hydrofluoric acid; MB, Monobond N.
Specimen preparation
A total of 120 lithium disilicate square shaped blocks (IPS e.max CAD, Ivoclar Vivadent, Schaan, Liechtenstein) with dimensions of 10 × 10 × 2 mm were fabricated for this study. Each specimen was subjected to wet grinding using a polishing machine (Automat A, Jean Wirtz, West Germany) for 90 s with 600-, 1,000-, and 1,200-grit silicon carbide papers under cold water irrigation. Surface preparation was carried out using a 30 μm diamond rotary cutting tool (Isomet low-speed saw, Buehler, United States) with water irrigation for 10 s, followed by air drying with an oil-free air compressor. The specimens were randomly divided into two main groups (n = 60). The first group was used as core material only, while the second group was veneered with a 2 mm layer of fluoroapatite ceramic (IPS e.max Ceram, Ivoclar Vivadent, Schaan, Liechtenstein). Each main group was further subdivided into three subgroups, resulting in six subgroups in total (n = 20 per subgroup) (Figure 1). The materials used in the study are summarized in Table 1.
Surface treatments
Surface treatments of the ceramic specimens were performed in accordance with the specific recommendations provided by the manufacturers of each repair system, as outlined in Table 2. The protocols included mechanical surface roughening using 50 μm alumina powder followed by either phosphoric acid or HF etching, depending on the repair system. For specimens treated with CLEARFIL CERAMIC PRIMER PLUS, either phosphoric or HF was applied prior to primer application. In contrast, specimens treated with Monobond N underwent HF etching followed by the application of the silane coupling agent. All primers were applied immediately after dispensing and were air-dried using mild or strong oil-free air as specified. These surface treatments aimed to optimize adhesion between the ceramic surfaces and the repair materials.
Repair with resin composite
In a customized putty mold with a hole in the middle (3 mm in diameter, 2 mm in height) resin adhesive (Tetric® N-Bond Universal, Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied to the surface using microbrush and rubbed for 20 s, then oil- and moisture-free compressed air was used until a glossy, after that it was light cured for 10 s, then the infrastructural ceramic was gradually covered with a composite resin (3M™ Filtek™ Z350 XT Universal Restorative, 3M ESPE, St. Paul, MN, United States) that was condensed on it. Each composite layer was light-polymerized for 20 s at 1 mm from surfaces using a light-emitting diode LED (Bluephase, Ivoclae vivdent Schaan, Liechtenstein) 800 mW/cm2 power polymerizing unit.
Shear bond strength testing
To provide conditions like the oral environment. All specimens were kept in water at 37 °C for 24 h, then thermocycled using thermocycling machine (SD Mechatrinik GmbH, Feldkirchen-Westerham, Bayern, Germany) at temperatures 5 °C–55 °C for 5,000 cycles with a 30-s dwell time. Customized mold was used to fix and seat the specimen in the shear testing jig. Mechanical testing equipment (Instron, Universal testing machine, Instron Corporation, Norwood, Massachusetts, United States) was used to measure the shear bond strengths with a crosshead speed of 0.5 mm/min. Megapascals (MPa) was used to translate the data from Newton as shown in Figure 2.
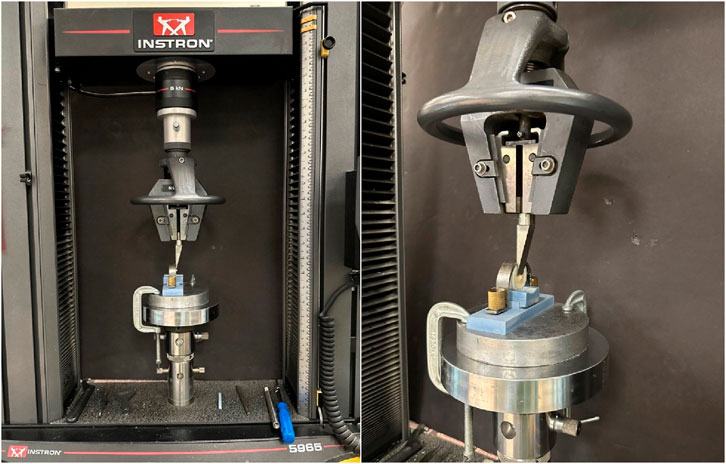
Figure 2. Specimens locked for shear bond strength testing in the universal instron testing machine.
Failure analysis
Scanning electron microscopy was used to study the specimen’s surface. To improve conductivity, a 15 nm coating of gold was applied to the samples. After that, the specimen was analyzed with a scanning electron microscope (SEM) Phenom-WorldTM (Phenom-World B.V. Dillenburgstraat 9T, Eindhoven 5652 AM, Netherlands) working in the secondary electron mode at a voltage of 15 kV. In addition to digital stereo microscope (Hirox, KH-7700, Tokyo, Japan). According to the manner of failure, the failure may be adhesive when it occurs at the substrate-resin interface, cohesive when it occurs inside the substrate or in the resin composite, or mixed-areas of adhesive and cohesive failure as shown in Figure 3.
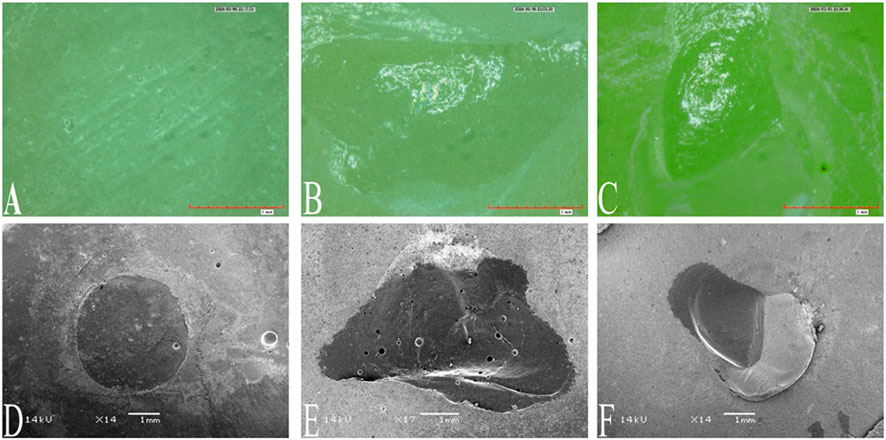
Figure 3. Types of failure. (A,D) showing an adhesive failure. (B,E) Showing cohesive failure. (C,F) showing mixed failure.
Statistical analysis
Two-way analysis of variance (ANOVA) was used in addition to one-way ANOVA and t-test. However, the level of significance was set at alpha 0.05 for any statistical test p-value less than that considered significant. For the failure analysis chi-square was used. Collected data entered IBM SPSS ve 26 for statistical Analysis.
Results
The investigation revealed statistically significant variations in SBS values among the three surface treatment protocols, highlighting the critical role of surface preparation in optimizing the bond between resin composites and lithium disilicate ceramics.
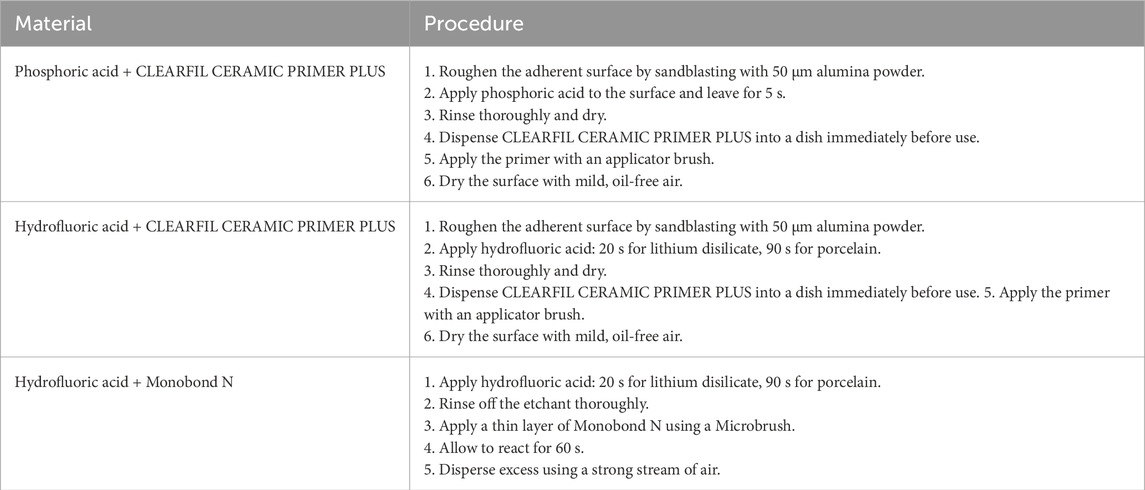
A two-way ANOVA was used to compare the effects of ceramic type and surface treatment process on SBS, as shown in Table 3. The independent factors were ceramic type and surface treatment process, and the dependent variable was the measured SBS. The analysis found that both ceramic type and the interaction between ceramic type and protocol had a statistically significant effect on SBS values (p < 0.05). Given the magnitude of the interaction effect, a one-way ANOVA was used to analyze and find specific subgroup differences across the ceramic types and surface treatments.
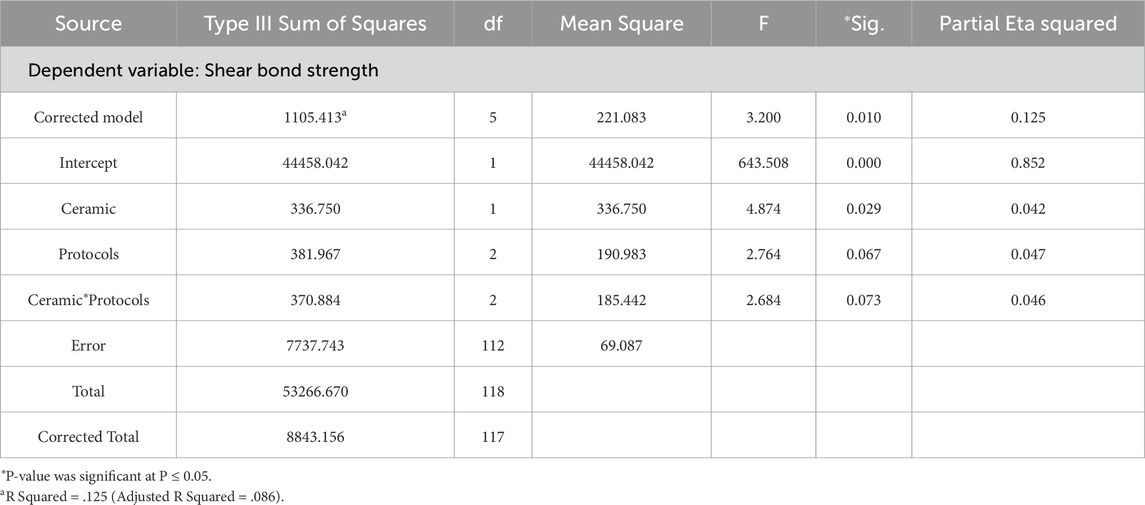
The SBS values for repaired ceramics using different surface treatment protocols are summarized in Table 4 and illustrated in Figure 4. For lithium disilicate, three surface treatment protocols were evaluated: phosphoric acid followed by Clearfil Ceramic Primer Plus (PA + CFCP), HF followed by Clearfil Ceramic Primer Plus (HF + CFCP), and HF followed by Monobond N (HF + MB). The mean SBS values for LDS were 17.36 ± 10.30 MPa for PA + CFCP, 22.90 ± 9.56 MPa for HF + CFCP, and 23.09 ± 8.93 MPa for HF + MB. The same protocols were also applied to porcelain specimens, yielding mean SBS values of 17.53 ± 7.61 MPa for PA + CFCP, 20.75 ± 6.04 MPa for HF + CFCP, and 14.92 ± 6.27 MPa for HF + MB. Each group consisted of 20 specimens, except for the HF + CFCP group in the porcelain category, which included 18 specimens due to sample loss. Statistical analysis indicated no significant differences in SBS among the protocols within the lithium disilicate group. However, a significant difference was observed among the surface treatment protocols in the porcelain group (p < 0.05). Post hoc analysis using Tukey’s Multiple Comparison Test revealed a statistically significant difference between the HF + CFCP and HF + MB protocols in the porcelain group, with HF + CFCP demonstrating superior bond strength.
In addition to bond strength values, Table 5 also presents the distribution of failure modes observed for each surface treatment protocol, along with the results of the Pearson Chi-Square tests. Failure modes were classified into three categories: adhesive, cohesive, and mixed. For lithium disilicate, the Chi-Square analysis revealed no statistically significant differences in the distribution of failure types among the three protocols (χ2 = 1.495, df = 4, p = 0.828), indicating that the nature of bond failure was relatively consistent regardless of the surface treatment used. In contrast, porcelain specimens demonstrated a significant difference in failure mode distribution across the protocols (χ2 = 11.452, df = 4, p = 0.022). This suggests that surface treatment had a measurable impact not only on bond strength but also on the type of failure observed. Specifically, the HF + CFCP group in the porcelain specimens showed a higher incidence of mixed failures, which typically reflect stronger, more reliable bonding, while the HF + MB group showed a greater proportion of adhesive failures, consistent with its lower bond strength. These findings further support the conclusion that the effectiveness of bonding protocols may differ based on ceramic type and should be carefully selected to optimize both bond strength and failure mode performance.
Discussion
Given the critical role of bond integrity in the success of ceramic repair, this study aimed to evaluate the effect of different surface treatment protocols on the SBS between resin composites and silica-based ceramics, specifically lithium disilicate and porcelain. A particular focus was placed on exploring alternatives to HF, which, despite its effectiveness, presents notable handling and safety concerns in clinical practice. According to the manufacturer, Clearfil Ceramic Primer Plus may be used in conjunction with phosphoric acid as a safer substitute for HF, provided that sandblasting is performed to enhance surface roughness. To investigate this, three surface treatment protocols were compared: (1) phosphoric acid combined with Clearfil Ceramic Primer Plus (PA + CFCP), (2) HF combined with Clearfil Ceramic Primer Plus (HF + CFCP), and (3) HF combined with Monobond N (HF + MB). Notably, the HF + MB group was treated without sandblasting to assess its potential as a simplified and time-efficient clinical alternative. The selection of fluoroapetite and lithium disilicate as test substrates reflects their widespread use in modern restorative dentistry, making the findings clinically relevant for guiding evidence-based repair strategies.
The findings of this study underscore the critical role of surface treatment techniques in influencing the SBS between resin composites and ceramic substrates, particularly in fluoroapatite-based ceramics. While the different surface treatment protocols applied to lithium disilicate did not show statistically significant differences, all three methods yielded relatively high SBS values. This suggests that lithium disilicate may be more tolerant or uniformly responsive to a range of bonding protocols. In contrast, fluoroapatite ceramics demonstrated greater variability in bonding performance depending on the surface treatment used. Notably, the HF + MB protocol resulted in significantly lower bond strength compared to HF + CFCP, highlighting the importance of primer selection in optimizing adhesion. This difference may be attributed to variations in the chemical composition and silane coupling efficiency between Monobond N and Clearfil Ceramic Primer Plus. The superior performance of the HF + CFCP protocol in the fluoroapatite group aligns with previous research emphasizing the necessity of appropriate silane application after etching to enhance bond durability (Dimitriadi et al., 2020). Overall, these findings emphasize the importance of tailoring surface treatment strategies to the specific ceramic material to achieve consistent and long-lasting adhesion in clinical practice.
Maawadh et al. (2020) highlight that replacing fractured ceramic restorations can be both challenging and costly, in addition to being an aggressive approach. An alternative solution involves the use of resin composites for ceramic repair, which are more cost-effective and offer easier handling (Ueda et al., 2021). Although the conventional method—combining HF with silane—is widely used, it presents several drawbacks, including toxicity and limited suitability for intraoral application (Prado et al., 2018). HF works by dissolving the glassy phase of the ceramic, thereby enhancing micromechanical retention and improving bond strength (Campos et al., 2016). Interestingly, the study observed that applying Clearfil Ceramic Primer Plus after sandblasting resulted in comparable outcomes regardless of whether phosphoric acid or HF was used. This may be attributed to the initial sandblasting process, which creates surface roughness, followed by acid etching that further enhances surface reactivity.
The analysis of failure modes offers valuable additional insight into the performance and reliability of the bonding protocols evaluated in this study. Failure types were classified as adhesive, cohesive, or mixed, allowing for a qualitative assessment of bond integrity alongside quantitative SBS measurements. For lithium disilicate, no significant differences in failure mode distribution were observed among the treatment groups, indicating that all protocols provided a similar level of bonding reliability. This consistency may be attributed to the inherently favorable bonding characteristics of lithium disilicate ceramics, which are generally responsive to a wide range of surface treatments.
In contrast, the porcelain (fluoroapatite) group demonstrated significant variation in failure mode distribution depending on the surface treatment applied, suggesting a greater sensitivity to protocol selection. Notably, the HF + Clearfil Ceramic Primer Plus (HF + CFCP) protocol resulted in a higher proportion of mixed failures—typically considered indicative of stronger, more stable bonds. In comparison, the HF + Monobond N (HF + MB) group showed a predominance of adhesive failures, which correlated with its lower SBS values and suggest a weaker bond. These findings underscore the critical role that the interaction between ceramic type and surface treatment protocol plays in determining both bond strength and failure behavior. Clinically, they highlight the importance of selecting a surface treatment approach that is specifically tailored to the ceramic substrate in order to achieve durable and predictable restoration outcomes.
The results of this investigation indicate that the use of Clearfil Ceramic Primer Plus in combination with either hydrofluoric or phosphoric acid and sandblasting yields SBS values for lithium disilicate that are comparable to those achieved with the HF + Monobond N protocol. In the case of porcelain, however, protocols involving Clearfil Ceramic Primer Plus demonstrated superior outcomes compared to the HF + Monobond N method. With regard to failure modes, adhesive failure was the most common type observed in the lithium disilicate group, with no statistically significant differences among the protocols. In contrast, the porcelain group showed significant variation in failure modes depending on the treatment protocol. Cohesive failure was most frequently observed in the sandblasting groups, aligning with the findings of Moravej-Salehi et al. (2016), who also reported a predominance of cohesive failures following sandblasting.
Uğur et al. (2023) concluded that bond strength is enhanced when methacryloyloxydecyl dihydrogen phosphate (MDP) and methacryloyloxypropyl trimethoxysilane (MPTS) are combined. Similarly, Carrilho et al. (2019) reported that 10-MDP adhesives can result in strong and durable bonding. Given its effectiveness with porcelain and its comparable performance to the Monobond N + HF combination in lithium disilicate, these findings support the broader use of Clearfil Ceramic Primer Plus with various etching agents. Sandblasting, as noted by Zarone et al. (2019), is an effective technique for generating surface micro-irregularities in lithium disilicate, which enhances micromechanical retention. Additionally, sandblasting can enhance bonding to porcelain, according to Moravej-Salehi et al. (2016). These findings imply that sandblasting, especially in procedures utilizing Clearfil Ceramic Primer Plus, significantly strengthens bonds. Similar outcomes were found in the study conducted by Bessa et al. (2025). According to their findings, surface treatment had a nearly significant effect on the SBS, although cleaning technique and age had a substantial impact. MEP showed to be a practical, less hazardous substitute for HF + silane, and higher SBS values were obtained by air-particle abrasion with Al2O3 and the application of Ivoclean. Bond strength was adversely affected by thermocycling, especially in those that received HF treatment.
This study was conducted under controlled laboratory conditions, which, while essential for standardization and reproducibility, may not fully replicate the complex environment of the oral cavity. Therefore, one limitation is the lack of in vivo validation, which would provide a more realistic assessment of the clinical performance and long-term durability of the tested bonding protocols. Future in vivo studies are recommended to evaluate how factors such as saliva, temperature fluctuations, occlusal forces, and oral microbiota influence bond strength and restoration longevity. Another limitation is that the study did not account for the potential formation of microcracks induced by the sandblasting process. These microcracks could compromise the structural integrity and long-term durability of ceramic restorations after repair. Investigating the extent and clinical significance of sandblasting-induced damage in future research would provide valuable insights into optimizing surface treatment techniques without adversely affecting ceramic strength. Additionally, incorporating sandblasting into the HF + Monobond N (HF + MB) group could offer further clarity. It would be beneficial to examine whether the introduction of mechanical surface roughening in this group enhances bond performance, as seen in other protocols. This modification could help determine whether the lower bond strength observed with HF + MB was due to the absence of sandblasting or other material-specific factors.
Conclusion
Within the limitations of this study, it can be concluded that:
• Clearfil Ceramic Primer Plus offers a promising alternative to traditional hydrofluoric acid-based surface treatments. When used over lithium disilicate ceramics for repair with composite resin, it demonstrated shear bond strength comparable to that achieved with hydrofluoric acid etching, suggesting it may serve as a safer and effective substitute.
• Furthermore, in the case of fluoroapatite/porcelain, Clearfil Ceramic Primer Plus produced superior shear bond strength with composite resin as compared to the conventional hydrofluoric acid and silane protocol, indicating its potential as a more reliable and efficient surface treatment option for both ceramic types.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
AAi: Project administration, Resources, Writing – original draft, Data curation, Supervision, Conceptualization, Writing – review and editing, Methodology. AAl: Data curation, Investigation, Methodology, Writing – original draft. MA: Writing – original draft, Data curation, Methodology, Investigation. AAn: Methodology, Data curation, Investigation, Writing – original draft. KA: Data curation, Methodology, Writing – original draft, Investigation. TA: Methodology, Writing – original draft, Investigation, Data curation. SH: Funding acquisition, Writing – review and editing, Formal Analysis, Software.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The research was funded by Ongoing Research Funding Program (ORF-2025-950), King Saud University, Riyadh, Saudi Arabia.
Acknowledgments
The authors appreciate the support from Ongoing Research Funding Program (ORF-2025-950), King Saud University, Riyadh, Saudi Arabia.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
AbuHaimed, T. S., Alzahrani, S. J., Farsi, S. A., AL-Turki, L. E., and Hajjaj, M. S. (2022). The effect of repeated pressing on the flexural strength, color stability, vickers hardness, and surface topography of heat-pressed lithium disilicate. Materials 15 (19), 6787. doi:10.3390/ma15196787
Bessa, M. S., Marinho, L. C. N., Miranda, L. M., Carvalho, I. H. G., Campos, B. O., Borges, B. C. D., et al. (2025). Repair bond strength of resin composite to CAD/CAM glass-ceramic: influence of cleaning methods, surface treatments, and aging. J. Dent. 154, 105568. doi:10.1016/j.jdent.2025.105568
Campos, F., Almeida, C. S., Rippe, M. P., De Melo, R. M., Valandro, L. F., and Bottino, M. A. (2016). Resin bonding to a hybrid ceramic: effects of surface treatments and aging. Oper. Dent. 41 (2), 171–178. doi:10.2341/15-057-L
Carrilho, E., Cardoso, M., Ferreira, M. M., Marto, C. M., Paula, A., and Coelho, A. S. (2019). 10-MDP based dental adhesives: adhesive interface characterization and adhesive stability-A systematic review. Materials 12, 790. doi:10.3390/ma12050790
Dimitriadi, M., Zinelis, S., Zafiropoulou, M., Silikas, N., and Eliades, G. (2020). Self-Etch silane primer: reactivity and bonding with a lithium disilicate ceramic. Mater. (Basel) 13 (3), 641. doi:10.3390/ma13030641
El-Mowafy, O., El-Aawar, N., and El-Mowafy, N. (2018). Porcelain veneers: an update. Dent. Med. Problems 55, 207–211. doi:10.17219/dmp/90729
Forster, A., Ungvári, K., Györgyey, Á., Kukovecz, Á., Turzó, K., and Nagy, K. (2014). Human epithelial tissue culture study on restorative materials. J. Dent. 42 (1), 7–14. doi:10.1016/j.jdent.2013.11.008
Lima, R. B. W., Muniz, I. A. F., Campos, D. E. S., Murillo-Gómez, F., Andrade, A. K. M., Duarte, R. M., et al. (2024). Effect of universal adhesives and self-etch ceramic primers on bond strength to glass-ceramics: a systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 131 (3), 392–402. doi:10.1016/j.prosdent.2022.01.011
Maawadh, A. M., Almohareb, T., Al-Hamdan, R. S., Al Deeb, M., Naseem, M., Alhenaki, A. M., et al. (2020). Repair strength and surface topography of lithium disilicate and hybrid resin ceramics with LLLT and photodynamic therapy in comparison to hydrofluoric acid. J. Appl. Biomaterials Funct. Mater. 18, 2280800020966938. doi:10.1177/2280800020966938
Moravej-Salehi, E., Moravej-Salehi, E., and Valian, A. (2016). Surface topography and bond strengths of feldspathic porcelain prepared using various sandblasting pressures. J. Investigative Clin. Dent. 7 (4), 347–354. doi:10.1111/jicd.12171
Moreno, M. B. P., Murillo-Gómez, F., and de Goes, M. F. (2019). Physicochemical and morphological characterization of a glass ceramic treated with different ceramic primers and post-silanization protocols. Dent. Mater. 35 (8), 1073–1081. doi:10.1016/j.dental.2019.05.003
Prado, M., Prochnow, C., Maria, A., Marchionatti, E., Baldissara, P., Valandro, F., et al. (2018). Ceramic surface treatment with a single-component primer: resin adhesion to glass ceramics. J. Adhes. Dent. 20 (2), 99–105. doi:10.3290/j.jad.a40303
Shi, H. Y., Pang, R., Yang, J., Fan, D., Cai, H. X., Jiang, H. B., et al. (2022). Overview of several typical ceramic materials for restorative dentistry. BioMed Res. Int. 2022, 8451445. doi:10.1155/2022/8451445
Shoorgashti, R., Ehsani, S. S., Ducret, M., and Rokhshad, R. (2024). Effect of surface treatments on the bond strength of computer-aided design and computer-aided manufacturing lithium disilicate to restorative materials: a systematic review. Eur. J. Prosthodont Restor. Dent. 32 (4), 423–433. doi:10.1922/EJPRD_2777Shoorgashi11
Torres, S. M. P., Borges, G. A., Spohr, A. M., Cury, A. A. D. B., Yadav, S., and Platt, J. A. (2009). The effect of surface treatments on the micro-shear bond strength of a resin luting agent and four all-ceramic systems. Oper. Dent. 34 (4), 399–407. doi:10.2341/08-87
Ueda, N., Takagaki, T., Nikaido, T., Takahashi, R., Ikeda, M., and Tagami, J. (2021). The effect of different ceramic surface treatments on the repair bond strength of resin composite to lithium disilicate ceramic. Dent. Mater. J. 40 (5), 1073–1079. doi:10.4012/dmj.2020-362
Uğur, M., Kavut, İ., Tanrıkut, Ö. O., and Cengiz, Ö. (2023). Effect of ceramic primers with different chemical contents on the shear bond strength of CAD/CAM ceramics with resin cement after thermal ageing. BMC Oral Health 23 (1), 210. doi:10.1186/s12903-023-02909-z
Warreth, A., and Elkareimi, Y. (2020). All-ceramic restorations: a review of the literature. Saudi Dent. J. 32, 365–372. doi:10.1016/j.sdentj.2020.05.004
Zarone, F., Di Mauro, M. I., Ausiello, P., Ruggiero, G., and Sorrentino, R. (2019). Current status on lithium disilicate and zirconia: a narrative review. BMC Oral Health 19 (1), 134. doi:10.1186/s12903-019-0838-x
Keywords: shear bond strength (SBS), surface treatments, hydrofluoric acid etching, lithium disilicate, air-particle abrasion, resin composite
Citation: Alqahtani A, AlHelal AA, Almutairi M, Alhassoon A, Alshahrani K, Alshahrani T and Habib SR (2025) Shear bond strength of resin composite to silica-based ceramic: a comparative study of different surface treatments. Front. Mater. 12:1654956. doi: 10.3389/fmats.2025.1654956
Received: 27 June 2025; Accepted: 11 August 2025;
Published: 29 August 2025.
Edited by:
Govindan Suresh Kumar, PSG College of Arts and Science, IndiaReviewed by:
Naresh Kumar, Dow University of Health Sciences, PakistanMuhammad Saad Shaikh, Jinnah Sindh Medical University, Pakistan
Copyright © 2025 Alqahtani, AlHelal, Almutairi, Alhassoon, Alshahrani, Alshahrani and Habib. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Syed Rashid Habib, c3loYWJpYkBrc3UuZWR1LnNh
 Abdulaziz Alqahtani1
Abdulaziz Alqahtani1 Syed Rashid Habib
Syed Rashid Habib