- 1Department of Health Sciences, University of Milan, Milan, Italy
- 2Prostate Cancer Program, Fondazione IRCCS Istituto Nazionale Dei Tumori, Milan, Italy
- 3Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy
- 4Department of Biomedical Sciences, Humanitas University, Milan, Italy
Background: Several studies have highlighted the benefits of empathy in healthcare settings. A correlation between clinicians’ empathy and patients’ adherence and satisfaction, as well as the ability for the clinician to accurately assess family members’ needs, has been found. However, empathy is often seen by clinicians as a risk factor for their wellbeing. This study aims to assess whether the level of empathy of clinicians working in critical care settings may expose them to moral distress, poor job satisfaction, and intention to quit their job.
Methods: Italian clinicians who attended the 2016 “Smart Meeting Anesthesia Resuscitation in Intensive Care” completed the Empathy Quotient questionnaire, the Moral Distress Scale-Revised, and two questions assessing job satisfaction and intention to quit the job. Multiple linear and logistic regressions were performed to determine if clinicians’ empathy influences moral distress, job satisfaction, and intention to quit. Age, gender, and profession were used as control variables.
Results: Out of 927 questionnaires distributed, 216 were returned (23% response rate) and 210 were used in the analyses. Respondents were 56% physicians, 24% nurses, and 20% residents. Over half of the clinicians (58%) were female. Empathy resulted the only significant predictor of job satisfaction (β = 0.193; p < 0.05). None of the variables included in the model predicted moral distress.
Conclusion: Empathy determined neither moral distress nor intention to quit. Findings suggest that empathy is not a risk factor for critical care clinicians in developing moral distress and the intention to quit their job. On the contrary, empathy was found to enhance clinicians’ job satisfaction.
Introduction
In psychology, the therapist’s empathy is widely acknowledged as a pivotal factor to promote patient change (Rogers, 1957). Definitions of empathy have varied (Bohart and Greenberg, 1997), though they generally have emphasized the therapist’s ability to understand the patient’s experience and feelings, and communicate this understanding to the patient (Rogers, 1957; Truax and Carkhuff, 1967). Empathy is generally described as a multidimensional construct encompassing an affective and a cognitive dimension (Baron-Cohen and Wheelwright, 2004). The affective dimension is described as feeling the patient emotions as if they were your own, but without ever losing the “as if” quality, and responding to the patient emotion with similar and appropriate emotions (Rogers, 1975). The cognitive dimension refers to the intellectual ability to understand the patient inner frame of reference, and is therefore related to the development of the theory of mind (Gladstein, 1983; Duan and Hill, 1996). Psychological literature generally distinguishes empathy from other related emotional responses, such as sympathy and personal distress. Sympathy or empathic concern has been defined as the feeling of sorrow or concern for the other person (Batson and Coke, 1983). The focus of the emotion is on the other person and differently from empathy, sympathy does not imply an exact match between one’s own emotions and the emotions of the other (Lennon and Eisenberg, 1987). Personal distress is the feeling of discomfort or self-concern that a person may feel in front of the other’s suffering. As the focus of the emotion is on the self rather than on the other, the experience of personal distress is unlikely to lead to altruistic behavior (Lennon and Eisenberg, 1987).
Several studies highlighted the benefits that empathy has for both patients and clinicians in healthcare settings. Clinicians’ empathy was found to be related to better clinical outcomes in diabetic patients (Hojat et al., 2011; Del Canale et al., 2012), increased patient satisfaction (Derksen et al., 2013), and a more accurate assessment of family members’ needs (Murphy et al., 1992; Moghaddasian et al., 2013). Other studies proved that empathy may be beneficial also for clinicians as it may promote self-efficacy and decrease burnout (Halpern, 2003; Krasner et al., 2009; Gleichgerrcht and Decety, 2013). Specifically, empathy was found to be inversely related to burnout among general practitioners (Torres et al., 2015) and medical students (Paro et al., 2014; von Harscher et al., 2017), and was found to decrease burnout and secondary traumatic stress among social workers (Wagaman et al., 2015).
Although the benefits of empathy in healthcare settings have been acknowledged, a series of studies highlighted that empathy generally diminishes during medical training as a result of the hidden curriculum and the experience in the actual healthcare environment (Hojat et al., 2009; Neumann et al., 2011). Clinicians frequently perceive empathy as a risk factor especially in those settings where closeness to death and suffering may be emotionally very difficult to manage, such as oncology, palliative, and critical care (Sanchez-Reilly et al., 2013; Riess, 2015). Clinicians may feel incapable of managing the emotions elicited in the encounter with critically ill patients (Picard et al., 2016) and therefore may prefer to engage in activities requiring little emotional investment (Hickey and Lewandowski, 1988; Stayt, 2007, 2009). This is particularly true if clinicians do not receive a training on emotions’ management or do not have the opportunity to discuss difficult cases during clinical supervisions (Berg et al., 1994).
Based on these premises, this study aims to assess whether the empathy of clinicians who work in critical care settings may be a risk factor for their psychological and occupational wellbeing. Specifically, we assessed if clinicians’ empathy predicted moral distress, poor job satisfaction, and intention to quit the job. Along with burnout, moral distress is another form of work-related distress which has been recently identified in the healthcare setting. Moral distress is the painful feeling that occurs when clinicians cannot carry out what they believe to be ethically appropriate (Lamiani et al., 2017a). Studies showed that moral distress is a relevant experience among critical care clinicians leading to depressive symptoms and job quitting (Lamiani et al., 2018). While a recent review confirmed that clinicians’ empathy is inversely correlated with burnout (Wilkinson et al., 2017), the relationship between empathy and moral distress has not been studied. Along with moral distress, we assessed the impact of clinicians’ empathy on job satisfaction and intention to quit the job. Job satisfaction and intention to quit are important outcomes of occupational wellbeing as they predict retention of healthcare professionals (Ellenbecker, 2004; De Gieter et al., 2011). Identifying factors that may promote clinicians’ job satisfaction and intention to remain is relevant for healthcare organizations which are striving to maintain a motivated workforce and reduce turnover (Lu et al., 2005).
Materials and Methods
Data Collection and Procedure
We conducted a cross-sectional study involving Italian critical care clinicians who attended the international conference “Smart Meeting Anesthesia Resuscitation in Intensive Care.” The conference was held in Milan, Italy, in May 2016. A survey composed of a series of questionnaires was developed to assess clinicians’ sociodemographic characteristics, empathy, moral distress, job satisfaction, and intention to quit the job. The survey was in Italian. Upon authorization by the Conference Scientific Committee, the survey was inserted in the Italian participants’ conference bags at registration. At the exit of the conference venue a desk was placed to collect completed surveys.
Participants
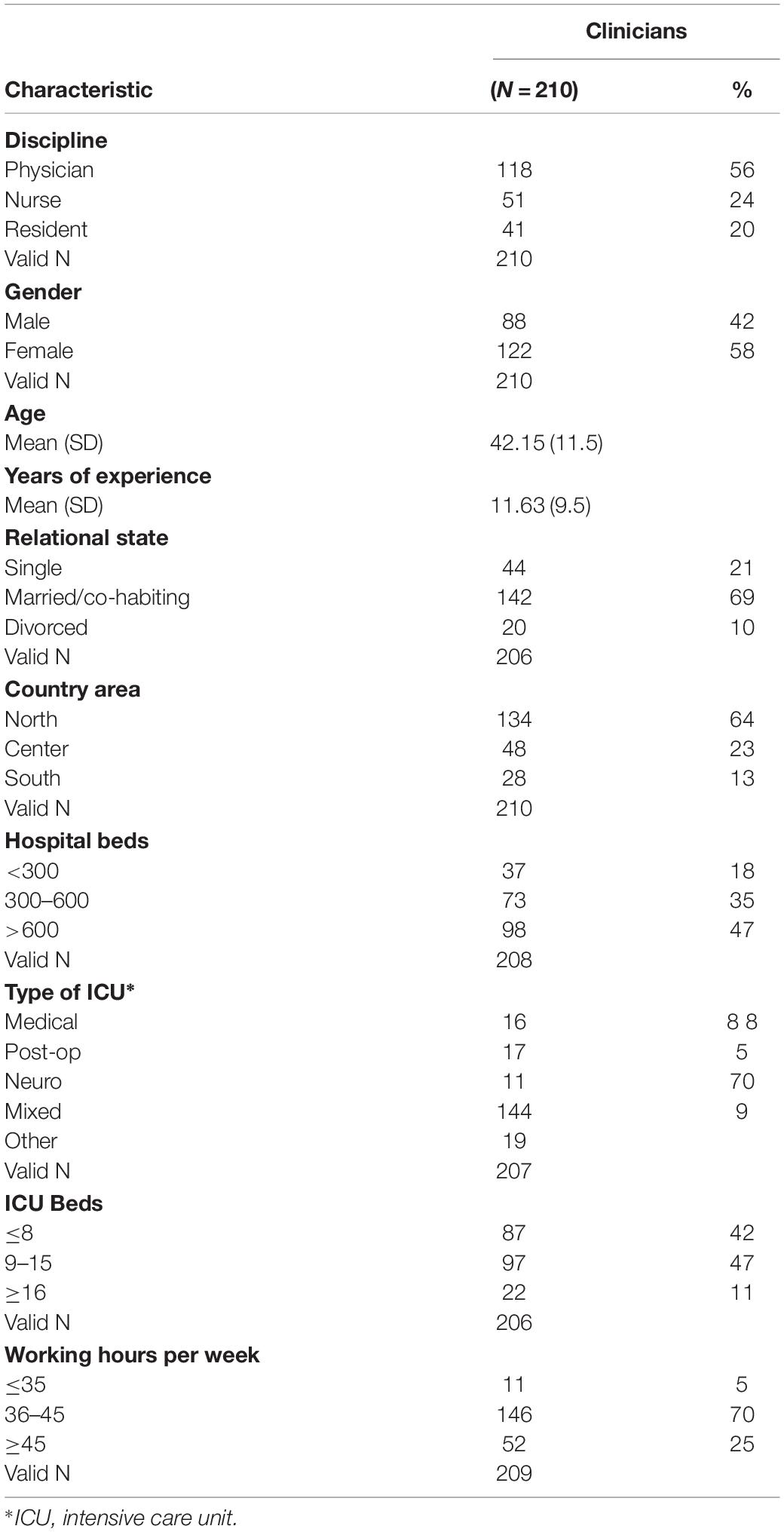
Participants were drawn from a convenience sample of 927 Italian clinicians (614 physicians, 138 nurses, and 175 residents) who attended the conference. Of these, 216 (23%) returned the survey. Of the 216 surveys returned, 6 could not be used in the analysis. Table 1 shows the sample characteristics of the 210 surveys used in the analysis. The majority of respondents were physicians (56%) and female (58%). Participants had a mean age of 42.15 years (SD = 11.5) and their average working experience amounted to 11.63 years (SD = 9.5). Over a half of participants were married/co-habiting (69%) and lived in the north of Italy (64%). Most participants (70%) worked 36–45 h per week in mixed ICUs (70%).
Ethics Statement
As the study did not involve patients and was purely observational, ethical approval was not required as per applicable institutional and national guidelines and regulations. The Scientific Committee of the SMART conference approved the survey administration. The study has been carried out in accordance with the Code of Ethics of the Declaration of Helsinki. All participants provided written informed consent granting permission to use the data for research purposes. The surveys were completely anonymous.
Measures
Empathy
The Italian validated version (Preti et al., 2011) of the empathic quotient (EQ) questionnaire was used to measure empathy. The EQ is a self-report questionnaire originally developed by Baron-Cohen and Wheelwright (2004) to provide a global measure of empathy, comprising the affective and cognitive dimensions (Lawrence et al., 2004). According to the authors of the measure, empathy is a multidimensional construct combining the ability to feel an appropriate emotion in response to another’s emotion and the ability to understand the others’ emotion (perspective-taking) and behave accordingly. Consistent with the theoretical framework of empathy, factor analysis revealed that the construct of empathy measured by the EQ comprises three factors: cognitive empathy, emotional reactivity, and social skills (Preti et al., 2011). However, a second-order factor analysis confirmed that the EQ scale has been developed to provide a global measure of empathy and many studies using EQ commonly report global scores (Baron-Cohen and Wheelwright, 2004; Bangash et al., 2013; Lachmann et al., 2018). The EQ is composed of 40 items measuring empathy and 20 filler-items. Responses to items are given on a four-point Likert scale ranging from 1 (strongly agree) to 4 (strongly disagree). Participants receive 0 for a non-empathic response, whatever the magnitude, and 1 or 2 for an empathic response depending on the strength of the reply. Responses on filler items are not included in the score counting. The EQ total score ranges from 0 to 80 with higher scores indicating a higher level of empathy. As we were interested in the global impact of empathy on clinicians’ wellbeing, the total empathy score was used in the analysis.
The Italian EQ has good internal consistency (Cronbach’s α = 0.79) and reliability (test–retest at 1 month Pearson’s r = 0.85) (Preti et al., 2011). In this study, Cronbach’s α-value for the EQ was 0.85.
Moral Distress
The Italian validated version of the Moral Distress Scale-Revised (MDS-R) (Hamric et al., 2012) was used to measure moral distress. The Italian MDS-R presented good reliability and psychometric properties (Lamiani et al., 2017b). The Italian MDS-R is composed of 14 items describing morally distressing situations. For each item, participants have to fill out a frequency scale, which assesses how often the situation is experienced, and an intensity scale, which measures how disturbing the situation is. Responses are given on a five-point Likert scale ranging from 0 (never) to 4 (very frequently) for the frequency scale, and from 0 (none) to 4 (great extent) for the intensity scale. The total MDS-R is obtained by summing the frequency × intensity scores and dividing the total by the number of items. The total score ranges from 0 to 16 with higher scores indicating a greater degree of moral distress. The Italian MDS-R scale has good internal consistency (Cronbach α = 0.81). In this study, Cronbach’s α-value for the MDS-R was 0.81.
Job Satisfaction
Job satisfaction was measured through the widely used one-item scale from Aiken et al. (2002) ranging from 1 (very unsatisfied) to 4 (very satisfied). This item has been used to assess job satisfaction in previous studies (Aiken et al., 2002; Dordoni et al., 2019).
Intention to Quit
Intention to quit was measured through the one-item question which is generally included at the end of the MDS-R. The question inquires if the person has ever thought of leaving or change his/her working position. The questions had two options (1 = No, I have never thought of leaving my position; 2 = Yes, I thought of leaving my position or I have already quit). This item has been used in several studies on moral distress (Hamric and Blackhall, 2007; Hamric et al., 2012).
Statistical Analysis
Statistical analysis was conducted using SPSS software for Window (22 version). First, descriptive analyses were conducted. Second, correlation analysis was run in order to examine bivariate correlations between study’s constructs and control variables (gender, age, discipline, working hours per week, and years of working experience). Multiple linear regression analyses were then conducted to investigate whether EQ predicted job satisfaction and moral distress. Multiple logistic regression was conducted to verify if the EQ predicted the intention to quit. In the regression models, we entered some covariates that were found in the literature to be significantly correlated with the study variables (gender, age, discipline, working hours per week, and years of working experience).
Results
Relationships Between Empathy, Moral Distress, Job Satisfaction, and Intention to Quit
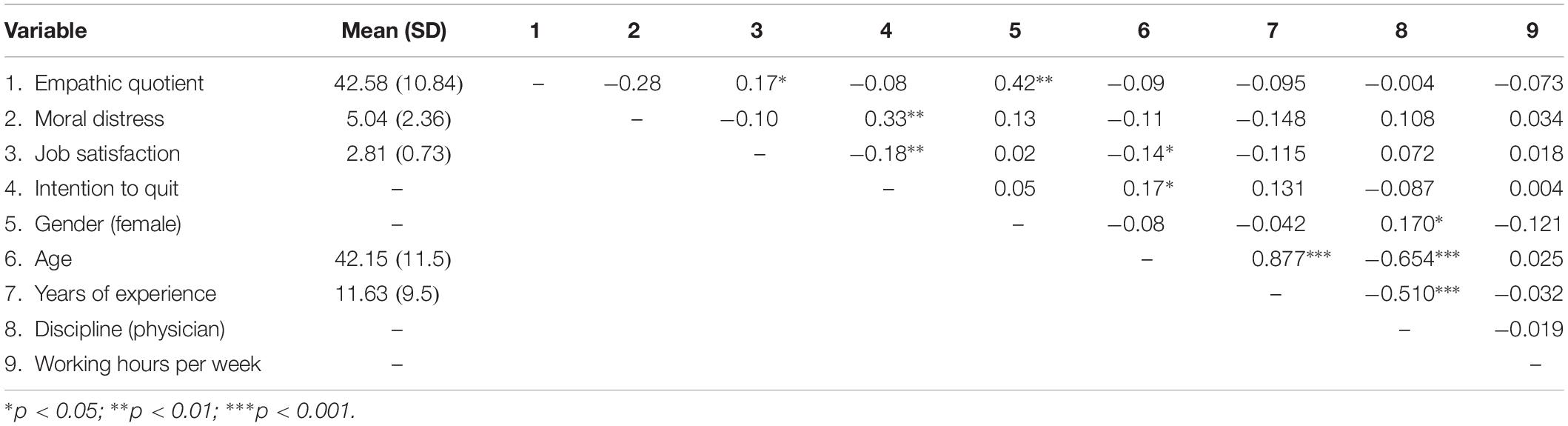
Table 2 shows means, standard deviations, and correlations between the study variables. Slightly over half of the participants (62%) stated that they would not quit their job, whereas 38% referred that they had thought of or had actually quit their job. Significant correlations were found between intention to quit and job satisfaction (r = −0.18, p < 0.01), and between intention to quit and moral distress (r = 0.33, p < 0.01). EQ was found to be related to job satisfaction (r = 0.17, p < 0.05).
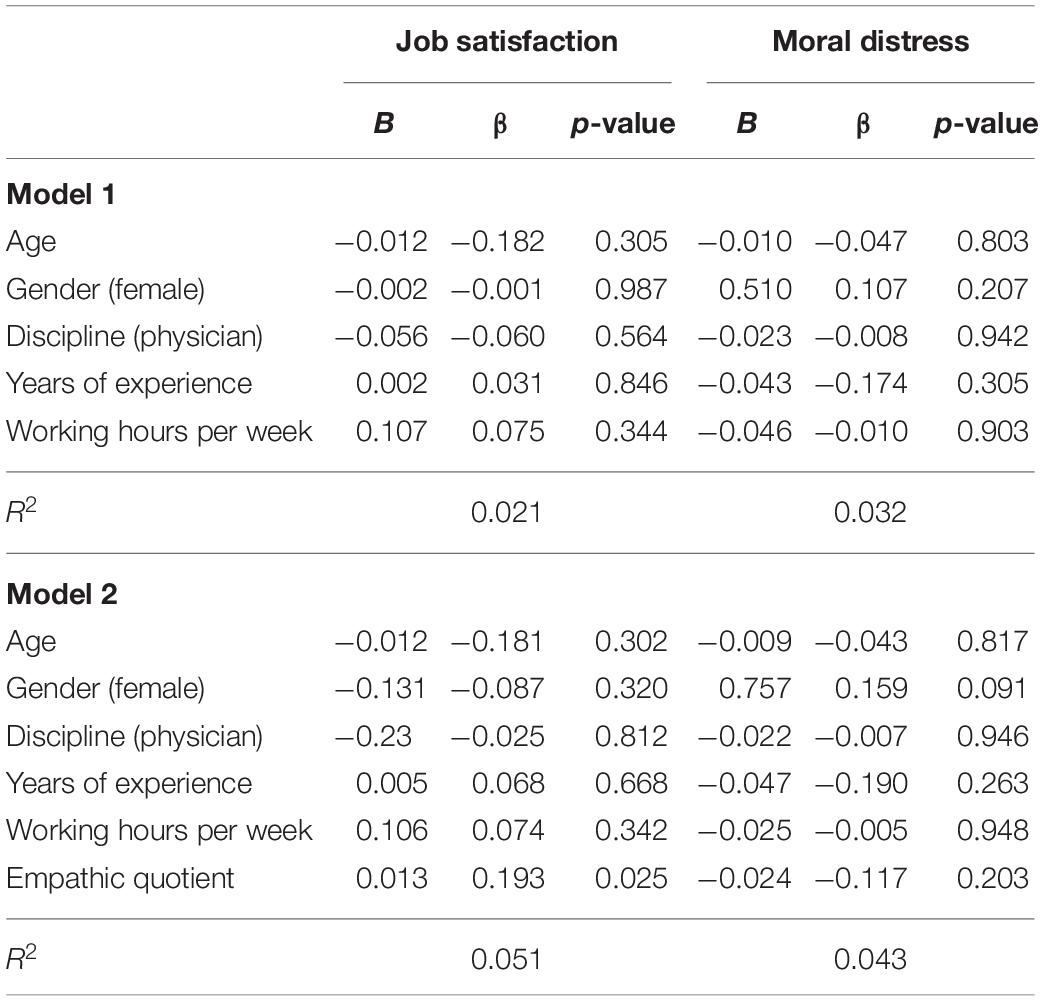
Stepwise multiple linear regression analysis was performed to explore the predictors of job satisfaction and moral distress (Table 3). EQ resulted to be the only significant predictor of job satisfaction (β = 0.193; p < 0.05), even when checking for covariates. None of the variables included in the model predicted moral distress.
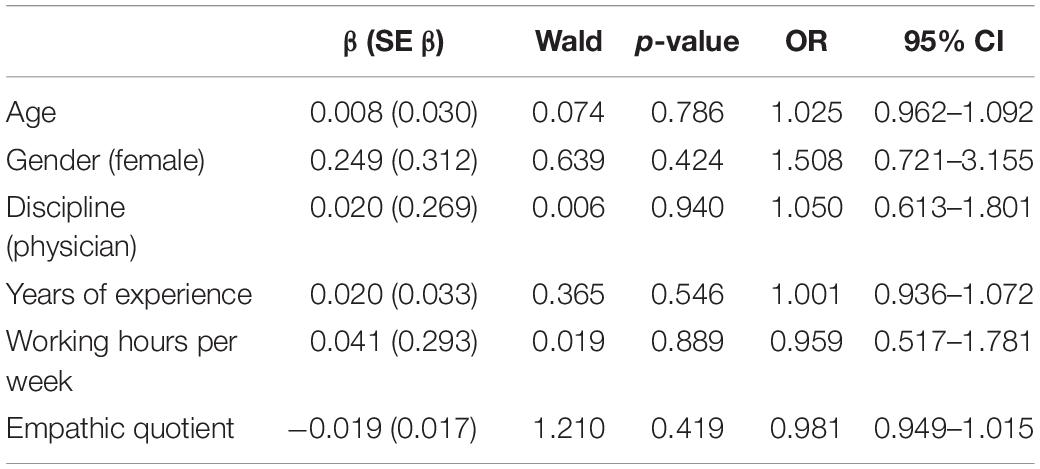
Multiple logistic regression models were run in order to test the effect of EQ on intention to quit the job (Table 4). Results showed no effect of EQ on intention to quit.
Discussion
Clinicians working in critical care settings are often exposed to emotionally and ethically challenging clinical situations (Donchin and Seagull, 2002). Recent studies showed that working in critical care settings may expose clinicians to stress-related conditions such as burnout, secondary traumatic stress, moral distress, and depression (Embriaco et al., 2007a, b, 2012; Berg et al., 2016; Moss et al., 2016; Lamiani et al., 2018). A common belief among clinicians is that being empathic could make them more vulnerable to the patients’ and families’ suffering and therefore may be a risk factor for their emotional wellbeing (Tanriverdi, 2013; Kerasidou and Horn, 2016). This study is the first to assess if empathy of clinicians working in a critical care setting could negatively affect their psychological and occupational wellbeing. Specifically, we assessed if empathy predicted moral distress, poor job satisfaction, and intention to quit the job.
Our findings suggest that empathy is not a risk factor for critical care clinicians’ wellbeing, as it does not predict moral distress or the intention to quit their job. On the contrary, empathy was found to enhance job satisfaction.
Specifically, we found that empathy does not predict moral distress nor correlates with it. Our findings suggest that empathy, as the capacity to perceive the internal frame of reference of another person with its emotional components (Rogers, 1959), may not be linked or lead to an increased violation of the clinician’s moral integrity. In other words, understanding and emotionally responding to the point of view of the other – be it a patient or a colleague – does not imply condescending to undertake professional actions that are perceived by clinicians as morally inappropriate. Consistently, the literature has increasingly acknowledged the need for clinicians to cultivate both empathy and moral resilience as pivotal qualities in patient care (Kerasidou and Horn, 2016; Rushton, 2016). Empathy may be accompanied by assertiveness and responsibility regarding the moral choices to carry on professionally, even if these may entail disagreements and misalignments with family members or colleagues (Halpern, 2007; Roeland et al., 2014). In the recent literature, this quality has been defined as “moral resilience.” Moral resilience is the capacity of an individual to sustain or restore his/her integrity in response to moral complexity, confusion, distress, or setbacks (Rushton, 2016). Moral resilience involves choosing how to respond to ethical challenges and uncertainty in ways that preserve one’s own integrity, minimize suffering, and allow to serve patients with highest purpose (Rushton, 2016).
Caring for critically or terminally ill patients often brings up the issue of clinicians’ emotional involvement and the related fear of being overwhelmed by the patients’ suffering. The common belief that empathy may be a risk factor for clinicians’ wellbeing probably lays in the confusion between empathy and sympathy (Kerasidou and Horn, 2016; Thirioux et al., 2016). Unlike sympathy, which entails an identification between self and the other (Thirioux et al., 2016), empathy implies the ability to enter the world of the other without losing the boundaries of the self and without confounding or identifying with the patient (Rogers, 1980). Empathy, therefore, is the ability to understand and feel the perspective of the other, without projecting one’s own emotions onto the other (Kerasidou and Horn, 2016). Despite some studies highlighted the positive effects of sympathy in promoting altruistic behaviors (Batson et al., 1987), other studies in the healthcare field showed that sympathy, rather than empathy, could expose clinicians to secondary traumatic stress (Crumpei and Dafinoiu, 2012) and lead to a disproportionate use of clinical resources (Nightingale et al., 1991). Crumpei and Dafinoiu (2012) found that sympathetic clinicians were more vulnerable to secondary traumatic stress than empathic clinicians, who did not report traumatic symptoms. Nightingale et al. (1991) found that sympathetic physicians, on average, had a greater preference for intubation, ordered more laboratory tests, and performed cardiopulmonary resuscitation for longer periods of time before declaring their efforts unsuccessful compared to empathic physicians. The literature shows that also the opposite tendency of sympathy, which is called alexithymia, may be problematic for clinicians’ wellbeing. Alexitimia is the difficulty to identify one’s own and the other’s emotions, which results in the tendency to ignore those emotions (Thirioux et al., 2016). Alexitimic traits were found to be associated with burnout and secondary traumatization among physicians (Gleichgerrcht and Decety, 2013). Specifically, Gleichgerrcht and Decety (2013) found that physicians who had difficulty in identifying emotions and regulating their negative arousal developed emotional exhaustion, detachment, and a low sense of accomplishment. Empathy, as the middle way between emotional over- and under involvement, seems protect clinicians from burnout and secondary traumatic stress (Torres et al., 2015; Wagaman et al., 2015). Consistently with the literature, our findings provide evidence that empathy is not a risk factor for developing moral distress.
Based on this study’s findings, we may hypothesize that other psychological factors, rather than empathy, may contribute to the development of moral distress, such as sympathy, lack of assertiveness, poor self-esteem, or lack of flexibility. As it happens in many stress-related conditions, also organizational factors may play an important role in contributing to moral distress, such as poor ethical climates, management styles, and working atmosphere. Further research should be conducted to assess these hypotheses.
In this study, we found that empathy does not predict clinicians’ intention to quit their job. On the contrary, it increases job satisfaction. In other words, more empathic clinicians reported being more satisfied with their job. Probably, the ability to feel and understand the perspective of the other allows clinicians to tailor their behaviors, negotiate different expectations, and therefore build more positive and satisfactory relationships with patients and colleagues. In the helping professions, where relationships play an important role, being empathic and thus being able to connect with patients without being overwhelmed, could constitute a source of job satisfaction. In the face of medicine’s limits and treatment failures, providing empathy to patients is sometimes the only source of meaning and healing (Sinclair et al., 2017).
This study has several limitations related to the research design and methodology. For what concerns the research design, as the literature lacks a model on moral distress, no underlying theory guided the choice of moral distress predictors. We explored the role of empathy, but we did not assess the role of other individual and organizational variables such as sympathy, assertiveness, and ethical climates in determining moral distress. Moreover, the use of the total empathy scores instead of the subscales’ scores may have covered the effect of emotional reactivity and cognitive empathy on moral distress, job satisfaction, and intention to quit. Due to the small sample size, no moderation nor mediation analyses have been conducted although these could have been informative. Even if in this study a direct relationship between empathy and moral distress was not found, future studies could assess the moderator or the mediator role of assertiveness and ethical climates. In addition, we assessed the effects of empathy only on moral distress, job satisfaction, and job quit, which are limited indicators of clinicians’ psychological and occupational wellbeing. For what concerns the methodology, our participants were drawn from a convenience sample of Italian clinicians who voluntarily completed the survey. This, along with the low response rate, may have introduced a self-selection bias and therefore the generalizability of our findings is limited. The findings are based on self-reported measures and therefore are subject to self-reported measures biases. Finally, the data were cross-sectional. Therefore, our conclusions have to be interpreted with caution, especially for what concerns the direction of causality.
Despite these limitations, our findings have important practical implications for healthcare organizations and for clinicians working in intensive care units. Empathy, as a protective factor for clinicians’ psychological and occupational wellbeing, should be cultivated and incorporated in the training of critical care clinicians. As empathy develops through experience and by increasing self-awareness of one’s identity and personal values and boundaries (Davis, 1990), it cannot be directly taught. Its development, however, can be cultivated and promoted by providing clinicians with experiential opportunities and appropriate resources. Clinical supervisions facilitated group discussions, simulated training programs with actors’ feedback and mindfulness training programs (Epstein et al., 2008; Sorensen and Iedema, 2009; Bell et al., 2014) can help clinicians to develop empathy by promoting self-reflection and opening up to different perspectives on patients care.
Data Availability Statement
The data that support the findings of this study are not publicly available. The informed consent signed by participants did not include the possibility to distribute the data to third parties.
Ethics Statement
As the study did not involve patients and was purely observational, ethical approval was not required as per applicable institutional and national guidelines and regulations. The Scientific Committee of the SMART conference approved the survey administration. The study has been carried out in accordance with The Code of Ethics of the Declaration of Helsinki. All participants provided written informed consent granting permission to use the data for research purposes. The surveys were completely anonymous.
Author Contributions
GL conceived and designed the research, supervised the work, acquired the data, analyzed and interpreted the data, and drafted and critically revised the manuscript. PD analyzed and interpreted the data, and drafted and critically revised the manuscript. EV conceived the research project, interpreted the data, and critically revised the manuscript. IB interpreted the data and critically revised the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Giovanni Mistraletti, MD, and Marika Pozzi, MS, for their assistance in data collection.
References
Aiken, L. H., Clarke, S. P., and Sloane, D. M. (2002). Hospital staffing, organization, and quality of care: cross-national findings. Nurs. Outlook 50, 187–194. doi: 10.1067/mno.2002.126696
Bangash, A. S., Ali, N. F., Shehzad, A. H., and Haqqi, S. (2013). Maintenance of empathy levels among first and final year medical students: a cross sectional study. F1000Research 2:157. doi: 10.12688/f1000research.2-157.v1
Baron-Cohen, S., and Wheelwright, S. (2004). The Empathy Quotient: an investigation of adults with Asperger syndrome or high functioning autism, and normal sex differences. J. Autism Dev. Disord. 34, 163–175. doi: 10.1023/b:jadd.0000022607.19833.00
Batson, C. D., and Coke, J. S. (1983). “Empathic motivation of helping behavior,” in Social Psychophysiology: A Source Book, eds J. T. Cacioppo, and K. E. Petty, (New York, NY: Guilford Press), 417–433.
Batson, C. D., Fultz, J., and Schoenrade, P. A. (1987). Distress and empathy: two qualitatively distinct vicarious emotions with different motivational consequences. J. Pers. 55, 19–39. doi: 10.1111/j.1467-6494.1987.tb00426.x
Bell, S. K., Pascucci, R., Fancy, K., Coleman, K., Zurakowski, D., and Meyer, E. C. (2014). The educational value of improvisational actors to teach communication and relational skills: perspectives of interprofessional learners, faculty, and actors. Patient Educ. Couns. 96, 381–388. doi: 10.1016/j.pec.2014.07.001
Berg, A., Hansson, U. W., and Hallberg, I. R. (1994). Nurses’ creativity, tedium and burnout during 1 year of clinical supervision and implementation of individually planned nursing care: comparisons between a ward for severely demented patients and a similar control ward. J. Adv. Nurs. 20, 742–749. doi: 10.1046/j.1365-2648.1994.20040742.x
Berg, G. M., Harshbarger, J. L., Ahlers-Schmidt, C. R., and Lippoldt, D. (2016). Exposing compassion fatigue and burnout syndrome in a trauma team: a qualitative study. J. Trauma Nurs. 23, 3–10. doi: 10.1097/JTN.0000000000000172
Bohart, A. C., and Greenberg, L. S. (1997). “Empathy: where are we and where do we go from here?,” in Empathy Reconsidered: New Directions in Psychotherapy, eds A. C. Bohart, and L. S. Greenberg, (Washington, DC: American Psychological Association), 419–450.
Crumpei, I., and Dafinoiu, I. (2012). The relation of clinical empathy to secondary traumatic stress. Procedia Soc. Behav. Sci. 33, 438–442. doi: 10.1016/j.sbspro.2012.01.159
Davis, C. M. (1990). What is empathy, and can empathy be taught? Phys. Ther. 70, 707–711. doi: 10.1093/ptj/70.11.707
De Gieter, S., Hofmans, J., and Pepermans, R. (2011). Revisiting the impact of job satisfaction and organizational commitment on nurse turnover intention: an individual differences analysis. Int. J. Nurs. Stud. 48, 1562–1569. doi: 10.1016/j.ijnurstu.2011.06.007
Del Canale, S., Louis, D. Z., Maio, V., Wang, X., Rossi, G., Hojat, M., et al. (2012). The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma. Italy. Acad. Med. 87, 1243–1249. doi: 10.1097/ACM.0b013e3182628fbf
Derksen, F., Bensing, J., and Lagro-Janssen, A. (2013). Effectiveness of empathy in general practice: a systematic review. Br. J. Gen. Pract. 63, e76–e84. doi: 10.3399/bjgp13X660814
Donchin, Y., and Seagull, F. J. (2002). The hostile environment of the intensive care unit. Curr. Opin. Crit. Care 8, 316–320. doi: 10.1097/00075198-200208000-00008
Dordoni, P., Kraus-Hoogeveen, S., van der Heijden, B., Peters, P., Setti, I., and Fiabane, E. (2019). Live to work or work to live? An age-moderated mediation model on the simultaneous mechanisms prompted by workaholism among healthcare professionals. Front. Psychol. 10:868. doi: 10.3389/fpsyg.2019.00868
Duan, C., and Hill, C. (1996). The current state of empathy research. J. Couns. Psychol. 43, 261–274. doi: 10.1037/0022-0167.43.3.261
Ellenbecker, C. H. (2004). A theoretical model of job retention for home health care nurses. J. Adv. Nurs. 47, 303–310. doi: 10.1111/j.1365-2648.2004.03094.x
Embriaco, N., Azoulay, E., Barrau, K., Kentish, N., Pochard, F., Loundou, A., et al. (2007a). High level of burnout in intensivists: prevalence and associated factors. Am. J. Respir. Crit. Care Med. 175, 686–692. doi: 10.1164/rccm.200608-1184OC
Embriaco, N., Papazian, L., Kentish-Barnes, N., Pochard, F., and Azoulay, E. (2007b). Burnout syndrome among critical care healthcare workers. Curr. Opin. Crit. Care 13, 482–488. doi: 10.1097/MCC.0b013e3282efd28a
Embriaco, N., Hraiech, S., Azoulay, E., Baumstarck-Barrau, K., Forel, J. M., Kentish-Barnes, N., et al. (2012). Symptoms of depression in ICU physicians. Ann. Intens. Care 2:34. doi: 10.1186/2110-5820-2-34
Epstein, R. M., Siegel, D. J., and Silberman, J. (2008). Self-monitoring in clinical practice: a challenge for medical educators. J. Contin. Educ. Health Profess. 28, 5–13. doi: 10.1002/chp.149
Gladstein, G. A. (1983). Understanding empathy: Integrating counseling, developmental, and social psychology perspectives. J. Couns. Psychol. 30, 467–482. doi: 10.1037/0022-0167.30.4.467
Gleichgerrcht, E., and Decety, J. (2013). Empathy in clinical practice: how individual dispositions, gender and experience moderate empathic concern, burnout and emotional distress in physicians. PLoS One 8:e61526. doi: 10.1371/journal.pone.0061526
Halpern, J. (2003). What is clinical empathy? J. Gen. Inter. Med. 18, 670–674. doi: 10.1046/j.1525-1497.2003.21017.x
Halpern, J. (2007). Empathy and patient–physician conflicts. J. Gen. Inter. Med. 22, 696–700. doi: 10.1007/s11606-006-0102-3
Hamric, A. B., and Blackhall, L. J. (2007). Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit. Care Med. 35, 422–429. doi: 10.1097/01.ccm.0000254722.50608.2d
Hamric, A. B., Borchers, C. T., and Epstein, E. G. (2012). Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Prim. Res. 3, 1–9. doi: 10.1080/21507716.2011.652337
Hickey, M., and Lewandowski, L. (1988). Critical care nurses’ role with families: a descriptive study. Heart Lung 17, 670–676.
Hojat, M., Louis, D. Z., Markham, F. W., Wender, R., Rabinowitz, C., and Gonnella, J. S. (2011). Physicians’ empathy and clinical outcomes for diabetic patients. Acad. Med. 86, 359–364. doi: 10.1097/ACM.0b013e3182086fe1
Hojat, M., Vergare, M. J., Maxwell, K., Brainard, G., Herrine, S. K., Isenberg, G. A., et al. (2009). The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad. Med. 84, 1182–1191. doi: 10.1097/ACM.0b013e3181b17e55
Kerasidou, A., and Horn, R. (2016). Making space for empathy: supporting doctors in the emotional labour of clinical care. BMC Med. Ethics 17:8. doi: 10.1186/s12910-016-0091-7
Krasner, M. S., Epstein, R. M., Beckman, H., Suchman, A. L., Chapman, B., Mooney, C. J., et al. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. J. Am. Med. Assoc. 302, 1284–1293. doi: 10.1001/jama.2009.1384
Lachmann, B., Sindermann, C., Sariyska, R. Y., Luo, R., Melchers, M. C., Becker, B., et al. (2018). The role of empathy and life satisfaction in internet and smartphone use disorder. Front. Psychol. 27:398. doi: 10.3389/fpsyg.2018.00398.2018
Lamiani, G., Borghi, L., and Argentero, P. (2017a). When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. J. Health Psychol. 22, 51–67. doi: 10.1177/1359105315595120
Lamiani, G., Setti, I., Barlascini, L., Vegni, E., and Argentero, P. (2017b). Measuring moral distress among critical care clinicians: validation and psychometric properties of the Italian Moral Distress Scale-Revised. Crit. Care Med. 45, 430–437. doi: 10.1097/CCM.0000000000002187
Lamiani, G., Dordoni, P., and Argentero, P. (2018). Value congruence and depressive symptoms among critical care clinicians: The mediating role of moral distress. Stress Health 34, 135–142. doi: 10.1002/smi.2769
Lawrence, E. J., Shaw, P., Baker, D., Baron-Cohen, S., and David, A. S. (2004). Measuring empathy: reliability and validity of the Empathy Quotient. Psychol. Med. 34, 911–920. doi: 10.1017/S003329170300162
Lennon, R., and Eisenberg, N. (1987). “Gender and age differences in empathy and sympathy,” in Empathy and Its Development, eds N. Eisenberg, and J. Strayer, (Cambridge: Cambridge University Press), 195–214.
Lu, H., While, A. E., and Barriball, K. L. (2005). Job satisfaction among nurses: a literature review. Int. J. Nurs. Stud. 42, 211–227.
Moghaddasian, S., Dizaji, S. L., and Mahmoudi, M. (2013). Nurses empathy and family needs in the intensive care units. J. Caring Sci. 2:197. doi: 10.5681/jcs.2013.024
Moss, M., Good, V. S., Gozal, D., Kleinpell, R., and Sessler, C. N. (2016). An official critical care societies collaborative statement - burnout syndrome in critical care healthcare professionals: a call for action. Chest 150, 17–26. doi: 10.1097/CCM.0000000000001885
Murphy, P. A., Forrester, D. A., Price, D. M., and Monaghan, J. F. (1992). Empathy of intensive care nurses and critical care family needs assessment. Heart Lung 21, 25–30.
Neumann, M., Edelhäuser, F., Tauschel, D., Fischer, M. R., Wirtz, M., Woopen, C., et al. (2011). Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad. Med. 86, 996–1009. doi: 10.1097/ACM.0b013e318221e615
Nightingale, S. D., Yarnold, P. R., and Greenberg, M. S. (1991). Sympathy, empathy, and physician resource utilization. J. Gen. Inter. Med. 6, 420–423. doi: 10.1007/bf02598163
Paro, H. B., Silveira, P. S., Perotta, B., Gannam, S., Enns, S. C., Giaxa, R. R., et al. (2014). Empathy among medical students: is there a relation with quality of life and burnout? PLoS One 9:e94133. doi: 10.1371/journal.pone.0094133
Picard, J., Catu-Pinault, A., Boujut, E., Botella, M., Jaury, P., and Zenasni, F. (2016). Burnout, empathy and their relationships: a qualitative study with residents in General Medicine. Psychol. Health Med. 21, 354–361. doi: 10.1080/13548506.2015.1054407
Preti, A., Vellante, M., Baron-Cohen, S., Zucca, G., Petretto, D. R., and Masala, C. (2011). The Empathy Quotient: a cross-cultural comparison of the Italian version. Cogn. Neuropsychiat. 16, 50–70. doi: 10.1080/13546801003790982
Riess, H. (2015). The impact of clinical empathy on patients and clinicians: understanding empathy’s side effects. AJOB Neurosci. 6, 51–53. doi: 10.1080/21507740.2015.1052591
Roeland, E., Cain, J., Onderdonk, C., Kerr, K., Mitchell, W., and Thornberry, K. (2014). When open-ended questions don’t work: the role of palliative paternalism in difficult medical decisions. J. Palliat. Med. 17, 415–420. doi: 10.1089/jpm.2013.0408
Rogers, C. R. (1957). The necessary and sufficient conditions of therapeutic personality change. J. Consult. Psychol. 21, 95–103. doi: 10.1037/h0045357
Rogers, C. R. (1959). “A theory of therapy, personality, and interpersonal relationships as developed in the client-centered framework,” in Psychology: A Study of a Science, ed. S. Koch, (New York, NY: McGraw-Hill), 184–256.
Rogers, C. R. (1975). Empathic: An unappreciated way of being. Couns. Psychol. 5, 2–10. doi: 10.1177/001100007500500202
Rushton, C. H. (2016). Moral resilience: a capacity for navigating moral distress in critical care. AACN Adv. Crit. Care 27, 111–119. doi: 10.4037/aacnacc2016275
Sanchez-Reilly, S., Morrison, L. J., Carey, E., Bernacki, R., O’Neill, L., Kapo, J., et al. (2013). Caring for oneself to care for others: physicians and their self-care. J. Support. Oncol. 11, 75–81. doi: 10.12788/j.suponc.0003
Sinclair, S., Beamer, K., Hack, T. F., McClement, S., Raffin Bouchal, S., Chochinov, H. M., et al. (2017). Sympathy, empathy, and compassion: a grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat. Med. 31, 437–447. doi: 10.1177/0269216316663499
Sorensen, R., and Iedema, R. (2009). Emotional labour: clinicians’ attitudes to death and dying. J. Health Org. Manag. 23, 5–22. doi: 10.1108/14777260910942524
Stayt, L. C. (2007). Nurses’ experiences of caring for families with relatives in intensive care units. J. Adv. Nurs. 57, 623–630. doi: 10.1111/j.1365-2648.2006.04143.x
Stayt, L. C. (2009). Death, empathy and self-preservation: the emotional labour of caring for families of the critically ill in adult intensive care. J. Clin. Nurs. 18, 1267–1275. doi: 10.1111/j.1365-2702.2008.02712.x
Tanriverdi, O. (2013). A medical oncologist’s perspective on communication skills and burnout syndrome with psycho-oncological approach (to die with each patient one more time: the fate of the oncologists). Med. Oncol. 30:530. doi: 10.1007/s12032-013-0530-y
Thirioux, B., Birault, F., and Jaafari, N. (2016). Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front. Psychol. 7:763. doi: 10.3389/fpsyg.2016.00763
Torres, O. Y., Aresté, M. E., Mora, J. R. M., and Soler-González, J. (2015). Association between sick leave prescribing practices and physician burnout and empathy. PLoS One 10:e0133379. doi: 10.1371/journal.pone.0133379
Truax, C. B., and Carkhuff, R. R. (1967). Toward Effective Counseling and Psychotherapy. Chicago: Aldine.
von Harscher, H., Desmarais, N., Dollinger, R., Grossman, S., and Aldana, S. (2017). The impact of empathy on burnout in medical students: new findings. Psychol. Health Med. 23, 295–303. doi: 10.1080/13548506.2017.1374545
Wagaman, M. A., Geiger, J. M., Shockley, C., and Segal, E. A. (2015). The role of empathy in burnout, compassion satisfaction, and secondary traumatic stress among social workers. Soc. Work 60, 201–209. doi: 10.1093/sw/swv014
Keywords: critical care, empathy, healthcare professionals, job satisfaction, moral distress, stress
Citation: Lamiani G, Dordoni P, Vegni E and Barajon I (2020) Caring for Critically Ill Patients: Clinicians’ Empathy Promotes Job Satisfaction and Does Not Predict Moral Distress. Front. Psychol. 10:2902. doi: 10.3389/fpsyg.2019.02902
Received: 14 March 2019; Accepted: 06 December 2019;
Published: 08 January 2020
Edited by:
Lesley L. Verhofstadt, Ghent University, BelgiumReviewed by:
Tine Vervoort, Ghent University, BelgiumFrancisco Manuel Morales, University of Granada, Spain
Copyright © 2020 Lamiani, Dordoni, Vegni and Barajon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giulia Lamiani, Z2l1bGlhLmxhbWlhbmlAdW5pbWkuaXQ=
 Giulia Lamiani
Giulia Lamiani Paola Dordoni
Paola Dordoni Elena Vegni
Elena Vegni Isabella Barajon
Isabella Barajon