- 1Curium-LUMC, Oegstgeest, Netherlands
- 2Youz, The Hague, Netherlands
Objective: Dropout rates are a prominent problem in youth psychotherapy. An important determinant of dropouts is the quality of the therapeutic relationship. This study aimed to evaluate the association between the therapeutic relationship and dropouts in an intensive mentalization-based treatment (MBT) for adolescents with personality disorders.
Methods: Patients (N = 105) included were either dropouts (N = 36) or completers (N = 69) of an intensive MBT. The therapeutic relationship was measured with the child version of the Session Rating Scale (C-SRS), which was completed by the patient after each group therapy session. For each patient, the treatment termination status (dropout or completer) was indicated by the treatment staff. The reliable change index (RCI) was calculated for the C-SRS to determine significant changes in the therapeutic relationship.
Results: While both groups started with similar scores on the C-SRS, the scores between dropouts and completers differed significantly at the end of the treatment period. On average, during therapy, an increase was seen in the scores of completers, and a decrease was seen in the scores of dropouts. While dropouts could not be predicted based on the C-SRS scores, a significant decrease (RCI) in C-SRS scores during the last two sessions occurred more often for dropouts than for completers.
Conclusion: Our findings show that to prevent dropouts, the patient’s judgment of the quality of the therapeutic relationship should be monitored continuously, and decreases discussed with the patient and the group.
Introduction
Dropout is a common phenomenon in child and adolescent therapy (De Haan et al., 2013; Owen et al., 2016; Hauber et al., 2017). When youngsters drop out of psychiatric treatment, their disorders are thought to persist or even worsen later in life. For instance, children with untreated disorders are more likely to become adults who rely on mental health services, having negative consequences for themselves, their surroundings, and society (Dulmus and Wodarski, 1996; Reis and Brown, 1999; Kessler et al., 2005). Premature termination of therapy is therefore considered a serious problem (Armbruster and Kazdin, 1994; Midgley and Navridi, 2006; Gopalan et al., 2010). Dropout percentages of 38.4% for outpatients (De Haan et al., 2015) and 34.4% for inpatients (De Boer et al., 2016) were found in adolescent mental health care. An important determinant for dropout is the quality of the therapeutic (patient–therapist) relationship (Kazdin and Wassell, 1998; Garcia and Weisz, 2002; Hawley and Weisz, 2005; Stevens et al., 2006; De Haan et al., 2013; Owen et al., 2016). For this reason, this study aimed to evaluate the association between the therapeutic relationship and dropout in an intensive mentalization-based treatment (MBT) for adolescents with personality disorders.
A therapeutic relationship or therapeutic alliance has commonly been defined as an agreement between the therapist and client on the goals for treatment, as well as ways to reach those goals, and the emotional or relational bond between the client and therapist (Bordin, 1979). Although several studies have been conducted on the relation between therapeutic relationship and dropout, it is hard to compare these studies because the time at which the therapeutic relationship was measured varies considerably (Robbins et al., 2003, 2006; Shelef et al., 2005; Cordaro et al., 2012). In several studies, trained observers rated therapeutic alliance based on one or two therapy sessions during the course of therapy. This approach, however, does not take the patients’ opinion about the relationship into account. Other studies measured the relationship from the patients’ point of view, but only after therapy had ended. These measurements would be strongly influenced by the way the patients felt at the time of termination. In a review on the therapeutic relationship within youth therapy, it is advised to measure the therapeutic relationship from the patients’ point of view during several sessions of the therapy process (Zack et al., 2007). If adolescents perceive the therapeutic relationship as supportive and agree with the topics and goals of the sessions, it will facilitate their engagement (Karver et al., 2006). One study, examining both the adolescents’ and the therapists’ perspectives on the therapeutic alliance, found that the client provided more information than the therapist did (Ormhaug et al., 2015). However, to this day, adolescent patients are hardly used as informants about the therapeutic alliance (De Haan et al., 2013).
In adult therapy, a moderately strong relationship between psychotherapy dropout and therapeutic alliance is found (Sharf et al., 2010). In youth therapy, studies on the relationship between the therapeutic alliance and dropout have been hindered in two ways: (1) the methods in which the therapeutic relationship could be measured and (2) the definition of dropout. First, most available measures for the therapeutic relationship in child and adolescent therapy are parent-report measures. The Therapeutic Alliance Scale for Children and Adolescents (TASC/A) is an exception and was designed to be administered to children and adolescents themselves (Shirk and Saiz, 1992; DeVet et al., 2003; Kazdin et al., 2005). The TASC/A was however designed to only be administered at one or two sessions throughout the course of therapy. The only available child-report instrument that measures the therapeutic relationship during all sessions is the child version of the Session Rating Scale (C-SRS) (Duncan et al., 2003, 2006; Miller and Duncan, 2004). This instrument is designed to be used at the end of every therapy session, and the child version of this tool makes it possible to assess the child’s or adolescent’s self-reported relationship with the therapist. Although designed for individual therapy, the instrument can also be used for group therapy. When used for group therapy, the therapeutic relationship is defined with three interacting elements: (1) a relational bond between the therapists, the group members, and the patient; (2) agreement on the goals of therapy; and (3) agreement on the tasks of therapy. The second topic that complicates research in this field is that there is also no agreement in the way dropout is defined. The definition varies across studies and influences which dropout predictors were found per study (De Haan et al., 2013, 2014a; Zack et al., 2007; Warnick et al., 2012). In this study, therapy dropout was defined as occurring when a participant discontinued the treatment programme before completing the treatment protocol, meaning that participants completing the treatment programme as planned were considered completers.
The aim of our study was to extend and specify insights on the association between the therapeutic relationship from the patients’ point of view and dropout during adolescent group psychotherapy. In accordance with Zack et al. (2007), we measured the therapeutic alliance of each psychotherapy session with an authorized Dutch version of C-SRS (Duncan et al., 2006; Hafkenscheid et al., 2006). Studies evaluating the (C-)SRS have confirmed the psychometric quality and usability of the instrument and have shown an association between therapeutic relationship and therapeutic change or outcome (Duncan et al., 2003; Campbell and Hemsley, 2009; Boon et al., 2012; Sundet, 2012; Owen et al., 2016). The association between the C-SRS and dropout has been studied in a sample of ethnic minority youth (De Haan et al., 2014a). Moreover, it was also shown that the scores on the C-SRS were not influenced by the patient’s knowledge of whether the scores would be observed by the therapists or not or whether the questionnaires were completed in the presence of the therapists. Moreover, the (C-)SRS scores were not significantly correlated with a measure of social desirability (Reese et al., 2013).
Materials and Methods
Setting
The studied facility, a department of De Jutters-Youz, a YMHC center in The Hague (one of the three most important cities of the Netherlands), offers a 5 day/week structured and integrative psychodynamic group psychotherapy programme. The aforementioned treatment commonly starts as a residential treatment and becomes an outpatient treatment halfway through. It is an MBT programme, manualized and adapted for adolescents (Bateman and Fonagy, 2006, 2012; Hauber, 2010), facilitated by a multidisciplinary team trained in MBT. The programme differs from the MBT programme for adolescents in England (Rossouw and Fonagy, 2012) in the psychodynamic group psychotherapy approach with an optimal group therapy size of six members instead of eight. The different components of the treatment programme mainly focus on the adolescents’ subjective experience of himself or herself and others and on the relationships with group members and treatment staff. Alongside the weekly group psychotherapy conducted by two therapists, other (non-verbal) group therapies such as art therapy and psychodrama therapy, as well as individual and family psychotherapy, are offered. In case medication is needed in addition to the treatment, this is prescribed by a psychiatrist in the team according to protocol. Weekends are spent at home.
In the weekly open group psychotherapy, as in the other components of the treatment programme, the therapists’ goal is to establish the group as a training ground for mentalizing. During the 1.5 h-long group therapy, all group members are invited to share their problems and to focus not only on what is shared but also on how things are shared by each group member. This often causes the therapeutic alliance to be a topic of conversation. Sometimes, one of the two group psychotherapists was also the individual therapist or EMDR therapist of one of the group members. In 2013, hoping to reduce dropout, the staff decided to measure the therapeutic relationship from the adolescents’ point of view and use it as input for the treatment offered. To this end, the C-SRS was administrated at the end of every weekly group psychotherapy. No sample size for power analysis was calculated beforehand, but the data of a 5-year period were used for this study.
Participants
The participants were a sample of 105 patients with clinically diagnosed personality disorders according to the DSM-III (APA, 2013) admitted between 2013 and 2018. Co-morbid pervasive developmental disorder and psychosis was set as an exclusion criterion. Intelligence was not measured but, based on the level of education, was estimated to be average to above average. Most patients (94.4%) had a native Dutch background, and the Dutch language was fluently spoken by all participants.
Upon arrival, patients and their parents were asked to sign a consent form to indicate that their data could be used anonymously for scientific research. At the start of the treatment, the mean age of the adolescents was 17.7 (SD = 1.7, range = 15–22) (females 81.0%). Average duration of treatment during this study was 215.2 days (SD = 100.8, range 21–640), for completers (M = 261.9, SD = 63.2, range = 168–640) and dropouts (M = 125.6, SD = 99.1, range = 21–343). Most of the patients (90.4%) were clinically diagnosed with a personality disorder often with co-morbid axis I disorders (mood disorder 48.5%, anxiety disorder including PTSS 57.3%, eating disorder 8.7%, ADHD 7.6%, substance dependence 3.9%, dissociative disorder 1.9%, and ASD 4.8%). Of the 94 patients diagnosed with a personality disorder, 49 (52.1%) were diagnosed as personality disorder NAO, 16 (17%) borderline, 16 (17%) avoidant, 2 (2.1%) dependent, and 1 (1.1%) antisocial.
Measures
C-SRS
The C-SRS (Miller and Duncan, 2004; Duncan et al., 2006) is a four-item visual analog instrument. The version for adolescents differs from the adult version of the SRS in that it uses emoticons: a smiley (positive) and a frowny face (negative). For this study, the authorized Dutch version of the C-SRS (Hafkenscheid et al., 2006) was used. The Dutch C-SRS has previously been used in research (Boon et al., 2012; De Haan et al., 2014b), and its reliability (internal consistency) was found to be satisfactory (Cronbach’s α = 0.86) (Hafkenscheid et al., 2010). As previously mentioned, therapeutic relationship was defined by three interacting elements: (1) a relational bond between the therapists, the group members, and the patient; (2) agreement on the goals of therapy; and (3) agreement on the tasks of therapy. In the C-SRS, these theoretical ideas are represented by four 10 cm visual analog scales with emoticons. Respondents are instructed to place a hash mark on a line. Negative responses are placed on the left (frowny faces) and positive responses on the right (smileys). The first item is a relationship scale, rating the session on a continuum from “The therapists and group members did not listen to me” to “The therapists and group members listened to me.” The second item is a goals-and-topics scale, rating the session on a continuum from “We did not do or talk about the things I wanted to work on or talk about” to “We did do or talk about what I wanted to work on or talk about.” The third item is an approach or method scale asking the patient to rate the session on a continuum from “I did not like the way the therapists and group members approached my problems today” to “I liked the way the therapists and the group members approached my problems today.” The fourth item examines how the patient perceived the session in total and the group alliance along the lines of “Overall, today’s session was not right for me—I did not feel part of the group” to “Overall, today’s session was right for me—I did feel part of the group.” Because the scores on the four items (the 10 cm line represents scores between 0 and 10) are added, the session total score will vary between 0 and 40: high average total scores are an indication of a high-quality therapeutic relationship.
Termination Status: Dropout and Completion of Therapy
In case premature termination was suggested by a patient, the patient’s family, or the treatment staff, a supportive reassessment of treatment was organized. Only when both the therapist and the patient (and family) agreed that therapy goals had been reached or when both agreed to terminate while therapy goals had only partly been reached was the patient classified as a “completer.” If the patient, therapist, or both stated that therapy was not yet completed, the exact reasons for termination were examined. In these cases, the patient was classified as a “dropout.” The intention was to classify the patients as “unilaterally terminated by the therapist” when the therapist wished to terminate therapy while the patient wished to continue. Among the included 105 patients, there were no cases of “unilaterally terminated by the therapist.” In the end, 36 patients were classified as dropouts, and 69 patients were classified as completers by the treatment staff.
Procedure
The treatment protocol contained a programme of MBT treatments 5 days/week, with the standard weekly programme including group therapy. The C-SRS was presented to the patients at the end of each weekly group therapy session, after which it was collected and viewed by the therapist. Our purpose was to let the patients fill in the form during every therapy session. Although therapists sometimes forgot to hand out the C-SRS, in general, the C-SRS was completed during most of the group therapy sessions. The first C-SRS was completed after the first therapy session. The C-SRS that was completed during the last session (planned in the case of completers and unplanned in the case of dropouts) was marked as the last C-SRS. The total amount of C-SRS forms completed by the patient largely depended on the length of therapy.
Statistical Analyses
All analyses were performed using SPSS, version 25.0 (IBM, 2017). First, whether the scores of the C-SRS violated the normality assumption was tested. This was not the case (skewness: dropouts.747, SE.393, Z = 1.90 and completers -0.315, SE.289, Z = 1.09; kurtosis: dropouts -0.806, SE.768, Z = 1.055 and completers.255, SE.570, Z = 0.45). Because the total scores were determined equally by all items, it was decided to exclude the item scores from further analyses.
Second, through a t-test, dropouts and completers were compared based on their C-SRS scores of the first session and the last session. To see if dropout was related to C-SRS scores over time, a mixed model analysis was performed with the C-SRS score as a dependent variable and time and dropout as independent variables.
Third, the reliable change index (RCI) for the C-SRS was calculated using the Jacobson and Truax (1991) formula. The standard error of measurement (SEM) was calculated (s√1 - rxx), DIFF = √2(SEM2), RCI = xt1 - xt2/SDIFF. A 95% reliability interval was used. The resulting categories were “deteriorated” (a significant decrease in score between two sessions), “no reliable change” (no significant increase or decrease in score between two sessions), and “improved” (a significant increase in score between two sessions). Based on all questionnaires (N = 2,378) with a reliability (Cronbach’s alpha) of.921 and SD of 8.15, the standard error was 3.24. The reliable change criterion was (1.96 ∗ 3.24) 6.35.
Fourth, a generalized estimating equation (GEE) analysis with an exchangeable working correlation matrix was performed to see if a decrease in C-SRS score could predict dropout, with the dichotomous variable “significant decrease (RCI) in the C-SRS score between two consecutive sessions” as the independent variable and “dropout within three sessions” as the dependent variable.
Last, a forward binary logistic regression analysis was performed with dropout vs. completer as the dependent variable and gender, age, diagnoses, and significant decreases (using RCI) during the last five sessions of therapy as independent variables.
Results
Descriptives
The 105 subjects attended group psychotherapy between March 2013 and October 2018, with an average number of group members of 5.0. The number of C-SRSs completed per participant ranged from 2 to 43 times (M = 22.07, SD = 10.45). The number of missed sessions (M = 3.53, SD = 4.97) was calculated by subtracting the attended sessions (M = 25.6, SD = 12.7) from number of planned sessions (M = 26.3, SD = 12.7). Based on the results, the percentage of missed sessions was calculated for each respondent. This percentage did not differ (p = 0.72) between completers (2.78%, SD = 0.58) and dropouts (3.27%, SD = 1.51). Of the 2,832 attended sessions, 2,367 C-SRS were completed (response 83.6%).
Dropouts vs. Completers
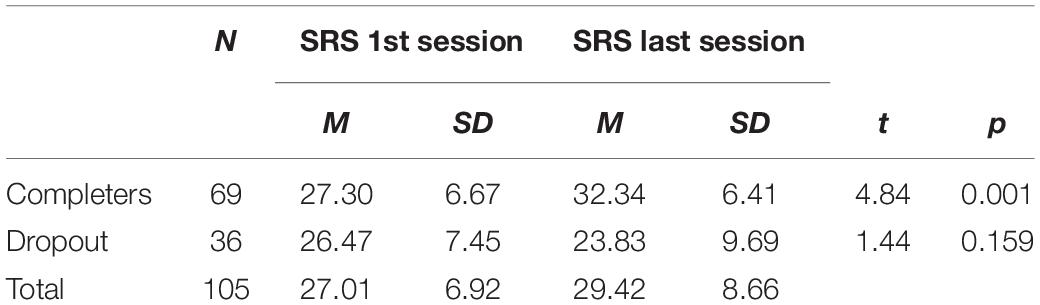
The treatment duration of the dropouts (M = 125.56 days, SD = 99.1) was significantly (t = 7.497, p < 0.001) lower than that of the completers (M = 261.91 days, SD = 63.3). Dropouts (N = 36) completed the C-SRS on average 13.42 times (SD = 11.38), and completers (N = 69) completed it on average 26.58 (SD = 6.33) times. These numbers differed significantly (t = 7.629, p < 0.001). Table 1 presents a comparison between first- and last-session scores of the C-SRS completers and dropouts. For completers, the C-SRS scores increased significantly between the first and last sessions, while the scores of the dropouts did not change. All the individual items of the C-SRS contributed equally to these results: a significant increase for completers and no significant change for the dropouts.
No significant difference was found (t = 0.583, p = 0.577) on the first C-SRS scores for dropouts vs. completers. The scores of the last session however differed significantly (t = 4.756; p < 0.001, Cohen’s d = 1.035) between both groups. Total C-SRS scores decreased by 0.86 points per session on average for the dropouts, while increasing by 0.18 points per session for the completers.
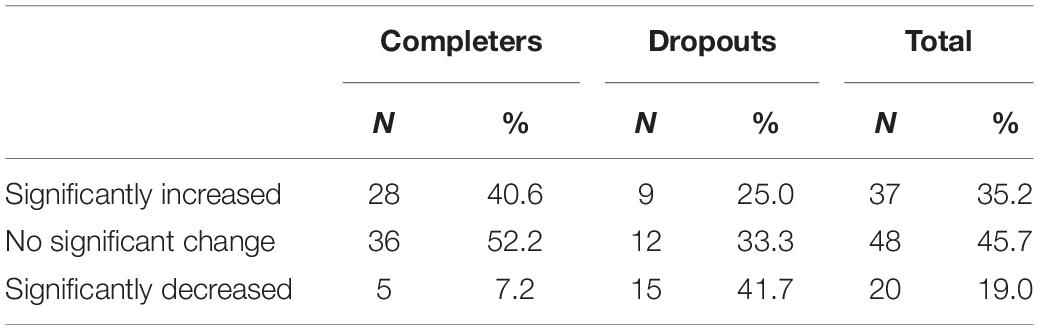
Mixed model analyses showed no differences (p = 0.665) in C-SRS scores over time between dropouts and completers, implying that dropout cannot be predicted from the progression of C-SRS scores. A GEE analysis did not reveal dropout to be a significant predictor of significant (RCI) decreases in C-SRS scores (p = 0.730). The next step was to identify the last five sessions of therapy and compare the differences in C-SRS scores between these sessions. No differences were found between completers and dropout in comparison of the fifth- and fourth-last sessions. On the other hand, comparison of the third-last and the second-last sessions showed that 7.1% (n = 3) of the completers (N = 42) had a significant (RCI) decrease in C-SRS score between these sessions, while for dropouts (N = 17), this was 35.3% (n = 6) (df = 1, χ2 = 7.419, p = 0.006). Subsequently, a comparison of the C-SRS score of the second-last and the last sessions showed that 4.0% (n = 2) of the completers (N = 50) had a significant (RCI) decrease in C-SRS score between these sessions, while for dropouts (N = 30), this was 26.7% (n = 8) (df = 1, χ2 = 8.808, p = 0.003) (Table 2). In conclusion, during the last three sessions, 7.2% (n = 5) of the completers showed a significant decrease in C-SRS scores, compared to 38.9% (n = 14) of the dropouts (df = 1, χ2 = 15.98, p < 0.001). Binary regression analysis (forward stepwise) shows that the model that fitted the data (χ2 = 5.50; p = 0.019) included only a significant decrease between the second to last and the last sections (p = 0.035) with an odds ratio (Exp B) of 4.38.
The differences between sessions for all respondents for all sessions (N = 1906) showed that 324 times (14.3%) a significant decrease (RCI) in C-SRS scores occurred. Table 2 shows the significant (RCI) decreases between first- and last-session C-SRS scores for completers and dropouts.
Discussion
The aim of this study was to gain deeper insights into the association between the quality of the therapeutic relationship and treatment termination status among high-risk adolescents receiving intensive MBT. We measured the therapeutic relationship during group therapy with the C-SRS, through which the adolescent rated the therapeutic group alliance. No differences were found in the initial scores of the C-SRS, indicating that dropouts and completers did not differ in the way that they experienced the therapeutic alliance at the start of therapy. On the other hand, the development of C-SRS scores during the course of therapy did differ for the two groups: completers showed improving scores of the therapeutic relationship during the course of therapy, while dropouts showed declining scores. These differences occurred mainly at the end of the treatment course. The results indicate that an improving therapeutic relationship during the course of therapy is associated with adherence to therapy, while a decreasing quality of the therapeutic relationship during the course of therapy is associated with the patient ending therapy prematurely (Norcross and Lambert, 2018). Furthermore, a significant drop in the therapeutic relationship between the next to last and final sessions was four times more likely to occur. This could mean that even though clients are about to drop out, they will still attend another session, giving the therapist a chance to repair the rupture in the therapeutic relationship. Our study showed that the rather short instrument (C-SRS), which can be easily applied in clinical practice to be completed by adolescent patients themselves, is a valuable instrument for measuring the quality of the therapeutic relationship.
A significant decrease in the therapeutic alliance in the last three sessions was a predictor of dropout. For dropouts, such a decrease occurred in 38.9% of the cases, while for completers, this was 7.2% of the cases. Because such a significant decrease in therapeutic group alliance occurred during the treatment process in 14.3% of all cases, only with hindsight was it clear that such decrease has led to dropout. To prevent dropping out of therapy, this means that every substantial decrease in C-SRS score is worth discussing. In this study, some participants spoke of being satisfied with the session, while on the C-SRS, they rated the therapeutic alliance of that same session as low. Probably, these patients avoided being openly honest about their negative feelings toward the group and therapist. By using the C-SRS, such unspoken inconsistency can be recognized, understood, and worked through in the next session, and thereby outcomes can be improved (Norcross and Lambert, 2018). In case the decrease in C-SRS score is caused by something that occurred in the working alliance with the therapists and/or the group members, differences in perspective and thoughts, beliefs, wishes, and feelings can be explored and validated (Bateman and Fonagy, 2012). This way, group psychotherapy is a shared attentional process which strengthens mentalizing capacities and interpersonal functioning.
We found that dropouts and completers did not differ in the way they experience the therapeutic alliance at the start of therapy, which is not in line with most research on this topic (De Haan et al., 2013). This could be explained by the emphasis placed on internal motivation prior to treatment. Among others, adolescents in this study were asked during the registration phase to write a motivation letter for the treatment. For youth therapists, paying attention to therapeutic alliance in general and especially at the start of the treatment may be particularly relevant due to distrust of adult authorities and a desire for autonomy (De Haan et al., 2013). Limitations of this study must be mentioned. The first limitation is that the generalizability of the results found in a sample of high-risk adolescents in group psychotherapy with other patients with personality pathology and patients with other pathology is yet to be determined. Second, it is not clear if the dropouts are the result of a decrease in the therapeutic alliance or a result of other factors, potentially even outside of the treatment. Third, the fact that in some cases one of the group therapists was also an attending patient’s individual therapist could influence the results. Fourth, the significant differences in treatment duration in the relatively small sample could influence the results due to diversity. Nevertheless, the C-SRS can help psychotherapists to timely intervene when breaks, which may lead to dropout, occur in the therapeutic alliance with adolescents with personality pathology. Future research on all elements of the therapeutic alliance including the view of the therapist for high-risk adolescents is needed.
Conclusion
In this study, the association between the quality of the therapeutic relationship from the patients’ point of view and dropout was examined in a seldom-studied adolescent group with personality pathology. This high-risk group of patients is often excluded from scientific research, although personality disorders often start and peak in middle to late adolescence (Hutsebaut et al., 2013; Shiner and Allen, 2013). The psychosocial and economic burden is high (Feenstra et al., 2012; Chanen and McCutcheon, 2013). Against this background, clinical practice is in need of more information regarding this difficult group. It is to be expected that the number of breaks in the therapeutic alliance are higher in this group than in a group with less severe psychopathology (Eubanks and Muran, 2018). Furthermore, as the size of the therapist effect—one element of the therapeutic alliance—is strongly related to initial client severity (Norcross and Lambert, 2018), it is also to be expected that the therapist effect in this adolescent group is substantial.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
KH performed the data collection and wrote the manuscript. AB contributed to the design of the research project, performed the statistical analyses in the study, and revised the manuscript. RV oversaw the research project and reviewed the manuscript. All authors read and approved the final manuscript.
Funding
This clinical practice study was not supported by a funding or a scholarship.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful and would like to thank all adolescents and colleagues who collaborated in this research.
References
Armbruster, P., and Kazdin, A. E. (1994). “Attrition in child therapy,” in Advances in Clinical Child Psychology, Vol. 16, eds T. H. Ollendick and T. J. Prinz (New York: Plenum), 81–108.
Bateman, A., and Fonagy, P. (2006). Mentalization Based Treatment for Borderline Personality Disorder: A Practical Guide. Oxford, UK: Oxford University Press.
Bateman, A., and Fonagy, P. (2012). Handbook of Mentalizing in Mental Health Practice. Arlington, VA: American Psychiatric Publishing, Inc.
Boon, A. E., De Boer, S. B. B., and Ravestijn, E. (2012). De Child outcome rating scale (C-ORS) en de Child session rating scale (C-SRS). Het belang van de therapeutische alliantie voor het behandelresultaat. [The Child outcome rating scale (C-ORS) and the Child session rating scale (C-SRS). The importance of the therapeutic alliance for treatment outcome]. Tijdschrift voor Psychotherapie 38, 73–87. doi: 10.1007/s12485-012-0008-y
Bordin, E. S. (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychother. Theory Res. Pract. 16, 252–260. doi: 10.1037/h0085885
Campbell, D. A., and Hemsley, S. (2009). Outcome Rating Scale and Session Rating Scale in psychological practice: clinical utility of ultra-brief measures. Clin. Psychol. 13, 1–9. doi: 10.1080/13284200802676391
Chanen, A. M., and McCutcheon, L. (2013). Prevention and early intervention for borderline personality disorder: current status and recent evidence. Br. J. Psychiatry 202, s24–s29. doi: 10.1192/bjp.bp.112.119180
Cordaro, M., Tubman, J. G., Wagner, E. F., and Morris, S. L. (2012). Treatment process predictors of completion or dropout among minority adolescents enrolled in a brief motivational substance abuse intervention. J. Child Adolesc. Subst. Abuse 21, 51–68. doi: 10.1080/1067828X.2012.636697
De Boer, S., Boon, A., De Haan, A., and Vermeiren, R. (2016). Treatment adherence in adolescent psychiatric inpatients with severe disruptive behaviour. Clin. Psychol. 22, 55–62. doi: 10.1111/cp.12111
De Haan, A., Boon, A., De Jong, J., Geluk, C., and Vermeiren, R. (2014a). Therapeutic relationship and dropout in youth mental health care with ethnic minority children and adolescents. Clin. Psychol. 1–9. doi: 10.1111/cp.12030
De Haan, A., Boon, A., De Jong, J., Hoeve, M., and Vermeiren, R. (2013). A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin. Psychol. Rev. 33, 698–711. doi: 10.1016/j.cpr.2013.04.005
De Haan, A., Boon, A., De Jong, J., Hoeve, M., and Vermeiren, R. (2015). Ethnic background, socioeconomic status, and problem severity as dropout risk factors in psychotherapy with youth. Child Youth Care Forum 44, 1–16. doi: 10.1007/s10566-014-9266-x
De Haan, A., Boon, A., Vermeiren, R., and De Jong, J. (2014b). Ethnic differences in DSM–classifications in youth mental health care practice. Int. J. Cult. Ment. Health 7, 284–296. doi: 10.1080/17542863.2013.789918
DeVet, K. A., Kim, Y. J., Charlot-Swilley, D., and Ireys, H. T. (2003). The therapeutic relationship in child therapy: perspectives of children and mothers. J. Clin. Child Adolesc. Psychol. 32, 277–283. doi: 10.1207/S15374424JCCP3202_13
Dulmus, C. N., and Wodarski, J. S. (1996). Assessment and effective treatments of childhood psychopathology: responsibilities and implications for practice. J. Child Adolesc. Group Ther. 6, 75–99. doi: 10.1007/BF02548502
Duncan, B. L., Miller, S. D., Sparks, J. A., Claud, D. A., Reynolds, L. R., Brown, J., et al. (2003). The session rating scale: preliminary psychometric properties of a ‘working’ alliance measure. J. Brief Ther. 3, 3–12.
Duncan, B. L., Sparks, J. A., Miller, S. D., Bohanske, R. T., and Claud, D. A. (2006). Giving youth a voice: a preliminary study of the reliability and validity of a brief outcome measure for children, adolescents, and caretakers. J. Brief Ther. 5, 71–87.
Eubanks, C. F., and Muran, J. C. (2018). Alliance rupture repair: a meta-analysis. Psychotherapy 55, 508–519. doi: 10.1037/pst0000185
Feenstra, D. J., Hutsebaut, J., Laurenssen, E. M. P., Verheul, R., Busschbach, J. J. V., and Soeteman, D. I. (2012). The burden of disease among adolescents with personality pathology: quality of life and costs. J. Personal. Disord. 26, 593–604. doi: 10.1521/pedi.2012.26.4.593
Garcia, J. A., and Weisz, J. R. (2002). When youth mental health care stops: therapeutic relationship problems and other reasons for ending youth outpatient treatment. J. Consult. Clin. Psychol. 70, 439–443. doi: 10.1037/0022-006X.70.2.439
Gopalan, G., Goldstein, L., Klingenstein, K., Sicher, C., Blake, C., and McKay, M. M. (2010). Engaging families into child mental health treatment: updates and special considerations. J. Can. Acad. Child Adolesc. Psychiatry 19, 182–196.
Hafkenscheid, A., Been, D., de Boer, S. B. B., Boon, A. E., Breukers, P., Crouzen, M., et al. (2006). Child Sessions Rating Scale, Dutch Version. Amstelveen: Sinai Centrum.
Hafkenscheid, A., Duncan, B. L., and Miller, S. D. (2010). The outcome and session rating scales: a cross-cultural examination of the psychometric properties of the Dutch translation. J. Brief Ther. 7, 1–12.
Hauber, K., Boon, A., and Vermeiren, R. R. (2017). Examining changes in personality disorder and symptomology in an adolescent sample receiving intensive mentalization based treatment - a pilot study. Child Adolesc. Psychiatry Ment. Health 11:58. doi: 10.1186/s13034-017-0197-9
Hawley, K. M., and Weisz, J. R. (2005). Youth versus parent working alliance in usual clinical care: distinctive associations with retention, satisfaction, and treatment outcome. J. Clin. Child Adolesc. Psychol. 34, 117–128. doi: 10.1207/s15374424jccp3401_11
Hutsebaut, J., Feenstra, D. J., and Luyten, P. (2013). Personality disorders in adolescence: label or opportunity? Clin. Psychol. Sci. Pract. 20, 445–451. doi: 10.1111/p.12052
Jacobson, N., and Truax, P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 59, 12–19. doi: 10.1037/0022-006X.59.1.12
Karver, M. S., Handelsman, J. B., Fields, S., and Bickman, L. (2006). Meta-analysis of therapeutic relationship vairables in youth and family therapy: the evidence for different relationship variables in the child and adolescent outcome literature. Clin. Psychol. Rev. 26, 50–65. doi: 10.1016/j.cpr.2005.09.001
Kazdin, A. E., Marciano, P. L., and Whitley, M. K. (2005). The therapeutic alliance in cognitive-behavioral treatment of children referred for oppositional, aggressive, and antisocial behaviour. J. Consult. Clin. Psychol. 73, 726–730. doi: 10.1037/0022-006X.73.4.726
Kazdin, A. E., and Wassell, G. (1998). Treatment completion and therapeutic change among children referred for outpatient therapy. Prof. Psychol. Res. Pract. 29, 332–340. doi: 10.1037/0735-7028.29.4.332
Kessler, R. C., Chiu, W. T., Demler, O., and Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 62, 617–627. doi: 10.1001/archpsyc.62.6.617
Midgley, N., and Navridi, E. (2006). An exploratory study of premature termination in child analysis. J. Infant Child Adolesc. Psychother. 5, 437–458. doi: 10.1080/15289160701382360
Miller, S. D., and Duncan, B. L. (2004). The Outcome and Session Rating Scale. Administration and Scoring Manual. Chicago, Il: Institute for the Study of therapeutic Change.
Norcross, J. C., and Lambert, M. J. (2018). Psychotherapy relationships that work III. Psychotherapy 55, 303–315. doi: 10.1037/pst0000193
Ormhaug, S. M., Shirk, S. R., and Wentzel-Larsen, T. (2015). Therapist and client perspectives on the alliance in the treatment of traumatized adolescents. Eur. J. Psychotraumatol. 6:27705. doi: 10.3402/ejpt.v6.27705
Owen, J., Miller, S. D., Seidel, J., and Chow, D. (2016). The working alliance in treatment of military adolescents. J. Consult. Clin. Psychol. 84, 200–210. doi: 10.1037/ccp0000035
Reese, R., Gillaspy, J., Owen, J. J., Flora, K., Cunningham, L., Archie, D., et al. (2013). The influence of demand characteristics and social desirability on clients’ ratings of the therapeutic alliance. J. Clin. Psychiatry 69, 696–709. doi: 10.1002/jclp.2194
Reis, B. F., and Brown, L. G. (1999). Reducing psychotherapy dropouts: maximizing perspective convergence in the psychotherapy dyad. Psychotherapy 36, 123–136.
Robbins, M. S., Liddle, H. A., Turner, C. W., Dakof, G. A., Alexander, J. F., and Kogan, S. M. (2006). Adolescent and parent therapeutic alliance as predictors of dropout in multidimensional family therapy. J. Fam. Psychol. 20, 108–116. doi: 10.1037/0893-3200.20.1.108
Robbins, M. S., Turner, C. W., Alexander, J. F., and Perez, G. A. (2003). Alliance and dropout in family therapy for adolescents with behavior problems: individual and systemic effects. J. Fam. Psychol. 17, 534–544. doi: 10.1037/0893-3200.17.4.534
Rossouw, T. I., and Fonagy, P. (2012). Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 51, 1304–1313. doi: 10.1016/j.jaac.2012.09.018
Sharf, J., Primavera, J., and Diener, M. (2010). Dropout and therapeutic alliance: a meta-analysis of adult individual psychotherapy. Psychother. Theory Res. Pract. Train. 47, 637–645. doi: 10.1037/a0021175
Shelef, K., Diamond, G. M., Diamond, G. S., and Liddle, H. A. (2005). Adolescent and parent alliance and treatment outcome in multidimensional family therapy. J. Consult. Clin. Psychol. 73, 689–698. doi: 10.1037/0022-006X.73.4.689
Shiner, R. L., and Allen, T. A. (2013). Assessing personality disorders in adolescents: seven guiding principles. Clin. Psychol. Sci. Pract. 20, 361–377. doi: 10.1111/cpsp.12047
Shirk, S. R., and Saiz, C. C. (1992). Clinical, empirical, and developmental perspectives on the therapeutic relationship in child psychotherapy. Dev. Psychopathol. 4, 713–728. doi: 10.1017/S0954579400004946
Stevens, J., Kelleher, K. J., Ward-Estes, B. S., and Hayes, J. (2006). Perceived barriers to treatment and psychotherapy attendance in child community mental health centers. Commun. Ment. Health J. 42, 449–458. doi: 10.1007/s10597-006-9048-5
Sundet, R. (2012). Therapist perspectives on the use of feedback on process and outcome: patient-focused research in practice. Can. Psychol. 53, 122–130. doi: 10.1037/a0027776
Warnick, E. M., Gonzalez, A., Weersing, V. R., Scahill, L. D., and Woolston, J. L. (2012). Defining dropout from youth psychotherapy: how definitions shape the prevalence and predictors of attrition. Child Adolesc. Ment. Health 17, 76–85. doi: 10.1111/j.1475-3588.2011.00606.x
Keywords: dropout, therapeutic relationship, residential mental health care, adolescents, MBT
Citation: Hauber K, Boon A and Vermeiren R (2020) Therapeutic Relationship and Dropout in High-Risk Adolescents’ Intensive Group Psychotherapeutic Programme. Front. Psychol. 11:533903. doi: 10.3389/fpsyg.2020.533903
Received: 10 February 2020; Accepted: 02 November 2020;
Published: 27 November 2020.
Edited by:
Serge Brand, University Psychiatric Clinic Basel, SwitzerlandReviewed by:
Roumen Kirov, Bulgarian Academy of Sciences (BAS), BulgariaRobert Vaughan, York St John University, United Kingdom
Copyright © 2020 Hauber, Boon and Vermeiren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kirsten Hauber, a2lyc3Rlbi5oYXViZXJAZ21haWwuY29t
 Kirsten Hauber
Kirsten Hauber Albert Boon1,2
Albert Boon1,2 Robert Vermeiren
Robert Vermeiren