Abstract
Background:
Minority stress theory views social support as a protective factor against the effects of minority-specific stressors like internalized homophobia (IH) on mental health in sexual minority populations. However, much of the empirical validation of this theory has been conducted within predominantly White samples, resulting in a limited understanding of how the theory applies to Black sexual minority individuals. Current examinations of social support fail to capture the nuances of how Black sexual minority men may access support systems differently, resulting in a need to investigate how social support, IH, and mental health operate for Black sexual minority men. This study examined relationships between IH, depression, and different types of social support (i.e., family, friends, Black community, gay community) using a mediation model.
Methods:
We used data from the POWER (Promoting Our Worth Equity and Resilience) Study, which recruited Black sexual minority men at Black Pride events across six cities in the United States from 2014 to 2017, to test four mediation pathways concurrently in Stata 17. Participants (N = 4,430) completed a questionnaire assessing a variety of health and life domains, including depression symptoms, internalized homophobia, and social support.
Results:
IH was positively associated with depression. Lower levels of family, friend, and Black community support were all positively associated with depression symptoms. Additionally, IH was positively associated with all types of support. Finally, family, friend, and Black community support partially mediated the relationship between IH and depression.
Conclusions and implications:
Results suggest that the relationship between social support and depression is complex for Black sexual minority men. Findings suggest family support is an important factor for clinical intervention efforts targeting depression, and that gay community support systems should assess how their environments can better support Black sexual minority men. Overall, findings demonstrate the necessity of future examination of how social support functions differently within Black sexual minority communities.
Introduction
In the United States, up to 9.4% of adults (National Center for Health Statistics, 2019; Jones, 2021), identify with a sexual minority identity (e.g., gay, bisexual, pansexual, queer) or report same-sex behavior. Of these sexual minorities, approximately 13.4% are Black or African American (United States Census Bureau, 2022). Despite comprising a small percentage of the U.S. population, Black sexual minority men (BSMM) face pronounced health disparities, including high rates of depression (Vincent et al., 2020) compared to their White peers. Leading explanations for high rates of behavioral health disparities facing BSMM point to the intersectional compounding of stressors (e.g., discrimination, violence, exclusion, internalized stigma) stemming from overlapping systems of oppression: racism and heterosexism (Graham et al., 2011, 2016; English et al., 2021). Growing evidence has elucidated a predictive relationship between intersectional, oppression-based stressors and negative behavioral health outcomes for BSMM, including depression and suicidality (Lytle et al., 2014; Sutter and Perrin, 2016). These threats have significant implications for the quality of life, social functioning, and the very lives of BSMM; however, there is a paucity of evidence regarding psychosocial mediators and moderators that could inform the development of interventions to prevent or mitigate these health threats.
Minority stress theory
Minority stress theory, originally presented by Brooks (1981) and then later advanced by Meyer (2003) been the prevailing framework applied to examine sexual minority stress. However, a key limitation of the data that supports the framework is its overwhelming dependency on predominantly White samples (Meyer, 2010; Moradi et al., 2010a,b). Key stress-related mechanisms and protective factors may operate differentially when it comes to Black populations. Minority stress theory posits that psychosocial support moderates the relationship between minority-specific stressors, like internalized homophobia, and mental health outcomes, such as depression. Black sexual minorities who experience internalized homophobia may access support systems differently than White sexual minorities, given specific racialized and cultural factors impacting sexual minority identity self-disclosure (Friedman et al., 2019).
Internalized homophobia, depression, and social support
In recent decades, theory and evidence have shown that internalized homophobia is a prominent psychosocial stressor contributing to depression in sexual minority men (Shidlo, 1994; Rowen and Malcolm, 2003; Newcomb and Mustanksi, 2010; Heiden-Rootes et al., 2020). Internalized homophobia is a cognitive, emotional, and behavioral process in which sexual minority individuals adopt the negative beliefs and attitudes that permeate society about sexual minority people (Amola and Grimmett, 2015). Research suggests that individuals often seek support from those in their social networks (e.g., friends, family members, communities) when faced with stressors (Pearlin and Bierman, 2013). However, sexual minorities and BSMM, in particular, may have fewer or unhelpful sources of social support because they may be more socially isolated due to shame, identity concealment, or past experiences with discrimination, rejection, and/or microaggressions (Meyer, 2010; Arnold et al., 2014; Smallwood et al., 2017).
Importance of mediation analysis for sexual minority populations
To examine the intermediate variables that influence the pathways between sexual minority-specific stressors and their outcomes, it is important to conduct mediation analyses. Mediation analyses are employed when an independent variable is posited to create change in an intervening variable (i.e., mediator) that, in turn, causes a change in an outcome (MacKinnon et al., 2002). A systematic review (Argyriou et al., 2021) identified 40 studies that examined mediators with sexual minority populations. Out of these 40 studies, only 9 of them studied social support as a mediator to depression, and none of them explored these mediators with samples of primarily BSMM.
A recent study (Puckett et al., 2015) of sexual minority adults found that social support mediated the relationship between internalized homophobia and mental health problems (i.e., depression, anxiety, and suicidal ideation), with higher internalized homophobia being associated with lower social support and lower social support being associated with more psychological distress. However, this study used a predominately White sample, and did not include an examination of multiple minorities. Additional research is needed to explicate these relationships, especially with BSMM, considering the multiple marginalizations and high rates of behavioral health disparities faced by this population (Vincent et al., 2020; English et al., 2021). Furthermore, much of the extant evidence relies on studies with largely White samples, with limited representation of BSMM (Meyer, 1995, 2003; Szymanski et al., 2008; Moradi et al., 2010a,b). Clarifying mechanisms underlying the relationships between internalized homophobia and mental health outcomes for BSMM is imperative, as these factors may operate differently for this unique group.
Purpose of current study
Given the critical gaps in knowledge on key mediating factors in BSMM’s pathways of psychosocial stressors and depression disparities, the purpose of this study was to examine which types of social support may mediate the relationship between internalized homophobia and depression symptoms among BSMM. This study examined various types of social support as potential mediators, including social support from various relationship groups including family, friends, sthe gay community, and the Black community. Based on prior research (though very limited with BSMM), we hypothesized that (a) internalized homophobia would be positively related to depression, (b) internalized homophobia would be inversely related to social support, and (c) social support would be inversely related to depression symptoms.
Methods
This study used data from the POWER (Promoting Our Worth, Equity, and Resilience) project (Eaton et al., 2018), a cross-sectional study of BSMM (N = 4,430) recruited at queer Black pride events in Atlanta, GA; Detroit, MI; Houston, TX; Memphis, TN; Philadelphia, PA; and Washington, DC from 2014–2017. At each pride event, the study team created an intercept zone, where individuals were approached, and invited to participate in the research study. Participants were provided $10 for survey completion.
To be eligible for the study, individuals must have been assigned male sex at birth, had a male sexual partner in their lifetime, self-identified as Black or African American, and be at least 18 years old. Survey assessments were anonymous. Eligible participants were provided informed consent. Participants completed an anonymous, computer-assisted self-interview (CASI) using an electronic tablet. Each participant was given a unique code. This code was based on a sequence of letters and numbers from the participant’s name, a family member’s name, birth date, and state of birth. Participants completed the self-report survey about demographics (racial/ethnic identity, age, income, education level, sexual identity), internalized homophobia, social support, and depression symptoms. Participants completing more than one survey were identified. Further detail regarding the process used to identify and remove repeated respondents has been described elsewhere (Eaton et al., 2018). The University of Pittsburgh Institutional Review Board approved all study procedures.
Measures
Socio-demographic characteristics were collected. Participants were asked about their age, highest level of education, annual income, and sexual orientation. Sexual identity was measured with the item, “Which of the following do you identify with?” Options included: gay/same gender loving, heterosexual or straight, bisexual, or other. Education was assessed with the item, “What is the highest level of education you completed?” Annual income was asked, “What would you say is your annual personal income before taxes?” Age and income level were treated continuously. Education, sexual orientation, year, and city of data collection were treated as categorical variables.
Internalized homophobia was measured using the 9-item Internalized Homophobia Scale (IHS; Herek et al., 1997; e.g., “I feel alienated from myself because of being gay/bisexual”), with 5-point response options ranging from Strongly Agree (0) to Strongly Disagree (4). The internal consistency reliability was very good (α = 0.92). Item scores were averaged, and ranged from 0 to 5, with the higher values indicating a higher degree of internalized homophobia. IHS has been applied to BSMM in previous research (Dawson et al., 2019) and had a high internal reliability within that sample (α = 0.88).
Social support from four sources (Black community, family, friends, and the gay community) was measured by asking, “To what degree do you feel you receive support from….” Each source of support was a separate item. Response options included None, A little, Somewhat, and A lot (coded as 0 to 4) for each source of support. Support items were reverse-coded in the analysis, with higher numbers indicating lower social support.
Depression symptoms in the past week were measured using the 10-item version of the Center for Epidemiological Studies (CES-D-10; Andresen et al., 1994) with 4-point response options ranging from Rarely or none of the time to Most or all of the time (0 to 3). Question scores were then summed to provide an overall score ranging from 0 to 30. A higher score indicates greater depression. The internal consistency reliability was acceptable (α = 0.75). The scale has been widely used and tested with Black and sexual minority populations (Conerly et al., 2002; L. F. Graham et al., 2011).
Data analysis
Data preparation, management, and analysis were performed using Stata 17. Descriptive statistics were used to describe all variables and the sample. To examine the relations between the primary independent variable (internalized homophobia), mediating variables, and outcome of depression, multiple pathways were analyzed, including a series of regressions, following the framework outlined by Baron and Kenny (1986). Before analysis, several assumptions were examined, and diagnostic tests were performed, including linearity between the variables, errors that are normally distributed, homoscedasticity of errors, and independence of the observations. Listwise deletion of missing data was performed with 4.6% (n = 236) of missing observations. Indirect effect analysis was completed using the RMediation package (Tofighi and MacKinnon, 2011). Total effects were also calculated.
Results
Sample description
Table 1 contains demographic information. The mean age of the participants was 31.1 years (SD = 10.1). In terms of sexual orientation identity, 79.7% (n = 4,089) of the sample identified as gay or same-gender loving, followed by bisexual (17.5%; n = 900), and another identity (1.5%; n = 77). Further, 36.2% (n = 1842) of participants reported having completed some college or technical school, followed by college graduate (35.7%; n = 1,815), High school/GED (21.0%; n = 1,068), and less than High school/GED (7.1%; n = 361). Participants also reported on average, 6.7 (SD = 4.9; range 0–30) depression symptoms, and on average, 1.3 (SD = 1.0; range 0–4) score on internalized homophobia.
Table 1
| Age, mean (SE) | 31.1 (SD = 10.1) |
| Education, No. (%) | |
| <High school/GED | 361 (7.09) |
| High school/GED | 1,068 (21.00) |
| Some college or technical school | 1,842 (36.22) |
| College graduate | 1,815 (35.68) |
| Sexual orientation identity, No. (%) | |
| Gay or same-gender loving | 4,089 (79.66) |
| Bisexual | 900 (17.53) |
| Other (e.g., heterosexual, MSM) | 77 (1.50) |
| Annual income | |
| $0–9,999 | 1,023 (20.24) |
| $10,000 – $29,999 | 1,344 (26.59) |
| $30,000 – $49,999 | 1,332 (26.36) |
| $50,000 – $69,999 | 385 (14.54) |
| $70,000 – $89,999 | 735 (7.62) |
| $90,000 – and up | 235 (4.65) |
| Depression symptomsa, mean (SD) | 6.66 (4.89) |
| Internalized homophobiab, mean (SD) | 1.34 (1.01) |
| Types of Supportc, mean (SD) | |
| Lower Friend | 0.71 (1.05) |
| Lower Gay Community | 1.05 (1.11) |
| Lower Black Community | 1.25 (1.10) |
| Lower Family | 1.03 (1.13) |
| City | |
| Atlanta | 1,472 (28.67) |
| Detroit | 658 (12.82) |
| Houston | 1,135 (22.11) |
| Memphis | 84 (1.64) |
| Philadelphia | 709 (13.81) |
| Washington, DC | 1,076 (20.96) |
| Year of data collection, No. (%) | |
| 2014 | 1,500 (29.22) |
| 2015 | 1,725 (33.60) |
| 2016 | 1,331 (25.93) |
| 2017 | 578 (11.26) |
Sample characteristics.
Analytic sample n = 4,430; aRange = 0 to 30, with higher values indicative of greater depression symptoms. bRange = 0 to 4, with higher values indicative of greater internalized homophobia. cRange = 0 to 3, with higher values indicative of lower levels of support.
Internalized homophobia, social support, and depression symptoms
We conducted a multiple mediation model to examine types of social support mediating the relationship between internalized homophobia and depression symptoms. Intercorrelations between variables in the mediation models are presented in Table 2. As shown in Figure 1, the direct effect of internalized homophobia was positively associated with depression symptoms. Lower family, friend, and Black community support (independent of each other) were associated with depression. The pathways to depression, indirect effects, and total effects of these mediators are shown in Table 3 symptoms.
Table 2
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Internalized homophobia | 1.0 | |||||
| 2. Depression symptoms | 0.29 | 1.0 | ||||
| 3. Lower friend support | 0.44 | 0.25 | 1.0 | |||
| 4. Lower gay community support | 0.36 | 0.20 | 0.58 | 1.0 | ||
| 5. Lower Black community support | 0.32 | 0.19 | 0.51 | 0.72 | 1.0 | |
| 6. Lower Family support | 0.37 | 0.23 | 0.67 | 0.50 | 0.51 | 1.0 |
Correlations between primary study variables.
All values were significant at the 0.001 alpha level.
Figure 1
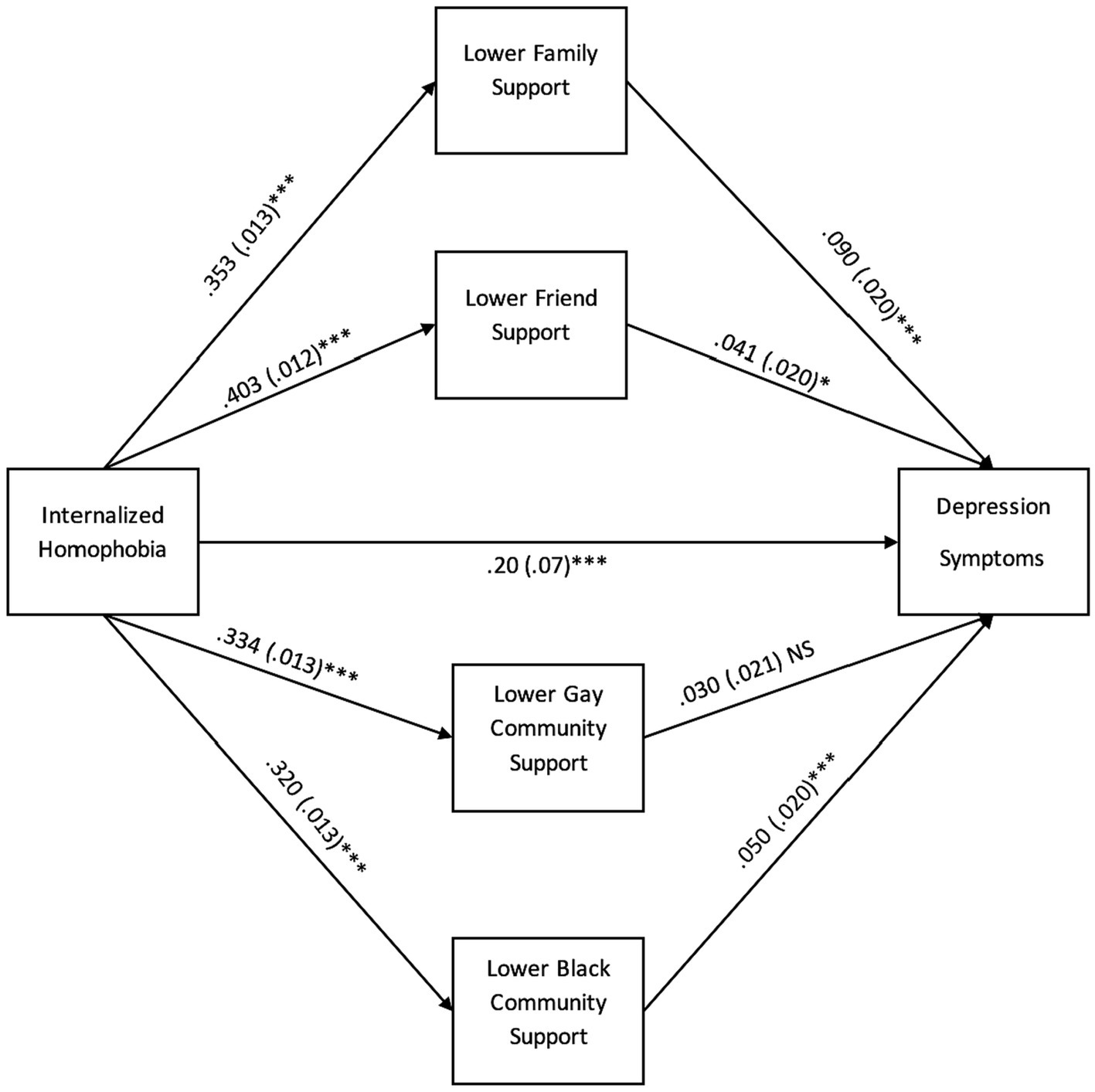
Mediation pathways to depression symptoms through multiple types of support. *p < 0.05, **p < 0.01, *** p < 0.001, NS, non-significant. Standard errors (SE) are in parentheses. All coefficients are standardized.
Table 3
| TE | β | SE | 95% CI | |
|---|---|---|---|---|
| Lower family (LFM) | 0.232 | |||
| IH → LFM | 0.353*** | 0.013 | [0.328, 0.378] | |
| LFM → DS | 0.090*** | 0.019 | [0.053, 0.127] | |
| IE | 0.032 | 0.007 | [0.019, 0.045] | |
| Lower friend (LFD) | 0.217 | |||
| IH → LFD | 0.403*** | 0.012 | [0.380, 0.426] | |
| LFD → IH | 0.040* | 0.020 | [0.002, 0.080] | |
| IE | 0.017 | 0.008 | [0.001, 0.032] | |
| Lower gay community (LGC) | NS | |||
| IH → LGC | 0.334*** | 0.013 | [0.309, 0.360] | |
| LGC → DS | 0.030 (NS) | 0.021 | [−0.012, 0.069] | |
| IE | 0.009 (NS) | 0.007 | [−0.004, 0.023] | |
| Lower Black community (LBC) | 0.214 | |||
| IH → LBC | 0.320 | 0.013 | [0.291, 0.343] | |
| LBC → DS | 0.050*** | 0.020 | [0.006, 0.085] | |
| IE | 0.015 | 0.006 | [0.002, 0.027] |
Pathway analysis to depression.
R 2 = 13.6% of the variance. Values are standardized path coefficients. IE, Indirect Effect; TE, Total Effect for significant variables; CI, Confidence Interval; DS, Depression Symptoms. *p < 0.05, **p < 0.01, ***p < 0.001, NS, non-significant.
Control variable results
We adjusted for age, sexual orientation, education level, income level, city of data collection, and year of data collection to the outcome of depression. These individual predictors were examined and indicated the following coefficients and p values: age (β = 0.031, SE = 0.01, z = 2.28, p = 0.022), sexual orientation (β = −0.02, SE = 0.01, z = −2.12, p = 0.034), education (β = −0.059, SE = 0.02, z = −3.89, p = 0.00), income level (β = −0.13, SE = 0.014, z = −8.66, p = 0.00), city of data collection (β = −0.02, SE = 0.014, z = −1.48, p = 0.14), year of data collection (β = −0.002, SE = 0.014, z = 0.20, p = 0.84).
Discussion
This is the first study to our knowledge to examine the relationship between internalized homophobia and depression as mediated by various types of support in a large sample of BSMM. Overall, the study extends our knowledge of how varying types of support may operate with these men in the context of internalized homophobia and depression. These findings are consistent with our hypotheses that family, friend, and Black support partially mediate the relationship between internalized homophobia and depression symptoms. However, we did not find evidence that lower gay community support is independently associated with depression symptoms or mediates the relationship between internalized homophobia and depression symptoms.
The mainstream gay community’s cultural norms within the United States largely privilege White Eurocentric norms (Han, 2007). Thus, it is unsurprising that there was no significant effect for gay community support relating to depression for Black sexual minority men. In contrast, the other forms of support were significant. Within the United States, the gay community, including gay advocacy organizations (Adams, 2019) and online dating platforms (Callander et al., 2015; Wade et al., 2021), have long been criticized for ascribing to mostly White standards (e.g., music, art) and social values (e.g., beauty esthetics, hyper-secularism) that do not serve Black men along with other racial minorities (Han et al., 2017; Pingel and Bauermeister, 2018; Worthen, 2018). Therefore, these environments, such as dating apps, social clubs, and informal networks, largely remain alienating to the culturally-specific psychosocial needs of queer men of color. For this current sociocultural landscape to shift, gay community events, platforms, and civic and social groups must make additional efforts to become more racially inclusive, affirming by further integrating the cultural mores of BSMMn and having leadership positions for BSMM. These issues are often found in societies with histories of colonization, enslavement, and/or modern forms of social oppression stemming from White European supremacy (e.g., Logie and Rwigema, 2014; Durban, 2021; Wahab, 2021).
Family support had the strongest association among all the mediators, demonstrating that familial relationships are a salient factor for mitigating depression in this population. Yet, examining and leveraging family ties to improve BSMM mental health is underutilized (Dawes et al., 2022). Studies (Ryan et al., 2010; Swendener and Woodell, 2017; Boyd et al., 2021) have shown that family acceptance of sexual minorities, which includes identity affirmation, improved communication, and family activities, can have a robust effect on improving sexual minorities’ self-concepts (e.g., self-esteem), and longer-term mental health outcomes. Mental health service providers and systems should assess family factors and develop interventions centered around families, including the family of origin and extended families, among BSMM struggling with internalized homophobia and depression. The aims of these interventions should focus on improving weak family links and maintaining strong ones between BSMM and their families. With anti-sexual minority bias and stigma potentially operating as primary influences on deleterious relationships, they must be targeted. Therefore, interventions should recognize the harmful influence of homophobia and heterosexism by addressing discrimination and other anti-queer bias that BSMM and their families often internalize. Research (Pingel and Bauermeister, 2018) shows that Black people are largely a religious population group; therefore, affirming religious communities and leaders offer a critical platform for mental health practitioners and systems to create collaborative relationships. Church and other religious groups may be able to educate Black families in intervening to reduce BSMM’s depression and its adverse consequences.
Implications for mental health systems and policy
Due to stigmatization and access to care issues, BSMM face inadequate mental health systems to meet their needs. Several barriers exist for BSMM to receive ideal treatment, such as payer source issues and unresponsive mental health systems and providers (Dawes et al., 2022). Low-income BSMM in particular may have limited access to mental health care due to relatively high-cost private pay session rates and overall disinvestment of community mental health centers (Morrissey and Goldman, 2020). Such barriers make it difficult to attend weekly or bi-weekly therapy sessions necessary for adequate depression treatment. Due to higher costs, residential or intensive outpatient groups may be an even greater challenge for those needing higher levels of treatment. Moreover, many mental health systems and providers choose not to take public or private insurance; conversely, when providers take insurance, BSMM often continue not to have access (Dawes et al., 2022). Thirty-four percent of the general public with private insurance report having difficulty locating an in-network therapist (Petersen, 2021). Furthermore, many BSMM work as contract employees, freelancers, or gig workers, who are not entitled to employer-sponsored health insurance or meeting income thresholds for public programs such as Medicaid (Gelles-Watnick and Anderson, 2021). Furthermore, public mental health funds may not provide the long-term treatment needed to address depression fully. These payer source issues create a sizeable obstacle regarding payer source targeting BSMM’s depression.
Mental health services and systems are largely led and provided by White heterosexual practitioners, creating a treatment milieu with few BSMM providers informing care (Callahan et al., 2018). These contemporary systems have been characterized as having policies and interpersonal biases that thwart affirming care for BSMM. To resolve this situation, recommendations include developing intersectional informed mental health training for providers and systems, supporting efforts to diversify the mental health workforce along the lines of sexual orientation and race, and developing systems policies that center BSMM’s needs and treatment concerns. Additionally, there are a growing number of individual and group-based mental health interventions focusing on intersectional oppression among BSMM that will need mental health system adoption for adequate further treatment proliferation (Jackson et al., 2022). Policymakers on the federal, state, and systems levels have a role in eliminating barriers to care, creating comprehensive mental health coverage policies, and ensuring that the mental health workforce is diverse and treatment approaches are intersectionally responsive to BSMM.
Limitations
Although the study has several strengths, it has certain limitations regarding the generalizability and causal inference of study results. The sample was a convenience sample of BSMM who attended pride events; therefore, there is a possible selection bias in that BSMM who may have high rates of internalized homophobia would likely not attend a pride event. These findings are limited by the cross-sectional design, with the mediators, predictors, and outcomes being measured concurrently. Therefore, there are concerns regarding temporal ordering and causal inference. Finally, the measurement of support variables could be more robust by adding additional items to measure the multidimensionality of social support for BSMM more precisely.
Future research
Future work should concentrate on longitudinal design and analysis to examine the temporal mechanisms of multiple forms of social support in mitigating internalized oppression and depression within BSMM. Further investigation is needed to identify the other formal social supports unique to queer Black communities that have not been identified or explored thus far, including Black spiritual community support, support from chosen family, or support from the queer Black community. Indeed, an intersectionality approach is needed to identify social stressors and oppressive systems affecting BSMM, investigate unique forms of internalized oppression, and develop effective interventions for these psychosocial stressors and mental health issues among BSMM. Strengthening this work with better detection of intermediate variables and their impact on depression prevention and clinical depression interventions for BSMM will promote mental health equity.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
HD conceptualized the study and led the study design. HD, TE, WH, AS, DW, and DM analyzed the data, interpreted the results, wrote, and edited parts of the manuscript. All authors approved the manuscript as submitted.
Funding
This research was supported by the National Institute of Nursing Research (grant R01NR013865), the National Institute of Allergy and Infectious Diseases (grant R21AI120777), and the National Institute of Mental Health (grant T32MH094174). Additionally, this research was partially supported by the Robert Johnson Foundation’s Health Policy Research Scholars program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Adams T. (2019). The Progression of the LGBTQ+ rights movement in the United States: The Human Rights Campaign [DePauw]. Available at: https://scholarship.depauw.edu/cgi/viewcontent.cgi?article=1105&context=studentresearch (Accessed April 21, 2023)
2
Amola O. Grimmett M. A. (2015). Sexual identity, mental health, HIV risk behaviors, and internalized homophobia among Black men who have sex with men. J. Couns. Dev.93, 236–246. doi: 10.1002/j.1556-6676.2015.00199.x
3
Andresen E. M. Malmgren J. A. Carter W. B. Patrick D. L. (1994). Screening for depression in well older adults: evaluation of a short form of the CES-D. Am. J. Prev. Med.10, 77–84. doi: 10.1016/S0749-3797(18)30622-6
4
Argyriou A. Goldsmith K. A. Rimes K. A. (2021). Mediators of the disparities in depression between sexual minority and heterosexual individuals: a systematic review. Arch. Sex. Behav.50, 925–959. doi: 10.1007/s10508-020-01862-0
5
Arnold E. A. Rebchook G. M. Kegeles S. M. (2014). ‘Triply cursed’: racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Cult. Health Sex.16, 710–722. doi: 10.1080/13691058.2014.905706
6
Baron R. M. Kenny D. A. (1986). The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol.51, 1173–1182. doi: 10.1037/0022-3514.51.6.1173
7
Boyd D. T. Ramos S. R. Quinn C. R. Jones K. V. Wilton L. Nelson L. E. (2021). Family support and sociocultural factors on depression among Black and Latinx sexual minority men. Int. J. Environ. Res. Public Health18:Article 13. doi: 10.3390/ijerph18136759
8
Brooks V. R. (1981). Minority stress and lesbian women. Lanham, MD: Lexington Books.
9
Callahan J. L. Smotherman J. M. Dziurzynski K. E. Love P. K. Kilmer E. D. Niemann Y. F. et al . (2018). Diversity in the professional psychology training-to-workforce pipeline: results from doctoral psychology student population data. Train. Educ. Profes. Psychol.12, 273–285. doi: 10.1037/tep0000203
10
Callander D. Newman C. E. Holt M. (2015). Is sexual racism really racism? Distinguishing attitudes toward sexual racism and generic racism among gay and bisexual men. Arch. Sex. Behav.44, 1991–2000. doi: 10.1007/s10508-015-0487-3
11
Conerly R. C. Baker F. Dye J. Douglas C. Y. Zabora J. (2002). Measuring depression in African American cancer survivors: the reliability and validity of the center for epidemiologic study—depression (CES-D) scale. J. Health Psychol.7, 107–114. doi: 10.1177/1359105302007001658
12
Dawes H. C. Williams D. Y. Klein L. Forte A. B. Gibbs D. J. McGarry B. et al . (2022). Experiences of queer people of color in mental health services and substance use treatment services: a systematic review. J. Soc. Soc. Work Res.14, 721–755. doi: 10.1086/721454
13
Dawson E. L. Mendoza M. C. B. Gaul Z. Jeffries W. L. IV Sutton M. Y. Wilson P. A. (2019). Resilience, condom use self-efficacy, internalized homophobia, and condomless anal sex among Black men who have sex with men, New York City. PLoS One14:e0215455. doi: 10.1371/journal.pone.0215455
14
Durban E. L. (2021). Whither homophobia? Rethinking a bad object for queer studies from the Black global south. QED8, 49–78. doi: 10.14321/qed.8.1.0049
15
Eaton L. A. Matthews D. D. Bukowski L. A. Friedman M. R. Chandler C. J. Whitfield D. L. et al . (2018). Elevated HIV prevalence and correlates of PrEP use among a community sample of Black men who have sex with men. J. Acquir. Immune Defic. Syndr.79, 339–346. doi: 10.1097/QAI.0000000000001822
16
English D. Carter J. A. Boone C. A. Forbes N. Bowleg L. Malebranche D. J. et al . (2021). Intersecting structural oppression and Black sexual minority men’s health. Am. J. Prev. Med.60, 781–791. doi: 10.1016/j.amepre.2020.12.022
17
Friedman M. R. Bukowski L. Eaton L. A. Matthews D. D. Dyer T. V. Siconolfi D. et al . (2019). Psychosocial health disparities among Black bisexual men in the U.S.: effects of sexuality nondisclosure and gay community support. Arch. Sex. Behav.48, 213–224. doi: 10.1007/s10508-018-1162-2
18
Gelles-Watnick R. Anderson M. (2021). Racial and ethnic differences stand out in the U.S. gig workforce. Pew Research Center. Available at: https://www.pewresearch.org/short-reads/2021/12/15/racial-and-ethnic-differences-stand-out-in-the-u-s-gig-workforce/ (Accessed May 05, 2021)
19
Graham L. F. Aronson R. E. Nichols T. Stephens C. F. Rhodes S. D. (2011). Factors influencing depression and anxiety among Black sexual minority men [research article]. Depres. Res. Treatment2011, 1–9. doi: 10.1155/2011/587984
20
Graham J. R. West L. M. Martinez J. Roemer L. (2016). The mediating role of internalized racism in the relationship between racist experiences and anxiety symptoms in a Black American sample. Cultur. Divers. Ethnic Minor. Psychol.22, 369–376. doi: 10.1037/cdp0000073
21
Han C. (2007). They don’t want to cruise your type: gay men of color and the racial politics of exclusion. Soc. Ident.13, 51–67. doi: 10.1080/13504630601163379
22
Han C. Ayala G. Paul J. P. Choi K.-H. (2017). West Hollywood is not that big on anything but white people: constructing “gay men of color”. Sociol. Q.58, 721–737. doi: 10.1080/00380253.2017.1354734
23
Heiden-Rootes K. Wiegand A. Thomas D. Moore R. M. Ross K. A. (2020). A national survey on depression, internalized homophobia, college religiosity, and climate of acceptance on college campuses for sexual minority adults. J. Homosex.67, 435–451. doi: 10.1080/00918369.2018.1550329
24
Herek G. Cogan J. Gillis J. R. Glunt E. (1997). Correlates of internalized homophobia in a community sample of lesbians and gay men. J. Gay Lesbian Med. Assoc.2, 17–25.
25
Jackson S. D. Wagner K. R. Yepes M. Harvey T. D. Higginbottom J. Pachankis J. E. (2022). A pilot test of a treatment to address intersectional stigma, mental health, and HIV risk among gay and bisexual men of color. Psychotherapy59, 96–112. doi: 10.1037/pst0000417
26
Jones J. M. (2021). LGBT identification in U.S. ticks up to 7.1%. Available at: https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx (Accessed September 17, 2022)
27
Logie C. H. Rwigema M.-J. (2014). “The normative idea of queer is a white person”: understanding perceptions of white privilege among lesbian, bisexual, and queer women of color in Toronto, Canada. J. Lesbian Stud.18, 174–191. doi: 10.1080/10894160.2014.849165
28
Lytle M. C. De Luca S. M. Blosnich J. R. (2014). The influence of intersecting identities on self-harm, suicidal behaviors, and depression among lesbian, gay, and bisexual individuals. Suicide Life Threat. Behav.44, 384–391. doi: 10.1111/sltb.12083
29
MacKinnon D. P. Lockwood C. M. Hoffman J. M. West S. G. Sheets V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychol. Methods7, 83–104. doi: 10.1037/1082-989X.7.1.83
30
Meyer I. H. (1995). Minority stress and mental health in gay men. J. Health Soc. Behav.36, 38–56. doi: 10.2307/2137286
31
Meyer I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull.129, 674–697. doi: 10.1037/0033-2909.129.5.674
32
Meyer I. H. (2010). Identity, stress, and resilience in lesbians, gay men, and bisexuals of color. Couns. Psychol.38, 442–454. doi: 10.1177/0011000009351601
33
Moradi B. DeBlaere C. Huang Y.-P. (2010a). Centralizing the experiences of LGB people of color in counseling psychology. Couns. Psychol.38, 322–330. doi: 10.1177/0011000008330832
34
Moradi B. Wiseman M. C. DeBlaere C. Goodman M. B. Sarkees A. Brewster M. E. et al . (2010b). Lgb of color and white individuals’ perceptions of heterosexist stigma, internalized homophobia, and outness: comparisons of levels and links. Couns. Psychol.38, 397–424. doi: 10.1177/0011000009335263
35
Morrissey J. P. Goldman H. H. (2020). “Division of labor: function shifts and realigned responsibilities in the evolving mental health services system” in The Palgrave handbook of American mental health policy. eds. GoldmanH. H.FrankR. G.MorrisseyJ. P. (New York: Springer International Publishing), 21–47.
36
National Center for Health Statistics . (2019). Key statistics from the national survey of family growth. National Center for Health Statistics. Available at: https://www.cdc.gov/nchs/nsfg/key_statistics_2015_2017.htm (Accessed November 6, 2019)
37
Newcomb M. E. Mustanski B. (2010). Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clin. Psychol. Rev.30, 1019–1029. doi: 10.1016/j.cpr.2010.07.003
38
Pearlin L. I. Bierman A. (2013). “Current issues and future directions in research into the stress process” in Handbook of the sociology of mental health. eds. AneshenselC. S.PhelanJ. C.BiermanA. (Dordrecht: Springer Netherlands), 325–340.
39
Petersen A. (2021). Why it’s so hard to find a therapist who takes insurance. Wall Street Journal. Available at:https://www.wsj.com/articles/why-its-so-hard-to-find-a-therapist-who-takes-insurance-11633442400 (Accessed October 5, 2021)
40
Pingel E. S. Bauermeister J. A. (2018). ‘Church hurt can be the worst hurt’: community stakeholder perceptions of the role of Black churches in HIV prevention among young Black gay and bisexual men. Cult. Health Sex.20, 218–231. doi: 10.1080/13691058.2017.1338756
41
Puckett J. A. Woodward E. N. Mereish E. H. Pantalone D. W. (2015). Parental rejection following sexual orientation disclosure: impact on internalized homophobia, social support, and mental health. LGBT Health2, 265–269. doi: 10.1089/lgbt.2013.0024
42
Rowen C. J. Malcolm J. P. (2003). Correlates of internalized homophobia and homosexual identity formation in a sample of gay men. J. Homosex.43, 77–92. doi: 10.1300/J082v43n02_05
43
Ryan C. Russell S. T. Huebner D. Diaz R. Sanchez J. (2010). Family acceptance in adolescence and the health of lgbt young adults. J. Child Adolesc. Psychiatr. Nurs.23, 205–213. doi: 10.1111/j.1744-6171.2010.00246.x
44
Shidlo A. (1994). “Internalized homophobia: conceptual and empirical issues in measurement” in Lesbian and gay psychology: Theory, research, and clinical applications (Thousand Oaks, CA: Sage Publications, Inc.), 176–205.
45
Smallwood S. W. Spencer S. M. Ingram L. A. Thrasher J. F. Thompson-Robinson M. V. (2017). Examining the relationships between religiosity, spirituality, internalized homonegativity, and condom use among African American men who have sex with men in the deep south. Am. J. Mens Health11, 196–207. doi: 10.1177/1557988315590835
46
Sutter M. Perrin P. (2016). Discrimination, mental health, and suicidal ideation among lgbtq people of color. J. Couns. Psychol.63, 98–105. doi: 10.1037/cou0000126
47
Swendener A. Woodell B. (2017). Predictors of family support and well-being among Black and Latina/o sexual minorities. J. GLBT Fam. Stud.13, 357–379. doi: 10.1080/1550428X.2016.1257400
48
Szymanski D. M. Kashubeck-West S. Meyer J. (2008). Internalized heterosexism: measurement, psychosocial correlates, and research directions. Couns. Psychol.36, 525–574. doi: 10.1177/0011000007309489
49
Tofighi D. MacKinnon D. P. (2011). RMediation: an R package for mediation analysis confidence intervals. Behav. Res. Methods43, 692–700. doi: 10.3758/s13428-011-0076-x
50
United States Census Bureau . (2022). United States Census Bureau. Available at: https://www.census.gov/quickfacts/fact/table/US/PST045221 (Accessed June 5, 2022)
51
Vincent W. Peterson J. L. Huebner D. M. Storholm E. D. Neilands T. B. Rebchook G. M. et al . (2020). Resilience and depression in young Black men who have sex with men: a social-ecological model. Stigma Health5, 364–374. doi: 10.1037/sah0000206
52
Wade R. M. Bouris A. M. Neilands T. B. Harper G. W. (2021). Racialized sexual discrimination (rsd) and psychological wellbeing among young sexual minority Black men (ysmbm) who seek intimate partners online. Sex. Res. Social Policy19, 1341–1356. doi: 10.1007/s13178-021-00676-6
53
Wahab A. (2021). “The darker the fruit”? Homonationalism, racialized homophobia, and neoliberal tourism in the St Lucian–US contact zone. Int. Fem. J. Polit.23, 80–101. doi: 10.1080/14616742.2020.1758589
54
Worthen M. G. F. (2018). “Gay equals white”? Racial, ethnic, and sexual identities and attitudes toward lgbt individuals among college students at a bible belt university. J. Sex Res.55, 995–1011. doi: 10.1080/00224499.2017.1378309
Summary
Keywords
internalized homophobia, depression, Black sexual minority, social support, mediation
Citation
Dawes HC, Eden TM, Hall WJ, Srivastava A, Williams DY and Matthews DD (2024) Which types of social support matter for Black sexual minority men coping with internalized homophobia? Findings from a mediation analysis. Front. Psychol. 15:1235920. doi: 10.3389/fpsyg.2024.1235920
Received
06 June 2023
Accepted
11 January 2024
Published
06 February 2024
Volume
15 - 2024
Edited by
Himadri RoyChaudhuri, Xavier School of Management, India
Reviewed by
Byron Brooks, Loyola University Chicago, United States
Mark Vicars, Victoria University, Australia
Updates
Copyright
© 2024 Dawes, Eden, Hall, Srivastava, Williams and Matthews.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hayden C. Dawes, hcdawes@live.unc.edu
†Present address: Hayden C. Dawes, Graduate School of Social Work and Social Research, Byrn Mawr College, Byrn Mawr, PA, United States
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.