Abstract
This narrative review explores the integration of mindfulness-based interventions (MBIs) into musculoskeletal (MSK) care, based on the premise that addressing the mind–body interface can enhance patient outcomes. First, we outline how chronic stress affects twelve physiological systems and contributes to the onset and persistence of MSK conditions. Second, we synthesise evidence showing that MBIs mitigate these stress effects through mechanisms such as improved attention regulation, interoceptive awareness, and reduced catastrophising. Third, we highlight Neuro-Emotional Technique (NET) as a practitioner-facilitated hybrid-MBI exemplar that targets unresolved emotional stress patterns and aligns with the biopsychosocial model of healthcare. We also note contraindications via red and yellow flag considerations, emphasising the importance of careful patient selection and responsible application. Taken together, this review provides a rationale for incorporating MBIs as adjuncts to conventional therapies, supporting recovery, fostering resilience, and advancing patient-centred MSK care.
Introduction
Healthcare has long grappled with the separation of mind and body, a concept deeply rooted in Western medicine’s historical and philosophical traditions. Although this separation facilitated the development of specialised treatments, it also led to a fragmented approach to patient care, overlooking the interconnected nature of mental and physical health (World Health Organization, 2024). In this narrative review, we propose that musculoskeletal (MSK) practitioners consider mindfulness-based interventions (MBIs) as part of an integrative approach to care – a perspective presented to, but not widely adopted by, this audience in recent years.
The literature on the practical application of mindfulness interventions in MSK therapies remains sparse. This review therefore draws together evidence on the interdependence between psychological and physical well-being, the effects of chronic stress on twelve major physiological systems, and how MBIs may counteract these detrimental stress effects (Robinson, 2023; Canadian Mental Health Association Ontario, 2014). In view of the influence of stress on conditions commonly managed in MSK practice, considering mind–body factors forms part of a comprehensive duty of care to provide safe and effective treatment.
Aim and scope
The aim of this narrative review is threefold. First, we outline how chronic stress contributes to MSK conditions across biological, psychological, and social domains. Second, we synthesise evidence demonstrating how MBIs mitigate stress-related mechanisms and provide a rationale for their application alongside MSK therapies. Third, we highlight Neuro-Emotional Technique (NET) as an exemplar of a practitioner-facilitated hybrid-MBI, illustrating how such approaches may be operationalised in MSK practice. Together, these aims address the impact of MBIs on health, review an example of good practice, and clarify clinical decision-making considerations for MSK practitioners.
Background: the historical context of mind–body dualism
The dichotomy between mind and body has been a subject of philosophical debate for centuries. In the 4th century BC, Plato lamented, “the great error of our day in the treatment of the human body [is] that physicians separate the mind from the body (Maté, 2024).” Despite this, the dualistic approach became entrenched in Western medicine, heavily influenced by René Descartes’ 17th-century philosophy, which posited that the mind and body are fundamentally distinct entities. This view shaped medical practice for centuries, emphasizing the treatment of physical symptoms while often neglecting psychological aspects of health (Mantri, 2008).
However, integrative healthcare approaches, such as those found in traditional Chinese medicine, Ayurveda, and other non-Western traditions, have long recognized the inseparability of mind and body in achieving optimal health (Fan, 2017). These, and other ancient traditions and philosophies, emphasize that physical symptoms often reflect underlying psychological distress and vice versa, ultimately founding what now know as “meditation” and “mindfulness.” While agreed definitions remain elusive due to contrasting cultural foundations and ideas (Chiesa, 2013; Awasthi, 2013; Baer, 2019; Grossman, 2011), Western pioneers like Hippocrates similarly advocated for treating patients holistically, considering both physical and psychological dimensions (Mantri, 2008).
Today, specialization in medical fields often leads to a narrow focus on specific conditions, neglecting the broader context of a patient’s overall health (Mantri, 2008). Although the concept of mind–body integration is becoming more widely accepted in holistic healthcare settings, its practical application remains limited in many mainstream complementary health practices. The interdisciplinary scientific field of psychoneuroimmunology (the study of the interactions between psychological states, the nervous system and the immune system) shows that poor mental or emotional health as a result of chronic or acute stress frequently overlaps with musculoskeletal pain and illness (Australian Institute of Health and Welfare, 2024; Mental Health Foundation UK, 2024b; Barbe and Barr, 2006; Aviña-Zubieta et al., 1997; Navarro-Ledesma et al., 2024; Malterud, 2010; Ahrens et al., 2012), with each influencing the other’s severity and progression (Doan et al., 2023). In this paper, the scientific evidence is discussed in detail for the purpose of aiding recognition of the many common ways stress-related illness presents to MSK practitioners, and the role of MBIs as adjunct lifestyle and treatment interventions for MSK therapies.
The need for a mind–body approach in MSK care
Musculoskeletal (MSK) practitioners, who focus on treating conditions related to the muscles, bones, and joints, often encounter patients with symptoms influenced by psychological factors. Conditions such as chronic back pain, fibromyalgia, tension headaches, and arthritis are frequently exacerbated by stress, anxiety, sleep loss, and emotional distress (Mills et al., 2019; Anxiety and Depression Association of America, 2024). This interconnection underscores the importance of adopting a holistic, integrative approach that addresses both physical and psychological health components (Dunn et al., 2024).
The holistic approach aligns with the biopsychosocial (BPS) model proposed by George Engel in 1977, which encourages healthcare providers to consider biological, psychological, and social factors in understanding health and disease (Engel, 1977). For MSK practitioners, this model offers a framework for addressing not just the physical symptoms but also the psychological and emotional contributors to a patient’s condition such as patient beliefs and expectations, and the influence of the interpersonal dynamics in clinical encounters on health outcomes. Ultimately, this approach can promote a more comprehensive understanding of their patients’ health, fostering recovery from physical ailments and enhancing overall well-being (Borrell-Carrió et al., 2004).
Understanding how chronic stress operates across these domains provides the foundation for examining its systemic physiological effects, outlined in the next section.
The effects of chronic stress on physical health
Stress is defined as a state of threatened homeostasis following exposure to adverse forces (Chrousos and Gold, 1992). Acute stress (lasting minutes or hours) may be adaptive and even beneficial (Dorn and Chrousos, 1993; Rudland et al., 2020). Chronic stress, however, persists for days, weeks, or months (Olff, 1999) and is a significant factor in the onset, progression, and exacerbation of many health conditions (American Psychological Association, 2022; Mental Health Foundation UK, 2024a; American Psychological Association, 2022). When physiological demands are exceeded (Koolhaas et al., 2011), chronic stress contributes to allostatic load (Salleh, 2008; McEwen, 1998; McEwen and Stellar, 1993; Juster et al., 2010), depletes the body’s adaptive capacity (Kazakou et al., 2023), resulting in maladaptation (Stratakis and Chrousos, 1995) and poorer health outcomes (Guidi et al., 2021; Parker et al., 2022).
These effects are mediated through the Hypothalamic–Pituitary–Adrenal (HPA) axis, the body’s central stress response system, and the Psycho-Immune-Neuroendocrine (PINE) network, which integrates neural, immune, and endocrine functions to maintain health (Kazakou et al., 2023; Hardy and Pollard, 2006; Chrousos, 2009; Mariotti, 2015; Morey et al., 2015; Charmandari et al., 2005; Chrousos and Kino, 2007; González-Díaz et al., 2017). Dysregulation of these psychophysiological systems contributes to widespread health impacts including chronic illness, musculoskeletal disorders, acute and chronic pain, and organ system dysfunction that can result due to unique genetic, epigenetic and environmental factors, and the influences of the past stressful experiences of the individual (Chapman et al., 2008).
This is particularly relevant for MSK practitioners as chronic stress contributes to the onset and persistence of many common musculoskeletal presentations (Salvagioni et al., 2017; NIB, 2021; Schneiderman et al., 2005), including tension-type headache (Bendtsen and Fernández-de-la-Peñas, 2011), neck, shoulder, and upper-limb pain (Cagnie et al., 2007; van den Heuvel et al., 2005; Bongers et al., 2006), temporomandibular joint pain (Fillingim et al., 2013; Manfredini et al., 2003; Manfredini et al., 2004), fibromyalgia (Paschali et al., 2021; McBeth and Silman, 2001), back pain (Linton, 2000), and myofascial trigger points (Bosque et al., 2023). Chronic stress can diminish function and contribute to illness across all major body systems (Figure 1).
Figure 1

The 12 body systems that chronic stress can affect.
These systemic mechanisms provide the biological and clinical context for understanding how stress is embedded within a biopsychosocial (BPS) model of MSK care.
The BPS model of stress in MSK care
Within the BPS model of MSK care, chronic stress functions at three levels: biologically through HPA and PINE dysregulation, psychologically through appraisal, attention, and avoidance patterns, and socially through contextual pressures such as workload or relationships. Mindfulness practices directly target these mechanisms (Maloney et al., 2024). By enhancing interoceptive awareness and attention regulation, and cultivating non-reactivity and acceptance, they can reduce muscle tension, pain sensitivity, catastrophizing, and fear-avoidance while improving adherence to active care (Todd and Aspell, 2022; Aboushaar and Serrano, 2024). This integration clarifies why stress-responsive MSK pain often improves when cognitive, affective, and behavioral dimensions are addressed alongside physical treatment (Dunn et al., 2024).
Because chronic stress operates across biological, psychological, and social domains, interventions that target multiple dimensions simultaneously are especially relevant. Mindfulness-based interventions (MBIs) represent one such approach. The following section therefore defines mindfulness and its principal categories before considering how different forms of MBIs apply to MSK practice.
Mindfulness and mindfulness based interventions (MBIs)
American professor Jon Kabat-Zinn, creator of Mindfulness-Based Stress Reduction (MBSR) program (Kabat-Zinn, 1990) and credited by many as the founder of the contemporary mindfulness movement, defines mindfulness as, “awareness that arises through paying attention, on purpose, in the present moment, non-judgementally,… in the service of self-understanding and wisdom (Mindful Staff, 2017).” The 9 attitudinal principles of mindfulness, according to Kabat-Zinn, are: nonjudging, patience, a beginner’s mind, trust, non-striving, acceptance, letting go, gratitude and generosity (Kabat-Zinn, 2024). These attitudes and principles can be applied across a broad spectrum of practices (Maloney et al., 2024) in two broad categories: Formal (high intensity) and Informal (low intensity).
-
Formal (high intensity) practices can be Dynamic (movement-based), Static (attention-based) or Hybrid practices that combine elements of both (Lutz et al., 2008; Dunn et al., 1999; Rao, 2011; Kabat-Zinn, 2003; Prakhinkit et al., 2014). They are usually facilitated by a practitioner or facilitator and often follow a given structure/process.
-
Informal (low intensity) practices tend to be less structured, less time-consuming [showing benefits in as little as a few minutes (Hanley et al., 2015; Palmer et al., 2023; Strohmaier et al., 2021; Pratt, 2024)] and more easily accessible (Vilhauer, 2024), helping increase stress resilience when performed daily (Manigault et al., 2021). Informal practices have been shown to be effective in reducing stress (Sparacio et al., 2024), and can be categorised broadly as either Daily Life Awareness practices or Brief Self-Directed practices.
Figure 2 provides a visual representation of the various categories and of MBIs, followed by some examples of each classification.
Figure 2
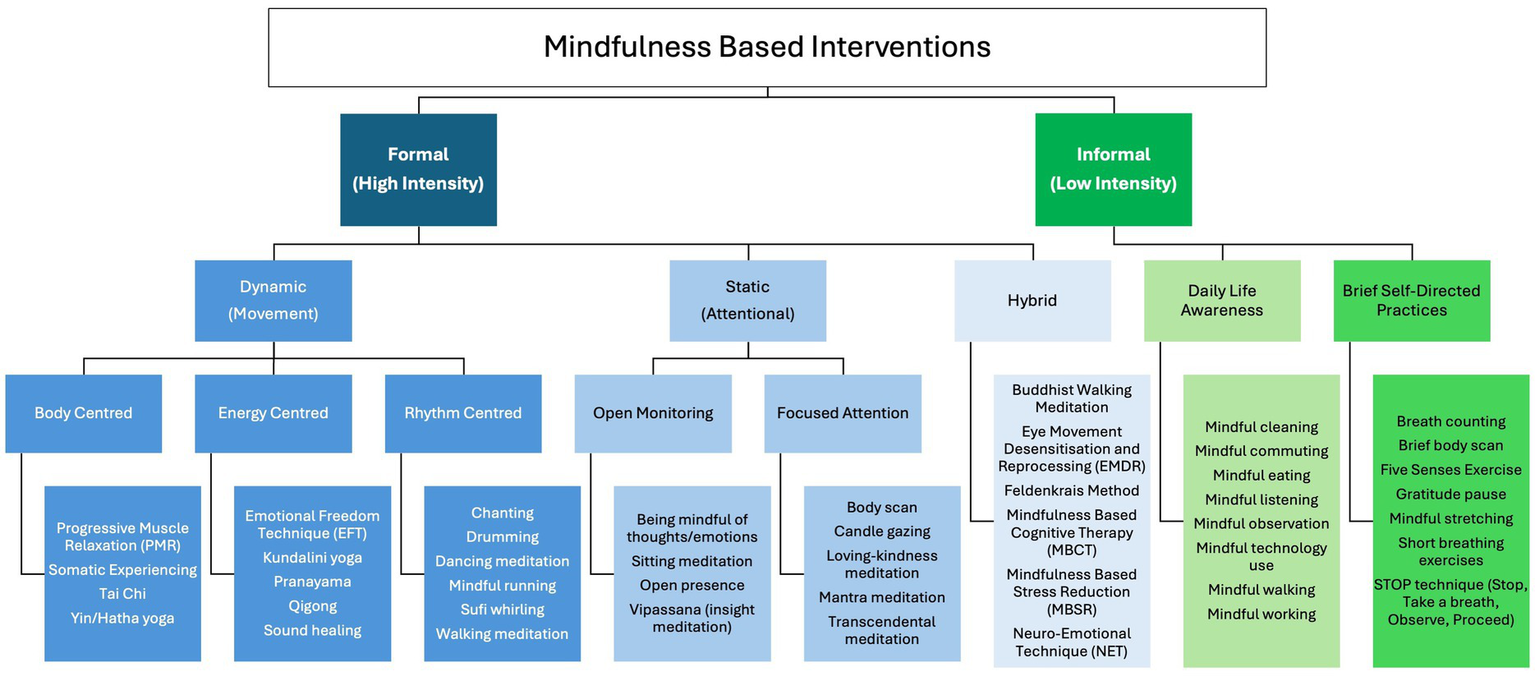
Categorisation of mindfulness based interventions (MBIs) including common examples.
Benefits of mindfulness-based interventions (MBIs)
Considering the pervasive health effects of chronic stress that anecdotally present in the practices of MSK practitioners, it is important to identify robust and reliable methods for counter-acting and relieving chronic stress alongside physical therapies. MBIs are practices that cultivate awareness, focus(attention), emotional regulation and acceptance of self and the present moment, with the goal of reducing chronic stress and enhancing well-being (Garland et al., 2017; Hölzel et al., 2011).
While the research assessing the effectiveness of mindfulness is continuing to evolve, and a greater number of high quality studies with larger sample sizes are needed (Zhang et al., 2021), a growing body of evidence supports the efficacy and safety of MBIs in addressing the physical and psychological effects of chronic stress (Carlson, 2012; Cardle et al., 2023; Pérez Fernández et al., 2022; Brown and Jones, 2013).
At the same time, the broader MBI literature is not without limitations. Systematic reviews consistently highlight heterogeneity in study designs, variability in intervention protocols, and modest effect sizes across conditions (Zhang et al., 2021; Ong et al., 2024). Publication bias and limited long-term follow-up data further constrain the strength of conclusions (Goldberg et al., 2022). In addition, while Table 1 summarises counter-stress effects across physiological systems, the current evidence does not permit firm conclusions about which types of MBIs (e.g., formal vs. informal, static vs. dynamic) are most efficient in producing these results (Preissner et al., 2025; Kakoschke et al., 2021). Comparative trials that directly examine format and delivery characteristics remain limited, and this represents an important area for future research.
Table 1
| Body system | Effects of chronic stress | Mechanisms of stress effects | Counter-stress effects of MBIs |
|---|---|---|---|
| Nervous system | Dysautonomia (Lucini et al., 2005), Neurotransmitter imbalances (Roth et al., 1988; Gray et al., 1989), Structural remodelling of brain areas (Mariotti, 2015; Hölzel et al., 2011; Lucassen et al., 2014; McEwen, 2007; Franklin et al., 2012; Gee et al., 2013; McEwen and Gianaros, 2011) | Chronic stress can cause dysregulation of the autonomic nervous system, leading to persistent “fight or flight” responses, fatigue, and exhaustion. It can also create neurotransmitter imbalances (e.g., dopamine, serotonin), affect brain structures like the pre-frontal cortex, and contribute to mood disorders such as depression or anxiety. | Enhanced cognitive functioning (McGreevey, 2011), structural brain changes in areas related to attention and emotional regulation (Tang et al., 2015), improved emotional regulation (Fox et al., 2014) |
| Endocrine system | Increased adrenaline and cortisol (Herman et al., 2016) leading to Hormonal dysregulation (Tsigos et al., 2000), Sleep disruption (Agorastos et al., 2020), Weight gain (Tsigos et al., 2000), Loss of bone density (Tsigos et al., 2000) | Prolonged stress activates the HPA axis, causing elevated cortisol levels, which may suppress immunity, accumulate visceral fat, and disrupt endocrine functions, affecting sleep, mood, digestion, reproductive health, cognitive function, and bone density. | Improved cortisol regulation (Pascoe et al., 2017), improved sleep quality (Black et al., 2015) and reduced fatigue (Zeng et al., 2019), reduced epigenetic expression of neuroendocrine dysfunction associated with type 2 diabetes (Yang et al., 2021) |
| Cardiovascular system | Heart disease and hypertension (Hemingway and Marmot, 1999; Gu et al., 2012), Increased risk of heart attack and stroke (Morey et al., 2015) | Stress-induced hormone release (e.g., adrenaline) can lead to heart disease, high blood pressure, and rhythm disturbances. Chronic stress also contributes to atherosclerosis, increasing the risk of heart attacks and strokes | Improved blood pressure (Thind et al., 2017; Wu et al., 2019; Gathright et al., 2019), reduced stress reactivity (Davis et al., 2015), reduced inflammation (Creswell et al., 2012; Black et al., 2013), improved lipid profile and BMI (Thind et al., 2017) |
| Immune SYSTEM | Inflammation (Mariotti, 2015; Black, 2002; Gu et al., 2012), Cancer (Kiecolt-Glaser et al., 2002), Autoimmunity (Stojanovich, 2010), Immunosuppression (Mariotti, 2015; Cacioppo et al., 1998) | Chronic stress overstimulates the neuroendocrine-immune axis, causing low-grade inflammation and heightened susceptibility to diseases (e.g., diabetes, cancer, auto-immune conditions) and mental health disorders. Increased HPA activation leads to immunosuppression, raising vulnerability to infections and slowing wound healing. | Reduced inflammation (Creswell et al., 2012; Black et al., 2013), enhanced immune function (Black and Slavich, 2016; Kaliman et al., 2014) |
| Digestive system | Inflammatory bowel conditions (IBS/IBD) (Collins, 2001; Labanski et al., 2020), Delayed gastric emptying and dysbiosis (Masere et al., 2009; Taché et al., 2001), disruption of gut microbiome (Chang et al., 2024) | Stress can cause or exacerbate gastrointestinal conditions like IBS and inflammatory bowel disease, affect digestive processes (e.g., motility, gastric emptying), and lead to dysbiosis (microbiota imbalance). | Improved biomarkers associated with IBD (González-Moret et al., 2020), increased gut microbial diversity (Wang et al., 2022) |
| Musculoskeletal system | Stress-related muscle tension (McFarlane, 2007), Arthritis (Buscemi et al., 2019), Pain (Finestone et al., 2008), Decreased bone density (Tsigos et al., 2000) | Chronic stress can increase muscle tension, causing pain and discomfort in areas like the back, neck, and shoulders. It can also lead to reduced bone density due to prolonged cortisol elevation, raising fracture risk. | Reduced pain and stress reactivity and better pain management (Davis et al., 2015; Riegner et al., 2024), reduced inflammation (Creswell et al., 2012; Black et al., 2013) |
| Metabolic system | Insulin resistance (Alam et al., 2016; Ahmed et al., 2015), Obesity (Chrousos, 2000; Streeten, 1993) | Stress can impair insulin sensitivity, contributing to Type 2 diabetes and conditions like Alzheimer’s (often called “Type 3 Diabetes”). Hormonal changes from stress can also increase cravings for high-sugar, high-fat foods, promoting weight gain. | Improved glucose and lipid metabolism (García-Campayo et al., 2018), enhanced glycaemic control (Thind et al., 2017; Dallman et al., 1993), reduced inflammation (Creswell et al., 2012; Black et al., 2013) |
| Reproductive system | Reduced fertility (Edwards et al., 2019), Menstrual irregularities and hormonal imbalances (Tsigos et al., 1999), Loss of Libido (Kyrou and Tsigos, 2008) | Stress affects fertility in both genders, with stress hormones disrupting menstrual cycles and reducing libido. | Reduced anxiety and depression (Spinelli et al., 2019), potential benefits in reproductive health (Ng et al., 2019), fertility (Li et al., 2016) and pregnancy (Dhillon et al., 2017; Abera et al., 2024), may reduce menopause-related stress (Liu et al., 2023) |
| Respiratory system | Asthma (Sandberg et al., 2000; Landeo-Gutierrez and Celedón, 2020), Hyperventilation (Suess et al., 1980), Increased Respiratory Infections (Graham et al., 1986; Drummond and Hewson-Bower, 1997) | Chronic stress can exacerbate respiratory conditions like asthma by triggering airway inflammation and hyperresponsiveness. It can also lead to hyperventilation and an increased frequency of respiratory infections due to a weakened immune response. | Reduced anxiety and stress (exacerbating factors for asthma) (Spinelli et al., 2019), reduced hyperventilation through breathwork (Balban et al., 2023), reduced respiratory infections (Zgierska et al., 2013; Barrett et al., 2012), improved asthma related clinical outcomes (Higgins et al., 2022) |
| Integumentary system | Hair Loss (Zhang et al., 2020), Skin disorders (e.g., Acne, Psoriasis) (Zhang et al., 2024; Chen and Lyga, 2014), Delayed wound healing (Gouin and Kiecolt-Glaser, 2012; Kiecolt-Glaser et al., 1995) | Stress affects the skin by increasing inflammatory processes and impairing the skin barrier function, leading to conditions such as acne and psoriasis. Additionally, chronic stress delays wound healing and may cause hair loss. | Reduced stress reactivity (Davis et al., 2015), better emotional regulation (Fox et al., 2014), improved inflammatory function (Black and Slavich, 2016), reduce inflammatory skin conditions (Graubard et al., 2021) such as psoriasis (Bartholomew et al., 2022) and atopic eczema (Harfenstellar, 2022) |
| Psychological wellbeing | Anxiety and depression (Mariotti, 2015; Won and Kim, 2016; Leonard, 2010; Kim et al., 2022), Cognitive decline (McEwen, 2007; Teixeira et al., 2015) | Chronic stress is a major risk factor for anxiety and depression due to chronic inflammation. It can also impair cognitive functions, such as memory, focus, and decision-making, due to the negative effects of stress hormones on the hypothalamus. | Reduced anxiety, depression, and distress (Kabat-Zinn et al., 1992; Hofmann et al., 2010; Spinelli et al., 2019; Ng et al., 2019), improved cognitive functioning (McGreevey, 2011), overall mental wellbeing (Gu et al., 2015), improved relationships (Carson et al., 2004), improved emotional regulation (González-Díaz et al., 2017; Fox et al., 2014), increased participation in healthy lifestyle behaviours (Rod et al., 2009) |
| Genome and Epigenome | Epigenetic modifications (Arzate-Mejia et al., 2024; Lutz et al., 2021; Muka et al., 2016), Altered Gene Expression (Cerniauskas et al., 2019; Musaelyan et al., 2020), Accelerated Aging (Yegorov et al., 2020; O'Donovan et al., 2012), Intergenerational health effects due to maternal gestational stress (Sandman et al., 2011; Cottrell and Seckl, 2009) | Stress can lead to epigenetic changes that alter gene expression without modifying the DNA sequence itself. These changes may accelerate aging processes and increase susceptibility to various diseases by affecting the regulation of genes involved in inflammation and immune response. | Epigenetic modifications counteracting stress effects (Gapp et al., 2016; McCreary et al., 2016), delayed biological aging (Horvath, 2013; Hannum et al., 2013; Chaix et al., 2017; Ren et al., 2012), enhanced genetic expression (Kaliman et al., 2014; Chaix et al., 2020). |
Chronic stress effects on body systems and the counter-stress effects of MBI.
Table 1 outlines the effects of chronic stress on different body systems and highlights current and emerging research of the counter-stress effects of MBIs.
When to use caution with MBIs
While MBIs have numerous benefits for countering the effects of chronic stress, they may not be universally suitable for everyone (Britton et al., 2021). For some individuals, particularly those with certain severe mental health conditions, MBIs can potentially trigger adverse effects. Identifying patients who exhibit “red” and “yellow” flags (Lustyk et al., 2009) is essential for making appropriate recommendations, as represented in our MSK decision flowchart (Figure 3).
Figure 3

Decision flowchart for MSK practitioners when considering MBIs.
Red flags are serious health indicators that require referral to a mental health specialist or emergency services, such as imminent harm to self or others, suicidal ideation, or self-harm. The MBSR standards of practice recognise this by excluding any participant with a psychological condition or suicidality (Santorelli, 2014; Dobkin et al., 2012). Research indicates that mindfulness practices may not be appropriate for people with severe psychological or psychiatric disorders, including but not limited to post-traumatic stress disorder (PTSD), acute anxiety, psychosis or severe depression (Van Dam et al., 2018; Creswell, 2017). (In contrast to older literature, more recent studies suggest that MBIs may indeed be beneficial for many sufferers of psychosis (Ellett, 2024), a reminder that this is still an evolving area of scientific enquiry).
Yellow flags include symptoms such as persistent low mood, emotional dysregulation and difficulty coping with stress. These indicators may be detected through clinical history taking or observation and, although less severe that red flags and adverse events (Binda et al., 2020), still require cautious monitoring by practitioners (Lindahl et al., 2017). Co-management with an appropriately qualified mental health professional should also be considered. Although some temporary emotional discomfort may be expected on the pathway to achieving the true benefits of mindfulness meditation (Binda et al., 2020; Lindahl et al., 2020) and should not be considered as harmful side effects (Baer and Kuyken, 2016), in a small number of cases self-reflective activities could exacerbate mental health symptoms, potentially leading to emotional numbness or distress, withdrawal, dissociation, increased anxiety, or even a resurgence of traumatic memories (Davidson and Kaszniak, 2015; Kuyken et al., 2022; Britton et al., 2021).
Therefore, before recommending MBIs it is important for MSK practitioners to implement clinical judgment and exercise appropriate caution in accordance with their scope of practice and duty of care (Farias and Wikholm, 2016). Careful patient selection and monitoring of patient responses for adverse reactions is essential to ensure that any emerging psychological complications are promptly identified and managed (Kuyken et al., 2008). To provide safe and effective care, MSK practitioners may consider establishing a referral network with qualified mental health professionals and seek to maintain open communication with these specialists when managing patients with complex psychological needs. Additionally, validated clinical tools known as Patient Reported Outcome Measures (PROMS) can assist with monitoring emotional wellbeing including the Depression, Anxiety and Stress Scale (DASS-21); (Antony et al., 1998; Lovibond and Lovibond, 1995), the Perceived Stress Scale (PSS) (Cohen et al., 1983), the Five Facet Mindfulness Questionnaire (FFMQ) (Baer et al., 2006), the Fear Avoidance Beliefs Questionnaire (FABQ) (Waddell et al., 1993), the Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001) and the Distress and Risk Assessment Method (DRAM) (Main and Waddell, 1991; Main et al., 1992). Taking a proactive approach ensures that patients receive appropriate and timely support, safeguarding both their physical and mental well-being.
Decision-making in MSK practice
In addition to recognising red and yellow flags, MSK practitioners must also exercise decision-making that balances clinical judgment, patient preference, and scope of practice. Indicators such as stress-related symptom exacerbation, high levels of catastrophising, maladaptive coping behaviours, or a history of stress-linked pain episodes may suggest suitability for adjunctive MBIs, whereas severe psychiatric illness, active trauma symptoms, or clear patient resistance may signal the need for referral instead. Practitioner training, access to referral networks, and resource availability further shape these decisions. By applying structured screening together with these broader clinical considerations, MBIs can be integrated safely and effectively into MSK practice as adjuncts to physical therapies.
For patients with no red or yellow flags, MSK practitioners can offer guidance to patients by suggesting MBIs that might be most appropriate according to the patient’s circumstances, personality and lifestyle by considering the individual needs, conditions, and histories and applying clinical judgement (Britton, 2019). This could involve providing recommendations for mindfulness resources or practices to try, referrals to suitably qualified mental health or mindfulness practitioners, or offering adjunct mindfulness-oriented techniques alongside, or in addition to, MSK therapies.
Neuro-emotional technique (NET) as an MBI for MSK therapies
Building on these findings, it is valuable to consider a practitioner-facilitated hybrid-MBI that exemplifies how such counter-stress effects can be integrated into musculoskeletal practice. Among the many MBIs, Neuro-Emotional Technique (NET) is highlighted here because it uniquely operationalises these principles within MSK practice through a practitioner-facilitated, structured method. Like the MBIs presented earlier in Table 1, NET has been associated with counter-stress effects across multiple systems, including neuroendocrine, immune, and musculoskeletal pathways, as highlighted below. It is therefore highlighted in this review as a representative model of how a practitioner-facilitated hybrid-MBI may operate within MSK care.
NET is a precision body–mind intervention (PBMI) (Bablis et al., 2024) that was developed by chiropractor Dr. Scott Walker in the 1980s using a 15-step methodology (Walker, 1996). Taught exclusively to registered health professionals, it is designed to identify and resolve emotional stress patterns known as Neuro-Emotional Complexes (NECs) (Walker, 1996), which are theorised to drive adverse physiological responses contributing to chronic pain and illness. NET combines elements from Traditional Chinese Medicine (TCM), Cognitive–Behavioural Therapy (CBT), and manual therapy (Foa and Jaycox, 1999), and employs the validated manual muscle test (Pollard et al., 2005; Cuthbert and Goodheart, 2007; Monti et al., 1999) as a biofeedback tool to detect stress-related responses. Recent publications suggest that NET reduces allostatic load (Bablis et al., 2024; Bablis et al., 2024) by addressing dysregulated stress response systems (HPA and PINE) (Stapelberg et al., 2015; Nold and Allers, 2020) already outlined earlier in this review. By resolving the emotional components of stress underlying chronic musculoskeletal pain and illness (Sharif et al., 2018), NET complements conventional physical therapies within a biopsychosocial model of care.
Mindfulness mechanisms and therapeutic process of NET
While the full 15-step NET procedure has been described in Walker’s manual (Walker, 1996) and reproduced in clinical trial protocols (Karpouzis et al., 2009), a condensed overview illustrates the therapeutic flow. NET typically involves: (1) identifying a stress-related physiological response via manual muscle testing, (2) linking this response to an unresolved emotional experience (the Neuro-Emotional Complex), (3) facilitating mindful awareness and cognitive reframing of the stressor, (4) applying a brief somatic intervention (such as spinal or acupoint stimulation) during recall, and (5) re-testing to confirm resolution (Walker, 1996; Karpouzis et al., 2009). This flow illustrates how NET engages somatic awareness, mindful attention, and cognitive reappraisal – mechanisms that underpin established mindfulness interventions.
Importantly, NET’s therapeutic elements can also be understood as cultivating Kabat-Zinn’s attitudinal foundations of mindfulness (Kabat-Zinn, 2024). Meridian-based somatic cueing (derived from TCM) directs non-judgmental awareness to bodily sensations and supports letting go. Cognitive–behavioural strategies such as reappraisal and exposure foster acceptance, patience, and non-striving. Manual therapy anchoring and practitioner touch cultivate trust, beginner’s mind, and embodied presence. Together, these components operationalise mindfulness attitudes in ways that are directly relevant to MSK practice (Table 2).
Table 2
| NET Component | Mindfulness attitude(s) | Clinical relevance in MSK care |
|---|---|---|
| Somatic cueing (TCM-informed) | Non-judging, letting go, awareness | Reduces vigilance and muscle tension |
| CBT-style reappraisal/exposure | Acceptance, patience, non-striving | Decreases catastrophising and fear-avoidance |
| Manual therapy anchoring and touch | Trust, beginner’s mind, embodied presence | Improves interoception and adherence to active care |
Integration of NET components with mindfulness attitudes and MSK clinical relevance.
NET incorporates elements from TCM, CBT, and manual therapy. Collectively these components embody all nine attitudes of mindfulness (non-judging, awareness, letting go, acceptance, patience, non-striving, trust, beginner’s mind, gratitude/generosity), each targeting mechanisms relevant to MSK pain and stress.
During the NET process some patients appear to experience what could be described as a brief sympathetic activation or “storm,” often characterised by heightened arousal responses such as sweating, increased heart rate, or a sudden sense of insight into the origin of their stress. We hypothesise that this state reflects a momentary convergence of multiple neural systems. Specifically, the procedure may engage the subconscious or autonomic components of the nervous system (through manual muscle testing), limbic circuits involved in emotional awareness and processing, and neocortical networks implicated in contextual appraisal and meaning-making. When these elements align, the patient may experience what we have termed the Somato-Limbic Integration Point (SLIP) - a transient integrative state where bodily sensation, affective awareness, and cognitive reframing co-occur.
Although the SLIP is currently a theoretical construct, it provides a framework for describing the rapid shifts in awareness sometimes observed in clinical practice. Preliminary neuroimaging research on NET supports the plausibility of such integrative mechanisms, with Monti et al. (2017, 2018) reporting changes in activation within limbic and cortical regions following treatment. Future studies will be needed to empirically test the SLIP hypothesis and clarify its neurobiological underpinnings.
Evidence and limitations of NET research
Research on NET has demonstrated positive outcomes across diverse conditions, including chronic low back pain (Bablis et al., 2022, 2023; Bablis and Pollard, 2016), pregnancy-related low back pain (Peterson et al., 2012), neck pain (Bablis et al., 2008), hypothyroidism (Bablis et al., 2024; Bablis and Pollard, 2004; Bablis and Pollard, 2009a), Polycystic Ovarian Syndrome (PCOS) (Bablis et al., 2006a), infertility (Bablis et al., 2006b), type 2 diabetes (Bablis et al., 2024), anxiety and depression (Jensen, 2010; Bablis and Pollard, 2009b), high cholesterol (Peterson, 1995), separation anxiety (Karpouzis et al., 2008), phobia resolution (Jensen and Ramasamy, 2009; Peterson, 1997) and ADHD (Karpouzis et al., 2009). Functional neuroimaging studies further suggest that NET influences brain physiology by reducing activation in regions associated with traumatic memories and distress (e.g., anterior cingulate gyrus, parahippocampus, insula, and brainstem) (Monti et al., 2017; Monti et al., 2018). In a randomized controlled trial of chronic low back pain, patients receiving NET in addition to standard care reported greater reductions in pain and disability (Oswestry Disability Index), lower pro-inflammatory cytokine levels (TNF-α, CRP, IL-1, IL-6), and improved quality of life (SF-36 domains) compared to standard care alone (Bablis et al., 2022).
To date, no published trials have reported unequivocally null or negative effects of NET on MSK outcomes. While the available evidence is encouraging, it remains preliminary, with modest sample sizes, study heterogeneity, and limited independent replication. These limitations highlight the importance of cautious interpretation and the need for further high-quality trials, including active-comparator and long-term follow-up studies, to establish NET’s role more definitively.
Clinical relevance of NET to MSK practice
Even so, NET is particularly relevant to MSK practitioners because it addresses the psychosocial stressors that can underlie or perpetuate pain. By offering a structured method for identifying and resolving emotional stress responses in the clinical setting, NET provides a practical way to support holistic care.
Addressing the mind–body interface may help clinicians avoid missing important contributors to persistent pain and dysfunction, while integrating interventions such as NET enables MSK practitioners to address both the physical manifestations and the stress-related mechanisms that sustain them. Taken together, these findings position NET as a practitioner-facilitated, hybrid-MBI that operationalises mindfulness principles and may be feasibly integrated into MSK care.
Conclusion
The profound interconnection between physical and mental health supports the need for a holistic approach in musculoskeletal (MSK) care. This review addressed three aims: (1) to show how chronic stress contributes to MSK conditions across biological, psychological, and social domains; (2) to synthesise evidence that mindfulness-based interventions (MBIs) can mitigate stress-related mechanisms and provide a scientific rationale for their use alongside MSK therapies; and (3) to present Neuro-Emotional Technique (NET) as an exemplar of a practitioner-facilitated hybrid-MBI, illustrating how such approaches may be applied in practice. Collectively, the evidence suggests that stress and unresolved emotional factors are not peripheral to MSK presentations but may substantially influence pain and dysfunction. Incorporating MBIs offers one pathway to address these influences, provided practitioners apply clinical judgement, implement red and yellow flag screening, and collaborate with mental health professionals where needed. While further high-quality research is required to strengthen the evidence base, integrating MBIs thoughtfully into MSK care has the potential to improve recovery, foster resilience, and support long-term health within a biopsychosocial model of care.
Statements
Author contributions
PB: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. RD: Conceptualization, Data curation, Project administration, Writing – original draft, Writing – review & editing. SB: Conceptualization, Writing – review & editing. HP: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- ACE
Adverse Childhood Experiences
- BPS
Biopsychosocial Model of Healthcare
- CBT
Cognitive Behavioural Therapy
- CRP
C-Reactive Protein
- DASS-21
Depression, Anxiety and Stress Scale
- DRAM
Distress and Risk Assessment Method
- ELS
Early Life Stress
- FABQ
Fear Avoidance Beliefs Questionnaire
- FFMQ
Five Facet Mindfulness Questionnaire
- IL-1
Interleukin-1
- IL-6
Interleukin-6
- HPA
Hypothalamic–Pituitary–Adrenal
- LBP
Low Back Pain
- MAPs
Mindful Awareness Programs
- MBI
Mindfulness-Based Intervention
- MBSR
Mindfulness-Based Stress Reduction
- MSK
Musculoskeletal
- NEC
Neuro-Emotional Complex
- NET
Neuro-Emotional Technique
- ODI
Oswestry Disability Index
- PBMI
Precision Body–Mind Intervention
- PHQ-9
Patient Health Questionnaire
- PINE network
Psycho-Immune-Neuroendocrine network
- PROMs
Patient Reported Outcome Measures
- PSS
Perceived Stress Scale
- PTSD
Post-Traumatic Stress Disorder
- RCT
Randomised Controlled Trial
- SF-36
Short Form Health Survey
- SLIP
Somato-Limbic Integration Point
- TCM
Traditional Chinese Medicine
- TNF-α
Tumour Necrosis Factor-α
Glossary
References
1
Abera M. Hanlon C. Daniel B. Tesfaye M. Workicho A. Girma T. et al . (2024). Effects of relaxation interventions during pregnancy on maternal mental health, and pregnancy and newborn outcomes: a systematic review and meta-analysis. PLoS One19:e0278432. doi: 10.1371/journal.pone.0278432
2
Aboushaar N. Serrano N. (2024). The mutually reinforcing dynamics between pain and stress: mechanisms, impacts and management strategies. Front. Pain Res.5:1445280. doi: 10.3389/fpain.2024.1445280
3
Agorastos A. Nicolaides N. Bozikas V. Chrousos G. Pervanidou P. (2020). Multilevel interactions of stress and circadian system: implications for traumatic stress. Front. Psych.10:1003. doi: 10.3389/fpsyt.2019.01003
4
Ahmed S. Mahmood Z. Zahid S. (2015). Linking insulin with Alzheimer's disease: emergence as type III diabetes. Neurol. Sci.36, 1763–1769. doi: 10.1007/s10072-015-2352-5
5
Ahrens C. Schiltenwolf M. Wang H. (2012). Zytokine im psychoneuroendokrin-immunologischen Kontext unspezifischer muskuloskeletaler Schmerzen [cytokines in psychoneuroendocrine immunological context of nonspecific musculoskeletal pain]. Schmerz26, 383–388. doi: 10.1007/s00482-012-1153-5
6
Alam F. Islam M. Sasongko T. Gan S. (2016). Type 2 diabetes mellitus and Alzheimer's disease: bridging the pathophysiology and management. Curr. Pharm. Des.22, 4430–4442. doi: 10.2174/1381612822666160527160236
7
American Psychological Association , “Stress in America2022,” (2022). Available online at: https://www.apa.org/news/press/releases/stress/2022/concerned-future-inflation (Accessed 16 May 2024).
8
American Psychological Association , “How stress affects your health,” (2022). Available online at: https://www.apa.org/topics/stress/health (Accessed 9 July 2024).
9
Antony M. Bieling P. Cox B. Enns M. Swinson R. (1998). Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol. Assess.10, 176–181. doi: 10.1037/1040-3590.10.2.176
10
Anxiety and Depression Association of America , “Chronic pain,” (2024). Available online at: https://adaa.org/understanding-anxiety/related-illnesses/other-related-conditions/chronic-pain (Accessed 11 September 2024).
11
Arzate-Mejia R. Carullo N. Mansuy I. (2024). The epigenome under pressure: on regulatory adaptation to chronic stress in the brain. Curr. Opin. Neurobiol.84:102832. doi: 10.1016/j.conb.2023.102832
12
Australian Institute of Health and Welfare , “Physical health of people with mental illness,” Australian government, (2024). Available online at: https://www.aihw.gov.au/reports/mental-health/physical-health-of-people-with-mental-illness (Accessed 9 July 2024].
13
Aviña-Zubieta J. Páez F. Galindo-Rodriguez G. (1997). Rheumatic manifestations of neurologic and psychiatric diseases. Curr. Opin. Rheumatol.9, 51–55. doi: 10.1097/00002281-199701000-00010
14
Awasthi B. (2013). Issues and perspectives in meditation research: in search for a definition. Front. Psychol.3:613. doi: 10.3389/fpsyg.2012.00613
15
Bablis P. Day R. Bablis S. Pollard H. (2024). Treatment of hypothyroidism and stress using neuro-emotional technique (NET): A case study. Cureus16:e58231. doi: 10.7759/cureus.58231
16
Bablis P. Day R. Pollard H. (2024). Treatment of type 2 diabetes and stress using neuro-emotional technique: case report. Front. Endocrinol.15:1382757. doi: 10.3389/fendo.2024.1382757
17
Bablis P. Pollard H. (2004). Hypothyroidism: a new model for conservative management in two cases. Chir J Aus34, 11–18.
18
Bablis P. Pollard H. (2009a). A mind–body treatment for hypothyroid dysfunction: A report of two cases. Complement. Ther. Clin. Pract.15, 67–71. doi: 10.1016/j.ctcp.2009.01.004
19
Bablis P. Pollard H. (2009b). Anxiety and depression profile of 188 consecutive new patients presenting to a neuro-emotional technique practitioner. J. Altern. Complement. Med.15, 121–127. doi: 10.1089/acm.2007.0805
20
Bablis P. Pollard H. (2016). Feasibility study of the short term effects of neuro emotional technique for chronic low back pain. Chir. J. Aus.44, 267–282.
21
Bablis P. Pollard H. Bonello R. (2008). Neuro emotional technique for the treatment of trigger point sensitivity in chronic neck pain sufferers: a controlled clinical trial. Chiropr. Osteopat.16:4. doi: 10.1186/1746-1340-16-4
22
Bablis P. Pollard H. McHardy A. (2006a). Two reports of resolution of polycystic ovary syndrome induced anovulation in females receiving neuro emotional technique. Chir J Aus36, 2–8.
23
Bablis P. Pollard H. Monti D. (2006b). Resolution of anovulation infertility using neuro emotional technique: a report of 3 cases. J. Chiropr. Med.5, 13–21. doi: 10.1016/S0899-3467(07)60128-1
24
Bablis P. Pollard H. Rosner A. (2022). Stress reduction via neuro-emotional technique to achieve the simultaneous resolution of chronic low back pain with multiple inflammatory and biobehavioural indicators: A randomized, double-blinded, placebo-controlled trial. J. Integr. Med.20, 135–144. doi: 10.1016/j.joim.2021.12.001
25
Bablis P. Pollard H. Rosner A. (2023). The endurance of neuro-emotional-technique effects on chronic low-Back pain - randomized, controlled trial with implications for cost savings. Nat Med J. Available at: https://www.researchgate.net/publication/375895335_The_Endurance_of_Neuro-Emotional-Technique_Effects_on_Chronic_Low-Back_Pain_Randomized_controlled_trial_with_implications_for_cost_savings
26
Baer R. (2019). 2019 assessment of mindfulness by self-report. Curr. Opin. Psychol.28, 42–48. doi: 10.1016/j.copsyc.2018.10.015
27
Baer R. Kuyken W. , “Is Mindfulness Safe?” Mindful.org - Healthy Mind, Healthy Life. (2016). Available online at: https://www.mindful.org/is-mindfulness-safe/ (Accessed 24 September 2025).
28
Baer R. Smith G. Hopkins J. Krietemeyer J. Toney L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment13, 27–45. doi: 10.1177/1073191105283504
29
Balban M. Neri E. Kogon M. Weed L. Nouriani B. Jo B. et al . (2023). Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Rep. Med.4:100895. doi: 10.1016/j.xcrm.2022.100895
30
Barbe M. Barr A. (2006). Inflammation and the pathophysiology of work-related musculoskeletal disorders. Brain Behav. Immun.20, 423–429. doi: 10.1016/j.bbi.2006.03.001
31
Barrett B. Hayney M. Muller D. Rakel D. Ward A. Obasi C. et al . (2012). Meditation or exercise for preventing acute respiratory infection: a randomized controlled trial. Ann. Fam. Med.10, 337–346. doi: 10.1370/afm.1376
32
Bartholomew E. Chung M. Yeroushalmi S. Hakimi M. Bhutani T. Liao W. (2022). Mindfulness and meditation for psoriasis: A systematic review. Dermatol Ther12, 2273–2283. doi: 10.1007/s13555-022-00802-1
33
Bendtsen L. Fernández-de-la-Peñas C. (2011). The role of muscles in tension-type headache. Curr. Pain Headache Rep.15, 451–458. doi: 10.1007/s11916-011-0216-0
34
Binda D. Greco C. Morone N. (2020). What are adverse events in mindfulness meditation?Glob. Adv. Health Med.11:6640. doi: 10.1177/2164957X221096640
35
Black P. (2002). Stress and the inflammatory response: a review of neurogenic inflammation. Brain Behav. Immun.16, 622–653. doi: 10.1016/s0889-1591(02)00021-1
36
Black D. Cole S. Irwin M. Breen E. St Cyr N. Nazarian N. et al . (2013). Yogic meditation reverses NF-κB and IRF-related transcriptome dynamics in leukocytes of family dementia caregivers in a randomized controlled trial. Psychoneuroendocrinology38, 348–355. doi: 10.1016/j.psyneuen.2012.06.011
37
Black D. O'Reilly G. Olmstead R. Breen E. Irwin M. (2015). Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA Intern. Med.175, 494–501. doi: 10.1001/jamainternmed.2014.8081
38
Black D. Slavich G. (2016). Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Ann. N. Y. Acad. Sci.1373, 13–24. doi: 10.1111/nyas.12998
39
Bongers P. Ijmker S. van den Heuvel S. Blatter B. (2006). Epidemiology of work related neck and upper limb problems: psychosocial and personal risk factors (part I) and effective interventions from a bio behavioural perspective (part II). J. Occup. Rehabil.16, 279–302. doi: 10.1007/s10926-006-9044-1
40
Borrell-Carrió F. Suchman A. Epstein R. (2004). The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann. Fam. Med.2, 576–582. doi: 10.1370/afm.245
41
Bosque M. Margalef R. Llaveria A. Santafe M. (2023). Stress increases the spontaneous release of ACh and may be involved in the generation and maintenance of myofascial trigger points in mouse. Behav. Brain Res.452:114572. doi: 10.1016/j.bbr.2023.114572
42
Britton W. (2019). Can mindfulness be too much of a good thing? The value of a middle way. Curr. Opin. Psychol.28, 159–165. doi: 10.1016/j.copsyc.2018.12.011
43
Britton W. Lindahl J. Cooper D. Canby N. Palitsky R. (2021). Defining and measuring meditation-related adverse effects in mindfulness-based programs. Clin. Psychol. Sci.9, 1185–1204. doi: 10.1177/2167702621996340
44
Brown C. Jones A. (2013). Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness-based pain management program. Clin. J. Pain29, 233–244. doi: 10.1097/AJP.0b013e31824c5d9f
45
Buscemi V. Chang W. Liston M. McAuley J. Schabrun S. (2019). The role of perceived stress and life stressors in the development of chronic musculoskeletal pain disorders: A systematic review. J. Pain20, 1127–1139. doi: 10.1016/j.jpain.2019.02.008
46
Cacioppo J. Berntson G. Malarkey W. Kiecolt-Glaser J. Sheridan J. Poehlmann K. et al . (1998). Autonomic, neuroendocrine, and immune responses to psychological stress: the reactivity hypothesis. Ann. N. Y. Acad. Sci.840, 664–673. doi: 10.1111/j.1749-6632.1998.tb09605.x
47
Cagnie B. Danneels L. Van Tiggelen D. De Loose V. Cambier D. (2007). Individual and work related risk factors for neck pain among office workers: a cross sectional study. Eur. Spine J.16, 679–686. doi: 10.1007/s00586-006-0269-7
48
Canadian Mental Health Association Ontario , “Connection between mental and physical health,” (2014). Available online at: https://ontario.cmha.ca/documents/connection-between-mental-and-physical-health/ (Accessed 9 July 2014).
49
Cardle P. Kumar S. Leach M. McEvoy M. Veziari Y. (2023). Mindfulness and chronic musculoskeletal pain: an umbrella review. J. Multidiscip. Healthc.16, 515–533. doi: 10.2147/JMDH.S392375
50
Carlson L. (2012). Mindfulness-based interventions for physical conditions: a narrative review evaluating levels of evidence. ISRN Psychiatry2012:651583. doi: 10.5402/2012/651583
51
Carson J. Carson K. Gil K. Baucom D. (2004). Mindfulness-based relationship enhancement. Behav. Ther.35, 471–494. doi: 10.1016/S0005-7894(04)80028-5
52
Cerniauskas I. Winterer J. de Jong J. Lukacsovich D. Yang H. Khan F. et al . (2019). Chronic stress induces activity, synaptic, and transcriptional remodeling of the lateral Habenula associated with deficits in motivated behaviors. Neuron104:e8, 899–915. doi: 10.1016/j.neuron.2019.09.005
53
Chaix R. Alvarez-López M. Fagny M. Lemee L. Regnault B. Davidson R. et al . (2017). Epigenetic clock analysis in long-term meditators. Psychoneuroendocrinology85, 210–214. doi: 10.1016/j.psyneuen.2017.08.016
54
Chaix R. Fagny M. Cosin-Tomás M. Alvarez-López M. Lemee L. Regnault B. et al . (2020). Differential DNA methylation in experienced meditators after an intensive day of mindfulness-based practice: implications for immune-related pathways. Brain Behav. Immun.84, 36–44. doi: 10.1016/j.bbi.2019.11.003
55
Chang H. Perkins M. Novaes L. Qian F. Zhang T. Neckel P. et al . (2024). Stress-sensitive neural circuits change the gut microbiome via duodenal glands. Cell187, 1–20. doi: 10.1016/j.cell.2024.07.019
56
Chapman C. Tuckett R. Song C. (2008). Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. J. Pain9, 122–145. doi: 10.1016/j.jpain.2007.09.006
57
Charmandari E. Tsigos C. Chrousos G. (2005). Endocrinology of the stress response. Annu. Rev. Physiol.67, 259–284. doi: 10.1146/annurev.physiol.67.040403.120816
58
Chen Y. Lyga J. (2014). Brain-skin connection: stress, inflammation and skin aging. Inflamm. Allergy Drug Targets13, 177–190. doi: 10.2174/1871528113666140522104422
59
Chiesa A. (2013). The difficulty of defining mindfulness: current thought and critical issues. Mindfulness4, 255–268. doi: 10.1007/s12671-012-0123-4
60
Chrousos G. (2000). The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: neuro-endocrine and target tissue-related causes. Int. J. Obes. Relat. Metab. Disord.24, S50–S55. doi: 10.1038/sj.ijo.0801278
61
Chrousos G. (2009). Stress and disorders of the stress system. Nat. Rev. Endocrinol.5, 374–381. doi: 10.1038/nrendo.2009.106
62
Chrousos G. Gold P. (1992). The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA267, 1244–1252.
63
Chrousos G. Kino T. (2007). Glucocorticoid action networks and complex psychiatric and/or somatic disorders. Stress10, 213–219. doi: 10.1080/10253890701292119
64
Cohen S. Kamarck T. Mermelstein R. (1983). A global measure of perceived stress. J. Health Soc. Behav.24, 385–396. doi: 10.2307/2136404
65
Collins S. (2001). Stress and the gastrointestinal tract IV. Modulation of intestinal inflammation by stress: basic mechanisms and clinical relevance. Am. J. Physiol. Gastrointest. Liver Physiol.280, G315–G318. doi: 10.1152/ajpgi.2001.280.3.G315
66
Cottrell E. Seckl J. (2009). Prenatal stress, glucocorticoids and the programming of adult disease. Front. Behav. Neurosci.3:19. doi: 10.3389/neuro.08.019.2009
67
Creswell J. (2017). Mindfulness interventions. Annu. Rev. Psychol.68, 491–516. doi: 10.1146/annurev-psych-042716-051139
68
Creswell J. Irwin M. Burklund L. Lieberman M. Arevalo J. Ma J. et al . (2012). Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav. Immun.26, 1095–1101. doi: 10.1016/j.bbi.2012.07.006
69
Cuthbert S. Goodheart G. J. (2007). On the reliability and validity of manual muscle testing: a literature review. Chiropr. Osteopat.15:4. doi: 10.1186/1746-1340-15-4
70
Dallman M. Strack A. Akana S. Bradbury M. Hanson E. Scribner K. et al . (1993). Feast and famine: critical role of glucocorticoids with insulin in daily energy flow. Front. Neuroendocrinol.14, 303–347. doi: 10.1006/frne.1993.1010
71
Davidson R. Kaszniak A. (2015). Conceptual and methodological issues in research on mindfulness and meditation. Am. Psychol.70, 581–592. doi: 10.1037/a0039512
72
Davis M. Zautra A. Wolf L. Tennen H. Yeung E. (2015). Mindfulness and cognitive-behavioral interventions for chronic pain: differential effects on daily pain reactivity and stress reactivity. J. Consult. Clin. Psychol.83, 24–35. doi: 10.1037/a0038200
73
Dhillon A. Sparkes E. Duarte R. (2017). Mindfulness-based interventions during pregnancy: a systematic review and meta-analysis. Mindfulness8, 1421–1437. doi: 10.1007/s12671-017-0726-x
74
Doan T. Ha V. Strazdins L. Chateau D. (2023). Healthy minds live in healthy bodies – effect of physical health on mental health: evidence from Australian longitudinal data. Curr. Psychol.42, 18702–18713. doi: 10.1007/s12144-022-03053-7
75
Dobkin P. Irving J. Amar S. (2012). For whom may participation in a mindfulness-based stress reduction program be contraindicated?Mindfulness3, 44–50. doi: 10.1007/s12671-011-0079-9
76
Dorn L. Chrousos G. (1993). The endocrinology of stress and stress system disorders in adolescence. Endocrinol. Metab. Clin. N. Am.22, 685–700. doi: 10.1016/S0889-8529(18)30158-0
77
Drummond P. Hewson-Bower B. (1997). Increased psychosocial stress and decreased mucosal immunity in children with recurrent upper respiratory tract infections. J. Psychosom. Res.43, 271–278. doi: 10.1016/s0022-3999(97)00002-0
78
Dunn B. Hartigan J. Mikulas W. (1999). Concentration and mindfulness meditations: unique forms of consciousness?Appl. Psychophysiol. Biofeedback24, 147–165. doi: 10.1023/a:1023498629385
79
Dunn M. Rushton A. Mistry J. Soundy A. Heneghan N. (2024). The biopsychosocial factors associated with development of chronic musculoskeletal pain. An umbrella review and meta-analysis of observational systematic reviews. PLoS One19:e0294830. doi: 10.1371/journal.pone.0294830
80
Edwards K. Edes A. Brown J. (2019). Stress, well-being and reproductive success. Adv. Exp. Med. Biol.1200, 91–162. doi: 10.1007/978-3-030-23633-5_5
81
Ellett L. (2024). Mindfulness for psychosis: current evidence, unanswered questions and future directions. Psychol. Psychother.97, 34–40. doi: 10.1111/papt.12480
82
Engel G. (1977). The need for a new medical model: a challenge for biomedicine. Science196, 129–136.
83
Fan D. (2017). Holistic integrative medicine: toward a new era of medical advancement. Front. Med.11, 152–159. doi: 10.1007/s11684-017-0499-6
84
Farias M. Wikholm C. (2016). Has the science of mindfulness lost its mind?BJPsych Bull40, 329–332. doi: 10.1192/pb.bp.116.053686
85
Fillingim R. Ohrbach R. Greenspan J. Knott C. Diatchenko L. Dubner R. et al . (2013). Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J. Pain14, T75–T90. doi: 10.1016/j.jpain.2013.06.009
86
Finestone H. Alfeeli A. Fisher W. (2008). Stress-induced physiologic changes as a basis for the biopsychosocial model of chronic musculoskeletal pain: a new theory?Clin. J. Pain24, 767–775. doi: 10.1097/AJP.0b013e3181790342
87
Foa E. Jaycox L. (1999). “Cognitive-behavioral theory and treatment of posttraumatic stress disorder” in Efficacy and cost-effectiveness of psychotherapy. ed. SpiegelD. (Arlington, VA, United States: American Psychiatric Publishing, Inc.).
88
Fox K. Nijeboer S. Dixon M. Floman J. Ellamil M. Rumak S. et al . (2014). Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci. Biobehav. Rev.43, 48–73. doi: 10.1016/j.neubiorev.2014.03.016
89
Franklin T. Saab B. Mansuy I. (2012). Neural mechanisms of stress resilience and vulnerability. Neuron75, 747–761. doi: 10.1016/j.neuron.2012.08.016
90
Gapp K. Bohacek J. Grossmann J. Brunner A. Manuella F. Nanni P. et al . (2016). Potential of environmental enrichment to prevent transgenerational effects of paternal trauma. Neuropsychopharmacology41, 2749–2758. doi: 10.1038/npp.2016.87
91
García-Campayo J. Puebla-Guedea M. Labarga A. et al . (2018). Epigenetic response to mindfulness in peripheral blood leukocytes involves genes linked to common human diseases. Mindfulness9, 1146–1159. doi: 10.1007/s12671-017-0851-6
92
Garland E. Hanley A. Baker A. Howard M. (2017). Biobehavioral mechanisms of mindfulness as a treatment for chronic stress: an RDoC perspective. Chronic Stress1, 1–14. doi: 10.1177/2470547017711912
93
Gathright E. Salmoirago-Blotcher E. DeCosta J. Balletto B. Donahue M. Feulner M. et al . (2019). The impact of transcendental meditation on depressive symptoms and blood pressure in adults with cardiovascular disease: a systematic review and meta-analysis. Complement. Ther. Med.46, 172–179. doi: 10.1016/j.ctim.2019.08.009
94
Gee D. Gabard-Durnam L. Flannery J. Goff B. Humphreys K. Telzer E. et al . (2013). Early developmental emergence of human amygdala-prefrontal connectivity after maternal deprivation. Proc. Natl. Acad. Sci. USA110, 15638–15643. doi: 10.1073/pnas.1307893110
95
Goldberg S. Riordan K. Sun S. Davidson R. (2022). The empirical status of mindfulness-based interventions: a systematic review of 44 meta-analyses of randomized controlled trials. Perspect. Psychol. Sci.17, 108–130. doi: 10.1177/1745691620968771
96
González-Díaz S. Arias-Cruz A. Elizondo-Villarreal B. (2017). Psychoneuroimmunoendocrinology: clinical implications. World Allergy Organ. J.10:19. doi: 10.1186/s40413-017-0151-6
97
González-Moret R. Cebolla A. Cortés X. Baños R. Navarrete J. de la Rubia J. et al . (2020). The effect of a mindfulness-based therapy on different biomarkers among patients with inflammatory bowel disease: a randomised controlled trial. Sci. Rep.10:6071. doi: 10.1038/s41598-020-63168-4
98
Gouin J. Kiecolt-Glaser J. (2012). The impact of psychological stress on wound healing: methods and mechanisms. Crit. Care Nurs. Clin. North Am.24, 201–213. doi: 10.1016/j.ccell.2012.03.006
99
Graham N. Douglas R. Ryan P. (1986). Stress and acute respiratory infection. Am. J. Epidemiol.124, 389–401. doi: 10.1093/oxfordjournals.aje.a114409
100
Graubard R. Perez-Sanchez A. Katta R. (2021). Stress and skin: an overview of mind body therapies as a treatment strategy in dermatology. Dermatol. Pract. Concept.11:e2021091. doi: 10.5826/dpc.1104a91
101
Gray T. Carney M. Magnuson D. (1989). Direct projections from the central amygdaloid nucleus to the hypothalamic paraventricular nucleus: possible role in stress-induced adrenocorticotropin release. Neuroendocrinology50, 433–446. doi: 10.1159/000125260
102
Grossman P. (2011). Defining mindfulness by how poorly i think i pay attention during everyday awareness and other intractable problems for psychology's (re)invention of mindfulness: comment on Brown et al. (2011). Psychol. Assess.23, 1034–1040. doi: 10.1037/a0022713
103
Gu J. Strauss C. Bond R. Cavanagh K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of meditation studies. Clin. Psychol. Rev.37, 1–12. doi: 10.1016/j.cpr.2015.01.006
104
Gu H. Tang C. Yang Y. (2012). Psychological stress, immune response, and atherosclerosis. Atherosclerosis223, 69–77. doi: 10.1016/j.atherosclerosis.2012.01.021
105
Guidi J. Lucente M. Sonino N. Fava G. (2021). Allostatic load and its impact on health: a systematic review. Psychother. Psychosom.90, 11–27. doi: 10.1159/000510696
106
Hanley A. Warner A. Dehili V. Canto A. Garland E. (2015). Washing dishes to wash the dishes: brief instruction in an informal mindfulness practice. Mindfulness6, 1095–1103. doi: 10.1007/s12671-014-0360-9
107
Hannum G. Fan J.-B. Guinney J. Zhao L. Zhang L. Hughes G. et al . (2013). Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol. Cell49, 359–367. doi: 10.1016/j.molcel.2012.10.016
108
Hardy K. Pollard H. (2006). The organisation of the stress response, and its relevance to chiropractors: a commentary. Chiropr. Osteopat.14:25. doi: 10.1186/1746-1340-14-25
109
Harfenstellar J. (2022). An open trial on the feasibility and efficacy of a mindfulness-based intervention with psychoeducational elements on atopic eczema and chronic itch. Psych4, 160–172. doi: 10.3390/psych4020014
110
Hemingway H. Marmot M. (1999). Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ318, 1460–1467. doi: 10.1136/bmj.318.7196.1460
111
Herman J. McKlveen J. Ghosal S. Kopp B. Wulsin A. Makinson R. et al . (2016). Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr Physiol6, 603–621. doi: 10.1002/cphy.c150015
112
Higgins E. Davidson R. Busse W. Klaus D. Bednarek G. Goldman R. et al . (2022). Clinically relevant effects of mindfulness-based stress reduction in individuals with asthma. Brain Behav. Immun. Health25:100509. doi: 10.1016/j.bbih.2022.100509
113
Hofmann S. Sawyer A. Witt A. Oh D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J. Consult. Clin. Psychol.78, 169–183. doi: 10.1037/a0018555
114
Hölzel B. Lazar S. Gard T. Schuman-Olivier Z. Vago D. Ott U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect. Psychol. Sci.6, 537–559. doi: 10.1177/1745691611419671
115
Horvath S. (2013). DNA methylation age of human tissues and cell types. Genome Biol.14:R115. doi: 10.1186/gb-2013-14-10-r115
116
Jensen A. (2010). A mind-body approach for precompetitive anxiety in power-lifters: 2 case studies. J. Chiropr. Med.9, 184–192. doi: 10.1016/j.jcm.2010.08.003
117
Jensen A. Ramasamy A. (2009). Treating spider phobia using neuro emotional technique: findings from a pilot study. J. Altern. Complement. Med.15, 1363–1374. doi: 10.1089/acm.2008.0595
118
Juster R. McEwen B. Lupien S. (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev.35, 2–16. doi: 10.1016/j.neubiorev.2009.10.002
119
Kabat-Zinn J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delacorte Press.
120
Kabat-Zinn J. (2003). Mindfulness-based stress reduction (MBSR). Constr. Hum. Sci.8, 73–107.
121
Kabat-Zinn J. (2024). “9 attitudes of mindfulness by Jon Kabat-Zinn,” MBSR training, Available online at: https://mbsrtraining.com/attitudes-of-mindfulness-by-jon-kabat-zinn/ (Accessed 13 September 2024).
122
Kabat-Zinn J. Massion A. Kristeller J. Peterson L. Fletcher K. Pbert L. et al . (1992). Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am. J. Psychiatry149, 936–943. doi: 10.1176/ajp.149.7.936
123
Kakoschke N. Hassed C. Chambers R. Lee K. (2021). The importance of formal versus informal mindfulness practice for enhancing psychological wellbeing and study engagement in a medical student cohort with a 5-week mindfulness-based lifestyle program. PLoS One16:e0258999. doi: 10.1371/journal.pone.0258999
124
Kaliman P. Alvarez-López M. Cosín-Tomás M. Rosenkranz M. Lutz A. Davidson R. (2014). Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators. Psychoneuroendocrinology40, 96–107. doi: 10.1016/j.psyneuen.2013.11.004
125
Karpouzis F. Pollard H. Bonello R. (2008). Separation anxiety disorder in a 13-year-old boy managed by the neuro emotional technique as a biopsychosocial intervention. J. Chiropr. Med.7, 101–106. doi: 10.1016/j.jcm.2008.05.003
126
Karpouzis F. Pollard H. Bonello R. (2009). A randomised controlled trial of the neuro emotional technique (NET) for childhood attention deficit hyperactivity disorder (ADHD): a protocol. Trials10:6. doi: 10.1186/1745-6215-10-6
127
Kazakou P. Nicolaides N. Chrousos G. (2023). Basic concepts and hormonal regulators of the stress system. Horm. Res. Paediatr.96, 8–16. doi: 10.1159/000523975
128
Kiecolt-Glaser J. Marucha P. Malarkey W. Mercado A. Glaser R. (1995). Slowing of wound healing by psychological stress. Lancet346, 1194–1196. doi: 10.1016/s0140-6736(95)92899-5
129
Kiecolt-Glaser J. Robles T. Heffner K. Loving T. Glaser R. (2002). Psycho-oncology and cancer: psychoneuroimmunology and cancer. Ann. Oncol.13, 165–169. doi: 10.1093/annonc/mdf655
130
Kim I. Lee J. Park S. (2022). The relationship between stress, inflammation, and depression. Biomedicine10:1929. doi: 10.3390/biomedicines10081929
131
Koolhaas J. Bartolomucci A. Buwalda B. de Boer S. Flügge G. Korte S. et al . (2011). Stress revisited: a critical evaluation of the stress concept. Neurosci. Biobehav. Rev.35, 1291–1301. doi: 10.1016/j.neubiorev.2011.02.003
132
Kroenke K. Spitzer R. Williams J. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med.16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
133
Kuyken W. Ball S. Crane C. Ganguli P. Jones B. Montero-Marin J. et al . (2022). Effectiveness and cost-effectiveness of universal school-based mindfulness training compared with normal school provision in reducing risk of mental health problems and promoting well-being in adolescence: the MYRIAD cluster randomised controlled trial. Evid. Based Ment. Health25, 99–109. doi: 10.1136/ebmental-2021-300396
134
Kuyken W. Byford S. Taylor R. Watkins E. Holden E. White K. et al . (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J. Consult. Clin. Psychol.76, 966–978. doi: 10.1037/a0013786
135
Kyrou I. Tsigos C. (2008). Chronic stress, visceral obesity and gonadal dysfunction. Hormones (Athens)7, 287–293. doi: 10.14310/horm.2002.1209
136
Labanski A. Langhorst J. Engler H. Elsenbruch S. (2020). Stress and the brain-gut axis in functional and chronic-inflammatory gastrointestinal diseases: A transdisciplinary challenge. Psychoneuroendocrinology111:104501. doi: 10.1016/j.psyneuen.2019.104501
137
Landeo-Gutierrez J. Celedón J. (2020). Chronic stress and asthma in adolescents. Ann. Allergy Asthma Immunol.125, 393–398. doi: 10.1016/j.anai.2020.07.001
138
Leonard B. (2010). The concept of depression as a dysfunction of the immune system. Curr. Immunol. Rev.6, 205–212. doi: 10.2174/157339510791823835
139
Li J. Long L. Liu Y. He W. Li M. (2016). Effects of a mindfulness-based intervention on fertility quality of life and pregnancy rates among women subjected to first in vitro fertilization treatment. Behav. Res. Ther.77, 96–104. doi: 10.1016/j.brat.2015.12.010
140
Lindahl J. Cooper D. Fisher N. Kirmayer L. Britton W. (2020). Progress or pathology? Differential diagnosis and intervention criteria for meditation-related challenges: perspectives from Buddhist meditation teachers and practitioners. Front. Psychol.11:1905. doi: 10.3389/fpsyg.2020.01905
141
Lindahl J. Fisher N. Cooper D. Rosen R. Britton W. (2017). The varieties of contemplative experience: a mixed-methods study of meditation-related challenges in Western Buddhists. PLoS One12:e0176239. doi: 10.1371/journal.pone.0176239
142
Linton S. (2000). A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976)25, 1148–1156. doi: 10.1097/00007632-200005010-00017
143
Liu H. Cai K. Wang J. Zhang H. (2023). The effects of mindfulness-based interventions on anxiety, depression, stress, and mindfulness in menopausal women: A systematic review and meta-analysis. Front. Public Health10:1045642. doi: 10.3389/fpubh.2022.1045642
144
Lovibond S. Lovibond P. (1995). Manual for the depression anxiety and stress scales (DASS21) second edition. Sydney, NSW: Psychology Foundation of Australia, 1–3.
145
Lucassen P. Pruessner J. Sousa N. Almeida O. Van Dam A. Rajkowska G. et al . (2014). Neuropathology of stress. Acta Neuropathol.127, 109–135. doi: 10.1007/s00401-013-1223-5
146
Lucini D. Di Fede G. Parati G. Pagani M. (2005). Impact of chronic psychosocial stress on autonomic cardiovascular regulation in otherwise healthy subjects. Hypertension46, 1201–1206. doi: 10.1161/01.HYP.0000185147.32385.4b
147
Lustyk M. Chawla N. Nolan R. Marlatt G. (2009). Mindfulness meditation research: issues of participant screening, safety procedures, and researcher training. Adv. Mind Body Med.24, 20–30.
148
Lutz P. Chay M. Pacis A. Chen G. Aouabed Z. Maffioletti E. et al . (2021). Non-CG methylation and multiple histone profiles associate child abuse with immune and small GTPase dysregulation. Nat. Commun.12:1132. doi: 10.1038/s41467-021-21365-3
149
Lutz A. Slagter H. Dunne J. Davidson R. (2008). Attention regulation and monitoring in meditation. Trends Cogn. Sci.12, 163–169. doi: 10.1016/j.tics.2008.01.005
150
Main C. Waddell G. (1991). A comparison of cognitive measures in low back pain: statistical structure and clinical validity at initial assessment. Pain46, 287–298. doi: 10.1016/0304-3959(91)90112-B
151
Main C. Wood P. Hollis S. Spanswick C. Waddell G. (1992). The distress and risk assessment method. A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine (Phila Pa 1976)17, 42–52. doi: 10.1097/00007632-199201000-00007
152
Maloney S. Kock M. Slaghekke Y. Radley L. Lopez-Montoyo A. Montero-Marin J. et al . (2024). Target mechanisms of mindfulness-based programmes and practices: a scoping review. BMJ Ment Health27:e300955. doi: 10.1136/bmjment-2023-300955
153
Malterud K. (2010). Kroniske muskelsmerter kan forklares på mange måter [Chronic muscular pain is not unexplainable]. Tidsskr. Nor. Laegeforen.130, 2356–2359. doi: 10.4045/tidsskr.09.0828
154
Manfredini D. Bandettini di Poggio A. Cantini E. Dell'Osso L. Bosco M. (2004). Mood and anxiety psychopathology and temporomandibular disorder: a spectrum approach. J. Oral Rehabil.31, 933–940. doi: 10.1111/j.1365-2842.2004.01335.x
155
Manfredini D. Landi N. Bandettini Di Poggio A. Dell'Osso L. Bosco M. (2003). A critical review on the importance of psychological factors in temporomandibular disorders. Minerva Stomatol.52, 321–326.
156
Manigault A. Slutsky J. Raye J. Creswell J. D. (2021). Examining practice effects in a randomized controlled trial: daily life mindfulness practice predicts stress buffering effects of mindfulness meditation training. Mindfulness12, 2487–2497. doi: 10.1007/s12671-021-01718-1
157
Mantri S. (2008). Holistic medicine and the Western medical tradition. Virtual Mentor10, 177–180. doi: 10.1001/virtualmentor.2008.10.3.mhst1-0803
158
Mariotti A. (2015). The effects of chronic stress on health: new insights into the molecular mechanisms of brain-body communication. Future Sci. OA1:FSO23. doi: 10.4155/fso.15.21
159
Masere C. Nakade Y. Zheng J. Babygirija R. Ludwig K. Takahashi T. (2009). Chronic restraint stress has no more stimulatory effects on colonic motility in rats. Neurosci. Lett.453, 147–150. doi: 10.1016/j.neulet.2009.02.042
160
Maté G. , “Goodreads Gabor Maté quotes,” Goodreads, (2024). Available online at: https://www.goodreads.com/quotes/8699371-while-all-of-us-dread-being-blamed-we-all-would (Accessed 16 May 2024).
161
McBeth J. Silman A. (2001). The role of psychiatric disorders in fibromyalgia. Curr. Rheumatol. Rep.3, 157–164. doi: 10.1007/s11926-001-0011-8
162
McCreary J. Erickson Z. Hao Y. Ilnytskyy Y. Kovalchuk I. Metz G. (2016). Environmental intervention as a therapy for adverse programming by ancestral stress. Sci. Rep.6:37814. doi: 10.1038/srep37814
163
McEwen B. (1998). Protective and damaging effects of stress mediators. N. Engl. J. Med.338, 171–179. doi: 10.1056/NEJM199801153380307
164
McEwen B. (2007). Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol. Rev.87, 873–904. doi: 10.1152/physrev.00041.2006
165
McEwen B. Gianaros P. (2011). Stress- and allostasis-induced brain plasticity. Annu. Rev. Med.62, 431–445. doi: 10.1146/annurev-med-052209-100430
166
McEwen B. Stellar E. (1993). Stress and the individual. mechanisms leading to disease. Arch. Intern. Med.153, 2093–2101.
167
McFarlane A. (2007). Stress-related musculoskeletal pain. Best Pract. Res. Clin. Rheumatol.21, 549–565. doi: 10.1016/j.berh.2007.03.008
168
McGreevey S. “Eight weeks to a better brain,” MGH communications, the Harvard gazette, (2011). Available online at: https://news.harvard.edu/gazette/story/2011/01/eight-weeks-to-a-better-brain/ (Accessed 23 May 2024).
169
Mental Health Foundation UK , “Stress: Statistics - results of our 2018 study.” (2024a). Available online at: https://www.mentalhealth.org.uk/explore-mental-health/statistics/stress-statistics (Accessed 9 July 2024).
170
Mental Health Foundation UK , “Physical health and mental health.” (2024b). Available online at: https://www.mentalhealth.org.uk/explore-mental-health/a-z-topics/physical-health-and-mental-health (Accessed 9 July 2024).
171
Mills S. Nicolson K. Smith B. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth.123, e273–e283. doi: 10.1016/j.bja.2019.03.023
172
Mindful Staff , “Jon Kabat-Zinn: Defining Mindfulness,” Mindful.org, (2017). Available online at: https://www.mindful.org/jon-kabat-zinn-defining-mindfulness/ (Accessed 22 May 2024].
173
Monti D. Sinnott J. Marchese M. Kunkel E. Greeson J. (1999). Muscle test comparisons of congruent and incongruent self-referential statements. Percept. Mot. Skills88, 1019–1028. doi: 10.2466/pms.1999.88.3.1019
174
Monti D. Tobia A. Stoner M. Wintering N. Matthews M. Conklin C. J. et al . (2018). Changes in cerebellar functional connectivity and autonomic regulation in cancer patients treated with the neuro emotional technique for traumatic stress symptoms. J. Cancer Surviv.12, 145–153. doi: 10.1007/s11764-017-0653-9
175
Monti D. Tobia A. Stoner M. Wintering N. Matthews M. He X. et al . (2017). Neuro emotional technique effects on brain physiology in cancer patients with traumatic stress symptoms: preliminary findings. J. Cancer Surviv.11, 438–446. doi: 10.1007/s11764-017-0601-8
176
Morey J. Boggero I. Scott A. Segerstrom S. (2015). Current directions in stress and human immune function. Curr. Opin. Psychol.5, 13–17. doi: 10.1016/j.copsyc.2015.03.007
177
Muka T. Koromani F. Portilla E. O'Connor A. Bramer W. Troup J. et al . (2016). The role of epigenetic modifications in cardiovascular disease: A systematic review. Int. J. Cardiol.212, 174–183. doi: 10.1016/j.ijcard.2016.03.062
178
Musaelyan K. Yildizoglu S. Bozeman J. Du Preez A. Egeland M. Zunszain P. et al . (2020). Chronic stress induces significant gene expression changes in the prefrontal cortex alongside alterations in adult hippocampal neurogenesis. Brain Commun.2:fcaa153. doi: 10.1093/braincomms/fcaa153
179
Navarro-Ledesma S. Hamed-Hamed D. Gonzalez-Muñoz A. Pruimboom L. (2024). Impact of physical therapy techniques and common interventions on sleep quality in patients with chronic pain: A systematic review. Sleep Med. Rev.76:101937. doi: 10.1016/j.smrv.2024.101937
180
Ng Q. Venkatanarayanan N. Loke W. Yeo W. Lim D. Chan H. et al . (2019). A meta-analysis of the effectiveness of yoga-based interventions for maternal depression during pregnancy. Complement. Ther. Clin. Pract.34, 8–12. doi: 10.1016/j.ctcp.2018.10.016
181
NIB , “The impact of stress in Australia,” (2021). Available online at: https://www.nib.com.au/the-checkup/impact-of-stress-in-australia (Accessed 16 May 2024].
182
Nold V. Allers K. , “Consequences of chronic stress on the PINE network,” (2020). Available online at: https://www.intechopen.com/chapters/76550 (Accessed 11 October 2023).
183
O'Donovan A. Tomiyama A. Lin J. Puterman E. Adler N. Kemeny M. et al . (2012). Stress appraisals and cellular aging: a key role for anticipatory threat in the relationship between psychological stress and telomere length. Brain Behav. Immun.26, 573–579. doi: 10.1016/j.bbi.2012.01.007
184
Olff M. (1999). Stress, depression and immunity: the role of defense and coping styles. Psychiatry Res.85, 7–15. doi: 10.1016/s0165-1781(98)00139-5
185
Ong N. Teo F. Ee J. Yau C. Thumboo J. Tan H. et al . (2024). Effectiveness of mindfulness-based interventions on the well-being of healthcare workers: a systematic review and meta-analysis. Gen. Psychiatr.37:e101115. doi: 10.1136/gpsych-2023-101115
186
Palmer R. Roos C. Vafaie N. Kober H. (2023). The effect of ten versus twenty minutes of mindfulness meditation on state mindfulness and affect. Sci. Rep.13:20646. doi: 10.1038/s41598-023-46578-y
187
Parker H. Abreu A. Sullivan M. Vadiveloo M. (2022). Allostatic load and mortality: a systematic review and meta-analysis. Am. J. Prev. Med.63, 131–140. doi: 10.1016/j.amepre.2022.02.003
188
Paschali M. Lazaridou A. Paschalis T. Napadow V. Edwards R. (2021). Modifiable psychological factors affecting functioning in fibromyalgia. J. Clin. Med.10:803. doi: 10.3390/jcm10040803
189
Pascoe M. Thompson D. Ski C. (2017). Yoga, mindfulness-based stress reduction and stress-related physiological measures: a meta-analysis. Psychoneuroendocrinology86, 152–168. doi: 10.1016/j.psyneuen.2017.08.008
190
Pérez Fernández J. Salaberria K. de Ocenda Á. R. (2022). Mindfulness-based pain management (MBPM) for chronic pain: a randomized clinical trial. Mindfulness13, 3153–3165. doi: 10.1007/s12671-022-02023-1
191
Peterson K. (1995). Two cases of spinal manipulation performed while the patient contemplated an associated stress event: the effect of the manipulation/contemplation on serum cholesterol levels in hypercholesterolemic subjects. Chir Technique7, 55–59.
192
Peterson K. (1997). The effects of spinal manipulation on the intensity of emotional arousal in phobic subjects exposed to a threat stimulus: a randomized, controlled, double-blind clinical trial. J. Manip. Physiol. Ther.20, 602–606.
193
Peterson C. Haas M. Gregory W. (2012). A pilot randomized controlled trial comparing the efficacy of exercise, spinal manipulation, and neuro emotional technique for the treatment of pregnancy-related low back pain. Chiropr. Man. Therap.20:18. doi: 10.1186/2045-709X-20-18
194
Pollard H. Lakay B. Tucker F. Watson B. Bablis P. (2005). Interexaminer reliability of the deltoid and psoas muscle test. J. Manip. Physiol. Ther.28, 52–56. doi: 10.1016/j.jmpt.2004.12.008
195
Prakhinkit S. Suppapitiporn S. Tanaka H. Suksom D. (2014). Effects of Buddhism walking meditation on depression, functional fitness, and endothelium-dependent vasodilation in depressed elderly. J. Altern. Complement. Med.20, 411–416. doi: 10.1089/acm.2013.0205
196
Pratt M. , “5 minutes of mindfulness brings real benefits, according to science,” (2024). Available online at: https://www.mindful.org/5-minutes-of-mindfulness-brings-real-benefits-according-to-science/ (Accessed 16 September 2024).
197
Preissner C. Vilier L. Bertelsmann N. Beckers K. de Ruijter D. de Vries H. et al . (2025). A systematic review on the effectiveness of unstandardized mindfulness interventions in improving dietary and physical activity outcomes in healthy adults. BMC Public Health25:1705. doi: 10.1186/s12889-025-22850-w
198
Rao K. (2011). Applied yoga psychology: studies of neurophysiology of meditation. J. Conscious. Stud.18, 161–198.
199
Ren H. Collins V. Clarke S. Han J. Lam P. Clay F. et al . (2012). Epigenetic changes in response to tai chi practice: a pilot investigation of DNA methylation marks. Evid. Based Complement. Alternat. Med.2012:841810. doi: 10.1155/2012/841810
200
Riegner G. Dean J. Wager T. Zeidan F. (2024). Mindfulness meditation and placebo modulate distinct multivariate neural signatures to reduce pain. Biol. Psychiatry, 97, 81–88. doi: 10.1016/j.biopsych.2024.08.023
201
Robinson J. , “How does mental health affect physical health?”. New York, NY, USA. (2023). Available online at: https://www.webmd.com/mental-health/how-does-mental-health-affect-physical-health (Accessed 9 July 2024).
202
Rod N. Grønbaek M. Schnohr P. Prescott E. Kristensen T. (2009). Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J. Intern. Med.266, 467–475. doi: 10.1111/j.1365-2796.2009.02124.x
203
Roth R. Tam S. Ida Y. Yang J. Deutch A. (1988). Stress and the mesocorticolimbic dopamine systems. Ann. N. Y. Acad. Sci.537, 138–147. doi: 10.1111/j.1749-6632.1988.tb42102.x
204
Rudland J. Golding C. Wilkinson T. (2020). The stress paradox: how stress can be good for learning. Med. Educ.54, 40–45. doi: 10.1111/medu.13830
205
Salleh M. (2008). Life event, stress and illness. Malays. J. Med. Sci.15, 9–18.
206
Salvagioni D. Melanda F. Mesas A. González A. Gabani F. Andrade S. (2017). Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One12:e0185781. doi: 10.1371/journal.pone.0185781
207
Sandberg S. Paton J. Ahola S. McCann D. McGuinness D. Hillary C. et al . (2000). The role of acute and chronic stress in asthma attacks in children. Lancet356, 982–987. doi: 10.1016/S0140-6736(00)02715-X
208
Sandman C. Davis E. Buss C. Glynn L. (2011). Prenatal programming of human neurological function. Int. J. Pept.2011:837596. doi: 10.1155/2011/837596
209
Santorelli S. (2014). Mindfulness-based stress reduction (MBSR): Standards of practice,” University of Massachusetts Medical School Center for mindfulness in medicine, health care, and society” Worcester, MA, USA
210
Schneiderman N. Ironson G. Siegel S. (2005). Stress and health: psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol.1, 607–628. doi: 10.1146/annurev.clinpsy.1.102803.144141
211
Sharif K. Watad A. Coplan L. Lichtbroun B. Krosser A. Lichtbroun M. et al . (2018). The role of stress in the mosaic of autoimmunity: an overlooked association. Autoimmun. Rev.17, 967–983. doi: 10.1016/j.autrev.2018
212
Sparacio A. IJzerman H. Ropovik I. Giorgini F. Spiessens C. Uchino B. (2024). Self-administered mindfulness interventions reduce stress in a large, randomized controlled multi-site study. Nat. Hum. Behav.8, 1716–1725. doi: 10.1038/s41562-024-01907-7
213
Spinelli C. Wisener M. Khoury B. (2019). Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials. J. Psychosom. Res.120, 29–38. doi: 10.1016/j.jpsychores.2019.03.003
214
Stapelberg N. Neumann D. Shum D. McConnell H. Hamilton-Craig I. (2015). From physiome to pathome: a systems biology model of major depressive disorder and the psycho-immune-neuroendocrine network. Curr. Psychiatr. Rev.11, 32–62. doi: 10.2174/157340051066614061
215
Stojanovich L. (2010). Stress and autoimmunity. Autoimmun. Rev.9, A271–A276. doi: 10.1016/j.autrev.2009.11.014
216
Stratakis C. Chrousos G. (1995). Neuroendocrinology and pathophysiology of the stress system. Ann. N. Y. Acad. Sci.771, 1–18. doi: 10.1111/j.1749-6632.1995.tb44666.x
217
Streeten D. (1993). Is hypothalamic-pituitary-adrenal hyperactivity important in the pathogenesis of excessive abdominal fat distribution?J. Clin. Endocrinol. Metab.77, 339–340. doi: 10.1210/jcem.77.2.8345038
218
Strohmaier S. Jones F. Cane J. (2021). Effects of length of mindfulness practice on mindfulness, depression, anxiety, and stress: a randomized controlled experiment. Mindfulness12, 198–214. doi: 10.1007/s12671-020-01512-5
219
Suess W. Alexander A. Smith D. Sweeney H. Marion R. (1980). The effects of psychological stress on respiration: a preliminary study of anxiety and hyperventilation. Psychophysiology17, 535–540. doi: 10.1111/j.1469-8986.1980.tb02293.x
220
Taché Y. Martinez V. Million M. Wang L. (2001). Stress and the gastrointestinal tract III. Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptors. Am. J. Physiol. Gastrointest. Liver Physiol.280, G173–G177. doi: 10.1152/ajpgi.2001.280.2.G173
221
Tang Y. Hölzel B. Posner M. (2015). The neuroscience of mindfulness meditation. Nat. Rev. Neurosci.16, 213–225. doi: 10.1038/nrn3916
222
Teixeira R. Díaz M. Santos T. Bernardes J. Peixoto L. Bocanegra O. et al . (2015). Chronic stress induces a hyporeactivity of the autonomic nervous system in response to acute mental stressor and impairs cognitive performance in business executives. PLoS One10:e0119025. doi: 10.1371/journal.pone.0119025
223
Thind H. Lantini R. Balletto B. Donahue M. Salmoirago-Blotcher E. Bock B. et al . (2017). The effects of yoga among adults with type 2 diabetes: a systematic review and meta-analysis. Prev. Med.105, 116–126. doi: 10.1016/j.ypmed.2017.08.017
224
Todd J. Aspell J. (2022). Mindfulness, interoception, and the body. Brain Sci.12:696. doi: 10.3390/brainsci12060696
225
Tsigos C. Kyrou I. Kassi E. Chrousos G. (2000). “Stress: endocrine physiology and pathophysiology” in Endotext [internet], editors: Feingold, KR; Anawalt, B; Blackman, MR (South Dartmouth, MA: MDText.com, Inc).
226
Tsigos C. Papanicolaou D. Kyrou I. Raptis S. Chrousos G. (1999). Dose-dependent effects of recombinant human interleukin-6 on the pituitary-testicular axis. J. Interf. Cytokine Res.19, 1271–1276. doi: 10.1089/107999099312948
227
Van Dam N. van Vugt M. Vago D. Schmalzl L. Saron C. Olendzki A. et al . (2018). Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect. Psychol. Sci.13, 36–61. doi: 10.1177/1745691617709589
228
van den Heuvel S. van der Beek A. Blatter B. Hoogendoorn W. Bongers P. (2005). Psychosocial work characteristics in relation to neck and upper limb symptoms. Pain114, 47–53. doi: 10.1016/j.pain.2004.12.008
229
Vilhauer M. “Meditation: How to meditate without a formal routine,” Psychology today, (2024). Available online at: https://www.psychologytoday.com/sg/blog/healthy-minds/202406/how-to-meditate-without-a-formal-routine (Accessed 10 Jul 2024).
230
Waddell G. Newton M. Henderson I. Somerville D. Main C. (1993). A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain52, 157–168. doi: 10.1016/0304-3959(93)90127-B
231
Walker S. (1996). NET seminar folder, Encinitas. USA: NET Inc.
232
Wang Z. Liu S. Xu X. Xiao Y. Yang M. Zhao X. et al . (2022). Gut microbiota associated with effectiveness and responsiveness to mindfulness-based cognitive therapy in improving trait anxiety. Front. Cell. Infect. Microbiol.12:719829. doi: 10.3389/fcimb.2022.719829
233
Won E. Kim Y. (2016). Stress, the autonomic nervous system, and the immune-kynurenine pathway in the etiology of depression. Curr. Neuropharmacol.14, 665–673. doi: 10.2174/1570159x14666151208113006
234
World Health Organization , “Constitution,” (2024). Available online at: https://www.who.int/about/governance/constitution (Accessed 9 July 2024).
235
Wu Y. Johnson B. Acabchuk R. Chen S. Lewis H. Livingston J. et al . (2019). Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin. Proc.94, 432–446. doi: 10.1016/j.mayocp.2018.09.023
236
Yang H. Koh E. Sung M. Kang H. (2021). Changes induced by mind-body intervention including epigenetic marks and its effects on diabetes. Int. J. Mol. Sci.22:1317. doi: 10.3390/ijms22031317
237
Yegorov Y. Poznyak A. Nikiforov N. Sobenin I. Orekhov A. (2020). The link between chronic stress and accelerated aging. Biomedicine8:198. doi: 10.3390/biomedicines8070198
238
Zeng Y. Xie X. Cheng A. (2019). Qigong or tai chi in cancer care: an updated systematic review and meta-analysis. Curr. Oncol. Rep.21:48. doi: 10.1007/s11912-019-0786-2
239
Zgierska A. Obasi C. Brown R. Ewers T. Muller D. Gassman M. et al . (2013). Randomized controlled trial of mindfulness meditation and exercise for the prevention of acute respiratory infection: possible mechanisms of action. Evid. Based Complement. Alternat. Med.2013:952716. doi: 10.1155/2013/952716
240
Zhang D. Lee E. Mak E. Ho C. Wong S. (2021). Mindfulness-based interventions: an overall review. Br. Med. Bull.138, 41–57. doi: 10.1093/bmb/ldab005
241
Zhang B. Ma S. Rachmin I. He M. Baral P. Choi S. et al . (2020). Hyperactivation of sympathetic nerves drives depletion of melanocyte stem cells. Nature577, 676–681. doi: 10.1038/s41586-020-1935-3
242
Zhang H. Wang M. Zhao X. Wang Y. Chen X. Su J. (2024). Role of stress in skin diseases: A neuroendocrine-immune interaction view. Brain Behav. Immun.116, 286–302. doi: 10.1016/j.bbi.2023.12.005
Summary
Keywords
mindfulness-based interventions, musculoskeletal therapy, chronic stress management, biopsychosocial model of healthcare, neuro-emotional technique, psychoneuroimmunology, mind–body interventions, stress physiology
Citation
Bablis P, Day RR, Bablis S and Pollard H (2025) Why mindfulness matters in musculoskeletal therapies: a narrative review. Front. Psychol. 16:1518141. doi: 10.3389/fpsyg.2025.1518141
Received
28 October 2024
Accepted
29 September 2025
Published
17 October 2025
Volume
16 - 2025
Edited by
Adelinda Araujo Candeias, University of Evora, Portugal
Reviewed by
Áthila Campos Girão, Federal University of São Paulo, Brazil
Suzana Pustivšek, Academic and Research Network of Slovenia, Slovenia
Updates
Copyright
© 2025 Bablis, Day, Bablis and Pollard.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ryan R. Day, rday@universalhealth.com.au
†ORCID: Peter Bablis, orcid.org/0000-0002-1574-7153
Ryan R. Day, orcid.org/0009-0008-4070-3460
Sophia Bablis, orcid.org/0009-0001-6165-5356
Henry Pollard, orcid.org/0000-0003-0269-5697
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.