- 1Department of Obstetrics, Affiliated Hospital of Jiangnan University, Wuxi, Jiangsu, China
- 2School of Wuxi Medical College, Jiangnan University, Wuxi, Jiangsu, China
- 3Department of Obstetrics, Women’s Hospital of Jiangnan University, Wuxi, Jiangsu, China
Introduction: Many studies suggest that psychological factors are intrinsically connected to the onset of preeclampsia. However, there are no relevant surveys on the psychological situation of this population. The aims of our study were to investigating the causes and prevalence of pregnancy stress in individuals at high risk of preeclampsia; exploring the correlation between pregnancy stress and anxiety, depression, and self-management capacity in this group. Our study provided evidence for the development of effective clinical management strategies and related psychological care for women at high risk of preeclampsia.
Methods: A cross-sectional survey was conducted on women at high risk of preeclampsia who came to Jiangnan University Hospital’s obstetrics outpatient clinic for antenatal care. Sociodemographic and obstetric-related characteristics, Pregnancy Stress Rating Scale (PSRS), Self-rating anxiety scale (SAS), Self-rating depression scale (SDS), Self-rating Questionnaire of Healthcare Management for Pregnancy (SQHMP) were included in this study. Data analysis covered descriptive statistics, univariate analysis, Spearman’s rank correlation, and multiple linear regression analysis.
Results: A total of 138 pregnant women at high risk of preeclampsia were enrolled in the study. Univariate analysis showed significant relationships between intergenerational relations (with mothers-in-law), pregnancy intention, and desired mode of delivery among pregnancy stress (p < 0.001). Median (IQR) scores were: PSRS 0.283 (0.133, 0.542), SAS 38.750 (32.500, 45.000), SDS 41.250 (33.750, 50.000), SQHMP 43.000 (35.000, 53.250). The score of Spearman’s rank correlation showed that pregnancy stress was positively correlated with anxiety, depression, and self-management capacity, respectively (r = 0.465, p < 0.001), (r = 0.437, p < 0.001), and (r = 0.585, p < 0.001). Multiple linear regression analysis showed that desired mode of delivery, anxiety, and self-management capacity were the main predictors of pregnancy stress.
Conclusion: The findings emphasize the need to focus on pregnancy stress in women at high risk of preeclampsia, especially those have presented higher levels of anxiety, depression, and self-management capacity. Based on these variables, healthcare professionals should increase screening for mental health in pregnant women at high risk of preeclampsia as well as provide additional psychological care.
1 Introduction
Preeclampsia is a serious pregnancy-specific condition characterized by new-onset hypertension and proteinuria after 20 weeks of gestation (Rana et al., 2020). It is estimated to affect approximately 2–8% of pregnancies worldwide (Gatford et al., 2020). In addition to raising the maternal risk of eclampsia, HELLP syndrome, and multi-organ dysfunction, preeclampsia can cause fetal growth restriction (FGR), preterm birth, and intrauterine fetal demise (Ives et al., 2020). However, to date, no single pathophysiology can have been able to explain the emergence of preeclampsia (Phipps et al., 2019). As the traditional medical care paradigm shifts, there is a growing emphasis on the role of maternal psychosocial factors in the prevention, treatment and regression of the disease (Freiberger et al., 2022). Previous research suggests that psychological factors are intrinsically connected to the onset of preeclampsia (Krishnamurti et al., 2019; Traylor et al., 2020).
Along with the physiological changes, pregnant women also face alterations in their social, economic, familial, and personal roles. This makes them particularly vulnerable to psychological changes and mood swings, ultimately leading to pregnancy stress (Wang et al., 2023; Heberlein et al., 2016; Niela-Vilen et al., 2023). Literature suggested that almost 80% of pregnant women both at home and abroad experienced varying levels of pregnancy stress (Na et al., 2022). Research on pregnancy stress in China has developed relatively later compared with Western countries, with significant regional variations in stress levels among pregnant women (Caiyun et al., 2020). As an economically developed city in the Yangtze River Delta region, Wuxi exposes women of childbearing age to characteristic urban stressors including work–family conflicts and high living costs (Shuxiu, 2021). Notably, studies have reported that the prevalence of preeclampsia in metropolitan areas in southern China ranges from 4.4 to 5.57%, which is at a high level both at home and abroad (Gatford et al., 2020; Caixia et al., 2019). Pregnant women are prone to anxiety and depression due to the numerous stressors they encounter (Delagneau et al., 2023). A survey of primiparous women showed that higher levels of psychological stress were associated with more anxiety and depression during pregnancy (Hang et al., 2017). Pregnant complications such as habitual abortion, gestational hypertension, and preterm labor may become more common if negative emotions persist (Bernard et al., 2019). In a meta-analysis by Shay et al. (2020), the results revealed that there was a 40% increased risk of preeclampsia among women who suffered adverse mood at any time during pregnancy. Another research reported that both pregnancy stress and risk factors for preeclampsia accounted for developing preeclampsia in a synergistic manner (Giurgescu et al., 2015; Yu et al., 2013). Especially in recent years, neuropsychoimmunological mechanisms explaining the causal relationship between stress and preeclampsia are becoming a topic of active research (Buglione-Corbett et al., 2018). Psychological stress during pregnancy induces sympathetic arousal and activation of the hypothalamic–pituitary–adrenal axis, which may promote endothelial dysfunction and increased inflammatory activity (László et al., 2013), finally leading to the occurrence of preeclampsia.
Preeclampsia management remains clinically challenging. Current interventions focus on intensive monitoring (blood pressure, proteinuria, organ function) and symptomatic treatment to prolong gestation safely (Amaral et al., 2017). Definitive treatment requires pregnancy termination, often necessitating iatrogenic preterm delivery when maternal-fetal risks escalate (Dimitriadis et al., 2023; Smith et al., 2020). As modifiable risk factors, psychosocial stressors (especially pregnancy stress, anxiety, and depression) and self-management capacity warrant further investigation regarding their association with preeclampsia development (Ngene and Moodley, 2024; Bosquet Enlow et al., 2021). In the past, more attentions have been paid to women who have already experienced preeclampsia than to those who are more likely to get preeclampsia. Moreover, there has not been much research done on quantifying and evaluating the psychological conditions associated with those at high risk of preeclampsia (Rahnemaei et al., 2020). Behavioral interventions during pregnancy may affect maternal stress and mental health (Bosquet Enlow et al., 2021). Several studies have highlighted the importance of personal self-management for improving preeclampsia awareness and some pregnancy outcomes in pregnant women at high risk for preeclampsia (Alnuaimi et al., 2020; Moulaei et al., 2021; Endeshaw et al., 2015). However, whether the positive effects caused by self-management are related to pregnancy stress, anxiety, and depression remains to be explored.
In conclusion, the aims of our study were to investigating the causes and prevalence of pregnancy stress in individuals at high risk of preeclampsia; exploring the correlation between pregnancy stress and anxiety, depression, and self-management capacity in this group. Having a thorough understanding of these factors supports the creation of clinical management plans and related psychological services. This encourages multifaceted prevention of unfavorable pregnancy outcomes.
2 Materials and methods
2.1 Study setting and participants
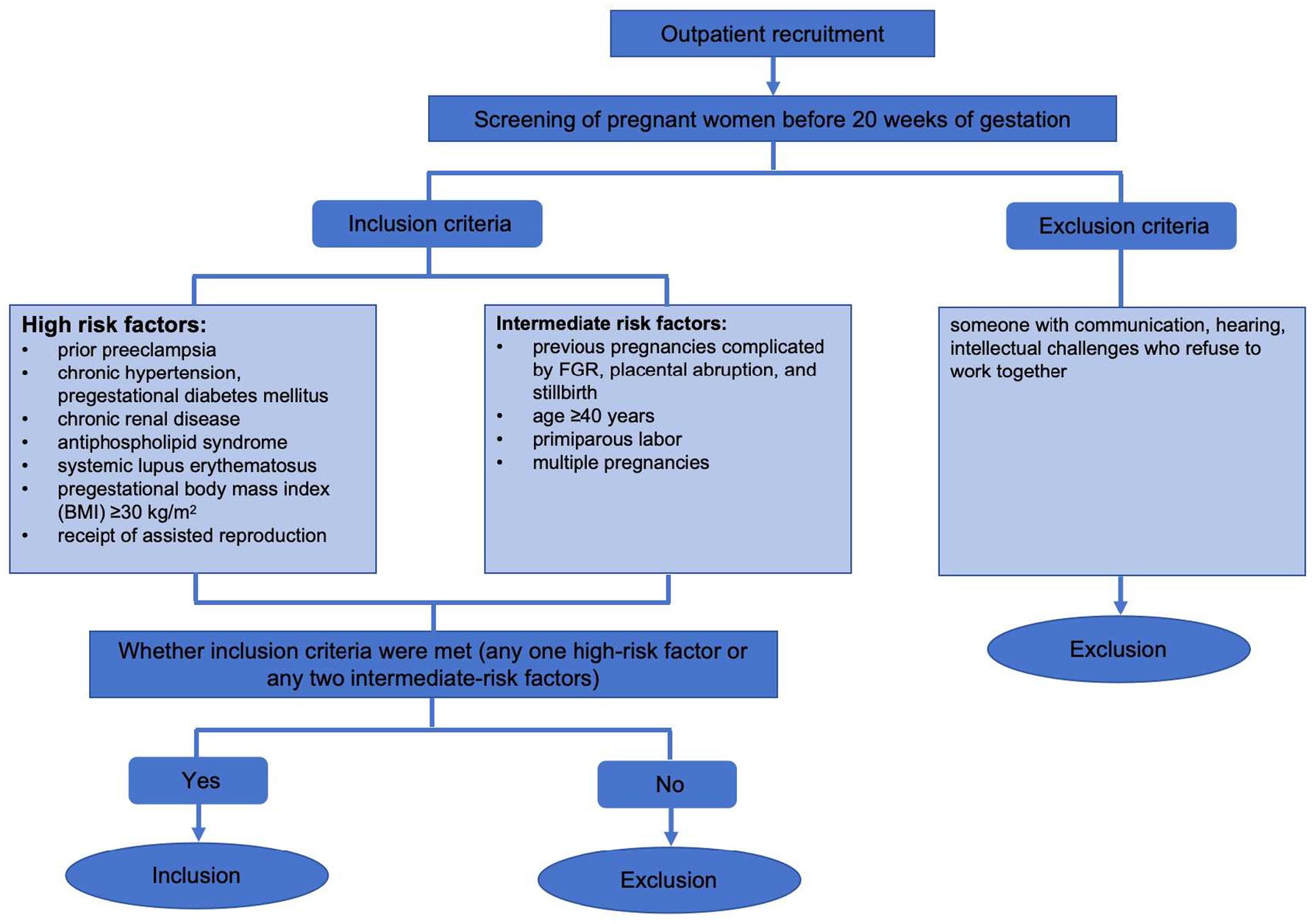
A cross-sectional relational design was used in this study. From May 2023 to August 2024, we looked into the women at high risk of preeclampsia before 20 weeks of pregnancy and came to obstetrical outpatient clinic affiliated Hospital of Jiangnan University in Wuxi City, Jiangsu Province, China, for antenatal care. The inclusion criteria for women were: any one high-risk factor or any two intermediate-risk factors (Yao Tang and Li, 2022). High risk factors: prior preeclampsia, chronic hypertension, pregestational diabetes mellitus, chronic renal disease, antiphospholipid syndrome, systemic lupus erythematosus, pregestational body mass index (BMI) ≥ 30 kg/m2, receipt of assisted reproduction; intermediate risk factors: previous pregnancies complicated by FGR, placental abruption, stillbirth, and multiple pregnancies, age ≥ 40 years, primiparous labor. Exclusion criteria: someone with communication, hearing, and intellectual challenges who refuse to work together. Based on the parameters of previous related studies (Tuxunnjiang et al., 2022) r = 0.278, 1-β = 0.9, the sample size was calculated to be 131 pregnant women using G power 3.1 software, which was further expanded by 5% considering invalid questionnaires at the time of sample retrieval. The estimation showed that the inclusion of at least 138 pregnant women at high risk of preeclampsia fulfilled this investigation. The detailed recruitment process was shown in Figure 1.
2.2 Ethical consideration
This study was approved by the Ethics Committee of the Affiliated Hospital of Jiangnan University (LS2024302) and the informed consent of the pregnant women has been obtained. The study was conducted in accordance with the guidelines of the Declaration of Helsinki.
2.3 Data collection
Before data collection, all researchers received standardized training. Using established protocols, they explained the study and obtained informed consent before conducting face-to-face interviews to ensure consistent questionnaire administration and interpretation. The data collection method was a combination of electronic medical record review and a paper questionnaire survey. Questionnaires were distributed and returned on the spot 150 questionnaires were handed out during the survey’s May to August 2024 period. Twelve of these were excluded from the analysis due to dropping out (Freiberger et al., 2022) and incomplete data (Traylor et al., 2020), leaving 138 questionnaires for final analysis.
2.4 Measures
2.4.1 Sociodemographic and obstetric-related characteristics
Age, education, residence, employment status, monthly per capita household income (RMB, renminbi, Chinese yuan), marital relationships and intergenerational relations (with mothers-in-law), sleep situation, pregnancy intention, and desired mode of delivery were all gathered using a self-designed questionnaire. Others were collected through medical records.
2.4.2 Pregnancy stress rating scale (PSRS)
The Pregnancy Stress Rating Scale (PSRS) is a self-reported assessment tool created in 1983 by Chen, a Chinese researcher from Taiwan. It gauges prenatal stress in expectant mothers (Chen, 2015). Four dimensions are represented by the scale: (a) parental role identification; (b) mother and child health and safety; (c) changes in body size and physical activity; and (d) additional stressors. The PSRS consists of 30 items, and the scale score = actual total pregnancy stress score/ number of all entries. Higher scores correspond to higher levels of pregnancy stress. With 0.000 for no stress, 0.001–1.000 for mild stress, 1.001–2.000 for moderate stress and 2.001–3.000 for severe stress (Tang et al., 2019). Prior research has demonstrated the scale’s validity in Chinese women (Cronbach’s α = 0.936–0.946) (Gao et al., 2023). The Cronbach’s alpha for the PSRS in this study was 0.939.
2.4.3 Self-rating anxiety scale (SAS)
The 20-item Self-Rating Anxiety Scale (SAS) was compiled by American doctor Zung (1971). The SAS is a self-reported assessment tool. Its total score can be as low as 0 and as high as 100, with the standardized score being the sum of the scores on the 20 items multiplied by 1.25. Based on the Chinese SAS criteria, which represent the subjective emotions of those who are prone to anxiety, a cut-off point for anxiety was established at a total score of 50. As the score increases, the anxiety increases. The cut-offs for the SAS standard scores were defined as: <50, no anxiety; 50–59, minimal to mild anxiety; 60–69, moderate to marked anxiety, >70, severe anxiety (Zhou et al., 2022). The Cronbach’s alpha for the SAS in this study was 0.705.
2.4.4 Self-rating depression scale (SDS)
The Self-rating depression scale (SDS) is a self-reported assessment tool. Its total score can be as low as 0 and as high as 100, with the standardized score being the sum of the scores on the 20 items multiplied by 1.25. Based on the Chinese SDS criteria, which represent the subjective emotions of those who are prone to depression, a cut-off point for depression was established at a total score of 50.Standard score is classified as: <50, no depression; 50–59, minimal to mild depression; 60–69, moderate to marked depression, >70, severe depression (Zhou et al., 2022). The Cronbach’s alpha for the SDS in this study was 0.848.
2.4.5 Self-rating questionnaire of healthcare management for pregnancy (SQHMP)
In order to evaluate pregnant women’s self-management capacity, Jinzhi Li (2011) created the Self-rating Questionnaire of Healthcare Management for Pregnancy (SQHMP) in 2013, which is also relies on self-reported. Each entry is scored from 1 to 5 points, with a total score of 25–125 points, higher scores mean that pregnant women have better self-management capacity. Strong reliability and validity were demonstrated by the questionnaire’s internal consistency reliability coefficient of 0.93, retest reliability Pearson’s correlation value of 0.96, and content validity index (CVI) of 0.91 (Xiao et al., 2024). The Cronbach’s alpha for the SQHMP in this study was 0.888.
2.4.6 Data analysis
SPSS 25.0 statistics software was used for statistical analysis after the gathered data was carefully checked and entered into Excel to create a database. In descriptive statistics, pregnant women are represented as n (%) in the general information. Since the data for the questionnaire score petition did not follow a normal distribution, we used median and interquartile spacing to represent them. The Mann–Whitney U test or the Kruskal-Wallis H test were employed in the univariate analysis of mothers’ stress when assessing the variations in pregnancy stress among obstetric and demographic characteristic variables. Since the data on pregnant stress, anxiety, depression and self-management skills during pregnancy in our sample did not conform to a normal distribution, the application of Spearman rank correlation analysis was considered. Multiple linear regression models were employed to determine factors that contribute to pregnancy stress in the end. All categorical variables included in the model were coded with appropriate dummy variables prior to inclusion in the model (Intergenerational relations: 1 = Cohesion, 2 = General, 3 = Occasional quarrel; Planned Pregnancy: 0 = Yes, 1 = No; Desired mode of delivery: 1 = Vaginal delivery, 2 = Cesarean delivery. SAS, SDS, and SQHM are substituted with the original value of the total score). Statistical significance was defined as p < 0.05, and all tests were two-sided.
3 Results
3.1 Demographics and clinical characteristics of obstetrics
Societal and obstetric attributes of the 138 individuals in the study population are shown in Table 1. All participants ranged in age from 18 to 43 years with a mean of (31.93 ± 5.10) years. For this pregnancy, the majority of women (68.1%) had a planned pregnancy. Table 1 displays the remaining obstetric clinical and sociodemographic features.
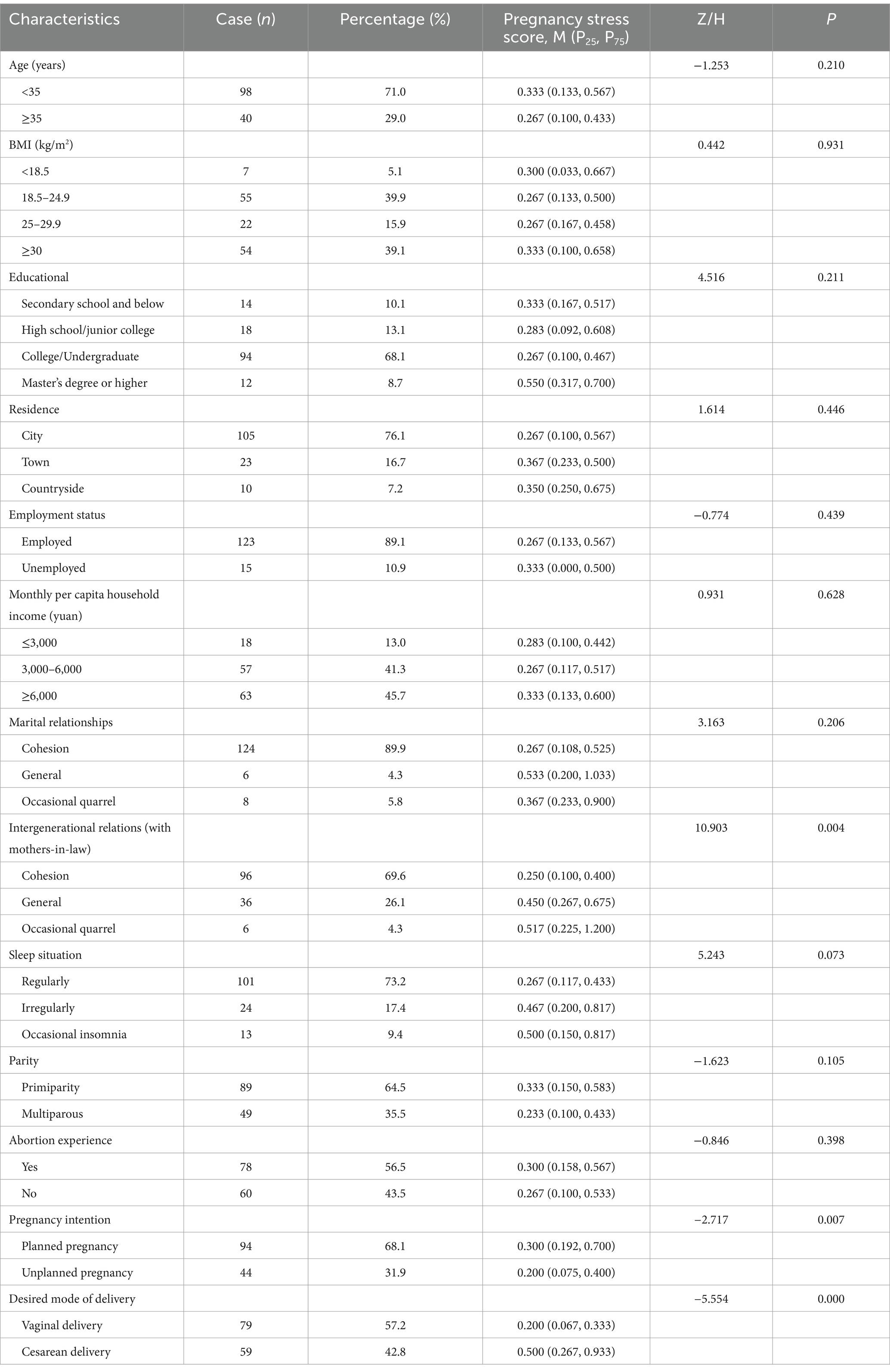
Table 1. Differences in sociodemographic and medical information variables according to pregnancy stress scores of participants (N = 138).
3.2 Univariate analysis of pregnancy stress
There were statistically significant differences in pregnancy stress among high-risk preeclampsia women, with intergenerational relations showing the strongest association (p = 0.004), followed by pregnancy intention (p = 0.007) and desired mode of delivery (p < 0.001). But age, BMI, education level, residence, employment status, monthly per capita household income, parity, and abortion experience did not differ statistically significantly (p > 0.05).
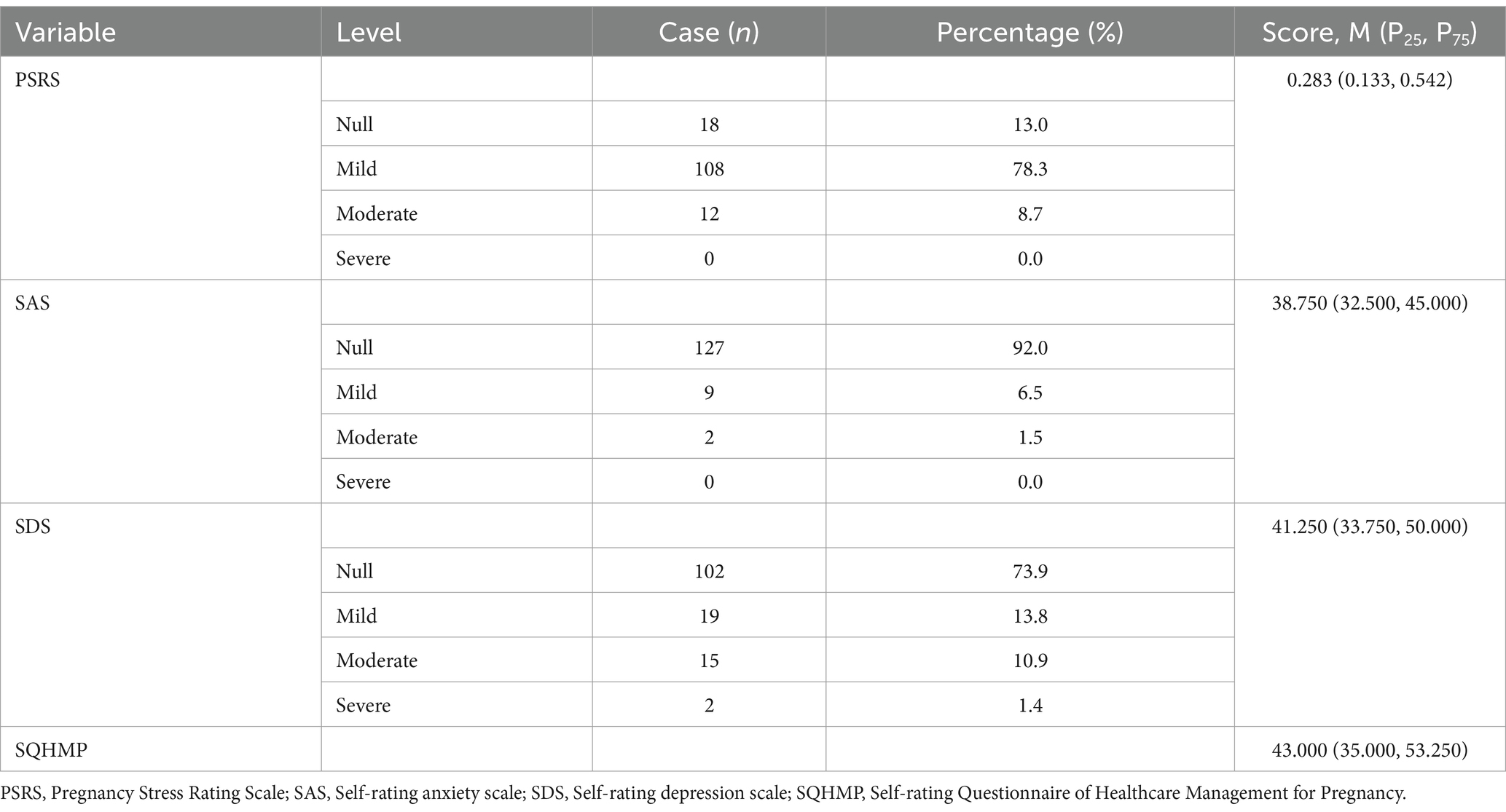
3.3 Scores for pregnant stress, anxiety, depression, and self-management
Stress, anxiety, depression, and self-management capacity scores during pregnancy took the form of 0.283 (0.133, 0.542), 38.750 (32.500, 45.000), 41.250 (33.750, 50.000), and 43.000 (35.000, 53.250). Of pregnant women at high risk for preeclampsia, our results showed that 8.7% had moderate pregnancy stress and 78.3% had mild pregnancy stress. Some pregnant women may feel depressed and anxious to some extent. In Table 2, the various distribution levels of their scores were displayed.
3.4 Correlations between pregnancy stress, anxiety, depression, and self-management capacity during pregnancy
Table 3 reveals that pregnancy stress was positively correlated with anxiety, depression, and self-management capacity (r = 0.465, p < 0.001), (r = 0.437, p < 0.001), (r = 0.585, p < 0.001). Anxiety was positively associated with depression (r = 0.754, p < 0.001), and with self-management capacity (r = 0.422, p < 0.001). Additionally, self-management capacity and depression were positively correlated (r = 0.400, p < 0.001).
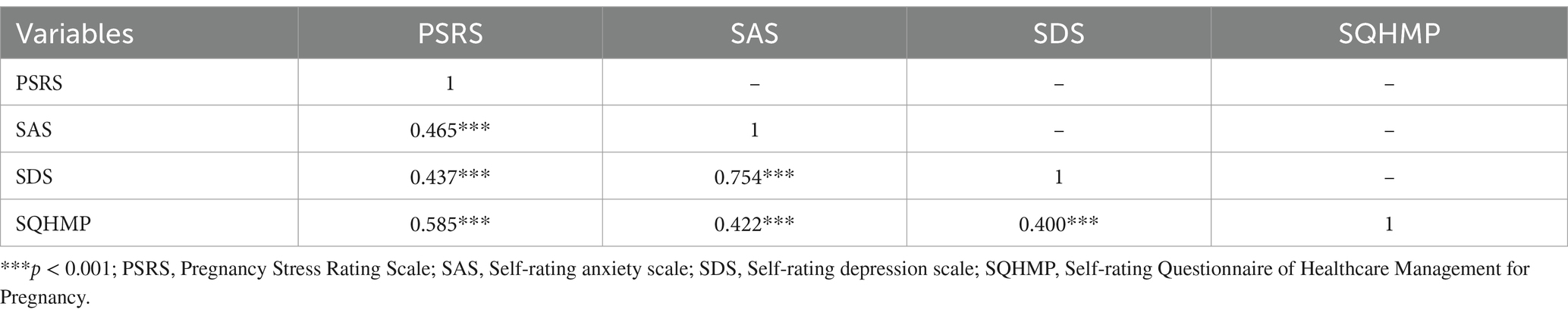
Table 3. Correlations among pregnancy stress, anxiety, depression, and self-management capacity (N = 138).
3.5 Regression analysis
Significant variables were entered into the regression equation model after conducting univariate analysis and Pearson correlation analysis. As shown in Table 4, the desired mode of delivery, anxiety, and self-management capacity were significantly associated with pregnancy stress. Specifically, the regression coefficient for desired mode of delivery was 0.206 (SE = 0.049, t = 4.168, p < 0.001); the SAS were 0.011 (SE = 0.005, t = 2.338, p < 0.05); and the regression coefficient for the SQHMP was 0.010 (SE = 0.002, t = 4.745, p < 0.001). The results indicated all above three variables had a significant positive impact on pregnancy stress. In contrast, the regression coefficients for intergenerational relationships (B = –0.040, p = –0.385), planned pregnancies (B = –0.036, p = 0.485), and SDS (B = 0.003, p = 0.404) did not reach significance levels. The overall regression model explains 47.7% of the variance in pregnancy stress (R2 = 0.477), After adjusting for the number of predictors, the model accounts for 45.3% of the variance (adjusted R2 = 0.453), This indicates that nearly half of the variability in pregnancy stress can be explained by the combination of intergenerational relations, pregnancy planning, desired mode of delivery, anxiety, depression, and self-management capacity. The results of the analysis were statistically significant (R2 = 0.477, F = 19.88, p < 0.001).
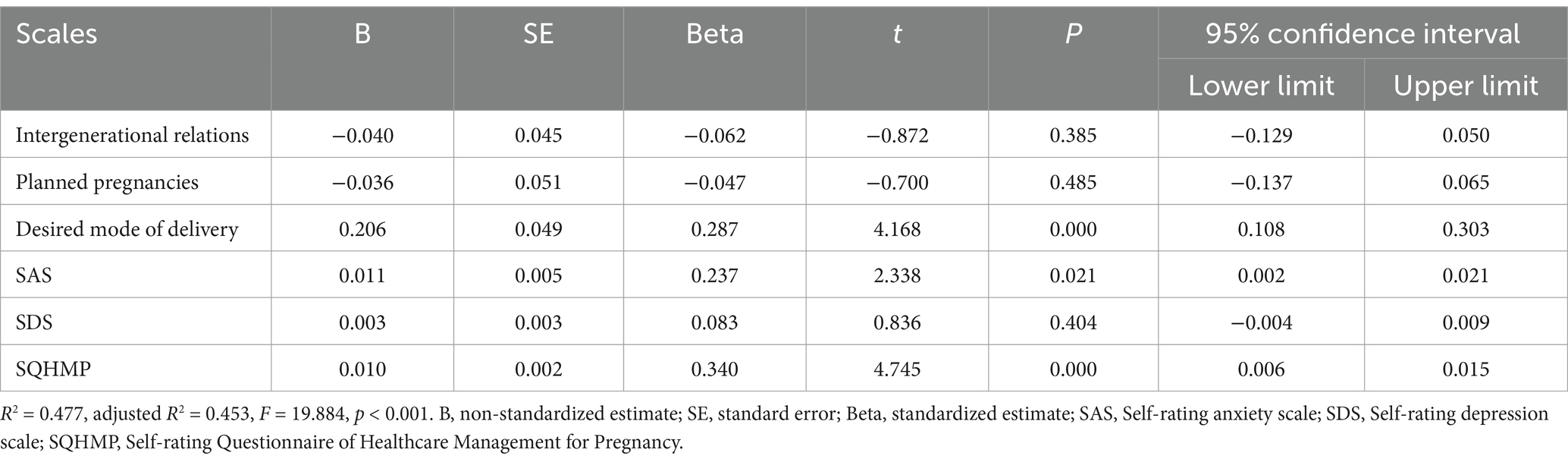
Table 4. Descriptive statistics of pregnancy stress, anxiety, depression and self-management ratings (N = 138).
4 Discussion
Our study focused on measuring pregnancy stress levels in individuals at high risk of preeclampsia, analyzing the factors that affect pregnancy stress, and exploring the relationship between them. The findings prove that there is a widespread sense of pregnancy stress among those who are at risk for preeclampsia. Pregnancy stress was substantially accompanied by feeling anxious, depressed, and self-management capacity for pregnant women. Importantly, our regression analysis revealed three key predictors of pregnancy stress: desired mode of delivery, anxiety levels, and self-management capacity, which collectively explained 45.3% of the variance in pregnancy stress after adjustment.
4.1 Current status of pregnancy stress in people at high risk of preeclampsia
The findings of this study showed that 78.3% of pregnant women at high risk of preeclampsia had mild pregnancy stress and 8.7% had moderate pregnancy stress, similar to the research findings of Na et al. (2022). Unexpectedly, pregnant women with preeclampsia risk factors did not experience greater levels of pregnancy stress. This could be explained by a lack of awareness among this population about preeclampsia and its risk factors, as well as bias toward potential outcomes caused by preeclampsia (Püschl et al., 2023). Frawley et al. (2020) found that 67.5% of pregnant women were uncertain about preeclampsia before pregnancy. This made us wonder if educating this demographic about preeclampsia prevention could actually make them more stressed and depressed during pregnancy. Further intervention studies are required in the future to elucidate this.
4.2 Factors that affect pregnancy stress in individuals who are at high risk of preeclampsia
An important element affecting the level of pregnancy stress in the pregnant women at high-risk preeclampsia is intergenerational relationships (with mother-in-law). The mother-in-law-daughter-in-law connection, a deeply embedded subject in Chinese culture, becomes more sensitive and delicate during the perinatal time (Qi et al., 2022). Pregnant women who had a subjective perception of “cohesion” on measures of intergenerational relationships with their mothers-in-law exhibited less pregnancy stress, as we found. Insufficient social support, especially insufficient interactions between generations, is a risk factor for prenatal mental health issues (Bedaso et al., 2021). In some patriarchal societies, such as India, many Middle Eastern, African and East Asian countries, women tend to live with their husbands’ families once married. So, it is inevitable that the relationship between mothers-in-law and daughters-in-law is deeply intertwined (Varghese and Roy, 2019). According to Riem et al. (2024) study, the mental health of pregnant women depends on the support provided by their husband’s parents and the quality of intergenerational relationships. Mrayan et al. (2016) said that the social support offered by traditional pregnancy notions could not always be good for new moms’ emotional health because of the tension between traditional and modern norms. Therefore, to balance family support and encourage a positive mindset concerning pregnancy and childbirth, the health care system must provide more assistance in coordinating prenatal education with the elder generation.
Another element that influences pregnant stress in those at high risk for preeclampsia is pregnancy intention. Interestingly, compared to women with unplanned pregnancies, those with planned pregnancies suffered higher levels of pregnancy stress. This finding is consistent with the results of the Rashidi et al. (2025) study. The reason for this is that, on the one hand, women with unplanned pregnancies often choose to terminate their pregnancies early in the pregnancy and are not included in the follow-up; on the other hand, women with planned pregnancies may instead suffer from greater psychological stress and anxiety due to the pursuit of the idealized expectation of becoming a “perfect mother.” Contrary to what we found, the Maxson and Miranda (2011) study found that women who had unplanned or untimely pregnancies had higher levels of depression, anxiety, and perceived stress. This may reflect that we included women with assisted reproductive pregnancies in our high-risk group for preeclampsia. Pregnancy stress was reported to be significantly higher in women who had received assisted reproduction than in those who had been naturally conceived. The major causes of this stress include worries about how the pregnancy would turn out, the mental and physical strain of the medical procedure, and the pressure from society (Öztürk et al., 2021). This was also confirmed by a cross-sectional survey of pregnancy stress between naturally conceived women and women who underwent assisted reproduction techniques, conducted by our scholar Xuehua Cao et al. (2011). Therefore, the inclusion of this population had the potential to confound the results. The further studies should be more cautious about investigating women undergoing assisted reproduction.
A particular factor that influences pregnancy stress in those at high risk for preeclampsia was the desired mode of delivery. Our research findings, similar to those reported by Luyan Liu (2009), demonstrated that pregnant women who wished for a caesarean section experienced higher levels of pregnancy stress compared to those who expected natural childbirth. A study by Xihong Zhou (2011) found that prenatal anxiety affected a woman’s choice of delivery method. Concern regarding the fetus and fear of labor pains have made psychological issues the primary cause of the rise in undiagnosed cesarean procedures. To lessen mothers’ negative feelings and lower the rate of cesarean sections, obstetricians should educate them about scientific health care and offer them comprehensive psychosocial assistance.
4.3 Relationship between pregnancy stress and anxiety and depression
Depression and anxiety were highly co-morbid during pregnancy, as evidenced by our study of high-risk preeclampsia patients. In a similar vein, Lee et al. (2021) confirmed a persistent association between anxiety and depression on women during pregnancy. A substantial number of studies have indicated that adverse emotional states during pregnancy can alter the immune system and physiology of the mother, such as vasoconstriction of the placenta and other small veins and arteries throughout the body, progressively leading to an increase in blood pressure and peripheral resistance (Traylor et al., 2020). According to the past study, women who experienced more distress in their first trimester were more likely to develop preeclampsia in their second trimester (Giurgescu et al., 2015; Kurki et al., 2000). Notably, a survey conducted by Dan Li et al. (2013) across pregnant women observed that unfavorable psychological states frequently resulted in inflated perceptions and emotions regarding life events, which might raise pregnancy stress levels. As a result, it is imperative that medical professionals examine pregnant patients at risk of preeclampsia for mental health issues and offer extra effective psychological support in order to relieve pregnancy stress.
4.4 Relationship between pregnancy stress and ability for self-management
Our research showed that self-management capacity had a positive correlation with pregnancy stress experienced. This finding suggested that moderate pregnancy stress motivated self-management behaviors to some extent, or that pregnant women with high self-management capacity were more inclined to perceive and report pregnancy stress. In a cross-sectional study of 440 pregnant women during the 2019 novel coronavirus (COVID-19) pandemic, maternal self-care was associated with COVID-19 disease perceived severity was positively associated. This result is similar to our findings, suggesting that pregnant women with high self-care are more able to perceive and report associated stressors and threats (Khazaeian et al., 2022). Similarly, another study on the similar relationship between general self-efficacy and pregnancy stress in women with preterm labor also indicated that high levels of self-efficacy may amplify pregnancy stress (Cho and Kim, 2024). However, the specific causal relationship between pregnancy stress and self-management ability needs to be explored in future prospective intervention studies. We also focused on pregnant women at high risk of preeclampsia but do not experience pregnancy stress, who appeared to lack the ability to manage their pregnancies. Interestingly, a lower incidence of preeclampsia was observed in pregnant women with enhanced self-management capacity, as evidenced by the findings of the Alnuaimi et al. (2020) study.
Given that psychosocial stress, including that associated with pregnancy, anxiety, depression, and self-management capacity, is to some extent an external factor, it can often be mitigated through appropriate interventions (Vollebregt et al., 2008). It is essential to gain insight into the correlation between adverse emotional states, such as those related to pregnancy, especially related to high-risk pregnancies with preeclampsia, and self-management capacity. And for those at high risk for preeclampsia, it ought to be that future clinical practice incorporate a quick evaluation of pregnancy stress in early prenatal care. Furthermore, pregnant women with high risk of preeclampsia but without pregnancy stress should also pay extra attention to self-management. Proactive prenatal care can help alleviate adverse pregnancy emotions and reduce stress in pregnant women at high risk of preeclampsia, thereby lowering their probability of developing preeclampsia and achieving satisfactory pregnancy outcomes.
5 Limitations
Several limitations must be acknowledged in this investigation. Firstly, the research instruments we utilized were four self-reported structured questionnaires that were subjective in nature. Secondly, limited sample size of the study does not permit a definitive conclusion regarding the efficacy of self-management capacity in a population afflicted with moderate-to-severe pregnancy stress. Our study investigated only one tertiary hospital in Wuxi, Jiangsu Province. A large-scale study of this population would be beneficial in elucidating the capacity to self-management across a spectrum of pregnancy stress levels. The future research multicenter studies should be conducted in areas or institutions that are diverse in terms of ethnocultural, socioeconomic background, geographic location, and prenatal care utilization. The generalizability of the findings for replication can be improved by expanding the sample and multicenter studies. While the current model was able to explain 47.7% of the variance in pregnancy stress, other important influences did exist that were not included. For example, social support. Future studies still need to incorporate more factors to create a more comprehensive model. Finally, the cross-sectional design only allows demonstrating an association among pregnancy stress, anxiety, depression, and the capacity to self-management in individuals at high risk of preeclampsia. And it is impossible to infer causality among these factors. In future longitudinal studies, a randomized controlled trial could be further conducted in a population at high risk for preeclampsia to observe whether pregnancy stress has a causal effect on anxiety, depression, and self-management ability. The research will also be included more objective indicators, such as variations in stress biomarkers like cortisol and catecholamines, as well as the prevalence of preeclampsia and complications, except subjective questionnaires.
6 Conclusion
In conclusion, it can be stated that stress related to pregnancy is a common occurrence among those at risk of developing preeclampsia. Pregnancy stress was found to be independently predicted by the mother-in-law relationship, pregnancy intention, preferred delivery method, anxiety, and capacity for self-management. Therefore, healthcare professionals can combine these predictors in their clinical work to quantify and assess the emotional health status of pregnant women at high risk of preeclampsia, and develop screening guidelines for pregnancy stress in this group. Our study also revealed a robust correlation among anxiety, depression, and the capacity to self-manage and cope with pregnancy stress in individuals at high risk for preeclampsia. As such, pregnant women who are screened for pregnancy stress and emotional distress can be given proper guidance to raise their awareness of self-management, so that they can face pregnancy and labor more comfortably.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Affiliated Hospital of Jiangnan University (LS2024302). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XC: Conceptualization, Data curation, Software, Writing – original draft. JW: Data curation, Formal analysis, Writing – original draft. LY: Data curation, Investigation, Validation, Writing – original draft. LC: Investigation, Supervision, Writing – original draft. YH: Conceptualization, Writing – review & editing. PG: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Youth National Natural Science Foundation of China (The role and mechanism of curcumin in regulating the gut placental axis in the prevention and treatment of preeclampsia, no. 82104919).
Acknowledgments
The authors express gratitude to all study participants and research staff who participated in the work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1537858/full#supplementary-material
References
Alnuaimi, K., Abuidhail, J., and Abuzaid, H. (2020). The effects of an educational programme about preeclampsia on women's awareness: a randomised control trial. Int. Nurs. Rev. 67, 501–511. doi: 10.1111/inr.12626
Amaral, L. M., Wallace, K., Owens, M., and LaMarca, B. (2017). Pathophysiology and current clinical Management of Preeclampsia. Curr. Hypertens. Rep. 19:61. doi: 10.1007/s11906-017-0757-7
Bedaso, A., Adams, J., Peng, W. B., and Sibbritt, D. (2021). The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod. Health 18:23. doi: 10.1186/s12978-021-01209-5
Bernard, N., Forest, J. C., Tarabulsy, G. M., Bujold, M., Bouvier, D., and Giguère, Y. (2019). Use of antidepressants and anxiolytics in early pregnancy and the risk of preeclampsia and gestational hypertension: a prospective study. BMC Pregnancy Childbirth 19:9. doi: 10.1186/s12884-019-2285-8
Bosquet Enlow, M., Petty, C. R., Hacker, M. R., and Burris, H. H. (2021). Maternal psychosocial functioning, obstetric health history, and newborn telomere length. Psychoneuroendocrinology 123:105043. doi: 10.1016/j.psyneuen.2020.105043
Buglione-Corbett, R., Deligiannidis, K. M., Leung, K., Zhang, N., Lee, M., Rosal, M. C., et al. (2018). Expression of inflammatory markers in women with perinatal depressive symptoms. Arch. Womens Ment. Health 21, 671–679. doi: 10.1007/s00737-018-0834-1
Caixia, Z., JunTao, L., and Jinsong, G. (2019). Incidence and clinical risk factors of preeclampsia in China. J. Reprod. Med. 28, 336–341.
Caiyun, Z., Fengjuan, J., Min-min, H., Hong, Z., and Liya, L. (2020). Progress on prenatal maternal stress among pregnant women in China. Chin. J. General Prac. 18, 1353–1357.
Chen, C. H. (2015). Revision and validation of a scale to assess pregnancy stress. J. Nurs. Res. 23, 25–32. doi: 10.1097/jnr.0000000000000047
Cho, H. J., and Kim, J. I. (2024). Moderating effect of general self-efficacy on the relationship between pregnancy stress, daily hassles stress, and preterm birth risk in women experiencing preterm labor: a cross-sectional study. J. Korean Acad. Nurs. 54, 329–339. doi: 10.4040/jkan.24008
Dan Li, X. X., Liu, J., and Ping, W. (2013). The relationship between life event and pregnancy stress: the mediating effect of mental health and the moderating effect of husband support. J. Psychol. Sci. 36, 876–883.
Delagneau, G., Twilhaar, E. S., Testa, R., van Veen, S., and Anderson, P. (2023). Association between prenatal maternal anxiety and/or stress and offspring's cognitive functioning: a meta-analysis. Child Dev. 94, 779–801. doi: 10.1111/cdev.13885
Dimitriadis, E., Rolnik, D. L., Zhou, W., Estrada-Gutierrez, G., Koga, K., Francisco, R. P. V., et al. (2023). Pre-eclampsia. Nat. Rev. Dis. Primers 9:22. doi: 10.1038/s41572-023-00417-6
Endeshaw, M., Abebe, F., Bedimo, M., and Asart, A. (2015). Diet and pre-eclampsia: a prospective multicentre case-control study in Ethiopia. Midwifery 31, 617–624. doi: 10.1016/j.midw.2015.03.003
Frawley, N., East, C., and Brennecke, S. (2020). Women's experiences of preeclampsia: a prospective survey of preeclamptic women at a single tertiary Centre. J. Obstet. Gynaecol. 40, 65–69. doi: 10.1080/01443615.2019.1615040
Freiberger, A., Beckmann, J., Freilinger, S., Kaemmerer, H., Huber, M., Nagdyman, N., et al. (2022). Psychosocial well-being in postpartum women with congenital heart disease. Cardiovisc. Diagn. Ther. 12, 389–399. doi: 10.21037/cdt-22-213
Gao, Y., Tang, X., Deng, R., Liu, J., and Zhong, X. (2023). Latent trajectories and risk factors of prenatal stress, anxiety, and depression in southwestern China-a longitudinal study. Int. J. Environ. Res. Public Health 20:818. doi: 10.3390/ijerph20053818
Gatford, K. L., Andraweera, P. H., Roberts, C. T., and Care, A. S. (2020). Animal models of preeclampsia causes, consequences, and interventions. Hypertension 75, 1363–1381. doi: 10.1161/HYPERTENSIONAHA.119.14598
Giurgescu, C., Sanguanklin, N., Engeland, C. G., White-Traut, R. C., Park, C., Mathews, H. L., et al. (2015). Relationships among psychosocial factors, biomarkers, preeclampsia, and preterm birth in African American women: a pilot. ANR. 28, e1–e6. doi: 10.1016/j.apnr.2014.09.002
Hang, Y., Zhihong, C., and Lijuan, Z. (2017). Mediating effect of self-efficacy on association between pregnancy pressure and antenatal depression. Military Nursing. 34, 21–24.
Heberlein, E. C., Picklesimer, A. H., Billings, D. L., Covington-Kolb, S., Farber, N., and Frongillo, E. A. (2016). The comparative effects of group prenatal care on psychosocial outcomes. Arch. Womens Ment. Health 19, 259–269. doi: 10.1007/s00737-015-0564-6
Ives, C. W., Sinkey, R., Rajapreyar, I., Tita, A. T. N., and Oparil, S. (2020). Preeclampsia-pathophysiology and clinical presentations JACC state-of-the-art review. J. Am. Coll. Cardiol. 76, 1690–1702. doi: 10.1016/j.jacc.2020.08.014
Jinzhi Li, F. T. (2011). Study of self-healthcare management level and influencing factors in pregnant women. Chin. J. Prev. Med. 45, 756–757.
Khazaeian, S., Khazaeian, S., and Fathnezhad-Kazemi, A. (2022). Association between awareness, perceived severity, and behavioral control of COVID -19 with self-Care and anxiety in pregnancy: a cross-sectional study. Women Health 62, 55–67. doi: 10.1080/03630242.2021.2014020
Krishnamurti, T., Davis, A. L., and Simhan, H. N. (2019). Worrying yourself sick? Association between pre-eclampsia onset and health-related worry in pregnancy. Pregn. Hypertension Int. J. Womens Cardiovascular Health. 18, 55–57. doi: 10.1016/j.preghy.2019.09.003
Kurki, T., Hiilesmaa, V., Raitasalo, R., Mattila, H., and Ylikorkala, O. (2000). Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet. Gynecol. 95, 487–490
László, K. D., Liu, X. Q., Svensson, T., Wikström, A. K., Li, J., Olsen, J., et al. (2013). Psychosocial stress related to the loss of a close relative the year before or during pregnancy and risk of preeclampsia. Hypertension 62, 183–189. doi: 10.1161/HYPERTENSIONAHA.111.00550
Lee, H., Kim, K. E., Kim, M. Y., Park, C. G., Han, J. Y., and Choi, E. J. (2021). Trajectories of depressive symptoms and anxiety during pregnancy and associations with pregnancy stress. Int. J. Environ. Res. Public Health 18:12. doi: 10.3390/ijerph18052733
Luyan Liu, J. L. (2009). Stresses in Primiparas and their husbands during pregnancy and its related factors. J. Nurs. Sci. 24, 39–41.
Maxson, P., and Miranda, M. L. (2011). Pregnancy intention, demographic differences, and psychosocial health. J. Womens Health. 20, 1215–1223. doi: 10.1089/jwh.2010.2379
Moulaei, K., Bahaadinbeigy, K., Ghaffaripour, Z., and Ghaemi, M. M. (2021). The design and evaluation of a Mobile based application to facilitate self-care for pregnant women with preeclampsia during COVID-19 prevalence. J. Biomed. Phys. Eng. 11, 551–560. doi: 10.31661/jbpe.v0i0.2103-1294
Mrayan, L., Cornish, F., Dhungana, N., and Parfitt, B. (2016). Transition to parenthood during the transition to modernity in Jordan: new parents' views on family and healthcare support systems. Appl. Nurs. Res. 32, 139–143. doi: 10.1016/j.apnr.2016.07.002
Na, O. Y., Jie, W., Jina, L., Ping, Y. E., and Jiayou, L. U. O. (2022). Relationship between pregnancy stress and anxiety and depression in early pregnancy. Chin. J. Clin. Psych. 30, 968–972.
Ngene, N. C., and Moodley, J. (2024). Preventing maternal morbidity and mortality from preeclampsia and eclampsia particularly in low- and middle-income countries. Best Pract. Res. Clin. Obstet. Gynaecol. 94:102473. doi: 10.1016/j.bpobgyn.2024.102473
Niela-Vilen, H., Ekholm, E., Sarhaddi, F., Azimi, I., Rahmani, A. M., Liljeberg, P., et al. (2023). Comparing prenatal and postpartum stress among women with previous adverse pregnancy outcomes and normal obstetric histories: a longitudinal cohort study. Sexual Rep. Healthcare Off. J.the Swedish Assoc. Midwives. 35:100820. doi: 10.1016/j.srhc.2023.100820
Öztürk, R., Herbell, K., Morton, J., and Bloom, T. (2021). "The worst time of my life": treatment-related stress and unmet needs of women living with infertility. J. Community Psychol. 49, 1121–1133. doi: 10.1002/jcop.22527
Phipps, E. A., Thadhani, R., Benzing, T., and Karumanchi, S. A. (2019). Pre-eclampsia: pathogenesis, novel diagnostics and therapies. Nat. Rev. Nephrol. 15, 275–289. doi: 10.1038/s41581-019-0119-6
Püschl, I. C., de Wolff, M. G., Broberg, L., Macklon, N., and Hegaard, H. K. (2023). Pregnant women's attitudes to and experiences with a smartphone-based self-test for prediction of pre-eclampsia: a qualitative descriptive study. BMJ Open 13:e065575. doi: 10.1136/bmjopen-2022-065575
Qi, W. J., Liu, Y., Lv, H. C., Ge, J., Meng, Y. C., Zhao, N., et al. (2022). Effects of family relationship and social support on the mental health of Chinese postpartum women. BMC Pregnancy Childbirth 22:10.
Rahnemaei, F. A., Fashami, M. A., Abdi, F., and Abbasi, M. (2020). Factors effective in the prevention of preeclampsia:a systematic review. Taiwan. J. Obstet. Gynecol. 59, 173–182. doi: 10.1016/j.tjog.2020.01.002
Rana, S., Lemoine, E., Granger, J. P., and Karumanchi, S. A. (2020). Preeclampsia: pathophysiology, challenges, and perspectives. Circ. Res. 126, E8–E. doi: 10.1161/CIRCRESAHA.118.313276
Rashidi, F., Ghahremani, F., Mahmoodi, Z., and Doulabi, M. A. (2025). The role of social determinants of health in woman's intention to pregnancy: a model with the mediation of social support. BMC Public Health 25:1062. doi: 10.1186/s12889-025-22223-3
Riem, M. M. E., Perrykkad, K., Watson, S. J., Wynter, K., Ijzendoorn, M. H. V., and Galbally, M. (2024). The role of lack of grandparental support in perinatal depression. J. Affect. Disord. 360, 198–205. doi: 10.1016/j.jad.2024.05.104
Shay, M., MacKinnon, A. L., Metcalfe, A., Giesbrecht, G., Campbell, T., Nerenberg, K., et al. (2020). Depressed mood and anxiety as risk factors for hypertensive disorders of pregnancy: a systematic review and meta-analysis. Psychol. Med. 50, 2128–2140. doi: 10.1017/S0033291720003062
Shuxiu, L. (2021). Research on child-rearing dilemma and its influence on fertility intention in the City Group of Yangtze River Delta region. Youth Expl. 3, 88–98.
Smith, C. A., Tuson, A., Thornton, C., and Dahlen, H. G. (2020). The safety and effectiveness of mind body interventions for women with pregnancy induced hypertension and or preeclampsia: a systematic review and meta-analysis. Complement. Ther. Med. 52:102469. doi: 10.1016/j.ctim.2020.102469
Tang, X., Lu, Z., Hu, D. H., and Zhong, X. N. (2019). Influencing factors for prenatal stress, anxiety and depression in early pregnancy among women in Chongqing, China. J. Affect Disord. 253, 292–302. doi: 10.1016/j.jad.2019.05.003
Traylor, C. S., Johnson, J. D., Kimmel, M. C., and Manuck, T. A. (2020). Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: an expert review. Amer. J. Obstet. Gynecol. MFM. 2:100229. doi: 10.1016/j.ajogmf.2020.100229
Tuxunnjiang, X. B. D., Wumaier, G. L. J. N. T., and Ting, J. (2022). The relationship between pregnancy stress and prenatal anxiety andsocial support in pregnant women. Modern. Prev. Med. 49, 2178–2183.
Varghese, R., and Roy, M. (2019). Coresidence with mother-in-law and maternal anemia in rural India. Soc. Sci. Med. 226, 37–46. doi: 10.1016/j.socscimed.2019.02.027
Vollebregt, K. C., van der Wal, M. F., Wolf, H., Vrijkotte, T. G. M., Boer, K., and Bonsel, G. J. (2008). Is psychosocial stress in first ongoing pregnancies associated with pre-eclampsia and gestational hypertension? Bjog-Int. J. Obstetrics Gynaecol. 115, 607–615. doi: 10.1111/j.1471-0528.2008.01665.x
Wang, Y. C., Gu, J., Zhang, F., and Xu, X. J. (2023). The mediating role of social support and resilience between self-efficacy and prenatal stress: a mediational analysis. BMC Pregnancy Childbirth 23:10. doi: 10.1186/s12884-023-06184-2
Xiao, Q. L., Jun, Y. C., and Hong, H. L. (2024). Investigation on the current status of standard pregnancy health Care and self-management behavior of rural women. Chin. Gen. Pract. 22, 1–7.
Xihong Zhou, L. L. (2011). Prenatal anxiety and its influence on delivery outcome. J. Central South Univ. 36, 803–808.
Xuehua Cao, L. M., Zhang, X., Qun, L. V., and Zhou, L. (2011). Stress and its causes of pregnant women undergoing assisted reproductive technology. Clin. Med. 8, 119–120.
Yao Tang, W. G., and Li, X. (2022). Interpretation of the 2021 ISSHP clinical guidelines for disorders of hypertension in pregnancy. Journal of practical. Obstet. Gynecol. 38, 832–838.
Yu, Y. X., Zhang, S. C., Wang, G. Y., Hong, X. M., Mallow, E. B., Walker, S. O., et al. (2013). The combined association of psychosocial stress and chronic hypertension with preeclampsia. Am. J. Obstet. Gynecol. 209:12. doi: 10.1016/j.ajog.2013.07.003
Zhou, Y., Huang, J. G., Baker, P. N., Liao, B. Z., and Yu, X. Y. (2022). The prevalence and associated factors of prenatal depression and anxiety in twin pregnancy: a cross-sectional study in Chongqing, China. BMC Pregnancy Childbirth 22:10. doi: 10.1186/s12884-022-05203-y
Keywords: preeclampsia, pregnancy stress, anxiety, depression, self-management capacity
Citation: Cong X, Wang J, Yang L, Cui L, Hua Y and Gong P (2025) Pregnancy stress in women at high risk of preeclampsia with their anxiety, depression, self-management capacity: a cross-sectional study. Front. Psychol. 16:1537858. doi: 10.3389/fpsyg.2025.1537858
Edited by:
Carmen María Galvez-Sánchez, University of Murcia, SpainReviewed by:
Quan Gan, Hubei Maternal and Child Health Hospital, ChinaSahbanathul Missiriya Jalal, King Faisal University, Saudi Arabia
Putri Karisa, Padjadjaran University, Indonesia
Mehmet Albayrak, Giresun University, Türkiye
Copyright © 2025 Cong, Wang, Yang, Cui, Hua and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yurong Hua, MTA5NjEyNTQ1QHFxLmNvbQ==; Ping Gong, MTA2MDcyOTE2NkBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Xing Cong
Xing Cong Jinmei Wang3†
Jinmei Wang3† Ping Gong
Ping Gong