- 1Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, United Kingdom
- 2Kent and Medway Medical School, University of Kent, Canterbury, United Kingdom
- 3Department of Brain Sciences, Imperial College London, London, United Kingdom
Introduction: Research has suggested that anxiety may be responsible for the elevated levels of psychotic-like experiences (PLEs) seen in Autism. However, there has been no previous systematic review examining this relationship.
Method: We conducted three separate searches of PubMed and Ovid (MEDLINE, PsycINFO, Global Health and EMBASE) until 31st June 2024 for articles reporting on the association between anxiety, Autism and PLEs. A total of 54 articles were reviewed, including research exploring the links between anxiety and PLEs (28 studies), Autism and PLEs (12 studies), Autism and anxiety (14 systematic reviews and meta-analyses).
Results: Studies of Anxiety and PLEs: Thirteen reported a significant positive correlation, and ten studies indicated that individuals with anxiety were more likely to experience PLEs. Studies of Autism and PLEs: Seven identified a significant positive correlation, with three longitudinal studies reporting that autistic traits predicted PLEs. Studies of Autism and Anxiety: Seven reviews revealed increased prevalence rates of anxiety disorders among autistic individuals, while 9 identified potential mediators of this relationship, such as intolerance of uncertainty and IQ.
Conclusions: These findings demonstrate the association of PLEs with Autism and anxiety disorders, suggesting that co-occurring Autism and anxiety may represent an at-risk group for psychosis. Such insights have important implications for psychosis prevention, indicating that anxiety intervention in autistic populations may reduce PLE incidence. However, application of these findings to autistic individuals is significantly limited by the lack of included studies utilizing clinical populations. Future research is needed to establish the causal role of anxiety in this relationship, particularly using clinical adult samples.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024555930.
1 Introduction
At the start of the 20th century, psychiatrist Eugen Bleuler considered autism to be a central feature of schizophrenia (Crespi, 2010). Following Leo Kanner's conceptualization of autism as a childhood disorder, Autistic Spectrum Disorder (ASD) was redefined as a distinct condition, despite sharing both neurodevelopmental and genetic factors with psychosis (Hajdúk et al., 2023). Subsequent theorists have therefore posited that Autism and psychosis sit on a continuum, forming part of a spectrum of major mental illnesses with overlapping symptoms (Craddock and Owen, 2010). There is also evidence to suggest that the two are diametrically opposed conditions: reciprocal copy number variant loci have been identified that may predispose individuals to either disorder depending on whether they are deleted or duplicated (Kirov et al., 2009). Alternatively, the causation model proposes that while Autism may increase vulnerability to developing psychosis, the two ultimately remain separate conditions (Esterberg et al., 2008). Although there are a number of conflicting theories intending to explain the relationship between Autism and psychosis, there appears to be consensus that the association is not simply by chance (Chisholm et al., 2015).
Understanding the relationship between Autism and psychosis is essential, as the co-occurring conditions are linked with poorer clinical outcomes, including increased rates of depression and suicide (Upthegrove et al., 2018; Hedley and Uljarević, 2018). Furthermore, autistic individuals are more likely to experience psychosis than the general population, with reported prevalence rates of up to 34% (Ribolsi et al., 2022; Arciniegas, 2015). The reason behind this elevated risk is not well understood, however one theory is that anxiety may mediate the pathway between Autism and psychosis (Demetriou et al., 2018). Previous research has highlighted the role of anxiety in the development and maintenance of psychosis among neurotypical populations, particularly in relation to positive symptoms (Freeman and Garety, 2003; Monsonet et al., 2022). For example, a longitudinal study found anxiety during adolescence to be predictive of psychosis at age 24 (Morales-Muñoz et al., 2022). Additionally, anxiety was reported to be associated with increased severity of hallucinations and delusions (Hartley et al., 2013). A recent meta-analysis identified that 29% of individuals with first-episode psychosis (FEP) experienced a co-occurring anxiety disorder (Wilson et al., 2020). This notable relationship may reflect the similar cognitive processes involved in the two conditions, such as persecutory thoughts and anticipating threat, which may increase vulnerability to developing psychosis when experiencing significant anxiety (Freeman, 2007). This is especially important as previous research has consistently reported high rates of anxiety disorders within autistic populations, ranging from 20 to 82% (Skokauskas and Gallagher, 2009; Hollocks et al., 2019; Bougeard et al., 2021). Moreover, co-occurring Autism and anxiety has been linked with poorer social relationships and increased likelihood of bullying, which are further risk factors for psychosis (Ambrose et al., 2021; Maiano et al., 2016). Notably, a recent study reported that 51.4% of participants with first-episode psychosis had experienced bullying during their lifetime (Kosteletos et al., 2024). This highlights the importance of considering environmental stressors, such as traumatic experiences, when discussing elevated rates of psychosis in Autism (Sætren et al., 2024).
One way of gaining insight into the relationship between Autism and psychosis may be through exploring psychotic-like experiences (PLEs), referring to transient or brief disturbances that resemble symptoms of psychosis, experienced among the general population (Hinterbuchinger and Mossaheb, 2021). PLEs are associated with later development of psychosis, and are particularly useful to study due to their prevalence among the general population, enabling larger sample sizes than research involving individuals with a psychosis diagnosis (Yung et al., 2006). Applied instruments such as the Community Assessment of Psychic Experiences (CAPE) conceptualize PLEs as the experience of psychosis symptoms without the presence of a disorder, often reflecting lower frequency or distress (Stefanis et al., 2002). In contrast, the DSM-5 emphasizes that the symptoms of schizophrenia must be persistent and associated with marked functional impairment (Rahman and Lauriello, 2016; American Psychiatric Association, 2022). A systematic review and meta-analysis conducted by Kiyono et al. (2020) reported that PLE prevalence among autistic individuals ranged from 6 to 45%, depending on the subtype, which is significantly higher than rates seen in the general population. Similarly, research has indicated that anxiety symptoms may be associated with increased rates of PLEs, with common mechanisms such as hypothalamic-pituitary-adrenal (HPA) axis dysregulation linking the two conditions (Yamasaki et al., 2018). Despite this, there are no known previous systematic reviews exploring the relationship between Autism, anxiety and PLEs.
Furthermore, research into this field faces several challenges. Firstly, the wide variety of diagnostic criteria used for both Autism and PLEs has resulted in incredibly heterogeneous findings within the literature, making comparison difficult (Kiyono et al., 2020). Additionally, several measures of anxiety and PLEs have not yet been validated within autistic populations, casting doubt on the validity of the conclusions drawn as they may not accurately capture these constructs in Autism (Mingins et al., 2021). While this issue does not apply to research measuring autistic traits in non-clinical populations, the application of these findings to individuals with an Autism diagnosis must be considered as a further challenge (Lisøy et al., 2022b). Regardless of these limitations, understanding the relationship between Autism, anxiety and PLEs has the potential to improve our understanding of vulnerability to psychosis (Catone et al., 2017). Exploring this could contribute to better clinical outcomes and more targeted interventions for both autistic individuals and the broader population (Yung et al., 2006). For instance, screening for anxiety symptoms among autistic individuals, or for autistic traits among individuals with an anxiety disorder, could allow for the early identification of individuals at risk of psychosis. Moreover, PLEs are not only indicative of psychosis but also of a wide range of mental health conditions (Kiyono et al., 2020). Consequently, exploring potential explanations for their prevalence is essential.
This review will examine the individual associations between Autism, anxiety and PLEs, to seek insight into the relationship between all three variables, which represents a current gap in the literature. In order to understand the increased prevalence of PLEs among autistic individuals, this review endeavors to explore whether anxiety increases vulnerability to PLEs among autistic individuals. Due to the current paucity of research on this topic, three individual searches combining the three variables will be conducted to address the research question.
2 Method
This review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021). Prior to conducting our search, a review protocol was developed and registered on PROSPERO (registration number: CRD42024555930).
2.1 Literature search
Three separate searches were conducted to thoroughly address the research question: (1) Anxiety and PLEs, (2) Autism and PLEs, and (3) Autism and Anxiety. Multi-component reviews such as our current study have been described previously in response to complex research questions (Gough et al., 2012). Searches were conducted using the databases PubMed and Ovid (MEDLINE, PsycINFO, Global Health and EMBASE), from inception until 30th June 2024. Therefore, the timeframe of our searches extends beyond previous reviews conducted by Kiyono et al. (2020) and Hollocks et al. (2019). The search terms used were: (Anxiety OR Anxiety Disorder OR Generalized anxiety disorder OR Social anxiety disorder OR Panic disorder OR Phobia) AND (Psychotic-like experience* OR Psychotic like experience* OR PLE); (Autism OR Autism spectrum condition OR Autism spectrum disorder OR ASD OR Asperger's syndrome) AND (Psychotic-like experience* OR Psychotic like experience* OR PLE). Furthermore, as Autism and anxiety is a well-researched area we conducted an additional search restricted to previous systematic reviews and meta-analyses, using the terms: (Anxiety OR Anxiety Disorder OR Generalized anxiety disorder OR Social anxiety disorder OR Panic disorder OR Phobia) AND (Autism OR Autism spectrum condition OR Autism spectrum disorder OR ASD OR Asperger's syndrome).
2.2 Study selection
After removing duplicates, the titles and abstracts of potentially relevant studies were screened by one author against the inclusion and exclusion criteria, before being confirmed by an independent rater. For searches 1 and 2, the inclusion criteria were: (1) observational studies, including cohort, cross-sectional and case control studies, (2) reporting findings on the relationship between either Autism and PLEs or Anxiety and PLEs, and (3) published in English. Additionally, there were no restrictions on age or gender, and a formal diagnosis of Autism or an anxiety disorder was not required. The exclusion criteria were the following: (1) studies evaluating interventions or treatments for Autism, anxiety, or psychosis without relevant data on the relationship between these conditions, (2) studies with insufficient data or incomplete reporting that prevents assessment of the relationship between Autism, anxiety, and PLEs, and (3) studies involving subpopulations not relevant to the research question, such as family members. For search 3, the inclusion criteria were: (1) systematic reviews and meta-analyses, (2) reporting findings on the relationship between Autism and Anxiety, and (3) published in English. The exclusion criteria were: (1) reviews evaluating interventions or treatments for Autism or anxiety without relevant data on the relationship between these conditions, and (2) reviews involving subpopulations not relevant to the research question.
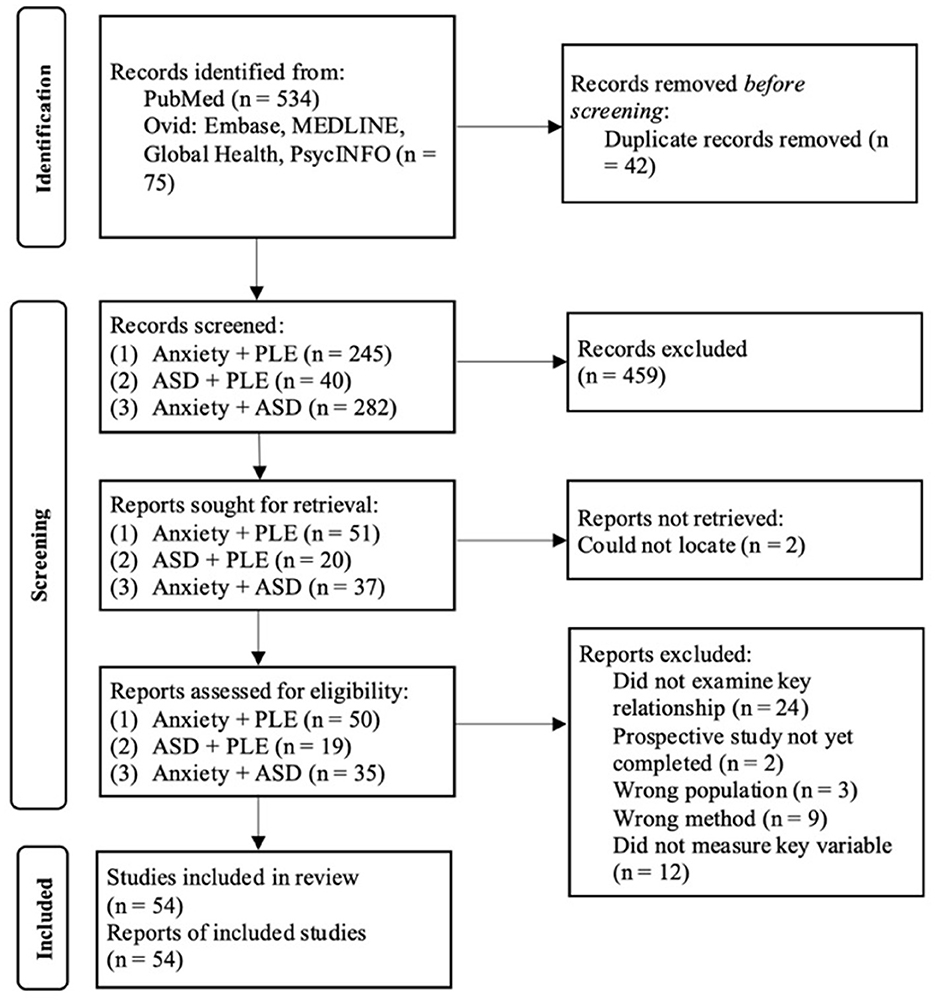
Studies that appeared to be eligible were retrieved for full-text assessment, conducted by one author and confirmed by an independent rater. Any uncertainty regarding study eligibility was resolved through discussion with a second author (see Supplementary material 1). Our initial search retrieved a total of 609 articles with 567 remaining after duplicates were removed. After titles and abstracts were screened, 459 articles were excluded leaving 108 for full-text evaluation. Following full-text evaluation, 54 articles met criteria for inclusion in this review. Articles were excluded for the following reasons: (1) they did not examine the relationship between the two key variables, (2) they involved the wrong population, (3) they used the wrong method, (4) they did not measure the key variable, (5) there was no full-text available and (6) it was a prospective study that had not yet been completed. The study selection process is summarized in the PRISMA flow diagram (see Figure 1).
2.3 Data extraction and quality assessment
The following variables of interest were extracted from the selected studies: author, year of study, study design, exclusion criteria, scales used (to measure anxiety, autistic traits or PLEs), and findings. Findings included means, standard deviations, effect sizes, p-values and correlation coefficients, where these measures were reported by the included studies. Microsoft Excel was used to create a data collection table and extraction was completed manually by one author. Quality of the included studies was assessed using the relevant Critical Appraisal Skills Programme (CASP) checklist. The CASP tool was selected as it provides checklists for both original research and previous systematic reviews and meta-analysis, allowing for a standardized assessment of quality to be used throughout (Ma et al., 2020). Studies were considered low quality if any of the first three questions were answered negatively, in accordance with previous guidance (Long et al., 2020).
2.4 Data synthesis and analysis
Due to the heterogeneity in study design and measures used among the included studies, a meta-analysis was not possible. Therefore, a narrative synthesis was conducted to address the research question.
3 Results
3.1 Study characteristics
3.1.1 Anxiety and psychotic-like experiences
This search included a total of 28 studies published between 2011 and 2024. The studies were conducted across various settings: 22 were carried out in Western countries (USA, UK, Australia, France), while seven were conducted in non-Western countries (China, Japan, Turkey). The majority of the included studies utilized student populations and community samples, with a variety of methods including online surveys and in-person assessments. Many samples were drawn from non-clinical populations (n = 20), while eight involved clinical populations with diagnoses such as anxiety disorders, mood disorders, schizophrenia and psychosis. Most (n = 23) studies employed a cross-sectional design, while five studies utilized a longitudinal design with follow-up periods ranging from 3 to 21 years. One study combined both cross-sectional and longitudinal methodologies. The total sample size across the included studies was 127,564, with individual sample sizes ranging from 57 to 34,653. The average sample size across the studies was approximately 4,500 participants. Participants' age ranged from 9 to 73 years old (average age = 25), as the included studies involved both child and adult populations. Gender distribution was reported in 25 studies, with a general trend toward a higher proportion of females. Specifically, 15 studies had a majority female sample, while eight had a majority male sample. Two studies had an equal number of males and females.
A variety of validated instruments were used to assess anxiety and PLEs across the included studies. Anxiety was frequently measured using the State-Trait Anxiety Inventory (STAI) and the Beck Anxiety Inventory (BAI) in adult student and community samples, whereas child and adolescent populations utilized age-appropriate tools such as the Spence Children's Anxiety Scale (SCAS) and the Development and Well-Being Assessment (DAWBA). The Generalized Anxiety Disorder-7 (GAD-7) and Depression Anxiety Stress Scales (DASS) were also used in general population samples, particularly in online survey-based studies. In clinical samples or national epidemiological studies, structured diagnostic tools such as the Composite International Diagnostic Interview (CIDI) and Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV (AUDADIS-IV) were employed, providing more rigorous diagnostic classification compared to self-report questionnaires.
PLEs were assessed using a similarly broad set of measures, with some variation depending on sample characteristics. The Community Assessment of Psychic Experiences (CAPE) was often used in student and community samples, reflecting its design to capture subclinical psychotic symptoms. The Prodromal Questionnaire (PQ) and Comprehensive Assessment of At-Risk Mental States (CAARMS) were more frequently used in studies involving clinical samples. In non-clinical samples, trait-like schizotypy were often assessed using instruments such as the Schizotypal Personality Questionnaire (SPQ), the Oxford-Liverpool Inventory of Feelings and Experiences (O-LIFE), and the Launay–Slade Hallucination Scale (LSHS). This variation in measurement tools across the included studies introduces notable heterogeneity; however, it also reflects appropriate methodological tailoring to the sample type.
3.1.2 Autism and psychotic-like experiences
This search included 12 studies published between 2011 and 2024. The majority were conducted in a Western setting (USA, UK, Norway, Holland), with only two studies carried out in non-Western countries (Kenya, Hong Kong). Nine of the included studies used a cross-sectional design, two of which were case-control studies. Three were longitudinal studies, with follow-up periods ranging from 10 to 17 years. Most studies used stratified sampling methods within non-clinical populations, however those involving participants with an Autism diagnosis were recruited through local mental health services. Four studies utilized clinical populations. Of these, two involved participants with an Autism diagnosis, one included autistic individuals and individuals with an ADHD diagnosis, and the final study assessed autistic traits in participants with psychosis. Sample sizes across the studies ranged from 52 to 14,853 participants, with an average sample size of approximately 4,299 participants. Most studies focused on autistic traits in non-clinical populations, with only three involving individuals with an Autism diagnosis. Participants' ages ranged from 9 to 41 years (average age = 24). Of the included studies, 11 reported gender distribution, with seven having a majority female sample.
Autistic traits were measured in non-clinical populations using the following self-report measures: Autism Quotient (AQ), Social Communication Disorder Checklist (SCDC), Autism Symptom SElf-ReporT for Adolescents and Adults (ASSERT) and the Comprehensive Autistic Trait Inventory. Three studies involving clinical populations used the AQ, while the fourth did not include a trait measure and relied solely on a confirmed Autism diagnosis, reflecting a more categorical approach. PLEs were assessed using a range of instruments, including the CAPE, SPQ, PQ, Psychosis-Like Symptoms interview (PLIKSi), Washington Early Recognition Center Affectivity and Psychosis (pWERCAP) and the Psychosis Screening Questionnaire (PSQ). The Diagnostic Interview for Children (DISC-C) was utilized in one study involving younger participants (mean age = 12.6).
3.1.3 Autism and anxiety
The final search included 14 systematic reviews and meta-analyses, published between 2011 and 2023. Specifically, six systematic reviews, four meta-analyses and four systematic reviews with meta-analyses. The number of studies included in each review ranged from 5 to 340. Moreover, the number of databases searched ranged from two to five, most commonly using PubMed, PsycINFO and Embase. Of the 14 reviews, 13 included populations with a primary Autism diagnosis and one involved individuals with a primary diagnosis of an anxiety disorder. Additionally, 10 reviews focused on children and adolescents, while four involved studies with adult participants. Three of the included reviews did not report conducting a quality assessment.
3.2 Quality assessment
The CASP checklists were used to assess methodological quality across studies. CASP assessment does not generate a cumulative score; instead, it provides a structured appraisal of key domains such as study design, bias and validity. This approach supports a nuanced evaluation of research strengths and limitations without oversimplifying quality into a numerical rating (Ma et al., 2020).
3.2.1 Cross-sectional studies
Across the included cross-sectional studies, the majority were of moderate to high quality, with consistent reporting of clear aims and appropriate methodology. However, attention to confounding factors and clarity in effect estimation were variable, which may affect the strength of some conclusions. See Supplementary Table 1 for full CASP assessment of cross-sectional studies.
3.2.2 Longitudinal studies
The included longitudinal studies were generally of high methodological quality. Most met all CASP criteria, with clear aims, robust measurement of exposures and outcomes, and well-described follow-up periods. Several studies fulfilled all or nearly all criteria, enhancing confidence in their findings. However, others demonstrated limitations in areas such as accounting for confounding factors or had incomplete follow-up which may impact the reliability of certain results. See Supplementary Table 2 for full CASP assessment of longitudinal studies.
3.2.3 Systematic reviews
The included systematic reviews varied in methodological quality. Most had clearly defined aims, appropriate search strategies, and included relevant studies. However, several reviews showed limitations in critical areas such as quality assessment of included studies and reporting of cost-benefit considerations. While certain reviews demonstrated high methodological rigor across all criteria, others lacked transparency in combining results or assessing the validity of findings. These variations in quality suggest that conclusions drawn from the systematic reviews should be interpreted with caution, particularly when based on those with less thorough appraisal or reporting. See Supplementary Table 3 for full CASP assessment of systematic reviews.
3.2.4 Systematic review and meta-analyses
All included systematic reviews with meta-analyses were of consistently high methodological quality. Each met the CASP criteria for clear focus, rigorous search strategies, inclusion of relevant studies, and thorough appraisal of validity and limitations. Notable reviews demonstrated comprehensive and transparent reporting, appropriate data synthesis, and thoughtful discussion of applicability and added value. The consistent strength of these reviews enhances confidence in the findings they report and their contribution to the overall synthesis. See Supplementary Table 4 for full CASP assessment of systematic review and meta-analyses.
3.3 Anxiety and psychotic-like experiences
From the total 54 studies, 28 reported findings on the relationship between anxiety and PLEs. Their characteristics and key findings are displayed in Table 1. Among these, 13 reported a significant positive correlation between anxiety and PLE scores. Ten studies reported odds ratios indicating that individuals with anxiety were more likely to experience PLEs. Conversely, three studies reported odds ratios suggesting that individuals experiencing PLEs were more likely to have an anxiety disorder. All five longitudinal studies reported that anxiety predicted PLEs at follow-up, or that PLEs predicted an anxiety disorder at follow-up. Four of the included studies explored potential mediators or factors involved in the relationship, including intolerance of uncertainty (IU) and other cognitive biases. Finally, five studies reported findings on specific anxiety disorders and PLEs, in addition to obsessive-compulsive disorder (OCD).
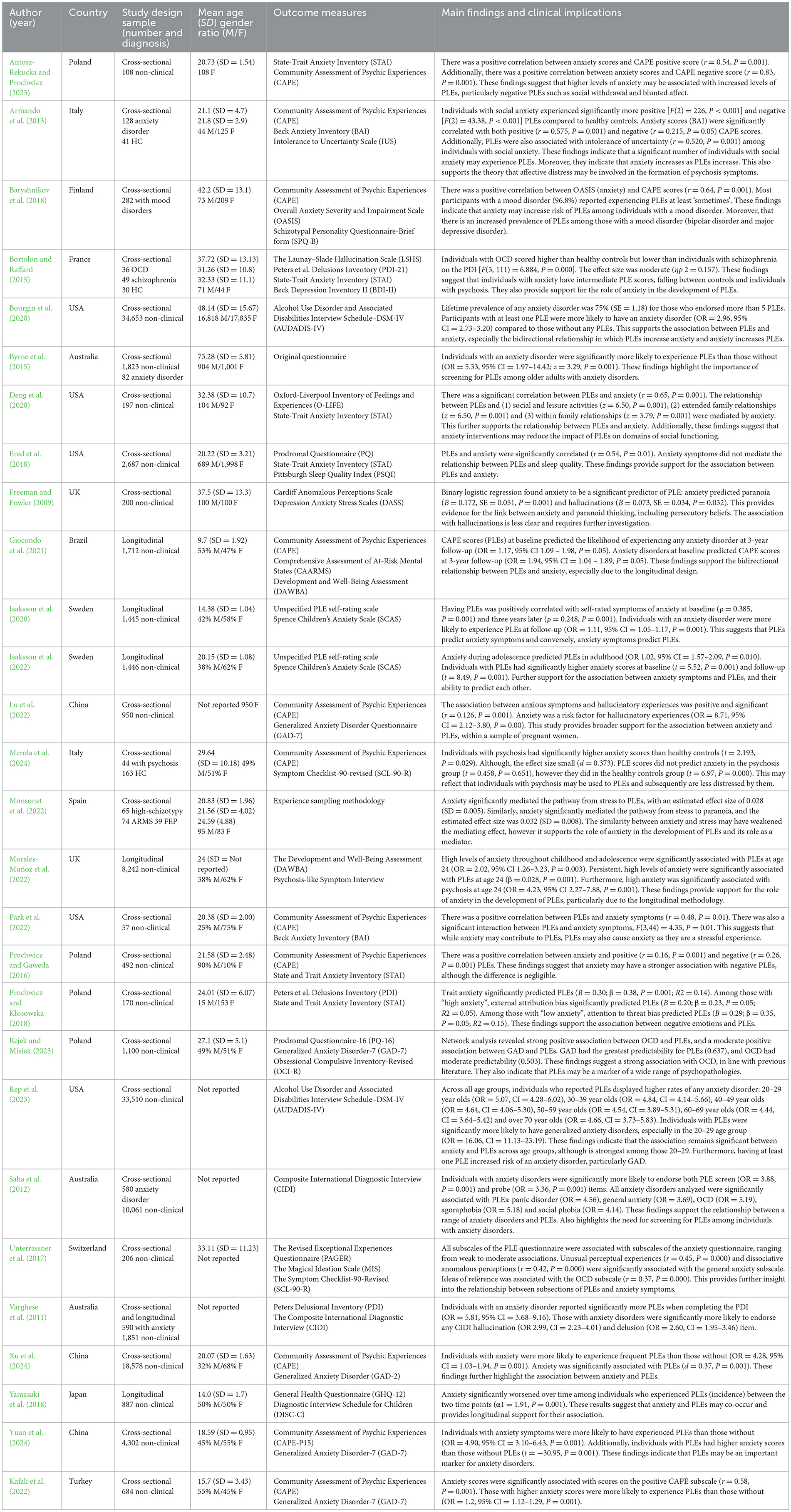
Table 1. Anxiety and psychotic-like experiences: characteristics and findings of studies meeting inclusion criteria (n = 28).
3.4 Autism and psychotic-like experiences
There were 12 studies examining the relationship between Autism and PLEs. Their characteristics and findings are presented in Table 2. From the total studies, seven reported a positive and significant correlation between autistic traits and PLE scores. In contrast, two studies reported that the association between autistic traits and PLE scores was positive but not significant. Three studies reported odds ratios indicating that individuals with higher autistic traits were more likely to experience PLEs. All three longitudinal studies reported that autistic traits significantly predicted PLEs. Similarly, all three studies involving individuals with a diagnosis of Autism reported that they were more likely to experience PLEs than those without. Six studies examined potential mediators and other relevant factors, including childhood trauma, social cognition and mentalizing biases. Importantly, two studies did not find a significant association between autistic traits and PLE scores.
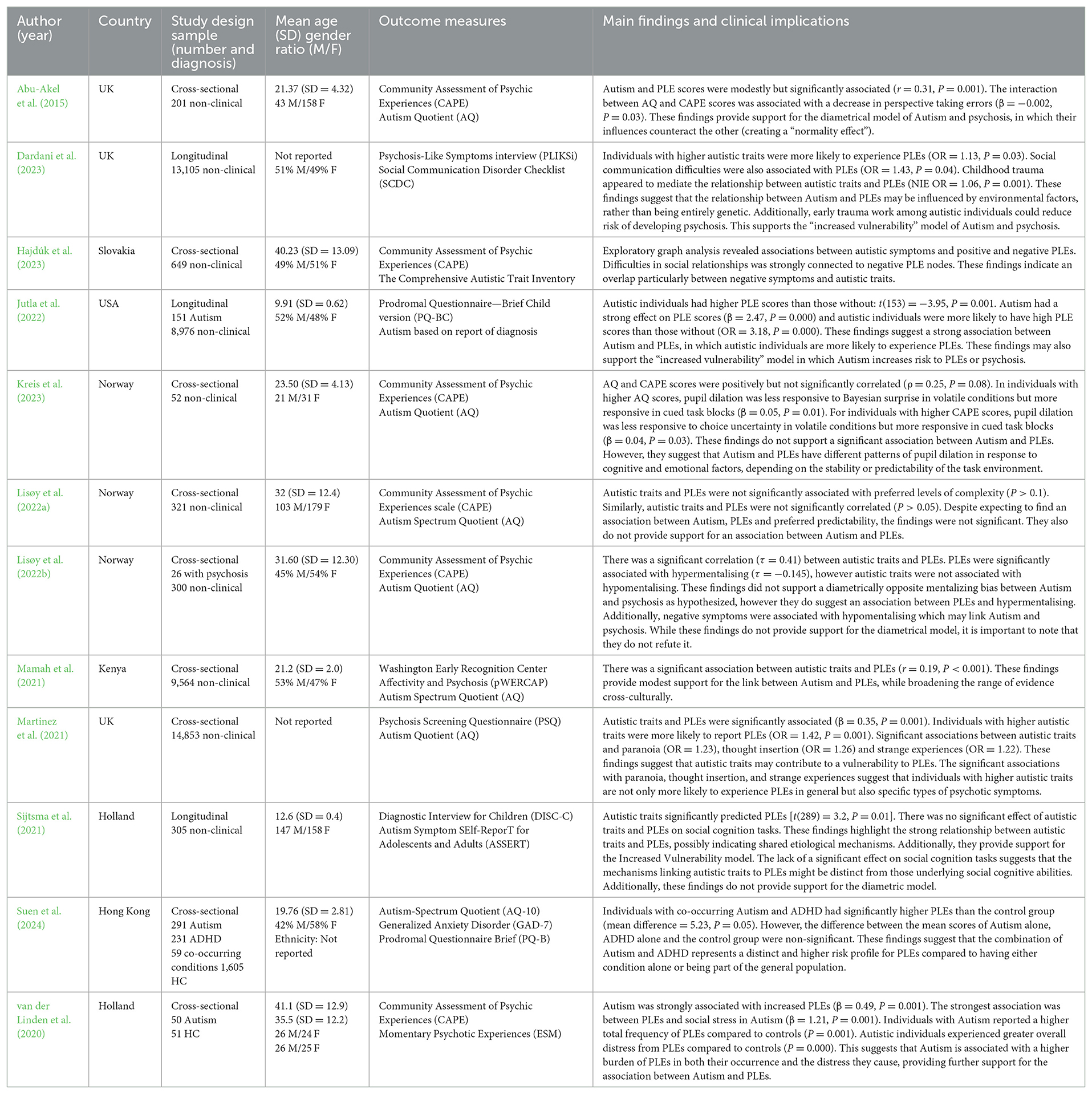
Table 2. Autism and psychotic-like experiences: characteristics and findings of studies meeting inclusion criteria (n = 12).
3.5 Autism and anxiety
There were 14 systematic reviews and meta-analyses exploring the relationship between Autism and anxiety. Their characteristics and findings are presented in Table 3. Of the included reviews, seven reported prevalence rates of anxiety disorders among individuals with an Autism diagnosis, with heterogeneous estimates possibly reflecting the varied populations including differences in age and IQ. Nine studies examined potential mediators and important factors involved in the relationship, including IU and sensory over-reactivity (SOR). Additionally, four of these reviews explored the relationship between IQ and anxiety in autistic individuals, with three concluding that higher IQ was associated with increased anxiety.
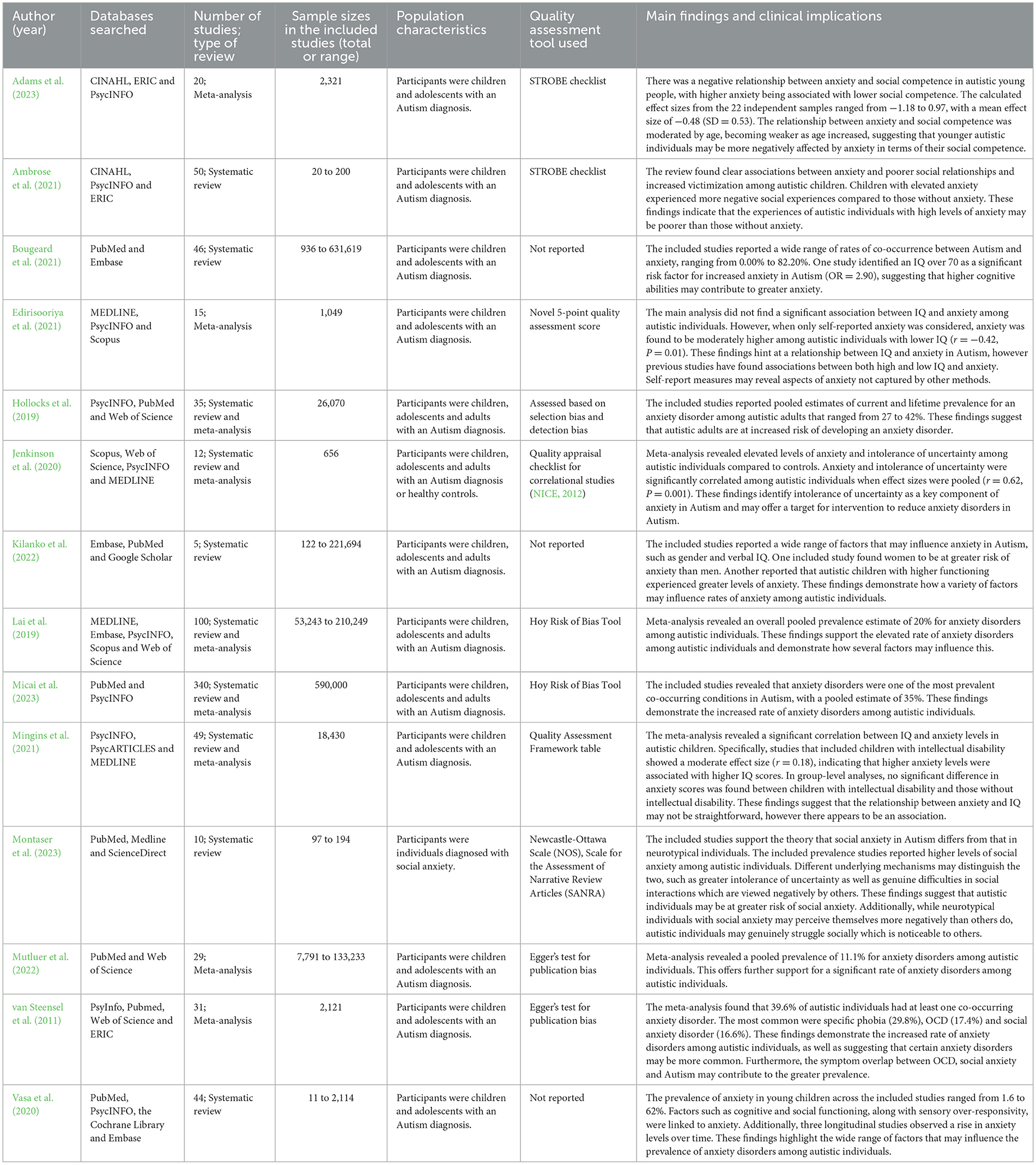
Table 3. Anxiety and autism: characteristics and findings of reviews meeting inclusion criteria (n = 14).
4 Discussion
This systematic review aimed to synthesize the literature examining whether anxiety increases vulnerability to PLEs in autistic individuals. Due to the lack of research directly exploring this topic, three separate searches were conducted to address the research question. Higher levels of anxiety were associated with increased frequency of PLEs, and there was evidence supporting a bidirectional relationship between the two. Additionally, autistic traits were linked to higher rates of PLEs, and autistic individuals were more likely to experience PLEs compared to healthy controls. Finally, an Autism diagnosis was consistently associated with increased rates of anxiety disorders.
4.1 Anxiety and psychotic-like experiences
A consistent finding of the current review was the association between anxiety scores and increased rates of PLEs within nonclinical populations, indicating that in individuals without a known Autism diagnosis, higher anxiety levels correlated with more frequent PLEs. There appears to be only one previous systematic review on this topic, focused on children and adolescents, which similarly reported evidence of a strong relationship between anxiety and PLEs that highlights the causal role of affective distress in the development of psychotic symptoms (Bird et al., 2018). Notably, the review reported that the strongest association was between anxiety and paranoia, a finding echoed by one of the studies included in the current review. These observations align with the theoretical model proposed by Freeman (2007), which posits that anxiety is central to the development of delusions and paranoid ideas. The model is supported by prior research linking anxiety, paranoia and persecutory beliefs suggesting that anxiety may create a state of heightened threat perception which increases vulnerability to misinterpreting anomalous experiences in the form of PLEs (Huppert and Smith, 2005; Wigman et al., 2012).
Another key finding was longitudinal evidence for a bidirectional relationship between anxiety and PLEs, where each increases the likelihood of developing the other. This is consistent with previous research highlighting the distress and anxiety caused by experiencing PLEs, suggesting a cyclical relationship in which anxiety and PLEs reinforce each other (Brett et al., 2014; Armando et al., 2010). Interestingly, the predictive link between anxiety and PLEs may reflect shared vulnerabilities, as research has identified common underlying neurobiological mechanisms in both conditions (Varghese et al., 2011). For instance, HPA dysregulation is consistently implicated in the relationship between anxiety and psychotic symptoms, with preliminary research suggesting a similar association with PLEs (Phillips et al., 2006; Walker et al., 2008). In addition, reduced cortical thickness in the temporal lobe has been linked with each condition, suggesting that structural brain abnormalities could underlie the susceptibility to both anxiety and PLEs (Vargas and Mittal, 2023; Zink et al., 2008). These findings emphasize the neurobiological similarities between PLEs and anxiety disorders, offering insight into their relationship when considered separately from Autism.
Furthermore, there is evidence to suggest that anxiety and PLEs may share similar underlying cognitive mechanisms. One example is the cognitive bias “jumping to conclusions”, in which individuals make hasty decisions based on limited evidence (So et al., 2008; Dudley et al., 2016). This bias is thought to mediate the pathway between anxiety and paranoia, as anxious individuals may be more prone to making quick, unfounded judgments that can lead to paranoid thinking (Lincoln et al., 2010). Similarly, one study in the current review reported that “external attribution” bias significantly predicted PLEs among participants with high anxiety (Prochwicz and Kłosowska, 2018). This reasoning bias is often implicated in the development of delusions, and therefore may reflect another important mechanism linking anxiety and PLEs (Janssen et al., 2006). Further research establishing the role of cognitive processes in this relationship could allow for the development of interventions addressing these faulty cognitions.
4.2 Autism and psychotic-like experiences
Autistic traits were consistently associated with increased frequency of PLEs in this review: five of the included studies reported significant associations within nonclinical samples, while two compared autistic participants to healthy controls. These findings are consistent with the only previous systematic review examining the topic, which similarly reported an increased rate of PLEs among autistic individuals (Kiyono et al., 2020). However, it is important to note that two studies in the current review did not find a significant association between the two variables. This may be explained in two ways: firstly, Kreis et al. (2023) only included 52 participants in their study, which may have been inadequate to detect a meaningful effect. Since both Autism and psychosis occur in approximately 1% of the population, research involving less than 100 participants may lack the statistical power to detect significant associations (Chisholm et al., 2015). Although the second study involved a suitable number of participants (n = 321), the heterogeneity in definitions and outcome measures used for both PLEs and autistic traits may account for these conflicting findings.
Within the wider literature, Autism is most frequently associated with the negative symptoms of psychosis, such as social withdrawal and flat affect (Trevisan et al., 2020). Central features of Autism, such as deficits in theory of mind and face processing, have been recognized in individuals with psychosis and may be linked with the development of negative symptoms (Catalan et al., 2018; Darke et al., 2021). This is a key distinction between Autism and anxiety, which is more often associated with positive symptoms, such as hallucinations and delusions (Huppert and Smith, 2005). However, the current review similarly found stronger evidence linking autistic traits with positive PLEs, contrasting broader psychosis research. Perhaps this may reflect subtle differences between PLEs and psychosis, or more likely, it could be due to several included studies focusing solely on the positive subscale of the CAPE questionnaire. While positive PLEs are more directly linked to the risk of developing psychosis, future research should explore the association between negative PLEs and Autism to determine whether it mirrors the established relationship between Autism and the negative symptoms of psychosis (Cowan and Mittal, 2021).
Drawing on theoretical models, IU is frequently identified as a causative factor in both conditions (Lisøy et al., 2022b). Interestingly, a recent study hypothesized that cognitive disturbances such as IU, combined with affective distress such as anxiety, may result in a faulty appraisal process which leads to the development of PLEs (Armando, 2023). This difficulty in coping with ambiguous situations may therefore link anxiety, Autism and PLEs. In addition, one study included in the current review found evidence of diminished pupil responses in both participants with higher autistic traits and those experiencing frequent PLEs. This finding supports previous research that identified aberrant norepinephrinergic signaling, indicated by diminished pupil response, as a shared mechanism underlying both Autism and psychosis (Thakkar et al., 2018; Zhao et al., 2022). Norepinephrinergic signaling plays a crucial role in stress response, and abnormalities in this system may contribute to IU in both conditions and subsequently the development of PLEs (Lawson et al., 2017; Kreis et al., 2023, 2022).
Furthermore, while anxiety and PLEs may share similar cognitive styles, research indicates that those characterizing Autism and PLEs may differ (Fernandes et al., 2018). Three of the studies included in the current review explored the cognitive processes involved in this relationship, and similarly identified important distinctions (Abu-Akel et al., 2015; Lisøy et al., 2022a; Sijtsma et al., 2021). Autistic traits and PLEs were found to counterbalance each other on a number of perspective-taking tasks, suggesting that the presence of higher autistic traits might have an attenuating effect on the cognitive errors associated with psychosis proneness (Abu-Akel et al., 2015). This aligns with previous literature asserting that cognitions in Autism may be more deliberate and methodical than the “jumping to conclusions” cognitive style often seen in anxiety and psychosis (Brosnan et al., 2014). In addition, PLEs were significantly associated with hypermentalizing, which highlights another potential cognitive mechanism involved in their development (Lisøy et al., 2022a). While the study did not find a contrasting link between autistic traits and hypomentalizing as anticipated, this may reflect the study's focus on subclinical autistic traits rather than individuals with an Autism diagnosis, who may display more pronounced impairments in mentalization (Chung et al., 2014).
Moreover, anxiety may influence the relationship between Autism and PLEs through the increased levels of distress experienced by autistic individuals in response to PLEs: one of the included studies reported that autistic individuals experienced heightened anxiety in reaction to PLEs, which served to increase both the frequency and the distress associated with these experiences (van der Linden et al., 2020). In addition, two studies highlighted the influence of shared environmental factors in explaining the relationship between Autism and PLEs. Experiences such as bullying and victimization, to which autistic individuals may be more vulnerable, may increase the risk of developing psychotic symptoms later in life (Sijtsma et al., 2021; Bortoletto et al., 2023). Similarly, childhood trauma was identified as a potential mediator in the relationship, offering further support for the role of environmental factors in the increased rates of PLEs seen in Autism (Dardani et al., 2023). Since the aforementioned environmental factors are commonly associated with high levels of stress and anxiety (Gong et al., 2022), these findings may also provide indirect evidence for the causal role of anxiety in PLEs in Autism.
Additionally, previous research has identified substantial neurobiological and genetic overlap between Autism and psychosis, which may elucidate the association between autistic traits and PLEs (de Lacy and King, 2013). A consistent finding is that Autism and psychosis appear to share similar white matter deficits, whilst displaying diametrically opposite patterns of gray matter volumetry (Mitelman et al., 2017). Specifically, Autism has been linked with increased gray matter volume, while reduced gray matter volume has been identified in psychosis (Mitelman et al., 2018). This may reflect the complex association between Autism and psychosis, in which similarities, such as difficulties in social interaction and flat affect, are juxtaposed by marked differences, including how sensory information is processed (Barlati et al., 2016). Furthermore, research has identified higher levels of oxidative biomarkers in both conditions that may be involved in the etiology of Autism and PLEs (Smaga et al., 2015). These findings, considered alongside evidence of shared environmental influences, indicate that stress and inflammation may be an important therapeutic target for preventing PLEs in autistic populations.
4.3 Autism and anxiety
Seven reviews found increased rates of anxiety disorders among autistic individuals, with pooled prevalence estimates ranging from 11 to 40% (Mutluer et al., 2022; van Steensel et al., 2011). Moreover, individual study estimates reported prevalence rates of as high as 80% (Salazar et al., 2015). These findings align with a previous umbrella review exploring common co-occurring conditions in Autism, which similarly found increased levels of anxiety in autistic individuals across the spectrum (Hossain et al., 2020). However, it is important to acknowledge the significant variability in the reported prevalence estimates, as this may introduce uncertainty when attempting to draw definitive conclusions. The discrepant findings of the included reviews likely reflect the heterogeneity of the participants involved, such as vast differences in age and ability, as well as the wide variety of methodologies used (Hobson and Petty, 2021). Nevertheless, the overall trend across the included reviews indicates a strong association between anxiety and Autism.
In addition, several of the included reviews examined potential factors involved in the relationship between anxiety and Autism. One meta-analysis reported a strong correlation between IU and anxiety among autistic participants (Jenkinson et al., 2020). This provides important support for the role of IU in the relationship between anxiety, Autism and PLEs, suggesting that heightened threat perception may be an important factor linking the three variables (South and Rodgers, 2017). Similarly, SOR was identified in one of the included reviews as a relevant mechanism involved in anxiety in Autism (Vasa et al., 2020). While SOR is not frequently associated with PLEs or psychosis, previous research has identified abnormalities in electrodermal response in both Autism and schizophrenia (Reynolds and Lane, 2008). This suggests that both autistic individuals and those with schizophrenia may have atypical ways of processing sensory information. In Autism, this may manifest as SOR, leading to heightened anxiety (Lydon et al., 2016); in schizophrenia, similar sensory processing issues may contribute to the sensory distortions or hallucinations that are characteristic of psychosis (Dawson and Schell, 2002).
Furthermore, three of the included reviews reported that higher IQ was associated with increased anxiety (Bougeard et al., 2021; Kilanko et al., 2022; Mingins et al., 2021), while one identified an association between lower IQ and anxiety (Edirisooriya et al., 2021). High IQ may be associated with a greater ability for abstract thinking and advanced cognitive processing, which would allow for greater worrying and internalization (Mingins et al., 2021). Conversely, individuals with lower IQ may be unable to develop coping strategies when dealing with unfamiliar situations, leading to increased levels of stress and anxiety (Edirisooriya et al., 2021). This may have important implications when considering the wider relationship between anxiety, Autism and PLEs, as it could highlight certain groups that are at greater risk of psychosis. Premorbid IQ deficits have been identified in individuals with schizophrenia, therefore exploring the role of IQ in PLEs and Autism may be a potential avenue for future research (Rajji et al., 2009).
4.4 Anxiety, autism, and psychotic-like experiences
Despite the lack of literature examining anxiety, Autism and PLEs, there is some research on anxiety disorders, Autism and psychosis, which can be used to further contextualize the findings of the current review. Studies conducted within adult populations often juxtapose individuals with social anxiety disorder (SAD), Autism and psychosis, as they are three prominent conditions characterized by social deficits (Chan et al., 2019; Pepper et al., 2019; Demetriou et al., 2020; Pepper et al., 2018). While this provides evidence of similarities in social functioning, it offers little perspective on the causal relationship between the three variables. Greater insight may instead be gained from previous research conducted among children: Kyriakopoulos et al. (2015) examined anxiety in 84 autistic children admitted to a specialist inpatient unit, finding that anxiety symptoms mediated the pathway between Autism and psychotic symptoms within this sample. Formal thought disorder, a syndrome associated with psychotic disorders, was highlighted as an important aspect that may be induced by anxiety in autistic children. This is corroborated by two previous case-control studies, in which anxiety scores were significantly associated with illogical thinking and loose associations in autistic children (Gaag et al., 2005; Solomon et al., 2008). Interestingly, this may implicate abnormal connectivity in certain brain structures, such as the frontotemporal network, in the relationship between anxiety, Autism and psychosis (Caplan et al., 2001). In addition, an earlier paper found that anxious children with pervasive developmental disorders, such as autism, presented with more severe psychotic symptoms (Weisbrot et al., 2005). Collectively, these findings provide preliminary evidence for the potential causal role of anxiety in the development of psychosis, however further research is needed in adult populations.
4.5 Limitations
This is the first review to synthesize literature exploring anxiety, Autism and PLEs, identifying an important area for future research. A key strength of this review is that the quality of the included studies was generally high (see Supplementary Tables 1–4). However, there are several limitations. Firstly, the lack of research directly examining anxiety, Autism and PLEs is a significant disadvantage, as it limits the extent to which the research question can be addressed beyond discussion of bilateral associations between the variables. Similarly, most research included in the current review was cross-sectional, which precludes any assessment of causality, particularly in relation to the causal role of anxiety; the limited number of longitudinal studies included in this review offer more robust insight into the temporal dynamics between anxiety and PLEs. Despite overall quality, clear effect was rated “Unclear” in 21 out of 31 cross-sectional studies (see Supplementary Table 1), meaning that any conclusions drawn must remain tentative. The huge heterogeneity of methods utilized in the included studies meant a meta-analysis was not possible, which would have strengthened the findings of this review. Furthermore, much of the included research involved measuring PLEs, autistic traits and anxiety scores within nonclinical populations. As the research question pertains to autistic individuals, it is unclear whether the included studies can be used to answer the research question or be applied to clinical populations.
A further limitation of the current review is the generalizability of the included studies, as many involved online questionnaires or student populations. While online questionnaires are both cost- and time-efficient, they may not capture samples that are reflective of the general population, including those who do not or cannot use computers (Gosling et al., 2010). Similarly, despite being easy to recruit, student populations are often socioeconomically and ethnically unrepresentative (Hanel and Vione, 2016). Studies conducted in broader populations frequently used sampling methods that involved contacting addresses in a certain region, excluding homeless populations and those in temporary accommodation, who may be at greater risk of PLEs (Byrne et al., 2015). Consequently, this may limit the generalizability and application of any conclusions drawn if the included studies are not representative. Finally, perhaps the most important limitation is that this review was conducted independently by one author. Collaboration is an important element of systematic reviews, and while initial screening was confirmed by an independent rater, decisions made at later stages may have benefited from a collaborator. Ultimately, bias may be inherent in the decisions made by one person.
4.6 Implications and future directions
This systematic review identified strong associations between anxiety, Autism and PLEs, suggesting that both anxiety symptoms and autistic traits are important factors in the emergence of PLEs. These findings have important implications for early intervention: firstly, they emphasize the importance of screening for PLEs in autistic individuals, as well as those with anxiety disorders, as this could lead to the early identification of individuals at greater risk of developing psychosis. Similarly, autistic individuals with a co-occurring anxiety disorder should be recognized as an at-risk group in mental health services, as they may benefit from individualized prevention strategies. For instance, interventions aimed at treating anxiety in autistic individuals may have the potential to reduce rates of transition to psychosis in this population. Additionally, the current review identified IU as an important mechanism in the relationship between the three variables, suggesting it may be a useful target for therapeutic intervention. Improving tolerance to uncertainty could benefit individuals at risk through reducing anxiety, and could inform relapse prevention work in autistic individuals who have already experienced a first episode of psychosis (Miller and McGuire, 2023). Other cognitive biases were proposed as important contributing factors, suggesting that Cognitive Behavioral Therapy may be especially useful in this population. Moreover, this review highlights the importance of addressing environmental influences, which may mediate the relationship between Autism and PLEs. Psychosocial interventions that address trauma and focus on reducing environmental stressors could therefore be effective in decreasing the incidence of PLEs in autistic individuals.
Nevertheless, further research is needed involving adult populations exploring anxiety, Autism and PLEs, which would allow for a future systematic review to be conducted involving all three search terms. For example, case-control studies could compare PLE frequency among autistic individuals and a co-occurring anxiety disorder to those without, providing important data for future meta-analysis. As availability of consistent datasets in the field increases, both standard and network meta-analyses would allow for more robust comparisons to be made. In particular, a network meta-analysis approach would enable researchers to account for the overlap between subclinical psychosis risk measures and diverse anxiety metrics, offering a more nuanced understanding of their interrelation and enhancing the precision of comparative analyses. It is important to note that OCD is no longer categorized as an anxiety disorder in the DSM-5, despite five of the included studies conceptualizing it as such (American Psychiatric Association, 2022). Previous research has highlighted a relationship between OCD and psychosis distinct from that of other anxiety disorders; therefore, this may have implications for the conclusions drawn from studies that have not accounted for this (Cunill et al., 2009; Martinho et al., 2023). As the field of research continues to develop, a systematic review specifically exploring the relationship between OCD, Autism and psychotic-like experiences may provide useful insight into the co-occurring conditions.
However, the current reliance on self-report methods may result in false estimations of PLE frequency, as both recall bias, and the abstract construct of PLEs, can make interpreting questions in a standardized way challenging (Kelleher and Cannon, 2011; Prochwicz and Gaweda, 2016). Despite this, interviews are thought to increase the chance of socially desirable answering in PLE research, due to the sensitive nature of the topic and the influence of mental health stigma (Kelleher and Cannon, 2011; Mamah et al., 2021). Instead, future research may benefit from utilizing observer-ratings in addition to self-report measures, in order to reduce bias and enhance methodological validity (Spitz et al., 2017). In addition, establishing standardized definitions of PLEs would allow for clearer comparison between studies (Hinterbuchinger and Mossaheb, 2021). Structural Equation Modeling (SEM) could be utilized to examine anxiety as a mediator in the relationship between autistic traits and PLEs (Gunzler et al., 2013). Future investigations should look deeper into the distress, insight and subjective quality of PLEs rather than simply the frequency, moving beyond prevalence estimates and taking a more phenomenological approach. Lastly, further longitudinal research is needed to disentangle the temporal and causal relationships between anxiety, PLEs, and autistic traits. Establishing the causal role of anxiety in the development of PLEs in Autism would be of significant benefit to the wider field of early intervention in psychosis (Bird et al., 2018).
5 Conclusions
This review has presented systematic evidence of the strong associations between anxiety, Autism and PLEs, identifying key mechanisms involved in these relationships. While providing useful insight into the etiology of PLEs in Autism, this review has also highlighted significant gaps in the literature, such as the lack of case-control studies and longitudinal research examining the causal role of anxiety. Future research addressing these gaps could guide the development of targeted psychological interventions, to reduce rates of psychosis transition and, ultimately, improve outcomes for autistic individuals.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MR: Writing – original draft, Writing – review & editing. SS: Writing – review & editing. RM: Writing – review & editing, Conceptualization, Methodology, Resources, Supervision, Visualization, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. SS was funded by Medical Research Council grant (MR/V037218/1).
Acknowledgments
We would like to acknowledge the Library at King's College London for providing access to the articles in this review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1549886/full#supplementary-material
References
Abu-Akel, A. M., Wood, S. J., Hansen, P. C., and Apperly, I. A. (2015). Perspective-taking abilities in the balance between autism tendencies and psychosis proneness. Proc. Biol. Sci. 282:20150563. doi: 10.1098/rspb.2015.0563
Adams, D., Ambrose, K., Simpson, K., Malone, S., and Dargue, N. (2023). The relationshipbetween anxiety and social outcomes in autistic children and adolescents: a meta-analysis. Clin. Child Fam. Psychol. Rev. 26, 706–720. doi: 10.1007/s10567-023-00450-7
Ambrose, K., Simpson, K., and Adams, D. (2021). The relationship between social and academic outcomes and anxiety for children and adolescents on the autism spectrum: a systematic review. Clin. Psychol. Rev. 90:102086. doi: 10.1016/j.cpr.2021.102086
American Psychiatric Association (2022). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn, text rev. doi: 10.1176/appi.books.9780890425787
Antosz-Rekucka, R., and Prochwicz, K. (2023). Depression and anxiety mediate the relationship between the retrospectively measured symptoms of premenstrual disorders and negative but not positive psychotic-like experiences. Sci. Rep. 13:17711. doi: 10.1038/s41598-023-44573-x
Armando, M. (2023). Prevalence of psychotic symptoms in a population of adolescents hospitalized for suicidal thoughts and behaviour. Early Interv. Psychiatry 17:33. doi: 10.1111/eip.13408
Armando, M., Lin, A., Girardi, P., Righetti, V., Dario, C., Saba, R., et al. (2013). Prevalence of psychotic-like experiences in young adults with social anxiety disorder and correlation with affective dysregulation. J. Nerv. Ment. Dis. 201, 1053–1059. doi: 10.1097/NMD.0000000000000050
Armando, M., Nelson, B., Yung, A. R., Ross, M., Birchwood, M., Girardi, P., et al. (2010). Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophr. Res. 119, 258–265. doi: 10.1016/j.schres.2010.03.001
Barlati, S., Deste, G., Ariu, C., and Vita, A. (2016). Autism spectrum disorder and schizophrenia: do they overlap? Int. J. Emerg. Ment. Health Hum. Resil. 18, 760–763. doi: 10.4172/1522-4821.1000318
Baryshnikov, I., Aaltonen, K., Koivisto, M., Melartin, T., Näätänen, P., Suominen, K., et al. (2018). Self-reported psychosis-like experiences in patients with mood disorders. Eur. Psychiatry 51, 90–97. doi: 10.1016/j.eurpsy.2016.07.005
Bird, J., Waite, F., and Freeman, D. (2018). Anxiety in the development of psychotic experiences in children and adolescents: a systematic review. Schizophr. Bull. 44:S335. doi: 10.1093/schbul/sby018.819
Bortoletto, R., Bassani, L., Garzitto, M., Lamberti, M., Simonati, A., Darra, F., et al. (2023). Risk of psychosis in autism spectrum disorder individuals exposed to psychosocial stressors: a 9-year chart review study. Autism Res. 16, 2139–2149. doi: 10.1002/aur.3042
Bortolon, C., and Raffard, S. (2015). Self-reported psychotic-like experiences in individuals with obsessive-compulsive disorder versus schizophrenia patients: characteristics and moderation role of trait anxiety. Compr. Psychiatry 57, 97–105. doi: 10.1016/j.comppsych.2014.10.011
Bougeard, C., Picarel-Blanchot, F., Schmid, R., Campbell, R., and Buitelaar, J. K. (2021). Prevalence of autism spectrum disorder and co-morbidities in children and adolescents: a systematic literature review. Front. Psychiatry 12:744709. doi: 10.3389/fpsyt.2021.744709
Bourgin, J., Tebeka, S., Mallet, J., Mazer, N., Dubertret, C., and Le Strat, Y. (2020). Prevalence and correlates of psychotic-like experiences in the general population. Schizophr. Res. 215, 371–377. doi: 10.1016/j.schres.2019.08.024
Brett, C., Heriot-Maitland, C., McGuire, P., and Peters, E. (2014). Predictors of distress associated with psychotic-like anomalous experiences in clinical and non-clinical populations. Br. J. Clin. Psychol. 53, 213–227. doi: 10.1111/bjc.12036
Brosnan, M., Chapman, E., and Ashwin, C. (2014). Adolescents with autism spectrum disorder show a circumspect reasoning bias rather than ‘jumping-to-conclusions'. J. Autism Dev. Disord. 44, 513–520. doi: 10.1007/s10803-013-1897-5
Byrne, G. J., Steele, S. J., and Pachana, N. A. (2015). Delusion-like experiences in older people with anxiety disorders. Int. Psychogeriatr. 27, 1191–1196. doi: 10.1017/S1041610215000113
Caplan, R., Guthrie, D., Tang, B., Nuechterlein, K. H., and Asarnow, R. F. (2001). Thought disorder in attention-deficit hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 40, 965–972. doi: 10.1097/00004583-200108000-00019
Catalan, A., Angosto, V., Díaz, A., Martínez, N., Guede, D., Pereda, M., et al. (2018). The relationship between theory of mind deficits and neurocognition in first episode-psychosis. Psychiatry Res. 268, 361–367. doi: 10.1016/j.psychres.2018.06.066
Catone, G., Marotta, R., Pisano, S., Lennox, B., Carotenuto, M., Gritti, A., et al. (2017). Psychotic-like experiences in help-seeking adolescents: dimensional exploration and association with different forms of bullying victimization - a developmental social psychiatry perspective. Int. J. Soc. Psychiatry 63, 752–762. doi: 10.1177/0020764017733765
Chan, E. H. C., Kong, S. D. X., Park, S. H., Song, Y. J. C., Demetriou, E. A., Pepper, K. L., et al. (2019). Validation of the social functioning scale: comparison and evaluation in early psychosis, autism spectrum disorder and social anxiety disorder. Psychiatry Res. 276, 45–55. doi: 10.1016/j.psychres.2019.03.037
Chisholm, K., Lin, A., Abu-Akel, A., and Wood, S. J. (2015). The association between autism and schizophrenia spectrum disorders: a review of eight alternate models of co-occurrence. Neurosci. Biobehav. Rev. 55, 173–183. doi: 10.1016/j.neubiorev.2015.04.012
Chung, Y. S., Barch, D., and Strube, M. (2014). A meta-analysis of mentalizing impairments in adults with schizophrenia and autism spectrum disorder. Schizophr. Bull. 40, 602–616. doi: 10.1093/schbul/sbt048
Cowan, H. R., and Mittal, V. A. (2021). Three types of psychotic-like experiences in youth at clinical high risk for psychosis. Eur. Arch. Psychiatry Clin. Neurosci. 271, 733–744. doi: 10.1007/s00406-020-01143-w
Craddock, N., and Owen, M. J. (2010). The Kraepelinian dichotomy–going, going… but still not gone. Br. J. Psychiatry 196, 92–95. doi: 10.1192/bjp.bp.109.073429
Crespi, B. J. (2010). Revisiting Bleuler: relationship between autism and schizophrenia. Br. J. Psychiatry 196, 495. doi: 10.1192/bjp.196.6.495
Cunill, R., Castells, X., and Simeon, D. (2009). Relationships between obsessive-compulsive symptomatology and severity of psychosis in schizophrenia: a systematic review and meta-analysis. J. Clin. Psychiatry 70:70. doi: 10.4088/JCP.07r03618
Dardani, C., Schalbroeck, R., Madley-Dowd, P., Jones, H. J., Strelchuk, D., Hammerton, G., et al. (2023). Childhood trauma as a mediator of the association between autistic traits and psychotic experiences: evidence from the Avon Longitudinal Study of Parents and Children cohort. Schizophr. Bull. 49, 364–374. doi: 10.1093/schbul/sbac167
Darke, H., Sundram, S., Cropper, S. J., and Carter, O. (2021). Dynamic face processing impairments are associated with cognitive and positive psychotic symptoms across psychiatric disorders. npj Schizophr. 7:36. doi: 10.1038/s41537-021-00166-z
Dawson, M. E., and Schell, A. M. (2002). What does electrodermal activity tell us about prognosis in the schizophrenia spectrum? Schizophr. Res. 54, 87–93. doi: 10.1016/S0920-9964(01)00355-3
de Lacy, N., and King, B. H. (2013). Revisiting the relationship between autism and schizophrenia: toward an integrated neurobiology. Annu. Rev. Clin. Psychol. 9, 555–587. doi: 10.1146/annurev-clinpsy-050212-185627
Demetriou, E. A., Park, S. H., Ho, N., Pepper, K. L., Song, Y. J. C., Naismith, S. L., et al. (2020). Machine learning for differential diagnosis between clinical conditions with social difficulty: autism spectrum disorder, early psychosis, and social anxiety disorder. Front. Psychiatry 11:545. doi: 10.3389/fpsyt.2020.00545
Demetriou, E. A., Song, Y. J. C., Park, S. H., Pepper, K. L., Naismith, S. L., Hermens, D. F., et al. (2018). Autism, early psychosis, and social anxiety disorder: a transdiagnostic examination of executive function cognitive circuitry and contribution to disability. Transl. Psychiatry 8:200. doi: 10.1038/s41398-018-0193-8
Deng, W. Y., Grove, T., and Deldin, P. (2020). Anxiety mediates the relationship between psychotic-like experiences and social functioning in the general population. Psychopathology 53, 95–102. doi: 10.1159/000507869
Dudley, R., Taylor, P., Wickham, S., and Hutton, P. (2016). Psychosis, delusions and the “jumping to conclusions” reasoning bias: a systematic review and meta-analysis. Schizophr. Bull. 42, 652–665. doi: 10.1093/schbul/sbv150
Edirisooriya, M., Dykiert, D., and Auyeung, B. (2021). IQ and internalising symptoms in adolescents with ASD. J. Autism Dev. Disord. 51, 3887–3907. doi: 10.1007/s10803-020-04810-y
Ered, A., Cooper, S., and Ellman, L. M. (2018). Sleep quality, psychological symptoms, and psychotic-like experiences. J. Psychiatr. Res. 98, 95–98. doi: 10.1016/j.jpsychires.2017.12.016
Esterberg, M. L., Trotman, H. D., Brasfield, J. L., Compton, M. T., and Walker, E. F. (2008). Childhood and current autistic features in adolescents with schizotypal personality disorder. Schizophr. Res. 104, 265–273. doi: 10.1016/j.schres.2008.04.029
Fernandes, J. M., Cajão, R., Lopes, R., Jerónimo, R., and Barahona-Corrêa, J. B. (2018). Social cognition in schizophrenia and autism spectrum disorders: a systematic review and meta-analysis of direct comparisons. Front. Psychiatry 9:504. doi: 10.3389/fpsyt.2018.00504
Freeman, D. (2007). Suspicious minds: the psychology of persecutory delusions. Clin. Psychol. Rev. 27, 425–457. doi: 10.1016/j.cpr.2006.10.004
Freeman, D., and Fowler, D. (2009). Routes to psychotic symptoms: trauma, anxiety and psychosis-like experiences. Psychiatry Res. 169, 107–112. doi: 10.1016/j.psychres.2008.07.009
Freeman, D., and Garety, P. A. (2003). Connecting neurosis and psychosis: the direct influence of emotion on delusions and hallucinations. Behav. Res. Ther. 41, 923–947. doi: 10.1016/S0005-7967(02)00104-3
Gaag, R. J. v. d., Caplan, R., Engeland, H. v., Loman, F., and Buitelaar, J. K. (2005). A controlled study of formal thought disorder in children with autism and multiple complex developmental disorders. J. Child Adolesc. Psychopharmacol. 15, 465–476. doi: 10.1089/cap.2005.15.465
Giocondo, J. G., Salum, G. A., Gadelha, A., Argolo, F. C., Simioni, A. R., Mari, J. J., et al. (2021). Psychotic-like experiences and common mental disorders in childhood and adolescence: bidirectional and transdiagnostic associations in a longitudinal community-based study. Schizophr. Bull. Open 2:sgab028. doi: 10.1093/schizbullopen/sgab028
Gong, Z., Reinhardt, J. D., Han, Z., Ba, Z., and Lei, S. (2022). Associations between school bullying and anxiety in children and adolescents from an ethnic autonomous county in China. Psychiatry Res. 314:114649. doi: 10.1016/j.psychres.2022.114649
Gosling, S. D., Sandy, C. J., John, O. P., and Potter, J. (2010). Wired but not WEIRD: the promise of the Internet in reaching more diverse samples. Behav. Brain Sci. 33:94. doi: 10.1017/S0140525X10000300
Gough, D., Thomas, J., and Oliver, S. (2012). Clarifying differences between review designs and methods. Syst. Rev. 1:28. doi: 10.1186/2046-4053-1-28
Gunzler, D., Chen, T., Wu, P., and Zhang, H. (2013). Introduction to mediation analysis with structural equation modeling. Shanghai Arch. Psychiatry 25:390. doi: 10.3969/j.issn.1002-0829.2013.06.009
Hajdúk, M., Straková, A., Januška, J., Ivančík, V., Dančík, D., Cavojská, N., et al. (2023). Connections between and within extended psychosis and autistic phenotypes and social relationships in the general population. J. Psychiatr. Res. 157, 36–42. doi: 10.1016/j.jpsychires.2022.11.022
Hanel, P. H., and Vione, K. C. (2016). Do student samples provide an accurate estimate of the general public? PLoS ONE 11:e0168354. doi: 10.1371/journal.pone.0168354
Hartley, S., Barrowclough, C., and Haddock, G. (2013). Anxiety and depression in psychosis: a systematic review of associations with positive psychotic symptoms. Acta Psychiatr. Scand. 128, 327–346. doi: 10.1111/acps.12080
Hedley, D., and Uljarević, M. (2018). Systematic review of suicide in autism spectrum disorder: current trends and implications. Curr. Dev. Disord. Rep. 5, 65–76. doi: 10.1007/s40474-018-0133-6
Hinterbuchinger, B., and Mossaheb, N. (2021). Psychotic-like experiences: a challenge in definition and assessment. Front. Psychiatry 12:582392. doi: 10.3389/fpsyt.2021.582392
Hobson, H., and Petty, S. (2021). Moving forwards not backwards: heterogeneity in autism spectrum disorders. Mol. Psychiatry 26, 7100–7101. doi: 10.1038/s41380-021-01226-7
Hollocks, M. J., Lerh, J. W., Magiati, I., Meiser-Stedman, R., and Brugha, T. S. (2019). Anxiety and depression in adults with autism spectrum disorder: a systematic review and meta-analysis. Psychol. Med. 49, 559–572. doi: 10.1017/S0033291718002283
Hossain, M. M., Khan, N., Sultana, A., Ma, P., McKyer, E. L. J., Ahmed, H. U., et al. (2020). Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: an umbrella review of systematic reviews and meta-analyses. Psychiatry Res. 287:112922. doi: 10.1016/j.psychres.2020.112922
Huppert, J. D., and Smith, T. E. (2005). Anxiety and schizophrenia: the interaction of subtypes of anxiety and psychotic symptoms. CNS Spectr. 10, 721–731. doi: 10.1017/S1092852900019714
Isaksson, J., Angenfelt, M., Frick, M. A., Olofsdotter, S., and Vadlin, S. (2022). Psychotic-like experiences from adolescence to adulthood: a longitudinal study. Schizophr. Res. 248, 1–7. doi: 10.1016/j.schres.2022.07.010
Isaksson, J., Vadlin, S., Olofsdotter, S., Åslund, C., and Nilsson, K. W. (2020). Psychotic-like experiences during early adolescence predict symptoms of depression, anxiety, and conduct problems three years later: a community-based study. Schizophr. Res. 215, 190–196. doi: 10.1016/j.schres.2019.10.033
Janssen, I., Versmissen, D., Campo, J., Myin-Germeys, I., Van Os, J., and Krabbendam, L. (2006). Attribution style and psychosis: evidence for an externalizing bias in patients but not in individuals at high risk. Psychol. Med. 36, 771–778. doi: 10.1017/S0033291706007422
Jenkinson, R., Milne, E., and Thompson, A. (2020). The relationship between intolerance of uncertainty and anxiety in autism: a systematic literature review and meta-analysis. Autism 24, 1933–1944. doi: 10.1177/1362361320932437
Jutla, A., Donohue, M. R., Veenstra-VanderWeele, J., and Foss-Feig, J. H. (2022). Reported autism diagnosis is associated with psychotic-like symptoms in the Adolescent Brain Cognitive Development cohort. Eur. Child Adolesc. Psychiatry 31, 1–10. doi: 10.1007/s00787-021-01738-1
Kafali, H. Y., Turan, S., Akpinar, S., Mutlu, M., Parlakay, A. Ö., Çöp, E., et al. (2022). Correlates of psychotic like experiences (PLEs) during Pandemic: an online study investigating a possible link between the SARS-CoV-2 infection and PLEs among adolescents. Schizophr. Res. 241, 36–43. doi: 10.1016/j.schres.2021.12.049
Kelleher, I., and Cannon, M. (2011). Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol. Med. 41, 1–6. doi: 10.1017/S0033291710001005
Kilanko, A., Obi-Azuike, C., Adaralegbe, N., Eze-Njoku, C., Urhi, A., Agbor, C., et al. (2022). The correlation between autistic childhood disorders and the development of anxiety and depression in adults: a systematic review. Cureus 14:e30093. doi: 10.7759/cureus.30093
Kirov, G., Rujescu, D., Ingason, A., Collier, D. A., O'Donovan, M. C., and Owen, M. J. (2009). Neurexin 1 (NRXN1) deletions in schizophrenia. Schizophr. Bull. 35, 851–854. doi: 10.1093/schbul/sbp079
Kiyono, T., Morita, M., Morishima, R., Fujikawa, S., Yamasaki, S., Nishida, A., et al. (2020). The prevalence of psychotic experiences in autism spectrum disorder and autistic traits: a systematic review and meta-analysis. Schizophr. Bull. Open 1:sgaa032. doi: 10.1093/schizbullopen/sgaa046
Kosteletos, I., Hatzimanolis, A., Xenaki, L. A., Ralli, I., Dimitrakopoulos, S., Gournellis, R., et al. (2024). The relationship between bullying and symptom presentation in first-episode psychosis. Psychiatriki 35, 17–25. doi: 10.22365/jpsych.2023.021
Kreis, I., Zhang, L., Mittner, M., Syla, L., Lamm, C., and Pfuhl, G. (2023). Aberrant uncertainty processing is linked to psychotic-like experiences, autistic traits, and is reflected in pupil dilation during probabilistic learning. Cogn. Affect. Behav. Neurosci. 23, 905–919. doi: 10.3758/s13415-023-01088-2
Kreis, I., Zhang, L., Moritz, S., and Pfuhl, G. (2022). Spared performance but increased uncertainty in schizophrenia: evidence from a probabilistic decision-making task. Schizophr. Res. 243, 414–423. doi: 10.1016/j.schres.2021.06.038
Kyriakopoulos, M., Stringaris, A., Manolesou, S., Radobuljac, M. D., Jacobs, B., Reichenberg, A., et al. (2015). Determination of psychosis-related clinical profiles in children with autism spectrum disorders using latent class analysis. Eur. Child Adolesc. Psychiatry 24, 301–307. doi: 10.1007/s00787-014-0576-1
Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., Mandy, W., et al. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry 6, 819–829. doi: 10.1016/S2215-0366(19)30289-5
Lawson, R. P., Mathys, C., and Rees, G. (2017). Adults with autism overestimate the volatility of the sensory environment. Nat. Neurosci. 20, 1293–1299. doi: 10.1038/nn.4615
Lincoln, T. M., Lange, J., Burau, J., Exner, C., and Moritz, S. (2010). The effect of state anxiety on paranoid ideation and jumping to conclusions. an experimental investigation. Schizophr. Bull. 36, 1140–1148. doi: 10.1093/schbul/sbp029
Lisøy, R. S., Biegler, R., Haghish, E. F., Veckenstedt, R., Moritz, S., and Pfuhl, G. (2022a). Seeing minds - a signal detection study of agency attribution along the autism-psychosis continuum. Cogn. Neuropsychiatry 27, 356–372. doi: 10.1080/13546805.2022.2075721
Lisøy, R. S., Pfuhl, G., Sunde, H. F., and Biegler, R. (2022b). Sweet spot in music-Is predictability preferred among persons with psychotic-like experiences or autistic traits? PLoS One 17:e0275308. doi: 10.1371/journal.pone.0275308
Long, H. A., French, D. P., and Brooks, J. M. (2020). Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res. Methods Med. Health Sci. 1, 31–42. doi: 10.1177/2632084320947559
Lu, D., Qiu, S., Xian, D., Zhang, J., Zhang, Y., Liu, X., et al. (2022). Psychotic-like experiences and associated socio-demographic factors among pregnant women in each trimester in China. Front. Psychiatry 13:927112. doi: 10.3389/fpsyt.2022.927112
Lydon, S., Healy, O., Reed, P., Mulhern, T., Hughes, B. M., and Goodwin, M. S. (2016). A systematic review of physiological reactivity to stimuli in autism. Dev. Neurorehabil. 19, 335–355. doi: 10.3109/17518423.2014.971975
Ma, L.-L., Wang, Y.-Y., Yang, Z.-H., Huang, D., Weng, H., and Zeng, X.-T. (2020). Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil. Med. Res. 7, 1–11. doi: 10.1186/s40779-020-00238-8
Maiano, C., Normand, C. L., Salvas, M. C., Moullec, G., and Aime, A. (2016). Prevalence of school bullying among youth with autism spectrum disorders: a systematic review and meta-analysis. Autism Res. 9, 601–615. doi: 10.1002/aur.1568
Mamah, D., Mutiso, V. N., and Ndetei, D. M. (2021). Psychotic-like experiences among 9,564 Kenyan adolescents and young adults. Psychiatry Res. 302:113998. doi: 10.1016/j.psychres.2021.113994
Martinez, A. P., Wickham, S., Rowse, G., Milne, E., and Bentall, R. P. (2021). Robust association between autistic traits and psychotic-like experiences in the adult general population: epidemiological study from the 2007 Adult Psychiatric Morbidity Survey and replication with the 2014 APMS. Psychol. Med. 51, 2707–2713. doi: 10.1017/S0033291720001373
Martinho, F. P., Magalhaes, D., Felicio, R., Ferreira, T. F., and Jorge, S. (2023). Obsessive-compulsive symptoms in first episode psychosis and risk states: systematic review with meta-analysis. Schizophr. Res. 255, 41–51. doi: 10.1016/j.schres.2023.03.024
Merola, G. P., Patti, A., Benedetti, D., Bozza, B., Ballerini, A., and Ricca, V. (2024). The role of psychotic-like experiences in the association between aberrant salience and anxiety: a psychopathological proposal based on a case-control study. Early Interv. Psychiatry 18, 535–546. doi: 10.1111/eip.13490
Micai, M., Fatta, L. M., Gila, L., Caruso, A., Salvitti, T., Fulceri, F., et al. (2023). Prevalence of co-occurring conditions in children and adults with autism spectrum disorder: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 155:105436. doi: 10.1016/j.neubiorev.2023.105436
Miller, M. L., and McGuire, J. F. (2023). Targeting intolerance of uncertainty in treatment: a meta-analysis of therapeutic effects, treatment moderators, and underlying mechanisms. J. Affect. Disord. 323, 283–295. doi: 10.1016/j.jad.2023.08.132
Mingins, J. E., Tarver, J., Waite, J., Jones, C., and Surtees, A. D. (2021). Anxiety and intellectual functioning in autistic children: a systematic review and meta-analysis. Autism 25, 18–32. doi: 10.1177/1362361320953253
Mitelman, S. A., Bralet, M. C., Haznedar, M. M., Hollander, E., Shihabuddin, L., Hazlett, E. A., et al. (2017). Diametrical relationship between gray and white matter volumes in autism spectrum disorder and schizophrenia. Brain Imaging Behav. 11, 1823–1835. doi: 10.1007/s11682-016-9648-9
Mitelman, S. A., Buchsbaum, M. S., Young, D. S., Haznedar, M. M., Hollander, E., Shihabuddin, L., et al. (2018). Increased white matter metabolic rates in autism spectrum disorder and schizophrenia. Brain Imaging Behav. 12, 1290–1305. doi: 10.1007/s11682-017-9785-9
Monsonet, M., Kwapil, T. R., and Barrantes-Vidal, N. (2022). A time-lagged study of predictors of paranoia and psychotic-like experiences in daily life across the schizotypy continuum. J. Psychopathol. Clin. Sci. 131, 98–108. doi: 10.1037/abn0000726
Montaser, J., Umeano, L., Pujari, H. P., Nasiri, S. M. Z., Parisapogu, A., Shah, A., et al. (2023). Correlations between the development of social anxiety and individuals with autism spectrum disorder: a systematic review. Cureus 15:e44841. doi: 10.7759/cureus.44841
Morales-Muñoz, I., Palmer, E. R., Marwaha, S., Mallikarjun, P. K., and Upthegrove, R. (2022). Persistent childhood and adolescent anxiety and risk for psychosis: a longitudinal birth cohort study. Biol. Psychiatry 92, 275–282. doi: 10.1016/j.biopsych.2021.12.003
Mutluer, T., Aslan Genç, H., Özcan Morey, A., Yapici Eser, H., Ertinmaz, B., Can, M., et al. (2022). Population-based psychiatric comorbidity in children and adolescents with autism spectrum disorder: a meta-analysis. Front. Psychiatry 13:856208. doi: 10.3389/fpsyt.2022.856208
NICE (2012). Appendix G Quality Appraisal Checklist - Quantitative Studies Reporting Correlations and Associations | Methods for the Development of NICE Public Health Guidance (Third Edition). Guidance | NICE. Available online at: https://www.nice.org.uk/process/pmg4/chapter/appendix-g-quality-appraisal-checklist-quantitative-studies-reporting-correlations-and
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Park, J. S., Damme, K. S., Kuhney, F. S., and Mittal, V. A. (2022). Anxiety symptoms, rule learning, and cognitive flexibility in non-clinical psychosis. Sci. Rep. 12:5649. doi: 10.1038/s41598-022-09620-z
Pepper, K. L., Demetriou, E. A., Park, S. H., Boulton, K. A., Hickie, I. B., Thomas, E. E., et al. (2019). Self-reported empathy in adults with autism, early psychosis, and social anxiety disorder. Psychiatry Res. 281:112604. doi: 10.1016/j.psychres.2019.112604
Pepper, K. L., Demetriou, E. A., Park, S. H., Song, Y. C., Hickie, I. B., Cacciotti-Saija, C., et al. (2018). Autism, early psychosis, and social anxiety disorder: understanding the role of social cognition and its relationship to disability in young adults with disorders characterized by social impairments. Transl. Psychiatry 8:233. doi: 10.1038/s41398-018-0282-8
Phillips, L. J., McGorry, P. D., Garner, B., Thompson, K. N., Pantelis, C., Wood, S. J., et al. (2006). Stress, the hippocampus and the hypothalamic-pituitary-adrenal axis: implications for the development of psychotic disorders. Aust. N. Z. J. Psychiatry 40, 725–741. doi: 10.1111/j.1440-1614.2006.01877.x
Prochwicz, K., and Gaweda, Ł. (2016). Depression and anxiety mediate the relationship between temperament and character and psychotic-like experiences in healthy subjects. Psychiatry Res. 246, 195–202. doi: 10.1016/j.psychres.2016.09.037
Prochwicz, K., and Kłosowska, J. (2018). The interplay between trait anxiety, cognitive biases and attentional control in healthy individuals with psychotic-like experiences. Psychiatry Res. 259, 44–50. doi: 10.1016/j.psychres.2017.09.085
Rahman, T., and Lauriello, J. (2016). Schizophrenia: an overview. Focus 14, 300–307. doi: 10.1176/appi.focus.20160006
Rajji, T., Ismail, Z., and Mulsant, B. (2009). Age at onset and cognition in schizophrenia: meta-analysis. Br. J. Psychiatry 195, 286–293. doi: 10.1192/bjp.bp.108.060723
Rejek, M., and Misiak, B. (2023). Dimensions of psychopathology associated with psychotic-like experiences: findings from the network analysis in a nonclinical sample. Eur. Psychiatry 66:e56. doi: 10.1192/j.eurpsy.2023.2429
Rep, C., Dubertret, C., Pignon, B., Sleurs, D., Tebeka, S., and Le Strat, Y. (2023). Psychotic-like experiences in general population: psychiatric comorbidity and impact on quality of life across lifespan. Schizophr. Res. 256, 52–62. doi: 10.1016/j.schres.2023.04.014
Reynolds, S., and Lane, S. J. (2008). Diagnostic validity of sensory over-responsivity: a review of the literature and case reports. J. Autism Dev. Disord. 38, 516–529. doi: 10.1007/s10803-007-0418-9
Ribolsi, M., Fiori Nastro, F., Pelle, M., Medici, C., Sacchetto, S., Lisi, G., et al. (2022). Recognizing psychosis in autism spectrum disorder. Front. Psychiatry 13:768586. doi: 10.3389/fpsyt.2022.768586
Sætren, S. S., Bjørnestad, J. R., Ottesen, A. A., Fisher, H. L., Olsen, D. A., Hølland, K., et al. (2024). Unraveling the concept of childhood adversity in psychosis research: a systematic review. Schizophr. Bull. 50, 1055–1066. doi: 10.1093/schbul/sbae085
Saha, S., Scott, J., Varghese, D., and McGrath, J. (2012). Anxiety and depressive disorders are associated with delusional-like experiences: a replication study based on a National Survey of Mental Health and Wellbeing. BMJ Open 2:e001001. doi: 10.1136/bmjopen-2012-001001
Salazar, F., Baird, G., Chandler, S., Tseng, E., O'sullivan, T., Howlin, P., et al. (2015). Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J. Autism Dev. Disord. 45, 2283–2294. doi: 10.1007/s10803-015-2361-5
Sijtsma, H., Lee, N. C., Hollarek, M., Walsh, R. J., van Buuren, M., Braams, B. R., et al. (2021). Social cognition and friendships in adolescents with autistic-like experiences and psychotic-like experiences. Front. Psychiatry 11:589824. doi: 10.3389/fpsyt.2020.589824
Skokauskas, N., and Gallagher, L. (2009). Psychosis, affective disorders and anxiety in autistic spectrum disorder: prevalence and nosological considerations. Psychopathology 43, 8–16. doi: 10.1159/000255958
Smaga, I., Niedzielska, E., Gawlik, M., Moniczewski, A., Krzek, J., Przegaliński, E., et al. (2015). Oxidative stress as an etiological factor and a potential treatment target of psychiatric disorders. Part 2. Depression, anxiety, schizophrenia and autism. Pharmacol. Rep. 67, 569–580. doi: 10.1016/j.pharep.2014.12.015
So, S. H.-w., Freeman, D., and Garety, P. (2008). Impact of state anxiety on the jumping to conclusions delusion bias. Aust. N. Z. J. Psychiatry 42, 879–886. doi: 10.1080/00048670802345466
Solomon, M., Ozonoff, S., Carter, C., and Caplan, R. (2008). Formal thought disorder and the autism spectrum: relationship with symptoms, executive control, and anxiety. J. Autism Dev. Disord. 38, 1474–1484. doi: 10.1007/s10803-007-0526-6
South, M., and Rodgers, J. (2017). Sensory, emotional and cognitive contributions to anxiety in autism spectrum disorders. Front. Hum. Neurosci. 11:20. doi: 10.3389/fnhum.2017.00020
Spitz, A., Studerus, E., Koranyi, S., Rapp, C., Ramyead, A., Ittig, S., et al. (2017). Correlations between self-rating and observer-rating of psychopathology in at-risk mental state and first-episode psychosis patients: influence of disease stage and gender. Early Interv. Psychiatry 11, 461–470. doi: 10.1111/eip.12270
Stefanis, N. C., Hanssen, M., Smirnis, N. K., Avramopoulos, D., Evdokimidis, J. K., Stefanis, C. N., et al. (2002). Evidence that three dimensions of psychosis have a distribution in the general population. Psychol. Med. 32, 347–358. doi: 10.1017/S0033291701005141
Suen, Y. N., Chau, A. P. Y., Wong, S. M. Y., Hui, C. L. M., Chan, S. K. W., Lee, E. H. M., et al. (2024). Comorbidity of autism spectrum and attention deficit/hyperactivity disorder symptoms and their associations with 1-year mental health outcomes in adolescents and young adults. Psychiatry Res. 331:115657. doi: 10.1016/j.psychres.2023.115657
Thakkar, K. N., Brascamp, J. W., Ghermezi, L., Fifer, K., Schall, J. D., and Park, S. (2018). Reduced pupil dilation during action preparation in schizophrenia. Int. J. Psychophysiol. 128, 111–118. doi: 10.1016/j.ijpsycho.2018.03.012
Trevisan, D. A., Foss-Feig, J. H., Naples, A. J., Srihari, V., Anticevic, A., and McPartland, J. C. (2020). Autism spectrum disorder and schizophrenia are better differentiated by positive symptoms than negative symptoms. Front. Psychiatry 11:548. doi: 10.3389/fpsyt.2020.00548
Unterrassner, L., Wyss, T. A., Wotruba, D., Haker, H., and Rössler, W. (2017). The intricate relationship between psychotic-like experiences and associated subclinical symptoms in healthy individuals. Front. Psychol. 8:1537. doi: 10.3389/fpsyg.2017.01537
Upthegrove, R., Abu-Akel, A., Chisholm, K., Lin, A., Zahid, S., Pelton, M., et al. (2018). Autism and psychosis: clinical implications for depression and suicide. Schizophr. Res. 195, 80–85. doi: 10.1016/j.schres.2017.08.028
van der Linden, K., Simons, C., van Amelsvoort, T., and Marcelis, M. (2020). Lifetime and momentary psychotic experiences in adult males and females with an autism spectrum disorder. Front. Psychiatry 11:555615. doi: 10.3389/fpsyt.2020.00766
van Steensel, F. J., Bögels, S. M., and Perrin, S. (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin. Child Fam. Psychol. Rev. 14, 302–317. doi: 10.1007/s10567-011-0097-0
Vargas, T. G., and Mittal, V. A. (2023). Brain morphometry points to emerging patterns of psychosis, depression, and anxiety vulnerability over a 2-year period in childhood. Psychol. Med. 53, 3322–3334. doi: 10.1017/S0033291721005304
Varghese, D., Scott, J., Welham, J., Bor, W., Najman, J., O'Callaghan, M., et al. (2011). Psychotic-like experiences in major depression and anxiety disorders: a population-based survey in young adults. Schizophr. Bull. 37, 389–393. doi: 10.1093/schbul/sbp083
Vasa, R. A., Keefer, A., McDonald, R. G., Hunsche, M. C., and Kerns, C. M. (2020). A scoping review of anxiety in young children with autism spectrum disorder. Autism Res. 13, 2038–2057. doi: 10.1002/aur.2395
Walker, E., Mittal, V., and Tessner, K. (2008). Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu. Rev. Clin. Psychol. 4, 189–216. doi: 10.1146/annurev.clinpsy.4.022007.141248
Weisbrot, D. M., Gadow, K. D., DeVincent, C. J., and Pomeroy, J. (2005). The presentation of anxiety in children with pervasive developmental disorders. J. Child Adolesc. Psychopharmacol. 15, 477–496. doi: 10.1089/cap.2005.15.477
Wigman, J. T., van Nierop, M., Vollebergh, W. A., Lieb, R., Beesdo-Baum, K., Wittchen, H.-U., et al. (2012). Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity—implications for diagnosis and ultra–high risk research. Schizophr. Bull. 38, 247–257. doi: 10.1093/schbul/sbr196
Wilson, R. S., Yung, A. R., and Morrison, A. P. (2020). Comorbidity rates of depression and anxiety in first episode psychosis: a systematic review and meta-analysis. Schizophr. Res. 216, 322–329. doi: 10.1016/j.schres.2019.11.035
Xu, B., Chen, C., and Wang, D. (2024). Current psychotic-like experiences among Chinese college students: prevalence, correlates, and its relationship with suicidal ideation. Psychol. Res. Behav. Manage. 17, 799–811. doi: 10.2147/PRBM.S451889
Yamasaki, S., Usami, S., Sasaki, R., Koike, S., Ando, S., Kitagawa, Y., et al. (2018). The association between changes in depression/anxiety and trajectories of psychotic-like experiences over a year in adolescence. Schizophr. Res. 195, 149–153. doi: 10.1016/j.schres.2017.10.019
Yuan, D., Li, Q., Zhan, N., Zhang, L., Wang, J., Liu, M., and Geng, F. (2024). Longitudinal associations of menstrual characteristics with mental health problems among Chinese girls. Eur. Child Adolesc. Psychiatry 33, 2547–2556. doi: 10.1007/s00787-023-02345-y
Yung, A. R., Buckby, J. A., Cotton, S. M., Cosgrave, E. M., Killackey, E. J., Stanford, C., et al. (2006). Psychotic-like experiences in nonpsychotic help-seekers: associations with distress, depression, and disability. Schizophr. Bull. 32, 352–359. doi: 10.1093/schbul/sbj018
Zhao, S., Liu, Y., and Wei, K. (2022). Pupil-linked arousal response reveals aberrant attention regulation among children with autism spectrum disorder. J. Neurosci. 42, 5427–5437. doi: 10.1523/JNEUROSCI.0223-22.2022
Keywords: psychosis, autism, risk, early intervention, anxiety
Citation: Rowe M, Shergill S and Maitra R (2025) The relationships between anxiety, psychotic-like experiences and autism: a systematic review. Front. Psychol. 16:1549886. doi: 10.3389/fpsyg.2025.1549886
Received: 22 December 2024; Accepted: 24 September 2025;
Published: 13 October 2025.
Edited by:
Alana J. McVey, Center for Behavioral Medicine, United StatesReviewed by:
Danilo Assis Pereira, Brazilian Institute of Neuropsychology and Cognitive Sciences (IBNeuro), BrazilChristiane Montag, Charité University Medicine Berlin, Germany
Copyright © 2025 Rowe, Shergill and Maitra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madeleine Rowe, bWFkZHlyb3dlNDhAZ21haWwuY29t
 Madeleine Rowe
Madeleine Rowe Sukhi Shergill
Sukhi Shergill Raka Maitra
Raka Maitra