- 1Department of Psychology, Lehman College, City University of New York, New York, NY, United States
- 2School of Nursing, Indiana University, Indianapolis, IN, United States
- 3Children's Mercy Hospital, Kansas City, MO, United States
- 4School of Medicine and Riley Children's Health, Indiana University, Indianapolis, IN, United States
Young children and their parents experience frequent and repeated exposure to potentially traumatic events during treatment for cancer. Active Music Engagement (AME) is a dyadic music therapy intervention that has been found to mitigate traumatic stress symptoms among parents who screened high for traumatic stress symptoms (TSS) and reported higher levels of child distress with cancer-related hospitalizations/treatment (child distress). The current study examined sociodemographic characteristics and risk factors that were associated with higher levels of parent TSS and child distress as a means to identify families that may benefit most from AME in the future. Data were collected from the parents (or guardians) of N =136 young children (Mage = 4.88 years, SD = 1.56 years, 44.1% female) who were undergoing treatment for cancer. Parents (or guardians) completed measures that captured child and respondent demographics as well as levels of parent TSS and child distress. A series of multivariable linear regression models revealed that poorer child health was associated with significantly higher levels of child distress and parent TSS, while more frequent participation in religious or spiritual practice were associated with lower levels of TSS. Higher levels of cumulative risk were associated with higher levels of child distress and parent TSS, but different, specific risk factors were more strongly associated with each of these outcomes: income-to-needs ratios below the federal poverty level (FPL) were associated with higher child distress, whereas single partner status and parental unemployment were associated with higher levels of parent TSS.
Introduction
During treatment for cancer, young children and their parents face frequent and repeated exposure to potentially traumatic events, which are defined as events that pose a threat to one's life and/or that evoke fear, horror, and helplessness (De Young et al., 2021; Graf et al., 2013; Kazak and Baxt, 2007; Pai and Kazak, 2006; Price et al., 2016). Due to their developmental stage, young children have an elevated risk for experiencing cancer as traumatic and their reliance on their parents to regulate the emotions raised by these experiences places added physical and emotional strain on their parent (Bates et al., 2022; De Young et al., 2021; Harper et al., 2013; Kazak and Baxt, 2007; Norberg and Boman, 2013). Young child and parent distress is interrelated and prevalent among families with children undergoing cancer treatment, with 40% to 83% of parents reporting traumatic stress symptoms (TSS) within the first month of their child's diagnosis (Bakula et al., 2020; Price et al., 2016; Rodriguez et al., 2011; Woolf et al., 2016). For some parents TSS decreases over time, but for others symptoms persist and are severe (18–33% at 6 months; 7–27% at >10 months post diagnosis) (Bemis et al., 2015; Bruce, 2006; Pai et al., 2007; Price et al., 2016; Woolf et al., 2016). Lowering parent distress and TSS during treatment is associated with lower child distress, improved health-related quality of life, and better psychosocial adjustment after treatment ends (Landolt et al., 2012; Nakajima-Yamaguchi et al., 2016; Pierce et al., 2017). Yet, few empirically validated interventions are available for parents and fewer still address the interrelated nature of child/parent distress (Bradt et al., 2021; Facchini and Ruini, 2021; Koyu and Törüner, 2023; Robb and Hanson-Abromeit, 2014; Rodríguez-Rodríguez et al., 2022; Tang et al., 2020).
Interactive or active music making has been used to address a wide range of developmental and health outcomes in young children across a variety of community and healthcare contexts. Although young children can benefit from receptive experiences like music listening (Nguyen et al., 2010), most music intervention studies have focused on active music making experiences (Facchini and Ruini, 2021; Rodríguez-Rodríguez et al., 2022; González-Martín-Moreno et al., 2021). The hands-on, creative, and improvisatory qualities of making music can provide a developmentally appropriate and immersive experience that supports self-expression, social connectedness, and emotion regulation (O'Callaghan et al., 2011; Harman and Shoemark, 2024; Silberstein et al., 2024; Uggla et al., 2016, 2018). In the last 10 years, there has been an increased number of studies examining the use of interactive music experiences to address the interrelated needs of the child with cancer, their parents (or caregiver), and their larger family system (Boyde et al., 2024; Giordano et al., 2021; Harman and Shoemark, 2024; Heiderscheit, 2022; Robb et al., 2023a; Silberstein et al., 2024; Uggla et al., 2019).
Active Music Engagement (AME) is a theoretically grounded dyadic intervention that uses music-based play to lower the interrelated distress experienced by young children and parents during cancer treatment (see Robb et al., 2023a). Prior studies found that AME not only improved child engagement and coping-related behaviors (Robb et al., 2008; Robb, 2000; Robb et al., 2017), but also mitigated TSS among parents who screened high for traumatic stress and reported higher levels of child distress with cancer-related hospitalizations/treatment (which we refer to as “child distress” in the remainder of the paper) (Robb et al., 2023b). Growing availability of music therapy services in US pediatric hospitals supports implementation of AME as an evidence-based intervention for parents at risk for sustained traumatic stress (Biard et al., 2025; Knott et al., 2020). However, understanding which parents are most likely to derive the greatest benefit from AME will be central to developing successful implementation strategies. Given that child distress and TSS moderated the effects of AME in previous trials (Robb et al., 2023b), identifying parents who may report higher levels of distress for their child and TSS for themselves would be an important first step in this effort.
Ecological systems theory (Bronfenbrenner, 1977; Bronfenbrenner and Morris, 2006) suggests that experiences of distress and TSS do not occur in isolation. Rather, the environments that families inhabit, and specifically the extent to which those environments feature sociodemographic risk factors, will influence the incidence and severity of these experiences. Moreover, the concept of cumulative environmental risk suggests that it may not be the presence or absence of a specific risk factor, but rather their accumulation that influences these experiences (Appleyard et al., 2005; Evans et al., 2013), although some risk factors may exhibit stronger associations with distress and TSS than others (Brown et al., 2021). Research on the association of sociodemographic risk factors and TSS in parents of children with cancer is limited, but emerging. Studies in the United States have focused on mothers of children with cancer and found TSS to be associated with partnership status (single vs. partnered), income/socioeconomic status, and education level (Bemis et al., 2015; Greening et al., 2017).
Both ecological systems theory (Bronfenbrenner, 1977; Bronfenbrenner and Morris, 2006) and the integrative model (García Coll et al., 1996) indicate that sociodemographic characteristics, including age, sex, and, in particular, race and ethnicity, can influence families' experiences in the environments they inhabit, and, thereby, their experiences of distress and TSS. Thus, identifying sociodemographic characteristics, as well as sociodemographic risk factors, associated with higher levels of child distress and TSS in parents during cancer treatment would allow us to more readily identify families that may benefit most from AME. This would have implications for participant screening, recruitment, and clinical service delivery. Therefore, in the current study we examined the associations of child distress (with cancer-related hospitalizations/treatment) and parent traumatic stress symptoms with: (1) child and parent (or guardian) sociodemographic characteristics, and (2) sociodemographic risk factors.
Method
This secondary analysis used data collected during a multisite trial examining mediators and moderators of AME, a music-based intervention designed to lower distress and improve health outcomes in children (ages 3–8 years) with cancer and their parents (R01NR1578). The Institutional Review Board of Indiana University (study identification #1511888386) approved all data collection procedures. For this study, we examined moderators of AME effects for parent TSS identified in the main trial (Robb et al., 2023a), along with sociodemographic information. Moderators included parent scores on a traumatic stress screener (PCL-6; Lang et al., 2012) and parent-reports of child distress with cancer-related hospitalization/treatment (PIES; Phipps et al., 2005). These measures and the sociodemographic information were collected at baseline, following informed consent. To be included in the main trial, the parent had to be (1) the primary caregiver of a child (ages 3–8 years) undergoing active cancer treatment, (2) at least 18 years of age at the time of consent, (3) able to be present for all intervention sessions, and (4) able to understand English. Active cancer treatment was defined as an expected treatment course of at least 3 days to receive moderate to high intensity chemotherapy (inpatient or outpatient).
Participants
Participants were N = 136 children (Mage = 4.88 years, SD = 1.56 years, 44.1% female) who were undergoing treatment for cancer. In all but six cases, the individual completing the study measures (see below) was the child's mother, stepmother, or foster mother (83.1% of measure respondents) or their father, stepfather, or foster father (12.5%). The remaining six respondents were children's guardians (in four cases) and/or grandparents or great-grandparents. On average, parents and guardians completing the study measures were 34.66 years old (SD = 7.00 years).
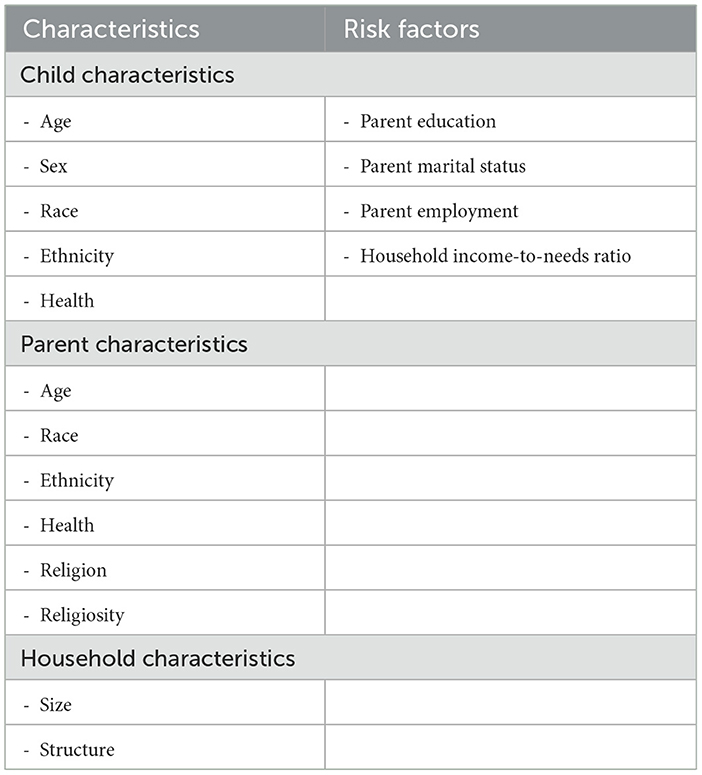
Table 1a displays the distribution of children as a function of their race and ethnicity. As can be seen in the table, although the majority of children were white (67.6%) and not Hispanic or Latino (15.4%), substantial numbers of children were identified as more than one race (17.6%) or Black or African American (10.3%), and 15.4% were identified as Hispanic or Latino. Similarly, while most parents and guardians identified as White (73.9%) and not as Hispanic or Latino (81.3%), 10.4% identified as Black or African American and 7.5% identified as more than one race and 13.4% of parents and guardians identified as Hispanic or Latino (see Table 1b). For purposes of analyses, child and parent race were coded dichotomously as not minoritized (White) or minoritized (not White). Similarly, child and parent ethnicity were coded as not minoritized (not Hispanic or Latino) or minoritized (Hispanic or Latino).
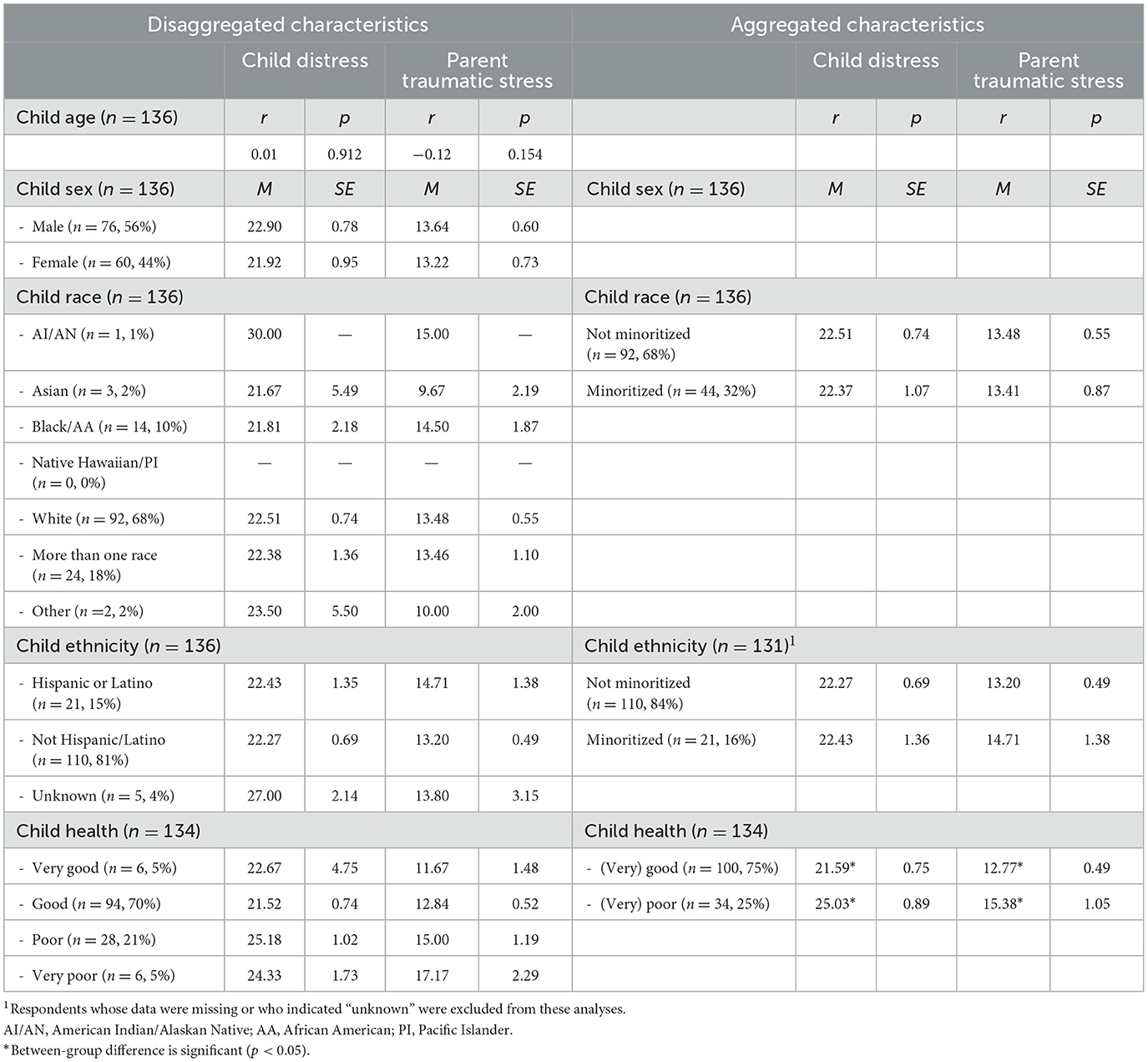
Table 1a. Levels of child distress with prior hospitalizations and parent traumatic stress as a function of child sociodemographic characteristics.
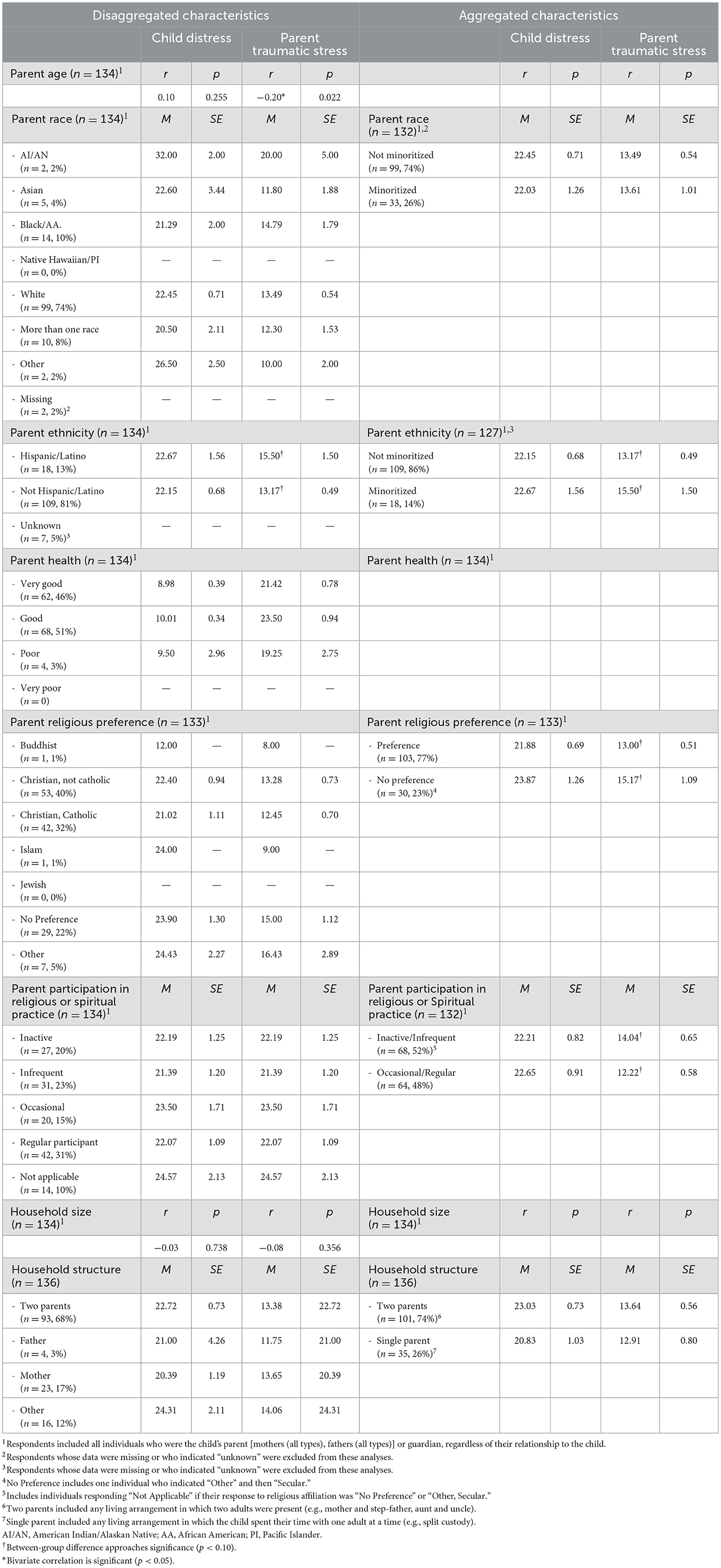
Table 1b. Levels of distress with prior hospitalizations and post-traumatic stress as a function of parent sociodemographic characteristics.
Measures
As noted above, children's parents (or guardians) completed a series of measures at baseline, including a family information form that captured child and respondent demographics, as well as child and respondent health, religion and religiosity, and household size and structure, and the PIES (Phipps et al., 2005) and PCL-6 (Lang et al., 2012). Each item for the PIES was answered on a five-point scale, with higher scores indicating higher levels of distress. Following the scoring guidelines for the PIES, child and parent distress scores were calculated as the sum of items 1 to 8 and 9 to 11, respectively. Each item for the PCL-6 was also answered on a five-point scale (Not at all = 1 to Extremely = 5) and an overall severity score was calculated as the sum of item responses (see Robb et al., 2023b; Supplementary Table 2 for the psychometric properties of this measure). An overall severity score of 14 or more indicates a high level of symptoms, and in this trial such a score triggered a referral to a social worker for additional support.
Four items from the family information form assessed factors that have commonly been used as indicators of sociodemographic risk in studies of pediatric cancer (e.g., Bemis et al., 2015) and in the developmental science literature more broadly (e.g., Burchinal et al., 2008): parental education, parental partner status, parental employment, and household income. The distribution of parents' and guardians' responses for each of these items is displayed in Table 2. Responses for each item were dichotomously recoded as indicative of sociodemographic risk or not based on thresholds used in prior research (Gassman-Pines and Yoshikawa, 2006; Holochwost et al., 2016). Thus, parental or guardian education of high school or less was coded as indicative of risk, as was single partner status and unemployment.
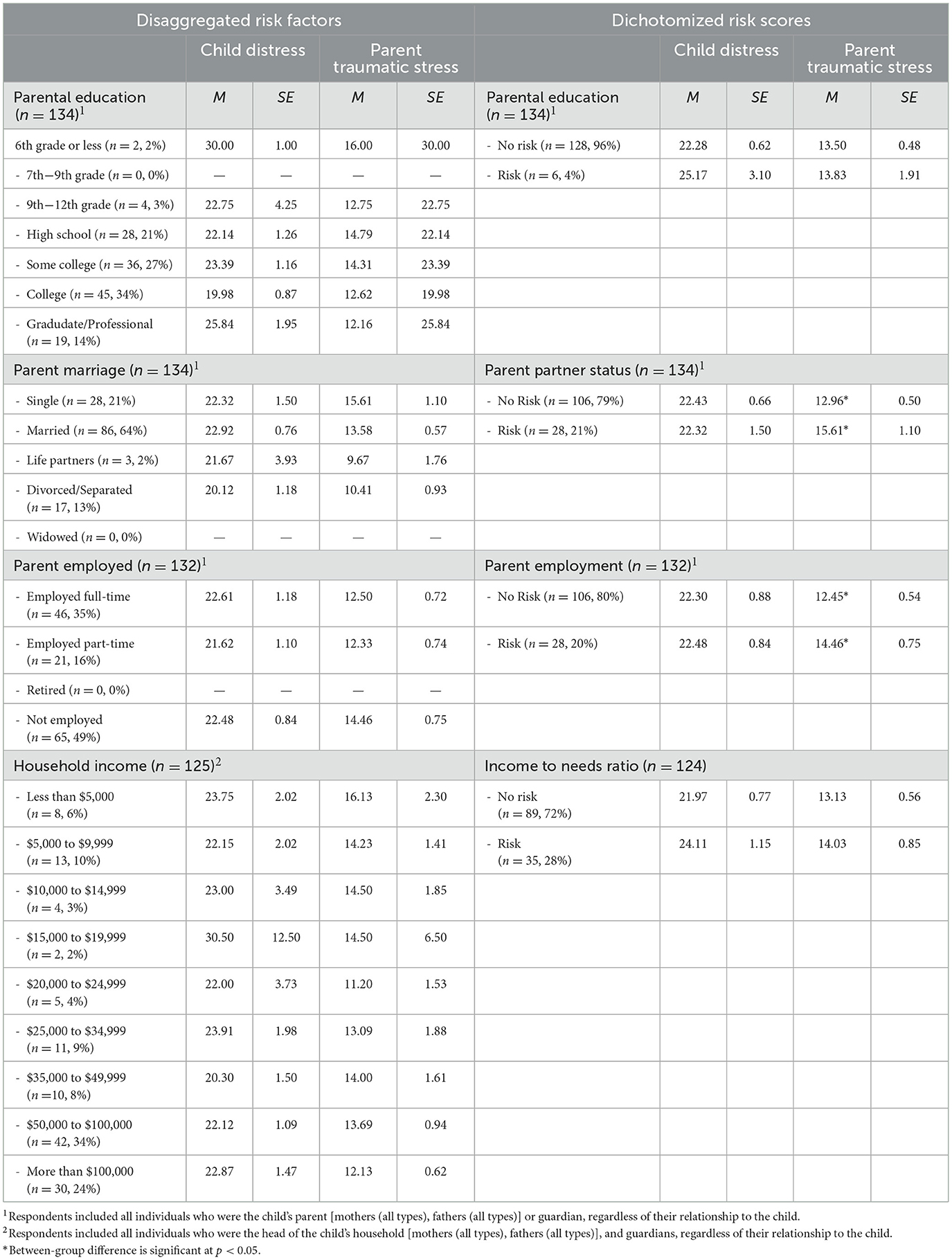
Table 2. Levels of distress with prior hospitalizations and post-traumatic stress as a function of sociodemographic risk.
Prior to dichotomization, household income was recoded as income-to-needs ratios (McLoyd, 1998). This was accomplished by taking the mid-point of the range respondents used to indicate household income (e.g., $7,500 for the range “$5,000 to $9,999”) or the minimum (“less than $5,000”) or maximum values (“more than $100,000”) when those were endorsed and then dividing that figure by the federal poverty level (FPL) for a household corresponding to the reported size for the year in which each family participated in the study. Thus, a family with an income corresponding precisely to the FPL would have an income-to-needs ratio (INR) of 1.0. An INR < 1.0 is indicative of sociodemographic risk (Gassman-Pines and Yoshikawa, 2006).
The four dichotomously coded risk factors were summed to yield a cumulative sociodemographic risk score for each family that provided data on all four risk factors (Burchinal et al., 2000). The mean level of cumulative risk was 1.03 (SD = 1.00). Forty-four families (35.2% for whom risk scores could be calculated) had a risk score of 0; the remaining families had scores of 1 (n = 48, 38.4%), 2 (n = 19, 15.2%), 3 (n = 13, 10.4%), or 4 (n = 1, 0.8%).
Data analyses
In the first, preliminary step of our analyses we examined indices of central tendency and variation in measures of child distress with prior hospitalization and parent traumatic stress scores. Given that both ecological systems theory (Bronfenbrenner and Morris, 2006) and the integrative model (García Coll et al., 1996) suggest that levels of cumulative sociodemographic risk may differ among members of minoritized racial and/or ethnic groups and their non-minoritized counterparts, we examined levels of cumulative risk as a function of minoritized racial and ethnic group identity to determine whether subsequent analyses in which cumulative risk was the focal predictor should include minoritized racial and/or ethnic group identity.
To examine the associations of child distress and parent traumatic stress with sociodemographic characteristics we first examined mean levels of distress as a function of each sociodemographic characteristic that was coded categorically (e.g., child race) and the bivariate correlation between levels of distress and each continuous characteristic (e.g., child age). All sociodemographic characteristics included in our analyses are listed in Table 3. A series of four multivariable linear regression models were then estimated to examine the unique associations of sociodemographic characteristics with levels of child distress (Models 1a and 1b) and parent traumatic stress symptoms (Models 2a and 2b). Each model included as independent variables the sociodemographic characteristics identified via the preliminary analyses as being associated with the dependent variable in question at a rate achieving or approaching significance (p < 0.10). To reduce the standard errors for each correlation coefficient, the aggregated versions of these characteristics were included rather than the disaggregated versions. The final model in each set included cumulative risk as a covariate in the form suggested by the nature of the association between cumulative risk and child distress or parent traumatic stress (see Figures 1, 2 below).
![Plot showing child distress with prior hospitalization as a function of cumulative risk scores (range=0, 4). Families with risk scores of 0 and 1 reported lower distress, while families with scores of 2 and 3 reported higher distress. A significant difference is noted between scores [0-1] and [2-3] with p-value .048.](https://www.frontiersin.org/files/Articles/1550051/fpsyg-16-1550051-HTML/image_m/fpsyg-16-1550051-g001.jpg)
Figure 1. Association between cumulative sociodemographic risk and child distress with prior hospitalizations.
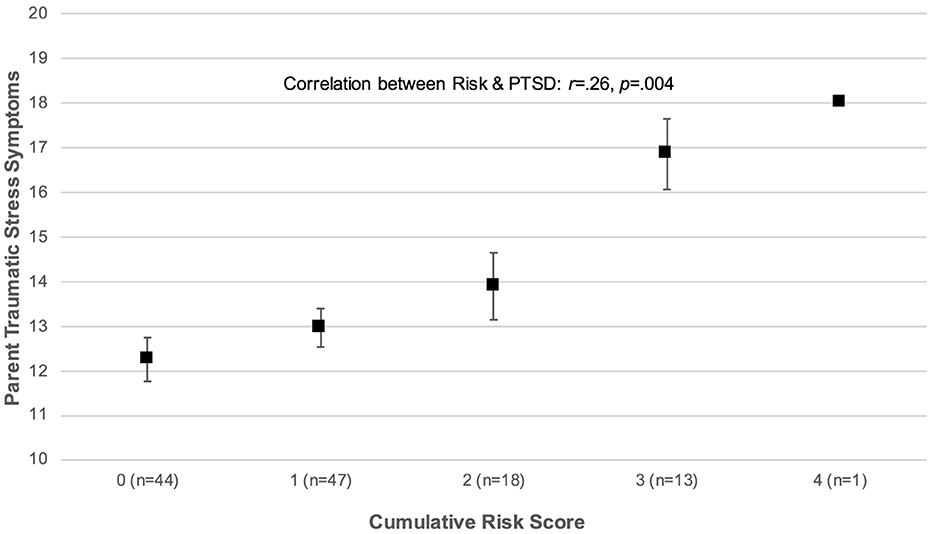
Figure 2. Association between cumulative sociodemographic risk and parent traumatic stress symptoms.
The associations of child distress and parent traumatic stress with sociodemographic risk were investigated in a similar fashion. We first examined mean levels of distress and traumatic stress as a function of each sociodemographic risk factor listed in Table 3 is both its original and dichotomized forms, and then examined the distribution of these scores as a function of cumulative sociodemographic risk. Six multivariable regression models were then estimated to examine the associations between sociodemographic risk and child distress (Models 3a through 3c), and between risk and parent traumatic stress symptoms (Models 4a through 4c). The first model in each set (Model a) examined the association between cumulative sociodemographic risk scores and the dependent variable in question; the next model in each set (Model b) examined the association of cumulative risk and the dependent variable while controlling for minoritized race, given that our preliminary analyses revealed a significant association between minoritized race and cumulative risk scores. The final model in each set (Model c) replaced the cumulative risk score with the dichotomized versions of the four risk factors that comprised the score (per Bemis et al., 2015), given that each risk factor may not exhibit an association of equal strength with distress or traumatic stress (Brown et al., 2021).
All analyses were conducted using SPSS (v. 28). Given the very low prevalence of missing data, the essentially descriptive nature of the analyses, and the fact that all other analyses were multivariate regressions (for which listwise deletion is robust to violations of the assumption that data are missing at random; Allison, 2002), missing data were accommodated using listwise deletion.
Results
Preliminary results
Parents and guardians (n = 134) reported a mean child distress score of 22.49 (SD = 6.99) out of a maximum possible score of 45. The average level of TSS was 13.37 (SD = 5.40) out of a maximum possible score of 30. Levels of cumulative risk were significantly higher among families in which children were identified as members of minoritized racial groups [t(121)= 2.78, p = 0.006]. A parallel association was not observed for ethnicity (p = 0.613).
Associations of child distress and parent traumatic stress with sociodemographic characteristics
The distributions of child distress scores and TSS by child sociodemographic characteristics are displayed in Table 1a. As can be seen in the table, there was no association between these scores and children's age or aggregated race (not minoritized vs. minoritized). However, children who were rated as being in poor or very poor health had significantly higher child distress scores [t(132) = −2.49, p = 0.014], and parents or guardians of these children reported significantly higher TSS [t(132) = −2.50, p = 0.014].
The distributions of child distress scores and TSS as a function of parent or guardian sociodemographic characteristics are presented in Table 1b. Parents and guardians who were younger reported significantly higher levels of TSS [r(134) = −0.20, p = 0.022], and parents and guardians who were Hispanic or Latino also reported higher TSS at a rate approaching significance [t(125) = −1.67, p = 0.098]. Parents and guardians who reported no religious preference reported higher TSS at a rate approaching significance [t(131) = 1.95, p = 0.053]. Parallel associations were observed when considering the frequency with which parents' and guardians' engaged in their religious or spiritual practice: those who reported that they were inactive or infrequent participants reported higher levels of TSS [t(128) = 1.96, p = 0.052) at a rate approaching significance when compared to parents and guardians who were occasional or regular participants.
A series of multivariable linear regression models revealed that poorer child health was associated with significantly higher levels of child distress (see Table 4, Model 1a: B = 3.44, SE = 1.38, p = 0.014) and that this association was observed after including cumulative risk as a covariate (Model 1b: B = 3.59, SE = 1.44, p = 0.014). Child health and the frequency of participation in religious or spiritual practice were the most salient sociodemographic characteristics when considering parents' and guardians' TSS. More frequent participation was associated with lower levels of TSS (Model 2a: B = –2.00, SE = 0.86, p = 0.022), and this association held after controlling for levels of cumulative risk (Model 2b: B = –2.12, SE = 0.89, p = 0.019). Poorer child health was also associated with higher levels of TSS before (Model 2a: B = 2.30, SE = 1.00, p = 0.023) and after controlling for risk scores (Model 2b: B = 2.70, SE = 1.01, p = 0.009).
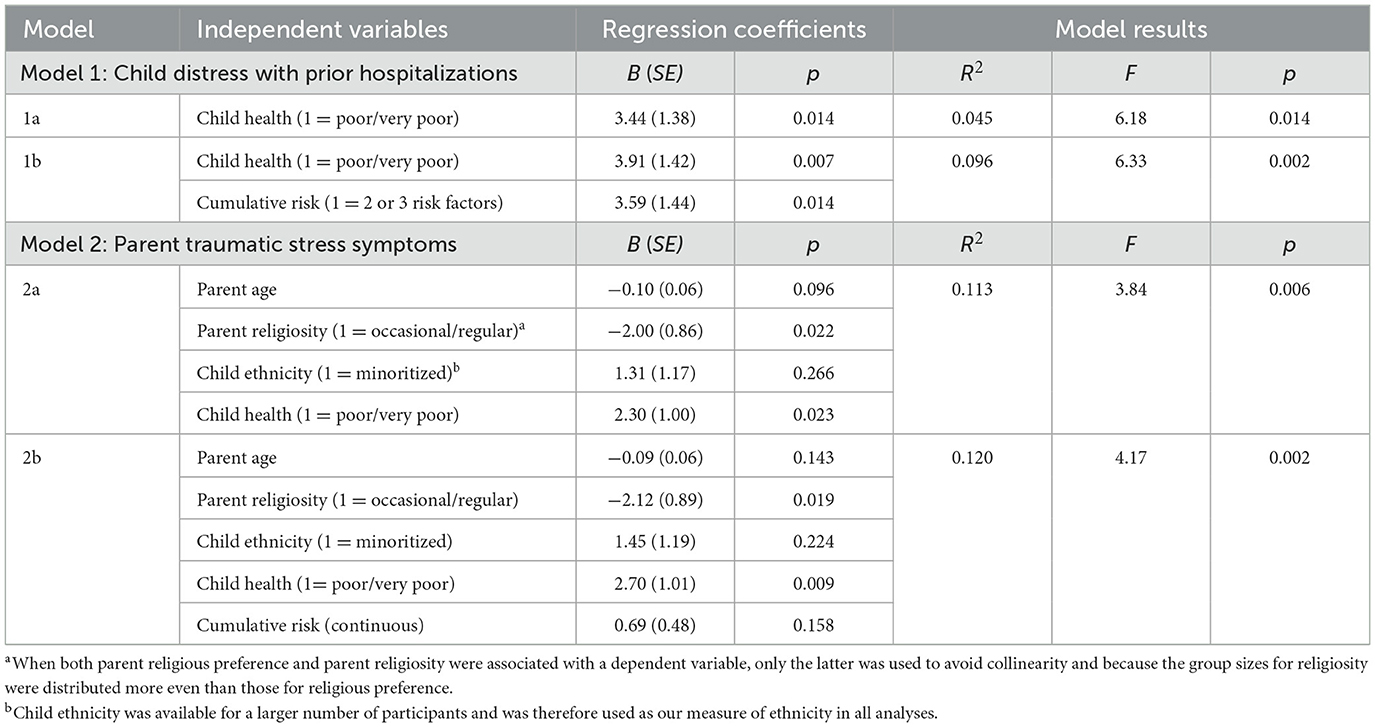
Table 4. Regressing levels of child distress with prior hospitalizations and parent traumatic stress symptoms on sociodemographic characteristics.
Associations of child distress and parent traumatic stress with sociodemographic risk
Table 2 presents child distress scores and TSS as a function of disaggregated and dichotomized risk factors. Although levels of child distress scores were higher for parents and guardians categorized as being at risk on the basis of their education, partner status, employment, and income-to-need ratios, these differences were not significant. However, TSS were significantly higher among parents and guardians who were categorized as being at risk on the basis of their partner status [t(132) = −2.34, p = 0.021] or their employment [t(130) = −2.19, p = 0.030].
Figure 1 displays levels of child distress as a function of cumulative sociodemographic risk. The figure suggests a non-linear association, such that there was a significant difference in child distress scores among families confronting 0 or 1 risk factors, relative to those confronting 2 or 3 factors [t(120) = −1.99, p = 0.048]. Therefore, subsequent analyses of the association between cumulative risk and child distress used a categorically-recoded risk as the focal predictor (0 = 0 or 1 risk factors; 1 = 2 or 3 risk factors). Figure 1 also revealed the presence of a bivariate outlier in the associations between cumulative risk and child distress as defined by Tukey (1977): the same respondent received a cumulative risk score of 4 but reported relatively low levels of child distress. This individual was excluded from subsequent analyses of the associations between sociodemographic risk and distress, given the potential for bivariate outliers to bias model estimates (Zimmerman, 1994). The distribution of parent and guardian TSS scores as a function of cumulative risk is displayed in Figure 2, and this distribution clearly depicts a positive, linear association between risk and TSS with no evidence of bivariate outliers [r(123) = 0.26, p = 0.004].
The results of the multivariable linear regression models indicated that although higher levels of categorically-coded cumulative risk scores were associated with significantly higher levels of child distress (see Table 5, Model 3a: B = 2.91, SE = 1.46, p = 0.048), adding minoritized child race as a covariate yielded overall model results that were not statistically significant [Model 3b: R2 = 0.035, F(2, 119) = 2.14, p = 0.122]. Replacing cumulative risk scores with the set of four risk factors to predict child distress resulted in a model that accounted for ~10% of the variance in child distress scores [Model 3c: R2 = 0.099, F(4, 99) = 2.72, p = 0.034], and families whose income-to-needs ratios were categorized as indicative of risk reported significantly higher levels of child distress after controlling for the categorization of the other three risk factors (B = 3.50, SE = 1.49, p = 0.021).
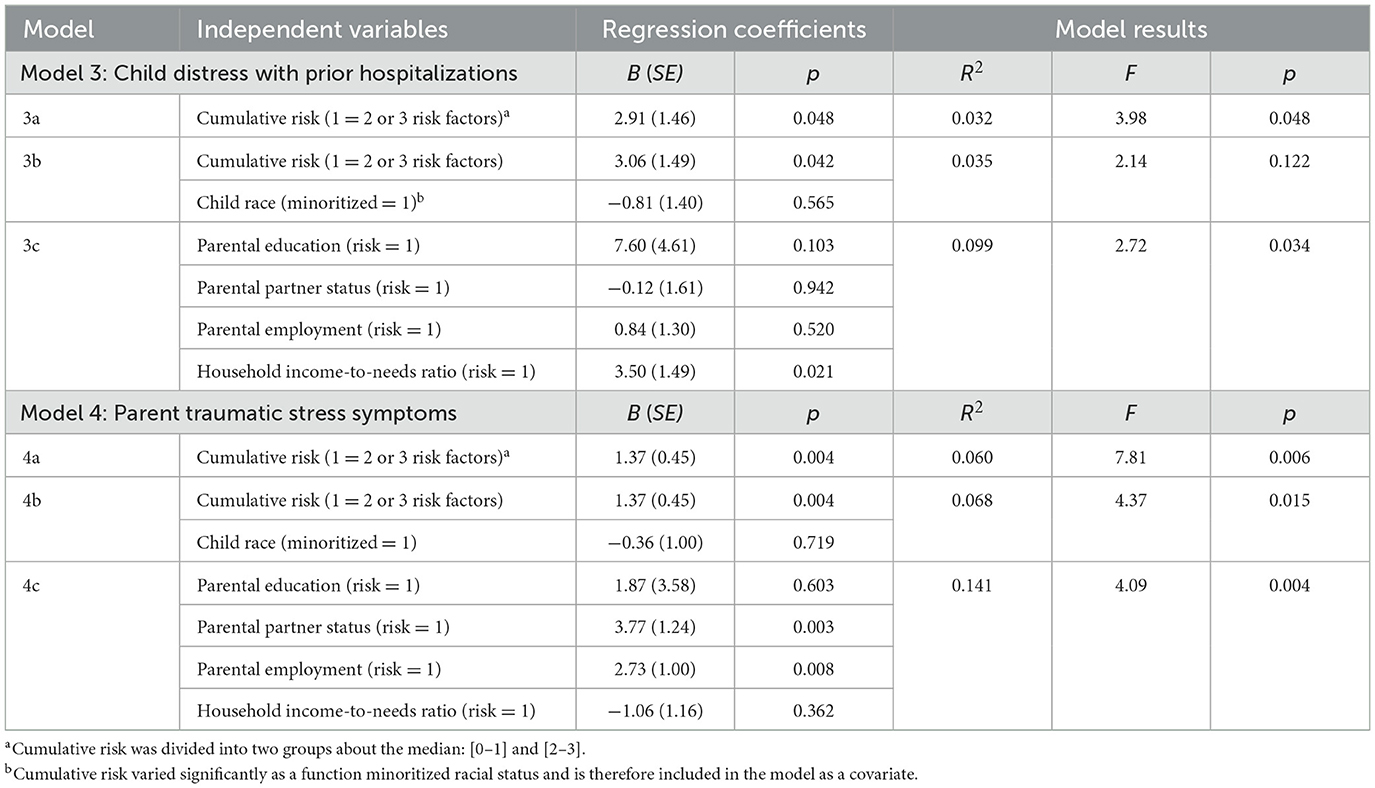
Table 5. Regressing levels of distress with prior hospitalizations and parent traumatic stress symptoms on sociodemographic risk.
Higher levels of cumulative risk were also associated with higher levels of TSS (Model 4a: B = 1.37, SE = 0.45, p = 0.004), and this association held after controlling for whether children were members of a minoritized racial group (Model 4b: B = 0.44, SE = 0.20, p = 0.025). Replacing cumulative risk scores with the dichotomized versions of each risk factor resulted in a model that accounted for substantially more variance in TSS scores [Model 4c: R2 = 0.141, F(4, 100) = 4.09, p = 0.004]. At risk categorizations of partner status (Model 4c: B = −3.77, SE = 1.24, p = 0.003) and employment (Model 4c: B = 2.73, SE = 1.00, p = 0.008) were each associated with significantly higher TSS scores.
Discussion
In our primary study, parents who derived the most benefit from an AME intervention reported high distress for their child and elevated traumatic stress symptoms for themselves (Robb et al., 2023b). The purpose of this secondary analysis was to better understand these parents by identifying sociodemographic characteristics and risk factors that were associated with higher levels of child distress and parent TSS. These findings provide additional information to guide subsequent research and the work of pediatric music therapists.
Our examination of sociodemographic characteristics showed that parents who rated their child's health as poor reported significantly higher distress in their child and higher TSS for themselves. In addition, these associations were robust to controls for cumulative risk and other sociodemographic characteristics that our preliminary analyses suggested may be related to TSS (i.e., parent age and minoritized child ethnicity). The finding that poor child health had a significant association with child distress is not surprising, but it is unclear how parents interpreted this question. Parent perceptions of their child's health during cancer treatment is influenced by numerous factors including their prognosis, treatment intensity, the presence or absence of side effects, social support, and cancer-related distress exhibited by their child (Patterson et al., 2004; Price et al., 2016; Schwartz-Attias et al., 2024). The PIES measures a child's distress with cancer and treatment-related experiences such as medical procedures, chemotherapy, hospitalization, and staff relationships (Phipps et al., 2005). As such, we would expect that parents who observe that their child is demonstrating more difficulties with their cancer treatment might also rate their child as having poor health. Importantly, poor child health also had a significant association with parent TSS. These findings are consistent with studies that have established parent perceptions about their child's health and wellbeing as a strong predictor of parent TSS during cancer treatment (Brosbe et al., 2011; Feng et al., 2024; Kahana et al., 2006; Norberg et al., 2012; Price et al., 2016) and offers an additional marker for identifying parents who may benefit from the AME intervention.
We also found that the frequency of parents' religious or spiritual practice had a significant association with TSS, such that more regular religious or spiritual practice was associated with lower levels of TSS. Researchers have explored the relationship of faith, religiosity, and spirituality to psychological distress. However, religiosity and spirituality are not the same, and neither of these complex, multi-dimensional constructs can be represented by religious practice alone (Villani et al., 2019). That said, participating in religious activities can provide a sense of community, bonding, and support for individuals and families (Dunbar, 2021), as religious communities often provide resources such as food, emotional support, material help, and social networking (Dolan et al., 2021). As such, the frequency of regular religious or spiritual practice may reflect the degree of social support families receive, and social support has been identified as an important factor that contributes to reduced psychological distress in parents during cancer treatment (Feng et al., 2024; Melguizo-Garín et al., 2023, 2022; Sloper, 2000; Schwartz-Attias et al., 2024; Tremolada et al., 2013).
Our analyses of the associations between sociodemographic risk factors (education, partner status, employment, and household income-to-needs ratios) and child distress indicated that families who experienced higher levels of cumulative risk (a score of 2 our greater) reported more distress in their child, relative to families who experienced lower levels of risk (a score of 1 or lower), and that this association was robust to controls for minoritized race. These findings are consistent with those reported by Bemis et al. (2015), who found that greater sociodemographic disadvantage predicted higher levels of distress for mothers of children with cancer, but that race was not associated with child or parent distress. Our analyses also indicated that including each sociodemographic factor together in one regression model accounted for a larger amount of the variance in child distress scores (~10%) than the cumulative risk score (~4%). In the former model, only income to needs ratio was associated with child distress, such that families with household incomes below the federal poverty level (i.e., families in poverty) reported significantly higher child distress. This finding is broadly consistent with the family stress model, which asserts that the stress associated with living in poverty may undermine parents' capacity to provide optimal emotional support for their children (Conger et al., 1994), and the stress of poverty is undoubtedly exacerbated by the economic and emotional burden of having a child with cancer (Bona et al., 2014; Eche-Ugwu et al., 2024).
We also observed a significant association between higher cumulative risk scores and higher TSS in parents. As with child distress, this association was robust to controls for minoritized race, and including each factor together in one regression model accounted for a larger portion of the variance in traumatic stress symptoms (~14%) than the cumulative risk score alone (~7%). In the model including each factor simultaneously, single partner status and parental unemployment were both significantly associated with higher levels of TSS. These findings are also consistent with those reported by Bemis et al. (2015), who found a significant association between single parenthood with greater TSS in parents of children with cancer. Like the frequency of participation in religious or spiritual practice, marital status and employment may signal the importance of social support for parents of children with cancer. Numerous studies (e.g., Klassen et al., 2012; Lundgren et al., 2023), have reported the isolating potential of childhood cancer treatment for parents. This is especially true for young children where one parent may be dedicated to the daily care of their hospitalized child, which may isolate them from family and their social networks, including coworkers. Being an unpartnered parent may compound this sense of isolation and stress (Granek et al., 2014).
This finding underscores the importance of recent studies examining the important role of music as social support for families of young children with cancer (Boyde et al., 2024; Giordano et al., 2021; Harman and Shoemark, 2024; Heiderscheit, 2022; Silberstein et al., 2024; Uggla et al., 2019). Musical engagement in both clinical and community settings has been found to increase social connectedness, decrease social isolation, and support relationships (Bourdaghs and Silverman, 2020; Loi et al., 2022; Murphy and McFerran, 2017). Although we could not identify any pediatric cancer studies that have explored sociodemographic factors associated with benefits from music therapy, a study of adult patients found that terminally ill, non-partnered cancer patients and patients without children reported greater improvements to their mood and feeling understood following a course of music therapy (Kordovan et al., 2016).
This study is not without limitations. By their nature, cumulative risk models endorse the concept of equifinality (Evans et al., 2013; Evans, 2003) whereby pathways may lead to the same (or at similar) outcomes (Cicchetti and Rogosch, 1996). However, it is possible that there may be specificity in the associations between risk factors and different outcomes, such that the association between a given risk factor and a given outcome is different in its strength or nature than the association between that risk factor and another outcome. Our results suggest that this is the case for child distress and parent TSS: while levels of cumulative sociodemographic risk predict child distress and TSS, there is also specificity in the associations between sociodemographic risk factors and each of these outcomes.
Moreover, data on each of the sociodemographic characteristics and risk factors included in our analyses were based on parents' or guardians' responses to a single item. While this may be appropriate for certain constructs (e.g., partner status), a single item cannot adequately assess complex, multidimensional constructs such as religious and spiritual practice (Villani et al., 2019). Finally, this analysis used cross sectional data collected during a single time point and does not investigate how these correlations may change over time. We know that distress patterns will change over the cancer treatment trajectory (Galtieri et al., 2024; Price et al., 2016), and as such, repeated and holistic assessment is best practice (Kazak et al., 2015; Pai et al., 2019).
Conclusions and recommendations
The impact of poverty and social support on child and parent distress is well established. Findings from the current study serve to expand our understanding of parents who reported lower TSS following AME. Our findings suggest that parent perceptions of their child's health are an important driver for both child distress and parent TSS, and AME may be particularly helpful for these families given our finding that changes in parent perceptions of their child's health and wellbeing is a likely mediator of AME effects (Robb et al., 2023b). We also found that families already experiencing sociodemographic disadvantage may derive more benefit from AME than families who present with less disadvantage, but that specific risk factors may differentiate parents who report higher levels of child distress from those who report higher TSS. These findings suggest the benefit of using these particular risk factors when attempting to identify families that may benefit from AME and the use of additional measures to assess these specific risk factors in greater detail. Finally, frequency of religious practice, unemployment, and being a single parent were associated with higher parent TSS and suggest that AME may bring an important form of social support to children and parents.
This is informative to AME implementation studies and clinical practice, and efforts to provide evidence-based care to families. In addition to considering sociodemographic risk factors, and consistent with the Standards for Psychosocial Care in Pediatric Cancer (Knott et al., 2022; Wiener et al., 2015), we recommend repeated screening of child and parent distress to identify changing needs and facilitate prompt referrals for AME and other supportive care services. We also recommend measuring social support as a potential moderator of AME benefit in future trials and the inclusion of modestly expanded item sets to index multidimensional constructs.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions. The de-identified data supporting the conclusions of this article can be obtained from the corresponding author via a written data-sharing agreement. Requests to access these datasets should be directed to c2hyb2JiQGl1LmVkdQ==.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Indiana University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
SH: Conceptualization, Writing – original draft, Writing – review & editing. EH: Writing – original draft, Writing – review & editing. KS: Writing – original draft, Writing – review & editing. SJ: Writing – review & editing. SR: Project administration, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The primary study was funded by a grant from the National Institute of Nursing Research (R01NR1578). Additional funding for this analysis was provided by the Walther Cancer Foundation through an endowed visiting professorship to Steven J. Holochwost and by a grant from the National Cancer Institute (T32CA117865) to Elizabeth Harman. Special thanks to the children and families who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Appleyard, K., Egeland, B., Van Dulmen, M. H., and Alan Sroufe, L. (2005). When more is not better: the role of cumulative risk in child behavior outcomes. J. Child Psychol. Psychiatr. 46, 235–245. doi: 10.1111/j.1469-7610.2004.00351.x
Bakula, D. M., Sharkey, C. M., Perez, M. N., Espeleta, H. C., Gamwell, K. L., Baudino, M., et al. (2020). The relationship between parent distress and child quality of life in pediatric cancer: a meta-analysis. J. Pediatr. Nurs. 50, 14–19. doi: 10.1016/j.pedn.2019.09.024
Bates, R. A., Militello, L., Barker, E., Villasanti, H. G., and Schmeer, K. (2022). Early childhood stress responses to psychosocial stressors: the state of the science. Dev. Psychobiol. 64:e22320. doi: 10.1002/dev.22320
Bemis, H., Yarboi, J., Gerhardt, C. A., Vannatta, K., Desjardins, L., Murphy, L. K., et al. (2015). Childhood cancer in context: sociodemographic factors, stress, and psychological distress among mothers and children. J. Pediatr. Psychol. 40, 733–743. doi: 10.1093/jpepsy/jsv024
Biard, M., Crouse, C., and Krater, C. (2025). Pediatric music therapy in the United States: a subsequent inquiry. J. Hosp. Administr. 14, 20–33. doi: 10.5430/jha.v14n1p20
Bona, K., Dussel, V., Orellana, L., Kang, T., Geyer, R., Feudtner, C., et al. (2014). Economic impact of advanced pediatric cancer on families. J. Pain Symptom Manag. 47, 594–603. doi: 10.1016/j.jpainsymman.2013.04.003
Bourdaghs, S., and Silverman, M. J. (2020). A neurological rationale for music therapy to address social connectivity among individuals with substance use disorders. Arts Psychother. 70:101681. doi: 10.1016/j.aip.2020.101681
Boyde, C., Berger, B., Längler, A., Neugebauer, L., Jacobsen, S. L., Swanick, R., et al. (2024). Interaction-focused music therapy with cancer-affected children and their significant others: a randomized controlled feasibility study with subsequent intervention (INMUT). Pilot Feasibility Stud. 10:86. doi: 10.1186/s40814-024-01490-8
Bradt, J., Dileo, C., Myers-Coffman, K., and Biondo, J. (2021). Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst. Rev. 10:CD006911. doi: 10.1002/14651858.CD006911.pub4
Bronfenbrenner, U. (1977). Toward and experimental ecology of human development. Am. Psychol. 32, 513–531. doi: 10.1037/0003-066X.32.7.513
Bronfenbrenner, U., and Morris, P. A. (2006). “The bioecological model of human development,” in Handbook of Child Psychology: Theoretical Models of Human Development, Vol. 1, 6th Edn. (Hoboken, NJ: John Wiley and Sons, Inc), 793–828.
Brosbe, M. S., Hoefling, K., and Faust, J. (2011). Predicting posttraumatic stress following pediatric injury: a systematic review. J. Pediatr. Psychol. 36, 718–729. doi: 10.1093/jpepsy/jsq115
Brown, E. D., Holochwost, S. J., Laurenceau, J. P., Garnett, M. L., and Anderson, K. E. (2021). Deconstructing cumulative risk: poverty and aspects of instability relate uniquely to young children's basal cortisol. Child Dev. 92, 1067–1082. doi: 10.1111/cdev.13512
Bruce, M. (2006). A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin. Psychol. Rev. 26, 233–256. doi: 10.1016/j.cpr.2005.10.002
Burchinal, M., Vernon-Feagans, L., Cox, M., and Investigators, K. F. L. P. (2008). Cumulative social risk, parenting, and infant development in rural low-income communities. Parenting 8, 41–69. doi: 10.1080/15295190701830672
Burchinal, M. R., Roberts, J. E., Hooper, S., and Zeisel, S. A. (2000). Cumulative risk and early cognitive development: a comparison of statistical risk models. Dev. Psychol. 36:793. doi: 10.1037/0012-1649.36.6.793
Cicchetti, D., and Rogosch, F. A. (1996). Equifinality and multifinality in developmental psychopathology. Dev. Psychopathol. 8, 597–600. doi: 10.1017/S0954579400007318
Conger, R. D., Ge, X., Elder Jr, G. H., Lorenz, F. O., and Simons, R. L. (1994). Economic stress, coercive family process, and developmental problems of adolescents. Child Dev. 65, 541–561. doi: 10.2307/1131401
De Young, A. C., Paterson, R. S., Brown, E. A., Egberts, M. R., Le Brocque, R. M., Kenardy, J. A., et al. (2021). Topical review: medical trauma during early childhood. J. Pediatr. Psychol. 46, 739–746. doi: 10.1093/jpepsy/jsab045
Dolan, J. G., Hill, D. L., Faerber, J. A., Palmer, L. E., Barakat, L. P., and Feudtner, C. (2021). Association of psychological distress and religious coping tendencies in parents of children recently diagnosed with cancer: a cross-sectional study. Pediatr. Blood Cancer 68:e28991. doi: 10.1002/pbc.28991
Dunbar, R. I. (2021). Religiosity and religious attendance as factors in wellbeing and social engagement. Religion Brain Behav. 11, 17–26. doi: 10.1080/2153599X.2020.1712618
Eche-Ugwu, I. J., Orellana, L., Becker, D., Bona, K., Avery, M., Feudtner, C., et al. (2024). Household material hardship and distress among parents of children with advanced cancer: a report from the PediQUEST response trial. Cancer 130, 3540–3548. doi: 10.1002/cncr.35432
Evans, G. W. (2003). A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev. Psychol. 39:924. doi: 10.1037/0012-1649.39.5.924
Evans, G. W., Li, D., and Whipple, S. S. (2013). Cumulative risk and child development. Psychol. Bull. 139:1342. doi: 10.1037/a0031808
Facchini, M., and Ruini, C. (2021). The role of music therapy in the treatment of children with cancer: a systematic review of literature. Complementary therapies in clinical practice 42:101289. doi: 10.1016/j.ctcp.2020.101289
Feng, S., Zhang, L., Lin, J., Sun, R.-W., Wang, R.-N., Qu, H.-F., et al. (2024). The mediating effect of positive expectations in the relationship between social support and post-traumatic stress disorder symptoms among parents of children with acute lymphoblastic leukemia. J. Psychiatr. Res. 176, 198–204. doi: 10.1016/j.jpsychires.2024.05.059
Galtieri, L. R., Perez, M. N., and Barakat, L. P. (2024). Quality of life of caregivers at the end of their child's pediatric cancer treatment: cancer-specific worry and material hardship. J. Pediatr. Psychol. 49, 348–355. doi: 10.1093/jpepsy/jsae014
García Coll, C., Lamberty, G., Jenkins, R., McAdoo, H. P., Crnic, K., Wasik, B. H., et al. (1996). An integrative model for the study of developmental competencies in minority children. Child Dev. 67, 1891–1914. doi: 10.2307/1131600
Gassman-Pines, A., and Yoshikawa, H. (2006). The effects of antipoverty programs on children's cumulative level of poverty-related risk. Dev. Psychol. 42:981. doi: 10.1037/0012-1649.42.6.981
Giordano, F., Rutigliano, C., De Leonardis, F., Rana, R., Neri, D., Brienza, N., et al. (2021). Covid-19 and absence of music therapy: Impact on mother-child dyad during invasive procedures in pediatric oncology. Arts Psychother. 75:101839. doi: 10.1016/j.aip.2021.101839
González-Martín-Moreno, M., Garrido-Ardila, E. M., Jiménez-Palomares, M., Gonzalez-Medina, G., Oliva-Ruiz, P., and Rodríguez-Mansilla, J. (2021). Music-based interventions in paediatric and adolescents oncology patients: a systematic review. Children 8:73. doi: 10.3390/children8020073
Graf, A., Bergstraesser, E., and Landolt, M. A. (2013). Posttraumatic stress in infants and preschoolers with cancer. Psychooncology 22, 1543–1548. doi: 10.1002/pon.3164
Granek, L., Rosenberg-Yunger, Z., Dix, D., Klaassen, R., Sung, L., Cairney, J., et al. (2014). Caregiving, single parents and cumulative stresses when caring for a child with cancer. Child 40, 184–194. doi: 10.1111/cch.12008
Greening, L., Stoppelbein, L., and Cheek, K. (2017). Racial/ethnic disparities in the risk of posttraumatic stress disorder symptoms among mothers of children diagnosed with cancer and Type-1 diabetes mellitus. Psychol. Trauma 9:325. doi: 10.1037/tra0000230
Harman, E., and Shoemark, H. (2024). Patterns of toxic stress and trauma for pediatric Hematopoietic Stem Cell Transplantation (HSCT): creating a model of responsive intervention. J. Psychosoc. Oncol. 42, 457–472. doi: 10.1080/07347332.2023.2276966
Harper, F. W., Peterson, A. M., Uphold, H., Albrecht, T. L., Taub, J. W., Orom, H., et al. (2013). Longitudinal study of parent caregiving self-efficacy and parent stress reactions with pediatric cancer treatment procedures. Psychooncology 22, 1658–1664. doi: 10.1002/pon.3199
Heiderscheit, A. (2022). Feasibility and acceptability of patient and family directed active music making during pediatric bone marrow transplant process. Eur. J. Investig. Health Psychol. Educ. 12, 1867–1877. doi: 10.3390/ejihpe12120131
Holochwost, S. J., Gariépy, J.-L., Propper, C. B., Gardner-Neblett, N., Volpe, V., Neblett, E., et al. (2016). Sociodemographic risk, parenting, and executive functions in early childhood: the role of ethnicity. Early Child. Res. Q. 36, 537–549. doi: 10.1016/j.ecresq.2016.02.001
Kahana, S. Y., Feeny, N. C., Youngstrom, E. A., and Drotar, D. (2006). Posttraumatic stress in youth experiencing illnesses and injuries: an exploratory meta-analysis. Traumatology 12, 148–161. doi: 10.1177/1534765606294562
Kazak, A. E., Abrams, A. N., Banks, J., Christofferson, J., Didonato, S., Grootenhuis, M. A., et al. (2015). Psychosocial assessment as a standard of care in pediatric cancer. Pediatr. Blood Cancer 62, S426–S459. doi: 10.1002/pbc.25730
Kazak, A. E., and Baxt, C. (2007). Families of infants and young children with cancer: a post-traumatic stress framework. Pediatr. Blood Cancer 49, 1109–1113. doi: 10.1002/pbc.21345
Klassen, A. F., Gulati, S., Granek, L., Rosenberg-Yunger, Z. R., Watt, L., Sung, L., et al. (2012). Understanding the health impact of caregiving: a qualitative study of immigrant parents and single parents of children with cancer. Qual. Life Res. 21, 1595–1605. doi: 10.1007/s11136-011-0072-8
Knott, D., Biard, M., Nelson, K. E., Epstein, S., Robb, S. L., and Ghetti, C. M. (2020). A survey of music therapists working in pediatric medical settings in the United States. J. Music Ther. 57, 34–65. doi: 10.1093/jmt/thz019
Knott, D., Krater, C., Maclean, J., Robertson, K., Stegenga, K., and Robb, S. L. (2022). Music therapy for chldren with oncology and hematological conditions and their families: advancing the standards of psychosocial care. J. Pediatr. Heamtol. Oncol. Nurs. 39, 49–59. doi: 10.1177/27527530211059726
Kordovan, S., Preissler, A., Kamphausen, A., Bokemeyer, C., and Oechsle, K. (2016). Prospective study on music therapy in terminally ill cancer patients during specialized inpatient palliative care. J. Palliat. Med. 14, 394–399. doi: 10.1089/jpm.2015.0384
Koyu, H. O., and Törüner, E. K. (2023). The effect of technology-based interventions on child and parent outcomes in pediatric oncology: a systemic review of experimental evidence. Asia-Pacific J. Oncol. Nurs. 10:100219. doi: 10.1016/j.apjon.2023.100219
Landolt, M. A., Ystrom, E., Sennhauser, F. H., Gnehm, H. E., and Vollrath, M. E. (2012). The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. J. Child Psychol. Psychiatr. 53, 767–774. doi: 10.1111/j.1469-7610.2011.02520.x
Lang, A. J., Wilkins, K., Roy-Byrne, P. P., Golinelli, D., Chavira, D., Sherbourne, C., et al. (2012). Abbreviated PTSD Checklist (PCL) as a guide to clinical response. Gen. Hosp. Psychiatr. 34, 332–338. doi: 10.1016/j.genhosppsych.2012.02.003
Loi, S. M., Flynn, L., Cadwallader, C., Stretton-Smith, P., Bryant, C., and Baker, F. A. (2022). Music and psychology & social connections program: protocol for a novel intervention for dyads affected by younger-onset dementia. Brain Sci. 12:503. doi: 10.3390/brainsci12040503
Lundgren, J., Thiblin, E., Lutvica, N., Reuther, C., Farrand, P., Woodford, J., et al. (2023). Concerns experienced by parents of children treated for cancer: a qualitative study to inform adaptations to an internet-administered, low-intensity cognitive behavioral therapy intervention. Psycho-Oncology 32, 237–246. doi: 10.1002/pon.6074
McLoyd, V. C. (1998). Socioeconomic disadvantage and child development. Am. Psychol. 53, 185. doi: 10.1037/0003-066X.53.2.185
Melguizo-Garín, A., Benítez-Márquez, M. D., Hombrados-Mendieta, I., and Martos-Méndez, M. J. (2023). Importance of social support of parents of children with cancer: a multicomponent model using partial least squares-path modelling. Int. J. Environ. Res. Public Health 20:1757. doi: 10.3390/ijerph20031757
Melguizo-Garín, A., Martos-Méndez, M. J., Hombrados-Mendieta, I., and Ruiz-Rodríguez, I. (2022). Relation between social support received and provided by parents of children, adolescents and young adults with cancer and stress levels and life and family satisfaction. Front. Psychol. 13:728733. doi: 10.3389/fpsyg.2022.728733
Murphy, M. A., and McFerran, K. (2017). Exploring the literature on music participation and social connectedness for young people with intellectual disability: A critical interpretive synthesis. J. Intellect. Disabil. 21, 297–314. doi: 10.1177/1744629516650128
Nakajima-Yamaguchi, R., Morita, N., Nakao, T., Shimizu, T., Ogai, Y., Takahashi, H., et al. (2016). Parental post-traumatic stress symptoms as predictors of psychosocial problems in children treated for cancer. Int. J. Environ. Res. Public Health 13:812. doi: 10.3390/ijerph13080812
Nguyen, T. N., Nilsson, S., Hellström, A. L., and Bengtson, A. (2010). Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomized clinical trial. J. Pediatr. Oncol. Nurs. 27, 146–155. doi: 10.1177/1043454209355983
Norberg, A. L., and Boman, K. K. (2013). Mothers and fathers of children with cancer: loss of control during treatment and posttraumatic stress at later follow-up. Psycho-Oncology 22, 324–329. doi: 10.1002/pon.2091
Norberg, A. L., Pöder, U., Ljungman, G., and Von Essen, L. (2012). Objective and subjective factors as predictors of post-traumatic stress symptoms in parents of children with cancer–A longitudinal study. PLoS ONE 7:e36218. doi: 10.1371/journal.pone.0036218
O'Callaghan, C., Baron, A., Barry, P., and Dun, B. (2011). Music's relevance for pediatric cancer patients: a constructivist and mosaic research approach. Support. Care Cancer 19, 779–788. doi: 10.1007/s00520-010-0879-9
Pai, A. L., Greenley, R. N., Lewandowski, A., Drotar, D., Youngstrom, E., and Peterson, C. C. (2007). A meta-analytic review of the influence of pediatric cancer on parent and family functioning. J. Family Psychol. 21:407. doi: 10.1037/0893-3200.21.3.407
Pai, A. L., and Kazak, A. E. (2006). Pediatric medical traumatic stress in pediatric oncology: family systems interventions. Curr. Opin. Pediatr. 18, 558–562. doi: 10.1097/01.mop.0000245358.06326.e9
Pai, A. L. H., Swain, A. M., Chen, F. F., Hwang, W. T., Vega, G., Carlson, O., et al. (2019). Screening for family psychosocial risk in pediatric hematopoietic stem cell transplantation with the psychosocial assessment tool. Biol. Blood Marrow Transplant. 25, 1374–1381. doi: 10.1016/j.bbmt.2019.03.012
Patterson, J. M., Holm, K. E., and Gurney, J. G. (2004). The impact of childhood cancer on the family: a qualitative analysis of strains, resources, and coping behaviors. Psycho-Oncology 13, 390–407. doi: 10.1002/pon.761
Phipps, S., Dunavant, M., Lensing, S., and Rai, S. N. (2005). Psychosocial predictors of distress in parents of children undergoing stem cell or bone marrow transplantation. J. Pediatr. Psychol. 30, 139–153. doi: 10.1093/jpepsy/jsi002
Pierce, L., Hocking, M. C., Schwartz, L. A., Alderfer, M. A., Kazak, A. E., and Barakat, L. P. (2017). Caregiver distress and patient health-related quality of life: psychosocial screening during pediatric cancer treatment. Psychooncology 26, 1555–1561. doi: 10.1002/pon.4171
Price, J., Kassam-Adams, N., Alderfer, M. A., Christofferson, J., and Kazak, A. E. (2016). Systematic review: a reevaluation and update of the integrative (Trajectory) model of pediatric medical traumatic stress. J. Pediatr. Psychol. 41, 86–97. doi: 10.1093/jpepsy/jsv074
Robb, S. L. (2000). The effect of therapeutic music interventions on the behavior of hospitalized children in isolation: developing a contextual support model of music therapy. J. Music Ther. 37, 118–146. doi: 10.1093/jmt/37.2.118
Robb, S. L., Clair, A. A., Watanabe, M., Monahan, P. O., Azzouz, F., Stouffer, J. W., et al. (2008). A non-randomized [corrected] controlled trial of the active music engagement (AME) intervention on children with cancer. Psychooncology 17, 699–708. doi: 10.1002/pon.1301
Robb, S. L., Haase, J. E., Perkins, S. M., Haut, P. R., Henley, A. K., Knafl, K. A., et al. (2017). Pilot randomized trial of active music engagement intervention parent delivery for young children with cancer. J. Pediatr. Psychol. 42, 208–219. doi: 10.1093/jpepsy/jsw050
Robb, S. L., and Hanson-Abromeit, D. (2014). A review of supportive care interventions to manage distress in young children with cancer and parents. Cancer Nurs. 37, E1–26. doi: 10.1097/NCC.0000000000000095
Robb, S. L., Russ, K. A., Holochwost, S. J., Stegenga, K., Perkins, S. M., Jacob, S. A., et al. (2023a). Protocol and biomarker strategy for a multi-site randomized controlled trial examining biological mechanisms and dosing of active music engagement in children with acute lymphoblastic leukemia and lymphoma and parents. BMC Complement Med. Ther. 23:90. doi: 10.1186/s12906-023-03909-w
Robb, S. L., Stegenga, K., Perkins, S. M., Stump, T. E., Moody, K. M., Henley, A. K., et al. (2023b). Mediators and moderators of active music engagement to reduce traumatic stress symptoms and improve well-being in parents of young children with cancer. Integr. Cancer Ther. 22:15347354231218266. doi: 10.1177/15347354231218266
Rodriguez, E. M., Dunn, M. J., Zuckerman, T., Vannatta, K., Gerhardt, C. A., and Compas, B. E. (2011). Cancer-related sources of stress for children with cancer and their parents. J. Pediatr. Psychol. 37, 185–197. doi: 10.1093/jpepsy/jsr054
Rodríguez-Rodríguez, R. C., Noreña-Peña, A., Chafer-Bixquert, T., Lorenzo Vásquez, A., González De Dios, J., and Solano Ruiz, C. (2022). The relevance of music therapy in paediatric and adolescent cancer patients: a scoping review. Glob. Health Action 15:2116774. doi: 10.1080/16549716.2022.2116774
Schwartz-Attias, I., Krulik, T., and Ronen, T. (2024). Well-being in parents of children with cancer: illness perceptions' mediating role for hope and social support. Front. Psychol. 15:1206520. doi: 10.3389/fpsyg.2024.1206520
Silberstein, A. K., Ligård, E., Edlund, S. M., and Ullsten, A. (2024). Family-centered music therapy as procedural support in the pediatric outpatient unit: a mixed methods pilot study. Music Sci. 7:20592043231225734. doi: 10.1177/20592043231225734
Sloper, P. (2000). Predictors of distress in parents of children with cancer: a prospective study. J. Pediatr. Psychol. 25, 79–91. doi: 10.1093/jpepsy/25.2.79
Tang, W. P., Chan, C. W., Leung, D. Y., and Chan, D. N. (2020). The effects of psychoeducational interventions on caregivers of children with cancer: a meta-analysis of randomized controlled trials. J. Child Health Care 24, 123–142. doi: 10.1177/1367493518814917
Tremolada, M., Bonichini, S., Aloisio, D., Schiavo, S., Carli, M., and Pillon, M. (2013). Post-traumatic stress symptoms among mothers of children with leukemia undergoing treatment: a longitudinal study. Psycho-Oncology 22, 1266–1272. doi: 10.1002/pon.3132
Uggla, L., Bonde, L. O., Hammar, U., Wrangsjö, B., and Gustafsson, B. (2018). Music therapy supported the health-related quality of life for children undergoing haematopoietic stem cell transplants. Acta Paediatr. 107, 1986–1994. doi: 10.1111/apa.14515
Uggla, L., Bonde, L. O., Svahn, B. M., Remberger, M., Wrangsjö, B., and Gustafsson, B. (2016). Music therapy can lower the heart rates of severely sick children. Acta Paediatr. 105, 1225–1230. doi: 10.1111/apa.13452
Uggla, L., Martenson Blom, K., Bonde, L. O., Gustafsson, B., and Wrangsjö, B. (2019). An explorative study of qualities in interactive processes with children and their parents in music therapy during and after pediatric hematopoietic stem cell transplantation. Medicines 6:28. doi: 10.3390/medicines6010028
Villani, D., Sorgente, A., Iannello, P., and Antonietti, A. (2019). The role of spirituality and religiosity in subjective well-being of individuals with different religious status. Front. Psychol. 10:1525. doi: 10.3389/fpsyg.2019.01525
Wiener, L., Kazak, A. E., Noll, R. B., Patenaude, A. P., and Kupst, M. J. (2015). Standards for the psychosocial care of children with cancer and their families: an intorudction to the special issue. Pediatr. Blood Cancer 62, S419–S424. doi: 10.1002/pbc.25675
Woolf, C., Muscara, F., Anderson, V. A., and Mccarthy, M. C. (2016). Early traumatic stress responses in parents following a serious illness in their child: a systematic review. J. Clin. Psychol. Med. Settings 23, 53–66. doi: 10.1007/s10880-015-9430-y
Keywords: music therapy, active music engagement, pediatric cancer, traumatic stress, sociodemographic risk
Citation: Holochwost SJ, Harman E, Stegenga K, Jacob SA and Robb SL (2025) Who benefits from active music engagement during cancer treatment? Associations of sociodemographic characteristics and risk factors with moderators of intervention effects. Front. Psychol. 16:1550051. doi: 10.3389/fpsyg.2025.1550051
Received: 02 January 2025; Accepted: 09 July 2025;
Published: 29 July 2025.
Edited by:
Panagis Galiatsatos, Johns Hopkins University, United StatesReviewed by:
Christine Tuden Neugebauer, Texas Tech University Health Sciences Center, United StatesLouise Eulau, Sophiahemmet University College, Sweden
Copyright © 2025 Holochwost, Harman, Stegenga, Jacob and Robb. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Steven J. Holochwost, c3RldmVuLmhvbG9jaHdvc3RAbGVobWFuLmN1bnkuZWR1
 Steven J. Holochwost
Steven J. Holochwost Elizabeth Harman
Elizabeth Harman Kristin Stegenga
Kristin Stegenga Seethal A. Jacob
Seethal A. Jacob Sheri L. Robb
Sheri L. Robb