- 1Xinxiang Medical University, Xinxiang, China
- 2Nursing Department, Changzhi People’s Hospital, Changzhi, China
- 3Joint and Spine Surgery Department, Changzhi People’s Hospital, Changzhi, China
- 4Out-patient Department, The First Affiliated Hospital of XinXiang Medical University, Xinxiang, China
Objectives: This study examined the psychosocial correlates of postoperative kinesiophobia in elderly patients with femoral neck fractures, with a focus on the roles of psychological resilience and social support in mitigating movement-related fear during rehabilitation.
Methods: A prospective observational study included 200 patients (≥65 years) undergoing femoral neck fracture surgery (January 2022–August 2024). Kinesiophobia was assessed using the Tampa Scale for Kinesiophobia (TSK), with scores >36 defining the kinesiophobia group (n = 120). Psychosocial factors were evaluated using the Social Support Rating Scale (SSRS), Connor-Davidson Resilience Scale (CD-RISC), General Self-Efficacy Scale (GSES), and Numeric Rating Scale (NRS) for pain. Functional independence was measured via the Functional Independence Measure (FIM). Group comparisons and logistic regression analyses identified risk factors, while Pearson correlation assessed relationships between psychosocial variables and TSK scores.
Results: The kinesiophobia incidence was 60% (mean TSK = 39.20 ± 4.10). Key risk factors included low education (OR = 1.122), multiple comorbidities (OR = 1.312), low SSRS (OR = 1.329), low CD-RISC (OR = 1.310), severe pain (OR = 1.324), and low FIM (OR = 1.204) (all p < 0.05). SSRS and CD-RISC scores showed significant negative correlations with TSK (r = −0.524 and −0.602, respectively). The kinesiophobia group had prolonged hospitalization (10.50 ± 2.10 vs. 7.50 ± 1.80 days) and higher complication rates (6.67% vs. 1.25%).
Conclusion: Postoperative kinesiophobia is prevalent and strongly associated with psychosocial vulnerabilities. Interventions targeting resilience, social support, and pain management may improve rehabilitation outcomes in this high-risk population.
Highlights
• This study provides the first comprehensive analysis of multiple influencing factors of postoperative kinesiophobia in elderly patients with femoral neck fractures.
• This study finds that a low education level is a significant risk factor for kinesiophobia.
• This study reveals that social support and psychological resilience are negatively correlated with kinesiophobia.
• This study confirms that severe pain significantly increases the incidence of kinesiophobia.
• This study offers new strategies and evidence for the prevention and intervention of postoperative kinesiophobia in elderly patients with femoral neck fractures.
Introduction
Femoral neck fractures account for approximately 53% of all hip fractures and predominantly affect individuals aged ≥65 years, making them a leading cause of disability and mortality in the elderly population (Kazley et al., 2018; Sundkvist et al., 2021). As global populations continue to age, the incidence of these fractures is rising, imposing significant burdens on quality of life and healthcare systems (Bäcker et al., 2021). Beyond physiological decline, aging is also associated with emotional vulnerability, reduced independence, and diminished social participation (Sanchís-Soler et al., 2025; Karapetyan et al., 2023; Salari et al., 2022).
While surgical intervention is the standard treatment, recovery in older adults is frequently hindered by psychological barriers, particularly kinesiophobia—an irrational and excessive fear of movement that limits engagement in rehabilitation (Wood et al., 2023; Ploutarchou et al., 2023). Rooted in the Fear-Avoidance Model, kinesiophobia develops when pain triggers catastrophic thinking and avoidance behaviors, leading to functional decline and heightened pain sensitivity (Knapik et al., 2011). This condition has been shown to impair physical therapy adherence, worsen pain perception, increase anxiety, and elevate the risk of postoperative complications (Dupuis et al., 2023; Wang et al., 2022; Li et al., 2023; Koçyiğit and Akaltun, 2020), thereby undermining the goals of healthy aging and frailty prevention (Claudino et al., 2021; Soong et al., 2025).
Although prior studies have identified factors such as pain intensity, low self-efficacy, poor resilience, and limited social support as contributors to kinesiophobia (Larsson et al., 2016; Knapik et al., 2011), most have relied on cross-sectional designs, small samples, or examined single variables in isolation (Xu and Chen, 2025; Fu et al., 2022). Few have explored the dynamic interaction between psychosocial, clinical, and functional variables, particularly in vulnerable elderly populations with multimorbidity, cognitive decline, and poor psychological adaptability (Nomoto et al., 2024; Huang et al., 2022; Alshehri et al., 2024). Additionally, standardized risk assessment models and integrated intervention pathways are lacking, especially in Chinese geriatric orthopedic settings.
Within the biopsychosocial model, constructs such as social support and psychological resilience have emerged as critical resources for facilitating recovery. Social support reduces isolation and enhances treatment engagement (Zhu et al., 2023; Zare et al., 2024), while resilience promotes emotional regulation and goal persistence (Soliman et al., 2022). These factors are mutually reinforcing: supportive environments enhance resilience, and resilient individuals actively mobilize support. According to Self-Determination Theory, social support fulfills the need for relatedness, while resilience fosters a sense of competence, both of which promote intrinsic motivation and functional recovery (Lim et al., 2020). Despite their theoretical relevance, these constructs remain inconsistently assessed and underutilized in clinical rehabilitation pathways.
This study aims to: (1) determine the prevalence of postoperative kinesiophobia in elderly patients following femoral neck fracture; (2) identify key psychosocial and clinical predictors using multivariate analysis; and (3) develop a practical clinical pathway that integrates physical rehabilitation with targeted psychological support. By applying validated psychological frameworks to a high-risk, under-researched population, this study addresses critical gaps in current orthopedic rehabilitation literature. Moreover, it proposes a phased, individualized intervention model based on empirical risk profiles, which may inform early screening, enhance functional recovery, and support social reintegration in elderly patients.
Materials and methods
Study design
This prospective observational study employed a structured data collection framework, covering a complete timeline from baseline assessment (within 24 h preoperatively) to postoperative follow-up (1 month after discharge). The aim was to investigate the prevalence and influencing factors of postoperative kinesiophobia in elderly patients with femoral neck fractures. Participants were elderly inpatients who underwent surgical treatment for femoral neck fractures between January 2022 and August 2024. A total of 200 patients were recruited using a convenience sampling method. The recruitment process included: (1) initial screening by orthopedic surgeons to identify patients eligible for surgery; (2) explanation of the study protocol by research assistants; and (3) completion of baseline assessment within 24 h after signing the informed consent form.
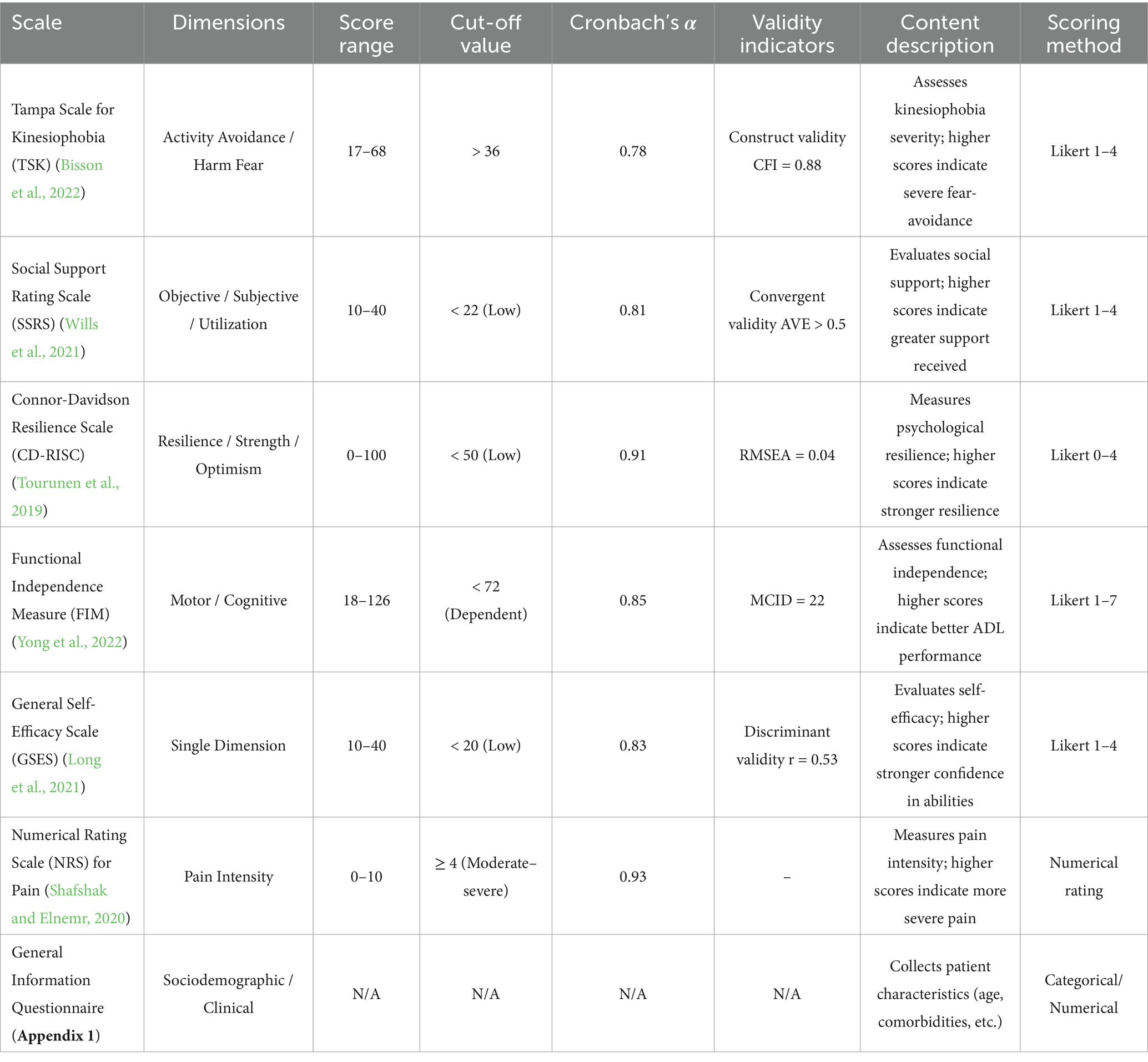
Data were collected using standardized instruments. On postoperative day 3, patients completed the Tampa Scale for Kinesiophobia (TSK), Social Support Rating Scale (SSRS), Connor-Davidson Resilience Scale (CD-RISC), Functional Independence Measure (FIM), and General Self-Efficacy Scale (GSES) (Table 1).
Sample size calculation
Sample size estimation was conducted using G*Power 3.1 software based on a priori analysis for multivariable logistic regression. The parameters were set as follows: odds ratio (OR) = 1.5, two-sided α = 0.05, power = 0.80, number of predictors = 17, and an estimated event probability of 0.60 (based on pilot data for the prevalence of kinesiophobia). The minimum required sample size was calculated to be 178. To account for an anticipated 20% attrition rate, the target sample size was adjusted to 214. Due to recruitment constraints during the Coronavirus Disease 2019 (COVID-19) pandemic, 200 participants were ultimately enrolled, corresponding to a statistical power of approximately 78.3%, which was deemed sufficient for the primary analysis.
Inclusion and exclusion criteria
Inclusion criteria were as follows: patients aged ≥ 65 years; radiographically confirmed unilateral femoral neck fracture; first-time diagnosis and surgical treatment for femoral neck fracture; and willingness to participate with signed informed consent.
Exclusion criteria included: (1) patients with visual, auditory, or speech impairments, or other conditions that prevented completion of questionnaire assessments; (2) history of depression, anxiety disorders, or cognitive impairment; (3) severe organic diseases (e.g., advanced cardiac, hepatic, renal disease), malignancies, or other severe somatic illnesses; and (4) in-hospital complications that could influence outcomes, such as infections or peripheral nerve injuries.
Cognitive impairment was assessed using the Mini-Mental State Examination (MMSE), with education-adjusted cut-off scores: ≤17 for illiterate individuals, ≤ 20 for primary school education, and ≤ 24 for secondary education or higher. Psychiatric history referred to mood disorders (e.g., depression, anxiety), formally diagnosed by a psychiatrist based on ICD-11 criteria. Patients with mild depressive symptoms (PHQ-9 < 10 and no history of psychiatric treatment) were not excluded. Severe organic comorbidities were defined as a Charlson Comorbidity Index (CCI) score ≥ 3 or end-stage organ failure (e.g., eGFR < 30 mL/min/1.73 m2).
Research tools
This study utilized a set of standardized scales and assessment tools to comprehensively evaluate patients’ psychological status, social support, functional independence, and pain perception (Table 1). A general information questionnaire was administered to collect sociodemographic and clinical characteristics, including sex, age, body mass index (BMI), residence, marital status, education level, smoking and alcohol history, and the number of comorbid chronic conditions (Appendix 1). The TSK was used to assess fear of movement, with total scores ranging from 17 to 68; higher scores indicated more severe kinesiophobia (Barnes and Dixon, 1995). The SSRS measured perceived social support, where elevated scores reflected stronger social support networks (Wills et al., 2021). Psychological resilience was evaluated using the CD-RISC, with higher scores denoting greater psychological adaptability (Tourunen et al., 2019). Pain intensity was quantified using the Numeric Rating Scale (NRS), where higher scores corresponded to more severe pain (Shafshak and Elnemr, 2020). Functional independence was assessed through the FIM, which evaluated activities of daily living, cognitive function, and social interaction capacity; higher scores indicated better functional independence (Yong et al., 2022). Finally, the GSES was employed to measure self-efficacy, with higher scores representing stronger confidence in overcoming challenges (Long et al., 2021).
Data collection method
Data were collected using structured questionnaires covering multiple domains, including demographic characteristics, psychosocial variables, functional status, pain intensity, and patient satisfaction. Investigators received pre-study training, and standardized written and verbal instructions were used during administration to ensure consistent interpretation and completion of items. Demographic and clinical data were recorded within 24 h of admission. Psychological and functional assessments, including the Tampa Scale for Kinesiophobia (TSK), Social Support Rating Scale (SSRS), Connor-Davidson Resilience Scale (CD-RISC), Functional Independence Measure (FIM), and General Self-Efficacy Scale (GSES), were conducted on postoperative day 3. This timing was chosen because most patients had achieved hemodynamic stability, regained full consciousness, and were capable of completing self-report instruments by that point (Fischer et al., 2021). FIM was performed by rehabilitation therapists on postoperative day 7 to reduce inter-rater variability.
Pain intensity was assessed using the NRS, based on the highest level of pain reported within 24 h after surgery. Patient satisfaction was measured using a structured questionnaire (Appendix 2) covering treatment experience, emotional well-being, and the rehabilitation process. As an observational study, no blinding or interventions were applied. To reduce bias, the following measures were implemented: (1) standardized instructions were provided to all participants; (2) scoring of instruments was based on predefined, objective criteria (e.g., level-specific FIM scores); (3) pain was self-reported to minimize assessor influence; and (4) psychological assessments were completed within a fixed window (72 ± 6 h postoperatively).
Statistical analysis
Statistical analyses were performed using SPSS version 26.0. Continuous variables were expressed as mean ± standard deviation (SD) and compared between groups using independent samples t-tests. Categorical variables were presented as frequencies and percentages, with group comparisons conducted via chi-square tests. Normality of continuous variables was assessed using the Shapiro–Wilk test (α = 0.05), and non-normally distributed or heteroscedastic data were analyzed using appropriate non-parametric or adjusted methods. Pearson correlation analysis was applied to examine associations among categorical variables, with homogeneity of variance verified using Levene’s test. Binary logistic regression was used to identify potential risk factors, following multicollinearity diagnostics on all independent variables using the Variance Inflation Factor (VIF), with all values < 2. Model fit was evaluated using the Hosmer-Lemeshow goodness-of-fit test. The multivariable model included adjustment for potential confounders such as education level (categorized as junior high, high school, and college), comorbidity burden (Charlson Comorbidity Index), social support (SSRS score categories), psychological resilience (CD-RISC tertiles), and pain intensity (NRS ≥ 4). All covariates showed acceptable collinearity (VIF < 3). Predictive performance of the model was assessed using receiver operating characteristic (ROC) curve analysis, with calculation of the area under the curve (AUC), sensitivity, and specificity. A two-tailed p-value < 0.05 was considered statistically significant.
Ethical approval
This study was approved by the Institutional Ethics Committee of the hospital. Written informed consent was obtained from all participants before enrollment, confirming their voluntary participation. All data were anonymized, and the study was conducted in full accordance with the ethical principles of the Declaration of Helsinki.
Results
Postoperative kinesiophobia in elderly patients with femoral neck fractures
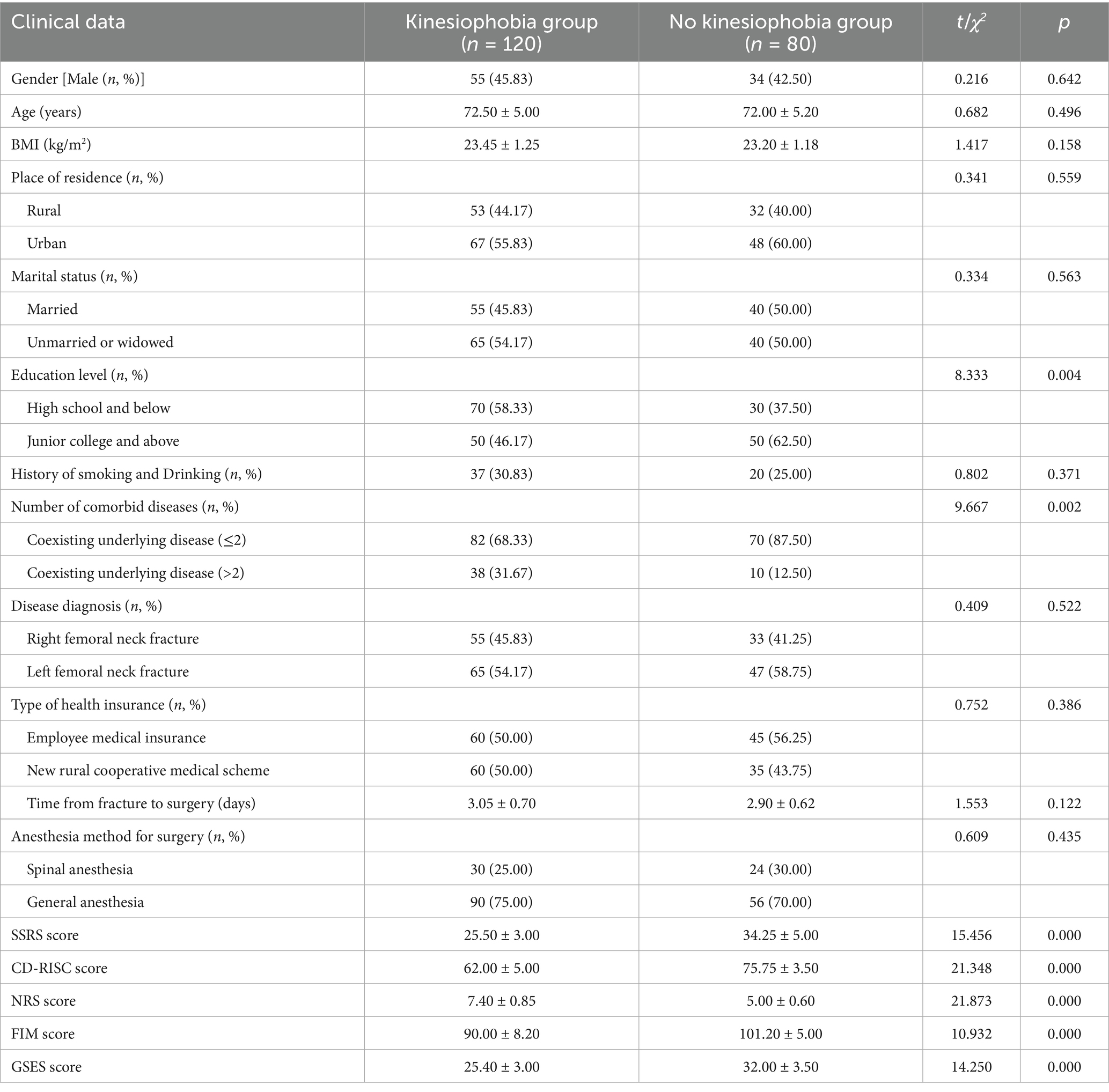
All 200 patients included in the final analysis completed the TSK. The total TSK scores ranged from 17 to 68, with a mean score of 39.20 ± 4.10. A total of 120 patients (60.0%) had TSK scores > 37, indicating clinically relevant kinesiophobia, while 80 patients (40.0%) scored ≤ 37. Based on these scores, patients were categorized into the kinesiophobia group (n = 120) and the non-kinesiophobia group (n = 80). The participant selection process is shown in Figure 1.
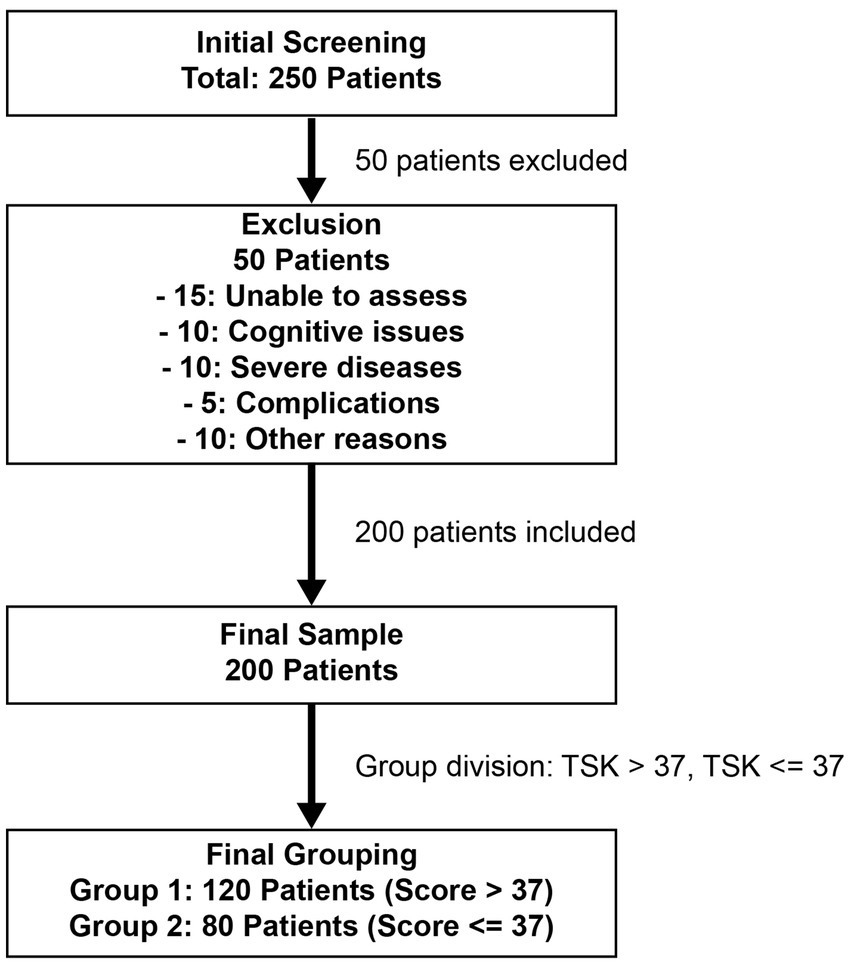
Figure 1. Flowchart of patient selection and grouping in the study of postoperative fear of movement in elderly femoral neck fracture patients.
Comparative analysis of clinical characteristics between kinesiophobia and non-kinesiophobia groups
In terms of educational level, 58.33% of patients in the kinesiophobia group had a high school education or below, compared to 37.50% in the non-kinesiophobia group (p = 0.004). Regarding comorbidity, 31.67% of patients in the kinesiophobia group had more than two comorbid conditions, versus 12.50% in the non-kinesiophobia group (p = 0.002). For psychosocial and functional measures, the kinesiophobia group had significantly lower scores in the SSRS (p < 0.001; Cohen’s d = 1.42; 95% CI: 1.25–1.58), CD-RISC (p < 0.001; d = 1.38; 95% CI: 1.20–1.55), Functional Independence Measure (FIM) (p < 0.001; d = 1.05; 95% CI: 0.89–1.21), and GSES (p < 0.001; d = 0.92; 95% CI: 0.76–1.08). In contrast, the Numeric Rating Scale (NRS) scores for pain were significantly higher in the kinesiophobia group (p < 0.001; d = 1.67; 95% CI: 1.50–1.84) (Tables 2, 3).
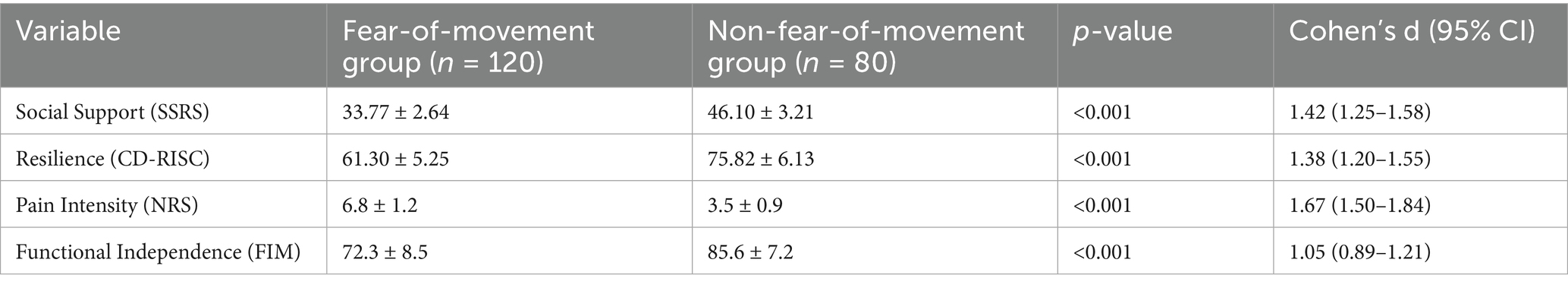
Table 3. Comparison of psychometric scores between fear-of-movement and non-fear-of-movement groups in elderly femoral neck fracture patients.
Influencing factors of postoperative kinesiophobia in elderly patients with femoral neck fractures
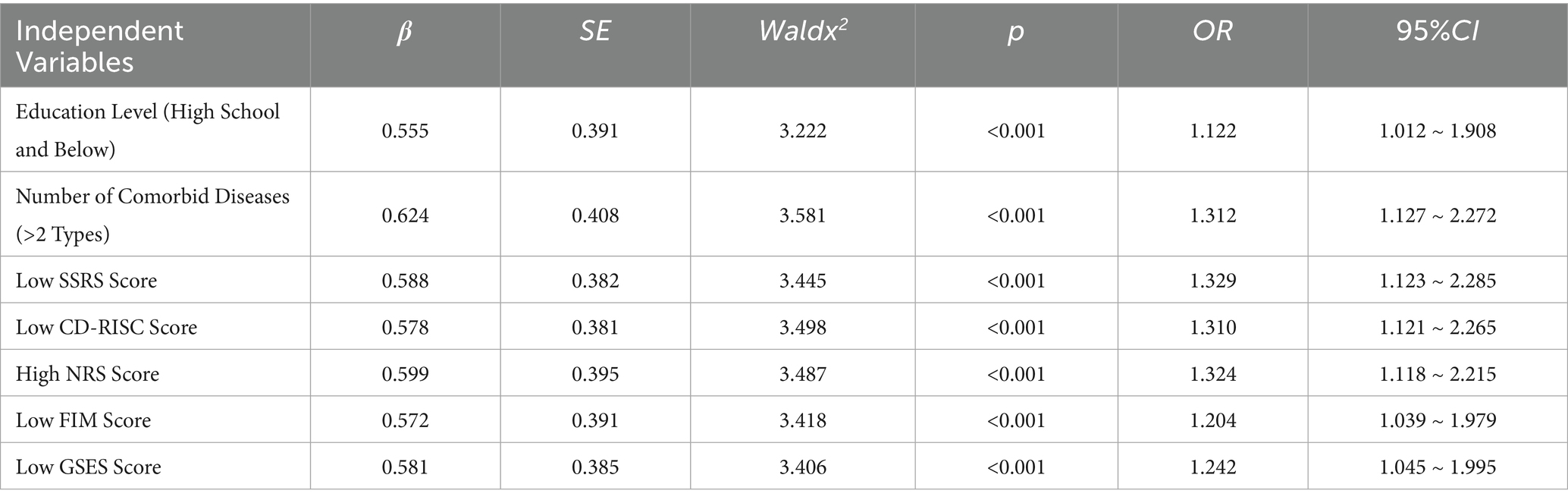
Logistic regression analysis was performed to identify factors associated with postoperative kinesiophobia in elderly patients with femoral neck fractures. Variable definitions and coding strategies are detailed in Table 4, including education level, number of comorbidities, social support (SSRS score), psychological resilience (CD-RISC score), pain perception (NRS score), functional independence (FIM score), and self-efficacy (GSES score). Regression results are presented in Table 5 and visualized in Figure 2A. Lower education level (β = 0.555, OR = 1.122, 95% CI: 1.012–1.908, p < 0.001) and ≥2 comorbidities (β = 0.624, OR = 1.312, 95% CI: 1.127–2.272; adjusted OR = 1.283, 95% CI: 1.102–1.842, p < 0.001) were identified as risk factors. Higher scores in SSRS (β = −0.446, p < 0.001), CD-RISC (β = −0.419, p < 0.001), FIM (β = −0.328, p = 0.002), and GSES (β = −0.311, p = 0.004) were associated with a lower likelihood of postoperative kinesiophobia, while higher NRS pain scores (β = 0.573, p < 0.001) were associated with increased risk. Model performance was evaluated by ROC analysis (Figure 2B), with an AUC of 0.872 (95% CI: 0.824–0.921). The optimal cutoff point (Youden index = 0.61) yielded a sensitivity of 84.2% and a specificity of 76.3%.
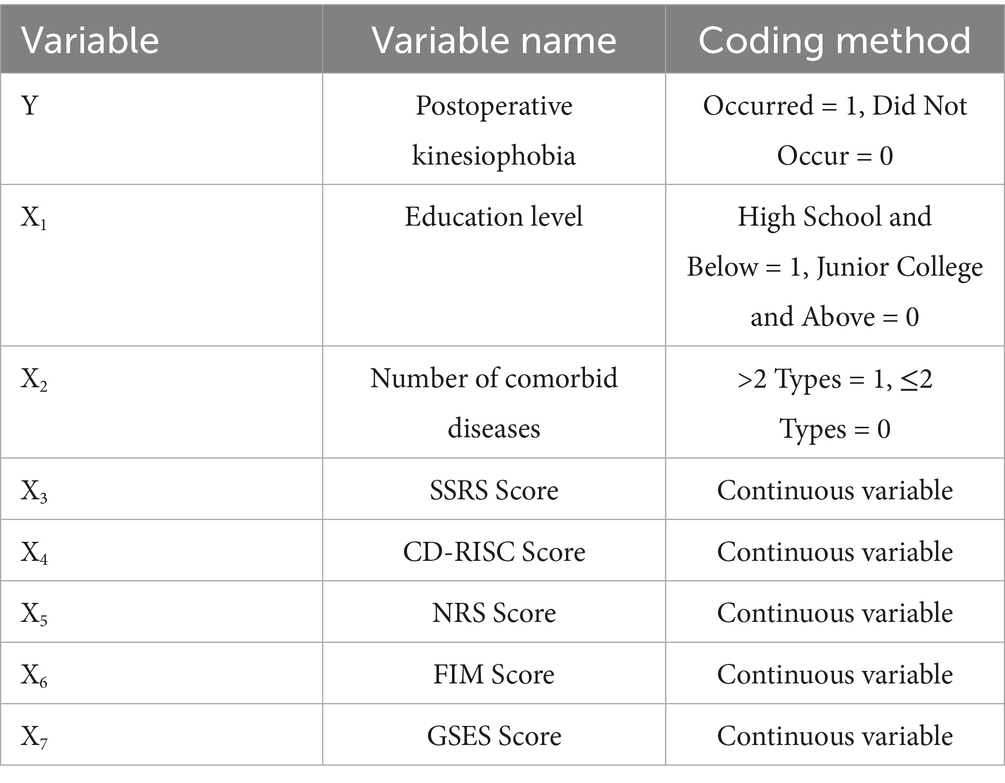
Table 4. Independent variable assignment for postoperative kinetic Logistic regression analysis of elderly patients with femoral neck fracture.
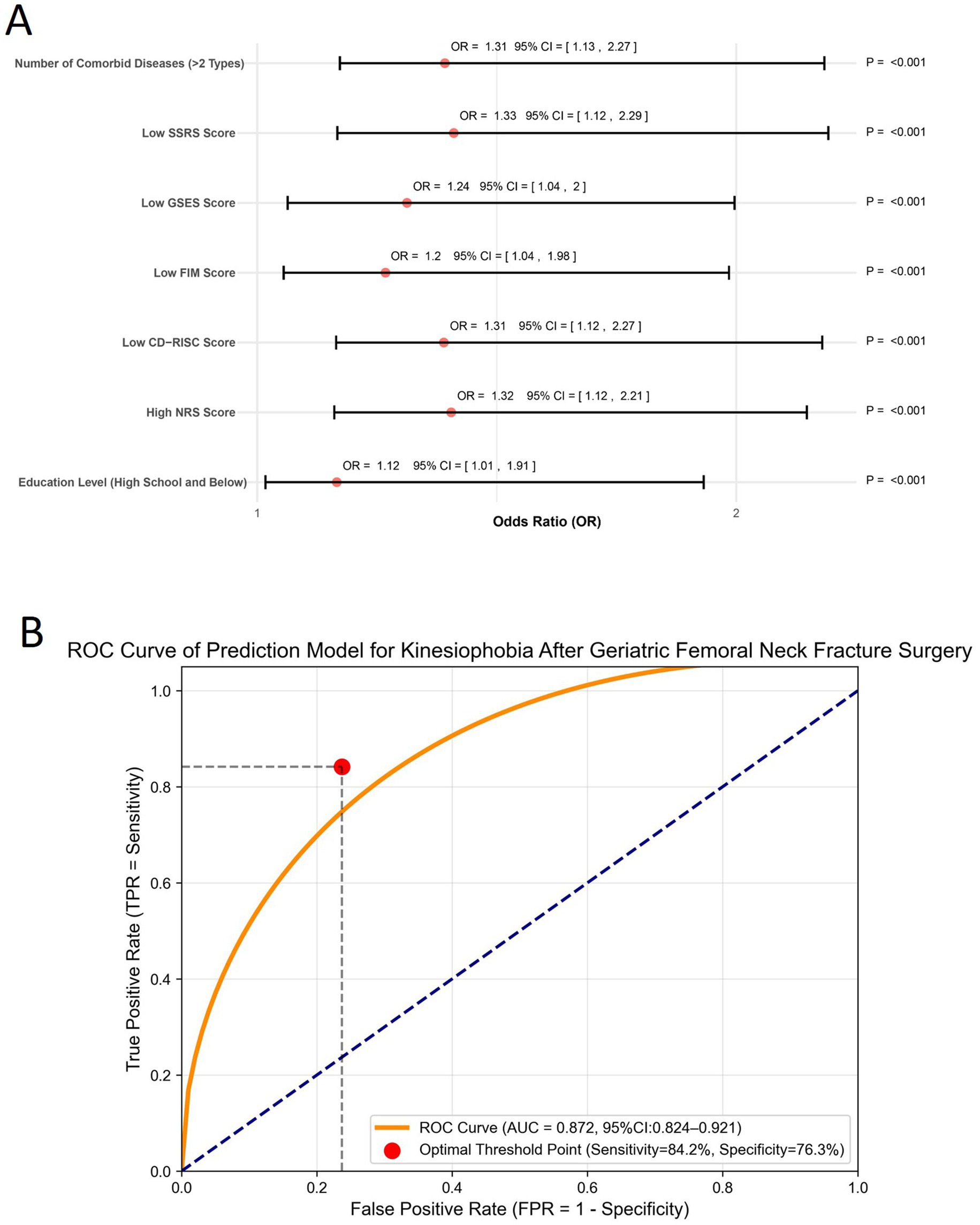
Figure 2. Multivariate regression analysis and model performance evaluation. (A) Forest plot presenting the odds ratios (ORs) and 95% confidence intervals (CIs) of independent variables included in the multivariate logistic regression model for postoperative kinesiophobia. (B) Receiver operating characteristic (ROC) curve of the prediction model. The curve displays the true positive rate (sensitivity) against the false positive rate (1 - specificity), with the optimal cutoff point indicated.
Postoperative social support, psychological resilience, and their relationship with kinesiophobia in elderly patients with femoral neck fractures
This study assessed levels of social support and psychological resilience in elderly patients following femoral neck fracture surgery. The mean SSRS score was 33.77 ± 2.64, and the mean CD-RISC score was 61.30 ± 5.25, indicating relatively low levels in the postoperative population. Correlation analysis showed a significant negative relationship between SSRS and TSK scores (r = −0.7057, p < 0.05), suggesting that higher social support was associated with milder kinesiophobia symptoms (Figure 3A). Similarly, CD-RISC scores were negatively correlated with TSK scores (r = −0.5912, p < 0.05), indicating that greater psychological resilience was also associated with lower levels of kinesiophobia (Figure 3B).
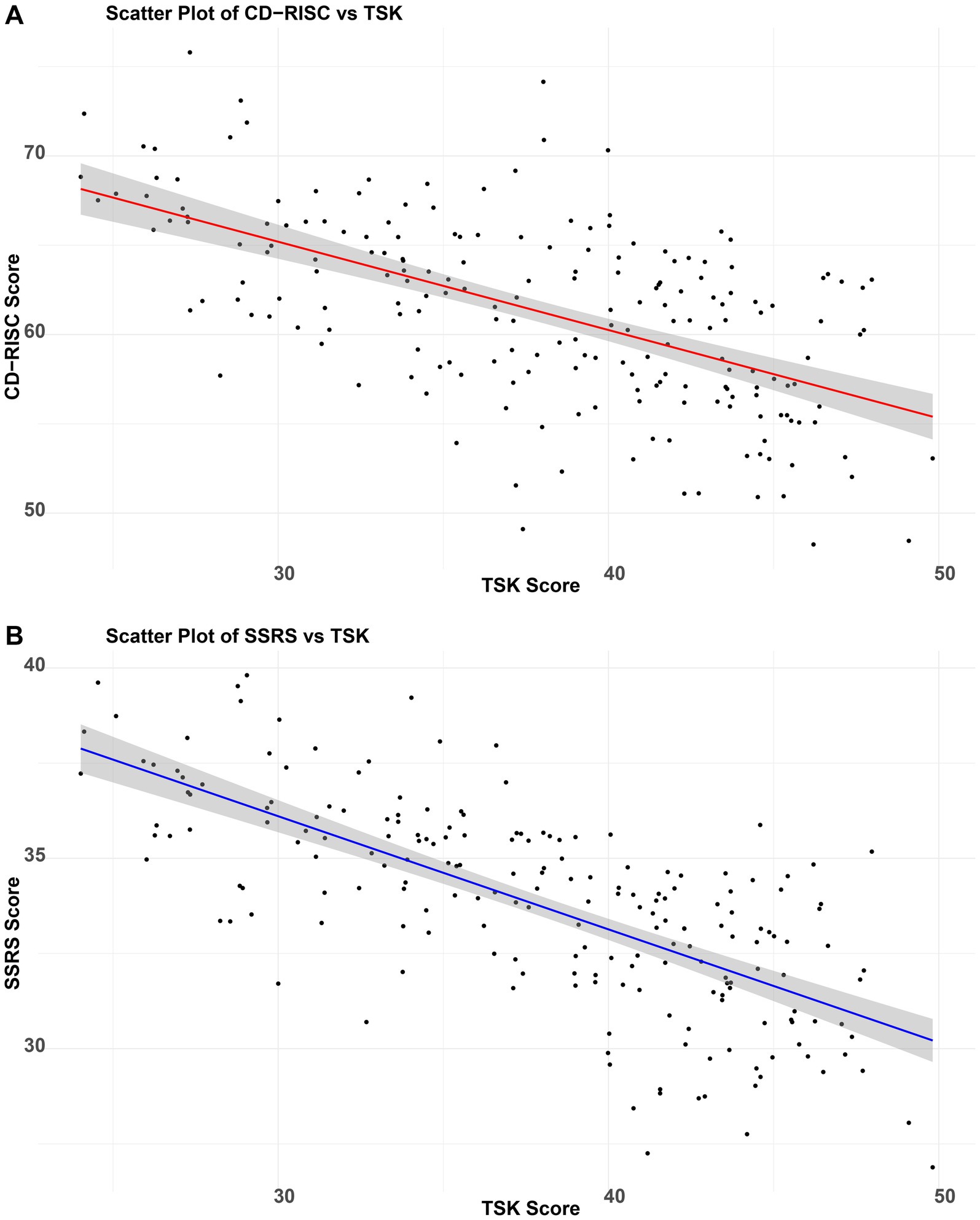
Figure 3. Impact of social support and psychological resilience on postoperative kinesiophobia in elderly patients with femoral neck fractures. (A) Correlation between SSRS and TSK scores in elderly femoral neck fracture patients; (B) Correlation between CD-RISC and TSK scores in elderly femoral neck fracture patients.
Association between hospital stay duration, complication rates, and postoperative kinesiophobia
The average postoperative hospital stay was significantly longer in the kinesiophobia group (10.50 ± 2.10 days) compared to the non-kinesiophobia group (7.50 ± 1.80 days) (t = 12.34, p < 0.001), with a large effect size (d = 1.58, 95% CI: 1.41–1.75). The incidence of postoperative complications (e.g., infection, thrombosis) was also higher in the kinesiophobia group (6.67%) than in the non-kinesiophobia group (1.25%) (χ2 = 4.12, p = 0.042).
Differences in patient satisfaction between kinesiophobia and non-kinesiophobia groups
The patient satisfaction survey (Appendix 2) revealed significantly lower overall satisfaction in the kinesiophobia group compared to the non-kinesiophobia group (68.2 ± 7.5 vs. 85.3 ± 5.1, t = 16.38, p < 0.001, d = 2.62). Domain-specific analysis demonstrated significant between-group differences across all assessed dimensions (p < 0.001), with particularly pronounced disparities in psychological support (2.9 ± 0.8 vs. 4.3 ± 0.7, d = 1.65) and functional recovery (2.8 ± 0.9 vs. 4.6 ± 0.7, d = 2.02). Notably, only 28% of kinesiophobia patients reported satisfaction with anxiety-relief interventions, compared to 82% in the non-kinesiophobia group (χ2 = 45.6, p < 0.001). Similarly, merely 25% of kinesiophobia patients expressed satisfaction with improvements in activity tolerance, significantly lower than the 85% satisfaction rate in controls. Additional significant differences emerged in pain management (3.2 ± 0.7 vs. 4.5 ± 0.6, d = 1.88), where only 32% of kinesiophobia patients considered analgesic regimens effective, and in social support (3.1 ± 0.7 vs. 4.5 ± 0.6, d = 1.58), particularly regarding access to family care resources (Table 6). Multivariate analysis identified poor overall satisfaction (OR = 1.402, 95% 1.214–2.153), inadequate pain management (OR = 1.289), and lack of psychological support (OR = 1.254) as independent risk factors for postoperative kinesiophobia (Table 7).
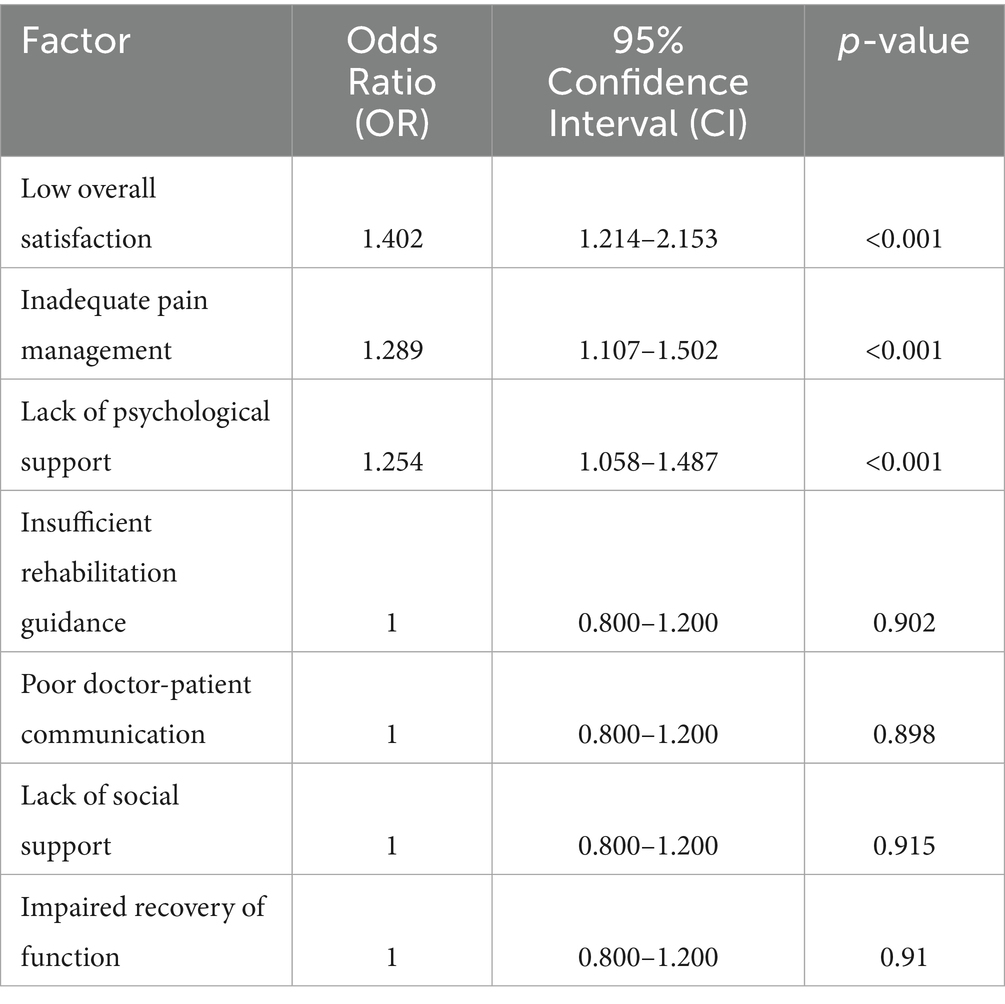
Table 7. Multivariate analysis of postoperative kinesiophobia risk factors (independent and non-significant factors).
Discussion
An excessive fear of movement characterizes Kinesiophobia, often manifested as intense anxiety and avoidance behaviors related to physical activity. Its theoretical foundation is rooted in the fear-avoidance model, which posits that individuals who excessively worry about pain or injury may develop movement-related fear, ultimately leading to avoidant behavior (Wideman et al., 2013). Previous studies have indicated that postoperative patients with kinesiophobia tend to overestimate the risks associated with activity, which may lead to missed opportunities for optimal functional recovery (Bisson et al., 2022). This results in delayed rehabilitation, increased risks of complications such as muscle atrophy and thrombosis, and severely compromised long-term health outcomes (see Figure 4).
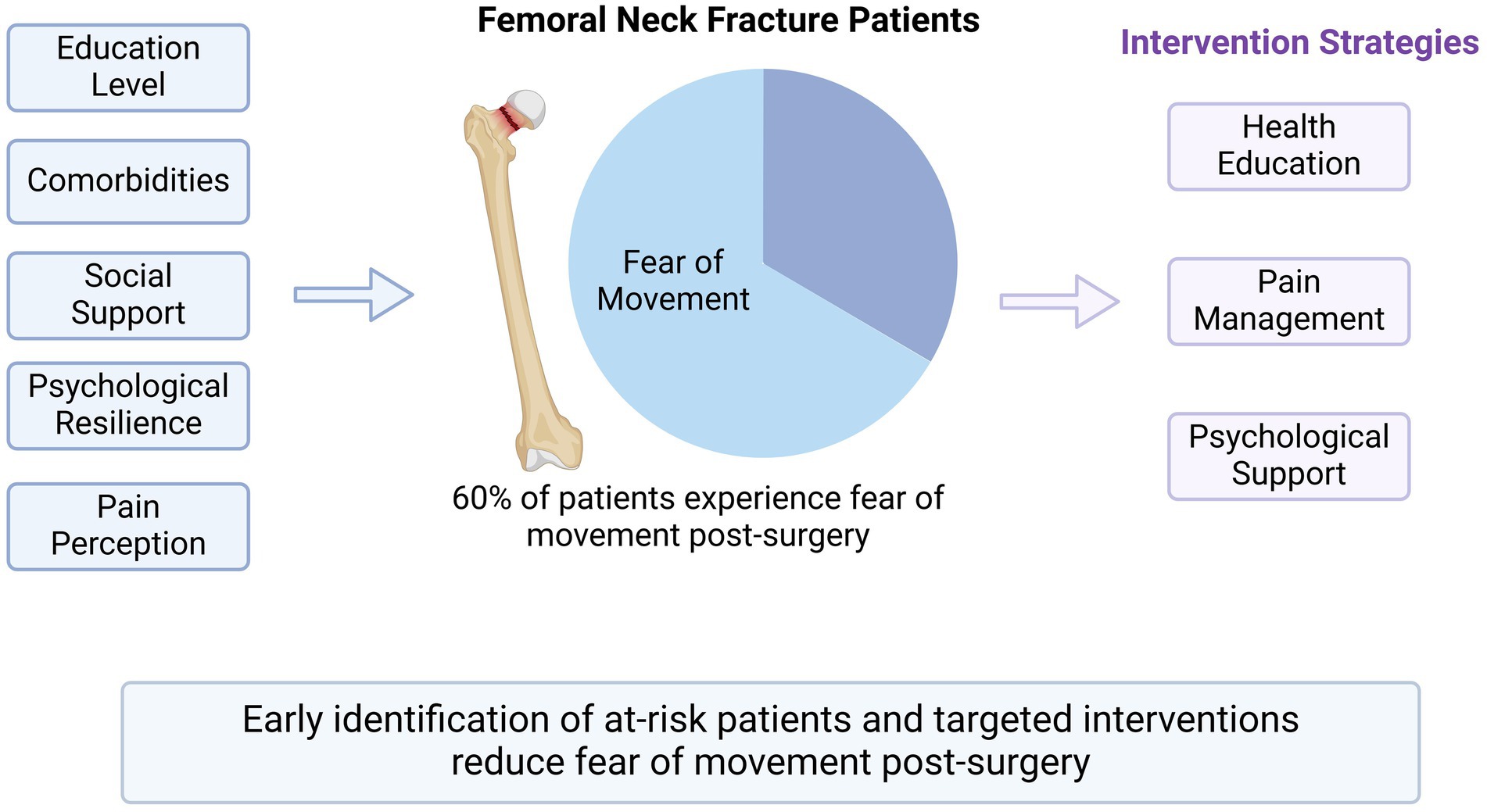
Figure 4. Factors influencing postoperative kinesiophobia and intervention strategies in elderly patients with femoral neck fractures.
In this study, the incidence of postoperative kinesiophobia among elderly patients with femoral neck fractures reached 60%, indicating a high prevalence in this population. This is comparable to the reported 77% incidence in patients with knee osteoarthritis (Losciale et al., 2024) and the 56% rate observed in those undergoing minimally invasive surgery for chronic low back pain. The varying rates across populations may be attributed to differences in disease type, surgical method, educational level, and social support. Our analysis also demonstrated a significant association between kinesiophobia and prolonged hospital stay as well as an increased risk of postoperative complications. Previous research has shown that kinesiophobia may extend hospitalization duration by an average of 30% (Li et al., 2019). A meta-analysis reported that for each standard deviation increase in kinesiophobia scores, the risk of developing deep vein thrombosis rose by 1.8 times (OR = 1.82, 95% CI: 1.24–2.68) (Keddie et al., 2018), while a prospective study indicated that patients with kinesiophobia were 2.3 times more likely to be readmitted within 3 months postoperatively (HR = 2.31, p = 0.003) (Gruneir et al., 2016). Collectively, these findings support the psychophysiological vicious cycle theory, wherein fear-induced avoidance behaviors contribute to muscle deconditioning and hemodynamic disturbances, thereby exacerbating poor surgical outcomes.
Multiple influencing factors were identified about postoperative kinesiophobia, including educational attainment, comorbidity burden, pain severity, self-efficacy, and psychosocial resources. Higher educational levels were associated with a lower risk of kinesiophobia, consistent with findings from studies on total knee arthroplasty patients (Du et al., 2025). Patients with limited education often face barriers in understanding rehabilitation information and engaging actively in recovery. In our study, only 35% of patients with low educational backgrounds actively sought rehabilitation guidance, reflecting both cognitive and behavioral disadvantages. This population also demonstrated lower perioperative compliance (Vu et al., 2024; Norekvål et al., 2020; Rolls et al., 2017). A comorbidity count of ≥2 significantly increased the risk of kinesiophobia (Zeng et al., 2024), likely due to elevated recovery challenges and psychological stress (Helminen et al., 2020). Moreover, higher pain scores (NRS) were strongly associated with kinesiophobia, aligning with the fear-avoidance framework (Wideman et al., 2013). Pain-related fear can disrupt gait and biomechanical stability, intensifying avoidance behavior. Individuals with low self-efficacy are particularly vulnerable to catastrophic interpretations of pain, perpetuating the fear-avoidance cycle (Brindisino et al., 2023; Brown et al., 2020; Terradas-Monllor et al., 2024).
Psychosocial factors also play a crucial role in the development of postoperative kinesiophobia. In this study, lower scores on the SSRS and the CD-RISC were significantly associated with increased kinesiophobia, and both were negatively correlated with TSK scores (Greenberg et al., 2021). These findings are consistent with prior evidence that enhanced social support alleviates postoperative anxiety and fear (Ji et al., 2022; Li et al., 2024). Self-efficacy, as a core psychological resource in regulating behavioral responses, was further confirmed as a protective factor in our study. Patients with lower self-efficacy scores had significantly higher rates of kinesiophobia (OR = 1.242), corroborating multiple prior findings (Cao et al., 2025; Zhang et al., 2022; Zelle et al., 2016; Westerdahl et al., 2024; Jakobsson et al., 2023). These results offer a theoretical foundation for identifying high-risk individuals and tailoring early interventions. Future research should further investigate the interactions between pain sensitivity, pain duration, and self-efficacy to inform precise and targeted intervention strategies.
Based on these mechanisms and findings, this study proposes several rehabilitation-based intervention strategies. For patients with low educational attainment, we recommend large-font illustrated brochures and animated videos demonstrating safe activity postures, supplemented by caregiver-assisted education. Screening using the simplified TSK-11 scale should be conducted within 24 h postoperatively, with high-risk individuals receiving graded exposure therapy. At the community level, the FRAIL scale can be used to assess home environment risks (e.g., anti-slip flooring, handrail installation), with rehabilitation professionals providing biweekly home visits for high-risk families. Pain management should also be prioritized as a core measure in the prevention of kinesiophobia. Rehabilitation strategies must center around functional recovery and incorporate patients’ educational levels, pain intensity, self-efficacy, social support, and resilience to develop staged and individualized care plans, thereby enhancing compliance and reducing long-term disability risk.
This study has several limitations. First, the single-center convenience sampling, conducted in a tertiary hospital, may have introduced selection bias and limits generalizability. Second, although the sample size met statistical requirements, the high prevalence of kinesiophobia suggests that a larger cohort would enhance external validity. Third, despite controlling for key confounders, unmeasured variables such as socioeconomic status and quality of home care may have influenced the accuracy of our assessment of social support. Fourth, the TSK was administered only once on postoperative day 3, which restricts understanding of the dynamic evolution of kinesiophobia symptoms.
Future research should consider the following directions: (1) establish multicenter prospective cohorts to improve representativeness; (2) apply stratified random sampling to include different healthcare levels and community-dwelling populations for greater ecological validity; (3) incorporate interventional studies using assessor blinding, third-party imaging assessments of function, and longitudinal symptom monitoring; (4) use WHO-SES scales to quantify socioeconomic status as a potential mediator or moderator; and (5) conduct multi-timepoint evaluations to map the trajectory of kinesiophobia and support precision intervention.
This study confirms a high incidence of postoperative kinesiophobia among elderly patients with femoral neck fractures, with strong associations observed across educational background, comorbidities, pain levels, social support, psychological resilience, and self-efficacy. Early identification of high-risk populations and the implementation of region-specific health education and personalized rehabilitation interventions may reduce the incidence of postoperative kinesiophobia, improve functional recovery, and ultimately enhance long-term patient independence and outcomes.
Conclusion
This study identified the multidimensional determinants of postoperative kinesiophobia in elderly patients with femoral neck fractures and established a core high-risk profile characterized by the triad of low educational attainment, multimorbidity, and limited psychological resources. Grounded in the Fear-Avoidance Model and Self-Determination Theory, we propose a three-tier translational intervention pathway: rapid risk stratification within 24 h postoperatively based on education and comorbidity indices; community nurse-led dual-module training targeting social support and psychological resilience; and integration of kinesiophobia management into the ERAS pathway for geriatric hip fractures to establish a closed-loop continuum from acute care to community rehabilitation.
Given the modifiability of multiple risk factors associated with kinesiophobia, we recommend the systematic incorporation of psychosocial assessments and health education into the perioperative care process to enhance rehabilitation adherence, reduce long-term disability risk, and promote individualized, precision-oriented management of geriatric fracture recovery. Future research should focus on the dynamic trajectories of kinesiophobia, the development of elderly-friendly digital intervention tools, and the long-term health economic outcomes of such strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was approved by the Clinical Ethics Committee of Changzhi People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KG: Formal analysis, Writing – original draft, Methodology, Investigation. LZ: Writing – original draft, Visualization, Conceptualization. MZ: Methodology, Writing – original draft. XH: Writing – original draft, Project administration. YH: Project administration, Writing – original draft. JH: Supervision, Writing – review & editing, Formal analysis. JC: Visualization, Writing – review & editing, Conceptualization. XS: Methodology, Writing – original draft, Resources. QW: Supervision, Methodology, Writing – original draft. QZ: Conceptualization, Methodology, Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1622585/full#supplementary-material
Abbreviations
BMI, Body Mass Index; β values, Regression Coefficients; CD-RISC, Connor-Davidson Resilience Scale; χ2, Chi-Square; FIM, Functional Independence Measure; GSES, General Self-Efficacy Scale; NRS, Numeric Rating Scale; OR, Odds Ratio; SD, Standard Deviation; SSRS, Social Support Rating Scale; TSK, Tampa Scale for Kinesiophobia.
References
Alshehri, S. H. S., Reddy, R. S., Alshahrani, M. S., Alnakhli, H. H., Gautam, A. P., ALMohiza, M. A., et al. (2024). Unraveling the impact of kinesiophobia on proprioception and balance: mediation by pain, mobility, and psychological wellbeing in post-total hip replacement recovery. PLoS One 19:e0314627. doi: 10.1371/journal.pone.0314627
Bäcker, H. C., Wu, C. H., Maniglio, M., Wittekindt, S., Hardt, S., and Perka, C. (2021). Epidemiology of proximal femoral fractures. J. Clin. Orthop. Trauma 12, 161–165. doi: 10.1016/j.jcot.2020.07.001
Barnes, N. W., and Dixon, C. (1995). A new measure of anaesthetic potency. Anaesth. Intensive Care 23, 523–524.
Bisson, E. J., Katz, L., Vader, K., Bossio, J. A., Wilson, R., and Duggan, S. (2022). Pain-related fear in adults living with chronic pain: development and psychometric validation of a brief form of the Tampa scale of Kinesiophobia. Arch. Phys. Med. Rehabil. 103, 875–881.e1. doi: 10.1016/j.apmr.2021.09.001
Brindisino, F., Garzonio, F., DI Giacomo, G., Pellegrino, R., Olds, M., and Ristori, D. (2023). Depression, fear of re-injury and kinesiophobia resulted in worse pain, quality of life, function and level of return to sport in patients with shoulder instability: a systematic review. J. Sports Med. Phys. Fitness 63, 598–607. doi: 10.23736/s0022-4707.22.14319-7
Brown, O. S., Hu, L., Demetriou, C., Smith, T. O., and Hing, C. B. (2020). The effects of kinesiophobia on outcome following total knee replacement: a systematic review. Arch. Orthop. Trauma Surg. 140, 2057–2070. doi: 10.1007/s00402-020-03582-5
Cao, Y., Zheng, H., Gu, Y., Hu, F., and Zhang, W. (2025). Mediating role of fall fear and exercise self-efficacy in the nexus between low back pain knowledge and kinesiophobia in pregnancy-related low back pain pregnant women. Sci. Rep. 15:6348. doi: 10.1038/s41598-025-90739-0
Claudino, J. G., Afonso, J., Sarvestan, J., Lanza, M. B., Pennone, J., Filho, C. A. C., et al. (2021). Strength training to prevent falls in older adults: a systematic review with Meta-analysis of randomized controlled trials. J. Clin. Med. 10:3184. doi: 10.3390/jcm10143184
Du, X., Shao, Y., Xue, J., and Kong, J. (2025). Prevalence and influencing factors of kinesiophobia after total knee arthroplasty: a systematic review and meta-analysis. J. Orthop. Surg. Res. 20:332. doi: 10.1186/s13018-025-05752-w
Dupuis, F., Cherif, A., Batcho, C., Massé-Alarie, H., and Roy, J.-S. (2023). The Tampa scale of Kinesiophobia. Clin. J. Pain 39, 236–247. doi: 10.1097/ajp.0000000000001104
Fischer, H., Maleitzke, T., Eder, C., Ahmad, S., Stöckle, U., and Braun, K. F. (2021). Management of proximal femur fractures in the elderly: current concepts and treatment options. Eur. J. Med. Res. 26:86. doi: 10.1186/s40001-021-00556-0
Fu, Y., Zhu, L.-J., Li, D.-C., Yan, J.-L., Zhang, H.-T., Xuan, Y.-H., et al. (2022). Evidence-based intervention on postoperative fear, compliance, and self-efficacy in elderly patients with hip fracture. World J. Clin. Cases 10, 3069–3077. doi: 10.12998/wjcc.v10.i10.3069
Greenberg, J., Lin, A., Popok, P. J., Kulich, R. J., Edwards, R. R., and Vranceanu, A.-M. (2021). Getting active mindfully: rationale and case illustration of a group mind-body and activity program for chronic pain. J. Clin. Psychol. Med. Settings 28, 706–719. doi: 10.1007/s10880-020-09758-w
Gruneir, A., Markle-Reid, M., Fisher, K., Reimer, H., Ma, X., and Ploeg, J. (2016). Comorbidity burden and health services use in community-living older adults with diabetes mellitus: a retrospective cohort study. Can. J. Diabetes 40, 35–42. doi: 10.1016/j.jcjd.2015.09.002
Helminen, E.-E., Arokoski, J. P., Selander, T. A., and Sinikallio, S. H. (2020). Multiple psychological factors predict pain and disability among community-dwelling knee osteoarthritis patients: a five-year prospective study. Clin. Rehabil. 34, 404–415. doi: 10.1177/0269215519900533
Huang, J., Xu, Y., Xuan, R., Baker, J. S., and Gu, Y. (2022). A mixed comparison of interventions for Kinesiophobia in individuals with musculoskeletal pain: systematic review and network meta-analysis. Front. Psychol. 13:886015. doi: 10.3389/fpsyg.2022.886015
Jakobsson, M., Hagströmer, M., Lotzke, H., von Rosen, P., and Lundberg, M. (2023). Fear of movement was associated with sedentary behaviour 12 months after lumbar fusion surgery in patients with low back pain and degenerative disc disorder. BMC Musculoskelet. Disord. 24:874. doi: 10.1186/s12891-023-06980-z
Ji, W., Sang, C., Zhang, X., Zhu, K., and Bo, L. (2022). Personality, preoperative anxiety, and postoperative outcomes: a review. Int. J. Environ. Res. Public Health 19:12162. doi: 10.3390/ijerph191912162
Karapetyan, T. A., Dorshakova, N. V., and Nikiforova, N. A. (2023). The present-day medical demographic situation in the republic of Karelia. Probl. Sots. Gig. Zdravookhranenniia Istor. Med. 31, 1331–1336. doi: 10.32687/0869-866x-2023-31-6-1331-1336
Kazley, J. M., Banerjee, S., Abousayed, M. M., and Rosenbaum, A. J. (2018). Classifications in brief: garden classification of femoral neck fractures. Clin. Orthop. Relat. Res. 476, 441–445. doi: 10.1007/s11999.0000000000000066
Keddie, S., Adams, A., Kelso, A. R. C., Turner, B., Schmierer, K., Gnanapavan, S., et al. (2018). No laughing matter: subacute degeneration of the spinal cord due to nitrous oxide inhalation. J. Neurol. 265, 1089–1095. doi: 10.1007/s00415-018-8801-3
Knapik, A., Saulicz, E., and Gnat, R. (2011). Kinesiophobia - introducing a new diagnostic tool. J. Hum. Kinet. 28, 25–31. doi: 10.2478/v10078-011-0019-8
Koçyiğit, B. F., and Akaltun, M. S. (2020). Kinesiophobia levels in fibromyalgia syndrome and the relationship between pain, disease activity, depression. Arch. Rheumatol. 35, 214–219. doi: 10.46497/archrheumatol.2020.7432
Larsson, C., Ekvall Hansson, E., Sundquist, K., and Jakobsson, U. (2016). Kinesiophobia and its relation to pain characteristics and cognitive affective variables in older adults with chronic pain. BMC Geriatr. 16:128. doi: 10.1186/s12877-016-0302-6
Li, L., Sun, Y., Qin, H., Zhou, J., Yang, X., Li, A., et al. (2023). A scientometric analysis and visualization of kinesiophobia research from 2002 to 2022: a review. Medicine 102:e35872. doi: 10.1097/md.0000000000035872
Li, N., Wang, Q., Wang, Y., Sun, A., Lin, Y., Jin, Y., et al. (2019). Fecal microbiota transplantation from chronic unpredictable mild stress mice donors affects anxiety-like and depression-like behavior in recipient mice via the gut microbiota-inflammation-brain axis. Stress 22, 592–602. doi: 10.1080/10253890.2019.1617267
Li, M., Yu, B., He, H., Li, N., and Gao, R. (2024). Impact of psychological resilience and social support on psycho-social adjustment in postoperative patients with primary hepatocellular carcinoma: mediating effects of fear of progression. Front. Psychol. 15:1461199. doi: 10.3389/fpsyg.2024.1461199
Lim, K. K., Matchar, D. B., Tan, C. S., Yeo, W., Østbye, T., Howe, T. S., et al. (2020). The association between psychological resilience and physical function among older adults with hip fracture surgery. J. Am. Med. Dir. Assoc. 21, 260–266.e2. doi: 10.1016/j.jamda.2019.07.005
Long, Q., Guo, J., Zhong, Q., Jiang, S., Wiley, J., and Chen, J. (2021). General self-efficacy and social support as mediators of the association between perceived stress and quality of life among rural women with previous gestational diabetes mellitus. J. Clin. Nurs. 30, 1026–1036. doi: 10.1111/jocn.15648
Losciale, J. M., Truong, L. K., Zhang, K., Silvester-Lee, T., Miciak, M., Pajkic, A., et al. (2024). Assessing the efficacy of the stop OsteoARthritis (SOAR) program: a randomized delayed-controlled trial in persons at increased risk of early onset post-traumatic knee osteoarthritis. Osteoarthr. Cartil. 32, 1001–1012. doi: 10.1016/j.joca.2024.04.003
Nomoto, Y., Nishi, Y., Nakagawa, K., Goto, K., Kondo, Y., Yamashita, J., et al. (2024). Persistent postsurgical pain in hip fracture patients. A prospective longitudinal study with multifaceted assessment. Br. J. Pain 19, 51–61. doi: 10.1177/20494637241300385
Norekvål, T. M., Allore, H. G., Bendz, B., Bjorvatn, C., Borregaard, B., Brørs, G., et al. (2020). Rethinking rehabilitation after percutaneous coronary intervention: a protocol of a multicentre cohort study on continuity of care, health literacy, adherence and costs at all care levels (the CONCARDPCI). BMJ Open 10:e031995. doi: 10.1136/bmjopen-2019-031995
Ploutarchou, G., Savva, C., Karagiannis, C., Pavlou, K., O’Sullivan, K., and Korakakis, V. (2023). The effectiveness of cognitive behavioural therapy in chronic neck pain: a systematic review with meta-analysis. Cogn. Behav. Ther. 52, 523–563. doi: 10.1080/16506073.2023.2236296
Rolls, C. A., Obamiro, K. O., Chalmers, L., and Bereznicki, L. R. E. (2017). The relationship between knowledge, health literacy, and adherence among patients taking oral anticoagulants for stroke thromboprophylaxis in atrial fibrillation. Cardiovasc. Ther. 35. doi: 10.1111/1755-5922.12304
Salari, N., Darvishi, N., Ahmadipanah, M., Shohaimi, S., and Mohammadi, M. (2022). Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 17:334. doi: 10.1186/s13018-022-03222-1
Sanchís-Soler, G., Sebastiá-Amat, S., and Parra-Rizo, M. A. (2025). Mental health and social integration in active older adults according to the type of sport practiced. Acta Psychol. 255:104920. doi: 10.1016/j.actpsy.2025.104920
Shafshak, T. S., and Elnemr, R. (2020). The visual analogue scale versus numerical rating scale in measuring pain severity and predicting disability in low back pain. J. Clin. Rheumatol. 27, 282–285. doi: 10.1097/rhu.0000000000001320
Soliman, G., Fortinsky, R. H., Mangione, K., Beamer, B. A., Magder, L., Binder, E. F., et al. (2022). Impact of psychological resilience on walking capacity in older adults following hip fracture. J. Am. Geriatr. Soc. 70, 3087–3095. doi: 10.1111/jgs.17930
Soong, R. Y., Low, C. E., Ong, V., Sim, I., Lee, C., Lee, F., et al. (2025). Exercise interventions for depression, anxiety, and quality of life in older adults with Cancer. JAMA Netw. Open 8:e2457859. doi: 10.1001/jamanetworkopen.2024.57859
Sundkvist, J., Brüggeman, A., Sayed-Noor, A., Möller, M., Wolf, O., and Mukka, S. (2021). Epidemiology, classification, treatment, and mortality of adult femoral neck and basicervical fractures: an observational study of 40,049 fractures from the Swedish fracture register. J. Orthop. Surg. Res. 16:561. doi: 10.1186/s13018-021-02701-1
Terradas-Monllor, M., Rierola-Fochs, S., Merchan-Baeza, J. A., Parés-Martinez, C., Font-Jutglà, C., Hernández-Hermoso, J. A., et al. (2024). Comparison of pain, functional and psychological trajectories between total and unicompartmental knee arthroplasties: secondary analysis of a 6-month prospective observational study. Arch. Orthop. Trauma Surg. 145:32. doi: 10.1007/s00402-024-05710-x
Tourunen, A., Siltanen, S., Saajanaho, M., Koivunen, K., Kokko, K., and Rantanen, T. (2019). Psychometric properties of the 10-item Connor–Davidson resilience scale among Finnish older adults. Aging Ment. Health 25, 99–106. doi: 10.1080/13607863.2019.1683812
Vu, M. T. T., Ho, H. Q., and Lin, G. (2024). Ehealth interventions of health literacy for stroke survivors: systematic review and meta-analysis. Public Health Nurs. 42, 516–523. doi: 10.1111/phn.13432
Wang, S., Sun, J., Yin, X., and Li, H. (2022). Effect of virtual reality technology as intervention for people with kinesiophobia: a meta-analysis of randomised controlled trials. J. Clin. Nurs. 32, 3074–3086. doi: 10.1111/jocn.16397
Westerdahl, E., Bergh, C., and Urell, C. (2024). Patient-reported physical activity, pain, and fear of movement after cardiac surgery: a descriptive cross-sectional study. Scand. Cardiovasc. J. 58:2393311. doi: 10.1080/14017431.2024.2393311
Wideman, T. H., Asmundson, G. G. J., Smeets, R. J. E. M., Zautra, A. J., Simmonds, M. J., Sullivan, M. J. L., et al. (2013). Rethinking the fear avoidance model: toward a multidimensional framework of pain-related disability. Pain 154, 2262–2265. doi: 10.1016/j.pain.2013.06.005
Wills, C., Ghani, S., Tubbs, A., Fernandez, F.-X., Athey, A., Turner, R., et al. (2021). Chronotype and social support among student athletes: impact on depressive symptoms. Chronobiol. Int. 38, 1319–1329. doi: 10.1080/07420528.2021.1927072
Wood, L., Bejarano, G., Csiernik, B., Miyamoto, G. C., Mansell, G., Hayden, J. A., et al. (2023). Pain catastrophising and kinesiophobia mediate pain and physical function improvements with Pilates exercise in chronic low back pain: a mediation analysis of a randomised controlled trial. J. Physiother. 69, 168–174. doi: 10.1016/j.jphys.2023.05.008
Xu, L., and Chen, W. (2025). The incidence and risk factors of phobic movement disorder after hip fracture internal fixation surgery. J. Orthop. Surg. Res. 20:323. doi: 10.1186/s13018-025-05750-y
Yong, J., MacDermid, J. C., Packham, T., Bobos, P., Richardson, J., and Moll, S. (2022). Performance-based outcome measures of dexterity and hand function in person with hands and wrist injuries: a scoping review of measured constructs. J. Hand Ther. 35, 200–214. doi: 10.1016/j.jht.2021.04.017
Zare, Z., Ghane, G., Shahsavari, H., Ahmadnia, S., and Ghiyasvandian, S. (2024). Social life after hip fracture: a qualitative study. J. Patient Exp. 11: 23743735241241174. doi: 10.1177/23743735241241174
Zelle, D. M., Corpeleijn, E., Klaassen, G., Schutte, E., Navis, G., and Bakker, S. J. L. (2016). Fear of movement and Low self-efficacy are important barriers in physical activity after renal transplantation. PLoS One 11:e0147609. doi: 10.1371/journal.pone.0147609
Zeng, Z., Shen, Y., Wan, L., Yang, X., Hu, Q., Luo, H., et al. (2024). Kinesiophobia in patients after cardiac surgery: a scoping review. BMC Cardiovasc. Disord. 24:469. doi: 10.1186/s12872-024-04140-2
Zhang, S., Wang, Z., Lin, X., Li, Y., Xue, Y., Ban, J., et al. (2022). Kinesiophobia and self-management behaviour related to physical activity in Chinese patients with coronary heart disease: the mediating role of self-efficacy. Nurs. Open 10, 105–114. doi: 10.1002/nop2.1283
Keywords: kinesiophobia, femoral neck fracture, psychological resilience, social support, geriatric rehabilitation
Citation: Guo K, Zhou L, Zhang M, Hu X, Han Y, Hou J, Cheng J, Shen X, Wang Q and Zhang Q (2025) Postoperative kinesiophobia in elderly patients with femoral neck fractures: a prospective study of psychological and social determinants. Front. Psychol. 16:1622585. doi: 10.3389/fpsyg.2025.1622585
Edited by:
Anna Maria Berardi, Université de Lorraine, FranceReviewed by:
María Antonia Parra Rizo, Miguel Hernández University of Elche, SpainDagmara Wasiuk-Zowada, Medical University of Silesia, Poland
Copyright © 2025 Guo, Zhou, Zhang, Hu, Han, Hou, Cheng, Shen, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Quanying Zhang, TGlmZWxpa2UxMTNAMTYzLmNvbQ==
†These authors share first authorship
 Kankai Guo1,2†
Kankai Guo1,2† Quanying Zhang
Quanying Zhang