- 1Child and Adolescent Neuropsychiatry Unit, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
- 2Department of Life Sciences and Public Health, Catholic University, Rome, Italy
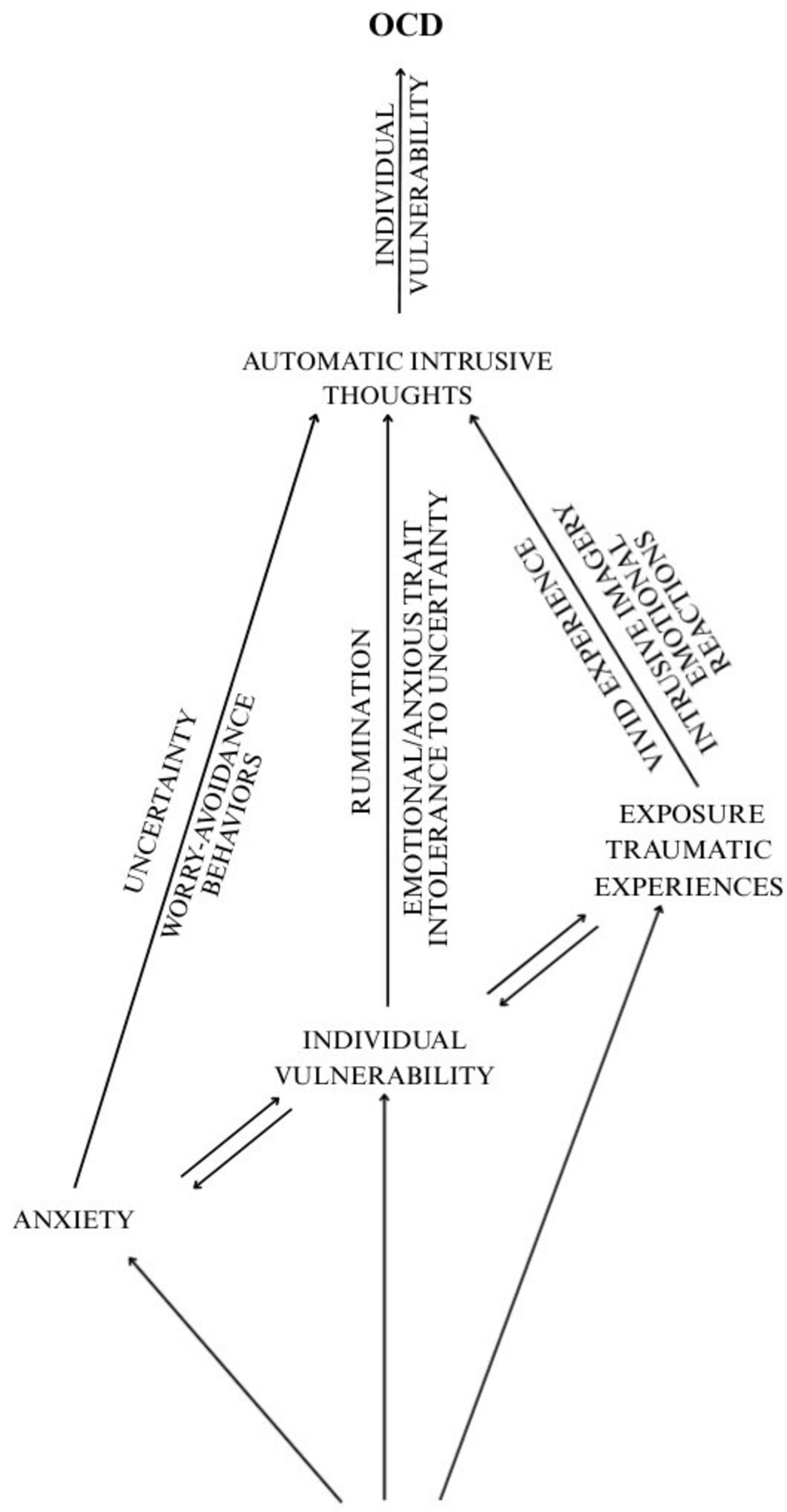
Adverse events (AEs), such as natural disasters, community violence and public health crises, impact global health and are associated with fear, anxiety and disorientation. AEs are related to both short-term and long-term mental health problems in children and adolescents. Particularly, research has shown a significantly higher prevalence of obsessive-compulsive disorder (OCD) in individuals with a history of trauma. This work aims to explore the obsessive-compulsive (OC) trajectories following an AE, considering the role played by individual vulnerability, anxiety and psychological consequences for children and adolescents. In this direction, Coronavirus Disease 2019 (COVID-19) pandemic has represented an ideal and unique AE of concomitant factors that can help to understand the obsessive trajectory. Our framework shows that intrusive flashbacks, following a traumatic experience, can turn into automatic intrusive thoughts that become persistent and emotionally intense, similar to obsessive reactions. Intrusive thoughts can evolve into obsessive patterns, leading to compulsive behaviors aimed at reducing discomfort. The nature of the traumatic event may influence the development of specific OC symptoms. Risk factors include individual vulnerability, such as developmental stage and emotional reactivity, which can exacerbate obsessive stress responses. Anxiety plays a key role, as increased stress can stimulate automatic intrusive thoughts and amplify OCD reactions, especially in younger individuals. Disruptions in daily life can further increase anxiety and maladaptive behaviors in children and adolescents, affecting psychological well-being. The psychological effects of AEs can continue well beyond the events themselves. It is necessary to monitor and support young people involved to prevent their development. Community and individual resources are essential to promote resilience following such events.
1 Introduction
Adverse events pose critical challenges to global health. Such events encompass a broad spectrum of phenomena, ranging from natural disasters (e.g., hurricanes, floods, earthquakes) to community violence (e.g., military conflict, terrorism, massacres) and public health crises, including epidemics (e.g., SARS, H1N1, Ebola, COVID-19) elicit widespread fear, anxiety and disorientation within the affected populations (Chrisman and Dougherty, 2014; Maboloc, 2024; Mulenga-Cilundika et al., 2022).
As significant psychosocial stressors, AEs may markedly impact individuals’ lives, with children and adolescents (and their families) standing at particular risk of short- and long-term adverse mental health outcomes (Lai et al., 2017; Sprang and Silman, 2013).
Specifically, elevated stress or anxiety during an AE has been shown to exacerbate OC symptoms in children and adolescents. Notably, individuals with a history of trauma exhibit a significantly higher prevalence of OCD (Palacio-Ortiz et al., 2020).
The present study aimed at examining the potential trajectories of OC symptomatology in children and adolescents following exposure to potentially traumatic events. The investigation considered the interplay of environmental factors associated with AEs, individual vulnerability and anxiety, as well as the broader psychological consequences stemming from the traumatic experience.
The term “OC symptoms” is used to refer to subclinical symptoms that do not significantly interfere with daily functioning or developmental tasks, while “OCD” is used to denote a clinically diagnosed disorder characterized by persistent behavioral and psychological patterns that disrupt functioning and are typically accompanied by anxiety and avoidance behaviors, as outlined in the DSM-5-TR (American Psychiatric Association, 2022).
2 Methodology
The study comprised a review of the relevant literature, in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Page et al., 2021). An in-depth analysis of academic works was conducted, and sources were carefully verified using electronic databases such as PubMed, CINAHL, PsycInfo, MedLine and the Cochrane Library. Keywords used in the search included: (“Adverse events”) AND (“Trauma”) AND (“Obsessive-compulsive symptoms/trajectories” OR “Automatic intrusive thoughts”) AND (“Children/teenagers”). The review was conducted on March 25, 2025 at 10:30 am, focusing on publications from the preceding 20 years. The inclusion criteria defined original research articles, observational articles (cross-sectional or retrospective) and theoretical or experimental works with psychosocial relevance, addressing pediatric populations during the Coronarovirus Disease 2019 (COVID-19) pandemic. Articles unrelated to the study objectives, duplicates across databases, case reports or case series, and studies aimed at instrument validation were excluded. No restrictions were applied regarding language or study design.
2.1 Trauma and OC symptoms: a clinical overlap
The clinical overlap between trauma and OCD is well-documented (Dykshoorn, 2014; Pinciotti et al., 2022), with both conditions characterized by intrusive thoughts, neutralizing behaviors and maladaptive reactions. Traumatic experiences often lead to intrusive symptoms such as flashbacks, hyperarousal, nightmares and irritability. These symptoms are episodic in nature, typically triggered by traumatic memories and marked by intense sensory recall. Moreover, the cognitive impact of trauma is significant: it can impair memory, reduce attentional capacity, contribute to the development of distorted thoughts and beliefs, and hinder the formation of a coherent and integrated memory of the traumatic experience. In contrast, OC symptoms are typically triggered by sudden, emotionally charged experiences perceived as threatening, and frequently manifest as repetitive, intrusive thoughts that are egodystonic. The cognitive profile of OCD often includes marked intolerance of uncertainty, perfectionism, an exaggerated sense of responsibility, overestimation of danger and difficulties with executive functioning (e.g., planning, organization, behavioral regulation) and memory. Under both conditions, children and adolescents may attempt to alleviate distress through compulsive neutralizing behaviors and/or avoidance strategies.
In the initial phase following a traumatic experience, individuals may relive the event through intrusive flashbacks and dysregulated emotional reactions. Over time, these flashbacks can evolve into automatic intrusive thoughts, consolidating the memory of the traumatic event. While these intrusive memories may gradually lose some of their maladaptive intensity, they retain a vivid and emotionally charged nature, acquiring characteristics similar to an “obsessive reaction” and becoming widespread and independent (Fostick et al., 2012; Table 1).
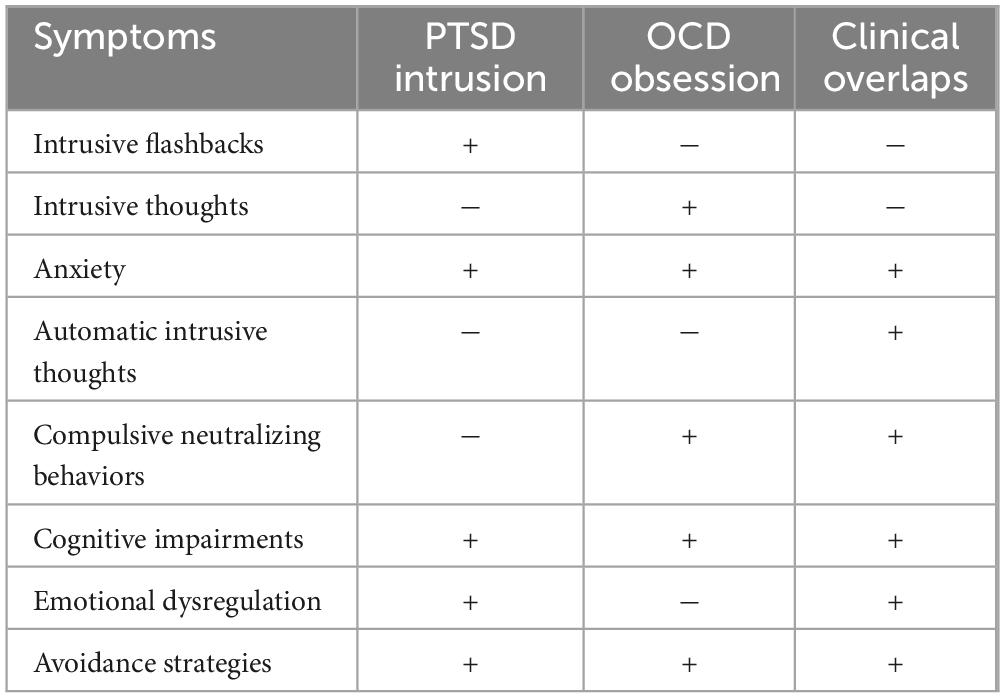
Table 1. Distinguishing features and overlaps between PTSD-related intrusions and OCD obsessions in children/adolescents.
Sasson et al. (2005) found that the specific attributes of a traumatic event influence the emergence of distinct OC symptomatology.
On a neurobiological level, the Cortico-Striato-Thalamo-Cortical Circuit (CSTC) has been identified as a primary brain system implicated in OCD. The CSTC consists of interconnected neural pathways from the cerebral cortex to the striatum, thalamus, and back to the cortex. It plays a crucial role in several cognitive functions, including motor control, motivation, learning and decision-making. In OCD, two regions within this circuit appear to be significantly implicated: the anterior cingulate cortex (ACC) and the orbitofrontal cortex (OFC), both of which are critical in the emergence and persistence of obsessive symptoms (Dougherty et al., 2018). The OFC is involved in risk assessment, behavioral regulation in response to environmental stimuli and the attribution of meaning to those stimuli. In the context of OCD, this function becomes dysregulated, leading to an overestimation of the negative consequences of a given action, the emergence of intrusive thoughts and a persistent perception of danger. Moreover, the ACC, which governs error monitoring, motivational drive and urgency, contributes to the compulsive dimension of OCD by generating the feeling that something is not “complete” or “correct,” thereby triggering compulsive behaviors. For example, the hygiene-related compulsions (e.g., excessive handwashing) observed among certain youth populations during the pandemic may reflect an environmentally conditioned response aimed at reducing anxiety and fear, underpinned by CSTC activation (Ornell et al., 2021).
At the neurotransmitter level, CSTC dysfunction is associated with reduced serotonergic and GABAergic inhibitory input from both medial prefrontal cortex interneurons and the midbrain raphe nuclei. This deficit leads to hyperactivity in the ACC and OFC, which in turn drives dopaminergic and glutamatergic hyperactivity in the striatum and thalamus, resulting in unchecked CSTC activity (Dougherty et al., 2018; Karthik et al., 2020).
The neurobiology of OCD and post-traumatic stress disorder (PTSD) also demonstrates notable overlap. Both conditions involve dysfunctions in specific brain areas—particularly the amygdala and prefrontal cortex— that are linked via circuits associated with stress and fear. The hyperactivation of these networks contribute to heightened anxiety and the emergence of intrusive thoughts or images. The amygdala, in particular, plays a central role in the consolidation of emotional memory, preserving experiences accompanied by strong emotional intensity and rendering them more lasting and meaningful. Thus, non-rational fear and anxiety may arise from traumatic events that have become fixed in emotional memory (Cheng et al., 2015).
2.2 The COVID-19 pandemic as a model of emerging OC symptoms
During the COVID-19 pandemic, Darvishi et al. (2020) documented that washing compulsions were 68 the most common OC symptom in a non-clinical sample of students. The authors found that young 69 people may have developed compulsive hand-washing behaviors after learning that this 70 recommended action helped alleviate their anxiety. These behaviors could be attributed to a fear of 71 contagion and an obsession with hygiene. It is therefore plausible that intrusive thoughts stemming 72 from a traumatic experience may become structured into obsessive patterns, triggering repetitive or 73 compulsive behaviors aimed at reducing the distress caused by such obsessions (Darvishi et al., 2020).
A key risk factor for the emergence of OC symptoms following an AE is individual vulnerability. 75 Secer and Ulas demonstrated that adverse environmental conditions (e.g., fear of contagion 76 during the COVID-19 pandemic), combined with subjective vulnerabilities (e.g., heightened 77 emotional reactivity, avoidance behaviors, anxiety-depression), can act as precipitating factors for 78 OC symptoms (Seçer and Ulaş, 2021). Similarly, Raymond et al. (2022) found that post-traumatic stress symptoms and 79 anxiety were common among young people with socio-emotional weakness, characterized by 80 anxious traits, intolerance to uncertainty, and a tendency toward rumination.
Adult studies, particularly those involving civilians and small samples of war veterans, have long documented the presence of OCD in individuals with a history of trauma (Kessler et al., 2005). For instance, Morina et al. (2016) studied a sample of 51 adult civilians (28 males) who survived the Kosovo War, finding that 35 and 39% scored above the clinical threshold for probable OCD and PTSD, respectively. Notably, participants exhibiting elevated PTSD symptoms were significantly more likely to present with OC symptoms, and vice versa (Morina et al., 2016).
In contrast, the scientific literature on pediatric populations remains comparatively limited. Nonetheless, understanding OCD symptom onset and development in children and adolescents exposed to trauma is crucial for elucidating the relationship between trauma and compulsive symptomatology.
The unique and large-scale AE of the COVID-19 pandemic offers a valuable context for examining the emergence of OCD symptom trajectories, particularly in pediatric populations. The pandemic simultaneously introduced multiple and varied stressors, including fear of contagion, stringent protection measures, environmental disruption, personal trauma and individual vulnerability. Moreover, different from isolated AEs (e.g., natural disasters, localized community crises), the pandemic was characterized by its global scale, prolonged nature and chronic uncertainty. It also featured significant social isolation, media saturation and environmental and familial stress.
Review articles and meta-analyses have documented these adverse effects (Ma et al., 2021) in children and adolescents.
Cunning and Hodes (2022) demonstrated that certain factors related to the pandemic (e.g., lockdown measures, heightened attention to hygiene, family-related adversities that intensified fear of contagion) were associated with increased OCD symptoms. Particular emphasis was placed on hygiene-related behaviors (e.g., handwashing) and contamination fears, as well as the role played by the media, which perpetuated anxiety through continuous updates on virus transmission, mortality rates and quarantine protocols. These factors collectively heightened the perceived threat among adolescents during the pandemic (Liu et al., 2020).
It is plausible that certain groups of adolescents possess a lower threshold for tolerating AEs, rendering them more susceptible to developing OC symptoms as a maladaptive coping mechanism (Chen et al., 2020). Supporting this hypothesis, Seçer and Ulaş (2021), in a study involving 598 high school students, found that adverse environmental conditions (e.g., fear of contagion during the pandemic), when combined with individual vulnerabilities (e.g., heightened emotional reactivity, avoidance behaviors, anxiety-depressive symptoms) significantly predicted the emergence of OCD symptoms. In particular, emotional reactivity and experiential avoidance were identified as key risk factors for broader psychosocial disturbance. These findings align with those of Raymond et al. (2022) who observed that anxiety and PTSD symptoms were prevalent among adolescents with socio-emotional vulnerabilities during the pandemic, characterized by anxious traits, intolerance of uncertainty and a tendency toward rumination. Consistently, anxiety has been highlighted as a critical dimension of individual vulnerability in the development of OC symptoms in young populations (Rueppel et al., 2024).
2.3 The role of anxiety and intolerance of uncertainty
Vulnerability to anxiety may constitute a significant risk factor in the development of OC symptoms. Anxiety and OCD share several clinical and behavioral features, including persistent rumination, excessive worry and avoidance behaviors. During the COVID-19 pandemic, the emotional burden— driven by an unfamiliar virus, absence of definitive treatment and potential lethality—was particularly intense, often leading to overwhelming anxiety and worry. These factors may have contributed to intrusive thoughts related to contagion and disease, which, in some cases, may have triggered OC symptomatology. Darvishi et al. (2020) investigated this phenomenon in a non-clinical sample of students during the pandemic, reporting that handwashing compulsions were the most commonly observed OC symptom. The authors further proposed that young people may have developed compulsive handwashing behaviors as a response to the relief they experienced after engaging in a recommended public health practice.
Intolerance of uncertainty has also been identified as a key factor in both anxiety and OC symptoms, particularly in high-risk or ambiguous situations (Gillett et al., 2018). This dynamic was particularly evident during the early stages of the COVID-19 pandemic, when unprecedented levels of uncertainty, coupled with lockdowns and stringent protective measures, created an environment that exacerbated OC symptoms. Data collected during March and April 2020 consistently supported this observation, demonstrating a sharp rise in OC symptomatology linked to the unique challenges of the pandemic (Singh et al., 2020).
It is difficult to understand the precise nature of obsessive thinking and its manifestations across varying emotional states, individual predispositions and environmental conditions. However, it is evident that children with specific vulnerabilities, when exposed to prolonged stress, persistent uncertainty and intense environmental stimuli, are more likely to develop repetitive thought patterns that may evolve into intrusive thoughts and, ultimately, obsessions. In individuals experiencing intense anxiety, obsessions are typically accompanied by heightened uncertainty, worry and avoidance behaviors. Among those with distinct socio-emotional vulnerabilities (e.g., anxious temperament, ruminative tendencies, intolerance to uncertainty), obsessive thinking may be further reinforced. In cases involving traumatic exposure, vivid subjective experiences and intrusive mental imagery (e.g., flashbacks of emotionally salient memories) often play a central role in activating and sustaining obsessive thoughts (Figure 1).
This body of evidence underscores the heightened psychological vulnerability of children and adolescents during AEs and the role of neurobiological plasticity in shaping responses to environmental stimuli.
3 Discussion
The impact of AEs on the lives of young individuals extends beyond their immediate emotional state, often inducing broader environmental, familial, and community stress. For instance, during the COVID-19 pandemic, lockdowns and necessary quarantine measures led to substantial lifestyle changes, accompanied by heightened anxiety, fear of infection, and pervasive concern. These dynamics compromised individuals’ ability to implement effective coping strategies, and the limited availability of psychiatric support services further exacerbated the situation (World Health Organization, 2020).
Understanding the relationship between AEs and the onset of OCD is crucial for advancing knowledge of its pathogenesis. Approximately 50% of adults with OCD report an early onset of symptoms before the age of 18 years (Geller et al., 2021). AEs and traumatic experiences may act as catalysts for obsessive trajectories, influencing clinical symptomatology and complicating long-term recovery. In children and adolescents, the obsessive consequences of AEs often persist long after the stressful event, exerting significant and enduring effects on their psychological well-being.
A cross-sectional survey (Habib and Zulfiqar, 2025) investigated the prevalence and comorbidity of PTSD and post-traumatic OCD among Afghan refugees in Pakistan, with a focus on the intergenerational transmission of PTSD. The study involved 48 male adults representing three generations of 16 refugee families. The results revealed a significant correlation between post-traumatic OCD and PTSD, indicating a substantial co-occurrence between the two disorders. Overall, 79.20% of participants received a diagnosis of post-traumatic OCD, with higher prevalence in the first generation (87.5%) compared to the second and third generations (75.0%). Additionally, PTSD prevalence varied significantly across generations, with a trend toward reduced symptom severity over time. These findings underline the need to address the comorbidity of both disorders in populations exposed to AEs, while also considering intergenerational negative outcomes in terms of mental health.
It is therefore imperative to closely monitor young individuals and provide continuous support to prevent the long-term development of psychological disorders. Lowe et al. (2015), in their study on psychological distress following Hurricane Sandy, emphasized the importance of leveraging both community and individual resources to foster resilience in post-disaster contexts.
3.1 Potential confounders and limitations of the reviewed studies
Many of the studies examined (most of which were conducted during the pandemic) were cross-sectional in nature, relying on self-report questionnaires or online surveys. Such methodologies limit the ability to assess formal psychiatric diagnoses or pre-existing subclinical conditions. As a result, the reported prevalence rates may be inflated or include false positives, particularly when the studies failed to account for participants with genetic predispositions to OCD or those from socio-economically disadvantaged backgrounds—both of which may increase vulnerability to psychopathology following AEs. AEs tend to disproportionately affect economically and socially marginalized populations, with chronic stress, limited access to care and overcrowded living conditions acting as potential confounding factors that may intensify anxiety and compulsive symptoms. Finally, accurate differentiation between normative and pathological behavior requires diagnoses in clinical settings, posing a further methodological limitation.
3.2 Limitations
The review itself is subject to several limitations. First, the data examined were predominantly derived from studies focused on the COVID-19 pandemic, potentially limiting the generalizability of the findings to other types of AEs and reducing analytical depth. Second, there was a lack of neurobiological evidence to support the correlation between AEs and OC manifestation in children and adolescents. Additionally, the lack of longitudinal studies of youth prevented a comprehensive and robust evaluation. Finally, the narrative and non-systematic nature of the review inherently constrained the scope and reliability of its conclusions.
4 Conclusion
In conclusion, adverse events (AEs) AES significantly impact the mental health of children and adolescents, often correlating with the development of OC symptoms. The interplay between trauma, individual vulnerability, and environmental stressors plays a crucial role in shaping the trajectory of these symptoms. The COVID-19 pandemic highlighted how environmental changes, such as fear and uncertainty, can exacerbate OC behaviors, especially in vulnerable youth.
It is essential that mental health services for children and adolescents ensure adequate and timely psychological and/or psychiatric support during exceptional circumstances (e.g., lockdowns, social restrictions). Such support should be coordinated with social welfare services and, more broadly, with local and national civil protection services. In crisis contexts, diverse and alternative intervention strategies must be considered. Remote modalities (e.g., telephone, online) may be necessary to provide psychological or educational assistance for both children and their caregivers. Additionally, innovative approaches aligned with the principles of digital psychiatry, such as those incorporating artificial intelligence and internet-based technologies, should be explored (Ćosić et al., 2020).
Emerging digital technologies hold promise for early screening and prevention among high-risk populations. Local health authorities should distribute accessible family guidelines promoting healthy cohabitation strategies and public health measures, and media outlets should play a central role in promoting awareness and disseminating reliable information. Finally, the psychological well-being of children should be monitored in both the short and long term, particularly among those demonstrating socio-emotional vulnerability. Early identification of obsessive or post-traumatic symptoms—and of trajectories suggestive of OC patterns—may support timely intervention and the strengthening of psychological resilience.
Understanding the links between trauma and OCD is vital for improving therapeutic strategies and fostering resilience in affected individuals.
Author contributions
FD: Conceptualization, Data curation, Supervision, Writing – original draft, Resources, Writing – review & editing. MP: Writing – review & editing, Supervision, Writing – original draft, Visualization. IB: Writing – original draft, Conceptualization, Writing – review & editing. SV: Project administration, Data curation, Writing – original draft, Resources, Visualization, Validation, Conceptualization, Writing – review & editing, Supervision, Methodology, Formal analysis, Investigation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Italian Ministry of Health with Current Research funds.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
American Psychiatric Association (2022). Diagnostic and statistical manual of mental disorders: DSM-5-TR™, text revision, 5th Edn. Washington, DC: American Psychiatric Association Publishing.
Chen, B., Sun, J., and Feng, Y. (2020). How have COVID-19 isolation policies affected young people’s mental health? – evidence from chinese college students. Front. Psychol. 11:1529. doi: 10.3389/fpsyg.2020.01529
Cheng, B., Huang, X., Li, S., Hu, X., Luo, Y., Wang, X., et al. (2015). Gray matter alterations in post-traumatic stress disorder, obsessive–compulsive disorder, and social anxiety disorder. Front. Behav. Neurosci. 9:219. doi: 10.3389/fnbeh.2015.00219
Chrisman, A. K., and Dougherty, J. G. (2014). Mass trauma. Child Adolesc. Psychiatr. Clin. N. Am. 23, 257–279. doi: 10.1016/j.chc.2013.12.004
Ćosić, K., Popović, S., Šarlija, M., and Kesedžić, I. (2020). Impact of human disasters and COVID-19 pandemic on mental health: Potential of digital psychiatry. Psychiatr. Danub. 32, 25–31. doi: 10.24869/psyd.2020.25
Cunning, C., and Hodes, M. (2022). The COVID-19 pandemic and obsessive–compulsive disorder in young people: Systematic review. Clin. Child Psychol. Psychiatry 27, 18–34. doi: 10.1177/13591045211028169
Darvishi, E., Golestan, S., Demehri, F., and Jamalnia, S. (2020). A cross-sectional study on cognitive errors and obsessive-compulsive disorders among young people during the outbreak of coronavirus disease 2019. Act. Nerv. Super. 62, 137–142. doi: 10.1007/s41470-020-00077-x
Dougherty, D. D., Brennan, B. P., Stewart, S. E., Wilhelm, S., Widge, A. S., and Rauch, S. L. (2018). Neuroscientifically informed formulation and treatment planning for patients with obsessive-compulsive disorder: A review. JAMA Psychiatry 75:1081. doi: 10.1001/jamapsychiatry.2018.0930
Dykshoorn, K. L. (2014). Trauma-related obsessive–compulsive disorder: A review. Health Psychol. Behav. Med. 2, 517–528. doi: 10.1080/21642850.2014.905207
Fostick, L., Nacasch, N., and Zohar, J. (2012). Acute Obsessive Compulsive Disorder (OCD) in veterans with Posttraumatic Stress Disorder (PTSD). World J. Biol. Psychiatry 13, 312–315. doi: 10.3109/15622975.2011.607848
Geller, D. A., Homayoun, S., and Johnson, G. (2021). Developmental considerations in obsessive compulsive disorder: Comparing pediatric and adult-onset cases. Front. Psychiatry 12:678538. doi: 10.3389/fpsyt.2021.678538
Gillett, C. B., Bilek, E. L., Hanna, G. L., and Fitzgerald, K. D. (2018). Intolerance of uncertainty in youth with obsessive-compulsive disorder and generalized anxiety disorder: A transdiagnostic construct with implications for phenomenology and treatment. Clin. Psychol. Rev. 60, 100–108. doi: 10.1016/j.cpr.2018.01.007
Habib, A., and Zulfiqar, N. (2025). A three-generation study of the prevalence and comorbidity of posttraumatic obsessive-compulsive disorder and posttraumatic stress disorder among afghan refugees. Genealogy 9:4. doi: 10.3390/genealogy9010004
Karthik, S., Sharma, L. P., and Narayanaswamy, J. C. (2020). Investigating the role of glutamate in obsessive-compulsive disorder: Current perspectives. Neuropsychiatr. Dis. Treat. 16, 1003–1013. doi: 10.2147/NDT.S211703
Kessler, R. C., Chiu, W. T., Demler, O., and Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-Month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 62:617. doi: 10.1001/archpsyc.62.6.617
Lai, B. S., Lewis, R., Livings, M. S., La Greca, A. M., and Esnard, A. (2017). Posttraumatic stress symptom trajectories among children after disaster exposure: A review. J. Trauma. Stress 30, 571–582. doi: 10.1002/jts.22242
Liu, M., Zhang, H., and Huang, H. (2020). Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health 20:1649. doi: 10.1186/s12889-020-09761-8
Lowe, S. R., Sampson, L., Gruebner, O., and Galea, S. (2015). Psychological resilience after hurricane sandy: The influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS One 10:e0125761. doi: 10.1371/journal.pone.0125761
Ma, L., Mazidi, M., Li, K., Li, Y., Chen, S., Kirwan, R., et al. (2021). Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 293, 78–89. doi: 10.1016/j.jad.2021.06.021
Maboloc, C. R. (2024). Natural disasters as a public health issue. J. Public Health 46, e534–e535. doi: 10.1093/pubmed/fdae039
Morina, N., Sulaj, V., Schnyder, U., Klaghofer, R., Müller, J., Martin-Sölch, C., et al. (2016). Obsessive-compulsive and posttraumatic stress symptoms among civilian survivors of war. BMC Psychiatry 16:115. doi: 10.1186/s12888-016-0822-9
Mulenga-Cilundika, P., Ekofo, J., Kabanga, C., Criel, B., Van Damme, W., and Chenge, F. (2022). Indirect effects of ebola virus disease epidemics on health systems in the democratic republic of the congo, guinea, sierra leone and liberia: A scoping review supplemented with expert interviews. Int. J. Environ. Res. Public. Health 19:13113. doi: 10.3390/ijerph192013113
Ornell, F., Braga, D. T., Bavaresco, D. V., Francke, I. D., Scherer, J. N., Von Diemen, L., et al. (2021). Obsessive-compulsive disorder reinforcement during the COVID-19 pandemic. Trends Psychiatry Psychother. 43, 81–84. doi: 10.47626/2237-6089-2020-0054
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Palacio-Ortiz, J. D., Londoño-Herrera, J. P., Nanclares-Márquez, A., Robledo-Rengifo, P., and Quintero-Cadavid, C. P. (2020). Trastornos psiquiátricos en los niños y adolescentes en tiempo de la pandemia por COVID-19. Rev. Colomb. Psiquiatr. 49, 279–288. doi: 10.1016/j.rcp.2020.05.006
Pinciotti, C. M., Fontenelle, L. F., Van Kirk, N., and Riemann, B. C. (2022). Co-Occurring obsessive-compulsive and posttraumatic stress disorder: A review of conceptualization, assessment, and cognitive behavioral treatment. J. Cogn. Psychother. 36, 207–225. doi: 10.1891/jcp-2021-0007
Raymond, C., Provencher, J., Bilodeau-Houle, A., Leclerc, J., and Marin, M.-F. (2022). A longitudinal investigation of psychological distress in children during COVID-19: The role of socio-emotional vulnerability. Eur. J. Psychotraumatol. 13:2021048. doi: 10.1080/20008198.2021.2021048
Rueppel, M., Becker, H. C., Iturra-Mena, A., Bilek, E. L., Monk, C. S., Phan, K. L., et al. (2024). Obsessive–Compulsive symptoms: Baseline prevalence, comorbidity, and implications in a clinically anxious pediatric sample. Child Psychiatry Hum. Dev. doi: 10.1007/s10578-023-01658-y [Epub ahead of print].
Sasson, Y., Dekel, S., Nacasch, N., Chopra, M., Zinger, Y., Amital, D., et al. (2005). Posttraumatic obsessive–compulsive disorder: A case series. Psychiatry Res. 135, 145–152. doi: 10.1016/j.psychres.2004.05.026
Seçer, İ, and Ulaş, S. (2021). An investigation of the effect of COVID-19 on OCD in youth in the context of emotional reactivity, experiential avoidance, depression and anxiety. Int. J. Ment. Health Addict. 19, 2306–2319. doi: 10.1007/s11469-020-00322-z
Singh, S., Roy, D., Sinha, K., Parveen, S., Sharma, G., and Joshi, G. (2020). Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 293:113429. doi: 10.1016/j.psychres.2020.113429
Sprang, G., and Silman, M. (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 7, 105–110. doi: 10.1017/dmp.2013.22
Keywords: adverse events, trauma, obsessive-compulsive symptoms/trajectories, automatic intrusive thoughts, children and adolescents
Citation: Demaria F, Pontillo M, Bertoncini I and Vicari S (2025) Obsessive trajectories in children and adolescents exposed to adverse events (coronavirus disease 2019: global crisis teaches). Front. Psychol. 16:1623629. doi: 10.3389/fpsyg.2025.1623629
Received: 07 May 2025; Accepted: 15 September 2025;
Published: 29 September 2025.
Edited by:
Małgorzata Stępień-Nycz, Jagiellonian University, PolandReviewed by:
Omar Shazley, Saint James School of Medicine, United StatesCopyright © 2025 Demaria, Pontillo, Bertoncini and Vicari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francesco Demaria, ZnJhbmNlc2NvLmRlbWFyaWFAb3BiZy5uZXQ=
 Francesco Demaria
Francesco Demaria Maria Pontillo
Maria Pontillo Ilaria Bertoncini1
Ilaria Bertoncini1 Stefano Vicari
Stefano Vicari