- 1General Hospital of Ningxia Medical University, Yinchuan, China
- 2School of Nursing, Ningxia Medical University, Yinchuan, China
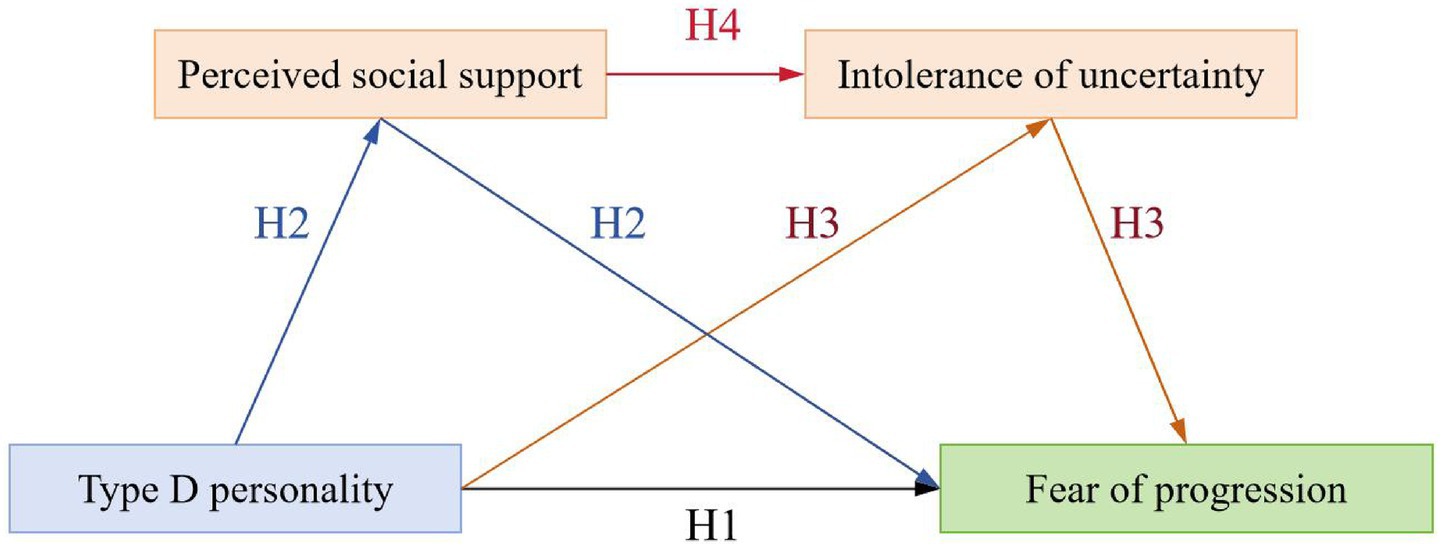
Objective: Fear of progression (FoP) significantly impacts multidimensional health outcomes in stroke patients. Although Type D personality predicts FoP, mechanisms underlying the association between Type D personality and FoP remain poorly understood. This study aimed to investigate the impact of Type D personality on FoP in first-ever stroke patients and the serial mediation role of perceived social support (PSS) and intolerance of uncertainty (IU).
Methods: This cross-sectional study employed convenience sampling to recruit 300 patients with first-ever stroke (228 males and 72 females; mean age 59.52 ± 12.72 years) from two tertiary hospitals in Yinchuan, China. Participants completed the following scales: the General Information Questionnaire, the 14-item Type D scale, the Multidimensional Scale of Perceived Social Support, the Intolerance of Uncertainty Scale-12, and the Fear of Progression Questionnaire-Short Form. SPSS 24.0 was used for Harman’s single-factor test, descriptive statistics, Pearson correlation analysis, and regression analysis, with serial mediation role examined using the PROCESS macro v3.5.
Results: Our results showed that: (1) the direct effect of Type D personality on FoP was significant. (2) PSS did not independently mediate the Type D personality-FoP relationship. (3) IU significantly mediated the Type D personality-FoP relationship. (4) PSS and IU demonstrated the significant serial mediation role between Type D personality and FoP.
Conclusion: Type D personality exerted a direct effect on FoP among first-ever stroke patients. The serial mediation model demonstrated that enhancing PSS could reduce IU, thereby alleviating FoP. Interventions targeting PSS enhancement and IU reduction constitute a promising approach to mitigate FoP in these patients, despite Type D traits’ inherent stability.
1 Introduction
According to the Global Burden of Disease Study 2024, stroke ranks as the third leading cause of global mortality (GBD 2021 Stroke Risk Factor Collaborators, 2024), and is a major contributor to death and disability among adults in China (Liu et al., 2025). Clinically, stroke manifests with complex and diverse symptoms, necessitates prolonged recovery, and exhibits high recurrence rates. Notably, 70–80% of survivors experience residual disabilities post-treatment (Yang et al., 2025). These enduring physical and psychological burdens, compounded by limited patient understanding and uncertainty regarding treatment and prognosis, foster a prevailing fear of progression among stroke patients (Yang et al., 2025).
Fear of Progression (FoP) refers to a patient’s fear of the biopsychosocial consequences associated with disease progression or the fear of disease recurrence (Dankert et al., 2003). As one of the most prevalent unmet psychological needs in stroke patients (Townend et al., 2006), FoP is frequently conceptualized as a ‘Damoclean threat’—an evocative metaphor emphasizing the constant vigilance and apprehension maintained by patients with stroke toward potential disease progression (Sharpe et al., 2023). While moderate FoP may serve as an adaptive response that promotes health behaviors (Ocalewski et al., 2021), excessive FoP can trigger pathological health anxiety, impair quality of life, and potentially elevate cerebrovascular event risk (Faezi et al., 2017; Simonelli et al., 2017). Therefore, FoP should be considered in the management of stroke patients.
1.1 Type D personality and FoP
Type D personality is a stable trait characterized by persistent negative affectivity and social inhibition (Denollet, 2005). Patients exhibiting this trait typically display pessimistic attitudes toward clinical prognosis and express frequent concerns about disease progression (Mols et al., 2012). Yin et al. (2023) reported a high prevalence of Type D personality among patients with stroke and identified it as a robust predictor of post-stroke depression. Furthermore, evidence from patients with lung cancer revealed that Type D personality significantly predicts elevated FoP (Lv, 2017). Similarly, a study of patients undergoing valvular heart surgery confirmed Type D personality as a risk factor for severe FoP (Wu et al., 2025). However, the relationship between Type D personality and FoP in first-ever stroke patients remains underexplored. Therefore, we hypothesize:
H1: Type D personality in patients with first-ever stroke positively predicts FoP.
1.2 The mediating role of perceived social support (PSS) in the relationship between Type D personality and FoP
Perceived social support (PSS) refers to an individual’s subjective appraisal of the availability and adequacy of resources provided by their social networks (Paykani et al., 2020). PSS represents a critical determinant for maintaining mental health (Tonsing et al., 2012). Substantial evidence indicates that Type D personality is associated with impaired PSS, as demonstrated by significantly lower PSS levels in Type D compared to non-Type D patients with coronary artery disease (Ginting et al., 2016). Furthermore, O'Riordan et al. (2020) identified reduced PSS as a mediator between a Type D personality and cardiovascular reactivity to acute stress. Crucially, lower PSS predicts heightened FoP in diverse clinical populations. Guan et al. (2024) documented a negative correlation between PSS and FoP in patients with stroke, while a study on patients with primary brain tumors confirmed that lower PSS significantly predicts increased FoP (Du et al., 2024). These findings suggest that PSS may significantly mediate the relationship between Type D personality and FoP. Consequently, we hypothesize:
H2: PSS mediates the relationship between Type D personality and FoP in first-ever stroke patients.
1.3 The mediating role of intolerance of uncertainty (IU) in the relationship between Type D personality and FoP
Intolerance of uncertainty (IU) is the tendency to react negatively to uncertain situations (Näsling et al., 2024). Individuals with high IU tend to catastrophically interpret uncertain future events, viewing uncertainty as highly threatening and unacceptable (Malivoire et al., 2019). Multiple studies consistently demonstrate that personality traits significantly predict IU levels (Bongelli et al., 2021; Zhang et al., 2022; Kumar et al., 2025). Given that stroke progression and outcomes are inherently uncertain, affected patients inevitably face substantial disease-related uncertainty (Salter et al., 2008). This challenge is particularly pronounced among individuals with a Type D personality, who exhibit markedly diminished tolerance for ambiguity (Grynberg et al., 2012). Critically, heightened IU predicts increased FoP in clinical populations. Curran et al. (2020) demonstrated the predictive role of IU for FoP in patients with cancer, while Shen et al. (2024) established a strong positive correlation wherein lower IU levels correspond to reduced FoP. These findings imply that the relationship between Type D personality and FoP may be significantly mediated by IU. Therefore, we hypothesize:
H3: IU mediates the relationship between Type D personality and FoP in first-ever stroke patients.
1.4 The serial mediation role of PSS and IU
According to the Stress and Coping Theory (Folkman et al., 1986), individuals’ coping resources can affect their coping responses. In response to a stressor, the availability of coping resources can affect stress appraisal, coping responses, and health outcomes. In this study, stroke is considered a significant health-related stressor, while PSS constitutes a critical coping resource. Patients with Type D personality tend to perceive insufficient social support, and this deficit in coping resources exacerbates their IU, thereby promoting maladaptive coping responses—such as FoP in first-ever stroke patients. Previous studies have also confirmed that PSS has a negative impact on IU. For instance, a survey by Ne'eman-Haviv et al. (2025) revealed that PSS was negatively associated with IU. This suggests that PSS and IU may serve as serial mediators linking Type D personality to FoP in first-ever stroke patients. Based on this, we propose the fourth hypothesis:
H4: Type D personality influences FoP through the serial mediation role of PSS and IU among first-ever stroke patients.
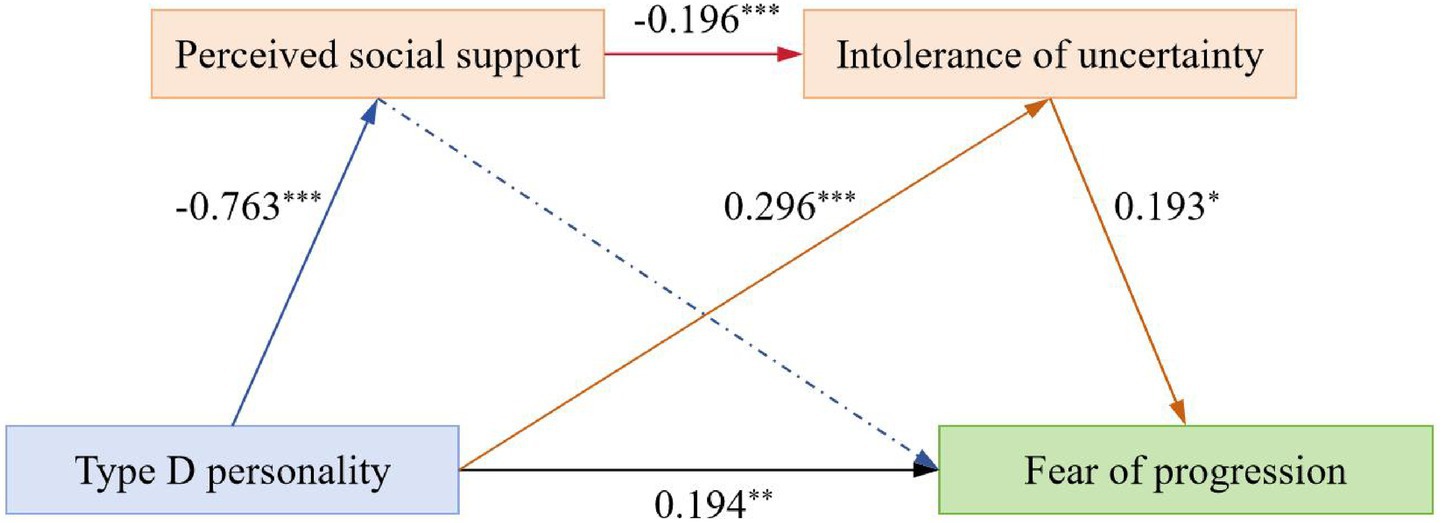
Consequently, this study aimed to investigate the impact of Type D personality on FoP among first-ever stroke patients and the serial mediation role of PSS and IU in this relationship. As illustrated in Figure 1, this study proposed a hypothesized model to examine the underlying mechanisms through which Type D personality influences FoP.
2 Materials and methods
2.1 Ethics statement
The research protocol involving human participants was approved by the Institutional Review Board of Ningxia Medical University (Approval No. 2023-044). All patients participated voluntarily, and informed consent was obtained after explanation of the study purpose. We adhered to the Declaration of Helsinki and ethical principles throughout the study.
2.2 Participants
This cross-sectional study recruited participants from neurology inpatient departments at two tertiary hospitals in Yinchuan City, Ningxia, China, between May and September 2023. The inclusion criteria comprised the following: (a) adult patients who were stroke survivors meeting cerebrovascular disease diagnostic criteria, with ischemic stroke or hemorrhagic stroke confirmed by neuroimaging modalities (computed tomography [CT] or magnetic resonance imaging [MRI]); (b) aged ≥18 years; (c) had an illness duration of ≤2 weeks from onset; (d) experienced a first-ever stroke; and (e) provided written informed consent. The exclusion criteria encompassed patients who: (a) exhibited severe linguistic barriers or cognitive impairments, precluding effective communication and scale assessment; (b) had documented psychiatric disorders; and (c) presented with other severe systemic diseases, such as heart failure and malignant tumors.
2.3 Sample size and data collection
Based on cross-sectional study sample size requirements and Kendall’s criterion (Guan et al., 2024), the minimum sample size should be 5–10 times the number of study variables. With 20 variables included in this research, 100–200 participants were required. Accounting for potential invalid responses (estimated at 10–20% of questionnaires), we recruited 300 participants for this investigation. Post hoc statistical power analysis was conducted using G*Power 3.1™. The analysis demonstrated a test power of 99.9%, confirming that the sample size of 300 provides robust capability to detect the hypothesized effects (Cohen, 1992).
Researchers received standardized training in data collection methods prior to the formal investigation. Data were collected via face-to-face interviews. First, the research team explained the study’s purpose to eligible participants; those willing to participate provided written informed consent. During data collection, researchers delivered standardized instructions for the assessment tools, after which participants completed questionnaires independently. Researchers remained available to clarify questions or address participant concerns. For individuals unable to self-complete questionnaires, researchers administered items orally and recorded responses. The average completion time was approximately 20–30 min per questionnaire. All questionnaires underwent immediate quality checks to identify and rectify missing data.
2.4 Measures
2.4.1 General information
We collected socio-demographic and clinical data using a General Information Questionnaire. These included variables such as gender, age group, education level, hospitalization costs, urban–rural distribution, employment status, marital status, Parental status, family financial situation, family history of stroke, types of stroke, complications, functional impairment, the number of other chronic diseases, daily living activities [evaluated using the Barthel Index (Oliveira et al., 2023)], and patients’ understanding of stroke-related knowledge.
2.4.2 Type D personality
The 14-item Type D scale (DS 14), developed by Denollet (2005), was used to detect an individual’s Type D personality traits. The scale contains 14 items and two subscales; seven items measure the Negative Affectivity dimension (NA, covering dysphoria, worry, and irritability), while seven items evaluate the Social Inhibition dimension (SI, covering discomfort in social interactions, reticence, and lack of social poise). The scale was scored on a 5-point Likert scale varying from 0 = “False” to 4 = “True.” Scores on both NA and SI range from 0 to 28. An individual was categorized as having a Type D personality if the total score was 10 or higher for the NA and SI. However, a previous study suggested that a Type D personality may be more accurately represented as a dimensional rather than a categorical construct (Ferguson et al., 2009). The Cronbach’s α coefficient of the DS 14 in this study was 0.913.
2.4.3 Perceived social support (PSS)
The Multidimensional Scale of Perceived Social Support (MSPSS), developed by Zimet et al. (1990), was used to measure PSS. The scale comprises 12 items across three subscales: Family Support, Friend Support, and Other Supports, which, respectively, reflect an individual’s perception of support from family members, friends, and other sources (e.g., leaders, colleagues, and relatives). Responses are rated on a seven-point Likert scale (1 = “strongly disagree” to 7 = “strongly agree”), with total scores ranging from 12 to 84. Higher scores indicate greater PSS. The Cronbach’s α coefficient of the MSPSS in this study was 0.927.
2.4.4 Intolerance of uncertainty (IU)
The Intolerance of Uncertainty Scale-12 (IUS-12) was used to assess each participant’s tolerance for the occurrence of future uncertainties. This scale was developed by Carleton et al. (2007). The scale includes 12 items and two subscales, namely, Prospective Anxiety (involves fear and anxiety based on future events) and Inhibitory Anxiety (describes uncertainty inhibiting action or experience). The IUS-12 uses a 5-point Likert scale without reverse scoring, meaning higher scores indicate greater IU. In this study, the Cronbach’s α coefficient for the IUS-12 was 0.881.
2.4.5 Fear of progression (FoP)
The Fear of Progression-Questionnaire-Short Form (FoP-Q-SF), developed by Mehnert et al. (2006), was used to measure participant’s FoP. The scale comprises two subscales: Physical Health (referring to patients’ concerns about their own physical health status, including fears of symptom worsening, functional decline, and treatment uncertainty) and Social-Family (reflecting patients’ fears about the disease’s impact on their social functions and family roles, covering concerns about social interaction difficulties, family responsibility burdens, work capability impairment, and relationship strain). The scale includes 12 items rated on a 5-level Likert scale, with total scores ranging from 12 to 60, with higher scores indicating higher levels of FoP. The Cronbach’s α coefficient of the FoP-Q-SF in this study was 0.848.
2.5 Statistical analyses
We analyzed data using SPSS 24.0. To enhance data reporting transparency and evaluate the appropriateness of statistical analyses, we examined the distributional characteristics of all continuous variables, including measures of central tendency, dispersion, and distributional shape (i.e., skewness and kurtosis). The results showed that skewness ranged from −0.404 to 0.698 and kurtosis from −0.454 to 0.105, indicating approximate normality (|values| < 1) (Mishra et al., 2019). This finding supported the application of parametric statistical methods (Vickers, 2005). Continuous variables were presented as mean ± standard deviation (M ± SD), while categorical variables were described as frequencies. Pearson’s bivariate correlation analysis was employed to explore the associations among variables, and multicollinearity among variables was assessed using the variance inflation factor (VIF), with a VIF < 5 indicating no significant collinearity issues (Kim, 2019). To test the serial mediation effect, Model 6 of the PROCESS 3.5 macro,1 developed by Hayes, was utilized. Statistical significance of indirect effects was tested via bias-corrected bootstrap confidence intervals (CI) with 5,000 resamples. Effects were considered significant if the 95% CI did not include zero. In all analyses, a 2-tailed p < 0.05 was considered statistically significant.
3 Results
3.1 Common method bias test
The results of the Harman’s single-factor test revealed that there were nine factors with eigenvalues exceeding 1, and the explanatory power of the first factor was 33.74%, which was below the critical threshold of 40%. Therefore, the data used in this study do not exhibit any discernible common method bias.
3.2 Statistical description and influencing factors of FoP
The socio-demographic and clinical characteristics of the 300 participants included in the study are presented in Tables 1, 2. Overall, 228 male (76.0%) and 72 female (24.0%) patients were included in the sample. The participants’ mean age was 59.52 ± 12.72 years, with 148 participants (49.3%) aged ≥ 60 years.
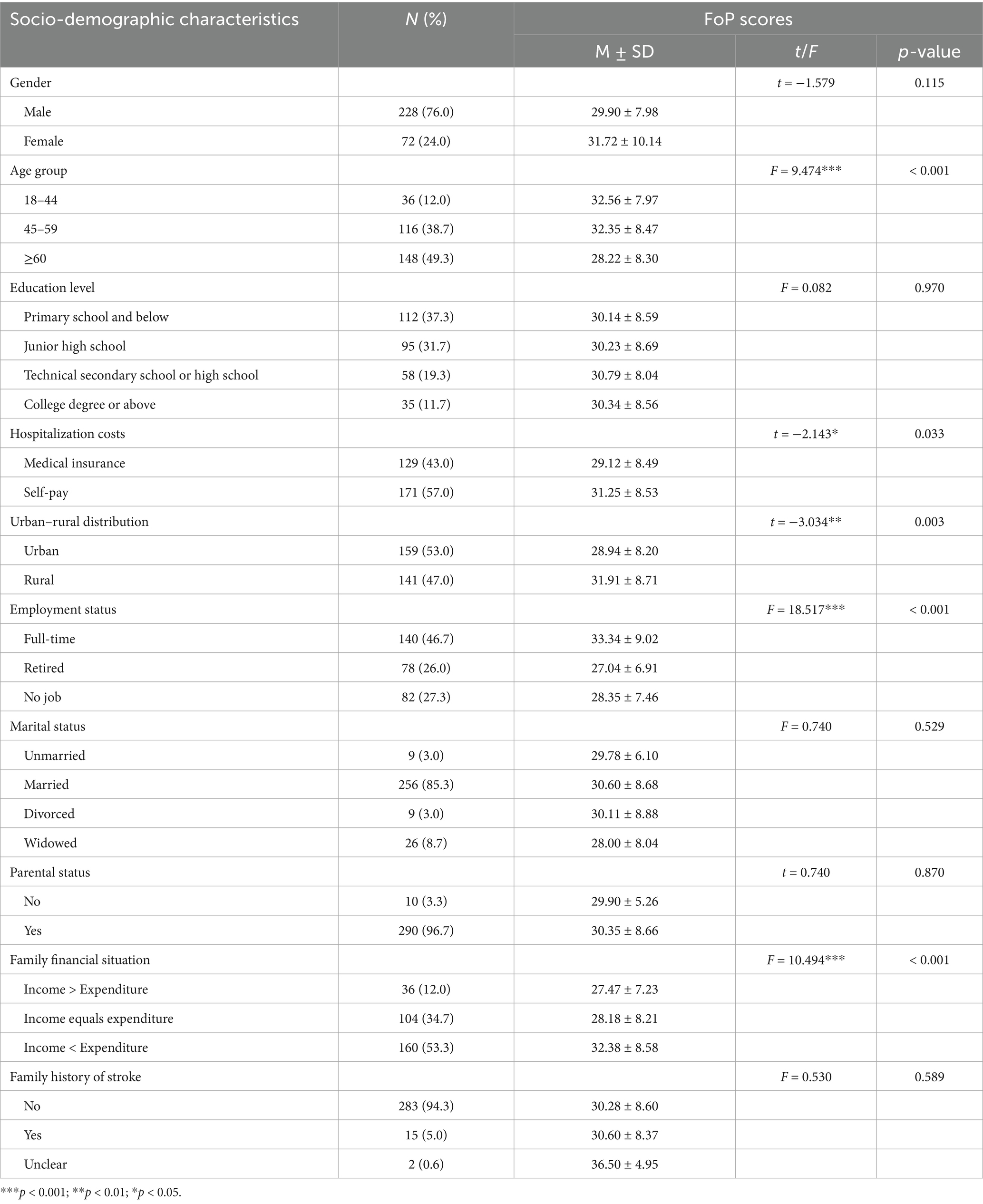
Table 1. Comparison of FoP scores in participants with different socio-demographic characteristics (N = 300).
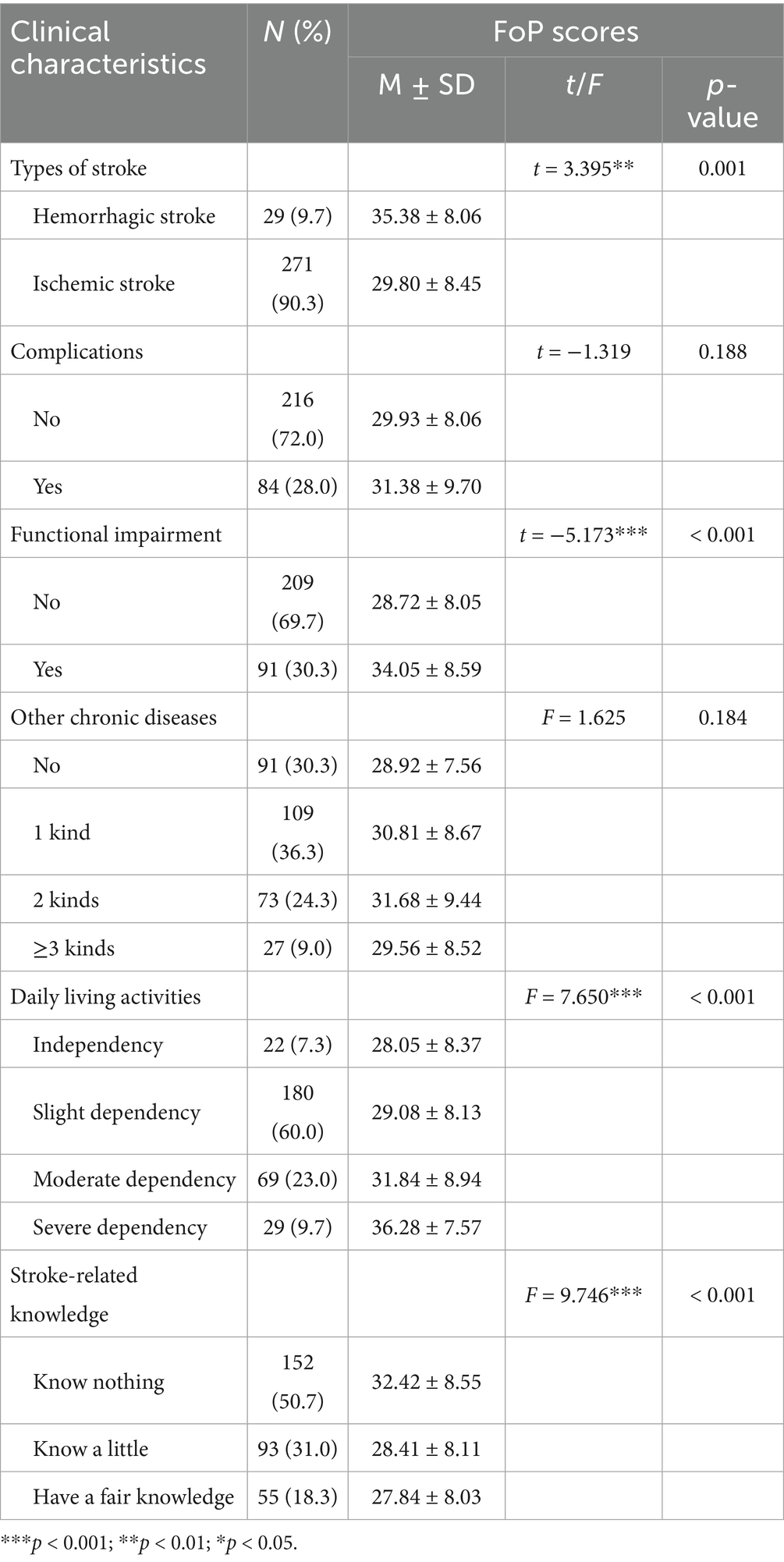
Table 2. Comparison of FoP scores in participants with different clinical characteristics (N = 300).
Univariable analyses indicated that FoP scores significantly differed across nine variables: age group, hospitalization costs, urban–rural residence, employment status, family financial status, stroke type, functional impairment, activities of daily living, and stroke-related knowledge (p < 0.05 for all; see Tables 1, 2).
3.3 Statistical description and correlation analysis
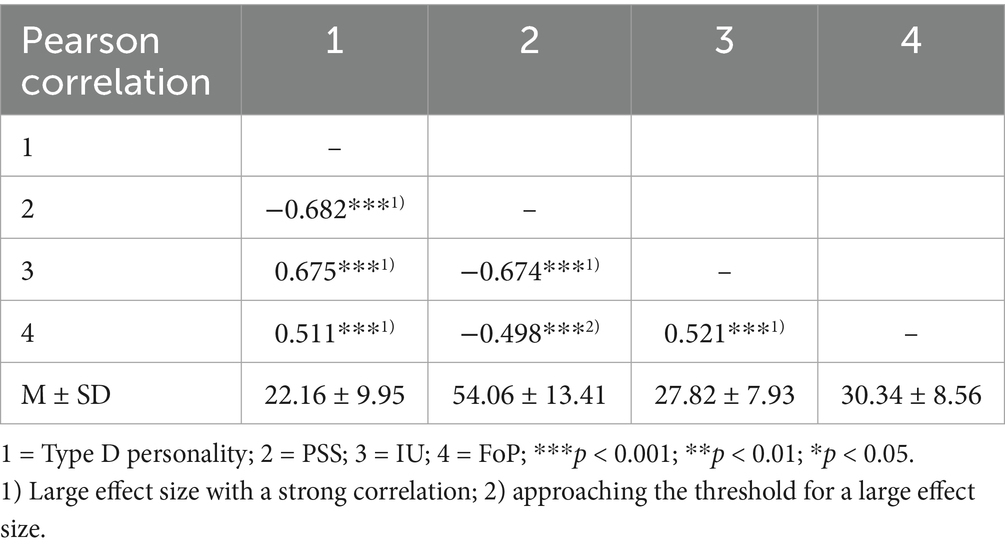
The total FoP score in patients with first-ever stroke ranged from 17 to 55 (mean scores: 30.34 ± 8.56). The mean scores of the other variables were as follows: Type D personality (22.16 ± 9.95), PSS (54.06 ± 13.41), and IU (27.82 ± 7.93), as shown in Table 3.
The correlations between variables were investigated using Pearson’s correlation analysis. The Pearson correlation coefficient (r) ranges from −1 to +1. Specifically, an absolute value of the Pearson correlation coefficient (|r|) of 0.1 reflects a small effect size with a weak correlation, |r| = 0.3 reflects a medium effect size with a moderate correlation, and |r| = 0.5 reflects a large effect size with a strong correlation (Cohen, 1992). Our results showed that Type D personality was positively correlated with FoP (r = 0.511, p < 0.001) and IU (r = 0.675, p < 0.001), and negatively correlated with PSS (r = −0.682, p < 0.001). Furthermore, PSS was negatively correlated with IU (r = −0.674, p < 0.001) and FoP (r = −0.498, p < 0.001). IU was positively correlated with FoP (r = 0.521, p < 0.001).
3.4 Serial mediation model testing
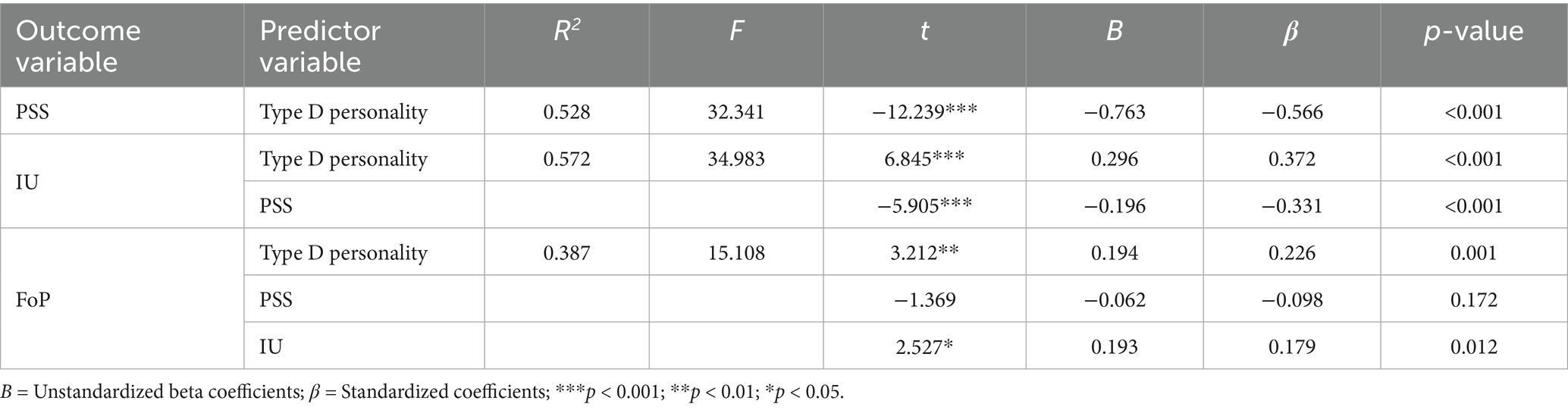
To test the mediating effects of PSS and IU between Type D personality and FoP, we used Model 6 from the PROCESS macro v3.5 developed by Hayes. Several socio-demographic and clinical characteristics significantly associated with FoP in univariate analysis were entered as control variables in the model.
As presented in Table 4, regression analysis showed that Type D personality negatively predicted PSS (B = −0.763, p < 0.001) and positively predicted IU (B = 0.296, p < 0.001), while PSS negatively predicted IU (B = −0.196, p < 0.001). In the full model accounting for all variables, Type D personality maintained a significant direct effect on FoP (B = 0.194, p = 0.001), and IU positively predicted FoP (B = 0.193, p = 0.012); however, PSS did not significantly predict FoP (B = −0.062, p = 0.172). Furthermore, all variables within the regression model had VIFs ranging from 1.103 to 2.376, which suggested the absence of substantial multicollinearity issues.
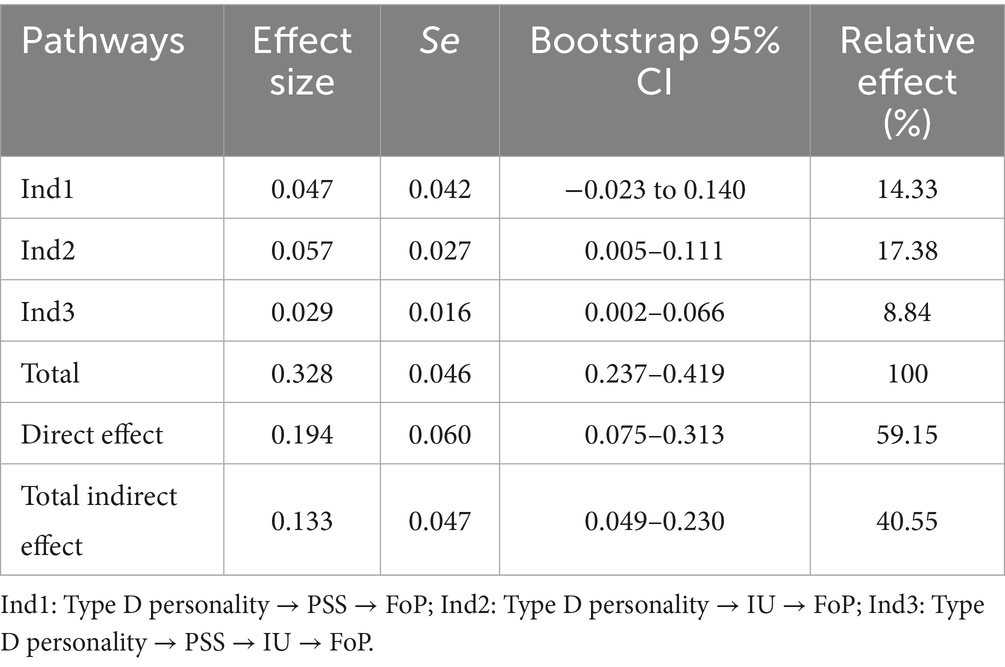
Further mediation analyses are presented in Table 5 and Figure 2. The direct effect of Type D personality on FoP was significant (95% CI [0.072, 0.316]); PSS did not independently mediate the relationship between Type D personality and FoP (95% CI [−0.023, 0.140]); however, IU significantly mediated the Type D personality-FoP relationship (95% CI [0.005, 0.111]). Furthermore, PSS and IU had a significant serial mediation role in the relationship between Type D personality and FoP (95% CI [0.002, 0.066]), accounting for 8.84% of the total effect.
4 Discussion
4.1 FoP in first-ever stroke patients
In this study, the mean score of FoP among first-ever stroke patients (30.34 ± 8.56) was lower than that reported by Guan et al. (2024). This divergence may be attributed to differences in stroke subtype composition. In this study, 90.3% of the participants had ischemic stroke while 9.7% had hemorrhagic stroke, whereas patients with hemorrhagic stroke comprised 35.4% of Guan et al. (2024)’s sample. As hemorrhagic stroke is clinically associated with higher acute mortality (Lim et al., 2024), patients with this subtype typically demonstrate heightened FoP, potentially explaining the elevated scores in Guan et al. (2024)’s study. Notably, the scores of patients with first-ever stroke on the two subscales—Physical Health and Social-Family—were essentially equivalent, demonstrating that the occurrence and progression of stroke impose comparably significant impacts on patients’ physical well-being and their family and social domains. Therefore, neurologists and nurses should implement routine FoP screening and deliver targeted interventions—including disease education and coping skills training—to mitigate FoP in high-risk first-ever stroke patients.
4.2 Type D personality in first-ever stroke patients
In this study, the prevalence of Type D personality in patients with first-ever stroke was 37.3%. This substantially exceeded the prevalence rate of 22.2% reported in the general population (Beutel et al., 2012). The mean Type D personality score in this study was 20.22 ± 8.69, which is similar to the score reported by Yin et al. (2023). Yao et al. (2022) conducted a study to examine the association between Type D personality and ischemic cerebrovascular disease; the results showed that Type D individuals had a higher frequency of acute ischemic stroke and white matter hyperintensity, which further elucidated the mechanism of Type D personality predisposing to stroke from the perspective of imaging. Our results also confirmed the high incidence of Type D personality in patients with stroke. Consequently, we propose that the DS-14 is a brief, well-validated measure of Type D personality, which can be incorporated into clinical research and practice to facilitate the identification of high-risk stroke patients by neurologists and nurses. For patients at high risk of Type D personality, interventions targeting enhanced social support and cognitive behavioral therapy should be considered (Purdy, 2013; Su and He, 2019).
4.3 Type D personality positively predicted FoP
Consistent with our first hypothesis, the results of this study indicated that Type D personality positively predicted FoP in patients with first-ever stroke. This aligns with the findings of previous research (Wu et al., 2025). Patients with stroke exhibiting Type D personality are more prone to being sensitive to the pain and burden of the disease. Heightened sensitivity increases their awareness of the disease threat, fostering excessive pessimism regarding prognosis. This pessimism, in turn, generates substantial concerns about treatment efficacy, financial issues, and future life. Moreover, due to deficits in emotional regulation skills and a lack of social support, these patients cannot effectively alleviate their negative emotions. As a result, they persist in a state of chronic stress characterized by FoP.
4.4 The serial mediation role of PSS and IU
The serial mediation model demonstrated a non-significant independent mediating effect of PSS between Type D personality and FoP, contradicting Hypothesis 2. However, IU maintained a significant independent mediating effect (Hypothesis 3 was supported). This demonstrates that the role of IU takes precedence over PSS’ mediating role when both are modeled concurrently, establishing IU as the primary mediator linking Type D personality to FoP.
Our study further confirmed the serial mediating role of PSS and IU in the pathway linking Type D personality to FoP among first-ever stroke patients, thus supporting Hypothesis 4. This finding aligns with the theoretical propositions of the Stress and Coping Theory, demonstrating a sequential pathway from the stressor (stroke event) through compromised coping resources (lower PSS resulting from type D personality) to threat appraisal (IU), culminating in the stress response (FoP). Specifically, Type D personality impairs patients’ capacity to proactively leverage social support. Given stroke severity and interindividual variability, even experienced clinicians cannot reliably predict disease progression. This prognostic uncertainty poses a significant challenge for stroke patients. However, diminished PSS predicts inadequate resources for coping with uncertain events in patients with stroke (Yu et al., 2022) and reinforces a persistent negative belief that disease-related uncertainty is intolerable and unacceptable (Malivoire et al., 2019), thereby exacerbating stroke survivors’ fears of disease deterioration or recurrence (Shen et al., 2024).
Our findings indicate that neurologists and nurses could mitigate FoP among patients with type D personality through enhancing of PSS or improvement of patients’ tolerance of uncertainty. Empirical studies demonstrate that nurse-led peer support interventions effectively enhance PSS in stroke survivors (Wan et al., 2024). Tai Chi and meaningful life interventions have also been shown to significantly boost PSS levels (Koren et al., 2021; Liu et al., 2024). Additionally, cognitive behavioral therapy can reduce the IU level by regulating disease perception and cognitive-emotional coping styles (Talkovsky and Norton, 2016).
5 Strengths and limitations
Our research confirms that PSS and IU exert a serial mediating effect on the relationship between Type D personality and FoP. This finding provides a theoretical basis and empirical support for developing interventions to mitigate FoP in patients with stroke, thereby extending previous research in this field. Despite this study’s contributions, certain limitations must be acknowledged. The use of a cross-sectional design constrains causal inference regarding the relationships among the variables. Moreover, convenience sampling was employed from two hospitals, with all participants being stroke survivors from the same region in China. This sampling method inevitably introduced selection bias, limiting the generalizability of this study’s findings. Finally, the results remain unvalidated in other stroke populations, particularly among recurrent stroke survivors.
Considering these limitations, future research should focus on: (1) Longitudinal studies to establish causal relationships or design intervention trials targeting enhanced PSS. (2) A multicenter investigation should be conducted, enrolling patients with stroke with diverse characteristics (e.g., recurrent stroke, comorbid dementia, or depression), to validate the model’s effectiveness across heterogeneous populations.
6 Conclusion
Type D personality significantly predicts FoP in first-ever stroke patients. Although such traits are generally stable and intervention—resistant, our serial mediation model demonstrates that while PSS alone does not mediate the Type D—FoP relationship, the PSS—IU serial pathway is significant. This implies enhancing PSS may reduce FoP by alleviating IU. These findings indicate that interventions targeting enhanced PSS and reduced IU represent a promising approach to alleviate FoP in these patients, despite the inherent stability of Type D personality traits.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the research protocol involving human participants was approved by the Institutional Review Board of Ningxia Medical University (Approval No. 2023-044). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XY: Formal analysis, Data curation, Writing – review & editing, Investigation, Writing – original draft. LW: Investigation, Writing – review & editing. XL: Funding acquisition, Supervision, Writing – review & editing. MC: Writing – review & editing, Formal analysis, Investigation. YZ: Formal analysis, Investigation, Writing – review & editing. SM: Formal analysis, Investigation, Writing – review & editing. JY: Formal analysis, Investigation, Writing – review & editing, Visualization. HW: Investigation, Writing – review & editing, Formal analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors declare that this study received financial support from the First-class Discipline Development Program (2024) of the School of Nursing, Ningxia Medical University (grant number: NYHLB202401), and the 2024 Newly Recruited Master’s Degree Training Program at the General Hospital of Ningxia Medical University.
Acknowledgments
We sincerely appreciate the considerable patience of all respondents during questionnaire completion and gratefully acknowledge all individuals who supported this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Beutel, M. E., Wiltink, J., Till, Y., Wild, P. S., Münzel, T., Ojeda, F. M., et al. (2012). Type D personality as a cardiovascular risk marker in the general population: results from the Gutenberg health study. Psychother. Psychosom. 81, 108–117. doi: 10.1159/000331776
Bongelli, R., Canestrari, C., Fermani, A., Muzi, M., Riccioni, I., Bertolazzi, A., et al. (2021). Associations between personality traits, intolerance of uncertainty, coping strategies, and stress in Italian frontline and non-frontline HCWs during the COVID-19 pandemic-a multi-group path-analysis. Healthcare (Basel) 9:1086. doi: 10.3390/healthcare9081086
Carleton, R. N., Norton, M. A., and Asmundson, G. J. (2007). Fearing the unknown: a shortversion of the intolerance of uncertainty scale. J. Anxiety Disord. 21, 105–117. doi: 10.1016/j.janxdis.2006.03.014
Curran, L., Sharpe, L., MacCann, C., and Butow, P. (2020). Testing a model of fear of cancer recurrence or progression: the central role of intrusions, death anxiety and threat appraisal. J. Behav. Med. 43, 225–236. doi: 10.1007/s10865-019-00129-x
Dankert, A., Duran, G., Engst-Hastreiter, U., Keller, M., Waadt, S., Henrich, G., et al. (2003). Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis. Rehabilitation (Stuttg) 42, 155–163. doi: 10.1055/s-2003-40094
Denollet, J. (2005). DS14: standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom. Med. 67, 89–97. doi: 10.1097/01.psy.0000149256.81953.49
Du, L., Cai, J., Yu, J., Chen, X., Yang, X., Xu, X., et al. (2024). Relations between posttraumatic growth and fear of progression among young and middle-aged primary brain tumor patients: the parallel mediating role of perceived social support and illness uncertainty. World Neurosurg. 184, e794–e802. doi: 10.1016/j.wneu.2024.02.048
Faezi, S. T., Paragomi, P., Shahali, A., Akhlaghkhah, M., Akbarian, M., Akhlaghi, M., et al. (2017). Prevalence and severity of depression and anxiety in patients with systemic sclerosis: an epidemiologic survey and investigation of clinical correlates. J. Clin. Rheumatol. 23, 80–86. doi: 10.1097/rhu.0000000000000428
Ferguson, E., Williams, L., O'Connor, R. C., Howard, S., Hughes, B. M., Johnston, D. W., et al. (2009). A taxometric analysis of type-D personality. Psychosom. Med. 71, 981–986. doi: 10.1097/PSY.0b013e3181bd888b
Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., and Gruen, R. J. (1986). Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. J. Pers. Soc. Psychol. 50, 992–1003. doi: 10.1037//0022-3514.50.5.992
GBD 2021 Stroke Risk Factor Collaborators (2024). Global, regional, and national burden of stroke and its risk factors, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet Neurol. 23, 973–1003. doi: 10.1016/s1474-4422(24)00369-7
Ginting, H., van de Ven, M., Becker, E. S., and Näring, G. (2016). Type D personality is associated with health behaviors and perceived social support in individuals with coronary heart disease. J. Health Psychol. 21, 727–737. doi: 10.1177/1359105314536750
Grynberg, D., Gidron, Y., Denollet, J., and Luminet, O. (2012). Evidence for a cognitive bias of interpretation toward threat in individuals with a type D personality. J. Behav. Med. 35, 95–102. doi: 10.1007/s10865-011-9351-7
Guan, X., Zhu, Q., and Qian, H. (2024). Relationship between post-traumatic stress disorder and fear of progression in stroke patients: the mediating role of perceived social support and coping styles. Top. Stroke Rehabil. 32, 1–9. doi: 10.1080/10749357.2024.2417646
Kim, J. H. (2019). Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 72, 558–569. doi: 10.4097/kja.19087
Koren, Y., Leveille, S., and You, T. (2021). Tai chi interventions promoting social support and interaction among older adults: a systematic review. Res. Gerontol. Nurs. 14, 126–137. doi: 10.3928/19404921-20210325-02
Kumar, S., Davidson, C. A., Saini, R., and Jain, R. (2025). The role of intolerance of uncertainty and religiousness in schizotypal personality and life satisfaction: a cross-sectional study. J. Psychol. 159, 92–110. doi: 10.1080/00223980.2024.2372578
Lim, M. J. R., Zheng, H., Zhang, Z., Sia, C. H., Tan, B. Y., Hock Ong, M. E., et al. (2024). Trends in hemorrhagic stroke incidence and mortality in a National Stroke Registry of a multi-ethnic Asian population. Eur. Stroke J. 9, 189–199. doi: 10.1177/23969873231202392
Liu, S., Cai, Y., Yao, S., Chai, J., Jia, Y., Ge, H., et al. (2024). Perceived social support mediates cancer and living meaningfully intervention effects on quality of life after breast cancer surgery. Future Oncol. 20, 1675–1687. doi: 10.1080/14796694.2024.2370237
Liu, R., Liu, J., Song, J., Peng, Y., Jin, G., and Li, J. (2025). Mediating effect of social support in the relationship of symptom burden and fear of disease progression in stroke patients. J. Stroke Cerebrovasc. Dis. 34:108215. doi: 10.1016/j.jstrokecerebrovasdis.2024.108215
Lv, X. (2017). Construction of a predictive model for supportive care needs of lung cancer patients. Hefei: Anhui Medical University.
Malivoire, B. L., Marcos, M., Pawluk, E. J., Tallon, K., Kusec, A., and Koerner, N. (2019). Look before you leap: the role of negative urgency in appraisals of ambiguous and unambiguous scenarios in individuals high in generalized anxiety disorder symptoms. Cogn. Behav. Ther. 48, 217–240. doi: 10.1080/16506073.2018.1508247
Mehnert, A., Herschbach, P., Berg, P., Henrich, G., and Koch, U. (2006). Fear of progression in breast cancer patients-validation of the short form of the fear of progression questionnaire (FoP-Q-SF). Z. Psychosom. Med. Psychother. 52, 274–288. doi: 10.13109/zptm.2006.52.3.274
Mishra, P., Pandey, C. M., Singh, U., Gupta, A., Sahu, C., and Keshri, A. (2019). Descript-ive statistics and normality tests for statistical data. Ann. Card. Anaesth. 22, 67–72. doi: 10.4103/aca.ACA_157_18
Mols, F., Denollet, J., Kaptein, A. A., Reemst, P. H., and Thong, M. S. (2012). The association between type D personality and illness perceptions in colorectal cancer survivors: a study from the population-based PROFILES registry. J. Psychosom. Res. 73, 232–239. doi: 10.1016/j.jpsychores.2012.07.004
Näsling, J., Åström, E., Jacobsson, L., and Ljungberg, J. K. (2024). Effect of psychotherapy on intolerance of uncertainty: a systematic review and meta-analysis. Clin. Psychol. Psychother. 31:e3026. doi: 10.1002/cpp.3026
Ne'eman-Haviv, V., Dolberg, P., Lev, S., and Kagan, M. (2025). Perceived social support, intolerance of uncertainty, and war-related stress: unraveling the nexus with treatment burden in adult-child caregivers during war. J. Gerontol. Soc. Work. 68, 467–481. doi: 10.1080/01634372.2024.2442013
Ocalewski, J., Michalska, P., Izdebski, P., Jankowski, M., and Zegarski, W. (2021). Fear of cancer progression and health behaviors in patients with colorectal cancer. Am. J. Health Behav. 45, 138–151. doi: 10.5993/ajhb.45.1.11
Oliveira, L. C., Ponciano, A., Tuozzo, C., Viswanathan, A., Rost, N. S., and Etherton, M. R. (2023). Poststroke disability: association between sex and patient-reported outcomes. Stroke 54, 345–353. doi: 10.1161/strokeaha.122.041502
O'Riordan, A., Howard, S., Brown, E., and Gallagher, S. (2020). Type D personality and cardiovascular reactivity to acute stress: the mediating effects of social support and negative social relationships. Psychophysiology 57:e13660. doi: 10.1111/psyp.13660
Paykani, T., Zimet, G. D., Esmaeili, R., Khajedaluee, A. R., and Khajedaluee, M. (2020). Perceived social support and compliance with stay-at-home orders during the COVID-19 outbreak: evidence from Iran. BMC Public Health 20:1650. doi: 10.1186/s12889-020-09759-2
Purdy, J. (2013). Chronic physical illness: a psychophysiological approach for chronic physical illness. Yale J. Biol. Med. 86, 15–28.
Salter, K., Hellings, C., Foley, N., and Teasell, R. (2008). The experience of living with stroke: a qualitative meta-synthesis. J. Rehabil. Med. 40, 595–602. doi: 10.2340/16501977-0238
Sharpe, L., Michalowski, M., Richmond, B., Menzies, R. E., and Shaw, J. (2023). Fear of progression in chronic illnesses other than cancer: a systematic review and meta-analysis of a transdiagnostic construct. Health Psychol. Rev. 17, 301–320. doi: 10.1080/17437199.2022.2039744
Shen, Z., Zhang, L., Shi, S., Ruan, C., Dan, L., and Li, C. (2024). The relationship between uncertainty and fear of disease progression among newly diagnosed cancer patients: the mediating role of intolerance of uncertainty. BMC Psychiatry 24:756. doi: 10.1186/s12888-024-06201-4
Simonelli, L. E., Siegel, S. D., and Duffy, N. M. (2017). Fear of cancer recurrence: a theoretical review and its relevance for clinical presentation and management. Psychooncology 26, 1444–1454. doi: 10.1002/pon.4168
Su, S. F., and He, C. P. (2019). Type D personality, social support, and depression among ethnic Chinese coronary artery disease patients undergoing a percutaneous coronary intervention: an exploratory study. Psychol. Rep. 122, 988–1006. doi: 10.1177/0033294118780428
Talkovsky, A. M., and Norton, P. J. (2016). Intolerance of uncertainty and transdiagnosticgroup cognitive behavioral therapy for anxiety. J. Anxiety Disord. 41, 108–114. doi: 10.1016/j.janxdis.2016.05.002
Tonsing, K., Zimet, G. D., and Tse, S. (2012). Assessing social support among south Asians: the multidimensional scale of perceived social support. Asian J. Psychiatr. 5, 164–168. doi: 10.1016/j.ajp.2012.02.012
Townend, E., Tinson, D., Kwan, J., and Sharpe, M. (2006). Fear of recurrence and beliefs about preventing recurrence in persons who have suffered a stroke. J. Psychosom. Res. 61, 747–755. doi: 10.1016/j.jpsychores.2006.09.006
Vickers, A. J. (2005). Parametric versus non-parametric statistics in the analysis of randomized trials with non-normally distributed data. BMC Med. Res. Methodol. 5:35. doi: 10.1186/1471-2288-5-35
Wan, X., Chan, D. N. S., Chau, J. P. C., Zhang, Y., Liao, Y., Zhu, P., et al. (2024). Effects of a nurse-led peer support intervention on psychosocial outcomes of stroke survivors: a randomised controlled trial. Int. J. Nurs. Stud. 160:104892. doi: 10.1016/j.ijnurstu.2024.104892
Wu, Y., Wang, X., Liu, L., Shi, X., Zhu, X., Cao, Y., et al. (2025). Fear of progression in Chinese patients after cardiac valve replacement: profiles, influencing factors, and mechanisms. Eur. J. Cardiovasc. Nurs. 24, 422–431. doi: 10.1093/eurjcn/zvae178
Yang, Z., Chen, C., Wang, M., Yang, Y., and Xu, L. (2025). Prevalence and factors influencing fear of disease progression in stroke patients: a systematic review and meta-analysis with a focus on China. BMJ Open 15:e091605. doi: 10.1136/bmjopen-2024-091605
Yao, J., Wu, H., Ma, Y., Xie, W., Lian, X., and Chen, X. (2022). The negative affectivity dimension of type D personality associated with increased risk for acute ischemic stroke and white matter hyperintensity. J. Psychosom. Res. 160:110973. doi: 10.1016/j.jpsychores.2022.110973
Yin, S., Li, N., and Wang, Y. (2023). Prognostic value of type D personality for post-strokedepression in ischemic stroke patients. J. Affect. Disord. 333, 172–176. doi: 10.1016/j.jad.2023.04.064
Yu, Z., Sun, D., and Sun, J. (2022). Social support and fear of cancer recurrence among Chinese breast cancer survivors: the mediation role of illness uncertainty. Front. Psychol. 13:864129. doi: 10.3389/fpsyg.2022.864129
Zhang, D., Fan, M., Meng, L., and Zheng, X. (2022). Neuroticism and fear of COVID-19 during the COVID-19 pandemic: testing the mediating role of intolerance of uncertainty and sense of control among Chinese high school students. Front. Psychol. 13:1010767. doi: 10.3389/fpsyg.2022.1010767
Keywords: stroke, type D personality, perceived social support, intolerance of uncertainty, fear of progression, serial mediation role
Citation: Yang X, Wang L, Liu X, Chen M, Zheng Y, Ma S, Yuan J and Wang H (2025) Type D personality and fear of progression among patients with first-ever stroke: the serial mediation role of perceived social support and intolerance of uncertainty. Front. Psychol. 16:1628451. doi: 10.3389/fpsyg.2025.1628451
Edited by:
Yibo Wu, Zhejiang University, ChinaReviewed by:
Barbara Benoliel, Walden University, United StatesMarianna Berinšterová, Prešovská univerzita v Prešove, Slovakia
Cansu Aykaç, Dokuz Eylul University, Türkiye
Copyright © 2025 Yang, Wang, Liu, Chen, Zheng, Ma, Yuan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohui Liu, bGl1eGlhb2h1aUBueG11LmVkdS5jbg==
 Xiaoping Yang
Xiaoping Yang Lijun Wang2
Lijun Wang2 Huijuan Wang
Huijuan Wang