- 1Department of Psychology, Air Force Hospital of Eastern Theater Command, Nanjing, China
- 2Department of Outpatient, Air Force Hospital of Eastern Theater Command, Nanjing, China
- 3Department of Orthopedics, Air Force Hospital of Eastern Theater Command, Nanjing, China
- 4Physical Examination Department of Nanjing Selection Center of Air Force Recruitment, Nanjing, China
Background: Individual blood pressure levels can be influenced by psychological factors.
Objective: This study aimed to investigate the relationship between hypertension and psychological states, as well as the underlying mechanisms, using a combination of cross-sectional comparison and experimental intervention.
Methods: A total of 102 individuals with hypertension and 108 individuals with normal blood pressure participating in pilot selection were recruited. Individuals with hypertension were divided into two intervention groups and a control group: one group received relaxation therapy alone, while the other received a combination of relaxation therapy and cognitive training. Questionnaires were administered to assess anxiety levels and perceived stress.
Results: The results showed a significant positive correlation between perceived stress and blood pressure in the BBG, and a marginal positive correlation between anxiety and blood pressure. No such correlations were found in the normal blood pressure group. Pre- and post-intervention analyses indicated that the intervention group exhibited a significant reduction in blood pressure compared to baseline levels, along with a notably higher retest pass rate. However, anxiety levels increased significantly across all groups.
Conclusion: These findings suggest that blood pressure is influenced by anxiety and perceived stress, and psychological interventions can effectively manage blood pressure. However, these interventions may not primarily operate through reducing anxiety, and further research is needed to explore the psychological mechanisms involved.
1 Introduction
Hypertension represents a major global health challenge, significantly contributing to cardiovascular disease and mortality (Dzau and Balatbat, 2019). Prolonged exposure to high-stress environments may further elevate the risk of its onset (Hahad et al., 2023). The relationship between occupational characteristics and hypertension has garnered considerable attention, with pilots being recognized as a high-risk group due to their prolonged exposure to high workloads, circadian rhythm disruptions, and high-stress environments (Kang, 2022; Maculewicz et al., 2022). Therefore, blood pressure indicators are very important for the selection of pilots.
Moreover, psychological state influences physiological state. Hypertension as a psychosomatic disorder, with links between perceived stress, anxiety (Mann, 2012; Spruill et al., 2019). A study demonstrated that anxiety modifies sympathetic firing patterns, activating the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis in patients, which results in elevated blood pressure (Lambert et al., 2010; Hamam et al., 2020). These findings have significant clinical implications for the early detection of hypertension and the implementation of psychological interventions (Lim et al., 2021). Psychological interventions, such as relaxation training and cognitive therapy, have been shown to be effective in reducing blood pressure (Dickinson et al., 2008; Li et al., 2021). A recent study involving 64 participants found that relaxation training combined with slow breathing exercises can effectively reduce blood pressure (Pathan et al., 2023). Another study involving 92 participants also found that cognitive-based psychological interventions contribute to reducing blood pressure (Clemow et al., 2018). However, cross-sectional comparisons of different psychological interventions are lacking, and the mechanisms of action are unclear (Tan and Morgan, 2015).
Blood pressure is an important indicator in pilot selection. It can be temporarily elevated by psychological factors such as tension during selection tests. This temporary increase may disqualify candidates from further participation. Therefore, it is necessary to investigate whether reductions in blood pressure following psychological interventions are associated with decreases in anxiety, and to explore effective interventions to minimize transient elevations during the initial screening of pilot selection.
The novelty of this study lies in the recruitment of pilot candidates as the study population. It compared anxiety and stress levels between the Normal Control Group (NCG) and the Hypertension Group (BBG), evaluated the effectiveness of two different psychological interventions in lowering blood pressure, and further explored the underlying psychological mechanisms. This research provides both theoretical and practical support for optimizing medical screening, which is of particular significance for specific occupational groups. The findings may help to reduce the risk of misdiagnosis caused by incomplete assessment of psychological and physiological states, thereby enhancing the accuracy and fairness of medical screening.
2 Materials and methods
2.1 Study design
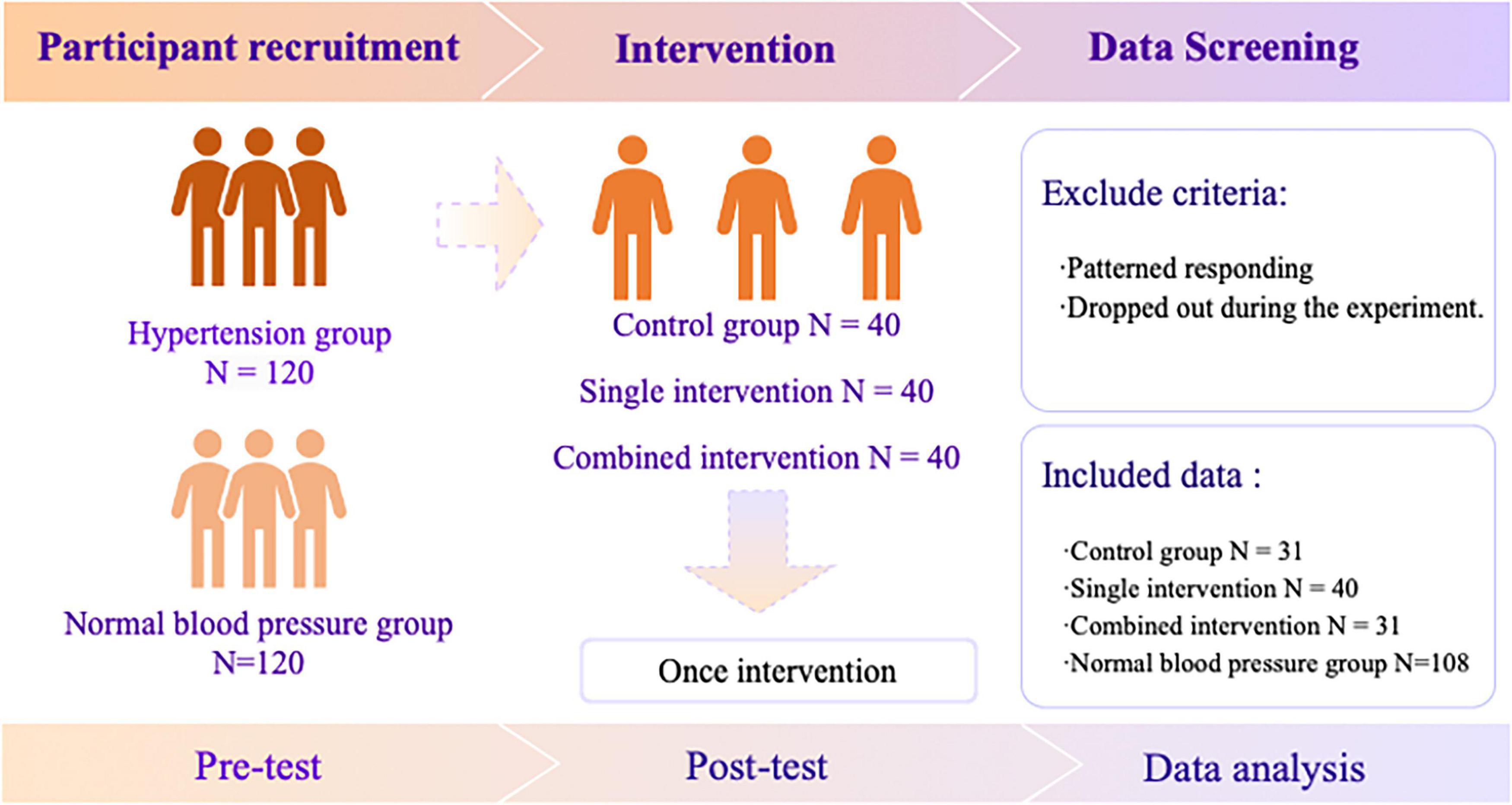
This study adopted a randomized controlled design to examine the psychological and physiological outcomes of interventions among pilots with hypertension. Participants were allocated into different groups through computer-generated randomization, and the procedures included recruitment, intervention, and follow-up assessments. The overall procedure is illustrated in Figure 1.
2.2 Participants
120 male participants with hypertension were recruited from pilot medical examination. Participants were recruited for this study if they met the following criteria: (1) Met the specified range of the 2018 Chinese Hypertension Prevention and Treatment Guidelines, where hypertension is defined as a systolic blood pressure ≥ 140 mm Hg and/or a diastolic blood pressure ≥ 90 mm Hg (1 mm Hg = 0.133 kPa) (Li-Sheng, 2019); (2) had no organic damage such as retinal lesions or electrocardiographic abnormalities; (3) had no history of hypertension or syncope; (4) had no family history of hypertension; (5) had no history of anemia, hyperthyroidism, adrenal cortical adenoma, or other diseases affecting the cardiovascular system.
As a control, 120 healthy male participants were recruited during the pilot medical examination. The studies involving human participants were reviewed and approved by the Medical Ethics Committee of The Air Force Hospital from Eastern Theater of the People’s Liberation Army (PLA).
2.3 Instrument
Anxiety was assessed using the Self-Rating Anxiety Scale, a 20-item measure in which items 5, 7, 10, and 13 are reverse-scored (Zung, 1971). A 4-point Likert scale was used, with 1 indicating “never” and 4 signifying “most or all of the time.” Higher scores reflected elevated levels of anxiety in individuals. The Cronbach’s αα in this study was 0.82.
Perceived stress was measured with Chinese Perceived Stress Scale, a 14-item measure in which items 4, 5, 6, 7, 9, 10, 12, and 13 are reverse-scored (Cohen et al., 1983; Yang and Huang, 2003). A 6-point Likert scale was used, with 1 being “never” and 6 being “always.” A higher total score indicates a higher perceived stress and a greater sense of uncontrollability. Cronbach’s α in this study was 0.78.
Blood pressure was measured using the Omron HEM-907XL, with the following standardized procedures: the measurements were taken three times, with a one-min interval between each measurement to ensure accuracy. The appropriate cuff size (22–32 cm) was selected based on the participant’s arm circumference. Participants were instructed to remain seated in a relaxed position, with their feet flat on the floor and their back supported. A resting period of at least five minutes was allowed before measurements were taken to ensure a stable baseline reading.
The pass rate refers to the probability that blood pressure meets the selection criteria for Air Force pilot recruitment.
2.4 Intervention
The single intervention group took part in relaxation training sessions lasting about 30 min. These sessions included guided techniques to promote physical and mental relaxation, such as controlled breathing exercises, progressive muscle relaxation and visualization methods to reduce stress and tension.
The combined intervention group received a more comprehensive approach. Participants first underwent a recognized intervention based on cognitive behavioral therapy (CBT). This phase involved structured activities that focused on identifying and challenging negative thought patterns, promoting adaptive coping strategies, and developing emotional regulation skills. This was followed by approximately 30 min of relaxation training, like the single intervention group. This sequential approach aimed to combine the cognitive benefits of CBT with the physiological and emotional relaxation benefits of the training to achieve more substantial and lasting effects on stress and blood pressure reduction. Both interventions were delivered under the guidance of trained professionals in a quiet and comfortable environment to maximize participants’ concentration and effectiveness.
Additionally, the Control group received no intervention.
2.5 Data collection
Before the start of the study, all 240 participants signed the informed consent form. Participants in the hypertension group were randomly assigned to their respective groups using the website https://www.randomizer.org/. The entire study was conducted at a dedicated medical examination center. Data were collected by three medical staff members responsible for aviation medical examinations, who were blinded to the study purpose. To ensure consistency, each participant’s psychological and blood pressure data were collected by the same assessor.
During the first blood pressure measurement, participants rested in the waiting room for 5 min prior to measurement, which was usually conducted between 8:00 and 10:00 a.m. In the afternoon, between 2:00 and 3:00 p.m., participants returned according to their assigned groups to receive either a single psychological intervention (approximately 30 min) or a combined psychological intervention (approximately 50 min), while the control group did not receive any intervention. At around 4:30 p.m., all groups rested in the waiting room for 5 min before the second blood pressure measurement.
2.6 Data analysis
SPSS 26.0 was used to compare the differences in anxiety, perceived stress, systolic blood pressure (SBP) and diastolic blood pressure (DBP) between the BBG and NCG. Additionally, Pearson correlation coefficients were calculated to examine the relationships between anxiety, perceived stress, SBP and DBP within each group. A two-way repeated measures analysis of variance was conducted to determine whether the interventions significantly affected anxiety, SBP, and DBP. A chi-square test was used to assess whether the pass rates between the three groups were significantly different.
2.7 Ethical consideration
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of The Air Force Hospital from Eastern Theater of the People’s Liberation Army (PLA). All participants provided written informed consent prior to participation.
3 Results
3.1 Descriptive statistics
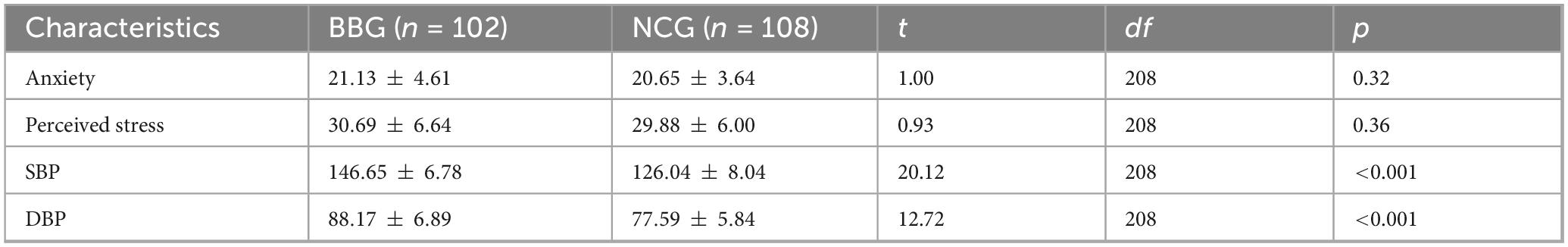
Table 1 revealed no significant differences between the BBG and NCG in terms of anxiety and perceived stress (both p > 0.05). However, a substantial difference was observed between the groups regarding systolic blood pressure (SBP) and diastolic blood pressure (DBP), with the BBG group showing significantly higher values than the NCG group (t = 20.61, p < 0.001, t = 10.73, p < 0.001). This result demonstrates that the grouping is effective.
3.2 Correlation analysis
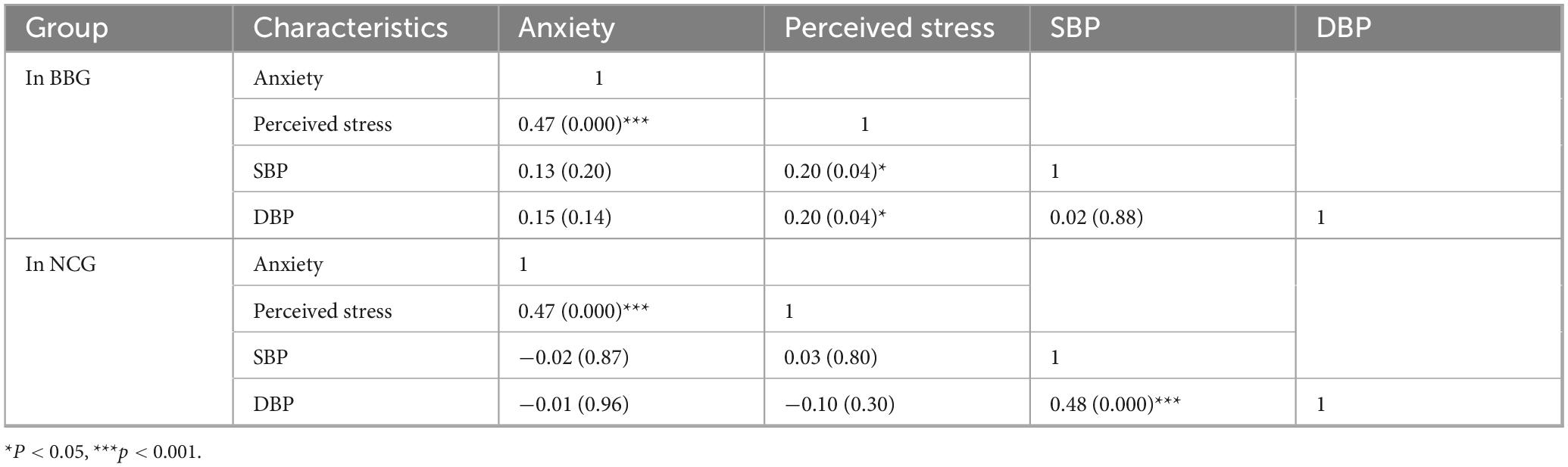
Table 2 showed a significant correlation positive correlation between anxiety and perceived stress (r = 0.47, p < 0.001) within BBG; however, no significant correlation was found between SBP and DBP. Anxiety showed marginally significant correlation with both SBP and DBP (r = 0.13, p = 0.20; r = 0.15, p = 0.13). Additionally, perceived stress showed a significant correlation with both SBP and DBP (r = 0.20, r = 0.20, both p < 0.05). Similarly, within the NCG group detected a significant positive correlation between anxiety and perceived stress (r = 0.47, p < 0.001) and between SBP and DBP (r = 0.48, p < 0.001).
The further analysis of the blood pressure and anxiety changes in the high-pressure group revealed a significant negative correlation between the change in blood pressure and the change in anxiety.
3.3 Effect of intervention method and pre- and post-intervention on the anxiety, SBP and DBP
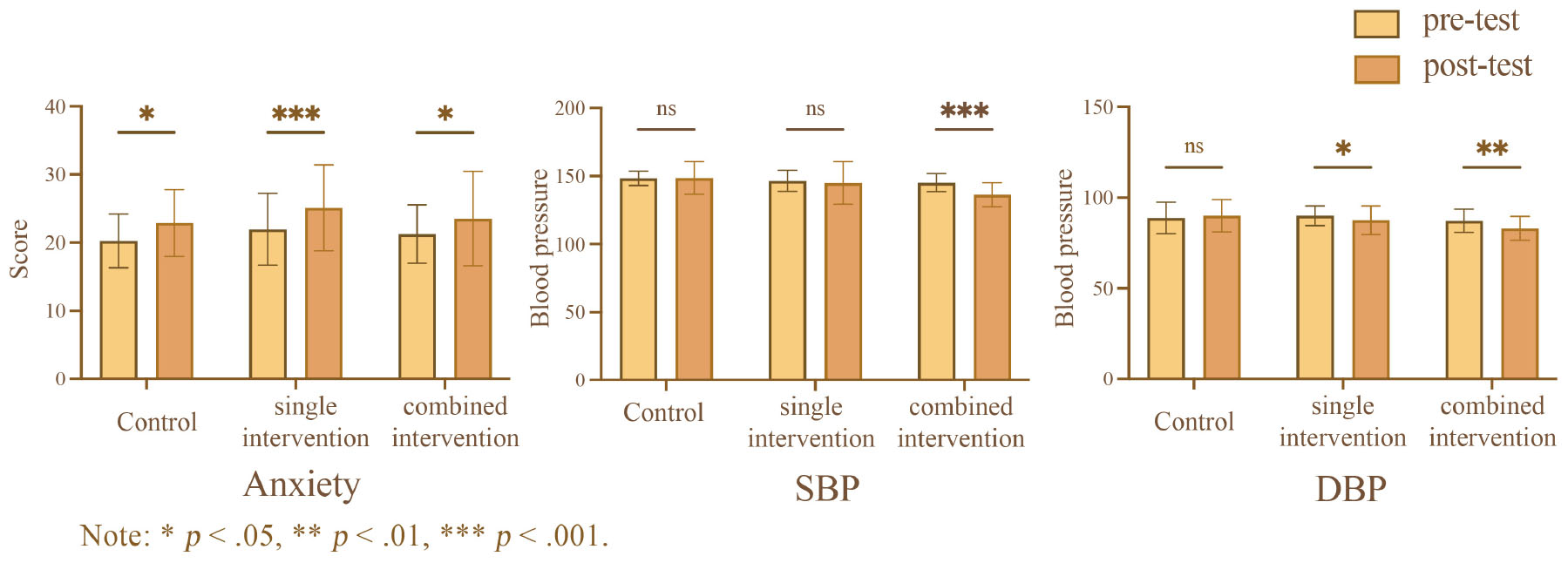
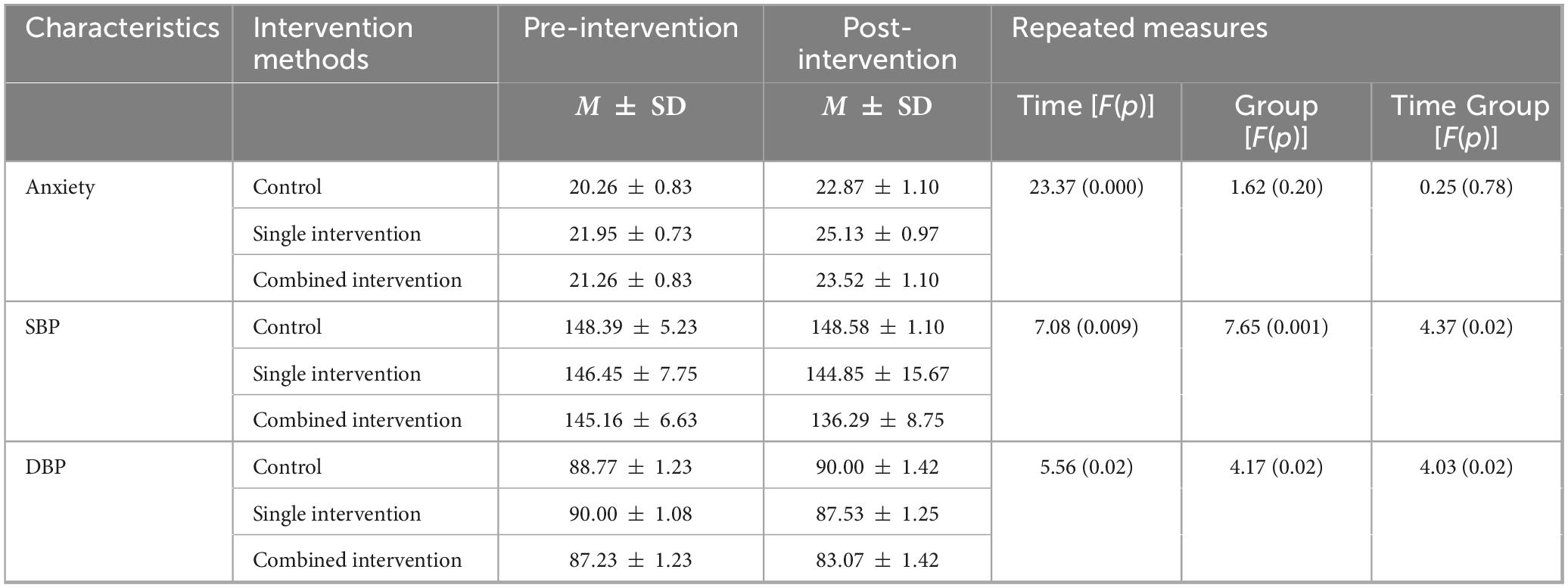
The results are presented in Figure 2 and Table 3, the results of two-way repeated measures ANOVA revealed a significant main effect of time on anxiety level was significant, anxiety levels in post-intervention (M = 23.84, SD = 0.61) were significantly higher than pre-intervention (M = 21.16, SD = 0.46), . A Tukey-adjusted simple effects analysis was conducted to examine changes in anxiety levels from pre-test to post-test across the three groups. In the control group, scores significantly increased from 20.26 (pre-test) to 22.87 (post-test), with a least-squares (LS) mean difference of −2.61, 95% CI [4.60,0.63], t(99) = 3.70, adjusted p < 0.05. The single intervention group also showed a significant increase, from 21.95 to 25.13, LS mean difference = −3.18, 95% CI [4.92,1.43], t(99) 5.11, adjusted p < 0.001. Similarly, the combined intervention group exhibited a significant increase from 21.26 to 23.52, LS mean difference = −2.26, 95% CI [4.24,0.28], t(99) = 3.20, adjusted p < 0.05.
The results of two-way repeated measures ANOVA showed that the main effect of time on SBP was significant, SBP in post-intervention (M = 143.24, SD = 1.28) were significantly lower than pre-intervention (M = 146.67, SD = 0.67), . A Tukey-adjusted simple effects analysis was conducted to examine changes in SBP from pre-test to post-test within each group. In the control group, there was no significant change in SBP (LS mean difference = −0.19, 95% CI [4.79, 4.41]), t(99) = 0.12, adjusted p < 0.93. Similarly, the single intervention group showed no significant difference in SBP between pre-test and post-test (LS mean difference = 1.60, 95% CI [2.45, 5.65]), t(99) = 1.11, adjusted p < 0.43. However, the combined intervention group demonstrated a significant reduction in SBP, with levels decreasing from 145.2 to 136.3 (LS mean difference = 8.87, 95% CI [4.27, 13.47]), t(99) = 5.41, adjusted p < 0.001.
The results of two-way repeated measures ANOVA indicated a main effect of time on DBP was significant, DBP in post-intervention (M = 86.86, SD = 0.79) were significantly lower than pre-intervention (M = 88.67, SD = 0.68), . A Tukey-adjusted simple effects analysis was conducted to examine changes in DBP from pre-test to post-test within each group. In the control group, there was no significant change in DBP (LS mean difference = −1.23, 95% CI [−3.96, 1.51]), t99 = 1.26, adjusted p = 0.38. The single intervention group showed a significant reduction in DBP between pre-test and post-test (LS mean difference = 2.48, 95% CI [0.07, 4.88]), t99 = 2.89, adjusted p < 0.05. Similarly, the combined intervention group demonstrated a significant decrease in DBP, with levels decreasing from 87.23 to 83.06 (LS mean difference = 4.16, 95% CI [1.43, 6.90]), t99 = 4.27, adjusted p < 0.01.
3.4 Effect of intervention methods on pass rates across three groups
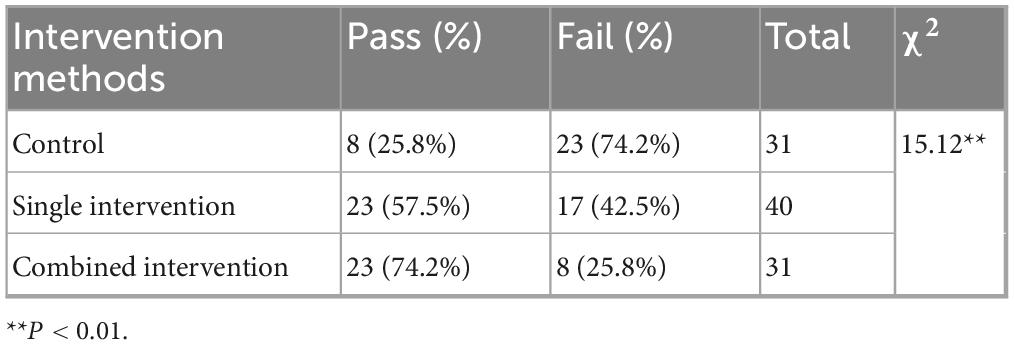
As shown in Table 4, a chi-square test was conducted to assess the differences in the pass rates across three groups: the control group, the single-intervention group, and the combined-intervention group. The results, summarized in Table 4, revealed significant differences in the pass rates among the three groups, χ2(2) = 15.12, p = 0.001. Specifically, the pass rates in both the single-intervention group (57.5%) and combined-intervention group (74.2%) were significantly higher than those in the control group (25.8%). However, no significant difference was observed between the single-intervention group and the combined-intervention group.
4 Discussion
The present study uncovered the correlation between psychological factors and blood pressure, as well as the effects of different interventions on both variables. The results indicated that although anxiety and perceived stress levels were similar between the hypertension group and the normal blood pressure group, perceived stress was positively correlated with blood pressure in the hypertension group, while anxiety showed a marginally significant correlation with blood pressure. Intervention outcomes indicated that comprehensive psychological interventions effectively reduced both systolic and diastolic blood pressure, whereas single interventions yielded limited effects. Additionally, compliance rates improved across all intervention groups, with the comprehensive intervention demonstrating the most significant effectiveness.
4.1 Psychological factors and blood pressure correlations in BBG and NCG
The findings revealed that in the BBG group, perceived stress was significantly positively correlated with blood pressure, and anxiety showed a marginally significant positive association, whereas no such patterns were observed in the NCG group. This is partially consistent with the results of some previous studies (Forte et al., 2022; Gavrilova and Zawadzki, 2023). One possible explanation for this phenomenon is heightened hypothalamic-pituitary-adrenal (HPA) axis activation in individuals with hypertension, likely due to their prolonged near-hypertensive state, which increases their susceptibility to stress and anxiety (Johnson, 2019; Qi et al., 2023). Therefore, the BBG group may show a correlation between psychological factors and blood pressure, while the NCG group does not. Another possible explanation is that hypertension is often comorbid with trait or chronic anxiety (Rosas et al., 2021, 2024). Concurrently, individuals with higher levels of trait anxiety are more likely to show high state anxiety and stress (Weger and Sandi, 2018; Saviola et al., 2020). As the participants in the NCG group had normal blood pressure, their trait anxiety levels might generally be lower, resulting in weaker associations with state anxiety and perceived stress levels. This could help explain the absence of significant relationships between blood pressure and anxiety or stress levels within this group. Furthermore, additional potential psychological factors, such as emotional regulation ability and personality traits, or physiological mechanisms, including vascular elasticity and heart rate variability (HRV), may also act as influence factors between normotensive and prehypertensive groups (Piotrowska-Półrolnik et al., 2019; Chapuis-de-Andrade et al., 2021; Yugar et al., 2023; Kim, 2023). These differences warrant further investigation.
4.2 The impact of different intervention methods on blood pressure
Post-intervention results indicated that both relaxation training alone and its combination with cognitive intervention significantly reduced blood pressure compared to the control group, with the combined intervention demonstrating the most pronounced effect. Furthermore, intervention groups showed a significantly higher rate of achieving target blood pressure levels. These findings support previous research showing that psychological interventions can help manage blood pressure (Huang et al., 2023; Chen et al., 2024). Possible mechanisms underlying these effects can be explained by the BERN framework, an operational model within mind-body medicine (MBM) that encompasses four multimodal intervention strategies: Behavior, Exercise, Relaxation, and Nutrition (Esch and Stefano, 2022). Based on this framework, psychological interventions including relaxation training may reduce blood pressure through two main mechanisms. First, relaxation training modulates the autonomic nervous system by enhancing parasympathetic activity and reducing sympathetic arousal, thereby lowering heart rate, decreasing vascular resistance, and inducing a self-regulated relaxation response. Second, it activates the central nervous system’s rewards and motivation circuits, engaging self-regulation processes and neurobiological signaling pathways, including the release of key messengers such as nitric oxide (NO) and dopamine, which further reduce stress responses and promote cardiovascular relaxation. This study found that the combination of relaxation training and cognitive intervention yielded the most effective results in blood pressure management, providing empirical support for future interventions. Future research could further explore and compare the effectiveness of other interventions, such as forest bathing, mindfulness, and the combination of relaxation training and cognitive intervention, in their impact on blood pressure (Lee et al., 2020; Peterfalvi et al., 2021).
4.3 Anxiety’s role in psychological interventions for blood pressure reduction
It is noteworthy that participants’ anxiety levels increased after the intervention, which is contrary to the findings of previous research studies (Wells et al., 2021; White et al., 2022). There are several possible explanations for this phenomenon. Firstly, it is possible that the intervention may have altered participants’ cognitive and expressive perceptions of anxiety, leading to a more sensitive and accurate self-report of anxiety, rather than a true increase in anxiety (Van Der Gucht et al., 2019). Secondly, Participants’ awareness that failure to achieve the required blood pressure standard in a single test could result in disqualification from the selection process may have increased their stress levels, leading to increased anxiety. Despite elevated anxiety levels, participants exhibited a decrease in blood pressure, suggesting that psychological interventions may not rely solely on anxiety reduction to impact blood pressure (Mann, 2012). Indeed, some studies have suggested that relaxation training could directly regulate physiological responses, such as reducing sympathetic nervous system activity and improving cardiovascular function (Barnes et al., 2001; Rusinova et al., 2024). This would therefore influence blood pressure independently of psychological stress or anxiety relief (Ketelhut et al., 2023). It is worth noting that there is a small difference in the level of anxiety increase between different intervention methods, indicating that differences in intervention methods may affect changes in anxiety levels. Although the overall anxiety level increased, the anxiety level of subjects who received relaxation training combined with cognitive intervention increased less than that of subjects who only received relaxation training. Some previous studies have also suggested that relaxation training and interventions combined with cognitive measures are effective in reducing anxiety (Smits et al., 2008; Montero-Marin et al., 2019; Roper et al., 2024). Based on previous studies, this study concluded that compared with single relaxation training combined with cognitive psychological intervention, it is more effective in lowering blood pressure and relieving anxiety.
5 Limitation
There are several limitations in the study. First, the study lacks follow-up data, so it is unclear whether the effects of the intervention are short term or long term. Future research should include follow-up assessments. Second, the study only focused on the relationship between anxiety and blood pressure, but other psychological factors may also affect blood pressure. Future studies could look at other factors. Third, the study only used questionnaires and experimental methods. Using other methods could get a broader perspective in the future study. Fourth, the durations of the single and combined psychological interventions differed. Although there was a certain interval between the interventions and the second measurement, the difference in intervention duration could still potentially affect blood pressure readings.
6 Conclusion
In conclusion, the findings of this study, which identified a correlation between blood pressure and anxiety-stress perception in individuals with hypertension, provide compelling evidence in support of the efficacy of combined cognitive and relaxation interventions in the management of anxiety and regulation of blood pressure.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of The Air Force Hospital from Eastern Theater of People’s Liberation Army. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
X-tD: Conceptualization, Investigation, Writing – original draft. M-jJ: Formal analysis, Resources, Writing – original draft. Z-yS: Project administration, Visualization, Writing – original draft. H-lS: Writing – review & editing. YW: Writing – review & editing. H-bZ: Supervision, Writing – review & editing. S-yW: Project administration, Supervision, Writing – review & editing. LG: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Air Force Equipment Internal Scientific Research Projects (KJ2020C001-D029).
Acknowledgments
We would like to thank all the participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Barnes, V. A., Treiber, F. A., and Davis, H. (2001). Impact of transcendental Meditation® on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. J. Psychosom. Res. 51, 597–605. doi: 10.1016/S0022-3999(01)00261-6
Chapuis-de-Andrade, S., Moret-Tatay, C., Quarti Irigaray, T., Breno Costa, D., Antonello, I. C. F., and Pinheiro Da Costa, B. E. (2021). Coping with stress and personality: A study in pregnancies complicated by hypertension. Clin. Psychol. Psychoth. 28, 1607–1619. doi: 10.1002/cpp.2603
Chen, Q., Liu, H., and Du, S. (2024). Effect of mindfulness-based interventions on people with prehypertension or hypertension: A systematic review and meta-analysis of randomized controlled trials. BMC Cardiovasc. Disord. 24:104. doi: 10.1186/s12872-024-03746-w
Clemow, L. P., Pickering, T. G., Davidson, K. W., Schwartz, J. E., Williams, V. P., Shaffer, J. A., et al. (2018). Stress management in the workplace for employees with hypertension: A randomized controlled trial. Transl. Behav. Med. 8, 761–770. doi: 10.1093/tbm/iby018
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24:385. doi: 10.2307/2136404
Dickinson, H. O., Beyer, F. R., Ford, G. A., Nicolson, D., Campbell, F., Cook, J. V., et al. (2008). Relaxation therapies for the management of primary hypertension in adults. Cochrane Database Syst. Rev. 1:CD004935. doi: 10.1002/14651858.CD004935.pub2
Dzau, V. J., and Balatbat, C. A. (2019). Future of hypertension: The need for transformation. Hypertension 74, 450–457. doi: 10.1161/HYPERTENSIONAHA.119.13437
Esch, T., and Stefano, G. B. (2022). The BERN framework of mind-body medicine: Integrating self-care, health promotion, resilience, and applied neuroscience. Front. Integr. Neurosci. 16:913573. doi: 10.3389/fnint.2022.913573
Forte, G., Favieri, F., Pazzaglia, M., and Casagrande, M. (2022). Mental and body health: The association between psychological factors, overweight, and blood pressure in young adults. JCM 11:1999. doi: 10.3390/jcm11071999
Gavrilova, L., and Zawadzki, M. J. (2023). Testing the associations between state and trait anxiety, anger, sadness, and ambulatory blood pressure and whether race impacts these relationships. Ann. Behav. Med. 57, 38–49. doi: 10.1093/abm/kaab098
Hahad, O., Rajagopalan, S., Lelieveld, J., Sørensen, M., Kuntic, M., Daiber, A., et al. (2023). Noise and air pollution as risk factors for hypertension: Part II–pathophysiologic insight. Hypertension 80, 1384–1392. doi: 10.1161/HYPERTENSIONAHA.123.20617
Hamam, M. S., Kunjummen, E., Hussain, S., Nasereldin, M., Bennett, S., and Miller, J. (2020). Anxiety, depression, and pain: Considerations in the treatment of patients with uncontrolled hypertension. Curr. Hypertens. Rep. 22:106. doi: 10.1007/s11906-020-01117-2
Huang, X., Xu, N., Wang, Y., Sun, Y., and Guo, A. (2023). The effects of motivational interviewing on hypertension management: A systematic review and meta-analysis. Patient Educ. Couns. 112:107760. doi: 10.1016/j.pec.2023.107760
Johnson, H. M. (2019). Anxiety and hypertension: Is there a link? A literature review of the comorbidity relationship between anxiety and hypertension. Curr. Hypertens. Rep. 21:66. doi: 10.1007/s11906-019-0972-5
Kang, M.-Y. (2022). Occupational risk factors for hypertension. J. Hypertens. 40, 2102–2110. doi: 10.1097/HJH.0000000000003238
Ketelhut, S., Querciagrossa, D., Bisang, X., Metry, X., Borter, E., and Nigg, C. R. (2023). The effectiveness of the Wim Hof method on cardiac autonomic function, blood pressure, arterial compliance, and different psychological parameters. Sci. Rep. 13:17517. doi: 10.1038/s41598-023-44902-0
Kim, H.-L. (2023). Arterial stiffness and hypertension. Clin. Hypertens. 29:31. doi: 10.1186/s40885-023-00258-1
Lambert, E., Dawood, T., Straznicky, N., Sari, C., Schlaich, M., Esler, M., et al. (2010). Association between the sympathetic firing pattern and anxiety level in patients with the metabolic syndrome and elevated blood pressure. J. Hypertens. 28, 543–550. doi: 10.1097/HJH.0b013e3283350ea4
Lee, E. K. P., Yeung, N. C. Y., Xu, Z., Zhang, D., Yu, C.-P., and Wong, S. Y. S. (2020). Effect and acceptability of mindfulness-based stress reduction program on patients with elevated blood pressure or hypertension: A meta-analysis of randomized controlled trials. Hypertension 76, 1992–2001. doi: 10.1161/HYPERTENSIONAHA.120.16160
Li, Y., Buys, N., Li, Z., Li, L., Song, Q., and Sun, J. (2021). The efficacy of cognitive behavioral therapy-based interventions on patients with hypertension: A systematic review and meta-analysis. Prev. Med. Rep. 23:101477. doi: 10.1016/j.pmedr.2021.101477
Lim, L.-F., Solmi, M., and Cortese, S. (2021). Association between anxiety and hypertension in adults: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 131, 96–119. doi: 10.1016/j.neubiorev.2021.08.031
Li-Sheng, L. (2019). 2018 Chinese guidelines for prevention and treatment of hypertension—a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J. Geriatr. Cardiol. 16, 182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
Maculewicz, E., Pabin, A., Kowalczuk, K., Dziuda, Ł, and Białek, A. (2022). Endogenous risk factors of cardiovascular diseases (CVDs) in military professionals with a special emphasis on military pilots. JCM 11:4314. doi: 10.3390/jcm11154314
Mann, S. J. (2012). Psychosomatic research in hypertension: The lack of impact of decades of research and new directions to consider. J. Clin. Hypertens. 14, 657–664. doi: 10.1111/j.1751-7176.2012.00686.x
Montero-Marin, J., Garcia-Campayo, J., Pérez-Yus, M. C., Zabaleta-del-Olmo, E., and Cuijpers, P. (2019). Meditation techniques v. Relaxation therapies when treating anxiety: A meta-analytic review. Psychol. Med. 49, 2118–2133. doi: 10.1017/S0033291719001600
Pathan, F. K. M., Pandian, J. S., Shaikh, A. I., Ahsan, M., Nuhmani, S., Iqbal, A., et al. (2023). Effect of slow breathing exercise and progressive muscle relaxation technique in the individual with essential hypertension: A randomized controlled trial. Medicine 102:e35792. doi: 10.1097/MD.0000000000035792
Peterfalvi, A., Meggyes, M., Makszin, L., Farkas, N., Miko, E., Miseta, A., et al. (2021). Forest bathing always makes sense: Blood pressure-lowering and immune system-balancing effects in late spring and winter in central Europe. IJERPH 18:2067. doi: 10.3390/ijerph18042067
Piotrowska-Półrolnik, M., Holas, P., Krejtz, I., and Symonides, B. (2019). Relationship between alexithymia and variability of blood pressure measured with ABPM in hypertensive patients. Gen. Hosp. Psychiatry 60, 1–5. doi: 10.1016/j.genhosppsych.2019.04.014
Qi, H., Wen, F.-Y., Xie, Y.-Y., Liu, X.-H., Li, B.-X., Peng, W.-J., et al. (2023). Associations between depressive, anxiety, stress symptoms and elevated blood pressure: Findings from the CHCN-BTH cohort study and a two-sample Mendelian randomization analysis. J. Affect. Disord. 341, 176–184. doi: 10.1016/j.jad.2023.08.086
Roper, A., Pacas Fronza, G., Dobkin, R. D., Beaudreau, S. A., Mitchell, L. K., Pachana, N. A., et al. (2024). A systematic review of psychotherapy approaches for anxiety in Parkinson’s disease. Clin. Gerontol. 47, 188–214. doi: 10.1080/07317115.2022.2074814
Rosas, C. E., Pirzada, A., Durazo-Arvizu, R. A., Sanchez-Johnsen, L. A., Perreira, K., Gallo, L., et al. (2021). Abstract P188: Anxiety is associated with six-year blood pressure change and incident hypertension: Findings from the hispanic community health study/study of Latinos. Circulation 143:488. doi: 10.1161/circ.143.suppl_1.P188
Rosas, C. E., Pirzada, A., Durazo-Arvizu, R., Gallo, L. C., Talavera, G. A., Elfassy, T., et al. (2024). Associations of anxiety symptoms with 6-year blood pressure changes and incident hypertension: Results from the hispanic community health study/study of Latinos. Ann. Behav. Med. 58, 488–497. doi: 10.1093/abm/kaae026
Rusinova, A., Volodina, M., and Ossadtchi, A. (2024). Short-term meditation training alters brain activity and sympathetic responses at rest, but not during meditation. Sci. Rep. 14:11138. doi: 10.1038/s41598-024-60932-8
Saviola, F., Pappaianni, E., Monti, A., Grecucci, A., Jovicich, J., and De Pisapia, N. (2020). Trait and state anxiety are mapped differently in the human brain. Sci. Rep. 10:11112. doi: 10.1038/s41598-020-68008-z
Smits, J. A. J., Berry, A. C., Tart, C. D., and Powers, M. B. (2008). The efficacy of cognitive-behavioral interventions for reducing anxiety sensitivity: A meta-analytic review. Behav. Res. Ther. 46, 1047–1054. doi: 10.1016/j.brat.2008.06.010
Spruill, T. M., Butler, M. J., Thomas, S. J., Tajeu, G. S., Kalinowski, J., Castañeda, S. F., et al. (2019). Association between high perceived stress over time and incident hypertension in black adults: Findings from the jackson heart study. JAHA 8:e012139. doi: 10.1161/JAHA.119.012139
Tan, M. P., and Morgan, K. (2015). Psychological interventions in cardiovascular disease: An update. Curr. Opin. Psychiatry 28, 371–377. doi: 10.1097/YCO.0000000000000181
Van Der Gucht, K., Dejonckheere, E., Erbas, Y., Takano, K., Vandemoortele, M., Maex, E., et al. (2019). An experience sampling study examining the potential impact of a mindfulness-based intervention on emotion differentiation. Emotion 19, 123–131. doi: 10.1037/emo0000406
Weger, M., and Sandi, C. (2018). High anxiety trait: A vulnerable phenotype for stress-induced depression. Neurosci. Biobehav. Rev. 87, 27–37. doi: 10.1016/j.neubiorev.2018.01.012
Wells, A., Reeves, D., Capobianco, L., Heal, C., Davies, L., Heagerty, A., et al. (2021). Improving the effectiveness of psychological interventions for depression and anxiety in cardiac rehabilitation: PATHWAY–a single-blind, parallel, randomized, controlled trial of group metacognitive therapy. Circulation 144, 23–33. doi: 10.1161/CIRCULATIONAHA.120.052428
White, V., Linardon, J., Stone, J. E., Holmes-Truscott, E., Olive, L., Mikocka-Walus, A., et al. (2022). Online psychological interventions to reduce symptoms of depression, anxiety, and general distress in those with chronic health conditions: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 52, 548–573. doi: 10.1017/S0033291720002251
Yang, T. Z., and Huang, H. T. (2003). An epidemiological study on stress among urban residents in social transition period. Chin. J. Epidemiol. 24: 760.
Yugar, L. B. T., Yugar-Toledo, J. C., Dinamarco, N., Sedenho-Prado, L. G., Moreno, B. V. D., Rubio, T. D. A., et al. (2023). The role of heart rate variability (HRV) in different hypertensive syndromes. Diagnostics 13:785. doi: 10.3390/diagnostics13040785
Keywords: hypertension, anxiety, perceived stress, relaxation training, cognitive behavioral therapy
Citation: Dou X-t, Ji M-j, Sun Z-y, Sun H-l, Wang Y, Zou H-b, Wang S-y and Gong L (2025) The impact of psychological factors on hypertension and its psychological intervention in pilot selection candidates. Front. Psychol. 16:1634423. doi: 10.3389/fpsyg.2025.1634423
Received: 24 May 2025; Accepted: 23 September 2025;
Published: 06 November 2025.
Edited by:
Yibo Wu, Zhejiang University, ChinaReviewed by:
Barbara Schmidt, University Hospital Jena, GermanyAndi Safutra Suraya, Universitas Muhammadiyah Gorontalo, Indonesia
Copyright © 2025 Dou, Ji, Sun, Sun, Wang, Zou, Wang and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hai-bin Zou, OTk0MDQ5ODU3QHFxLmNvbQ==; Si-yang Wang, d3N5MTk5MDEyMTRAc2luYS5jb20=; Lin Gong, MTgzNjA3ODg4N0BxcS5jb20=
†These authors have contributed equally to this work
 Xue-ting Dou
Xue-ting Dou Ming-jing Ji2†
Ming-jing Ji2† Zhong-yang Sun
Zhong-yang Sun Si-yang Wang
Si-yang Wang