- School of Journalism and Communication, Chongqing University, Chongqing, China
Purpose: Human papillomavirus (HPV) poses a substantial health risk to men, yet male vaccination remains under-prioritized in China. This study examines how five Protection Motivation Theory (PMT) cognitions (perceived severity, perceived vulnerability, response efficacy, self-efficacy, and response cost), together with descriptive norms and media trust, shape Chinese men’s willingness to receive the HPV vaccine. We further assess both direct effects and indirect (mediated) pathways linking these factors to vaccination willingness.
Participants and methods: A nationwide online quota survey collected 3,013 valid responses from men aged 18–45 across 120 Chinese cities. Five-point Likert scales assessed perceived severity, perceived vulnerability, response efficacy, self-efficacy, and response cost (Protection Motivation Theory constructs), as well as descriptive norms, media trust, and HPV vaccination willingness. Structural equation modeling (AMOS 29.0) estimated direct paths while controlling for age, education, income, and marital status as covariates, and bias-corrected bootstrapping was used to test indirect (mediated) effects.
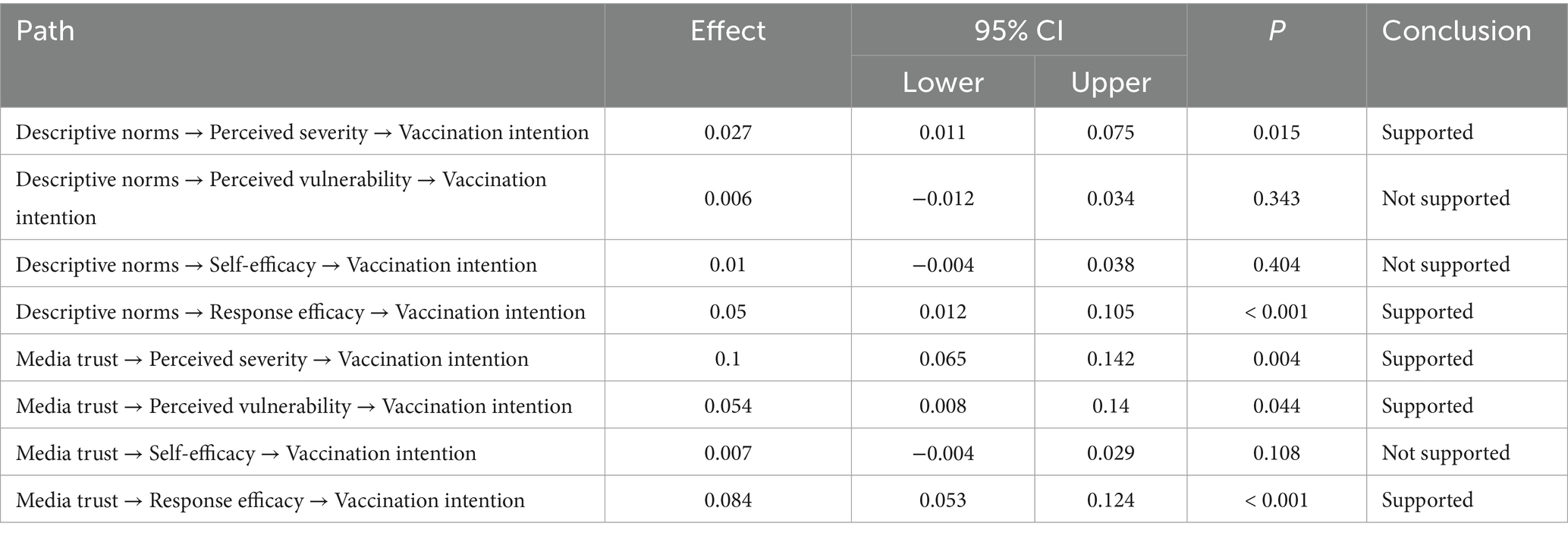
Results: Vaccination willingness was positively associated with perceived severity (β = 0.307, 95% CI [0.241, 0.372]), perceived vulnerability (β = 0.175, 95% CI [0.052, 0.303]), response efficacy (β = 0.297, 95% CI [0.228, 0.357]), self-efficacy (β = 0.133, 95% CI [0.041, 0.215]), descriptive norms (β = 0.183, 95% CI [0.126, 0.239]), and media trust (β = 0.133, 95% CI [0.052, 0.251]) (all p < 0.01). Perceived response cost was negatively associated with willingness (β = −0.314, 95% CI [−0.372, −0.246], p < 0.001). Descriptive norms indirectly promoted willingness via perceived severity and response efficacy; media trust exerted three indirect paths through perceived severity, perceived vulnerability, and response efficacy.
Conclusion: Men’s cognitive appraisal of HPV risks and their coping efficacy underpin vaccination intentions. Social cues (descriptive norms) and reliable information sources (media trust) reinforce these cognitions, amplifying willingness both directly and through PMT constructs. Interventions should normalise male vaccination, enhance message credibility, and alleviate financial or procedural burdens to broaden HPV vaccine uptake among men.
Introduction
Human Papillomavirus (HPV) infection ranks among the most common sexually transmitted diseases worldwide, with virtually every sexually active individual likely to contract HPV at some point during their lifetime (World Health Organization, 2017). According to statistical data from the World Health Organization (WHO), HPV infections constitute 15–20% of globally transmitted sexual diseases, with approximately 630,000 new cancer cases annually linked to HPV infection (Zou et al., 2022). The International Agency for Research on Cancer (IARC) reports that roughly 58.4% of new cervical cancer cases are concentrated in Asia, with China alone accounting for about 18% of these cases (Singh et al., 2023). HPV not only serves as the primary causative agent for cervical cancer in women, but epidemiological studies also indicate that HPV infection can lead to genital warts, intraepithelial neoplasia, and invasive cancers in men (World Health Organization, 2024; Staadegaard et al., 2022). Consequently, HPV infection has emerged as a significant public health challenge globally, particularly in developing nations (Patel et al., 2018).
Currently, HPV vaccines have demonstrated remarkable safety and efficacy in preventing HPV-related diseases, including cervical and genital cancers. Evidence-based medical research confirms that increasing HPV vaccination coverage can significantly reduce the incidence of cervical cancer in women and genital cancers in men (Garland et al., 2016; Markowitz et al., 2016). China lags approximately ten years behind most developed countries in promoting HPV vaccination (Pan et al., 2016). Although data indicates that HPV vaccine batch approval volumes have shown significant growth, becoming a core category in the non-mandatory vaccination market (Wang, 2021), the current vaccination coverage remains extremely low due to HPV vaccines not yet being included in China’s National Immunization Program (NIP) (Deng et al., 2021). Vaccination rates among adolescents are below 3%, while the overall population vaccination rate remains under 6% (C-CPCoGPM A, 2021). Furthermore, males were previously excluded from HPV vaccination programs until January 18th, when Merck held press conferences in Beijing, Shanghai, and Guangzhou to announce the official launch of the quadrivalent HPV vaccine for males in China.
There is growing recognition that vaccinating boys not only effectively reduces the incidence of human papillomavirus infections and related diseases in male populations, but also significantly diminishes passive infection risks among females by disrupting the transmission chain, thus creating a synergistic effect of herd immunity protection (Georgousakis et al., 2012; Kim et al., 2021). This gender-linked prevention mechanism has emerged as a crucial direction for optimizing HPV prevention strategies (Fu et al., 2024). Nevertheless, existing research still predominantly focuses on women’s willingness and behaviors regarding HPV vaccination (Zhang Z. et al., 2023). This gendered medical practice further reinforces the public perception stereotype of “male non-vulnerability” resulting in significant knowledge gaps about HPV vaccines among male populations (Varer Akpinar and Alanya Tosun, 2023; Xie et al., 2023). Limited knowledge about HPV, low risk perception, and vaccine costs —which are a primary deterrent given that the multi-dose series is not included in China’s National Immunization Program (NIP) and can cost upwards of 2,000–4,000 RMB (approx. 300–600 USD) for the full series— have led to relatively low willingness and rates of HPV vaccination among males (Chen et al., 2021; Liu et al., 2023; Yao et al., 2022; Zhang S. et al., 2023). Given these circumstances, developing pathways to enhance health literacy and promote vaccination behaviors among age-appropriate males has become a priority issue for interdisciplinary health communication research and a core concern for public health decision-making.
Health behavior change theories provide multidimensional frameworks for analyzing HPV vaccination decision-making mechanisms, with different theoretical perspectives revealing various pathways through which individual cognition and external environments influence vaccination willingness (Prestwich et al., 2015). The Protection Motivation Theory has been widely applied in vaccination research due to its systematic explanation of how threat assessment (perceived severity and vulnerability) and coping assessment (response efficacy and self-efficacy) drive health decisions (Alwreikat, 2024; Fan et al., 2025; Luo et al., 2024; Okuhara et al., 2022; Tong et al., 2021). According to PMT, individuals’ protective behaviors are motivated by two appraisal processes: threat appraisal and coping appraisal. Threat appraisal encompasses perceived severity (beliefs about the seriousness of the health threat) and perceived vulnerability (beliefs about one’s vulnerability to the threat). Coping appraisal comprises response efficacy (beliefs about the effectiveness of the recommended action) and self-efficacy (confidence in one’s ability to perform the action). The net motivation is also weighed against response costs (perceived barriers to performing the behavior). A Canadian study examining vaccination willingness across different HPV vaccine target populations found that response efficacy correlates with positive vaccination willingness, while perceived vulnerability alone cannot serve as an independent predictor of vaccination willingness (Liu et al., 2016). A study from China further confirmed PMT’s effectiveness in predicting factors influencing vaccine uptake. Except for response costs, other PMT variables significantly influenced HPV vaccination willingness among male groups through direct or indirect pathways. Knowledge levels and perceived severity indirectly affected vaccination willingness through chain mediation effects, while perceived vulnerability, response efficacy, and self-efficacy directly predicted vaccination willingness (C-CPCoGPM A, 2021).
Protection Motivation Theory (PMT) offers a systematic account of how threat appraisal (perceived severity and perceived vulnerability) and coping appraisal (response efficacy and self-efficacy) motivate preventive action. Yet classic critiques argue that PMT, in its canonical form, under-specifies social-contextual forces—notably the role of social norms in shaping intentions and behavior (Fishbein, 2007). Building on this insight, we extend PMT by incorporating two contextual determinants that are theoretically poised to inform PMT cognitions and downstream intentions: descriptive norms and media trust.
Following Rimal and Real, social norms are group-level expectations that guide behavior (Rimal and Real, 2003); a useful distinction is between descriptive norms (what most people do) and injunctive norms (what most people approve) (Cialdini et al., 1990). In vaccination contexts, injunctive cues embedded in public policy may face efficacy constraints under conditions of institutional distrust, whereas descriptive norms can cultivate a perceived “normalcy of vaccination” through social observation, thereby motivating uptake (Jaffe et al., 2022). Empirical work documents robust links between descriptive norms and HPV vaccination intentions across settings—including among men (Peterson et al., 2022; Xiao and Borah, 2021; Yarmohammadi et al., 2023). Moreover, norm exposure can shape risk perception and efficacy beliefs, which in turn influence willingness (Stout et al., 2020; Wang et al., 2023). In the present framework, descriptive norms are expected to directly promote vaccination willingness and indirectly do so by reinforcing PMT cognitions.
Media function as central infrastructures for risk information acquisition and social interaction; accordingly, individuals’ exposure to and trust in these sources shape information processing and health behavior (Li and Bautista, 2020; Lin and Lagoe, 2013). Because lay audiences often cannot directly verify complex scientific claims, trust in knowledge authorities becomes a necessary cognitive shortcut for attitude formation (Blöbaum, 2016). Consequently, information sources with higher credibility often have more pronounced effects on attitude changes (Petty and Cacioppo, 1984), and people filter information according to their trust in media, with varying degrees of trust in different information channels determining different behavioral intentions (Zhao et al., 2020). In vaccination contexts, higher media trust is consistently associated with stronger vaccination willingness (Chen et al., 2023; Glauberman et al., 2024; Limbu and Gautam, 2023; Pérez et al., 2016). Beyond direct effects, media trust has cognitive and affective impacts (Ball-Rokeach and DeFleur, 1976). And may operate through PMT variables—e.g., amplifying perceived severity and vulnerability and reinforcing response efficacy—to shape motivation (Li and Sun, 2021). Within our extension, media trust therefore serves as a contextual driver that both directly promotes willingness and indirectly strengthens PMT cognitions.
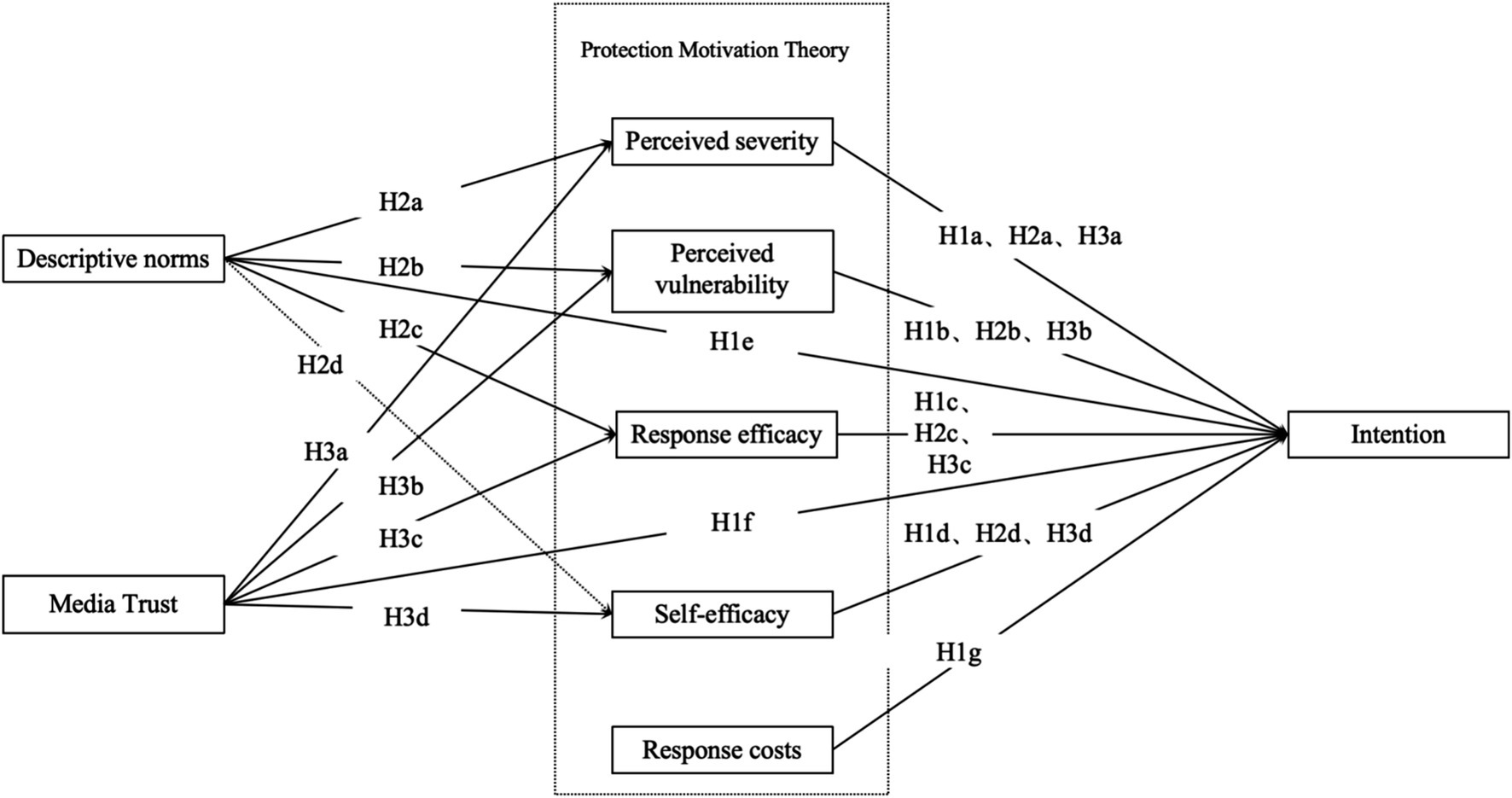
Based on the above, this study proposes the following research hypotheses:
H1: (a) Perceived severity, (b) perceived vulnerability, (c) response efficacy, (d) self-efficacy, (e) descriptive norms, and (f) media trust positively correlate with male HPV vaccination willingness; (g) response cost negatively correlates with male HPV vaccination willingness.
H2: (a) Perceived severity, (b) perceived vulnerability, (c) self-efficacy, and (d) response efficacy will mediate the relationship between descriptive norms and men' s HPV vaccination willingness.
H3: (a) Perceived severity, (b) perceived vulnerability, (c) self-efficacy, and (d) response efficacy will mediate the relationship between media trust and men' s HPV vaccination willingness.
Based on the theoretical integration above, this study proposes a comprehensive conceptual framework (see Figure 1).
Materials and methods
Survey methods
This study employed a multi-stage sampling design with quota sampling at the final stage across 120 cities in mainland China (23 provinces, 5 autonomous regions, and all 4 municipalities). Between March 15 and April 1, 2025, we first selected 120 survey sites: all provincial capitals, all four municipalities, and 2–6 randomly selected prefecture-level cities within each province and autonomous region. Within each selected city, trained local survey administrators recruited eligible men aged 18–45 and supervised on-site completion of the online questionnaire. Quota targets were used within cities to approximate demographic diversity. A total of 3,200 questionnaires were distributed and 3,013 valid responses were obtained, yielding an effective response rate of 94.16%.
Each sample city engaged at least one survey administrator or team for data collection. Individual administrators were responsible for collecting 30–90 questionnaires, while survey teams handled 100–200 questionnaires. Administrators conducted one-on-one, face-to-face questionnaire distribution through the “WJX.cn” platform.1 Respondents completed the questionnaire by accessing a unique link, with administrators ensuring informed consent and assigning a unique identifier to each submission. When respondents possessed cognitive ability but limited mobility, administrators provided one-on-one assistance and completed the questionnaire on their behalf. This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Academic Board of the School of Journalism and Communication, Chongqing University (9 January 2025 of approval). Online informed consent was obtained from all subjects involved in the study.
Study population
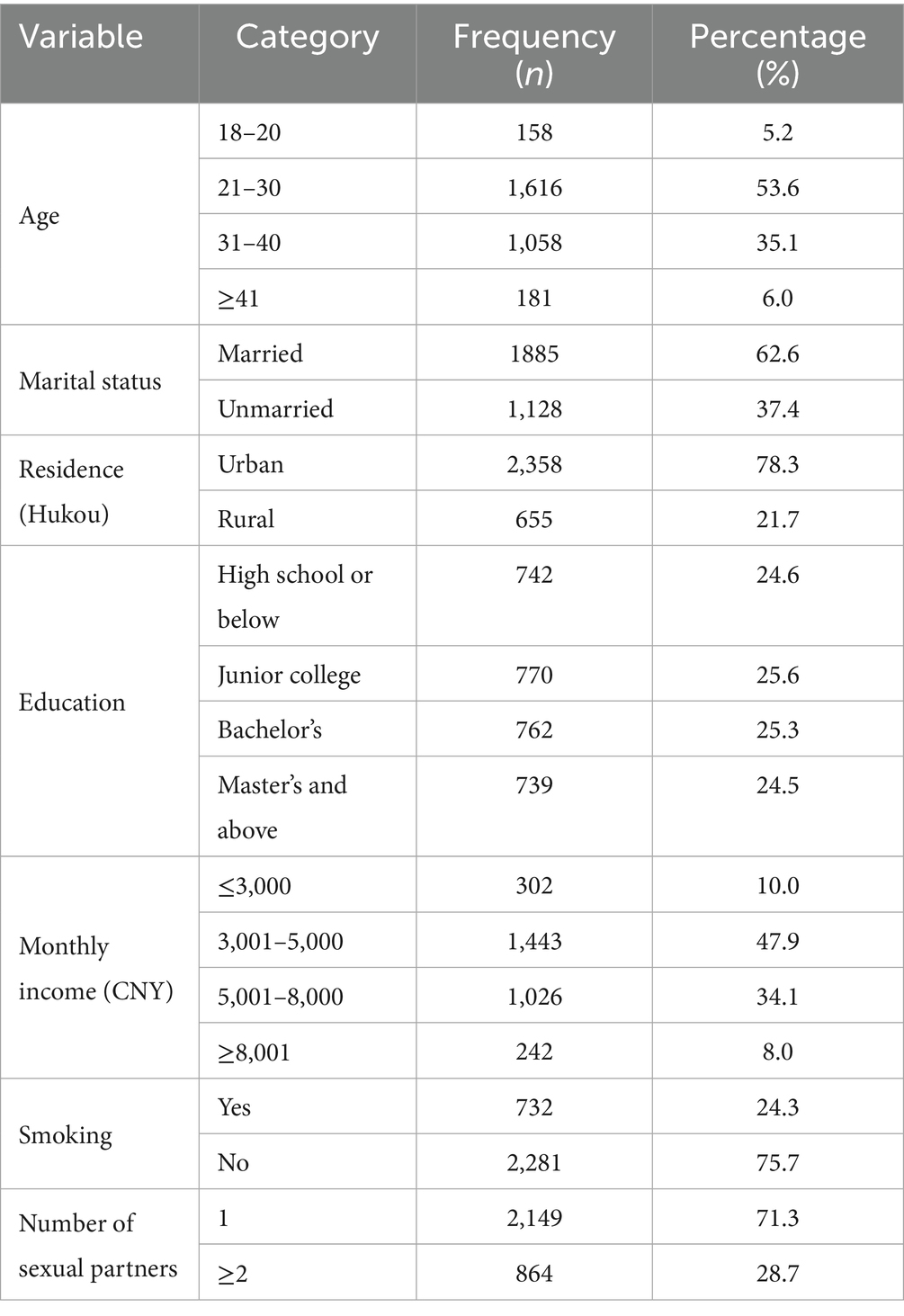
The China Comprehensive Cervical Cancer Prevention and Control Guidelines indicates that the appropriate age range for HPV vaccination is 9–45 years. We targeted men aged 18–45 because (i) the recommended vaccination window extends up to 45 years, (ii) 18 marks legal adulthood for independent consent, and (iii) this range captures sexually active men with higher exposure risk, for whom vaccination may yield both direct protection and indirect benefits via transmission interruption. Using SPSS 26.0, we analyzed the sociodemographic characteristics of the 3,013 male participants (Table 1).
Inclusion criteria: (i) males aged 18–45; (ii) Chinese citizenship; (iii) permanent residents of China (time away ≤1 month per year); (iv) voluntary participation with signed informed consent; (v) ability to complete the online questionnaire independently or with administrator assistance; (vi) comprehension of the meaning expressed in each questionnaire item.
Exclusion criteria: (i) individuals with impaired consciousness or mental disorders; (ii) current participants in similar research studies; (iii) unwilling participants.
Questionnaire design and variable measurement
General demographic information questionnaire
The questionnaire collected the following demographic and behavioral variables: age, marital status, household registration status, highest educational attainment, average monthly personal income (CNY), smoking status, and number of sexual partners.
Protection motivation questionnaire
Based on Protection Motivation Theory (PMT), this study adapted the dimensional structure and measurement methods from the Breast Cancer PMT Scale (Zhang et al., 2021), modified for cultural appropriateness and gender specificity for male HPV vaccination behaviors. The revised questionnaire included five core dimensions with 16 items, rated on a five-point Likert scale (1 = “strongly disagree” to 5 = “strongly agree”). The dimensions, definitions, measurement items, and scoring methods were as follows:
Perceived vulnerability included 3 items measuring individuals’ risk perception of HPV infection. Perceived severity contained 3 items assessing individuals’ perception of potential health consequences from HPV infection. Perceived self-efficacy comprised 4 items measuring individuals’ confidence in completing HPV vaccination. Response efficacy included 3 items evaluating individuals’ acknowledgment of HPV vaccination effectiveness. The response cost contained 3 items measuring perceived barriers to HPV vaccination in terms of economic, psychological, and time costs. Each PMT subscale score was computed as the mean of its items (1 = strongly disagree to 5 = strongly agree). Higher values indicate stronger perceived severity/vulnerability/efficacy or higher perceived cost. Example items include: severity—"HPV infection may cause serious illness”; vulnerability—"I am likely to be exposed to HPV in my lifetime”; response efficacy—"HPV vaccination can effectively prevent HPV infection”; self-efficacy—"I can complete all required vaccine doses on schedule”; response cost—"The vaccine is too expensive or time-consuming for me”.
Descriptive norms scale
Descriptive norms were measured using items adapted from Liu et al. (2024), which assess the perceived prevalence of protective behavior among salient others. The revised scale contained four items rated on a five-point Likert scale (1 = “strongly disagree” to 5 = “strongly agree”). Higher scores indicate stronger perceived normative support for HPV vaccination among male peers and close contacts. Items included: “Most of my male friends are willing to get HPV vaccination,” “Among my male colleagues or classmates, most plan to get HPV vaccination in the future,” “My close male family members (e.g., brothers, father) support and consider getting HPV vaccination,” and “Most male members in my social circle (e.g., close friends, partners) consider HPV vaccination a necessary health choice”.
Media trust scale
This study developed a media trust scale for the male HPV vaccination context by integrating Li and Sun’s (2021) “traditional-social-interpersonal” three-dimensional media trust scale and Zhou et al.’s (2023) “official-social” two-dimensional media trust scale. The scale comprised 10 items covering official/traditional media (national and local television broadcasts, government websites), social media (official new media accounts and health-related self-media accounts), and interpersonal communication (WeChat groups, verbal exchanges with relatives and friends). Respondents rated their trust in information from these sources over the past month using a 5-point Likert scale (1 = “very untrustworthy” to 5 = “very trustworthy”); higher scores indicated stronger overall media trust.
Male HPV vaccination willingness scale
Based on Fishbein et al.’s scale (Fishbein, 2008), this study developed a contextualized 4-item “vaccination willingness” scale addressing both “free vaccination scenarios” and “self-funded vaccination scenarios costing no less than 2,000 yuan.” Respondents self-reported their vaccination likelihood using a 5-point Likert scale (1 = “extremely unlikely” to 5 = “extremely likely”). While willingness may differ between free and self-funded scenarios, the core construct measured was the general psychological intention to vaccinate. A preliminary Principal Component Analysis (PCA) confirmed that all four items loaded strongly onto a single factor. More importantly, the scale showed high internal consistency (Cronbach’s α = 0.873). This suggests that despite the cost difference, the items collectively tap into a unidimensional construct of “general vaccination willingness.” Therefore, the average score of the four items was used in the final model to represent this latent variable.
Statistical analysis
Statistical Analysis. Descriptive statistics, reliability, and validity checks were conducted in SPSS 26.0. Structural equation modeling (SEM) was conducted in AMOS 29.0 with standardized variables. Age, education, income, and marital status were included as controls in all structural models. Model fit was evaluated using CMIN/DF, RMSEA, GFI, TLI, IFI, and CFI. Indirect effects were tested with bias-corrected bootstrapping (5,000 resamples, 95% CIs). Multicollinearity was assessed via variance inflation factors (VIF < 5).
Item-level missing data were minimal (all variables <3%). Missing responses in the structural equation modeling were handled using full information maximum likelihood (FIML) in AMOS 29.0, which allows all available cases to be retained under a missing-at-random assumption.
Results
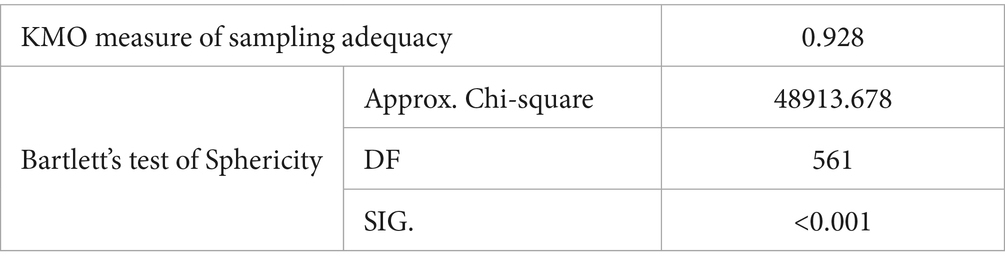
Suitability assessment
To assess the underlying factor structure of all measurement items, a principal component analysis (PCA) was conducted on the 34 items comprising the eight latent constructs. Prior to extraction, sampling adequacy was verified. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was 0.928, and Bartlett’s test of sphericity yielded a χ2 value of 48,913.678 (df = 561, p < 0.001). These statistics indicate that the data are well-suited for PCA analysis (Table 2).
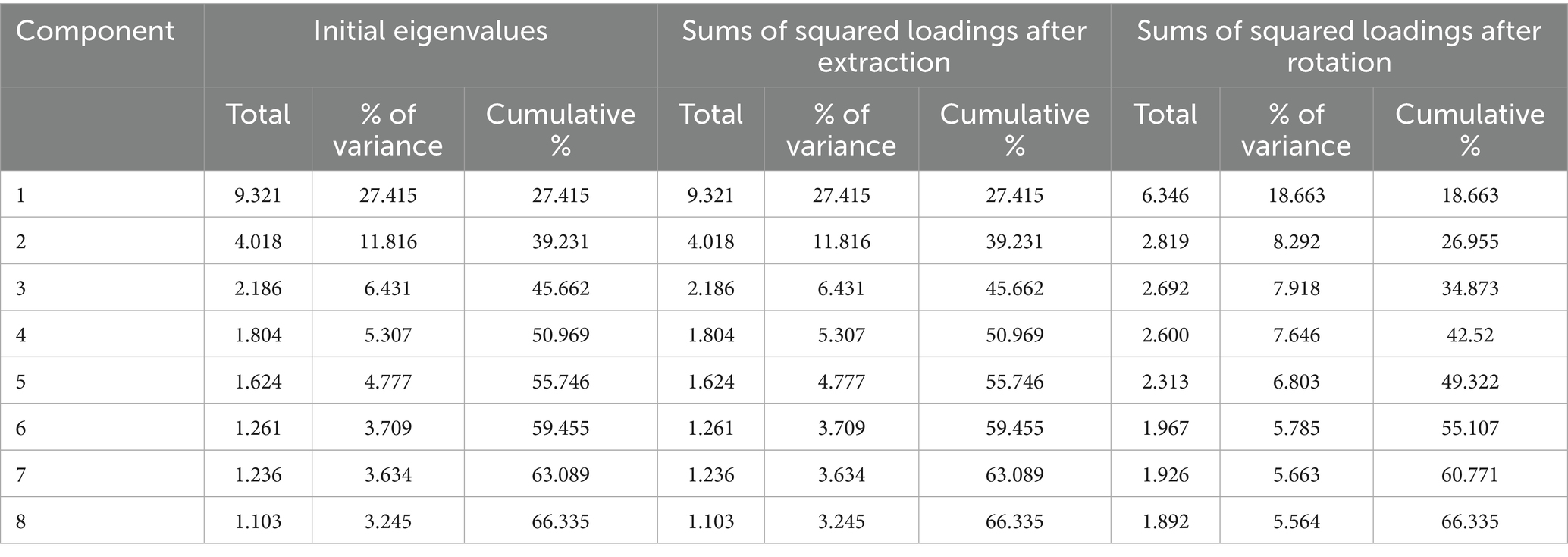
Principal component analysis
PCA extracted eight principal components that together explained 66.335% of the total variance—exceeding the 60% benchmark commonly applied in behavioral science. In the unrotated solution, the first component accounted for 27.415% of the variance, which is below the 40% threshold suggested for detecting common-method bias; hence, common-method bias is unlikely to compromise further analyses (Table 3).
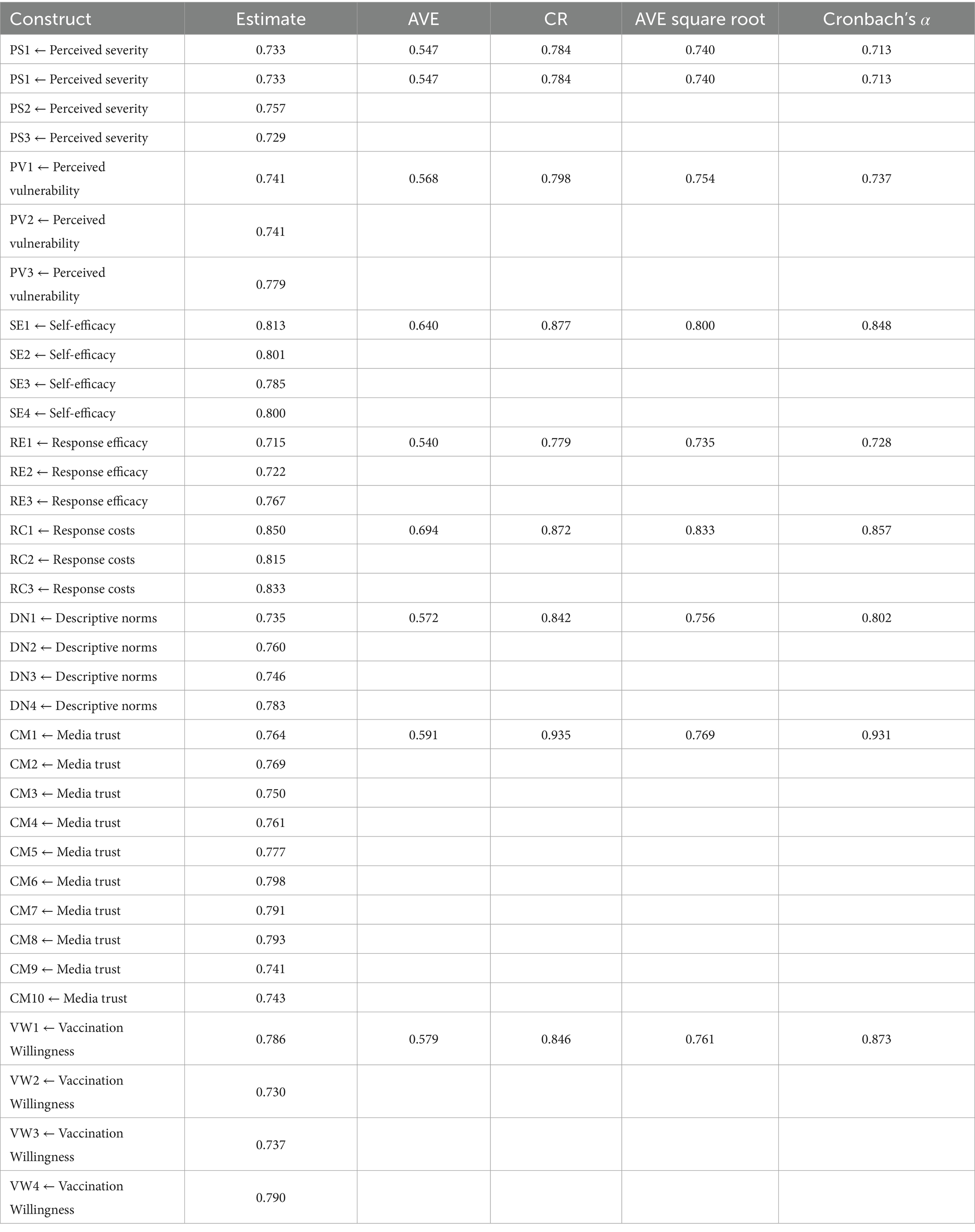
Reliability and validity assessment
Cronbach’s α coefficients for the eight latent constructs span 0.713 (Perceived Severity) to 0.931 (Media Trust), exceeding the conventional 0.70 threshold and confirming strong internal consistency across all scales. Confirmatory factor analysis shows that standardised factor loadings range from 0.715 to 0.850, well above the 0.50 criterion; average variance extracted (AVE) values fall between 0.540 and 0.694; and composite reliability (CR) indices range from 0.779 to 0.935. Together, these indicators demonstrate satisfactory convergent validity and reliability.
Discriminant validity, assessed via the Fornell–Larcker criterion, is likewise adequate: for every construct, the square root of its AVE (0.735–0.833) surpasses all corresponding inter-construct correlations reported in Table 4, indicating that each construct is empirically distinct. Collectively, the measurement model therefore exhibits robust internal consistency, convergent validity, and discriminant validity, providing a sound basis for subsequent structural modelling.
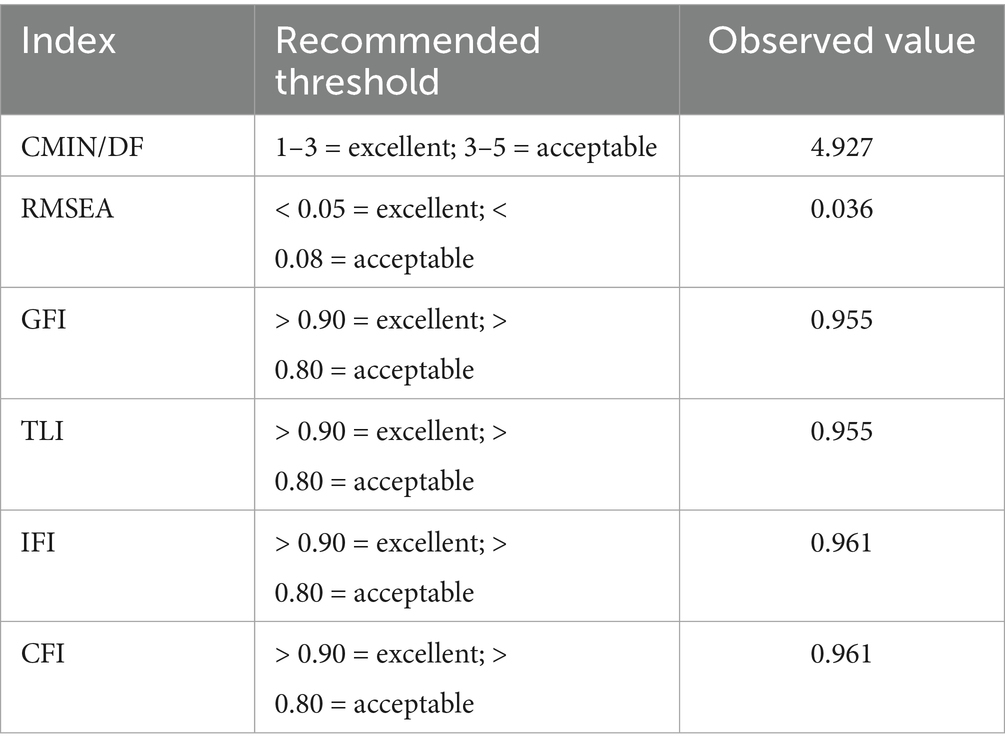
Main-effect testing
The proposed structural equation model was evaluated in AMOS 29.0. After model refinement, the fit statistics met recommended thresholds (Table 5). CMIN/DF was 4.927 (between 3 and 5 indicates adequate fit), RMSEA was 0.036 (< 0.05 denotes excellent fit), and incremental indices (GFI = 0.955, TLI = 0.955, IFI = 0.961, CFI = 0.961) all exceeded the 0.90 criterion. Collectively, these indices provide strong evidence that the structural model reproduces the observed covariance matrix with satisfactory fidelity.
To rule out multicollinearity among the exogenous predictors, variance-inflation factors were computed using the formula VIFj = 1/(1−Rj2) where denotes the coefficient of determination obtained by regressing predictor j on all other predictors (Fang and Wen, 2018). All VIF values were < 5, confirming that multicollinearity is not a concern in the present analysis.
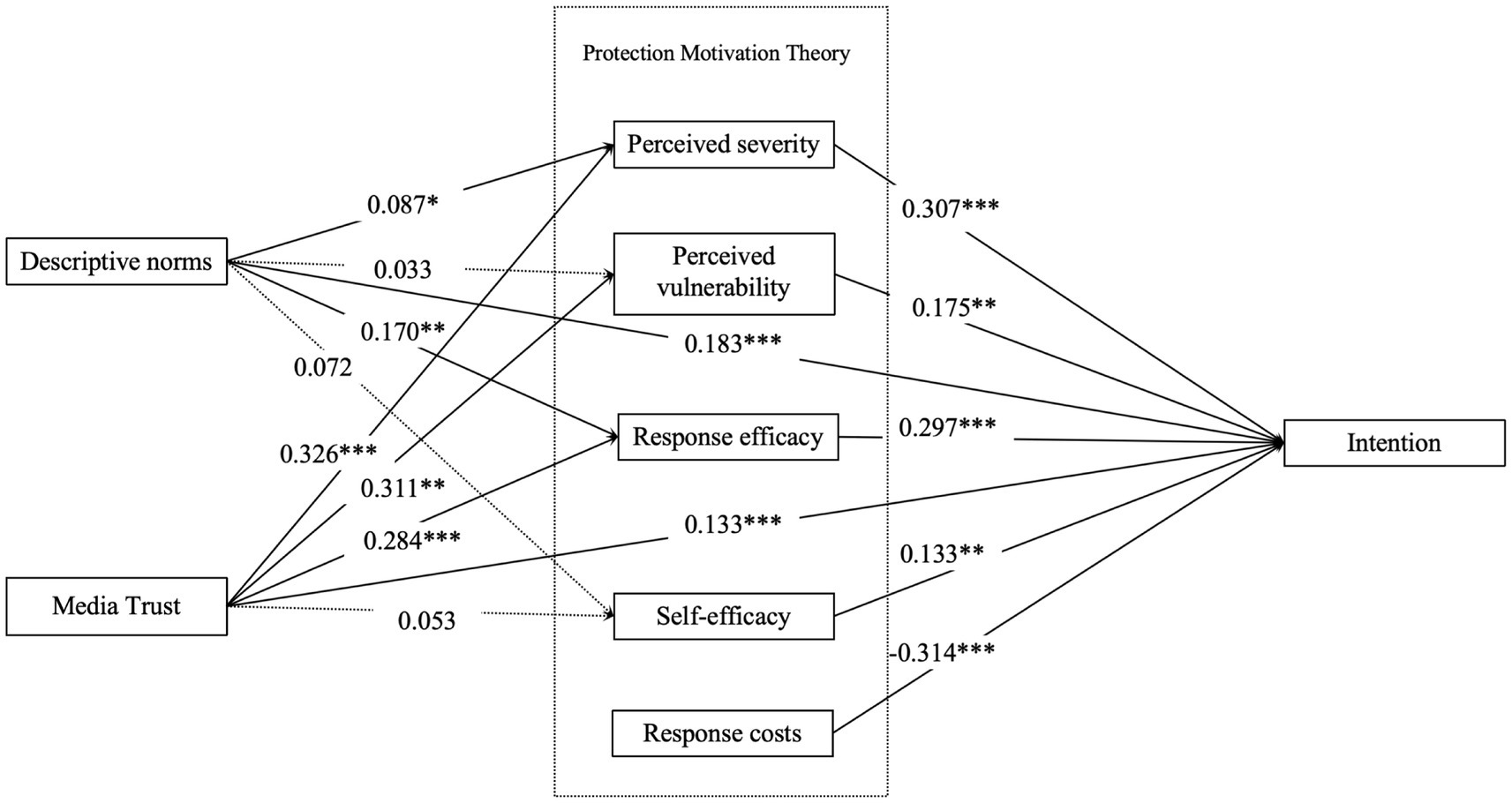
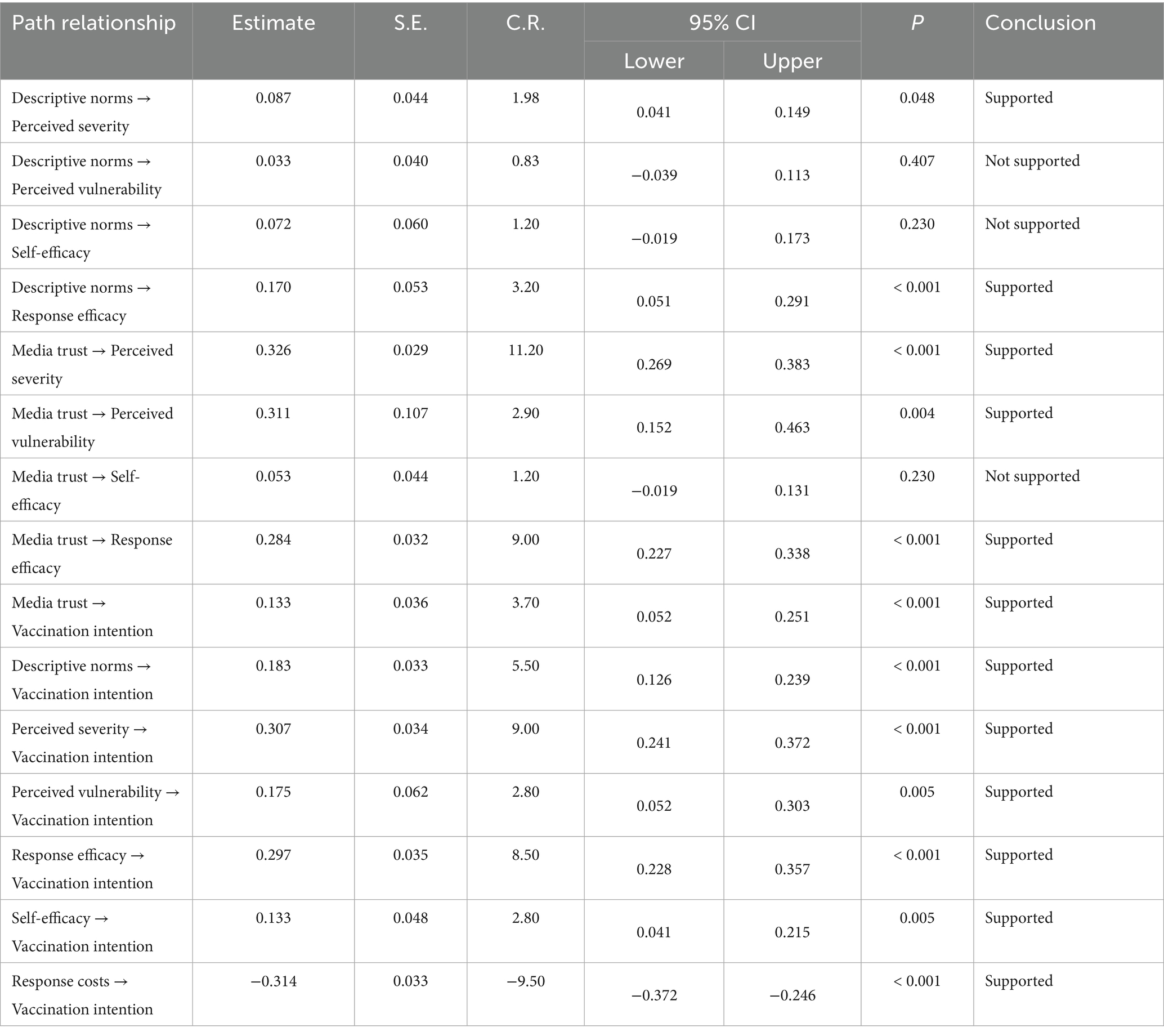
Figure 2 and Table 6 report standardized structural paths. The results show how sociocognitive predictors (descriptive norms, media trust) shape PMT appraisals, which in turn determine men’s HPV vaccination intention.
Descriptive norms, conceptualized as the perceived prevalence of HPV vaccination among salient others, had a selective influence on PMT cognitions. Descriptive norms were positively associated with response efficacy (β = 0.170, 95% CI [0.051, 0.291], p < 0.001) and perceived severity (β = 0.087, 95% CI [0.041, 0.149], p < 0.05). By contrast, paths to perceived vulnerability (β = 0.033, 95% CI [−0.039, 0.113], p = 0.407), and self-efficacy (β = 0.072, 95% CI [−0.019, 0.173], p = 0.230) were not significant. Thus, norms in this context appear to validate “this works” more than they communicate urgency or procedural know-how. Importantly, descriptive norms also showed a direct positive association with HPV vaccination intention (β = 0.183, 95% CI [0.126, 0.239], p < 0.001), indicating that perceiving vaccination as normative among peers corresponds to greater willingness to be vaccinated (see Table 7).
Media trust, defined as confidence in the credibility and reliability of vaccine-related information sources, showed a broader pattern of influence on PMT appraisals. Higher media trust was associated with higher perceived severity of HPV (β = 0.326, 95% CI [0.269, 0.383], p < 0.001), higher perceived vulnerability (β = 0.311, 95% CI [0.152, 0.463], p < 0.05), and higher response efficacy (β = 0.284, 95% CI [0.227, 0.338], p < 0.001). The path from media trust to self-efficacy was positive in direction but not statistically significant (β = 0.053, 95% CI [−0.019, 0.131], p = 0.230). In addition, media trust showed a direct positive association with HPV vaccination intention (β = 0.133, 95% CI [0.052, 0.251], p < 0.001), suggesting that confidence in trusted information environments is linked to greater willingness to be vaccinated.
HPV vaccination intention (i.e., willingness to receive the HPV vaccine) was shaped by both threat appraisal and coping appraisal. Perceived severity (β = 0.307, 95% CI [0.241, 0.372], p < 0.001) and perceived vulnerability (β = 0.175, 95% CI [0.052, 0.303], p < 0.05) showed positive associations with intention, indicating that when men view HPV as serious and personally relevant, they are more willing to vaccinate. Coping appraisal variables were also important: response efficacy (β = 0.297, 95% CI [0.228, 0.357], p < 0.001) and self-efficacy (β = 0.133, 95% CI [0.041, 0.215], p < 0.05) were both positively associated with intention, indicating that men are more willing to vaccinate when they believe vaccination works and believe they can carry it out. Perceived response cost demonstrated a significant negative association with intention (β = −0.314, 95% CI [−0.372, −0.246], p < 0.001), underscoring cost and logistical burden as deterrents.
Mediation analysis
Following the debate over percentile versus bias-corrected bootstrap procedures for mediation testing (Zhao et al., 2010) and drawing on the simulation evidence provided by (Chin et al., 2003), we employed the bias-corrected bootstrap routine in AMOS 29.0 with 5,000 resamples. An indirect effect was deemed significant when zero was excluded from the 95% bias-corrected confidence interval (CI).
For descriptive norms, two indirect pathways to vaccination intention emerged as statistically reliable. The indirect effect operating through perceived severity was significant (indirect effect = 0.027, 95% CI [0.011, 0.075], p < 0.05), indicating that perceiving HPV vaccination as common in one’s peer environment is associated with heightened perceived severity of HPV, which in turn predicts stronger intention to vaccinate. The pathway through response efficacy was also significant (indirect effect = 0.050, 95% CI [0.012, 0.105], p < 0.001), suggesting that descriptive norms may increase willingness to vaccinate by strengthening the belief that HPV vaccination is an effective and protective response. By contrast, the indirect pathways via perceived vulnerability (indirect effect = 0.006, 95% CI [−0.012, 0.034], p = 0.343) and via self-efficacy (indirect effect = 0.010, 95% CI [−0.004, 0.038], p = 0.404) were not statistically significant, as their confidence intervals included zero. Taken together, these findings indicate that descriptive norms motivate men’s HPV vaccination intention primarily by amplifying perceived threat severity and perceived response efficacy, rather than by elevating perceived susceptibility or one’s confidence in performing the behavior. Consistent with this pattern, H2a and H2d were supported, whereas H2b and H2c were not.
For media trust, several mediational paths to vaccination intention were significant. Greater trust in media was indirectly associated with stronger vaccination intention via perceived severity (indirect effect = 0.100, 95% CI [0.065, 0.142], p < 0.05) and via perceived vulnerability (indirect effect = 0.054, 95% CI [0.008, 0.140], p < 0.05), implying that trusted information sources heighten both perceived seriousness of HPV and perceived personal susceptibility, which in turn promote intention to vaccinate. Media trust was also indirectly related to vaccination intention through response efficacy (indirect effect = 0.084, 95% CI [0.053, 0.124], p < 0.001), consistent with the interpretation that credible information strengthens confidence in the effectiveness of HPV vaccination. By contrast, the pathway via self-efficacy alone was not statistically reliable (indirect effect = 0.007, 95% CI [−0.004, 0.029], p = 0.108). Overall, these results suggest that media trust shapes men’s HPV vaccination intention chiefly by increasing perceived threat relevance (severity and vulnerability) and confidence in the vaccine’s effectiveness, rather than by enhancing perceived behavioral capability. In line with this pattern, H3a, H3b, and H3d were supported, whereas H3c was not.
Discussion
This study uncovered how various dimensions of Protection Motivation Theory (PMT)—including perceived severity, perceived vulnerability, response efficacy, self-efficacy, and response cost—along with extended dimensions such as descriptive norms and media trust, directly and indirectly influence male HPV vaccination willingness.
Our data reveals that male respondents exhibited low levels of both perceived severity (M = 2.375, SD = 0.913) and perceived vulnerability (M = 2.264, SD = 1.098) regarding HPV infection risk. This phenomenon can be analyzed from two perspectives: First, within the public narrative surrounding HPV vaccines, long-term feminized marketing and patriarchal discourse have symbolically framed HPV vaccines as a “girls’ vaccine,” reinforcing stereotypes of “male non-vulnerability” in public discourse while placing the primary vaccination responsibility on women (Singh et al., 2023; Varer Akpinar and Alanya Tosun, 2023). The Ripple Effect in risk perception indicates that public risk perception of crisis events diminishes in a gradient from center to periphery: the greater the distance from the risk source, the lower the subjective risk (Erdem and Swait, 2004; Kasperson et al., 1988). Consequently, we can infer that males perceive themselves as being “pushed away” from the risk center, creating a symbolic distance that leads them to subjectively become peripheral observers. Second, this asymptomatic high-exposure state may induce an optimism bias prompting males to maintain optimistic health beliefs by underestimating their personal risk. When the “female vaccine” narrative positions males on the periphery (Ripple Effect), and their asymptomatic state simultaneously fosters this optimism bias, these two mechanisms compound to further diminish male risk perception.
This study found that perceived severity and perceived vulnerability have significant positive effects on male HPV vaccination willingness, consistent with previous research findings (Fu et al., 2024; Newman et al., 2013). A study based on attribution theory also identified perceived severity and perceived vulnerability as important factors influencing HPV vaccination willingness among American college students (Vorpahl and Yang, 2018). These results support the driving role of HPV health threat perceptions in behavioral decision-making. Specifically, males’ assessment of the severity of HPV infection consequences (such as penile cancer risk and reproductive health damage) directly influences their vaccination willingness—the greater the perceived risk, the more willing they are to receive the HPV vaccine (Pask and Rawlins, 2016). This aligns with previous research conclusions among Chinese male populations (Zhou et al., 2025). However, the effect size of perceived vulnerability is relatively low, possibly stemming from the pervasive cognitive bias among males that they are not susceptible to HPV virus, which they perceive as only affecting women (Kim, 2013; McPartland et al., 2005).
The results show that response efficacy and self-efficacy have significant positive effects on male HPV vaccination willingness. Similar studies have also found that response efficacy and self-efficacy play important roles in predicting HPV vaccination willingness (Huang et al., 2021). Efficacy beliefs play a crucial role in motivating males’ willingness to engage in HPV-related protective behaviors (Pask and Rawlins, 2016). This finding is highly consistent with the core proposition of Protection Motivation Theory: when individuals evaluate health threats and coping strategies, they are more likely to develop motivation and take corresponding actions if they believe the coping behavior is effective and they are confident in implementing it (Maddux and Rogers, 1983; Rogers, 1975). In the context of this study, males are naturally more willing to be vaccinated if they are confident that HPV vaccines can effectively prevent infection (high response efficacy) and that they can successfully complete the vaccination process (high self-efficacy). This also echoes the theoretical construction of the “confidence” dimension in the Vaccine Hesitancy Model, emphasizing that vaccination confidence is a key driver of vaccination behavior (Schmid et al., 2017).
Additionally, we found that response cost negatively affects vaccination willingness, suggesting that financial expenditure, time investment, complicated procedures, or social evaluation pressures may weaken males’ willingness to receive HPV vaccines. A five-year tracking study from mainland China pointed out that difficulty in scheduling appointments and high vaccination costs significantly constrained public willingness to receive HPV vaccines (Huang et al., 2024; Okunade et al., 2017). Two studies conducted in Ethiopia and Nigeria identified the same issue (Mihretie et al., 2022). This is consistent with the cost–benefit trade-off proposed by PMT and overlaps with the “convenience/cost” dimension in the 3C model (MacDonald, 2015). In promoting HPV vaccines for males, reducing direct and indirect costs—such as providing low-cost or free vaccines, establishing campus and workplace vaccination sites, simplifying appointment processes, and ensuring barrier-free information access—can significantly increase coverage rates (Razai et al., 2021).
Beyond traditional PMT variables, this study introduced descriptive norms from social norm theory and media trust variables to further explore the influence of these social factors on male HPV vaccination willingness. Social norm theory emphasizes that individual behavior is influenced not only by personal cognition but also by the behavior of their social groups (Cialdini et al., 1991). Descriptive norms can effectively stimulate individual vaccination behavior by shaping perceptions of “vaccination normalcy.” Results indicate that descriptive norms have a significant positive effect on male HPV vaccination willingness, a finding consistent with other studies on HPV vaccination willingness, supporting the important role of descriptive norms in health behaviors (Catalano et al., 2017; Peterson et al., 2022; Wang et al., 2017). Descriptive norms drive behavioral choices by presenting empirical evidence that specific behaviors are effective. Their core mechanism provides individuals with a “decision-making shortcut”: when people perceive that a certain behavior is widely adopted, they infer, based on the logic that “the majority is correct,” that the behavior must have inherent value or practical advantages, thereby promoting emulation motivation (Cialdini et al., 1991). Descriptive norms reflect individuals’ perception of vaccination behavior in their social circles—the more they see people around them being vaccinated, the more likely they are to identify with and imitate this behavior. When individuals perceive that a behavioral norm has formed broad consensus or gained majority approval among similar groups, this reinforced group interreference effect produces irresistible influence (Xiao and Borah, 2021).
The study also found that media trust significantly positively correlates with male HPV vaccination willingness—the higher males’ trust in vaccine information sources, the stronger their willingness to be vaccinated. In other words, media trust can, to some extent, enhance males’ acceptance of HPV vaccines, thereby promoting increased vaccination willingness. This research finding is consistent with similar studies on public HPV vaccination willingness (Anandarajah et al., 2024). With the diversification of information dissemination and the proliferation of false information, individuals’ trust in media has become an important factor influencing their health decisions (Li et al., 2025). According to Osgood’s Congruity Theory, there is a balanced relationship between people (P), information sources (S), and objects (O)—the more the audience (P) trusts the information source’s (S) claims, the more consistent the information source’s (S) claims about the object (O) are with the audience’s (P) claims about the object (O), and vice versa (Werner and James, 2000). In this process, media trust can be viewed as a simplification strategy people employ when dealing with uncertain and uncontrollable complex environments (Johnson et al., 2015; Zhang et al., 2019). Furthermore, according to the Information Adoption Model (IAM), source credibility influences system users’ perception of information usefulness as a peripheral route, thereby affecting users’ intentions and behaviors (Mo et al., 2022). This finding reveals the importance of improving information transparency and credibility when promoting and disseminating HPV vaccine information to males through media, especially against the backdrop of false information and vaccine conspiracy theories. How to construct a stable relationship between “high media trust and high vaccination willingness” becomes key to increasing vaccination rates.
Through mediation effect analysis, we found that descriptive norms primarily influence vaccination willingness through perceived severity and response efficacy, while media trust produces significant mediating effects through perceived severity, perceived vulnerability, and response efficacy.
First, the influence of descriptive norms on male HPV vaccination willingness is reflected not only in direct effects but also indirectly through perceived severity and response efficacy. This is consistent with previous similar research, where scholars found that social norms can directly influence vaccination willingness and can also produce indirect effects through factors such as response efficacy (Fadda et al., 2015). Social norms, as implicit rules, profoundly govern individual decision-making and behavioral patterns, with their mechanisms originating from humans’ continuous questioning and reflection on “what constitutes appropriate behavior in specific situations (Mollen et al., 2010).” According to Stimulus-Organism-Response (S-O-R) theory, external stimuli (such as persuasive information) need to be processed internally at the organism level (including emotional and cognitive responses) before ultimately influencing behavioral intentions (Wu, 2022). Following this analytical path, we can infer that descriptive norms, as exogenous behavioral reference cues and stimuli, form mediating and moderating effects by influencing males’ perceived severity of HPV virus infection and response efficacy at cognitive and psychological levels, ultimately affecting their vaccination willingness. This result suggests that individuals’ cognition of social group vaccination behavior enhances their perception of HPV infection severity while also boosting their confidence in vaccination effectiveness. Contrary to expectations, however, self-efficacy did not play a mediating role between descriptive norms and vaccination willingness. Previous research indicates that external persuasive factors must be combined with high-intensity self-efficacy to effectively drive individuals to adopt constructive behavioral changes (Pérez et al., 2016). A cohort analysis of American college students showed that perceiving “peers commonly being vaccinated” as a descriptive norm not only directly enhances vaccination willingness but also increases vaccination willingness by improving self-efficacy similar to masculinity (Peterson et al., 2022). However, our research data does not support the above assertion, and the specific reasons warrant further exploration in future studies.
Second, media trust, as an external contextual cue, can positively shape men’s threat appraisal of HPV infection (i.e., perceived severity and perceived vulnerability) and their coping appraisal (i.e., response efficacy), thereby increasing their willingness to receive the HPV vaccine. Zhang et al. (2019) reported that public engagement with social media can strengthen trust in the information environment, which subsequently elevates perceived vulnerability and perceived severity and, through these appraisals, increases men’s willingness to be vaccinated. Our findings provide empirical evidence for the logical pathway of “trust—threat appraisal/coping appraisal—health behavior.” To our knowledge, this study is the first to reproduce this mediating effect on the issue of male HPV vaccination willingness, indicating that media trust can consistently function through PMT variables across vaccine types. According to the Influence of Presumed Media Influence (IPMI) model, the media shapes risk attitudes through both direct and indirect mechanisms: first, the direct pathway affects individual cognition through the provision of risk information; second, the indirect pathway influences individuals’ normative beliefs and preventive behaviors by shaping their perceptions of “others’ breadth of information exposure and degree of influence” and social references (Li et al., 2025). Based on the above, we can infer that media trust utilizes the second pathway as a transformative mediator through cognitive processing (control-reflective type) and psychological processing (impulsive-reflexive type), thereby influencing male HPV vaccination willingness or actual behavior.
The indirect paths from descriptive norms and media trust to vaccination willingness via self-efficacy were not significant. This suggests that, in the present context, these factors function less as action-enabling cues (i.e., increasing perceived ability to obtain the vaccine) and more as salience-enhancing cues that increase perceived severity, perceived vulnerability, and response efficacy, which did significantly mediate willingness. Culturally, HPV vaccination in China is still framed as primarily female, and male vaccination is not yet routinized; structurally, men face cost (≥1,700 CNY), access, and procedural barriers. As a result, men may recognize HPV as relevant and vaccination as effective, but still lack confidence in their ability to practically obtain the vaccine. The non-significant self-efficacy pathway therefore reflects contextual constraints rather than the irrelevance of self-efficacy as a construct.
This study’s findings, particularly regarding descriptive norms and media trust, offer significant practical implications for health communication strategies. First, interventions should shift from focusing solely on individual risk to actively ‘normalizing’ male vaccination. Campaigns using messages like “The majority of men your age are considering the HPV vaccine” could leverage descriptive norms to enhance perceived severity and response efficacy. Second, given that media trust is a critical gateway to influencing both threat and coping appraisals, public health authorities must collaborate with high-credibility media sources. This includes partnering with authoritative state media, verified medical professionals (KOLs) on social media, and interpersonal health advisors to build a trusted information ecosystem, which in turn reinforces the core cognitions that drive vaccination willingness.
Limitations
The findings of this study should be interpreted in light of several limitations, which also provide clear avenues for future research. First, and most significantly, the study relies on a cross-sectional design. This design precludes our ability to draw firm causal conclusions. While our mediation analysis is grounded in the theoretical framework of PMT, the identified paths represent statistically significant indirect associations rather than confirmed causal chains. We must, therefore, caution against interpreting these results as definitive proof of a temporal or causal sequence. Future longitudinal or experimental studies are essential to validate the causal directionality of these relationships.
Second, our study is subject to measurement limitations. All variables were captured via self-report, which introduces the risk of common method variance (CMV) and social desirability bias. Although Harman’s single-factor test did not suggest that CMV was a pervasive issue, this test is not definitive. Furthermore, on a sensitive topic such as vaccination, responses regarding willingness may be influenced by perceived social expectations. We also measured vaccination willingness rather than actual behavior. While intention is a strong predictor, the “intention-behavior gap” is well-documented. Future research would be strengthened by incorporating objective measures, such as verified vaccination records, to complement self-reported data.
Third, our theoretical framework, while extended, has notable boundaries. We focused exclusively on descriptive norms (perceptions of what others do), omitting injunctive norms (perceptions of what others approve of). Given that both types of norms can uniquely and interactively influence health decisions, future research would benefit from testing a “dual-norm” framework to provide a more comprehensive understanding of social influence. Furthermore, our media trust scale was a composite measure combining traditional, social, and interpersonal sources. While parsimonious and reliable, this approach may conflate distinct trust mechanisms. Future work should disaggregate these sources to examine their potentially differential impacts on PMT cognitions.
Finally, our findings must be considered within the context of our sample. Our data was drawn exclusively from Chinese men aged 18–45. Consequently, the results may not be generalizable to other genders, age groups (such as adolescents, a primary target for vaccination), or cultural contexts outside of mainland China. We also acknowledge our sample has a significant urban skew (78.3%), and future studies should explicitly compare urban–rural dynamics. Moreover, although our response rate was high (94.16%) due to face-to-face administration, we did not collect data on individuals who refused to participate. This introduces a potential non-response bias, as our sample might slightly over-represent individuals who are more willing to engage with health-related topics.
Conclusion
This study deeply analyzes the influence mechanisms of male HPV vaccination willingness by integrating Protection Motivation Theory with descriptive social norms and social trust. The main research conclusions are as follows: First, perceived severity and vulnerability cognition in threat appraisal, along with response efficacy and self-efficacy in coping appraisal, collectively constitute the fundamental driving forces of behavioral decision-making. Second, descriptive norms and media trust both directly positively influence male willingness to receive HPV vaccines and indirectly influence male HPV vaccination willingness through perceived severity, response efficacy, and perceived severity, perceived vulnerability, and response efficacy, respectively. Third, response cost has a significant negative impact on vaccination willingness.
Theoretically, this study breaks through the single-pathway health behavior explanatory model, validating an integrated framework of psychological cognitive factors interacting with social norms and media trust, providing new evidence of cross-theoretical integration for health communication research. Practically, the study proposes a three-dimensional intervention strategy: First, reduce cost barriers through policy subsidies and process optimization; second, reshape male cognition through precise risk communication and efficacy enhancement training; third, create a social atmosphere of “male vaccination normalcy” through coordinated communication via authoritative medical channels, community opinion leaders, and digital platforms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Academic Board of the School of Journalism and communication, Chongqing University (9 January 2025 of approval). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZG: Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft. YG: Conceptualization, Data curation, Funding acquisition, Project administration, Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Alwreikat, A. (2024). Vaccination hesitancy: applying the protection motivation theory on parents’ information behavior. Inf. Dev. 1:102666669241261637. doi: 10.1177/02666669241261637
Anandarajah, A., Shato, T., Humble, S., Barnette, A. R., Brandt, H. M., Klesges, L. M., et al. (2024). The association of caregiver attitudes, information sources, and trust with HPV vaccine initiation among adolescents. Hum. Vaccin. Immunother. 20:2300879. doi: 10.1080/21645515.2023.2300879
Ball-Rokeach, S. J., and DeFleur, M. L. (1976). A dependency model of mass-media effects. Commun. Res. 3, 3–21. doi: 10.1177/009365027600300101
Blöbaum, B. (2016). “Trust and communication in a digitized world” in Models and concepts of trust research (Heidelberg: Springer).
Catalano, H. P., Knowlden, A. P., Birch, D. A., Leeper, J. D., Paschal, A. M., and Usdan, S. L. (2017). Using the theory of planned behavior to predict HPV vaccination intentions of college men. J. Am. Coll. Heal. 65, 197–207. doi: 10.1080/07448481.2016.1269771
C-CPCoGPM A (2021). Expert consensus on HPV vaccine application in Guangdong Province for cervical-cancer elimination. Chin. Med. J. 9, 1303–1315. doi: 10.3760/cma.j.cn431274-20210819-00911
Chen, M. M., Mott, N., Clark, S. J., Harper, D. M., Shuman, A. G., Prince, M. E., et al. (2021). HPV vaccination among young adults in the US. JAMA 325, 1673–1674. doi: 10.1001/jama.2021.0725
Chen, S. X., Ye, F. T.-f., Cheng, K. L., Ng, J. C., Lam, B. C., Hui, B. P., et al. (2023). Social media trust predicts lower COVID-19 vaccination rates and higher excess mortality over 2 years. PNAS Nexus 2:pgad318. doi: 10.1093/pnasnexus/pgad318
Chin, W. W., Marcolin, B. L., and Newsted, P. R. (2003). A partial least squares latent variable modeling approach for measuring interaction effects: results from a Monte Carlo simulation study and an electronic-mail emotion/adoption study. Inf. Syst. Res. 14, 189–217. doi: 10.1287/isre.14.2.189.16018
Cialdini, R. B., Kallgren, C. A., and Reno, R. R. (1991). A focus theory of normative conduct: a theoretical refinement and reevaluation of the role of norms in human behavior. Adv. Exp. Soc. Psychol. 24, 201–234. doi: 10.1016/S0065-2601(08)60330-5
Cialdini, R. B., Reno, R. R., and Kallgren, C. A. (1990). A focus theory of normative conduct: recycling the concept of norms to reduce littering in public places. J. Pers. Soc. Psychol. 58, 1015–1026. doi: 10.1037/0022-3514.58.6.1015
Deng, C., Chen, X., and Liu, Y. (2021). Human papillomavirus vaccination: coverage rate, knowledge, acceptance, and associated factors in college students in mainland China. Hum. Vaccin. Immunother. 17, 828–835. doi: 10.1080/21645515.2020.1797368
Erdem, T., and Swait, J. (2004). Brand credibility, brand consideration, and choice. J. Consum. Res. 31, 191–198. doi: 10.1086/383434
Fadda, M., Depping, M. K., and Schulz, P. J. (2015). Addressing issues of vaccination literacy and psychological empowerment in the measles-mumps-rubella (MMR) vaccination decision-making: a qualitative study. BMC Public Health 15, 1–13. doi: 10.1186/s12889-015-2200-9
Fan, J., Wang, Q., Deng, Y., Liang, J., Walker, A. N., and You, H. (2025). Explanation of intention toward influenza vaccination among cardiovascular disease patients: an application of the extended protection motivation theory. Public Health 242, 228–235. doi: 10.1016/j.puhe.2025.03.010
Fang, J., and Wen, Z.-L. (2018). Moderated mediation analysis based on structural equation modeling. J. Psychol. Sci. 41, 453–458. Availble at: https://jps.ecnu.edu.cn/EN/Y2018/V41/I2/475
Fishbein, M. (2007). Prediction and change of health behavior: applying the reasoned action approach : Psychology Press. (New Jersey: Lawrence Erlbaum Associates).
Fishbein, M. (2008). A reasoned action approach to health promotion. Med. Decis. Mak. 28, 834–844. doi: 10.1177/0272989X08326092
Fu, X., Guo, X., Lu, J., Zhou, W., and Lu, Y. (2024). Acceptance of human papillomavirus vaccine among boys in Asia: a narrative review. Hum. Vaccin. Immunother. 20:2429894. doi: 10.1080/21645515.2024.2429894
Garland, S. M., Kjaer, S. K., Muñoz, N., Block, S. L., Brown, D. R., DiNubile, M. J., et al. (2016). Impact and effectiveness of the quadrivalent human papillomavirus vaccine: a systematic review of 10 years of real-world experience. Rev. Infect. Dis. 63, 519–527. doi: 10.1093/cid/ciw354
Georgousakis, M., Jayasinghe, S., Brotherton, J., Gilroy, N., Chiu, C., and Macartney, K. (2012). Population-wide vaccination against human papillomavirus in adolescent boys: Australia as a case study. Lancet Infect. Dis. 12, 627–634. doi: 10.1016/S1473-3099(12)70031-2
Glauberman, G., Liebermann, E., Kornides, M. L., Matsunaga, M., Lim, E., Zimet, G., et al. (2024). Attitudes toward adolescent HPV vaccination after the COVID-19 pandemic: a National Survey of mothers. Vaccine 12:976. doi: 10.3390/vaccines12090976
Huang, Y., Ling, J., Zhao, X., Lv, Q., Wang, L., Wu, Q., et al. (2024). Are HPV vaccines well accepted among parents of adolescent girls in China? Trends, obstacles, and practical implications for further interventions: a five-year follow-up study. Vaccine 12:1073. doi: 10.3390/vaccines12091073
Huang, R., Wang, Z., Yuan, T., Nadarzynski, T., Qian, H.-Z., Li, P., et al. (2021). Using protection motivation theory to explain the intention to initiate human papillomavirus vaccination among men who have sex with men in China. Tumour Virus Res. 12:200222. doi: 10.1016/j.tvr.2021.200222
Jaffe, A. E., Graupensperger, S., Blayney, J. A., Duckworth, J. C., and Stappenbeck, C. A. (2022). The role of perceived social norms in college student vaccine hesitancy: implications for COVID-19 prevention strategies. Vaccine 40, 1888–1895. doi: 10.1016/j.vaccine.2022.01.038
Johnson, F., Rowley, J., and Sbaffi, L. (2015). Modelling trust formation in health information contexts. J. Inf. Sci. 41, 415–429. doi: 10.1177/0165551515577914
Kasperson, R. E., Renn, O., Slovic, P., Brown, H. S., Emel, J., Goble, R., et al. (1988). The social amplification of risk: a conceptual framework. Risk Anal. 8, 177–187. doi: 10.1111/j.1539-6924.1988.tb01168.x
Kim, H. W. (2013). Gender differences in knowledge and health beliefs related to behavioral intentions to prevent human papillomavirus infection. Asia Pacific J. Public Health 25, 248–259. doi: 10.1177/1010539512444307
Kim, D., Lee, H., and Kim, M. (2021). Overview of human papillomavirus vaccination policy changes and its impact in the United States: lessons learned and challenges for the future. Public Health Nurs. 38, 396–405. doi: 10.1111/phn.12873
Li, L., and Bautista, J. R. (2020). Incorporating communication factors in the theory of planned behavior to predict Chinese university students’ intention to consume genetically modified foods. Int. J. Commun. 14:22.
Li, Y., Gao, R., Li, T., and Wen, N. (2025). How social media amplifies HPV risk: applying the influence of presumed media influence model to the risk amplification framework. J. Risk Res. 28, 59–77. doi: 10.1080/13669877.2025.2485058
Li, Z., and Sun, X. (2021). Analysis of the impact of media trust on the public’s motivation to receive future vaccinations for COVID-19 based on protection motivation theory. Vaccine 9:1401. doi: 10.3390/vaccines9121401
Limbu, Y. B., and Gautam, R. K. (2023). The determinants of COVID-19 vaccination intention: a meta-review. Front. Public Health 11:1162861. doi: 10.3389/fpubh.2023.1162861
Lin, C. A., and Lagoe, C. (2013). Effects of news media and interpersonal interactions on H1N1 risk perception and vaccination intent. Commun. Res. Rep. 30, 127–136. doi: 10.1080/08824096.2012.762907
Liu, R. W., Cheng, Y., and Foerster, T. A. (2024). Modeling the relationship between perceived descriptive norms and willingness to practice COVID-19 preventative behaviors: a test of the mediation and moderation mechanisms in the theory of normative social behavior. Health Commun. 39, 339–351. doi: 10.1080/10410236.2023.2165257
Liu, S., Liu, K., Fu, L., and Liu, Z. (2023). Research progress on the preventive efficacy of HPV vaccination in males. New Medicine 54, 783–786. Available at: https://kns.cnki.net/kcms2/article/abstract?v=hQtzIo_70oEC7bFvXYIX93sF7XM5Lg7Up3V7A8-LKHqS0JrH3delfVVxk9Nq8YLtL3hNU23qqCJLZNCM3sR8FDb04s6FMHxRYf7EcGBt_Mv36g2igZoXbd1o_9V3yQdAJtw_Y1qhPibD5o0897YeTF6abSEbCpIYjySsU-rMySz8ewz_TWC_rg==&uniplatform=NZKPT&language=CHS
Liu, R., Li, Y., Wangen, K. R., Maitland, E., Nicholas, S., and Wang, J. (2016). Analysis of hepatitis B vaccination behavior and vaccination willingness among migrant workers from rural China based on protection motivation theory. Hum. Vaccin. Immunother. 12, 1155–1163. doi: 10.1080/21645515.2015.1123358
Luo, C., He, Y., Xu, Y., Yang, X., and Wang, H. (2024). How does loss-versus-gain message framing affect HPV vaccination intention? Mediating roles of discrete emotions and cognitive elaboration. Curr. Psychol. 43, 9443–9456. doi: 10.1007/s12144-023-05131-w
MacDonald, N. E. (2015). Vaccine hesitancy: definition, scope and determinants. Vaccine 33, 4161–4164. doi: 10.1016/j.vaccine.2015.04.036
Maddux, J. E., and Rogers, R. W. (1983). Protection motivation and self-efficacy: a revised theory of fear appeals and attitude change. J. Exp. Soc. Psychol. 19, 469–479. doi: 10.1016/0022-1031(83)90023-9
Markowitz, L. E., Liu, G., Hariri, S., Steinau, M., Dunne, E. F., and Unger, E. R. (2016). Prevalence of HPV after introduction of the vaccination program in the United States. Pediatrics 137. doi: 10.1542/peds.2015-1968
McPartland, T. S., Weaver, B. A., Lee, S.-K., and Koutsky, L. A. (2005). Men's perceptions and knowledge of human papillomavirus (HPV) infection and cervical cancer. J. Am. Coll. Heal. 53, 225–230. doi: 10.3200/JACH.53.5.225-230
Mihretie, G. N., Liyeh, T. M., Ayele, A. D., Belay, H. G., Yimer, T. S., and Miskr, A. D. (2022). Knowledge and willingness of parents towards child girl HPV vaccination in Debre Tabor town, Ethiopia: a community-based cross-sectional study. Reprod. Health 19:136. doi: 10.1186/s12978-022-01444-4
Mo, M., Kuang, Y., Zhu, Q., Li, X., and Yue, Q. (2022). Factors influencing users’ intention to adopt online consultation information. Modern Inform. 42, 57–68. Available at: https://kns.cnki.net/kcms2/article/abstract?v=uSrlZFhNZxKHRWQKMIPG0ADJBAN0wZxUyBA1gibPIpn_1QbdmUaSCeJ3iYJgjYlWVlkhImMPdDDeNtQRYp9iZHYp0AGZ7gXGVq53yzoKtWGrtmHllj2h_b48NlnWYzfVrKq6MKxx4M7udMPLf0Cqptk5ScFSqlbygHfGDAwz5CH06wfgYGw==&uniplatform=NZKPT&language=CHS
Mollen, S., Ruiter, R. A., and Kok, G. (2010). Current issues and new directions in psychology and health: what are the oughts? The adverse effects of using social norms in health communication. Psychology & Health. 25, 265–270. doi: 10.1080/0887044090326281
Newman, P. A., Logie, C. H., Doukas, N., and Asakura, K. (2013). HPV vaccine acceptability among men: a systematic review and meta-analysis. Sex. Transm. Infect. 89, 568–574. doi: 10.1136/sextrans-2012-050980
Okuhara, T., Okada, H., Goto, E., Tsunezumi, A., Kagawa, Y., and Kiuchi, T. (2022). Encouraging HPV vaccination via an evolutionary theoretical approach: a randomized controlled study in Japan. Vaccine 10:701. doi: 10.3390/vaccines10050701
Okunade, K. S., Sunmonu, O., Osanyin, G. E., and Oluwole, A. A. (2017). Knowledge and acceptability of human papillomavirus vaccination among women attending the gynaecological outpatient clinics of a university teaching hospital in Lagos Nigeria. J. Trop. Med. 2017, 1–6. doi: 10.1155/2017/8586459
Pan, X.-F., Li, R., Pan, A., and Larson, H. (2016). Human papillomavirus vaccine approval in China: a major step forward but challenges ahead. Lancet Infect. Dis. 16, 1322–1323. doi: 10.1016/S1473-3099(16)30450-9
Pask, E. B., and Rawlins, S. T. (2016). Men’s intentions to engage in behaviors to protect against human papillomavirus (HPV): testing the risk perception attitude framework. Health Commun. 31, 139–149. doi: 10.1080/10410236.2014.940670
Patel, C., Brotherton, J. M., Pillsbury, A., Jayasinghe, S., Donovan, B., Macartney, K., et al. (2018). The impact of 10 years of human papillomavirus (HPV) vaccination in Australia: what additional disease burden will a nonavalent vaccine prevent? Eurosurveillance 23:1700737. doi: 10.2807/1560-7917.ES.2018.23.41.1700737
Pérez, S., Fedoruk, C., Shapiro, G. K., and Rosberger, Z. (2016). Giving boys a shot: the HPV vaccine’s portrayal in Canadian newspapers. Health Commun. 31, 1527–1538. doi: 10.1080/10410236.2015.1089466
Peterson, L. M., Orr, J. A., Rogelberg, S. D., and Olsen, N. (2022). Social–contextual factors interact with masculinity to influence college men’s HPV vaccination intentions: the role of descriptive norms, prototypes, and physician gender. J. Behav. Med. 45, 825–840. doi: 10.1007/s10865-022-00350-1
Petty, R. E., and Cacioppo, J. T. (1984). The elaboration likelihood model of persuasion. Advances in Experimental Social Psychology. 19, 123–205. doi: 10.1016/S0065-2601(08)60214-2
Prestwich, A., Webb, T. L., and Conner, M. (2015). Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr. Opin. Psychol. 5, 1–5. doi: 10.1016/j.copsyc.2015.02.011
Razai, M. S., Oakeshott, P., Esmail, A., Wiysonge, C. S., Viswanath, K., and Mills, M. C. (2021). COVID-19 vaccine hesitancy: the five Cs to tackle behavioural and sociodemographic factors. J. R. Soc. Med. 114, 295–298. doi: 10.1177/01410768211018951
Rimal, R. N., and Real, K. (2003). Understanding the influence of perceived norms on behaviors. Commun. Theory 13, 184–203. doi: 10.1111/j.1468-2885.2003.tb00288.x
Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change1. J. Psychol. 91, 93–114. doi: 10.1080/00223980.1975.9915803
Schmid, P., Rauber, D., Betsch, C., Lidolt, G., and Denker, M.-L. (2017). Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One 12:e0170550. doi: 10.1371/journal.pone.0170550
Singh, D., Vignat, J., Lorenzoni, V., Eslahi, M., Ginsburg, O., Lauby-Secretan, B., et al. (2023). Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO global cervical Cancer elimination initiative. Lancet Glob. Health 11, e197–e206. doi: 10.1016/S2214-109X(22)00501-0
Staadegaard, L., Rönn, M. M., Soni, N., Bellerose, M. E., Bloem, P., Brisson, M., et al. (2022). Immunogenicity, safety, and efficacy of the HPV vaccines among people living with HIV: a systematic review and meta-analysis. Eclinicalmedicine 52, 1–19. doi: 10.1016/j.eclinm.2022.101585
Stout, M. E., Christy, S. M., Winger, J. G., Vadaparampil, S. T., and Mosher, C. E. (2020). Self-efficacy and HPV vaccine attitudes mediate the relationship between social norms and intentions to receive the HPV vaccine among college students. J. Community Health 45, 1187–1195. doi: 10.1007/s10900-020-00837-5
Tong, K. K., He, M., Wu, A. M., Dang, L., and Chen, J. H. (2021). Cognitive factors influencing COVID-19 vaccination intentions: an application of the protection motivation theory using a probability community sample. Vaccine 9:1170. doi: 10.3390/vaccines9101170
Varer Akpinar, C., and Alanya Tosun, S. (2023). Knowledge and perceptions regarding human papillomavirus (HPV) and willingness to receive HPV vaccination among university students in a north-eastern city in Turkey. BMC Womens Health 23:299. doi: 10.1186/s12905-023-02455-4
Vorpahl, M. M., and Yang, J. Z. (2018). Who is to blame? Framing HPV to influence vaccination intentions among college students. Health Commun. 33, 620–627. doi: 10.1080/10410236.2017.1289436
Wang, G. S. (2021). Analysis and prospects of vaccine launch in China. Chin. J. Vaccines Immun. 27:116. doi: 10.19914/j.CJVI.2021016
Wang, L. D.-L., Lam, W. W. T., and Fielding, R. (2017). Determinants of human papillomavirus vaccination uptake among adolescent girls: a theory-based longitudinal study among Hong Kong Chinese parents. Prev. Med. 102, 24–30. doi: 10.1016/j.ypmed.2017.06.021
Wang, Y., Wei, Y., and Zhang, S. (2023). Influence of descriptive norms on influenza vaccination intention: the mediating role of risk perception and moderating role of reference groups. Public Adm. Rev. 5, 138–161.
Werner, J. S. J., and James, W. T. (2000). Communication theories: Origins, methods and uses in the mass media : Huaxia Publishing House.
World Health Organization (2017). Human papillomavirus vaccines: WHO position paper, May 2017–recommendations. Vaccine 35, 5753–5755. doi: 10.1016/j.vaccine.2017.05.06
World Health Organization. (2024). Human papillomavirus (HPV) and cancer. Available online at: https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cancer
Wu, M. (2022). What drives people to share misinformation on social media during the COVID-19 pandemic: a stimulus-organism-response perspective. Int. J. Environ. Res. Public Health 19:11752. doi: 10.3390/ijerph191811752
Xiao, X., and Borah, P. (2021). Do norms matter? Examining norm-based messages in HPV vaccination promotion. Health Commun. 36, 1476–1484. doi: 10.1080/10410236.2020.1770506
Xie, L., Ren, J., Min, S., Zhu, X., Xu, D., Qiao, K., et al. (2023). Knowledge, attitude, and perception regarding HPV-related diseases and vaccination among the general public in Guizhou Province of China. Vaccine 41, 1119–1131. doi: 10.1016/j.vaccine.2022.12.027
Yao, P.-Y., Lin, C.-Y., Ko, N.-Y., Zou, H., Lee, C.-W., and Strong, C. (2022). Predicting human papillomavirus vaccine uptake in men who have sex with men the influence of vaccine price and receiving an HPV diagnosis. BMC Public Health 22:28. doi: 10.1186/s12889-021-12396-y
Yarmohammadi, S., Mousavi, S., Ajori, L., Mohammadzade, F., and Marashi, T. (2023). Impact of attitude, subjective norms and perceived behavioral control on health behaviors among women with low-risk HPV, and the mediating role of behavioral intention: an interventional study. Int. J. Health Promot. Educ. 61, 70–82. doi: 10.1080/14635240.2021.1995776
Zhang, H., Du, J., and Wang, R. (2019). Media credibility: the impact of privately-owned websites on state-owned televisions in the context of China. J Asian Pacif. Commun. 29, 188–210. doi: 10.1075/japc.00030.zha
Zhang, S., Grant, L. H., Geipel, J., Cui, Z., and Keysar, B. (2023). The impact of informational intervention on HPV vaccination intention among heterosexual men. Vaccine 11:1653. doi: 10.3390/vaccines11111653
Zhang, Z., Shi, J., Zhang, X., Guo, X., and Yu, W. (2023). Willingness of parents of 9-to-18-year-old females in China to vaccinate their daughters with HPV vaccine. Vaccine 41, 130–135. doi: 10.1016/j.vaccine.2022.11.016
Zhang, M., Wei, W., Li, Q., Chen, X., Zhang, M., Zuo, D., et al. (2021). Determinants of intention to participate in breast cancer screening among urban Chinese women: an application of the protection motivation theory. Int. J. Environ. Res. Public Health 18:11093. doi: 10.3390/ijerph182111093
Zhao, X., Lynch, J. G. Jr., and Chen, Q. (2010). Reconsidering baron and Kenny: myths and truths about mediation analysis. J. Consum. Res. 37, 197–206. doi: 10.1086/651257
Zhao, E., Wu, Q., Crimmins, E. M., and Ailshire, J. A. (2020). Media trust and infection mitigating behaviours during the COVID-19 pandemic in the USA. BMJ Glob. Health 5:e003323. doi: 10.1136/bmjgh-2020-003323
Zhou, X., Gao, H., and Wang, J. (2025). A computational framework analysis of public attitudes toward male human papillomavirus infection and its vaccination in China: based on Weibo data. Healthcare 13, 1–17. doi: 10.3390/healthcare13030287
Zhou, Y., Zhang, A., Liu, X., Tan, X., Miao, R., Zhang, Y., et al. (2023). Protecting public’s wellbeing against COVID-19 infodemic: the role of trust in information sources and rapid dissemination and transparency of information over time. Front. Public Health 11:1142230. doi: 10.3389/fpubh.2023.1142230
Keywords: HPV vaccine, males, protection motivation theory, descriptive norms, media trust
Citation: Gong Z and Guo Y (2025) The influence of descriptive norms and media trust on male HPV vaccination willingness: an extended protection motivation theory approach. Front. Psychol. 16:1640345. doi: 10.3389/fpsyg.2025.1640345
Edited by:
Wei Wu, Guangdong Provincial Center for Disease Control and Prevention, ChinaReviewed by:
Sijia Li, The University of Hong Kong, Hong Kong SAR, ChinaSheng Bao, Jinan University, China
Copyright © 2025 Gong and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Guo, amFtZXMuZ3VvQGNxdS5lZHUuY24=
 Zhuliu Gong
Zhuliu Gong Yi Guo
Yi Guo