- 1General Hospital of Ningxia Medical University, Yinchuan, Ningxia, China
- 2School of Nursing, Ningxia Medical University, Yinchuan, Ningxia, China
Background: Overweight/obesity is associated with an increased risk of depression, which compromises the mental health of affected individuals. This study aimed to identify distinct depressive subtypes among overweight/obese individuals and examine associated multilevel factors based on the socio-ecological model (SEM), for guiding interventions enhancing mental health in this population.
Methods: Data were derived from the Psychology and Behavior Investigation of Chinese Residents in 2021 (PBICR 2021). Assessment instruments included a General Information Questionnaire, the Patient Health Questionnaire-9, the Eating Behavior Scale-Short Form, the Family Health Scale-Short Form, and the Perceived Social Support Scale. Latent profile analysis (LPA) was employed to identify depressive subtypes, and multinomial logistic regression was used to examine associated multilevel factors across the identified subtypes. Analyses were conducted using SPSS 24.0 and Mplus 8.3.
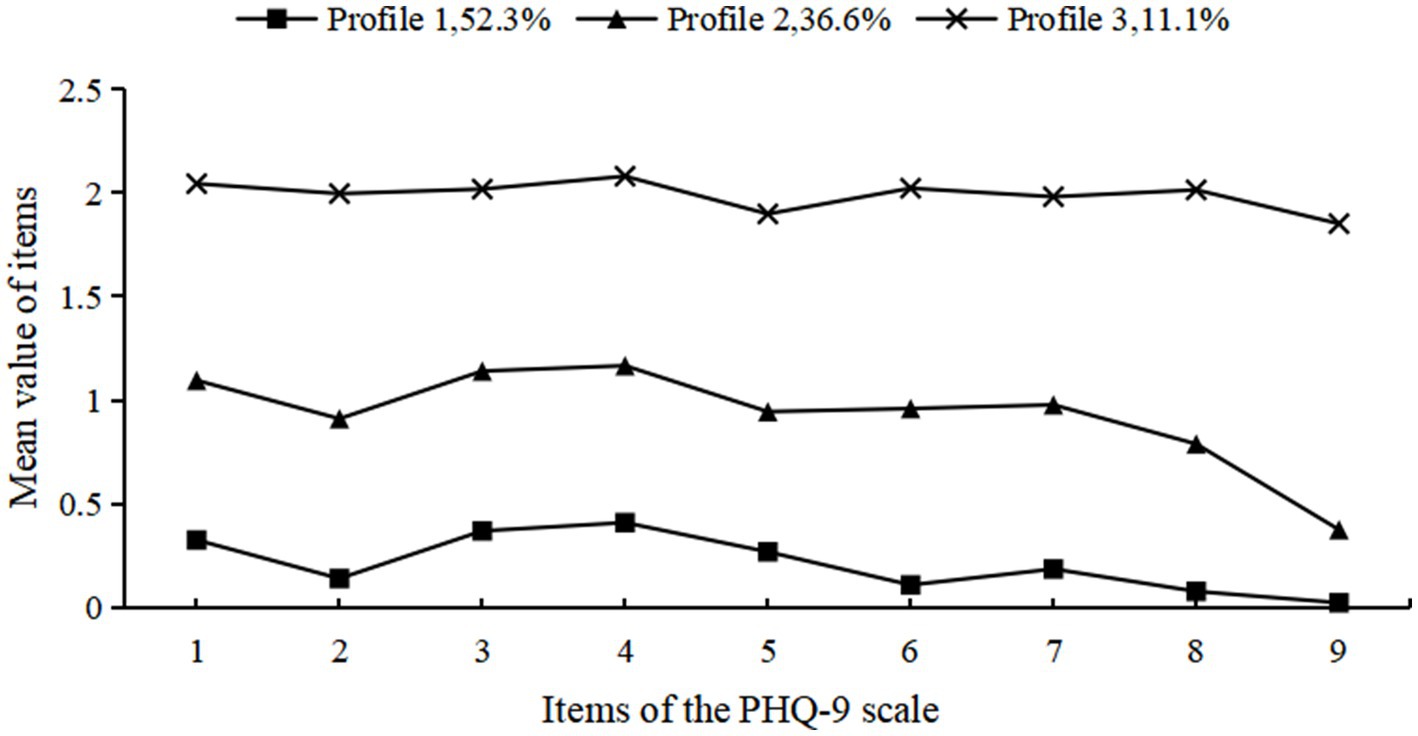
Results: This study included 2,588 participants classified into low-level (52.3%), moderate-level (36.6%), and high-level depression (11.1%) groups. Compared to the low-level group, high-level depression was significantly associated with age (18–45 years), current medication count (≥3, excl. supplements), out-of-pocket medical expenditures, higher abnormal eating behavior scores, and lower family health and social support scores. Similarly, moderate-level depression showed significant associations with female gender, age (18–45 years), having chronic conditions, current medication count (≥3, excl. supplements), out-of-pocket medical expenditures, higher abnormal eating behavior scores, and lower family health and social support scores.
Conclusion: Depression demonstrates significant heterogeneity in overweight/obese individuals, with three distinct latent profiles identified. These findings highlight the need for future primary healthcare to prioritize personalized, depression subtype-specific interventions for overweight/obese individuals, guided by multidimensional factors identified through SEM, to improve mental health.
1 Introduction
Overweight and obesity are defined as abnormal or excessive fat accumulation posing health risks (Park et al., 2022). No country to date has successfully curbed the rising rates of adult overweight and obesity (Collaborators GBD 2021 Adult BMI, 2025). China currently has the world’s largest overweight/obesity epidemic, with 402 million affected adults (Collaborators GBD 2021 Adult BMI, 2025). Overweight/obesity is associated with increased risk and earlier onset of non-communicable diseases such as diabetes and cardiovascular diseases, as well as adverse psychosocial outcomes including low self-esteem and depression (Latzer and Stein, 2013). Substantial evidence confirms a significant association between overweight/obesity and depression (Cui et al., 2018; Gerardo et al., 2025). Compared with non-obese individuals, adults with obesity exhibit a 23–36% higher likelihood of developing depression and a 14–34% increased odds of major depressive disorder (Fulton et al., 2022). The harms caused by depression to overweight/obese individuals include impairment of personal well-being and quality of life, weakening their willingness to seek and adhere to treatment interventions, and the interaction between metabolic and emotional disorders can make despair, overeating and lack of exercise persist, thus forming a vicious cycle (Fulton et al., 2022).
To our knowledge, most studies assess depressive levels in overweight/obese individuals using depression scale scores or cutoff values. However, this “variable-centered” approach overlooks individual heterogeneity, resulting in findings that fail to accurately capture the actual depressive status of this population. Latent profile analysis (LPA) is a “person-centered” statistical method that identifies distinct latent subgroups within a population by analyzing individuals’ response patterns across multiple observed variables. Unlike traditional classification approaches that rely on fixed cutoffs (e.g., categorizing individuals as depressed or non-depressed), LPA offers a more nuanced understanding by grouping individuals who share similar symptom profiles (Chen et al., 2024). This approach provides more precise and objective classification results by capturing the underlying heterogeneity in population characteristics. LPA has been extensively utilized to identify depressive subtypes across diverse populations. For instance, Hou et al. identified three distinct depressive subtypes among older adults living alone using LPA (Hou and Zhang, 2023). Keins et al. (2021) demonstrated the existence of four clinically relevant depressive subtypes in patients with intracerebral hemorrhage through LPA. Nevertheless, the identification of depressive subgroups using LPA remains unexplored in overweight/obese populations.
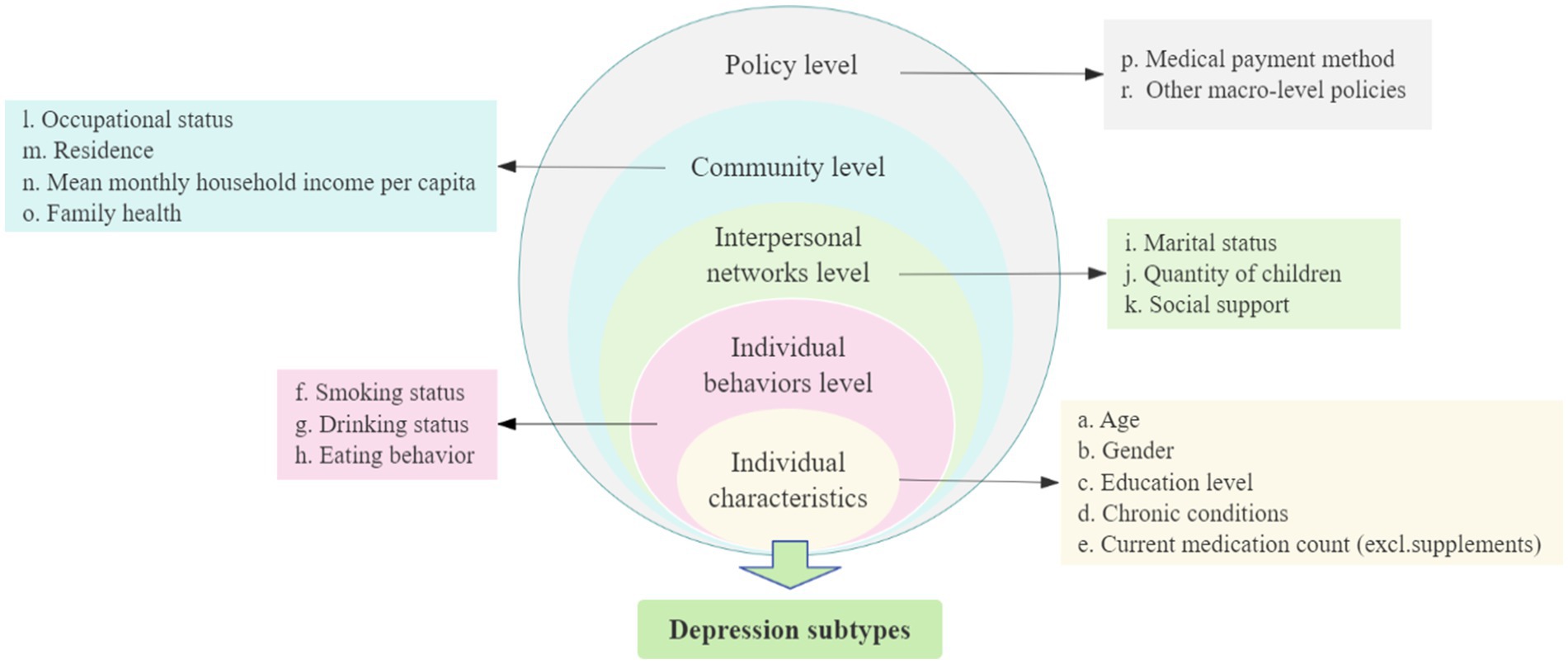
Additionally, previous studies on influencing factors of depression primarily focused on demographic characteristics and psychosocial factors, exhibiting a relatively narrow scope and lacking systematic exploration (Song et al., 2023; Bai et al., 2024). To address this limitation, the present study employs the social-ecological model (SEM) to identify depression-related factors in overweight/obese individuals (Figure 1). The SEM posits that individual health is jointly shaped by five interconnected levels: individual characteristics (intrinsic individual demographic, biological, and fundamental health characteristics), individual behaviors level (individual behavioral patterns and health-related behaviors), interpersonal networks level (social relationships and support systems), community level (living/working conditions and socioeconomic status), and public policy (local, state, and national laws and policies) (McLeroy et al., 1988). This multi-level framework facilitates comprehensive analysis of health determinants and supports the development of systematic health improvement strategies. The SEM has been widely used to examine health determinants across populations. For example, Jung et al. (2025) applied this model to analyze multilevel factors influencing future anxiety in Korean residents, while Huang and Tan (2024) employed a five-level socio-ecological framework to investigate cervical cancer screening participation among Singaporean women.
Therefore, this study aims to identify distinct depressive subtypes among overweight/obese individuals using LPA, and identify associated multilevel factors based on the SEM, to guide interventions that enhance mental health in this population.
2 Materials and methods
2.1 Survey design and participants
Our data were derived from a large-scale cross-sectional survey, the Psychology and Behavior Investigation of Chinese Residents in 2021 (PBICR 2021).1 This survey was conducted from July 10 to September 15, 2021. The project team surveyed using a multistage sampling method across 31 provinces/autonomous regions/municipalities in mainland China. Using the random number table method, 120 cities were selected, including the capital and two to six prefectural cities in each province/autonomous region. Based on data from the Seventh National Population Census of China (2021), quota sampling was applied to selected residents from these 120 cities (quota attributes: sex, age, and urban–rural distribution), ensuring the distributions of these variables in the final sample aligned with population characteristics.
According to the Guidelines for the diagnosis and treatment of obesity in China (National Health Commission of the People's Republic of China, Medical Administration Bureau, 2025) body mass index (BMI) remains the standard metric for defining overweight and obesity. BMI = weight (kg)/height (m)2, the criteria are: underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 24.0 kg/m2), overweight (24.0 kg/m2 ≤ BMI < 28.0 kg/m2), and obesity (BMI ≥ 28.0 kg/m2). Thus, individuals with BMI ≥ 24.0 kg/m2 were selected from the PBICR 2021 database as the study cohort, comprising 2,588 participants.
The inclusion criteria comprised the following: (a) participants held Chinese nationality; (b) aged ≥ 18 years; (c) BMI ≥ 24.0 kg/m2; (d) volunteered to participate in the research and completed a consent form; (e) could understand the content of each item in the questionnaire. The exclusion criteria included: (a) participants with unconsciousness or severe mental disorders; (b) those unwilling to cooperate or be involved in similar projects.
2.2 Research instruments
2.2.1 General information questionnaire
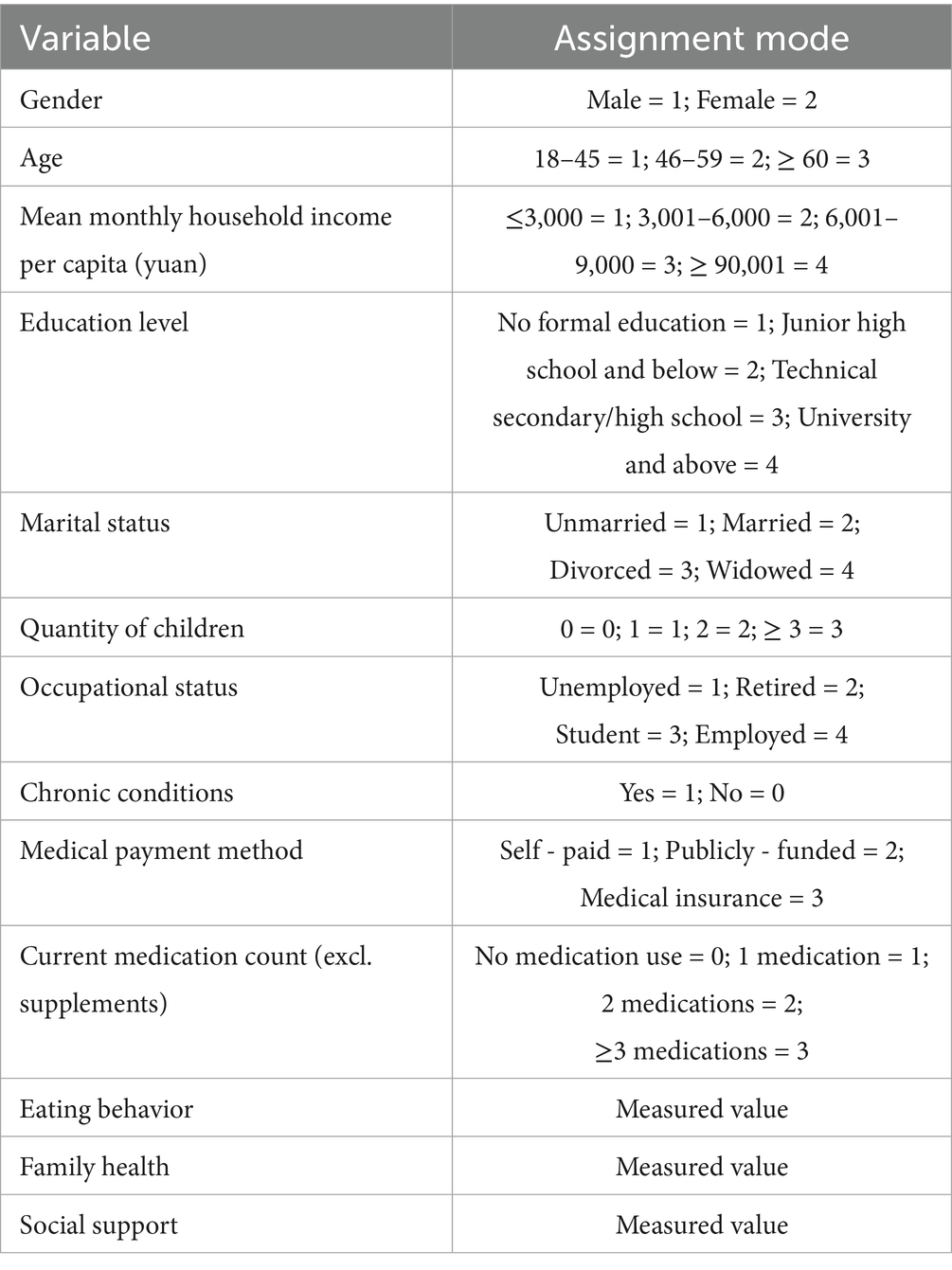
This included residence, gender, age, mean monthly household income per capita, education level, marital status, occupational status, chronic conditions, quantity of children, medical payment method, current medication count (excl. supplements), smoking status, and drinking status.
2.2.2 Patient health questionnaire-9 (PHQ-9)
The PHQ-9, developed by Spitzer et al. (1999), was used to measure individuals’ depression symptoms. This scale consists of 9 items, each scored 0–3 (0 = “not at all” to 3 = “nearly every day”), with a total score range of 0–27. The PHQ-9 score of ≥ 10 was used as the cut-off value for depression. In this study, Cronbach’s α coefficient for the PHQ-9 was 0.934.
2.2.3 Eating behavior scale-short form (EBS-SF)
The EBS-SF, simplified and revised by Tayama et al. (2017) based on the Sakata Eating Behavior Scale, was used to measure individuals’ eating behavior. This scale consists of 7 items assessing: eating rhythm abnormalities, satiety perception, eating habits, body constitution cognition, meal content, emotional eating, and motivation to eat. Each item is scored on a 4-point Likert scale (1 = “strongly disagree” to 4 = “strongly agree”). Total scores range from 7 to 28, with higher scores indicating poorer eating behaviors. In this study, Cronbach’s α coefficient for the EBS-SF was 0.857.
2.2.4 Family health scale-short form (FHS-SF)
The FHS-SF, developed by Crandall et al. (2020), was used to measure individuals’ family health. This scale consists of 10 items; each item is scored on a 5-point Likert scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). Items 6, 9, and 10 are scored inversely. We created binary variables for each of the ten FHS-SF items. Responses of 4 or higher (indicating agreement or strong agreement) were scored as 1 and responses lower than 4 (neutrality or disagreement with the statement) received a score of 0. Total scores range from 0 to 10, with higher scores indicating a higher level of family health. The Cronbach’s α coefficient for the FHS-SF in this study was 0.841.
2.2.5 Scale of perceived social support (SPSS)
The SPSS, developed by Zimet et al. (1990), was used to measure social support. The scale comprises 12 items across three subscales: Family Support, Friend Support, and Other Supports. Responses are rated on a 7-point Likert scale (1 = “strongly disagree” to 7 = “strongly agree”), with total scores ranging from 12 to 84. Higher total scores indicate better social support. The Cronbach’s α coefficient for the SPSS in this study was 0.957.
2.3 Statistical analysis
First, SPSS 24.0 was used to statistically describe the study population, non-normal continuous variables were represented by median (M) and quartile (IQR), and categorical variables were represented by frequency (N) and percentile (%). Second, the 9 items of PHQ-9 were used as observed variables for LPA by Mplus 8.3. Model selection was guided by the following criteria: (a) The Akaike information criterion (AIC), Bayesian information criterion (BIC), and sample size adjusted BIC (aBIC) gradually decrease with the increase of the number of categories, the smaller the value the better the model fit. (b) Lo–Mendell–Rubin likelihood ratio test (LMR) and Bootstrapped likelihood ratio test (BLRT) correspond to p-value < 0.05, which represents k is more appropriate than k-1 category. (c) Entropy represents the accuracy indicator to evaluate the category classification, ≥ 0.8 means the classification accuracy is > 90%. (d) Diagonal values > 0.7 in the classification probability matrix indicate reliable class assignment. In addition, to the above indicators, practical significance and interpretability are also to be considered. Third, on the basis of determining the optimal model. SPSS 24.0 was used to perform Chi-square or Kruskal-Wallis tests to compare the differences in sociodemographic variables, eating behavior, family health and social support between profiles, and statistically significant indicators were subjected to multinomial logistic regression to analyze the factors associated with depression in overweight/obese individuals when different subgroups were compared. In all analyses, a 2-tailed p < 0.05 was considered statistically significant.
3 Results
3.1 Common method bias test
Common method bias was assessed using two distinct strategies in this study (Podsakoff et al., 2003). (a) The results of the Harman’s single-factor test revealed that there were five factors with eigenvalues exceeding 1, and the explanatory power of the first factor was 30.18%, which was below the critical threshold of 40%. The results indicated no substantial common method bias. (b) We employed the unmeasured latent method factor (ULMF) approach to assess common method bias. All observed indicators were loaded onto both theoretical constructs and a latent method factor in the CFA model. Results showed that model fit indices (CFI = 0.885, RMSEA = 0.070, SRMR = 0.071) remained unchanged after adding the method factor, indicating no significant improvement in model fit. This suggests that common method bias was not substantial in our study.
3.2 Statistical description
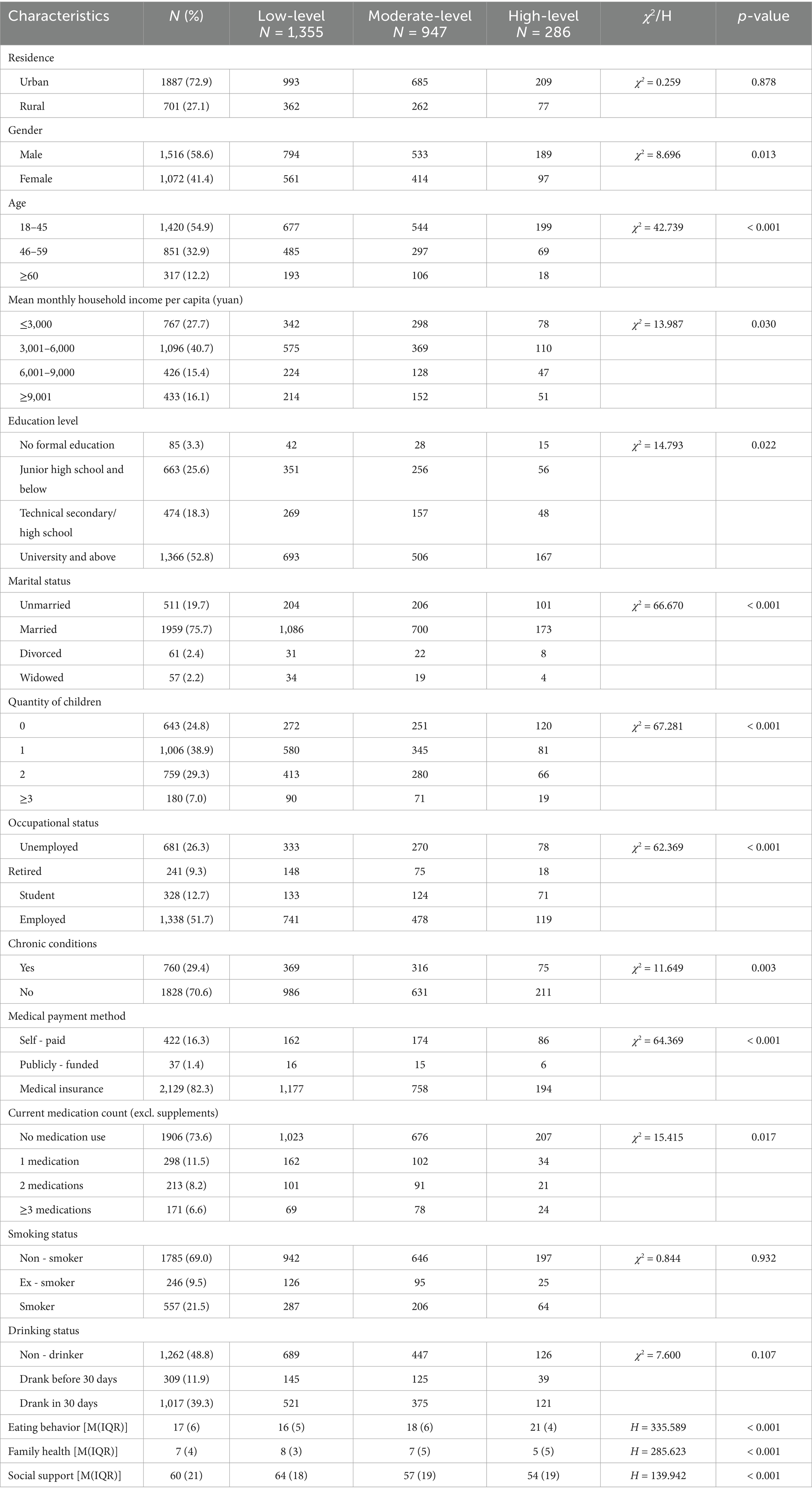
The study included 2,588 overweight/obese participants (1,516 males [58.6%] and 1,072 females [41.4%]), with 1,887 (72.9%) urban and 701 (27.1%) rural residents. The majority were aged 18–45 years (54.9%), and most families reported a mean monthly household income per capita of 3,001–6,000 yuan (40.7%). The continuous variables in this study were expressed as M (IQR): eating behavior score = 17 (6), family health score = 38 (10), and social support score = 60 (22). As shown in Table 1.
3.3 Latent profile analysis of depression in overweight/obese individuals
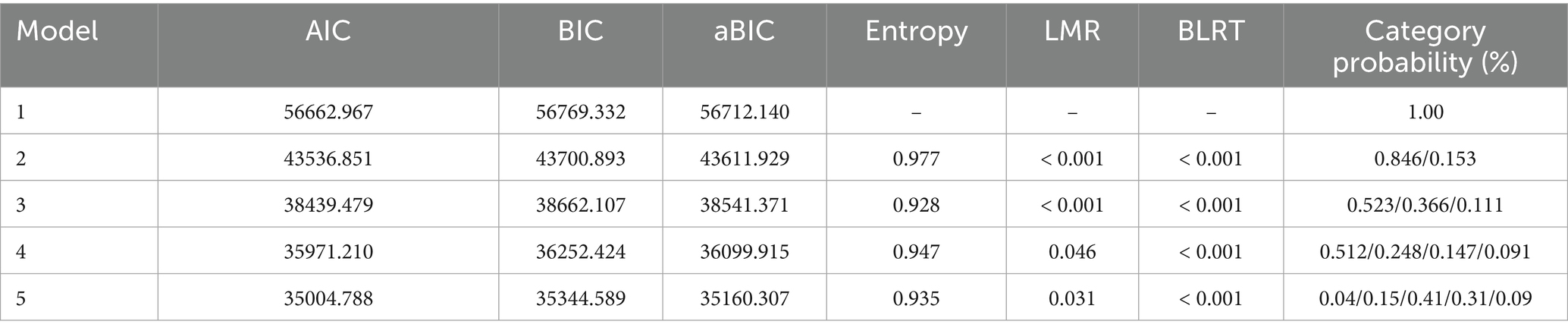
Using the 9 items of PHQ-9 as explicit variables, the optimal number of potential categories was explored, fitting 1 to 5 models, with fit indices presented in Table 2. As the number of categories increased, AIC, BIC, and aBIC values showed continuous decreases, reaching minima in the 5-category model. Entropy values for categories 2–5 all exceeded 0.9, while both LMR and BLRT tests yielded p-values < 0.05.
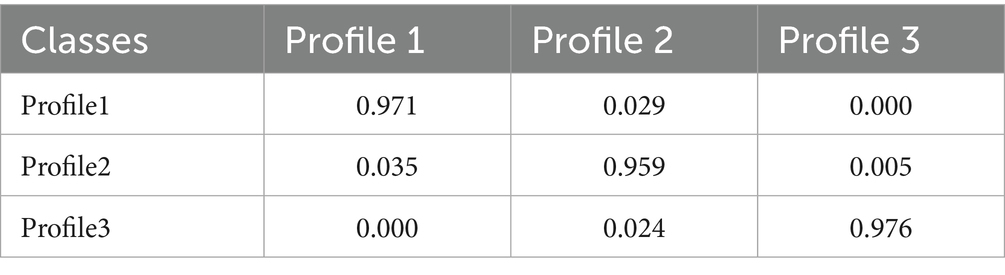
Considering the practical significance of measurement, due to the relatively low proportion of people in certain categories of profile 4 and profile 5 models, and more analogies may disperse effective information, so the models of these two potential categories were not selected. In all categories, profile 2 model had the highest AIC, BIC and aBIC values. Combined with the model comparison results, classification accuracy and practical significance, this study considers the model with three potential categories to be the optimal model for depression in overweight/obese individuals. Additionally, Table 3 showed the attribution probability matrix for the 3 potential profiles. The average probability of attribution of each class to its corresponding potential profile ranged from 95.9 to 97.6% (all > 95%), indicating that the results of the model for the three potential profiles in this study were plausible.
According to our study findings, we observed three distinct profiles of depression among the participants (Figure 2). The first group, comprising 1,355 individuals (52.3%), exhibited the lowest level of depression and was classified as the “low-level depression.” The second group, consisting of 947 individuals (36.6%), demonstrated moderate depression levels and was labeled the “moderate-level depression.” The third group, including 286 individuals (11.1%), displayed the most severe depression symptoms and was designated as the “high-level depression.” These findings highlight the heterogeneous nature of depression in overweight/obese individuals and emphasize the need for tailored interventions addressing each subgroup’s unique psychological characteristics.
3.4 Differences among latent depression profiles
Results from the Chi-square and Kruskal-Wallis tests revealed statistically significant differences (all p < 0.05) among the three subgroups in the following variables: gender, age, mean monthly household income per capita, education level, marital status, number of children, occupational status, chronic conditions, medical payment method, current medication count (excl. supplements), eating behavior, family health, and social support. As shown in Table 1.
3.5 Multivariate analysis of potential profiles of depression in overweight/obese individuals
“Low–level depression” was referenced in this study, with depression subtypes as the dependent variable (low- = 1, moderate- = 2, and high- level depression = 3), demographic and continuous variables that were statistically significant in the univariate analysis as independent variables (variable assignments are shown in Table 4), and correlates explored through multinomial logistic regression. Compared to the low-level group, high-level depression was significantly associated with age (18–45 years), current medication count (≥ 3, excl. supplements), out-of-pocket medical expenditures, higher abnormal eating behavior scores, and lower family health and social support scores (all p < 0.05). Similarly, moderate-level depression showed significant associations with female, age (18–45 years), having chronic conditions, current medication count (≥ 3, excl. supplements), out-of-pocket medical expenditures, higher abnormal eating behavior scores, and lower family health and social support scores (all p < 0.05).
4 Discussion
4.1 Potential profile characteristics of depression in overweight/obese individuals
We identified three distinct depressive subtypes in overweight/obese individuals, consistent with Kong and Zhang (2023): low-, moderate-, and high-level depression groups, highlighting substantial heterogeneity in depressive phenotypes. The low-level depression group (52.3%) exhibited lower scores across all scale items compared to the other two groups, yet showed significantly higher mean scores for item 3 (‘difficulty falling asleep, waking up at night, or excessive sleep’) and item 4 (‘feeling tired or lacking energy’) relative to other items within this subgroup. This suggests that despite overall low-level depression, these individuals experience specific sleep disturbances and fatigue—likely attributable to higher prevalence of sleep apnea and other sleep disorders in overweight/obese individuals (Rodrigues et al., 2021; Chaput et al., 2023), which impair sleep quality and contribute to tiredness. Traditional binary classification (depressed vs. non-depressed) based on scale cutoffs would overlook these individuals, whereas LPA reveals that even those with low-level depression require targeted interventions, particularly for sleep and fatigue management, to prevent symptom progression (Table 5).
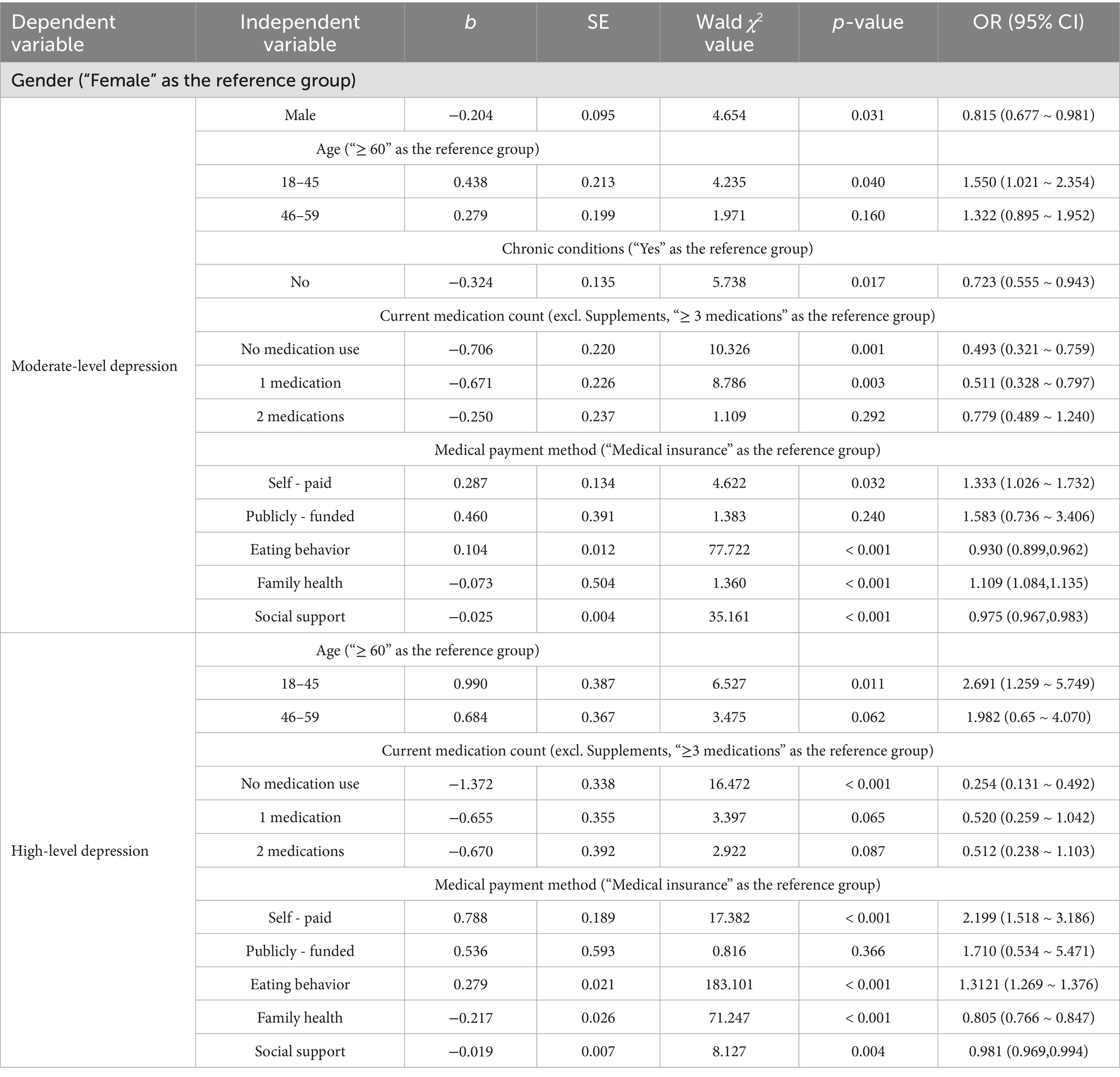
Table 5. Multivariate logistic regression analysis of different potential factors in overweight/obese individuals.
The moderate-level depression group accounted for 36.6% of the sample, with significantly higher mean scores on item 3 (“difficulty falling asleep, nighttime awakening, or excessive sleep”) and item 4 (“feeling tired or lacking energy”) than other items. This pattern suggests that overweight/obese individuals in the moderate-depression subgroup also experience pronounced sleep disturbances and fatigue. Compared to the low-level depression group, all scale items in the moderate group showed higher mean scores (albeit lower than the high-level group), suggesting substantial instability—these individuals may regress to low-level depression or progress to high-level depression. Consequently, timely identification and targeted interventions become crucial to prevent transition to more severe depression.
The high-level depression group comprised 11.1% of the sample, showing the most severe depressive symptoms among the three groups. Luppino et al. (2010) reported a bidirectional association between overweight and clinical depression, with a stronger correlation observed in obesity, potentially attributable to increased social discrimination, stigmatization, and body image dissatisfaction experienced by overweight/obese individuals. Furthermore, poor dietary habits and metabolic disorders (including chronic inflammation and insulin resistance) are strongly linked to depressive severity in this population (Miller and Raison, 2016; Chen et al., 2021). Consequently, this subgroup represents the highest-risk category among the three phenotypes, requiring intensive interventions to understand their psychological state, alleviate emotional distress, and enhance quality of life.
4.2 Associated factors of potential profiles of depression in overweight/obese individuals
4.2.1 Individual characteristics
4.2.1.1 Gender
In our study, female participants demonstrated a significantly higher likelihood of being classified into the moderate-level depression group. This finding aligns with existing literature, as Johann and Ehlert (2022) documented that women exhibit approximately twice the risk of developing depression compared to men throughout the lifespan. Further supporting this observation, Tang and Zhang (2022) demonstrated that females generally display greater sensitivity to social evaluation and stronger need for social affirmation than males, coupled with reduced resilience to negative feedback. These psychological characteristics may explain why overweight/obese women tend to experience heightened body image concerns and greater distress in response to negative social evaluations, consequently contributing to their elevated depressive symptoms.
4.2.1.2 Chronic conditions
In this study, individuals with chronic conditions were more likely to exhibit moderate-level depression. This finding is consistent with previous study (Liu et al., 2023). Zhou et al. (2023) indicated that chronic conditions, characterized by prolonged incurability and necessitating lifelong treatment, impose not only considerable psychological and physiological burdens on patients but also substantial economic strains and productivity losses for families, thereby increasing susceptibility to depression. For overweight/obese individuals with chronic conditions, the dual challenge of managing both body weight and chronic illnesses likely intensifies physical and mental stress, consequently elevating depressive symptoms.
4.2.1.3 Age
This study found that overweight/obese individuals aged 18–45 demonstrated elevated depressive symptoms. As reported by Strand et al. (2021), BMI serves as the strongest predictor of body image disparities in adults. This age group, predominantly comprising university students and working professionals, faces heightened career and familial demands, resulting in increased self-image concerns (Aruna et al., 2024). Overweight/obesity can induce body dissatisfaction and weight-related stigma, which negatively impact self-esteem and psychological well-being (Timkova et al., 2024). Furthermore, these individuals frequently experience weight-based discrimination, teasing, and bullying. Such prejudice, prevalent across multiple social domains including workplaces, educational settings, and interpersonal relationships, significantly contributes to various psychological comorbidities, particularly depression, anxiety, and social isolation (Puhl and King, 2013).
4.2.1.4 Current medication count (excl. supplements)
This study indicated that overweight/obese individuals prescribed ≥3 medications exhibited more severe depressive symptoms. This observation aligns with previous research. Assari and Bazargan (2019) reported that polypharmacy is associated with elevated psychological distress, while Kyler et al. (2023) showed that nearly half of obese individuals receive multiple medication regimens. This phenomenon results from the high prevalence of obesity-related comorbidities (e.g., diabetes, dyslipidemia, hypertension and metabolic syndrome) (Ramón-Arbués et al., 2019), which necessitate polypharmacy. The increased number of medications, combined with side effects, drug interactions, and financial burdens—can exacerbate psychological stress and predispose to depression (Assari et al., 2019).
4.2.2 Individual behaviors level
4.2.2.1 Eating behavior
We found that overweight/obese individuals with abnormal eating behaviors had more severe depressive symptoms, consistent with previous studies (Masheb and Grilo, 2006). Emotional eating, binge eating, and food addiction are common coping ways for many overweight/obese people to cope with negative emotions such as stress and anxiety (Isnard et al., 2003; Esen Öksüzoğlu et al., 2024). Fulton et al. (2022) demonstrated that the mental consequences of obesity stem from poor diet, lack of exercise, and visceral fat accumulation, and the resulting metabolic and vascular dysfunctions, including inflammation, insulin and leptin resistance, and hypertension, have become major risks for the development of depression and anxiety. For example, high-fat and high-sugar diets can cause chronic low-grade inflammation, and proinflammatory cytokines (TNF-α, IL-6) are closely related to the occurrence of depression (Miller and Raison, 2016). Dietary modification and physical activity represent fundamental strategies for establishing healthy eating habits in overweight/obese populations. Empirical evidence suggests the Mediterranean diet is particularly suitable for this demographic (Khandelwal, 2020). Furthermore, yoga practice, aerobic exercise, and regular sleep patterns have been shown to enhance stress management, thereby facilitating healthier dietary behaviors (Watts et al., 2018; Khandelwal, 2020). Regarding psychological support, Hanson et al. (2019) demonstrated that mindfulness-based eating interventions effectively improve maladaptive eating behaviors in obese individuals.
4.2.3 Interpersonal networks level
4.2.3.1 Social support
Our data demonstrated that higher social support was associated with lower depressive symptoms in overweight/obese individuals, consistent with the findings of Timkova et al. (2024). Social support, as a critical external resource available to individuals, plays a positive role in enhancing health-promoting behaviors, improving self-worth, and reducing anxiety and depression (Langford et al., 1997). For overweight/obese individuals, establishing specialized health management institutions, regular supervision and follow-up by healthcare professionals, and creating healthy workplaces can help them feel social acceptance and support. Additionally, support from peers and family is also important social support resources. Adequate social support can not only facilitate active weight management but also enhance their ability to cope with difficulties and negative emotions.
4.2.4 Community level
4.2.4.1 Family health
We found that better family health was associated with less severe depressive symptoms in overweight/obese individuals. Hao et al. (2023) reported that decreased family health functioning directly influences individual depressive symptoms. Healthy family social and emotional processes can promote health resilience and are associated with better mental health, physical health, and overall well-being (e.g., reduced depression, hypertension and chronic pain) (Chew et al., 2018). Good family health implies adequate internal emotional communication among family members, accessible health resources, and external social support, and emphasizes the adoption of healthy lifestyles to promote individual physical and mental health (Mei et al., 2022). Thus, optimal family health not only helps overweight/obese individuals adopt healthy eating habits and maintains regular routines but also enables effective coping with negative emotions and protects psychological well-being when facing stigma or stress. These findings highlight the importance of addressing family health functioning in overweight/obese individuals, suggesting that promoting family health is a key strategy to improve their mental health outcomes.
4.2.5 Policy level
4.2.5.1 Medical payment method
The results demonstrated that overweight/obese individuals with out-of-pocket medical expenses exhibited more severe depressive symptoms. Studies have shown that negative societal stereotypes about obesity lead to unfair treatment of obese individuals in job seeking and salary levels, which may limit their economic income (Judge and Cable, 2011; Campos-Vazquez and Gonzalez, 2020). Out-of-pocket medical expenses further exacerbate their financial strain and psychological distress, thus exacerbating depressive symptoms (Zhou et al., 2023). To address this issue, public health policies should prioritize implementing medical expense subsidies for overweight/obese populations while enforcing anti-discrimination legislation in workplaces to ensure equitable employment opportunities and income levels.
4.2.5.2 Other macro-level policies
It is noteworthy that the “Healthy Diet Initiative” and “National Fitness Program” advocated in the “Healthy China 2030” action plan,2 along with the “whole-population, life-cycle coverage and precision weight management” proposed in the “National Weight Management Year” implementation plan,3 collectively demonstrate China’s policy-level efforts toward scientific weight management and chronic disease control. These initiatives provide a distinctive Chinese public health solution for advancing the United Nations Sustainable Development Goal 3 (SDG-3) - “Ensure healthy lives and promote well-being for all at all ages”.
4.2.5.3 Strengths and limitations
In this study, First, employing LPA, the study identified distinct depression subtypes among overweight/obese individuals. Second, grounded in the SEM, the study systematically explores multi-level associated factors of depression subtypes, transcending traditional single-dimensional analyses. Third, the nationwide cross-sectional study design incorporated a large, nationally representative sample of 2,588 Chinese participants, enhancing the generalizability of the findings. Collectively, this research provides evidence-based insights for formulating targeted multi-level interventions among overweight/obese individuals.
Several potential limitations of this study should be acknowledged. Firstly, due to the cross-sectional study design, we cannot infer causal implications. Secondly, as a result of the self-reported information and the self-assessed scales in the study, reporting bias may exist. Finally, although the study examined multiple factors related to depression subtypes among overweight/obese individuals within the SEM framework, only one policy-environmental factor (medical payment method) was considered in this study. Future studies should enrich the policy-environmental dimension of the model by incorporating specific contextual variables, such as regional mental health policies or urban infrastructure.
5 Conclusion
Depression in overweight/obese individuals was categorized into three subtypes: low-, moderate-, and high-level depression groups. An in-depth understanding of these factors across five SEM levels helped formulate more targeted and multidimensional intervention strategies. Significant differences were observed across these groups in age, gender, chronic conditions, medication use, eating behavior, family health, social support, and medical payment method. Therefore, interventions for high-risk populations should not only address weight management and physical health improvement but also prioritize mental health.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The studies involving humans were approved by Jinan University Ethics Committee (Approval No. JNUKY-2021-018). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
XY: Conceptualization, Writing – review & editing, Writing – original draft. MC: Software, Writing – review & editing, Data curation. XL: Writing – review & editing, Supervision. LW: Methodology, Writing – review & editing. YW: Writing – review & editing, Methodology. YZ: Writing – review & editing. SM: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors declare that this study received financial support from the 2024 Newly Recruited Master’s Degree Training Program at the General Hospital of Ningxia Medical University.
Acknowledgments
We sincerely appreciate the considerable patience of all respondents during questionnaire completion and gratefully acknowledge all individuals who supported this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^https://www.x-mol.com/groups/pbicr
2. ^https://www.gov.cn/xinwen/2019-07/15/content_5409694.htm
3. ^https://www.gov.cn/zhengce/zhengceku/202406/content_6959543.htm
References
Aruna, R., Muruganandam, P., and Niveatha, S. (2024). Eating habit, body image, and gender - is there any association? - a comparative study among medical students from southern India. J. Educ. Health Promot. 13:326. doi: 10.4103/jehp.jehp_72_24
Assari, S., and Bazargan, M. (2019). Polypharmacy and psychological distress may be associated in African American adults. Pharmacy (Basel). 7. doi: 10.3390/pharmacy7010014
Assari, S., Wisseh, C., and Bazargan, M. (2019). Obesity and polypharmacy among African American older adults: gender as the moderator and multimorbidity as the mediator. Int. J. Environ. Res. Public Health 16. doi: 10.3390/ijerph16122181
Bai, S., Wang, J., Liu, J., Miao, Y., Zhang, A., and Zhang, Z. (2024). Analysis of depression incidence and influence factors among middle-aged and elderly diabetic patients in China: based on CHARLS data. BMC Psychiatry 24:146. doi: 10.1186/s12888-023-05473-6
Campos-Vazquez, R. M., and Gonzalez, E. (2020). Obesity and hiring discrimination. Econ. Hum. Biol. 37:100850. doi: 10.1016/j.ehb.2020.100850
Chaput, J. P., McHill, A. W., Cox, R. C., Broussard, J. L., Dutil, C., da Costa, B. G. G., et al. (2023). The role of insufficient sleep and circadian misalignment in obesity. Nat. Rev. Endocrinol. 19, 82–97. doi: 10.1038/s41574-022-00747-7
Chen, G. Q., Peng, C. L., Lian, Y., Wang, B. W., Chen, P. Y., and Wang, G. P. (2021). Association between dietary inflammatory index and mental health: a systematic review and dose-response Meta-analysis. Front. Nutr. 8:662357. doi: 10.3389/fnut.2021.662357
Chen, T., Su, L., Yu, J., Zhao, H., Xiao, H., and Wang, Y. (2024). Latent profile analysis of anticipatory grief in family caregivers of patients with chronic heart failure and its influencing factors. BMC Palliat. Care 23:291. doi: 10.1186/s12904-024-01621-1
Chew, J., Carpenter, J., and Haase, A. M. (2018). Young people's experiences of living with epilepsy: the significance of family resilience. Soc. Work Health Care 57, 332–354. doi: 10.1080/00981389.2018.1443195
Collaborators GBD 2021 Adult BMI (2025). Global, regional, and national prevalence of adult overweight and obesity, 1990-2021, with forecasts to 2050: a forecasting study for the global burden of disease study 2021. Lancet 405, 813–838. doi: 10.1016/s0140-6736(25)00355-1
Crandall, A., Weiss-Laxer, N. S., Broadbent, E., Holmes, E. K., Magnusson, B. M., Okano, L., et al. (2020). The family health scale: reliability and validity of a short- and long-form. Front. Public Health 8:587125. doi: 10.3389/fpubh.2020.587125
Cui, J., Sun, X., Li, X., Ke, M., Sun, J., Yasmeen, N., et al. (2018). Association between different indicators of obesity and depression in adults in Qingdao, China: a cross-sectional study. Front Endocrinol (Lausanne). 9:549. doi: 10.3389/fendo.2018.00549
Esen Öksüzoğlu, M., Akdemir, D., Akgül, S., and Özdemir, P. (2024). Predictors of emotional eating behaviors in adolescents with overweight and obesity. Arch. Pediatr. 31, 527–532. doi: 10.1016/j.arcped.2024.07.007
Fulton, S., Décarie-Spain, L., Fioramonti, X., Guiard, B., and Nakajima, S. (2022). The menace of obesity to depression and anxiety prevalence. Trends Endocrinol. Metab. 33, 18–35. doi: 10.1016/j.tem.2021.10.005
Gerardo, G., Peterson, N., Goodpaster, K., and Heinberg, L. (2025). Depression and obesity. Curr. Obes. Rep. 14:5. doi: 10.1007/s13679-024-00603-x
Hanson, P., Shuttlewood, E., Halder, L., Shah, N., Lam, F. T., Menon, V., et al. (2019). Application of mindfulness in a tier 3 obesity service improves eating behavior and facilitates successful weight loss. J. Clin. Endocrinol. Metab. 104, 793–800. doi: 10.1210/jc.2018-00578
Hao, R., Jin, H., Zuo, J., Wu, Y., Sun, X., and Hu, J. (2023). The multiple mediating effect of family health and perceived social support on depressive symptoms in older adults: a cross-sectional national survey in China. J. Affect. Disord. 327, 348–354. doi: 10.1016/j.jad.2023.01.097
Hou, B., and Zhang, H. (2023). Latent profile analysis of depression among older adults living alone in China. J. Affect. Disord. 325, 378–385. doi: 10.1016/j.jad.2022.12.154
Huang, Q., and Tan, L. Y. (2024). Exploring factors influencing cervical Cancer screening participation among Singaporean women: a social ecological approach. Cancers (Basel) 16. doi: 10.3390/cancers16203475
Isnard, P., Michel, G., Frelut, M. L., Vila, G., Falissard, B., Naja, W., et al. (2003). Binge eating and psychopathology in severely obese adolescents. Int. J. Eat. Disord. 34, 235–243. doi: 10.1002/eat.10178
Johann, A., and Ehlert, U. (2022). Similarities and differences between postpartum depression and depression at other stages of female life: a systematic review. J. Psychosom. Obstet. Gynaecol. 43, 340–348. doi: 10.1080/0167482x.2021.1962276
Judge, T. A., and Cable, D. M. (2011). When it comes to pay, do the thin win? The effect of weight on pay for men and women. J. Appl. Psychol. 96, 95–112. doi: 10.1037/a0020860
Jung, H. W., Choi, M., and Lee, K. S. (2025). Determinants of future anxiety across individual, house-hold, and regional levels in South Korea using a social ecological model. Sci. Rep. 15:3428. doi: 10.1038/s41598-025-87387-9
Keins, S., Abramson, J. R., Castello, J. P., Pasi, M., Charidimou, A., Kourkoulis, C., et al. (2021). Latent profile analysis of cognitive decline and depressive symptoms after intracerebral hemorrhage. BMC Neurol. 21:481. doi: 10.1186/s12883-021-02508-x
Khandelwal, S. (2020). Obesity in midlife: lifestyle and dietary strategies. Climacteric 23, 140–147. doi: 10.1080/13697137.2019.1660638
Kong, L., and Zhang, H. (2023). Latent profile analysis of depression in non-hospitalized elderly patients with hypertension and its influencing factors. J. Affect. Disord. 341, 67–76. doi: 10.1016/j.jad.2023.08.114
Kyler, K. E., Hall, M., Antoon, J. W., Goldman, J., Grijalva, C. G., Shah, S. S., et al. (2023). Polypharmacy among medicaid-insured children with and without documented obesity. Pharmacotherapy 43, 588–595. doi: 10.1002/phar.2755
Langford, C. P., Bowsher, J., Maloney, J. P., and Lillis, P. P. (1997). Social support: a conceptual analysis. J. Adv. Nurs. 25, 95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x
Latzer, Y., and Stein, D. (2013). A review of the psychological and familial perspectives of childhood obesity. J. Eat. Disord. 1:7. doi: 10.1186/2050-2974-1-7
Liu, R., He, W. B., Cao, L. J., Wang, L., and Wei, Q. (2023). Association between chronic disease and depression among older adults in China: the moderating role of social participation. Public Health 221, 73–78. doi: 10.1016/j.puhe.2023.06.003
Luppino, F. S., de Wit, L. M., Bouvy, P. F., Stijnen, T., Cuijpers, P., Penninx, B. W., et al. (2010). Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatry 67, 220–229. doi: 10.1001/archgenpsychiatry.2010.2
Masheb, R. M., and Grilo, C. M. (2006). Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. Int. J. Eat. Disord. 39, 141–146. doi: 10.1002/eat.20221
McLeroy, K. R., Bibeau, D., Steckler, A., and Glanz, K. (1988). An ecological perspective on health promotion programs. Health Educ. Q. 15, 351–377. doi: 10.1177/109019818801500401
Mei, D., Deng, Y., Li, Q., Lin, Z., Jiang, H., Zhang, J., et al. (2022). Current status and influencing factors of eating behavior in residents at the age of 18~60: a cross-sectional study in China. Nutrients 14. doi: 10.3390/nu14132585
Miller, A. H., and Raison, C. L. (2016). The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 16, 22–34. doi: 10.1038/nri.2015.5
National Health Commission of the People's Republic of China, Medical Administration Bureau (2025). Guidelines for the diagnosis and treatment of obesity in China (2024 edition). Med. J. PUMCH. 16, 90–108.
Park, M., Jaiswal, V., Kim, K., Chun, J., Lee, M. J., Shin, J. H., et al. (2022). Mulberry leaf supplements effecting anti-inflammatory genes and improving obesity in elderly overweight dogs. Int. J. Mol. Sci. 23. doi: 10.3390/ijms232315215
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., and Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 88, 879–903. doi: 10.1037/0021-9010.88.5.879
Puhl, R. M., and King, K. M. (2013). Weight discrimination and bullying. Best Pract. Res. Clin. Endocrinol. Metab. 27, 117–127. doi: 10.1016/j.beem.2012.12.002
Ramón-Arbués, E., Martínez-Abadía, B., Gracia-Tabuenca, T., Yuste-Gran, C., Pellicer-García, B., Juárez-Vela, R., et al. (2019). Prevalence of overweight/obesity and its association with diabetes, hypertension, dyslipidemia and metabolic syndrome: a cross-sectional study of a sample of workers in Aragón, Spain. Nutr. Hosp. 36, 51–59. doi: 10.20960/nh.1980
Rodrigues, G. D., Fiorelli, E. M., Furlan, L., Montano, N., and Tobaldini, E. (2021). Obesity and sleep disturbances: the "chicken or the egg" question. Eur. J. Intern. Med. 92, 11–16. doi: 10.1016/j.ejim.2021.04.017
Song, C., Yao, L., Chen, H., Song, Y., and Liu, L. (2023). Prevalence and factors influencing depression among empty nesters in China: a meta-analysis. BMC Geriatr. 23:333. doi: 10.1186/s12877-023-04064-0
Spitzer, R. L., Kroenke, K., and Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 282, 1737–1744. doi: 10.1001/jama.282.18.1737
Strand, M., Fredlund, P., Boldemann, C., and Lager, A. (2021). Body image perception, smoking, alcohol use, indoor tanning, and disordered eating in young and middle-aged adults: findings from a large population-based Swedish study. BMC Public Health 21:128. doi: 10.1186/s12889-021-10158-4
Tang, J., and Zhang, T. (2022). Causes of the male-female ratio of depression based on the psychosocial factors. Front. Psychol. 13:1052702. doi: 10.3389/fpsyg.2022.1052702
Tayama, J., Ogawa, S., Takeoka, A., Kobayashi, M., and Shirabe, S. (2017). Item response theory-based validation of a short form of the eating behavior scale for Japanese adults. Medicine (Baltimore) 96:e8334. doi: 10.1097/md.0000000000008334
Timkova, V., Mikula, P., and Nagyova, I. (2024). Psychosocial distress in people with overweight and obesity: the role of weight stigma and social support. Front. Psychol. 15:1474844. doi: 10.3389/fpsyg.2024.1474844
Watts, A. W., Rydell, S. A., Eisenberg, M. E., Laska, M. N., and Neumark-Sztainer, D. (2018). Yoga's potential for promoting healthy eating and physical activity behaviors among young adults: a mixed-methods study. Int. J. Behav. Nutr. Phys. Act. 15:42. doi: 10.1186/s12966-018-0674-4
Zhou, P., Wang, S., Yan, Y., Lu, Q., Pei, J., Guo, W., et al. (2023). Association between chronic diseases and depression in the middle-aged and older adult Chinese population-a seven-year follow-up study based on CHARLS. Front. Public Health 11:1176669. doi: 10.3389/fpubh.2023.1176669
Keywords: body mass index, depression, depressive subtypes, multilevel factors, mental health
Citation: Yang X, Chen M, Liu X, Wang L, Wang Y, Zheng Y and Ma S (2025) Latent depressive profiles and associated factors among overweight/obese individuals based on the socio-ecological model: a cross-sectional national survey in China. Front. Psychol. 16:1644701. doi: 10.3389/fpsyg.2025.1644701
Edited by:
Yibo Wu, Zhejiang University, ChinaReviewed by:
Romeu Paulo Martins Silva, Federal University of Acre, BrazilCristianne Confessor Castilho Lopes, Universidade da Região de Joinville, Brazil
Chiradeep Sarkar, University of Mumbai, India
Copyright © 2025 Yang, Chen, Liu, Wang, Wang, Zheng and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohui Liu, bHhobm11QHNpbmEuY29t
 Xiaoping Yang
Xiaoping Yang Miaomiao Chen2
Miaomiao Chen2