- 1Norwegian Center for Violence and Traumatic Stress Studies, Oslo, Norway
- 2Department of Psychology, University of Oslo, Oslo, Norway
- 3Department of Psychology, Oslo New University College, Oslo, Norway
- 4National Centre for Emergency Primary Health Care, NORCE Research AS, Bergen, Norway
- 5Centre for Child and Adolescent Mental Health, Eastern and Southern Norway, Oslo, Norway
- 6Department of Criminology, Law, and Justice, University of Illinois, Chicago, Chicago, IL, United States
Introduction: It is well-known that social support is related to mental health following sexual assault (SA). Recent research suggests that social reactions to disclosure may also affect mental health; however, few studies have accounted for general social support, and most have been conducted many years after the assault. This study aimed to examine whether social reactions are uniquely linked to mental health when adjusting for perceived social support in recent victims of SA.
Methods: In this cross-sectional study, participants were recruited from Sexual Assault Centers (SACs) and through social media. The sample comprised 173 female participants (mean age = 26 years, SD = 8.6) who had experienced a SA within the last 6 months and had disclosed the SA to someone. We used linear regression analyses to assess associations between social reactions to disclosure, social support, and post-traumatic stress reactions (PTSR) and anxiety/depression symptoms.
Results: Although positive social reactions to disclosure were most common, negative social reactions were highly prevalent even in this early phase after SA. Negative social reactions of the Unsupportive acknowledgment type were significantly associated with more PTSR (b = 0.36, 95% CI = 0.14, 0.57), while perceived social support was significantly associated with fewer symptoms of anxiety/depression (b = −0.20, 95% CI = −0.32, −0.08).
Conclusions: Social reactions and social support were differentially associated with PTSR and anxiety/depression symptoms, indicating that certain aspects of social relationships may play different roles in the recovery process. Our results call for early interventions following SA to reduce negative reactions to disclosure and facilitate the provision of positive social support to victims.
Introduction
Sexual assault (SA) is a broad term that includes forcible, intoxicated, and attempted rape, as well as other sexual activity without consent (Tjaden and Thoennes, 2000). In the early aftermath of SA, most victims experience a high level of distress (Steenkamp et al., 2012). In contrast to many other types of traumas (Bonanno, 2005), resilience or rapid recovery does not appear to be common in SA victims. On the contrary, in women, rape is the type of trauma that carries the highest risk of post-traumatic stress disorder (PTSD) (Kessler et al., 2013). A recent meta-analysis indicated that 42% met the criteria for PTSD 1 year after the assault (Dworkin et al., 2023). The consequences of SA seem to affect mental health broadly, including an increased risk of depression and anxiety (Dworkin et al., 2017).
Perceived (positive) social support is closely related to mental health following traumatic events (Thoits, 2011). Social support has traditionally been conceptualized as a buffer that protects the individual from negative mental health symptom development in the face of adversity (Cohen and Wills, 1985), although longitudinal studies indicate a reciprocal relationship between PTSD symptoms and perceived support (Wang et al., 2021). Perceived support denotes the perception that emotional, cognitive, and instrumental support would be available if required (Joseph, 1999; Santini et al., 2015). Thus, through positive interaction with other people, individuals in distress may be better able to regulate emotions, achieve control over negative thought patterns, and make adaptive plans for problem solving or help seeking. Additionally, mental health symptoms may interfere with social skills, which can result in social isolation or social rejection (Kaniasty and Norris, 2008).
Most studies on mental health following traumatic events only measure the positive aspects of social relationships, such as perceived social support, even though researchers have long argued that negative aspects of social encounters also need attention. Negative and positive aspects of social interaction may be viewed as separate constructs, and negative encounters may be more harmful than positive encounters are helpful (Lincoln, 2000). Several concepts have been developed to capture such negative encounters, such as barriers to social support, social constraints, lack of support, and feeling let-down (Lepore and Ituarte, 1999; Andrews et al., 2003; Thoresen et al., 2014). One promising area of research investigates social reactions to victim disclosure of interpersonal violence, and how such reactions can affect mental health.
The concept of social reactions from other people post-trauma was developed within the field of interpersonal traumas such as SA and interpersonal violence, likely due to the social stigma attached to these experiences. The idea that unsupportive reactions from other people may cause harm to SA victims is not new. For example, Davis and colleagues argued that people may feel threatened or helpless when confronted with rape victims in acute distress, resulting in unsupportive behavior such as withdrawal, criticism, or inappropriate help (Davis et al., 1991). Reactions such as withdrawal or devaluation can signal a threat of exclusion, or the perception of being undesirable to others. Such social threats are likely to induce shame (Gilbert, 2000), loneliness (Thoresen et al., 2018), and withdrawal (Birkeland et al., 2020), and thereby contribute to mental health problems.
Research in this area was spurred by the development of the Social Reactions Questionnaire (Ullman, 2000), a standardized measure of social reactions to SA victims' disclosures. Social reactions comprise things people do and say in response to a victim's disclosure of SA. When considering both negative and positive social reactions to disclosure, negative reactions appear strongly linked to greater symptoms, while positive reactions seem not to provide protection, have lesser impact, or even be associated with more symptoms (Dworkin et al., 2019). Dworkin et al.'s (2019) review particularly stressed the negative impact of reactions such as controlling, distraction, and treating the survivor differently (including withdrawal). Another study, using a different measure, pointed to the negative consequences of social devaluation and discrediting (Nöthling et al., 2022). A recent meta-analysis documented a robust association between negative social reactions and psychological symptoms in SA victims (Dworkin et al., 2019). There are however two main shortcomings of the research on social reactions to disclosure. First, these studies generally do not account for social support, leaving it unclear whether social reactions represent an additional factor influencing mental health. To understand the unique potential contributions to mental health, both concepts should be assessed. To the best of our knowledge, only two previous studies have examined both, and they indicated that social support and negative reactions play different roles in the post-assault adjustment process (Ullman et al., 2007; Littleton, 2010). Second, almost all the studies on social reactions have been conducted several years after the assault, and as time passes, it may be challenging to recall specific social reactions.
Both perceived social support and social reactions are concepts related to the quality of victims' social interactions. Perceived social support typically refers to general supportive relationships, like having someone to confide in, while social reactions to disclosure focus on victimization-specific social experiences. Social reactions to disclosure may be an important additional social factor that can add to our understanding of how mental health problems evolve or are maintained following trauma in general or SA in particular.
Given the relative lack of research on aspects of social support in relationship to symptomatology soon after SA, the current study objectives were to assess the associations between social reactions to disclosure and mental health (post-traumatic stress and anxiety/depression) while adjusting for perceived social support in recent victims of SA. We hypothesized that negative social reactions would be associated with both PTSR and anxiety/depression when adjusted for perceived social support.
Materials and methods
Participants and procedure
This study derives data from the first wave of the TRUST study, which is an ongoing, longitudinal observational study of mental health and recovery in recent Norwegian victims of SA. The TRUST study recruited participants through Norwegian Sexual Assault Centers (SACs) and through social media, with the aim to recruit victims who had, and had not, sought help at a SAC following the recent assault. Inclusion criteria included being at least 16 years of age, understand Norwegian or English, and having experienced SA in the past 12 months. Recruitment to the study started in January 2023. The social media campaign was launched during October-November 2023 and repeated in September-October 2024.
Recruitment through SACs
In total, 20 of the 23 Norwegian SACs have signed a written agreement to cooperate with the TRUST study. At the SACs, victims receive medical care, forensic examinations (if suitable), and psychosocial support. SAC staff members inform patients about the ongoing study and ask for their permission to show a 2-minute information video. Alternatively, if this strategy is unsuitable in the acute treatment, the patient is given a leaflet explaining the study.
Recruitment through social media
The Norwegian communication agency Try designed and launched a social media recruitment campaign pro bono for this study. As most SA victims do not seek medical help in the acute phase (Thoresen and Hjemdal, 2014), the aim was to recruit individuals in the community who had experienced SA within the last year. The campaign consisted of a collaboration with social media influencers, relevant organizations, and a targeted campaign on Facebook and Instagram. The advertisement poster text was: “Have you experienced sexual assault in the past year?” By participating in the TRUST study you can help others who have similar experiences. By clicking “read more,” potential participants were directed to the study web page containing information about the study and a direct portal to the consent form.
Potential participants were asked to enter their contact information on the study web page, which was transferred encrypted to the University of Oslo Server for sensitive data. Those who entered their contact information received a text message or an e-mail (depending on their preference) 1–3 days later with a link to a web site presenting the study information (https://trust.nkvts.no/eng/). Individuals willing to participate were asked to consent through a secure identity confirmation system (“BankID”). Participants could choose between web questionnaires or telephone interviews. Interviews were conducted by members of the TRUST research team (healthcare personnel with experience in research interviews and one master of science in psychology). Upon completion of the questionnaire/interview, data was transferred encrypted (without local storage) to the University of Oslo Server for sensitive data (TSD).
A temporary data file was created in May 2024, at which time we had achieved a sufficient sample size to answer our research questions (N = 519). We selected participants who had experienced SA during the last 6 months (n = 201). Unfortunately, we had to exclude the few participants of male sex due to the very low number (n = 4, none of whom identified as female). Of the remaining 197 participants, the 173 reporting that they had disclosed the SA to someone (in addition to SAC personnel) constituted our final sample.
Ethical considerations
The TRUST study recruits individuals recently exposed to SA and asks them to share highly sensitive information. Although trauma research participants most often value the experience positively (Jaffe et al., 2015), the study team has taken steps to counteract any potential negative experiences: 1. Potential participants could use the time they needed to consider participation after being presented with the study information; 2. SAC staff and other health personnel were not informed about participation, and participation in the study could not affect health services in any way; 3. Potential adverse reactions to the study were assessed, and those who needed support were offered consultation(s) at an independent stress and trauma clinic; 4. Participants could choose if they wanted to complete an online questionnaire, or be interviewed by one of the researchers on telephone. Each participant has signed an informed consent, and the TRUST study is approved by the Regional Committee for Medical and Health Research (REK 398925/2022) in accordance with Norwegian law. The data file was deidentified and data storage is approved by SIKT (Norwegian Agency for Shared Services in Education and Research).
Lived experience collaboration
The TRUST study was designed in close collaboration with individuals with lived experience (survivors) and people working with survivors, including representatives of the Norwegian Association against Sexual Abuse and the Norwegian PTSD Association, and professionals working with SA victims (such as at sexual assault resource and self-help centers and at SACs).
Measures
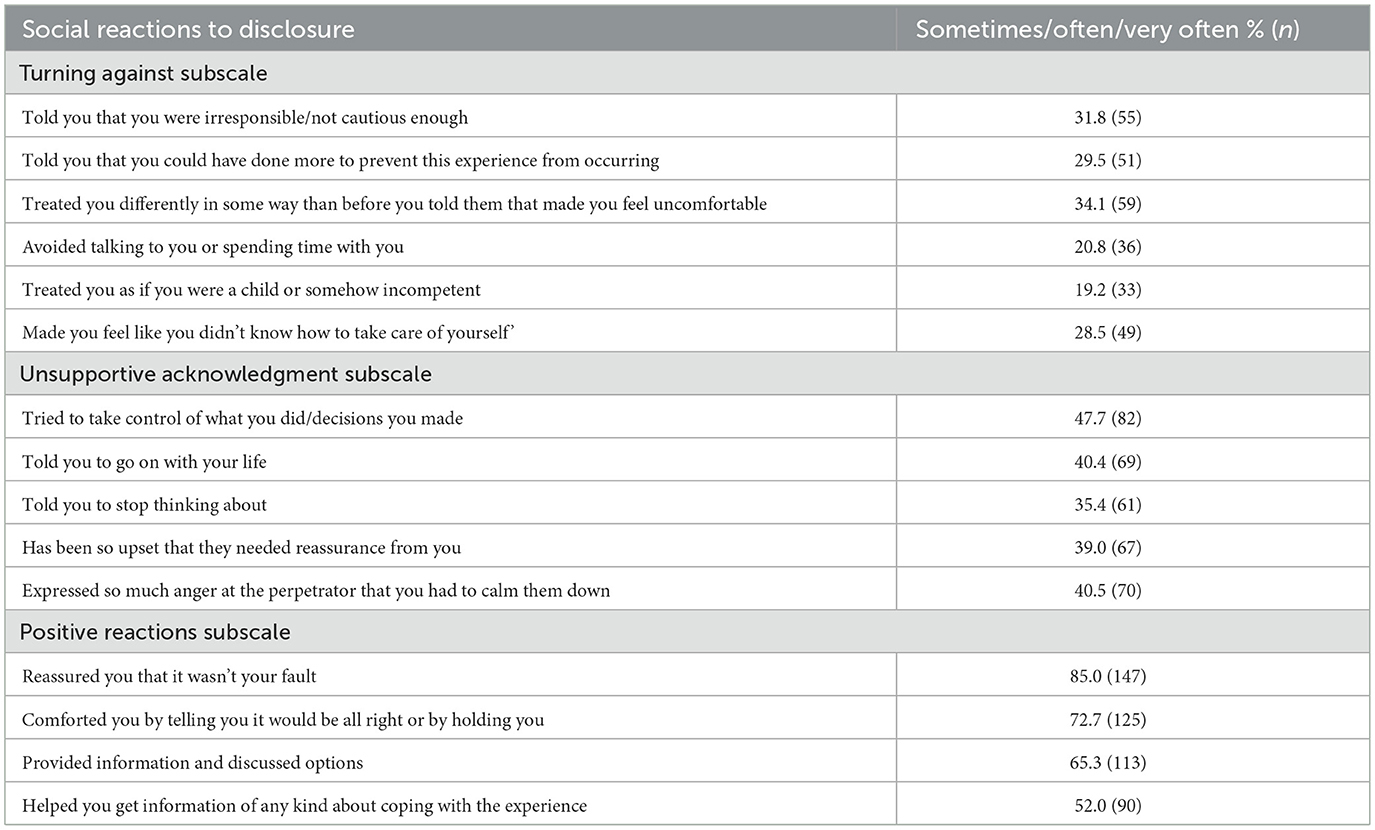
Social reactions to disclosure: Participants were asked if they had disclosed the SA to anyone (in addition to SAC personnel). The 173 participants who had disclosed to at least one person were administered the Social Reactions Questionnaire—shortened (SRQ-S) (Ullman et al., 2017). This instrument assesses frequency of reactions to disclosure from the social network or from formal providers received within three subdomains; turning against (blame, stigma and infantilizing); unsupportive acknowledgment (control, distract, egocentric); and positive reactions (emotional support, tangible aid). The shortened version has good construct validity and internal consistency at baseline and over time. The instrument was translated in collaboration with the developer Sarah Ullman and a Norwegian translation agency. Two adaptations were made due to cultural or translational difficulties: The question “Reassured you that you are a good person” (SRQ-S no 2) was replaced with “Told you it was not your fault” (SRQ no 1) and the question “Made decisions or did things for you” (SRQ-S no 8) was not included. The Norwegian version of the SRQ-S comprised 15 items (see Table 1) scored on a scale from “Never” (0) to “Always” (4). In our sample, Cronbach's alphas were 0.86 for the Turning against subscale, 0.72 for Unsupportive acknowledgment, and 0.74 for Positive reactions.
Current perceived social support was measured by Duke-UNC Functional Social Support Questionnaire (FSSQ) (Broadhead et al., 1988). The scale comprises seven items: Having people around you that care about what happens to you; receiving love and care from close ones; having someone to talk to about work/school/study problems; having trusted people you can talk to about personal or family problems; being included in social activities with others; getting useful advice about important things in life; and being cared for when sick. Respondents are asked to evaluate each item on a 5-point scale: “As much as I would like” (5); “Almost as much as I would like” (4); “Somewhat, but would like more” (3); “Less than I would like” (2); and “Much less than I would like” (1). The FSSQ has been shown to be valid and reliable (Broadhead et al., 1988). Cronbach's alpha in the present study was 0.91.
PTSR since the assault were measured by the International Trauma Questionnaire (ITQ), (Cloitre et al., 2018), Norwegian version by Bækkelund et al. (2019). The ITQ corresponds to ICD-11 diagnosis of PTSD, and comprises two items for each subscale (re-experiencing, avoidance, and hypervigilance), measured on a scale from “Not at all” (0) to “Extremely” (4). Participants were asked to report PTSR symptoms related to the index SA (the assault that preceded their attendance to a SAC/their participation in the study). We used the recommended scoring method to indicate a clinical level of symptoms: A score of ≥2 (“moderately”) on at least one item from each of the three subscales. Cronbach's alpha in the present study was 0.80.
Anxiety and Depression symptoms (last week) were measured by a 10-item version of the Hopkins Symptom Checklist-25 (HSCL) (Derogatis et al., 1974), measuring symptoms of depression and anxiety (suddenly scared for no reason; feeling fearful; faintness, dizziness, or weakness; feeling tense or uneasy; blaming yourself for things; feeling blue; feelings of worthlessness; feeling everything is an effort; feeling hopeless about the future; problem sleeping) on a scale from “Not bothered” (1) to “Bothered a great deal” (4). This abbreviated version of HSCL has shown good psychometric properties and has previously been found to correlate highly (r = 0.97) with the HSCL-25 in a general population sample. We used their recommended cutoff value of >1.85 to indicate a clinically significant level of symptoms (Tambs and Moum, 1993). For this study, Cronbach's α was 0.89.
Control variables included victimization history, assault characteristics, help-seeking, and socio-demographic variables. Victimization history was measured by five questions: Before age 18: (1) Did a parent or caregiver ever slap you repeatedly, beat you, or otherwise attack or harm you?; (2) Did someone do sexual things with you, or made you do sexual things with them, when you could not say no, were forced or pressured?; From age 18: (3) Have you previously experienced one or more SA(s)?; (4) Have you ever been kicked, hit, beat up or otherwise physically harmed by a romantic partner/spouse?; (5) Have you ever been kicked, hit, beat up or otherwise physically harmed by someone else in your family, an acquaintance or someone else? Response format for all items were “yes” or “no.” Questions were adapted from the Stressful Life Event Screening Questionnaire (SLESQ) (Goodman et al., 1998), Norwegian version (Thoresen and Øverlien, 2009) and The Child and Adolescent Trauma Screen 2 (CATS-2) (Sachser et al., 2022); Norwegian version by Norwegian Center for Violence and Traumatic Stress Studies (https://www.nkvts.no//content/uploads/2022/11/TRAUME-OG-PTSD-SCREENING-TRAPS-II-norsk.pdf). Item 3 was created for this study. Following the results from a Swedish study of recent rape victims (Tiihonen Möller et al., 2014), we constructed a dichotomous variable indicating 0–1 vs. 2 or more “yes” answers to categories of previous victimization experiences.
Assault characteristics included: (1) Relationship to the perpetrator (dichotomous dummy variable indicating “close” (current/ex romantic partner or family member) vs. “other” (unknown, known less than 24 h, friend/colleague/fellow student, authority person or other); (2) completed penetration (yes or no); (3) the perpetrator's use of physical force or threats to harm (e.g., holding down or threats of violence) (yes or no); (4) the perpetrator's actual use of physical violence during the assault (yes or no); and (5) victim intoxication at the time of the assault (being so sleepy, unconscious, or drunk that the individual could not consent or oppose to what was happening) (yes or no). Time since assault was recorded as a categorical variable: 1–6 days, 1–2 weeks, 3–4 weeks, 1–3 months, 3–6 months.
Help-seeking at a SAC
Participants were asked if they had sought help at a SAC as a result of the recent SA (yes/no).
Sociodemographic variables included age, biological sex (“What is your biological sex”) and gender (“Do you identify as another gender?” and “If yes, which gender?”), national background (born in Norway by Norwegian-born parents or not). Among the 173 participants of female sex, all self-identified as women. Education level indicated whether or not the participant had completed 13 years of education. A dichotomous variable of self-perceived financial situation was constructed indicating whether or not the participants perceived their financial situation to be worse than most people.
Statistical analyses
We used Pearson's r to examine correlations between continuous variables and independent sample t-tests to assess differences between SAC seekers and non-SAC-seekers on mental health, social reactions, and social support. To assess associations between the three SRQ subscales, social support and mental health, we performed a series of linear regression analyses, separately for post-traumatic stress and anxiety/depression. First, unadjusted associations are presented. Secondly, all variables were included in an adjusted model (SRQ subscales, social support, age, national background, help-seeking, time since assault, assault characteristics, and victimization history). In the adjusted model, multicollinearity was assessed by variance inflation factor (VIF), with the most commonly used thresholds of 5 and 10 used for indications of problematic and highly problematic multicollinearity (Kim, 2019). Sensitivity analyses were conducted to determine if adjustment for education level and perceived financial situation would substantially alter the regression coefficients of the social reactions and social support variables. Regressions were performed without bootstrapping, but due to observed skewness in two of the SRQ subscales, we performed bootstrapping (10,000 bootstrap replications) and compared confidence intervals with BCa (bias corrected and accelerated) and without bootstrapping.
“Half rule” was used for scale variables, i.e., mean scores were calculated based on the means of valid items within each scale (Fairclough, 2010) as long as at least half the questions were answered. No participant had more than three missing items on scale variables, and mean scores were calculated for all participants. Because of few missing values, 172 of the 173 participants were included in the regression analyses. All tests were two-tailed, with a significance level of p < 0.05. Statistical analyses were performed using IBM SPSS statistics for Windows, version 29, bootstrapping was performed in the R package boot.
This study was preregistered in OSF: https://osf.io/nx437/. We made no major changes to the planned analyses, except that we performed bootstrapping due to observed skewness in two of the SRQ subscales and included the demographic variables age and national background in the SRQ subscales regressions.
Results
The 173 female participants had a mean age of 26 years (SD = 8.6, range 16–71), 86.7% (n = 150) was born in Norway by Norwegian-born parents, 85.0% (n = 147) had completed 13 years of education, and 29.1% (n = 48) reported that they had a financial situation “worse than most people.” The perpetrator was a partner, ex-partner or family member in 17.4% (n = 30) of the SAs. Most assaults included sexual penetration (80.9%, n = 140). The perpetrator used physical force or threats to harm in 38.7% (n = 67), and actual physical violence in 25.4% (n = 44) of the assaults. About half (50.9%, n = 88) of the participants reported that they were not able to consent or defend themselves due to intoxication. In total, 47.4% (n = 82) had two or more experiences of previous physical violence and/or SA. In total, 53.8% (n = 93) had sought help at a SAC after the assault. Most participants (88.4%, n = 153) responded on a web questionnaire, while the rest (11.6%, n = 20) chose to be interviewed by telephone.
Symptom levels were very high among participants. The mean PTSR score was 2.4 (SD = 0.9) on a scale from 0 to 4, where a score of 2 indicates “moderately” and 3 indicates “quite a bit.” The mean anxiety/depression score was 3.0 (SD = 0.7) on a scale from 1 to 4, where 3 indicates “bothered quite a bit.” Symptom levels showed little variation according to number of months since the SA for both PTSR and anxiety/depression (mean PTSR scores ranged from 2.4 to 2.5, and mean anxiety/depression scores ranged from 2.9 to 3.1, depending on the number of months since SA). A clinically significant level of PTSR was observed in 68.6% of participants (n = 118), and in 69.2% (n = 74) of those for whom more than a month had passed since the SA. A clinically significant level of anxiety/depression symptoms was observed in 90.8% (n = 157) of participants. Symptom levels were significantly higher in participants who had sought help at a SAC (mean PTSR = 2.6, SD = 0.8) and mean anxiety/depression = 3.1, SD = 0.6) compared to those who had not (mean PTSR = 2.3, SD = 1.0) and mean anxiety/depression = 2.8, SD = 0.8), t-test p < 0.001 for both comparisons. Neither the negative social reactions nor social support differed significantly between SAC- and non-SAC seekers (t-test p-values = 0.313–0.758). However, SAC-seekers reported more positive social reactions (SAC-seekers mean = 2.4, SD = 0.9; non-SAC-seekers mean = 1.9, SD = 0.9, t-test p-value < 0.001).
Social reactions to disclosure
Our sample constituted only participants who had disclosed the SA to someone. Participants reported a variety of social reactions to disclosure of the SA (Table 1). Positive reactions were more frequently reported than negative reactions. Particularly, participants perceived that other people had reassured them that what happened wasn't their fault. The most frequently reported negative social reactions were in the “Unsupportive acknowledgment subscale,” namely others trying to take control, expressing excessive anger, and telling the victim to go on with her life. One of five to one of three victims reported negative social reactions of the “Turning against” type. For example, about a third of the victims reported that other people had treated them differently in a negative way after disclosure.
Correlations between scale variables are displayed in Table 2. The two SRQ negative reactions subscales were strongly correlated, and both were moderately and negatively associated with social support. The SRQ subscale “Turning against” was negatively associated with the SRQ positive reactions subscale, while the SRQ subscale “Unsupportive acknowledgement” was not significantly associated with positive reactions. PTSR were moderately positively associated with anxiety/depression symptoms. The p-values with adjustment for multiple tests within this group of 15 correlation coefficients were computed using the Holm procedure. Then, the p-value for scale variable 1 vs. 6 was 0.003, 2 vs. 3 was 0.012, 2 vs. 4 0.028, 4 vs. 6 was 0.005. All other significant correlations still had p < 0.001.
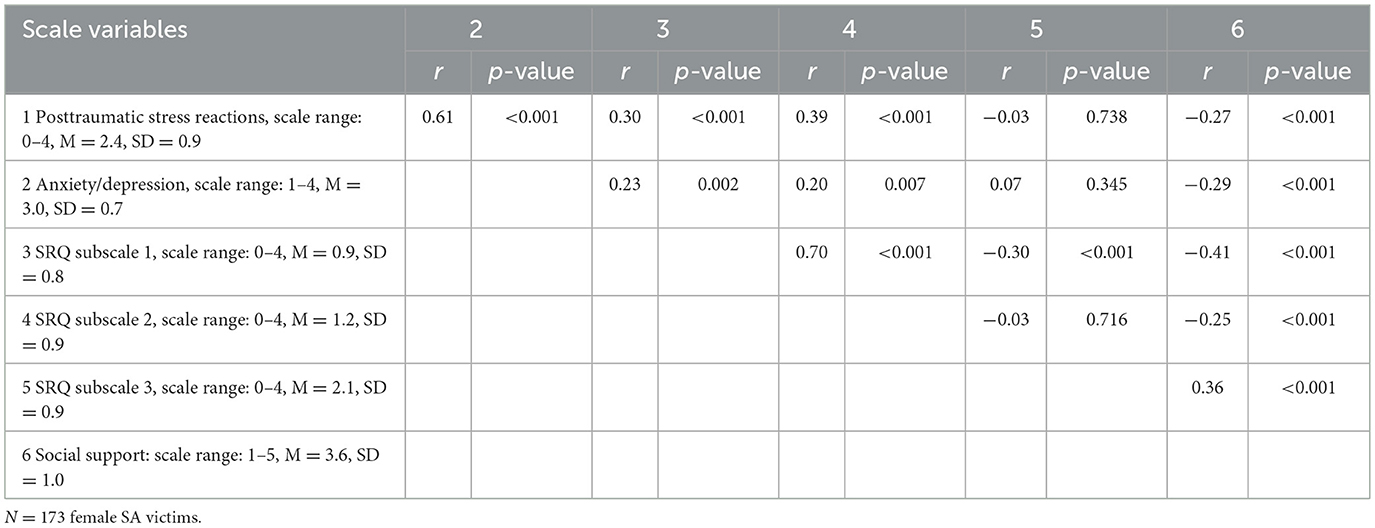
Table 2. Correlations between scale variables (Pearson's r), range, means (M) and standard deviations (SD).
Associations between social reactions, social support, and PTSR
Univariably, both SRQ negative reactions subscales, as well as social support, were significantly associated with PTSR, while SRQ positive reactions subscale was not (Table 3). In the adjusted model, only the SRQ negative reactions subscale “Unsupportive acknowledgment” remained significantly associated with PTSR. The association between social support and PTSR was not statistically significant in the adjusted model. No indications of problems with multicollinearity were detected, VIFs were 2.63,2.23, 1.51 and 1.42 for the SRQ variables and social support, respectively.
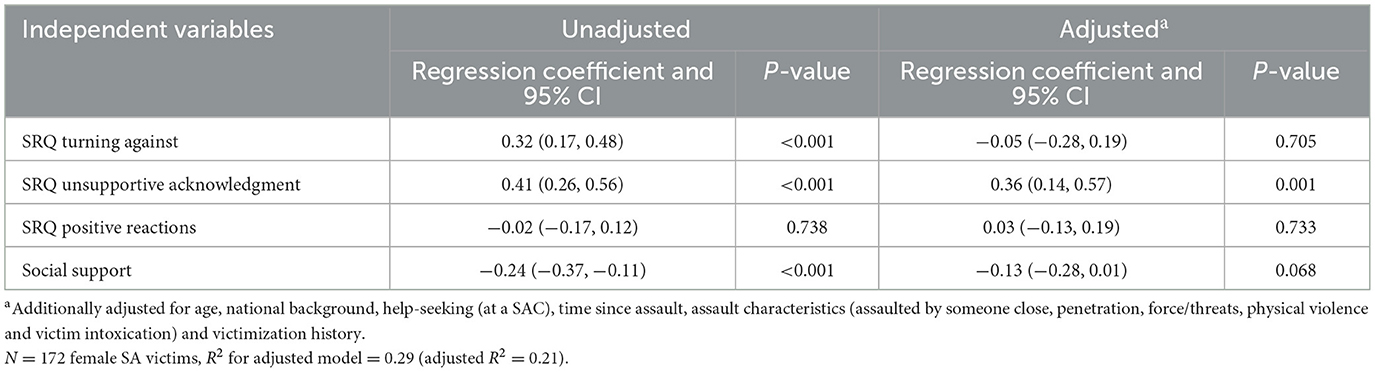
Table 3. Unadjusted and adjusted associations between independent variables and post-traumatic stress symptoms using linear regressions.
Associations between social reactions, social support, and anxiety/depression
As with PTSR, both SRQ negative reactions subscales, as well as social support, were significantly associated with anxiety/depression symptoms in the unadjusted models (Table 4). However, only social support remained significantly related to less anxiety/depression in the adjusted model. The SRQ “Positive reactions” subscale was significantly associated with more anxiety/depression symptoms in the adjusted model. The VIFs were the same as for PTSR.
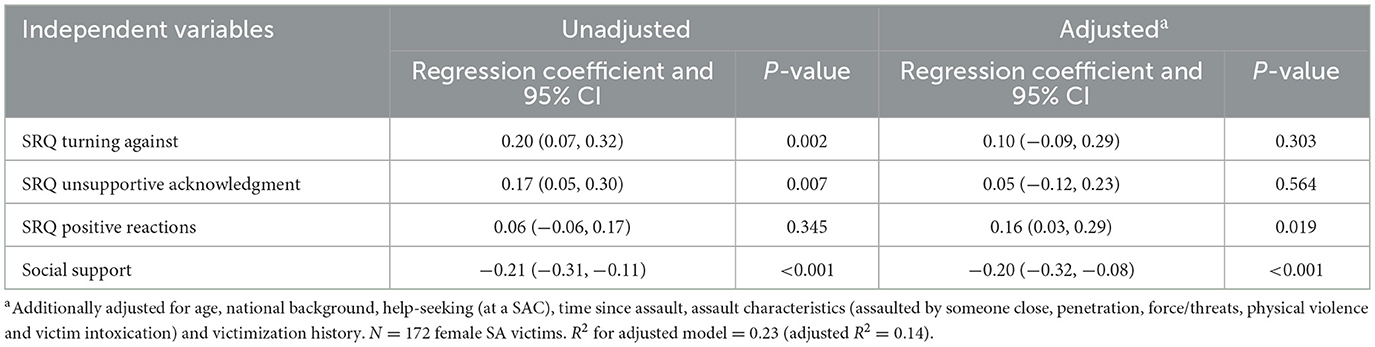
Table 4. Unadjusted and adjusted associations between independent variables and anxiety/depression symptoms using linear regressions.
Appendices 1, 2 display results for all variables included in the adjusted model for Tables 3, 4.
Sensitivity analyses were performed to examine whether adjustment for education level and perceived financial situation would result in any noticeable change in the regression coefficients for SRQ and social support with PTSR and anxiety/depression, respectively. No large changes were observed (not displayed) and the same factors remained significantly associated with the outcome variables. No major differences were identified when regression analyses were compared with bootstrap results. In some cases, confidence intervals were somewhat wider with bootstrap (see electronic Appendix 3).
Discussion
The main results of this study showed that social reactions to disclosure were associated with PTSR in recent victims of SA, even when adjusted for perceived social support and that social support was significantly associated with less anxiety/depression symptoms. Our findings suggest that other people's reactions to victims' disclosure are closely associated with mental health difficulties, particularly PTSR, even in the early aftermath of the assault.
Consistent with previous research, positive social reactions were most common (Filipas and Ullman, 2001; Jónsdóttir et al., 2024). However, many victims received reactions that are considered negative, such as other people trying to take control, telling the victim to stop thinking about it, or treating the victim differently in a negative way. Such negative reactions are thought to convey to the victim; for example, that she is somehow responsible for the assault, is unable to take care of herself, is over-reacting, or is damaged by the assault (Dworkin et al., 2019). In line with previous research (Relyea and Ullman, 2015) unsupportive acknowledgment were more common than turning against reactions and were also more strongly associated with post-traumatic stress reactions (PTSR). These types of responses may be unhelpful not because they involve denial or victim-blaming, but because they lack sufficient sensitivity to the victim's needs—such as when others attempt to take control of the situation or urge the victim to stop thinking about the experience.
Based on previous literature, we hypothesized that negative social reactions would be associated with both PTSR and anxiety/depression beyond the effects of previous victimization, assault characteristics, and time since assault, and that the social reactions-mental health links would remain statistically significant, even when adjusting for perceived social support. Our findings partly supported these hypotheses. As expected, negative social reactions to disclosure, particularly Unsupportive acknowledgment, were significantly associated with higher levels of PTSR in this early phase after SA, even when adjusted for social support. Thus, efforts to reduce these negative social reactions, even relatively soon after SA, appear crucial for achieving symptom relief—particularly taking into account the high symptom levels reported both here and in previous studies (Steenkamp et al., 2012).
However, social support, but not negative social reactions, was significantly associated with anxiety/depression in the adjusted model. This finding was unexpected, as a recent meta-analysis showed that most studies report associations between social reactions and a broad range of psychopathology, including anxiety and depression (Dworkin et al., 2019). However, there are exceptions. For example, one of the few studies included in the meta-analysis that focused on recent SAs, found that social reactions were associated with fear, but not with PTSD symptoms nor depression (Orchowski and Gidycz, 2015). Further, an intervention study aimed at improving social reactions, indicated reduced symptoms of PTSD, but not of depression, in subsequent SA victims (Edwards et al., 2021). Moreover, in a study on reasons for non-disclosure of SA, specific reasons for non-disclosure were related to PTSD, but not to depression (Carson et al., 2020). These findings suggest that social reactions and social support may have different associations with different symptoms. Further research is needed to understand how social reactions affect different types of symptoms over time, and across geographic locations and samples.
Our finding of evidence that social support, but not social reactions, was associated with anxiety/depression in the adjusted model needs further consideration. It is often assumed that negative aspects of social interactions, such as feeling let-down, social support barriers, interpersonal friction, and social constraints, have a greater detrimental impact on mental health than the (potentially) protective effects of social support (Zoellner et al., 1999; Andrews et al., 2003; Thoresen et al., 2014). In our study, the regression coefficient for social support was largely unaffected by adjustment for social reactions, indicating that positive aspects of social interactions, more than negative aspects, were important for anxiety/depression. A few previous studies have simultaneously investigated social support and social reactions to disclosure of SA; and they indicate that social support and negative disclosure reactions may play unique roles in the post-assault recovery process (Ullman et al., 2007; Littleton, 2010). As Littleton suggests, social support may be key to preserving a sense of self-worth following trauma, which may be specifically important for depression symptoms (Littleton, 2010). Also, in the case of other types of trauma, positive and negative aspects of social interactions may have unique impacts on mental health (Charuvastra and Cloitre, 2008; Thoresen et al., 2014), representing separate pathways to symptoms or recovery. Future research should aim to identify specific aspects of social interactions, both positive and negative, that can inform treatment and prevention of symptomatology for victims of SA.
This study was cross-sectional and therefore could not determine the temporal relationships between social support, social reactions, and mental health outcomes. While a lack of social support and negative social reactions may contribute to poorer mental health, it is also possible that individuals with more severe symptoms receive less support and more negative reactions—or perceive support and reactions more negatively. The potential temporal relationship between negative social reactions to disclosure and mental health is unclear due to the lack of longitudinal studies, expect for one study indicating a bidirectional relationship (Ullman and Peter-Hagene, 2016). Concerning social support, a recent meta-analysis similarly suggests a reciprocal relationship between social support and mental health (Wang et al., 2021). Some studies indicate that social support may have a buffering effect in the early stages following trauma, while mental health problems may contribute to a decline in social support over time (Kaniasty and Norris, 2008). An alternative explanation is that the commonly observed associations between social factors and mental health may not reflect causality but instead be driven by unrecognized third variables.
In sum, results underscore the potential importance of the social environment following SA. This conclusion is consistent with many previous studies pointing to the importance of post-trauma factors for recovery (Brewin et al., 2000; Trickey et al., 2012; Maercker and Hecker, 2016) and underscores the need for social-ecological models to understand and change social and systemic conditions for recovery (Campbell et al., 2009; Jewkes et al., 2022).
User panel/lived experience: The results and interpretations in this study were discussed with the TRUST study's lived experience representatives. They related the study findings on social reactions and social support to their personal and professional experiences and gave examples of how negative social reactions can be truly hurtful. For future research, it was suggested to further our understanding of how negative social reactions may influence shame. Additionally, they addressed the need to understand the role of intimate partner violence in the social context of recovery after SA.
Limitations
The current study relied on cross-sectional data, and causal relationships between social reactions, social support, and psychological symptoms could not be determined. The small number of male participants prevented us from examining male victims and potential gender differences. Selection bias is likely, and the sample cannot be considered representative of all SA victims. Specifically, it is likely that victims who have disclosed the assault are overrepresented in our study. All measures were based on retrospective self-report, with the risk of biases or forgetting. The high level of psychological symptoms in our sample may have affected the participants' responses, posing a potential threat to the validity of the data.
Unmeasured variables may have affected our results, for example we lacked information about pre-assault mental health problems. It should also be noted that social reactions characterized by researchers as “negative” or “positive” are not always perceived as such by victims (Dworkin et al., 2018). Although the correlations between social reactions subscales and social support were only moderate, these constructs are likely not entirely independent and may potentially influence one another in complex ways that were beyond the scope of the present study. For instance, negative social reactions could shape an individual's perception of available social support and vice versa. Lastly, the associations between social variables and mental health outcomes were observed within a certain time period after the SA (< 6 months), and such associations may potentially change over time. Despite these limitations, this study had several strengths included recruitment shortly after SA (within 6 months), with both help-seeking and non-help-seeking participants, the ability to investigate social reactions and social support simultaneously, and a sufficient sample size with very little missing data.
Conclusions
Our results show that social factors may be of high importance for the recovery process in the early aftermath of SA. Negative social reactions to disclosure, particularly unsupportive acknowledgment, were associated with more post-traumatic stress reactions while general social support was associated with less anxiety/depression symptoms.
Early interventions for SA victims could, where appropriate, include consultations with family or friends, to achieve more helpful reactions from the social network. Specifically, family and friends may be encouraged to refrain from certain negative reactions, such as taking control, overreacting, or urging the SA victim to stop thinking about what happened, while fostering general social support by being present and engaging in shared activities. Clinicians can assist SA victims in finding safe ways to disclose, prepare for, and deal with potential unhelpful social reactions. A previous study has shown preliminary support for social network interventions in SA victims (Edwards et al., 2022), but more research is needed in this area. Such interventions can be implemented in SACs or in other sexual assault support centers as well as in college/university clinics. Additionally, professionals across disciplines, such as law enforcement, the justice system, victim services, and healthcare, should be informed about supportive and potentially harmful responses to victims' disclosures of sexual assault.
Research is needed to understand how SA interferes with social relations, and to pinpoint the specific aspects of social relationships that are of importance for specific mental health symptoms at different time periods after SA. The mechanisms involved in the relationship between social reactions and mental health, such as for example shame and self-blame, also need further exploration. Finally, there is also a need to develop and test interventions focusing on navigating and improving social relationships in the aftermath of SA.
Data availability statement
The datasets presented in this article are not readily available because the data set includes highly sensitive information and there are legal restrictions to sharing data. Researchers can get access to the data set, but only after applying to (and acceptance from) the Regional Committee for Medical and Health Research. Requests to access the datasets should be directed to c2lyaS50aG9yZXNlbkBua3Z0cy5ubw==.
Ethics statement
The study involving humans was approved by the Regional Committee for Medical and Health Research (REK398925/2022). The study includes participants aged 16 and over. According to Norwegian law, the age of consent for participation in research is 16 years (except for medical interventions and drug trials). Children under the age of 16 must have parental consent. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. No potentially identifiable images or data are presented in this study.
Author contributions
ST: Conceptualization, Methodology, Writing – original draft, Validation, Investigation, Data curation, Funding acquisition, Formal analysis, Project administration, Writing – review & editing. IB: Writing – original draft, Funding acquisition, Writing – review & editing, Validation, Project administration, Conceptualization, Methodology, Data curation, Investigation. GJ: Validation, Funding acquisition, Writing – original draft, Investigation, Data curation, Writing – review & editing, Conceptualization. TW-L: Writing – original draft, Investigation, Validation, Formal analysis, Writing – review & editing, Methodology. SU: Methodology, Writing – review & editing, Conceptualization, Writing – original draft, Validation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Norwegian Research Council (grant number 343236) and the Norwegian Ministry of Justice and Public Security. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We would like to thank all our participants who were willing to share their experiences in this study, and to Norwegian Sexual Assault Care Centers who informed patients about the study. We are also indebted to the following user panel/lived experiences representatives, who have influenced the study design and given feedback on the current article: Kine Pedersen Aamodt from the organization “You Don't Own Me,” Line Kolstad Rødseth from the Norwegian Association against Sexual Abuse, Rannveig Kvifte Andresen from Dixi Resource Center Against Sexual Assault, Ingvild Hestad Torkelsen from Nok., the umbrella organization for Norwegian Resource Centers Against Sexual Assault, and Charlotte Elvedal and Lotte Fischer from the Norwegian Council for Mental Health. We would also like to thank Anne L. Andreassen, Lisa U. Arntzen, Akiah A. Ottesen, and Andrea N. Rustand for their major contributions to the design and data collection in the TRUST study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Gen AI was used in the creation of this manuscript. Chat GPT was used in specific sections of this manuscript purely for language editing purposes. The author(s) take full responsibility for the manuscript and for the use of Chat GPT.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1648804/full#supplementary-material
References
Andrews, B., Brewin, C. R., and Rose, S. (2003). Gender, social support, and PTSD in victims of violent crime. J. Trauma. Stress 16, 421–427. doi: 10.1023/A:1024478305142
Bækkelund, H., Sele, P., and Berg, A. O. (2019). International Trauma Questionaire (ITQ) Norwegian version. Vikersund. Available online at: www.modum-bad.no: Forskningsinstituttet Modum Bad.
Birkeland, M. S., Strøm, I. F., Myhre, M. C., and Thoresen, S. (2020). Am I an island? A network analysis exploring aspects of social landscapes after childhood violence. Psychol. Trauma Theory Res. Pract. Policy 12:356. doi: 10.1037/tra0000483
Bonanno, G. A. (2005). Resilience in the face of potential trauma. Curr. Dir. Psychol. Sci. 14, 135–138. doi: 10.1111/j.0963-7214.2005.00347.x
Brewin, C. R., Andrews, B., and Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol. 68:748. doi: 10.1037/0022-006X.68.5.748
Broadhead, W., Gehlbach, S. H., De Gruy, F. V., and Kaplan, B. H. (1988). The duke-UNC functional social support questionnaire: measurement of social support in family medicine patients. Med. Care 26, 709–723. doi: 10.1097/00005650-198807000-00006
Campbell, R., Dworkin, E., and Cabral, G. (2009). An ecological model of the impact of sexual assault on women's mental health. Trauma Violence Abuse 10, 225–246. doi: 10.1177/1524838009334456
Carson, K. W., Babad, S., Brown, E. J., Brumbaugh, C. C., Castillo, B. K., and Nikulina, V. (2020). Why women are not talking about it: reasons for nondisclosure of sexual victimization and associated symptoms of posttraumatic stress disorder and depression. Violence Against Women 26, 271–295. doi: 10.1177/1077801219832913
Charuvastra, A., and Cloitre, M. (2008). Social bonds and posttraumatic stress disorder. Annu. Rev. Psychol. 59:301. doi: 10.1146/annurev.psych.58.110405.085650
Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., et al. (2018). The international trauma questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr. Scand. 138, 536–546. doi: 10.1111/acps.12956
Cohen, S., and Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychol. Bull. 98:310. doi: 10.1037/0033-2909.98.2.310
Davis, R. C., Brickman, E., and Baker, T. (1991). Supportive and unsupportive responses of others to rape victims: effects on concurrent victim adjustment. Am. J. Community Psychol. 19, 443–451. doi: 10.1007/BF00938035
Derogatis, L. R., Lipman, R. S., Rickels, K., Uhlenhuth, E. H., and Covi, L. (1974). The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav. Sci. 19, 1–15. doi: 10.1002/bs.3830190102
Dworkin, E. R., Brill, C. D., and Ullman, S. E. (2019). Social reactions to disclosure of interpersonal violence and psychopathology: a systematic review and meta-analysis. Clin. Psychol. Rev. 72:101750. doi: 10.1016/j.cpr.2019.101750
Dworkin, E. R., Jaffe, A. E., Bedard-Gilligan, M., and Fitzpatrick, S. (2023). PTSD in the year following sexual assault: a meta-analysis of prospective studies. Trauma Violence Abuse 24, 497–514. doi: 10.1177/15248380211032213
Dworkin, E. R., Menon, S. V., Bystrynski, J., and Allen, N. E. (2017). Sexual assault victimization and psychopathology: a review and meta-analysis. Clin. Psychol. Rev. 56, 65–81. doi: 10.1016/j.cpr.2017.06.002
Dworkin, E. R., Newton, E., and Allen, N. E. (2018). Seeing roses in the thorn bush: sexual assault survivors' perceptions of social reactions. Psychol. Violence 8:100. doi: 10.1037/vio0000082
Edwards, K. M., Waterman, E. A., Dardis, C. M., Ullman, S. E., Rodriguez, L. M., and Dworkin, E. R. (2021). A program to improve social reactions to sexual and dating violence disclosures reduces posttraumatic stress in subsequently victimized participants. Psychol. Trauma Theory Res. Pract. Policy 13:368. doi: 10.1037/tra0000927
Edwards, K. M., Waterman, E. A., Ullman, S. E., Rodriguez, L. M., Dardis, C. M., and Dworkin, E. R. (2022). A pilot evaluation of an intervention to improve social reactions to sexual and partner violence disclosures. J. of Inter Viol., 37, 2510–2534. doi: 10.1177/0886260520934437
Fairclough, D. L. (2010). Design and Analysis of Quality of Life Studies in Clinical Trials. Chapman and Hall/CRC. doi: 10.1201/9781420061185
Filipas, H. H., and Ullman, S. E. (2001). Social reactions to sexual assault victims from various support sources. Violence Victims 16, 673–692.
Gilbert, P. (2000). The relationship of shame, social anxiety and depression: The role of the evaluation of social rank. Clin. Psychol. Psychother. 7, 174–189. doi: 10.1002/1099-0879(200007)7:3<174::AID-CPP236andgt;3.0.CO;2-U
Goodman, L. A., Corcoran, C., Turner, K., Yuan, N., and Green, B. L. (1998). Assessing traumatic event exposure: general issues and preliminary findings for the Stressful Life Events Screening Questionnaire. J. Trauma. Stress 11, 521–542. doi: 10.1023/A:1024456713321
Jaffe, A. E., DiLillo, D., Hoffman, L., Haikalis, M., and Dykstra, R. E. (2015). Does it hurt to ask? A meta-analysis of participant reactions to trauma research. Clin. Psychol. Rev. 40, 40–56. doi: 10.1016/j.cpr.2015.05.004
Jewkes, R., Mhlongo, S., Chirwa, E., Seedat, S., Myers, B., Peer, N., et al. (2022). Pathways to and factors associated with rape stigma experienced by rape survivors in South Africa: analysis of baseline data from a rape cohort. Clin. Psychol. Psychother. 29, 328–338. doi: 10.1002/cpp.2637
Jónsdóttir, E. K., Sigurvinsdottir, R. S., Ullman, S. E., and Ásgeirsdóttir, B.B. (2024). Disclosures and social reactions to sexual violence: factor structure of the social reactions questionnaire shortened and sex differences in Iceland. Nordic Psychol. 76, 548–567. doi: 10.1080/19012276.2024.2380983
Joseph, S. (1999). “Social support and mental health following trauma,” in Post-Traumatic Stress Disorders: Concepts and Therapy, ed. W. Yule (New York, NY: John Wiley), 71–91.
Kaniasty, K., and Norris, F. H. (2008). Longitudinal linkages between perceived social support and posttraumatic stress symptoms: sequential roles of social causation and social selection. J. Trauma. Stress 21, 274–281. doi: 10.1002/jts.20334
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., and Nelson, C. B. (2013). “Posttraumatic stress disorder in the National Comorbidity Survey,” in Fear and Anxiety ed S. Hyman (New York, NY: Routledge), 22–34.
Kim, J. H. (2019). Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 72, 558–569. doi: 10.4097/kja.19087
Lepore, S., and Ituarte, P. H. (1999). Optimism about cancer enhances mood by reducing negative social interactions. Cancer Res. Ther. Control 8, 165–174.
Lincoln, K. D. (2000). Social support, negative social interactions, and psychological well-being. Soc. Serv. Rev. 74, 231–252. doi: 10.1086/514478
Littleton, H. L. (2010). The impact of social support and negative disclosure reactions on sexual assault victims: a cross-sectional and longitudinal investigation. J. Trauma Dissoc. 11, 210–227. doi: 10.1080/15299730903502946
Maercker, A., and Hecker, T. J. (2016). Broadening perspectives on trauma and recovery: a socio-interpersonal view of PTSD. Eur. J. Psychotraumatol. 7:29303. doi: 10.3402/ejpt.v7.29303
Nöthling, J., Abrahams, N., Jewkes, R., Mhlongo, S., Lombard, C., Hemmings, S. M. J., et al. (2022). Risk and protective factors affecting the symptom trajectory of posttraumatic stress disorder post-rape. J. Affect. Disord. 309, 151–164. doi: 10.1016/j.jad.2022.04.032
Orchowski, L. M., and Gidycz, C. A. (2015). Psychological consequences associated with positive and negative responses to disclosure of sexual assault among college women: a prospective study. Violence Against Women 21, 803–823. doi: 10.1177/1077801215584068
Relyea, M., and Ullman, S. E. (2015). Unsupported or turned against: understanding how two types of negative social reactions to sexual assault relate to postassault outcomes. Psychol. Women Q. 39, 37–52. doi: 10.1177/0361684313512610
Sachser, C., Berliner, L., Risch, E., Rosner, R., Birkeland, M. S., Eilers, R., et al. (2022). The child and Adolescent Trauma Screen 2 (CATS-2)–validation of an instrument to measure DSM-5 and ICD-11 PTSD and complex PTSD in children and adolescents. Eur. J. Psychotraumatol. 13:2105580. doi: 10.1080/20008066.2022.2105580
Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., and Haro, J. M. (2015). The association between social relationships and depression: a systematic review. J. Affect. Disord. 175, 53–65. doi: 10.1016/j.jad.2014.12.049
Steenkamp, M. M., Dickstein, B. D., Salters-Pedneault, K., Hofmann, S. G., and Litz, B. T. (2012). Trajectories of PTSD symptoms following sexual assault: is resilience the modal outcome? J. Trauma. Stress 25, 469–474. doi: 10.1002/jts.21718
Tambs, K., and Moum, T. (1993). How well can a few questionnaire items indicate anxiety and depression? Acta Psychiatr. Scand. 87, 364–367. doi: 10.1111/j.1600-0447.1993.tb03388.x
Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 52, 145–161. doi: 10.1177/0022146510395592
Thoresen, S., Aakvaag, H. F., Strøm, I. F., Wentzel-Larsen, T., Birkeland, M. S. J. S.S., and Medicine (2018). Loneliness as a mediator of the relationship between shame and health problems in young people exposed to childhood violence. Soc. Sci. Med. 211, 183–189. doi: 10.1016/j.socscimed.2018.06.002
Thoresen, S., and Hjemdal, O. K. (2014). Vold og voldtekt i Norge. En nasjonal forekomststudie av vold i et livsløpsperspektiv. Oslo: Nasjonalt kunnskapssenter om vold og traumatisk stress. Available online at: https://www.nkvts.no//content/uploads/2015/11/vold_og_voldtekt_i_norge.pdf (Accessed February 17, 2025).
Thoresen, S., Jensen, T. K., Wentzel-Larsen, T., and Dyb, G. (2014). Social support barriers and mental health in terrorist attack survivors. J. Affect. Disord. 156, 187–193. doi: 10.1016/j.jad.2013.12.014
Thoresen, S., and Øverlien, C. (2009). Trauma victim: yes or no? Why it may be difficult to answer questions regarding violence, sexual abuse, and other traumatic events. Violence Against Women 15, 699–719. doi: 10.1177/1077801209332182
Tiihonen Möller, A., Bäckström, T., Söndergaard, H. P., and Helström, L. (2014). Identifying risk factors for PTSD in women seeking medical help after rape. PLoS ONE 9:e111136. doi: 10.1371/journal.pone.0111136
Tjaden, P., and Thoennes, N. (2000). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women: Findings From the National Violence Against Women Survey: Research report. National Institute of Justice. Available online at: https://www.ojp.gov/pdffiles1/nij/183781.pdf (Accessed February 17, 2025). doi: 10.1037/e514172006-001
Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., and Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin. Psychol. Rev. 32, 122–138. doi: 10.1016/j.cpr.2011.12.001
Ullman, S. E. (2000). Psychometric characteristics of the social reactions questionnaire. Psychol. Women Q. 24, 257–271. doi: 10.1111/j.1471-6402.2000.tb00208.x
Ullman, S. E., and Peter-Hagene, L. C. (2016). Longitudinal relationships of social reactions, PTSD, and revictimization in sexual assault survivors. J. Interpers. Violence 31, 1074–1094. doi: 10.1177/0886260514564069
Ullman, S. E., Relyea, M., Sigurvinsdottir, R., and Bennett, S. (2017). A short measure of social reactions to sexual assault: the social reactions questionnaire-shortened. Violence Vict. 32, 1096–1115. doi: 10.1891/0886-6708.VV-D-16-00066
Ullman, S. E., Townsend, S. M., Filipas, H. H., and Starzynski, L. L. (2007). Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychol. Women Q. 31, 23–37. doi: 10.1111/j.1471-6402.2007.00328.x
Wang, Y., Chung, M. C., Wang, N., Yu, X., and Kenardy, J. (2021). Social support and posttraumatic stress disorder: a meta-analysis of longitudinal studies. Clin. Psychol. Rev. 85:101998. doi: 10.1016/j.cpr.2021.101998
Keywords: sexual assault, PTSD, anxiety/depression, social reactions to disclosure, social support, victimization
Citation: Thoresen S, Blix I, Johnsen GE, Wentzel-Larsen T and Ullman SE (2025) Social reactions to disclosure and perceived social support are each uniquely associated with mental health in the first 6 months following sexual assault. Front. Psychol. 16:1648804. doi: 10.3389/fpsyg.2025.1648804
Received: 17 June 2025; Accepted: 22 August 2025;
Published: 23 September 2025.
Edited by:
Anton Kurapov, University of Salzburg, AustriaReviewed by:
Zulkarnain Zulkarnain, Balilkpapan State Polytechnic, IndonesiaJihyeon Choi, Chatham University, United States
Copyright © 2025 Thoresen, Blix, Johnsen, Wentzel-Larsen and Ullman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Siri Thoresen, c2lyaS50aG9yZXNlbkBua3Z0cy5ubw==
 Siri Thoresen
Siri Thoresen Ines Blix
Ines Blix Grethe E. Johnsen4
Grethe E. Johnsen4 Tore Wentzel-Larsen
Tore Wentzel-Larsen