- 1Department of Health Policy and Management, Chung Shan Medical University, Taichung, Taiwan
- 2Department of Medical Management, Chung Shan Medical University Hospital, Taichung, Taiwan
- 3Department of Applied Foreign Languages, Chung Shan Medical University, Taichung, Taiwan
- 4Department of Medical Humanities, School of Medicine, Chung Shan Medical University, Taichung, Taiwan
- 5Department of Medical Education, Chung Shan Medical University Hospital, Taichung, Taiwan
Objective: Unaddressed moral distress may result in psychological, emotional, and physical consequences. The study was to develop and validate a Moral Distress Scale for Healthcare Students and Providers (MDS-HSP) within the Taiwanese healthcare education and clinical contexts, providing a framework for administrators and policymakers to recognize and respond to moral distress in training and practice settings.
Methods: Following an extensive literature review and expert discussions, the study performed an exploratory factor analysis (EFA) using SPSS with a sample of 332 participants to determine the hidden structure of the MDS-HSP and evaluate its initial psychometric properties. A subsequent confirmatory factor analysis (CFA) using AMOS with a separate sample of 240 participants was performed to verify the identified factor structure. The testing process included the assessments of validity, reliability, and goodness-of-fit analysis.
Results: Following the EFA, the initial 72 items were refined to 42 items across six factors: “acquiescence to patients’ rights violations” (8 items), “lack of professional competence” (9 items), “disrespect for patients’ autonomy” (10 items), “futile treatment” (5 items), “organizational and social climate” (6 items), and “not in patients’ best interest” (4 items). The CFA confirmed the same six scale factors and 42 items. Both EFA and CFA supported the proposed factor structure and demonstrated adequate validity and reliability.
Conclusion: The study provided empirical evidence supporting the MDS-HSP as a reliable tool for assessing moral distress experienced by healthcare students and providers. Its use may inform educational strategies, institutional policies, and ethical support mechanisms within healthcare and academic settings.
1 Introduction
As medical technology and information continue to advance rapidly, healthcare professionals are increasingly confronted with complex caregiving demands, often within the constraints of limited resources and the pressure for cost-efficiency. In such high-stakes environments, ethical ideals often collide with the complexities of real-world clinical environments (Topol, 2013). However, many institutions still lack standardized ethical guidelines to navigate these challenges, leaving caregivers feeling overwhelmed, helpless, and demoralized. As a result, healthcare providers often find themselves disoriented and emotionally distressed when making decisions in morally ambiguous situations (Austin et al., 2017; Hamric and Blackhall, 2007).
Jameton (1984) first introduced moral distress and described it as the psychological discomfort of knowing the morally appropriate course of action to take but failing to act on it because of external constraints. In examining the impacts of moral distress on neonatal intensive care unit nurses, Jameton (1984) highlighted how institutional or systemic barriers can hinder nurses from delivering optimal care but feel compelled to carry out actions they consider morally wrong. The definition of moral distress has been expanded over time to encompass a wider range of ethical challenges, including the psychological and physical tolls that result from such distress. Moral distress emerges when individuals are forced to act against their moral beliefs, preventing them from upholding their core values and resulting in a sense of powerlessness to alter the situation (Godshall, 2021; Jameton, 1993; Salari et al., 2022). In healthcare, moral distress arises primarily when professionals must administer treatments that they know are ineffective or do not serve the patient’s best interests, especially true in circumstances of futile medical care (Rice et al., 2008). This type of distress is prevalent among nurses working in high-pressure settings such as acute care units, obstetrics, pediatric wards, and acute psychiatric departments (Ferrell, 2006; Jansen et al., 2020). Compared to other healthcare professionals, nurses tend to experience moral distress both more frequently and intensely (Corley, 2002; Hamric and Blackhall, 2007; Sporrong et al., 2006).
Moral distress impacts not only nurses but also other healthcare providers, including doctors, physiotherapists, occupational therapists, speech therapists, pharmacists, dietitians, etc., (Brazil et al., 2010; Hamric, 2010; Ulrich and Grady, 2018). It presents a significant challenge for healthcare providers, particularly those working in high-pressure environments, such as emergency medical units, intensive care units, etc., (Lamiani et al., 2017), where they are frequently exposed to moral distress and psychological strain, especially during the pandemic. A meta-analysis of moral distress revealed that it is more frequently experienced by providers when they feel they are administering excessive care. It is less common when palliative care options are suggested (Prentice et al., 2016). ICU healthcare providers are more likely to suffer moral distress when faced with end-of-life situations, ethical dilemmas, and complicated family dynamics (Coughlin, 2021). Whitehead et al. (2015) noted that moral distress in ICU settings often comes from a lack of consistent care, pressure to follow family requests that conflict with the patient’s best interests, and adverse effects of ineffective communication. Additional challenges involve administering treatments that may be deemed inappropriate or ineffective, making life-or-death decisions, and withholding information from patients or their families–all of which can intensify moral distress (Corley, 1995; Ferrell, 2006; Fujii et al., 2021). Some other factors that may cause moral distress are poor teamwork, working with incompetent colleagues, fear of judgment from colleagues, improper allocation of medical resources, shortages of staff and resources, the continuation of treatments that merely prolong suffering, and the use of interventions deemed futile, which can cause unnecessary pain to the patient (Al-Humadi et al., 2021; Beltrão et al., 2023; Haghighinezhad et al., 2019).
If left unaddressed, moral distress may bring in a range of adverse emotional and psychological outcomes, such as anger, anxiety, shame, guilt, sadness, frustration, emotional numbness, cynicism, or self-criticism (Burston and Tuckett, 2012; Jameton, 1984, 2017; Jansen et al., 2020; Parker and Tavella, 2021; Rushton, 2018). Furthermore, they may emotionally disengage from their patients and distance themselves from others (Lamiani et al., 2017; Wilson et al., 2013). Physically, they may suffer from burnout, compassion fatigue, headaches, stomach issues, sleep disturbances, weight changes, palpitations, and medical errors (Delfrate et al., 2018; Rushton, 2018). Ultimately, unresolved moral distress may undermine healthcare quality, diminish patient satisfaction, and increase staff turnover (Burston and Tuckett, 2012; Huffman and Rittenmeyer, 2012; McCarthy and Gastmans, 2015).
Addressing the detrimental impacts of moral distress on healthcare personnel, organizations, and the overall healthcare system is an urgent concern (Aultman and Wurzel, 2014; Musto et al., 2015). Therefore, developing tools for early identification and accurate assessment of moral distress is essential, as this provides a foundation for designing effective intervention strategies (Lachman, 2016). Corley et al.’s (2001) Moral Distress Scale (MDS) is the pioneering instrument developed to measure moral distress, grounded in Jameton’s (1984) original conceptualization. The 38-item scale was initially developed to assess how often and severely nurses, especially those working in the ICU, experience moral distress (Corley et al., 2001). Despite its widespread use, the original MDS demonstrated acceptable internal consistency but lacked confirmatory factor analysis and was validated only in nurses. Hamric et al. (2012) modified the tool to 21 questions to assess moral distress. Today, the revised tool, MDS-Revised, remains the commonly employed measure to assess how often and how severely healthcare providers experience moral distress in diverse hospital settings (Hamric and Epstein, 2017). The MDS-R reduced the number of items but retained similar limitations regarding construct validity and generalizability. Different versions of the scale have been adapted to fit the unique needs of various healthcare practitioners, including Wocial and Weaver’s (2013) Moral Distress Thermometer (MDT) and Epstein et al.’s (2019) Measure of Moral Distress for Healthcare Practitioners (MMD-HP). These versions have shown robust validity and reliability across diverse healthcare professions but may require cultural adaptation.
Moreover, several challenges may emerge when considering direct adaptation of the MDS-R or MMD-HP into the Taiwanese context. First, moral distress varies depending on each individual’s cultural background and the unique circumstances of the healthcare setting (Horton et al., 2007). Additionally, the moral distress and ethical dilemmas embedded in these tools reflect Western healthcare systems and do not sufficiently resonate with the socio-cultural dynamics of the Taiwanese healthcare system, especially issues such as family authority and role-based power imbalances (Yeh et al., 2010). Given that environmental and cultural factors influence the experience and response to moral distress (Hamric et al., 2012; Tian et al., 2021), existing tools might not completely reflect the unique moral distress experienced by healthcare students and providers in Taiwanese culturally specific healthcare environments. Moreover, linguistic equivalence alone is insufficient to convey culturally embedded concepts, such as filial piety and collective decision-making, which profoundly shape clinical ethics in Taiwan (Yeh et al., 2010). These systemic, cultural, and linguistic differences make direct adaptation problematic and therefore justify the development of a culture-specific instrument (Picconi et al., 2023).
Hence, without cultural adaptation and validation, the use of these tools in Taiwan may result in incomplete or misleading assessments of moral distress. Consequently, to address this gap, the study intended to go through a systematic review to develop and validate a scale (MDS-HSP) for assessing moral distress in this population based on Taiwanese cultural contexts.
2 Methodology
2.1 Procedure and participants
Grounded in an extensive literature review on moral distress, ethical tensions, moral dilemmas, and related psychological distress, the researchers initially identified 83 potential items capturing various facets of moral distress. To refine this item pool, a series of expert panel discussions (Boateng et al., 2018) was conducted with three professionals specializing in psychometrics, medical humanities, and medical education. Each expert independently evaluated the items using a 6-point relevance scale (0: not relevant; 5: extremely relevant). Items scoring below 4 or lacking inter-rater agreement were eliminated from further consideration. This process constituted a formal evaluation of content validity by the expert panel prior to item testing. Through iterative discussions and consensus-building, the item set was streamlined to 72 items. A 9-point Likert scale was adopted, where 1 represented the absence of distress and 9 denoted the highest level of moral distress, with higher scores reflecting more intense experiences of moral distress.
The researchers carried out a pilot study, employing exploratory factor analysis (EFA) on data collected from 332 participants comprising medical and healthcare students and providers. To validate the identified factor structure, confirmatory factor analysis (CFA) was subsequently carried out on an independent sample of 240 participants. Participants were healthcare students and providers in Taiwan aged 18 or older who completed the survey; those under 18, outside healthcare roles, or with incomplete responses were excluded. The Institutional Review Board of Chung Shan Medical University Hospital granted approval for the research (IRB No. 112008).
2.2 Data analysis
The study first evaluated the normality of the data using skewness and kurtosis. According to Hair et al. (2018), skewness and kurtosis values within ±2.58 (p < 0.01) or ±1.96 (p < 0.05) are generally considered indicative of a normal distribution. Byrne (2010) further noted that kurtosis values of 7 or higher suggest a deviation from normality. Kline (2016) suggested that an absolute skewness value exceeding 3.0 (|γ1| > 3.0) indicates severe skewness, and an absolute kurtosis value exceeding 10.0 (|γ2| > 10.0) indicates a potential problem. To uncover and confirm the underlying factor structure, the study conducted an EFA using SPSS version 14.0 (IBM Corp, 2016) on data from 332 participants, followed by CFA with AMOS version 24.0 (Arbuckle, 2016) on a separate sample of 240 individuals. Factor extraction was guided by eigenvalue assessment, principal component analysis (PCA), and Promax rotation to accommodate potential correlations among factors. Sampling adequacy and the acceptability of data for factor analysis were assessed through the Kaiser-Meyer-Olkin (KMO; Kaiser, 1970; Kaiser and Rice, 1974) and Bartlett’s test of sphericity (Bartlett, 1950, 1951). Model fit was assessed for both EFA and CFA using a range of statistical indicators, including the chi-square to degrees of freedom ratio (χ2/df; Hooper et al., 2008), Tucker-Lewis Index (TLI; Bentler, 1990), Comparative Fit Index (CFI; Bentler, 1990), and the Root Mean Square Error of Approximation (RMSEA; Hooper et al., 2008). Furthermore, the psychometric evaluation of the scale included tests for convergent and discriminant validity, along with reliability analysis using composite alpha and Cronbach’s alpha.
3 Results
3.1 Preliminary data analysis and suitability for factor analysis
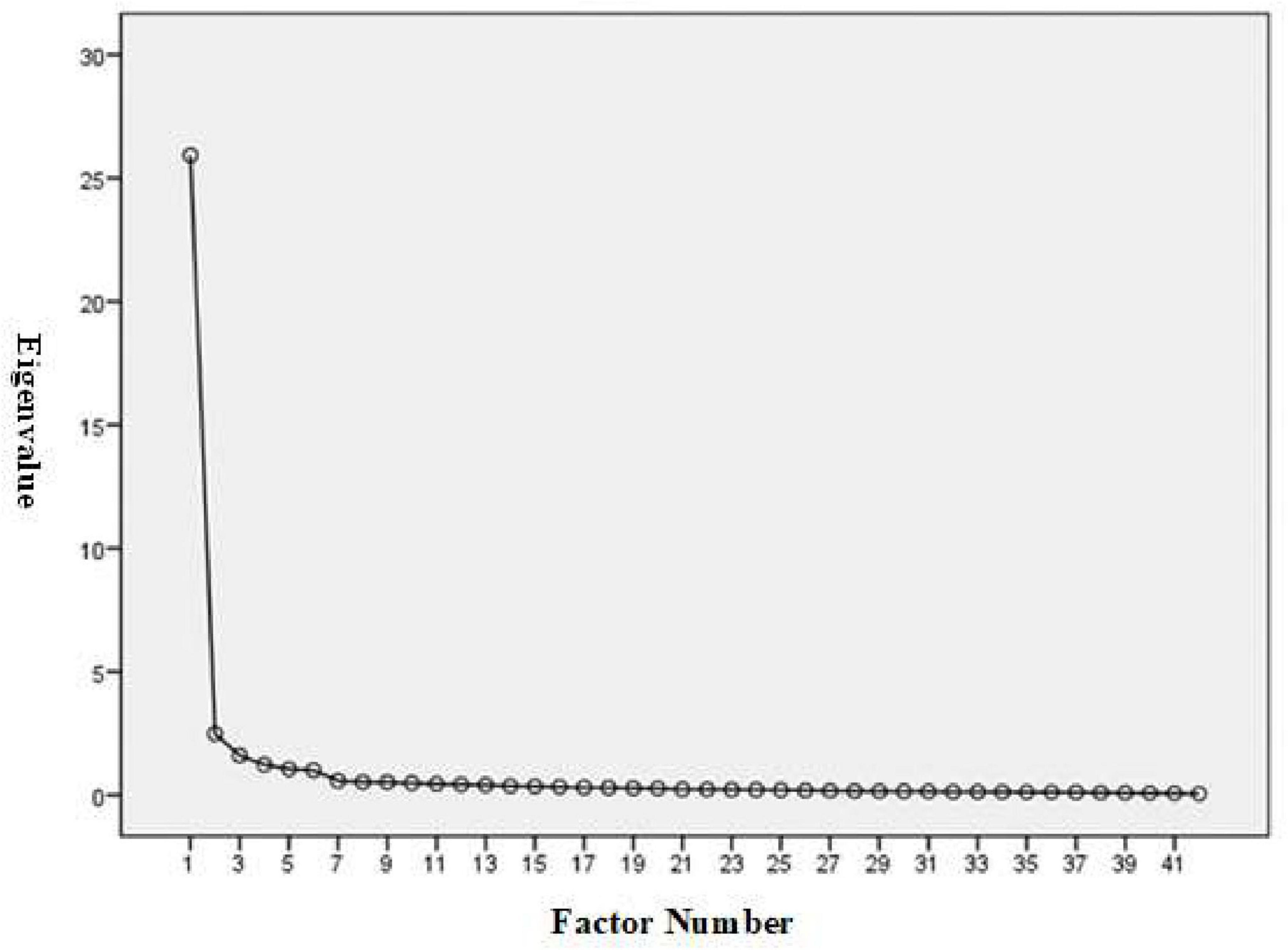
A total of 332 completed questionnaires were obtained from healthcare students and providers across Taiwan. The researchers assessed outliers and multivariate normality by examining skewness and kurtosis. Preliminary analysis revealed no extreme values, with skewness ranging within ±1 and kurtosis within ±2, indicating adequate normality. To assess whether the dataset was suitable for EFA, two statistical tests were conducted. The KMO yielded an exceptionally high value of 0.975, well above the accepted criterion of 0.6 (Kaiser, 1970; Kaiser and Rice, 1974), indicating excellent sampling adequacy. Bartlett’s test of sphericity also yielded a highly significant result (Approx. = 16,704.881; df = 861; p < 0.001), indicating that the factors were appropriately correlated for factor analysis (Bartlett, 1950, 1951). These outcomes validated the appropriateness of proceeding with factor extraction. The scree plot analysis for the MDS-HSP instrument indicated that a six-factor solution is the most appropriate structural representation of the data (Figure 1).
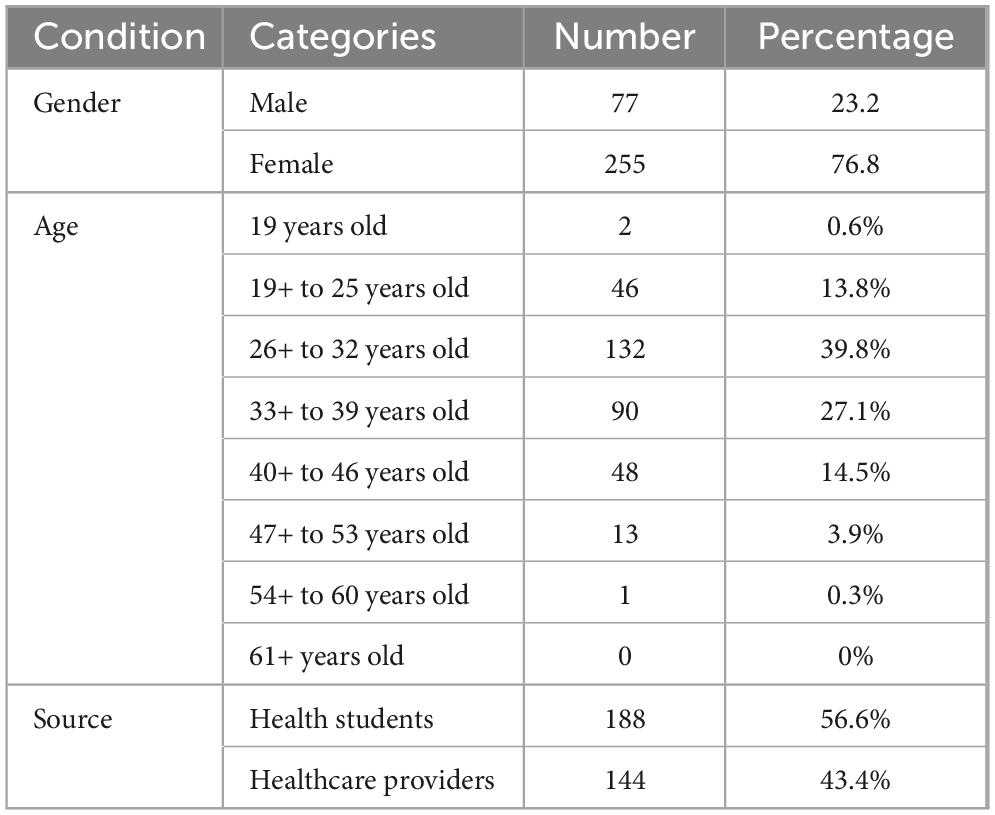
Among the 332 participants, 77 participants (23.2%) were male, and 255 participants (76.8%) were female. There were 2 participants (0.6%) who were below the age of 19, 46 participants (13.8%) who were between the ages of 19 and 25, 132 participants (39.8%) who were between the ages of 26 and 32, 90 participants (27.1%) who were between the ages of 33 and 39, 48 participants (14.5%) who were between the ages of 40 and 46, and 13 participants (3.9%) who were between the age of 47 and 53, 1 participant (0.3%) who was between the ages of 54 and 60, and 0 participant (0%) who was 61 years old or older. Healthcare students comprised 188 (56.6%) of these participants, while healthcare providers comprised 144 (43.4%). The participants’ demographic details are shown in Table 1.
3.2 Exploratory factor analysis (EFA)
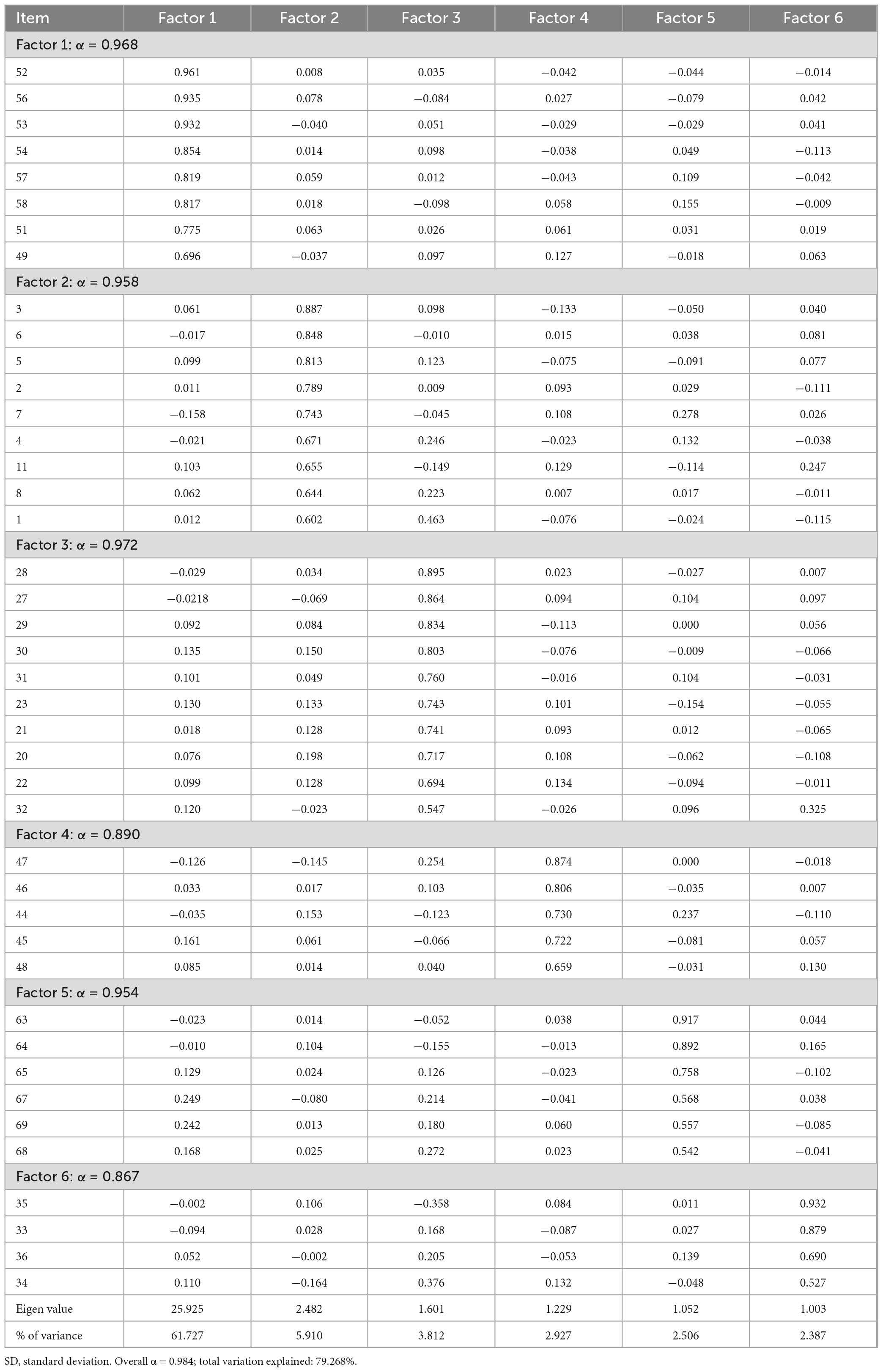
To examine the MDS-HSP scale’s construct and internal consistency validity, the researchers employed EFA, using PCA with Promax rotation and an eigenvalue threshold of 1.0. Items were retained if they demonstrated a loading of ≥0.50 on their designated factor and <0.50 on unrelated factors. This analysis identified six distinct factors encompassing a total of 42 items, collectively accounting for 79.268% of the total variance. The first factor, “acquiescence to patients’ rights violations,” comprised 8 items and explained the largest portion of variance at 61.727%. The second factor, “lack of professional competence,” included 9 items and contributed 5.910%. The third, “disrespect for patients’ autonomy,” encompassed 10 items and accounted for 3.812% of the variance. The fourth factor, “futile treatment,” consisted of 5 items and explained 2.927%. The fifth, “organizational and social climate,” was composed of 6 items and contributed 2.506%, while the sixth and final factor, “not in patients’ best interest,” contained 4 items and explained 2.387%. Each factor exhibited an eigenvalue exceeding the threshold of 1.0, specifically: 25.925, 2.482, 1.601, 1.229, 1.052, and 1.003, thereby confirming the statistical significance and multidimensional nature of the scale structure (see Table 2).
3.2.1 Validities and reliability of the MDS-HSP scale
First written in English, the MDS-HSP scale was later translated into Chinese. To ensure linguistic accuracy and conceptual equivalence, a bilingual expert later back-translated the version into English, allowing for comparison with the initial draft. Content validity was further established through expert evaluation. Additionally, three university students were involved in refining the wording of certain items to improve clarity and ease of understanding.
Cronbach’s alpha coefficients were calculated to assess the internal consistency of the MDS-HSP scale. According to Churchill (1979), a value above 0.8 is generally considered ideal, while 0.7 marks the threshold for acceptable reliability. The overall Cronbach’s alpha for the full scale was 0.984, proving exceptional internal reliability. The analysis also revealed high reliability across all six subscales, with alpha values of 0.968, 0.958, 0.972, 0.890, 0.954, and 0.867, respectively. The results affirmed that both the individual factors and the entire MDS-HSP scale provided stable and consistent measurement of moral distress among participants (Table 2).
3.2.2 Descriptive statistics for the eFA-model MDS-HSP scale
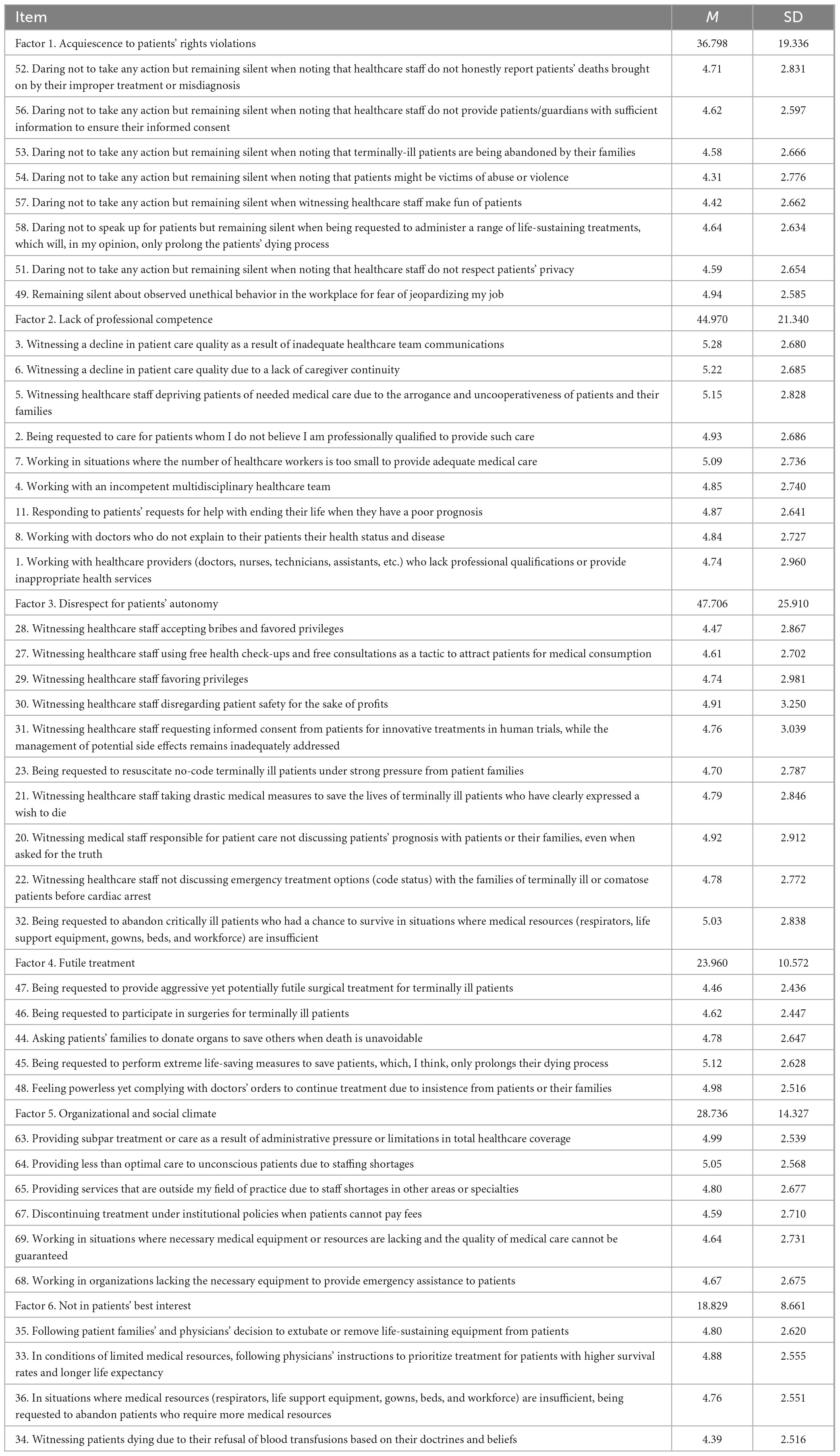
Table 3 shows descriptive statistics for the MDS-HSP scale’s six factors, including item descriptions, mean scores (M), and standard deviations (SD).
3.3 CFA for the MDS-HSP scale
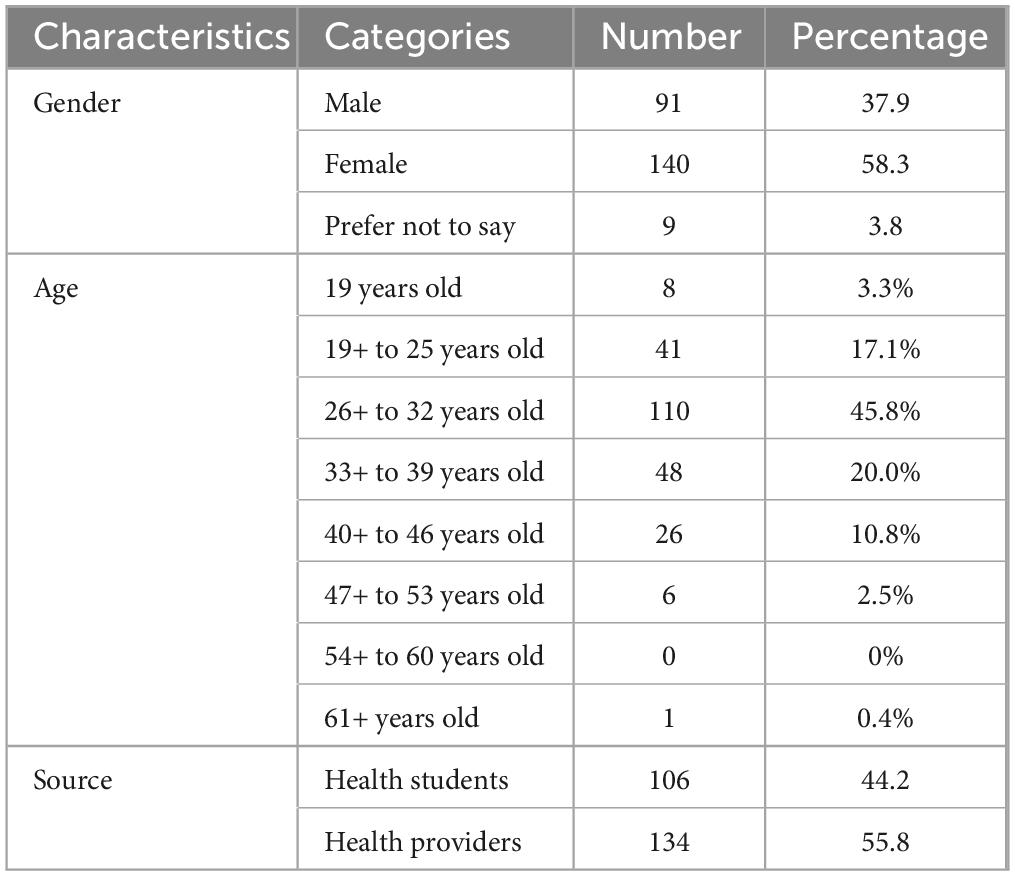
The study further performed CFA using data from 240 participants in order to further confirm the acquired factor structure, of whom 91 participants (37.9%) were male, 140 participants (58.3%) were female, and 9 participants (3.8%) preferred not to say. There were 8 participants (3.3%) who were below the age of 19, 41 participants (17.1%) who were between the ages of 19 and 25, 110 participants (45.8%) who were between the ages of 26 and 32, 48 participants (20.0%) who were between the ages of 33 and 39, 26 participants (10.8%) who were between the ages of 40 and 46, and 6 participants (2.5%) who were between the age of 47 and 53, 0 participant (0%) who were between the ages of 54 and 60, and 1 participant (0.4%) who were 61 years old or older. Healthcare students comprised 106 (44.2%) of these participants, while healthcare providers comprised 134 (55.8%). The participants’ demographic details are shown in Table 4.
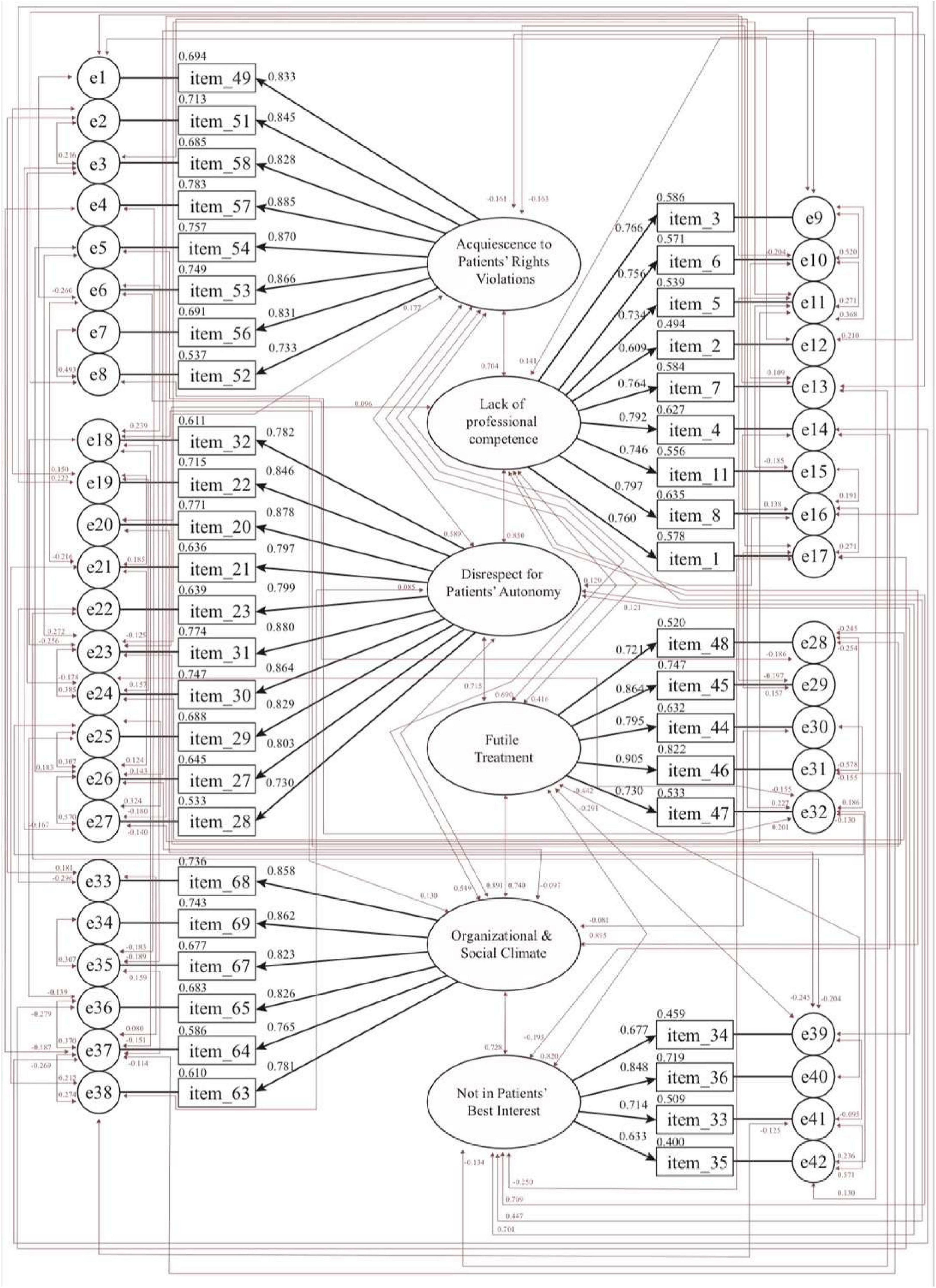
The CFA, done with the AMOS (Arbuckle, 2016), validated the same six scale factors and 42 items (Figure 2). No items were deleted from the factors of “acquiescence to patients’ rights violations” (8 items; factor loadings: 0.733–0.885), “lack of professional competence” (9 items; factor loadings: 0.609–0.797), “disrespect for patients’ autonomy” (10 items; factor loadings: 0.730–0.880), “futile treatment” (5 items; factor loadings: 0.721–0.906), “organizational and social climate” (6 items; factor loadings: 0.765–0.862), and “not in patients’ best interest” (4 items; factor loadings: 0.633–0.848), respectively.
3.3.1 Goodness of fit
To thoroughly assess the suitability of both the EFA and CFA models, the study utilized a range of fit statistics. Among them, the χ2/df was adopted to gauge how closely the observed data matched the model’s expectations. A p-value under 0.05 indicates only a slight divergence between the actual data and the model. Nonetheless, the ideal χ2/df cutoff remains debated, with some scholars arguing that a value between 2.0 and 5.0 is acceptable (Tabachnick and Fidell, 2007; Wheaton et al., 1977), while others proposed a more rigorous standard of below 2.0 to indicate a superior fit (Koufteros, 1999; Schumacker and Lomax, 2010). Additional validation came from the TLI and CFI, with scores above 0.90 generally reflecting an acceptable fit, and values of 0.95 or higher signaling an exceptional fit (Hu and Bentler, 1999; Schermelleh-Engel and Moosbrugger, 2003; Tucker and Lewis, 1973). The RMSEA was also employed to examine how closely the model mirrored the actual data structure (Chen, 2007; Hooper et al., 2008). Hu and Bentler (1999) asserted that RMSEA values under 0.08 point to a reasonable fit, with values below 0.05 reflecting optimal superior model fit. Table 5 lists all fit indices applied in evaluating the MDS-HSP scale’s structure through both exploratory and confirmatory factor analysis. For the EFA model of the MDS-HSP, the model had a chi-square-to-degrees-of-freedom ratio (χ2/df) of 2.401, a TLI of 0.87, a CFI of 0.88, and an RMSEA of 0.08. The CFA model has a χ2/df of 1.097, a TLI of 0.99, a CFI of 0.99, and an RMSEA of 0.02, all exceeding commonly accepted thresholds (Hu and Bentler, 1999). These results provide strong support for the six-factor structure of the MDS-HSP.
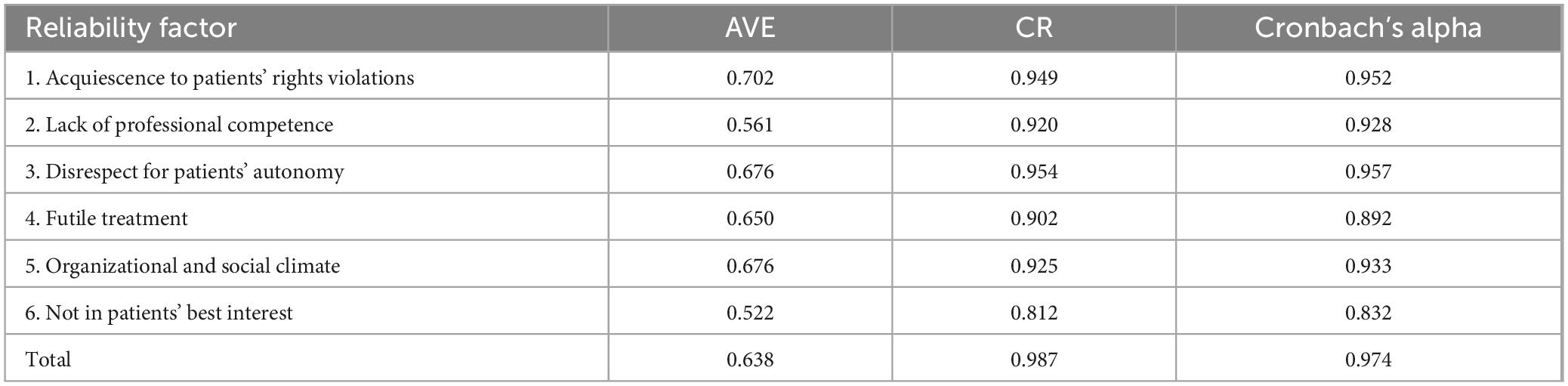
3.3.2 Reliability and validity
To assess the reliability and consistency of the CFA-based MDS-HSP scale, the researchers analyzed both composite reliability (CR) and Cronbach’s alpha. All scores were above the 0.70 cutoff, reflecting high reliability and stable psychometric properties (Churchill, 1979; Hair et al., 2018). Specifically, CR scores for the six factors and the overall instrument fell between 0.812 and 0.987, while Cronbach’s alpha values fell between 0.832 and 0.974. These high coefficients, covering factors of “acquiescence to patients’ rights violations,” “lack of professional competence,” “disrespect for patients’ autonomy,” “futile treatment,” “organizational and social climate,” and “not in patients’ best interest” confirmed the scale’s internal consistency and reliability (see Table 6). To determine whether the MDS-HSP scale items effectively captured the underlying constructs, the study assessed convergent validity through Average Variance Extracted (AVE) and CR scores. Convergent validity is supported when the AVE exceeds 0.50, yet remains lower than the corresponding CR, which should surpass 0.60 (Hair et al., 2018; Pallant, 2013). Table 6 summarizes the AVE and CR values for each of the six identified MDS-HSP scale factors: “acquiescence to patients’ rights violations” (AVE: 0.702; composite alpha: 0.949), “lack of professional competence” (AVE: 0.561; composite alpha: 0.920), “disrespect for patients’ autonomy” (AVE: 0.676; composite alpha: 0.954), “futile treatment” (AVE: 0.650; composite alpha: 0.902), “organizational and social climate” (AVE: 0.676; composite alpha: 0.925), and “not in patients’ best interest” (AVE: 0.522; composite alpha: 0.812). Significantly, each AVE value was lower than its corresponding CR, which consistently exceeded 0.70, highlighting robust reliability across all scale factors (Hair et al., 2018; Pallant, 2013).
4 Discussion
The objective of this research was to develop a medical distress scale (MDS-HSP Scale) to assess medical distress among medical students and providers in Taiwanese clinical and healthcare settings. The study validated the MDS-HSP Scale’s psychometric qualities using EFA to look at the hidden factor structure and CFA to make sure the dataset matched the model. A preliminary 42-item MDS-HSP Scale was initially developed by the researchers using the EFA. Six factors on this scale accounted for 79.268% of the variance: “acquiescence to patients’ rights violations” (8 items), “lack of professional competence” (9 items), “disrespect for patients’ autonomy” (10 items), “futile treatment” (5 items), “organizational and social climate” (6 items) and “not in patients’ best interest” (4 items).
The EFA findings showed that factor loadings are between 0.961 and 0.527, all higher than Hair et al.’s (2018) proposed threshold of 0.50. By analyzing the mean scores across six distinct factors, the researchers further investigated the diverse aspects of moral distress experienced by healthcare students and providers. Participants had the highest score on the “lack of professional competence” factor (Mean = 4.997 per item: 44.970÷9 = 4.997), followed by the “futile treatment” (Mean = 4.792), “organizational and social climate” (Mean = 4.789), “disrespect for patients’ autonomy” (4.771), and “not in patients’ best interest” (4.707). They gained the lowest scores on the “acquiescence to patients’ rights violations” (Mean = 4.600). This suggests that healthcare students and providers experience the most significant moral distress when they perceive themselves or others as lacking expertise and training to provide appropriate care. This finding corresponds with previous research by Epstein and Hamric (2009) and Oh and Gastmans (2015), indicating that moral distress frequently arises when healthcare providers feel inadequately prepared to manage complex clinical situations.
The second highest mean score was observed in the “futile treatment” factor, indicating significant distress associated with providing treatments perceived as non-beneficial. This is particularly evident in critical and end-of-life care settings, where providers may feel compelled to continue aggressive interventions despite ethical concerns. Hamric et al. (2012) noted that institutional pressures to prolong treatment can intensify moral conflict, especially when such interventions contradict a provider’s professional judgment. Close behind was the “organizational and social climate” factor. This highlights the impact of a negative or unsupportive workplace environment on moral distress. The finding corresponds with Hamric and Epstein’s (2017) study, emphasizing that a lack of open communication, ethical support, and collaborative decision-making within an organization significantly increases the likelihood of moral distress among healthcare providers. Moral distress was also notably associated with “disrespect for patient autonomy” (Mean = 4.771) and “not in patients’ best interest” (Mean = 4.600). Participants reported considerable distress when witnessing actions that undermined ethical principles or disregarded patient autonomy and rights. As Berlinger and Berlinger (2017) noted, excluding patients from decision-making or overriding their preferences can significantly contribute to moral distress. Similarly, some actions may raise moral concerns; however, their ambiguous nature makes it difficult to determine whether they harm patients or go against their best interests. As Johnstone and Hutchinson (2015) pointed out, determining what constitutes a patient’s best interest can be highly subjective, particularly in culturally diverse or ethically complex situations, which may contribute to the comparatively lower distress levels reported in this factor. The lowest mean score was associated with the “acquiescence to patients’ rights violations” factor (Mean = 4.600), still falling within the moderate range of moral distress. This may suggest that healthcare providers often feel powerless when institutional protocols or physician orders conflict with their ethical commitment to uphold patient dignity (Ulrich et al., 2010a).
To rigorously confirm the underlying factor structure, CFA was conducted, yielding the same 42 items with strong factor loadings, in the range of 0.609–0.906, surpassing the benchmark set by Hair et al. (2018). Based on multiple indices, the model’s overall fit was deemed robust and acceptable (Hu and Bentler, 1999). While the EFA-derived MDS-HSP scale already demonstrated acceptable fit indices, the CFA-derived model achieved even better fit. This was evidenced by notable improvements: the TLI and CFI rose by 0.12 and 0.11, respectively, while both the RMSEA and the χ2/df dropped significantly, by 0.06 and 1.304, respectively (p < 0.05). The MDS-HSP scale also met the criteria for convergent validity. Regarding convergent validity, findings indicated that the AVE values for constructs–such as “acquiescence to patients’ rights violations,” “lack of professional competence,” “disrespect for patients’ autonomy,” “futile treatment,” “organizational and social climate,” and “not in patients’ best interest”–were all above the suggested benchmark of 0.50 (Hair et al., 2018; Malhotra, 2008) and lower than their CR scores, exceeding. Therefore, because all AVEs exceeded 0.50 and were lower than their corresponding CRs, which all surpassed 0.60, the scale’s convergent validity is well established. Reliability testing also revealed excellent internal consistency in both the CFA-derived and EFA-derived versions of the scale. Across the full scale and all six factors, both the CR and Cronbach’s alphas ranged from 0.812 to 0.987, well exceeding the accepted minimum of 0.70 (Cunha et al., 2016; Hair et al., 2018), further confirming the scale’s robustness and trustworthiness.
Compared with the MDS and MDS-R, the MDS-HSP demonstrates higher overall reliability, with a Cronbach’s alpha of 0.974 and subscale values ranging from 0.832 to 0.957. By comparison, Corley et al.’s (2001) MDS reported an overall alpha of 0.96, with subscale alphas between 0.82 and 0.97, while Hamric et al.’s (2012) MDS-R showed an alpha of 0.89 for nurses and lower reliability for physicians, ranging from 0.67 in smaller samples to 0.88 in larger cohorts. These results indicate that the MDS-HSP provides robust reliability for measuring moral distress in healthcare settings. The results showed that both EFA and CFA supported the proposed factor structure and demonstrated adequate validity and reliability. Consequently, the scale can serve as a diagnostic and evaluative instrument in educational and clinical settings. Hence, it allows healthcare instructors and administrators to identify which aspects of moral distress are most pronounced and design targeted interventions accordingly. For example, educational interventions such as simulation-based training, clinical skills workshops, and mentorship programs may address distress related to lack of professional competence (Berger, 2014), while institutional policies, organizational cultures, and more straightforward guidelines on end-of-life care can mitigate distress associated with futile treatment (Dzeng et al., 2015; Eagle et al., 2015). Enhancing organizational communication, ethical support, and team-based decision-making may reduce distress linked to negative social climate (Hamric and Epstein, 2017), whereas structured communication, shared decision-making, and patient-centered care can help reduce distress associated with respecting patient autonomy or decisions not in patients’ best interest (Johnstone and Hutchinson, 2015; Zolnierek and DiMatteo, 2009). Reporting mechanisms can also help manage distress related to acquiescence to rights violations (Ulrich et al., 2010b).
Some factors of the MDS-HSP, such as organizational climate and futile treatment, reflect ethical challenges common across healthcare settings internationally and may be generalizable. Other factors–particularly “acquiescence to patients’ rights violations” and perceptions of “disrespect for patients’ autonomy”–are influenced by Taiwan’s cultural context, including hierarchical decision-making, family-centered care, and respect for authority, highlighting the scale’s culturally specific relevance (Ko et al., 2018; Kramer et al., 2002).
Overall, the MDS-HSP provides a framework to connect empirical assessment of moral distress with practical educational and institutional strategies, while acknowledging the cultural differences shaping healthcare providers’ experiences in Taiwan. It will help healthcare instructors and administrators identify ethical challenges and moral distress in clinical practice and design appropriate educational interventions, training programs, or institutional policies to reduce moral distress, thereby facilitating professional well-being and effective care delivery. This recognition can also foster broader cultural understanding of the moral complexities healthcare providers face. Nevertheless, this study has certain limitations. The sample was restricted to Taiwanese participants, limiting the generalizability of the findings to other cultural and clinical contexts. Cultural and contextual factors deeply impact moral distress, and differences in healthcare systems, professional roles, social values, and ethical standards across regions can shape how individuals perceive and respond to such distress. Consequently, the current scale may not fully reflect the complexities of moral distress in settings that differ significantly in cultural, ethical, or socioeconomic conditions. Future research should aim to validate the MDS-HSP scale in diverse healthcare systems and cultural contexts, including adaptations for cross-cultural use. Future research may also focus on longitudinal validation, cross-cultural application, and the effects of targeted interventions on moral distress levels over time.
5 Conclusion
This study offers empirical support for the MDS-HSP, confirming its validity and reliability for measuring moral distress in healthcare students and providers within the Taiwanese cultural context. Both exploratory and confirmatory factor analyses demonstrated its strong psychometric properties, establishing the MDS-HSP as a dependable assessment tool. Use of this instrument may guide the development of educational programs, institutional policies, and ethical support frameworks in both healthcare and academic settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Chung Shan Medical University Hospital granted approval for the research. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
H-CL: Methodology, Validation, Data curation, Investigation, Formal analysis, Conceptualization, Writing – review & editing, Supervision, Software, Writing – original draft. Y-HW: Project administration, Conceptualization, Resources, Visualization, Methodology, Validation, Writing – review & editing, Writing – original draft, Investigation, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The National Science and Technology Council (Taiwan) supported the research.
Acknowledgments
The researchers are grateful to all study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Al-Humadi, S., Bronson, B., Muhlrad, S., Paulus, M., Hong, H., and Cáceda, R. (2021). Depression, suicidal thoughts, and burnout among physicians during the COVID-19 pandemic: A survey-based cross-sectional study. Acad. Psychiatry 45, 557–565. doi: 10.1007/s40596-021-01490-3
Aultman, J., and Wurzel, R. (2014). Recognizing and alleviating moral distress among obstetrics and gynecology residents. J. Graduate Med. Educ. 6, 457–462. doi: 10.4300/JGME-D-13-00256.1
Austin, C. L., Saylor, R., and Finley, P. J. (2017). Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychol. Trauma Theory Res. Pract Policy 9, 399–406. doi: 10.1037/tra0000201
Bartlett, M. S. (1950). Tests of significance in factor analysis. Br. J. Psychol. 3, 77–85. doi: 10.1111/j.2044-8317.1950.tb00285.x
Bartlett, M. S. (1951). A further note on tests of significance in factor analysis. Br. J. Psychol. 4, 1–2. doi: 10.1111/j.2044-8317.1951
Beltrão, J. R., Beltrão, M. R., Bernardelli, R. S., Franco, R. S., Epstein, E. G., and Corradi-Perini, C. (2023). Adaptation and validation of the Brazilian version of the Measure of moral distress for healthcare professionals (MMD-HP BR) in the context of palliative care. BMC Palliative Care 22:154. doi: 10.1186/s12904-023-01277-3
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychol. Bull. 107, 238–246. doi: 10.1037/0033-2909.107.2.238
Berger, J. T. (2014). Moral distress in medical education and training. J. General Internal Med. 29, 395–398. doi: 10.1007/s11606-013-2665-0
Berlinger, N., and Berlinger, A. (2017). Culture and moral distress: What’s the connection and why does it matter? AMA J. Ethics 19, 608–616. doi: 10.1001/journalofethics.2017.19.6.msoc1-1706
Boateng, G. O., Neilands, T. B., Frongillo, E. A., Melgar-Quiñonez, H. R., and Young, S. L. (2018). Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front. Public Health 6:149. doi: 10.3389/fpubh.2018.00149
Brazil, K., Kassalainen, S., Ploeg, J., and Marshall, D. (2010). Moral distress experienced by health care professionals who provide home-based palliative care. Soc. Sci. Med. 71, 1687–1691. doi: 10.1016/j.socscimed.2010.07.032
Burston, A. S., and Tuckett, A. G. (2012). Moral distress in nursing: Contributing factors, outcomes and interventions. Nursing Ethics 20, 312–324. doi: 10.1177/0969733012462049
Byrne, B. M. (2010). Structural equation modeling with AMOS: Basic concepts, applications, and programming. New York, NY: Routledge.
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Modeling Multidisciplinary J. 14, 464–504. doi: 10.1080/10705510701301834
Churchill, G. A. (1979). A paradigm for developing better measures of marketing constructs. J. Mark. Res. 16, 64–73. doi: 10.2307/3150876
Corley, M. C. (1995). Moral distress of critical care nurses. Am. J. Crit. Care 4, 280–285. doi: 10.4037/ajcc1995.4.4.280
Corley, M. C. (2002). Nurse moral distress: A proposed theory and research agenda. Nursing Ethics 9, 636–650. doi: 10.1191/0969733002ne557oa
Corley, M. C., Elswick, R. K., Gorman, M., and Clor, T. (2001). Development and evaluation of a moral distress scale. J. Adv. Nurs. 33, 250–256. doi: 10.1046/j.1365-2648.2001.01658.x
Coughlin, M. E. (2021). Transformative nursing in the NICU: Trauma-informed, age-appropriate care, 2nd Edn. Berlin: Springer.
Cunha, C. M., Almeida Neto, O. P., and Stackfleth, R. (2016). Main psychometric evaluation methods of measuring instruments reliability. Revista Atenção à Saúde 14, 98–103. doi: 10.13037/ras.vol14n49.3671
Delfrate, F., Ferrara, P., Spotti, D., Terzoni, S., Lamiani, G., Canciani, E., et al. (2018). Moral distress (MD) and burnout in mental health nurses: A multicenter survey. Medicina del Lavoro 109, 97–109. doi: 10.23749/mdl.v109i2.6876
Dzeng, E., Colaianni, A., Roland, M., Chander, G., Smith, T. J., Kelly, M. P., et al. (2015). Influence of institutional culture and policies on do-not-resuscitate decision making at the end of life. JAMA Internal Med. 175, 812–819. doi: 10.1001/jamainternmed.2015.0295
Eagle, K. A., Vaishnava, P., and Froehlich, J. B. (2015). Perioperative cardiovascular care for patients undergoing noncardiac surgical intervention. JAMA Internal Med. 175, 835–839. doi: 10.1001/jamainternmed.2015.0150
Epstein, E. G., and Hamric, A. B. (2009). Moral distress, moral residue, and the crescendo effect. J. Clin. Ethics 20, 330–342. doi: 10.1086/JCE200920406
Epstein, E. G., Whitehead, P. B., Prompahakul, C., Thacker, L. R., and Hamric, A. B. (2019). Enhancing understanding of moral distress: The measure of moral distress for health care professionals. AJOB Empirical Bioethics 10, 113–124. doi: 10.1080/23294515.2019.1586008
Ferrell, B. R. (2006). Understanding the moral distress of nurses witnessing medically futile care. Oncol. Nurs. Forum 33, 922–930. doi: 10.1188/06.ONF.922-930
Fujii, T., Katayama, S., Miyazaki, K., Nashiki, H., Niitsu, T., Takei, T., et al. (2021). Translation and validation of the Japanese version of the measure of moral distress for healthcare professionals. Health Qual. Life Outcomes 19:120. doi: 10.1186/s12955-021-01765-1
Godshall, M. (2021). Coping with moral distress during COVID-19. Nursing 51, 55–58. doi: 10.1097/01.NURSE.0000731840.43661.99
Haghighinezhad, G., Atashzadeh-Shoorideh, F., Ashktorab, T., Mohtashami, J., and Barkhordari-Sharifabad, M. (2019). Relationship between perceived organizational justice and moral distress in intensive care unit nurses. Nurs. Ethics 26, 460–470. doi: 10.1177/0969733017712082
Hair, J., Black, W., Babin, B., and Anderson, R. (2018). Multivariate data analysis, 8th Edn. Boston, MA: Cengage Learning EMEA.
Hamric, A. B. (2010). Moral distress and nurse-physician relationships. Virtual Mentor 12, 6–11. doi: 10.1001/virtualmentor.2010.12.1.ccas1-1001
Hamric, A. B., and Blackhall, L. J. (2007). Nurse-physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Crit. Care Med. 35, 422–429. doi: 10.1097/01.CCM.0000254722.50608.2D
Hamric, A. B., and Epstein, E. G. (2017). A health system-wide moral distress consultation service: Development and evaluation. HEC Forum 29, 127–143. doi: 10.1007/s10730-016-9315-y
Hamric, A. B., Borchers, C. T., and Epstein, E. G. (2012). Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Primary Res. 3, 1–9. doi: 10.1080/21507716.2011.652337
Hooper, D., Coughlan, J., and Mullen, M. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic J. Bus. Res. Methods 6, 53–60.
Horton, K., Tschudin, V., and Forget, A. (2007). The value of nursing: A literature review. Nurs. Ethics 14, 716–740. doi: 10.1177/0969733007082112
Hu, L., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidisciplinary J. 6, 1–55. doi: 10.1080/10705519909540118
Huffman, D. M., and Rittenmeyer, L. (2012). How professional nurses working in hospital environments experience moral distress: A systematic review. Crit. Care Nurs. Clin. North Am. 24, 91–100. doi: 10.1016/j.ccell.2012.01.004
Jameton, A. (1993). Dilemmas of moral distress: Moral responsibility and nursing practice. AWHONN’s Clin. Issues Perinat. Women’s Health Nurs. 4, 542–551.
Jameton, A. (2017). What moral distress in nursing history could suggest about the future of health care. AMA J. Ethics 19, 617–628. doi: 10.1001/journalofethics.2017.19.6.mhst1-1706
Jansen, T. L., Hem, M. H., Dambolt, L. J., and Hanssen, I. (2020). Moral distress in acute psychiatric nursing: Multifaceted dilemmas and demands. Nurs. Ethics 27, 1315–1326. doi: 10.1177/0969733019877526
Johnstone, M. J., and Hutchinson, A. (2015). “Moral distress”—Time to abandon a flawed nursing construct? Nurs. Ethics 22, 5–14. doi: 10.1177/0969733013505312
Kaiser, H. F. (1970). A second generation Little Jiffy. Psychometrika 35, 401–417. doi: 10.1007/BF02291817
Kaiser, H. F., and Rice, J. (1974). Little Jiffy, Mark IV. Educ. Psychol. Meas. 34, 111–117. doi: 10.1177/001316447403400115
Kline, R. B. (2016). Principles and practice of structural equation modeling, 4th Edn. New York, NY: The Guilford Press.
Ko, H.-K., Chin, C.-C., Hsu, M.-T., and Lee, S.-L. (2018). Phenomenon of moral distress through the aspect of interpretive interactionism. Nurs. Ethics 26, 1484–1493. doi: 10.1177/0969733018766579
Koufteros, X. A. (1999). Testing a model of pull production: A paradigm for manufacturing research using structural equation modeling. J. Operations Manag. 17, 467–488. doi: 10.1016/S0272-6963(99)00002-9
Kramer, E. J., Kwong, K., Lee, E., and Chung, H. (2002). Cultural factors influencing the mental health of Asian Americans. Western J. Med. 176, 227–231.
Lachman, V. D. (2016). Moral resilience: Managing and preventing moral distress and moral residue. Medsurg Nurs. 25, 121–124.
Lamiani, G., Borghi, L., and Argentero, P. (2017). When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. J. Health Psychol. 22, 51–67. doi: 10.1177/1359105315595120
Malhotra, N. K. (2008). Pesquisa de marketing: Uma orientação aplicada [Marketing research: An applied orientation], 6th Edn. São Paulo: Bookman. Portuguese
McCarthy, J., and Gastmans, C. (2015). Moral distress: A review of the argument-based nursing ethics literature. Nurs. Ethics 22, 131–152. doi: 10.1177/0969733014557139
Musto, L. C., Rodney, P. A., and Vanderheide, R. (2015). Toward interventions to address moral distress: Navigating structure and agency. Nurs. Ethics 22, 91–102. doi: 10.1177/0969733014534879
Oh, Y., and Gastmans, C. (2015). Moral distress experienced by nurses: A quantitative literature review. Nurs. Ethics 22, 15–31. doi: 10.1177/0969733013502803
Pallant, J. (2013). SPSS survival manual: A step by step guide to data analysis using SPSS, 4th Edn. Crows Nest, NSW: Allen & Unwin.
Parker, G., and Tavella, G. (2021). Burnout: Modeling, measuring, and managing. Australas. Psychiatry 29, 625–627. doi: 10.1177/10398562211037332
Picconi, L., Fairfield, B., Sergi, M. R., Cataldi, F., Padulo, C., Brugnera, A., et al. (2023). Development and validation of a short form of the Geriatric Anxiety Scale (GAS-12) among Italian older adults. Clin. Gerontol. 46, 544–560. doi: 10.1080/07317115.2022.2120445
Prentice, T., Janvier, A., Gillam, L., and Davis, P. G. (2016). Moral distress within neonatal and paediatric intensive care units: A systematic review. Arch. Dis. Childh. 101, 701–708. doi: 10.1136/archdischild-2015-309410
Rice, E. M., Rady, M. Y., Hamrick, A., Verheijde, J. L., and Pendergast, D. K. (2008). Determinants of moral distress in medical and surgical nurses at an adult acute tertiary care hospital. J. Nurs. Manag. 16, 360–373. doi: 10.1111/j.1365-2834.2007.00798.x
Rushton, C. H. (2018). Moral resilience: Transforming moral suffering in healthcare. New York, NY: Oxford University Press.
Salari, N., Shohaimi, S., Khaledi-Paveh, B., Kazeminia, M., Bazrafshan, M. R., and Mohammadi, M. (2022). The severity of moral distress in nurses: A systematic review and meta-analysis. Philos. Ethics Humanit. Med. 17:13. doi: 10.1186/s13010-022-00126-0
Schermelleh-Engel, K., and Moosbrugger, H. (2003). Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 8, 23–74. doi: 10.23668/psycharchives.12784
Schumacker, R. E., and Lomax, R. G. (2010). A beginner’s guide to structural equation modeling, 3rd Edn. New York, NY: Routledge.
Sporrong, S. K., Höglund, A. T., and Arnetz, B. (2006). Measuring moral distress in pharmacy and clinical practice. Nurs. Ethics 13, 416–427. doi: 10.1191/0969733006ne880oa
Tabachnick, B. G., and Fidell, L. S. (2007). Using multivariate statistics, 5th Edn. New York, NY: Allyn and Bacon.
Tian, X., Jin, Y., Chen, H., and Jiménez-Herrera, M. F. (2021). Instruments for detecting moral distress in clinical nurses: A systematic review. Inquiry 58:46958021996499. doi: 10.1177/0046958021996499
Topol, E. J. (2013). The creative destruction of medicine: How the digital revolution will create better healthcare. New York, NY: Basic Books.
Tucker, L. R., and Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika 38, 1–10. doi: 10.1007/BF02291170
Ulrich, C. M., Hamric, A. B., and Grady, C. (2010a). Moral distress: A growing problem in the health professions? Hastings Center Rep. 40, 20–22. doi: 10.1353/hcr.0.0222
Ulrich, C. M., Taylor, C., Soeken, K., O’Donnell, P., Farrar, A., Danis, M., et al. (2010b). Everyday ethics: Ethical issues and stress in nursing practice. J. Adv. Nurs. 66, 2510–2519. doi: 10.1111/j.1365-2648.2010.05425.x
Wheaton, B., Muthen, B., Alwin, D. F., and Summers, G. (1977). Assessing reliability and stability in panel models. Sociol. Methodol. 8, 84–136. doi: 10.2307/270754
Whitehead, P. B., Herbertson, R. K., Hamric, A. B., Epstein, E. G., and Fisher, J. M. (2015). Moral distress among healthcare professionals: Report of an institution-wide survey. J. Nurs. Scholarship 47, 117–125. doi: 10.1111/jnu.12115
Wilson, M. A., Goettemoeller, D. M., Bevan, N. A., and McCord, J. M. (2013). Moral distress: Levels, coping and preferred interventions in critical care and transitional care nurses. J. Clin. Nurs. 22, 1455–1466. doi: 10.1111/jocn.12128
Wocial, L. D., and Weaver, M. T. (2013). Development and psychometric testing of a new tool for detecting moral distress: the moral distress thermometer. J. Adv. Nurs. 69, 167–174. doi: 10.1111/j.1365-2648.2012.06036.x
Yeh, M. Y., Wu, S. M., and Che, H. L. (2010). Cultural and hierarchical influences: Ethical issues faced by Taiwanese nursing students. Med. Educ. 44, 475–484. doi: 10.1111/j.1365-2923.2009.03589.x
Keywords: moral distress, scale development, healthcare education, psychometric validation, factor analysis
Citation: Liao H-C and Wang Y-H (2025) Psychometric development of a moral distress scale for healthcare education and practice. Front. Psychol. 16:1661414. doi: 10.3389/fpsyg.2025.1661414
Received: 07 July 2025; Accepted: 05 September 2025;
Published: 26 September 2025.
Edited by:
Dubravka Svetina Valdivia, Indiana University Bloomington, United StatesReviewed by:
Maria Rita Sergi, Università degli Studi “Gabriele d’Annunzio”, ItalyMehrdad Esmailian, Isfahan University of Medical Sciences, Iran
Copyright © 2025 Liao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ya-Huei Wang, eWh1ZWlAY3NtdS5lZHUudHc=
 Hung-Chang Liao
Hung-Chang Liao Ya-Huei Wang
Ya-Huei Wang