- Renmin Hospital of Wuhan University, Wuhan, China
Objectives: Exploring Factors Influencing the Level of Hope in Stroke Patients and Its Relationship with Social Participation.
Methods: We conducted a cross-sectional study at Wuhan University People’s Hospital from March to June 2024 and performed a correlation analysis on the sample data. Using convenience sampling, we enrolled 122 stroke patients who met the inclusion criteria. Participants completed questionnaires assessing social participation (Impact on Participation and Autonomy Questionnaire, IPA), hope (Herth Hope Index, HHI), activities of daily living (Barthel Index), and sociodemographic/disease characteristics. Data were analyzed using SPSS 26.0 with descriptive statistics, t-tests, ANOVA, Pearson correlation, and multiple linear regression. All statistical tests were two-tailed with significance set at p < 0.05. Effect sizes were reported with 95% confidence intervals.
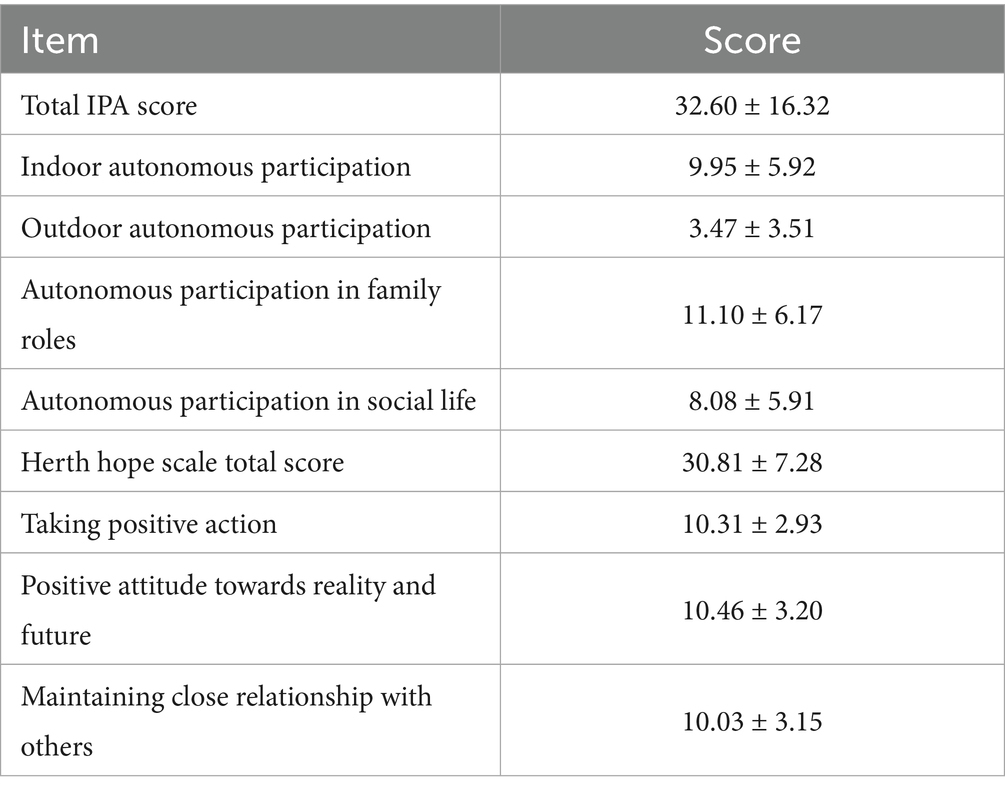
Results: Participants demonstrated moderate social participation impairment (IPA: 32.60 ± 16.32), with the most pronounced limitations in autonomous participation in family roles (subscore: 11.10 ± 6.17). Hope levels averaged within the moderate range (HHI: 30.81 ± 7.28). Furthermore, significant negative correlations existed between all dimensions of social participation and all dimensions of hope (p < 0.01). Regression analysis indicated that Barthel Index and social participation were key factors influencing hope levels among stroke patients.
Conclusion: This study demonstrates that stroke survivors exhibit moderate impairments in social participation and hope levels. These findings suggest that rehabilitation programs should prioritize social participation enhancement while providing targeted interventions for female patients and those with lower socioeconomic status or poorer functional ability. Further longitudinal research is needed to establish causal relationships and optimize intervention strategies.
1 Introduction
Stroke is the second leading cause of death in the world and the third leading cause of death and disability combined. The global cost of stroke is estimated to exceed $721 billion (0.66% of global GDP) (Nandan et al., 2023). Acute stroke patients often suffer from varying degrees of psychological disorders, neurological deficits, and limitations in performing daily living tasks, and most survivors retain varying degrees of disability despite effective rehabilitation and treatment (Wu et al., 2019), with participation dysfunction being the most prominent sequela (Cieza and Kostansjek, 2021). Social participation, an important outcome indicator of disease recovery (Pokryszko-Dragan et al., 2020), refers to participation in life situations, which is the behavioral process and subjective experience of an individual who actively participates in family or social activities and integrates into the family or social environment (Qu et al., 2024). Limited social participation can negatively affect patients’ mental health and life satisfaction, among others (Ge et al., 1844). Studies have shown (Masuccio et al., 2024) that the level of social participation can contribute to emotional regulation, enhance rehabilitation potential, and promote stroke recovery. Hope is a potential psychological force that influences people’s behavior and the way they deal with things, and different levels of hope can reflect different attitudes toward the disease (Western, 2007). Hopeful beliefs can make stroke patients feel confident and courageous, helping them adapt to and overcome difficulties (Ni et al., 2021). The higher the level of hope, the more positive the patients’ attitude toward the disease. The opposite is true for patients with low levels of hope. Systematic reviews (Kruithof et al., 2013; Northcott et al., 2016) have found associations between poor social support and depression, reduced quality of life, and worse physical recovery among stroke survivors. Perceived social support shows significant temporal associations with greater community participation (Erler et al., 2019), lower depression levels (Volz et al., 2016), and better functional status following stroke onset (Tsouna-Hadjis et al., 2000; Villain et al., 2017). Hope may be an essential coping strategy and a psychological resource for patients with chronic illness, including stroke survivors. Most relevant studies (Alaszewski and Wilkinson, 2015; Bright et al., 2020; Bright et al., 2011; Cross and Schneider, 2010; Levy et al., 2022; Soundy et al., 2014; Tutton et al., 2012; Visvanathan et al., 2019) have adopted a qualitative approach to investigate the relevance of hope in the perspectives and recovery experiences of stroke survivors. Additionally, impaired functional status increases patients’ emotional distress, feelings of hopelessness, and perceived stress while hindering social interactions and the rehabilitation process (Fong et al., 2022). Therefore, the degree of disability in stroke patients may influence their level of hope.
To our knowledge, no empirical studies have examined the relationship between social participation feeling and hope or the potential mediating role of hope in improving the functional outcomes of stroke survivors. This study aims to: (1) assess social participation and hope levels in stroke survivors, (2) examine their interrelationship, and (3) identify modifiable associated factor of hope to develop evidence-based nursing interventions for improving psychosocial outcomes.
2 Materials and methods
2.1 Participants
This cross-sectional study employed correlation analysis to examine the relationships between key variable. The study was approved by the Ethics Committee of Renmin Hospital of Wuhan University (approval number: WDRY2024-K065). The study was conducted in accordance with the Declaration of Helsinki. Stroke patients admitted to the People’s Hospital of Wuhan University from March and June 2024 were selected for the study using a convenience sampling method. Inclusion criteria: (1) those who had cerebral infarction or cerebral hemorrhage confirmed by CT or MRI and met the diagnostic criteria in the Chinese guidelines for the diagnosis and treatment of acute stroke (Liu et al., 2023); (2) aged ≥18 years (3) non-acute stage, currently in stable condition, clearly conscious, with normal speech comprehension; and (4) patients who gave informed consent to this study and participated voluntarily. Exclusion criteria: (1) suffering from mental illness or mild cognitive impairment, unable to cooperate with the study; (2) suffering from disabilities, malignant tumors, and other serious physical diseases or other cerebrovascular diseases such as Parkinson’s, epilepsy, etc.; (3) complaining of severely impaired vision and hearing.
The researchers explained the study’s purpose and significance to participants, emphasizing that their participation was anonymous, data would remain confidential, and results would be used solely for research purposes. After obtaining informed consent from the patient, the questionnaire was distributed, and the on-site survey was conducted in a one-on-one format. Patients completed the survey independently and objectively. If they encountered difficulties, the investigators assisted by reading the questions aloud and recording their responses. The questionnaires were collected on the spot, and a total of 130 questionnaires were distributed, of which eight questionnaires were excluded: 5 for the same answers for each question, and 3 for deviation from the inclusion criteria. And the valid recovery rate of the questionnaires was 93.84%.
2.2 Measures
2.2.1 Demographic data
Sociodemographic and clinical characteristics of stroke patients were collected during rehabilitation, including gender, age, religion, marital status, residential area (urban/rural), education level, health insurance type, employment status, monthly household income per capita, stroke type (ischemic/hemorrhagic), first-onset status, and number of post-stroke sequelae (e.g., hemiplegia, speech impairment, sensory deficits, and dysphagia).
2.2.2 Social participation
The Impact on Participation and Autonomy (IPA) questionnaire (He et al., 2025) was used for the survey. The scale consists of 25 items with four dimensions, namely, indoor autonomy (7 items), outdoor autonomy (5 items), family role autonomy (7 items), and social life autonomy (6 items). Each item was assigned a score from 0 to 4, ranging from “very likely to participate” to “very unlikely to participate,” with higher scores indicating poorer levels of social participation. Previous validation studies have established the scale’s strong reliability and validity. The most recent evaluation reported a Cronbach’s alpha coefficient of 0.962 (He et al., 2025), confirming its internal consistency. This instrument has been extensively utilized across various clinical research contexts. In this study, Cronbach’s coefffcient α for the IPA scale was 0.924, with the values of α for the dimensions ranging from 0.834 to 0.878.
2.2.3 Hope
Hope was measured using the Herth Hope Index (HHI) (Snyder et al., 1991), which consists of 12 items and three dimensions: a positive attitude towards reality and the future, taking positive action, and maintaining close relationships with others. The Herth Hope Index (HHI) utilizes a 4-point Likert scale (1 = completely disagree to 4 = completely agree), with items 3 and 6 reverse-scored. Total scores are calculated by summing all items, where higher scores indicate greater levels of hope. All 12 items had a significant loading on one of the three factors as originally formed subscales of the HHS. The HHI has a high level of reliability with reported Cronbach’s alpha ranging from 0.74 to 0.84, and ranging from 0.77 to 0.79 in the present study (Dorsett et al., 2017). In this study, Cronbach’s α for the HHI scale was 0.82, and the Cronbach’s α for the dimensions were between 0.780 and 0.827.
2.2.4 Barthel index
This scale is the most frequently used clinical method for assessing self-care ability. It focuses on seven self-management activities, including eating, dressing, personal hygiene, toileting, bathing, bowel control, and urination control. In addition, three mobility activities were focused on, namely bed and chair transfers, walking, and walking up and down stairs. Different items and levels are scored 0, 5, 10, and 15 out of a total of 100 points. Self-care scoring criteria: 60 or more points are considered basic self-care; 40–60 points are considered as needing help; <40 points are considered as basically needing full help. The Cronbach’s α coefficient for the Barthel Index is 0.860 (Cid-Ruzafa and Damián-Moreno, 1997). In this study, Cronbach’s coefffcient α for the BI was 0.885.
2.3 Data analysis
Statistical analyses were performed using SPSS 26.0 (IBM Corp, Armonk, NY). Categorical variables were presented as frequencies and percentages. We performed the Kolmogorov—Smirnov test to assess normality of distribution. Descriptive statistics characterized the subjects’ sociodemographic characteristics: categorical variables were presented as counts and percentages, while continuous variables were expressed as mean ± standard deviation (SD). Between-group comparisons were conducted using independent samples t-tests (two groups) or one-way ANOVA (multiple groups). Pearson correlation analysis examined relationships between hope levels and social participation. Multiple linear regression analysis assessed the influence of demographic characteristics and social participation on hope levels. A two-tailed p-value <0.05 was considered statistically significant.
3 Results
3.1 Stroke patients’ level of social participation and level of hope scores
The total social participation level of the 122 patients was (32.60 ± 16.32); the total hope level was (30.81 ± 7.28) (see Table 1).
3.2 Comparison of Herth Hope Scale scores of stroke patients with different general information
The results showed that the comparison of Herth Hope Scale scores of stroke patients with different genders, educational levels, family income levels, and Barthel indexes showed statistically significant differences (p < 0.01) (see Table 2).
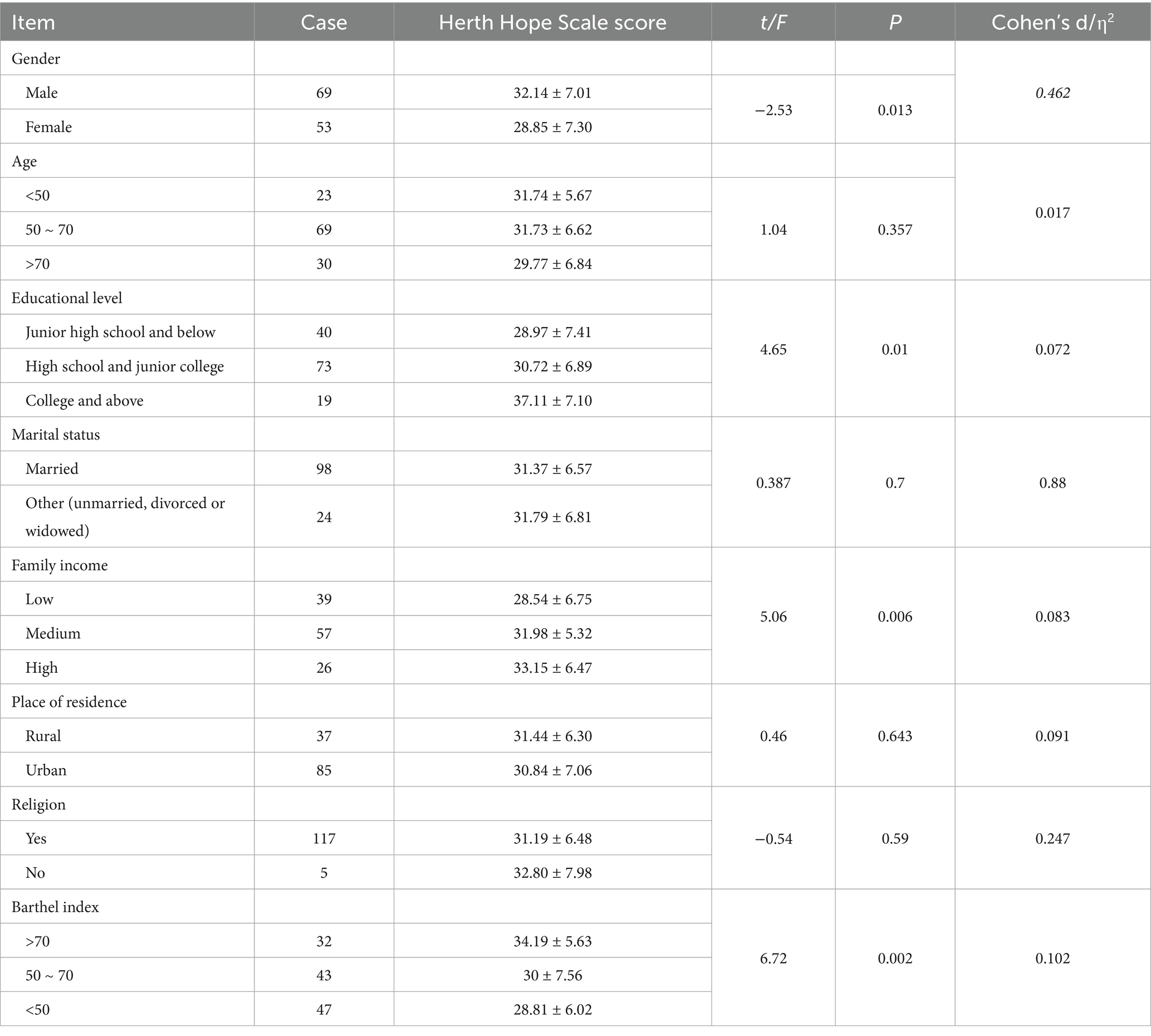
Table 2. Comparison of Herth Hope Scale scores in 122 stroke patients with different general information (score, x ± s).
A total of 122 participants completed the questionnaire in this study. Among them, 56.56% were male; 18.85% were under 50 years old; 32.79% had an educational attainment of junior high school or below; and 80.33% were married. Other demographic characteristics of the participants are shown in Table 2. The results showed that the comparison of Herth Hope Scale scores of stroke patients with different genders, educational levels, family income levels, and Barthel indexes showed statistically significant differences (p < 0.01) (see Table 2).
3.3 Correlation analysis between the level of social participation and the level of hope of stroke patients
Spearman correlation analysis revealed that social participation in stroke patients showed significant negative correlations with the total Hope Scale score and all subscale dimensions (p < 0.05). Scores for taking proactive actions and maintaining a positive attitude towards reality and future exhibited significant negative correlations with all four dimensions of the IPA (p < 0.05). Maintaining close relationships with others showed significant negative correlations with all other IPA dimensions except the outdoor independent participation dimension, as shown in Table 3.
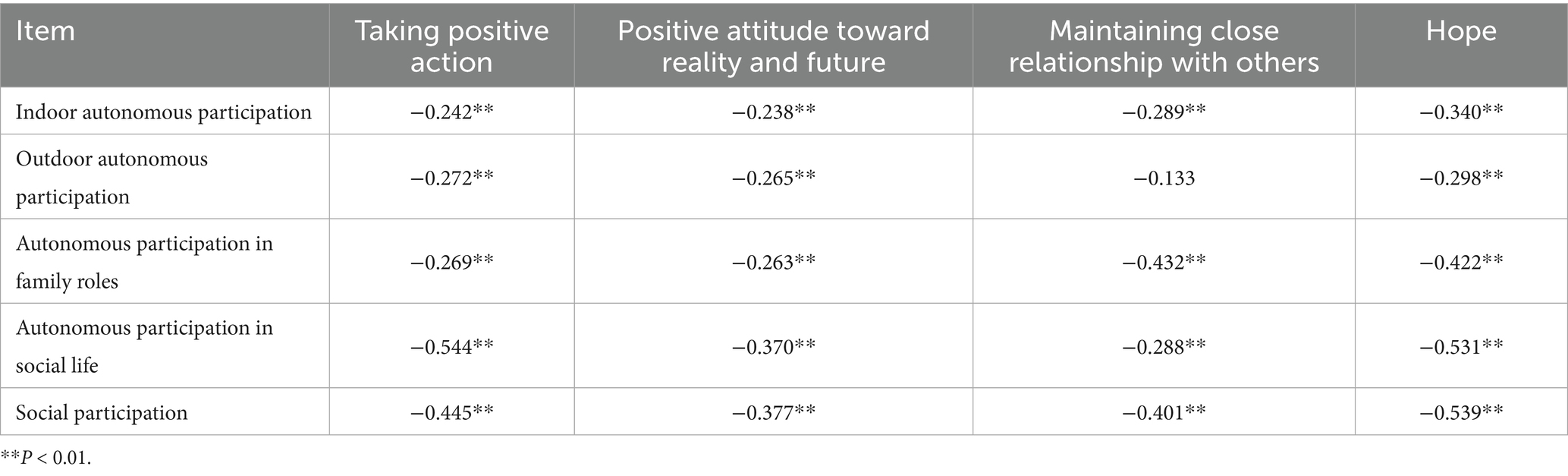
Table 3. Correlation analysis between social participation and level of hope in 122 stroke patients (r-value).
3.4 Multiple linear regression analysis of the influence of general information and social participation level of stroke patients on their hope level
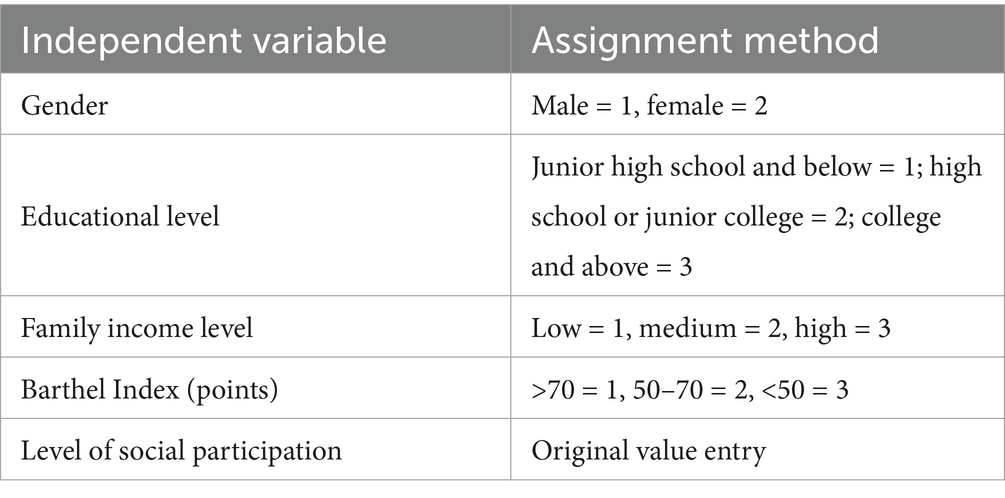
Multiple linear regression analysis was carried out with the variables with statistically significant differences in the univariate analysis and the social participation level as the independent variables, and with the total score of the Herth Hope Scale of patients as the dependent variable, and the method of assigning the values of the independent variables is shown in Table 4.
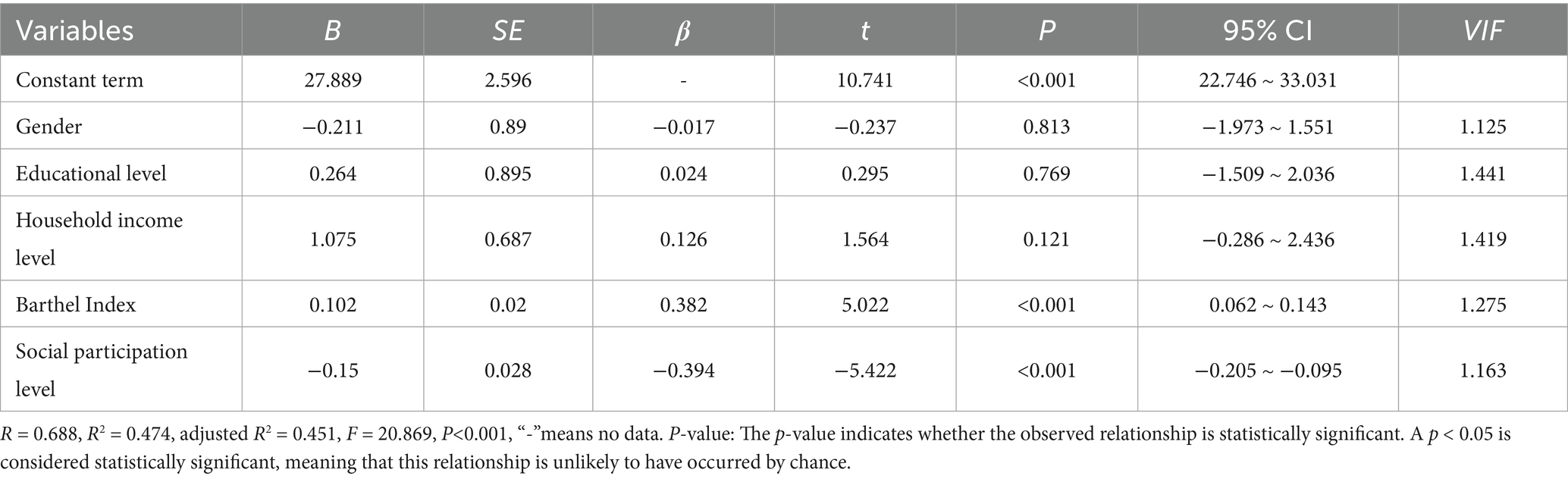
Multicollinearity tests revealed that the variance inflation factor values for all included variables were below 10.0, confirming the absence of multicollinearity among variables. The Durbin-Watson statistic was 1.798, falling within the acceptable range of 0–4 and indicating independent data. Furthermore, residual analysis demonstrated that residuals followed a normal distribution. The results of the multiple linear regression analysis revealed that the Barthel Index and social participation were significant predictors of stroke patients’ desired level of functioning (p < 0.05) after inclusion in the regression equation, explaining 47.4% of the total variance. This finding indicates that the Barthel Index and social participation are key factors influencing stroke patients’ desired level of functioning (see Table 5 for details).
4 Discussion
4.1 Current status of social participation of stroke patients
In this study, stroke patients’ total social participation score was 32.60 ± 16.32, indicating a relatively low level in real-world settings, suggesting that stroke patients generally exhibit good social participation and autonomy. Across various dimensions, patients demonstrated strong performance in indoor activities, outdoor activities, autonomy in social life, and autonomy in general household roles. Multiple studies indicate that advances in healthcare and rehabilitation technologies have significantly increased opportunities for stroke patients to engage in diverse indoor and outdoor activities. VR-based rehabilitation therapy enables stroke patients to engage in realistic scenarios within a safe environment, thereby enhancing motivation, compliance, and neuroplasticity. This approach facilitates improvements in patients’ ability to perform daily tasks both indoors and outdoors (Aderinto et al., 2023). Furthermore, the implementation of personalized rehabilitation plans can enhance functional status, balance, mobility, and walking ability post-stroke, increasing participation in both indoor and outdoor activities (Langhammer and Lindmark, 2012). Reduced family role participation may reflect overprotection by caregivers and decreased household activity involvement (Šaňák et al., 2024). Conversely, patients received heightened social support post-stroke, leaving social relationships less affected (Deb-Chatterji et al., 2022), explaining the higher social autonomy scores. Prior research (Gurková et al., 2025) indicates that enhanced social participation improves quality of life.
4.2 Current status of hope levels in stroke patients
Hope represents a fundamental psychological construct that persists across the lifespan, reflecting an individual’s goal-directed expectations and motivations (Wu et al., 2025). The results of this study showed that the total score of hope level of stroke patients was (30.81 ± 7.28), which was above the medium level, and the hope level of stroke patients was affected by patients’ genders, educational levels, family income levels, and ability to perform activities of daily living (p < 0.05) similar to the results of Boru Sun et al. (2024). Our research indicates that men exhibit slightly higher levels of hope than women. Across diverse cultural contexts, women are often assigned caregiving roles, reflected in their traditional responsibilities for nurturing and household affairs. This transition from “caregiver” to “care recipient” coupled with perceptions of difficulty fulfilling family and parental obligations, leads women to experience more severe anxiety (Röding et al., 2003). This anxiety is significantly correlated with their levels of hope (Wang et al., 2019), thereby diminishing their sense of hope. This finding is inconsistent with the results of Labrosciano et al. (2025), possibly because our study sample size was too small to accurately represent the overall level of hope among stroke patients. Additionally, Matérne et al. (2025) found that men face greater difficulties in adapting after stroke and experience lower quality of life, which is inconsistent with our findings. One possible reason is that this study only included individuals aged 40–64 in its quantitative analysis, primarily focusing on middle-aged stroke patients. On the other hand, it may be because that study (n = 51) shares the same limitation as our study—a sample size too small to adequately represent the overall stroke patient population.
There is a positive correlation between patients’ literacy level and hope level, which may be because patients with a high literacy level have stronger cognition and coping ability to better adjust their mentality and face the disease positively. Patients with good family economic conditions have higher levels of hope. Good economic conditions can provide patients with better medical resources and life protection, reduce the economic and mental burden of patients, and thus raise the level of hope.
Furthermore, the findings of this study indicate that activities of daily living (ADL) capacity can significantly influence the level of hope among stroke patients. This aligns with the results reported by Fong et al. (2022). This may be attributed to the fact that improved ADL capacity fosters patients’ sense of autonomy and self-efficacy, both of which are key contributors to hope (Cheng et al., 2025). Consequently, patients with stronger ADL abilities tend to exhibit higher levels of hope. These results highlight vulnerable patient subgroups requiring targeted psychosocial interventions: older adults, those with limited education, low-income individuals, and patients with severe ADL impairment. Multidisciplinary approaches incorporating cognitive-behavioral strategies, family counseling, and community support programs may effectively enhance hope in these populations.
4.3 Analysis of the correlation between the level of social participation and the level of hope in stroke patients
The results of this study showed that the level of social participation of stroke patients was negatively correlated with the total score and the scores of each dimension of the Herth Hope Scale (p < 0.05). The results of multiple linear regression analysis showed that the level of social participation can positively affect the level of hope of patients. Social participation reflects patients’ perceptions of participation positivity, controlling and realizing their potential, and feeling the difficulties of social participation, which not only focuses on the satisfaction status of individual needs, but also attaches importance to the embodiment of personal social value (Zhou et al., 2022). It has been shown that social participation is conducive to enhancing psychological health (Douglas et al., 2017; Lin and Ren, 2021), life satisfaction, and wellbeing (Sun and Lyu, 2020). Social participation can divert patients’ attention from the role of “patient” and alleviate anxiety and depression (Chen et al., 2022); interaction with family, friends, and society can provide different kinds of resource exchange; work participation can significantly improve patients’ self-esteem and stabilize their emotions, which is important for maintaining positive attitudes and improving life satisfaction (Quan et al., 2016).
Studies have shown (Ge et al., 2021) that implementing interventions for stroke patients can increase the level of hope and adherence to functional exercise, improve neurological function, and enhance the ability to perform activities of daily living. The higher the level of social participation, the easier it is for patients to adapt to the change of social and family roles after the disease, the faster they can adjust their own psychological state (Zhao et al., 2020), and strive to seek medical and family support and help, actively cooperate with clinical treatment and rehabilitation training, and improve their own self-care ability, which is conducive to the improvement of the level of hope. On the contrary, patients with lower levels of social participation, facing different degrees of physical dysfunction, complications, and heavy medical burden, are prone to negative emotions such as low self-esteem and avoidance, so that the level of hope decreases (Mai et al., 2022).
Studies have shown (Zuo et al., 2023) that individuals with a high level of social engagement are more likely to have a desirable outcome when facing external challenges. Healthcare professionals should prioritize assessing the social participation levels of stroke patients and implement targeted cognitive-behavioral interventions. Key objectives include addressing patients’ low self-esteem, mitigating their lack of confidence in rehabilitation, and alleviating concerns about long-term prognosis. By guiding patients to develop accurate perceptions of their health status and fostering realistic expectations about recovery, clinicians can enhance patients’ self-efficacy in disease management. This approach cultivates a resilient, proactive mindset, ultimately elevating hope levels and optimizing health outcomes in stroke survivors.
The hope level among stroke patients remains suboptimal, particularly in females, individuals with lower educational attainment, limited economic income, and impaired activities of daily living. Targeted interventions are needed to enhance patients’ social participation, thereby fostering hope. During rehabilitation, a dual focus on physical recovery and psychological reconstruction is essential. Additionally, modifying patients’ living environments and cultivating supportive social contexts can improve outcomes. Comprehensive assessment and utilization of social support systems are critical to increasing participation rates and perceived engagement, ultimately promoting greater wellbeing.
5 Limitations of the study
First, the cross-sectional design limits the ability to establish a causal relationship between social participation and hope levels. Future longitudinal or mixed-methods studies are needed to determine causal pathways. Secondly, our study’s reliance on univariate significance for variable selection may overlook potential factors, leading to estimation bias. For instance, factors such as age, disease duration, stroke type, and comorbidities may also influence patients’ levels of hope. Future research should theoretically define covariates and construct models to comprehensively assess stroke patients’ levels of hope. Third, the study relied on self-reported questionnaires, which may introduce response bias. Participants’ answers may not accurately reflect actual circumstances. Future studies could incorporate multidimensional hope assessments (e.g., Herth Hope Index, Snyder Hope Scale) to enhance construct validity. Finally, this study employed convenience sampling with a small sample size from a single institution, limiting the generalizability of findings. Future large-scale, multicenter studies are needed to ensure the reliability of research outcomes.
6 Conclusion
This study highlights the critical role of enhancing social participation and hope levels among stroke patients. Findings indicate that both social participation and hope levels among stroke patients are moderate, with a positive correlation between the two. This provides new directions for developing interventions aimed at elevating hope levels in stroke patients.
Additionally, the findings reveal that individual characteristics—such as gender, educational attainment, household income, and activities of daily living (ADL) ability—influence hope levels among stroke patients. Future interventions should therefore be tailored to address these specific characteristics, thereby effectively elevating hope levels in this population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of Renmin Hospital of Wuhan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ML: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TL: Conceptualization, Data curation, Methodology, Supervision, Writing – review & editing. JY: Data curation, Software, Writing – review & editing. JW: Data curation, Writing – review & editing. HW: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research/publication was supported by the Hubei Provincial Health Commission -Renmin Hospital of Wuhan University Joint Fund (Nursing Special Fund) (Grant No. 2023KFH011). The authors sincerely acknowledged the institutional support for this research.
Acknowledgments
The authors gratefully acknowledge all participating patients for their invaluable contributions to this research. We extend our sincere appreciation to our research team members Wang Dan, Wang Lijuan, and He Juanfeng for their dedicated efforts in data collection and manuscript preparation. Special thanks to the clinical staff at Renmin Hospital of Wuhan University for their support throughout the study duration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aderinto, N., Olatunji, G., Abdulbasit, M. O., Edun, M., Aboderin, G., and Egbunu, E. (2023). Exploring the efficacy of virtual reality-based rehabilitation in stroke: a narrative review of current evidence. Ann. Med. 55:2285907. doi: 10.1080/07853890.2023.2285907
Alaszewski, A., and Wilkinson, I. (2015). The paradox of hope for working age adults recovering from stroke. Health 19, 172–187. doi: 10.1177/1363459314555242
Bright, F. A., Kayes, N. M., McCann, C. M., and McPherson, K. M. (2011). Understanding hope after stroke: a systematic review of the literature using concept analysis. Top. Stroke Rehabil. 18, 490–508. doi: 10.1310/tsr1805-490
Bright, F. A. S., McCann, C. M., and Kayes, N. M. (2020). Recalibrating hope: a longitudinal study of the experiences of people with aphasia after stroke. Scand. J. Caring Sci. 34, 428–435. doi: 10.1111/scs.12745
Chen, T. T., Li, J. B., and Yang, Y. (2022). Social determinants affecting changes in mental health of rural-urban migrant population in Chengdu: an Oaxaca-blinder decomposition analysis. Sichuan Da Xue Xue Bao Yi Xue Ban 53, 656–662. doi: 10.12182/20220760303
Cheng, J., Jiang, X., Liao, X., Zhou, L., Qin, L., and Liu, H. (2025). The impact of chronic illness resources, fear of recurrence, hope, and health locus of control on self-management behaviors in post-stroke patients: a cross-sectional study. Front. Med. 12:1598945. doi: 10.3389/fmed.2025.1598945
Cid-Ruzafa, J., and Damián-Moreno, J. (1997). Disability evaluation: Barthel’s index. Rev. Esp. Salud Publica 71, 127–137. doi: 10.1590/S1135-57271997000200004
Cieza, A., and Kostansjek, N. (2021). The international classification of functioning, disability and health: the first 20 years. Dev. Med. Child Neurol. 63:363. doi: 10.1111/dmcn.14799
Cross, A., and Schneider, M. (2010). A preliminary qualitative analysis of the impact of hope on stroke recovery in women. Top. Stroke Rehabil. 17, 484–495. doi: 10.1310/tsr1706-484
Deb-Chatterji, M., Pinho, J., Flottmann, F., Meyer, L., Broocks, G., Brekenfeld, C., et al. (2022). Health-related quality of life after thrombectomy in young-onset versus older stroke patients: a multicenter analysis. J. Neurointerv. Surg. 14, 1145–1150. doi: 10.1136/neurintsurg-2021-017991
Dorsett, P., Geraghty, T., Sinnott, A., and Acland, R. (2017). Hope, coping and psychosocial adjustment after spinal cord injury. Spinal Cord Ser. Cases 3:17046. doi: 10.1038/scsandc.2017.46
Douglas, H., Georgiou, A., and Westbrook, J. (2017). Social participation as an indicator of successful aging: an overview of concepts and their associations with health. Aust. Health Rev. 41, 455–462. doi: 10.1071/ah16038
Erler, K. S., Sullivan, V., McKinnon, S., and Inzana, R. (2019). Social support as a predictor of community participation after stroke. Front. Neurol. 10:1013. doi: 10.3389/fneur.2019.01013
Fong, T. C. T., Lo, T. L. T., and Ho, R. T. H. (2022). Indirect effects of social support and hope on quality of life via emotional distress among stroke survivors: a three-wave structural equation model. Front. Psych. 13:919078. doi: 10.3389/fpsyt.2022.919078
Ge, H., Dong, S., Su, W., Guan, W., Yu, Q., Liu, Y., et al. Relationship between social participation and depressive symptoms in patients with multimorbidity: the chained mediating role of cognitive function and activities of daily living. BMC Public Health 24:1844. doi: 10.1186/s12889-024-19157-7
Ge, C., Zhang, H., Zhu, G., Cao, A., and Zhang, J. (2021). Intervention study of Snyder’s hope theory on the stigma of stroke in young and middle-aged patients: a randomised trial. Ann. Palliat. Med. 10, 5721–5728. doi: 10.21037/apm-21-441
Gurková, E., Bartoníčková, D., Šaňák, D., Šaňáková, Š., Zapletalová, J., and Štureková, L. (2025). Relationship between social support, functional outcomes and health-related quality of life in working-aged adults at three months after ischemic stroke: results from the FRAILTY study. Health Qual. Life Outcomes 23:8. doi: 10.1186/s12955-025-02337-3
He, Y. N., Qin, X. H., Lv, J. H., and Guo, Y. P. (2025). Impact on participation and autonomy questionnaire (IPA): reliability and validity of the Chinese version for stroke survivors. Int. J. Gen. Med. 18, 1721–1729. doi: 10.2147/ijgm.S506798
Kruithof, W. J., van Mierlo, M. L., Visser-Meily, J. M., van Heugten, C. M., and Post, M. W. M. (2013). Associations between social support and stroke survivors’ health-related quality of life--a systematic review. Patient Educ. Couns. 93, 169–176. doi: 10.1016/j.pec.2013.06.003
Labrosciano, K., Dorrian, J., Lowies, B., Russell, R., and Lushington, K. (2025). Adult Hope scale: validation in older adults. Aust. J. Psychol. 77:2532077. doi: 10.1080/00049530.2025.2532077
Langhammer, B., and Lindmark, B. (2012). Functional exercise and physical fitness post stroke: the importance of exercise maintenance for motor control and physical fitness after stroke. Stroke Res. Treat. 2012:864835. doi: 10.1155/2012/864835
Levy, T., Christie, L. J., Killington, M., Laver, K., Crotty, M., and Lannin, N. A. (2022). “Just that four letter word, hope”: stroke survivors’ perspectives of participation in an intensive upper limb exercise program; a qualitative exploration. Physiother. Theory Pract. 38, 1624–1638. doi: 10.1080/09593985.2021.1875525
Lin, H., and Ren, H. (2021). The influence of interpersonal Behaviors and population density on grip strength of elderly people: an analysis of the direct vs. indirect effects via social participation. Front. Public Health 9:755695. doi: 10.3389/fpubh.2021.755695
Liu, L., Li, Z., Zhou, H., Duan, W., Huo, X., Xu, W., et al. (2023). Chinese Stroke Association guidelines for clinical management of ischaemic cerebrovascular diseases: executive summary and 2023 update. Stroke Vasc. Neurol. 8:e3. doi: 10.1136/svn-2023-002998
Mai, S., Cai, J., and Li, L. (2022). Factors associated with access to healthcare services for older adults with limited activities of daily living. Front. Public Health 10:921980. doi: 10.3389/fpubh.2022.921980
Masuccio, F. G., Grange, E., Di Giovanni, R., Rolla, M., and Solaro, C. M. (2024). Post-Stroke depression in older adults: an overview. Drugs. Aging. 41, 303–318. doi: 10.1007/s40266-024-01104-1
Matérne, M., Jarl, G., Simpson, G., Appelros, P., Thermaenius, I., and Lindvall, M. A. (2025). Gender matters: factors important for quality of life in midlife after stroke. Front. Neurol. 16:20250904. doi: 10.3389/fneur.2025.1590900
Nandan, A., Zhou, Y. M., Demoe, L., Waheed, A., Jain, P., and Widjaja, E. (2023). Incidence and risk factors of post-stroke seizures and epilepsy: systematic review and meta-analysis. J. Int. Med. Res. 51:3000605231213231. doi: 10.1177/03000605231213231
Ni, Y., Huang, L., Tong, C., Qian, W., and Fang, Q. (2021). Analysis of the levels of hope and influencing factors in infertile women with first-time and repeated IVF-ET cycles. Reprod. Health 18:200. doi: 10.1186/s12978-021-01248-y
Northcott, S., Moss, B., Harrison, K., and Hilari, K. (2016). A systematic review of the impact of stroke on social support and social networks: associated factors and patterns of change. Clin. Rehabil. 30, 811–831. doi: 10.1177/0269215515602136
Pokryszko-Dragan, A., Marschollek, K., Chojko, A., Karasek, M., Kardyś, A., Marschollek, P., et al. (2020). Social participation of patients with multiple sclerosis. Adv. Clin. Exp. Med. 29, 469–473. doi: 10.17219/acem/115237
Qu, W., Yan, Z., Wei, H., Zhang, S., Wang, X., Liu, M., et al. (2024). Heterogeneity of social participation in patients three months after total knee arthroplasty: a latent profile analysis. BMC Musculoskelet. Disord. 25:619. doi: 10.1186/s12891-024-07744-z
Quan, P., Huang, D., Yu, Y., and Ruiming, L. I. U. (2016). Mediation role of Hope between self-efficacy and subjective well-being. Iran. J. Public Health 45, 390–391.
Röding, J., Lindström, B., Malm, J., and Ohman, A. (2003). Frustrated and invisible--younger stroke patients’ experiences of the rehabilitation process. Disabil. Rehabil. 25, 867–874. doi: 10.1080/0963828031000122276
Šaňák, D., Gurková, E., Štureková, L., Šaňáková, Š., Zapletalová, J., Franc, D., et al. (2024). Quality of life in patients with excellent 3-month clinical outcome after first-ever ischemic stroke: a time to redefine excellent outcome? Eur. Neurol. 87, 1–10. doi: 10.1159/000535685
Snyder, C. R., Harris, C., Anderson, J. R., Holleran, S. A., Irving, L. M., Sigmon, S. T., et al. (1991). The will and the ways: development and validation of an individual-differences measure of hope. J. Pers. Soc. Psychol. 60, 570–585. doi: 10.1037//0022-3514.60.4.570
Soundy, A., Stubbs, B., Freeman, P., Coffee, P., and Roskell, C. (2014). Factors influencing patients’ hope in stroke and spinal cord injury: a narrative review. Int. J. Ther. Rehabil. 21, 210–218. doi: 10.12968/ijtr.2014.21.5.210
Sun, J., and Lyu, S. (2020). Social participation and urban-rural disparity in mental health among older adults in China. J. Affect. Disord. 274, 399–404. doi: 10.1016/j.jad.2020.05.091
Sun, B., Wang, N., Li, K., Yang, Y., and Zhang, F. (2024). The mediating effects of hope on the relationships of social support and self-esteem with psychological resilience in patients with stroke. BMC Psychiatry 24:340. doi: 10.1186/s12888-024-05744-w
Tsouna-Hadjis, E., Vemmos, K. N., Zakopoulos, N., and Stamatelopoulos, S. (2000). First-stroke recovery process: the role of family social support. Arch. Phys. Med. Rehabil. 81, 881–887. doi: 10.1053/apmr.2000.4435
Tutton, E., Seers, K., Langstaff, D., and Westwood, M. (2012). Staff and patient views of the concept of hope on a stroke unit: a qualitative study. J. Adv. Nurs. 68, 2061–2069. doi: 10.1111/j.1365-2648.2011.05899.x
Villain, M., Sibon, I., Renou, P., Poli, M., and Swendsen, J. (2017). Very early social support following mild stroke is associated with emotional and behavioral outcomes three months later. Clin. Rehabil. 31, 135–141. doi: 10.1177/0269215515623600
Visvanathan, A., Mead, G., Dennis, M., Whiteley, W., Doubal, F., and Lawton, J. (2019). Maintaining hope after a disabling stroke: a longitudinal qualitative study of patients’ experiences, views, information needs and approaches towards making treatment decisions. PLoS One 14:e0222500. doi: 10.1371/journal.pone.0222500
Volz, M., Möbus, J., Letsch, C., and Werheid, K. (2016). The influence of early depressive symptoms, social support and decreasing self-efficacy on depression 6 months post-stroke. J. Affect. Disord. 206, 252–255. doi: 10.1016/j.jad.2016.07.041
Wang, X., Shang, S., Yang, H., Ai, H., Wang, Y., Chang, S., et al. (2019). Associations of psychological distress with positive psychological variables and activities of daily living among stroke patients: a cross-sectional study. BMC Psychiatry 19:381. doi: 10.1186/s12888-019-2368-0
Western, H. (2007). Altered living: coping, hope and quality of life after stroke. Br. J. Nurs. 16, 1266–1270. doi: 10.12968/bjon.2007.16.20.27573
Wu, X. J., Ke, K., Liu, H., Zhan, S. P., Wang, L., and He, J. F. (2025). Social isolation in the young and middle-aged patients with stroke: role of social support, family resilience and hope. Front. Psych. 16:1499186. doi: 10.3389/fpsyt.2025.1499186
Wu, S., Wu, B., Liu, M., Chen, Z., Wang, W., Anderson, C. S., et al. (2019). Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 18, 394–405. doi: 10.1016/s1474-4422(18)30500-3
Zhao, Y., Xu, X., Dupre, M. E., Xie, Q., Qiu, L., and Gu, D. (2020). Individual-level factors attributable to urban-rural disparity in mortality among older adults in China. BMC Public Health 20:1472. doi: 10.1186/s12889-020-09574-9
Zhou, X., Du, M., and Hu, Y. (2022). The effect of self-management programs on post-stroke social participation: a systematic review and meta-analysis. Clin. Rehabil. 36, 1141–1152. doi: 10.1177/02692155221095477
Keywords: stroke, rehabilitation, social participation, hope, correlational study
Citation: Liu M, Liu Y, Li T, Yang J, Wang J and Wang H (2025) Association between social participation and hope levels in stroke patients: a cross-sectional study. Front. Psychol. 16:1674893. doi: 10.3389/fpsyg.2025.1674893
Edited by:
Rita Chiaramonte, University of Catania, ItalyReviewed by:
Vahid Yousofvand, Shahid Beheshti University of Medical Sciences, IranShogo Sawamura, Heisei College of Health Sciences, Japan
Copyright © 2025 Liu, Liu, Li, Yang, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Liu, MTUzMzcyMTg4ODhAMTYzLmNvbQ==
 Miao Liu
Miao Liu Yan Liu
Yan Liu Tian Li
Tian Li