- 1Nursing Department, Air Force Medical University, Xi'an, China
- 2Traumatic Orthopedics, Army Hospital, Kashgar, Xinjiang, China
- 3Nursing Department, The PLA 77 Group Army Hospital, Leshan, Sichuan, China
- 4TCM Rehabilitation Department, Army 947 Hospital, Kashgar, Xinjiang, China
- 5Nursing Department, No. 980 Hospital of PLA Joint Logistics Support Force, Shijiazhuang, Hebei, China
Purpose: This study aims to investigate the associations among social support, quality of life, and demoralization in patients with inflammatory bowel disease (IBD), and to test the hypothesized mediating role of social support between quality of life and demoralization.
Methods: A cross-sectional study was conducted using a convenience sampling approach. A total of 293 patients with inflammatory bowel disease (IBD) were recruited from the gastroenterology departments of three tertiary-level hospitals in Xi’an, China, between January and July 2024. Data were collected using a general information questionnaire, the Chinese version of the Demoralization Scale-II (DS-II), the Social Support Rating Scale (SSRS), and the Inflammatory Bowel Disease Questionnaire (IBDQ). Internal consistency reliabilities (Cronbach’s α) were 0.801, 0.825, and 0.986 for the DS-II, SSRS, and IBDQ, respectively. Correlation analyses and structural equation modeling (SEM) with bootstrapping (5,000 resamples, bias-corrected) were used to examine relationships and test mediation.
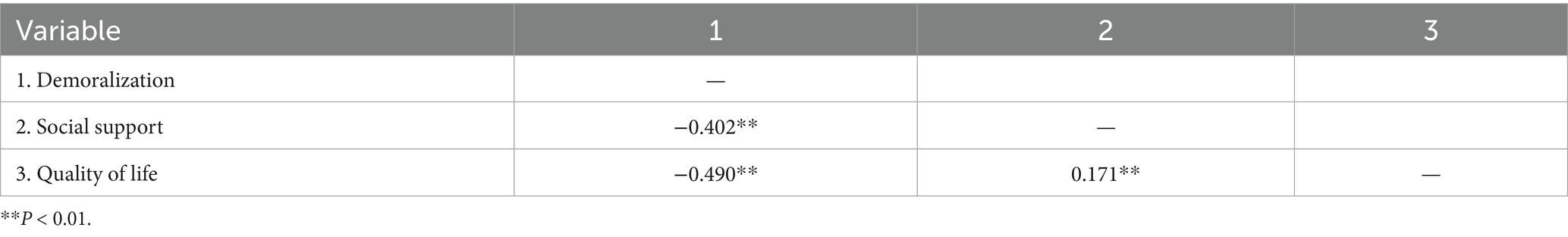
Results: Social support was positively correlated with quality of life (r = 0.171, 95% CI [0.052, 0.285], p < 0.01), and negatively correlated with demoralization (r = −0.402, 95% CI [−0.499, −0.295], p < 0.01). Quality of life was negatively correlated with demoralization (r = −0.490, 95% CI [−0.575, −0.395], p < 0.01). Social support partially mediated the relationship between quality of life and demoralization, accounting for 22.12% of the total effect (indirect effect = −0.125, 95% CI [−0.178, −0.082]).
Conclusion: Social support plays a significant partial mediating role in the relationship between quality of life and demoralization in IBD patients. These cross-sectional findings suggest that interventions aimed at enhancing social support may help mitigate demoralization and improve quality of life, though longitudinal or experimental studies are needed to confirm causal pathways.
1 Introduction
Inflammatory bowel disease (IBD), encompassing Crohn’s disease and ulcerative colitis, is a group of chronic, relapsing–remitting gastrointestinal disorders that impose a substantial burden on patients’ lives (Bisgaard et al., 2022). Beyond significant physical symptoms and complications, IBD profoundly impacts psychosocial well-being, often leading to diminished quality of life—a critical patient-reported outcome and a primary therapeutic goal. The incidence of IBD has been rising globally (Ng et al., 2017), with China now having the highest number of cases in Asia; forecasts suggest the number of IBD patients in China will reach 1.5 million by 2025 (Xu et al., 2023; Zhang, 2020).
A key psychological correlate in this population is demoralization, characterized by feelings of helplessness, hopelessness, loss of meaning, and impaired coping capacity (Frank, 1974). Unlike depression, which emphasizes affective and neurovegetative symptoms, demoralization reflects a subjective inability to cope and loss of purpose, often arising in response to persistent stress or illness (Robinson et al., 2016). This state of existential distress is increasingly recognized as a significant contributor to poor quality of life in chronic illness. Conversely, social support—derived from family, friends, and healthcare providers—represents a crucial psychosocial resource that may buffer stress, foster adaptive coping, and enhance resilience (Zhang, 2020).
Theoretical frameworks such as the Conservation of Resources theory (Hobfoll, 1989) and the Stress-Buffering Model (Cohen and Wills, 1985) posit that social support can mitigate the impact of stressors on mental health. While negative associations between demoralization and quality of life in IBD are established, and the protective role of social support is acknowledged, the mediating mechanisms linking these constructs remain insufficiently elucidated. Specifically, whether social support attenuates the link between demoralization and quality of life in IBD patients is not well understood.
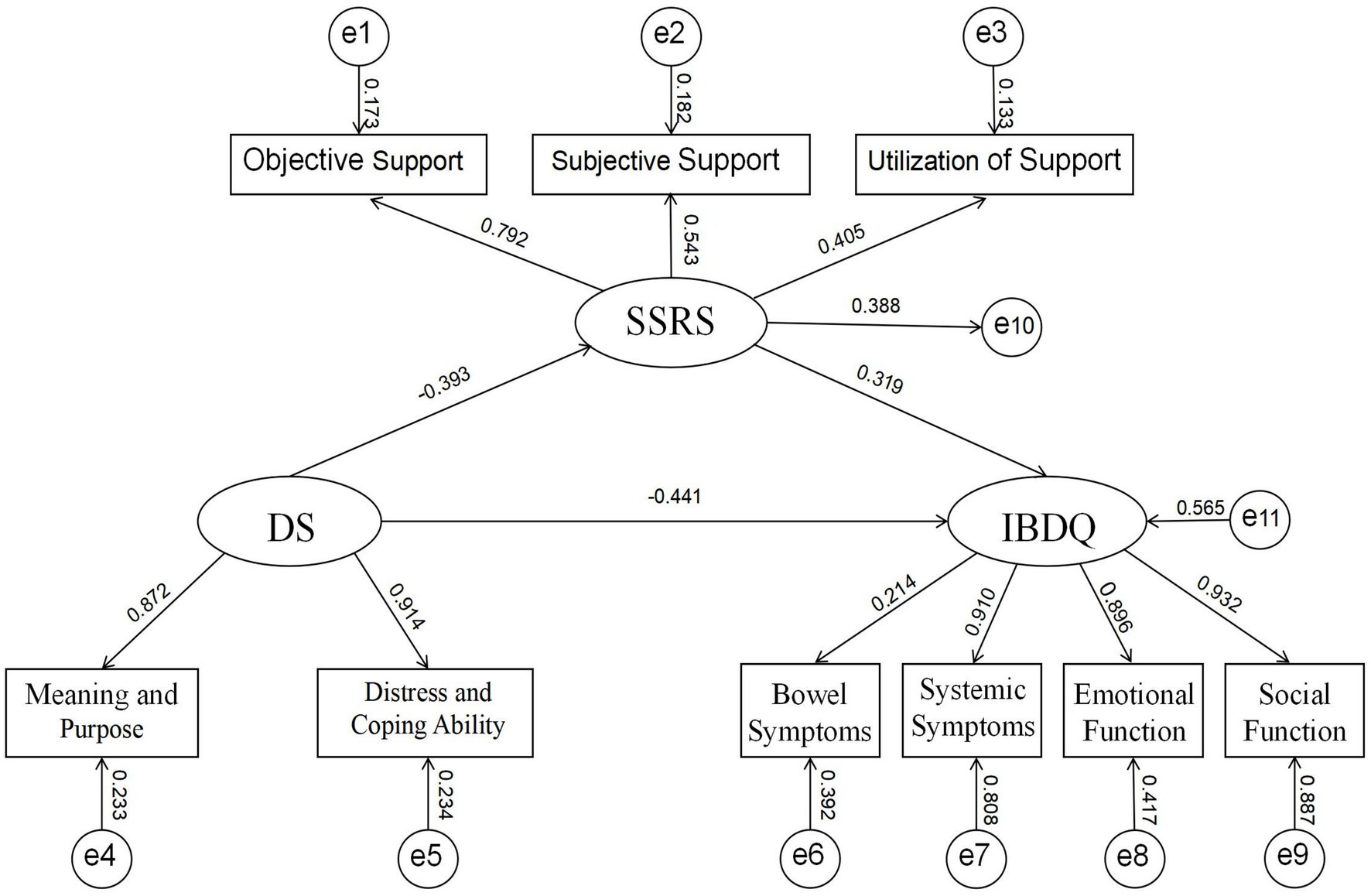
Therefore, this study aims to investigate the associations among quality of life, social support, and demoralization in IBD patients, and to test the hypothesized mediating role of social support between quality of life and demoralization. We propose a theoretical model (Figure 1) in which higher quality of life is associated with greater social support, which in turn is associated with lower demoralization. The findings may inform the development of targeted psychosocial interventions for this population.
2 Materials and methods
2.1 Study design and participants
This was a cross-sectional observational study. A convenience sample of 293 patients with IBD was recruited from the gastroenterology departments of three tertiary hospitals in Xi’an, China, between January and July 2024. Participants included 107 patients in the active phase and 186 in clinical remission.
2.2 Inclusion criteria
(1) Aged ≥18 years;
(2) Diagnosed with IBD according to the Chinese Consensus on Diagnosis and Management of Inflammatory Bowel Disease (Beijing) (Wu et al., 2018);
(3) Cognitively intact with normal verbal communication abilities;
(4) Provided written informed consent.
2.3 Exclusion criteria
(1) Comorbid primary diseases or life-threatening malignancies;
(2) Severe complications (e.g., intestinal obstruction, perforation, or colorectal cancer).
This study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Air Force Medical University (also known as Xijing Hospital) (approval no.: KY20232129-C-1). Written informed consent was obtained from all participants prior to their enrollment in the study.
2.4 Sample size justification
Sample size was estimated using Monte Carlo power analysis for SEM with latent variables, based on anticipated small-to-medium effect sizes (β ≈ 0.20–0.30) for the mediation paths. With 5,000 replications and 80% power at α = 0.05, a minimum of 240 participants was required. Accounting for a 20% attrition rate, 293 participants were enrolled.
2.5 Measures
2.5.1 Demographic and clinical characteristics questionnaire
Developed by the researchers, this tool collected data on age, gender, education, marital status, occupation, payment method, IBD duration, disease phase, and history of IBD-related surgery.
2.5.2 Chinese version of demoralization scale-II (DS-II)
The 16-item DS-II (Robinson et al., 2016) was used in its validated Chinese version (Wu et al., 2021). It assesses two dimensions: Meaning and Purpose (8 items) and Distress and Coping Ability (8 items), rated on a 3-point Likert scale. Total scores range from 0 to 32, with higher scores indicating greater demoralization. Cronbach’s α in this study was 0.801.
2.5.3 Social support rating scale (SSRS)
The 10-item SSRS (Xiao, 1994) assesses Subjective Support (4 items), Objective Support (3 items), and Utilization of Support (3 items). Total scores classify support as low (≤22), medium (23–44), or high (45–66). Cronbach’s α was 0.825 in this study.
2.5.4 Inflammatory bowel disease questionnaire (IBDQ)
The 32-item IBDQ (Guyatt et al., 1989) was used in its Chinese version (Parkes et al., 2025) to assess Bowel Symptoms (10 items), Systemic Symptoms (5 items), Emotional Function (12 items), and Social Function (5 items). Items are scored 1–7; total scores range from 32 to 224, with higher scores indicating better quality of life. Cronbach’s α was 0.986.
2.6 Data collection
A total of 320 questionnaires were distributed. After excluding incomplete or invalid responses, 293 valid questionnaires were retained (effective response rate: 91.56%). Data were double-entered into Excel to ensure accuracy.
2.7 Data quality control
Common method variance was assessed using an unmeasured latent method factor approach, indicating average method variance of 18.3%, below the severe concern threshold. Missing data were minimal (mean rate = 1.2%) and handled using Full Information Maximum Likelihood (FIML) in SEM analyses, supported by sensitivity analyses showing robust results.
2.8 Statistical analysis
Data were analyzed using SPSS 26.0 and AMOS 27.0. Descriptive statistics summarized demographic and clinical characteristics. Pearson correlations examined relationships among key variables. Structural equation modeling (SEM) tested the mediating effect of social support. Model fit was assessed using χ2/df, CFI, TLI, GFI, and RMSEA. Bias-corrected bootstrap analysis (5,000 resamples) was used to test the significance of the indirect effect. Statistical significance was set at p < 0.05 (two-tailed). Assumptions of normality, linearity, and homoscedasticity were checked and met.
3 Results
3.1 Participant characteristics
A total of 293 IBD patients participated (mean age: 44.67 ± 12.93 years; range: 18–82). Other demographic and clinical characteristics are presented in Table 1.
3.2 Quality of life, social support, and demoralization scores
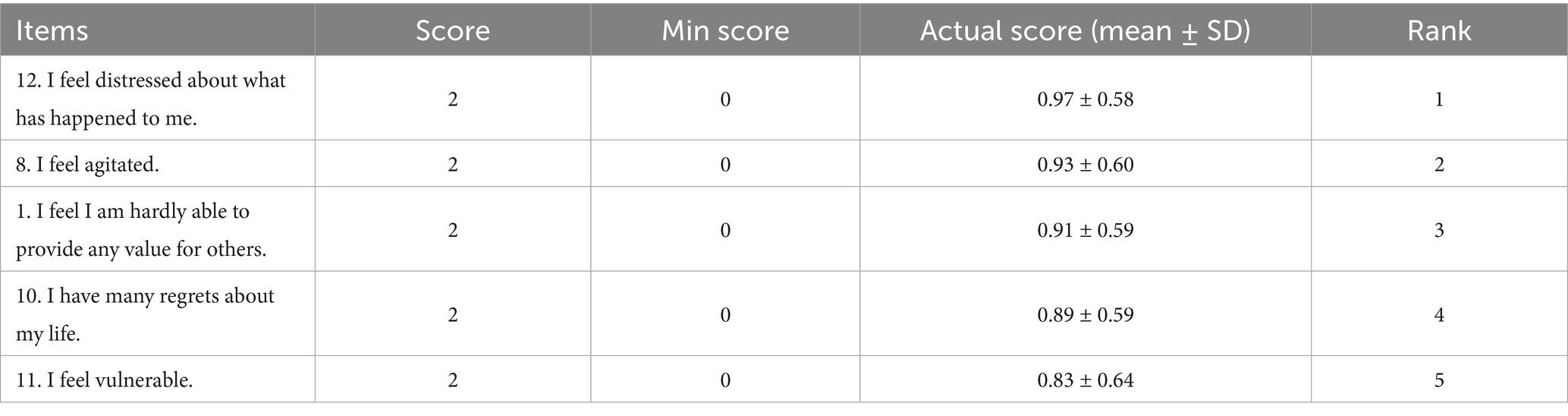
The mean total IBDQ score was 167.01 ± 37.776, indicating a moderate quality of life. The mean SSRS score was 24.23 ± 5.54, indicating moderate-to-low social support. The mean DS-II score was 11.13 ± 6.71, indicating moderate demoralization; 127 patients (43.34%) scored in the moderate range (Wu et al., 2021; Xiao, 1994; Guyatt et al., 1989; Parkes et al., 2025; Byron et al., 2020; Fu et al., 2020; Woźniewicz and Cosci, 2023; Zhu et al., 2021; Vehling and Kissane, 2018; Liu et al., 2024). Dimension scores are shown in Table 2.
3.3 Correlations among key variables
Social support was positively correlated with quality of life (r = 0.171, 95% CI [0.052, 0.285], p < 0.01) and negatively correlated with demoralization (r = −0.402, 95% CI [−0.499, −0.295], p < 0.01). Quality of life was negatively correlated with demoralization (r = −0.490, 95% CI [−0.575, −0.395], p < 0.01) (see Table 3).
3.4 Mediating effect of social support
SEM results supported the hypothesized model (Figure 1). Fit indices were: χ2/df = 2.011, IFI = 0.918, CFI = 0.923, GFI = 0.914, RMSEA = 0.063 (90% CI [0.048, 0.078]), indicating good fit.
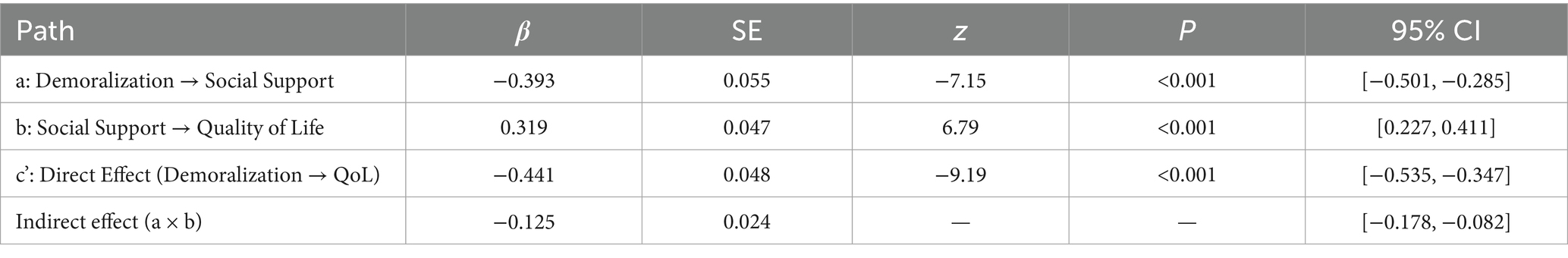
Path coefficients (Table 4) showed:
• Social support positively predicted quality of life (β = 0.319, p < 0.01)
• Demoralization negatively predicted quality of life (β = −0.441, p < 0.01)
• Social support negatively predicted demoralization (β = −0.393, p < 0.01)
The indirect effect was −0.125 (95% CI [−0.178, −0.082]), accounting for 22.12% of the total effect. Bootstrap results confirmed the significance of the mediation.
4 Discussion
4.1 Key findings and theoretical implications
This cross-sectional study confirms the intricate interrelationships among quality of life, social support, and demoralization in Chinese patients with IBD. Consistent with our hypothesis, social support was identified as a significant partial mediator in the relationship between quality of life and demoralization, accounting for 22.12% of the total effect. This finding illuminates a potential psychosocial mechanism, suggesting that the detrimental impact of impaired quality of life on a patient’s psychological state is not only direct but also operates indirectly by eroding the very fabric of their social support system. This aligns with the Conservation of Resources (COR) theory (Hobfoll, 1989), where quality of life can be viewed as a key personal resource. The loss of this resource (poor QoL) may hinder an individual’s capacity to invest in and maintain other critical resources, such as robust social networks, thereby increasing vulnerability to demoralization—a state characterized by resource depletion and an inability to cope effectively.
4.2 The plight of social support and its clinical relevance
The overall level of social support in our cohort was moderate-to-low, with notably deficient scores in the domains of objective support and support utilization. This disparity suggests that patients may perceive available support in theory but face tangible barriers in accessing practical help or are reluctant to actively seek it, potentially due to disease-related stigma or a desire to avoid being a burden (Byron et al., 2020; Fu et al., 2020). This deficiency in actionable support creates a critical intervention point. Our mediation model implies that enhancing tangible social support—such as facilitating access to community services, providing clear information on healthcare navigation, and counseling families on effective support strategies—could disrupt the pathway to demoralization. This approach moves beyond mere emotional reassurance to provide practical resources that bolster a patient’s sense of control and self-efficacy.
4.3 Demoralization in the context of chronic illness
The observed level of demoralization in our sample underscores its clinical significance in IBD, a finding consistent with research in other chronic and life-threatening conditions (Robinson et al., 2016; Zhu et al., 2021). Unlike depression, which is often the focus of clinical attention, demoralization encapsulates the profound existential crisis and loss of purpose that can accompany a relentless, unpredictable disease like IBD. The comparable scores in the Distress and Coping Ability and Meaning and Purpose dimensions reveal that patients are not only struggling with immediate emotional distress but are also grappling with a fractured sense of life meaning and future trajectory (Vehling and Kissane, 2018). This highlights the necessity of integrating meaning-centered interventions or dignity therapy into standard IBD care, aiming to help patients reconstruct a sense of purpose and coherence in life despite their illness.
4.4 The vicious cycle of QoL, social function, and demoralization
The strong negative correlation between demoralization and quality of life, particularly with the emotional and social function domains of the IBDQ, points to a potential vicious cycle. Demoralization can lead to social withdrawal and isolation, which in turn diminishes opportunities for positive social interactions and support, further exacerbating feelings of meaninglessness and hopelessness (Liu et al., 2024). Conversely, impairments in social function due to debilitating symptoms (e.g., urgency, fatigue) can directly fuel demoralization by preventing participation in valued life roles and activities (Byron et al., 2020). Therefore, interventions must be multifaceted, targeting both the intrapersonal dimension (managing emotions, finding meaning) and the interpersonal dimension (facilitating social reintegration, enhancing communication skills) to break this cycle effectively.
4.5 Limitations and future directions
The interpretations of our findings must be considered in light of several limitations. Firstly, the cross-sectional design precludes definitive causal inference. While our model is theoretically grounded, longitudinal or interventional studies are required to confirm the direction of causality and the efficacy of support-focused interventions. Secondly, the use of a convenience sample from tertiary hospitals in one city may limit the generalizability of our findings to the broader IBD population in China. Thirdly, reliance on self-reported measures is susceptible to biases. Future research should incorporate objective clinical indices (e.g., disease activity scores, endoscopic findings) and physician-reported outcomes to triangulate findings. Furthermore, exploring these relationships across different disease phases (active vs. remission) and phenotypes (CD vs. UC) could yield more nuanced insights for personalized care. Finally, qualitative studies are highly recommended to delve deeper into the lived experiences of demoralization and the specific nature of support needs from the patients’ perspective, informing the development of more culturally sensitive and patient-centered interventions.
5 Conclusion
This study provides evidence that social support partially mediates the relationship between quality of life and demoralization in IBD patients. While causal inferences cannot be drawn, the findings suggest that enhancing social support may be a promising target for interventions aimed at reducing demoralization and improving quality of life. Future longitudinal and interventional studies are needed to confirm these pathways and evaluate the efficacy of psychosocial support programs in this population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of the First Affiliated Hospital of Air Force Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JJ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Writing – original draft, Writing – review & editing, Validation, Visualization. HG: Data curation, Funding acquisition, Methodology, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing, Formal analysis. SL: Formal analysis, Supervision, Visualization, Writing – review & editing, Investigation. PS: Writing – review & editing, Data curation, Investigation, Software. JZ: Supervision, Validation, Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Visualization, Writing – review & editing. YZ: Software, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Clinical Medicine +X Research Center, Air Force Medical University (LHJJ24hl04).
Acknowledgments
We thank the patients who participated in this study. They provided important information and gave us the confidence to carry out this significant work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bisgaard, T. H., Allin, K. H., Keefer, L., Ananthakrishnan, A. N., and Jess, T. (2022). Depression and anxiety in inflammatory bowel disease: epidemiology, mechanisms and treatment. Nat. Rev. Gastroenterol. Hepatol. 19, 717–726. doi: 10.1038/s41575-022-00634-6
Byron, C., Cornally, N., Burton, A., and Savage, E. (2020). Challenges of living with and managing inflammatory bowel disease: a meta-synthesis of patients' experiences. J. Clin. Nurs. 29, 305–319. doi: 10.1111/jocn.15080
Cohen, S., and Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychol. Bull. 98, 310–357.
Frank, J. D. (1974). Psychotherapy: the restoration of morale. Am. J. Psychiatry 131, 271–274. doi: 10.1176/ajp.131.3.271
Fu, H., Kaminga, A. C., Peng, Y., Feng, T., Wang, T., Wu, X., et al. (2020). Associations between disease activity, social support and health-related quality of life in patients with inflammatory bowel diseases: the mediating role of psychological symptoms. BMC Gastroenterol. 20:11. doi: 10.1186/s12876-020-1166-y
Guyatt, G., Mitchell, A., Irvine, E. J., Singer, J., Williams, N., Goodacre, R., et al. (1989). A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 96, 804–810. doi: 10.1016/0016-5085(89)90905-0
Hobfoll, S. E. (1989). Conservation of resources. A new attempt at conceptualizing stress. Am. Psychol. 44, 513–524. doi: 10.1037/0003-066X.44.3.513
Liu, M., Qin, F., and Wang, D. (2024). A study of the mediating effect of social support on self-disclosure and demoralization in Chinese older adult homebound breast cancer patients. Front. Psychol. 15:1365246. doi: 10.3389/fpsyg.2024.1365246
Ng, S. C., Shi, H. Y., Hamidi, N., Underwood, F. E., Tang, W., Benchimol, E. I., et al. (2017). Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet (London, England) 390, 2769–2778. doi: 10.1016/S0140-6736(17)32448-0
Parkes, G., Akbar, A., Beales, I., Buckley, M., Creed, T., Din, S., et al. (2025). Health-related quality of life outcomes among vedolizumab-treated patients with inflammatory bowel disease in the UK and Ireland: a 52-week observational study (OCTAVO). J. Patient-Rep. Outcomes 9:80. doi: 10.1186/s41687-025-00846-9
Robinson, S., Kissane, D. W., Brooker, J., Michael, N., Fischer, J., Franco, M., et al. (2016). Refinement and revalidation of the demoralization scale: the DS-II-internal validity. Cancer 122, 2251–2259. doi: 10.1002/cncr.30015
Vehling, S., and Kissane, D. W. (2018). Existential distress in cancer: alleviating suffering from fundamental loss and change. Psychooncology 27, 2525–2530. doi: 10.1002/pon.4872
Woźniewicz, A., and Cosci, F. (2023). Clinical utility of demoralization: a systematic review of the literature. Clin. Psychol. Rev. 99:102227. doi: 10.1016/j.cpr.2022.102227
Wu, W. J., Li, Q., Quan, M. M., Yan, C. X., Zhang, Q., Shi, B. X., et al. (2021). Chinese adaptation and reliability/validity assessment of the second edition of the lost motivation scale. Nurs. Res. 35, 3218–3223. doi: 10.12102/j.issn.1009-6493.2021.18.004
Wu, K. C., Liang, J., Ran, Z. H., Qian, J. M., Yang, H., Chen, M. H., et al. (2018). Consensus on the diagnosis and treatment of inflammatory bowel disease. Beijing China J. Pract. Int. Med. 38, 796–813. doi: 10.19538/j.nk2018090106
Xiao, S. Y. (1994). Theoretical basis and research application of social support rating scale. J. Clin. Psychiatry 2, 98–100.
Xu, L., He, B., Sun, Y., Li, J., Shen, P., Hu, L., et al. (2023). Incidence of inflammatory bowel disease in urban China: a nationwide population-based study. Clin. Gastroenterol. Hepatol. 21, 3379–3386.e29. doi: 10.1016/j.cgh.2023.08.013
Zhang, P. (2020). A study on the relationship between demoralization, social support, and quality of life in lung cancer patients undergoing chemotherapy [D]. Shandong University of Traditional Chinese Medicine. doi: 10.27282/d.cnki.gsdzu.2020.000423
Keywords: inflammatory bowel disease, demoralization, social support, quality of life, mediating effect
Citation: Ji J, Gu H, Lei S, Shen P, Zheng J and Zhang Y (2025) The role of social support in the association between quality of life and demoralization in patients with inflammatory bowel disease: a cross-sectional study. Front. Psychol. 16:1689939. doi: 10.3389/fpsyg.2025.1689939
Edited by:
Annunziata Romeo, University of Turin, ItalyReviewed by:
Ahmet Sapanci, Düzce Üniversitesi, TürkiyeIsmail Ismail, Polytechnic of Health Makassar, Indonesia
Copyright © 2025 Ji, Gu, Lei, Shen, Zheng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Zheng, aGVwaW5nemhlbmdqaWVAMTYzLmNvbQ==; Yinling Zhang, enlsLXlsekAxNjMuY29t
†These authors have contributed equally to this work
 Jingrui Ji
Jingrui Ji Haoran Gu2†
Haoran Gu2† Yinling Zhang
Yinling Zhang