- 1Department of Nursing, Naval Medical University, Shanghai, China
- 2School of Sociology and Political Science, Shanghai University, Shanghai, China
- 3Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
- 4Department of Nephrology, Shanghai Changzheng Hospital, Naval Medical University, Shanghai, China
Background: Psychological problems are prevalent among maintenance hemodialysis (MHD) patients, and development of scientific, feasible and effective psychological promotion strategies can effectively improve their mental health. A series of studies were conducted to develop a group-based positive psychological intervention for MHD patients. The feasibility and effectiveness of the protocol were verified by a study.
Methods: A cross-sectional survey of 246, including interviews with 13 patients, was conducted to determine the status and factors influencing mental health. A scoping review of 65 studies was performed to develop a protocol for the group-based positive psychological intervention for MHD was based on the PERMA theory and lasted for 4 weeks. Furthermore, experts, medical workers and patients who completed the intervention were interviewed to refine the program. Fifty-two patients were recruited from a hemodialysis center in Shanghai from December 2023 to January 2024. The primary outcome was benefit finding (BF). The secondary outcomes were well-being, quality of life (QoL), and the accessibility and implementation of the program, which were evaluated through interviews and researcher logs.
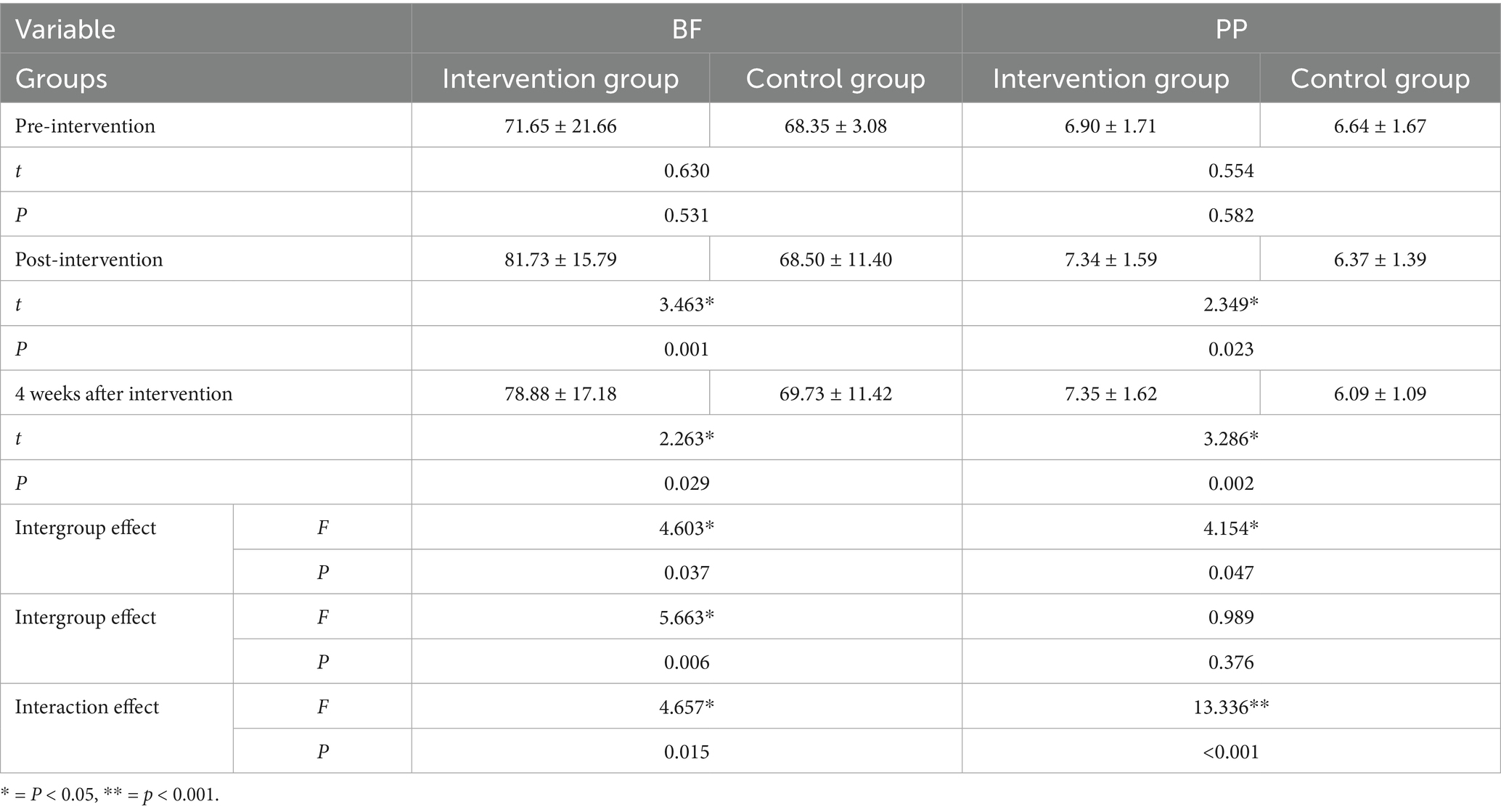
Results: A total of 84 patients were recruited, 52 of whom ultimately participated in the study, including 26 patients in the intervention group and 26 patients in the control group. Twenty-four patients (92.31%) completed all interventions, and 26 patients (100%) completed more than 7 interventions. There were statistically significant differences in the intergroup effect (F = 4.603, p = 0.037 < 0.05), time effect (F = 5.663, p = 0.006 < 0.05) and interaction effect (F = 4.657, p = 0.015 < 0.05) of BF between the two groups. Moreover, through the intervention, the patients’ well-being and QoL in terms of the physical health dimension score improved.
Conclusion: This study developed a group-based positive psychological intervention for MHD patients by conducting a scoping review, a cross-sectional study, qualitative interviews and expert group meetings. This study further optimized and verified the protocol of the intervention by analyzing the barriers to and facilitators of the intervention, conducting expert group meetings and performing the experiment. The intervention had a positive effect on physical and mental health for MHD patients.
Clinical trial registration: Benefit Finding Promotion Program of Maintenance Hemodialysis Patients: An Empirical Study Based on the Implementation Science, identifier [https://www.chictr.org.cn/showproj.html?proj=209809, ChiCTR2300077469].
1 Introduction
The burden of chronic kidney disease (CKD) is increasing annually. It is associated with high disability rates, high medical costs and low awareness rates and has thus emerged as a serious global public health problem (GBD Chronic Kidney Disease Collaboration, 2020). According to the sixth China Chronic Disease and Risk Factor Surveillance, there were an estimated 82 million adults with CKD in mainland China from 2018 to 2019 (Wang et al., 2023). Maintenance hemodialysis (MHD) is the primary method of renal replacement therapy for individuals with kidney failure (Thurlow et al., 2021). Notably, China has one of the highest prevalence rates of MHD. According to the Chinese National Renal Data System (CNRDS), the number of registered individuals on MHD in China reached 7,844,265 by the end of 2022. As the number of MHD patients increases annually, the direct and indirect socioeconomic losses also become greater (Liang et al., 2024). Although dialysis can extend the life of patients, it is also characterized by a series of physiological and psychological challenges that require attention. Hemodialysis does not fully mimic the function of a normal healthy kidney; therefore, MHD patients may experience inappetence, nausea, vomiting, diarrhea, dry and itchy skin, limb edema, restless leg syndrome, joint pain, and sleep disorders (Raja and Seyoum, 2020; Scherer et al., 2017; Wang et al., 2024). Furthermore, MHD patients may experience changes in their body image, such as skin pigmentation, arteriovenous fistuloma formation, an oral ammonia smell, and facial puffiness (Johansen et al., 2021; Marthoenis et al., 2021; Wu et al., 2019). These symptoms may make patients reluctant to engage in social interactions, increase sensitivity and shame, and lead to perceived discrimination (He et al., 2022; Zheng et al., 2020). Previous studies have shown that most MHD patients suffer from depression, anxiety, sadness, and pain (Al-Shammari et al., 2021; Tian et al., 2021). These results suggest that there is an urgent need to attach importance to the psychological status of MHD patients.
Benefit Finding (BF) is as an important and novel concept in positive psychology (Helgeson et al., 2006), BF refers to the perception of an individual’s positive response to adverse life events, which manifests as positive cognitive and behavioral adaptation to adverse events (Sun et al., 2022; Yang et al., 2024a). BF can encompass a greater sense of personal strength, greater appreciation for life, enhanced relationships, spiritual growth, and new life opportunities (Aspinwall and Tedeschi, 2010). Furthermore, BF is considered an indicator of mental health (Yan et al., 2023). Previous studies have shown that higher levels of BF in individuals are correlated with higher levels of happiness and fewer negative emotions during illness (Wepf et al., 2022). Our research team has been committed to examining BF among MHD patients. Our studies have revealed that MHD patients have multiple BFs, including the search for meaning, gaining a sense of mastery, and self-enhancement (Gong et al., 2024) which was lower than that of older adults with chronic diseases (78.85 ± 16.70) (Zhang, 2018) and stroke patients (97.47 ± 17.64) (Wang, 2021) in China. BF was also found to be related to age, duration of HD, family support, other support, positive coping, and self-efficacy (Yang et al., 2024c). These findings provide a reference for the next step in the development of BF interventions.
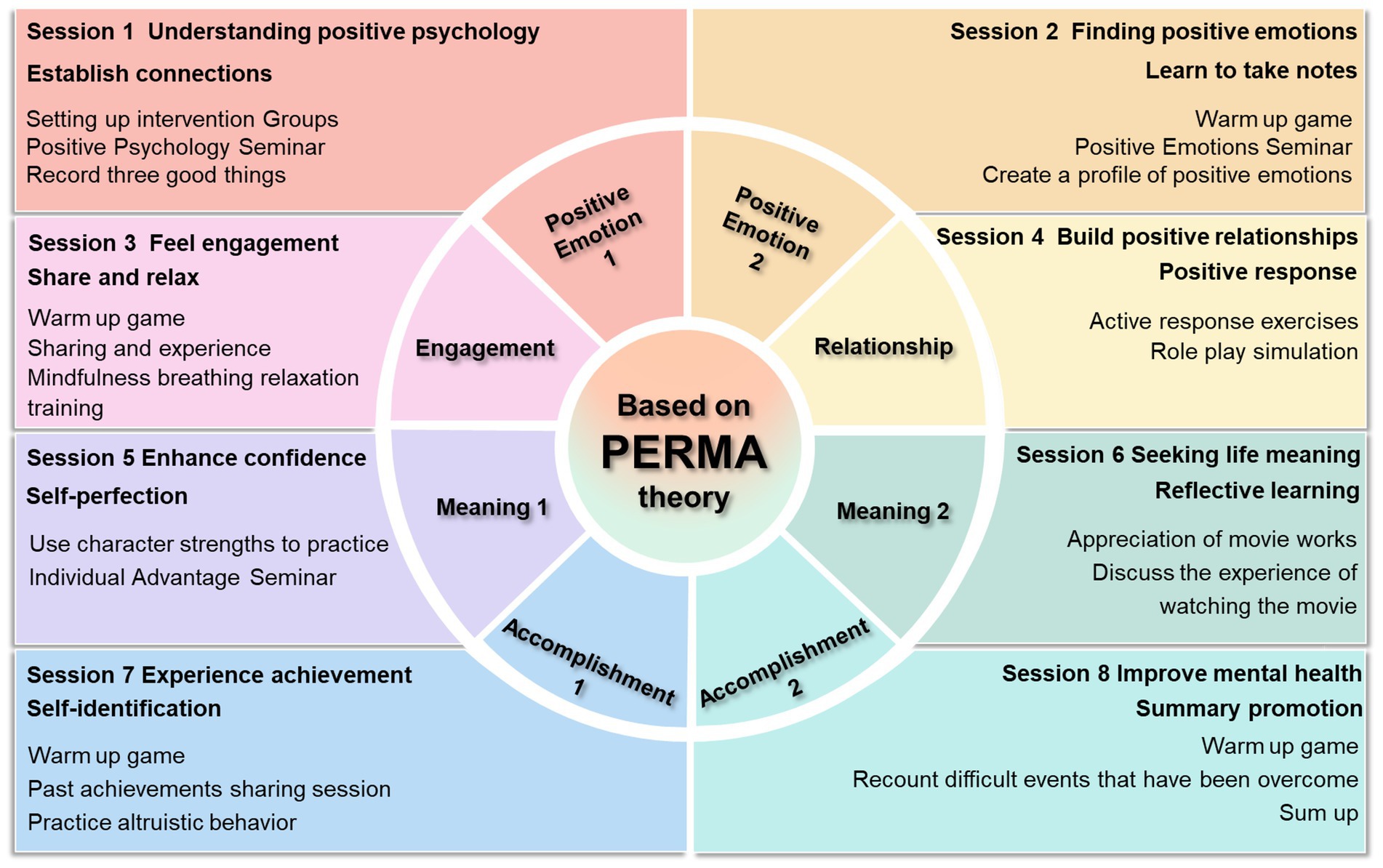
Positive psychology has received considerable attention from the majority of researchers, thereby changing the status quo in psychological research, which had been dominated by negative psychology. Seligman proposed well-being theory, which comprises five elements of well-being, namely, positive emotion, engagement, positive relationships, meaning, and accomplishment (i.e., the PERMA theory) (Gander et al., 2016). This model focuses not only on medical issues but also on interpersonal relationships, interactions, communication, support from one’s surroundings, and personal values and achievements. In the context of positive psychology, the PERMA theory has achieved certain results in terms of improving the mental health of people, such as college students (Yang et al., 2024b) and breast cancer patients (Fang et al., 2023). This theory has been used to provide guidance to patients with respect to producing positive emotions during negative events. Therefore, the PERMA theory provides a basis for developing mental health intervention programs. The five elements of the PERMA theory enable researchers to observe and implement psychological interventions.
Therefore, on the basis of previous studies and guided by the PERMA theory, this study initially constructed a group-based positive psychological intervention for promoting BF in MHD patients and verified the scientific validity feasibility and effectiveness of the intervention to provide a theoretical and practical reference for future practice, to promote positive psychology in MHD patients and to improve mental health and QoL among MHD patients.
2 Methods
This study aimed to develop and validate a group-based positive psychological intervention for promoting BF in MHD patients. This study was conducted from March 2019 to January 2024 and included qualitative interviews, cross-sectional surveys, scoping reviews, interviews about barriers and facilitators factors for implementing the intervention, expert consultations, pretrials, and class trials. This study was approved by an Institutional Ethics Committee (Number: 20220715).
2.1 Development of the group-based positive psychological intervention for MHD patients
The development of the group-based positive psychological intervention comprised six sequential steps: (a) a comprehensive review of the literature to understand the conceptual connotation of BF; (b) a cross-sectional investigation in MHD patients to verify the level of BF and its influencing factors; (c) semistructured interviews with MHD patients to examine into the experience and external manifestations of BF; (d) a scoping review to summarize successful psychological interventions in previous studies; (e) the selection of intervention methods and strategies based on theory; (f) a demonstration through expert group meetings; and (g) a pretest to verify the clinical applicability and modify and improve the program.
Overall, the review of the literature suggested that BF is a widespread psychological experience among people with chronic diseases and that BF is affected by a variety of factors (Yang et al., 2024c). No consensus has been reached regarding the effect of demographic factors, such as age, education level, and economic income, on BF (Zimmaro et al., 2021). However, negative emotions such as anxiety and depression were found to be negatively correlated with BF (Mei et al., 2023; Zhu et al., 2022). Moreover, previous studies have reported that BF is positively correlated with social support (Qiu et al., 2022), positive coping (Li et al., 2023) and general self-efficacy (Helgeson et al., 2006) in patients. The BF of HD patients is lower than that of patients with other chronic diseases. Significant differences in BF scores were found between different age groups, HD duration categories, and degrees of HD-related knowledge. Taking BF as the dependent variable, the results of multiple linear regression analysis revealed that age, duration of HD, family support, other support, positive coping, and self-efficacy combined to explain 43.8% of the total variation.
The a semistructured interviews with MHD patients revealed that BF manifested in 3 ways (Gong et al., 2024): (a) the search for meaning, including approved hemodialysis, the desire to live; (b) gaining a sense of mastery, including adjusting self-psychology, developing healthy living habits, and learning hemodialysis-related behavior management; and (c) self-enhancement, including excavating external resources and affirming self-worth. These findings indicate that BF could help patients to develop a positive psychological framework by strengthening disease knowledge education, building a psychological mutual assistance platform, forming a multidisciplinary nursing team, providing effective social support resources, and cultivating patients’ self-health management. These approaches would improve the level and ability of benefit finding among MHD patients, help them to experience positive incentives, promote their physical and mental health, and improve their QoL.
Additionally, a scoping review was conducted to summarize mature and effective psychological interventions that promote BF based on the PERMA theory. The Embase, Cochrane Database of Systematic Reviews, PubMed, Web of Science, China National Knowledge Infrastructure, Sino-Med, Chongqing VIP, and Wan-fang databases were searched from inception to February 2023. We summarized and analyzed the relevant literature, including studies that examined psychological interventions to promote BF based on the PERMA theory. A total of 65 studies were included, and the results were as follows: (a) the goal of the interventions was to bring about long-term effects; (b) the interventions guided patients to reveal their true thoughts; (c) the interventions improved their ability to cope with negative events; (d) the form of the interventions was mainly offline, supplemented by online; (e) the themes of the interventions were simple and easy to understand; (f) the frequency of the interventions was usually 1–2 times per week; and (g) the outcome indicators focused on the positive factors influencing BF. Under the guidance of the PERMA theory, a group-based positive psychological intervention for promoting BF in MHD patients was initially developed, and 8 senior experts were invited to attend an expert meeting to refine the program.
To further optimize the program, a descriptive qualitative research method was used to conduct semistructured interviews with stakeholders based on the i-PARIHS framework. Barriers to and facilitators of the application of the intervention in clinical practice were assessed and analyzed at 3 levels: Innovation, Recipient, and Context (inner context at local and organizational level and outer context at wider system and policy level) (Harvey and Kitson, 2016). A total of 21 stakeholders were interviewed; 11 barriers and 9 facilitators to the application of the program in clinical practice were analyzed. Countermeasures against these barriers were identified via literature review, group discussion and brainstorming (see Supplementary Material 1), and six experts were invited again to refine the intervention. Then, 6 MHD patients were tested to verify the feasibility, operability and acceptability of the group-based positive psychological intervention for promoting BF. Based on these findings, group programs can ultimately be implemented (see Figure 1).
2.2 Feasibility trial of the group-based positive psychological intervention for MHD patients
2.2.1 Participants
Using a quasi-experimental study design, 52 MHD patients from a 3A hospital in Shanghai were selected as the study subjects from December 2023 to January 2024.
The inclusion criteria were as follows: (a) hemodialysis was performed as a kidney replacement treatment in line with the International Association of Nephrology ESRD diagnostic criteria (Webster et al., 2017); (b) age ≥18 years; (c) maintenance hemodialysis duration ≥3 months, with stable disease conditions; (d) clear consciousness, no cognitive impairment, and ability to communicate normally; (e) ability to independently use smartphones and the WeChat apps; and (f) signed informed consent forms and participated voluntarily. The exclusion criteria were as follows: (a) had undergone surgery recently; (b) had serious malignant diseases other than kidney disease; and (c) could not tolerate the intervention for approximately 1 h. The shedding criterion was participation in 8 interventions <6 times.
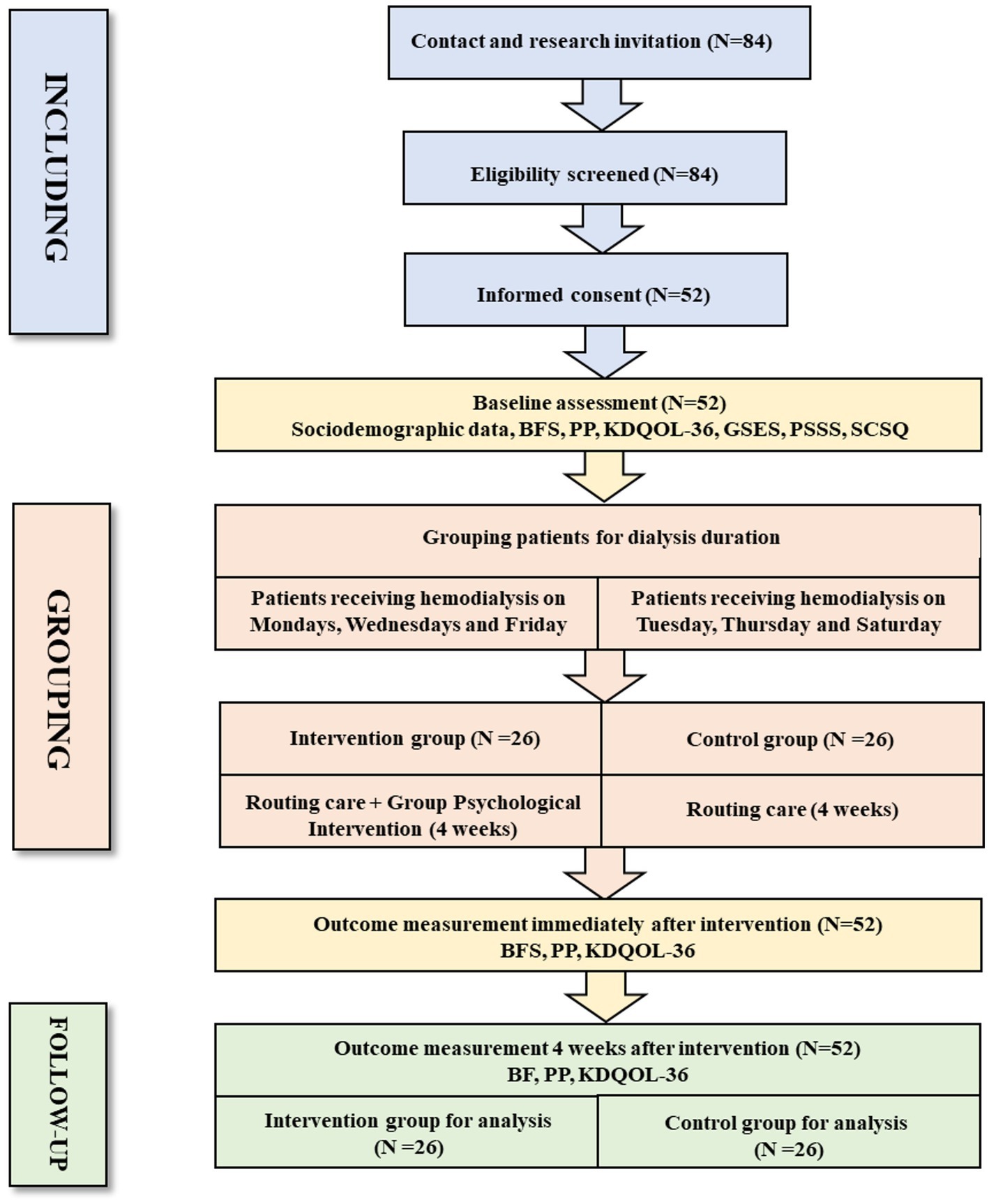
Since MHD patients receive hemodialysis at a fixed time and frequency (three times a week, Monday, Wednesday, Friday or Tuesday, Thursday, and Saturday), a convenience sampling method was used, and patients receiving treatment on a single day of the week (Monday, Wednesday, and Friday) were included in the intervention group, while patients receiving treatment on other days were included in the control group to avoid contamination in the study (see Figure 2).
2.2.2 Establish a professional intervention team
We established a multi-disciplinary intervention team that included individuals who have obtained certificates of competency in psychological counseling and services. Our research team and clinical staff assisted with the implementation of the intervention by helping with field control, participating in activities, demonstrating and introducing simulations, distributing and recycling intervention props, etc. Psychological experts supervised the entire process to control the quality of intervention. All team members were familiar with the content of the intervention program.
2.2.3 Outcome measures
Informed consent was obtained from all individuals before the questionnaires were distributed. The main outcome measure was BF, and the secondary outcome measures were well-being, QoL, and general sociodemographic data. Coping styles, perceived social support, and self-efficacy were only measured at baseline. The psychometric assessment comprised different self-report measures: the Benefit Finding Scale (BFS) (Yan et al., 2023), the Kidney Disease Quality of Life scale (KDQOL-36) (Hays et al., 1994), the PERMA-Profiler (PP) (Yan, 2023), the Perceived Social Support Scale (PSSS) (Zhang et al., 2018), the General Self-efficacy Scale (GSES) (Wang et al., 2001), the Simplified Coping Style Questionnaire (SCSQ)(Xie, 1998). All the measures were completed at baseline (pre-intervention), postintervention, and 4 weeks after the intervention ended.
RE-AIM was used as the guiding framework to evaluate the application process of the program, including accessibility and implementation. Accessibility was evaluated by the participation rate, which was the proportion of participants who provided informed consent to participate in the study among the number of recruited people who met the inclusion criteria. The intervention included two dimensions: authenticity (interveners) and adherence (patients). Authenticity refers to the specific implementation of the intervention, such as whether it is implemented according to the original plan and whether the process is adjusted. Adherence refers to the percentage of patients who complete specific items of the intervention protocol.
2.2.4 Intervention measures
The control group received standard care measures, including psychological support, guidance on dialysis-related knowledge, precautions during dialysis, dietary guidance, exercise guidance, and medication guidance, all provided by hemodialysis unit medical staff.
The intervention group received the group-based positive psychological intervention for MHD patients in addition to standard care. Patients were grouped in teams of 6–8 individuals, with interventions conducted once weekly on Mondays and Fridays. Each session lasted approximately 40 min over a 4-week period. Specific interventions included icebreaker games, themed group discussions, creating positive emotion portfolios, strengths-based exercises, role-playing, and other positive psychology practices. WeChat group chats facilitated information dissemination and supported intervention delivery, including: completing the online Strengths Finder assessment, summarizing intervention content, addressing patient inquiries and fostering communication.
2.2.5 Data analysis
All analyses were performed via IBM SPSS software version 26 (IBM SPSS Inc. Chicago, Illinois, United States). The general demographic characteristics were described via counts and percentages. A t-test of two independent samples was used to compare groups at the same time, repeated-measures ANOVA was used to compare the overall change trend at different times, and one-way repeated-measures ANOVA was used to understand the change trend within different groups.
3 Results
3.1 Participant characteristics
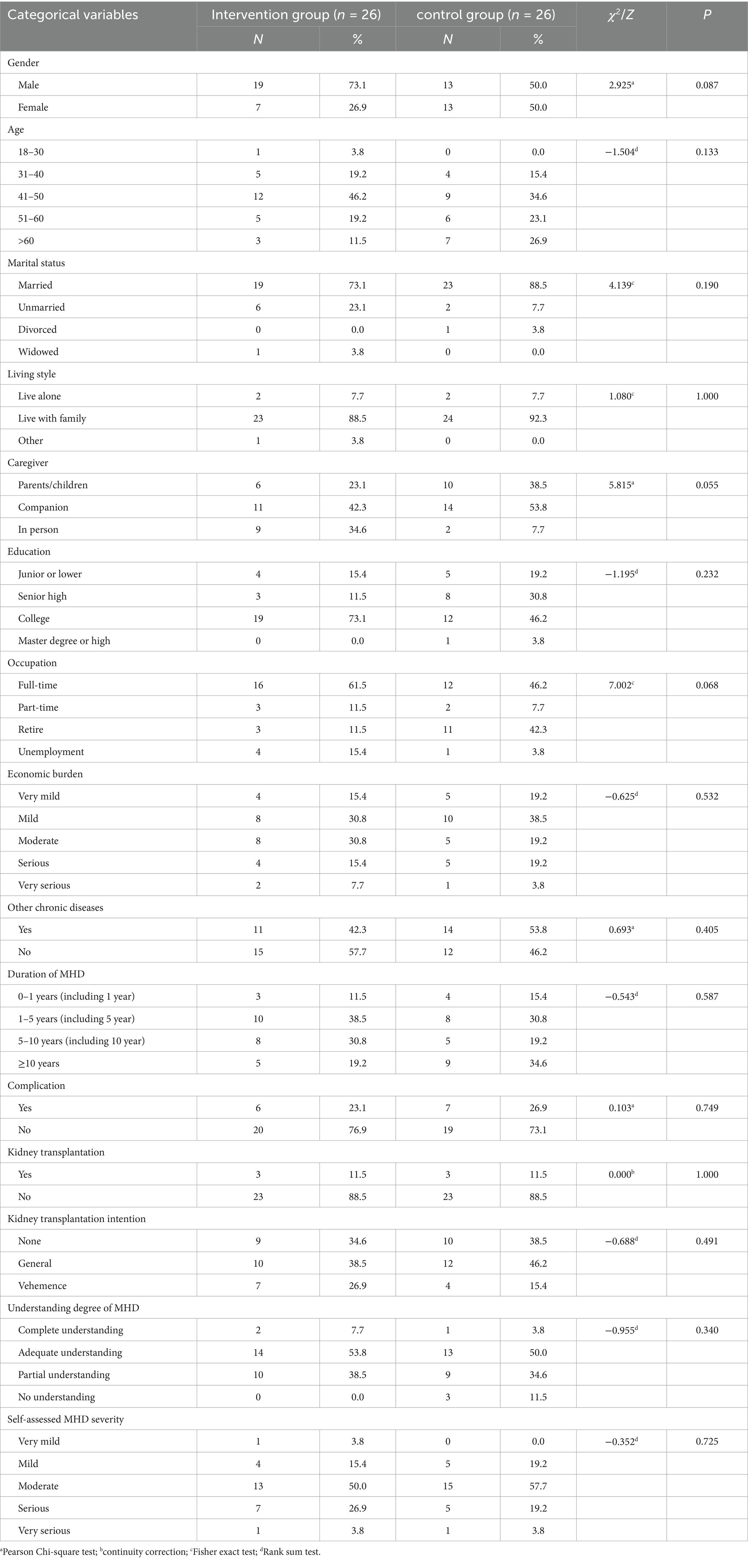
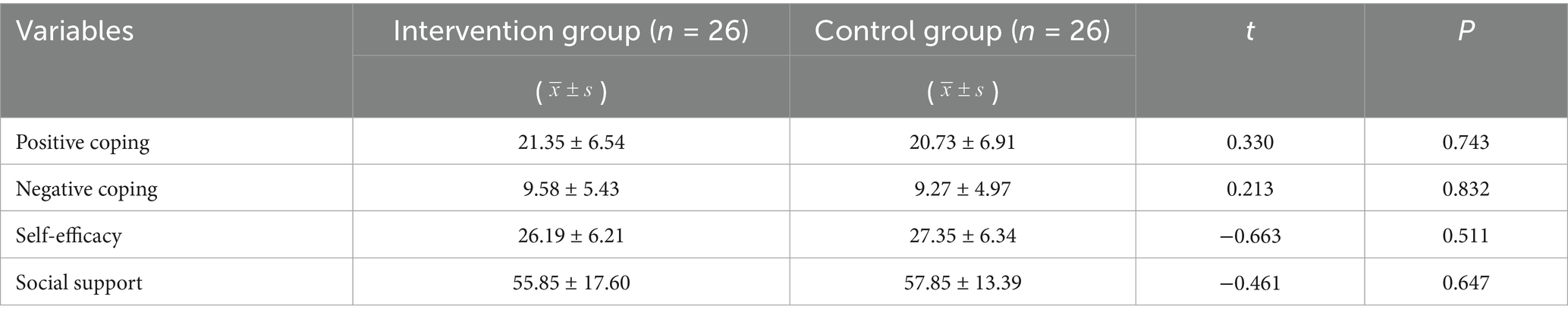
A total of 52 questionnaires were sent out, and 52 were recovered, thus yielding an effective recovery rate of 100%. The results revealed no statistically significant difference in the baseline data between the two groups of MHD patients (p > 0.05) as shown in Tables 1, 2.
3.2 Acceptability and implementation of the interventions
3.2.1 Accessibility
A total of 84 MHD patients who met the inclusion and exclusion criteria were recruited from November to December 2023, among whom 35 did not participate in the study. A total of 52 MHD patients ultimately participated in the study, with a participation rate of 61.9% (see Figure 2). During the recruitment of study subjects, we used research logs to record in detail the reasons for MHD patients’ reluctance to participate in the study. Through content analysis, the following four themes were summarized: (a) lack of motivation to participate; (b) difficulty in understanding the program; (c) doubtful effects of the intervention; and (d) restrictions on health status (see Supplementary Material 2).
3.2.2 Implementation
During the implementation of this study, 24 patients (92.31%) completed all 8 interventions, and 26 patients (100%) completed more than 7 interventions. The group-based positive psychological intervention program was implemented two times each week for a total of 4 weeks and included a total of 21 specific interventions. Specifically, 20 interventions were successfully implemented in accordance with the original plan and rules. In the second intervention (finding positive emotions), some patients lacked interest in the warm-up game and were unwilling to participate. Therefore, the implementers adjusted according to the scene situation and moved on to the next step in advance (see Supplementary Material 3).
3.3 Effectiveness of the interventions
3.3.1 Comparison of BF and well-being scores between the two groups
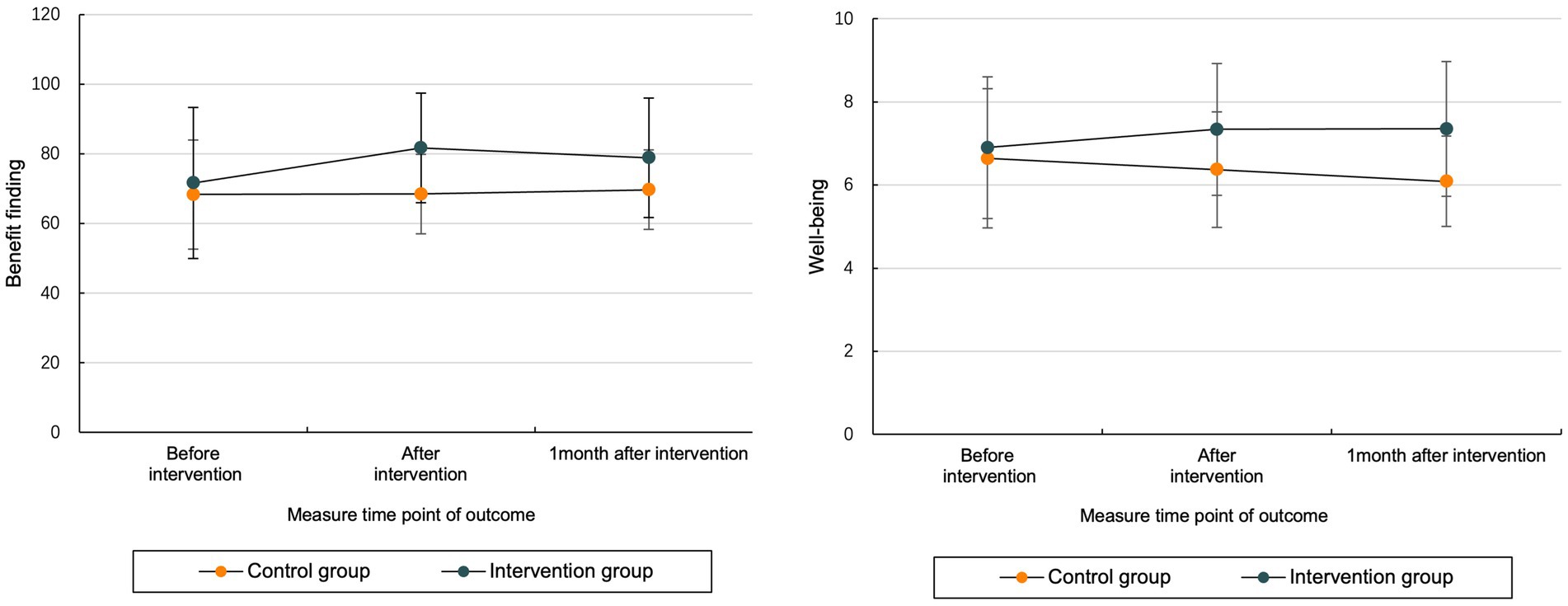
The results of repeated-measures ANOVA revealed that there were interaction effects between intervention and time in BF and well-being scores in MHD patients, indicating that the magnitude of change in BF and well-being at three time points (before, after, and 4 weeks after intervention) over time was statistically significant (see Table 3 and Figure 3).
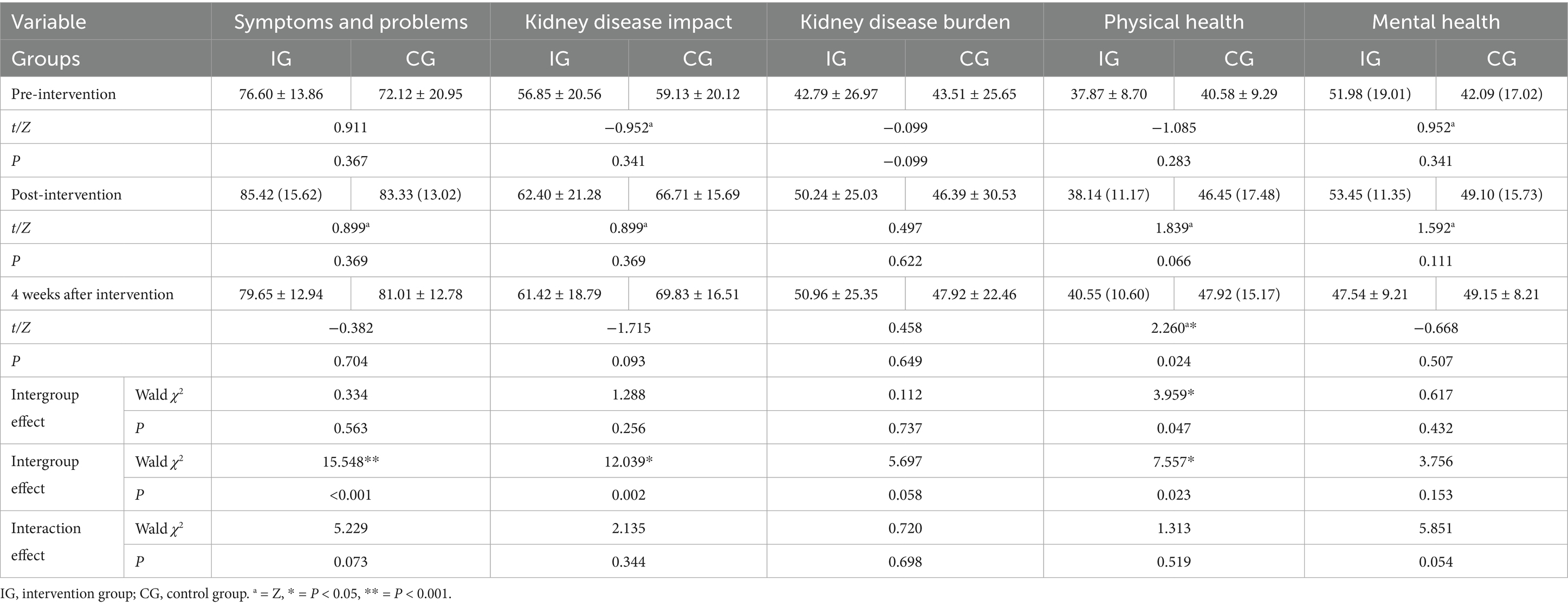
3.3.2 Comparison of QoL scores between the two groups
The results of the generalized estimation equation revealed that there were interaction effects between the intervention and time on the KDQOLTM-SF36 scores of MHD patients. The KDQOLTM-SF36 has five dimensions: physical health, mental health, symptoms and problems, kidney disease burden, and kidney disease impact. The results revealed that there was an intergroup effect on physical health between the two groups (p < 0.05), that there was a time effect on symptoms and problems, that there were effects on kidney disease and physical health (p < 0.05), and that there was no interaction effect in any dimension (p > 0.05) (see Table 4).
4 Discussion
This study synthesized a variety of research methods to developed and validate a group-based positive psychological intervention for MHD patients in China. To our knowledge, this is the first study to promote BF in MHD patients by integrating the investigation, development and implementation of an intervention.
In the process of long-term hemodialysis, MHD patients face three kinds of physiological, psychological and social problems, namely, economic burden, depression, fatigue, weakness, pain, and sleep disorders (Huang, 2019; Ng et al., 2021), and they have strong needs for care and great psychological pressure (Ahmad and Al Nazly, 2015); thus, psychological intervention is urgently needed to improve their mental health. BF is an important concept in positive psychology, and numerous studies have demonstrated. BF is an important concept in positive psychology, and numerous studies have demonstrated this concept. With flourishing as the optimal psychological state, the PERMA theory has five elements that make the construction of intervention plans more observable and operational. Moreover, many previous studies have applied this theory to carry out group-based positive psychological interventions among college students (Yang et al., 2024b), patients with breast cancer (Fang et al., 2023) and Chinese adults (Nie et al., 2024), thus providing a valuable reference for the development of this research.
Previous studies on psychological interventions in MHD patients have focused more on improving negative emotions, whereas fewer studies have explored improving positive emotions. In fact, positive mental health is more conducive to physical rehabilitation, and its effect is more sensitive and obvious than that of alleviating negative emotions. The cross-sectional findings from this study revealed that the level of benefit found was lower in patients with MHD than in other patients with chronic diseases, which suggests that the factors influencing BF should be considered when providing patients with adequate emotional assistance and information, thus enhancing their self-efficacy, increasing perceived social support and improving positive coping skills with respect to dialysis-related problems. Furthermore, BF is likely to improve QoL by summarizing the mature and effective intervention measures in previous studies, such as character strength exercises, the establishment of positive emotion files, and the recording of three good things, The PERMA theory involves the rational use of five elements: positive emotions (experiencing hedonic emotions such as joy and cheerfulness); better engagement (feeling purpose and connection to one’s activities, e.g., experiencing absorption in tasks); positive relationships (feeling others’ support, being cared about, and being satisfied with one’s social relationships); meaning (experiencing a sense of purpose and being connected to something greater that exceeds oneself); and accomplishment (mastering difficulties and attaining goals and feeling a sense of pride) (Seligman, 2018). These factors are consistent with the results of previous cross-sectional surveys and qualitative interviews, and BF among MHD patients is strongly associated with PERMA’ five elements, which is a concrete manifestation of positive relationships. Patients with MHD tend to search for meaning, gain mastery and self-enhancement, which is what they find meaning and accomplishment (Gong et al., 2024). While previous studies have predominantly focused on the well-being outcomes of the PERMA model (Zhang et al., 2025), there is a lack of research on its deep integration with BF. This synergy can yield more applicable interventions and practical operational pathways, particularly for patients with MHD.
The results of the feasibility study show that accessibility was indicated by the participation rate of the study subjects recruited, with 61.9% of MHD patients willing to participate, indicating that most of the patients hoped to improve their mental health. Furthermore, 38.1% of the MHD patients failed to complete the intervention. The reasons for non-completion included a lack of motivation, difficulty in understanding, doubts about effectiveness, and limitations in health conditions. The compliance of the intervention group patients was high: 24 patients (92.31%) completed 8 interventions, and 2 patients completed the intervention 7 times (7.69%) because of personal reasons. In conclusion, the noninvasive psychological intervention developed herein was acceptable, operable and feasible. The program also has good extensibility; the fidelity of implementation was 95.24% (20/21), and only one intervention was not carried out. Through communication with MHD patients through feedback from the implementation of the program, after completing the intervention regarding mastery of psychological adjustment skills and methods and close communication with other patients, some patients were more prone to self-disclosure, some patients felt that their mental health had improved, and some patients hoped to continue participating in these interventions to consolidate the effect. It is recommended that the program continue to be promoted to obtain sustainable benefits.
The self-reported results of MHD patients revealed that BF and well-being effectively improved after the intervention, and the degree of improvement in the intervention group was significantly greater than that in the control group, which are similar as Liu (Liu et al., 2025). Furthermore, our results align with the established efficacy of PERMA-based models in other patient populations. For instance, such interventions have been shown to reduce fear and enhance psychological capital, overall well-being, and QoL in stroked patients (Luo et al., 2025), as well as alleviate fatigue and improve both QoL and psychological well-being in cancer patients (Hu et al., 2025). However, there was no significant effect on QoL. The main reason may be that the program focuses mainly on the expression of patients’ inner emotions, while it is not effective for health behaviors, especially those related to physical activity (such as work and limited activity). In addition, differences in the individual health level and cognitive style of patients may affect their subjective judgment of the impact and burden of kidney disease, and differences in disease severity and dialysis complications may also affect QoL (Dembowska et al., 2022). While some studies report an acceptable quality of life in MHD patients, factors such as number of complications, income, and years on dialysis are established determinants (AlRowaie et al., 2023; Yonata et al., 2022). Specifically, Complications like pruritus, sexual dysfunction, and physical limitations are strongly associated with a significantly poorer QoL (Alencar et al., 2020). Although these somatic and socioeconomic factors are not easily modifiable through brief psychological interventions, the efficacy of such interventions in improving QoL is well-documented (Yan et al., 2025). Therefore, personalized interventions can be designed to improve the QoL of MHD patients by accounting for individual differences and external environmental factors.
4.1 Limitations
This study is the first application of a group-based positive psychological intervention for promoting BF in MHD patients. The sample size was small, and it was a single-center, quasi-experimental study. More high-quality, large-sample, multicenter experimental studies are needed in the future to further clarify the application effect of the program and further improve the program content and optimize the implementation process so that the program can be promoted and applied in clinical practice. Additionally, this study’s findings are influenced by its cultural context. Given our focus on a mainland Chinese population, the applicability of the results to other communities may be limited due to cultural differences.
5 Conclusion
The MHD patients are affected by factors such as disease and long-term treatment and often face heavy physical and mental health burdens. The status and prognosis of CKD cannot easy be changed for most MHD patients. Therefore, changing their understanding of the disease, discovering the benefits of dialysis, and seeking ways to coexist with dialysis are effective strategies to reduce negative psychological reactions, promote the production of positive emotions, and maintain mental health. On the basis of the literature review, cross-sectional investigation, qualitative interviews and expert group meetings, this study developed a group-based positive psychological intervention for promoting BF in MHD patients and further optimized and verified the final version of the program through interviews with promoting and hindering factors, expert group meetings and a feasibility study. The program has clinical application and promotion value, which can effectively improve the level of BF and well-being and improve the physical and mental health of MHD patients.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Committee on Ethics of Medicine, Naval Medical University (Number: 20220715). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JY: Writing – review & editing, Formal analysis, Methodology, Writing – original draft, Data curation, Investigation, Conceptualization. Y-QL: Software, Writing – original draft, Data curation, Methodology, Conceptualization, Investigation, Writing – review & editing. X-YG: Data curation, Writing – review & editing, Methodology, Writing – original draft, Investigation, Formal analysis. Y-HC: Formal analysis, Investigation, Writing – review & editing. JChe: Writing – review & editing, Supervision, Resources. L-lL: Validation, Investigation, Writing – review & editing. Y-RW: Formal analysis, Methodology, Writing – review & editing. Y-QQ: Writing – review & editing, Investigation. JW: Writing – review & editing, Methodology, Conceptualization. JChu: Validation, Funding acquisition, Conceptualization, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Military Health Special Research Project [grant number 22BJZ09], Basic medical research project of Naval Medical University [grant number 2021MS02], and School of Nursing PI team project [grant number 22KYP02].
Acknowledgments
The authors thank all investigators and supporters involved in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1693019/full#supplementary-material
SUPPLEMENTARY MATERIAL 1 | Barriers and facilitators based on the i-PARIHS framework to promote the BF of MHD patients.
SUPPLEMENTARY MATERIAL 2 | Reasons for MHD patients not participating in the study.
SUPPLEMENTARY MATERIAL 3 | Barriers, facilitators factors and countermeasures in the implementation of intervention program.
References
Ahmad, M. M., and Al Nazly, E. K. (2015). Hemodialysis: stressors and coping strategies. Psychol. Health Med. 20, 477–487. doi: 10.1080/13548506.2014.952239
Alencar, S. B. V., de Lima, F. M., Dias, L. D. A., Dias, V. D. A., Lessa, A. C., Bezerra, J. M., et al. (2020). Depression and quality of life in older adults on hemodialysis. Braz J Psychiatry 42, 195–200. doi: 10.1590/1516-4446-2018-0345
AlRowaie, F., Alaryni, A., AlGhamdi, A., Alajlan, R., Alabdullah, R., Alnutaifi, R., et al. (2023). Quality of life among peritoneal and Hemodialysis patients: a cross-sectional study. Clin Pract 13, 1215–1226. doi: 10.3390/clinpract13050109
Al-Shammari, N., Al-Modahka, A., Al-Ansari, E., Al-Kandari, M., Ibrahim, K. A., Al-Sanea, J., et al. (2021). Prevalence of depression, anxiety, and their associations among end-stage renal disease patients on maintenance hemodialysis: a multi-center population-based study. Psychol. Health Med. 26, 1134–1142. doi: 10.1080/13548506.2020.1852476
Aspinwall, L. G., and Tedeschi, R. G. (2010). The value of positive psychology for health psychology: progress and pitfalls in examining the relation of positive phenomena to health. Ann. Behav. Med. 39, 4–15. doi: 10.1007/s12160-009-9153-0
Dembowska, E., Jaroń, A., Gabrysz-Trybek, E., Bladowska, J., Gacek, S., and Trybek, G. (2022). Quality of life in patients with end-stage renal disease undergoing Hemodialysis. J. Clin. Med. 11:1584. doi: 10.3390/jcm11061584
Fang, H., Zeng, Y., Liu, Y., and Zhu, C. (2023). The effect of the PERMA model-based positive psychological intervention on the quality of life of patients with breast cancer. Heliyon 9:e17251. doi: 10.1016/j.heliyon.2023.e17251
Gander, F., Proyer, R. T., and Ruch, W. (2016). Positive psychology interventions addressing pleasure, engagement, meaning, positive relationships, and accomplishment increase well-being and ameliorate depressive symptoms: a randomized, placebo-controlled online study. Front Psychol 7:686. doi: 10.3389/fpsyg.2016.00686
GBD Chronic Kidney Disease Collaboration (2020). Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 395, 709–733. doi: 10.1016/S0140-6736(20)30045-3
Gong, Y., Gao, X., Chen, J., Liu, L., Wu, J., Li, Y., et al. (2024). Benefit finding experience in maintenance hemodialysis patients: a qualitative research. Chin. J. Nurs. 59, 164–169. doi: 10.3761/j.issn.0254-1769.2024.02.005
Harvey, G., and Kitson, A. (2016). PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement. Sci. 11:33. doi: 10.1186/s13012-016-0398-2
Hays, R. D., Kallich, J. D., Mapes, D. L., Coons, S. J., and Carter, W. B. (1994). Development of the kidney disease quality of life (KDQOL) instrument. Qual. Life Res. 3, 329–338. doi: 10.1007/BF00451725
He, L., Li, Q., and Gan, X. (2022). Influence of stigma on psychological distress among young and middle-aged maintenance hemodialysis patients. Chin. J. Nurs. 57, 2585–2591. doi: 10.3761/j.issn.0254-1769.2022.21.004
Helgeson, V. S., Reynolds, K. A., and Tomich, P. L. (2006). A meta-analytic review of benefit finding and growth. J. Consult. Clin. Psychol. 74, 797–816. doi: 10.1037/0022-006X.74.5.797
Hu, X., Li, Q., and Tang, L. (2025). Effect of PERMA-based psychological intervention and predictive care in malignant tumor patients following chemotherapy. Future Oncol. 21, 1639–1645. doi: 10.1080/14796694.2025.2497257
Huang, Y. (2019). Research progress on common complications of hemodialysis in end-stage kidney disease and prevention. Chin. Nurs. Res. 33, 828–831. doi: 10.12102/j.issn.1009-6493.2019.05.022
Johansen, K. L., Chertow, G. M., Foley, R. N., Gilbertson, D. T., Herzog, C. A., Ishani, A., et al. (2021). US renal data system 2020 annual data report: epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 77, A7–A8. doi: 10.1053/j.ajkd.2021.01.002
Li, L., Zhong, H. Y., Xiao, T., Xiao, R. H., Yang, J., Li, Y. L., et al. (2023). Association between self-disclosure and benefit finding of Chinese cancer patients caregivers: the mediation effect of coping styles. Support Care Cancer 31:684. doi: 10.1007/s00520-023-08158-8
Liang, Y., Zhao, X., and Wei, T. (2024). Research report on the development of China's hemodialysis. Chin. J. Blood Purificat. 23, 321–329. doi: 10.3969/j.issn.1671-4091.2024.05.001
Liu, J., Liu, J., Wang, R., Ng, M. S. N., Wu, X., and Chen, J. (2025). Positive living with dialysis: the effect of a positive psychology intervention in patients receiving maintenance hemodialysis. Appl. Psychol. Health Well Being 17:e70078. doi: 10.1111/aphw.70078
Luo, Y., Su, Z., Zhu, L., Huang, Y., Liu, Z., Dechen, W., et al. (2025). The impact of a PERMA model-based positive psychology intervention on fear of stroke recurrence: a randomized controlled trial. Front. Psychol. 16:1498078. doi: 10.3389/fpsyg.2025.1498078
Marthoenis, M., Syukri, M., Abdullah, A., Tandi, T. M. R., Putra, N., Laura, H., et al. (2021). Quality of life, depression, and anxiety of patients undergoing hemodialysis: significant role of acceptance of the illness. Int. J. Psychiatry Med. 56, 40–50. doi: 10.1177/0091217420913382
Mei, Y. X., Xiang, D. D., Zhang, Z. X., Twumwaah Budu, J., Lin, B. L., and Chen, S. Y. (2023). Family function, self-efficacy, care hours per day, closeness and benefit finding among stroke caregivers in China: a moderated mediation model. J. Clin. Nurs. 32, 506–516. doi: 10.1111/jocn.16290
Ng, M. S. N., Chan, D. N. S., Cheng, Q., Miaskowski, C., and So, W. K. W. (2021). Association between financial hardship and symptom burden in patients receiving maintenance Dialysis: a systematic review. Int. J. Environ. Res. Public Health 18:9541. doi: 10.3390/ijerph18189541
Nie, Y. Z., Zhang, X., Hong, N. W., Zhou, C., Huang, Q. Q., Cao, S. Y., et al. (2024). Psychometric validation of the PERMA-profiler for well-being in Chinese adults. Acta Psychol. 246:104248. doi: 10.1016/j.actpsy.2024.104248
Qiu, X., Zhang, K., Zhang, Y., and Sun, L. (2022). Benefit finding and related factors of patients with early-stage Cancer in China. Int. J. Environ. Res. Public Health 19:4284. doi: 10.3390/ijerph19074284
Raja, S. M., and Seyoum, Y. (2020). Intradialytic complications among patients on twice-weekly maintenance hemodialysis: an experience from a hemodialysis center in Eritrea. BMC Nephrol. 21:163. doi: 10.1186/s12882-020-01806-9
Scherer, J. S., Combs, S. A., and Brennan, F. (2017). Sleep disorders, restless legs syndrome, and uremic pruritus: diagnosis and treatment of common symptoms in Dialysis patients. Am. J. Kidney Dis. 69, 117–128. doi: 10.1053/j.ajkd.2016.07.031
Seligman, M. (2018). PERMA and the building blocks of well-being. J. Posit. Psychol. 13, 333–335. doi: 10.1080/17439760.2018.1437466
Sun, L., Liu, K., Li, X., Zhang, Y., and Huang, Z. (2022). Benefit-finding experiences of cervical cancer survivors in rural Yunnan province, China: a qualitative study. Nurs. Open 9, 2637–2645. doi: 10.1002/nop2.962
Thurlow, J. S., Joshi, M., Yan, G., Norris, K. C., Agodoa, L. Y., Yuan, C. M., et al. (2021). Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am. J. Nephrol. 52, 98–107. doi: 10.1159/000514550
Tian, N., Chen, N., and Li, P. K. (2021). Depression in dialysis. Curr. Opin. Nephrol. Hypertens. 30, 600–612. doi: 10.1097/MNH.0000000000000741
Wang, X. (2021). Study on status and influencing factors of benefit finding among elderly stroke patients. M.D., Xinxiang, China: Xinxiang Medical University.
Wang, C., Hu, Z., and Liu, Y. (2001). Evidences for reliability and validity of the Chinese version of general self-efficacy scale. Chin. J. Appl. Psychol. 7, 37–40. doi: 10.3969/j.issn.1006-6020.2001.01.007
Wang, L., Xu, X., Zhang, M., Hu, C., Zhang, X., Li, C., et al. (2023). Prevalence of chronic kidney disease in China: results from the sixth China chronic disease and risk factor surveillance. JAMA Intern. Med. 183, 298–310. doi: 10.1001/jamainternmed.2022.6817
Wang, L., Zhang, M., Xiao, W., Li, J., and Ge, Y. (2024). Research progress on symptom groups of hemodialysis patients. Chin. J. Nurs. Educ. 21, 124–128. doi: 10.3761/j.issn.1672-9234.2024.01.020
Webster, A. C., Nagler, E. V., Morton, R. L., and Masson, P. (2017). Chronic kidney disease. Lancet 389, 1238–1252. doi: 10.1016/S0140-6736(16)32064-5
Wepf, H., Joseph, S., and Leu, A. (2022). Benefit finding moderates the relationship between young carer experiences and mental well-being. Psychol. Health 37, 1270–1286. doi: 10.1080/08870446.2021.1941961
Wu, Q., Li, J., Li, R., and Wang, L. (2019). Analysis of related factors affecting the long-term survival rate of hemodialysis patients. Chin. J. Blood Purificat. 18, 543–546. doi: 10.3969/j.issn.1671-4091.2019.08.008
Xie, Y. (1998). A preliminary study of the reliability and validity of the brief coping style scale. Chin. J. Clin. Psychol. 2, 53–54. doi: 10.16128/j.cnki.1005-3661.1998.02.018
Yan, H. (2023). Study on status of flourishing and its influencing factors among maintenance hemodialysis patient. M.D., Shanghai, China: Naval Medical University.
Yan, H., Yang, J., Luo, C., Zhang, L., Tian, Y., Cui, S., et al. (2023). Development and psychometric assessment of the benefit finding scale for Chinese older adults with chronic diseases. Res. Gerontol. Nurs. 16, 44–52. doi: 10.3928/19404921-20230105-03
Yan, S., Zhu, X., Huo, Z., Wang, Z., and Cui, H. (2025). Psychological intervention for depression and anxiety in Hemodialysis patients: a meta-analysis. Actas Esp. Psiquiatr. 53, 154–164. doi: 10.62641/aep.v53i1.1628
Yang, J., Li, Y. Q., Gong, Y. L., Yan, H. L., Chen, J., Liu, L. L., et al. (2024a). Benefit finding in individuals undergoing maintenance hemodialysis in Shanghai: a latent profile analysis. Front. Psychol. 15:1292175. doi: 10.3389/fpsyg.2024.1292175
Yang, J., Tan, Y., and Yao, C. (2024b). Can a PERMA model-based positive psychological intervention affect the SIA and SWB of vocational college students majoring in nursing in China? Front. Psychol. 15:1337064. doi: 10.3389/fpsyg.2024.1337064
Yang, J., Yan, H. L., Li, Y. Q., Zhang, L., Qiu, X. Y., Tian, Y. H., et al. (2024c). Benefit finding in chronic kidney disease patients receiving hemodialysis: a cross-sectional study. BMC Nephrol. 25:46. doi: 10.1186/s12882-024-03480-7
Yonata, A., Islamy, N., Taruna, A., and Pura, L. (2022). Factors affecting quality of life in Hemodialysis patients. Int J Gen Med 15, 7173–7178. doi: 10.2147/ijgm.S375994
Zhang, L. (2018). Study on status of benefit finding and its influencing factors among elderly patients with chronic diseases. M.D., Shanghai, China: Naval Medical University.
Zhang, L., Chen, X., and Wan, H. (2025). Effects of a personalized PERMA-based intervention on the mental health of junior high school students: a randomized clinical trial. Front. Psychol. 16:1535744. doi: 10.3389/fpsyg.2025.1535744
Zhang, F., Zhu, S., and Deng, P. (2018). Evaluation of perceived social support scale used in study of social support among hospitalized patients in China. Chin. Nurs. Res. 32, 2048–2052. doi: 10.12102/j.issn.1009-6493.2018.13.015
Zheng, W., Lu, C., Lv, G., and Wang, F. (2020). Status of stigma and its influencing factors in 222 maintenance hemodialysis patients. J. Nurs. 27, 44–48. doi: 10.16460/j.issn1008-9969.2020.14.044
Zhu, P., Chen, C., Liu, X., Gu, W., and Shang, X. (2022). Factors associated with benefit finding and mental health of patients with cancer: a systematic review. Support Care Cancer 30, 6483–6496. doi: 10.1007/s00520-022-07032-3
Keywords: maintenance hemodialysis, psychological intervention, mental health, benefit finding, well-being, quality of life
Citation: Yang J, Li Y-Q, Gao X-Y, Cao Y-H, Chen J, Liu L-l, Wang Y-R, Qian Y-Q, Wu J and Chu J (2025) Development and feasibility pilot study of positive psychological intervention for maintenance hemodialysis patients in China. Front. Psychol. 16:1693019. doi: 10.3389/fpsyg.2025.1693019
Edited by:
Ali Saffet Gonul, Ege University, TürkiyeReviewed by:
Rajat Sanker Roy Biswas, Chattagram Maa-O-Shishu Hospital Medical College, BangladeshKriti Vashishtha, Manipal University Jaipur, India
Copyright © 2025 Yang, Li, Gao, Cao, Chen, Liu, Wang, Qian, Wu and Chu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Wu, cWluZ3FpbmcyMDAzMDUxMUAxNjMuY29t; Jing Chu, Y2h1amluZzE5OTlAc21tdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Jie Yang
Jie Yang Yong-Qi Li
Yong-Qi Li Xin-Yue Gao
Xin-Yue Gao Yong-Hui Cao1
Yong-Hui Cao1 Yue-Qin Qian
Yue-Qin Qian Jing Chu
Jing Chu