Abstract
Background:
Eating behavior is a multidimensional construct shaped by physical, emotional, and psychological factors. This study investigated the relationships and effects of self-esteem, emotional appetite, and food addiction on eating attitudes among young adults, while also assessing the role of demographic variables in relation to eating attitudes (EAT-26 scores).
Methods:
Data were collected from 766 participants (171 women, 595 men) using the Eating Attitudes Test-26 (EAT-26), Rosenberg Self-Esteem Scale (RSB), Emotional Appetite Questionnaire (EMAQ), and Yale Food Addiction Scale (YFAS).
Results:
Among the participants, 71.7% had a healthy weight, 13.0% were underweight, and 15.2% were overweight or obese. Significant associations were observed between the EAT-26 eating preoccupation subscale and educational level, smoking, skipping snacks, eating out (p < 0.05), and body mass index (BMI) (p < 0.01). The restriction subscale was positively correlated with BMI and perceived adequate nutrition (p < 0.01), whereas the social pressure subscale was negatively correlated with educational status, BMI (p < 0.01), and skipping snacks (p < 0.05). The EAT-26 total score was significantly associated with self-esteem (RSB), negative emotional appetite (EMAQ negative), and food addiction (YFAS) (p < 0.01). Further analyses identified gender (B = −2.00; p < 0.05), negative emotional appetite (B = 0.03; p < 0.05), and food addiction (B = 0.496; p < 0.01) as significant predictors of EAT-26.
Conclusion:
The results indicate that eating behavior is most strongly influenced by food addiction, negative emotional appetite, and low self-esteem, underscoring the decisive role of psychological factors.
1 Introduction
Food addiction, eating attitudes, self-esteem, and emotional appetite are interrelated psychological factors that significantly influence eating behaviors, particularly among young adults. Low self-esteem, negative eating attitudes, and heightened emotional appetite have been associated with an increased risk of food addiction and eating disorders. The reported prevalence in the literature ranges from 13.2 to 18.2% (Borisenkov et al., 2020; Bozkurt et al., 2024), alongside a documented rise in disordered eating attitudes and behaviors (Paterna et al., 2021).
Depression and stress increase the tendency toward uncontrolled eating, which arises as a way of coping with negative emotions. This tendency is significantly associated with symptoms of eating addiction (EA) (Fernández et al., 2022). Studies have shown that eating addiction has a positive correlation with mental health symptoms such as eating disorders, depression, and anxiety (Burrows et al., 2018; Cinelli et al., 2020). The emergence of the healthy and clean eating movement has contributed, in some cases, to an oppression with the consumption of high-quality, health-oriented foods. When this oppression escalates, it can result in pathological orthorexic behaviors and restrictive dietary practices, a condition known as orthorexia nervosa (ON). Despite its prevalence, the relationship between eating behavior, emotional appetite, and food addiction is complex and multifaceted. It has been reported that individuals with low self-esteem are more likely to exhibit maladaptive eating behaviors as a coping mechanism for emotional distress (Sanlier et al., 2017).
Emotional states significantly influence eating behavior, with factors such as self-esteem, impulse control, and emotional coping mechanisms playing a particularly decisive role among young adults. Emotional appetite refers to the tendency to eat in response to emotional states rather than physiological hunger. Negative emotional states such as stress and depression are associated with uncontrolled eating and eating as a coping mechanism (Fernández et al., 2022; Rossi, 2025). Eating disorders are associated with higher body mass index, emotional eating, and uncontrolled eating behaviors (Sanlier et al., 2017; Sanlier et al., 2017). Another study reported that food addiction elevates the risk of eating disorders, identifying body mass index (BMI) as the most influential factor. The findings further indicated that women are more likely than men to experience both anorexia nervosa and food addiction (Rose et al., 2018). Emotional eating and delicious eating motivations are reported to be more common among individuals who had food addictions (FA) (Bozkurt et al., 2024). Young people with a stronger emotional appetite often engage in uncontrolled eating behaviors, potentially worsening food addiction (Rossi, 2025). Within the brain reward system, dopamine, which plays a role in the development of addiction and is the most important neurotransmitter, comes to the fore. D2 receptors, which are elements of the dopaminergic system, are affected by sugar consumption. Sugar addiction creates the sense of pleasure through the brain’s reward system. Long-term sugar consumption seems to reduce the level of D2 receptors. Acute sugar consumption results in intense opioid and dopamine release. Furthermore, acetylcholine release is delayed, resulting in increased food intake. Chronic sugar consumption results in dopamine deficiency and dysfunction in the prefrontal cortex, the reward center. When sugar consumption is absent, withdrawal symptoms develop, leading to compulsive eating disorder (DiNicolantonio et al., 2018). There appears to be a significant overlap between added sugar consumption and drug-like effects such as overeating, cravings, tolerance, withdrawal, cross-sensitization, cross-tolerance, cross-dependence, reward, and opioid effects, including sugar addiction and dependence on the natural endogenous opioids released by sugar intake (Serin and Şanlıer, 2018). Processed foods are made palatable by adding large amounts of fat, sugar, or salt and are widely consumed. Therefore, these foods promote overeating, which is the leading cause behind obesity and associated metabolic diseases (Bozkurt et al., 2024; Bjorlie et al., 2022; Gearhardt and DiFeliceantonio, 2023).
Among adolescents with morbid obesity, negative moods combined with difficulties in impulse control, emotional eating, and food addiction are linked to a lower quality of life. These emotional regulation strategies have been shown to be crucial in managing eating behaviors and preventing food addiction (Rose et al., 2018). They might perceive themselves as overweight. This issue highlights the relationship between body image and eating behaviors (Lipsky et al., 2022).
One study found positive correlations between emotional eating and food addiction scores among men and women, and psychological distress scores were positively correlated with body mass index (BMI). Among educated young adults, the use of food consumption to regulate negative moods has been reported to put individuals at risk for overweight and obesity (Bourdier et al., 2018). In addition, it has been reported that eating disorders such as cognitive restraint, uncontrolled eating, and emotional eating also contribute to an increased risk of food addiction among students (Alim et al., 2021). In addition, the promotion of an idealized body image within the media influences societal perceptions, equating thinness with beauty. Inconsistencies between one’s desired and actual body lead individuals to feel anxious about their bodies and develop body dissatisfaction over time. As distorted body perceptions cause psychological distress, they are effective in the development of disordered eating behaviors (Paterna et al., 2021; Sahin and Sanlier, 2025). These findings highlight the complex interactions between emotional states, eating behaviors, and food addiction among young adults. Ultimately, these dynamics highlight the importance of examining psychosocial factors that contribute to the likelihood of developing eating disorders.
This study aims to investigate the relationships between self-esteem (RSB), emotional eating (EMAQ), food addiction (YFAS), and eating attitudes (EAT-26) among young adults aged 20 to 30 years old. It also examines how demographic factors are related to EAT-26 scores and the extent to which they may influence these attitudes.
2 Materials and methods
2.1 Procedure and participants
For this cross-sectional study, a total of 766 adult volunteers, including 171 (22.3%) women and 595 (77.7%) men aged 20–30 living in Ankara (the capital of Turkey), were reached. A total of 915 people were sent the study link. However, only 766 of them completed the survey completely and accurately, resulting in an 83.7% response rate. The study was carried out between November 2024 and March 2025. The questionnaire package prepared by the researchers was sent to the participants via Google Forms links shared on WhatsApp, Instagram, and Facebook, which are connected to the researchers’ systems. Data were collected using the convenience sampling technique. Before implementing the questionnaire package, a pilot study was conducted among 48 participants, and unexplained points were examined and minor modifications and adjustments were made to questions that were unclear. Participants under the age of 20 or over the age of 30, those who were pregnant or breastfeeding, and those with mental illness were not included in the research. To ensure the survey’s comprehensibility and accuracy, participants with mental illness, pregnant women, and breastfeeding women were excluded from the study.
This study aimed to investigate the relationships and predictive effects of self-esteem, emotional appetite, and food addiction on eating attitudes among young adults. In addition, it examined the associations and potential influences of demographic characteristics on EAT-26 scores.
The hypotheses formulated in line with the study objective are as follows:
Demographic characteristics are significantly associated with eating attitudes.
Self-esteem is significantly associated with eating attitudes.
Emotional appetite is significantly associated with eating attitudes.
Food addiction is significantly associated with eating attitudes.
The research model containing all the hypotheses proposed in the study is presented in Figure 1.
Figure 1
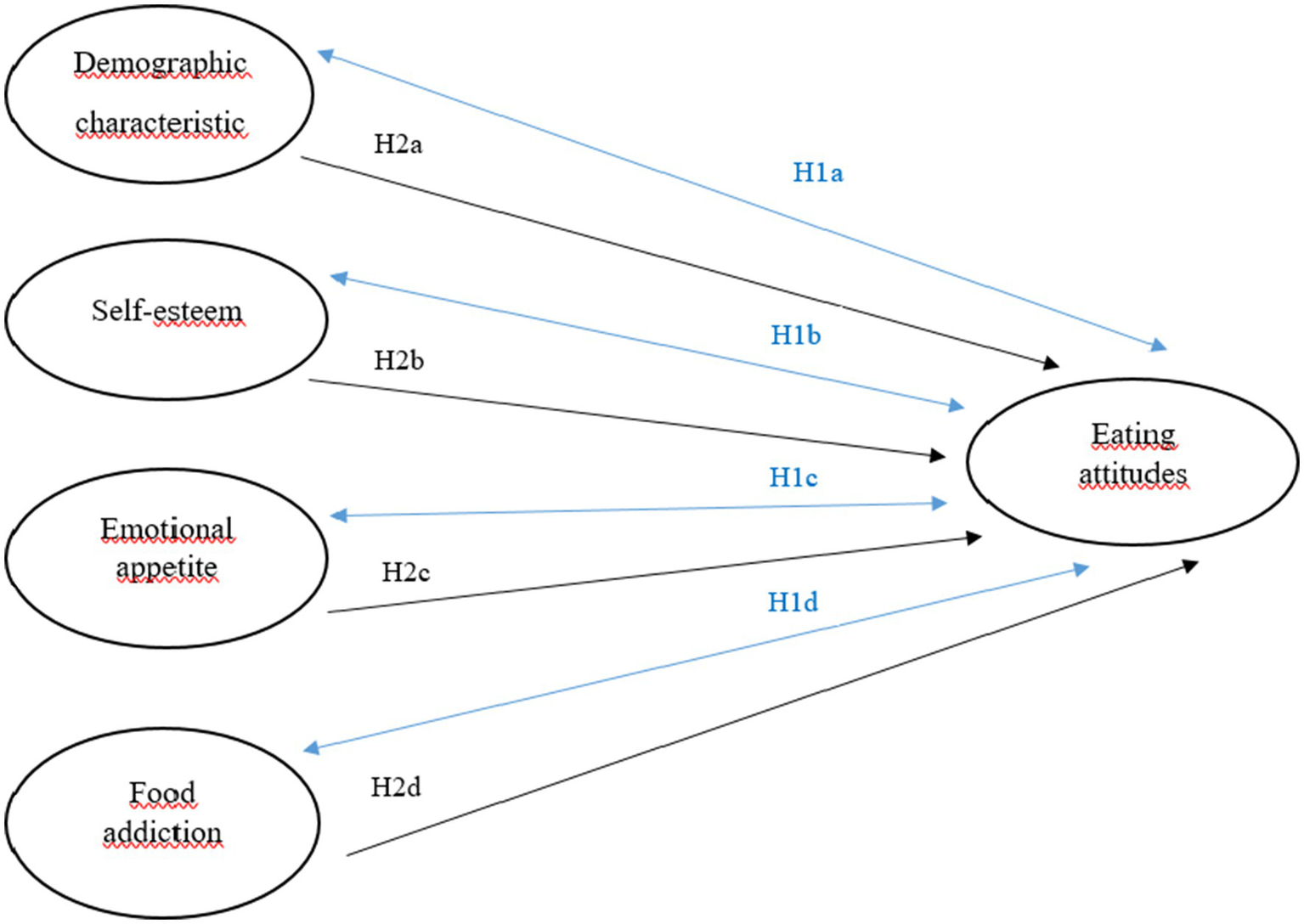
Hypothesized research model.
2.2 Demographic information
Questions about sociodemographic characteristics such as gender (male/female), age (years), and length of education (years), as well as current smoking status (yes/no) and the presence of any health problems (yes/no) were provided. Additionally, participants reported their height (cm) and body weight (kg) based on self-reported information.
2.3 Instrumentation
The questionnaire, after revision, was arranged into four distinct sections:
Rosenberg Self-Esteem Scale (RSES) (10 statements) (Gearhardt and DiFeliceantonio, 2023)
Yale Food Addiction Scale (YFAS) (25 statements) (Lipsky et al., 2022)
Eating Attitudes Test (EAT-26) (26 statements) (Bourdier et al., 2018)
Emotional Appetite Questionnaire (EMAQ) (22 statements) (Alim et al., 2021).
2.3.1 Rosenberg self-esteem scale (RBS)
The Rosenberg Self-Esteem Scale, originally developed by Rosenberg (1965), was employed in this study to assess self-esteem. This self-report instrument comprises 63 multiple-choice items divided into 12 subscales, each of which may also be applied independently in research. The Self-Esteem Subscale of the RBS Scale is a 4-point Likert-type scale that comprises the first 10 items of the scale. These 10 items were used in this study. Since responses are scored in single, double, or triple groups, the total score range of the subscale is 0–6. According to Rosenberg (1965), individuals scoring between 0 and 1 points are considered to have high self-esteem, those with scores ranging from 2 to 4 are regarded as having moderate self-esteem, and those scoring 5 to 6 points are identified as having low self-esteem.
2.3.2 Yale food addiction scale
The Yale Food Addiction Scale (YFAS) was developed by Gearhardt et al. (2009). This scale consists of 27 items that assess participants’ food addiction status by inquiring about seven criteria related to their eating habits over the past 12 months. The first 18 questions of the scale are five-point Likert-type questions. However, responses to questions 19–24 are either “yes.” or “no.” Information on how many times an individual has attempted to reduce or stop eating certain foods in the past year is obtained from question 25, while information on foods that individuals find difficult to control is obtained from questions 26 and 27. Questions 17, 18, and 23, which are prerequisites for other questions, are not included in the scoring. Each question is scored as 0 or 1 based on the response given to the items. Subsequently, the total score for the questions under each dependency criterion (tolerance, withdrawal, clinical significance, etc.) is calculated. The degree of addiction is proportional to the number of symptoms. Questions 15 and 16 are clinically significant in identifying food addiction, and those who scored at least 1 point on these questions and had 3 or more symptoms were defined as “food addicts” (Gearhardt et al., 2009). In addition to providing a continuous symptom count, the YFAS also yields a dichotomous diagnostic classification. The Cronbach’s alpha coefficient of the scale used in this study was found to be 0.811.
2.3.3 Eating attitudes test-26 (EAT-26)
The Eating Attitudes Test (EAT-26) assesses the risk of eating disorders by evaluating eating-related attitudes, emotions, and behaviors. Scores range from 0 to 78, and a cutoff score of ≥20 is used. Higher scores reflect an increased risk of eating disorders. Total scores of 20 or higher are considered to be in the clinical range. Individuals scoring 20 or higher are classified as “At Risk for Eating Disorders,” while those scoring below 20 are classified as “Not At Risk for Eating Disorders.” Responses are scored as follows: always = 3, usually = 2, often = 1, other options = 0. Only item 26 is reverse-scored: never = 3; rarely = 2; sometimes = 1; other options = 0 (Garner and Garfinkel, 1979).
2.3.4 Emotional eating scale (EMAQ)
The scale consists of 22 items and does not include a cut-off score. A Likert-type scale was used, designed according to a 9-point scoring system (Nolan et al., 2010). In the EMAQ, emotional eating is evaluated through 14 items addressing positive and negative emotions and 8 items focusing on both positive and negative situations. If an individual consumes significantly less food than normal in certain emotions and situations, they mark numbers 1–4; if there is no change in food consumption, they mark number 5; if they consume significantly more food than normal, they mark numbers 6–9. The EMAQ negative score is calculated by summing responses to negative emotions and situations, while the positive score is derived from responses to positive emotions and situations.
2.4 Anthropometric measurements
Information regarding participants’ height and body weight was obtained based on their self-reports. The body mass index (BMI) was calculated by dividing body weight by the square of height and evaluated using the World Health Organisation’s BMI classification. Body weight (kg), and the obtained data were divided into three groups: underweight (BMI < 18.5 kg/m2), healthy weight (18.5 ≤ BMI ≤ 24.9 kg/m2) and overweight (BMI ≥ 25.0 kg/m2) (World Health Organization, 2010; World Health Organization, 2000).
All participants were fully informed about the purpose of the study prior to completing the questionnaire through the system, and informed consent was obtained in line with the principles of the Declaration of Helsinki (World Medical Association). It took approximately 20 min to complete the survey.
2.5 Data analysis
Artificial Neural Network method, a subtype of artificial intelligence and machine learning, was used in the research. Although artificial neural network analysis is a topology research method developed for operations research, unlike other operations analysis, it is also used in applications of decision selection problems in different fields. The method is based on producing nonlinear predictions and provides more compatible results in complex data and models with linearization deviations. An analysis used in the study is, it is an Artificial Neural Network method, which is a subtype of artificial intelligence and machine learning. Although artificial neural network analysis is a topology research method developed for operations research, unlike other operations analysis, it is also used in applications of decision selection problems in different fields. The method is based on producing non-linear predictions and provides more compatible results in complex data and models with linearization deviations. With the artificial neural networks method, clustering and desired classification levels are higher, and multi-layered and efficient results can be obtained in multivariate decision and prediction analyses. In this context, a multilayer perceptron model was applied for the Artificial Neural Network analysis used in the study. All analyses were carried out in the SPSS 25.0 program with a 95% Confidence Interval and a significant level of 0.05.
3 Results
A total of 766 volunteers, including 171 females and 595 males, participated in this descriptive cross-sectional study. The majority of participants were male (77.7%). The highest rates participation was from the health sciences (58.2%) departments, followed by tourism (19.1%) department and education (18.5%) departments. In reaction to the BMI, 13.0% of the participants were underweight, 71.8% had a healthy weight, and 15.2% of the participants were overweight/obese. In addition, 14.5% of the participants were smoking and 14.5% were drinking alcohol. Within the whole sample, 43.2% of the participants thought that they have an adequate, balanced, healthy diet, and 97.0% of them stated that they eat out, and 57.4% of them eat at school or workplace restaurants, the majority skip breakfast or lunch, 71.5% eat out of home 1–6 times a week, and 58.1% eat at school-work restaurants (Table 1).
Table 1
| Characteristics | n | % | |
|---|---|---|---|
| Gender | Male | 595 | 77.7 |
| Female | 171 | 22.3 | |
| Faculty | Health sciences | 446 | 58.2 |
| Education | 142 | 18.5 | |
| Tourism | 146 | 19.1 | |
| Engineering and management | 32 | 4.2 | |
| BMI (kg/m2) | Under weight | 100 | 13.0 |
| Healthy weight | 550 | 71.8 | |
| Overweight | 116 | 15.2 | |
| Smoking | No | 655 | 85.5 |
| Yes | 111 | 14.5 | |
| Alcohol | No | 655 | 85.5 |
| Yes | 111 | 14.5 | |
| Balanced, healthy diet | No | 435 | 56.8 |
| Yes | 331 | 43.2 | |
| Skipping main meal | No | 215 | 28.1 |
| Sometimes | 335 | 43.7 | |
| Yes | 216 | 28.2 | |
| Type of skipped meal | Breakfast | 245 | 44.5 |
| Lunch | 283 | 51.4 | |
| Dinner | 23 | 4.1 | |
| Eating out | No | 23 | 3.0 |
| Yes | 743 | 97.0 | |
| Type of meal eaten out | Breakfast | 46 | 6.2 |
| Lunch | 526 | 70.8 | |
| Dinner | 171 | 23.0 | |
| Eating out (frequency) | 1–3 times in a month | 46 | 6.2 |
| 1–6 times a week | 531 | 71.5 | |
| Everyday | 166 | 22.3 | |
| Eating out (place) | School-job restaurant | 432 | 58.1 |
| Restaurant | 71 | 9.6 | |
| Kebap house | 53 | 7.1 | |
| Fast-food | 187 | 25.2 | |
Baseline characteristics of participants (n = 766).
The internal consistency of the scales employed in the study was assessed using Cronbach’s alpha coefficient. High reliability levels were observed in the EMAQ negative (α = 0.862), EMAQ positive (α = 0.841), YFAS (α = 0.811), and EAT-26 Eating Obsession (α = 0.819) subscales. The reliability level for RSB (α = 0.729) and EAT-26 Total (α = 0.773) was found to be acceptable. The reliability level for the EAT-26 Restriction and Social Pressure subscales was moderate, with α = 0.641. Participants’ RSB scores ranged from 10.0 to 55.0, with a total score average of 23.2 ± 4.63. The EMAQ negative average was 59.8 ± 21.05, and the EMAQ positive average was 43.5 ± 12.73. The total YFAS average is 5.4 ± 4.40. EAT-26 total scores range from 0.0 to 51.0, with an average of 21.49 ± 8.28 (Table 2).
Table 2
| Scales | Cronbach alpha | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| RSB total | 0.729 | 10.0 | 40.0 | 23.27 | 4.63 |
| EMAQ negative | 0.862 | 12.0 | 150.0 | 59.87 | 21.05 |
| EMAQ positive | 0.841 | 3.0 | 88.0 | 43.55 | 12.73 |
| YFAS total | 0.811 | 0.0 | 26.0 | 5.49 | 4.40 |
| EAT-26 dieting | 0.819 | 0.0 | 28.0 | 10.03 | 5.72 |
| EAT-26 bulimia and food preoccupation | 0.641 | 0.0 | 17.0 | 6.62 | 2.98 |
| EAT-26 oral control | 0.641 | 0.0 | 12.0 | 4.84 | 2.68 |
| EAT-26 total | 0.773 | 0.0 | 51.0 | 21.49 | 8.28 |
Descriptive statistics for scale scores with Cronbach Alpha internal consistency level.
RSB: Rosenberg Self Esteem Scale, EMAQ: The Emotional Appetite Questionnaire, YFAS: The Yale Food Addiction Scale, EAT-26: Eating Attitudes Test Short Form.
The preoccupation with eating sub-scale of EAT-26 was significantly correlated with the participants’ faculty (r = 0.080; p < 0.05), BMI (r = 0.246; p < 0.01), smoking (r = 0.084; p < 0.05), skipped snack (r = 0.092; p < 0.05), and eating out (place) (r = 0.086; p < 0.05). The restriction subscale of EAT-26 was significantly correlated with BMI (r = 0.100; p < 0.01) and adequate nutrition (r = 0.108; p < 0.01). The social pressure sub-scale of EAT-26 was significantly correlated with the participants’ faculty (r = −0.094; p < 0.01), BMI (r = −0.345; p < 0.01), and skipping snacks (r = −0.080; p < 0.01). EAT-26 total was significantly correlated with gender (r = 0.083; p < 0.05) and BMI (r = 0.083; p < 0.05) (Table 3).
Table 3
| Demographic characteristics | Dieting | Bulimia and food preoccupation | Oral control | EAT-26 SF total |
|---|---|---|---|---|
| Gender | 0.036 | 0.048 | 0.044 | 0.083 * |
| Faculty | 0.080 * | −0.064 | −0.094 ** | −0.002 |
| BMI | 0.246 ** | 0.100 ** | −0.345 ** | 0.083 * |
| Smoking | 0.084 * | 0.024 | 0.028 | 0.063 |
| Alcohol | 0.026 | 0.015 | 0.016 | 0.024 |
| Adequate nutrition | −0.018 | 0.108 ** | −0.038 | 0.005 |
| Skipping main meal | −0.007 | −0.062 | 0.028 | −0.013 |
| Skipped main meal | 0.066 | 0.067 | −0.052 | 0.047 |
| Skipping snack | 0.016 | −0.038 | −0.080 * | −0.025 |
| Skipped snack | 0.092 * | 0.013 | −0.004 | 0.056 |
| Eating outside | −0.019 | −0.033 | 0.011 | −0.020 |
| Outside meal | 0.013 | −0.007 | −0.047 | −0.016 |
| Eating outside frequency | −0.017 | −0.065 | 0.043 | −0.015 |
| Eating outside place | 0.086 * | −0.019 | 0.012 | 0.046 |
Correlation between EAT-26 and demographic characteristics.
*p < 0.05, **p < 0.01, BMI: Body Mass Index, EAT-26: Eating Attitudes Test Short Form.
There were statistically significant correlations between the preoccupation with eating subscale and RSB total (r = −0.149; p < 0.01), EMAQ negative (r = 0.222; p < 0.01), and YFAS total (r = 0.466; p < 0.01). The restriction subscale was significantly correlated with EMAQ positive (r = −0.141; p < 0.01). The social pressure sub-scale was significantly correlated with EMAQ negative (r = −0.088; p < 0.01) and EMAQ positive (r = 0.149; p < 0.01). The EAT-26 total score was significantly correlated with RSB total (r = −0.103; p < 0.01), EMAQ negative (r = 0.133; p < 0.01), and YFAS total (r = 0.323; p < 0.01) (Table 4).
Table 4
| Scales | Dieting | Bulimia and food preoccupation | Oral control | EAT-26 total |
|---|---|---|---|---|
| RSB total | −0.149 ** | 0.032 | −0.020 | −0.103 ** |
| EMAQ negative | 0.222 ** | 0.036 | −0.088 * | 0.133 ** |
| EMAQ positive | −0.069 | −0.141 ** | 0.149 ** | −0.024 |
| YFAS total | 0.466 ** | −0.070 | 0.054 | 0.323 ** |
Correlation between EAT 26 and RSB, EMAQ, and YFAS scales.
*p < 0.05, **p < 0.01. RSB: Rosenberg Self Esteem Scale, EMAQ: The Emotional Appetite Questionnaire, YFAS: The Yale Food Addiction Scale, EAT-26: Eating Attitudes Test Short Form.
Generalized linear model at multivariable level showed that the effects of gender (B = −2.00), EMAQ negative (B = 0.03; p < 0.05), and YFAS total (B = 0.496; p < 0.01) on EAT-26 were statistically significant (Table 5).
Table 5
| Parameter | B | Std. error | 95% Wald confidence ınterval | Hypothesis test | |||
|---|---|---|---|---|---|---|---|
| Lower | Upper | Wald chi-square | df | p-value | |||
| (Intercept) | 19.85 | 2.68 | 14.61 | 25.10 | 55.00 | 1 | 0.000 |
| [Gender = Female] | −2.00 | 0.71 | −3.39 | −0.62 | 8.04 | 1 | 0.005 |
| [Gender = Male] | 0a | . | . | . | . | . | . |
| [BMI = Underweight] | −2.18 | 2.14 | −6.36 | 2.01 | 1.04 | 1 | 0.308 |
| [BMI = Healthy weight] | −0.52 | 2.00 | −4.44 | 3.40 | 0.07 | 1 | 0.794 |
| [BMI = Overweight] | −0.53 | 2.11 | −4.67 | 3.61 | 0.06 | 1 | 0.802 |
| [BMI = Obese] | 0a | . | . | . | . | . | . |
| RSB Total | −0.08 | 0.06 | −0.20 | 0.05 | 1.50 | 1 | 0.221 |
| EMAQ Negative | 0.03 | 0.01 | 0.01 | 0.06 | 5.22 | 1 | 0.022 |
| YFAS Total | 0.50 | 0.07 | 0.36 | 0.63 | 53.24 | 1 | 0.000 |
| (Scale) | 61.38b | 3.14 | 55.52 | 67.86 | |||
Generalized linear model (scale logit) for effects of correlated factors on EAT-26 SF total score.
Dependent Variable: EAT26_Total. Model: (Intercept), Gender, BMI, RSB_Total, EMAQ_Negative, YFAS_Total. aSet to zero because this parameter is redundant, bMaximum likelihood estimate. RSB: Rosenberg Self Esteem Scale, EMAQ: The Emotional Appetite Questionnaire, YFAS: The Yale Food Addiction Scale.
Both synaptic weights over and under zero results showed artificial neural network results consistency (Figure 2).
Figure 2
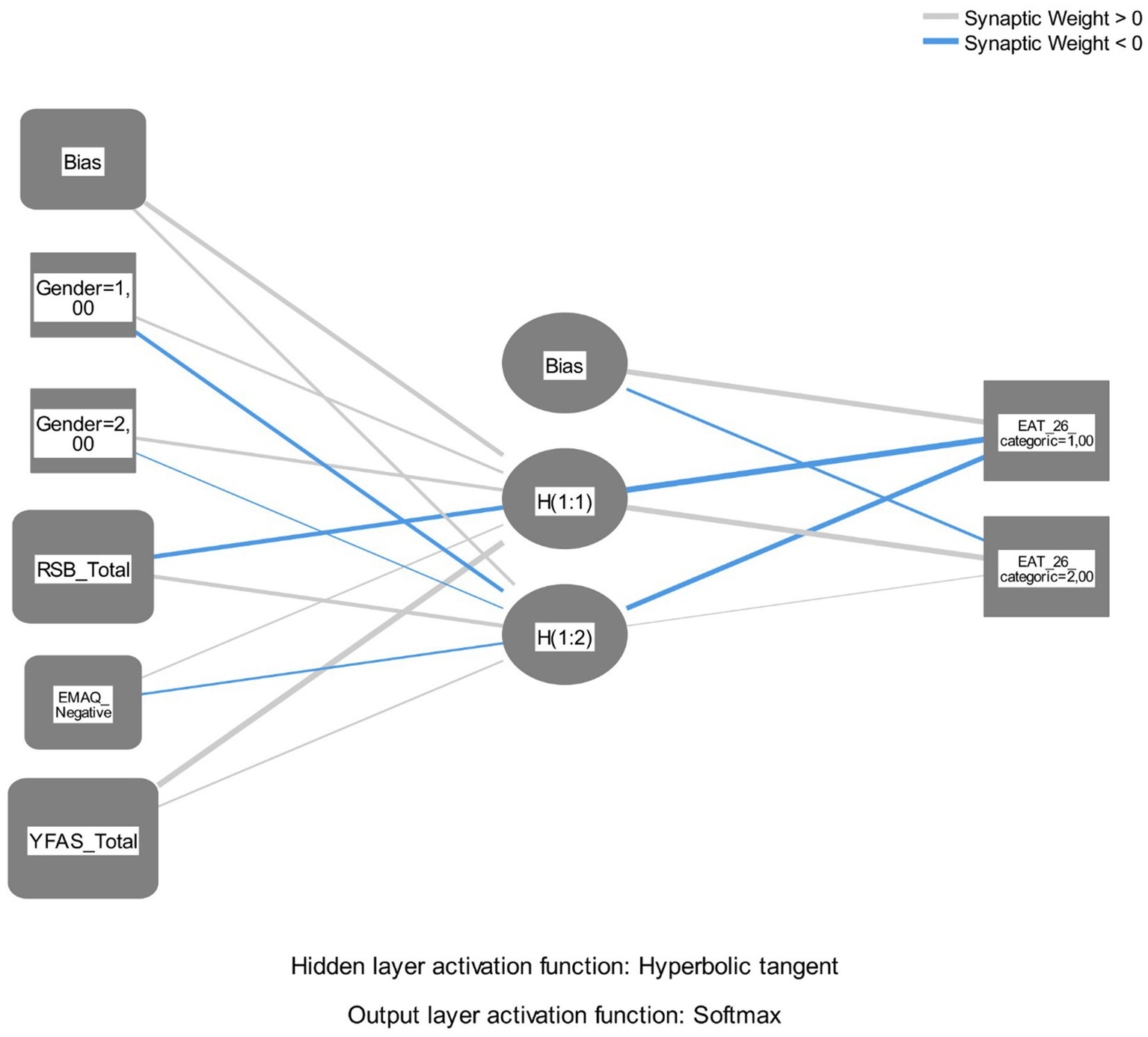
Artificial neural networks multilayer perceptron path results.
Hidden layer parameter values showed that YFAS had the highest value (0.950) followed by RSB (−0.538; absolute value) and EMAQ negative (0.302) in H(1:1) layer. In H(1:2) layer, RSB (0.536) had the highest value, followed by EMAQ negative (0.371; absolute value) and YFAS (0.340) (Table 6). According to the model summary output, the artificial neural network correctly classified 62.9% of the training data and 64.9% of the testing data, corresponding to incorrect prediction rates of 37.1 and 35.1%, respectively. These findings show that food addiction, self-esteem, and emotional eating are key predictors of disordered eating attitudes in the ANN model.
Table 6
| Predictor | Predicted | ||||
|---|---|---|---|---|---|
| Hidden layer 1 | Output layer | ||||
| H(1:1) | H(1:2) | EAT-26 = Under mean | EAT-26 = Over mean | ||
| Input layer | (Bias) | 0.544 | 0.429 | ||
| Gender = Female | 0.371 | −0.527 | |||
| Gender = Male | 0.469 | −0.235 | |||
| RSB Total | −0.538 | 0.536 | |||
| EMAQ Negative | 0.302 | −0.371 | |||
| YFAS Total | 0.950 | 0.340 | |||
| Hidden layer 1 | (Bias) | 0.603 | −0.409 | ||
| H(1:1) | −0.817 | 0.617 | |||
| H(1:2) | −0.579 | 0.044 | |||
Artificial neural networks multilayer perceptron layer levels.
RSB: Rosenberg Self Esteem Scale, EMAQ: The Emotional Appetite Questionnaire, YFAS: The Yale Food Addiction Scale.
The Gain and Lift curves presented in Figure 3 show that the multi-layer perceptron artificial neural network model performed better than random classification. Consistent with the model’s prediction threshold, the sensitivity obtained from the H(1:1) neuron in the hidden layer (66.9%) is higher than that of the H(1:2) neuron (64.9%). These findings support the internal consistency of the model and show that the neurons in the hidden layer contribute significantly to the classification process. The lift values obtained being above 1 reveal that the model is more effective than the random model, especially in identifying the positive class (those with EAT-26 scores above the average). These results support the sufficient predictive capacity of the artificial neural network model and the possibility of classification based on psychological variables associated with EAT-26 (Figure 2).
Figure 3
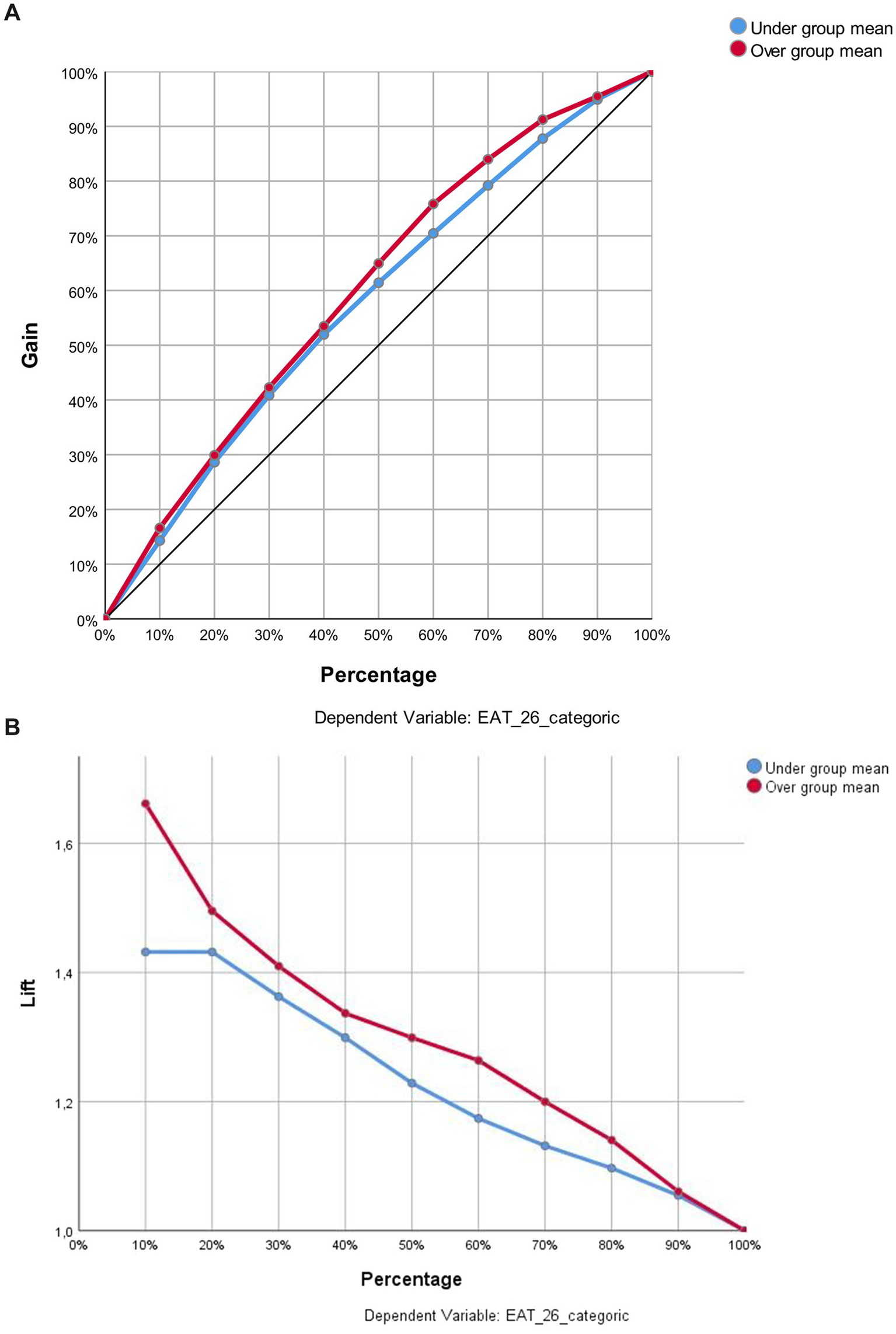
(A,B) Gain and lift charts for the classification performance of the model on eat-26 categories.
4 Discussion
Food addiction and disordered eating behaviors represent significant psychiatric concerns, influencing both the clinical manifestation and the effectiveness of treatment. Eating disorders have gained global attention due to their connection with social, cultural, and psychological factors that influence eating attitudes and behaviors. These mental health issues, characterized by maladaptive eating behaviors and body image concerns, have risk factors such as early dieting, excessive weight loss habits, depression, body dissatisfaction, and social media influences (Tisko and Casas, 2023; Lonergan et al., 2020; Toklu Baloglu and Caferoglu Akin, 2024).
This study examined the effect of self-esteem, emotional appetite, and food addiction on eating attitudes in young adults aged 20–30. A total of 766 volunteers, including 171 females and 595 males, participated in this descriptive cross-sectional study. The BMI range was 13.0% underweight, 71.8% healthy weight and 15.2% overweight/obese. Participants of 97.0% of them stated that they eat outside the home, and 57.4% of them eat at school or workplace restaurants, the majority skip breakfast or lunch, 71.5% eat out of home 1–6 times a week, and 58.1% eat at school-work restaurants (Table 1). As the frequency of eating out increases, especially when fast food and high-calorie foods are preferred, gaining weight and the risk of obesity may increase. Each additional meal eaten at fast food or sit-down restaurant per week is associated with a measurable increase in BMI (Bhutani et al., 2018). According to Petrovics et al. (2021), obesity and overweight were observed more frequently in men, whereas women scored higher on eating patterns such as uncontrolled eating, cognitive restraint, and emotional eating, which were linked to reduced self-esteem. Gender appears to be the main determinant of uncontrolled and emotional eating, whereas BMI shows a comparatively weaker effect. Similar studies have demonstrated a positive association between food addiction, eating disorders, and BMI, with findings indicating that women face a greater risk than men regarding both food addiction and eating disorders (Şengör and Gezer, 2019).
The relationship between eating behavior, emotional appetite, and food addiction is complex and multifaceted. Emotional appetite refers to eating in response to emotional cues rather than hunger. It is emphasized that individuals with a high tendency toward emotional eating are more likely to exhibit symptoms of food addiction (Borisenkov et al., 2020; Sanlier et al., 2017), and that emotional eating is positively associated with food addiction (Borisenkov et al., 2020). People experiencing stress and depression often resort to emotional eating, which can increase their risk of developing food addiction (Fernández et al., 2022). The positive and significant relationship among eating-related variables (eating styles, binge eating and bulimia) with food addiction was demonstrated (Escrivá-Martínez et al., 2023). Low self-esteem is linked to less healthy eating attitudes and a greater risk of food addiction (Sanlier et al., 2017).
In this study, the EAT-26 eating concern subscale was found to be significantly associated with educational level, BMI, smoking, skipping snacks, and eating out. Furthermore, the EAT-26 dieting subscale was significantly related to BMI, while the social pressure subscale was negatively associated with educational level and BMI. The total EAT-26 score was also significantly associated with gender and BMI (p < 0.01; p < 0.05) (Table 3). Our results are similar to those of other studies (Kim et al., 2016; Magni et al., 2024). Emotional eating acts as a precursor to food addiction and is often an maladaptive coping strategy for emotional distress (Bozkurt et al., 2024; Fernández et al., 2022; Rossi, 2025). Uncontrolled eating and frequent thoughts about food can make young people more vulnerable to addictive eating habits by mediating the relationship between emotional states and food addiction (Fernández et al., 2022; Rossi, 2025). Psychological distress (stress, depression, anxiety) can increase the likelihood of food addiction by encouraging emotional and uncontrolled eating behaviors (Brytek-Matera et al., 2021; Skinner et al., 2021). Mindful eating practices are associated with lower rates of food addiction, suggesting that interventions targeting awareness may help reduce risk (Kaya Cebioğlu et al., 2022). This situation highlights the critical role of cognitive factors in directing maladaptive coping mechanisms such as emotional eating. Furthermore, emotional eating can often serve as a precursor to excessive eating behaviors stemming from food addiction. In particular, emotional eating triggered by negative emotional states is considered a significant predictor of food addiction among adolescents (Rose et al., 2018).
The eating concern subscale was negatively correlated with RSB, EMAQ negative and YFAS, while the restriction subscale was positively correlated with EMAQ positive, the social pressure subscale of EMAQ negative and EMAQ positive, the EAT-26 score was significantly associated with RSB, EMAQ negative, and YFAS (Table 4). A study has shown that EAT-26 is positively correlated with EMAQ negative scores, indicating that individuals at higher risk of eating disorders are more likely to engage in negative emotional eating behaviors (Barnhart et al., 2024). Emotional eating triggered by negative emotions seems to play a significant role in both the onset and persistence of disordered eating behaviors. Our findings indicate that emotional appetite influences both eating behaviors and food addiction. Previous research has also shown that eating behavior, shaped by physical, psychological, and social factors, impacts individuals’ dietary habits and overall health (Dugué et al., 2016; Alexatou et al., 2025). Adolescents with low self-esteem may use food as a coping mechanism, leading to disordered eating patterns (Sanlier et al., 2017). Studies have found that EAT-26 scores are particularly positively associated with food addiction and emotional eating in response to negative emotions (Cinelli et al., 2020; Sanlier et al., 2017; Sanlier et al., 2017). The YFAS has been reported to be positively correlated with EMAQ-negative scores, indicating that individuals with higher levels of food addiction are more likely to exhibit emotional eating behaviors in response to negative affect. This suggests that emotional eating plays a role in both the development and maintenance of food addiction (Burrows et al., 2018; Sanlier et al., 2017; Barnhart et al., 2024).
The findings of this study reveal that psychosocial variables such as self-esteem, emotional appetite, and food addiction are significantly related to eating behavior. In particular, it shows that an increase in emotional appetite is significantly related to food addiction and problematic eating behavior, while a decrease in self-esteem is significantly related to unhealthy eating behavior. Eating attitudes emerge as a decisive factor in explaining eating behaviors in young adults, based on their meaningful relationships with these psychosocial variables. Mental images play a role in the development of various psychological disorders and show a strong relationship with emotional processes. In the context of eating disorders, negative emotions and the mechanisms used to regulate these emotions are among the key determinants (Dugué et al., 2016; Alexatou et al., 2025). Although evidence highlights a strong relationship between emotional appetite, eating behaviors, and food addiction, this does not mean that all individuals who exhibit emotional eating tendencies will develop food addiction. Factors such as resilience, coping strategies, and social support can reduce these risks.
A multivariate generalized linear model showed that gender EMAQ negative, and YFAS total had statistically significant effects on EAT-26 (Table 5). Emotional states such as stress, loneliness, and boredom are strongly associated with overeating, especially among adolescent girls. Women generally report higher rates of eating addiction, emotional eating, and disordered eating behaviors (Petrovics et al., 2021; Skinner et al., 2021). Body image and subjective body shape also influence self-esteem and eating attitudes, particularly in girls (Petrovics et al., 2021). In this study, the effect of gender on EAT-26 scores was found to be statistically significant. Women’s EAT-26 scores were significantly lower than men’s, suggesting that unhealthy eating attitudes may be more pronounced among men and that this group may represent a potential risk in terms of eating attitudes. This result may be attributed not only to individual differences but also to broader social, cultural, and environmental factors. The predominance of male participants in the sample should be considered when interpreting gender-related findings. However, the inclusion of gender in the GLM model helped to partially control for this imbalance, contributing to a more reliable interpretation of the results. Adolescents’ eating behaviors are influenced by various factors such as peer pressure, media exposure, and family dynamics, and these factors can either reduce or intensify the impact of self-esteem and emotional states on eating habits.
Disordered eating attitudes (as measured by EAT-26) are most strongly linked to higher BMI, female gender, lower self-esteem, negative emotional eating, and food addiction. Social and educational factors also play roles, especially in how individuals respond to social pressure and snacking cues. Interventions should consider these interconnected psychosocial and demographic factors for effective prevention and treatment. Disordered eating attitudes (as measured by EAT-26) are most strongly linked to higher BMI, female gender, lower selfesteem, negative emotional eating, and food addiction. The risk of disordered eating is best predicted by the interaction of BMI, gender, and age, rather than any single factor alone (Jahrami et al., 2019). Food addiction and negative emotional eating are strong, independent predictors of disordered eating attitudes, often co-occurring and more prevalent in women and those with higher BMI (Bozkurt et al., 2024; Rose et al., 2018; Yua et al., 2018; Pape et al., 2021). Higher self-esteem can protect against the negative impact of high BMI and body-related shame on disordered eating (Petrovics et al., 2021; Razmus et al., 2023). Disordered eating attitudes (as measured by EAT-26) are most strongly linked to higher BMI, female gender, lower self-esteem, negative emotional eating, and food addiction. Social and educational factors also play roles, especially in how individuals respond to social pressure and snacking cues. Interventions should consider these interconnected psychosocial and demographic factors for effective prevention and treatment.
Considering that junk food products, ultra-processed food, fast food etc. are products with a low nutritional value and are hypercaloric, with the risk of causing a food addiction to develop and significantly alter the state of health. Especially when these types of food predominate in the diet and are accompanied by an unhealthy lifestyle (Mititelu et al., 2023). The higher energy density and oro-sensory characteristics of ultra-processed foods, fast food, etc., may also allow for greater energy intake in a shorter period of time. However, increased unhealthy feeding rates may lead to an increased energy intake, potentially due to a delayed signaling of satiety (Teo et al., 2022).
5 Conclusion and recommendation
As a result, statistically significant correlations were found between EAT-26, Rosenberg RSB, YFAS, and EMAQ. The findings indicate that low self-esteem is associated with problematic eating attitudes and food addiction, while increased levels of negative emotional eating are significantly associated with both unhealthy eating attitudes and food addiction. According to GLM and artificial neural network analyses, the variables with the strongest influence on eating attitudes are food addiction and negative emotional appetite. Model outputs revealed that these psychological variables significantly affected EAT-26 scores and that eating attitudes can be evaluated as a multidimensional psychosocial structure. The findings suggest that eating attitudes may be an important determinant in understanding the risk of food addiction among young adults. In this context, low self-esteem, negative emotional eating tendencies, and high levels of food addiction are important factors associated with unhealthy eating behaviors. A better understanding of the relationships between these variables can contribute to the promotion of healthy eating habits and the development of intervention programs. In particular, it can be said that focusing on emotional appetite and food addiction is important in education and intervention programs aimed at preventing eating disorders. Low self-esteem and emotional eating are significant risk factors for food addiction and disordered eating behaviors. These relationships are complex and often reinforce each other, highlighting the importance of addressing psychological and emotional factors in interventions.
Food addiction, disordered eating attitudes, low self-esteem, and emotional appetite are deeply interconnected. Addressing emotional and cognitive factors especially self-esteem and emotional eating can be crucial for preventing and treating food addiction and related eating disorders.
6 Limitations and strengths
A notable strength of this study is its status as one of the limited investigations exploring the links between eating behavior, emotional appetite, and food addiction within a traditionally structured country like Turkey. The research is based on a large male sample and employs multidimensional analyses. The study provides detailed insights into the associations between variables such as age, gender, education, tobacco and alcohol use, body mass index, self-esteem, emotional eating, and food addiction, and eating attitudes. Notably, eating attitudes were identified as an important risk factor among male individuals. The overlap between the results of two different modeling approaches, GLM and ANN, enhances the reliability of the findings. The Artificial Neural Network (ANN) model, in particular, captured the links between eating attitudes and self-esteem, emotional appetite, and food addiction not only in a linear context but also in a more powerful and flexible way through its multi-layered, learning-based structure. The model outputs revealed the effects of these variables on the EAT-26 with high classification accuracy.
Nevertheless, the cross-sectional nature of the study restricts the ability to draw causal inferences. In addition, reliance on self-reported height and weight data may have introduced potential measurement errors. We acknowledge that BMI values were self-reported, which may introduce some measurement bias. However, self-reported BMI is widely used in large-scale epidemiological and nutrition studies and has been shown to be highly correlated with objectively measured BMI. Given the large sample size and the nature of the data collection process, direct anthropometric measurements were not feasible. Therefore, we decided to retain BMI in the analyses while clearly acknowledging this limitation in the manuscript. The predominance of male participants in the sample may also reduce generalizability. The study was conducted on a sample of individuals aged 19–30 living in a large city, which restricts the generalizability of the findings to all age groups in Turkey. Therefore, it is important to replicate the study in other regions/countries.
Statements
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The study received ethical approval from the Non-Interventional Ethics Committee of Ankara Medipol University on November 6, 2024 (Decision No: 136). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
NS: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. OA: Data curation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank the volunteers who participated in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Alexatou O. Papadopoulou S. K. Mentzelou M. Deligiannidou G. E. Dakanalis A. Giaginis C. (2025). Exploring the impact of emotional eating among university students: a literature review. Med Sci (Basel).13:56. doi: 10.3390/medsci13020056
2
Alim N. E. Gokustun K. K. Caliskan G. Besler Z. N. (2021). Do disordered eating behaviors have an effect on food addiction?Health Behav Policy Rev.8, 319–330. doi: 10.14485/HBPR.8.4.4
3
Barnhart W. R. Kalantzis M. Gaggiano C. Braden A. L. (2024). The relation between questionnaire-measured self-reported emotional eating and disordered eating behaviors: a meta-analysis of nearly three decades of research. Appetite198:107343. doi: 10.1016/j.appet.2024.107343
4
Bhutani S. Schoeller D. A. Walsh M. C. McWilliams C. (2018). Frequency of eating out at both fast-food and sit-down restaurants was associated with high body mass index in non-large metropolitan communities in Midwest. Am. J. Health Promot.32, 75–83. doi: 10.1177/0890117116660772
5
Bjorlie K. Forbush K. T. Chapa D. A. N. Richson B. N. Johnson S. N. Fazzino T. L. (2022). Hyper-palatable food consumption during binge-eating episodes: a comparison of intake during binge eating and restricting. Int. J. Eat. Disord.55, 688–696. doi: 10.1002/eat.23692
6
Borisenkov M. F. Popov S. V. Pecherkina A. A. Dorogina O. I. Martinson E. A. Vetosheva V. I. et al . (2020). Food addiction in young adult residents of Russia: associations with emotional and anthropometric characteristics. Eur. Eat. Disord. Rev.28, 465–472. doi: 10.1002/erv.2731
7
Bourdier L. Orri M. Carre A. Gearhardt A. N. Romo L. Dantzer C. et al . (2018). Are emotionally driven and addictive-like eating behaviors the missing links between psychological distress and greater body weight?Appetite120, 536–546. doi: 10.1016/j.appet.2017
8
Bozkurt O. Çamli A. Kocaadam-Bozkurt B. (2024). Factors affecting food addiction: emotional eating, palatable eating motivations, and BMI. Food Sci. Nutr.12, 6841–6848. doi: 10.1002/fsn3.4333
9
Brytek-Matera A. Obeid S. Akel M. Hallit S. (2021). How does food addiction relate to obesity? Patterns of psychological distress, eating behaviors and physical activity in a sample of Lebanese adults: the MATEO study. Int. J. Environ. Res. Public Health18:10979. doi: 10.3390/ijerph182010979
10
Burrows T. Kay-Lambkin F. Pursey K. Skinner J. Dayas C. (2018). Food addiction and associations with mental health symptoms: a systematic review with meta-analysis. J. Hum. Nutr. Diet.31, 544–572. doi: 10.1111/jhn.12532
11
Cinelli G. Criscuolo M. Bifone C. Chianello I. Castiglioni M. C. De Lorenzo A. et al . (2020). Food addiction in a group of Italian adolescents diagnosed for eating disorder. Nutrients12:1524. doi: 10.3390/nu12051524
12
DiNicolantonio J. J. O'Keefe J. H. Wilson W. L. (2018). Sugar addiction: is it real? A narrative review. Br. J. Sports Med.52, 910–913. doi: 10.1136/bjsports-2017-097971
13
Dugué R. Keller S. Tuschen-Caffier B. Jacob G. A. (2016). Exploring the mind's eye: contents and characteristics of mental images in overweight individuals with binge eating behaviour. Psychiatry Res.246, 554–560. doi: 10.1016/j.psychres.2016.10.028
14
Escrivá-Martínez T. Galiana L. Herrero R. Rodríguez-Arias M. Fernández-Aranda F. Gearhardt A. N. et al . (2023). Food addiction and its relationship with other eating behaviours among Spanish university students. J. Eat. Disord.11:60. doi: 10.1186/s40337-023-00772-5
15
Fernández M. S. Pilatti A. Pautassi R. M. (2022). Eating-to-cope motives and uncontrolled eating as mediators between negative emotional states and food addiction among Argentinean young adults. Int J Ment Health Addict.18, 1–19. doi: 10.1007/s11469-022-00934-7
16
Garner D. M. Garfinkel P. E. (1979). The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol. Med.9, 273–279. doi: 10.1017/S0033291700030762
17
Gearhardt A. N. Corbin W. R. Brownell K. D. (2009). Preliminary validation of the Yale food addiction scale. Appetite52, 430–436. doi: 10.1016/j.appet.2008.12.003
18
Gearhardt A. N. DiFeliceantonio A. G. (2023). Highly processed foods can be considered addictive substances based on established scientific criteria. Addiction118, 589–598. doi: 10.1111/add.16065
19
Jahrami H. Saif Z. Faris M. A. I. Levine M. P. (2019). The relationship between risk of eating disorders, age, gender and body mass index in medical students: a meta-regression. Eat. Weight Disord.24, 169–177. doi: 10.1007/s40519-018-0618-7
20
Kaya Cebioğlu İ. Dumlu Bilgin G. Kavsara H. K. Gül Koyuncu A. Sarioğlu A. Aydin S. et al . (2022). Food addiction among university students: the effect of mindful eating. Appetite177:106133. doi: 10.1016/j.appet.2022.106133
21
Kim J. Choue R. Lim H. (2016). Differences of socio-psychology, eating behavior, diet quality and quality of life in south Korean women according to their weight status. Clin Nutr Res.5, 161–171. doi: 10.7762/cnr.2016.5.3.161
22
Lipsky L. Haynie D. Cummings J. Nansel T. (2022). Food addiction, weight perception, dieting, and maladaptive eating behaviors in US young adults: an observational, prospective, nationally representative cohort study. Curr. Dev. Nutr.6:138. doi: 10.1093/cdn/nzac051.054
23
Lonergan A. R. Bussey K. Fardouly J. Griffiths S. Murray S. B. Hay P. et al . (2020). Protect me from my selfie: examining the association between photo-based social media behaviors and self-reported eating disorders in adolescence. Int. J. Eat. Disord.53, 755–766. doi: 10.1002/eat.23256
24
Magni O. Detopoulou P. Fappa E. Perrea A. Levidi D. Dedes V. et al . (2024). Eating attitudes, stress, anxiety, and depression in dietetic students and association with body mass index and body fat percent: a cross-sectional study. Diseases.12:108. doi: 10.3390/diseases12050108
25
Mititelu M. Oancea C. N. Neacșu S. M. Musuc A. M. Gheonea T. C. Stanciu T. I. et al . (2023). Evaluation of junk food consumption and the risk related to consumer health among the Romanian population. Nutrients15:3591. doi: 10.3390/nu15163591
26
Nolan L. J. Halperin L. B. Geliebter A. (2010). Emotional appetite questionnaire: construct validity and relationship with BMI. Appetite54, 314–319. doi: 10.1016/j.appet.2009.12.004
27
Pape M. Herpertz S. Schroeder S. Seiferth C. Färber T. Wolstein J. et al . (2021). Food addiction and its relationship to weight- and addiction-related psychological parameters in individuals with overweight and obesity. Front. Psychol.12:736454. doi: 10.3389/fpsyg.2021.736454
28
Paterna A. Alcaraz-Ibáñez M. Fuller-Tyszkiewicz M. Sicilia A. (2021). Internalization of body shape ideals and body dissatisfaction: A systematic review and meta-analysis. Int J Eat Disord, 16:1575–1600. doi: 10.1002/eat.23568
29
Petrovics P. Nagy A. Sandor B. Palfi A. Szekeres Z. Toth K. et al . (2021). Examination of self-esteem, body image, eating attitudes and cardiorespiratory performance in adolescents. Int. J. Environ. Res. Public Health18:13172. doi: 10.3390/ijerph182413172
30
Razmus M. Czubak-Paluch K. Brytek-Matera A. (2023). The relationship between body mass index and food preoccupation in women: a moderated mediation of body-related self-conscious emotions and self-esteem. Eur. Eat. Disord. Rev.31, 188–196. doi: 10.1002/erv.2955
31
Rose M. H. Nadler E. P. Mackey E. R. (2018). Impulse control in negative mood states, emotional eating, and food addiction are associated with lower quality of life in adolescents with severe obesity. J. Pediatr. Psychol.43, 443–451. doi: 10.1093/jpepsy/jsx127
32
Rosenberg M. (1965). Society and the adolescent self-image. Princeton, NJ: Princeton University Press.
33
Rossi A. A. (2025). Tying food addiction to uncontrolled eating: the roles of eating-related thoughts and emotional eating. Nutrients17:369. doi: 10.3390/nu17030369
34
Sahin E. Sanlier N. (2025). Relationships among nutrition knowledge level, healthy eating obsessions, body image, and social media usage in females: a cross-sectional study. BMC Public Health25:1711. doi: 10.1186/s12889-025-22689-1
35
Sanlier N. Baser F. Mortas H. Navruz Varli S. Macit M. S. Tatar T. (2017). Structural modeling the relationship of food addiction and eating attitudes of young adults with emotional appetite and self-esteem. Ecol. Food Nutr.56, 514–529. doi: 10.1080/03670244.2017.1388232
36
Sanlier N. Navruz Varli S. Macit M. S. Mortas H. Tatar T. (2017). Evaluation of disordered eating tendencies in young adults. Eat. Weight Disord.22, 623–631. doi: 10.1007/s40519-017-0430-9
37
Şengör G. Gezer C. (2019). Food addiction and its relationship with disordered eating behaviours and obesity. Eat. Weight Disord.24, 1031–1039. doi: 10.1007/s40519-019-00662-3
38
Serin Y. Şanlıer N. (2018). Emotional eating, the factors that affect food intake, and basic approaches to nursing care of patients with eating disorders. J. Psychiatr. Nurs.9, 135–146. doi: 10.14744/phd.2018.23600
39
Skinner J. Jebeile H. Burrows T. (2021). Food addiction and mental health in adolescents: a systematic review. Lancet Child Adolesc Health.5, 751–766. doi: 10.1016/S2352-4642(21)00126-7
40
Teo P. S. Lim A. J. Goh A. T. Choy J. Y. M. McCrickerd K. Forde C. G. (2022). Texture-based differences in eating rate influence energy intake for minimally processed and ultra-processed meals. Am. J. Clin. Nutr.116, 244–254. doi: 10.1093/ajcn/nqac068
41
Tisko M. G. Casas J. F. (2023). An examination of the associations between internet activities, body positivity content, and eating disorder symptomatology. Mod. Psychol. Stud.29:19.
42
Toklu Baloglu H. Caferoglu Akin Z. (2024). A cross-sectional descriptive analysis of technology addiction in adolescents: associations with food addiction, emotional eating, and body weight status. J. Health Popul. Nutr.43:187. doi: 10.1186/s41043-024-00675-4
43
World Health Organization (2000). Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ. Tech. Rep. Ser.894, i–xii,1-253.
44
World Health Organization . (2010). A healthy lifestyle –WHO recommendations. https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle-who-recommendations (Accessed May 13, 2025)
45
Yua Z. Indelicato N. A. Fuglestad P. Tan M. Bane L. Stice C. (2018). Sex differences in disordered eating and food addiction among college students. Appetite129, 12–18. doi: 10.1016/j.appet.2018.06.028
Summary
Keywords
young people, food addiction, self-esteem, emotional appetite, eating attitude
Citation
Sanlier N and Alyakut O (2025) The association between food addiction, eating attitudes, self-esteem, and emotional appetite: a cross-sectional study. Front. Psychol. 16:1703745. doi: 10.3389/fpsyg.2025.1703745
Received
12 September 2025
Accepted
28 October 2025
Published
14 November 2025
Volume
16 - 2025
Edited by
Boris C. Rodríguez-Martín, International University of La Rioja, Spain
Reviewed by
Ximena Díaz-Torrente, Universidad del Desarrollo, Chile
Filipe Reis Teodoro Andrade, University of Heidelberg, Germany
Updates
Copyright
© 2025 Sanlier and Alyakut.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nevin Sanlier, nevintekgul@gmail.com
ORCID: Nevin Sanlier, orcid.org/0000-0001-5937-0485
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.