Abstract
Background:
This study investigated the role of psychosomatic dysregulation as a mediating factor in the association between attachment insecurity and prolonged grief symptoms.
Methods:
A cross-sectional design was used to survey 227 adults who had lost a loved one due to oncological (n = 138) or traumatic causes (n = 89) (74.0% female; age = 48.11 ± 11.53 years). The two groups did not differ significantly in terms of age, gender, marital status, or living arrangement. Participants completed the relationship questionnaire, the psychosomatic dysregulation inventory, and the traumatic grief inventory SR +.
Results:
The severity of prolonged grief symptoms did not significantly differ between groups, although participants in the oncological loss group reported slightly higher symptom severity compared to the traumatic loss group. The prevalence of probable PGD was similar between groups, with 13.8% of the oncological group and 10.1% of the traumatic group meeting diagnostic criteria. Results of mediation analysis showed that psychosomatic dysregulation partially mediated the relationship between attachment anxiety and prolonged grief symptoms, whereas no significant mediation was observed for attachment avoidance.
Discussion:
These findings point out the importance of addressing psychosomatic processes in individuals with high attachment anxiety, in line with the hyperactivation model of the anxious attachment system, to better understand and support their grief responses.
1 Introduction
1.1 Definition and prevalence of prolonged grief disorder
Prolonged grief disorder (PGD) is a pathological response to the loss of a loved one that was recently included in major diagnostic systems, such as the International Classification of Diseases (ICD-11) (World Health Organization, 2018) and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) (American Psychiatric Association, 2022). According to these classifications, PGD is characterized by chronic (at least 6 months for ICD-11, at least 12 months for DSM-5 TR) and severe symptoms of separation distress (e.g., intense longing or/and persistent preoccupation for the deceased) along with cognitive, affective and behavioral symptoms (e.g., difficulty to accept the loss, emotional numbness, difficulty in engaging in social and leisure activities). These reactions exceed social and cultural norms for the patient’s context and cause significant disability and a need for clinical attention (World Health Organization, 2018; American Psychiatric Association, 2022).
Recent systematic reviews (Lundorff et al., 2017; Yuan et al., 2024) and empirical studies indicated a prevalence of PGD in bereaved adults of the general population ranging from 3 to 10% (Rosner et al., 2021; Shevlin et al., 2023; Treml et al., 2022), while the prevalence of any PGD symptoms (PGDS) is about threefold (Yuan et al., 2024). In Italy, characterized by a paucity of research on pathological grief, a recent study reported a prevalence of probable PGD of 7.7% among individuals who lost a loved one at least 12 months beforehand (Musetti et al., 2025). Certain populations seem to be at heightened risk for PGD (Rosner et al., 2021). Family caregivers of individuals with chronic and life-threatening illnesses, including neurological (Aoun et al., 2020; Crawley et al., 2023; Leonardi et al., 2012) and oncological diseases (Coelho et al., 2022; Sardella et al., 2023; Zordan et al., 2019), showed higher levels of PGD, respectively 20% (Schulz et al., 2006) and 14.2% (Kustanti et al., 2022). Similarly, individuals bereaved by sudden or violent losses, such as suicide, homicide, or accidents, tend to experience elevated rates of PGD, with around 49% affected (Djelantik et al., 2020). The difference in PGD rates between traumatic deaths and chronic illnesses has traditionally been explained in terms of anticipatory grief, the notion that in illness pathways, the possibility of “anticipating” the loss, in the case of chronic illness, may mitigate the intensity of bereavement, consequently reducing the psychopathological risk (Rogalla, 2020). However, as highlighted in the literature, the role of anticipatory grief is far from clear. Some studies have shown that, contrary to early hypotheses, high levels of pre-loss grief combined with poor preparation for bereavement are associated with worse, rather than better, post-loss outcomes (Nielsen et al., 2016).
Unfortunately, only a few studies have directly compared PGD or PGDS in individuals bereaved by chronic illness with those who lost a loved one to unnatural or traumatic causes (Cleiren et al., 1994; Miyabayashi and Yasuda, 2007). Moreover, no study has specifically focused on bereaved caregivers of cancer patients compared with individuals experiencing traumatic bereavement.
1.2 The contributory role of attachment insecurity and psychosomatic dysregulation
Attachment theory offers a meaningful framework for understanding individual differences in grief responses. Bowlby conceptualized attachment as an innate motivational system that drives humans to seek and maintain emotional closeness with caregivers and, later in adulthood, with others significant in their lives (Bowlby, 1969, 1988). The death of a close person can profoundly disrupt this system, compromising the mourner’s sense of safety and emotional regulation (Bowlby, 1980). Empirical research has highlighted two dimensions of attachment insecurity– attachment anxiety and avoidance—that originate in childhood and affect emotional responses and beliefs about the self and others throughout life (Ainsworth et al., 1978; Brennan et al., 1998; Hazan and Shaver, 1987). Individuals with attachment anxiety tend to frequently experience concerns that attachment figures may not be available in times of need. This dimension is often characterized by a negative self-image and heightened emotional sensitivity, leading to excessive dependence on others and difficulties in regulating emotions and bodily states (Mikulincer et al., 2003; Mikulincer and Shaver, 2019, 2022; Schimmenti and Caretti, 2018). Furthermore, attachment anxiety is associated with a higher risk of PGDS (Lai et al., 2015; Majd et al., 2024; Xu et al., 2015). By contrast, individuals with attachment avoidance tend to maintain emotional distance from others, inhibit their needs for care and feelings of vulnerability. They often express mistrust toward others’ intentions and tend to rely on self-reliant coping (Brennan et al., 1998). Although this strategy may offer short-term protection from emotional pain, it has been associated with physiological dysregulation and reduced engagement in adaptive coping mechanisms, potentially contributing to long-term psychopathological risk (Mikulincer and Shaver, 2019). However, meta-analytic evidence has not supported a direct association between attachment avoidance and PGDS (Buur et al., 2024). In this vein, some studies have proposed more complex explanatory models, suggesting that the effect of attachment avoidance on PGDS might emerge indirectly. For instance, a recent study found that attachment avoidance moderated the relationship between social support and PGDS, reducing the protective effect of social support (Lenzo et al., 2022).
In this framework, psychosomatic dysregulation may represent a key mechanism through which attachment insecurity may increase the risk for PGDS. The notion of psychosomatic dysregulation refers to a condition where difficulties in managing emotions and psychological states are expressed as physical symptoms or diseases that lack an objective medical cause (Schimmenti, 2017). Psychosomatic dysregulation denotes a disruption in the integration of bodily and affective processes, rooted in altered interoceptive and autonomic functioning, where emotional meaning fails to emerge from physiological states, leading to somatic expression rather than symbolic representation (Schimmenti, 2017). This condition is different from that of emotional dysregulation, which refers to the reduced ability to modulate, integrate, and express affective states within conscious experience and the social context and derives mainly from disorders in psychological regulatory networks. In brief, emotion dysregulation concerns the difficulty in managing emotions within awareness and relationships, whereas psychosomatic dysregulation concerns the failure to translate bodily states into emotional awareness, resulting in the body becoming the main stage of emotional communication (Schimmenti, 2017). Psychosomatic dysregulation is a cross-cutting mechanism that can occur in various clinical conditions, including apparently unrelated conditions like pediatric vasovagal syncope, where disturbances in autonomic and emotional regulation lead to syncopal episodes (Caretti et al., 2025). To stay on the topic of PGD, repeated experiences of insecure care can compromise the coordination between physiological activation and attribution of affective meaning (Maunder and Hunter, 2001). Over time, this can consolidate into a persistent tendency to communicate emotional needs somatically (Maunder and Hunter, 2001). Such a mode of operation, characterized by poor integration between systems, can hinder symbolic loss processing and impair adaptive pain regulation mechanisms, thus increasing vulnerability to PGD. A recent systematic review pointed out that PGDS are associated with somatic symptoms such as hypertension, insomnia, and other health concerns (Cunningham et al., 2025). Among bereaved family caregivers, sleep disturbances and impaired physical functioning reflecting wider difficulties in emotion regulation are common and persist long after the loss (Miller et al., 2020; Pohlkamp et al., 2019). Moreover, previous research consistently found that difficulties in emotion regulation and impaired reflective functioning (i.e., difficulties in understanding own and others’ mental states) were related to more severe PGDS (Giunta et al., 2024; Boelen et al., 2011; Lenferink et al., 2018; Milman et al., 2019). Despite these promising findings, research on the mediator role of psychosomatic dysregulation in the bereaved—particularly in those who lost a loved one to cancer or a traumatic accident—is still lacking. One study found that difficulties in recognizing emotions (i.e., alexithymia) were associated with PGDS (Lai et al., 2014). However, it remains unclear whether and how attachment insecurity may affect PGDS through psychosomatic dysregulation, a potential pathway that has received limited empirical attention to date.
Based on these premises, this study aimed to achieve two main objectives. First, we sought to compare the severity of PGDS and the prevalence of probable PGD between individuals who experienced bereavement due to oncological loss versus those who faced traumatic loss. We hypothesized that differences between these two groups would be smaller than traditionally assumed. Second, we aimed to explore the possible mediating role of psychosomatic dysregulation in the relationship between attachment styles and depressive symptoms. We hypothesized that psychosomatic dysregulation would mediate the relationship between insecure attachment styles and PGDS. The hypothesized model is illustrated in Figure 1.
Figure 1
Model depicting the potential mediating role of psychosomatic dysregulation in the relationships between insecure attachment insecurity and the severity of prolonged grief symptoms.
2 Methods
2.1 Participants and procedures
The present study was part of a broader research project aiming at the Italian validation of the Traumatic Grief Inventory Self-Report Version Plus (TGI-SR+) (Lenferink et al., 2022). A cross-sectional observational design was adopted, comparing individuals bereaved by oncological or traumatic loss on psychological outcomes related to prolonged grief. Data was collected between July 2023 and August 2024. Participants in the oncological loss group were recruited through direct contact with coordinators of three Local Health Units of the Italian National Health Service (INHS) in Central and Southern Italy. These coordinators subsequently invited family caregivers of deceased end-of-life cancer patients to participate in the study. Inclusion criteria were age between 18 and 65 years and self-reported adequate fluency in the Italian language. Exclusion criteria included experiencing a loss within the past year and having a preexisting or current diagnosis of a severe mental disorder (e.g., bipolar disorder, psychosis) or dementia. Among the caregivers contacted, 156 agreed to participate on a voluntary basis. Two participants were excluded due to a preexisting or current severe mental disorder, while a further 16 participants were excluded because they were older than 65 years, resulting in a final sample of 138 participants. The comparison group (n = 89) was drawn from the sample involved in the Italian validation of the TGI-SR+, including individuals who had experienced a traumatic loss (e.g., accident, natural disaster, heart attack, suicide), and matching participants based on age and gender. Participants in this group were selected to match the oncological loss group in terms of age and gender. The study was conducted in accordance with the 1964 Helsinki Declaration and its subsequent amendments. Approval was obtained from the Ethics Review Board of Psychology Research of the University of Catania (Prot. n° Ierb-Edunict-2023.01.16/5). All participants provided informed consent prior to participation, and their privacy was protected in accordance with the European Union General Data Protection Regulation (EU GDPR 2016/679).
2.2 Measures
Demographic information comprised age, gender, educational background, and occupational status. Bereavement-related information included time since the loss, kinship relationship to the deceased, and cause of death. The following instruments were administered:
The Traumatic Grief Inventory Self-Report Version Plus (TGI-SR+) (Lenferink et al., 2022). The TGI-SR + is a self-report instrument to assess PGD according to DSM-5-TR criteria (American Psychiatric Association, 2022). It consists of 22 items rated on a 5-point Likert scale ranging from “Never” (World Health Organization, 2018) to “Always” (Rosner et al., 2021). Higher scores indicate a greater severity of PGDS, with each item reflecting a symptom experienced by the individual during the last year. To meet the DSM-5-TR criteria for PGD (American Psychiatric Association, 2022), participants should rate as “often” or “always” at least one out of two items assessing Criterion B (separation distress; items 1 and 3); at least three out of eight items assessing Criterion C (cognitive, emotional, and behavioral symptoms; items 6, 9, 10, 11, 18, 19, 21, and one between items 2 and 8); and the single item assessing Criterion D (functional impairment; item 13). The original version (Lenferink et al., 2022) demonstrated good internal consistency, with McDonald’s omega values of 0.92 for DSM-5-TR PGDS in both bereaved community samples and individuals who lost loved ones in traffic accidents. For probable DSM-5-TR PGD belonging, Lenferink and colleagues (Lenferink et al., 2022) identified the optimal cut-off score as ≥71 of the total score of the TGI-SR+. In the current study, the Italian version of the TGI-SR + (Lenzo et al., 2025; Sideli et al., 2022) showed excellent internal consistency with a McDonald’s omega value of 0.95 for both samples.
The relationship questionnaire (RQ) (Bartholomew and Horowitz, 1991). The RQ is a self-report instrument to assess four prototypical attachment styles, based on the positive or negative representations of self or others. Participants rate their agreement with four first-person statements, each corresponding to a specific attachment style, using a 7-point Likert scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). The four prototypical attachment styles include: (a) secure attachment (RQ Secure), reflecting a positive view of both self and others; (b) dismissing attachment (RQ Dismissing), characterized by a positive view of self and a negative view of others; (c) preoccupied attachment (RQ Preoccupied), marked by a negative view of self and a positive view of others; and (d) fearful attachment (RQ Fearful), involving negative view of both self and others. In the present study, we employed the Italian version of the RQ, which has shown adequate psychometric properties (Carli, 1995). Following previous research (Brennan et al., 1998), two composite measures of attachment insecurity were calculated: attachment avoidance [(dismissing + fearful)—(secure + preoccupied)] and attachment anxiety [(preoccupied + fearful)—(secure + dismissing)].
The psychosomatic dysregulation inventory (PDI) (Caretti et al., 2019). The PDI consists of 101 items that assess various somatic symptoms using a 4-point Likert scale from 0 (“Never”) to 3 (“Very often or always”). Its development was informed by integrative perspectives combining neurobiological models of attachment with theories of psychosomatic functioning, drawing on work by Damasio (1996), Panksepp (1998), and Porges (2001). For this study, we used the short version of the PDI, which includes 20 items aimed at identifying risk for psychosomatic dysregulation. Specifically, this short version focuses on bodily symptoms and altered interoceptive experiences that indicate impairments in emotion recognition and regulation. This short form has demonstrated excellent internal consistency and good convergent and predictive validity in both clinical and nonclinical samples (Schimmenti, 2017). In the current study, the PDI showed excellent internal consistency with Cronbach’s alpha values of 0.90 for the oncological group and 0.93 for the traumatic group, respectively.
2.3 Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics version 29 and PROCESS macro for SPSS version 4.3 (Hayes, 2022). Descriptive statistics were computed for sociodemographic and bereavement-related variables. Group comparisons between participants who experienced an oncological loss and those who experienced a traumatic loss were conducted using independent samples t-tests for continuous variables and chi-square tests or Fisher’s exact tests for categorical variables. Two separate mediation analyses were conducted to examine the mediating role of psychosomatic dysregulation in the relationship between attachment insecurity dimensions (i.e., attachment anxiety and attachment avoidance) and the severity of PGDS. In each model, attachment anxiety and attachment avoidance were the independent variables, psychosomatic dysregulation was the mediator, and the severity of PGDS was the outcome variable. Type of loss (oncological vs. traumatic) and time since loss were included as covariates. The significance of indirect effects was evaluated using the bootstrapping method with 5,000 resamples and bias-corrected accelerated 95% confidence intervals (CIs) (Preacher and Hayes, 2004). Unstandardized regression coefficients (B), standardized coefficients (β), and standard errors (SE) were reported for all paths. An indirect effect was considered significant when the 95% confidence interval did not include zero. All statistical tests were two-tailed, and significance was set at p < 0.05.
3 Results
3.1 Characteristics of the participants
Table 1 shows the demographic and loss-related characteristics of the sample by oncological [n = 138] and traumatic group [n = 89]. The two groups did not significantly differ neither in age oncological loss group, 47.64 (SD = 12.01) vs. traumatic loss group, [48.94 years (SD = 10.89), t (225) = 0.44, p = 0.66], nor in gender distribution [74.6% female (n = 103) vs. 73.0% (n = 65), χ2(1) = 0.07, p = 0.79]. Moreover, no significant differences were found between groups regarding marital status, with the most frequent category being “married/cohabitant,” representing 44.2% [n = 61] of the oncological loss group and 53.9% [n = 48] of the traumatic loss group [χ2(2) = 3.39, p = 0.18]. No significant difference was also found in living arrangement, with most participants in both groups living with others [oncological loss group, 75.4% (n = 104) vs. traumatic loss group, 79.8% (n = 71), χ2(1) = 0.60, p = 0.44]. However, a significant difference was found between groups in terms of educational level, with participants in the traumatic loss group were more likely to have a graduate or post-graduate degree [64% (n = 57) vs. 45.7% (n = 63), χ2(1) = 7.35, p = 0.007]. Regarding loss-related characteristics, participants in the oncological loss group reported a significantly more recent loss compared to those in the traumatic loss group [M = 3.50 years, SD = 3.47 vs. M = 13.11 years, SD = 10.97, t (224) = −9.56, p < 0.001]. Furthermore, in the oncological loss group, most of the participants were sons or daughters of the deceased [66.7%, n = 92], whereas in the traumatic loss group, the distribution was more heterogeneous, with 44.9% [n = 40] losing an “Other” significant other (i.e., grandfather, cousin, mother-in-law) and 43.8% [n = 39] as sons or daughters.
Table 1
| Characteristics | Oncological loss (n = 138) | Traumatic loss (n = 89) | Statistic | p |
|---|---|---|---|---|
| Age, M (SD) | 47.64 (12.01) | 48.94 (10.89) | t (225) = 0.44 | 0.66 |
| 73.0% (n = 65) | ||||
| Gender, % (n) female | 74.6% (n = 103) | χ 2(1) = 0.07 | 0.79 | |
| Education, % (n) | χ 2(2) = 7.35 | 0.007 | ||
| Middle or high school diploma | 54.3% (n = 75) | 36.0% (n = 32) | ||
| Graduate or post-graduate | 45.7% (n = 63) | 64.0% (n = 57) | ||
| Marital status, % (n) | χ 2(2) = 3.39 | 0.18 | ||
| Single | 30.4% (n = 42) | 30.3% (n = 27) | ||
| Married/Cohabitant | 44.2% (n = 61) | 53.9% (n = 48) | ||
| Separated/divorced/widowed | 25.4% (n = 35) | 15.7% (n = 14) | ||
| Living arrangement, % (n) | χ 2(1) = 0.60 | 0.44 | ||
| Lives alone | 24.6% (n = 34) | 20.2% (n = 18) | ||
| Lives with others | 75.4% (n = 104) | 79.8% (n = 71) | ||
| Time since the loss, M (SD) | 3.50 (3.47) | 13.11 (10.97) | t (224) = −9.56 | <0.001 |
| Kinship to deceased, % (n) | FFH = 38.96 | <0.001 | ||
| Son/daughter | 66.7% (n = 92) | 43.8% (n = 39) | ||
| Sibling | 6.5% (n = 9) | 6.7% (n = 6) | ||
| Spouse | 16.7% (n = 23) | 4.5% (n = 4) | ||
| Other | 10.1% (n = 14) | 44.9% (n = 40) |
Demographic and loss-related characteristics of the sample by group.
M, mean; SD, standard deviation. Chi-square, t-test and Fisher–Freeman–Halton exact test statistics refer to between-group comparisons. There is one missing data for time since the loss in the oncological group.
3.2 Severity of PGDS and prevalence of probable diagnosis
The mean TGI-SR + total score did not significantly differ between the oncological and the traumatic group [55.13 (SD = 21.58) in vs. 49.87 (SD = 18.82), t (225) = 1.885, p = 0.061]. A probable diagnosis of PGD, defined in accordance with DSM-5-TR criteria operationalized through the TGI-SR + algorithm, was identified in 13.8% of the caregivers [n = 19] and in 10.1% of the individuals in the traumatic bereavement group [n = 9]. The difference in prevalence between the two groups was not statistically significant [χ2(1) = 0.669, p = 0.414], indicating a comparable proportion of individuals meeting criteria for probable PGD across the two samples.
3.3 Mediation analyses
Figures 2a,b present the results of the mediation analyses. As shown in Figure 2a, attachment anxiety had a significant direct effect on PGDS [b = 1.08, SE = 0.28, p < 0.001, 95% CI (0.53, 1.63)], and psychosomatic dysregulation significantly mediated this relationship [indirect effect = 0.91, BootSE = 0.19, 95% CI (0.56, 1.30)]. Specifically, higher attachment anxiety was associated with greater psychosomatic dysregulation [b = 0.06, SE = 0.01, p < 0.001, 95% CI (0.04, 0.07)], which in turn predicted more severe PGDS [b = 15.37, SE = 2.25, p < 0.001, 95% CI (10.93, 19.80)]. The model reached a R2 of 0.35.
Figure 2
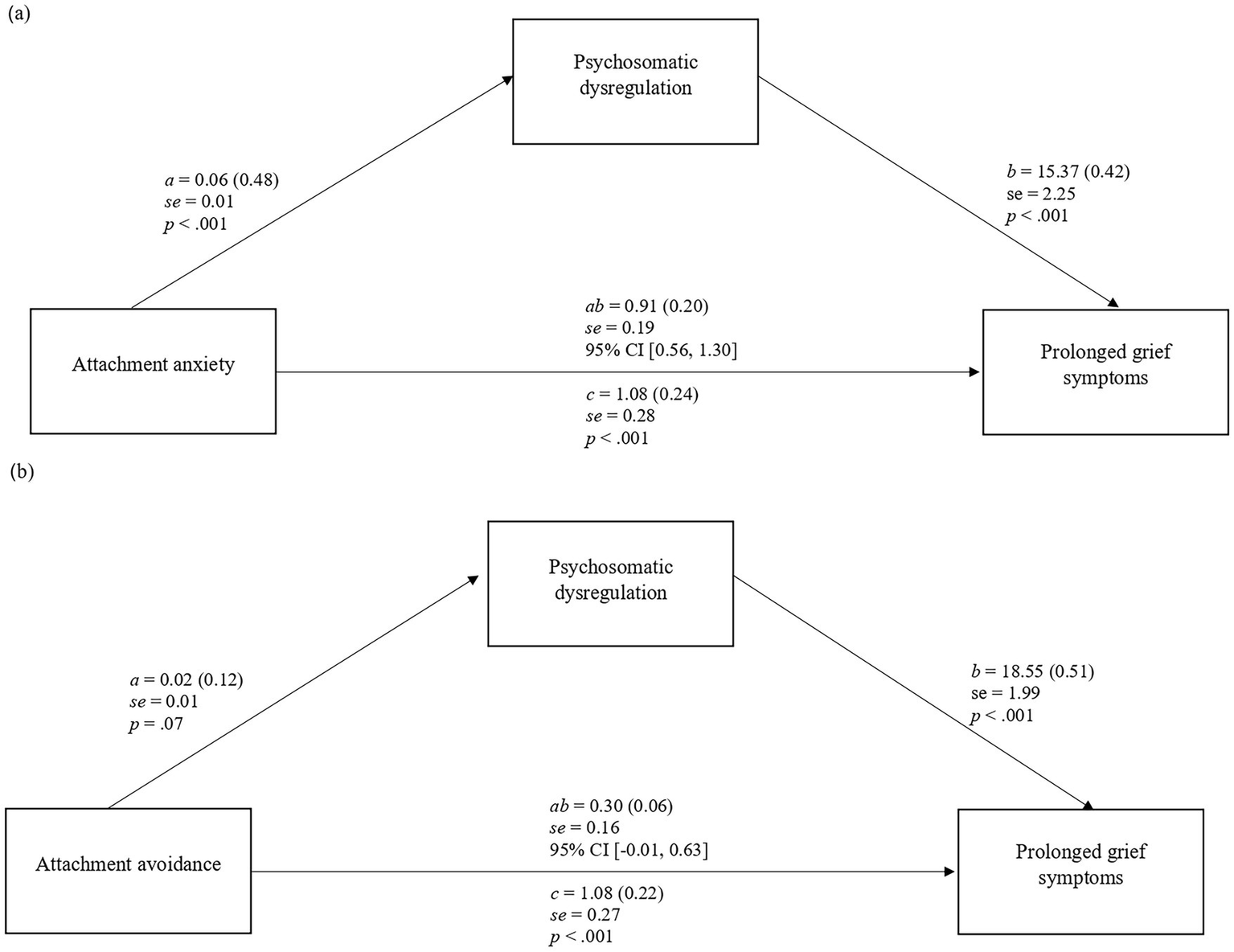
(a,b) Simple mediation model of attachment orientation on severity of prolonged grief symptoms through psychosomatic dysregulation. Values are unstandardized B coefficients (standardized coefficients are in parentheses). SE, standard error of B. a, effect of X on M; b, effect of M on Y; c, direct effect of X on Y; ab, indirect effect.
Regarding Figure 2b, attachment avoidance showed a significant direct effect on PGDS [b = 1.08, SE = 0.27, p < 0.001, 95% CI (0.54, 1.61)]. Psychosomatic dysregulation did not significantly mediate the relationship between attachment avoidance and prolonged grief [indirect effect = 0.30, BootSE = 0.16, 95% CI (−0.01, 0.63)]. Attachment avoidance was marginally associated with psychosomatic dysregulation [b = 0.02, SE = 0.01, p = 0.07, 95% CI (0.00, 0.03)]. The model achieved a R2 of 0.35. Type of loss (oncological vs. traumatic) and time since loss were included as covariates but did not show consistent significant effects in both models.
4 Discussion
To the best of our knowledge, this study is the first to compare PGDS in individuals who have lost a loved one due to an oncological condition with those who have experienced a loss from an immediate unnatural cause, such as suicide, heart attack, natural disaster, or accident.
According to our first hypothesis, the oncological loss group and the traumatic loss group did not show significant differences in the likelihood of receiving a diagnosis of PGD. Our findings suggest that the type of loss, whether anticipated through a long period, such as cancer, or sudden and unexpectedness, such as traumatic, may not entirely determine the likelihood of a diagnosis of PGD. Put another way, both types of bereavement may lead to persistent and maladaptive grief reactions. This finding is coherent with previous studies highlighting that cancer-related losses are associated with high levels of PGDS (Coelho et al., 2022; Sardella et al., 2023; Zordan et al., 2019). It is also consistent with recent findings on anticipatory grief, which highlight how prolonged caregiving under the burden of a loved one’s progressive decline can lead to maladaptive pain reactions following a loss (Nielsen et al., 2016). Together with the unexpectedness of traumatic grief, it should also be considered the prolonged stress related to a chronic disease among people who have lost their loved ones.
It is worth noting that those bereaved due to cancer in our study experienced a more recent loss compared to those bereaved due to a traumatic loss. Although some studies have found that a shorter time since loss is associated with higher symptom severity (Schwartz et al., 2018), others have found no significant relationship (Boelen and Lenferink, 2022). Our results contribute to this debate on the role of time during grief, suggesting that while it may shape symptom intensity to some extent, psychological mechanisms underlying grief may play a relevant role in determining who is at higher risk of PGD. It is therefore plausible that time since loss interacts with other individual and contextual variables, shaping the manifestation and persistence of grief symptoms rather than determining them in isolation. In this vein, the second aim was to investigate the mediating role of psychosomatic dysregulation in the relationship between insecure attachment orientations and the severity of PGDS. It is not surprising that individuals with high attachment anxiety tend to experience more severe grief reactions, as demonstrated by previous research (Lai et al., 2015; Xu et al., 2015; Majd et al., 2024). Indeed, attachment anxiety is characterized by hyperactivation strategies, including heightened vigilance to threats, distress when separated from significant others, and difficulties in regulating negative emotions (Mikulincer and Shaver, 2019, 2022). Our findings revealed that psychosomatic dysregulation had a mediating role in the path originating from attachment anxiety to PGDS. It is reasonable to hypothesize that it represents a key pathway through which attachment anxiety may lead to prolonged grief reactions. Difficulties in modulating emotions and bodily states may heighten somatic arousal, worsen sleep quality, and increase health complaints, which in turn reinforce distress associated with the loss, fostering a vicious cycle. These findings seem to be consistent with evidence that bereavement is often accompanied by bodily and somatic symptoms, and that difficulties in emotion regulation are associated with pathological grief severity. A different pattern emerged for attachment avoidance that requires further research. Our findings revealed a direct effect on PGDS, despite psychosomatic dysregulation did not mediate this association. Individuals with attachment avoidance tend to suppress attachment needs, maintain emotional distance, and rely on self-reliant coping strategies (Brennan et al., 1998). Psychosomatic dysregulation, indeed, involves difficulties perceiving internal states and sharing them in social contexts, including those related to loved ones. In the context of grief, these bereaved tend to deactivate their attachment system, thus often displaying a lack of awareness or minimization of their internal states in the relationship. However, this insecure attachment orientation does not protect them from prolonged PGDS, but it may outline other pathways to the disorders. Although literature reported a non-significant association between attachment avoidance and PGDS (Buur et al., 2024), some recent research highlighted some other pathways (Lenzo et al., 2022; Giunta et al., 2024). Thus, it is plausible to hypothesize that attachment avoidance showed a significant effect through mechanisms other than psychosomatic dysregulation—for example, such as poor reflective functioning (Giunta et al., 2024)—or increased physiological stress reactivity that remains unrecognized (Mikulincer and Shaver, 2019). Future research should investigate these complex pathways from attachment to grief reactions.
Findings from this study may have significant clinical implications, highlighting the need for tailored psychological interventions in order to increase therapeutic efficacy in PGD. For example, in individuals with attachment anxiety, characterized by an overactivation of the attachment system and difficulties in emotional regulation (Mikulincer and Shaver, 2019, 2022), approaches centered on the development of affective regulation strategies could be indicated, such as cognitive-behavioral therapy focused on grief and mindfulness techniques (Srivastava et al., 2025). Differently, in subjects with avoidant attachment, who tend to suppress relational needs and emotional states (Brennan et al., 1998; Mikulincer and Shaver, 2019), a gradual approach oriented toward mentalization and emotional awareness could be useful, such as psychodynamic therapy focused on grief or interventions based on mentalization-based therapy (Srivastava et al., 2025). These considerations highlight the significance of a differentiated and multimodal therapeutic approach that integrates both top-down and bottom-up components, while also considering attachment orientation as a clinically relevant variable.
Although this study offers insight into the relationship between attachment insecurity and PGDS, some limitations should be considered. Firstly, the cross-sectional design inherently restricts causal interpretations and precludes a comprehensive understanding of the potentially reciprocal dynamics underlying the observed associations. Psychosomatic dysregulation, for instance, may function both as a contributing factor to the intensification of PGD and as a process exacerbated by the emotional burden of prolonged grief. Secondly, some sample characteristics such as the predominance of female participants in both groups may introduce a sampling bias, which could affect the external validity and limit the generalizability of the results, especially for male bereaved. Thirdly, even though the time since loss was statistically controlled for in the mediation analyses, its potential residual influence cannot be entirely ruled out. Lastly, the use of self-report instruments to assess attachment, psychosomatic dysregulation, and PGDS (TGI-SR+, RQ, PDI), though validated and widely used, entails potential biases related to social desirability and self-perception.
In sum, this study points out that psychosomatic dysregulation partially mediates the association between attachment anxiety and PGDS, whereas no mediation was found for attachment avoidance, suggesting distinct underlying pathways. These findings highlight the central relevance of bodily process and emotional regulation in grief reactions. Psychological interventions that foster body–mind integration for bereaved individuals with attachment anxiety, independently by the type of loss, may be efficacy for PGDS.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethic Review Board of Psychology Research of the University of Catania (Prot. n° Ierb-Edunict-2023.01.16/5). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
VL: Writing – review & editing, Writing – original draft, Methodology, Project administration, Formal analysis, Supervision, Conceptualization. ST: Formal analysis, Writing – original draft, Data curation, Writing – review & editing. MQ: Writing – review & editing, Methodology, Writing – original draft, Conceptualization, Supervision. VB: Writing – review & editing, Investigation. FC: Writing – review & editing, Investigation. LL: Writing – review & editing, Investigation. VC: Supervision, Writing – original draft, Writing – review & editing. AS: Writing – review & editing, Supervision, Methodology, Writing – original draft, Conceptualization. LS: Supervision, Writing – original draft, Formal analysis, Project administration, Methodology, Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AbbreviationDSM-5-TR, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision; ICD-11, International Classification of Diseases; PDI, Psychosomatic Dysregulation Inventory; PGD, Prolonged Grief Disorder; PGDS, Prolonged Grief Disorder Symptoms; RQ, Relationship Questionnaire; TGI-SR+, Traumatic Grief Inventory Self-Report Version Plus.
References
1
Ainsworth M. D. S. Blehar M. C. Water E. Wall S. (1978). Patterns of attachment: a psychological study of the strange situation. Hillsdale, NJ: Erlbaum.
2
American Psychiatric Association (2022). Diagnostic and statistical manual of mental disorders, fifth edition, text revision (DSM-5-TR). Washington, D.C.: American Psychiatric Association Publishing.
3
Aoun S. M. Kissane D. W. Cafarella P. A. Rumbold B. Hogden A. Jiang L. et al . (2020). Grief, depression, and anxiety in bereaved caregivers of people with motor neurone disease: a population-based national study. Amyotroph. Lateral Scler. Frontotemporal Degener.21, 593–605. doi: 10.1080/21678421.2020.1790610
4
Bartholomew K. Horowitz L. M. (1991). Attachment styles among young adults: a test of a four-category model. J. Pers. Soc. Psychol.61, 226–244. doi: 10.1037/0022-3514.61.2.226
5
Boelen P. A. De Keijser J. Van Den Hout M. A. Van Den Bout J. (2011). Factors associated with outcome of cognitive–behavioural therapy for complicated grief: a preliminary study. Clin. Psychol. Psychother.18, 284–291. doi: 10.1002/cpp.720
6
Boelen P. A. Lenferink L. I. (2022). Prolonged grief disorder in DSM-5-TR: early predictors and longitudinal measurement invariance. Aust. N. Z. J. Psychiatry56, 667–674. doi: 10.1177/00048674211025728
7
Bowlby J. (1969). Attachment and loss: vol. 1: attachment. New York, NY: Basic Books.
8
Bowlby J. (1980). Attachment and loss: vol. 3. Sadness and depression. New York, NY: Basic Books.
9
Bowlby J. (1988). “A secure base: clinical applications of attachment theory” in Psychotherapy: theory, research, practice, training (New York, NY: Routledge).
10
Brennan K. A. Clark C. L. Shaver P. R. (1998). Self-report measurement of adult attachment: an integrative overview. In SimpsonJ. A.RholesW. S. (Eds.), Attachment theory and close relationships (New York, NY: The Guilford Press), 46–76.
11
Buur C. Zachariae R. Komischke-Konnerup K. B. Marello M. M. Schierff L. H. O’Connor M. (2024). Risk factors for prolonged grief symptoms: a systematic review and meta-analysis. Clin. Psychol. Rev.107:102375. doi: 10.1016/j.cpr.2023.102375
12
Caretti V. Schimmenti A. Porcelli P. Temperani D. Temperani A. Tizi C. et al . (2019). Psychosomatic dysregulation inventory: Italian validation in a clinical sample. Psychother. Psychosom.88:20.
13
Caretti V. Sideli L. Guccione C. Cuzzocrea G. Guido C. A. Spalice A. et al . (2025). Autonomic nervous system regulation and attachment patterns in children with vasovagal syncope: a theoretical framework in light of the polyvagal theory. Mediterr. J. Clin. Psychol.13, 1–19. doi: 10.13129/2282-1619/mjcp-4646
14
Carli L. (1995). Attaccamento e rapporto di coppia: Il modello di Bowlby nell’interpretazione del ciclo di vita.Milano: Raffaello Cortina Editore.
15
Cleiren M. Diekstra R. F. Kerkhof A. J. Van der Wal J. (1994). Mode of death and kinship in bereavement: focusing on “who” rather than “how.”. Crisis15, 22–36.
16
Coelho A. Roberto M. Barros L. Barbosa A. (2022). Family caregiver grief and post-loss adjustment: a longitudinal cohort study. Palliat. Support. Care20, 348–356. doi: 10.1017/S147895152100095X
17
Crawley S. Sampson E. L. Moore K. J. Kupeli N. West E. (2023). Grief in family carers of people living with dementia: a systematic review. Int. Psychogeriatr.35, 477–508. doi: 10.1017/S1041610221002787
18
Cunningham J. Shevlin M. Cerda C. McElroy E. (2025). ICD-11 prolonged grief disorder, physical health, and somatic problems: a systematic review. Clin Psychol Eur.7:e14351. doi: 10.32872/cpe.14351
19
Damasio A. R. (1996). The somatic marker hypothesis and the possible functions of the prefrontal cortex. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci.29, 1413–1420.
20
Djelantik A. A. A. M. J. Smid G. E. Mroz A. Kleber R. J. Boelen P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: systematic review and meta regression analysis. J. Affect. Disord.265, 146–156. doi: 10.1016/j.jad.2020.01.034
21
Giunta S. Mannino G. Sideli L. Quattropani M. C. Lenzo V. (2024). Reflective functioning mediates the relationship between insecure adult attachment and the severity of prolonged grief symptoms. Health Psychol Res [Internet].12:122543. doi: 10.52965/001c.122543
22
Hayes A. F. (2022). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. 3rd Edn. New York, NY: The Guilford Press.
23
Hazan C. Shaver P. (1987). Romantic love conceptualized as an attachment process. J. Pers. Soc. Psychol.52, 511–524. doi: 10.1037/0022-3514.52.3.511
24
Kustanti C. Y. Chu H. Kang X. L. Huang T. W. Jen H. J. Liu D. et al . (2022). Prevalence of grief disorders in bereaved families of cancer patients: a meta-analysis. Palliat. Med.36, 305–318. doi: 10.1177/02692163211066747
25
Lai C. Luciani M. Galli F. Morelli E. Cappelluti R. Penco I. et al . (2015). Attachment style dimensions can affect prolonged grief risk in caregivers of terminally ill patients with cancer. Am. J. Hospice Palliative Med.32, 855–860. doi: 10.1177/1049909114547945
26
Lai C. Luciani M. Morelli E. Galli F. Cappelluti R. Penco I. et al . (2014). Predictive role of different dimensions of burden for risk of complicated grief in caregivers of terminally ill patients. Am. J. Hosp. Palliat. Med.31, 189–193. doi: 10.1177/1049909113490227
27
Lenferink L. I. M. Eisma M. C. Smid G. E. De Keijser J. Boelen P. A. (2022). Valid measurement of DSM-5 persistent complex bereavement disorder and DSM-5-TR and ICD-11 prolonged grief disorder: the traumatic grief inventory-self report plus (TGI-SR+). Compr. Psychiatry112:152281. doi: 10.1016/j.comppsych.2021.152281
28
Lenferink L. I. M. Wessel I. Boelen P. A. (2018). Exploration of the associations between responses to affective states and psychopathology in two samples of people confronted with the loss of a loved one. J. Nerv. Ment. Dis.206, 108–115. doi: 10.1097/NMD.0000000000000781
29
Lenzo V. Fontana A. Santoro G. Cuzzocrea G. Miniati V. Quattropani M. C. et al . (2025). Psychometric properties of the Italian traumatic grief inventory-self report plus (TGI-SR+). Death Stud.30, 1–9. doi: 10.1080/07481187.2025.2537978
30
Lenzo V. Sardella A. Musetti A. Petralia M. C. Grado I. Quattropani M. C. (2022). Failures in reflective functioning and reported symptoms of anxiety and depression in bereaved individuals: a study on a sample of family caregivers of palliative care patients. Int. J. Environ. Res. Public Health19:11930. doi: 10.3390/ijerph191911930
31
Leonardi M. Giovannetti A. M. Pagani M. Raggi A. Sattin D. On Behalf of the National Consortium (2012). Burden and needs of 487 caregivers of patients in vegetative state and in minimally conscious state: results from a national study. Brain Inj.26, 1201–1210. doi: 10.3109/02699052.2012.667589
32
Lundorff M. Holmgren H. Zachariae R. Farver-Vestergaard I. O’Connor M. (2017). Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J. Affect. Disord.212, 138–149. doi: 10.1016/j.jad.2017.01.030
33
Majd M. Chen M. A. Chirinos D. A. Brown R. L. LeRoy A. S. Murdock K. W. et al . (2024). Trajectories of depressive symptoms early in the course of bereavement: patterns, psychosocial factors and risk of prolonged grief. Stress. Health40:e3340. doi: 10.1002/smi.3340
34
Maunder R. G. Hunter J. J. (2001). Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosom. Med.63, 556–567. doi: 10.1097/00006842-200107000-00006
35
Mikulincer M. Florian V. Hirschberger G. (2003). The existential function of close relationships: introducing death into the science of love. Personal. Soc. Psychol. Rev.7, 20–40. doi: 10.1207/S15327957PSPR0701_2
36
Mikulincer M. Shaver P. R. (2019). Attachment orientations and emotion regulation. Curr. Opin. Psychol.25, 6–10. doi: 10.1016/j.copsyc.2018.02.006
37
Mikulincer M. Shaver P. R. (2022). An attachment perspective on loss and grief. Curr. Opin. Psychol.45:101283. doi: 10.1016/j.copsyc.2021.11.003
38
Miller L. M. Utz R. L. Supiano K. Lund D. Caserta M. S. (2020). Health profiles of spouse caregivers: the role of active coping and the risk for developing prolonged grief symptoms. Soc. Sci. Med.266:113455. doi: 10.1016/j.socscimed.2020.113455
39
Milman E. Neimeyer R. A. Fitzpatrick M. MacKinnon C. J. Muis K. R. Cohen S. R. (2019). Rumination moderates the role of meaning in the development of prolonged grief symptomatology. J. Clin. Psychol.75, 1047–1065. doi: 10.1002/jclp.22751
40
Miyabayashi S. Yasuda J. (2007). Effects of loss from suicide, accidents, acute illness and chronic illness on bereaved spouses and parents in Japan: their general health, depressive mood, and grief reaction. Psychiatry Clin. Neurosci.61, 502–508. doi: 10.1111/j.1440-1819.2007.01699.x
41
Musetti A. Franceschini C. Quattropani M. C. Prigerson H. G. Lenzo V. (2025). Prevalence and correlates of prolonged grief disorder symptom severity in a large sample of Italian adults. BJPsych Open.11:e162. doi: 10.1192/bjo.2025.10763
42
Nielsen M. K. Neergaard M. A. Jensen A. B. Bro F. Guldin M. B. (2016). Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin. Psychol. Rev.44, 75–93. doi: 10.1016/j.cpr.2016.01.002
43
Panksepp J. (1998). Affective neuroscience: the foundations of human and animal emotions. Oxford: Oxford University Press.
44
Pohlkamp L. Kreicbergs U. Sveen J. (2019). Bereaved mothers’ and fathers’ prolonged grief and psychological health 1 to 5 years after loss — a nationwide study. Psychooncology28, 1530–1536. doi: 10.1002/pon.5112
45
Porges S. W. (2001). The polyvagal theory: phylogenetic substrates of a social nervous system. Int. J. Psychophysiol.42, 123–146. doi: 10.1016/S0167-8760(01)00162-3
46
Preacher K. J. Hayes A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput.36, 717–731. doi: 10.3758/BF03206553
47
Rogalla K. B. (2020). Anticipatory grief, proactive coping, social support, and growth: exploring positive experiences of preparing for loss. Omega81, 107–129. doi: 10.1177/0030222818761461
48
Rosner R. Comtesse H. Vogel A. Doering B. K. (2021). Prevalence of prolonged grief disorder. J. Affect. Disord.287, 301–307. doi: 10.1016/j.jad.2021.03.058
49
Sardella A. Musetti A. Caponnetto P. Quattropani M. C. Lenzo V. (2023). Prolonged grief disorder and symptoms of anxiety and depression among bereaved family caregivers in the context of palliative home care. Eur. J. Investig. Health Psychol. Educ.13, 490–500. doi: 10.3390/ejihpe13020037
50
Schimmenti A. (2017). Psychosomatics between attachment trauma and affective neuroscience. The psychosomatic dysregulation inventory (PDI): development and preliminary data. Mediterr. J. Clin. Psychol.5, 179–180.
51
Schimmenti A. Caretti V. (2018). “Attachment, trauma, and alexithymia” in Alexithymia [internet]. eds. LuminetO.BagbyR. M.TaylorG. J.. 1st ed (Cambridge: Cambridge University Press), 127–141.
52
Schulz R. Boerner K. Shear K. Zhang S. Gitlin L. N. (2006). Predictors of complicated grief among dementia caregivers: a prospective study of bereavement. Am. J. Geriatr. Psychiatry14, 650–658. doi: 10.1097/01.JGP.0000203178.44894.db
53
Schwartz L. E. Howell K. H. Jamison L. E. (2018). Effect of time since loss on grief, resilience, and depression among bereaved emerging adults. Death Stud.42, 537–547. doi: 10.1080/07481187.2018.1430082
54
Shevlin M. Redican E. Hyland P. Murphy J. Karatzias T. McBride O. et al . (2023). Symptoms and levels of ICD-11 prolonged grief disorder in a representative community sample of UK adults. Soc. Psychiatry Psychiatr. Epidemiol.58, 1535–1547. doi: 10.1007/s00127-023-02469-1
55
Sideli L. Schimmenti A. Lenzo V. Miniati V. Cuzzocrea G. Santoro G. et al Italian translation of the Traumatic Grief Inventory-Self Report Plus (TGI-SR+) [Internet]. (2022). Available online at: https://osf.io/rqn5k/ (Accessed August 27, 2025).
56
Srivastava T. Lee K. Ehrenkranz R. Cozzolino P. J. Wise F. A. Burns M. et al . (2025). The efficacy of psychotherapeutic interventions for prolonged grief disorder: a systematic review. J. Affect. Disord.380, 561–575. doi: 10.1016/j.jad.2025.03.173
57
Treml J. Brähler E. Kersting A. (2022). Prevalence, factor structure and correlates of DSM-5-TR criteria for prolonged grief disorder. Front. Psych.13:880380. doi: 10.3389/fpsyt.2022.880380
58
World Health Organization (2018). International statistical classification of diseases and related health problems. 11th Edn. Geneva: World Health Organization.
59
Xu W. Fu Z. He L. Schoebi D. Wang J. (2015). Growing in times of grief: attachment modulates bereaved adults’ posttraumatic growth after losing a family member to cancer. Psychiatry Res.230, 108–115. doi: 10.1016/j.psychres.2015.08.035
60
Yuan M. D. Liu J. F. Zhong B. L. (2024). Prevalence of prolonged grief disorder and its symptoms among bereaved individuals in China: a systematic review and meta-analysis. Gen. Psychiatry37:e101216. doi: 10.1136/gpsych-2023-101216
61
Zordan R. D. Bell M. L. Price M. Remedios C. Lobb E. Hall C. et al . (2019). Long-term prevalence and predictors of prolonged grief disorder amongst bereaved cancer caregivers: a cohort study. Palliat. Support. Care17, 507–514. doi: 10.1017/S1478951518001013
Summary
Keywords
prolonged grief disorder, attachment, psychosomatic dysregulation, cancer, mediation analysis, oncology, trauma
Citation
Lenzo V, Triscari S, Quattropani MC, Bordino V, Cibelli F, Lombardo L, Caretti V, Schimmenti A and Sideli L (2025) When the body speaks of loss: psychosomatic dysregulation as a mediator between insecure attachment and prolonged grief symptoms in oncological and traumatic bereavement. Front. Psychol. 16:1708285. doi: 10.3389/fpsyg.2025.1708285
Received
18 September 2025
Accepted
24 October 2025
Published
13 November 2025
Volume
16 - 2025
Edited by
Pamela Bryden, Wilfrid Laurier University, Canada
Reviewed by
Antonella Granieri, University of Turin, Italy
Dario Alparone, Université de Bretagne Occidentale, France
Updates
Copyright
© 2025 Lenzo, Triscari, Quattropani, Bordino, Cibelli, Lombardo, Caretti, Schimmenti and Sideli.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vittorio Lenzo, vittorio.lenzo@unict.it
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.