- 1Moral and Psychological Education Research Center, Zhejiang University of Finance and Economics, Hangzhou, China
- 2Department of Early Childhood Education, Faculty of Education, Shenzhen Polytechnic University, Shenzhen, China
- 3College of Education, Wenzhou University, Wenzhou, China
- 4School of Public Basic Studies, Wenzhou Polytechnic, Wenzhou, China
by Zhou, H., Liu, X., Wu, J., Liao, C., and Zhao, S. (2025). Front. Psychol. 16:1651664. doi: 10.3389/fpsyg.2025.1651664
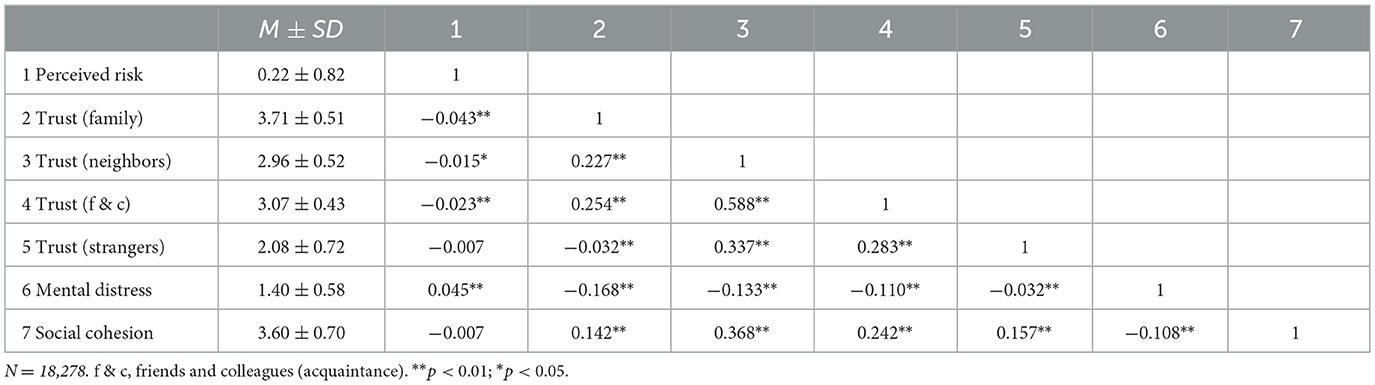
There was a mistake in Table 2 as published. The column headings were missing; variables “trust (neighbors)” and “trust (f & c)” were misplaced. The corrected Table 2 appears below.
A correction has been made to section 3 Results, 3.2 Preliminary analysis, Paragraph 2. The descriptive text introducing Table 2 has been adjusted so that “trust (neighbors)” and “trust (f & c)” now appear in their correct locations:
“The correlation matrix (zero-order Pearson's correlation coefficients) is shown in Table 2. As expected, perceived pandemic risk is significantly positively correlated with mental distress (r = 0.045, p < 0.01). It is also significantly negatively correlated with family trust (r = −0.043, p < 0.01), neighbor trust (r = −0.015, p < 0.05), and acquaintance trust (r = −0.023, p < 0.01), while the negative correlation with stranger trust (r = 0.007, p > 0.05) is not significant. Additionally, family trust (r = −0.168, p < 0.01), neighbor trust (r = −0.133, p < 0.01), acquaintance trust (r = −0.110, p < 0.01), and stranger trust (r = 0.032, p < 0.01) are all significantly negatively correlated with mental distress. Furthermore, social cohesion is not significantly negatively correlated with perceived pandemic risk (r = −0.007, p > 0.05) but is significantly negatively correlated with mental distress (r = −0.108, p < 0.01). It is also significantly positively correlated with family trust (r = 0.142, p < 0.01), neighbor trust (r = 0.368, p < 0.01), acquaintance trust (r = 0.242, p < 0.01), and stranger trust (r = 0.157, p < 0.01).”
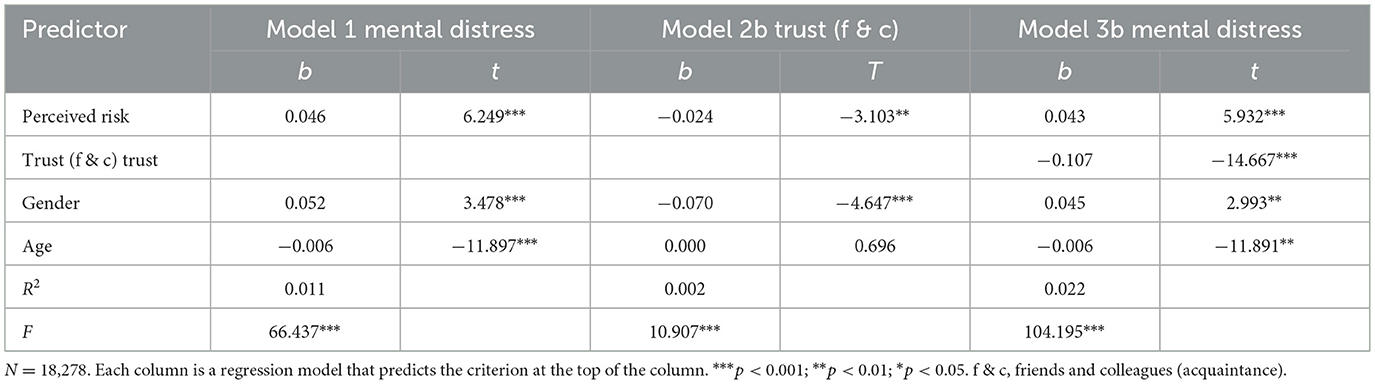
There was a mistake in Table 4 and its caption as published. The predictor labels have been realigned; Table 4 now contains “Trust (f & c)” as the mediator variable throughout all models.
The corrected Table 4 and its caption appear below.
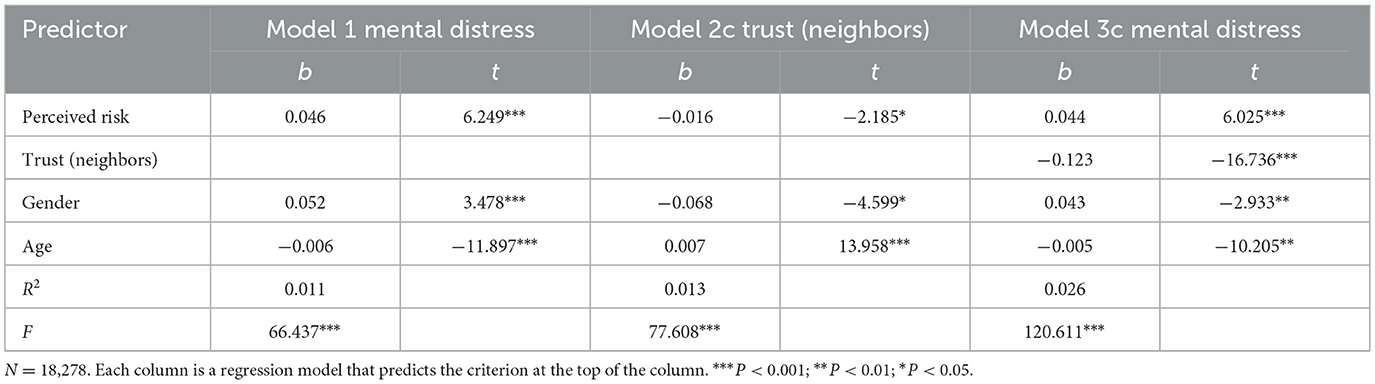
There was a mistake in Table 5 and its caption as published. The predictor labels have been realigned; Table 5 now contains “Trust (f & c)” as the mediator variable throughout all models.
The corrected Table 5 and its caption appear below.
The original version of this article has been updated.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: COVID-19 pandemic, perceived risk, interpersonal trust, social cohesion, mental distress
Citation: Zhou H, Liu X, Wu J, Liao C and Zhao S (2025) Correction: The perceived COVID-19 pandemic risk and mental distress in China: the mediating role of interpersonal trust and the moderating role of social cohesion. Front. Psychol. 16:1714759. doi: 10.3389/fpsyg.2025.1714759
Received: 28 September 2025; Accepted: 30 October 2025;
Published: 12 November 2025.
Edited and reviewed by: Gerald Matthews, George Mason University, United States
Copyright © 2025 Zhou, Liu, Wu, Liao and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanjing Liao, Y2psaWFvQHd6dS5lZHUuY24=; Shengyu Zhao, MjAwNjE1MDAwN0B3enB0LmVkdS5jbg==
 Hao Zhou
Hao Zhou Xiangqian Liu1
Xiangqian Liu1 Jing Wu
Jing Wu Chuanjing Liao
Chuanjing Liao Shengyu Zhao
Shengyu Zhao