Abstract
Background:
The 2023 Kahramanmaraş earthquakes were among the most devastating disasters in modern Türkiye, with severe consequences for survivors’ mental health. While post-disaster psychopathology has been widely studied, less is known about positive psychological outcomes such as resilience and well-being in this context.
Objective:
This study examined levels of depression, anxiety, post-traumatic stress symptoms, well-being, and resilience among earthquake survivors, explored group differences, and identified predictors of key psychological outcomes.
Methods:
A cross-sectional survey was conducted with 642 adult survivors across 11 heavily affected cities, nearly 2 years after the earthquakes. Data were collected between September 2024 and January 2025, corresponding to 19–22 months after the earthquakes. Participants completed validated self-report measures: BDI-II, BAI, PCL-5, WEMWBS, and CD-RISC. Analyses included group comparisons, correlations, hierarchical regressions predicting well-being and resilience, and logistic regression predicting probable PTSD (PCL-5 ≥ 47).
Results:
Survivors reported moderate depression (M = 22.1), mild–moderate anxiety (M = 19.4), and near-threshold PTSD symptoms (M = 40.0). Overall, 31.0% of participants exceeded the PCL-5 cut-off for probable PTSD (95% CI: 27.4–34.8%). Well-being (M = 35.6) and resilience (M = 56.0) were below normative values. Women reported higher depression than men, while trauma-exposed participants had significantly worse outcomes across all measures. Bivariate correlations showed strong associations between distress, reduced well-being, and diminished resilience. Hierarchical regressions indicated that depression and PTSD symptoms were the primary predictors of both lower well-being (R2 = 0.45) and resilience (R2 = 0.32). Logistic regression revealed that female gender (OR = 1.80, p = 0.024) and depression severity (OR = 1.10, p = 0.001) significantly increased the likelihood of probable PTSD.
Conclusion:
Nearly 2 years after the earthquakes, survivors experienced substantial psychological distress alongside reduced well-being and resilience. Clinical symptoms, particularly depression and PTSD, more strongly associated with outcomes than sociodemographic or exposure variables. These findings highlight the need for interventions that both alleviate trauma-related psychopathology and strengthen resilience and well-being as part of long-term disaster recovery.
Introduction
The twin earthquakes that struck southeastern Türkiye on 6 February 2023 represent one of the most devastating natural disasters in recent history, causing extensive destruction across 11 provinces. With moment magnitudes of 7.7 and 7.6, the events leveled large sections of urban areas in Kahramanmaraş, Hatay, Gaziantep, Adıyaman, Malatya, and surrounding regions, resulting in more than 50,000 fatalities and the displacement of millions of residents (Şenol Balaban et al., 2025). Beyond the severe physical damage, disasters of this scale are consistently associated with heightened risks for a broad range of psychological difficulties (Heanoy and Brown, 2024; Şam et al., 2025; Satıcı et al., 2024; Balbay et al., 2024), particularly post-traumatic stress disorder (PTSD) (Sirotich and Camisasca, 2024), depression, and anxiety (Güler et al., 2024) among survivors. Epidemiological evidence indicates that nearly one-third of disaster-exposed individuals may experience clinically significant psychopathology—such as PTSD, depressive disorders, or anxiety disorders—during the post-disaster period (Fong et al., 2022; Hosseinnejad et al., 2022; Tahernejad et al., 2023). Earthquakes, due to their sudden onset and life-threatening nature, appear to be especially potent in this regard: a meta-analysis of 46 studies reported that approximately 23–30% of earthquake survivors meet criteria for PTSD within the first post-disaster year, with even higher rates observed in severely affected communities (Dai et al., 2016).
Research on previous large-scale earthquakes consistently identifies several groups and characteristics associated with heightened psychological vulnerability. Women, for example, frequently report higher levels of post-disaster psychological morbidity than men, a pattern that has been documented across diverse cultural and disaster contexts (McKinzie and Clay-Warner, 2021). Elevated trauma exposure—such as being trapped under collapsed structures, sustaining physical injuries, losing close relatives, or witnessing severe destruction—is also strongly associated with greater post-disaster mental health difficulties (Schwind et al., 2019). Socioeconomic and demographic factors, including low income, limited educational attainment, and in some studies older age, further correspond to increased risk for PTSD and depression (Mao and Agyapong, 2021; Çınaroğlu et al., 2025),. While the earlier study in which I contributed as a second author examined the psychological effects of the 2023 earthquakes among indirectly exposed non-victims, the present investigation is distinct in directly assessing survivors residing in 11 severely affected cities nearly 2 years after the disaster. Conversely, robust social support and adaptive coping capacities appear to buffer individuals against persistent trauma-related symptoms (Can Gür, 2024). Collectively, these observations are consistent with the broader disaster mental health literature, which highlights a dose–response pattern between trauma severity and psychological distress and underscores the protective role of psychosocial resources in fostering resilience.
The 2023 Kahramanmaraş earthquakes provide a critical context for examining the psychological consequences of large-scale natural disasters. Given the unprecedented magnitude of this event in modern Türkiye, there remains an urgent need to document its mental-health impact and to identify factors that may mitigate or exacerbate survivors’ psychological outcomes. Early reports have already indicated widespread distress among affected populations (Çınaroğlu et al., 2025), including previous work in which I contributed as a second author. That prior study synthesized existing evidence through a systematic review and meta-analysis, whereas the present investigation contributes original, large-scale primary data collected directly from survivors nearly 2 years after the disaster. Empirical findings from the region support the severity of the psychosocial burden: for example, a cross-sectional survey conducted in a severely affected district (Nurdağı, Gaziantep) found that more than 51% of adult survivors screened positive for psychological distress in the months following the earthquakes, with particularly elevated risk among women, injured individuals, and those who had lost first-degree relatives (Tomak et al., 2024). Additional early assessments from the affected provinces similarly reported high rates of probable PTSD, with some estimates suggesting that over half of adult survivors met screening thresholds within the first post-disaster year (Yakşi and Eroğlu, 2024; Taşkın et al., 2025; Tanrikulu and Kayaoglu, 2024). Key earthquake-related stressors—such as persistent aftershock anxiety, bereavement, extensive property destruction, and the loss of one’s broader community environment—have been identified as major contributors to these psychological reactions. While these findings underscore the profound and widespread mental health burden created by the 2023 earthquakes, they also highlight the heterogeneity of survivors’ experiences; not all individuals are affected to the same degree. Identifying the predictors of heightened vulnerability, and understanding the mechanisms through which risk accumulates, is therefore essential for developing targeted and effective post-disaster interventions (Ural et al., 2024).
Beyond the prevention and treatment of psychiatric disorders, there is increasing recognition of the importance of examining positive mental health constructs in disaster research. Traditional post-disaster studies have largely emphasized trauma-related symptoms—such as PTSD, depression, and anxiety—while comparatively underrepresenting survivors’ resilience and overall well-being. Yet resilience, broadly conceptualized as the capacity to adapt, recover, or grow in the face of adversity, is now understood to be a critical component of post-disaster adjustment (Oliva and Lazzeretti, 2019; Zhao et al., 2020). Higher levels of psychological resilience have been associated with reduced likelihood of developing PTSD and other mental health difficulties following traumatic events (Snijders et al., 2018). Empirical evidence from prior earthquake contexts similarly indicates that individuals possessing stronger resilience resources—such as effective coping strategies, robust social support, and dispositional optimism—tend to report fewer PTSD symptoms and demonstrate more rapid psychological recovery (Xi et al., 2020; Chen et al., 2022; Ikizer et al., 2016).
In recent years, theoretical models in mental health have emphasized the importance of evaluating both negative and positive indicators of psychological functioning following major traumatic events. The dual-continuum model of mental health posits that psychological distress (e.g., PTSD, depression, anxiety) and psychological well-being operate on related but distinct continua; thus, the presence of distress does not automatically preclude well-being, and improvements in one domain do not necessarily guarantee changes in the other. Complementing this view, contemporary resilience theory conceptualizes resilience as a dynamic system of psychological and social resources—such as coping self-efficacy, emotional regulation, and meaning-making—that buffer the adverse effects of trauma exposure and support adaptive functioning over time. From a broader ecological perspective, disaster mental health frameworks (e.g., Norris et al., 2008) propose that post-disaster adjustment reflects an interplay between risk factors (e.g., trauma severity, bereavement, demographic vulnerabilities) and protective resources (e.g., resilience, coping capacities, social support), with both losses and gains in these resources shaping survivors’ psychological trajectories. Together, these theoretical perspectives provide the conceptual foundation for the present study by framing psychological distress, resilience, and well-being as interconnected yet distinct components of post-disaster functioning, and by highlighting the importance of assessing them simultaneously to capture the full psychological impact of the 2023 Kahramanmaraş earthquakes.
In parallel, mental well-being—encompassing domains such as life satisfaction, positive affect, and a sense of meaning or quality of life—represents an important outcome in its own right (Arguvanlı Çoban and Gün Koşar, 2025). Disasters can significantly erode subjective well-being; declines in life satisfaction and overall quality of life have been documented across multiple earthquake-affected populations. Following the 2023 Kahramanmaraş earthquakes, many survivors continue to report diminished well-being nearly 2 years after the event, particularly in emotional and social domains, with women and older adults often exhibiting greater vulnerability (Samanci Tekin and Aydin, 2024; Yanardağ et al., 2025),. Evaluating well-being alongside psychological distress therefore provides a more holistic understanding of the disaster’s impact and aligns with the World Health Organization’s definition of mental health as encompassing not merely the absence of illness but also the presence of positive psychological functioning (World Health Organization, 2022).
A growing body of disaster mental-health research emphasizes that psychological distress, resilience, and well-being form an interconnected system that jointly shapes survivors’ post-traumatic adjustment. Psychological distress—including PTSD symptoms, depression, and anxiety—reflects the emotional and physiological burden imposed by traumatic exposure, and elevated levels of distress are consistently linked to impaired functioning, reduced life satisfaction, and greater vulnerability to chronic psychopathology. In contrast, resilience represents a constellation of adaptive psychological resources, such as effective coping strategies, emotional regulation, optimism, and perceived competence, that enable individuals to withstand or recover from adversity. Resilience is understood not merely as the absence of distress but as an active, dynamic process that can buffer survivors against the negative consequences of trauma. Well-being, encompassing positive affect, life satisfaction, and psychological vitality, constitutes another distinct dimension of mental health: according to the dual-continuum model, well-being can vary independently of symptom severity and offers a broader lens through which to understand survivors’ functioning in the aftermath of disaster. Empirical studies have repeatedly shown that individuals with higher resilience tend to report lower levels of PTSD, depression, and anxiety, while simultaneously exhibiting greater well-being. Conversely, elevated distress is associated with both diminished resilience and lower subjective well-being, suggesting that distress can erode the psychological resources necessary for positive adaptation. Taken together, this literature highlights the importance of examining distress, resilience, and well-being not as isolated constructs but as mutually influencing dimensions of post-disaster mental health—an approach that is particularly relevant in large-scale traumatic events such as the 2023 Kahramanmaraş earthquakes.
Building on this background, the present study was designed to address these knowledge gaps through a systematic evaluation of earthquake-related psychological outcomes nearly 2 years after the 2023 Kahramanmaraş disaster. The study pursued three primary objectives: (1) to quantify levels of psychological distress—including PTSD symptoms, anxiety, and depression—as well as positive mental health indicators such as well-being and resilience among adult survivors; (2) to examine subgroup differences in these outcomes based on demographic characteristics and degree of trauma exposure; and (3) to identify variables associated with key psychological indicators, particularly PTSD symptom severity, overall mental well-being, and resilience.
By delineating these patterns, the study aims to support the development of targeted mental health interventions and to enhance understanding of the psychological processes that influence adaptation in the aftermath of a large-scale disaster. More broadly, the findings seek to address a significant gap in the current literature by situating the psychological impact of the 2023 earthquakes within a comprehensive framework that emphasizes not only the mitigation of trauma-related symptoms but also the promotion of resilience and well-being as integral components of long-term recovery.
Study design
This study employed a multi-center, cross-sectional analytic design to investigate the psychological consequences of the 2023 Kahramanmaraş earthquakes. Data were collected from 11 severely affected cities in Türkiye, yielding a final sample of 642 adults. The research aimed to comprehensively assess depressive symptoms, anxiety, post-traumatic stress symptoms, mental well-being, and resilience among survivors, and to examine these outcomes in relation to a wide range of sociodemographic and earthquake-related variables. In addition to descriptive and comparative analyses, correlational tests were conducted to evaluate associations among psychological constructs, and multivariate models were used to identify variables linked with resilience, well-being, and probable PTSD caseness. Data collection followed a standardized protocol across all sites. Participants completed a Sociodemographic Information Form and a battery of validated self-report instruments, including the Beck Depression Inventory-II (BDI-II), Beck Anxiety Inventory (BAI), PTSD Checklist for DSM-5 (PCL-5), Warwick–Edinburgh Mental Well-Being Scale (WEMWBS), and Connor–Davidson Resilience Scale (CD-RISC). The study was designed and reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional research.
Setting and participants
Data collection was conducted across 11 severely impacted cities over a three-month period between September 2024 and January 2025, corresponding to approximately 19–22 months after the earthquakes. This timing was intentionally selected to capture not only the acute psychological responses to the disaster but also the persistence of distress and resilience nearly 2 years post-event, thereby providing insight into longer-term patterns of adjustment. The affected cities varied considerably in the extent of destruction, displacement, and availability of recovery resources; however, clustering by city was not modeled, an issue later acknowledged as a limitation.
The research team consisted of the principal investigator and four master’s-level clinical psychology students, all residing in the affected regions and familiar with the local context. The author additionally visited field sites to supervise procedures and support standardized data collection. Participants were recruited through a multi-modal convenience sampling strategy, including direct outreach in temporary shelters, community centers, and local organizations, as well as recruitment via personal networks, WhatsApp groups, social media platforms, and community contacts. This approach enabled inclusion of both displaced individuals and residents living in the broader community.
A total of 753 individuals were initially approached. After applying eligibility criteria and excluding incomplete or invalid responses, the final analytic sample consisted of 642 adults. Inclusion criteria required participants to be at least 18 years old, to have resided in one of the earthquake-affected cities at the time of the disaster, and to be free of current psychiatric diagnoses, psychiatric medication use, or ongoing psychotherapy. These criteria were implemented to estimate symptom levels among survivors not currently receiving mental health treatment; however, this approach likely underestimates the broader post-disaster psychological burden and is addressed in the Limitations section. Individuals with cognitive impairments or other conditions impairing questionnaire completion were also excluded.
Measures
Sociodemographic information form
Sociodemographic data were collected using a structured form that included age, gender, education level, marital status, employment status, household income, and earthquake-related experiences. Earthquake exposure was assessed through a set of dichotomous indicators capturing whether participants had lost family members, sustained injuries, or experienced displacement as a direct result of the disaster. The study did not incorporate a graded or standardized exposure-severity index capable of quantifying the extent of financial loss, degree of property damage, duration of displacement, or other humanitarian and social consequences. Accordingly, exposure was operationalized in a broad binary format (direct loss vs. no major loss), which supports subgroup comparisons but does not capture the full variability or multidimensional nature of earthquake-related adversity.
Beck Depression Inventory-II (BDI-II)
Depressive symptoms were assessed using the Beck Depression Inventory–II (BDI-II), a widely utilized self-report instrument developed as a revision of the original Beck Depression Inventory (Beck et al., 1996). The BDI-II consists of 21 items aligned with DSM-IV diagnostic criteria for depressive disorders, with each item rated on a 4-point scale (0–3), yielding total scores ranging from 0 to 63. Factor-analytic research generally supports a two-factor structure encompassing cognitive–affective and somatic–performance components. The Turkish adaptation of the instrument was validated by Kapci et al. (2008) in a sample comprising 362 nonclinical adults and 176 clinical outpatients diagnosed with depressive disorders. The scale demonstrated excellent internal consistency (Cronbach’s α = 0.90 in the nonclinical group and 0.89 in the clinical group), high test–retest reliability (r = 0.94), and strong convergent and discriminant validity. Cut-off scores established for the Turkish population are consistent with the original version: 0–12 indicates minimal depressive symptoms, 13–18 mild, 19–28 moderate, and 29–63 severe depression.
Beck Anxiety Inventory (BAI)
Anxiety symptoms were measured using the Beck Anxiety Inventory (BAI), a 21-item self-report instrument developed by Beck et al. (1993) to assess the severity of anxiety experienced during the preceding week. Each item is scored on a 4-point Likert scale ranging from 0 (“not at all”) to 3 (“severely”), yielding total scores between 0 and 63. Factor-analytic studies typically identify two principal dimensions: somatic anxiety and subjective anxiety. The Turkish adaptation of the BAI was validated by Ulusoy et al. (1998) in clinical and nonclinical samples, demonstrating excellent internal consistency (Cronbach’s α = 0.93), acceptable test–retest reliability (r = 0.75), and moderate correlations with depressive symptom measures, supporting discriminant validity. Exploratory factor analysis confirmed the two-factor structure, and the scale has been shown to effectively distinguish individuals with clinically significant anxiety from other diagnostic groups.
PTSD Checklist for DSM-5 (PCL-5)
Post-traumatic stress symptoms were assessed using the PTSD Checklist for DSM-5 (PCL-5), a 20-item self-report instrument developed by Weathers et al. (2018) in accordance with the DSM-5 diagnostic framework. Items correspond to the four core PTSD symptom clusters—re-experiencing, avoidance, negative alterations in cognition and mood, and hyperarousal—and are rated on a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”), producing total scores between 0 and 80. The Turkish validation of the PCL-5 was conducted by Boysan et al. (2017) in a mixed sample of psychiatric outpatients and community participants. The scale demonstrated excellent internal consistency (α = 0.94 for the total score), with subscale reliabilities ranging from 0.78 to 0.87, and test–retest reliability coefficients between 0.64 and 0.78 over a two-week interval. Convergent validity was supported through strong correlations with measures of trauma-related symptoms, depression, and anxiety. For Turkish populations, a cut-off score of 47 has been recommended for identifying probable PTSD, yielding a sensitivity of 0.76 and a specificity of 0.69.
Warwick-Edinburgh Mental Well-Being Scale (WEMWBS)
Mental well-being was measured using the Warwick–Edinburgh Mental Well-Being Scale (WEMWBS), originally developed by Tennant et al. (2007) to assess hedonic and eudaimonic components of positive mental health. The instrument comprises 14 positively worded items rated on a 5-point Likert scale (1 = “none of the time” to 5 = “all of the time”), producing total scores ranging from 14 to 70, with higher scores reflecting greater well-being. The Turkish adaptation of the WEMWBS was validated by Keldal (2015) in a sample of 371 adults aged 16 to 70. Consistent with the original version, factor-analytic findings supported a unidimensional structure, accounting for 51% of the variance. The scale demonstrated excellent internal consistency (Cronbach’s α = 0.92) and strong test–retest reliability over a one-week interval (r = 0.83). Criterion validity was evidenced through significant correlations with measures of subjective well-being, life satisfaction, and happiness, supporting its use as a reliable and valid indicator of psychological well-being in Turkish populations.
Connor-Davidson Resilience Scale (CD-RISC)
Resilience was assessed using the Connor–Davidson Resilience Scale (CD-RISC), a 25-item self-report instrument developed by Connor and Davidson (2003) to evaluate individuals’ capacity to cope with and adapt to adversity. Items are rated on a 5-point scale ranging from 0 (“not true at all”) to 4 (“true nearly all the time”), yielding total scores between 0 and 100. The original validation supported a five-factor structure encompassing personal competence, trust in one’s instincts, positive acceptance of change, sense of control, and spiritual influences. The Turkish validation of the CD-RISC was conducted by Karaırmak (2010) in a sample of 246 earthquake survivors. Exploratory and confirmatory factor analyses supported a three-factor model—tenacity and personal competence, tolerance of negative affect, and tendency toward spirituality—explaining 52% of the total variance. The scale demonstrated excellent internal consistency (Cronbach’s α = 0.92), with subscale reliabilities ranging from 0.79 to 0.93. Strong correlations with measures of self-esteem, hope, optimism, and affect further supported its construct validity within Turkish populations.
Power analysis and sample size determination
A priori power analyses were conducted using G*Power 3.1 to determine the minimum sample size required for the planned statistical procedures. All calculations were based on two-tailed tests with an alpha level of 0.05 and desired statistical power of 1–β = 0.90. For independent-samples t tests, detecting a small-to-moderate effect size (Cohen’s d = 0.25) requires a total sample of approximately 500 participants under balanced group conditions. For one-way ANOVA designs with typical sociodemographic groupings (approximately four groups), identifying a small effect (f = 0.15) necessitates roughly 550 participants. For bivariate correlations, a small association (r = 0.15) similarly requires an estimated sample of 575 individuals. Multiple linear regression models with up to ten predictors require approximately 550–600 participants to detect a small-to-moderate effect increment (f2 = 0.03). The final sample size of N = 642 therefore met or exceeded all a priori estimates, ensuring ≥ 0.90 statistical power across the primary analyses involving depression, anxiety, PTSD symptoms, mental well-being, and resilience.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics (version 30). Prior to analysis, the dataset was screened for accuracy, missing values, and adherence to distributional assumptions. Descriptive statistics were used to summarize sociodemographic characteristics and psychological outcome variables. Group differences were examined using independent-samples t tests or one-way ANOVAs, with non-parametric alternatives applied when normality or homogeneity assumptions were violated. Bonferroni adjustments were used for post hoc comparisons, and chi-square tests were employed for analyses involving categorical variables. Effect sizes for all group comparisons (Cohen’s d for t tests and partial η2 for ANOVAs), along with 95% confidence intervals, are reported in the comparative tables to aid interpretation and account for family-wise error across multiple tests.
Associations among continuous variables were evaluated using Pearson correlation coefficients. Hierarchical multiple regression analyses were conducted to identify variables associated with mental well-being and resilience, while logistic regression was used to estimate the odds of meeting the threshold for probable PTSD (PCL-5 ≥ 47). All statistical tests were two-tailed with an alpha level of 0.05, and standardized effect size estimates (Cohen’s d, partial η2, odds ratios, standardized β coefficients) were reported.
Multicollinearity diagnostics were conducted before running the regression models. Variance inflation factors for depression, anxiety, and PTSD symptoms were all below 2.5, and tolerance values exceeded 0.40, indicating no problematic multicollinearity. Sensitivity analyses in which distress variables were entered separately produced comparable patterns of significance, further supporting the stability and robustness of the regression results.
Missing data were minimal (<3% per variable) and were handled using listwise deletion, resulting in complete-case analyses for all multivariate models. Consequently, sample sizes vary slightly across models depending on the availability of complete data for included predictors. Both R2 and adjusted R2 values are reported to provide more accurate estimates of explained variance.
To enhance methodological transparency and align the manuscript with reporting standards for observational research, a STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist and a participant-flow diagram summarizing recruitment, exclusions, and final sample size have been included in the Supplementary Table S5.
Results
Sample characteristics
The final sample comprised 642 adults residing in 11 cities affected by the 2023 Kahramanmaraş earthquakes. Participants ranged in age from 19 to 58 years (M = 35.4, SD = 10.8). Of the total sample, 346 individuals (53.9%) were female. Educational attainment varied, with 160 participants (24.9%) reporting primary education or below, 219 (34.1%) having completed high school, and 263 (41.0%) holding a university degree. Regarding marital status, 342 participants (53.3%) were married, 235 (36.6%) were single, and 65 (10.1%) were divorced. At the time of data collection, 418 participants (65.1%) were employed and 224 (34.9%) were unemployed. In terms of earthquake-related exposure, 371 participants (57.8%) reported experiencing direct losses or displacement, whereas 271 (42.2%) reported no major losses associated with the disaster.
Psychological measures
Participants reported elevated levels of psychological distress across all standardized instruments. The mean BDI-II score was 22.1 (SD = 10.5), indicating moderate depressive symptomatology. Anxiety levels were similarly elevated, with a mean BAI score of 19.4 (SD = 9.2), corresponding to the mild-to-moderate range. PTSD symptoms were also substantial; the mean PCL-5 score of 40.0 (SD = 15.3) approached the recommended cutoff for probable PTSD.
In contrast, indicators of positive psychological functioning were notably lower than normative expectations. The mean WEMWBS score of 35.6 (SD = 9.7) was substantially below established population norms, which typically fall within the 47–50 range in the original UK validation and approximately 48.1 in the Turkish validation. This reflects an 11–14-point decrement relative to expected levels of well-being. Similarly, resilience scores were reduced: the mean CD-RISC score of 56.0 (SD = 14.2) fell below normative international values (70–82) as well as below Turkish norms for earthquake-exposed adults (62–65). Thus, the sample demonstrated diminished resilience alongside elevated distress nearly 2 years after the disaster.
All instruments exhibited excellent internal consistency in the current sample (Cronbach’s α = 0.90–0.94), aligning with reliability estimates reported in prior Turkish validation studies. Descriptive statistics and internal consistency coefficients for each measure are presented in Table 1.
Table 1
| Measure | Possible range | M (SD) | Cronbach’s α |
|---|---|---|---|
| Beck Depression Inventory–II (BDI-II) | 0–63 | 22.1 (10.5) | 0.90 |
| Beck Anxiety Inventory (BAI) | 0–63 | 19.4 (9.2) | 0.93 |
| PTSD Checklist – DSM-5 (PCL-5) | 0–80 | 40.0 (15.3) | 0.94 |
| Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) | 14–70 | 35.6 (9.7) | 0.92 |
| Connor-Davidson Resilience Scale (CD-RISC) | 0–100 | 56.0 (14.2) | 0.92 |
Descriptive statistics and reliability of psychological measures (N = 642).
Group differences in psychological outcomes
Group comparisons across gender, marital status, education level, employment status, and trauma exposure are summarized in Table 2. Women reported significantly higher depressive symptoms than men (p = 0.032, d = 0.40), whereas no gender-based differences emerged for anxiety, PTSD symptoms, well-being, or resilience. Marital status was associated with anxiety levels, with single participants exhibiting higher anxiety scores than married individuals (p = 0.033); no additional marital-status differences were observed across the other outcomes.
Table 2
| Outcome | Gender (M vs. F) | Marital (Single vs. Married) | Trauma (No vs. Yes) |
|---|---|---|---|
| BDI-II | 20.5 (11.0) vs. 23.7 (9.8), p = 0.032* | 23.6 (9.9) vs. 21.1 (10.9), p = 0.144 | 19.1 (10.5) vs. 24.1 (10.1), p = 0.001** |
| BAI | 18.4 (9.9) vs. 20.5 (8.3), p = 0.117 | 21.6 (8.9) vs. 18.4 (9.4), p = 0.033* | 17.9 (9.6) vs. 20.5 (8.8), p = 0.046* |
| PCL-5 | 39.0 (15.5) vs. 41.0 (15.1), p = 0.376 | 43.4 (16.1) vs. 39.5 (14.9), p = 0.123 | 36.5 (15.4) vs. 42.3 (14.8), p = 0.009** |
| WEMWBS | 36.4 (9.3) vs. 34.8 (10.0), p = 0.240 | 34.0 (10.7) vs. 36.2 (9.3), p = 0.164 | 37.4 (10.2) vs. 34.3 (9.1), p = 0.025* |
| CD-RISC | 55.0 (14.4) vs. 57.0 (14.0), p = 0.318 | 55.0 (15.1) vs. 55.6 (14.0), p = 0.791 | 59.7 (15.0) vs. 53.5 (13.2), p = 0.002** |
Group comparisons of psychological outcomes by gender, marital status, and trauma exposure.
*, **indicates statistical significance at the p < 0.05 and p < 0.01 level (two-tailed).
Educational attainment showed a modest association with psychological functioning. Participants with university degrees demonstrated slightly higher resilience scores compared to those with primary education (p = 0.047). Trends toward significance were noted for depression and anxiety (both p ≈ 0.05); however, these associations did not remain significant in subsequent multivariate analyses. Employment status was unrelated to any of the outcomes assessed (all p > 0.50).
Trauma exposure was the most consistent and robust factor differentiating psychological outcomes. Participants who reported direct losses or displacement exhibited significantly higher depression (p = 0.001), anxiety (p = 0.046), and PTSD symptoms (p = 0.009), as well as lower well-being (p = 0.025) and resilience (p = 0.002), compared with those who did not experience major losses. These findings underscore the substantial psychological impact associated with severe earthquake-related exposure.
Bivariate correlations
Pearson correlations among the psychological measures are shown in Table 3. Depression, anxiety, and PTSD symptoms were strongly interrelated (rs = 0.65–0.67, p < 0.001). Higher depression and PTSD scores were significantly associated with lower well-being (r = −0.54 and −0.63, respectively, p < 0.001). Resilience was inversely related to all distress measures (rs = −0.40 to −0.48, p < 0.001) and positively associated with well-being (r = 0.48, p < 0.001). All correlations were statistically significant, underscoring the consistent link between psychological distress and diminished well-being and resilience.
Table 3
| Variable | BDI-II | BAI | PCL-5 | WEMWBS | CD-RISC |
|---|---|---|---|---|---|
| BDI-II | – | 0.67** | 0.65** | −0.54** | −0.46** |
| BAI | 0.67** | – | 0.65** | −0.48** | −0.40** |
| PCL-5 | 0.65** | 0.65** | – | −0.63** | −0.48** |
| WEMWBS | −0.54** | −0.48** | −0.63** | – | 0.48** |
| CD-RISC | −0.46** | −0.40** | −0.48** | 0.48** | – |
Pearson correlation matrix for key psychological measures.
**indicates that the correlation is statistically significant at the p < 0.001 level (two-tailed).
The heatmap in Figure 1 displays Pearson correlations among depression (BDI-II), anxiety (BAI), PTSD symptoms (PCL-5), mental well-being (WEMWBS), and resilience (CD-RISC). Warmer colors indicate stronger positive associations, and cooler colors indicate stronger negative associations. All correlations were statistically significant (p < 0.001). Analyses and visualizations were generated using IBM SPSS Statistics 30.
Figure 1
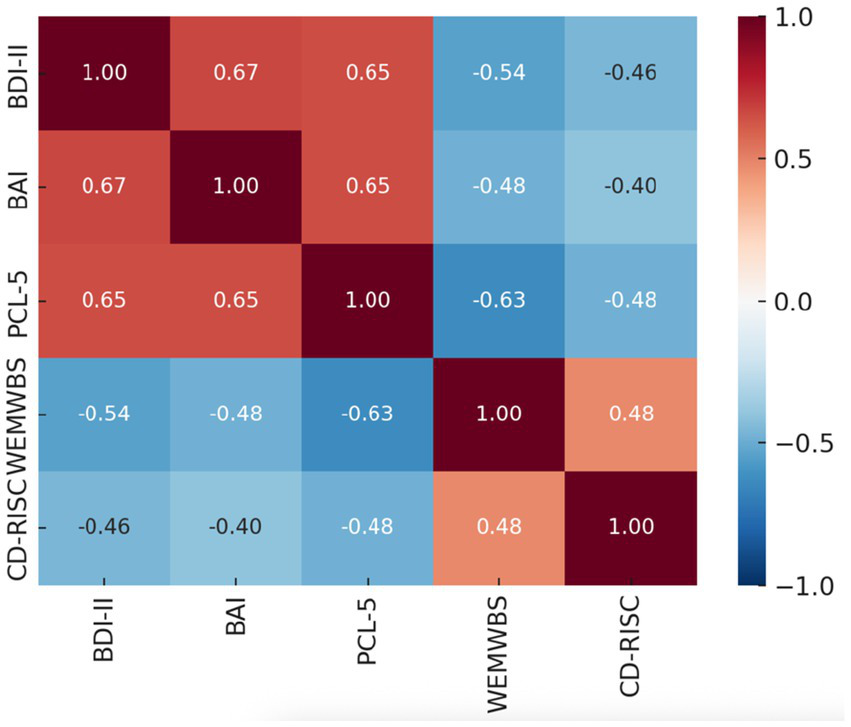
Heatmap Pearson correlation matrix of psychological measures.
Scatterplots in Figure 2 depict Pearson correlations between psychological distress variables (e.g., depression, anxiety, PTSD symptoms) and mental well-being (WEMWBS), with fitted regression lines for visualization. Analyses and visualizations were generated using IBM SPSS Statistics 30.
Figure 2
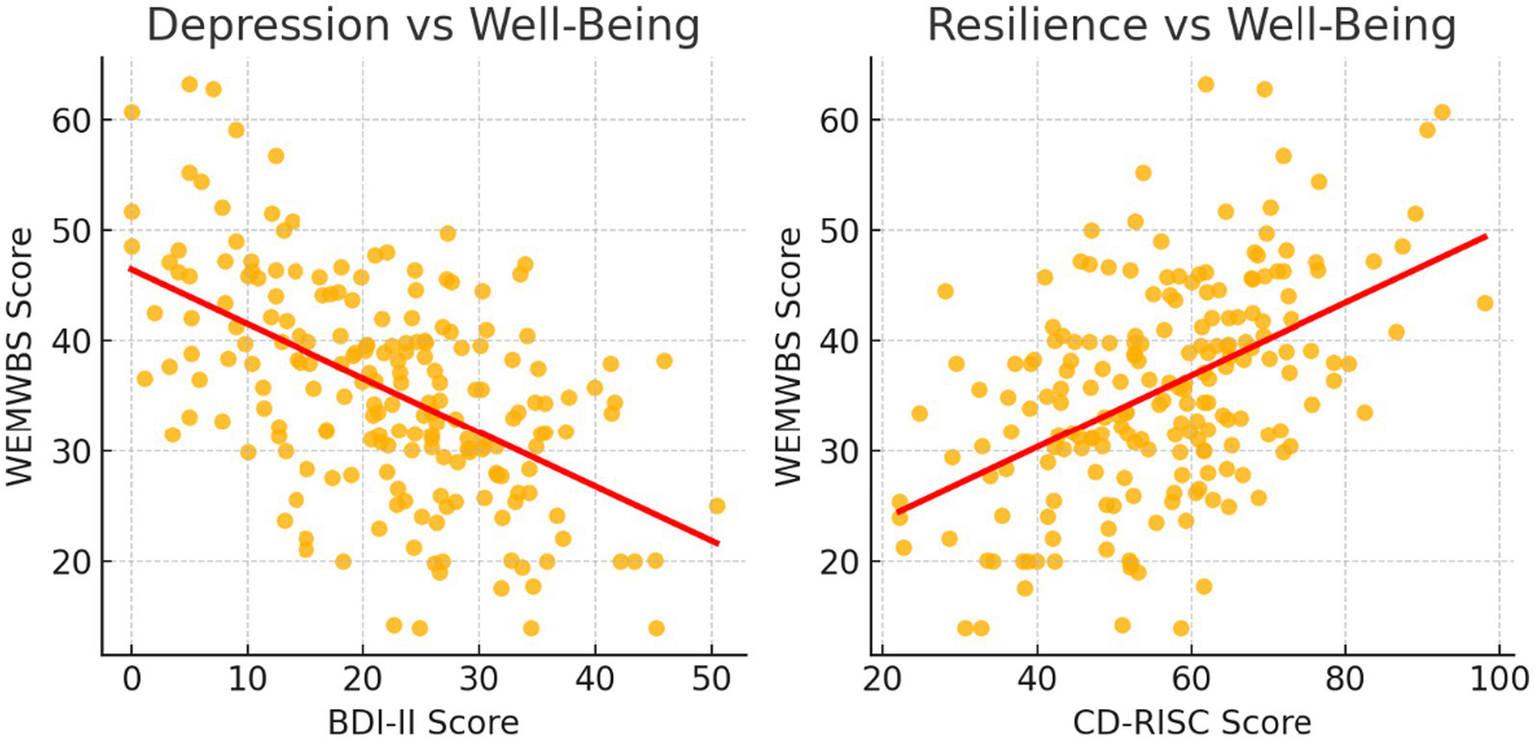
Scatterplots showing Pearson associations between distress and well-being.
Hierarchical regression predicting mental well-being
Results of the hierarchical regression are presented in Table 4. In Step 1, demographic and exposure variables explained 9% of the variance in well-being (R2 = 0.09, p = 0.07), with no significant individual predictors. Trauma exposure showed a marginal effect (β = −0.11, p = 0.08), but gender, marital status, education, and employment were nonsignificant. Adding depression (BDI-II), anxiety (BAI), and PTSD symptoms (PCL-5) in Step 2 significantly improved the model (ΔR2 = 0.36, p < 0.001). The final model accounted for 45% of the variance in well-being, R2 = 0.45, F (9, 190) = 18.83, p < 0.001. Depression (β = −0.24, p = 0.005) and PTSD symptoms (β = −0.28, p = 0.001) independently predicted lower well-being, whereas anxiety was not significant (β = −0.09, p = 0.18). Demographic and exposure variables were no longer significant after distress measures were entered. These findings indicate that depressive and PTSD symptoms, rather than sociodemographic characteristics, were the primary determinants of diminished well-being. Full regression coefficients are presented in Supplementary Table S1.
Table 4
| Predictor | Step 1 β | p | Step 2 β | p |
|---|---|---|---|---|
| Age | −0.05 | 0.47 | −0.02 | 0.78 |
| Female (gender) | −0.06 | 0.30 | −0.04 | 0.50 |
| Married (vs. unmarried) | +0.04 | 0.53 | +0.02 | 0.71 |
| Education (ordinal) | +0.10 | 0.13 | +0.07 | 0.24 |
| Employed (vs. unemployed) | +0.03 | 0.73 | +0.01 | 0.90 |
| Trauma exposure (yes) | −0.11 | 0.08 | −0.05 | 0.41 |
| BDI-II (depression) | – | – | −0.24** | 0.005 |
| BAI (anxiety) | – | – | −0.09 | 0.18 |
| PCL-5 (PTSD symptoms) | – | – | −0.28** | 0.001 |
Hierarchical regression predicting mental well-being (WEMWBS).
Model R2: 0.09 (Step 1), 0.45 (Step 2); Adjusted R2: 0.06 (Step 1), 0.43 (Step 2); ΔR2: 0.36*** (p < 0.001), added in Step 2; Model N = 642.
Standardized coefficients (β) reported. Adjusted R2 values added per reviewer recommendation. ΔR2 reflects variance explained by distress variables added in Step 2.
Figure 3 illustrates the standardized regression coefficients predicting mental well-being (WEMWBS). In the final model (R2 = 0.45), depression (β = −0.24, p = 0.005) and PTSD symptoms (β = −0.28, p = 0.001) were the only significant predictors of lower well-being. Anxiety and all demographic/exposure variables were nonsignificant, indicating that clinical symptom burden, rather than background characteristics, primarily determined survivors’ well-being. Analyses and visualizations were conducted using IBM SPSS Statistics 30.
Figure 3
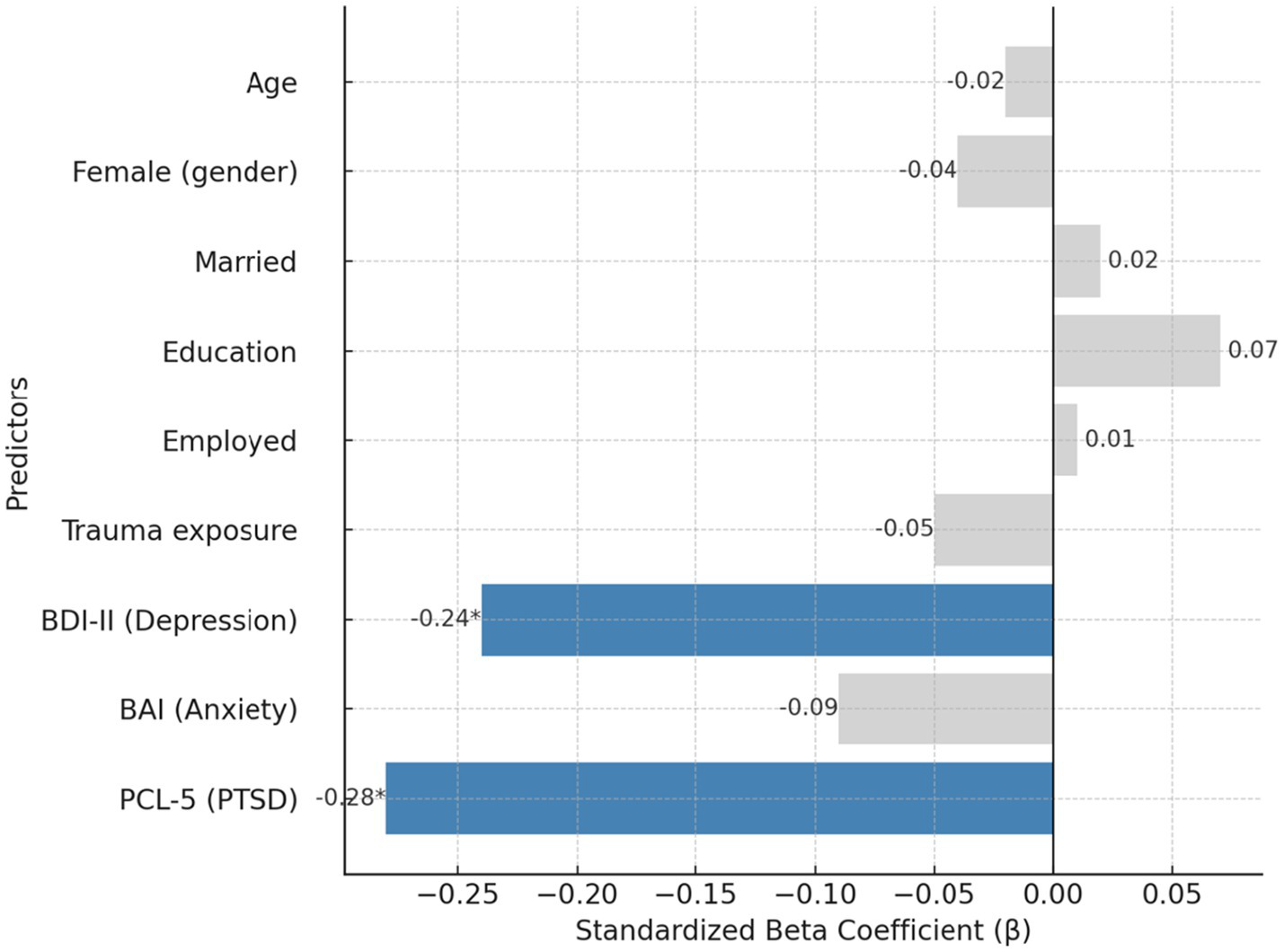
Predictors of mental well-being in hierarchical regression.
Hierarchical regression predicting resilience
Results are shown in Table 5. In Step 1, demographic and exposure variables accounted for only 7% of the variance in resilience (R2 = 0.07, p = 0.12), with no significant predictors. Weak trends for education (β = 0.12, p = 0.06) and trauma exposure (β = −0.10, p = 0.11) did not reach significance. In Step 2, adding depression, anxiety, and PTSD symptoms significantly improved the model (ΔR2 = 0.25, p < 0.001). The final model explained 32% of the variance (R2 = 0.32, F (9,190) = 10.76, p < 0.001). Depression (β = −0.22, p = 0.004) and PTSD symptoms (β = −0.26, p = 0.001) were significant negative predictors, while anxiety was nonsignificant (β = −0.07, p = 0.25). All demographic and exposure variables, including education, were nonsignificant once psychological distress was considered. These results demonstrate that resilience is primarily determined by current levels of depression and PTSD, not by background sociodemographic characteristics. Detailed coefficients are reported in Supplementary Table S2.
Table 5
| Predictor | Step 1 β | p | Step 2 β | p |
|---|---|---|---|---|
| Age | +0.02 | 0.78 | +0.04 | 0.62 |
| Female (gender) | +0.06 | 0.33 | +0.08 | 0.22 |
| Married (vs. unmarried) | +0.04 | 0.52 | +0.03 | 0.65 |
| Education (ordinal) | +0.12 | 0.06 | +0.06 | 0.30 |
| Employed (vs. unemployed) | +0.01 | 0.90 | +0.00 | 0.98 |
| Trauma exposure (yes) | −0.10 | 0.11 | −0.04 | 0.54 |
| BDI-II (Depression) | – | – | −0.22** | 0.004 |
| BAI (Anxiety) | – | – | −0.07 | 0.25 |
| PCL-5 (PTSD symptoms) | – | – | −0.26** | 0.001 |
Hierarchical regression predicting resilience (CD-RISC).
Model R2: 0.07 (Step 1), 0.32 (Step 2); Adjusted R2: 0.04 (Step 1), 0.30 (Step 2); ΔR2: 0.25*** (p < 0.001), added in Step 2; Model N = 642.
CD-RISC = Connor–Davidson Resilience Scale. Adjusted R2 values added per reviewer recommendation.
Figure 4 displays the standardized regression coefficients predicting psychological resilience. In the final model (R2 = 0.32), depression (β = −0.22, p = 0.004) and PTSD symptoms (β = −0.26, p = 0.001) were significant negative predictors of resilience. Anxiety and all demographic/exposure variables were nonsignificant, indicating that current clinical symptoms—not background characteristics—were the primary determinants of resilience. Analyses and visualizations were generated using IBM SPSS Statistics 30.
Figure 4
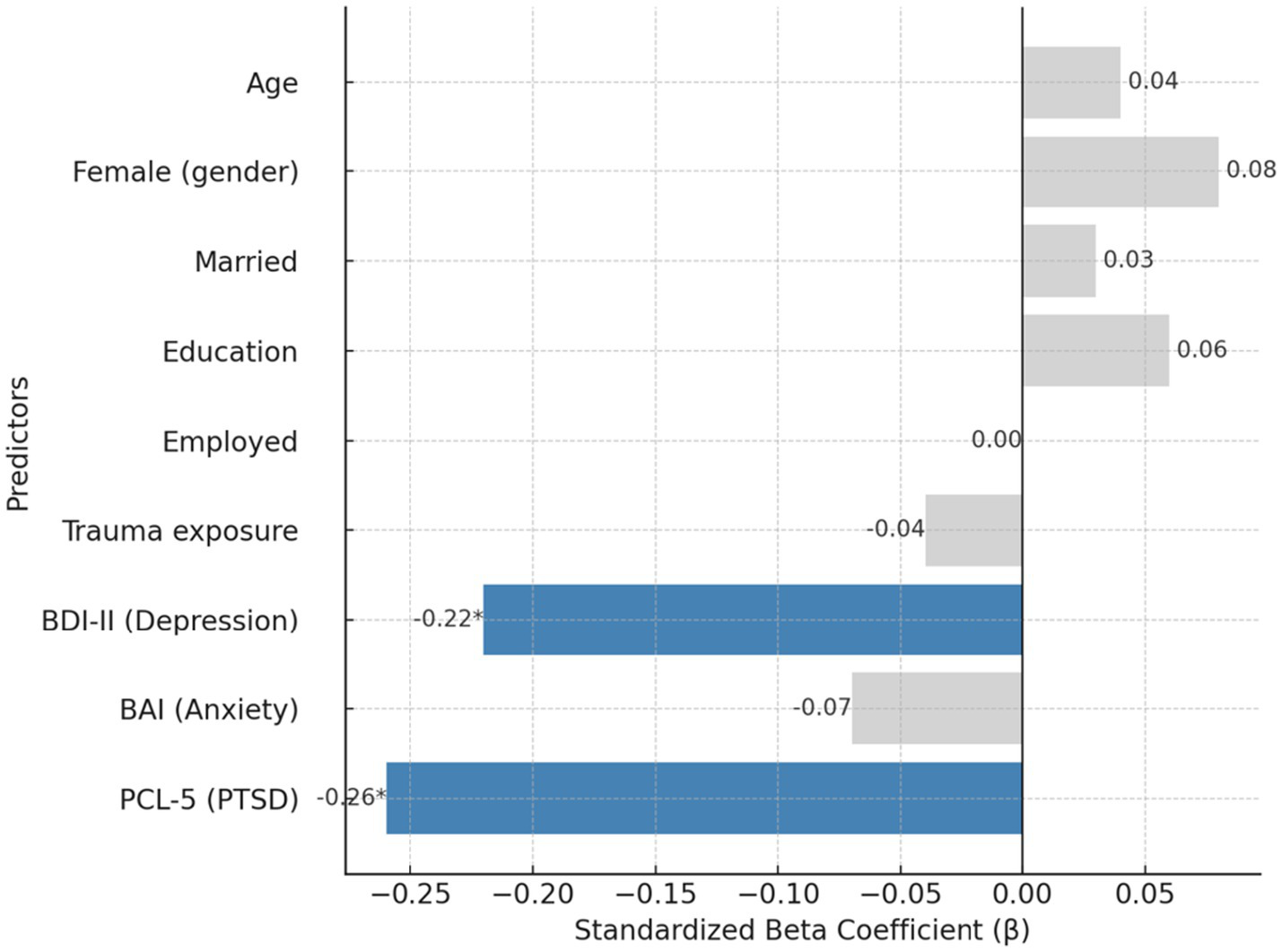
Predictors of resilience (CD-RISC) in hierarchical regression.
Logistic regression predicting probable PTSD diagnosis
A logistic regression was conducted to identify predictors of probable PTSD, defined as a PCL-5 score ≥ 47. The overall model was statistically significant, χ2 (8) = 58.9, p < 0.001, with good fit (Nagelkerke R2 = 0.50) and an overall classification accuracy of 82% (sensitivity = 80%, specificity = 83%). Results are shown in Table 6. Depressive symptoms were the strongest predictor: each one-point increase on the BDI-II was associated with a 10% increase in the odds of meeting PTSD criteria (OR = 1.10, 95% CI [1.04–1.16], p = 0.001). Female gender was also a significant predictor (OR = 1.80, 95% CI [1.08–2.99], p = 0.024), consistent with prior findings of elevated PTSD risk among women. No other demographic variables (age, marital status, education, employment) or trauma exposure independently predicted PTSD when controlling for psychological symptoms. Anxiety symptoms were also nonsignificant (OR = 1.02, 95% CI [0.98–1.06], p = 0.298). The complete regression model is provided in Supplementary Table S3.
Table 6
| Predictor | Odds ratio (OR) | 95% CI for OR | p |
|---|---|---|---|
| Female (vs. male) | 1.80 | 1.08–2.99 | 0.024* |
| Age (years) | 0.99 | 0.96–1.02 | 0.501 |
| Married (vs. unmarried) | 0.78 | 0.50–1.23 | 0.279 |
| Education level (ordinal) | 0.90 | 0.75–1.08 | 0.338 |
| Employed (vs. unemployed) | 1.02 | 0.60–1.72 | 0.947 |
| Trauma exposure (yes) | 1.23 | 0.83–1.83 | 0.307 |
| BDI-II (Depression) | 1.10 | 1.04–1.16 | 0.001** |
| BAI (Anxiety) | 1.02 | 0.98–1.06 | 0.298 |
Logistic regression predicting probable PTSD diagnosis (PCL-5 ≥ 47).
Model χ2 (8) = 58.9, p < 0.001; Nagelkerke R2 = 0.50; classification accuracy = 82%. OR > 1 indicates higher odds of PTSD diagnosis.
*, **indicates statistical significance at the p < 0.05 and p < 0.01 level (two-tailed).
These findings indicate that depressive symptom severity and female gender significantly increased the likelihood of probable PTSD, while other background factors did not add explanatory power beyond current psychological distress. Beyond accuracy, sensitivity, and specificity, the logistic model demonstrated strong discriminative performance, with an area under the ROC curve of 0.87 (95% CI: 0.84–0.90). Calibration was adequate, as indicated by a non-significant Hosmer–Lemeshow goodness-of-fit test (p > 0.05), and graphical inspection of predicted versus observed probabilities showed no systematic miscalibration.
Figure 5 shows the predicted probabilities of meeting the PTSD cut-off (PCL-5 ≥ 47) across levels of depression severity (BDI-II), stratified by gender. Higher depression scores markedly increased PTSD risk, and female survivors consistently exhibited higher predicted probabilities than males at comparable symptom levels. These findings correspond to the logistic regression results, where depression (OR = 1.10, p = 0.001) and female gender (OR = 1.80, p = 0.024) were significant predictors, while trauma exposure and other demographic variables were nonsignificant. Analyses and visualizations were generated using IBM SPSS Statistics 30.
Figure 5
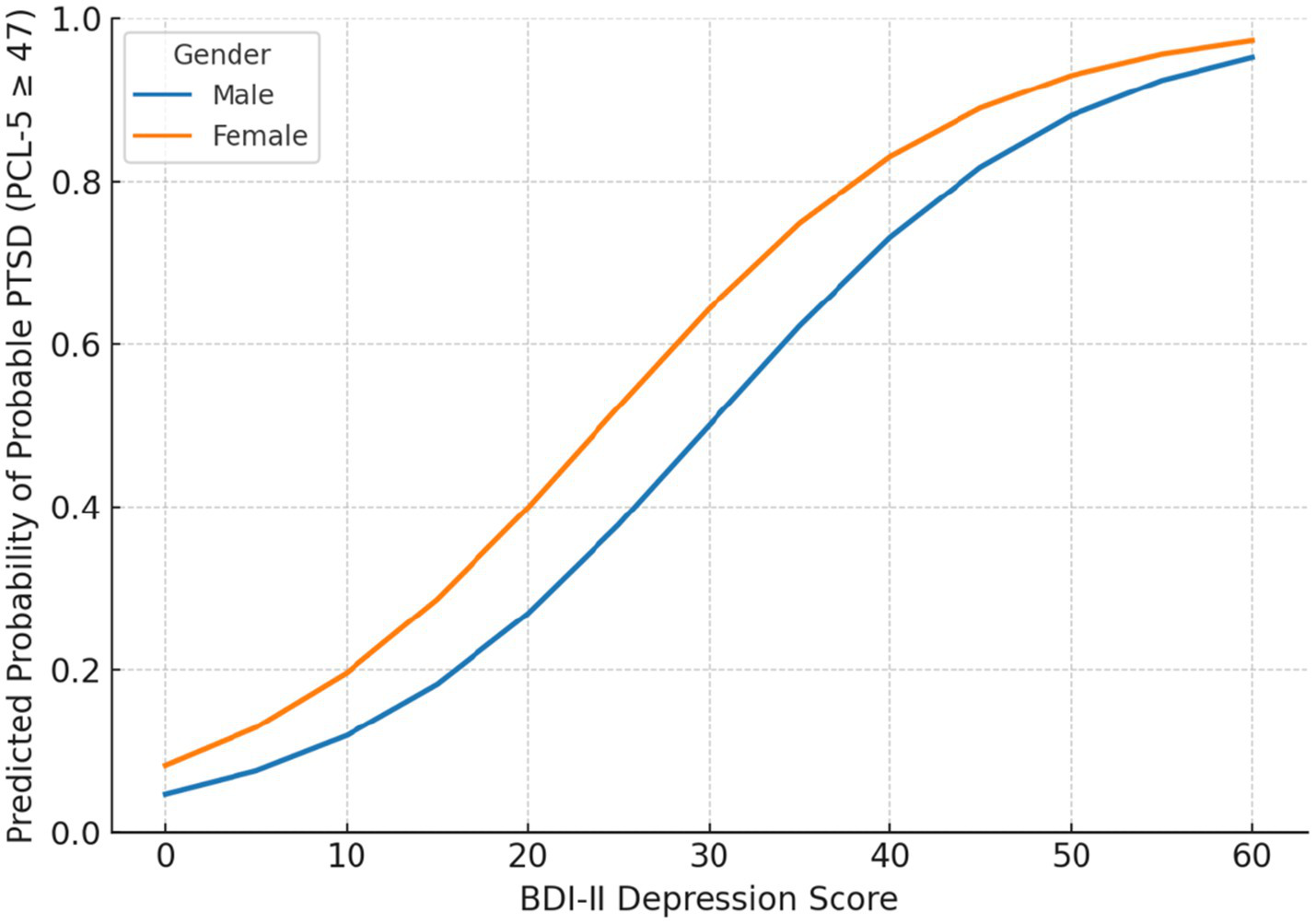
Predicted probability of probable PTSD (PCL-5 ≥ 47) by gender and depression severity.
Overall, 31% of participants scored above the PCL-5 cut-off for probable PTSD, and mean scores indicated moderate levels of depression and anxiety. Consistent with the Turkish validation of the PCL-5 (Boysan et al., 2017), the ≥47 threshold was used to define probable PTSD. Using this cut-off, 31.0% of participants screened positive for probable PTSD (95% CI: 27.4–34.8%). To assess the robustness of prevalence estimates, a sensitivity analysis was conducted using a more inclusive threshold (PCL-5 ≥ 33). Under this criterion, 48.9% of participants screened positive (95% CI: 45.0–52.7%). Logistic regression results remained substantively unchanged when re-estimated with the lower threshold, indicating that model inferences were stable across cut-off values. Female participants and those exposed to direct trauma had significantly higher symptom levels. Well-being and resilience were inversely associated with PTSD and depression, and multivariate models showed that these distress variables explained substantially more variance than demographic characteristics.
Discussion
In this multi-site cross-sectional study of adults who survived the 2023 Kahramanmaraş earthquakes, the findings provide compelling evidence of both the substantial psychological burden imposed by the disaster and the important associations between resilience, well-being, and post-disaster adjustment. Consistent with expectations and with prior research on major earthquakes, levels of psychological distress were markedly elevated across the sample. A considerable proportion of participants reported clinically significant symptoms of PTSD, depression, and anxiety, and the results suggest that many survivors continued to experience pronounced distress nearly 2 years after the event. This pattern aligns with early reports from the affected region indicating that more than half of adults exposed to the February 2023 earthquakes may experience PTSD-related symptoms (Lok et al., 2025; Yılmaz and Doğan, 2025). Elevated levels of depression and anxiety accompanied the PTSD burden, reflecting the broad and persistent spectrum of trauma-related psychopathology frequently observed following large-scale catastrophic events.
Despite the growing body of research conducted in the immediate aftermath of the February 2023 Kahramanmaraş earthquakes, there remains a notable lack of large-scale, theoretically grounded studies examining survivors’ long-term psychological adjustment. The present study makes several unique contributions to this emerging literature. First, it represents one of the largest multi-site assessments of adult survivors nearly 2 years after the disaster, capturing persistent patterns of distress, resilience, and well-being across 11 heavily affected cities. This design provides a rare and timely perspective on the prolonged psychological impact of the earthquake sequence, extending beyond the short-term reactions documented in earlier reports. Second, by simultaneously evaluating psychological distress, resilience, and well-being within a unified theoretical framework, the study moves beyond traditional symptom-focused disaster research and offers a more holistic understanding of mental health during protracted recovery. Third, the use of rigorous multivariate models enables the identification of the factors most strongly associated with long-term adjustment, highlighting the central role of depression and PTSD symptoms compared with demographic or exposure variables. Together, these contributions advance the field by providing high-quality, late-phase evidence on the psychological consequences of the 2023 earthquakes and by underscoring the importance of integrating both negative and positive mental health constructs in post-disaster research.
Importantly, beyond these adverse outcomes, the findings also revealed substantial impairments in positive mental health: overall well-being scores were considerably lower than normative benchmarks, and many survivors reported difficulties experiencing positive affect or life satisfaction in the aftermath of the disaster (Kaplan et al., 2024). Taken together, these results highlight that the psychological consequences of the earthquakes extend well beyond diagnosable psychiatric disorders, affecting survivors’ broader psychosocial functioning and perceived quality of life. Notably, even individuals who did not meet criteria for probable PTSD or clinically significant depression exhibited reduced well-being, underscoring the need for comprehensive, multidimensional approaches to post-disaster recovery.
The examination of group differences provided insight into which subgroups of survivors were most psychologically affected. Consistent with prior disaster research, female participants reported significantly higher depressive symptoms than males, although gender differences were not observed for PTSD or anxiety in the unadjusted comparisons (Fu et al., 2021; Cénat and Derivois, 2014). Notably, when multivariate models accounted for overall symptom burden, female gender emerged as a significant predictor of probable PTSD, indicating an elevated risk for meeting diagnostic thresholds among women. This pattern has been widely documented in post-disaster contexts and may reflect intersecting biological, social, and caregiving-related factors that heighten vulnerability among women (Khatri et al., 2019).
Trauma exposure severity was also strongly associated with psychological outcomes. Survivors who experienced life-threatening or highly distressing events—such as entrapment under collapsed structures, severe injury, the loss of immediate family members, or witnessing extensive destruction—reported substantially higher PTSD, depression, and anxiety symptoms than those with less severe exposure (Wu et al., 2014). These results are consistent with the dose–response pattern frequently described in disaster literature, whereby greater exposure to traumatic stressors is associated with greater psychological distress. In the present sample, individuals who lost first-degree relatives or whose homes were entirely destroyed were among those with the highest levels of symptom severity, a finding that aligns with emerging evidence from the 2023 earthquakes.
By contrast, survivors who did not experience major personal losses—such as bereavement or significant property destruction—reported relatively lower, though still elevated, levels of psychological symptoms. Importantly, the analyses revealed limited evidence that demographic variables such as age, education, marital status, or employment played a major role in differentiating psychological outcomes, a pattern also noted in other studies of large-scale disasters where symptoms remain high across groups regardless of socioeconomic status. Although age has been identified as a risk factor in some contexts—with both older and younger adults reported as more vulnerable in different studies—the present study did not find age to be a significant predictor of distress, potentially reflecting the complex interaction of risk and resilience factors within this cohort (Kun et al., 2013; Kongshøj and Berntsen, 2023). Taken together, these subgroup findings indicate that women—particularly in adjusted models—and individuals with severe earthquake-related exposure bear a disproportionate psychological burden. These observations underscore the need to prioritize these groups in post-disaster mental health interventions.
Beyond characterizing overall distress levels, a central aim of this study was to identify factors associated with key psychological outcomes—namely PTSD severity, mental well-being, and resilience. The regression analyses yielded several important observations. Consistent with expectations, trauma-related variables demonstrated strong associations with PTSD symptom severity in the bivariate analyses. Survivors who experienced highly distressing events, such as bereavement or entrapment under rubble, exhibited significantly higher PCL-5 scores, in line with previous evidence indicating that such events constitute potent risk factors for post-traumatic stress (Chan et al., 2012). However, in the multivariate logistic regression model, trauma exposure did not remain a statistically significant independent predictor after accounting for psychological symptom variables. Instead, female gender and depressive symptom severity emerged as the most robust predictors of probable PTSD, underscoring their salience as markers of elevated vulnerability.
Although resilience was not explicitly examined as a predictor of probable PTSD in the multivariate models, the bivariate analyses revealed a strong inverse association between resilience and PTSD symptoms. This finding aligns with theoretical frameworks (Thompson et al., 2018) and longitudinal research demonstrating that higher resilience—characterized by optimism, adaptive coping strategies, and strong social support—is associated with reduced PTSD symptom severity (Kamphuis et al., 2021; Prati and Pietrantoni, 2009; Weinberg et al., 2016). While causal inferences cannot be drawn from the cross-sectional design, the observed pattern is consistent with evidence suggesting that resilience may play a protective role in mitigating the long-term psychological effects of traumatic events.
When predictors of mental well-being, as measured by WEMWBS scores, were examined, the analyses revealed a pattern that closely aligned with the findings for PTSD. Survivors with lower levels of psychological distress—specifically fewer symptoms of PTSD, depression, and anxiety—reported significantly higher well-being. PTSD symptom severity demonstrated a strong inverse association with well-being: individuals with minimal PTSD symptoms exhibited the highest levels of psychological well-being, whereas those with severe symptoms scored markedly lower on the WEMWBS. Consistent with this relationship, the regression analyses indicated that lower PTSD and depressive symptom levels were significant predictors of higher well-being, underscoring the close link between distress reduction and improvements in subjective mental health.
However, distress reduction was not the sole determinant of well-being. Resilience again emerged as an independent positive correlate. Even after accounting for psychological symptoms, individuals with higher resilience reported substantially greater well-being. This suggests that resilience supports more than the absence of psychopathology; it also contributes meaningfully to the presence of positive mental health attributes such as optimism, purpose, and life satisfaction. One possible explanation is that resilient survivors may draw upon adaptive coping strategies and psychological resources that allow them to maintain or restore well-being despite ongoing adversity. A modest trend was also observed in which older age was associated with slightly higher well-being (and lower PTSD), although this association did not reach strong statistical significance in the fully adjusted models. If substantiated in future research, this trend may reflect the influence of accumulated life experience or previous exposure to hardship, as some studies have suggested (Yayla et al., 2025; Ardalan et al., 2011). Nevertheless, given the mixed evidence regarding age-related differences in disaster contexts, additional research is warranted. Overall, these findings highlight the critical role of psychosocial resources—particularly resilience, and the social support elements embedded within it—in promoting positive adaptation. At the same time, they reinforce that elevated distress is intrinsically linked to diminished well-being, emphasizing the need for interventions that simultaneously reduce symptoms and strengthen survivors’ resilience capacities.
Predictors of resilience were also examined. Although the cross-sectional design precludes causal inference, the correlational analyses revealed a consistent pattern: resilience was negatively associated with all indicators of psychological distress and positively associated with mental well-being. Survivors who reported higher resilience tended to exhibit lower levels of PTSD, depression (BDI-II), and anxiety (BAI), alongside higher WEMWBS scores. These findings suggest that resilience, distress, and well-being lie on interconnected continua, such that individuals functioning well in one domain often demonstrate strengths in the others. It is plausible that resilience both shapes and is shaped by mental health. For example, individuals with higher resilience may possess coping skills, adaptive cognitive appraisals, or stronger support networks that enable them to navigate post-disaster challenges more effectively, thereby reducing psychological symptoms. Conversely, lower levels of distress may allow survivors to better mobilize and sustain their resilience resources. Demographic factors showed limited explanatory value in this context; aside from a non-significant trend toward slightly higher resilience among males, variables such as age, education, marital status, and employment did not meaningfully differentiate resilience levels. Instead, unmeasured experiential and psychosocial variables—such as perceived social support, coping behaviors, and processes of meaning-making—are likely to play a more prominent role in shaping resilience (Theron and Theron, 2014; Çınaroğlu, 2024). Overall, the central implication is that resilience is closely intertwined with psychological outcomes. Strengthening survivors’ resilience capacities may therefore represent a key pathway for enhancing both symptom recovery and broader well-being in the aftermath of large-scale disasters.
The present findings align closely with the broader literature on disaster mental health and carry several important implications for both intervention and theoretical models. First, the high prevalence of PTSD and depressive symptoms observed in this sample confirms that mental health services must constitute a central component of disaster response efforts following the 2023 earthquakes. The psychological burden in the affected region remains substantial, with evidence pointing to widespread trauma- and grief-related reactions nearly 2 years after the event. This underscores the need for comprehensive, large-scale mental health interventions—including systematic screening and outreach initiatives to identify individuals experiencing significant PTSD, anxiety, or depression, followed by accessible and appropriate treatment options. Trauma-focused therapies, such as Trauma-Focused Cognitive Behavioral Therapy and Eye Movement Desensitization and Reprocessing, should be prioritized for survivors with severe PTSD, whereas psychoeducation and supportive counseling may be effective for individuals with moderate levels of distress (Leiva-Bianchi et al., 2018; Saltini et al., 2018). The findings also suggest that certain subgroups warrant particular attention. Women, bereaved individuals, and those who sustained severe injuries or displacement appear to be at heightened risk and may benefit from proactive monitoring and early therapeutic intervention. Culturally sensitive approaches that incorporate locally validated tools and take into account community norms surrounding emotional expression are essential for promoting engagement and enhancing treatment acceptability (Çınaroğlu, 2025). Given the scale of mental health needs and the limitations in available professional capacity, scalable and resource-efficient strategies are critical. Psychological First Aid (PFA), delivered by trained non-specialists, has demonstrated value in similar disaster contexts, and was deployed widely in Türkiye after the earthquakes. The present findings highlight the need to sustain and expand such support. Over the medium and long term, community-based programs—including peer support groups, community health worker outreach, and integration of mental health services into primary care—may contribute to ongoing recovery.
Evidence from prior large-scale disasters supports the importance of community resources and social connectedness. Experiences from previous Turkish earthquakes, including the 1999 Marmara quake, show that strengthening social networks and mobilizing community structures can substantially mitigate trauma-related outcomes. Enhancing social connectedness through community centers, group activities, or commemorative gatherings may help counteract isolation and hopelessness, both of which contribute to chronic PTSD and depression. Observations from other major crises indicate that disaster-related mental health needs often persist long after the initial emergency phase and may result in sustained increases in service utilization; for example, Barlattani et al. (2024) reported prolonged elevations in psychiatric admissions following both the L’Aquila earthquake and the COVID-19 lockdown. Situating the current findings within this larger context suggests that the considerable symptom burden and reduced resilience observed nearly 2 years after the 2023 Kahramanmaraş earthquakes are likely to generate extended mental health service needs. These insights reinforce the importance of implementing integrated long-term trauma care, proactive outreach, and resilience-building interventions to ensure continuity of support throughout the prolonged course of post-disaster recovery.
Beyond the treatment of psychopathology, the present findings underscore the importance of interventions aimed at strengthening resilience and enhancing well-being as integral components of holistic post-disaster recovery. The observed association between resilience and more favorable psychological outcomes indicates that fostering resilience is not merely an abstract or long-term ideal but a practical and attainable intervention target with meaningful implications for survivors’ mental health. Strategies designed to enhance resilience may include structured training programs focused on problem-solving, emotion regulation, and stress-management skills, which can be implemented through brief workshops or group-based formats within temporary housing communities.
Strengthening familial and social support systems represents another important avenue for intervention. Approaches that incorporate family members or peer-based models—such as buddy systems, supportive listening groups, or peer mentoring—may reinforce survivors’ sense of connectedness and belonging, thereby bolstering their resilience. Evidence from prior research suggests that even low-intensity interventions, such as facilitating communication with social networks through mobile devices or organizing community gatherings, can produce measurable improvements in well-being following disasters (Bryant et al., 2017). Psychoeducation focused on common post-traumatic reactions and the normalization of help-seeking can further empower survivors and reduce feelings of helplessness (Hisli Sahin et al., 2011).
From a public health standpoint, collaboration with community leaders and leveraging local cultural strengths—such as spiritual coping practices, communal rituals, and traditions of mutual aid—may amplify resilience at the community level. Consistent with findings from this study, survivors have reported relying on prayer and social support as primary coping strategies, a pattern also observed by Akçay et al. (2024). Integrating such culturally meaningful coping practices into mental health programming—for example, by providing spaces for collective prayer, remembrance activities, or community-based support meetings alongside psychological services—may enhance engagement, cultural acceptability, and overall intervention effectiveness.
In terms of theoretical implications, the dual emphasis on psychological distress and positive mental health aligns closely with contemporary conceptualizations of mental health. The findings lend support to the “dual continuum” framework, which posits that mental health encompasses both the absence of mental illness and the presence of positive well-being. This distinction was evident in the current sample; some survivors who exhibited relatively low levels of clinical symptoms nonetheless reported diminished well-being, whereas others with high levels of well-being endorsed fewer symptoms. Such patterns illustrate that these dimensions, while related, are distinct constructs that must be assessed and addressed in parallel to obtain a comprehensive understanding of post-disaster functioning. The inclusion of both WEMWBS and CD-RISC in this study therefore provides a more nuanced and multidimensional picture of survivor outcomes than would reliance on PTSD or depression measures alone.
The results also highlight the interaction between risk factors (e.g., trauma severity, female gender) and protective factors (e.g., resilience, social support) in shaping psychological trajectories following disaster exposure. This dynamic interplay is consistent with ecological models of disaster mental health and aligns with Norris et al.’s disaster response framework (Norris et al., 2008), which emphasizes that both resource loss and resource gain processes contribute to psychological outcomes. Although resilience was not included as a direct predictor of PTSD in the multivariate models, its strong correlations with both distress and well-being reinforce theoretical models of resilience and post-traumatic growth, suggesting that interventions fostering meaning-making, coping self-efficacy, and empowerment may promote not only symptom reduction but also positive psychological development after trauma.
Additionally, the findings add to ongoing discussions regarding the role of sociocultural factors in disaster recovery. Although the present analyses did not identify strong effects for variables such as education, marital status, or employment, other factors—such as ethnicity or income—were not assessed. Prior work (e.g., Kizilhan et al., 2024) suggests that in large-scale catastrophes, psychosocial impacts may cut across conventional socioeconomic boundaries, with elevated symptoms observed broadly across population groups. This phenomenon may reflect a “shared trauma” effect, in which communal exposure produces a more uniform distribution of psychological consequences. Further research is needed to examine these sociocultural processes and their implications for theory and intervention.
Limitations
Despite its strengths, this study has several limitations. First, the cross-sectional design provides only a snapshot nearly 2 years after the earthquakes, precluding causal inferences and leaving the trajectory of psychological symptoms and resilience unknown. Longitudinal follow-up is needed to clarify directionality (e.g., whether resilience buffers PTSD or vice versa) and to detect delayed-onset disorders. Second, although the sample was large and drawn from 11 heavily affected cities, the sites differed in the degree of destruction, displacement, and access to resources, creating natural heterogeneity in survivor experiences. The analyses did not model clustering by city, and therefore city-level differences may have influenced psychological outcomes; this should be considered when interpreting the findings. Third, participation was voluntary and limited to individuals accessible in affected areas, which may exclude survivors who relocated or were severely impaired. Fourth, all data were based on self-report questionnaires. Although validated instruments were used, biases such as underreporting, overreporting, and shared method variance remain possible, and prevalence estimates reflect probable—rather than clinically diagnosed—conditions. Fifth, contextual factors such as social support, coping strategies, community resources, and pre-disaster mental health were not directly measured, limiting the ability to account for their effects. Another important limitation concerns the lack of a quantifiable exposure-severity index. Although the study distinguished between participants with and without major earthquake-related losses, exposure was captured in a binary format and did not include graded measures of humanitarian, financial, structural, or social loss (e.g., extent of property destruction, financial damage, duration of displacement, or loss of livelihood). This limits the ability to examine dose–response relationships or determine which specific types or intensities of earthquake-related adversity are most strongly associated with depression, anxiety, PTSD symptoms, resilience, and well-being. As a result, interpretations of exposure effects should be viewed with caution, and future research would benefit from employing validated multi-domain exposure-severity instruments. The decision to use a simplified, dichotomous exposure indicator was also influenced by the practical constraints of conducting multi-site fieldwork nearly 2 years after the earthquakes. Because data were collected across 11 cities with substantial variability in destruction, displacement, and recovery conditions, obtaining standardized, objective, and multi-domain exposure metrics (e.g., degree of property damage, financial loss, duration of homelessness, or detailed bereavement characteristics) was not feasible in a consistent manner across sites. To preserve comparability and measurement integrity across all data-collection locations, a binary exposure classification was adopted. This rationale is now explicitly stated to provide clarity regarding the methodological choices. Another limitation relates to the restricted sampling frame. Individuals with current psychiatric diagnoses, psychiatric medication use, or ongoing psychotherapy were excluded to focus on untreated, community-dwelling survivors. However, these criteria inadvertently removed high-risk groups who are more likely to exhibit severe PTSD, depression, anxiety, and reduced well-being. As a result, the estimates presented in this study likely underestimate the true psychological burden among the broader survivor population, and the findings should be interpreted with this reduced generalisability in mind. Also, although regression models identified statistical associations between distress variables, well-being, and resilience, the cross-sectional design precludes any causal inference. The temporal ordering of symptoms and positive psychological resources cannot be established, and all observed relationships should be interpreted as correlations rather than causal effects. Longitudinal designs are needed to determine directionality and examine potential causal pathways. Finally, the focus on adults restricts generalizability to children, adolescents, or other vulnerable groups such as the elderly or individuals with disabilities. Future research should incorporate validated, multi-domain exposure-severity instruments to enable more granular modeling of disaster-related adversity and to clarify how specific forms and intensities of loss influence psychological distress, resilience, and well-being.
Conclusion
This study offers a comprehensive and nuanced portrayal of the psychological aftermath of the 2023 Kahramanmaraş earthquakes. The findings indicate that nearly 2 years after the disaster, a substantial proportion of survivors continue to experience elevated levels of trauma-related distress, highlighting an ongoing public mental health challenge that requires sustained attention. At the same time, the results also reveal meaningful signs of resilience; many individuals demonstrate the capacity to adapt, recover, or maintain aspects of well-being despite prolonged adversity.
These dual observations underscore the need for a balanced, two-pronged approach to post-disaster mental health care. On the one hand, accessible and evidence-based clinical services remain essential for survivors experiencing significant PTSD, depression, or anxiety. On the other hand, preventive and strengths-oriented interventions aimed at enhancing resilience and well-being are equally critical. Mental health support will be most effective when it addresses both symptom reduction and the promotion of adaptive psychological resources, including coping efficacy, social connectedness, and meaning-making.
As Türkiye progresses through a prolonged recovery process, the integration of mental health services into broader rebuilding efforts—ranging from primary care settings in temporary housing areas to community-led support initiatives—will be vital. The present findings support such integrated models and offer empirical guidance for targeted outreach, particularly for subgroups at elevated risk, such as women, bereaved individuals, and survivors with severe exposure.
Ultimately, promoting psychological recovery extends beyond mitigating distress; it involves restoring hope, agency, and social cohesion among survivors. By identifying key correlates of both vulnerability and resilience, this study contributes to the evidence base needed to inform long-term disaster mental health strategies. Continued investment in research, service capacity, and community-based interventions will be essential for fostering sustained recovery and supporting affected populations as they work toward renewed well-being.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Istanbul Nişantaşı University Ethical Committee (Approval number: 20240822-49). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The author would like to thank her graduate students in the Clinical Psychology program for their assistance (Merve Bildik, Büşra Toker, Eli,f Pulat and Yaren İlmaz) with data collection across the affected sites. She also sincerely thanks all participants for generously sharing their time and experiences, which made this research possible. The author confirms that all individuals acknowledged have provided permission to be named. No financial or material support was received for this study.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. The author used ChatGPT-5.1 Pro exclusively for grammar correction, language refinement, and formatting purposes during the manuscript preparation process. No generative AI tools were used to create, analyze, interpret, or synthesize scientific content. All intellectual work, including study design, data analysis, interpretation, and conclusions, was performed solely by the author.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1730083/full#supplementary-material
References
1
Akçay S. Beydili Gürbüz E. Koca E. (2024). Trauma levels after the 2023 Kahramanmaraş earthquakes in Türkiye. J. Soc. Serv. Res.50, 519–530. doi: 10.1080/01488376.2024.2339967
2
Ardalan A. Mazaheri M. Vanrooyen M. Mowafi H. Nedjat S. Naieni K. H. et al . (2011). Post-disaster quality of life among older survivors five years after the bam earthquake: implications for recovery policy. Ageing Soc.31, 179–196. doi: 10.1017/S0144686X10000772
3
Arguvanlı Çoban S. Gün Koşar Y. (2025). Relationship between post-traumatic stress disorder and spiritual well-being in older adult earthquake survivors: a cross-sectional correlational study. J. Relig. Spiritual. Aging37, 153–166. doi: 10.1080/15528030.2024.2437792
4
Balbay E. G. Annakkaya A. N. Balbay Ö. (2024). Earthquake and sleep health effects. Turk. J. Sleep Med.11, 141–146. doi: 10.4274/jtsm.galenos.2023.87059
5
Barlattani T. Salfi F. Socci V. Renzi G. D’Amelio C. Russo A. et al . (2024). Patterns of psychiatric admissions across two major health crises: L’Aquila earthquake and COVID-19 pandemic lockdown. BMC Psychiatry24:658. doi: 10.1186/s12888-024-06078-3
6
Beck A. T. Epstein N. Brown G. Steer R. A. (1993). Beck anxiety inventory. J. Consult. Clin. Psychol.61, 588–592.
7
Beck A. T. Steer R. A. Brown G. (1996). Beck depression inventory–II. San Antonio, TX: Psychological Corporation.
8
Boysan M. Guzel Ozdemir P. Ozdemir O. Selvi Y. Yilmaz E. Kaya N. (2017). Psychometric properties of the Turkish version of the PTSD checklist for diagnostic and statistical manual of mental disorders, (PCL-5). Psychiatry Clin. Psychopharmacol.27, 300–310. doi: 10.1080/24750573.2017.1342769
9
Bryant R. A. Gallagher H. C. Gibbs L. Pattison P. MacDougall C. Harms L. et al . (2017). Mental health and social networks after disaster. Am. J. Psychiatry174, 277–285. doi: 10.1176/appi.ajp.2016.1511140
10
Can Gür G. (2024). Shattered ground, resilient souls: examining coping strategies, social support, and earthquake exposure’s effects on post-traumatic stress disorder symptoms among adolescent and young adults survivors of the 2023 earthquake in Türkiye. Curr. Psychol.43, 21745–21755. doi: 10.1007/s12144-024-05995-6
11
Cénat J. M. Derivois D. (2014). Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adult survivors of earthquake in Haiti after 30 months. J. Affect. Disord.159, 111–117. doi: 10.1016/j.jad.2014.02.025,
12
Chan C. L. Wang C. W. Ho A. H. Qu Z. Y. Wang X. Y. Ran M. S. et al . (2012). Symptoms of posttraumatic stress disorder and depression among bereaved and non-bereaved survivors following the 2008 Sichuan earthquake. J. Anxiety Disord.26, 673–679. doi: 10.1016/j.janxdis.2012.05.002,
13
Chen X. Y. Liu X. Shi X. Chen H. Fan F. (2022). Psychological resilience and posttraumatic growth in adolescent survivors of earthquake: a 10-year cohort study. J. Psychiatr. Res.155, 331–337. doi: 10.1016/j.jpsychires.2022.09.021,
14
Çınaroğlu M. (2024). Islamic coping, post traumatic stress disorder (PTSD) and Islam oriented trauma focused cognitive behavioral therapy (IO-TF-CBT) in post-Kahramanmaraş earthquake period. Eskiyeni.52, 351–376. doi: 10.37697/eskiyeni.1410050
15
Çınaroğlu M. (2025). Comparing the effectiveness of trauma-focused cognitive behavioral therapy (CBT) and Islamic trauma-focused CBT in reducing posttraumatic stress disorder symptoms among Muslim earthquake survivors. Spirit. Clin. Pract. doi: 10.1037/scp0000401
16
Çınaroğlu M. Yılmazer E. Noyan Ahlatcioglu E. Ülker S. V. Hızlı Sayar G. (2025). Psychological impact of the 2023 Kahramanmaraş earthquakes: a systematic review and meta-analysis of PTSD, depression, and anxiety among Turkish adults. Front. Public Health13:1664212. doi: 10.3389/fpubh.2025.1664212
17
Çınaroğlu M. Yılmazer E. Sayar G. H. (2025). Psychological impact of the 2023 Kahramanmaraş earthquakes on non-victims: a cross-sectional study. BMC Public Health25:597. doi: 10.1186/s12889-025-21901-6,
18
Connor K. M. Davidson J. R. (2003). Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress. Anxiety18, 76–82. doi: 10.1002/da.10113,
19
Dai W. Chen L. Lai Z. Li Y. Wang J. Liu A. (2016). The incidence of post-traumatic stress disorder among survivors after earthquakes: a systematic review and meta-analysis. BMC Psychiatry16:188. doi: 10.1186/s12888-016-0891-9,
20
Fong K. N. Law Y. M. Luo L. Zhao Z. E. Chen H. Ganesan B. et al . (2022). Post-traumatic stress disorder (PTSD) after an earthquake experience: a cross-sectional survey of Wenchuan earthquake victims with physical disabilities 10 years later. Int. J. Disaster Risk Reduct.80:103225. doi: 10.1016/j.ijdrr.2022.103225
21
Fu M. Hall B. J. Xi J. Guo J. (2021). Gender differences in trajectories of mental health symptoms among Chinese earthquake survivors. J. Psychiatr. Res.142, 117–124. doi: 10.1016/j.jpsychires.2021.07.034,
22
Güler A. Gül S. Yıldırım M. (2024). Social comparison, resilience, life satisfaction, depression, and anxiety among earthquake survivors in Turkey. Int. J. Disaster Risk Reduct.105:104426. doi: 10.1016/j.ijdrr.2024.104426
23
Heanoy E. Z. Brown N. R. (2024). Impact of natural disasters on mental health: evidence and implications. Healthcare (Basel)12:1812. doi: 10.3390/healthcare12181812,
24
Hisli Sahin N. Yilmaz B. Batigun A. (2011). Psychoeducation for children and adults after the Marmara earthquake: an evaluation study. Traumatology17, 41–49. doi: 10.1177/1534765610395624
25
Hosseinnejad M. Yazdi-Feyzabadi V. Hajebi A. Bahramnejad A. Baneshi R. Sarabi R. E. et al . (2022). Prevalence of posttraumatic stress disorder following the earthquake in Iran and Pakistan: a systematic review and meta-analysis. Disaster Med. Public Health Prep.16, 801–808. doi: 10.1017/dmp.2020.411,
26
Ikizer G. Karanci A. N. Doğulu C. (2016). Exploring factors associated with psychological resilience among earthquake survivors from Turkey. J. Loss Trauma21, 384–398. doi: 10.1080/15325024.2015.1108794
27
Kamphuis W. Delahaij R. Duel J. Geuze E. Vermetten E. (2021). The relationship between resilience resources and long-term deployment-related PTSD symptoms: a longitudinal study in Dutch veterans. Mil. Behav. Health9, 267–274. doi: 10.1080/21635781.2020.1864528
28
Kapci E. G. Uslu R. Turkcapar H. Karaoglan A. (2008). Beck depression inventory II: evaluation of the psychometric properties and cut-off points in a Turkish adult population. Depress. Anxiety25, E104–E110. doi: 10.1002/da.20371,
29
Kaplan V. Alkasaby M. Düken M. E. Kaçkin Ö. Riad A. (2024). The impact of earthquakes on women: assessing women's mental health in aftermath of the Kahramanmaraş-centred earthquake in Türkiye. J. Public Health (Oxf.)46, e510–e519. doi: 10.1093/pubmed/fdae059,
30
Karaırmak Ö. (2010). Establishing the psychometric qualities of the Connor–Davidson resilience scale (CD-RISC) using exploratory and confirmatory factor analysis in a trauma survivor sample. Psychiatry Res.179, 350–356. doi: 10.1016/j.psychres.2009.09.012,
31
Keldal G. (2015). Warwick-Edinburgh Mental İyi Oluş Ölçeği’nin Türkçe formu: geçerlik ve güvenirlik çalışması. J. Happiness Well-Being3, 103–115.
32
Khatri G. K. Tran T. D. Fisher J. (2019). Prevalence and determinants of symptoms of antenatal common mental disorders among women who had recently experienced an earthquake: a systematic review. BMC Psychiatry19:47. doi: 10.1186/s12888-018-1986-2,
33
Kizilhan J. I. Neumann J. Aslan S. Aladag E. Dogan A. Mese A. et al . (2024). Psychological impact of the earthquake 2023 in Turkey. Discov. Public Health21:71. doi: 10.1186/s12982-024-00198-7
34
Kongshøj I. L. L. Berntsen D. (2023). Is young age a risk factor for PTSD? Age differences in PTSD-symptoms after hurricane Florence. Traumatology29, 211–221. doi: 10.1037/trm0000389
35
Kun P. Tong X. Liu Y. Pei X. Luo H. (2013). What are the determinants of post-traumatic stress disorder: age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health127, 644–652. doi: 10.1016/j.puhe.2013.04.018,
36
Leiva-Bianchi M. Cornejo F. Fresno A. Rojas C. Serrano C. (2018). Effectiveness of cognitive-behavioural therapy for post-disaster distress in post-traumatic stress symptoms after Chilean earthquake and tsunami. Gac. Sanit.32, 291–296. doi: 10.1016/j.gaceta.2017.07.018,
37
Lok N. Bademli K. Uzun G. Selçuk Tosun A. (2025). Determinants of post-traumatic stress disorder in individuals rescued from rubble in the 2023 Kahramanmaraş earthquake: fear of death, hopelessness, and the meaning of life. Curr. Psychol.44, 14799–14808. doi: 10.1007/s12144-025-08217-9
38
Mao W. Agyapong V. I. (2021). The role of social determinants in mental health and resilience after disasters: implications for public health policy and practice. Front. Public Health9:658528. doi: 10.3389/fpubh.2021.658528,
39
McKinzie A. E. Clay-Warner J. (2021). The gendered effect of disasters on mental health: a systematic review. Int. J. Mass Emerg. Disasters39, 227–262. doi: 10.1177/028072702103900202
40
Norris F. H. Stevens S. P. Pfefferbaum B. Wyche K. F. Pfefferbaum R. L. (2008). Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. Am. J. Community Psychol.41, 127–150. doi: 10.1007/s10464-007-9156-6,
41
Oliva S. Lazzeretti L. (2019). “Adaptation, adaptability and resilience: the recovery of Kobe after the great Hanshin earthquake of 1995” in The role of art and culture for regional and urban resilience. (Eds.) PhilipC.LucianaL. (Abingdon, UK: Routledge), 67–87.
42
Prati G. Pietrantoni L. (2009). Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. J. Loss Trauma14, 364–388. doi: 10.1080/15325020902724271
43
Saltini A. Rebecchi D. Callerame C. Fernandez I. Bergonzini E. Starace F. (2018). Early eye movement desensitisation and reprocessing (EMDR) intervention in a disaster mental health care context. Psychol. Health Med.23, 285–294. doi: 10.1080/13548506.2017.1344255,
44
Şam M. Sever G. Yildiz Yüksel H. Aliyev R. (2025). Earthquake effects on youth: understanding psychological challenges and support needs. BMC Psychol.13:72. doi: 10.1186/s40359-025-02373-0,
45
Samanci Tekin C. Aydin G. (2024). Impacts of disasters on women: the case of Kahramanmaras earthquake sequence. Arch. Womens Ment. Health28, 795–804. doi: 10.1007/s00737-024-01543-0,
46
Satıcı S. A. Okur S. Deniz M. E. Karaağaç Z. G. Yılmaz F. B. Kütük H. et al . (2024). The development and initial validation of the earthquake fear scale: its links to personality traits, psychological distress, harmony in life, and mental wellbeing. Stress. Health40:e3306. doi: 10.1002/smi.3306,
47
Schwind J. S. Norman S. A. Brown R. Frances R. H. Koss E. Karmacharya D. et al . (2019). Association between earthquake exposures and mental health outcomes in Phulpingdanda Village after the 2015 Nepal earthquakes. Community Ment. Health J.55, 1103–1113. doi: 10.1007/s10597-019-00404-w,
48
Şenol Balaban M. Doğulu C. Akdede N. Akoğlu H. Karakayalı O. Yılmaz S. et al . (2025). Emergency response, and community impact after February 6, 2023 Kahramanmaraş Pazarcık and Elbistan earthquakes: reconnaissance findings and observations on affected region in Türkiye. Bull. Earthq. Eng.23, 1053–1081. doi: 10.1007/s10518-024-01867-3
49
Sirotich A. C. Camisasca E. (2024). PTSD risk factors in earthquake survivors and their families: a systematic review. Eur. J. Psychotraumatol.15:2365477. doi: 10.1080/20008066.2024.2365477,
50
Snijders C. Pries L. K. Sgammeglia N. Al Jowf G. Youssef N. A. De Nijs L. et al . (2018). Resilience against traumatic stress: current developments and future directions. Front. Psych.9:676. doi: 10.3389/fpsyt.2018.00676,
51
Tahernejad S. Ghaffari S. Ariza-Montes A. Wesemann U. Farahmandnia H. Sahebi A. (2023). Post-traumatic stress disorder in medical workers involved in earthquake response: a systematic review and meta-analysis. Heliyon.9:e12794. doi: 10.1016/j.heliyon.2023.e12794,
52
Tanrikulu A. B. Kayaoglu K. (2024). Prevalence and determinants of probable posttraumatic stress disorder among university students eight months after the 2023 Kahramanmaraş earthquake doublet. Dusunen Adam J. Psychiatr. Neurol. Sci.37, 102–110. doi: 10.14744/DAJPNS.2024.00245
53
Taşkın M. Kemal BAS Ucak EF (2025). Post-traumatic stress disorder (PTSD) in disaster survivors 1 year after the 2023 Kahramanmaraş earthquake in Turkey. Eur. J. Trauma Dissociation.9:100504. doi: 10.1016/j.ejtd.2025.100504
54
Tennant R. Hiller L. Fishwick R. Platt S. Joseph S. Weich S. et al . (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual. Life Outcomes5:63. doi: 10.1186/1477-7525-5-63,
55
Theron L. C. Theron A. M. (2014). Meaning-making and resilience: case studies of a multifaceted process. J. Psychol. Afr.24, 24–32. doi: 10.1080/14330237.2014.904099
56
Thompson N. J. Fiorillo D. Rothbaum B. O. Ressler K. J. Michopoulos V. (2018). Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J. Affect. Disord.225, 153–159. doi: 10.1016/j.jad.2017.08.049,
57
Tomak L. Demirel T. Demir I. (2024). Evaluation of the demographic characteristics and general health status of earthquake survivors affected by the 2023 Kahramanmaraş earthquake; a section from Gaziantep Nurdağı district. BMC Public Health24:937. doi: 10.1186/s12889-024-18444-7,
58
Ulusoy M. Sahin N. H. Erkmen H. (1998). Turkish version of the Beck anxiety inventory: psychometric properties. J. Cogn. Psychother.12, 163–172.
59
Ural A. Yalçın E. Aydın E. I. Akarsu R. H. (2024). Women's experiences in the aftermath of the Kahramanmaraş earthquakes in Türkiye: a phenomenological study. Int. J. Disaster Risk Reduct.110:104617. doi: 10.1016/j.ijdrr.2024.104617
60
Weathers F. W. Bovin M. J. Lee D. J. Sloan D. M. Schnurr P. P. Kaloupek D. G. et al . (2018). The clinician-administered PTSD scale for DSM–5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol. Assess.30, 383–395. doi: 10.1037/pas0000486,
61
Weinberg M. Besser A. Zeigler-Hill V. Neria Y. (2016). Bidirectional associations between hope, optimism and social support, and trauma-related symptoms among survivors of terrorism and their spouses. J. Res. Pers.62, 29–38. doi: 10.1016/j.jrp.2016.03.002
62
World Health Organization (2022). World mental health report: Transforming mental health for all. Geneva: World Health Organization.
63
Wu Z. Xu J. He L. (2014). Psychological consequences and associated risk factors among adult survivors of the 2008 Wenchuan earthquake. BMC Psychiatry14:126. doi: 10.1186/1471-244X-14-126,
64
Xi Y. Yu H. Yao Y. Peng K. Wang Y. Chen R. (2020). Post-traumatic stress disorder and the role of resilience, social support, anxiety and depression after the Jiuzhaigou earthquake: a structural equation model. Asian J. Psychiatr.49:101958. doi: 10.1016/j.ajp.2020.101958,
65
Yakşi N. Eroğlu M. (2024). Determinants of posttraumatic stress disorder (PTSD) among children and adolescents in the subacute stage of Kahramanmaraş earthquake, Turkey. Arch. Public Health82:199. doi: 10.1186/s13690-024-01434-x,
66
Yanardağ R. Tunç A. Dökme Yağar S. Yağar F. (2025). Life satisfaction, perception of loneliness and death anxiety of older adults living in container cities after the 2023 Kahramanmaraş earthquakes. J. Gerontol. Soc. Work., 1–15. doi: 10.1080/01634372.2025.2471986
67
Yayla M. E. Gümüştakim R. Ş. Ayhan Başer D. (2025). Quality of life and post-traumatic stress disorder among elderly earthquake survivors: a focus on the February earthquake in Turkey. Psychogeriatrics25:e13201. doi: 10.1111/psyg.13201,
68
Yılmaz H. Ö. Doğan G. (2025). Relationship among post-quake traumatic stress, insomnia, and eating behaviour: analysis of directly and indirectly affected individuals from the Kahramanmaraş (Türkiye) earthquake. Int. J. Environ. Health Res.35, 839–849. doi: 10.1080/09603123.2025.2453047,
69
Zhao L. He F. Zhao C. (2020). A framework of resilience development for poor villages after the Wenchuan earthquake based on the principle of “build back better.”. Sustainability12:4979. doi: 10.3390/su12124979
Summary
Keywords
Kahramanmaraş earthquakes, post-traumatic stress disorder, depression, anxiety, resilience, well-being
Citation
Yılmazer E (2025) Psychological distress, resilience, and well-being among survivors of the 2023 Kahramanmaraş earthquakes: a multi-site cross-sectional study. Front. Psychol. 16:1730083. doi: 10.3389/fpsyg.2025.1730083
Received
22 October 2025
Revised
21 November 2025
Accepted
25 November 2025
Published
10 December 2025
Volume
16 - 2025
Edited by
Francesca Pacitti, University of L'Aquila, Italy
Reviewed by
Abanoub Riad, Masaryk University, Czechia
Tommaso Barlattani, University of L'Aquila, Italy
Nurullah Yelboga, Sirnak University, Türkiye
Updates
Copyright
© 2025 Yılmazer.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eda Yılmazer, edayilmazer@beykoz.edu.tr
ORCID: Eda Yılmazer, orcid.org/0009-0009-3377-5025
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.