Abstract
Purpose:
This study aimed to assess the evidence of the association between positive psychological resources and quality of life in patients with cancer.
Methods:
Electronic searching was performed to retrieve articles from PubMed, Web of Science, Embase, CNKI, and CBM (from inception to 7 April 2022). Summary correlation coefficient (r) values were extracted from each study, and 95% CIs were calculated by the random-effect model. Subgroup and sensitivity analyses were performed to investigate potential heterogeneity.
Results:
In total, sixty-six articles were included in the present study. The pooled r for resilience was 0.71 (95%CI: 0.55, 0.87), hope 0.50 (95%CI: 0.43, 0.56), self-efficacy 0.53 (95%CI: 0.46, 0.61), self-esteem 0.46 (95%CI: 0.28, 0.63), and optimism 0.30 (95%CI: 0.19, 0.40). For subgroup analysis, no significant differences were found between minors and adults.
Conclusion:
This study indicated that resilience, hope, optimism, self-esteem, and self-efficacy were positively correlated with quality of life in patients with cancers. Therefore, intervention programs should be focused on increasing state-like positive psychological resources to improve the quality of life in patients with cancer.
Introduction
Cancer is ranked as the major cause of death in countries with both more and less economic development, which is the most important barrier to enhancing life expectancy. Although medical anti-cancer therapies, radiation, and surgical oncology have made great progress, these, in turn, threaten patients’ mental health and quality of life. Previous research has found that patients with cancer have a more difficult time dealing with negative emotions and have a lower quality of life during the disease-free survivor stage (Chen et al., 2018; MacDonald et al., 2021; Perez-Tejada et al., 2021). This may be due to side effects of aggressive cancer therapy, financial hardship, difficulties in accessing affordable health insurance, and limited employment opportunities (Park, 2005; Kirchhoff et al., 2011; Nipp et al., 2017; Miller et al., 2019). Ultimately, patients with cancers are vulnerable to threats to their physical and psychological well-being. However, a longitudinal study (Lam et al., 2010) found that patients with cancer with high levels of psychological adaptation coped better with adversity during the disease, had fewer psychiatric disorders, and had a higher quality of life. Therefore, increasingly studies thought that positive psychological resources could help explain individual variation in the quality of life in patients with cancer.
Positive psychological resources have been associated with increasing attention to the oncology field in the past 30 years. Positive psychological resources include many constructs. Several state-like positive psychological constructs have been identified in the fields of positive psychology and psycho-oncology (Bao et al., 2017; Pitichat et al., 2018). The most common state-like constructs are resilience, hope, optimism, self-esteem, and self-efficacy in the context of cancer (Yang et al., 2014, 2016). These constructs are individuals’ positive psychological state of development and ability to maintain or restore relatively stable psychological and physical function when confronted with life-threatening events (Seiler and Jenewein, 2019). Therefore, this study focused on the role of resilience, hope, optimism, self-esteem, and self-efficacy in improving the quality of life among patients with cancer. Several studies found that patients with cancer with a high level of resilience were more able to cope with disease adjustment and maintain mental health (Park, 2005; Lam et al., 2010; Nipp et al., 2017). Resilience is considered as a developable capability characterized by a relatively stable psychological trait that reduces, adapts to, and even overcomes the destructive impacts caused by adverse factors in the face of disasters or stressors and a certain promoting role in alleviating the negative impact of traumatic pressure on individuals and maintaining the normal psychological state of the body (Richardson, 2002).
Snyder (Snyder et al., 1991; Snyder, 2000) conceptualized hope as a positive motivational state based on an inactively deprived sense of successful agency (achieving goals by available will power and determination) and pathways (pursuing goals by creating alternative routines). Optimism is a psychological trait that is considered to the degree of the general expectation that positive outcomes will happen rather than bad things (Carver et al., 2010; Carver and Scheier, 2014). Compared with pessimists, research on optimism stated that optimists were capable of adapting to and dealing with the negative impacts of cancer by accepting the reality, placing the light and humor among patients with cancer (Thieme et al., 2017). Furthermore, several studies have confirmed that general self-efficacy has a bearing on adjustment and management of patients with cancer (Fang et al., 2017; Hinz et al., 2019). In the cancer context, self-efficacy is defined as a positive belief in individual competence to deal with cancer and behaviors that occur during dealing with a cancer diagnosis, cancer treatment, and transitioning to patients with cancer (Luszczynska et al., 2005; Chirico et al., 2017). Self-esteem refers to an individual’s subjective evaluation of their worth and is derived from a person’s perceptions of self-evaluation about their self-competence and efficacy (Carpenito, 2017).
Quality of life is generally considered a multidimensional concept that includes physical, psychological, and social well-being, feelings of health and symptoms associated with illness or treatment (Felce and Perry, 1995). Quality of life is usually assessed subjectively by the patient, and if this is impossible, the assessment may be made by a doctor, nurse, or caregiver. It has already been an important indicator that monitors the process of cancer treatment and prognosis or rehabilitation effect in the recent years (Ferrell et al., 1998). At present, an extensive body of research has found that positive psychological resources are associated with quality of life and well-being of patients with cancer. For instance, Li et al. (2016) found that hope and resilience were positively associated with quality of life in adult patients with bladder cancer. Besides, Chung et al. (2021) suggested that greater resilience was associated with better quality of life and lower depressive symptoms, and Ho et al. (2021) found that self-esteem was significantly related to health-related quality of life in childhood patients with cancer. Other studies reported that patients with cancer with a high level of optimism and self-efficacy were likely to experience greater QoL (Wong and Fielding, 2007; Chu et al., 2021). However, a small number of studies thought that positive self-esteem and self-efficacy were not associated with quality of life (Mystakidou et al., 2013; Tonsing and Ow, 2018), or the association between them was very weak (Thieme et al., 2017; Vidthya et al., 2019). This variability in the included studies may be due to differences in demographic variables of participants, disease characteristics, measuring methods, and study quality.
In summary, the present study aimed to conduct a meta-analytic review that investigated associations among resilience, hope, optimism, self-esteem, self-efficacy, and quality of life in patients with cancer.
Materials and Methods
Study Selection and Procedures
According to the PRISM statement (Page et al., 2021), the present meta-analysis was performed and reported. We conducted an electronic search to retrieve articles from PubMed, Web of Science, Embase, CNKI, and CBM (from inception to 7 April 2022). In addition, relevant references were included by screening manually, and language was not limited. Our meta-analysis used these search terms: neoplasms, tumor, cancer, quality of life, resilience, hope, optimism, self-efficacy, and self-esteem. The PubMed search strategy is detailed in the Supplementary Material. This study included these articles that explored the association of positive psychological resources with quality of life in patients with cancer. However, case reports, review articles, comments, and letters were excluded from our study. Besides, this study excluded duplicated publications on the same study participants.
The primary data of eligible articles were extracted by three authors independently. The included primary data were the name of the first author, the year of publication, study location, sample size, the mean age of participants, cancer types, and the measuring instruments of quality of life and positive psychological resources, and Spearman and Pearson’s correlation coefficient (r).
The Joanna Briggs Institute (JBI) guidelines (The Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party: Supporting Document for the Joanna Briggs Institute levels of Evidence and Grades of Recommendation, 2014) were used to assess the study’s quality. The JBI guidelines contain 10 items: the purpose of the study, sampling method, characteristic description, reliability and validity of the tool, authenticity of the information, ethical issues, statistical analysis, statement of results, and research value. It is scored from 0 to 2 (0 = “not meeting the requirements,” 1 = “mentioned but not described in detail,” 2 = “detailed and comprehensive description”), and the total score ranges from 0 to 20. When the literature score is > the maximum score of 70%, it can be considered that the study quality is relatively high. Two authors evaluated the study quality of included articles, and the third author solved disagreements in this meta-analysis.
Statistical Analysis
Heterogeneity was tested by the Q statistic (P < 0.05 = heterogeneity) and the inconsistency index (I2 > 50% = heterogeneity) (Higgins et al., 2003; Zamora et al., 2006; Leeflang et al., 2008), and publication was tested by the Egger method (Egger et al., 1997) (p < 0.05 = publication bias) and funnel plot (asymmetric plots = publication bias). A random-effect model was used rather than the fixed-effect model due to high heterogeneity (Wong and Fielding, 2007). Subgroup analysis was used to find whether effects were related to the factors as follows: participants’ group, the measuring instruments of quality of life, and positive psychological resources. In addition, sensitivity analysis was used to adjust for one possible atypical study.
R V4.0.2 was used to perform a meta-analysis in this study.
Results
Our meta-analysis retrieved 14,052 results. A total of 13,986 studies were excluded due to duplicate (5,700), review and meta-analysis (1,029), meeting (1,378), randomized controlled trial (1,208), and based on title and abstract (4,132) and full-text (510). Finally, there were 66 (Supplementary Material) articles that were included in this study (Figure 1). All the articles presented a clear research purpose, sufficient research basis, authentic information, correct statistical analysis method, appropriate and correct statement of analysis results, and research value. Only two articles adopted random sampling, and others used convenient sampling. We found that resilience, hope, optimism, and self-esteem were assessed by generic instruments in all included studies. As regards self-efficacy, ten out of 23 studies used specific instruments, including the Cancer Behavior Inventory (CBI), Cancer Survivors’ Self-Efficacy Scale (CSSES), Self-Efficacy Scale for Self-Management of Breast Cancer (SESSM-B), Symptom-Management Self-Efficacy Scale-Breast Cancer (SMSES-B), and Strategies Used by People to Promote Health (SUPPH). Besides, seven out of 66 studies involved minors. Cancer types mainly include breast, cervical, colorectal, lung, and prostate cancer. The sample size ranged from 39 to 953 (Table 1).
FIGURE 1
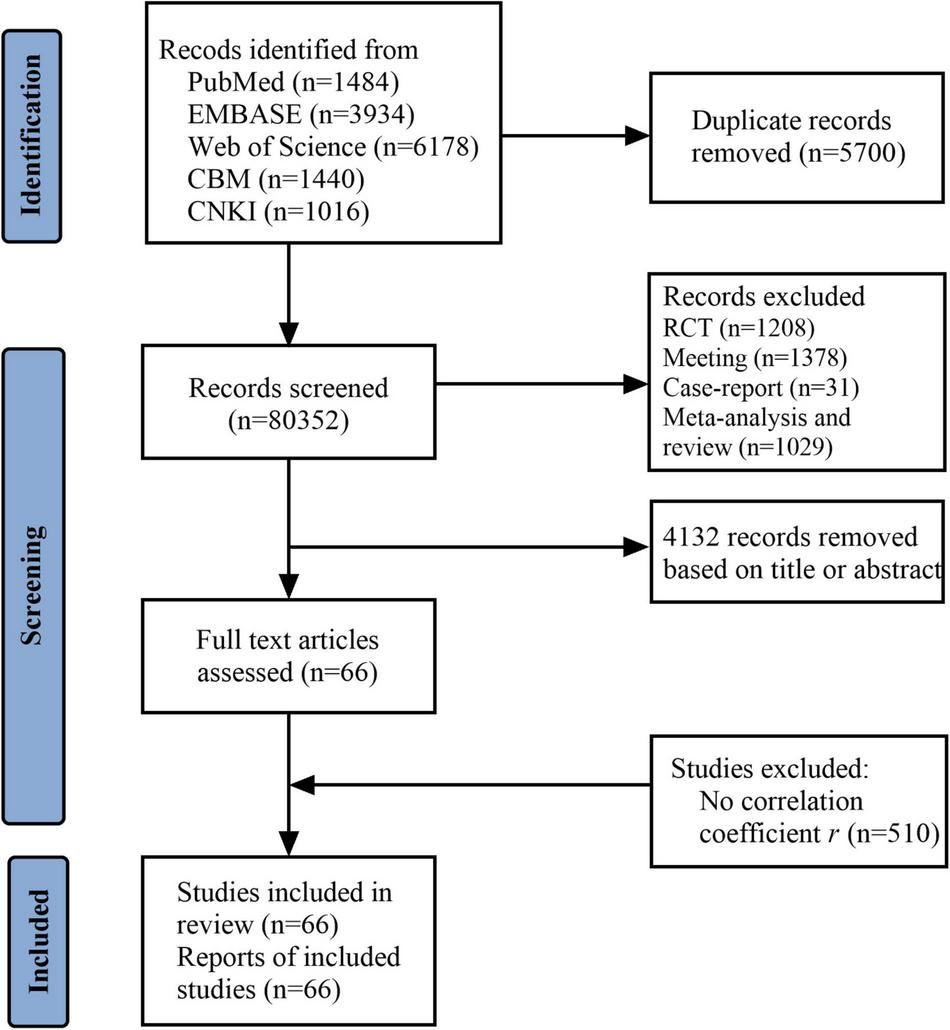
Study flow diagram.
TABLE 1
| Study | Location | Sample size | Mean age (year) | Cancer type | Positive psychological resources (PPR) | Instruments for assessing PPR | Instruments for assessing QoL | Study quality |
| Johansson et al., 2018 | Sweden | 39 | 71.7 | Colorectal | Self-efficacy | MFS | EORTC QLQ-C30 | 19 |
| Koch et al., 2017 | Germany | 40 | 49.2 | Breast | Self-esteem | RSES | FACT-B | 19 |
| Wu et al., 2015 | Taiwan | 40 | 16.4 | Mixed | Resilience | RS | MMOL-AF | 18 |
| Colby and Shifren, 2013 | United States | 51 | 58.47 | Breast | Optimism | LOT | FLIC | 18 |
| Haas, 2011 | United States | 73 | 60.12 | Breast | Self-efficacy | PAAI | MQOL | 19 |
| Maeir et al., 2022 | Israel | 73 | 50.85 | Mixed | Self-efficacy | NGSE | FACT-GP | 18 |
| Zheng and Pan, 2021 | China | 76 | 54.6 | Cervical | Self-efficacy | SUPPH | FACT-G | 18 |
| Mystakidou et al., 2013 | Greece | 90 | 61.17 | Breast | Self-efficacy | GSE | LASA | 18 |
| Finck et al., 2018 | Germany | 95 | 55.7 | Breast | Optimism | LOT | EORTC QLQ-C30 | 19 |
| Zhang et al., 2017 | China | 98 | 47.02 | Breast | Resilience | CD-RISC | FACT-B | 19 |
| Clarke et al., 2019 | United Kingdom | 98 | 64 | Head and neck | Resilience | CD-RISC | UW-QoL | 18 |
| Rammant et al., 2022 | United States | 99 | 63 | Bladder | self-efficacy | GSE | FACT-BI | 19 |
| Chen et al., 2019 | China | 100 | 45.65 | Cervical, endometrial, ovarian | Resilience | CD-RISC | FACT-G | 18 |
| Chu et al., 2021 | United States | 112 | 58.89 | Breast | Self-efficacy | CBI | FACT-G | 17 |
| Kwak et al., 2017 | South Korea | 115 | 11–18 | Mixed | Self-efficacy | SES | PedsQL 4.0 | 18 |
| Zhao and Wang, 2019 | China | 118 | 67.45 | Mixed | Resilience | RS-14 | FACT-G | 18 |
| Wan, 2021 | China | 119 | 45.4 | Breast | Resilience | CD-RISC | FACT-G | 19 |
| Liu et al., 2021 | China | 120 | 20–50 | Breast | Resilience | CD-RISC | FACT-G | 18 |
| Shen et al., 2020 | China | 121 | 47.01 | Breast | Hope, Self-efficacy | HHI, GSES | FACT-B | 17 |
| Zhong et al., 2019 | China | 124 | 49.54 | Breast | Resilience | CD-RISC | FACT-B | 19 |
| Sjoquist et al., 2013 | Australia | 126 | 62.1 | Ovarian | Hope | HHI | FACT-G | 18 |
| Li et al., 2019 | China | 128 | 46.89 | Breast | Resilience | CD-RISC | FACT-B | 18 |
| Tong, 2020 | China | 128 | 64.7 | Gastric | Self-efficacy | GSES | SQLI | 19 |
| Young et al., 2014 | South Korea | 129 | 52.09 | Breast | Resilience | RS | FACT-B | 18 |
| Liu, 2021 | China | 129 | 56.4 | Colorectal | Resilience | CD-RISC | FACT-G | 18 |
| Tonsing and Ow, 2018 | Singapore | 129 | 17.3 | Mixed | Self-esteem | RSES | QoL-CSS | 17 |
| Perez-Tejada et al., 2021 | Spain | 134 | 54.4 | Breast | Self-esteem | RSES | QLACS | 19 |
| Xu et al., 2021 | China | 134 | 52.6 | Breast | Resilience | CD-RISC | FACT-B | 18 |
| Choi et al., 2022 | South Korea | 136 | 58.8 | Gastric | Self-esteem | SES | QOL-CS | 18 |
| Chung et al., 2021 | Hong Kong | 138 | 10.6 | Leukemia or Brain tumor or Lymphoma | Resilience, self-esteem | RS-10, RSES | PedsOL 3.0 | 18 |
| Park et al., 2021 | South Korea | 140 | 48.9 | Breast | Self-efficacy | SESSM-B | FACT-B | 17 |
| Luo et al., 2022 | China | 146 | 6.2 | Mixed | Resilience | CD-RISC | SF-6D | 19 |
| Zhang et al., 2015 | China | 147 | 57.51 | Lung | Self-efficacy | SUPPH | FACT-L | 18 |
| Lee et al., 2001 | Taiwan | 150 | 44.8 | Breast | Self-esteem | RSES | OLI-cancer | 17 |
| Jiao et al., 2020 | China | 160 | 18 + | Colorectal | Resilience | CD-RISC | EORTC QLQ-C30 | 18 |
| Mazanec et al., 2010 | Frances | 163 | 58.24 | Mixed | Optimism | LOT | FACT-G | 17 |
| Zhao D. J. et al., 2020 | China | 172 | 57.3 | Lung | Resilience | CD-RISC | FACT-L | 18 |
| Ho et al., 2021 | Hong Kong | 176 | 12.56 | Mixed | Hope, self-esteem | HHI, RSES | PedsOL 4.0 | 19 |
| Hu et al., 2016 | China | 193 | 67.38 | Liver cancer | Hope | HHI | FACT-Hep | 17 |
| Ye et al., 2014 | China | 193 | 55.46 | Mixed | Hope | HHI | FACT-G | 18 |
| Sharif Nia et al., 2021 | Iran | 200 | 51.31 | Mixed | Hope | AHS | EORTC QLQ-C30 | 18 |
| Chin et al., 2021 | Taiwan | 201 | 53.6 | Breast | Self-efficacy | SMSES-B | EORTC QLQ-C30 | 19 |
| Groarke et al., 2020 | United Kingdom | 204 | 65.24 | Prostate | Resilience | CD-RISC | PORPUS-P | 18 |
| Bo et al., 2019 | South Korea | 204 | 54.2 | Mixed | Self-efficacy | CSSES | SF-36 | 18 |
| Wang et al., 2017 | China | 206 | 54.6 | Mixed | Self-efficacy | GSES | QOL-CS | 17 |
| Martins et al., 2018 | Portugal | 211 | 13.29 | Mixed | Hope | CHS | DCGM-12 | 19 |
| Yu et al., 2021 | China | 217 | 56.24 | Breast | Self-efficacy | SUPPH | FACT-B | 18 |
| Wu et al., 2013 | China | 224 | 47.54 | Breast | Hope | HHI | FACT-B | 17 |
| Zhang et al., 2020 | China | 230 | 56.13 | Oral | Hope | HHI | FACT-H&N | 19 |
| Zhou et al., 2022 | China | 231 | 48.15 | Breast | Resilience | CD-RISC | FACT-B | 18 |
| Zhao Y. Q. et al., 2020 | China | 237 | 18 + | Cervical | Self-efficacy | SUPPH | FACT-Cx | 18 |
| Yeung and Lu, 2014 | China | 238 | 55.7 | Mixed | Self-efficacy | CBI | QOL-CS | 17 |
| Gong et al., 2016 | China | 265 | 50.24 | Cervical | Hope | HHI | WHOQOL-BREF | 18 |
| Chen et al., 2017 | China | 273 | 46.91 | Breast | Resilience | CD-RISC | QOL-CS | 17 |
| He et al., 2019 | China | 284 | 49 | Lung, breast and liver | Resilience | CD-RISC | EORTC QLQ-C30 | 18 |
| McAteer and Gillanders, 2019 | United Kingdom | 286 | 67 | Prostate | Self-esteem | MSES | FACT-G | 19 |
| Sharour et al., 2019 | Jordan | 320 | 51.9 | Colorectal | Hope | HHI | FACT-C | 19 |
| Wong and Fielding, 2007 | Hong Kong | 334 | 64.66 | Lung | Optimism | LOT | FACT-G | 18 |
| Omran and Mcmillan, 2018 | United States | 341 | 57.9 | Mixed | Self-efficacy | CBI | MQOL-C | 18 |
| Thieme et al., 2017 | Germany | 354 | 61.2 | Breast and gynecological | Optimism, self-efficacy | LOT, GSES | EORTC QLQ-C30 | 17 |
| Li et al., 2016 | China | 365 | 63.76 | Bladder | Resilience, hope | RS-14, AHS | FACT-BL | 19 |
| Yuan et al., 2022 | China | 404 | 67.06 | Prostate | self-efficacy | GSES | FACT-P | 18 |
| Schofield et al., 2016 | Australia | 429 | 67 | Metastatic colorectal | Hope | SHS, LOT | EQ-5D | 18 |
| Li et al., 2021 | China | 450 | 47.76 | Breast | Hope | HHI | FACT-B | 17 |
| Chen et al., 2018 | China | 452 | 62.1 | Lung | Self-efficacy | GSES | SF-36 | 19 |
| Vidthya et al., 2019 | Malaysia | 953 | 46.45 | Mixed | Self-esteem | RSES | WHOQOL-BREF | 17 |
Characteristics of included studies.
AHS, Adult Hope Scale; CBI, Cancer Behavior Inventory; CD-RISC, Connor-Davidson resilience scale; CHS, Children’s Hope Scale; CSSES, Cancer Survivors’ Self-Efficacy Scale; GSE, General Self-efficacy beliefs Scale; HHI, Herth Hope Index; LOT, Life Orientation Test; MFS, Maintain Function Scale; MSES, Masculine Self-Esteem Scale; NGSE, New General Self-Efficacy Scale; PAAI, Physical Activity Assessment Inventory; RSES, Rosenberg Self-Esteem Scale; SES, Self-Efficacy-Scale; SESSM-B, Self-Efficacy Scale for Self-Management of Breast Cancer; SHS, State Hope Scale; SMSES-B, Symptom-Management Self-Efficacy Scale-Breast Cancer; SQLI, Spitzer Quality of Life Index; SUPPH, Strategies Used by People to Promote Health.
GCGM, DISABKIDS Chronic Generic Measure; EORTC QLQ, European Organization for Research and Treatment of Cancer quality of life, Questionnaire; EQ-5D, European Quality of Life-5 Dimensions; FACT-B, Functional Assessment of Cancer Therapy Breast cancer; FACT-BL, Functional Assessment of Cancer Therapy-Bladder; FACT-C, Functional Assessment of Cancer Therapy-Colorectal cancer; FACT-G, Functional Assessment of Cancer Therapy-General; FACT-H&N, Functional Assessment of Cancer Therapy-Head and Neck; FACT-Hep, Functional Assessment of Cancer Therapy-Hepatobiliary; FACT-L, Functional Assessment of Cancer Therapy-Lung; FLIC, Functional Living Index-Cancer; LASA, Linear Analog Scale Assessment; MMQL-AF, Minneapolis-Manchester Quality of Life Instrument-Adolescent Form; MQOL, McGill Quality of Life Questionnaire; MQOL-C, Multidimensional Quality of Life Scale-Cancer; PedsQL, Pediatric Quality-of-Life; QLACS, Quality of Life in Adult Cancer Survivors; QLI, Quality-of-Life Index; QOL-CS, Quality of Life-Cancer Survivors; SF, Short Form; UW-QoL, University of Washington quality of life; WHOQOL-BREF, World Health Organization’ s Quality of Life Questionnaire-Brief.
Resilience and Quality of Life
In total, twenty-one studies involving 3,310 patients with cancer examined the association of resilience with quality of life in patients with cancer. The meta-analysis of these studies found a large and significant overall effect size of r = 0.71 with CIs excluding zero (95%CI: 0.55, 0.87) (Figure 2). In addition, the results of the subgroup analysis indicated that the impact of resilience on quality of life was not different between minors (k = 3, r = 0.58, 95%CI: 0.40, 0.76) and adults (k = 18, r = 0.73, 95%CI: 0.54, 0.91) (Table 2 and Supplementary Figure A).
FIGURE 2
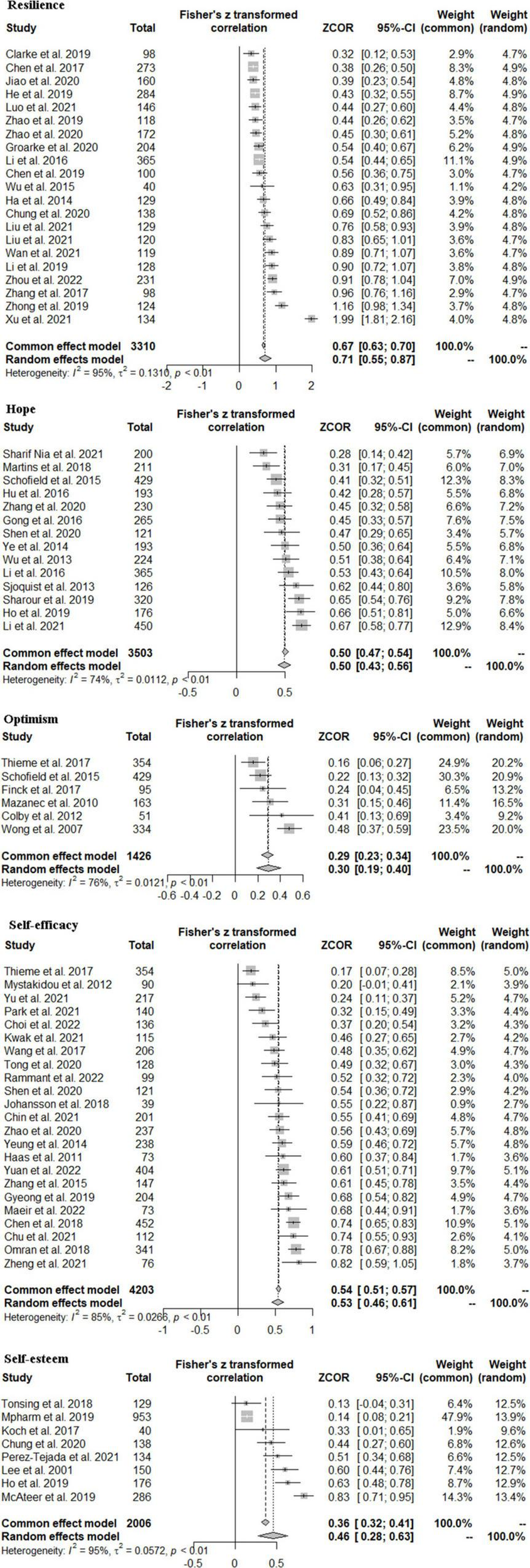
Effect sizes of the correlation between five positive psychological resources and quality of life.
TABLE 2
| Subgroup | k | r (95%CI) | I2 (%) | P-value |
| Resilience | ||||
| Participants | 0.251 | |||
| Minors | 3 | 0.58 (0.40, 0.76) | 58.0 | |
| Adults | 18 | 0.73 (0.54, 0.91) | 95.5 | |
| Hope | ||||
| Participants | 0.934 | |||
| Minors | 2 | 0.48 (0.14, 0.83) | 91.5 | |
| Adults | 12 | 0.50 (0.43, 0.56) | 70.9 | |
| Specific instruments for quality of life | 0.123 | |||
| No | 2 | 0.43 (0.35, 0.50) | 0.0 | |
| Yes | 12 | 0.51 (0.43, 0.58) | 75.2 | |
| Self-efficacy | ||||
| Specific instruments for self-efficacy | 0.228 | |||
| No | 13 | 0.49 (0.39, 0.59) | 85.5 | |
| Yes | 10 | 0.58 (0.47, 0.70) | 84.1 | |
| Specific instruments for quality of life | 0.053 | |||
| No | 4 | 0.52 (0.43, 0.60) | 53.4 | |
| Yes | 19 | 0.65 (0.54, 0.76) | 84.9 | |
| Self-esteem | ||||
| Participants | 0.659 | |||
| Minors | 3 | 0.40 (0.12, 0.69) | 89.1 | |
| Adults | 5 | 0.49 (0.24, 0.73) | 96.6 |
Correlations between positive psychological resources and quality of life in cancer patients: subgroup analysis.
Hope and Quality of Life
The meta-analysis of fourteen studies involving 3,503 patients with cancer, revealed a large and significant overall effect size of r = 0.50 with CIs excluding zero (95%CI: 0.43, 0.56) (Figure 2). In subgroup analysis, no differences were found between minors’ group (k = 2, r = 0.48, 95%CI: 0.14, 0.83) and adults’ group (k = 12, r = 0.50, 95%CI: 0.43, 0.56) (Table 2 and Supplementary Figure A). In addition, the results of subgroup analysis indicated that the impact of resilience based on a quality-of-life specific scale (k = 12, r = 0.51, 95%CI: 0.43, 0.58) was similar to studies based on a generic scale (k = 2, r = 0.43, 95%CI: 0.35, 0.50) (Table 2 and Supplementary Figure B).
Optimism and Quality of Life
In total, six studies, involving 1,426 patients with cancer, examined the relationship between self-esteem and quality of life, and yielded a significant and medium overall effect size of r = 0.30 with all CIs excluding zero (95%CI: 0.19, 0.40) (Figure 2) and thus statistically significant.
Self-Efficacy and Quality of Life
In total, twenty-three studies involving 4,203 patients with cancer examined the association between self-efficacy and quality of life. The current meta-analysis of these studies yielded a significant and large effect size of r = 0.53 with CIs excluding zero (95%CI: 0.46, 0.61) (Figure 2). Besides, there were no differences in instruments for assessing self-efficacy (p = 0.228) and quality of life (p = 0.053) (Table 2 and Supplementary Figures B,C).
Self-Esteem and Quality of Life
In total, eight studies, involving 2,006 patients with cancer, explored the relationship between self-esteem and quality of life and yielded a significant and medium overall effect size of r = 0.46 with confidence intervals excluding zero (95%CI: 0.28, 0.63) (Figure 2). Differences were not found between minor participants and adult participants (p = 0.659) (Table 2 and Supplementary Figure A).
Sensitivity Analysis and Publication Bias
Sensitivity analysis showed that all the pooled r for quality of life in patients with cancer were stable, which indicated that our results were reliable. The result of the Egger test indicated that there was no publication bias in this meta-analysis (resilience: p = 0.226; hope: p = 0.420; self-efficacy: p = 0.660). The Egger test of optimism and self-esteem was not analyzed due to the small number of studies (n < 10). Figure 3 presents the funnel plot.
FIGURE 3
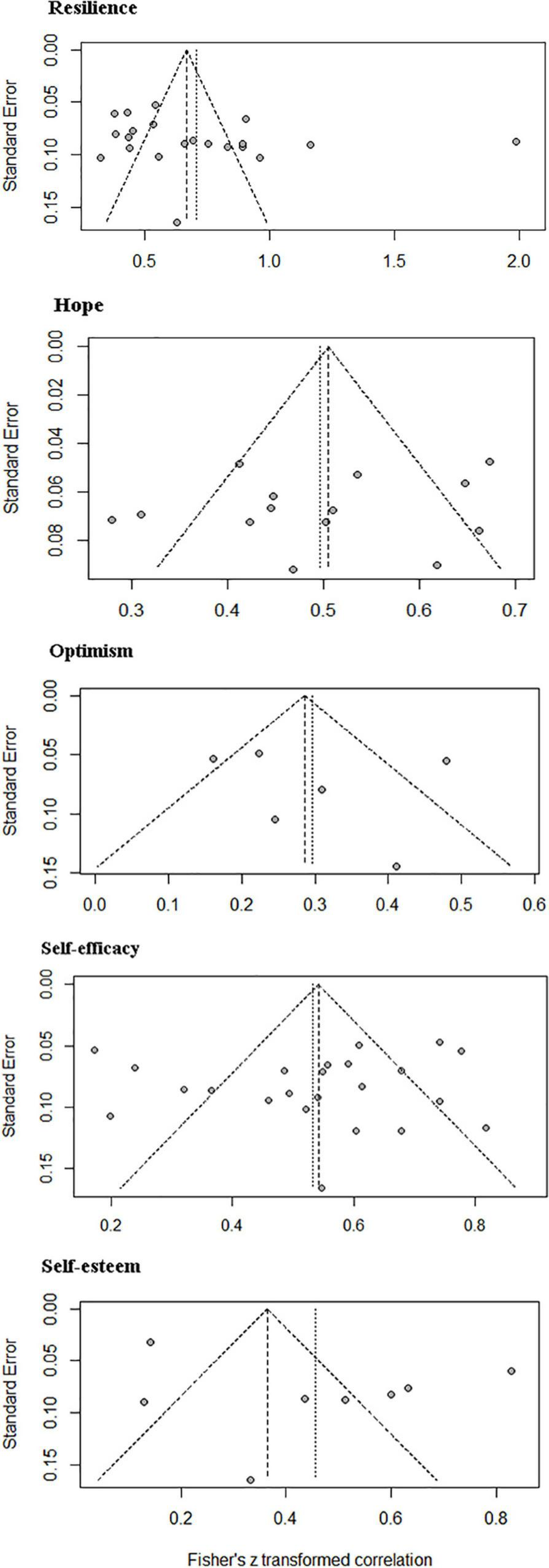
Publication bias based on the funnel plots.
Discussion
The present study aimed to conduct a meta-analysis of the empirical literature on the association of state-like positive psychological resources with quality of life among patients with cancer. The current study focused on five state-like positive psychological variables (resilience, hope, optimism, self-efficacy, and self-esteem) and quality of life of patients with cancer. The meta-analysis showed that quality of life of patients with cancer was positively and significantly associated with resilience, hope, optimism, self-efficacy, and self-esteem, which were consistent with previous studies (Wong and Fielding, 2007; Li et al., 2016; Chu et al., 2021; Chung et al., 2021; Ho et al., 2021).
Patients with cancer face multiple adversities within their illness, including both the physical impact of the disease, such as pain and discomfort, and treatment, as well as the psychological aspects of the knowledge of having a potentially life-threatening illness, which thereby causes poor quality of life during cancer treatment. Generally, resilience, hope, optimism, self-efficacy, and self-esteem are both stable, state-like positive psychological variables that can act as protective factors against adversity to improve quality of life. Protective factors are circumstances or attributes that help individuals deal more effectively with stressful events. These five state-like positive psychological constructs can act as protective factors against the subjective experience of hardship, specifically of receiving a potentially adverse cancer diagnosis. These variables may help patients with cancer overcome and/or become proactive in the context of cancer diagnosis and treatment by making patients more confident in coping with cancer, and less susceptible to negative mood states that negatively impact quality of life. These findings were supported by prior evidence (Coopersmith, 1967; Snyder et al., 1991; Martínez-Correa et al., 2006; Duggal et al., 2016).
Specifically, evidence suggests that high-resilient people strategically elicit positive emotions through the use of humor, relaxation techniques, and optimistic thinking to proactively cultivate their positive emotions (Tugade and Fredrickson, 2004). Then, positive emotionality emerges as the crucial element of resilience. A study found that resilience had an indirect impact on quality of life of patients with cancer by influencing social support (Zhang et al., 2017). According to this theory of Snyder, hope is conceptualized as a positive motivational state based on an interactively derived sense of successful agency (goal-directed energy) and pathways (planning to meet goals) (Snyder et al., 1991; Snyder, 2000). Rousseau (2000) found that hope could be developed by learning to control one’s symptoms, exploring one’s faith, and strengthening interpersonal relationships. Another study found that highly hopeful individuals reported significantly higher levels of personal adjustment and global life satisfaction, and less psychological distress (Gilman et al., 2006). An optimistic attitude plays a crucial role in effectively coping with disease diagnosis, treatment, prognosis, and in enhancing the quality of life (Rousseau, 2000). Furthermore, compared with pessimists, optimistic patients with cancer reported greater survival rates a year after diagnosis (Allison et al., 2003). Highly efficacious patients with cancer characterized by a sense of agency or control may perceive some causal relationship between coping behaviors executed and certain desired outcomes, including the level of the type of quality of life (Merluzzi et al., 2001). Andrea et al. conducted a meta-analysis involving 3,162 patients with cancer and found that there was a large significant overall effect size of r = 0.73 for the association of self-efficacy with quality of life (Chirico et al., 2017). Low self-esteem patients mean self-contempt, self-disappointment, self-rejection, and lack of self-respect for themselves. Based on the theory of Rosenberg (1965), a high level of self-esteem implies that they have high self-respect for who they are within limits, and do not assume that they are superior in any way to anyone else. A cancer diagnosis tends to affect the patients’ body image, which negatively causes changes in self-esteem. Even the easiest daily routine may be disrupted, and patients need to be aware of these long-term consequences that negatively influence their quality of life and mental health.
In this study, subgroup analysis indicated that no differences were found in participant groups (minors and adults), and measuring instruments (generic and specific instruments). However, these state-like variables and integration processes in patients with cancer are significantly different from those in other populations due to the complex treatment and potential fatality in the former. Moreover, the current evaluation scales are based on participants with depression and anxiety or the general population (Carver et al., 2010; Carver and Scheier, 2014). For instance, the Connor Davidson Resilience Scale (CD-RISC) was developed based on a sample with anxiety symptoms. In this study, only self-efficacy was used with specific instruments to assess the level of self-efficacy in patients with cancer. Therefore, it is crucial to develop scales specifically for patients with cancer to gauge their mental health with greater reliability. Besides, most studies investigated the effect of optimism on quality of life in adult patients with cancer, but few studies examined the association between children and adolescent patients. Hence, future studies can benefit from examining the impact of optimism on the quality of life in minors with cancer.
Limitations
The present meta-analysis has some limitations. At first, there is a dearth of longitudinal studies on positive psychological resources and quality of life among patients with cancer. Although a cross-sectional study is easier to be performed, a longitudinal study is more valuable in terms of answering questions concerning the long-term relations between positive psychological resources and quality of life in patients with cancer. Second, the subgroup analysis of the children or adolescent group and the adult group could not be performed for every meta-analysis in this study due to the limited number of studies concerning the association of self-efficacy and optimism with quality of life among patients with cancer. Therefore, there is a need for additional research on the impact of self-efficacy and optimism on quality of life in children or adolescents with cancer. Besides, although this study has investigated each positive psychological resource individually, it is significant to recognize that some positive psychological variables may co-vary. For instance, highly hopeful individuals tend to effectively buffer the impact of stressful and negative life events, and successfully reach their end goals, so they possess more resilience (Ong et al., 2006). Thus, hope might trump the effects of resilience on quality of life. Besides, the optimistic attitude inherent in hopeful individuals plays a crucial role in improving health-related quality of life. Therefore, further research needs to examine their covariation and unique and interactive relation with quality of life among patients with cancer. Finally, most studies were written in English in this study, which may lead to language bias. However, Thornton and Lee thought that there was a similar bias in all meta-analyses that did not review all studies. Therefore, despite, this limitation, this study’s outcomes are reliable and warranted.
Clinical Implications
Although these five stake-like variables are defined in different models, they may affect mental health and quality of life among patients with cancer by different mechanisms, these variables have two significant points in common. Namely, these constructs are positive coping with styles or protective factors to fight cancers and they are dynamic and developmental resources. Therefore, these variables could be increased through intervention to better improve the quality of life in patients with cancer. Furthermore, increasing research has found that interventions based on positive psychological resources could cope with mental problems and enhance the quality of life in patients with cancer. For example, in a randomized and controlled trial, Promoting Resilience in Stress Management (PRISM), a psychosocial intervention for adolescents and young adults with cancer, enhances resilience resources via four skills-based training sessions, compared with the usual care (UC) may improve health-related quality of life, especially in psychosocial domains of well-being (Steineck et al., 2019). Berg et al. (2020) developed and tested Achieving Wellness After Kancer in Early life (AWAKE), a scalable 8-week app-based program consisting of educational videos, mood/activity tracking, and telephone-based coaching to promote hope and quality of life in young adult cancer survivors, which evidence that the AWAKE supports patients cope with cancer-related sequelae and reestablish goals across life domains after experiencing cancer. Evidence suggests that nurse-administered self-efficacy interventions given on five monthly occasions and designed to enhance patients’ self-care self-efficacy have significantly higher scores on quality of life and self-care self-efficacy than the control group and significantly less symptom distress (Lev et al., 2001). Besides, beauty care interventions (Richard et al., 2019) and Framed Portrait Experience interventions (Saita and Acquati, 2020) are similar to enhancing self-esteem and self-efficacy among patients with cancer. Therefore, interventions based on state-like positive psychological constructs should be emphasized and developed in the field of oncology psychology to enhance the quality of life.
Conclusion
The current meta-analysis provided a comprehensive summary of the current literature on state-like positive psychological constructs and quality of life in patients with cancer. Results of this study indicated that state-like variables, including resilience, hope, optimism, self-esteem, and self-efficacy were positively correlated with quality of life in patients with cancer. Therefore, intervention programs should be focused on increasing state-like positive psychological resources to improve the quality of life in patients with cancer.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The original contributions presented in this study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
XZ searched databases, selected studies, extracted information, assessed study quality, analyzed data, drafted, and revised manuscript. ST contributed to study selection, data extraction, and quality assessment. XZ and YY assessed study and revised manuscript. YY conceived the hypothesis, developed the study methods, and revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.883157/full#supplementary-material
References
1
AllisonP. J.GuichardC.FungK.GilainL. (2003). Dispositional optimism predicts survival status 1 year after diagnosis in head and neck cancer patients.J. Clin. Oncol.21543–548. 10.1200/JCO.2003.10.092
2
BaoY.LiL.GuanY.WangW.LiuY.WangP.et al (2017). Prevalence and associated positive psychological variables of anxiety and depression among patients with central nervous system tumors in China: a cross-sectional study.Psychooncology26262–269. 10.1002/pon.4128
3
BergC. J.VanderpoolR. C.GetachewB.PayneJ. B.JohnsonM. F.SandridgeY.et al (2020). A Hope-Based Intervention to Address Disrupted Goal Pursuits and Quality of Life Among Young Adult Cancer Survivors.J. Cancer Educ.351158–1169. 10.1007/s13187-019-01574-7
4
BoG. L.LeeT. S.KimS. H. (2019). Mediation effect of self-efficacy on the relationship between perceived self-management support and health-related quality of life among cancer survivors. J. Korean Acad. Nurs.49, 298–306. 10.4040/jkan.2019.49.3.298
5
CarpenitoL. J. (2017). Nursing Diagnosis: Application to Clinical Practice, 15th Edn. Philadelphia, PA: Wolters Kluwer.
6
CarverC. S.ScheierM. F. (2014). Dispositional optimism.Trends Cogn. Sci.18293–299.
7
CarverC. S.ScheierM. F.SegerstromS. C. (2010). Optimism.Clin. Psychol. Rev.30879–889.
8
ChenH. L.LiuK.YouQ. S. (2018). Self-efficacy, cancer-related fatigue, and quality of life in patients with resected lung cancer.Eur. J. Cancer Care27:e12934. 10.1111/ecc.12934
9
ChenH. P.GaoL. L.JiangM. T.ZhengX. (2019). The correlation research on resilience and the quality of life among postoperative patients with gynecological malignant oncology in chemotherapy. J. Nurs. Adm.19, 799–802.
10
ChenY. M.YangY. X.YanS. Y.DingX. Y.YaoH.YaoJ. P. (2017). Correlation between symptom distress, resilience and life quality in patients with breast cancer undergoing chemotherapy. Ningxia Med. J.39.
11
ChinC. H.TsengL. M.ChaoT. C.WangT. J.WuS. F.LiangS. Y. (2021). Self-care as a mediator between symptom-management self-efficacy and quality of life in women with breast cancer. PLoS One16:e0246430. 10.1371/journal.pone.0246430
12
ChiricoA.LucidiF.MerluzziT.AliverniniF.LaurentiisM.BottiG.et al (2017). A meta-analytic review of the relationship of cancer coping self-efficacy with distress and quality of life.Oncotarget836800–36811. 10.18632/oncotarget.15758
13
ChoiJ.KimS.ChoiM.HyungW. J. (2022). Factors affecting the quality of life of gastric cancer survivors. Support. Care Cancer30, 3215–3224. 10.1007/s00520-021-06683-y
14
ChuQ.WongC. C. Y.ChenL.ShinL. J.ChenL.LuQ. (2021). Self-stigma and quality of life among Chinese American breast cancer survivors: a serial multiple mediation model.Psychooncology30392–399. 10.1002/pon.5590
15
ChungJ. O. K.LiW. H. C.CheungA. T.HoL. L. K.XiaW.ChanG. C. F.et al (2021). Relationships among resilience, depressive symptoms, self-esteem, and quality of life in children with cancer.Psychooncology30194–201. 10.1002/pon.5548
16
ClarkeG.AsieduY. A.HerdK.SharmaS. (2019). Exploring the relation between patients’ resilience and quality of life after treatment for cancer of the head and neck. Br. J. Oral Maxillofac. Surg.57, 1044–1048. 10.1016/j.bjoms.2019.09.007
17
ColbyD. A.ShifrenK. (2013). Optimism, mental health, and quality of life: a study among breast cancer patients. Psychol. Health Med.18, 10–20. 10.1080/13548506.2012.686619
18
CoopersmithS. (1967). The Antecedents of Self-Esteem.San Francisco: W. H. Freeman and Company.
19
DuggalD.Sacks-ZimmermanA.LibertaT. (2016). The Impact of Hope and Resilience on Multiple Factors in Neurosurgical Patients.Cureus8:e849. 10.7759/cureus.849
20
EggerM.Davey SmithG.SchneiderM.MinderC. (1997). Bias in meta-analysis detected by a simple, graphical test.Bmj315629–634.
21
FangY.MingjunW.PengqiongL.YuqianS.YiC.XiuhuiZ.et al (2017). Effects of Self-efficacy and Hope on Posttraumatic Stress Disorder of Breast Cancer Inpatients.Revista De La Facultad De Ingenieria3291–94.
22
FelceD.PerryJ. (1995). Quality of life: its definition and measurement.Res. Dev. Disabil.1651–74.
23
FerrellB. R.GrantM.FunkB.Otis-GreenS.GarciaN. (1998). Quality of life in breast cancer. Part II: Psychological and spiritual well-being.Cancer Nurs.211–9. 10.1097/00002820-199802000-00001
24
FinckC.BarradasS.ZengerM.HinzA. (2018). Quality of life in breast cancer patients: associations with optimism and social support. Int. J. Clin. Health Psychol.18, 27–34. 10.1016/j.ijchp.2017.11.002
25
GilmanR.DooleyJ.FlorellD. (2006). Relative Levels of Hope and Their Relationship With Academic and Psychological Indicators Among Adolescents.J. Soc. Clin. Psychol.25166–178.
26
GongP. F.XiaB. R.LouG.WangW. B.ZhangL. Y.TianX.et al (2016). Mediating effect of hope level on correlation between perceived social support and quality of life among postoperative cervical cancer patients. Chin. J. Public Health32, 965–967. 10.11847/zgggws2016-32-07-23
27
GroarkeA.CurtisR.SkeltonJ.GroarkeJ. M. (2020). Quality of life and adjustment in men with prostate cancer: interplay of stress, threat and resilience. PLoS One15:e0239469. 10.1371/journal.pone.0239469
28
HaasB. K. (2011). Fatigue, self-efficacy, physical activity, and quality of life in women with breast cancer. Cancer Nurs.34, 322–334. 10.1097/NCC.0b013e3181f9a300
29
HeY. J.WangD. M.MaZ. Y. (2019). The association between mindfulness and quality of life in cancer patients: mediating role of resilience. J. MuDanJiang Med. Univ.40, 127–129.
30
HigginsJ. P.ThompsonS. G.DeeksJ. J.AltmanD. G. (2003). Measuring inconsistency in meta-analyses.Bmj327557–560. 10.1136/bmj.327.7414.557
31
HinzA.FriedrichM.KuhntS.ZengerM.SchulteT. (2019). The influence of self-efficacy and resilient coping on cancer patients’ quality of life.Eur. J. Cancer Care28:e12952. 10.1111/ecc.12952
32
HoL.LiW.CheungA. T.HoE.LamK.ChiuS. Y.et al (2021). Relationships among hope, psychological well-being and health-related quality of life in childhood cancer survivors.J. Health Psychol.261528–1537. 10.1177/1359105319882742
33
HuS. H.WangW. L.ZuoX. F.ZhangZ. H.ZhangC. J.RenC. X. (2016). Mediating effect of aspiration level on the relationship between family function and quality of life among elderly patients with hepatocellular carcinoma. Chin. J. Clin. Psychol.24.
34
JiaoT. T.LiL.WangZ. X. (2020). Correlation between resilience and quality of life in patients with colon cancer. Today Nurse27, 15–17.
35
JohanssonA. C.BrinkE.CliffordsonC.AxelssonM. (2018). The function of fatigue and illness perceptions as mediators between self-efficacy and health-related quality of life during the first year after surgery in persons treated for colorectal cancer. J. Clin. Nurs.27, e1537–e1548. 10.1111/jocn.14300
36
KirchhoffA. C.KrullK. R.NessK. K.ParkE. R.OeffingerK. C.HudsonM. M.et al (2011). Occupational outcomes of adult childhood cancer survivors: A report from the childhood cancer survivor study.Cancer1173033–3044. 10.1002/cncr.25867
37
KochA. K.RabsilberS.LaucheR.KümmelS.DobosG.LanghorstJ.et al (2017). The effects of yoga and self-esteem on menopausal symptoms and quality of life in breast cancer survivors-A secondary analysis of a randomized controlled trial. Maturitas105, 95–99. 10.1016/j.maturitas.2017.05.008
38
KwakY.KimY.ChoiE. S.ImH. J. (2021). Self-efficacy, post-traumatic growth, and quality of life of pediatric cancer survivors: a cross-sectional study. Eur. J. Oncol. Nurs.54:102019. 10.1016/j.ejon.2021.102019
39
LamW. W.BonannoG. A.ManciniA. D.HoS.ChanM.HungW. K.et al (2010). Trajectories of psychological distress among Chinese women diagnosed with breast cancer.Psychooncology191044–1051. 10.1002/pon.1658
40
LeeH. L.KuN. P.DowW. J.PaiL. (2001). Factors related to quality of life in breast cancer patients receiving chemotherapy. J. Nurs. Res.9, 57–68. 10.1097/01.jnr.0000347563.99811.ed
41
LeeflangM. M. G.DeeksJ. J.GatsonisC.BossuytP. M. M. (2008). Systematic Reviews of Diagnostic Test Accuracy.ACP J. Club149889–897.
42
LevE. L.DaleyK. M.ConnerN. E.ReithM.FernandezC.OwenS. V. (2001). An intervention to increase quality of life and self-care self-efficacy and decrease symptoms in breast cancer patients.Sch. Inq. Nurs. Pract.15277–294.
43
LiM. Y.YangY. L.LiuL.WangL. (2016). Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: a cross-sectional study.Health Qual. Life Outcomes14:73. 10.1186/s12955-016-0481-z
44
LiT. X.TanH. H.ChenY.JiangJ. F.XiongM. (2019). Analysis the relationship between psychological resilience and quality of life and its influencing factors in breast cancer patients during postoperative chemotherapy. Oncol. Prog.17, 2343–2347.
45
LiY.ZhouZ.NiN.LiJ.LuanZ.PengX. (2021). Quality of life and hope of women in China receiving chemotherapy for breast cancer. Clin. Nurs. Res.14:10547738211046737.
46
LiuF.PangJ. M.WangX. Y.WangY. (2021). The mediating effect of psychological resilience of breast cancer patients on reproductive concern and quality of life. Mod. Clin. Nurs.20, 7–12.
47
LiuG. L. (2021). Correlation between psychological resilience and quality of life in patients with rectal cancer after radiotherapy. Med. High. Vocat. Educ. Mod. Nurs.4, 522–526.
48
LuoY. H.LiW. H. C.CheungA. T.HoL. L. K.XiaW.HeX. L.et al (2022). Relationships between resilience and quality of life in parents of children with cancer. J. Health Psychol.27, 1048–1056. 10.1177/1359105321990806
49
LuszczynskaA.ScholzU.SchwarzerR. (2005). The general self-efficacy scale: multicultural validation studies.J. Psychol.139439–457. 10.3200/JRLP.139.5.439-457
50
MacDonaldC.TheurerJ. A.FungK.YooJ.DoyleP. C. (2021). Resilience: an essential element in head and neck cancer survivorship and quality of life.Support Care Cancer293725–3733. 10.1007/s00520-020-05873-4
51
MaeirT.NahumM.MakranzC.TsabariS.PeretzT.GilboaY. (2022). Predictors of quality of life among adults with self-reported cancer related cognitive impairment. Disabil. Rehabil.1–7. 10.1080/09638288.2022.2050954
52
MartinsA. R.CrespoC.SalvadorÁ.SantosS.CaronaC.CanavarroM. C. (2018). Does hope matter? Associations among self-reported hope, anxiety, and health-related quality of life in children and adolescents with cancer. J. Clin. Psychol. Med. Settings25, 93–103. 10.1007/s10880-018-9547-x
53
Martínez-CorreaA.Reyes del PasoG. A.García-LeónA.González-JareñoM. I. (2006). [Relationship between dispositional optimism/pessimism and stress coping strategies].Psicothema1866–72.
54
MazanecS. R.DalyB. J.DouglasS. L.LipsonA. R. (2010). The relationship between optimism and quality of life in newly diagnosed cancer patients. Cancer Nurs.33, 235–243. 10.1097/NCC.0b013e3181c7fa80
55
McAteerG.GillandersD. (2019). Investigating the role of psychological flexibility, masculine self-esteem and stoicism as predictors of psychological distress and quality of life in men living with prostate cancer. Eur. J. Cancer Care28:e13097. 10.1111/ecc.13097
56
MerluzziT. V.NairnR. C.HegdeK.Martinez SanchezM. A.DunnL. (2001). Self-efficacy for coping with cancer: revision of the Cancer Behavior Inventory (version 2.0).Psychooncology10206–217. 10.1002/pon.511
57
MillerK. D.NogueiraL.MariottoA. B.RowlandJ. H.YabroffK. R.AlfanoC. M.et al (2019). Cancer treatment and survivorship statistics, 2019.CA Cancer J. Clin.69363–385. 10.3322/caac.21565
58
MystakidouK.TsilikaE.ParpaE.GogouP.PanagiotouI.VassiliouI.et al (2013). Relationship of general self-efficacy with anxiety, symptom severity and quality of life in cancer patients before and after radiotherapy treatment.Psychooncology221089–1095. 10.1002/pon.3106
59
NippR. D.KirchhoffA. C.FairD.RabinJ.HylandK. A.KuhlthauK.et al (2017). Financial Burden in Survivors of Childhood Cancer: A Report From the Childhood Cancer Survivor Study.J. Clin. Oncol.353474–3481. 10.1200/JCO.2016.71.7066
60
OmranS.McmillanS. (2018). Symptom severity, anxiety, depression, self- efficacy and quality of life in patients with cancer. Asian Pac. J. Cancer Prev.19, 365–374. 10.22034/APJCP.2018.19.2.365
61
OngA. D.EdwardsL. M.BergemanC. S. (2006). Hope as a source of resilience in later adulthood.Personal. Ind. Differ.411263–1273.
62
PageM. J.McKenzieJ. E.BossuytP. M.BoutronI.HoffmannT. C.MulrowC. D.et al (2021). Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement.J. Clin. Epidemiol.134103–112. 10.1016/j.jclinepi.2021.02.003
63
ParkE. R. (2005). Health insurance coverage in survivors of childhood cancer: the Childhood Cancer Survivor Study.J. Clin. Oncol.239187–9197. 10.1200/JCO.2005.01.7418
64
ParkJ. H.JungY. S.KimJ. Y.BaeS. H. (2021). Determinants of quality of life in women immediately following the completion of primary treatment of breast cancer: a cross-sectional study. PLoS One16:e0258447. 10.1371/journal.pone.0258447
65
Perez-TejadaJ.Aizpurua-PerezI.LabakaA.VegasO.UgartemendiaG.ArregiA. (2021). Distress, proinflammatory cytokines and self-esteem as predictors of quality of life in breast cancer survivors.Physiol. Behav.230:113297. 10.1016/j.physbeh.2020.113297
66
PitichatT.ReichardR. J.Kea-EdwardsA.MiddletonE.NormanS. M. (2018). Psychological Capital for Leader Development.J. Leader. Organ. Stud.2547–62.
67
RammantE.LeungT. M.GoreJ. L.BerryD.GivenB.LeeC. T.et al (2022). Associations of self-efficacy, social support and coping strategies with health-related quality of life after radical cystectomy for bladder cancer: a cross-sectional study. Eur. J. Cancer Care18:e13571. 10.1111/ecc.13571
68
RichardA.HarbeckN.WuerstleinR.WilhelmF. H. (2019). Recover your smile: Effects of a beauty care intervention on depressive symptoms, quality of life, and self-esteem in patients with early breast cancer.Psychooncology28401–407. 10.1002/pon.4957
69
RichardsonG. E. (2002). The metatheory of resilience and resiliency.J. Clin. Psychol.58307–321.
70
RosenbergM. (1965). Society and the adolescent self-image. Soc. Forces3, 255–256.
71
RousseauP. (2000). Hope in the terminally ill.West J. Med.173117–118.
72
SaitaE.AcquatiC. (2020). Evaluating the Framed Portrait Experience as an Intervention to Enhance Self-Efficacy and Self-Esteem in a Sample of Adolescent and Young Adult Cancer Survivors: Results of a Pilot Study.J. Adolesc. Young Adult Oncol.9111–114. 10.1089/jayao.2019.0063
73
SchofieldP. E.StocklerM. R.ZanninoD.TebbuttN. C.PriceT. J.SimesR. J.et al (2016). Hope, optimism and survival in a randomised trial of chemotherapy for metastatic colorectal cancer. Support. Care Cancer24, 401–408.
74
SeilerA.JeneweinJ. (2019). Resilience in cancer patients.Front. Psychiatry10:208. 10.3389/fpsyt.2019.00208
75
Sharif NiaH.LehtoR. H.SeyedfatemiN.MohammadinezhadM. (2021). A path analysis model of spiritual well-being and quality of life in Iranian cancer patients: a mediating role of hope. Support. Care Cancer29, 6013–6019. 10.1007/s00520-021-06172-2
76
SharourL. A.OmariO. A.SalamehA. B.YehiaD. (2019). Health-related quality of life among patients with colorectal cancer. J. Res. Nurs.25114–125. 10.1177/1744987119846177
77
ShenA.QiangW.WangY.ChenY. (2020). Quality of life among breast cancer survivors with triple negative breast cancer–role of hope, self-efficacy and social support. Eur. J. Oncol. Nurs.46:101771. 10.1016/j.ejon.2020.101771
78
SjoquistK. M.FriedlanderM. L.O’ConnellR. L.VoyseyM.KingM. T.StocklerM. R.et al (2013). Hope, quality of life, and benefit from treatment in women having chemotherapy for platinum-resistant/refractory recurrent ovarian cancer: the gynecologic cancer intergroup symptom benefit study. Oncologist18, 1221–1228. 10.1634/theoncologist.2013-0175
79
SnyderC. R. (2000). “There is Hope,” in Handbook of Hope Theory, Measures and Applications, ed.SnyderC. R. (San Diego, CA: Academic Press), 3–21.
80
SnyderC. R.IrvingL. M.AndersonJ. R. (1991). “Hope and Health,” in Handbook of Social and Clinical Psychology: The Health Perspective, edsSnyderC. R.ForsythD. R. (New York: Pergamon Press).
81
SteineckA.BradfordM. C.LauN.ScottS.Yi-FrazierJ. P.RosenbergA. R. (2019). A Psychosocial Intervention’s Impact on Quality of Life in AYAs with Cancer: A Post Hoc Analysis from the Promoting Resilience in Stress Management (PRISM) Randomized Controlled Trial.Children6:124. 10.3390/children6110124
82
The Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party: Supporting Document for the Joanna Briggs Institute levels of Evidence and Grades of Recommendation (2014). The Joanna Briggs Institute. Available online at: https://jbi.global/grade/support(accessed January, 2014).
83
ThiemeM.EinenkelJ.ZengerM.HinzA. (2017). Optimism, pessimism and self-efficacy in female cancer patients.Jpn. J. Clin. Oncol.47849–855. 10.1093/jjco/hyx079
84
TongX. J. (2020). Mediating and regulating effects of self-efficacy on health literacy and quality of life in patients with gastric cancer undergoing chemotherapy. World Chin. J. Digestol.28, 167–171.
85
TonsingK. N.OwR. (2018). Quality of Life, Self-Esteem, and Future Expectations of Adolescent and Young Adult Cancer Survivors.Health Soc. Work4315–21. 10.1093/hsw/hlx047
86
TugadeM. M.FredricksonB. L. (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences.J. Pers. Soc. Psychol.86320–333. 10.1037/0022-3514.86.2.320
87
VidthyaS.SherinaM. S.RampalL.FadhilahS. I.UmmavathyP. (2019). Self-esteem among cancer patients receiving chemotherapy in selected.Med. J. Malaysia74405–412.
88
WanM. (2021). Correlation and influencing factors of psychological resilience and quality of life in patients with breast cancer during chemotherapy. Med. Innov. China18, 142–145.
89
WangQ.ZhangX. Q.WangQ. P. (2017). The specialties of illness perception, and its connection with self-efficacy and quality of life in cancer chemotherapy patients. Anhui Med. Pharm. J.21, 1538–1541.
90
WongW. S.FieldingR. (2007). Quality of life and pain in Chinese lung cancer patients: Is optimism a moderator or mediator?Qual. Life Res.1653–63. 10.1007/s11136-006-9106-z
91
WuJ.WuS. Q.XiongW. J.LvL. H.JiangJ.LuoJ.et al (2013). Correlation between quality of life and hope, coping style in breast cancer patients. Pract. Prev. Med.20.
92
WuW. W.TsaiS. Y.LiangS. Y.LiuC. Y.JouS. T.BerryD. L. (2015). The mediating role of resilience on quality of life and cancer symptom distress in adolescent patients with cancer. J. Pediatr. Oncol. Nurs.32, 304–313. 10.1177/1043454214563758
93
XuY.ZhangH. Y.JiangC. Y.YanY. W. (2021). Correlation among supportive care needs, psychological resilience and quality of life in breast cancer patients receiving postoperative chemotherapy. Chin. J. Breast Dis.15, 352–358.
94
YangY. L.LiuL.LiM. Y.ShiM.WangL. (2016). Psychological Disorders and Psychosocial Resources of Patients with Newly Diagnosed Bladder and Kidney Cancer: A Cross-Sectional Study.PLoS One11:e0155607. 10.1371/journal.pone.0155607
95
YangY. L.LiuL.WangX. X.WangY.WangL. (2014). Prevalence and associated positive psychological variables of depression and anxiety among Chinese cervical cancer patients: a cross-sectional study.PLoS One9:e94804. 10.1371/journal.pone.0094804
96
YeZ. Y.GaoX. X.ChengY. Q. (2014). The relationship between hope, coping style and quality of life among advanced cancer patients. Chin. Nurs. Manage.14.
97
YeungN. C.LuQ. (2014). Affect as a mediator between self-efficacy and quality of life among Chinese cancer survivors in China. Eur. J. Cancer Care23, 149–155.
98
YoungH. B.JungJ. E.YoungC. S. (2014). Effects of resilience, post-traumatic stress disorder on the quality of life in patients with breast cancer. Korean J. Women Health Nurs.20, 83–91. 10.4069/kjwhn.2014.20.1.83
99
YuJ. J.ChenY. Y.LiuC. T.Oo YangH. J. (2021). Correlation analysis of self-efficacy with anxiety, depression and quality of life in middle-aged and elderly patients with breast cancer undergoing chemotherapy. Clin. Med. Res. Pract.6, 9–11.
100
YuanJ.LinM. Y.YangB.ShiL. L.ZhaoB. Y.WangZ. F.et al (2022). Mediating role of finical toxicity between self-efficacy and quality of life in patients with prostate cancer. Nurs. J. Chin. PLA39, 4–8.
101
ZamoraJ.AbrairaV.MurielA.KhanK.CoomarasamyA. (2006). Meta-DiSc: a software for meta-analysis of test accuracy data.BMC Med. Res. Methodol.6:31. 10.1186/1471-2288-6-31
102
ZhangH.ZhaoQ.CaoP.RenG. (2017). Resilience and Quality of Life: Exploring the Mediator Role of Social Support in Patients with Breast Cancer.Med. Sci. Monit.235969–5979. 10.12659/msm.907730
103
ZhangS. M.GuW.GaoM.ChenP. (2015). Self-efficacy as a mediator between social support and quality of life in lung cancer patients receiving chemotherapy. China J. Health Psychol.23:e0246430. 10.1371/journal.pone.0246430
104
ZhangY.CuiC.WangY.WangL. (2020). Effects of stigma, hope and social support on quality of life among Chinese patients diagnosed with oral cancer: a cross-sectional study. Health Qual. Life Outcomes18:112. 10.1186/s12955-020-01353-9
105
ZhaoD. J.KangS. R.HaoN.WuR.MoL. L.XiaoY. H. (2020). Evaluation of resilience and quality of life in patients with advanced lung cancer and their relationship. J. Cancer Control Treat.33, 679–684.
106
ZhaoY. Q.LiuR. Y.HuoJ. (2020). Correlation of self-feeling burden, self - efficacy and quality of life in patients with cervical cancer during radiotherapy. Chin. Nurs. Res.34, 4159–4163.
107
ZhaoX. X.WangY. M. (2019). Study on the relationship between quality of life and social support and psychological resilience in elderly patients with end-stage cancer. Mod. Oncol.27, 852–855.
108
ZhengH. X.PanC. (2021). Effects of negative emotional self-efficacy and social support on quality of life of postoperative patients with cervical cancer. Matern. Child Health Care China36, 3335–3339.
109
ZhongM. S.LiX. B.TangN.ChenX.FanT. T. (2019). Role of resilience in relationship between perceived social support and quality of life of breast cancer patients. Chin. Nurs. Res.33, 237–240.
110
ZhouK. N.NingF.WangW.LiX. M. (2022). The mediator role of resilience between psychological predictors and health-related quality of life in breast cancer survivors: a cross-sectional study. BMC Cancer22:57. 10.1186/s12885-022-09177-0
Summary
Keywords
positive psychological resources, quality of life, cancer, meta-analysis, self-efficacy
Citation
Zhao X, Tong S and Yang Y (2022) The Correlation Between Quality of Life and Positive Psychological Resources in Cancer Patients: A Meta-Analysis. Front. Psychol. 13:883157. doi: 10.3389/fpsyg.2022.883157
Received
24 February 2022
Accepted
12 May 2022
Published
16 June 2022
Volume
13 - 2022
Edited by
Sebastian Filep, Hong Kong Polytechnic University, Hong Kong SAR, China
Reviewed by
Josef Jenewein, Medical University of Graz, Austria; Anabel Melguizo-Garin, University of Malaga, Spain; Lu Lin, The First Affiliated Hospital of Soochow University, China
Updates
Copyright
© 2022 Zhao, Tong and Yang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ye Yang, magicye32@163.com
This article was submitted to Positive Psychology, a section of the journal Frontiers in Psychology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.