Abstract
Objective:
The COVID-19 pandemic has had a major impact on the delivery of psychological treatment. Due to social distancing requirements, the provision moved to videoconferencing psychotherapy (VCP). There is a paucity of empirical data supporting the efficacy of EMDR therapy as a VCP. This stage 1 pilot study tested an EMDR therapy scripted protocol, such as Virtual Blind 2 Therapist (VB2Tr), on frontline mental health workers as a VCP regarding fitness for purpose, distinctiveness, relevance, and efficiency.
Methods:
A total of 24 participants were recruited for the study. The design included a one-session treatment intervention with pre, post, 1-month, and 6-month follow-up (FU) measurements. This treatment session used a “Blind 2 Therapist” EMDR therapy scripted protocol as videoconference psychotherapy that involves non-disclosure of traumatic memory. The research explored the treatment effect on the core characteristics of trauma memory, including subjective disturbance, belief systems, memory intensity (MI), vividness, and levels of emotionality. Additionally, the research explored participants’ experiences of adverse and benevolent childhood experiences (ACEs/BCEs) during their childhood.
Results:
Regarding the four tests, namely, fitness for purpose, distinctiveness, relevance, and efficiency, results are favourably suggesting potential clinical benefits of using EMDR as videoconference psychotherapy. Although this is a proof-of-concept study showing positive results, no clinical population or control group was used. The purpose of the study is to explore the potential for scalability toward a larger clinical trial. The treatment intervention was achieved irrespective of either ACEs/BCEs during childhood.
Conclusion:
The research tentatively supports the case for EMDR therapy as a credible treatment when used as video conference psychotherapy and in using the Blind 2 Therapist protocol. However, more research is needed to scale toward a clinical trial.
Clinical Trial Registration:
Clinical Trial Registration:https://www.isrctn.com/ISRCTN12099530, identifier ISRCTN12099530.
Introduction
In an attempt to reduce the risk of infections from COVID-19, many mental healthcare providers are closing their doors to patients requiring face-to-face therapy and instead of creating videoconferencing psychotherapy (VCP), remote access technology, e-health tools, and Internet interventions (Turgoose et al., 2018; Wind et al., 2020a). Several comprehensive reviews highlight the effectiveness of videoconferencing psychotherapy (VCP) and therapist-guided interventions for conditions such as anxiety, major depressive disorders, and trauma (Anderson et al., 2003; Ruskin et al., 2004; Christopher Frueh et al., 2007; Germain et al., 2010; Osenbach et al., 2013; Rousmaniere et al., 2014; Berryhill et al., 2018, 2019; Karyotaki et al., 2018a,b; Tuerk et al., 2018; Turgoose et al., 2018; Watts et al., 2020; Weinberg, 2020a; Wind et al., 2020b). Contemporary research supports VCP as “feasible” and “acceptable” as a mode of psychological treatment delivery, providing high satisfaction and effectiveness (Simpson and Reid, 2014; Dores et al., 2020; Viswanathan et al., 2020; Weinberg, 2020b; Wells et al., 2020; Wind et al., 2020b; Wright and Caudill, 2020; Aafjes-van Doorn et al., 2021; Hoffman, 2021). Furthermore, VCP provides a viable alternative to providing continuity of care in times of social, economic, and health upheaval (Crowe et al., 2020).
There are several distinct barriers toward the equitable provision and access to evidence-based, face-to-face/in-person psychological treatments, with a paucity of suitably qualified mental health workers to sufficiently address the global burden of mental illness and psychological trauma (Farrell et al., 2020). With relatively few providers trained in the therapies underpinned by a solid empirical evidence base, those who live in rural or remote communities are further restricted. The barriers to care are compounded further by disability, poverty, and stigma (Myers et al., 2008; Morland et al., 2011; Tuerk et al., 2018). VCP provides alternative flexibility and equity of access than in-person therapy, with potential for financial efficiencies and cost savings, enhanced reach, flexible implementation, improved cultural adaptability and sensitivity, and improved equity when compared with in-person therapy (Barak et al., 2008; Morland et al., 2011; Backhaus et al., 2012; Bolton et al., 2014; Wild et al., 2016; Baños et al., 2017).
Despite potential benefits, VCP does require critical consideration. One factor is the impact that VCP has on the therapeutic alliance when assuming the “In person,” traditional model, which is the gold standard for psychotherapy. Recent studies (Germain et al., 2010; Simpson and Reid, 2014; Berger, 2017) acknowledge that an effective therapeutic alliance is essential in underlying successful therapy. Table 1 outlines the advantages and disadvantages of using V and how they can be adapted to promote greater effectiveness (Dores et al., 2020; Viswanathan et al., 2020; Weinberg, 2020b; Wells et al., 2020; Wind et al., 2020b; Wright and Caudill, 2020; Aafjes-van Doorn et al., 2021; Hoffman, 2021).
TABLE 1
| Advantages | Disadvantages | Adaptation factors to promote greater effectiveness |
| ° Greater flexibility ° Cultural adaptability ° Enhanced reach ° Better use of scarce resources ° Cost efficiencies ° Increased accessibility ° No geographical restrictions ° Environmentally – reduces carbon footprint ° Responds to the need for rural services for veterans ° Convenience and affordability for disabled people | ° Technology knowledge, application, functioning, and reliability, including challenges ° Poor internet connections, particularly in low socioeconomic areas ° Body language restricted to head and face ° Privacy into the home environment ° Creating safe space, time, and relationships ° Cultural considerations and norms ° Risk management & triage ° Geographical factors, legislation, professional indemnity, logistics ° Insurance cover and liability | ° Adjusting for more restricted access to non-verbal communication ° More regular “checking in” with clients ° Requesting more information and clarification on specific points ° More focus on facial expressions and bodily gestures ° More frequent emotion checking ° Enhanced preparation before sessions ° More control of the space ° The therapists assuming a greater sense of ownership and responsibility for the therapeutic alliance within the therapy work ° Client centredness – the Therapist “tailoring” their approach more to the client individual and specific needs |
Advantages, disadvantages, and adaption factors in VCPs.
The reality of the COVID-19 pandemic ostensibly has removed choice for a great many individuals, with the options being VCP intervention, no intervention, or an extensive and uncertain period of waiting. The current advances in VCP technology enable it to offer an innovative solution as a viable alternative to in-person therapies.
The World Health Organisation (2020) has expressed concern over the psychological impact of the pandemic and social distancing on the mental health of a broad sector of society. The psychosocial consequences include increases in loneliness, anxiety, depression, gender-based violence, insomnia, substance misuse, self-injurious activity, and suicidal behaviour (Cullen et al., 2020; Ghebreyesus, 2020; Kavoor, 2020; Khan et al., 2020; Kumar and Nayar, 2020; Talevi et al., 2020; Usher et al., 2020). However, COVID-19 is not “ground zero” when considering the mental well-being of a population. Those clients with pre-existing mental health issues before the pandemic started risk further minimisation of their lived experience, and potential to fall out’ of existing service provision. It is essential to acknowledge that events that pre-date COVID-19 may still influence an individual’s response. Two considerations are exposure to adverse childhood experiences (ACEs) and benevolent childhood experiences (BCEs). Exposure to ACEs is the single most potent global public health issue when considering social inequality, lifelong impact on health and behaviour, and social deprivation. Arguably the COVID-19 pandemic further compounds antecedent ACEs. Social inequalities such as these create significant barriers when accessing services, either in person or via VCP (Felitti et al., 1998; Brown et al., 2009; Kim et al., 2010; Burke et al., 2011; Bellis et al., 2014a,b, 2015, 2017, 2019; Islam et al., 2021).
Videoconferencing psychotherapy interventions have primarily focussed on prolonged exposure (Strachan et al., 2012; Hernandez-Tejada et al., 2014; Yuen, 2015; Acierno et al., 2016; Clapp et al., 2016; Acierno, 2017; Tuerk et al., 2018), behavioural activation (Luxton et al., 2015; Acierno et al., 2016; Acierno, 2017), cognitive processing therapy (Morland et al., 2011; Fortney et al., 2015; Grubbs et al., 2015; Maieritsch et al., 2016), and CBT (Olthuis et al., 2016a,b). Currently, limited research publications support EMDR therapy, which uses VCP to treat post-traumatic stress disorder (PTSD) (Todder et al., 2007; Todder and Kapln, 2007; Lightstone et al., 2015). However, a recent study (Bongaerts et al., 2021) has used home-based psychotherapy, delivered by telehealth, as a treatment intervention for complex PTSD. The intervention was delivered in an intensive format, offering both prolonged exposure and eye movement desensitisation and reprocessing [EMDR therapy]. Six participants took part in the study, with two-thirds losing their PTSD or complex-PTSD diagnostic status, demonstrating that the telehealth intervention was both safe and effective (Bongaerts et al., 2021). However, the sample size in their study was small, with just six participants, and only four of the six losing their diagnosis. The safety and effectiveness determinants of the EMDR therapy intervention indicate more extensive and more representative sample sizes.
Eye movement desensitisation and reprocessing therapy, an empirically supported intervention for PTSD and complex PTSD (Christopher Frueh et al., 2007; American Psychological Society, 2017; ISTSS, 2018; Bisson et al., 2019; de Jongh et al., 2019b; Karatzias et al., 2019, 2020), was developed in the late 1980s by an American psychologist, Francine Shapiro. Its primary foci are on the treatment of pathogenic memories and their associated stress symptoms using the model of pathogenesis and change known as adaptative information processing (Hase et al., 2017; Valiente-Gómez et al., 2017). Shapiro (2018) considered trauma memories in a range of mental health disorders and not just PTSD and complex PTSD. Within the AIP theoretical framework, a meta-theory unique to EMDR therapy, the model assumes that the human brain can usually process memories of adverse life events to complete integration. The essence of EMDR therapy involves four distinct aspects, namely, preparation, access, stimulation, and integration [PACI]. What gives EMDR therapy a specific distinctness relates to bifocal physical stimulation, a working memory taxation device that enables the client to attend to internal and external stimuli (de Jongh et al., 2019a,b, 2020). The hypothesised working mechanism of EMDR therapy is still under investigation (Matthijssen et al., 2021). However, most evidence supports the working memory account. Working memory has a limited capacity. Therefore, dual taxation sets up a competing situation. Consequently, the emotional intensity of the pathogenic memory, with all its subjective levels of disturbance, is gradually lost and eventually reconsolidated into a less disturbing and reduced emotional form. Within the EMDR therapy literature, the dominant empirical evidence supports physical eye movements; however, other forms of bifocal physical stimulation can include acoustic, somatic, or multiple forms such as is used within EMDR 2.0 (de Jongh et al., 2020).
The core characteristics of the EMDR B2T protocol are to access and activate a pathogenic memory. However, the primary distinction between this protocol and the standard protocol is that the client does not reveal details about the memory itself, other than its emotional and somatic content and an indication of their subjective unit of distress (SUD). Clients are not under pressure to disclose any of the trauma content during trauma processing using B2T. Table 2 highlights the core components of the EMDR therapy B2T, its context regarding the eight phases of therapy, and the assessment phase (Phase 3 of the standard protocol of EMDR therapy).
TABLE 2
| EMDR therapy: 8 phases | EMDR therapy Phase 3 Standard Protocol – Assessment Structure | EMDR therapy Phase 3 Assessment Blind 2 Therapist structure and VB2Tr version |
| Phase 1: history taking | Target Memory | Target memory – cue word |
| Phase 2: preparation | Worst Image | Emotions |
| Phase 3: assessment | Negative Cognition | Subjective Unit of disturbance (SUD 0–10) |
| Phase 4: desensitisation | Positive Cognition | Location of body sensation |
| Phase 5: installation | Validity of Cognition (1–7) | |
| Phase 6: body scan | Emotion | |
| Phase 7: closure | Subjective Unit of Disturbance (0–10) | |
| Phase 8: re-evaluation | Location of body sensation |
EMDR Blind 2 Therapist protocol in context, adapted from Wolpe and Lazarus (1966), Shapiro (2018, 1995, 2001), and Farrell et al. (2020).
Many empirically supported treatments for PTSD contain various elements and degrees of exposure. These rely upon the client’s ability and willingness to disclose the memory of the adverse life event causing a stress response. When pathogenic memories involve shame, guilt, disgust, fear of retribution, lack of language, and non-disclosure self-protection/preservation factors, disclosure may not even be a viable option for a client. A study published from research carried out in Northern Iraq tested the “Blind 2 Therapist” (B2T) protocol, an adaption of EMDR therapy. This study demonstrated the safety, effectiveness, efficiency, and relevance as a treatment intervention for both “shame-based” and “fear of retribution” trauma (Farrell et al., 2020). However, an evaluation of EMDR B2T as a VCP method of delivery has not occurred to date. Therefore, this study aimed to test the virtual version of B2T (referred to as VB2Tr), delivered as a VCP, as a suitable clinical intervention in the desensitisation and reprocessing of a pathogenic memory.
As indicated earlier, within the existing EMDR therapy literature, there is a paucity of research regarding the use of VCP EMDR (Bongaerts et al., 2021). In addressing this aspect, any potential study would have to address two significant aims:
- 1.
What adaptations, if any, would be required to use EMDR therapy as a VCP?
- 2.
Do we critically consider the potential advantages/disadvantages of EMDR therapy as a VCP?
Therefore, the purpose of this study was to determine whether the application of VCP EMDR therapy would be associated with (1) fitness for purpose – safe and effective, (2) distinctiveness – alterations in the core components of a pathogenic memory regarding intensity, vividness, and emotionality, (3) relevance, and (4) efficiency.
A directional hypothesis predicts a positive or negative change between two variables in a specific population. These changes were measured at pre, post, 1-month, and 6-month FUs. The research study hypotheses were as follows:
Hypothesis 1: Fitness for purpose – Virtual Blind 2 Therapist EMDR (VB2Tr), when delivered as VCP, will have no impact on the SUD and the validity of cognition (VOC) regarding a pathogenic memory when measured at post-treatment, 1-month, and 6-month in comparison to a pre-measure.
Hypothesis 2: Distinctiveness – VB2Tr, as a VCP, will have no impact on reducing MI, memory emotionality (ME), and memory vividness (MV) of a pathogenic memory following intervention when measured at post-treatment, 1-month, and 6-month in comparison to a pre-measure.
Hypothesis 3: Relevance – when using VB2Tr, ACEs or BCEs will influence the processing of a pathogenic memory.
Hypothesis 4: Efficiency – as VB2Tr takes longer in time than the 60–90 min recommended by www.emdria.org, it would be more expensive as a clinical intervention.
Methodology: Research Design
Ethical approval for the study was granted by the University of Worcester (United Kingdom) [CBPS1920031-R2]. Consequently, all the methods used for the study were carried out in strict adherence to the ethical approval granted and in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects. Additionally, the study was registered as a clinical trial ID ICSRCTN12099530 [30/06/2021]. This stage 1 pilot study used a pre-test/post-test design for taking measures before and after a one-session treatment using the EMDR VB2Tr protocol, including 1-month and 6-month FUs to determine the impact of the treatment intervention on the pilot cohort. The rationale for an experimental design as a stage 1 research project was to determine proof of concept before proceeding to stage 2, involving a quasi-experimental design utilising a distinct control group. The longer-term strategy is for phases 1 and 2 to support a more significant funding application, utilising a randomised control design incorporating a delayed treatment paradigm.
Participants
As this was a “proof of concept” study, and consistent with the COVID-19 focus, the research study participants were frontline, mental health workers engaged in active clinical practice during the first period of lock down in the United Kingdom. The design of the study incorporated a self-selecting (volunteer) sampling approach, with participants recruited via advertising on psychotherapy Internet forums. Inclusion criteria were as follows:
- •
Clinically active using online treatment platforms – remote working.
- •
Encountered an adverse life event that generated a presently held, subjective level of disturbance (SUD+).
- •
Willingness to be a client for a one-session intervention using the EMDR therapy Blind 2 Therapists protocol (VB2Tr) as a VCP, using the remotEMDR platform.
- •
No expectation to disclose anything about the target adverse memory.
A sample size of 17 was deemed sufficient to compare findings from the original study, which used the EMDR Blind 2 Therapist protocol with participants from Northern Iraq (Bennett-Levy and Lee, 2014; Chigwedere et al., 2020; Collard and Clarke, 2020; Farrell et al., 2020; Scott et al., 2021). A total of N = 24 was recruited for the study.
Measures Used for the Study
The pre-test/post-test design utilised the following measures:
- •
Subjective unit of disturbance (SUD) is a 0–10 scale for measuring subjective levels of distress or disturbance currently experienced by an individual (Wolpe and Lazarus, 1966).
- •
The validity of the cognition scale (VOC) provides a rapid assessment of cognitive structure on an emotional/somatic level rather than an intellectual level (Shapiro, 2018, 1995, 2001). Both the SUD and VOC have documented validity, reliability, and correlations with several physiological indices of distress.
- •
Memory vividness (MV) and emotionality (ME) – a subjective unit of measurement (0–10) of the vividness of the target memory, either positive or negative (Andrade et al., 1997; Gunter and Bodner, 2008; Maxfield et al., 2008; Engelhard et al., 2010; Schubert et al., 2011, 2016; van den Hout et al., 2011; Leer and Engelhard, 2020).
- •
Memory intensity (MI) is a subjective unit of measurement (0–10) of the intensity of the target memory, either positive or negative (van der Kolk, 2003, 2007, 2015).
- •
Adverse childhood experience scale (ACE) collects crucial information based upon the prevalence of adversity during childhood in ten categories before the age of 18: emotional abuse (recurrent), physical abuse (recurrent), sexual abuse (contact), physical neglect, emotional neglect, substance misuse in the household, mental illness in the household, mother treated violently, divorce or parental separation, and criminal behaviour in the household (Felitti et al., 1998; Burke et al., 2011). With each category counting as one point, with ten categories, the highest possible ACE score is 10 (Felitti et al., 1998; Brown et al., 2009; Felitti, 2010; Narayan et al., 2017; Afifi et al., 2020; Aronson et al., 2020; Finkelhor, 2020; Struck et al., 2021). An additional component of the ACEs was to test the study participant groups for comparability with the original CDC-Kaiser Permanente Study (Felitti et al., 1998). A further comparison was integrated using ACEs replication data carried out within the United Kingdom by Bellis et al. (2015).
- •
The BCEs scale is a new instrument designed to assess positive early life experiences in adults with a history of childhood adverse experiences. Ostensibly, BCEs are a counterpart to the ACE questionnaire. The BCEs (Narayan et al., 2018) are multiculturally sensitive and applicable, regardless of socioeconomic position, urban-rural background, or immigration status. The BCEs items utilise a developmental psychology framework, integrated with ecological systems theory (Narayan et al., 2017; Crandall, 2019, Crandall, 2020; Merrick et al., 2019; Karatzias et al., 2020; Malti, 2020; Merrick and Narayan, 2020; Starbird and Story, 2020; Doom et al., 2021).
- •
Each treatment session was timed (minutes) using the metric period recommended by EMDRIA sessions; 60–90 minutes, measuring from commencement of Phase 3 – assessment, to the completion of Phase 7 – closure (including debrief).
- •
The cost per session (£s/€s) was calculated at £56.49 (€66.36) using economic modelling from the University of Worcester.
After 1 month of each VB2Tr session, another research team member carried out Phase 8 – re-evaluation, conducted a qualitative interview, and obtained 1-month FU data – additional psychometric data were also collected at 6 months.
Treatment
The research utilised a 1-treatment session intervention (EMDR VB2Tr as a VCP), which was a partial replication of a previous study (Farrell et al., 2020). This study used a beta-tested software programme called remotEMDR1, a technology that enabled the delivery of EMDR as a VCP. The remotEMDR is a synchronous programme that offers various visual and acoustic forms of bifocal physical stimulation and includes an integrative video platform, giving EMDR therapists complete control within the session.
The EMDR therapy VB2Tr protocol, adapted for VCP usage, originated from the original B2T (Farrell and Reid, 2020), including pathogenic MV, intensity, and emotionality metrics.
An EMDR Europe Accredited Senior Trainer and Consultant carried out each of the VB2Tr treatment sessions, and each was digitally recorded and made available for treatment fidelity checking. EMDR Europe Consultants and Co-researchers carried out these fidelity checks for the project. The EMDR Foundation Fidelity Rating Scale (EFRS) – version 2 was developed initially by van der Kolk (2007), subsequently revised and updated by Maxfield et al. (2018).
VB2Tr sessions incorporated multiple consent points, including initial recruitment, the commencement of the VB2Tr session, permission to record digitally, and permission to utilise the research participants’ data at the end of the VB2Tr session.
Statistical Analysis
Statistical analysis utilised the Statistical Package for Social Sciences (SPSS version 26.0; Chicago, IL, United States) to include means and standard deviations calculated for SUD, VOC, MV, ME, and MI before treatment, post-treatment, and at 1-month and 6-month FUs (Table 3). Skewness and kurtosis were estimated in the data sets to evaluate the normality of the outcome measures, and frequencies of total and individual scores for ACEs and BCEs. This detailed examination and alpha testing included generalised estimating equations (GEE) to compare before/after the intervention and FU changes in SUD, VOC, MV, ME, and MI. ACEs and BCEs were added as the covariates in the modelling exercise. The GEE model accounts for time variations and correlations among repeated measurements and does not require the dependent variable to be normally distributed (Locascio and Atri, 2011). Gamma with log link was selected as the outcome variables were skewed. The presence of negative values for SUD, MV, ME, and MI measures was handled by adding a constant value to the data before the analysis. As for descriptive statistics, we used mean ± standard deviation (±SD) for numerical variables and percentage (%) for categoric variables. The p-values of <0.05 were considered significant. The overall effect size was calculated using Hedges’ g.
TABLE 3
| Pre SUD | Post SUD | SUD-1-mth FU | SUD-6mth FU | Retro VOC Pre | VOC Post | VOC 1-mth FU | VOC 6-mth FU | |
| Mean | 7.75 | 0.17 | 0.55 | 0.35 | 2 | 6.96 | 6.86 | 6.89 |
| Median | 8 | 0 | 0 | 0 | 2 | 7 | 7 | 7 |
| STD | 1.39 | 0.48 | 0.74 | 0.59 | 0.78 | 0.2 | 0.35 | 0.32 |
Descriptives – subjective unit of disturbance (SUD) and validity of cognition (VOC): pre, post, 1-month, and 6-month FUs (N = 24).
Results
Of the N = 24 research participants who took part in the study, all completed the VB2Tr treatment session and post-treatment, 1-month, and 6-month FU measures. There were no dropouts from the study. Tables 3, 4 highlight the descriptive data regarding various measures, namely, SUD, VOC, MV, ME, and MI, and pre, post, 1-month, and 6-month FUs.
TABLE 4
| Memory vividness | Memory emotionality | Memory intensity | ||||||||||
| Pre | Post | 1-mth FU | 6-mth FU | Pre | Post | 1-mth FU | 6-mth FU | Pre | Post | 1-mth FU | 6-mth FU | |
| Mean | 8.04 | 1.42 | 0.227 | 0.579 | 8.33 | 0.417 | 0.0909 | 0.211 | 8.46 | 0.0417 | 0.409 | 0.474 |
| Median | 8 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 8 | 0 | 0 | 0 |
| Standard deviation | 1.78 | 2.41 | 1.82 | 1.46 | 1.43 | 0.717 | 2.2 | 1.23 | 1.41 | 0.999 | 1.99 | 1.68 |
| Minimum | 5 | 0 | −7 | −3 | 6 | 0 | −8 | −4 | 6 | −4 | −6 | −6 |
| Maximum | 10 | 8 | 2 | 2 | 10 | 2 | 3 | 1 | 10 | 2 | 1 | 1 |
Descriptives – memory vividness (MV), memory emotionality (ME), and memory intensity (MI): pre, post, 1-month, and 6-month FUs (N = 24).
Hypothesis 1. Figure 1 shows the decrease in SUD and the increase in the VOC at the post, 1-month, and 6-month FUs.
FIGURE 1
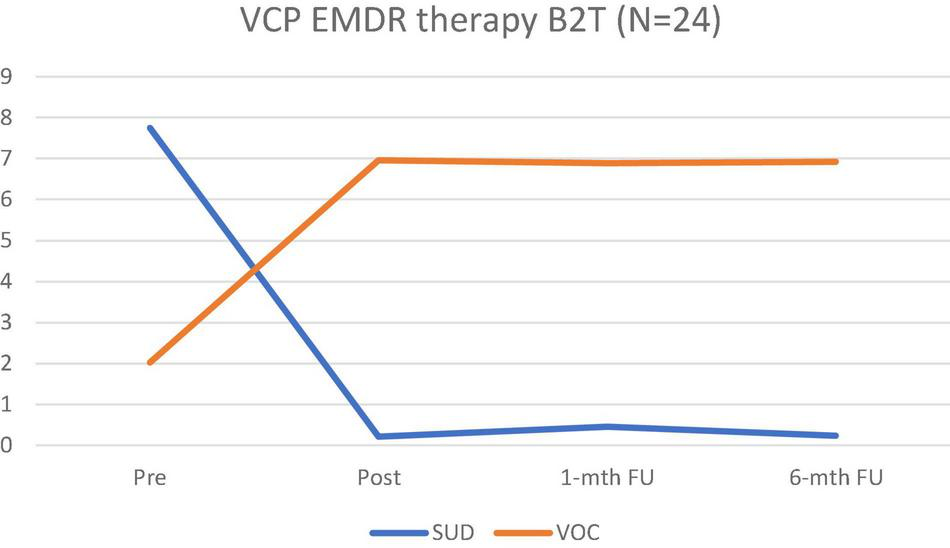
Alterations in SUD and VOC scores at pre, post, 1-month, and 6-month FUs.
Additionally, Table 5 highlights the mean, standard deviation, skewness, kurtosis, baseline, and p values for the SUD and VOC at pre, post, 1-month, and 6-month FUs and the maintenance of the VB2Tr treatment effect in more detail.
TABLE 5
| Mean (SD) | Skewness (SE) | Kurtosis (SE) | B (SE) | p value | |
| Pre-SUD | 7.75 (1.39) | −0.15 (0.47) | −0.95 (0.92) | 0 | |
| Post-SUD | 0.21 (0.49) | 2.72 (0.47) | 7.73 (0.92) | −1.02 (0.03) | <0.001* |
| 1 m FU SUD | 0.64 (0.79) | 0.78 (0.49) | −0.89 (0.95) | −0.94 (0.05) | <0.001* |
| 6mFU SUD | 0.23 (0.95) | −1.74 (0.51) | 6.99 (0.99) | −0.99 (0.01) | <0.001* |
| Pre-VOC | 2.02 (0.79) | −0.08 (0.47) | −1.36 (0.92) | 0 | |
| Post-VOC | 6.96 (0.20) | −4.90 (0.47) | 24.00 (0.92) | 1.22 (0.07) | <0.001* |
| 1 m FU VOC | 6.87 (0.31) | −2.60 (0.49) | 5.63 (0.95) | 1.21 (0.08) | <0.001* |
| 6 m FU VOC | 6.92 (0.25) | −3.34 (0.52) | 11.19 (1.01) | 1.22 (0.08) | <0.001* |
Means, SD, skewness, and kurtosis for SUD and VOC at pre, post, 1-month, and 6-month FUs.
*Statistically significant.
There was a substantial reduction in SUD after receiving EMDR in comparison with the baseline assessment (B = −1.02, SE = 0.03, p < 0.001). The decrease in SUD was maintained in the FU assessments at 1 month (B = -0.94, SE = 0.05, p < 0.001) and 6 months (B = -0.99, SE = 0.04, p < 0.001) in comparison with the baseline. Simultaneously, there was an increase in VOC after receiving EMDR in comparison with the baseline assessment (B = 1.22, SE = 0.07, p < 0.001). The increase was maintained after 1-month (B = 1.21, SE = 0.08, p < 0.001) and 6-month (B = 1.22, SE = 0.08, p < 0.001) post intervention.
The results of this study indicate that VB2Tr decreased the SUD and increased the VOC in the treatment of a pathogenic memory tested at pre, post, 1-month, and 6-month FUs, suggesting that using VB2Tr as a VCP demonstrated a treatment effect on the pathogenic memory when measured by the SUD and VOC. Furthermore, there was a statistically significant difference between pre-treatment (M = 7.75, SD = 1.39) and 6-month FU (M = 0.35, SD = 0.59), with a Hedges’ g effect size value (g = 6.71) suggesting high practical significance. Therefore, we rejected the directional hypothesis that there is no difference in the SUD or VOC when using the VB2Tr EMDR intervention as a VCP.
Hypothesis 2. Figure 2 shows a reduction in the nature and characteristics of the pathogenic memory, including MV, emotionality, and intensity. For some research participants, alterations in memory characteristics indicated positive change rather than disturbance (negative), and therefore positive change is presented as a minus score.
FIGURE 2
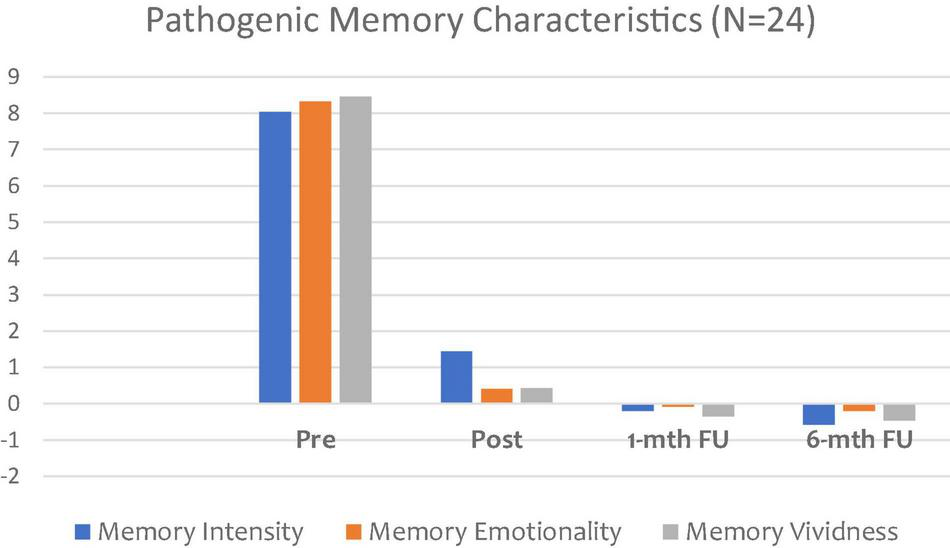
Changes in pathogenic memory subjective characteristics.
As Figure 2 demonstrates, the VB2Tr intervention clearly impacted on the three areas of pathogenic distinctiveness, namely, MV, emotionality, and intensity, with results maintained at both 1-month and 6-month FU. There were significant decreases in MV (B = -0.42, SE = 0.05, p < 0.001), ME (B = -0.61, SE = 0.03, p < 0.001), and MI (B = -0.77, SE = 0.04, p < 0.001) following the intervention. These effects were maintained in the first month FU for ME (B = -0.65, SE = 0.06, p < 0.001), MI (B = -0.79, SE = 0.03, p < 0.001), MV (B = -0.60, SE = 0.07, p < 0.001) and sustained after 6 months for MV (B = -0.58, SE = 0.03, p < 0.001), ME (B = -0.62, SE = 0.03, p < 0.001), MI (B = -0.79, SE = 0.04, p < 0.001). Overall, these results indicate changes that were consistently, statistically significant at p < 0.001. Additionally, the results demonstrate a favourable dose effect, with potential evidence in support of resilience and post-traumatic growth, as indicated by the treatment effect emphasis between pre and 6-month FU. This represents a significant finding from this study.
Therefore, it would be reasonable to assume that when VB2Tr is delivered as a VCP, it has the potential to instigate distinct changes to core components of the pathogenic memory, suggesting evidence of memory reconsolidation. Regarding hypothesis 2, distinctiveness – VB2Tr, as a VCP, will have no impact in reducing MI, ME, and MV of a pathogenic memory following intervention when measured at post-treatment, 1-month, and 6-month in comparison with a pre-measure. Therefore, the directional hypothesis is not supported.
Hypothesis 3. Figures 3, 4 demonstrate that exposure to ACEs or BCEs did not influence the processing of the pathogenic memory or the intervention outcome following the utilisation of VB2Tr.
FIGURE 3
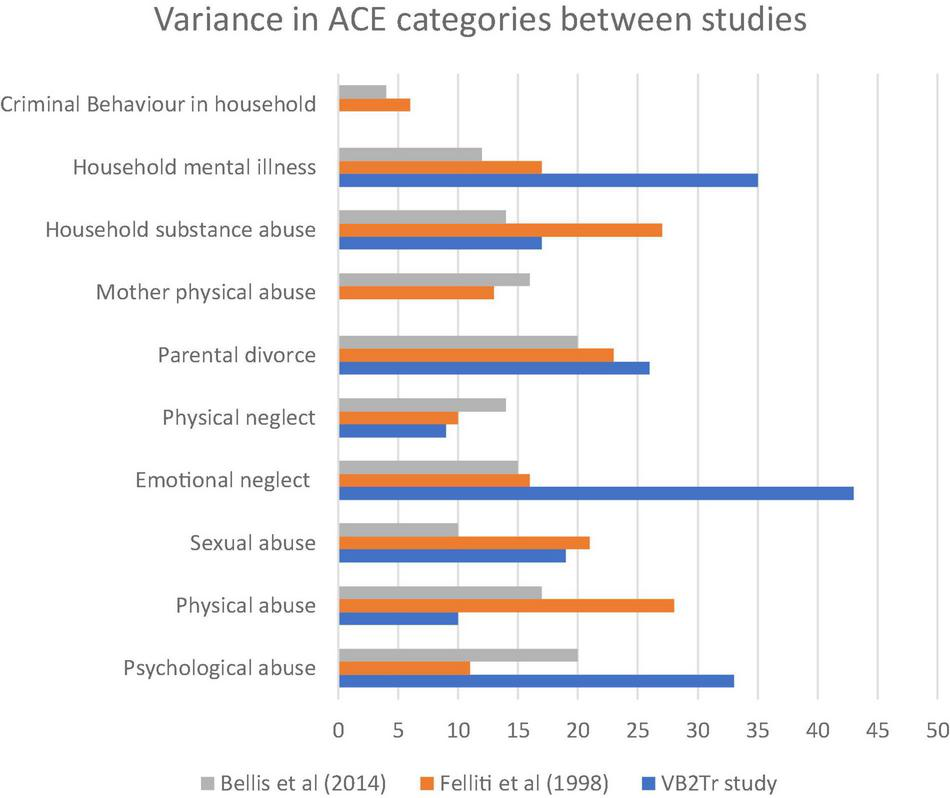
ACE by category between studies.
FIGURE 4
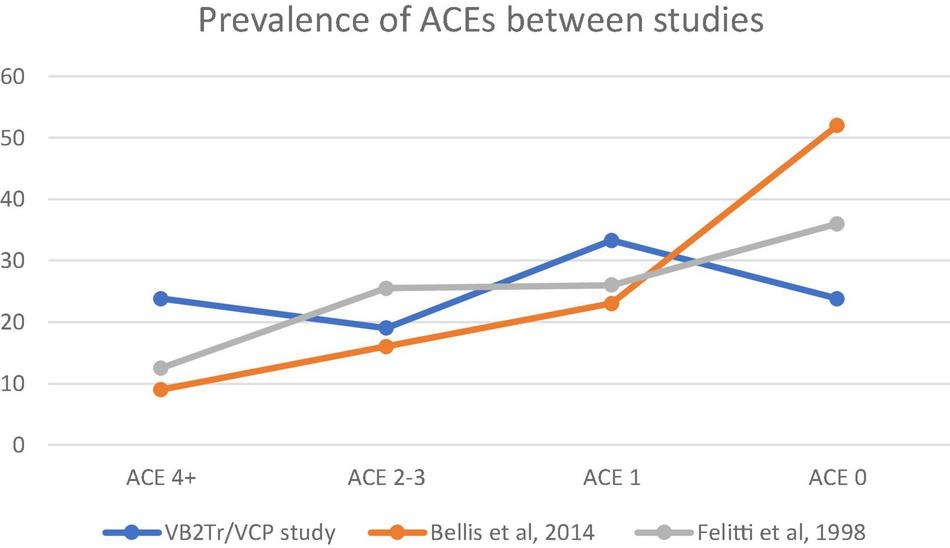
Prevalence of ACE scores between the three groups: VB2Tr.
As explained previously, testing the relevance hypothesis compared the study participant group with the original primary studies (Felitti et al., 1998; Bellis et al., 2014a,b, 2015, 2017, 2019). A single factor ANOVA explored the between-group variances. This one-way analysis of variance is a technique used to compare two or more samples when utilising numerical or categorical data.
Figure 4 highlights the prevalence of ACEs between studies (Felitti et al., 1998; Bellis et al., 2014b). A descriptive review of the results suggests higher exposure to 4 + ACEs within the VB2Tr participant group; however, results yielded an F(3,4) = 8.45, p-value < 0.03*, suggesting that there were, in fact, differences between the three groups in terms of the prevalence of ACEs, therefore, the directional hypothesis is not supported.
Table 6 provides more descriptive data about the VB2Tr participant group relating to specific exposure to ACEs. The results focussed on exposure to physical abuse, physical neglect, mother physical abuse, and criminal behaviour in the household.
TABLE 6
| ACEs | Incidence | Sig. (2-test) |
| Psychological abuse | 7 (33%) | 0.189 |
| Physical abuse | 2 (10%) | <0.001* |
| Sexual abuse | 4 (19%) | 0.007 |
| Emotional neglect | 9 (43%) | 0.664 |
| Physical neglect | 2 (9%) | <0.001* |
| Parental divorce | 6 (26%) | 0.035 |
| Mother physical abuse | 0 (0%) | <0.001* |
| Household substance abuse | 4 (17%) | 0.003 |
| Household mental illness | 8 (35%) | 0.210 |
| Criminal behaviour in household | 0 (0%) | <0.001* |
Types of adverse childhood experiences (ACE).
*p < 0.001.
Although an ANOVA revealed a distinction between the three groups, it is essential to highlight the elevated incidence of exposure to psychological abuse, emotional neglect, household mental illness, absence of exposure to mother physical abuse, and criminal behaviour in the household VB2Tr research participant group. Figure 5 ranks the scores of the ten questions of the original ACEs questionnaire from most prevalent (1) to least (10).
FIGURE 5

Groupwise ranking of ACEs between groups, *p < 0.001.
Figure 6 compares the frequency of both ACEs and BCEs from the VB2Tr research population. The mean ACE was 1.8 (SD 1.68) and the BCE was 7.6 (SD 2.06). The correlation between ACEs and BCEs is r(22) = -0.48.
FIGURE 6
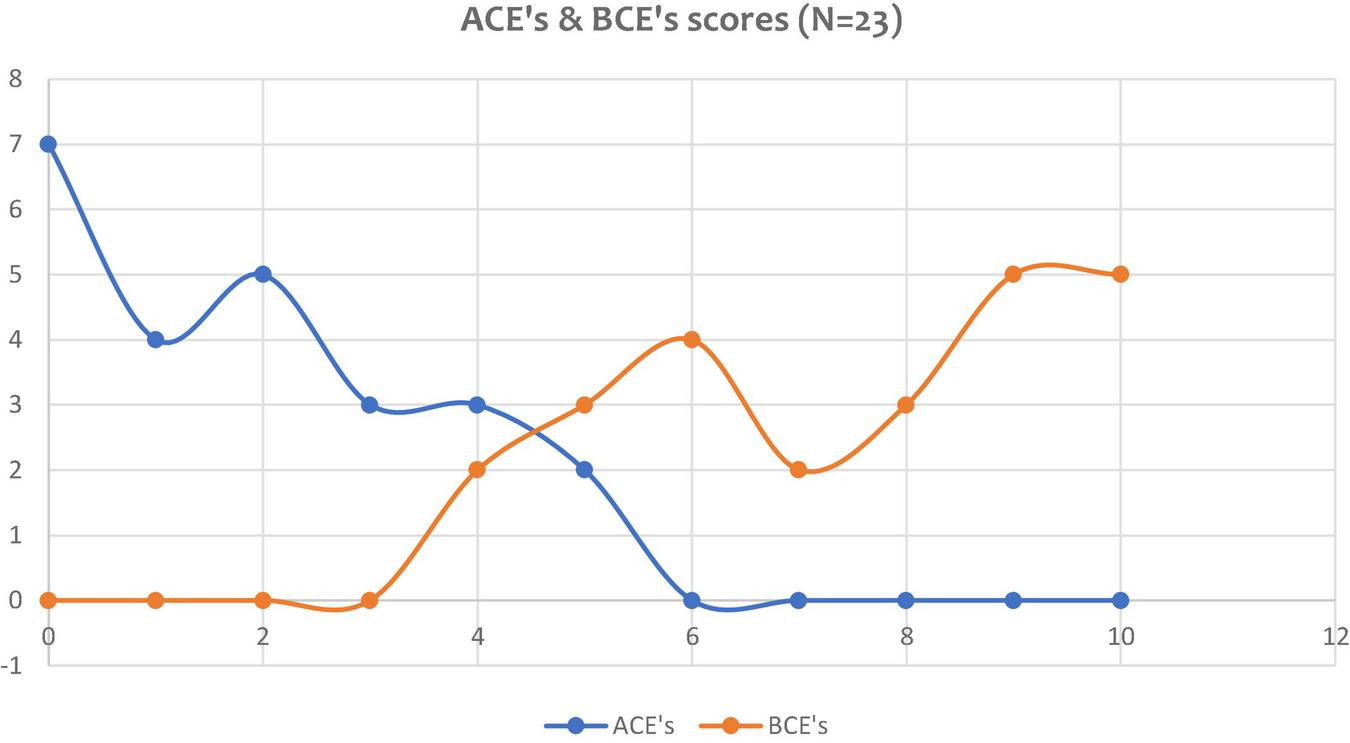
Frequency of ACE and BCE scores of the research participants.
For the BCEs, the mean for the sample was 7.6 (SD = 2.06), and the median was 8. As shown in Table 7, most participants reported having eight (17.4%), nine (21.7%), and ten (21.7%) benevolent experiences in their childhood. All participants reported at least four BCEs. Table 5 displays the frequency of each type of BCEs in the current sample. Results suggest that having “At least one good friend” (96%) and “Opportunities to have a good time” (91%) were the most frequent benevolent experiences.
TABLE 7
| BCEs | Incidence | Sig. (2-test) |
| At least one caregiver with whom you felt safe | 18 (78%) | 0.011 |
| At least one good friend | 22 (96%) | <0.001* |
| Beliefs that gave you comfort | 16 (70%) | 0.093 |
| Enjoyment at school | 18 (78%) | 0.011 |
| At least one teacher that cared | 20 (87%) | <0.001* |
| Good neighbours | 17 (74%) | 0.035 |
| An adult (not a parent/caregiver or the person from *11) who could provide you with support or advice | 12 (52%) | 1.000 |
| Opportunities to have a good time | 21 (91%) | <0.001* |
| Like yourself or feel comfortable with yourself | 12 (52%) | 1.000 |
| Predictable home routine, like regular meals and a regular bedtime | 20 (87%) | <0.001* |
Types of BCEs.
*Statistically significant.
In exploring further into hypothesis 3, relevance – first, results seem to indicate that neither ACEs nor BCEs scores did not influence the outcome of the intervention. Second, although 75% of the research participants admitted their motivation for participation was based firmly on “non-disclosure,” results indicated 87.5% did disclose their target memory to the treating clinician. Of these 87.5%, Table 8 highlights the categories of target memories disclosed.
TABLE 8
| ° Sexual assault (3) |
| ° Child abuse (4) |
| ° Parental neglect (1) |
| ° Fatal road traffic collision (1) |
| ° Occupational bullying (4) |
| ° Complicated grief (2) |
| ° Episodes involving shame and humiliation (6) |
Disclosed target memory themes and frequencies chosen by research participants for VB2Tr as a VCP.
As indicated earlier, using VB2Tr demonstrates a distinct treatment effect with Table 8, highlighting clinical applicability. In addition, desensitisation and reprocessing of these trauma memories occurred irrespective of either ACEs or BCEs. These results were consistent at 1-month and 6-month FU. Consequently, this data set supports the assertion of hypothesis 3, therefore, the directional hypothesis is not supported in relation to ACEs and BCEs.
In testing hypothesis 4, efficiency – the administration of VB2Tr was tested against the period recommended by EMDRIA sessions; 60–90 min. Results for this study used a time metric (minutes) from the commencement of Phase 3, assessment, to the completion of Phase 7, closure (including debrief). Of the N = 24 research participants, the average VB2Tr session was 57 min and 27 s, with an SD of 17 min 27 s. Results highlight that the treatment sessions were below the 60 min threshold.
Testing the costing element of hypothesis 4 required economic modelling using University of Worcester financial algorithms. The UW costing model used for each VB2Tr treatment session was calculated at £56.49 (€66.36). Of the 24 clinical sessions of VB2Tr carried out, the mean cost per session was £54.02 (€63.45). This represented potential modest savings of £2.47 (€2.91) per session. However, Figure 7 indicates the variation in treatment costs for each individual session. One of the distinct advantages of remote intervention is the reduction in client-related costs such as travel time, transportation, and parking.
FIGURE 7
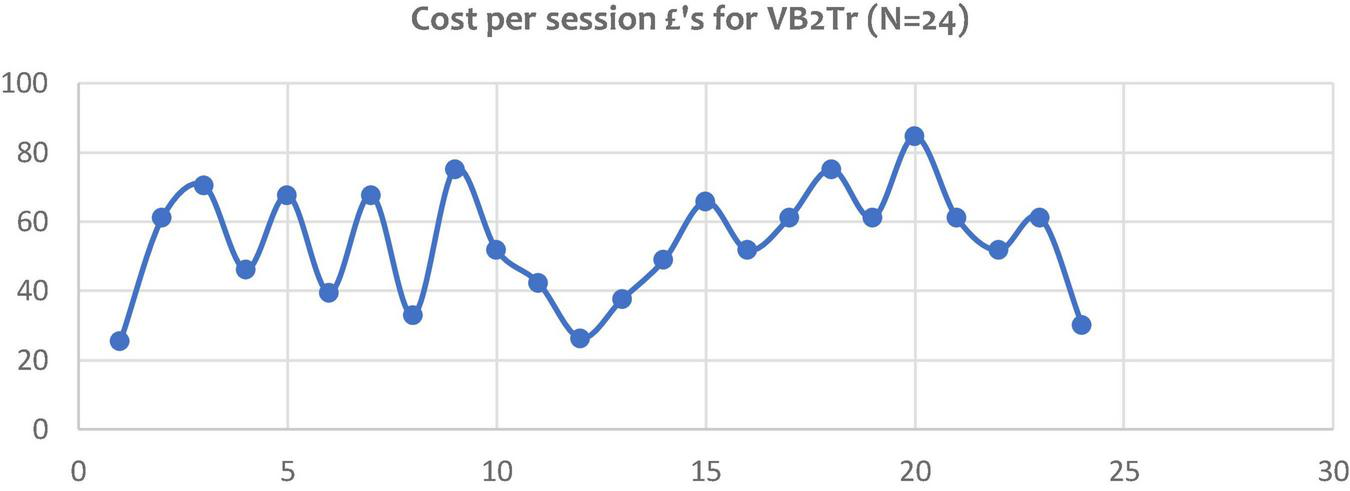
Variance in cost of VB2Tr treatment sessions carried out as a VCP.
Results indicate savings in terms of time and efficiency, with additional health economic benefits. The results of hypothesis 4 results suggest the rejection of the directional hypothesis.
Discussion
The rationale for this study was to ascertain how EMDR therapy could be used as a VCP considering the current COVID-19 pandemic, where social distancing is a vital strategy in reducing infection rates. However, more specifically, this research wanted to explore the potential use of the EMDR therapy VB2Tr protocol virtual version as a VCP, in order to determine its fitness for purpose, distinctiveness, relevance, and efficiency.
The memory targets identified in Table 8 suggest that the research participants worked on distressing pathogenic memories of major adverse life events and that the intervention (VB2Tr) suggests a treatment effect. Despite a large effect size (Hedges’ g = 6.71), this should be regarded with caution to not overgeneralise. As the primacy of this research was to demonstrate “proof of concept,” the evidence from this study suggests potential considerations for both scalability and progression to a clinical population with a distinct diagnosis such as PTSD or complex PTSD. For this reason, future research should utilise both an experimental design and a clinical population, both of which would potentially deliver a more realistic treatment effect size.
To the best of our knowledge, this is the first EMDR therapy study that has examined both ACEs and BCEs. The most significant ACEs were emotional neglect, exposure to household mental illness, and psychological abuse up to 18 years of age. However, exposure to physical abuse by the mother and criminal behaviour in the household, with exposure to physical abuse and physical neglect, presented as the more prevalent ACEs in this research population.
The BCEs highlighted positive early life experiences in adults who built resilience and provided a counterbalance to ACEs. These positive childhood experiences include effective caregiving, quality parenting, close relationships with other significant adults, effective schooling, and community. Higher BCEs are associated with more favourable long-term development (Masten, 2014). Within the participant group, the most decisive factors included having at least one good friend, at least one teacher who cared, opportunities to have a good time, and a predictable home routine. Although the data set indicates high levels of BCEs, caution is required as the study participants were highly trained mental health professionals and are not a clinical population. Other interesting observable aspects from the dataset highlight a dichotomy between having an adult (other than a caregiver) who could support and advice and liking or feeling comfortable with oneself. More research is needed to understand further the impact that ACEs and BCEs have on and explore further if and how BCEs act as a potential resilience to counteract the impact of ACEs. However, the results of this study highlight that trauma processing occurred using VB2Tr irrespective of the research participants’ ACE or BCE scores.
Regarding testing hypotheses 1 through 4, the results from the study indicate a treatment effect from using the remotEMDR software to carry out VB2Tr as a VCP. Although the alterations in SUD and VOC are highly consistent with the more comprehensive empirical support for EMDR therapy, the data highlighting personal changes to the characteristics of the pathogenic memory targeted from processing is undoubtedly intriguing. Again, caution is necessary as the sample size is relatively small and would need further testing with a clear clinical population with a more formal medico-legal diagnosis.
In testing hypothesis 3, relevance, the results for disclosure (90%) appear consistent with the previous B2T study in Northern Iraq (Farrell et al., 2020), highlighting a clear clinical benefit in using both B2T and VB2Tr EMDR therapy protocols. This VB2Tr study adds to the literature demonstrating equal effectiveness and suggests a potential correlation between non-disclosure and the level of SUD. Desensitisation and reprocessing of the pathogenic memory increase the probability of disclosure with results of 87.5% for this VB2Tr study. The clinical advantages of this make this an effective tool for use as a trauma treatment intervention, highlighting a distinct benefit of using EMDR therapy for undisclosed trauma memories compared to other trauma-focussed interventions. Again, caution is required as further research is needed to investigate this aspect.
The use of three additional subjective measures, namely, MI, MV, and ME, within this study suggests an argument for including these within the EMDR therapy B2T and the VB2Tr protocol, but also within the standard protocol. These measures appear particularly useful in understanding the subjective experience of the trauma memory targeted for processing. Further research and investigation are needed to pursue this argument further.
Although this was only a 1-treatment session study, the data set reveals an interesting health economic argument, with an average session cost of £56.49 (€66.36). Although the study yielded modest economic savings of £2.47 (€2.91) per session, the cumulative implications of this, in addition to the clinical benefits, suggest a particularly compelling argument.
As indicated earlier, there are two major flaws in this study. First, the research participant group, although frontline mental health workers working under extraordinary circumstances, is not a non-clinical population. However, in mitigation, this is a “proof of concept” study. Second, relating to methodology, this was a straightforward pre-test–post-test research design. A future study would need to utilise a more robust experimental framework. However, results from this study suggest a more empirical foundation upon which future studies can build. As the study involved non-disclosure of trauma memory, randomisation was not possible for both ethical and moral reasons. Scaling up to a full randomised control study would not be possible; however, a quasi-experimental design would be a viable alternative.
To summarise, the research results suggest VB2Tr EMDR therapy to be an effective, fit-for-purpose, safe-to-use trauma treatment intervention. Additionally, the results highlight its clinical relevance and applicability as a trauma intervention. Furthermore, the remotEMDR software provided a highly effective platform for delivering EMDR therapy as a VCP. Although the researchers acknowledge that other platforms exist, results from this study are based entirely on remotEMDR.
Conclusion
This research study demonstrated encouraging evidence in support of EMDR therapy as VCP in treating a pathogenic (trauma) memory. In addition, the study explored specific factors influenced by the treatment intervention. The results of this study highlight the potential of using EMDR therapy, in this case using the B2T protocol as a VCP. Furthermore, results suggest the intervention has clinical applicability. Caution does need to be exercised regarding both the lack of a clinical population and the need for a more experimental design. However, results from this study demonstrate “proof of concept.”
However, to have an intervention that appears effective with either shame-based or fear-based trauma memories suggests great potential regarding clinical applicability. To have such an intervention that works on trauma memories that clients are unwilling to disclose due to fear, blame, or prejudice suggests distinct advantages for EMDR therapy in the repertoire of empirically supported trauma treatment interventions. Furthermore, to have such an intervention that appears safe and effective adds more temerity to this assertion. This study highlights how the VB2Tr EMDR therapy scripted protocol alters core characteristics of the pathogenic memory itself, including memory disturbance, emotionality, intensity, and vividness. The results also demonstrate that these changes occur irrespective of either ACEs or BCEs. Another critical finding relates to resilience and post-traumatic growth factors more powerful when considering a stark choice for clients, such as disclosure of the memory or no treatment, they choose no treatment. Providing a credible alternative in this critical decision-making juncture suggests distinct clinical benefits and applicability. Potential health efficiency arguments highlighted by this research are tentative yet worthy of further investigation and critical consideration.
It does need to be acknowledged that psychological treatment through the medium of videoconferencing may not suit some people. These reasons may be technological, safety factors, security, and/or individual choice. Understandably, this must be respected and accommodated. This study highlights that when individuals are given a choice between “disclosure” or “no treatment,” the research participants in this study chose the latter and not the former. This raises an interesting ethical question: is it better to do something, than nothing? Being able to offer clients greater choice is essential. In a world of increasing uncertainty and insecurity, the need for having suitable, evidence-based alternatives to “in-person” is paramount.
In summary, these results demonstrate proof of concept and put forward the case for further research and investigation. The stage 2 aspect of the study will further test the EMDR intervention as a VCP with a defined, clinical control group. The research supports the case for EMDR therapy as a credible treatment when used as a VCP.
The COVID-19 pandemic has challenged existing mental health and psychology services enormously. As the global burden of psychological trauma continues unabated, and we remain in an environment of scarcity in resources, any intervention that provides distinct choice and effectiveness in treating shame- or fear-based memories is a compelling argument, and much-needed treatment approach. The EMDR therapy “Blind 2 Therapist” appears to be a distinctly helpful psychotherapeutic tool in this endeavour. The fact that such an intervention has the potential health efficiency benefits strengthens this argument further. Any intervention, virtual or not, which improves accessibility and reach must be welcomed.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The EMDR therapy Virtual Blind 2 therapist (VB2Tr) protocol used for the study is available at: https://trnireland.ie/. Additional original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the University of Worcester, Worcester, United Kingdom. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DF conceived the study, carried out the VB2Tr treatment sessions, and was the chief investigator for the project. LK, PM, and ZZ were part of the research team, acquired the FU date, and conducted the qualitative interviews. AF, DF, and MK carried out the data analysis. The primary author was the principal investigator. All authors contributed to the overall article and approved the submitted version for publication.
Conflict of interest
NG is the co-founder and CEO of remotEMDR. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
References
1
Aafjes-van DoornK.BékésV.ProutT. A. (2021). Grappling with our therapeutic relationship and professional self-doubt during COVID-19: will we use video therapy again?Counsell. Psychol. Quarterly34473–484. 10.1080/09515070.2020.1773404
2
AciernoR.GrosD. F.RuggieroK. J.Hernandez-TejadaM. A.KnappR. G.LejuezC. W.et al (2016). Behavioral activation and therapeutic exposure for posttraumatic stress disorder: a noninferiority trial of treatment delivered in person versus home-based telehealth. Depress. Anxiety33, 415–423. 10.1002/da.22476
3
AciernoR. (2017). A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: in person versus home-based telehealth.Behav. Res. Therapy8957–65. 10.1016/j.brat.2016.11.009
4
AfifiT. O.TaillieuT.SalmonS.DavilaI. G.Stewart-TufescuA.FortierJ.et al (2020). Adverse childhood experiences (ACEs), peer victimization, and substance use among adolescents.Child Abuse Neglect106:104504. 10.1016/j.chiabu.2020.104504
5
American Psychological Society (2017). Clinical Practice Guideliness for the Treatment of PTSD.Washington, DC: APA.
6
AndersonP.RothbaumB. O.HodgesL. F. (2003). Virtual reality exposure in the treatment of social anxiety.Cogn. Behav. Practice10240–247. 10.1016/S1077-7229(03)80036-6
7
AndradeJ.KavanaghD.BaddeleyA. (1997). Eye-movements and visual imagery: a working memory approach to the treatment of post-traumatic stress disorder.Br. J. Clin. Psychol.36209–223. 10.1111/j.2044-8260.1997.tb01408.x
8
AronsonK. R.PerkinsD. F.MorganN. R.BleserJ. A.VogtD.CopelandL. A.et al (2020). The impact of adverse childhood experiences (ACEs) and combat exposure on mental health conditions among new post-9/11 veterans.Psychol. Trauma: Theory Res. Practice Policy12698–706. 10.1037/tra0000614
9
BackhausA.AghaZ.MaglioneM. L.ReppA.RossB.ZuestD.et al (2012). Videoconferencing psychotherapy: a systematic review.Psychol. Serv.9111–131. 10.1037/a0027924
10
BañosR. M.EtchemendyE.MiraA.RivaG.GaggioliA.BotellaC. (2017). Online positive interventions to promote well-being and resilience in the adolescent population: a narrative review.Front. Psychiatry8:10. 10.3389/fpsyt.2017.00010
11
BarakA.HenL.Boniel-NissimM.ShapiraN. (2008). A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions.J. Technol. Hum. Services26109–160. 10.1080/15228830802094429
12
BellisM. A.HardcastleK.FordK.HughesK.AshtonK.QuiggZ.et al (2017). Does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences - a retrospective study on adult health-harming behaviours and mental well-being.BMC Psychiatry17:110. 10.1186/s12888-017-1260-z
13
BellisM. A.HughesK.FordK.Ramos RodriguezG.SethiD.PassmoreJ. (2019). Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis.Lancet Public Health4e517–e528. 10.1016/S2468-2667(19)30145-8
14
BellisM. A.HughesK.LeckenbyN.HardcastleK. A.PerkinsC.LoweyH. (2015). Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey.J. Public Health37445–454. 10.1093/pubmed/fdu065
15
BellisM. A.HughesK.LeckenbyN.JonesL.BabanA.KachaevaM.et al (2014a). Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries.Bull. World Health Organ.92641–655. 10.2471/BLT.13.129247
16
BellisM. A.LoweyH.LeckenbyN.HughesK.HarrisonD. (2014b). Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population.J. Public Health (United Kingdom)3681–91. 10.1093/pubmed/fdt038
17
Bennett-LevyJ.LeeN. K. (2014). Self-practice and self-reflection in cognitive behaviour therapy training: what factors influence trainees’ engagement and experience of benefit?Behav. Cogn. Psychotherapy4248–64. 10.1017/S1352465812000781
18
BergerT. (2017). The therapeutic alliance in internet interventions: a narrative review and suggestions for future research.Psychotherapy Res.27511–524. 10.1080/10503307.2015.1119908
19
BerryhillM. B.CulmerN.WilliamsN.Halli-TierneyA.BetancourtA.RobertsH.et al (2019). Videoconferencing psychotherapy and depression: a systematic review.Telemed. e-Health25435–446. 10.1089/tmj.2018.0058
20
BerryhillM. B.Halli-TierneyA.CulmerN.WilliamsN.BetancourtA.KingM.et al (2018). Videoconferencing psychological therapy and anxiety: a systematic review.Family Practice3653–63. 10.1093/fampra/cmy072
21
BissonJ. I.BerlinerL.CloitreM.ForbesD.JensenT. K.LewisC.et al (2019). The international society for traumatic stress studies new guidelines for the prevention and treatment of posttraumatic stress disorder: methodology and development process.J. Trauma Stress32475–483. 10.1002/jts.22421
22
BoltonP.BassJ. K.ZanganaS. A. S.KamalT.MurrayM. M. I.KaysenD.et al (2014). A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan. Northern Iraq.BMC Psychiatry14:360. 10.1186/s12888-014-0360-2
23
BongaertsH.VoorendonkE. M.van MinnenA.de JonghA. (2021). Safety and effectiveness of intensive treatment for complex PTSD delivered via home-based telehealth.Eur. J. Psychotraumatol.12:1860346. 10.1080/20008198.2020.1860346
24
BrownD. W.AndaR. F.TiemeierH.FelittiV. J.EdwardsV. J.CroftJ. B.et al (2009). Adverse childhood experiences and the risk of premature mortality.Am. J. Prev. Med.37389–396. 10.1016/j.amepre.2009.06.021
25
BurkeN. J.HellmanJ. L.ScottB. G.WeemsC. F.CarrionV. G. (2011). The impact of adverse childhood experiences on an urban pediatric population.Child Abuse Negl.35408–413. 10.1016/j.chiabu.2011.02.006
26
ChigwedereC.Bennett-LevyJ.FitzmauriceB.DonohoeG. (2020). Personal practice in counselling and CBT trainees: the self-perceived impact of personal therapy and self-practice/self-reflection on personal and professional development.Cogn. Behav. Therapy50422–438. 10.1080/16506073.2020.1846608
27
Christopher FruehB.GrubaughA. L.ElhaiJ. D.BuckleyT. C. (2007). US department of veterans affairs disability policies for posttraumatic stress disorder: administrative trends and implications for treatment, rehabilitation, and research.Am. J. Public Health972143–2145. 10.2105/AJPH.2007.115436
28
ClappJ. D.KempJ. J.CoxK. S.TuerkP. W. (2016). Patterns of change in response to prolonged exposure: implications for treatment outcome.Depress. Anxiety33807–815. 10.1002/da.22534
29
CollardJ.ClarkeM. (2020). Experiential learning for trainee therapists through a shame attack exercise.Cogn. Behav. Therapist13. 1–16.
30
CrandallA. (2019). ACEs and counter-ACEs: how positive and negative childhood experiences influence adult health.Child Abuse Neglect.96:104089. 10.1016/j.chiabu.2019.104089
31
CrandallA. (2020). The influence of adverse and advantageous childhood experiences during adolescence on young adult health.Child Abuse Neglect.108:104644. 10.1016/j.chiabu.2020.104644
32
CroweM.InderM.FarmarR.CarlyleD. (2020). Delivering psychotherapy by video conference in the time of COVID-19: some considerations.J. Psychiatric Mental Health Nurs.28751–752. 10.1111/jpm.12659
33
CullenW.GulatiG.KellyB. D. (2020). Mental health in the COVID-19 pandemic.QJM113311–312.
34
de JonghA.AmannB. L.HofmannA.FarrellD.LeeC. W. (2019a). The status of EMDR therapy in the treatment of posttraumatic stress disorder 30 years after its introduction.J. EMDR Practice Res.13261–269. 10.1891/1933-3196.13.4.261
35
de JonghA.BicanicI.MatthijssenS.AmannB. L.HofmannA.FarrellD.et al (2019b). The current status of EMDR therapy involving the treatment of complex posttraumatic stress disorder.J. EMDR Practice Res.13284–290. 10.1891/1933-3196.13.4.284
36
de JonghA.GroenlandG. N.SanchesS.BongaertsH.VoorendonkE. M.van MinnenA. (2020). The impact of brief intensive trauma-focused treatment for PTSD on symptoms of borderline personality disorder.Eur. J. Psychotraumatol.11:1721142. 10.1080/20008198.2020.1721142
37
DoomJ. R.SeokD.NarayanA. J.FoxK. R. (2021). Adverse and benevolent childhood experiences predict mental health during the COVID-19 pandemic.Adv. Resilience Sci.2193–204. 10.1007/s42844-021-00038-6
38
DoresA. R.GeraldoA.CarvalhoI. P.BarbosaF. (2020). The use of new digital information and communication technologies in psychological counseling during the COVID-19 pandemic.Int. J. Environ. Res. Public Health17:7663. 10.3390/ijerph17207663
39
EngelhardI. M.van den HoutM. A.JanssenW. C.van der BeekJ. (2010). Eye movements reduce vividness and emotionality of “flashforwards”.Behav. Res. Ther.48442–447. 10.1016/j.brat.2010.01.003
40
FarrellD.ReidK. (2020). Eye Movement Desensitization and Reprocessing (EMDR) Therapy Scripted Protocols and Summary Sheets.New York, NY: Springer publishing.
41
FarrellD.KiernanM. D.de JonghA.MillerP. W.BumkeP.AhmadS.et al (2020). Treating implicit trauma: a quasi-experimental study comparing the EMDR Therapy Standard Protocol with a ‘Blind 2 Therapist’ version within a trauma capacity building project in Northern Iraq.J. Int. Human. Act.5:3.
42
FelittiV. J. (2010). “The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: implications for healthcare,” in The Hidden Epidemic: The Impact of Early Life Trauma on Health and Disease, edsLaniusR.VermettenE. (New York, NY: Cambridge University Press).
43
FelittiV. J.AndaR. F.NordenbergD.WilliamsonD. F.SpitzA. M.EdwardsV.et al (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study.Am. J. Prev. Med.14245–258. 10.1016/s0749-3797(98)00017-8
44
FinkelhorD. (2020). Trends in adverse childhood experiences (ACEs) in the United States.Child Abuse Negl.108:104641. 10.1016/j.chiabu.2020.104641
45
FortneyJ. C.PyneJ. M.KimbrellT. A.HudsonT. J.RobinsonD. E.SchneiderR.et al (2015). Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial.JAMA Psychiatry7258–67. 10.1001/jamapsychiatry.2014.1575
46
GermainV.MarchandA.BouchardS.GuayS.DrouinM. S. (2010). Assessment of the therapeutic alliance in face-to-face or videoconference treatment for posttraumatic stress disorder.Cyberpsychol. Behav. Soc. Network.1329–35. 10.1089/cyber.2009.0139
47
GhebreyesusT. A. (2020). Addressing mental health needs: an integral part of COVID-19 response.World Psychiatry19129–130. 10.1002/wps.20768
48
GrubbsK. M.FortneyJ. C.PyneJ. M.HudsonT.MooreW. M.CusterP.et al (2015). Predictors of initiation and engagement of cognitive processing therapy among veterans with PTSD enrolled in collaborative care.J. Trauma Stress28580–584. 10.1002/jts.22049
49
GunterR. W.BodnerG. E. (2008). How eye movements affect unpleasant memories: support for a working-memory account.Behav. Res. Ther.46913–931. 10.1016/j.brat.2008.04.006
50
HaseM.BalmacedaU. M.OstacoliL.LiebermannP.HofmannA. (2017). The AIP model of EMDR therapy and pathogenic memories.Front. Psychol.8:1578. 10.3389/fpsyg.2017.01578
51
Hernandez-TejadaM. A.ZollerJ. S.RuggieroK. J.KazleyA. S.AciernoR. (2014). Early treatment withdrawal from evidence-based psychotherapy for PTSD: telemedicine and in-person parameters.Int. J. Psychiatry Med.4833–55. 10.2190/PM.48.1.d
52
HoffmanL. (2021). Existential–Humanistic therapy and disaster response: lessons from the COVID-19 pandemic.J. Human. Psychol.6133–54. 10.1177/0022167820931987
53
IslamT.PitafiA. H.AryaV.WangY.AkhtarN.MubarikS.et al (2021). Panic buying in the COVID-19 pandemic: a multi-country examination.J. Retail. Consumer Serv.59:102357. 10.1016/j.jretconser.2020.102357
54
ISTSS (2018). ISTSS Posttraumatic Stress Disorder Prevention and Treatment Guidelines Methodology and Recommendations.Chicago, IL: ISTSS.
55
KaratziasT.MurphyP.CloitreM.BissonJ.RobertsN.ShevlinM.et al (2019). Psychological interventions for ICD-11 complex PTSD symptoms: systematic review and meta-analysis.Psychol. Med.491761–1775. 10.1017/S0033291719000436
56
KaratziasT.ShevlinM.FyvieC.GrandisonG.GaroziM.LathamE.et al (2020). Adverse and benevolent childhood experiences in Posttraumatic Stress Disorder (PTSD) and complex PTSD (CPTSD): implications for trauma-focused therapies.Eur. J. Psychotraumatol.11:1793599. 10.1080/20008198.2020.1793599
57
KaryotakiE.EbertD. D.DonkinL.RiperH.TwiskJ.BurgerS.et al (2018a). Do guided internet-based interventions result in clinically relevant changes for patients with depression? an individual participant data meta-analysis.Clin. Psychol. Rev.6380–92. 10.1016/j.cpr.2018.06.007
58
KaryotakiE.KemmerenL.RiperH.TwiskJ.HoogendoornA.KleiboerA.et al (2018b). Is self-guided internet-based cognitive behavioural therapy (iCBT) harmful? an individual participant data meta-analysis.Psychol. Med.482456–2466. 10.1017/S0033291718000648
59
KavoorA. R. (2020). COVID-19 in people with mental illness: challenges and vulnerabilities.Asian J. Psychiatry51:102051. 10.1016/j.ajp.2020.102051
60
KhanK. S.MamunM. A.GriffithsM. D.UllahI. (2020). The mental health impact of the COVID-19 pandemic across different cohorts.Int. J. Mental Health Add. Online ahead of print. 10.1007/s11469-020-00367-0
61
KimP.ThomasJ.WilkJ.CastroC.HogeC. (2010). Stigma, barriers to care, and use of mental health services among active duty and national guard soldiers after combat.Psychiatric Services61582–588. 10.1176/appi.ps.61.6.582
62
KumarA.NayarK. R. (2020). COVID 19 and its mental health consequences.J. Mental Health301–2. 10.1080/09638237.2020.1757052
63
LeerA.EngelhardI. M. (2020). Side effects of induced lateral eye movements during aversive ideation.J. Behav. Therapy Exp. Psychiatry68:101566. 10.1016/j.jbtep.2020.101566
64
LightstoneA. J.BaileyS. K.VorosP. (2015). Collaborative music therapy via remote video technology to reduce a veteran’s symptoms of severe, chronic PTSD.Arts Health7123–136. 10.1080/17533015.2015.1019895
65
LocascioJ. J.AtriA. (2011). An overview of longitudinal data analysis methods for neurological research.Dementia Geriatric Cogn. Disorders Extra1330–357. 10.1159/000330228
66
LuxtonD. D.PruittL. D.O’BrienK.KramerG. (2015). An evaluation of the feasibility and safety of a home-based telemental health treatment for posttraumatic stress in the US military.Telemed. E-Health21880–886. 10.1089/tmj.2014.0235
67
MaieritschK. P.SmithT. L.HessingerJ. D.AhearnE. P.EickhoffJ. C.ZhaoQ. (2016). Randomized controlled equivalence trial comparing videoconference and in person delivery of cognitive processing therapy for PTSD.J. Telemed. Telecare22238–243. 10.1177/1357633X15596109
68
MaltiT. (2020). Kindness: a perspective from developmental psychology.Eur. J. Dev. Psychol.18629–657. 10.1080/17405629.2020.1837617
69
MastenA. S. (2014). Global perspectives on resilience in children and youth.Child Dev.856–20. 10.1111/cdev.12205
70
MatthijssenS. J. M. A.BrouwersT. C.van den HoutM. A.KlugkistI. G.de JonghA. (2021). A randomized controlled dismantling study of Visual Schema Displacement Therapy (VSDT) vs an abbreviated EMDR protocol vs a non-active control condition in individuals with disturbing memories.Eur. J. Psychotraumatol.12:1883924. 10.1080/20008198.2021.1883924
71
MaxfieldL.MelnykW. T.HaymanG. C. A. (2008). A working memory explanation for the effects of eye movements in EMDR.J. EMDR Practice Res.2247–261. 10.1891/1933-3196.2.4.247
72
MaxfieldL.StickgoldR.SmythN. J. (2018). EMDR Fidelity Rating Scale (EFRS).Grafton, WI: EMDR Research Foundation.
73
MerrickJ. S.NarayanA. J. (2020). Assessment and screening of positive childhood experiences along with childhood adversity in research, practice, and policy.J. Children Poverty26269–281. 10.1080/10796126.2020.1799338
74
MerrickJ. S.NarayanA. J.DePasqualeC. E.MastenA. S. (2019). Benevolent Childhood Experiences (BCEs) in homeless parents: a validation and replication study.J. Fam. Psychol.33493–498. 10.1037/fam0000521
75
MorlandL. A.HynesA. K.MacKintoshM. A.ResickP. A.ChardK. M. (2011). Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort.J. Trauma Stress24465–469. 10.1002/jts.20661
76
MyersK. M.ValentineJ. M.MelzerS. M. (2008). Child and adolescent telepsychiatry: utilization and satisfaction.Telemed. E-Health14131–137. 10.1089/tmj.2007.0035
77
NarayanA. J.IppenC. G.HarrisW. W.LiebermanA. F. (2017). Assessing angels in the nursey: a pilot study of childhood memories of benevolent caregiving as protective influences.Infant Mental Health J.38461–474. 10.1002/imhj.21653
78
NarayanA. J.RiveraL. M.BernsteinR. E.HarrisW. W.LiebermanA. F. (2018). Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: a pilot study of the benevolent childhood experiences (BCEs) scale.Child Abuse Neglect.7819–30. 10.1016/j.chiabu.2017.09.022
79
OlthuisJ. V.WattM. C.BaileyK.HaydenJ. A.StewartS. H. (2016a). Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults.Cochrane Database Systematic Rev.3:CD011565. 10.1002/14651858.CD011565.pub2
80
OlthuisJ. V.WozneyL.AsmundsonG. J. G.CrammH.Lingley-PottieP.McGrathP. J. (2016b). Distance-delivered interventions for PTSD: a systematic review and meta-analysis.J. Anxiety Disord.449–26. 10.1016/j.janxdis.2016.09.010
81
OsenbachJ. E.O’BrienK. M.MishkindM.SmolenskiD. J. (2013). Synchronous telehealth technologies in psychotherapy for depression: a meta-analysis.Depress. Anxiety301058–1067. 10.1002/da.22165
82
RousmaniereT.AbbassA.FredericksonJ.HenningI.TaubnerS. (2014). Videoconference for psychotherapy training and supervision: two case examples.Am. J. Psychotherapy68231–250. 10.1176/appi.psychotherapy.2014.68.2.231
83
RuskinP. E.Silver-AylaianM.KlingM. A.ReedS. A.BradhamD. D.HebelJ. R.et al (2004). Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment.Am. J. Psychiatry1611471–1476. 10.1176/appi.ajp.161.8.1471
84
SchubertS. J.LeeC. W.DrummondP. D. (2011). The efficacy and psychophysiological correlates of dual-attention tasks in eye movement desensitization and reprocessing (EMDR).J. Anxiety Disord.251–11. 10.1016/j.janxdis.2010.06.024
85
SchubertS. J.LeeC. W.DrummondP. D. (2016). Eye movements matter, but why? psychophysiological correlates of EMDR therapy to treat trauma in timor-leste.J. EMDR Practice Res.1070–81. 10.1891/1933-3196.10.2.70
86
ScottJ.YapK.BunchK.HaarhoffB.PerryH.Bennett-LevyJ. (2021). Should personal practice be part of cognitive behaviour therapy training? results from two self-practice/self-reflection cohort control pilot studies.Clin. Psychol. Psychotherapy28150–158. 10.1002/cpp.2497
87
ShapiroF. (1995). Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures.New York, NY: Guilford Press.
88
ShapiroF. (2001). Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures, 2nd Edn. New York, NY: Guilford Press.
89
ShapiroF. (2018). “Eye movement desensitization and reprocessing (EMDR) therapy,” in Basic Principles, Protocols, and Procedures, Edn 3 Edn, (New York, NY: Guilford Press). 10.1186/s13063-019-3760-2
90
SimpsonS. G.ReidC. L. (2014). Therapeutic alliance in videoconferencing psychotherapy: a review.Australian J. Rural Health22280–299.
91
StarbirdA. D.StoryP. A. (2020). Consequences of childhood memories: narcissism, malevolent, and benevolent childhood experiences.Child Abuse Negl.108:104656. 10.1016/j.chiabu.2020.104656
92
StrachanM.GrosD. F.YuenE.RuggieroK. J.FoaE. B.AciernoR. (2012). Home-based telehealth to deliver evidence-based psychotherapy in veterans with PTSD.Contemporary Clin. Trials33402–409. 10.1016/j.cct.2011.11.007
93
StruckS.Stewart-TufescuA.AsmundsonA. J. N.AsmundsonG. G. J.AfifiT. O. (2021). Adverse childhood experiences (ACEs) research: a bibliometric analysis of publication trends over the first 20 years.Child Abuse Neglect.112:104895. 10.1016/j.chiabu.2020.104895
94
TaleviD.SocciV.CaraiM.CarnaghiG.FaleriS.TrebbiE.et al (2020). Mental health outcomes of the covid-19 pandemic.Rivista Di Psichiatria55137–144. 10.1708/3382.33569
95
TodderD.KaplnZ. (2007). Rapid eye movements for acute stress disorder using video conference communication.Telemed. E-Health13461–463. 10.1089/tmj.2006.0058
96
TodderD.MatarM.KaplanZ. (2007). Acute-phase trauma intervention using a videoconference link circumvents compromised access to expert trauma care.Telemed. J. E-Health1365–67. 10.1089/tmj.2006.0039
97
TuerkP. W.KellerS. M.AciernoR. (2018). Treatment for anxiety and depression via clinical videoconferencing: evidence base and barriers to expanded access in practice.FOCUS16363–369. 10.1176/appi.focus.20180027
98
TurgooseD.AshwickR.MurphyD. (2018). Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder.J. Telemed. Telecare24575–585. 10.1177/1357633X17730443
99
UsherK.DurkinJ.BhullarN. (2020). The COVID-19 pandemic and mental health impacts.Int. J. Mental Health Nurs.29315–318. 10.1111/inm.12726
100
Valiente-GómezA.Moreno-AlcázarA.TreenD.CedrónC.ColomF.PérezV.et al (2017). EMDR beyond PTSD: a systematic literature review.Front. Psychol.8:1668. 10.3389/fpsyg.2017.01668
101
van den HoutM. A.EngelhardI. M.BeetsmaD.SlofstraC.HornsveldH.HoutveenJ.et al (2011). EMDR and mindfulness. eye movements and attentional breathing tax working memory and reduce vividness and emotionality of aversive ideation.J. Behav. Therapy Exp. Psychiatry42423–431. 10.1016/j.jbtep.2011.03.004
102
van der KolkB. A. (2003). Psychological Trauma.Washington, DC: American Psychiatric Pub.
103
van der KolkB. A. (2007). A randomized clinical trial of eye movement desensitization and reprocessing (EMDR), fluoxetine, and pill placebo in the treatment of posttraumatic stress disorder: treatment effects and long-term maintenance.J. Clin. Psychiatry6837–46. 10.4088/jcp.v68n0105
104
van der KolkB. A. (2015). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma.London: Penguin Books.
105
ViswanathanR.MyersM. F.FanousA. H. (2020). Support groups and individual mental health care via video conferencing for frontline clinicians during the COVID-19 pandemic.Psychosomatics61538–543. 10.1016/j.psym.2020.06.014
106
WattsS.MarchandA.BouchardS.GosselinP.LangloisF.BellevilleG.et al (2020). Telepsychotherapy for generalized anxiety disorder: impact on the working alliance.J. Psychotherapy Int.30208–225. 10.1037/int0000223
107
WeinbergH. (2020a). Online group psychotherapy: challenges and possibilities during COVID-19-A practice review.Group Dyn.24201–211. 10.1037/gdn0000140
108
WeinbergH. (2020b). Online group psychotherapy: challenges and possibilities during COVID-19—a practice review.Group Dyn. Theory Res. Practice24201–211.
109
WellsS. Y.MorlandL. A.WilhiteE. R.GrubbsK. M.RauchS. A. M.AciernoR.et al (2020). Delivering prolonged exposure therapy via videoconferencing during the COVID-19 pandemic: an overview of the research and special considerations for providers.J. Trauma Stress33380–390. 10.1002/jts.22573
110
WildJ.Warnock-ParkesE.GreyN.StottR.WiedemannM.CanvinL.et al (2016). Internet-delivered cognitive therapy for PTSD: a development pilot series.Eur. J. Psychotraumatol.7:10.3402/ejpt.v7.31019. 10.3402/ejpt.v7.31019
111
WindT. R.RijkeboerM.AnderssonG.RiperH. (2020a). The COVID-19 pandemic: the ‘black swan’ for mental health care and a turning point for e-health.Int. Intervent.20:100317. 10.1016/j.invent.2020.100317
112
WindT. R.RijkeboerM.AnderssonG.RiperH. (2020b). The COVID-19 pandemic: the ‘black swan’ for mental health care and a turning point for e-health.Int. Intervent.20:100317. 10.1016/j.invent.2020.100317
113
WolpeJ.LazarusA. A. (1966). Behavior Therapy Techniques: A Guide to the Treatment of Neuroses.New York, USA.
114
World Health Organisation (2020). Mental Health and Psychosocial Considerations During the COVID-19 Outbreak, 18 March 2020:(No. WHO/2019-nCoV/MentalHealth/2020.1).Geneva: World Health Organization.
115
WrightJ. H.CaudillR. (2020). Remote treatment delivery in response to the COVID-19 pandemic.Psychotherapy Psychosomat.89130–132. 10.1159/000507376
116
YuenE. K. (2015). Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results.J. Clin. Psychol.71500–512. 10.1002/jclp.22168
Summary
Keywords
EMDR therapy, pathogenic memory, adverse and benevolent childhood experiences, videoconference psychotherapy, Blind 2 Therapist
Citation
Farrell D, Fadeeva A, Zat Z, Knibbs L, Miller P, Barron I, Matthess H, Matthess C, Gazit N and Kiernan MD (2022) A Stage 1 Pilot Cohort Exploring the Use of EMDR Therapy as a Videoconference Psychotherapy During COVID-19 With Frontline Mental Health Workers: A Proof of Concept Study Utilising a Virtual Blind 2 Therapist Protocol. Front. Psychol. 13:901855. doi: 10.3389/fpsyg.2022.901855
Received
22 March 2022
Accepted
19 April 2022
Published
06 July 2022
Volume
13 - 2022
Edited by
Antonio Onofri, Azienda Sanitaria Locale Roma 1, Italy
Reviewed by
Sara Ugolini, Centro Clinico De Sanctis, Italy; Mo MirMotahari, King’s College London, United Kingdom
Updates
Copyright
© 2022 Farrell, Fadeeva, Zat, Knibbs, Miller, Barron, Matthess, Matthess, Gazit and Kiernan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Derek Farrell, d.farrell@worc.ac.uk
This article was submitted to Psychology for Clinical Settings, a section of the journal Frontiers in Psychology
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.