- 1Centre for Social and Early Emotional Development, School of Psychology, Deakin University, Geelong, VIC, Australia
- 2Neami National, Preston, VIC, Australia
- 3Eastern Health, Box Hill, VIC, Australia
- 4Department of Paediatrics, University of Melbourne, Parkville, VIC, Australia
- 5Centre for Adolescent Health, Murdoch Children’s Research Institute, Parkville, VIC, Australia
Introduction: The COVID-19 pandemic has led to significant challenges for frontline healthcare workers’ (FHW), raising many mental health and wellbeing concerns for this cohort. To facilitate identification of risk and protective factors to inform treatment and interventions, this study investigated key predictors of psychological distress and subjective wellbeing in FHWs.
Methods: During the Omicron wave of the COVID-19 pandemic (January 2022), Victorian (Australia) doctors, nurses, allied health and non-medical staff from Emergency Departments, Intensive Care units, Aged Care, Hospital In The Home, and COVID Wards completed a cross-sectional survey consisting of the Kessler 6 item (Psychological Distress), Personal Wellbeing Index (Subjective Wellbeing), Coronavirus Health Impact Survey tool (COVID-19 related factors) and occupational factors. Multivariable linear regressions were used to evaluate unadjusted and adjusted associations. Relative weight analysis was used to compare and identify key predictors.
Results: Out of 167 participants, 18.1% screened positive for a probable mental illness and a further 15.3% screened positive for low wellbeing. Key risk factors for greater psychological distress included COVID infection worries, relationship stress and younger age. For both psychological distress and lower wellbeing, health status and supervisor support were key protective factors, while infection risks were key risk factors. Only positive changes in relationship quality was protective of lower wellbeing.
Conclusion: This study highlights the significance of social determinants and individual level factors alongside work related factors, in influencing FHWs’ mental health and wellbeing during public health crises, such as the COVID-19 pandemic. Findings suggest that future interventions and supports should take a more holistic approach that considers work, social and individual level factors when supporting FHWs’ mental health and wellbeing.
Introduction
Since the beginning of the COVID-19 pandemic, healthcare systems have been under significant pressure, leading to unprecedented challenges for healthcare workers worldwide. During this time, high rates of COVID-19 infections have led to concerning surges in hospital admissions (Verelst et al., 2020; Berger et al., 2022). This has translated into an increased and prolonged risk of COVID-19 infection among healthcare workers (Nguyen et al., 2020; Quigley et al., 2021; World Health Organisation, 2021), as well as a surge in their workloads (Billings et al., 2021; Spányik et al., 2022) and a complete change in their working procedures (Digby et al., 2021; Hunt et al., 2022). Under these conditions, healthcare workers have been working under significant challenges, both physically and mentally.
Existing research suggests that working in hospitals during the pandemic have contributed to high rates of burnout (Magnavita et al., 2021), insomnia (Salari et al., 2020; Sahebi et al., 2021; Lee et al., 2023) and psychological distress. High prevalence of mental health disorders have also been documented in this cohort, such as depression (Yan et al., 2021; Lee et al., 2023), anxiety (Raoofi et al., 2021; Yan et al., 2021; Lee et al., 2023), and PTSD (Yan et al., 2021; Lee et al., 2023). Emerging evidence also links healthcare roles during the pandemic with a deterioration in overall wellbeing, suggesting that COVID-19 impacts on healthcare workers have spanned across multiple life domains during this time (McGuinness et al., 2022). This is concerning as COVID-19 outbreaks are persisting and continue to escalate the stress on healthcare systems worldwide (World Health Organisation, 2022), placing healthcare workers at high risk of continued and cumulative impacts on their mental health and wellbeing.
Healthcare workers working in frontline settings with high-risk COVID-19 infections may be particularly vulnerable, such as those working in emergency departments, intensive care units and COVID wards, as proximity to risk during disasters can significantly increase an individual’s vulnerability to mental illness (May and Wisco, 2016). Studies of coronavirus outbreaks support this contention, highlighting that healthcare workers directly caring for infected patients in frontline settings have high risks of mental health impacts (De Brier et al., 2020; Kisely et al., 2020; Muller et al., 2020). These findings were also consistent during the COVID-19 pandemic, with studies demonstrating that frontline healthcare workers (FHWs) experienced more anxiety, depression, and traumatic stress than their non-frontline counterparts (Lai et al., 2020; Wang et al., 2020; Kim and Lee, 2022). Long-term mental health consequences are also a concern as findings on past coronavirus outbreaks suggest that some FHWs can be affected up to 2 years after outbreaks (Liu et al., 2012; Galli et al., 2020; Chau et al., 2021). Given these findings, there is a clear need to identify FHWs at greatest risk and key predictors of their psychological distress and wellbeing to inform interventions and supports that are critical during the COVID-19 pandemic and future infectious disease outbreaks.
Most studies strongly support that work-related stressors are key predictors of psychological distress in FHWs during the COVID-19 pandemic, such as work-related infection risks, level of work experience and organisational support (De Brier et al., 2020; Kisely et al., 2020; al Falasi et al., 2021). Thus, recommendations and interventions for FHWs to date have largely revolved around workplace supports and enhancing infection control procedures. However, the impacts of the COVID-19 pandemic have been wide-ranging, and few have investigated other important determinants of FHWs’ mental health beyond work, such as social and pandemic related determinants. Studies on the general community have shown that pandemic and social stressors can also lead to significantly greater distress and lower wellbeing. These stressors include lockdowns (Westrupp et al., 2021a,b), community infection risks (Fitzpatrick et al., 2020; Kim et al., 2022) and relational impacts (Cassinat et al., 2021; Sheen et al., 2021; Wang et al., 2021). Emerging qualitative evidence also support these findings in FHWs, showing that these social stressors have placed significant burden on FHWs during the COVID-19 pandemic (Schaffer et al., 2022; Sheen et al., 2022). These findings, therefore, highlight the need to further our understanding of key predictors of psychological distress and wellbeing amongst FHWs during the COVID-19 pandemic that considers stressors beyond work, such as pandemic and social stressors.
Nevertheless, studies have largely been conducted early in the pandemic and there is currently a dearth of research on more recent waves of COVID-19 outbreaks, such as the Omicron wave. Updated findings is thus necessary, especially when the extended nature of the COVID-19 pandemic places FHWs at high risk of continued and cumulative mental health and wellbeing impacts. Continued understanding and investigation into key predictors of FHWs’ psychological distress and wellbeing during the COVID-19 pandemic is critical to inform and enhance the effectiveness of future interventions and facilitate targeted interventions for highly vulnerable FHWs, during the COVID-19 pandemic and in future infectious disease outbreaks.
Research aims
This study aimed to investigate key predictors of psychological distress and subjective wellbeing among FHWs during the COVID-19 pandemic. Specifically, this study aimed to examine to what extent did demographics, health factors, COVID-infection factors, occupational factors, lockdown stressors and relational factors have an effect on psychological distress and subjective wellbeing in FHWs during the COVID-19 pandemic.
Methods
This study followed and adhered to the reporting guidelines of the STROBE guidelines for cross-sectional studies (Supplementary File S1).
Study design
This study used cross-sectional data collected in the third timepoint of a longitudinal cohort study on FHWs’ working in Victoria, Australia. The data used in this study was collected between late January 2022 to early March 2022 using an online survey, administered on RedCap.
Recruitment
Participants were recruited state-wide in Victoria (Australia) from a large metropolitan health service (Eastern Health), and five major Australian healthcare associations: Australian medical association Vic (AMAVic), Australian Nursing and Midwifery Federation Vic (ANMFVic), Aged & Community Care Providers Association (ACCPA), Victorian Healthcare Association (VHA) and Health Services Union (HSU). Participants were eligible to participate if they worked in any capacity in Victorian (Australia) hospitals and in any of the following departments: the Emergency Departments, Intensive Care Units, COVID Wards, Hospital in the Home or Aged Care. These departments were chosen to represent frontline healthcare working sites and to recruit FHWs, as they posed the highest risk of COVID-19 infection in Victoria, Australia.
Ethics
Study and ethics approval (HEAG 2020-296) was obtained from Deakin University High Risk Ethics Committee, Eastern Health’s Ethics Committee, and all partnering healthcare associations prior to the commencement of recruitment and data collection. Participants provided their consent and voluntarily participated. To ensure confidentiality, participant’s data were all de-identified prior to data-analysis.
Context
During the data collection period, the general community were experiencing the easing of COVID-19 restrictions in Victoria, Australia (Premier of Victoria, 2022a). However, Victoria (Australia) was just coming out of the Omicron wave and largest ever surge of positive COVID-19 cases and hospitalisation since the start of the COVID-19 pandemic, which started in November and peaked in mid-January 2022 (State Government of Victoria, 2023). As such, the Victorian government declared a code brown emergency due to the influx of COVID-19 patients in hospitals (Premier of Victoria, 2022b). This meant that hospitals could configure or shutdown non-essential services to free staff, redeploy staff to higher priority departments, and ask staff to return from leave.
Measures
The survey collected data using individual items and scales from the Coronavirus Health Impact Survey tool (CRISIS) (Nikolaidis et al., 2021). Individual CRISIS items used in the survey included two demographic items: age and gender, two health related items: self-reported physical health and pre-COVID-19 mental health, two lockdown related items: self-reported stress with lockdown restrictions and time spent outdoors, and three COVID-infection related items: self-reported risk of infection from work, risk of infection from the community, and COVID-19 diagnosis.
A modified version of the COVID-19 infection worries scale from the CRISIS tool was also used in the survey. COVID-19 infection worries was measured using a validated scale score of four items measuring to what extent participants were worried about (1) being infected, (2) their family being infected, and the impacts of infection on their (3) mental health and (4) physical health. The original scale was found to have high internally consistency with a coefficient Omega of >0.8 and good unidimensionality (CFI > 0.95) (Nikolaidis et al., 2021). In our study, to reflect worries of infection more accurately, we removed the items that related to reading and talking about COVID-19, and hope that the pandemic will end soon. Our modified version had good internal consistency (McDonald’s ω = 0.88) and unidimensionality (CFI = 0.96).
To measure relational factors, two items from the CRISIS tool measuring (1) changes in relationship quality with regards to family and (2) changes in relationship quality with regards to social contacts were combined to avoid multi-collinearity in regression models and derive a single scale score of overall changes in relationship quality. This scale showed moderate internal consistency (McDonald’s ω = 0.60). Overall relationship stress was measured using a single scale score derived from the mean of two items measuring (1) relationship stress with regards to family and (2) relationship stress with regards to friends (5-point Likert scale, 1 = Not at all to 5 = Extremely). This scale showed good internal consistency (McDonald’s ω = 0.76).
To measure occupational factors, participants were asked to specify their occupation, whether they provided direct care to COVID-19 patients in the last 2 weeks, and a self-report rating of their supervisor’s support for mental health and wellbeing during the COVID-19 pandemic.
To measure psychological distress participants responded on a Likert scale from 1 (none of the time) to 4 (all of the time) to items on the Kessler Psychological Distress Scale- Six item (K6) scale, which has good internal consistency and reliability with a Cronbach’s alpha of 0.89 (Kessler et al., 2003). In this study Cronbach’s alpha and McDonald’s Omega was both 0.88 and CFI was 0.95 showing good internal consistency and unidimensionality. Scores were summed to produce a final score. A cut-point of 19 was used to indicate the presence of a probable mental health disorder. This cut-point has been shown to have high specificity (96%) but lower sensitivity (36%) in detecting health disorder diagnosed through clinical interviews (Kessler et al., 2003). The Kessler Psychological Distress Scale has also shown to have good measurement invariance across different age groups (Sunderland et al., 2013) and gender (Drapeau et al., 2010), as well being validated across a wide range of populations from different countries and culture (Donker et al., 2010; Oakley Browne et al., 2010; Andersen et al., 2011; Fernandes et al., 2011; Bu et al., 2017), including Australia (Slade et al., 2011).
To measure Subjective wellbeing participants completed the Personal Wellbeing Index (PWI), which has shown to have good internal consistency and reliability with a Cronbach’s alpha between 0.7 to 0.85 in the Australian population. Test–retest reliability over 1 to 2 weeks have shown to be good with an intra-class correlation of 0.84. In this study, internal consistency (Cronbach’s alpha = 0.92, McDonald’s Omega = 0.92) and unidimensionality of the PWI was good (CFI = 0.98). The PWI has seven domains that consistently form one factor, explaining 50% of the variance in the domain “satisfaction as a whole” in the Australian population (International Wellbeing Group, 2013). The seven domains are measured on a Likert scale from 0 (no satisfaction at all) to 10 (completely satisfied), which were totaled, averaged, and multiplied by 10 to produce the single mean PWI score. The PWI has been validated in Australia (International Wellbeing Group, 2013) and across a wide range of countries and cultures, showing good measurement invariance (Żemojtel-Piotrowska et al., 2017; Jovanović et al., 2019).
Data analysis procedure
To address missing values observed in the data, missing data were multiply imputed in R using the MICE package (van Buuren and Groothuis-Oudshoorn, 2011). Fifty imputations were conducted and 5 iterations, which was conservative given that missingness did not exceed 11%. To assist imputations, auxiliary variables were used in the imputation. Outcome variables (i.e., K6 and PWI total scores) were not imputed and were only computed after imputation to reduce any potential bias during the imputation process. All analyses were conducted and pooled using Rubin’s rule (Rubin, 2004).
T-tests were used to compare sample means with normative data that was nationally representative of the Australian population and collected at similar timepoints as the current study. Normative data was taken from the Australian Unity Wellbeing Index national 2022 report (Khor et al., 2022) for PWI scores and the Australian National University national COVID-19 tracking poll (Biddle and Gray, 2022) for K6 scores. Univariate associations between predictors and outcome variables were analysed using unadjusted linear regressions.
Multivariable linear regression was used to estimate the total effect (i.e., includes both the direct and indirect effects) of each predictor on psychological distress and subjective wellbeing while adjusting for covariates. For each predictor, a minimally sufficient adjustment set (MSAS) was identified. MSAS is the minimum set of covariates to adjust in models to estimate the total effect and avoid distorted and biasing associations that can occur in typical regression models where covariate adjustment is based only on significance of results (Rohrer, 2018; Griffith et al., 2020). To identify MSAS for each predicter, directed acyclic graphs (DAG) were developed (Rohrer, 2018), using DAGitty1 (Textor et al., 2016). The DAG is a graph that represents a theoretical framework around the causal relationships between variables, which is represented by arrows that are “directed” and imply a casual sequence. Once the theoretical framework was developed, Daggity applied the Pearl’s single and back door criterion (Pearl, 2009; Rohrer, 2018) to find the MSAS for each predictor’s model. When developing the DAG, the authors followed current recommendations (Tennant et al., 2021) and to ensure that omitted relationships were justified, all assumed relationships were tested for conditional independence in the data using polychoric correlations with the Lavaan package (Rosseel, 2012) in R based on current protocols (Ankan et al., 2021). The final relationships assumed in our DAG are presented in the supplements (Supplementary File S2). Multivariate linear regressions were then conducted individually, controlling for each predictors’ MSAS (see Table 1 for MSAS for each predictor).
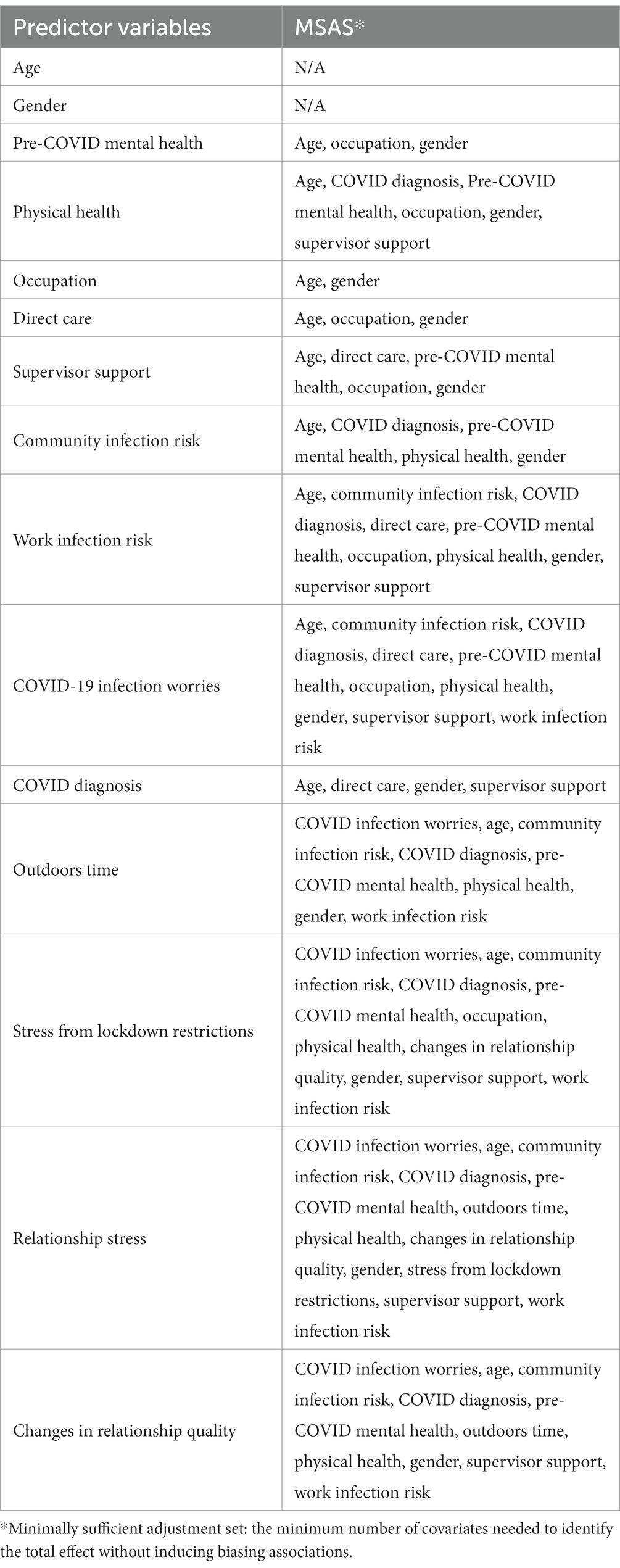
Table 1. Minimum sufficient adjusted sets (MSAS) for each predictor examined in each regression models.
Regression models were tested for heteroscedasticity using Breusch-Pagan test. Only subjective wellbeing models were found to be significantly heteroscedastic. Thus, utilising the sandwich package in R (Zeileis, 2004; Zeileis et al., 2020), Heteroscedasticity-Consistent (HC) standard errors, specifically the recommended HC3 estimator (Long and Ervin, 2000), were used in subjective wellbeing regression models. Using Gpower 3.1, post hoc power analysis showed that at alpha level 0.05, the sample size was large enough to detect statistical significance in effects ( ) above 4.7% for psychological distress and 4.6% for subjective wellbeing.
To identify key predictors and compare the unique contribution of each predictors’ total effect on K6 and PWI scores, relative importance analysis was conducted using relaimpo R package using the Lindemann-Merenda-Gold (LMG) method (Groemping, 2006). This analysis partitions variance explained in outcome variables by averaging over orderings and accounting for intercorrelations among covariates. This produces an unbiased for individual predictors that is decomposed and adjusts for other covariates, which is not typically accounted for in common estimates of decomposed that are biased by multi-collinearity (Groemping, 2006; Tonidandel and LeBreton, 2011).
Significance thresholds were all set at 0.05 for all analyses. Confidence intervals (95% CI) were computed by bootstrapping based on 1,000 bootstrap resamples from each of the 50 imputed datasets in R (Schomaker and Heumann, 2018) and pooling them together using Rubin’s rule (Rubin, 2004).
Results
Descriptive statistics
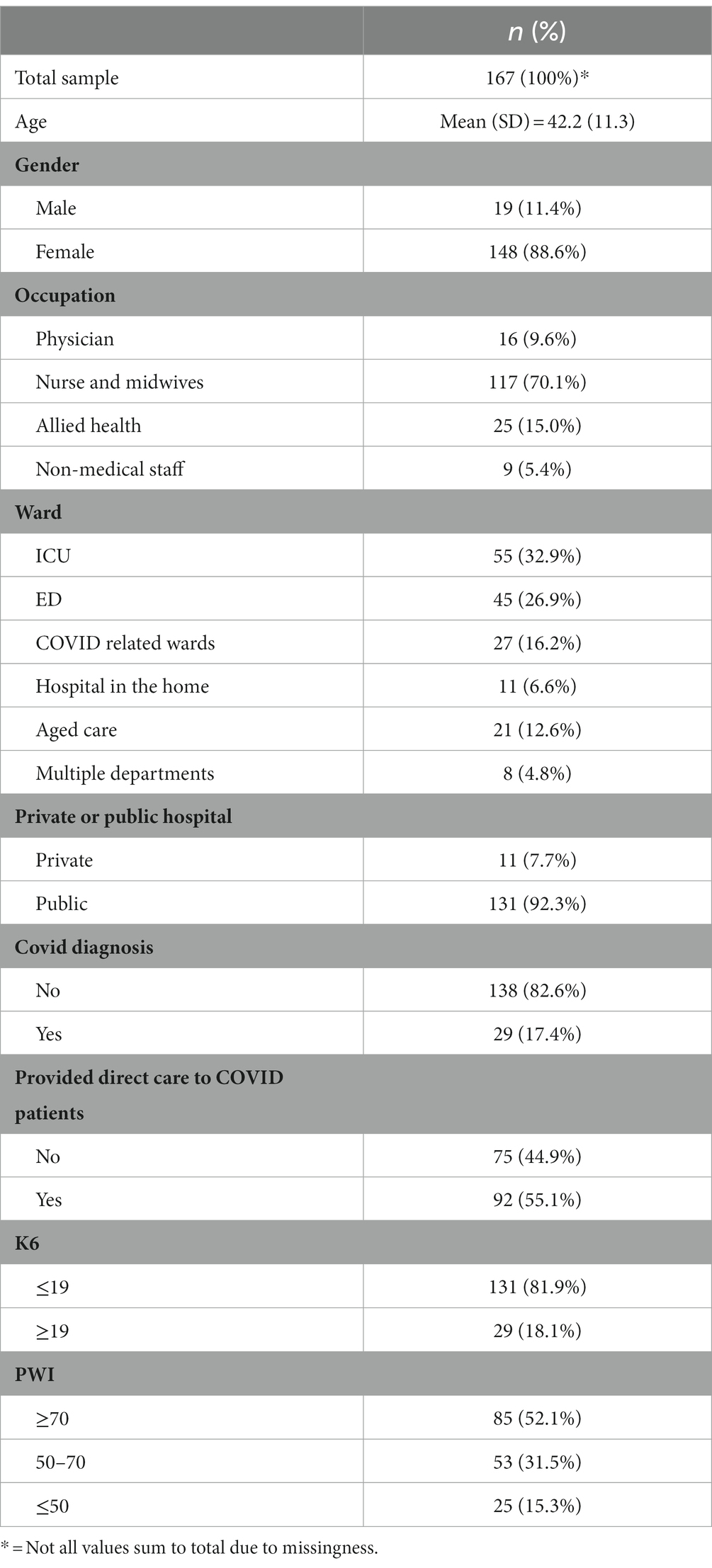
One hundred and seventy-two Victorian frontline healthcare workers completed the survey. Two participants that noted “other” as their gender and three responses that did not identify their gender were removed due to extreme uneven distribution in analyses with gender as a predictor, leaving a total of 167 responses. Details of participants’ characteristics are displayed in Table 2. In brief, the majority of respondents were female (88.6%), nurses and midwives (70.1%), and working in ICU (32.9%). When compared to previous data obtained from a large state-wide health service (Holton et al., 2020), the sample shows a good representation of the nursing population but an overrepresentation of allied health staff and under representation of physicians. Most respondents worked in public hospitals (92.3%). Only 17.4% of participants had been diagnosed with COVID-19 since the start of the pandemic. Approximately half of participants (55.1%) worked directly with COVID-19 patients.
The K6 measure was completed by 161 participants. Mean psychological distress among participants was 13.70 (SD = 4.96), which was significantly higher (t = 5.4, p < 0.001) compared to normative data (Normative mean = 11.6) that was collected during the same period as this study (Biddle and Gray, 2022). Using the recommended cut off of 19, 18.1% of the sample screened positive for a probable mental health disorder.
The PWI measure was completed by 163 participants. Mean SWI was 67.17 (SD = 18.22), significantly lower (p < 0.001) than aggregated normative data (normative mean = 75.5; Khor et al., 2022). Overall, 25 participants had SWI mean scores lower than 50, indicating that 15.3% of participants were experiencing concerningly low levels of wellbeing. Sample means were also consistently significantly lower (p < 0.05) than normative data in all sub-domains except for standard of living (p < 0.05; Figure 1). Based on Cohens’ D effect sizes, these significant mean differences were small (Cohens’ D: 0.2–0.5) for all sub-domains except for future security (Cohens’ D < 0.2), which was negligible.
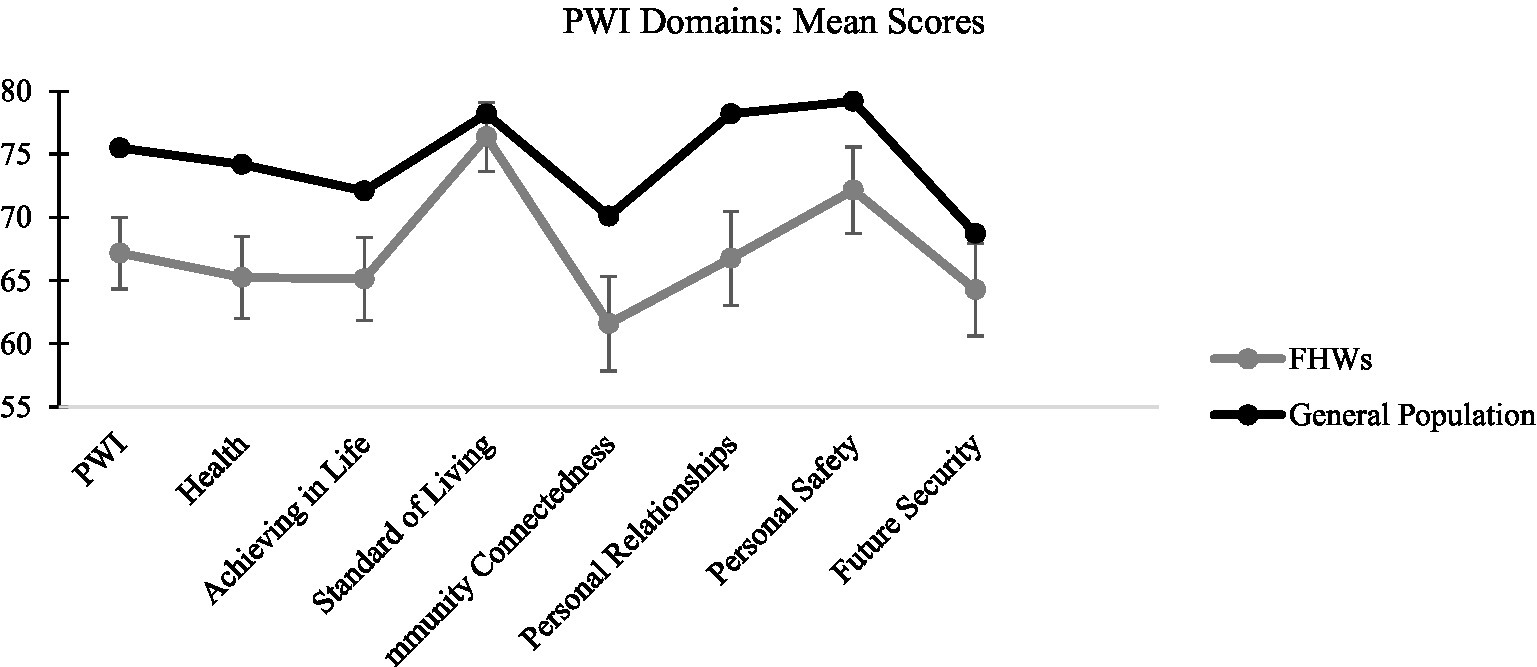
Figure 1. Means and standard deviations for FHWs in this study and the Australian Unity Wellbeing Index Norm on the PWI and sub-domains.
Regression and relative importance analysis-Psychological distress (K6) and Regression and relative importance analysis-Subjective wellbeing (PWI)
The results for the adjusted and unadjusted regression analyses, and relative importance analysis for psychological distress are displayed in Table 3. In the multivariate models adjusting for the MSAS, significant total effects were found for age, both health factors, supervisor support, all COVID infection related factors and relationship stress. Results show that younger age, higher perceived work infection risk, high perceived community infection risk, more COVID infection worries, a previous positive COVID-diagnosis and more relationship stress were significant risk factors and associated with higher levels of psychological distress. Better supervisor support, better pre-covid mental health, and better physical health were found to be protective and significantly associated with lower psychological distress.
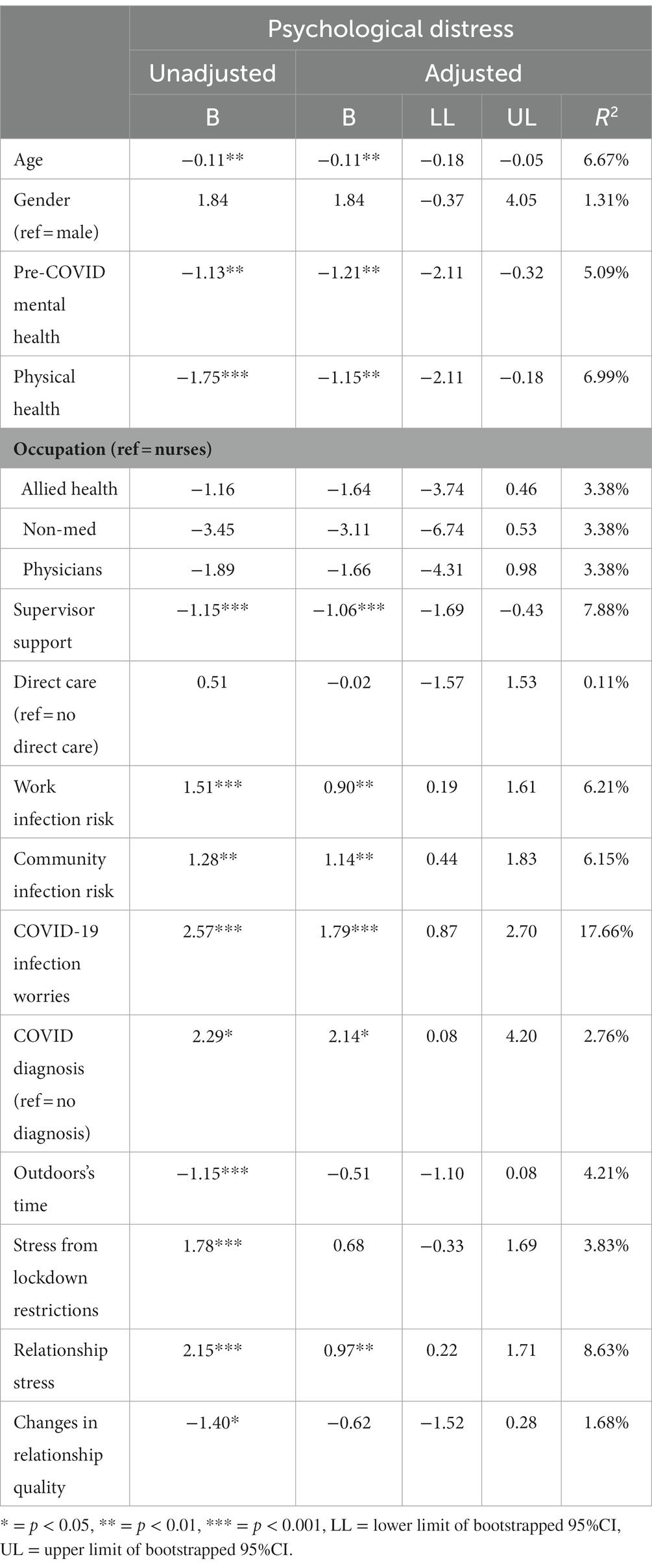
Table 3. Results of the unadjusted (univariate) and adjusted (multivariate) regressions for psychological distress.
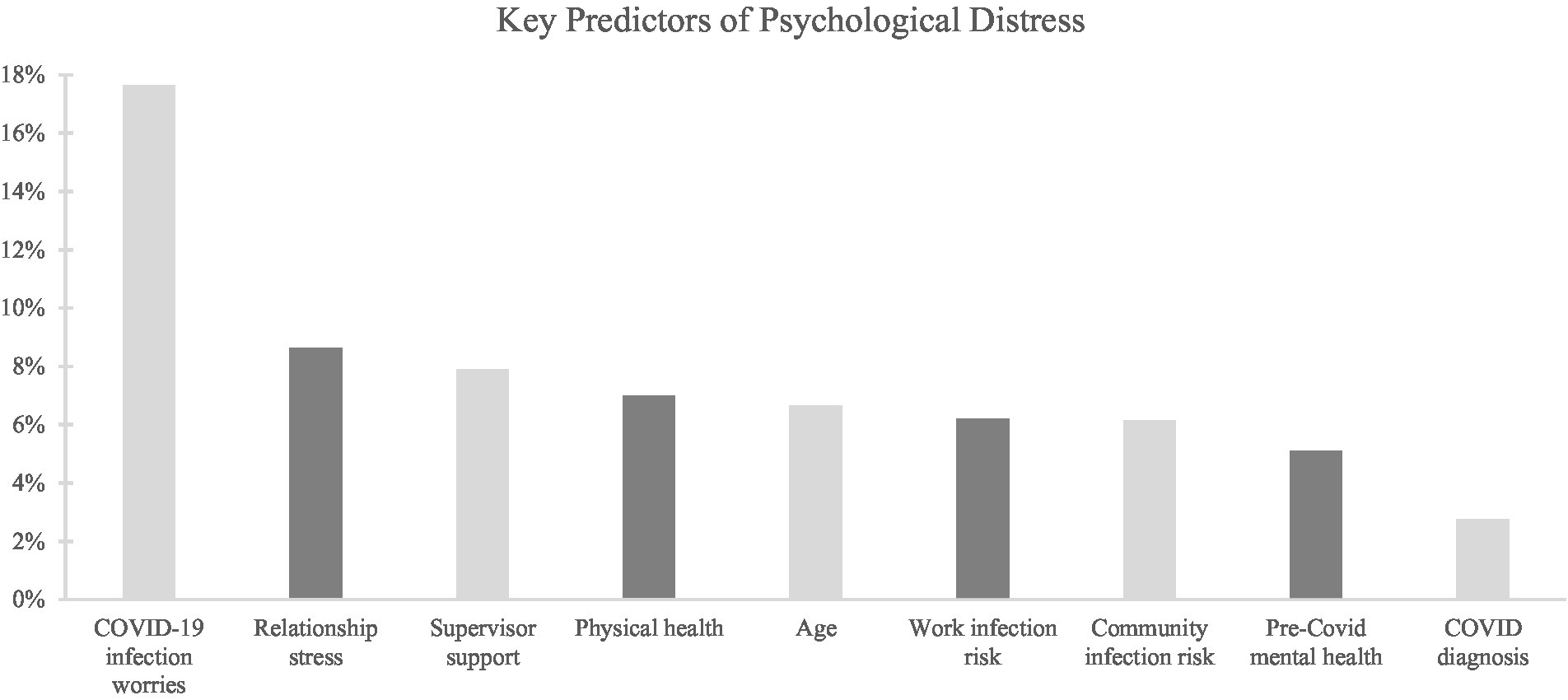
Based on the results of the relative importance analysis, COVID worries ( =17.66%) explained the most unique variance in psychological distress and was considered a large effect based on Cohen’s proposed magnitude for effect sizes. All other significant predictors explained moderate amounts of unique variance in psychological distress, ranging from 2.76 to 8.63% (Predictor ranking displayed in Figure 2).
Regression and relative importance analysis-PWI
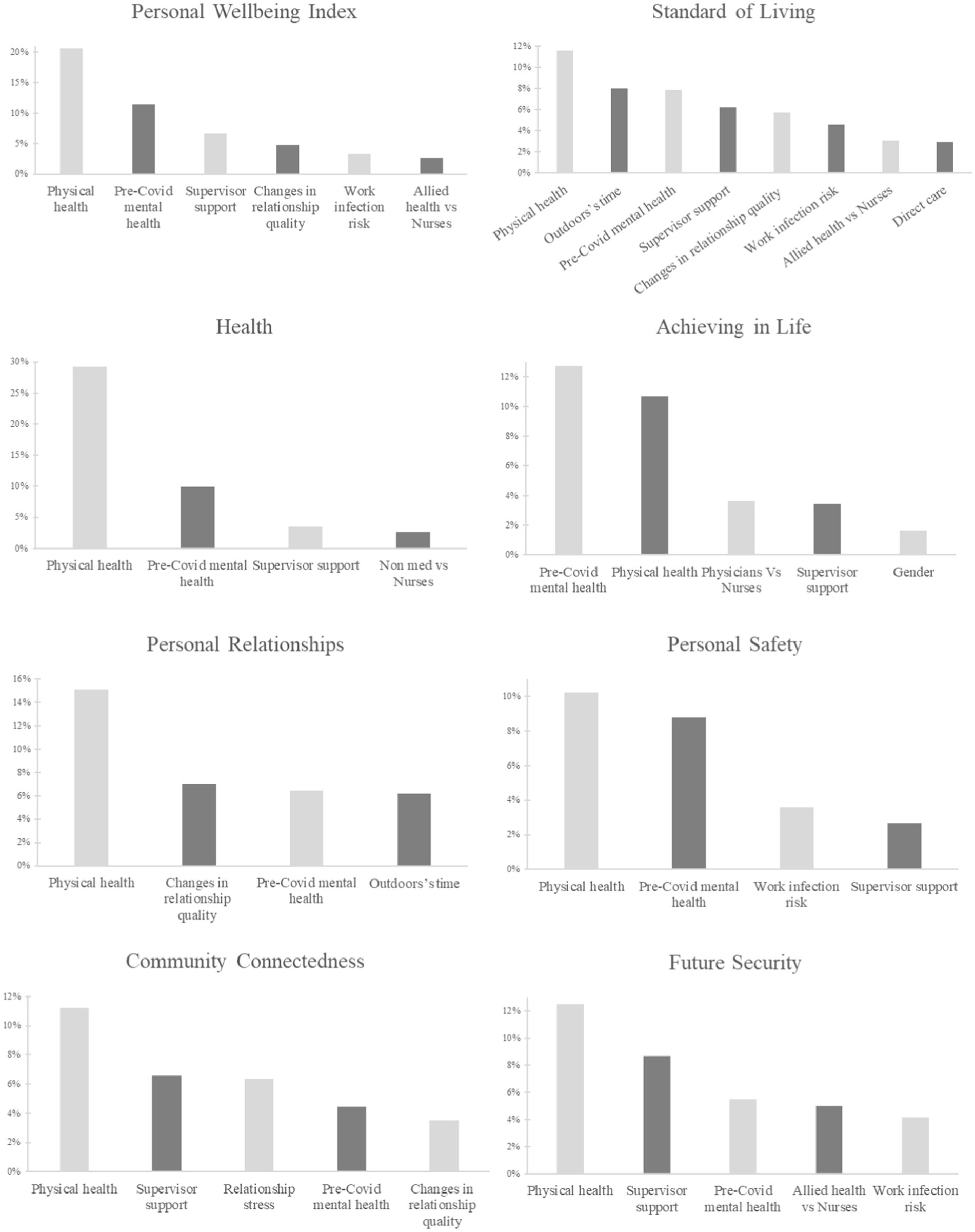
The results for the PWI and its sub-domains’ regression analyses are presented in Tables 4–6. After adjusting for the MSAS, significant total effects on PWI were found for both health factors, occupation, supervisor support, work infection risk and changes in relationship quality. Results show that a higher rating of pre-COVID mental health, physical health and supervisor support were all significantly associated with a higher overall subjective wellbeing. Positive changes in relationship quality were also associated with a higher subjective wellbeing. Being a nurse was associated with a lower subjective wellbeing, however, only when compared to allied health staff. Higher perceived work infection risk was associated with lower subjective wellbeing. When analysed within the PWI sub-domains, pre-COVID mental health, physical health and supervisor support were consistently significant predictors in all domains except for personal relationships, where supervisor support had no significant effect. In terms of occupation, being a nurse was associated with a lower satisfaction in standard of living, and future security when compared to allied health, and a lower satisfaction of health when compared to non-medical staff. Nurses also had lower satisfaction in their achievement in life when compared to physicians. Work infection risk was only a significant predictor of standard of living, personal safety, and future security. Relationship quality was only predictive of standard of living, personal relationships, and community connectedness.
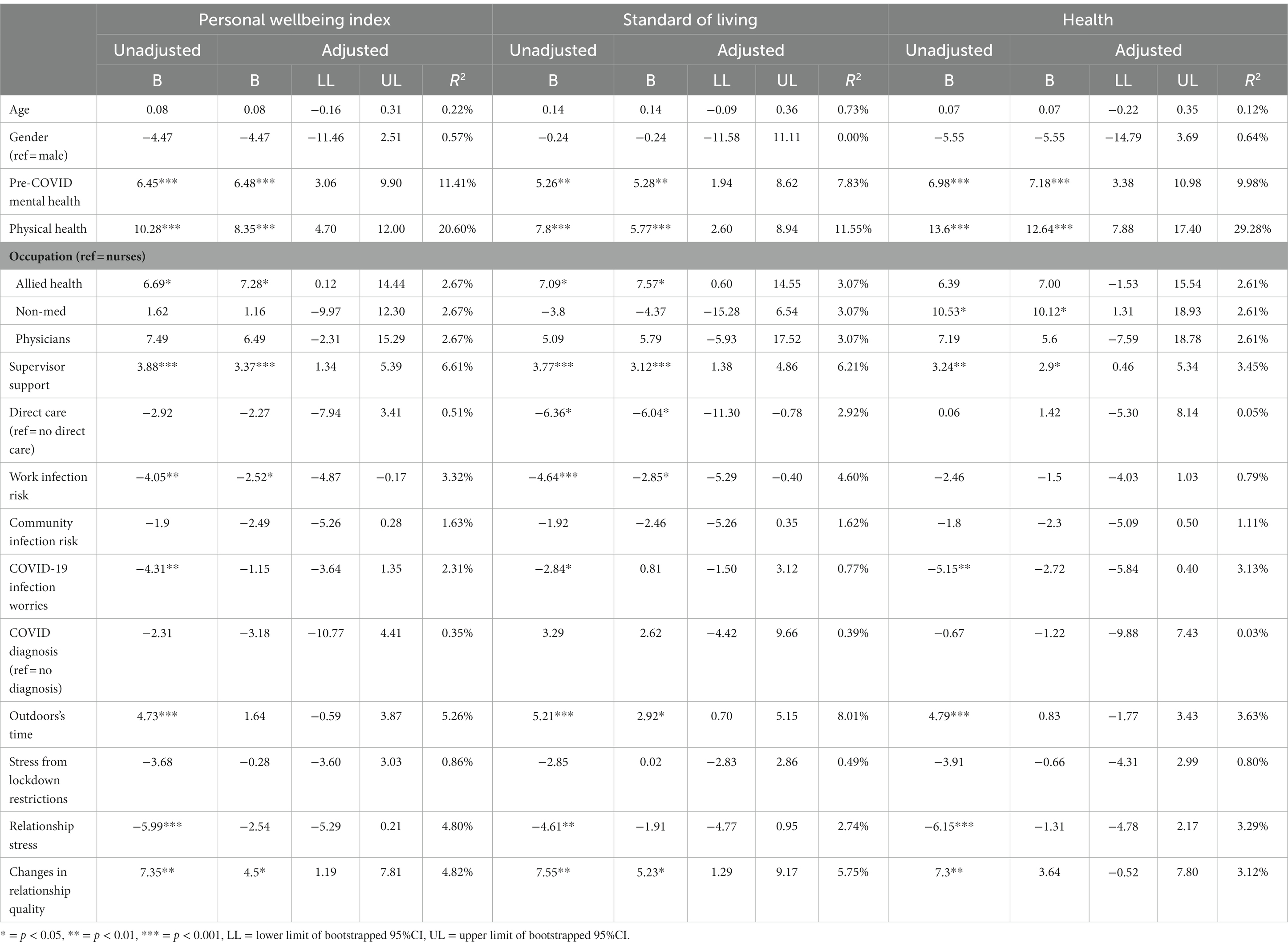
Table 4. Results of the unadjusted (univariate) and adjusted (multivariate) regressions for PWI, standard of living, and health domains.
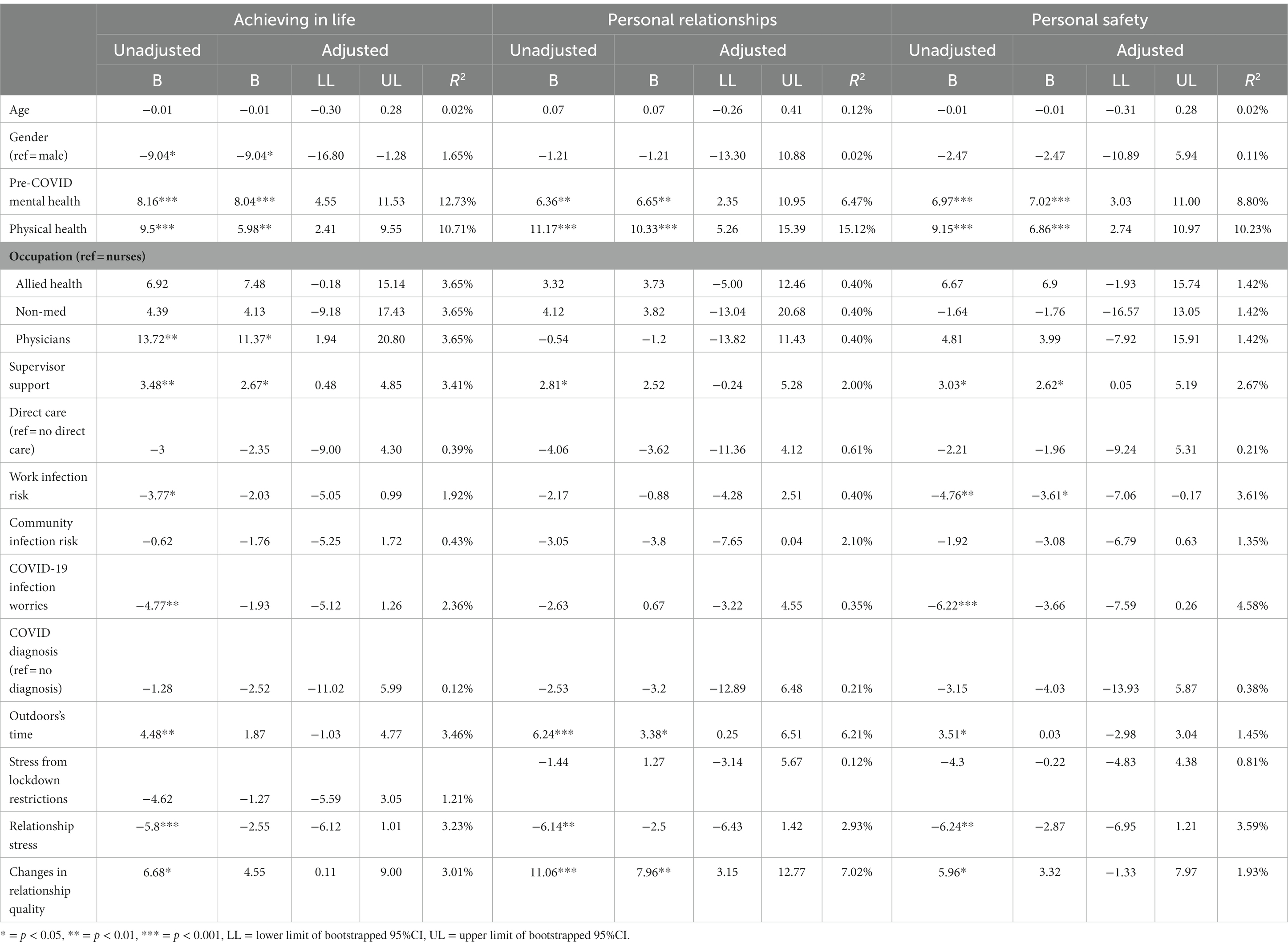
Table 5. Results of the unadjusted (univariate) and adjusted (multivariate) regressions for achieving in life, personal relationships, and personal safety domains.
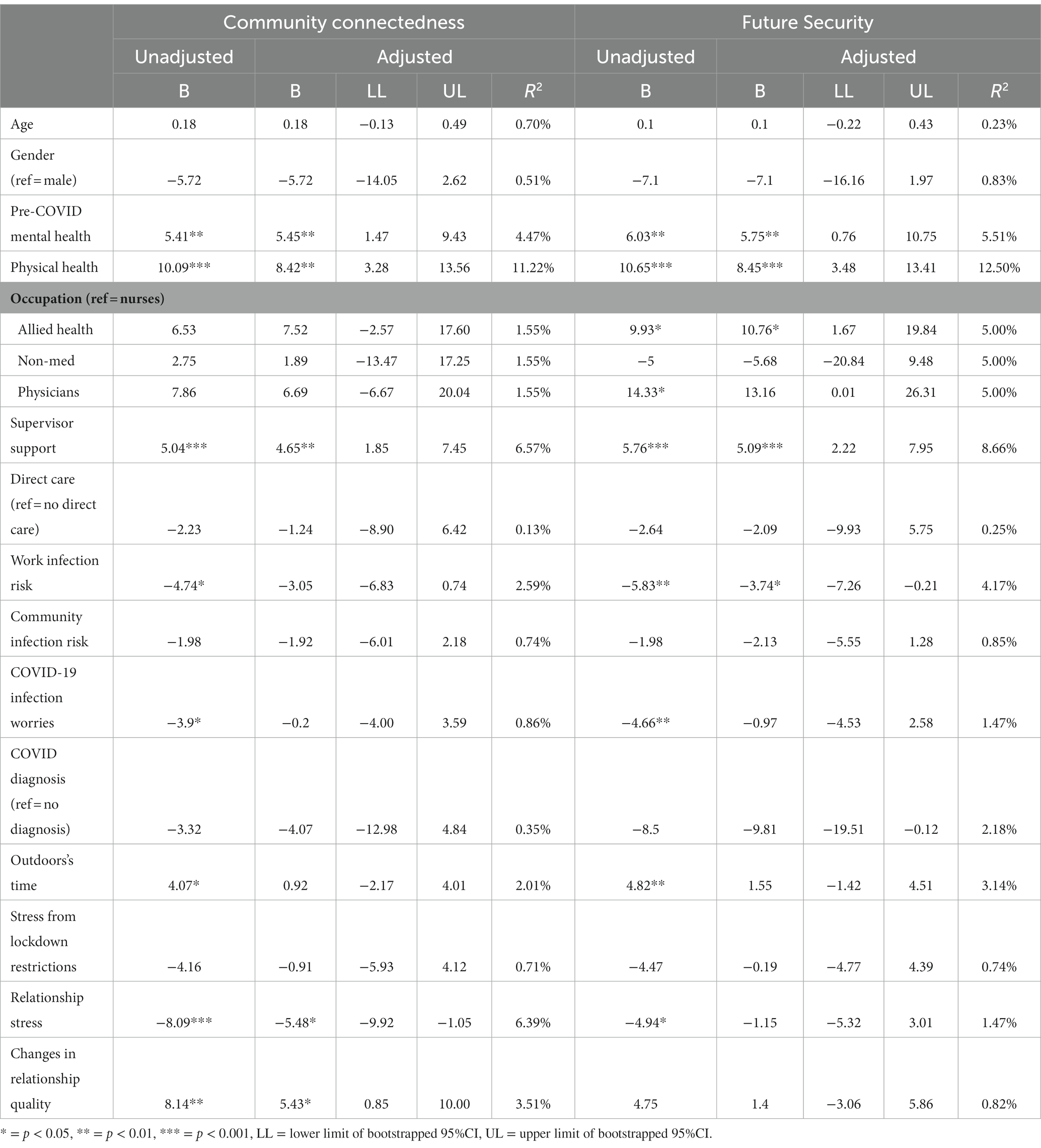
Table 6. Results of the unadjusted (univariate) and adjusted (multivariate) regressions for Community Connectedness and Future Security domains.
Based on the relative importance analysis, physical health had a large effect ( = 20.60%) and explained the most variance in overall subjective wellbeing. The other significant predictors explained moderate amounts of variance in subjective wellbeing, ranging from 2.67 to 11.41% in . Physical health also consistently explained the most variance in all domains, except for achieving in life, where pre-COVID-mental health explained the most variance. Ranking of predictors variance explained in overall subjective wellbeing and in its sub-domains are shown in Figure 3.
Discussion
To the authors knowledge, this study is one of the first Australian, and one of few studies globally, to investigate COVID-19’s mental health and wellbeing impacts on FHWs in 2022 during the Omicron wave. Specifically, the current study investigated the predictors of psychological distress and subjective wellbeing in Victorian (Australia) FHWs during the Omicron wave in January 2022. When compared to population norms assessed during the same time (Biddle and Gray, 2022; Khor et al., 2022), sample means in this study showed significantly higher psychological distress and lower wellbeing. Findings also identified multifactorial predictors of FHWs’ psychological distress and wellbeing during the Omicron wave, which included COVID infection related factors, age, health factors, relational factors, and supervisor support.
Consistent with previous findings, this study affirms the need for interventions targeting infection related factors during the COVID-19 pandemic and future infectious disease outbreaks. Specifically, infection risks and COVID-19 diagnosis were found to be predictive of psychological distress, with COVID-19 infection worries identified as the strongest independent risk factor. Notably, the effect of COVID-19 infection worries on FHWs’ psychological distress was found to be independent of perceived risk of infection or a COVID-19 diagnosis. This suggest that psychological distress associated with COVID-19 worries may persist at high levels among FHWs even when risk of infection is minimal. This likely explains why despite improvements in infection control procedures, increased vaccination uptake and an overall decrease in infection rates (Braun et al., 2021; Damluji et al., 2021; Dunbar et al., 2021), there continues to be persisting anxiety around COVID-19 infections among FHWs (Hendricksen et al., 2022; Feng et al., 2023; Scott et al., 2023). It appears that more needs to be done to manage FHWs’ concerns and anxieties with being infected, which seems to be wide-ranging. Studies suggest that, in addition to health concerns, FHWs also have significant worries around the social impacts of COVID-19 infections, such as social isolation, infecting vulnerable family members, disrupted family routines and for some, being stigmatised after infection (Schaffer et al., 2022; Sheen et al., 2022). These findings highlight the need to go beyond infection control when attempting to reduce anxiety in FHWs around COVID-19 infections, such as integrating supports focused on mitigating the social impacts of being infected, as well as psychological interventions that target FHWs’ anxiety management around COVID.
In this study, younger FHWs have also been found to be an at-risk group for higher levels of psychological distress, consistent with previous findings on FHWs (Kisely et al., 2020; Moitra et al., 2021; Czepiel et al., 2022), as well as on the general public (Xiong et al., 2020; Dragioti et al., 2022). With regards to younger FHWs, it has been suggested that their vulnerability to psychological distress may be due to their lack of specialised experience and training (Lee et al., 2021; Van Wert et al., 2022), which is not only essential for infection control, but to also protect against mental health issues as they can likely bolster confidence at work and mitigate infection related anxieties (De Brier et al., 2020; Kisely et al., 2020). Additionally, given the high rates of psychological distress in the general public (Xiong et al., 2020; Dragioti et al., 2022), it is important to consider the social impacts of the pandemic on younger FHWs. Studies on the general public have found concerning levels of loneliness among younger adults that have led to increased distress (Li and Wang, 2020). It is likely that as emerging adults, they have yet to develop strong social connections and supports, which are important to protect against mental health impacts during traumatic events such as the COVID-19 pandemic (McGuire et al., 2018; Kaniasty et al., 2020). This is significant as social support has been implicated to play an important role in FHWs’ mental health resilience, especially in younger FHWs (Hou et al., 2020). Nevertheless, it is evident that younger FHWs are in need of targeted interventions and, given recent findings, it appears that social support interventions may be beneficial, especially when tailored to enhance their confidence at work, improve work related stress management and increase their social connectedness and support at work (Mohamed et al., 2022; Musgrove et al., 2022).
With regards to wellbeing, health factors have emerged as the strongest predictor. Specifically, better physical health and mental health status were found to be highly protective of lower wellbeing, which also extended to psychological distress, however, to a lower extent. This indicates that better health states can potentially buffer COVID-19 impacts on FHWs’ mental health, as well as their wellbeing across multiple life domains. Wellbeing findings in particular, are noteworthy as the few studies that have considered it confirms that FHWs’ wellbeing has been disproportionately affected compared to the general public during the COVID-19 pandemic (McFadden et al., 2021; McGuinness et al., 2022). Adding to this, the current study found that wellbeing impacts on FHWs were evident across a wide range of life domains, including their health, relationships, community connectedness, future security, life achievements and safety. To date wellbeing outcomes in FHWs have been largely overlooked and many may conflate wellbeing and mental health outcomes together. However, this study shows that wellbeing intervention targets needs to be considered on its own as key predictors identified for wellbeing were different to those for psychological distress. Health status as a key predictor suggest that wellbeing interventions may require more long-term approaches that maintain optimal physical and mental health. This could involve targeting persisting issues that have been documented to affect health statuses in FHWs regardless of infectious disease outbreaks, such as burnout and excessive workloads (Kim et al., 2011; Adriaenssens et al., 2015; Salvagioni et al., 2017; Verougstraete and Hachimi Idrissi, 2020).
This study has also found relational factors as important indicators of psychological distress and wellbeing among FHWs. We found that greater familial and social relationship stress was a risk factor for psychological distress, while positive changes to these relationships were protective of lower wellbeing. These findings further support the notion that social factors play a critical role in FHWs’ mental health and wellbeing (Lim et al., 2010; McKinley et al., 2019). It highlights the importance of not only enhancing social relationships but also safeguarding it for FHWs during times of crisis. This is important because it is well documented that, while FHWs have poor help seeking behaviour with regards to mental health (Halter Margaret, 2004; Brooks et al., 2011; Galbraith et al., 2014; Wijeratne et al., 2021), they rely heavily on social support to manage it (Labrague, 2021; Schug et al., 2021). Thus, during times when widespread stigma and social rejection of FHWs are common, such as infectious disease outbreaks (Gómez-Durán et al., 2020; Schubert et al., 2021; Yuan et al., 2021; Ding et al., 2022), they can easily be left isolated and more vulnerable to mental health and wellbeing issues. Moreover, healthcare work during this time may have also placed additional stressors on FHWs’ social contacts and personal relationships, such as increased familial anxiety due to infection risks, poor work-life balance and stigma as a FHW family (Ali et al., 2020; Evanoff et al., 2020; Schaffer et al., 2022; Sheen et al., 2022). FHWs are currently experiencing tremendous challenges, and these findings underscore the importance of protecting FHWs social relationships, which can have multi-fold effects on their mental health and wellbeing.
Lastly, another key predictor of both mental health and wellbeing in FHWs to consider is supervisor support. In line with previous studies (Evanoff et al., 2020; Feingold et al., 2021; Greco et al., 2022), findings show that support from supervisors during the pandemic can play an important role in influencing FHWs mental health and wellbeing. This echoes the call for increased focus on supervisors’ capabilities with regards to supporting FHWs’ mental health and wellbeing (Carmassi et al., 2020; Hennein et al., 2021). While providing extensive mental health support may be out of scope for supervisors, they are still in unique positions to provide a range of social, work, and emotional support directly to FHWs that can influence their mental health and wellbeing. For example, Evanoff et al. (2020) found that family specific supervisory support was strongly associated with better mental health and wellbeing among FHWs. Another study also found that ethical leadership from supervisors was significantly associated with lower levels of work-related stress, which includes promoting and modelling openness, integrity, and trustworthiness (Zhou et al., 2015). It is also important to note that supervisors themselves have been experiencing additional stress and psychological burden beyond those experienced by their staff during the pandemic (Middleton et al., 2021), likely due to the additional support they are required to provide their staff. Thus, it follows that to ensure organisational support for FHWs are effectively implemented and managed, organisations need to consider strategies to elevate the additional burden on supervisors during this time. Nevertheless, supervisor support is likely an important pathway for organisations to influence FHWs mental health and wellbeing, and therefore should be a core focus in organisational mental health and wellbeing strategies.
Limitations
When interpreting findings in this study, several limitations should be considered. Firstly, as a cross-sectional study, it is not evident that the distress observed in this study is indicative of an acute reaction or persisting distress, which should be investigated further in longitudinal studies. Additionally, causal links between variables should be interpreted with caution. While the use of DAGs in this study provides a framework around causality between investigated variables, it relies on the assumptions in the DAGs. Other models may exist and the model in this study is not intended to be a proposal for a theoretical framework around FHWs’ mental health and wellbeing. The use of the DAG in this study is intended to be a way to systematically adjust for covariates to estimate effects and provide transparency around assumed relationships (Ferguson et al., 2020). Secondly, mediation analysis was beyond the scope of this study, however, the results points to several mediating relationships among the investigated variables and should be considered when interpreting results and in future research. It is thus recommended that future research investigate these mediating relationships further through structural equation modelling or mediation analyses. Thirdly; there was a low representation of physicians, which may have impacted the generalisability of results for this cohort. Lastly, due to the small sample size, precision of estimates may be weak, thus effects and mean differences with population norms should be interpreted and generalised with caution.
Conclusion
In sum, the COVID-19 pandemic continues to place undue pressure on FHWs’ mental health and wellbeing. Findings indicate that FHWs mental health and wellbeing are associated with a wide range of factors that includes work-related and social determinants. It is thus important to consider a wide range of factors, including those beyond work, when developing targeted interventions and support for FHWs’ mental health and wellbeing, to ensure their effectiveness. Nevertheless, findings reinforce the need for ongoing research, development, and implementation of targeted interventions for FHWs who continue to face significant challenges.
Data availability statement
The datasets presented in this article are not readily available because the datasets investigated and presented in this study are not available for public use as ethical approvals for this study does not include public availability of participants data. Requests to access the datasets should be directed to YnJpYW4ubGVlQGRlYWtpbi5lZHUuYXU=.
Ethics statement
The studies involving human participants were reviewed and approved by Deakin University High Risk Ethics Committee and Eastern Health’s Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
BL, ML, LB, CAO, and JS was involved in the conceptualisation and design of this study. BL was responsible for the formal analysis, data curation, and investigation under the supervision of ML, LB, CAO, and JS. BL prepared the original manuscript draft, which was then review and edited by ML, LB, CAO and JS. All authors contributed to the article and approved the submitted version.
Funding
Preparation of this paper was supported by using award money from the Victorian COVID-19 Research Fund-Stream B, State Government of Victoria. The funders of this study had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. CAO is supported by a NHMRC Investigator Grant GNT1175086.
Acknowledgments
The authors would like to acknowledge and thank the participants in this study for their time and effort spent completing the surveys in this study. They would also like to thank the participating institutions, associations and the project advisory group for their contribution and assistance with this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1200839/full#supplementary-material
Footnotes
References
Adriaenssens, J., De Gucht, V., and Maes, S. (2015). Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int. J. Nurs. Stud. 52, 649–661. doi: 10.1016/j.ijnurstu.2014.11.004
al Falasi, B., al Mazrouei, M., al Ali, M., al Dhamani, M., al Ali, A., al Kindi, M., et al. (2021). Prevalence and determinants of immediate and Long-term PTSD consequences of coronavirus-related (CoV-1 and CoV-2) pandemics among healthcare professionals: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 18:2182. doi: 10.3390/ijerph18042182
Ali, H., Cole, A., Ahmed, A., Hamasha, S. D., and Panos, G. (2020). Major stressors and coping strategies of frontline nursing staff during the outbreak of coronavirus disease 2020 (COVID-19) in Alabama. J. Multidiscip. Healthc. 13, 2057–2068. doi: 10.2147/jmdh.s285933
Andersen, L. S., Grimsrud, A., Myer, L., Williams, D. R., Stein, D. J., and Seedat, S. (2011). The psychometric properties of the K10 and K6 scales in screening for mood and anxiety disorders in the south African stress and health study. Int. J. Methods Psychiatr. Res. 20, 215–223. doi: 10.1002/mpr.351
Ankan, A., Wortel, I. M. N., and Textor, J. (2021). Testing graphical causal models using the R package “dagitty”. Curr. Protoc. 1:e45. doi: 10.1002/cpz1.45
Berger, E., Winkelmann, J., Eckhardt, H., Nimptsch, U., Panteli, D., Reichebner, C., et al. (2022). A country-level analysis comparing hospital capacity and utilisation during the first COVID-19 wave across Europe. Health Policy 126, 373–381. doi: 10.1016/j.healthpol.2021.11.009
Biddle, N., and Gray, M. (2022). Tracking Wellbeing Outcomes during the COVID-19 Pandemic (January 2022): Riding the Omicron Wave. ANU Centre for Social Research and Methods: Australian National University, Canberra.
Billings, J., Ching, B. C. F., Gkofa, V., Greene, T., and Bloomfield, M. (2021). Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv. Res. 21. doi: 10.1186/s12913-021-06917-z
Braun, K. M., Moreno, G. K., Buys, A., Somsen, E. D., Bobholz, M., Accola, M. A., et al. (2021). Viral sequencing to investigate sources of SARS-CoV-2 infection in US healthcare personnel. Clin. Infect. Dis. 73, e1329–e1336. doi: 10.1093/cid/ciab281
Brooks, S. K., Gerada, C., and Chalder, T. (2011). Review of literature on the mental health of doctors: are specialist services needed? J. Ment. Health 20, 146–156. doi: 10.3109/09638237.2010.541300
Bu, X.-Q., You, L.-M., Li, Y., Liu, K., Zheng, J., Yan, T.-B., et al. (2017). Psychometric properties of the Kessler 10 scale in Chinese parents of children with Cancer. Cancer Nurs. 40, 297–304. doi: 10.1097/NCC.0000000000000392
Carmassi, C., Foghi, C., Dell'Oste, V., Cordone, A., Bertelloni, C. A., Bui, E., et al. (2020). PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 292:113312. doi: 10.1016/j.psychres.2020.113312
Cassinat, J. R., Whiteman, S. D., Serang, S., Dotterer, A. M., Mustillo, S. A., Maggs, J. L., et al. (2021). Changes in family chaos and family relationships during the COVID-19 pandemic: evidence from a longitudinal study. Dev. Psychol. 57, 1597–1610. doi: 10.1037/dev0001217
Chau, S. W. H., Wong, O. W. H., Ramakrishnan, R., Chan, S. S. M., Wong, E. K. Y., Li, P. Y. T., et al. (2021). History for some or lesson for all? A systematic review and meta-analysis on the immediate and long-term mental health impact of the 2002-2003 severe acute respiratory syndrome (SARS) outbreak. BMC Public Health 21:670. doi: 10.1186/s12889-021-10701-3
Czepiel, D., Hoek, H. W., van der Markt, A., Rutten, B. P. F., Veling, W., Schirmbeck, F., et al. (2022). The association between exposure to COVID-19 and mental health outcomes among healthcare workers. Public Health 10:896843. doi: 10.3389/fpubh.2022.896843
Damluji, A. A., Wei, S., Bruce, S. A., Haymond, A., Petricoin, E. F., Liotta, L., et al. (2021). Seropositivity of COVID-19 among asymptomatic healthcare workers: a multi-site prospective cohort study from northern Virginia, United States. Lancet Reg Health Am 2:100030. doi: 10.1016/j.lana.2021.100030
De Brier, N., Stroobants, S., Vandekerckhove, P., and De Buck, E. (2020). Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLoS One 15:e0244052. doi: 10.1371/journal.pone.0244052
Digby, R., Winton-Brown, T., Finlayson, F., Dobson, H., and Bucknall, T. (2021). Hospital staff well-being during the first wave of COVID-19: staff perspectives. Int. J. Ment. Health Nurs. 30, 440–450. doi: 10.1111/inm.12804
Ding, S., Deng, S., Zhang, Y., Wang, Q., Liu, Z., Huang, J., et al. (2022). Experiences and needs of front-line nurses during the COVID-19 pandemic: A systematic review and qualitative meta-synthesis. Front Public Health. 10:805631. doi: 10.3389/fpubh.2022.805631
Donker, T., van Straten, A., Marks, I., and Cuijpers, P. (2010). Brief self-rated screening for depression on the internet. J. Affect. Disord. 122, 253–259. doi: 10.1016/j.jad.2009.07.013
Dragioti, E., Li, H., Tsitsas, G., Lee, K. H., Choi, J., Kim, J., et al. (2022). A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 94, 1935–1949. doi: 10.1002/jmv.27549
Drapeau, A., Beaulieu-Prévost, D., Marchand, A., Boyer, R., Préville, M., and Kairouz, S. (2010). A life-course and time perspective on the construct validity of psychological distress in women and men. Measurement invariance of the K6 across gender. BMC Med. Res. Methodol. 10:68. doi: 10.1186/1471-2288-10-68
Dunbar, E., Godbout, E., Pryor, R., Rozycki, H. J., and Bearman, G. (2021). Impact of coronavirus disease 2019 (COVID-19) vaccination program on healthcare worker infections in an academic hospital. Infect. Control Hosp Epidemiol 43, 680–681. doi: 10.1017/ice.2021.62
Evanoff, B. A., Strickland, J. R., Dale, A. M., Hayibor, L., Page, E., Duncan, J. G., et al. (2020). Work-related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. J. Med. Internet Res. 22:e21366. doi: 10.2196/21366
Feingold, J. H., Peccoralo, L., Chan, C. C., Kaplan, C. A., Kaye-Kauderer, H., Charney, D., et al. (2021). Psychological impact of the COVID-19 pandemic on frontline health care workers during the pandemic surge in New York City. Chronic Stress (Thousand Oaks) 5:2470547020977891. doi: 10.1177/2470547020977891
Feng, X., Yang, C., Yang, H., Wang, K., Xu, Y., Zhang, X., et al. (2023). Anxiety, depression, and somatic symptom disorders in health care workers at high altitude during the rapid spread of the SARS-CoV-2 omicron variant: a prospective cohort study. Front. Psych. 13:1018391. doi: 10.3389/fpsyt.2022.1018391
Ferguson, K. D., McCann, M., Katikireddi, S. V., Thomson, H., Green, M. J., Smith, D. J., et al. (2020). Evidence synthesis for constructing directed acyclic graphs (ESC-DAGs): a novel and systematic method for building directed acyclic graphs. Int. J. Epidemiol. 49, 322–329. doi: 10.1093/ije/dyz150
Fernandes, M. C., Srinivasan, K., Stein, A. L., Menezes, G., Sumithra, R. S., and Ramchandani, P. G. (2011). Assessing prenatal depression in the rural developing world: a comparison of two screening measures. Arch. Womens Ment. Health 14, 209–216. doi: 10.1007/s00737-010-0190-2
Fitzpatrick, K.M., Harris, C., and Drawve, G. (2020). “Fear of COVID-19 and the Mental Health Consequences in America ”. (USA: Educational Publishing Foundation).
Galbraith, N. D., Brown, K. E., and Clifton, E. (2014). A survey of student Nurses' attitudes toward help seeking for stress. Nurs. Forum 49, 171–181. doi: 10.1111/nuf.12066
Galli, F., Pozzi, G., Ruggiero, F., Mameli, F., Cavicchioli, M., Barbieri, S., et al. (2020). A systematic review and provisional Metanalysis on psychopathologic burden on health care workers of coronavirus outbreaks. Front. Psych. 11:1001. doi: 10.3389/fpsyt.2020.568664
Gómez-Durán, E. L., Martin-Fumadó, C., and Forero, C. G. (2020). Psychological impact of quarantine on healthcare workers. Occup. Environ. Med. 77, 666–674. doi: 10.1136/oemed-2020-106587
Greco, E., Graziano, E. A., Stella, G. P., Mastrodascio, M., and Cedrone, F. (2022). The impact of leadership on perceived work-related stress in healthcare facilities organisations. J. Organ. Chang. Manag. 35, 734–748. doi: 10.1108/JOCM-07-2021-0201
Griffith, G. J., Morris, T. T., Tudball, M. J., Herbert, A., Mancano, G., Pike, L., et al. (2020). Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat. Commun. 11. doi: 10.1038/s41467-020-19478-2
Groemping, U. (2006). Relative importance for linear regression in R: the package relaimpo. J. Stat. Softw. 17, 1–27. doi: 10.18637/jss.v017.i01
Halter Margaret, J. (2004). Stigma & help seeking related to depression: a study of nursing students. J. Psychosoc. Nurs. Ment. Health Serv. 42, 42–51. doi: 10.3928/02793695-20040201-07
Hendricksen, M., Mitchell, S. L., Palan Lopez, R., Roach, A., Hendrix Rogers, A., Akunor, H., et al. (2022). ADVANCE-C: a qualitative study of experiences caring for nursing home residents with advanced dementia during the COVID-19 pandemic. J. Gerontol. B Psychol. Sci. Soc. Sci. 77, 1938–1946. doi: 10.1093/geronb/gbac093
Hennein, R., Mew, E. J., and Lowe, S. R. (2021). Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS One 16:e0246602. doi: 10.1371/journal.pone.0246602
Holton, S., Wynter, K., Trueman, M., Bruce, S., Sweeney, S., Crowe, S., et al. (2020). Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust. Health Rev. 45:297. doi: 10.1071/ah20203
Hou, T., Zhang, T., Cai, W., Song, X., Chen, A., Deng, G., et al. (2020). Social support and mental health among health care workers during coronavirus disease 2019 outbreak: a moderated mediation model. PLoS One 15:e0233831. doi: 10.1371/journal.pone.0233831
Hunt, A., Ting, J., Schweitzer, D., Laakso, E. L., and Stewart, I. (2022). Personal protective equipment for COVID−19 among healthcare workers in an emergency department: an exploratory survey of workload, thermal discomfort and symptoms of heat strain. Emerg. Med. Australas. 35, 483–488. doi: 10.1111/1742-6723.14152
International Wellbeing Group (2013). Personal Wellbeing Index : 5th. Melbourne: Australian Centre on Quality of Life, Deakin University.
Jovanović, V., Cummins, R. A., Weinberg, M., Kaliterna, L., and Prizmic-Larsen, Z. (2019). Personal wellbeing index: a cross-cultural measurement invariance study across four countries. J. Happiness Stud. 20, 759–775. doi: 10.1007/s10902-018-9966-2
Kaniasty, K., de Terte, I., Guilaran, J., and Bennett, S. (2020). A scoping review of post-disaster social support investigations conducted after disasters that struck the Australia and Oceania continent. Disasters 44, 336–366. doi: 10.1111/disa.12390
Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., et al. (2003). Creening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189. doi: 10.1001/archpsyc.60.2.184
Khor, S., Capic, T., Cummins, R.A., Fuller-Tyszkiewicz, M., Olsson, C.A., Hutchinson, D., et al. (2022). Subjective Wellbeing in Australia during the Second Year of the Pandemic. Geelong: Australian Centre on Quality of Life, School of Psychology, Deakin University.
Kim, H., Ji, J., and Kao, D. (2011). Burnout and physical health among social workers: a three-year longitudinal study. Soc. Work 56, 258–268. doi: 10.1093/sw/56.3.258
Kim, H. J., and Lee, G. H. (2022). A comparative study of the psychological impacts of tasks related and unrelated to COVID-19 on nurses: a cross-sectional study. J Yeungnam Med Sci 39, 216–222. doi: 10.12701/yujm.2021.01361
Kim, A. W., Nyengerai, T., and Mendenhall, E. (2022). Evaluating the mental health impacts of the COVID-19 pandemic: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Psychol. Med. 52, 1587–1599. doi: 10.1017/s0033291720003414
Kisely, S., Warren, N., McMahon, L., Dalais, C., Henry, I., and Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 369:m1642. doi: 10.1136/bmj.m1642
Labrague, L. J. (2021). Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J. Nurs. Manag. 29, 1893–1905. doi: 10.1111/jonm.13336
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Lee, J., Lee, H. J., Hong, Y., Shin, Y.-W., Chung, S., and Park, J. (2021). Risk perception, unhealthy behavior, and anxiety due to viral epidemic among healthcare workers: the relationships with depressive and insomnia symptoms during COVID-19. Front. Psych. 12:615387. doi: 10.3389/fpsyt.2021.615387
Lee, B. E. C., Ling, M., Boyd, L., Olsson, C., and Sheen, J. (2023). The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: a systematic review and meta-analysis. J. Affect. Disord. 330, 329–345. doi: 10.1016/j.jad.2023.03.012
Li, L. Z., and Wang, S. (2020). Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 291:113267. doi: 10.1016/j.psychres.2020.113267
Lim, J., Bogossian, F., and Ahern, K. (2010). Stress and coping in Australian nurses: a systematic review. Int. Nurs. Rev. 57, 22–31. doi: 10.1111/j.1466-7657.2009.00765.x
Liu, X., Kakade, M., Fuller, C. J., Fan, B., Fang, Y., Kong, J., et al. (2012). Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 53, 15–23. doi: 10.1016/j.comppsych.2011.02.003
Long, J. S., and Ervin, L. H. (2000). Using heteroscedasticity consistent standard errors in the linear regression model. Am. Stat. 54, 217–224. doi: 10.1080/00031305.2000.10474549
Magnavita, N., Chirico, F., Garbarino, S., Bragazzi, N. L., Santacroce, E., and Zaffina, S. (2021). SARS/MERS/SARS-CoV-2 outbreaks and burnout syndrome among healthcare workers. An umbrella systematic review. Int. J. Environ. Res. Public Health 18:4361. doi: 10.3390/ijerph18084361
May, C. L., and Wisco, B. E. (2016). Defining trauma: how level of exposure and proximity affect risk for posttraumatic stress disorder. Psychol. Trauma Theory Res. Pract. Policy 8, 233–240. doi: 10.1037/tra0000077
McFadden, P., Ross, J., Moriarty, J., Mallett, J., Schroder, H., Ravalier, J., et al. (2021). The role of coping in the wellbeing and work-related quality of life of UK health and social care workers during COVID-19. Int. J. Environ. Res. Public Health 18:815. doi: 10.3390/ijerph18020815
McGuinness, S. L., Johnson, J., Eades, O., Cameron, P. A., Forbes, A., Fisher, J., et al. (2022). Mental health outcomes in Australian healthcare and aged-care workers during the second year of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 19:4951. doi: 10.3390/ijerph19094951
McGuire, A. P., Gauthier, J. M., Anderson, L. M., Hollingsworth, D. W., Tracy, M., Galea, S., et al. (2018). Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: effects for displaced and nondisplaced residents. J. Trauma. Stress. 31, 223–233. doi: 10.1002/jts.22270
McKinley, N., Karayiannis, P. N., Convie, L., Clarke, M., Kirk, S. J., and Campbell, W. J. (2019). Resilience in medical doctors: a systematic review. Postgrad. Med. J. 95, 140–147. doi: 10.1136/postgradmedj-2018-136135
Middleton, R., Loveday, C., Hobbs, C., Almasi, E., Moxham, L., Green, H., et al. (2021). The COVID-19 pandemic – a focus on nurse managers’ mental health, coping behaviours and organisational commitment. Collegian 28, 703–708. doi: 10.1016/j.colegn.2021.10.006
Mohamed, B. A., Fowler, W. K., Thakkar, M., and Fahy, B. G. (2022). The BUDDYS system: a unique peer support strategy among anaesthesiology residents during the COVID-19 pandemic. Turk J Anaesthesiol Reanim 50, S62–s67. doi: 10.5152/tjar.2021.21247
Moitra, M., Rahman, M., Collins, P. Y., Gohar, F., Weaver, M., Kinuthia, J., et al. (2021). Mental health consequences for healthcare workers during the COVID-19 pandemic: a scoping review to draw lessons for LMICs. Front. Psychiatry 12:602614. doi: 10.3389/fpsyt.2021.602614
Muller, A. E., Hafstad, E. V., Himmels, J. P. W., Smedslund, G., Flottorp, S., Stensland, S. Ø., et al. (2020). The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 293:113441. doi: 10.1016/j.psychres.2020.113441
Musgrove, E., Bil, D., Bridson, T., and McDermott, B. (2022). Australian healthcare workers experiences of peer support during COVID-19: hand-n-hand peer support. Australas. Psychiatry 30, 722–727. doi: 10.1177/10398562221128214
Nguyen, L. H., Drew, D. A., Graham, M. S., Joshi, A. D., Guo, C.-G., Ma, W., et al. (2020). Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 5, e475–e483. doi: 10.1016/s2468-2667(20)30164-x
Nikolaidis, A., Paksarian, D., Alexander, L., Derosa, J., Dunn, J., Nielson, D. M., et al. (2021). The coronavirus health and impact survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci. Rep. 11:8139. doi: 10.1038/s41598-021-87270-3
Oakley Browne, M. A., Wells, J. E., Scott, K. M., and McGee, M. A. (2010). The Kessler PSychological distress scale in Te Rau Hinengaro: the New Zealand mental health survey. Aust. N Z J. Psychiatry 44, 314–322. doi: 10.3109/00048670903279820
Premier of Victoria (2022a). Pandemic code brown to support hospitals. Available at: https://www.premier.vic.gov.au/pandemic-code-brown-support-hospitals. (Accessed June 22, 2023).
Quigley, A. L., Stone, H., Nguyen, P. Y., Chughtai, A. A., and MacIntyre, C. R. (2021). Estimating the burden of COVID-19 on the Australian healthcare workers and health system during the first six months of the pandemic. Int. J. Nurs. Stud. 114:103811. doi: 10.1016/j.ijnurstu.2020.103811
Raoofi, S., Pashazadeh Kan, F., Rafiei, S., Khani, S., Hosseinifard, H., Tajik, F., et al. (2021). Anxiety during the COVID-19 pandemic in hospital staff: systematic review plus meta-analysis. BMJ Support Palliat Care 13, 127–135. doi: 10.1136/bmjspcare-2021-003125
Rohrer, J. M. (2018). Thinking clearly about correlations and causation: graphical causal models for observational data. Adv. Methods Pract. Psychol. Sci. 1, 27–42. doi: 10.1177/2515245917745629
Rosseel, Y. (2012). Lavaan: an R package for structural equation modeling. J. Stat. Softw. 48, 1–36. doi: 10.18637/jss.v048.i02
Sahebi, A., Abdi, K., Moayedi, S., Torres, M., and Golitaleb, M. (2021). The prevalence of insomnia among health care workers amid the COVID-19 pandemic: an umbrella review of meta-analyses. J. Psychosom. Res. 149:110597. doi: 10.1016/j.jpsychores.2021.110597
Salari, N., Khazaie, H., Hosseinian-Far, A., Ghasemi, H., Mohammadi, M., Shohaimi, S., et al. (2020). The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Glob. Health 16:92. doi: 10.1186/s12992-020-00620-0
Salvagioni, D. A. J., Melanda, F. N., Mesas, A. E., González, A. D., Gabani, F. L., and Andrade, S. M. D. (2017). Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One 12:e0185781. doi: 10.1371/journal.pone.0185781
Schaffer, G. E., Kilanowski, L., and Lee, B. E. (2022). A qualitative investigation of the impact of COVID-19 on United States frontline health care workers and the perceived impact on their family members. Int. J. Environ. Res. Public Health 19:10483. doi: 10.3390/ijerph191710483
Schomaker, M., and Heumann, C. (2018). Bootstrap inference when using multiple imputation. Stat. Med. 37, 2252–2266. doi: 10.1002/sim.7654
Schubert, M., Ludwig, J., Freiberg, A., Hahne, T. M., Romero Starke, K., Girbig, M., et al. (2021). Stigmatization from work-related COVID-19 exposure: a systematic review with Meta-analysis. Int. J. Environ. Res. Public Health 18:6183. doi: 10.3390/ijerph18126183
Schug, C., Morawa, E., Geiser, F., Hiebel, N., Beschoner, P., Jerg-Bretzke, L., et al. (2021). Social support and optimism as protective factors for mental health among 7765 healthcare Workers in Germany during the COVID-19 pandemic: results of the VOICE study. Int. J. Environ. Res. Public Health 18:3827. doi: 10.3390/ijerph18073827
Scott, H. R., Stevelink, S. A. M., Gafoor, R., Lamb, D., Carr, E., Bakolis, I., et al. (2023). Prevalence of post-traumatic stress disorder and common mental disorders in health-care workers in England during the COVID-19 pandemic: a two-phase cross-sectional study. Lancet Psychiatry 10, 40–49. doi: 10.1016/s2215-0366(22)00375-3
Sheen, J., Aridas, A., Tchernegovski, P., Dudley, A., McGillivray, J., and Reupert, A. (2021). Investigating the impact of isolation during COVID-19 on family functioning – an Australian snapshot. Front. Psychol. 12:722161. doi: 10.3389/fpsyg.2021.722161
Sheen, J., Clancy, E. M., Considine, J., Dwyer, A., Tchernegovski, P., Aridas, A., et al. (2022). “Did You bring it home with You?” a qualitative investigation of the impacts of the COVID-19 pandemic on Victorian frontline healthcare workers and their families. Int. J. Environ. Res. Public Health 19:4897. doi: 10.3390/ijerph19084897
Slade, T., Grove, R., and Burgess, P. (2011). Kessler psychological distress scale: normative data from the 2007 Australian National Survey of mental health and wellbeing. Aust. N Z J Psychiatry 45, 308–316. doi: 10.3109/00048674.2010.543653
Spányik, A., Simon, D., Rigó, A., Griffiths, M. D., and Demetrovics, Z. (2022). Subjective COVID-19-related work factors predict stress, burnout, and depression among healthcare workers during the COVID-19 pandemic but not objective factors. PLoS One 17:e0270156. doi: 10.1371/journal.pone.0270156
State Government of Victoria (2023). Victorian COVID-19 Data. Available at: https://www.coronavirus.vic.gov.au/victorian-coronavirus-covid-19-data (Accessed June 22, 2023).
Sunderland, M., Slade, T., Carragher, N., Batterham, P., and Buchan, H. (2013). Age-related differences in internalizing psychopathology amongst the Australian general population. J. Abnorm. Psychol. 122, 1010–1020. doi: 10.1037/a0034562
Tennant, P. W. G., Murray, E. J., Arnold, K. F., Berrie, L., Fox, M. P., Gadd, S. C., et al. (2021). Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int. J. Epidemiol. 50, 620–632. doi: 10.1093/ije/dyaa213
Textor, J., van der Zander, B., Gilthorpe, M. S., Liśkiewicz, M., and Ellison, G. T. H. (2016). Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int. J. Epidemiol. 45, 1887–1894. doi: 10.1093/ije/dyw341
Tonidandel, S., and LeBreton, J. M. (2011). Relative importance analysis: a useful supplement to regression analysis. J. Bus. Psychol. 26, 1–9. doi: 10.1007/s10869-010-9204-3
van Buuren, S., and Groothuis-Oudshoorn, K. (2011). Mice: multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67. doi: 10.18637/jss.v045.i03
Van Wert, M. J., Gandhi, S., Gupta, I., Singh, A., Eid, S. M., Haroon Burhanullah, M., et al. (2022). Healthcare worker mental health after the initial peak of the COVID-19 pandemic: a US medical center cross-sectional survey. J. Gen. Intern. Med. 37, 1169–1176. doi: 10.1007/s11606-021-07251-0
Verelst, F., Kuylen, E., and Beutels, P. (2020). Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Eur. Secur. 25:2000323. doi: 10.2807/1560-7917.es.2020.25.13.2000323
Verougstraete, D., and Hachimi Idrissi, S. (2020). The impact of burn-out on emergency physicians and emergency medicine residents: a systematic review. Acta Clin. Belg. 75, 57–79. doi: 10.1080/17843286.2019.1699690
Wang, M.-T., Henry, D. A., Del Toro, J., Scanlon, C. L., and Schall, J. D. (2021). COVID-19 employment status, dyadic family relationships, and child psychological well-being. J. Adolesc. Health 69, 705–712. doi: 10.1016/j.jadohealth.2021.07.016
Wang, L. Q., Zhang, M., Liu, G. M., Nan, S. Y., Li, T., Xu, L., et al. (2020). Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J. Psychiatr. Res. 129, 198–205. doi: 10.1016/j.jpsychires.2020.07.008
Westrupp, E. M., Greenwood, C. J., Fuller-Tyszkiewicz, M., Olsson, C. A., Sciberras, E., Mikocka-Walus, A., et al. (2021a). Parent and child mental health trajectories April 2020 to May 2021: strict lockdown versus no lockdown in Australia. Aust. N Z J Psychiatry 56, 1491–1502. doi: 10.1177/00048674211065365
Westrupp, E. M., Stokes, M. A., Fuller-Tyszkiewicz, M., Berkowitz, T. S., Capic, T., Khor, S., et al. (2021b). Subjective wellbeing in parents during the COVID-19 pandemic in Australia. J. Psychosom. Res. 145:110482. doi: 10.1016/j.jpsychores.2021.110482
Wijeratne, C., Johnco, C., Draper, B., and Earl, J. (2021). Doctors' reporting of mental health stigma and barriers to help-seeking. Occup. Med. (Lond) 71, 366–374. doi: 10.1093/occmed/kqab119
World Health Organisation (2021). COVID-19 Weekly Epidemiological Update, 31 January 2021. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20210202_weekly_epi_update_25.pdf (Accessed June 22, 2023).
World Health Organisation (2022). Tracking SARS-CoV-2 Variants. Available at: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (Accessed June 22, 2023).
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., et al. (2020). Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 277, 55–64. doi: 10.1016/j.jad.2020.08.001
Yan, H., Ding, Y., and Guo, W. (2021). Mental health of medical staff during the coronavirus disease 2019 pandemic: a systematic review and Meta-analysis. Psychosom. Med. 83, 387–396. doi: 10.1097/psy.0000000000000922
Yuan, K., Huang, X.-L., Yan, W., Zhang, Y.-X., Gong, Y.-M., Su, S.-Z., et al. (2021). A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action. Mol. Psychiatry 27, 19–33. doi: 10.1038/s41380-021-01295-8
Zeileis, A. (2004). Econometric computing with HC and HAC covariance matrix estimators. J. Stat. Softw. 11, 1–17. doi: 10.18637/jss.v011.i10
Zeileis, A., Köll, S., and Graham, N. (2020). Various versatile variances: an object-oriented implementation of clustered Covariances in R. J. Stat. Softw. 95, 1–36. doi: 10.18637/jss.v095.i01
Żemojtel-Piotrowska, M., Piotrowski, J., Cieciuch, J., Adams, B., Osin, E., Ardi, R., et al. (2017). Measurement invariance of personal well-being index (PWI-8) across 26 countries. J. Happiness Stud. 18, 1697–1711. doi: 10.1007/s10902-016-9795-0
Keywords: healthcare, doctors, nurses, COVID, pandemic, public and global mental health, risk factors, protective factors indent: first line: 1.27 cm formatted: normal
Citation: Lee BEC, Ling M, Boyd L, Olsson CA and Sheen J (2023) Key predictors of psychological distress and wellbeing in Australian frontline healthcare workers during COVID-19 (Omicron wave). Front. Psychol. 14:1200839. doi: 10.3389/fpsyg.2023.1200839
Edited by:
Juan Gómez-Salgado, University of Huelva, SpainReviewed by:
Samir Al-Adawi, Sultan Qaboos University, OmanCristian Ramos-Vera, Cesar Vallejo University, Peru
Antonio Serpa Barrientos, National University of San Marcos, Peru
Copyright © 2023 Lee, Ling, Boyd, Olsson and Sheen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian En Chyi Lee, YnJpYW4ubGVlQGRlYWtpbi5lZHUuYXU=
†ORCID: Craig A. Olsson https://orcid.org/0000-0002-5927-2014
 Brian En Chyi Lee
Brian En Chyi Lee Mathew Ling1,2
Mathew Ling1,2 Craig A. Olsson
Craig A. Olsson Jade Sheen
Jade Sheen