- 1American Center for Psychiatry and Neurology, Abu Dhabi, United Arab Emirates
- 2Department of Clinical Psychology, Utrecht University, Utrecht, Netherlands
- 3Co-eur, Utrecht, Netherlands
- 4Department of Medical and Clinical Psychology, Tilburg University, Tilburg, Netherlands
- 5Department of Clinical Psychology, Leiden University, Leiden, Netherlands
- 6Stichting Arkin GGZ, Amsterdam, Netherlands
Introduction: The Gulf Cooperation Council is experiencing socio-economic transformations, which coincides with exposure to Western beauty ideals and internalization of the Western thin-ideal, and consequently the development of body uneasiness. The present study psychometrically evaluates the Body Uneasiness Test, suitable for use in the Gulf Cooperation Council.
Methods: After translation and back-translation, the Body Uneasiness Test was administered in a clinical sample (N = 169; all completed English version), and a community-based convenience sample (N = 544; n = 202, 37.1% in Arabic) between July 2024 and July 2025. Criterion validity was determined by two receiver-operating-characteristic curve analyses, one with sample type, and one with the Body Shape Questionnaire as a reference. A confirmatory factor analysis was used to determine the factor structure and T-scores and cutoff scores were established for females and males.
Results: Internal consistency was good (ω = 0.70–0.96), convergent validity was supported (r = 0.66–0.93), and the Body Uneasiness Test discriminated well between both samples (AUC = 0.70–0.94). Sensitivity to change was established in a subsample of 20 patients and was large (Cohen’s d = 1.97–2.20). Modified five- and eight-factor structures were confirmed.
Discussion: Though some Gulf countries were underrepresented, the Body Uneasiness Test shows strong promise as a valid assessment tool for use in the Gulf Cooperation Council. However, item redundancy or overlap should be reviewed, and raw scores should first be normalized when utilizing the Body Uneasiness Test. Future research should examine test–retest reliability and further examine sensitivity to change.
1 Introduction
Body uneasiness, is associated with constructs like preoccupation with shape/weight and body dissatisfaction (Melisse and Dingemans, 2025). This phenomenon is one of the predisposing factors for eating disorders (Stice et al., 2010). However, body uneasiness is not universal, but a culturally bound syndrome (Awad et al., 2020), and historically associated with Caucasian females (Melisse et al., 2020). Consequently, related research is heavily concentrated on Western samples (Pike and Dunne, 2015).
In Western societies, body uneasiness is associated with the internalization of thin-ideal beauty standards. These standards prioritize slenderness and low body-fat (Stice et al., 2010). In contrast, traditional beauty ideals in Arab societies historically favor a curvier body. Such a physique is often associated with fertility and wealth (Melisse et al., 2020). This suggests that Arab females experience lower levels of body uneasiness (Landor et al., 2024). However, recent literature shows that the Gulf Cooperation Council (GCC; GCCcouncil, 2021) is dealing with socio-economic transformations. This coincides with exposure to Western beauty ideals, and consequent thin-ideal internalization. This may result in an increase of body uneasiness and eating disorders prevalences (Cuzzolaro et al., 2006; Melisse et al., 2024).
Modesty and coverage may offer some protection against body uneasiness by reducing appearance-related pressures and minimizing body surveillance (Swami et al., 2010). Conversely, it is also suggested that modesty and gender norms might paradoxically be associated with body uneasiness in some contexts (Alteneiji, 2023; Al-Mutawa et al., 2019). While body coverage is often viewed as a religious obligation and a cultural marker of social respectability (Alteneiji, 2023), some females report internal conflict. They find it challenging to balance adherence to modest dress codes and the globalized thin-ideal. Media and peer comparison amplify these pressures. This may result in discomfort or compulsive self-monitoring (Barzoki and Alamdar, 2024). However, most self-reports measuring body image fail to fully capture such aspects of body uneasiness.
The two-part Body Uneasiness Test (BUT; Cuzzolaro et al., 2006) is a self-report instrument measuring various aspects of negative body image, such as body avoidance, and compulsive self-monitoring (BUT-A). The second section (BUT-B) assesses concerns toward specific body parts. Prior studies conducted in Western societies show five subscales of the BUT-A, and eight for the BUT-B (Cuzzolaro et al., 2006; Marano et al., 2007; Pokrajac-Bulian et al., 2015). Examining the psychometric characteristics of the BUT in the GCC yields significant benefits for understanding and addressing body uneasiness within the Arab context. Its validation may contribute to more accurate diagnoses, improved assessment of treatment outcomes for eating disorders, and enhance knowledge into the cultural aspects on body uneasiness (Cornelissen and Tovée, 2021).
The aim of the present study is to examine the psychometric properties (internal consistency, convergent validity, incremental validity, criterion-related validity, sensitivity to change and factor structure) and to establish norms, including percentile scores and normalized T-scores, of the BUT in the GCC among individuals with an eating disorder and in the general population.
2 Materials and methods
2.1 Design and procedure
The present study is predominantly a cross-sectional psychometric validation study comparing a clinical sample of individuals diagnosed with an eating disorder characterized by overvaluation of shape/weight (n = 169) with a community-based convenience sample (n = 544). Additionally, sensitivity to change was assessed using longitudinal data from a smaller clinical subsample (n = 20). The BUT was validated against the Body Shape Questionnaire (BSQ) to measure negative body image. Participants received information about the study and provided informed consent by ticking a box in Qualtrics (2024). For minors, consent was obtained from a parent or caretaker. Subsequently, demographics and the self-reports were administered. Participants could complete the self-reports in English or Arabic. All data were collected anonymously through a web-browser or mobile-app, and obtained and stored in online survey platform Qualtrics. The study was approved on June 11, 2024 by the Ethics Review Board of the American Center for Psychiatry and Neurology, Abu Dhabi (ACPN_0064).
2.2 Participants and recruitment
Data collection took place between June 2024 and July 2025. Inclusion criteria for both samples were Gulf Cooperation Council (GCC; Bahrain, Kuwait, Oman, Saudi Arabia, Qatar, the United Arab Emirates) residency and aged ≥14. Residents from Bahrain and Oman were eligible but not actively recruited, resulting in possible underrepresentation. The clinical sample included Emiratis and expatriates from the Gulf, North Africa, and the Levant, and was recruited from one of two specialized eating disorder centers in the United Arab Emirates (UAE). Web-based treatment was offered for patients from other GCC countries. Participants first had a diagnostic interview with a clinical psychologist. Subsequently, they were invited to participate in the study, before they commenced treatment. At post-treatment, they completed the BUT again. The community-based sample was recruited via social media platforms, and WhatsApp groups (Melisse et al., 2025), which were chosen because it is challenging to gather data from GCC residents, who are less inclined to participate in research (Melisse et al., 2022a).
2.3 Measures
Background variables: A pre-established checklist was used to administer demographics and to assess the presence of comorbid psychopathology: participants were asked to indicate (tick) which of the listed diagnoses were present.
2.4 Body uneasiness test (BUT)
The BUT (Cuzzolaro et al., 2006) is a self-report measuring several dimensions of negative body image among individuals with and without an eating disorder. It has two sections, the BUT-A and the BUT-B. The items on both sections are answered on a 6-point Likert scale from 0 (never) to 5 (always) regarding the frequency of these feelings. Higher scores indicate greater body uneasiness. The BUT-A has 34 items, measuring negative body image, compulsive self-monitoring, avoidance, and estrangement feelings toward the body. The BUT-A Global Severity Index (GSI) is the averaged score on all items, and ranges between 0 and 5. Though cutoff scores vary over cultures, the Italian and the Dutch version have a cutoff of >1.2 indicating clinical levels of body uneasiness (Cuzzolaro et al., 2006; Van Uffelen et al., 2025). Subscales of the BUT-A are weight phobia (items 9, 10, 18, 21, 24, 31, 32, 33), body image concerns (3, 4, 6, 12, 15, 22, 23, 25, 34), avoidance (5, 8, 13, 16, 19, 30), compulsive self-monitoring (1, 11, 17, 20, 27) and depersonalization (2, 7, 14, 26, 28, 29). The BUT-B has 37 items, assessing uneasiness, shame, or disgust (“I hate…”) with specific body parts and functions (odor, noises, sweat, blushing). The total score of the BUT-B involves two parts, (i) the Positive Symptom Total (PST), operationalized as the sum of items scored higher than 0 (range 0–37), and (ii) the Positive Symptom Distress Index (PSDI): the averaged total score on the PST items (range 0–5). Dutch cutoffs are >15.5 and >1.9 for the BUT-B PST and PSDI, respectively (Van Uffelen et al., 2025). The BUT-B subscales are indicated by roman numerals: B I: Mouth (11, 10, 8, 9, 12, 7), B II: Face Shape (3, 2, 15, 14, 6, 13), B III: Thighs (29, 28, 25, 24, 30), B IV: Legs (31, 32, 33, 21, 1), B V: Arms (20, 23, 22, 19, 26), B VI: Mustache (18, 16, 17), B VII: Skin (4, 5), B VIII: Blushing (27, 34, 35, 36, 37). Prior studies showed that the BUT subscales have sufficient internal consistency (Cronbach’s α > 0.70), and good test–retest reliability (r > 0.70) (Cuzzolaro et al., 2006; Marano et al., 2007; Pokrajac-Bulian et al., 2015).
To establish an Arabic version (see Supplementary Appendix 1), two independent translators (one with eating disorder expertise, one certified) translated the BUT. A third expert compared translations, and a consensus meeting was held to finalize this version. For the back-translation, three new translators repeated this process. Discrepancies between the back-translation and the original were resolved by consensus (Swami and Barron, 2019). The translations were piloted: students rated comprehension of all Arabic items on a 4-point Likert scale (1, I do not understand at all, 4, Completely clear). The translation was understandable (comprehensiveness rating: M = 3.2, SD = 0.3). However, none of the participants in the clinical sample preferred the Arabic version over the English one. In the community-based sample, n = 342/544, 62.9% participants completed the BUT in English, and n = 202/544, 37.1% in Arabic.
2.5 Body shape questionnaire (BSQ)
The BSQ (Cooper et al., 1987), a self-report questionnaire measuring negative body image over the past 28 days, was validated for use in Arab societies (Melisse et al., 2022b). Internal consistency of the BSQ was excellent in the present study (McDonald’s ω = 0.95).
2.6 Eating disorder examination questionnaire (EDE-Q)
The EDE-Q (Fairburn and Beglin, 2008), a self-report questionnaire measuring eating disorder pathology over the past 28 days, was validated for use in Arab societies (Melisse et al., 2021). Internal consistency of the EDE-Q was excellent in the present study (McDonald’s ω = 0.89).
2.7 Power
The confirmatory factor analysis (CFA) required 3–20 times the number of items as a minimum sample size with an absolute range of 100–1,000 (Mundfrom et al., 2005). The minimum thresholds for the present study were met with at least 102 participants for the BUT-A and 111 for the BUT-B. Sample size recommendations for establishing normalized T-scores generally range from 100 to 200 per subgroup (Wolf et al., 2013). Consequently, age-based subgroups were adequately sized (>200). However, the male subgroup (N = 86) was below this threshold, which may reduce the appropriateness of male-specific norms.
2.8 Statistical analysis
Software and assumptions: The analyses were performed in SPSS v29 (IBM Corp, 2024), R and R package Lavaan, version 0.6–5 (Rosseel, 2012) for CFA. Norms were established with the RNOmni package version 1.0.1 (McCaw, 2019), nls and nlstools (Wu and Estabrook, 2016), and mirt (Chalmers, 2012). Assumptions were checked. All results were reported in accordance with the Standards for Reporting of Diagnostic Accuracy Studies guidelines (Cohen et al., 2016). Group comparisons were made with independent sample t-tests, Chi-square tests, and Mann–Whitney U tests.
Reliability and validity: Internal consistency of the measures were calculated by Cronbach’s α and McDonald’s ω (≥0.70 acceptable, ≥0.90 excellent) (MacDonald, 1999). Convergent validity was determined by the association of the BUT-A-GSI/BUT-B and BSQ scores. Criterion-related validity (known-groups validity) was determined by comparing BUT-A/BUT-B means of the clinical versus population-based samples using t-tests, or Wilcoxon rank-sum tests for non-normal data (Wilcoxon et al., 1963). Adjusted t-values and degrees of freedom were used if homogeneity was violated (Ramseyer and Tcheng, 1973). Receiver-operating-characteristic (ROC) analysis and area-under-the-curve (AUC). AUC calculation examined how well the BUT distinguished clinical status (per BSQ) and groups membership. AUCs of >0.70 were deemed acceptable (Swets, 1988). Sensitivity to change was established in a clinical subsample with a dependent sample t-test, the correlation between change scores (change from pre- to post-treatment) on the BUT and BSQ were calculated.
Norms: Cut-off values for clinical significance were determined as explained in the Supplementary Appendix 2 (Jacobson and Truax, 1991; Jacobson et al., 1999). Additionally, norms were established by calculating normalized T-scores, and Percentile Rankorder (PR) scores. First, the effect of age and sex was examined to assess the need of age- and gender specific norms. Cross-walk tables and formulas to transform raw scores into normalized T-scores and PR-scores were established based on the frequency of responses in the clinical sample, using: , where m indicates the number of participants with a score < Raw Score (RS), and k indicates the number of participants with exactly RS and N indicates the size of the normative sample (Crawford and Garthwaite, 2009). First, as raw scores of the community-based sample were skewed to the right, scores were normalized through the Rankit approach (Ipsen and Jerne, 1944; Bliss et al., 1956). RankNorm yields percentile ranks, which were converted to normalized Z-scores using the probit function, which calculates the inverse of the cumulative distribution function (Solomon and Sawilowsky, 2009). Resulting Z-scores were converted to T-scores by T = 10*Z + 50. The procedure is described elsewhere in more detail (de Beurs et al., 2025).
Construct validity: The factor structures of the BUT-A and BUT-B were examined by confirmatory factor analysis (CFA). The response options were considered ordered, and polychoric correlations were used. The DWLS estimator was used with NLMINB as the optimization method, and we report robust fit indices. When the RMSEA was <0.05 (0.5–0.8 acceptable) and the TLI and CFI were >0.95, the model had a good fit (Hu and Hu and Bentler, 1999).
3 Results
3.1 Participants
For the clinical sample, 169 participants were recruited, who all met the inclusion criteria. There were no missing data. The sample was predominantly female (n = 151/169, 89.3%), Emirati (n = 64/169, 37.9%), diagnosed with anorexia nervosa (n = 84/169, 49.7%) and mean age and BMI were 26.0 (SD = 9.1) years, and 25.1 (SD = 8.8) kg/m2, respectively. Mean scores were: BUT-A-GSI = 2.48 (SD = 1.25); BUT-B-PST = 19.18 (SD = 10.46); BUT-B-PSDI = 1.45 (SD = 1.05). For the community-based convenience sample, 89.8%, N = 544/606 participants had <5% missing data, n = 471/544 (87.4%) were female, and Kuwaiti 227/544 (41.7%). Mean age and BMI were 26.7 (SD = 12.1) years, and 23.5 (SD = 6.0) kg/m2. Mean BUT scores were: BUT-A-GSI = 1.15 (SD = 1.08); BUT-B-PST = 11.74 (SD = 6.89); BUT-B-PSDI = 0.79 (SD = 0.88). The gender imbalance potentially limited generalizability of the results to males. Table 1 displays the demographics of both samples and shows that the clinical sample had higher scores on the self-reports, had more comorbid psychopathology, were Emirati and from the Eastern Mediterranean region and there were differences in their daily life and highest level of education.
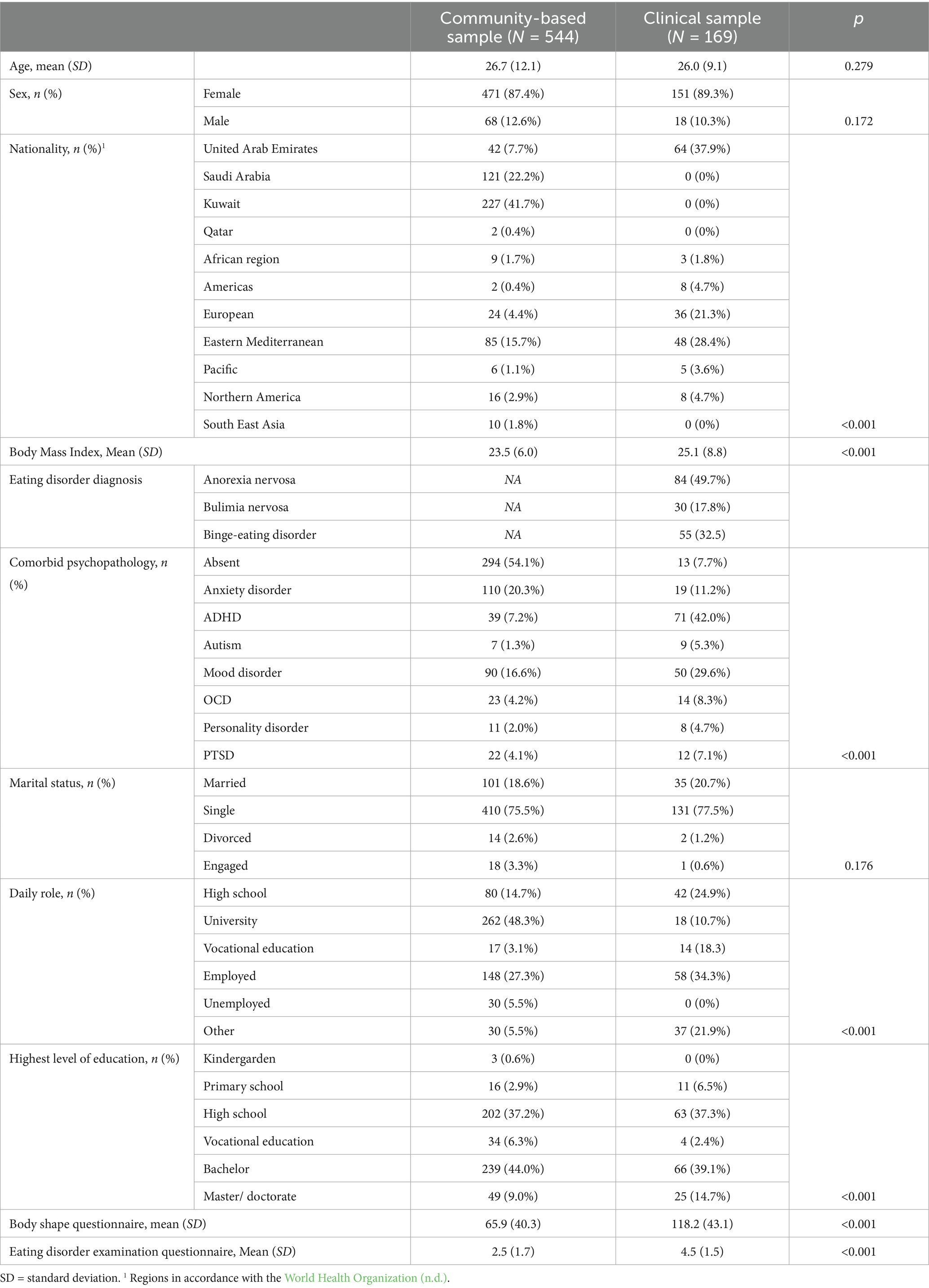
Table 1. Demographic characteristics and statistical comparisons of the clinical sample diagnosed with an eating disorder (N = 169) and a community-based convenience sample (N = 544).
3.2 Psychometric properties
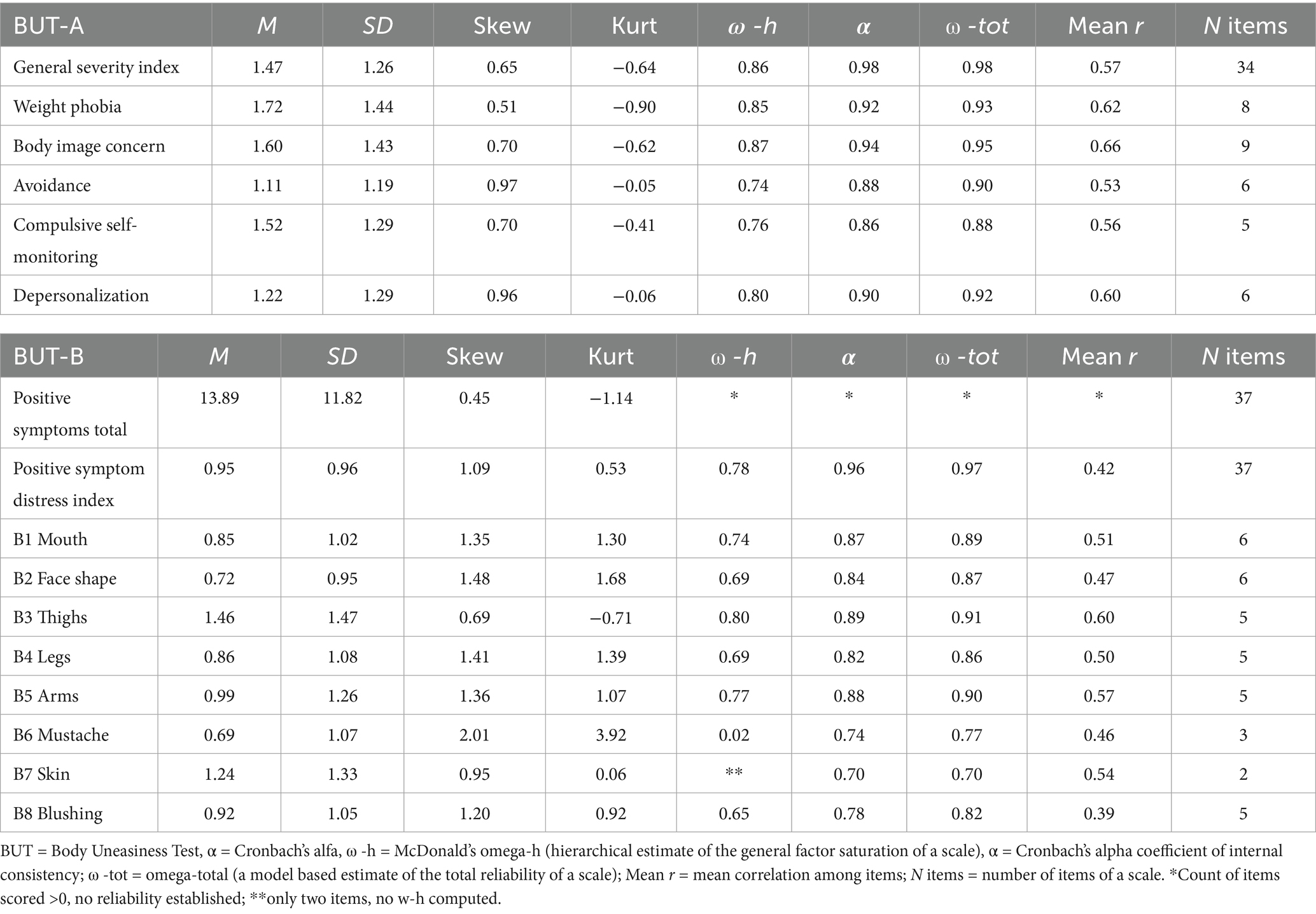
Table 2 shows the mean scores on the BUT-A and B and their subscales for the samples combined, Table 3 for both samples separately. Given the difference between females and males and between in age, Supplementary Table 2a presents mean scale scores for females and males separately and Supplementary Table 2b present the mean scores for two age groups.
3.2.1 Internal consistency
The descriptive item and scale statistics are depicted in Supplementary Tables 1, 2. Most items had a skewed responses distribution. The overrepresentation of zero-scores indicated floor effects. This skewness potentially affects factor structures and limits the interpretability of psychometric outcomes. Table 2 shows that internal consistencies of the BUT-A-GSI and scale scores were high (McDonalds ω-total = 0.88–0.98) and varied between acceptable to excellent in the BUT-B (McDonalds ω-total = 0.70 -. 96).
3.2.2 Convergent and incremental validity
The convergent validity was supported (p < 0.001): BSQ and BUT-A-GSI, and the BSQ and BUT-B-PST scores were strongly correlated in the clinical sample (BUT-A-GSI: r = 0.93; BUT-B-PST: r = 0.72), and in the community-based sample (BUT-A: r = 0.86; BUT-B-PST: r = 0.72).
In the clinical sample, 78.6% of the BUT-A-GSI scores was explained by the EDE-Q global-score [R2 = 0.79, F(1, 169) = 407.3, p < 0.001]. The BUT-A scores were strongly correlated with the EDE-Q global-score (r = 0.89, p < 0.001). The BUT-B-PST scores were also fairly associated with the EDE-Q global-score, BUT-B-PST: Adjusted R2 = 0.44, r = 0.66, p = <0.001, F(1, 169) = 87.2. This indicated that the BUT added value by assessing specific aspects of body uneasiness not captured by the EDE-Q. The results were somewhat less convincing in the community-based sample, but still substantial correlations were found, BUT-A-GSI: Adjusted R2 = 0.47, r = 0.66, p = <0.001, F(1,543) = 261.5; BUT-B-PST: Adjusted R2 = 0.34, r = 0.58, p = <0.001, F(1,543) = 98.4. Though the convergent and incremental validity were high, they could indicate redundancy between measures.
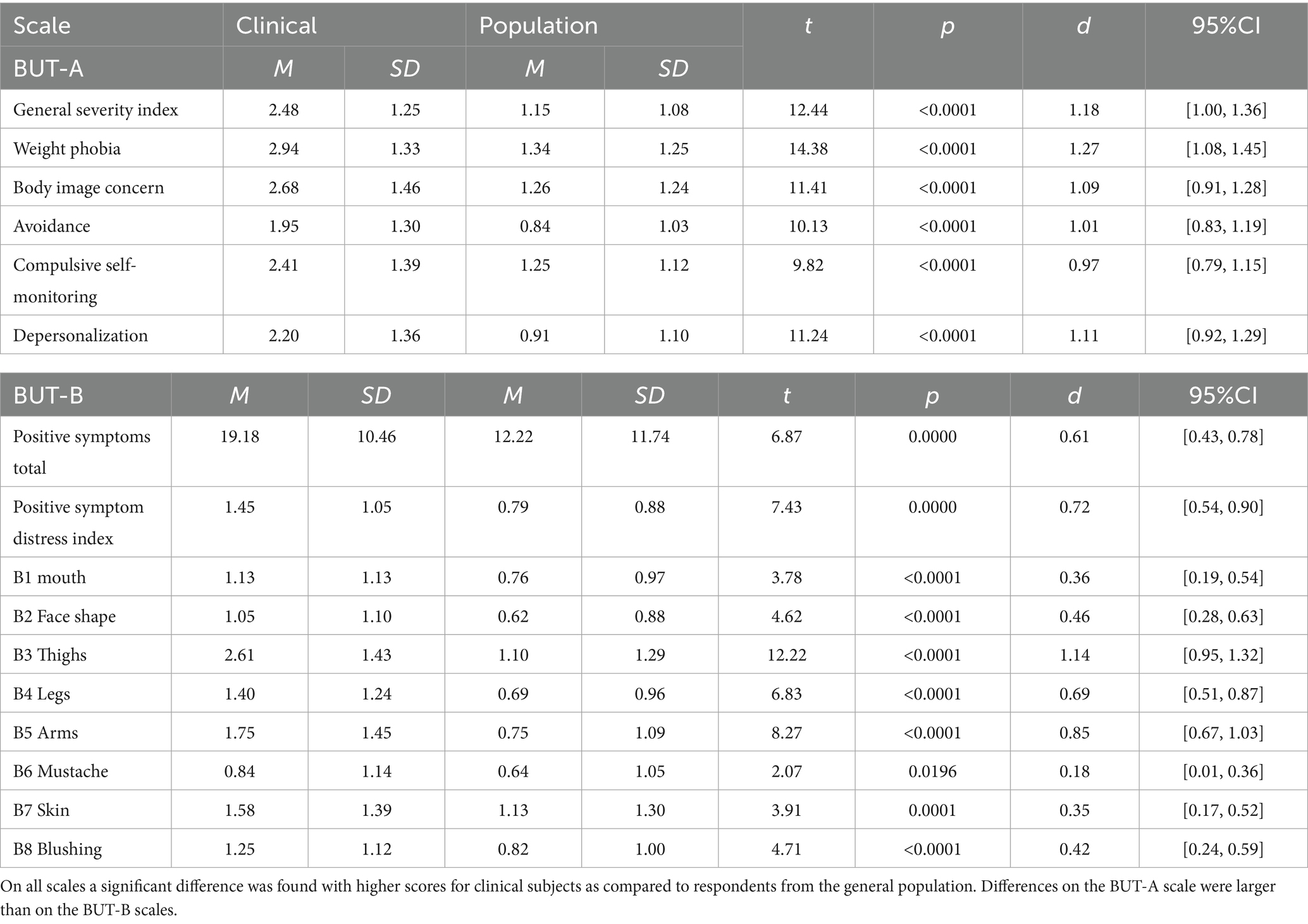
Table 3 shows the results of comparing scale scores of both samples with independent t-tests. Cohen’s d indicated a large effect size (d ≈ 0.80) for the majority of scales, with the exception of B1, B2, and B6–B8, which showed medium effects (d ≈ 0.50).
3.2.3 Criterion-related validity
The BUT-A-GSI and the BUT-B-PST accurately measured a negative body image according to the BSQ among individuals with an eating disorder. High AUCs were revealed (p < 0.001) for the BUT-A-GSI [AUC = 0.94 (0.93–0.95),] and the BUT-B-PST [AUC = 0.89 (0.87–0.91)]. In addition, when sample type was used as a criterion, a high AUC (p < 0.001) was revealed for the BUT-A-GSI [AUC = 0.87 (0.83–0.90)], and an acceptable AUC for the BUT-B-PST [AUC = 0.70 (0.65–0.76)]. This indicated that the BUT accurately discriminated between the clinical and the community-based sample. An individual in the clinical sample had an 87% more likelihood of having a higher score on the BUT-A, and 70% more on the BUT-B compared to an individual from the community-based sample. Additionally, Table 3 shows that according to one-sided t-tests that the clinical sample had higher scores compared to the non-clinical sample on the BUT-A-GSI, BUT-B-PST, and the BUT-B-PDSI.
3.2.4 Sensitivity to change
In the clinical sample, sensitivity to change was demonstrated [paired samples t-test: BUT-A-GSI: t(19) = 12.5, p = <0.001, Cohen’s d = 1.97 (1.75, 2.20); BUT-B-PST: t(19) = 12.3, p = <0.001, Cohen’s d = 2.20 (1.97, 2.44)], which was similar to the sensitivity to change of the BSQ [paired samples t-test: BSQ: t(19) = 12.8, p = <0.001]. Additionally, a strong positive correlation was found between change scores on the BUT and the BSQ [r = 0.82, p < 0.001, Cohen’s d = 1.39 (1.09, 1.67)], further demonstrating similarity in sensitivity to change of both measures. However, it should be noted that these analyses were performed in a small subset of 20 clinical participants pre-post treatment, and these results should be interpreted with caution.
3.2.5 Confirmatory factor analysis
Table 4 shows sufficient fit for the modified five-factor model of the BUT-A, with better fit than competing models. Modification indices suggested that some items overlapped conceptually, e.g., feeling detached from your body and feeling that your body does not belong to you (items 28 and 29), and being in front of the mirror and looking at oneself (items 1 and 11). Allowing these similar items’ error to correlate improved model-fit. Additionally, cross-loadings were allowed for item 2 on both the compulsive self-monitoring and weight phobia factors, and for item 29 on the weight phobia factor. Table 4 also indicated that for the BUT-B a modified eight-factor structure showed good fit. Modification indices allowing for correlated error terms between item pairs: 16–17 (mustache-beard), 24–25 (stomach-abdomen), 29–31 (thighs-legs), 27–28 (buttocks-hips), and 22–23 (chest-breasts) improved fit further. The overlap between items indicated that some items load on more than one latent trait and therefore items address closely related topics. The shared variance was not fully accounted for by the broader factor structure.
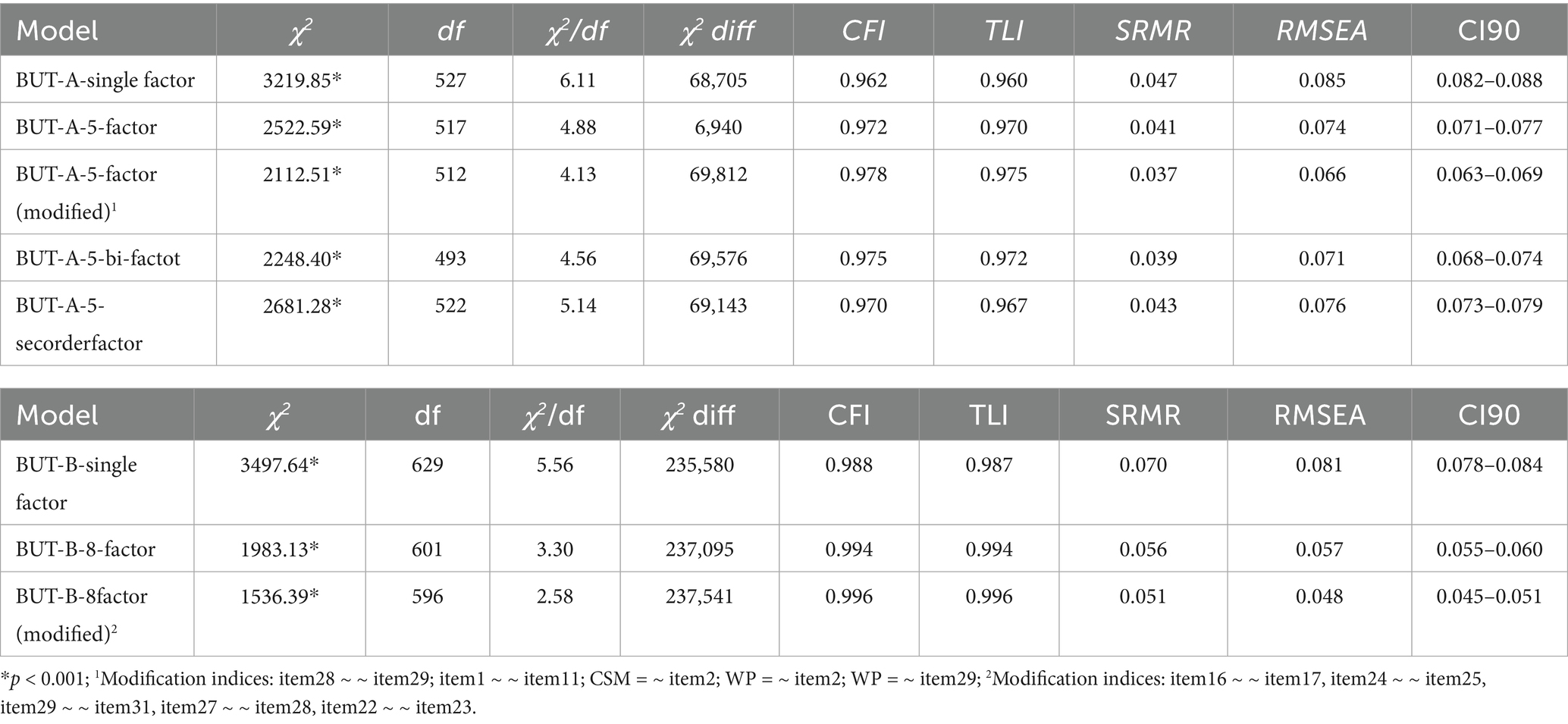
Table 4. Indicators of unidimensionality (robust; response categories considered to be ordered); baseline χ2 = 71924.50 for the BUT-A, and indicators of unidimensionality (robust; response categories considered to be ordered); baseline χ2 = 239077.87 for the BUT-B.
3.2.6 Norms
Supplementary Table 3 offers a crosswalk from a selection of raw scores for the General Severity Index score of the BUT-A to population-based T-scores and population based and clinical PR-scores. Additionally, Supplementary Table 3 provides a clinical utilization example. Generally, T- and PR-scores are interpreted as shown in Supplementary Appendix 2. Supplementary Tables 3a–8a present crosswalk tables for the BUT-A, and its subscales for females and males, separately. Given the gender-differences (BUT-A: p = 0.018; BUT-B: p = 0.048), Supplementary Tables 9–10a do so for the BUT-B-PST and BUT-B-PSDI.
3.2.7 Cut-off values
3.2.7.1 Screening
Supplementary Table 3 shows that overall, the originally proposed cutoff score of >1.2 for the BUT-A corresponds to T > 53.5, which is close to the general population mean of T = 50 and represents an only mildly elevated score. The earlier cut-off values proposed (Cuzzolaro et al., 2006) were based on ROC analysis and provide an optimal balance of sensitivity and specificity. The ROC analysis of the present data indicated a cut-off value of RS > 1.62 as providing optimal sensitivity (92%) and specificity (64.6%).
3.2.7.2 Reliable and clinically significant change
Supplementary Appendix 2 and Supplementary Table 12 present cut-off values for Clinical Significant Change and Reliable Change (Jacobson et al., 1999). These analyses suggest an RCI-95 of 0.41, which corresponds roughly to a shift in T-score of 5 points. Furthermore, the cut-off value for recovery for the GCC is RS > 1.77 (T > 57.1) for the BUT-A-GSI. Suggested cut-off values for recovery for the BUT-B-PST and BUT-B-PSDI were RS > 15.9 (T > 55.2) and RS >1.09 (T > 56.1), respectively.
4 Discussion
The aim of the present study was to psychometrically evaluate the BUT in the GCC. Reliability, validity, clinical utility were supported and the original five-factor structure of the BUT-A and the eight-factor structure of the BUT-B were confirmed in the combined clinical and community-based samples. Modification indices suggested that some items measure similar concepts, which should be considered when interpreting the factor structure: body ownership (feeling detached from your body, and feeling your body does not belong to you), self-observation (being in front of the mirror, and looking at oneself), and body parts: mustache-beard, stomach-abdomen, thighs-legs, buttocks-hips, and chest-breasts. These overlaps are likely due to linguistic/cultural adaptation, as they were not reported by Pokrajac-Bulian et al. (2015), who examined modification indices. Allowing correlated error terms between items improved model fit, and future work should review conceptually overlapping pairs and consider removal of redundant items. Consequently, future work could establish a shortened version, or conduct an Item Response Theory (IRT) analysis (De Beurs et al., 2022) to refine the scales. In addition, gender specific norms were established. Furthermore, sensitivity to change was confirmed in a small clinical subsample. Moreover, there was an overrepresentation of zero-responses, especially in the community-based sample. Subsequently, a limitation of the BUT may be that cultural minimization of body concerns and reluctance to endorse sensitive items can affect responses (Thompson et al., 2004). Therefore, it is necessary to utilize normalized T-scores for norm tables, because raw scores should first be normalized with a curvilinear conversion formula. Finally, zero-inflation could impact the factor analytic results. Future research could employ zero-inflated factor analytic techniques, such as Factor Mixture Modeling (Lubke and Muthen, 2005), Zero-Inflated IRT (De Boeck et al., 2011), or All-Zero Inflated Exploratory Factor Analysis (Flora and Curran, 2004), to explicitly account for the impact of structural zero-responses on factor loadings and model parameters.
The present study has several limitations. Although the BUT was available in Arabic and found understandable, all participants in the clinical sample preferred the English version over the Arabic one. This was in accordance with other work in the UAE (Melisse et al., 2025), and might be because the therapy sessions were mainly held in English, more modernized individuals were seeking therapy, most citizens being bilingual, social desirability or sample bias toward English speaking populations (Alkhadari et al., 2016; Griffiths et al., 2015; Gulf Articles, 2025). This preference could also reflect the dominance of English in health-care services in the UAE (Al-Yateem et al., 2023). Future studies should examine whether the language of administration of the BUT affects responses, if the BUT is equally suitable for less bilingual individuals and future validation in a purely Arab speaking sample is recommended. An important limitation was the absence of test–retest reliability, which prevented drawing conclusion of the stability of scores on the measure over a short test–retest interval. Consequently, assessing test–retest reliability is recommended for future research. Sensitivity to change was based on pre-posttreatment data of 20 participants only, since a small sample had completed treatment within the studies time window. Its interpretation warrants caution. Finally, generalizability might be limited due to underrepresentation of some GCC countries, self-selection from convenience sampling via social media, and a smaller male sample. Especially, norms for males should be interpreted with caution. A strength of the study was the large sample size, the more remarkable given the socially reclusive population (Al-Darmaki, 2003), and the implementation of app based use. Finally, this was the second study in the region including a clinical sample (el Khazen-Hadati et al., 2024), future work could benefit from cross-cultural comparisons, and integration into clinical practice.
In conclusion, the BUT shows strong promise as a valid assessment tool for use in the GCC, the original five-factor structure of the BUT-A and the eight-factor structure of the BUT-B were confirmed. However, item redundancy or item overlap should be reviewed, and raw scores should be normalized when utilizing the BUT norms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, upon reasonable request.
Ethics statement
The studies involving humans were approved on June 11, 2024 by the Ethics Review Board of the American Center for Psychiatry and Neurology, Abu Dhabi (registration number ACPN_0064). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
BM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Writing – original draft. CK: Writing – review & editing. EB: Formal analysis, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We wish to express our gratitude to all respondents who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI sttaement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1690293/full#supplementary-material
References
Al-Darmaki, F. R. (2003). Attitudes towards seeking professional psychological help: what really counts for United Arab Emirates university students. Soc. Behav. Personal. Int. J. 31, 497–508. doi: 10.2224/sbp.2003.31.5.497
Alkhadari, S., Alsabri, A. O., Mohammad, I. H. A., Atwan, A. A., Alqudaihi, F., and Zahid, M. A. (2016). Prevalence of psychiatric morbidity in the primary health clinic attendees in Kuwait. J. Affect. Disord. 195, 15–20. doi: 10.1016/j.jad.2016.01.037
Al-Mutawa, N., Schuilenberg, S.-J., Justine, R., and Kulsoom Taher, S. (2019). Modesty, objectification, and disordered eating patterns: a comparative study between veiled and unveiled Muslim women residing in Kuwait. Med. Princ. Pract. 28, 41–47. doi: 10.1159/000495567
Alteneiji, E. (2023). Value changes in gender roles: perspectives from three generations of Emirati women. Cogent Soc. Sci. 9. doi: 10.1080/23311886.2023.2184899
Al-Yateem, N., Hijazi, H., Saifan, A. R., Ahmad, A., Masa'Deh, R., Alrimawi, I., et al. (2023). Quality and safety issue: language barriers in healthcare, a qualitative study of non-Arab healthcare practitioners caring for Arabic patients in the UAE. BMJ Open Online 13. doi: 10.1136/bmjopen-2023-076326
Awad, G. H., Kashubeck-West, S., Bledman, R. A., Coker, A. D., Stinson, R. D., and Mintz, L. B. (2020). The role of enculturation, racial identity, and body mass index in the prediction of body dissatisfaction in African American women. J. Black Psychol. 46, 3–28. doi: 10.1177/0095798420904273
Barzoki, M. H., and Alamdar, F. S. (2024). Body shame and sexual attractiveness: a grounded theory research among Iranian women. Sex. Cult. 29, 336–356. doi: 10.1007/s12119-024-10269-1
Bliss, C., Greenwood, M. L., and White, E. S. (1956). A rankit analysis of paired comparisons for measuring the effect of sprays on flavor. Biometrics 12, 381–403. doi: 10.2307/3001679
Chalmers, R. P. (2012). mirt: a multidimensional item response theory package for the R environment. J. Statistic. Softw. 48.
Cohen, J. F., Korevaar, D. A., Altman, D. G., Bruns, D. E., Gatsonis, C. A., Hooft, L., et al. (2016). STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ open, 6:e012799. doi: 10.1136/bmjopen-2016-012799
Cooper, P. J., Taylor, M. J., Cooper, Z., and Fairburn, C. G. (1987). The development and validation of the body shape questionnaire. Int. J. Eat. Disord. 6, 485–494. doi: 10.1002/1098-108X(198707)6:4<485::AID-EAT2260060405>3.0.CO;2-O
Cornelissen, P. L., and Tovée, M. J. (2021). Targeting body image in eating disorders. Curr. Opin. Psychol. 41, 71–77. doi: 10.1016/j.copsyc.2021.03.013
Crawford, J. R., and Garthwaite, P. H. (2009). Percentiles please: the case for expressing neuropsychological test scores and accompanying confidence limits as percentile ranks. Clin. Neuropsychol. 23, 193–204. doi: 10.1080/13854040801968450
Cuzzolaro, M., Vetrone, G., Marano, G., and Garfinkel, P. E. (2006). The body uneasiness test (BUT): development and validation of a new body image assessment scale. Eating and weight disorders - studies on anorexia. Bulimia Obesity 11, 1–13. doi: 10.1007/BF03327738
De Beurs, E., Böhnke, J. R., and Fried, E. I. (2022). Common measures or common metrics? A plea to harmonize measurement results. Clin. Psychol. Psychother. 29, 1755–1767. doi: 10.1002/cpp.2742
de Beurs, E., Giltay, E. J., and Carlier, I. V. (2025). Community norms for the symptom questionnaire (SQ-48): normalised T-scores and percentile rank order scores. Clin. Psychol. Psychother. 32:e70056. doi: 10.1002/cpp.70056
De Boeck, P., Bakker, M., Zwitser, R., Nivard, M., Hofman, A., Tuerlinckx, F., et al. (2011). The estimation of item response models with the lmer function from the lme4 package in R. J. Statistic. Softw. 39.
el Khazen-Hadati, C., Kassie, S. A., Bertl, B., Sidani, M. F., Melad, M. A. W., and Ammar, A. (2024). Psychometric properties of the eating disorder examination questionnaire (EDE-Q) and the clinical impairment assessment (CIA) using a heterogenous clinical sample from Arab countries. SAGE Open 14. doi: 10.1177/21582440241299528
Fairburn, C. G., and Beglin, S. J. (2008). Eating disorder examination- questionnaire (6.0). New York: Guilford Press.
Flora, D. B., and Curran, P. J. (2004). An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol. Methods 9, 466–491. doi: 10.1037/1082-989X.9.4.466
GCCcouncil. (2021). Secretariat General of the Gulf Cooperation Council, The Cooperation Council for the Arab States of the Gulf, GCC [Online]. Cooperation Council for the Arab States of the Gulf Available. Available online at: gcc-sg.org/en-us/Pages/default.aspx (Accessed January 1, 2024)
Griffiths, S., Mond, J. M., Murray, S. B., Thornton, C., and Touyz, S. (2015). Stigma resistance in eating disorders. Soc. Psychiatry Psychiatr. Epidemiol. 50, 279–287. doi: 10.1007/s00127-014-0923-z
Gulf Articles. (2025). Mental health awareness rises in the Gulf. [Online]. Available online at: Gulfarticles.com and https://www.gulfarticles.com/mental-health-awareness-gulf/?utm_source=chatgpt.com (Accessed August 13, 2025)
Hu, L. T., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 6, 1–55. doi: 10.1080/10705519909540118
Ipsen, J., and Jerne, N. K. (1944). Graphical evaluation of the distribution of small experimental series. Acta Pathol. Microbiol. Scandinavica, 21, 343–361.
Jacobson, N. S., Roberts, L. J., Berns, S. B., and McGlinchey, J. B. (1999). Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. J. Consult. Clin. Psychol. 67, 300–307. doi: 10.1037/0022-006X.67.3.300
Jacobson, N. S., and Truax, P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 59, 12–19. doi: 10.1037//0022-006x.59.1.12
Landor, A. M., Ramseyer Winter, V. L., Thurston, I. B., Chan, J., Craddock, N., Ladd, B. A., et al. (2024). The sociostructural-intersectional body image (SIBI) framework: understanding the impact of white supremacy in body image research and practice. Body Image 48:101674. doi: 10.1016/j.bodyim.2023.101674
Lubke, G. H., and Muthen, B. (2005). Investigating population heterogeneity with factor mixture models. Psychol. Methods 10, 21–39. doi: 10.1037/1082-989X.10.1.21
MacDonald, R. P. (1999). Test theory: a unified treatment, Mahwah [etc.]. Mahwah: Lawrence Erlbaum Associates.
Marano, G., Cuzzolaro, M., Vetrone, G., Garfinkel, P. E., Temperilli, F., Spera, G., et al. (2007). Validating the body uneasiness test (BUT) in obese patients. Eating and weight disorders - studies on anorexia. Bulimia Obesity 12, 70–82. doi: 10.1007/BF03327581
Melisse, B., Blankers, M., De Beurs, E., and Van Furth, E. F. (2022a). Correlates of eating disorder pathology in Saudi Arabia: BMI and body dissatisfaction. J. Eat. Disord. 10:126. doi: 10.1186/s40337-022-00652-4
Melisse, B., De Beurs, E., and Van Furth, E. F. (2020). Eating disorders in the Arab world: a literature review. J. Eat. Disord. Online 8:59. doi: 10.1186/s40337-020-00336-x
Melisse, B., and Dingemans, A. (2025). Redefining diagnostic parameters: the role of overvaluation of shape and weight in binge-eating disorder: a systematic review. J. Eat. Disord. 13:9. doi: 10.1186/s40337-025-01187-0
Melisse, B., Fakhri, H., Kennedy, L., Figueiras, M. J., Alshebali, M., Abu Taha, H., et al. (2025). Prevalence, phenotype and correlates of avoidant/restrictive food intake disorder symptoms in the Gulf cooperation council: an underserved region. Int. J. Eat. Disord. 58, 1060–1071. doi: 10.1002/eat.24400
Melisse, B., Van Furth, E., and De Beurs, E. (2021). The eating disorder examination-questionnaire: norms and validity for Saudi nationals. Eat. Weight Disord. Stud. Anorex., Bulim. Obes. 27, 139–150. doi: 10.1007/s40519-021-01150-3
Melisse, B., Van Furth, E., and De Beurs, E. (2022b). The Saudi-Arabic adaptation of the body shape questionnaire (BSQ34): psychometrics and norms of the full version and the short version (BSQ8C). Front. Psychol. 13:1046075. doi: 10.3389/fpsyg.2022.1046075
Melisse, B., van Furth, E., and Hoek, H. W. (2024). Systematic review of the epidemiology of eating disorders in the Arab world. Curr. Opin. Psychiatry 37, 388–396. doi: 10.1097/yco.0000000000000960
Mundfrom, D. J., Shaw, D. G., and Ke, T. L. (2005). Minimum sample size recommendations for conducting factor analyses. Int. J. Test. 5, 159–168. doi: 10.1207/s15327574ijt0502_4
Pike, K., and Dunne, P. (2015). The rise of eating disorders in Asia: a review. J. Eat. Disord. 3:33. doi: 10.1186/s40337-015-0070-2
Pokrajac-Bulian, A., Tončić, M., and Anić, P. (2015). Assessing the factor structure of the body uneasiness test (BUT) in an overweight and obese Croatian non-clinical sample. Eating and weight disorders - studies on anorexia. Bulimia Obesity 20, 215–222. doi: 10.1007/s40519-014-0166-8
Qualtrics. (2024). Qualtrics XM Platform: User Manual. Available online at: https://www.qualtrics.com/support/survey-platform/getting-started/qualtrics-topics-a-z/ (Accessed December 20, 2024).
Ramseyer, G. C., and Tcheng, T.-K. (1973). The robustness of the Studentized range statistic to violations of the normality and homogeneity of variance assumptions. Am. Educ. Res. J. 10, 235–240. doi: 10.3102/00028312010003235
Rosseel, Y. (2012). lavaan: an R package for structural equation modeling. J. Stat. Softw. 48, 1–36. doi: 10.18637/jss.v048.i02
Solomon, S. R., and Sawilowsky, S. S. (2009). Impact of rank-based normalizing transformations on the accuracy of test scores. J. Mod. Appl. Stat. Methods 8:9. doi: 10.22237/jmasm/1257034080
Stice, E., Ng, J., and Shaw, H. (2010). Risk factors and prodromal eating pathology. J. Child Psychol. Psychiatry 51, 518–525. doi: 10.1111/j.1469-7610.2010.02212.x
Swami, V., and Barron, D. (2019). Translation and validation of body image instruments: challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image 31, 204–220. doi: 10.1016/j.bodyim.2018.08.014
Swami, V., Frederick, D. A., Aavik, T., Alcalay, L., Allik, J., Anderson, D., et al. (2010). The attractive female body weight and female body dissatisfaction in 26 countries across 10 world regions: results of the international body project I. Personal. Soc. Psychol. Bull. 36, 309–325. doi: 10.1177/0146167209359702
Swets, J. A. (1988). Measuring the accuracy of diagnostic systems. Science 240, 1285–1293. doi: 10.1126/science.3287615
Thompson, J. K., van den Berg, P., Roehrig, M., Guarda, A. S., and Heinberg, L. J. (2004). The sociocultural attitudes towards appearance scale-3 (SATAQ-3): development and validation. Int. J. Eat. Disord. 35, 293–304. doi: 10.1002/eat.10257
Van Uffelen, L., De Beurs, E., and Melisse, B. (2025). Psychometric evaluation and clinical norms of a Dutch version of the body uneasiness test among individuals with eating disorder pathology. J. Clin. Psychol. (In press).
Wilcoxon, F., Katti, S., and Wilcox, R. A. (1963). Critical values and probability levels for the Wilcoxon rank sum test and the Wilcoxon signed rank test. NY: American Cyanamid Pearl River.
Wolf, E. J., Harrington, K. M., Clark, S. L., and Miller, M. W. (2013). Sample size requirements for structural equation models: an evaluation of power, Bias, and solution propriety. Educ. Psychol. Meas. 73, 913–934. doi: 10.1177/0013164413495237
World Health Organization. (n.d.). Regional offices. Available online at: https://www.who.int/about/who-we-are/regional-offices (Accessed August 19, 2025).
Keywords: body uneasiness test (BUT), Arab, validation, body image, psychometric properties, normative data, factor structure
Citation: Melisse B, el Khazen C and de Beurs E (2025) Psychometric evaluation of the body uneasiness test in the Arab Gulf region. Front. Psychol. 16:1690293. doi: 10.3389/fpsyg.2025.1690293
Edited by:
Jennifer Jordan, University of Otago, Christchurch, New ZealandReviewed by:
Zypher G. Jude Regencia, De La Salle University, PhilippinesHannah Kennedy-Smith, University of Otago, Christchurch, New Zealand
Copyright © 2025 Melisse, el Khazen and de Beurs. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernou Melisse, YmVybm91bWVsaXNzZUBvdXRsb29rLmNvbQ==
†ORCID: Bernou Melisse, orcid.org/0000-0003-2636-5262
Carine el Khazen, orcid.org/0000-0002-9783-2414
Edwin de Beurs, orcid.org/0000-0003-3832-8477
 Bernou Melisse
Bernou Melisse Carine el Khazen
Carine el Khazen Edwin de Beurs
Edwin de Beurs