- 1School of Rehabilitation Sciences, McMaster University, Hamilton, ON, Canada
- 2CanChild Centre for Childhood Disability Research, McMaster University, Hamilton, ON, Canada
Objective: This study aimed to identify school problems and levels of cognitive activity in youths aged 5–18 years with a concussion during the recovery stages of return to school (RTS).
Study Design: In a prospective cohort, participants completed in-person assessments at three time points: First Visit Post-injury, Symptom Resolution Visit, and Follow-Up Visit. These time points varied based on the participants’ recovery progress. The post-concussion symptom scale (PCSS) and a cognitive activity scale were completed every 2 days until symptom resolution was achieved. Participants and their parents completed a school questionnaire detailing how their concussion had impacted their school learning/performance and their level of concern about their injury as well as the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT).
Results: Sixty-three percent (N = 44/70) of participants returned to school by the First Visit Post-injury (average 7.7 days following injury), and of these, 50% (N = 22) were experiencing school problems. Sixty-five participants (out of 70) returned to school at the Follow-Up Visit, and of these, 18% reported school problems. There was a significant difference in the school problems reported by parents and youth. At the First Visit Post-injury, the youth reported more problems (p = 0.02), and the In-Person Symptom Resolution Visit with parents reported more problems (p = 0.01). The cognitive activity score increased, while the PCSS score decreased from RTS Stage 1 to Stage 5.
Conclusions: This study identified that 50% of youth experienced school problems at the First Visit Post-injury, whereas only 18% reported school problems at the Follow-Up Visit. There is a significant difference in the perception of school problems reported by youth and their parents at different stages of recovery. The amount and complexity of cognitive activity increased with decreasing symptoms and increasing RTS stage. Findings can guide youth with a concussion and their parents in supporting a cautious return to school with accommodations. Healthcare providers and researchers can use this knowledge to better support youth in their return to school and understand the importance of gathering information from youth and their parents to gain the best insight into recovery.
Introduction
In Ontario, the annual incidence of concussion is 1% of the population, with children having the highest incidence (3,600 per 100,000 individuals) (1, 2). A concussion has detrimental impacts on a child's physical, psychological, and academic performance (3–5), affecting school attendance (6), participation in sports or social activities (7), and quality of life (8–10). Although many children become symptom-free within 2 weeks, approximately one-third of children experience prolonged symptoms past 1 month, referred to as persistent post-concussion symptoms (PCS) (11, 12). For clarity, we will be referring individuals aged 5–18 years as youth in the context of our study.
To help guide youth in their recovery from concussion, our research team developed evidence-based return to activity (RTA) and return to school (RTS) protocols (13, 14). These protocols [now updated (15)] are based on the Sports Concussion Consensus statements (16, 17), highlighting best practices in managing concussion recovery. The importance of returning to school cautiously is emphasized in current post-concussion recovery protocols (18). Our group recently observed that youth (aged 5–18 years) return to school faster than they return to activity (35 and 38 days, respectively) and that 21% of youth were symptomatic at the full return to school (19). Similarly, Baker et al. (20) observed that one-third of concussed youth (defined in their paper as 13–19 years old) reported experiencing concussion-related symptoms and/or difficulties after returning to school (20).
Recently, Russell et al. (6) observed that following a sports-related concussion, children missed a median of 4 days of school and experienced a 1.0% decrease in their overall grade-point average (6). Upon a child's return to school, stressors such as missed activities (21) and a new curriculum can leave a child feeling overwhelmed (6), thus decreasing their academic performance (20). Furthermore, school problems and lowered grades may amplify a child's feelings of social isolation and lower their self-esteem (22). As such, it is important to determine a youth's perceived school problems following a concussion. Furthermore, it is important to assess whether youth and parents differ in their perception of a youth's school problems and concerns following a concussion.
At the outset of this study, we hypothesized that youth would experience school problems following a concussion and that cognitive activity would increase over time as symptoms resolve. The specific aims of this research were to (1) examine youths’ perception of school problems and characterize school problems experienced by youth and (2) determine the concerns related to school and academic performance of youth with a concussion and their parents. The secondary objective was to examine the cognitive activity reported by participants (23) and changing patterns of symptom scale (post-concussion symptom scale, PCSS) (24) scores as youth progress through the RTS guidelines.
Materials and methods
Study design
Participants from the Back2Play Study were recruited between November 2014 and December 2016 from the McMaster Children's Hospital Emergency Department, community referrals from primary physicians, and sports medicine clinics in Hamilton, Ontario, Canada. Participants were eligible if they were 5–18 years old, had a confirmed diagnosis of a concussion from a physician, and were symptomatic at the time of recruitment. The median time from injury to study enrolment was 7.8 days (mean: 34.8 days, minimum: 2.9 h, and maximum: 320.9 days). Those with other injuries were allowed to participate, including those with nonaccidental injuries. Youth were considered ineligible if they were unable to speak English, had a significant brain injury requiring resuscitation, were admitted to the pediatric critical care unit, and/or required surgical intervention. Informed verbal and written assent and consent were obtained from participants and their parents. The study was approved by the Hamilton Integrated Research Ethics Board (#14-376).
This prospective longitudinal cohort study had three measurement time points. Participants attended two or three in-person assessments. Some participants only had First Visit and a Follow-Up Visit because their symptoms resolved in under 28 days (N = 51). For participants whose symptoms lasted longer than 28 days, they had three visits, with the third visit being 3 months post symptom resolution.
Following recruitment, participants wore an ActiGraph (ActiGraph LLC, Pensacola, FL, United States) to record the amount of movement and sleep (reported elsewhere) (25) and completed surveys every 48 h using REDCap (26) (Research Electronic Data Capture, a browser-based data management application). The surveys included the (1) PCSS (24), a common concussion evaluation consisting of a 22-symptom checklist scored on a 0–6 severity scale (where 0 denotes “not experiencing symptom” and 6 denotes “severely experiencing symptom”), (2) a self-report of the stage of RTA/RTS guidelines, and (3) a cognitive activity scale, adapted from Brown et al. (23) (Table 1). The PCSS score and cognitive scale score were assessed at the RTS stage entry and exit. Stage entry was defined as the first of two consecutive reports of a stage, whereas stage exit was reported as the last report of a stage. The time spent in each stage varied per participant.
At each in-person visit, participants completed the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) reported here and quality of life and balance tests that are reported elsewhere (27–29). This manuscript aimed to depict school performance, concerns, and description of the amount and type of cognitive activity in youth during recovery from a concussion.
Pediatric concussion recovery guidelines
RTS stages were participant-reported. Standard guidance and an explanation of the guidelines were provided at the outset of the study. Participants were given printed copies of the guidelines for reference. Participants progressed to the next stage after 48 h in any given stage without an increase in symptoms. Participant stage progression was self-determined. During Stage 1 of RTS, youth and their families were informed that “rest” does not equal social isolation, but rather youth were encouraged to participate in home/leisure activities as tolerated without worsening symptoms (i.e., make their bed, walk around the house) (17). Youth were also advised that they should begin getting ready to get back to school gradually, and if symptoms persist, they must progress to returning to school with accommodation. At Stage 2 of the RTS guidelines, youth were encouraged to begin simple cognitive activity at home for a maximum of 30 min (15 min of screen time twice daily, begin reading) without aggravating symptoms (17). At Stage 3, youth were encouraged to build up their back-to-school routines by increasing cognitive activity in a school environment with accommodations (17). These accommodations could be within their timetable, curriculum choices, environmental modifications, and adjustments in school activity participation as dictated by the individual child's needs and symptom profile. By RTS Stage 4, it was recommended that youth return back to full days of school, attending less than 5 days a week if needed (17). Youth were also encouraged to complete as much homework as possible and complete a maximum of one test per week. Finally, at Stage 5, the final stage of RTS, youth gradually returned to normal school routines (17). Although the focus of this manuscript is on cognitive activity and problems, it is important to note that participants were also following the RTA stages for physical activity simultaneously.
School information and performance questionnaires (child)
Participants aged 9.5–18 years, recruited after July 2015, completed school performance and information questionnaires, reporting on symptoms and experiences that occurred within the “past week” (Figure 1). The questionnaire focused on school problems, defined as new problems or existing problems that have gotten worse since injury, as well as school concerns, which examined areas of concern, as well as the degree of concern. The participants were first asked the following questions: Have you returned to school yet? Participants responded “not applicable” if they were on holiday/summer vacation. Only if participants responded “yes” they were asked “Do you have any school problems since your injury (either new or existing problems that have gotten worse since the injury)?”. If participants responded yes to this question, branching logic provided the question, “What kinds of school problems are you having SINCE YOUR INJURY? Check ALL that apply, either NEW problems or existing problems that have gotten WORSE since the injury”. Questions regarding class troubles/difficulties, vulnerable times of day, and grades affected were also posed to participants who reported school problems. Participants were also asked, “Have your grades been affected?” and “Do you have troubles with any classes/subjects since your injury?” (Figure 1). For these questions (classes posing difficulties, vulnerable times of day, grades affected, how can your school help), participants could select multiple answers. Participants who had not yet returned to school or were at school but had not experienced new or worsening school problems were not asked these subsequent branching series of questions.
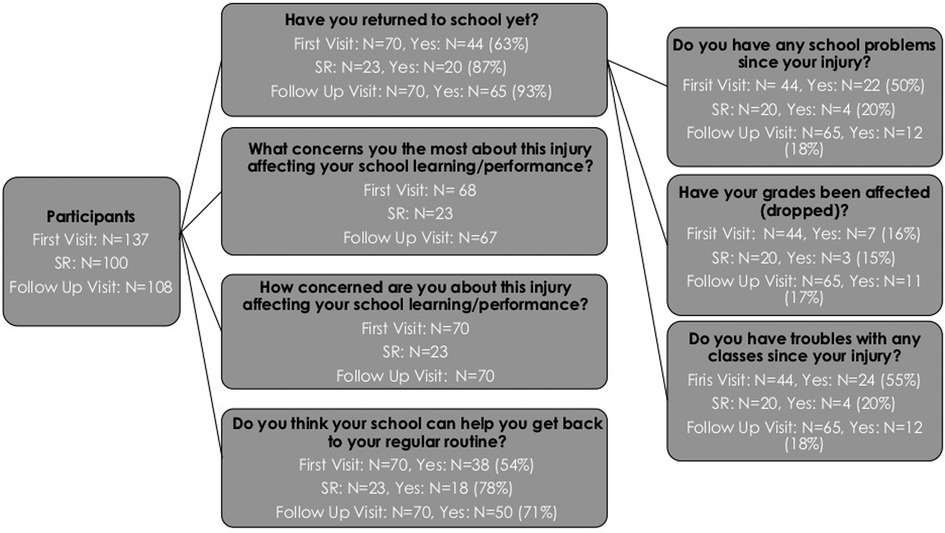
Figure 1. REDCap Question stems. Participants attended 3 in person assessments: First visit post injury, In Person Symptom resolution (if applicable), and Follow Up visit which occurred 3 months post symptom-resolution or 6 months post enrolment, whichever came first. Only participants recruited aged 9.5-18 years of age, recruited after July 2015, completed a school performance and information questionnaires. One hundred participants achieved symptom resolution within the study period, only 44 attended in person visits and were delivered the school information questionnaire.
School information and performance questionnaires (parent)
At each in-person visit, parents completed a report of their child's school problems. These questions included: “How many school days has your child missed since his/her injury (since the last survey)?”, “Does your child have troubles with any classes/subjects since the injury?”, and “How concerned are you (not concerned, mildly, moderately, very) about this injury affecting your child's school learning and performance?”. Note that the survey question related to missed school days did not explicitly ask parents to cite days missed due to concussion alone.
Statistical analysis
Descriptive statistics were performed for all data. Data were assessed for normality; if data were not normally distributed, the median was reported. To assess our first aim, examining youths’ perception of school problems, youth-reported school problems are reported as percentages and proportions of participants at the First, Symptom Resolution, and Follow-Up Visit. Our second aim, youth- and parent-reported school concerns, is also reported as percentages and proportions of participants expressing school concerns at the First, Symptom Resolution, and Follow-Up Visit. To examine the proportion of youth and parents who reported school concerns and problems, chi-square tests were performed. Median time from injury to the First Visit Post-injury and the number of missed school days were reported as mean ± standard deviation. As for our secondary aims, to test the difference between the cognitive scale scores at the entry and exit of each stage of the RTS guidelines, a Wilcoxon signed-rank test was performed. All data were analyzed using SAS version 9.4 and SPSS Statistics version 23.0, with significance set at p < 0.05.
Results
Participant demographics
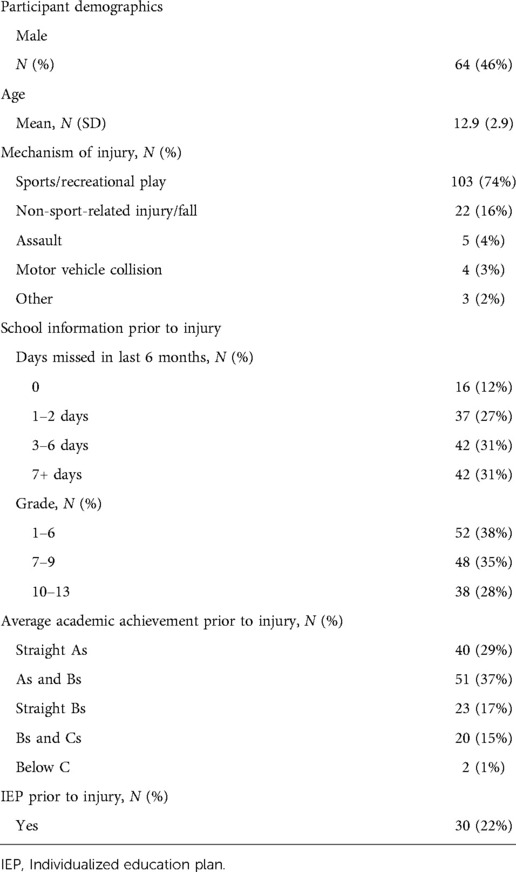
The study cohort included 64 boys (46%) and 75 girls (54%) with a median age of 13.4 years, with 74% having sport-related injuries (Table 2). The median time from injury to study enrolment was 7.8 days (mean: 34.8 days, minimum: 2.9 h, and maximum: 320.9 days). Most participants were either straight A or A/B students prior to their concussion (29% were A and 37% were A/B). Fifty-six percent of participants (N = 76) had symptoms persisting longer than 1 month. The median time to full return to school time was 35 days, and the median return time to full sports competition was 38 days (19). Of note, our cohort intentionally included a heterogeneous sample of youth. The possible time from injury was any time within 1 year, assuming participants were still symptomatic (30).
Participant recruitment
Some participants only had a First and Follow-Up Visit because their symptoms resolved in 28 days (N = 51). Participants who did not experience symptom resolution within the 6-month study period (N = 16) or achieved symptom resolution close to their scheduled Follow-Up Visit (N = 4) also only had a First and Follow-Up Visit. Participants who had symptoms for >28 days and experienced symptom resolution within the 6-month time period had an In-Person Symptom Resolution Visit (N = 44). Of the 100 participants who achieved symptom resolution within the study period (Figure 1), 44 completed the In-Person Symptom Resolution Visit and were provided the school information questionnaire. Twenty-six participants withdrew before symptom resolution could be determined.
Aim 1: youth-reported perceived school problems
Of the 137 participants who consented to the study, 51% (N = 70) completed the school information questionnaire due to the age requirement (between 9.5 and 18 years old) and the time of study enrolment (after July 2015). Of these 70 participants, 63% (N = 44) had returned to school by the First Visit Post-injury Visit. Of the 44 participants who had returned to school, 50% (N = 22) reported experiencing school problems (new problems or problems that worsened since injury). Of those experiencing school problems (N = 22), the most common school problems were headaches (82%, N = 18/22), inability to pay attention in class (77%, N = 17/22), and being overly tired (73%, N = 16/22). Note that participants could select multiple answers, so data were not mutually exclusive.
Of the 44 participants who had returned to school by the First Visit Post-injury, 16% (N = 7/44) reported that their grades were affected. Grades were affected by 1 letter (e.g., A to B) for three participants and by 2 (e.g., A to C) or more letters (e.g., A to D) for two participants (Table 3). Of the 44 participants who had returned to school at the First Visit Post-injury, 55% (N = 24/44) reported experiencing trouble with classes (Figure 1). The most common subjects in which participants experienced difficulty were Mathematics (63%, N = 15), English (50%, N = 12), and Science (N = 10, 42%), compared to Art (4%, N = 1) or Music (25%, N = 6). At the First Visit Post-injury, 14 participants reported experiencing problems in both the morning and afternoon.
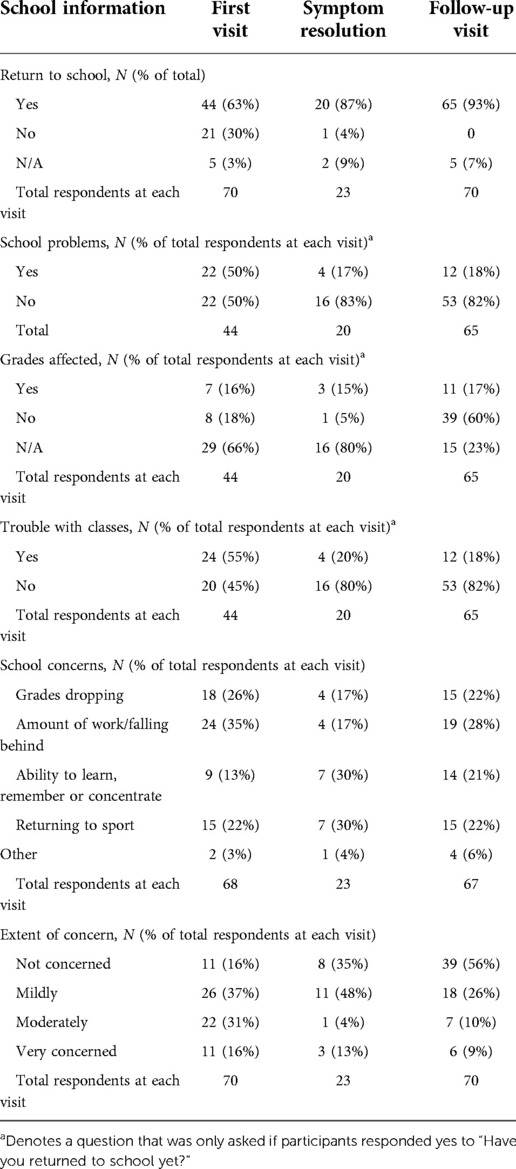
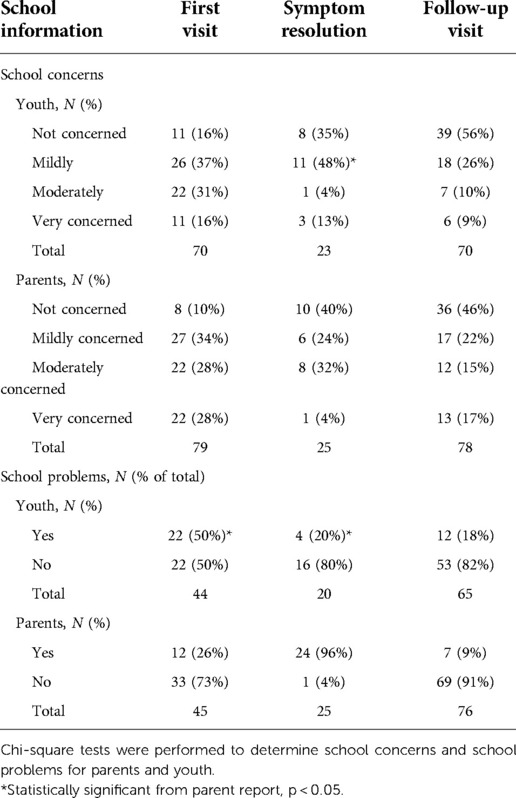
Table 3. School concerns and problems reported for youth with concussion at first visit, symptom resolution and follow-up visit.
Forty-four participants needed an In-Person Symptom Resolution Visit because they had persistent symptoms for >28 days (three visits in total) compared to the youth who recovered within 1 month post-injury (two visits). These participants also received a school information questionnaire, which 52% (N = 23/44) completed. Of the participants who completed the school information questionnaire (N = 23), 87% (N = 20/23) had returned to school. Of the 20 participants who had returned to school at the In-Person Symptom Resolution Visit, 20% (N = 4) reported experiencing school problems.
At the Follow-Up Visit, 70 participants completed the school information questionnaire, of which 93% (N = 65) had returned to school (Figure 1). Of the 65 participants who had returned to school at the Follow-Up Visit, 18% (N = 12) were experiencing school problems and 17% (N = 11) had their grades affected (Figure 1). Grades were most affected in English (36%, N = 4) and Science (36%, N = 4). Of the 65 participants who had returned to school at the Follow-Up Visit, 18% (N = 12) were experiencing trouble with classes (Table 3). The most common post-concussive difficulties for participants that led to difficulty with subjects were the inability to pay attention in class (75%), homework taking longer (75%), and difficulty understanding material (75%). At the Follow-Up Visit, of the 12 participants who reported school problems, 50% (N = 6) of participants reported experiencing class problems in both the morning and afternoon.
Aim 2: youth-reported school concerns (type of concern and degree of concern)
At the First Visit and Follow-Up Visit, participants (Figure 1) reported that their greatest school concerns were the amount of work/falling behind, grades dropping, and returning to sport (Table 3). At the First Visit and Follow-Up Visit, participants reported their concern on how their injury would affect their learning and performance (Figure 1). The extent of this concern at the First Visit Post-injury was “mild” for 37% of participants (N = 26/70) and “very concerned” for 16% of participants (N = 11/70, Table 3). At the Follow-Up Visit, the extent of this concern was “none” for 56% of participants (N = 39/70), “mild” for 26% of participants (N = 18/70), and “very concerned” for 9% of participants (N = 6/70, Table 3).
Parent-reported missed school
At each visit, parents were asked, How many school days has your child missed since his/her injury? At the First Visit, parents (N = 77) reported that their child missed 12.3 ± 16.6 days of school, whereas at the In-Person Symptom Resolution Visit, parents (N = 24) reported that their child missed 16.0 ± 17.7 days of school and at the Follow-Up Visit, parents (N = 74) reported that 16.2 ± 14.5 days of school were missed.
Secondary aims: cognitive scale score and PCSS at stage entry and exit
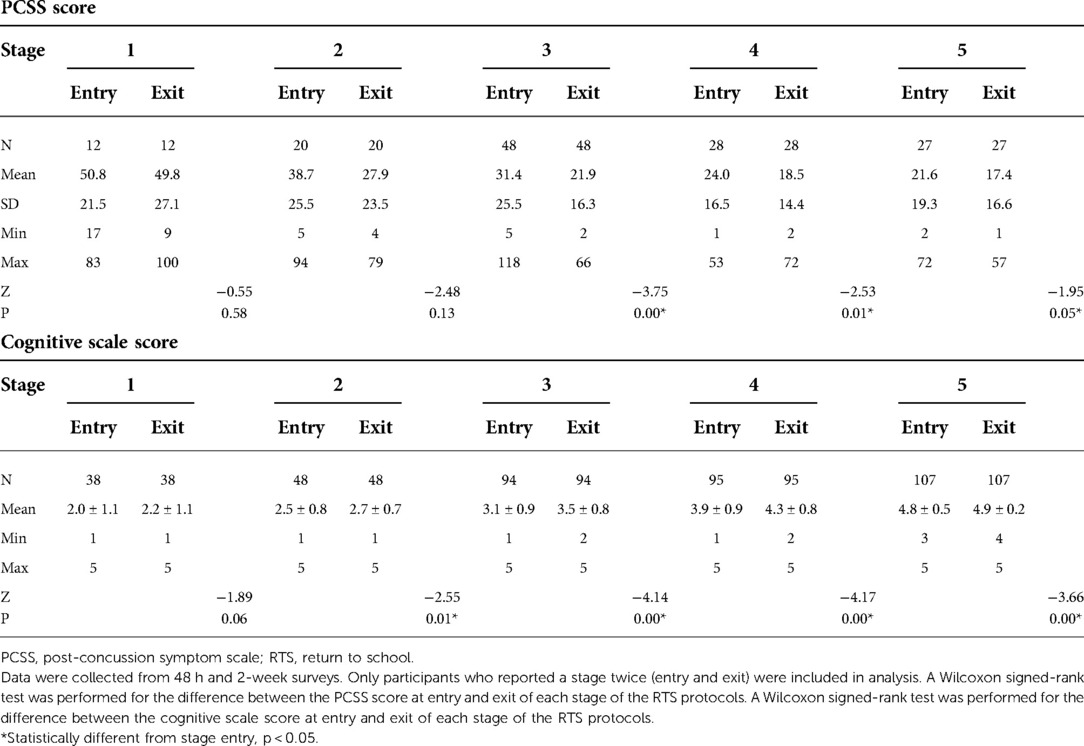
There was a significant difference (p < 0.05) in the cognitive activity scale score for RTS stage entry and exit for Stages 2, 3, 4, and 5 (Table 4). The cognitive activity score increased from 2.0 ± 1.1 at RTS Stage 1 to 4.9 ± 0.2 at RTS Stage 5, corresponding to a full return to cognitive activity [Figure 2(1)].
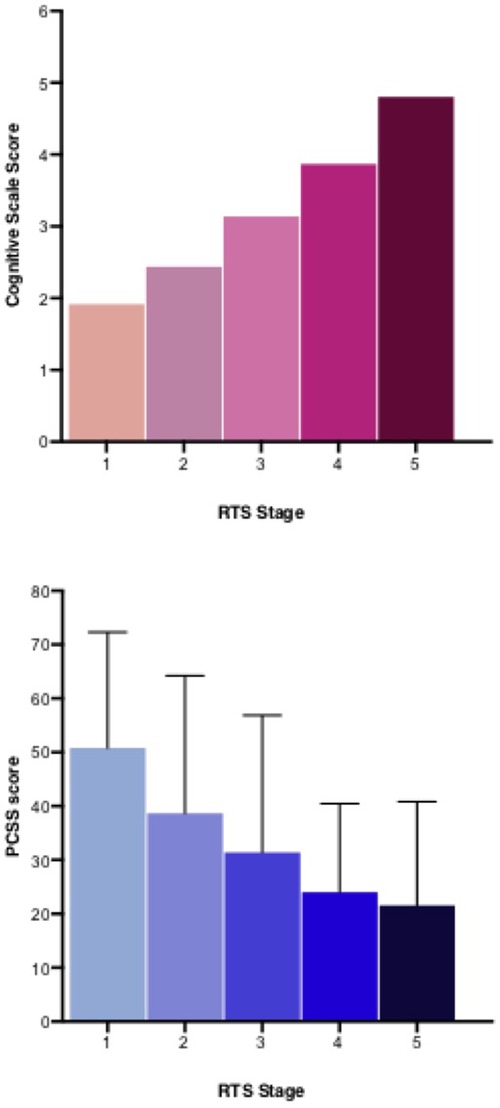
Figure 2. Post-concussion symptom scale (PCSS) and cognitive scale score at return to school stage entry.
The PCSS score decreased from 50.8 ± 21.5 at RTS Stage 1 to 17.4 ± 16.6 at RTS Stage 5 [Figure 2(2)]. There was a significant difference in the PCSS score at stage entry and exit for RTS Stage 3 (31.4 ± 25.5 to 21.9 ± 16.3 p = 0.01). Similarly, there was a significant difference in stage entry and exit at RTS Stage 4 (24.0 ± 16.5 to 18.5 ± 14.4) and Stage 5 (21.6 ± 19.3 to 17.4 ± 16.6) (Table 4).
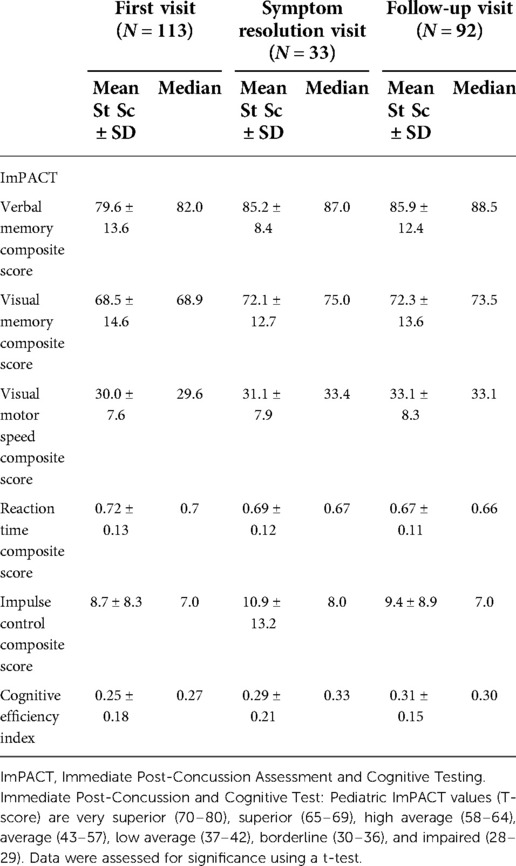
Secondary aims: ImPACT score at First Visit, Symptom Resolution, and Follow-Up Visit
The cognitive efficiency index, which is a subtest of the ImPACT and measures cognitive recovery following a concussion, increased from the First to Follow-Up Visit (0.25 ± 0.18 to 0.31 ± 0.15, p > 0.05, Table 5).
Secondary aims: parents vs. youth return to school and school problems
At the First Visit, there was a significant difference (p = 0.02) in the school problems reported by parents (N = 45) and youth (N = 44) (Figure 3A). Here, 50% (N = 22) of youth reported school problems, whereas only 26% of parents (N = 12) reported that their child had school problems (Table 4). At the In-Person Symptom Resolution Visit, there was also a significant difference (p = 0.01) in the school problems reported by parents and youth (Figure 3B). Here, four youth (20%) reported school problems, whereas 96% of parents (N = 24) reported that their child had school problems (Table 6). No significant difference was observed between parents and youth at the Follow-Up Visit.
Participants and their parents were also asked, How concerned are you about this injury affecting your/your child's school learning and performance? Participants and their parents reported similar concerns about school learning and performance at the First Visit Post-injury and Follow-Up Visit (Table 6). At the In-Person Symptom Resolution Visit, there was a significant difference (p = 0.04) in participants' and their parents' concern about the injury affecting their/their child's school learning and performance. Forty-eight percent of youth (N = 11/23) reported “mild concern” vs. 24% (N = 6/25) of parents (Table 6).
Discussion
The aim of the present analyses was to describe school problems, school concerns, and cognitive activity patterns in youth during recovery from a concussion. Youth and their parents were assessed over time for perceived school problems as they recovered from their concussions. At the First Visit Post-injury (7.7 days), 50% of youth reported experiencing school problems, whereas only 18% of youth reported school problems at the Follow-Up Visit (133 days). Other literature reports high rates of perceived school problems, such as Ransom et al. (31), who examined academic problems among 349 concussed youth. The authors observed that 77%–88% of youth reported school problems as a result of concussion symptoms and diminished academic skills (31). This was much more prevalent in youth still experiencing concussion symptoms than those who had recovered, a pattern also seen in our cohort. Youth in our study perceived school problems in Mathematics, Science, and English/Writing classes. Symptoms of not being able to pay attention in class, being overly tired, homework taking longer, and difficulty understanding material all contributed to troubles in these classes. This is also similar to other findings in the literature, with Mathematics, reading/language, and Science being the most problematic (32).
Perceived school problems decreased across all three visits, with most problems being identified early on at the First Visit, so this suggests that issues at school generally improve over time. A small percentage of youth experience more significant problems such as a decrease in grades, which does not seem to change over time. Seventeen percent of participants, who prior to their injury were mostly straight A or A/B students, experienced a decrease in grades at the Follow-Up Visit. These findings are similar to other groups (33), including a scoping review (34) that reported a significant decline in academic performance following a concussion.
It is interesting that there is often some disagreement between parents’ and children's perceptions of academic problems (35). We observed a significant difference at two time points (p < 0.05), with the First Visit Post-injury difference being 50% of youth and only 26% of parents perceiving school problems. A reversal of this pattern was seen at the Symptom Resolution Visit with 20% of youth and 96% of parents identifying school concerns. Parent and child reporting about the same phenomena are often divergent (35), with no established or predictable directional reason for these differences.
In terms of concussion symptoms, children often report higher symptom levels than parents (36–38). Poor agreement between children and parents has also been observed for sleep problems (38) and neurocognitive symptoms (39, 40). To the best of our knowledge, only one study has investigated whether the child and parent report of symptom agreement varies over time. Liu and Hicks (40) observed that parents tended to report lower symptom severity in the first 2 weeks post-concussion and higher severity after 4 weeks (40). These findings are similar to our observations regarding school problems in which parents perceived fewer school problems at the First Visit Post-injury than the youth and more school problems at the Symptom Resolution Visit than youth. This reinforces that both should be sampled to get the whole family's perspective of what they are experiencing.
As anticipated, the amount and complexity of cognitive activity measured on a numeric scale increased with progression through RTS stages as symptoms decreased. This suggests that cognitive activity was modified according to protocols and symptom profiles. We also observed an increase in performance scores in all subtests of the ImPACT (i.e., verbal memory, visual memory, visual motor, impulse control, and cognitive efficiency index score) from the First to Follow-Up Visit. Similarly, Tjarks et al. (41) also observed an increase in ImPACT composite scores for youth aged 12–19 years over time, suggesting participants were progressively recovering from concussions. These results, an increase in the amount and complexity of cognitive activity as symptoms decrease, would be expected when a child was adhering to the RTS guidelines.
Despite several strengths, including longitudinal assessments (6 months following recruitment) and measures of cognitive activity and function, this investigation is not without limitations. First, data on race and socioeconomic status were not collected. Second, some participants were recruited during summer vacation or holiday break when the school questionnaire was not applicable. With this, we were unable to obtain school information from all participants. Third, our cohort intentionally included a heterogeneous sample of youth with varying time from injury any time within 1 year, as long as participants were still symptomatic (30). This meant the sample included youth with concussions experiencing both acute and prolonged symptoms due to the nature of the research question. As such, it is possible that the large variation in time to symptom resolution is due to the prolonged symptoms of some participants. Finally, although we were able to retain most participants, some were lost to follow-up or never achieved symptom resolution within the study period. Finally, there was no official record of preinjury school performance; this information was provided by parent and youth self-reports.
Implications
Findings from this study may help guide youth recovering from a concussion and their parents as they return to school. We note the importance of returning to school cautiously and with accommodations to prevent a rise in symptoms that may be associated with an increase in cognitive activity. It is important that youth with a concussion and their parents monitor symptoms as they begin to increase their levels of cognitive activity to ensure that they are progressing through the stages at an appropriate rate. Also, given the significant difference between parent and youth reports of school problems, it is vital that parents and youth discuss these experiences with their healthcare providers to create a complete picture of the youth’s recovery. This finding is also important for future researchers, who should be encouraged to survey both parents and youth to capture all relevant information.
Conclusions
Youths perceive a number of problems and concerns after concussions that are perceived to improve over time. Note that these are new problems and concerns that pre-date the youths’ concussion. A small percentage of youth experience more significant academic problems evidenced by a decrease in grades that do not improve over 6 months. There is a significant difference in the perception of school problems reported by youth and their parents at different stages of recovery. The amount and complexity of cognitive activity increased with decreasing symptoms and increasing RTS stage.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Informed verbal and written assent and consent were obtained from participants and their parents. The study was approved by the Hamilton Integrated Research Ethics Board (#14-376).
Author contributions
CADM contributed to the study design, methodology, supervision, funding acquisition, data curation, formal analysis, and writing/reviewing the manuscript. JJ contributed to data curation, formal analysis, and writing/reviewing the manuscript. SR contributed to methodology, supervision, data curation, formal analysis, and reviewing the manuscript. KS contributed to data curation, formal analysis, and reviewing the manuscript. C-YL contributed to methodology, data curation, and writing the manuscript. RY authorship contribution data curation, formal analysis, and reviewing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This project was supported by the Canadian Institutes of Health Research (CIHR) (Grant number 31257 to CADM).
Acknowledgments
The authors thank the participating families in this study for their effort and commitment and all of the Back to Play team members for their hard work and support throughout all stages of this project. The authors also thank CHIR for funding and the McMaster Children's Hospital Emergency Department staff and physicians for recruitment support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
RTA, return to activity; RTS, return to school; PCSS, post-concussion symptom scale.
References
1. Canadian Institute for Health Information (CIHI). Head’s up on sports related brain injuries (2018). Retrieved from: https://secure.cihi.ca/estore/productFamily.htm?pf=PFC3763&lang=en&media=0
2. Langer L, Levy C, Bayley M. Increasing incidence of concussion: true epidemic or better recognition? J Head Trauma Rehabil. (2019) 35:E60–6. doi: 10.1097/HTR.0000000000000503
3. Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. (2017) 51(12):941–8. doi: 10.1136/bjsports-2017-097729
4. Wilmoth K, Tan A, Hague C, Tarkenton T, Silver CH, Didehbani N, et al. Current state of the literature on psychological and social sequelae of sports-related concussion in school-aged children and adolescents. J Exp Neurosci. (2019) 13:117906951983042. doi: 10.1177/1179069519830421
5. Taylor GH, Orchinik LJ, Minich N, Dietrich A, Nuss K, Wright M, et al. Symptoms of persistent behavior problems in children with mild traumatic brain injury. Physiol Behav. (2016) 176(12):139–48. doi: 10.1097/HTR.0000000000000106
6. Russell K, Selci E, Black B, Cochrane K, Ellis M. Academic outcomes following adolescent sport-related concussion or fracture injury: a prospective cohort study. PLoS One. (2019) 14:e0215900. doi: 10.1371/journal.pone.0215900
7. Hodges A, Ameringer S. The symptom experience of adolescents with concussion. J Spec Pediatr Nurs. (2019) 24(4):e12271. doi: 10.1111/jspn.12271
8. Stazyk K, DeMatteo C, Moll S, Missiuna C. Depression in youth recovering from concussion: correlates and predictors. Brain Inj. (2017) 31(5):631–8. doi: 10.1080/02699052.2017.1283533
9. Yeates KO, Kaizar E, Rusin J, Bangert B, Dietrich A, Nuss K, et al. Reliable change in postconcussive symptoms and its functional consequences among children with mild traumatic brain injury. Arch Pediatr Adolesc Med. (2012) 166(7):615–22. doi: 10.1001/archpediatrics.2011.1082
10. Novak Z, Aglipay M, Barrowman N, Yeates KO, Beauchamp MH, Gravel J, et al. Association of persistent postconcussion symptoms with pediatric quality of life. JAMA Pediatr. (2016) 170:e162900. doi: 10.1001/jamapediatrics.2016.2900
11. Davis GA, Anderson V, Babl FE, Gioia GA, Giza CC, Meehan W, et al. What is the difference in concussion management in children as compared with adults? A systematic review. Br J Sports Med. (2017) 51(12):949–57. doi: 10.1136/bjsports-2016-097415
12. Zemek R, Barrowman N, Freedman SB, Gravel J, Gagnon I, McGahern C, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. (2016) 315(10):1014–25. doi: 10.1001/jama.2016.1203
13. DeMatteo C, Stazyk K, Singh SK, Giglia L, Hollenberg R, Malcolmson CH, et al. Development of a conservative protocol to return children and youth to activity following concussive injury. Clin Pediatr (Phila). (2015) 54(2):152–63. doi: 10.1177/0009922814558256
14. DeMatteo C, Stazyk K, Giglia L, Mahoney W, Singh SK, Hollenberg R, et al. A balanced protocol for return to school for children and youth following concussive injury. Clin Pediatr (Phila). (2015) 54(8):783–92. doi: 10.1177/0009922814567305
15. DeMatteo C, Randall S, Falla K, Lin CY, Giglia L, Mazurek MF, et al. Concussion management for children has changed: new pediatric protocols using the latest evidence. Clin Pediatr (Phila). (2020) 59(1):5–20. doi: 10.1177/0009922819879457
16. McCrory P, Meeuwisse W, Dvořák J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. (2017) 51(11):838–47. doi: 10.1136/bjsports-2017-097699
17. McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorák J, Echemendia RJ, et al. Consensus statement on concussion in sport—the 4th international conference on concussion in sport held in Zurich, November 2012. PM R. (2013) 5(4):255–79. doi: 10.1016/j.ptsp.2013.03.002
18. Taylor HG, Dietrich A, Nuss K, Wright M, Rusin J, Bangert B, et al. Post-concussive symptoms in children with mild traumatic brain injury. Neuropsychology. (2010) 24(2):148–59. doi: 10.1037/a0018112
19. DeMatteo CA, Randall S, Lin CYA, Claridge EA. What comes first: return to school or return to activity for youth after concussion? Maybe we don’t have to choose. Front Neurol. (2019) 10:1–21. doi: 10.3389/fneur.2019.00792
20. Baker JG, Leddy JJ, Darling SR, Rieger BP, Mashtare TL, Sharma T, et al. Factors associated with problems for adolescents returning to the classroom after sport-related concussion. Clin Pediatr (Phila). (2015) 54(10):961–8. doi: 10.1177/0009922815588820
21. Stein CJ, MacDougall R, Quatman-Yates CC, Myer GD, Sugimoto D, Dennison RJ, Meehan WP Young athletes’ concerns about sport-related concussion: the patient’s perspective. Clin J Sport Med. (2016) 26(5):386–90. doi: 10.1097/JSM.0000000000000268
22. Ellis MJ, Ritchie LJ, Koltek M, Hosain S, Cordingley D, Chu S, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. (2015) 16(6):709–18. doi: 10.3171/2015.5.PEDS15220
23. Brown NJ, Mannix RC, O’Brien MJ, Gostine D, Collins MW, Meehan WP. Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics. (2014) 133(2):e299–304. doi: 10.1542/peds.2013-2125
24. Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. (1998) 13(2):9–26. doi: 10.1097/00001199-199804000-00004
25. Berger I, Obeid J, Timmons BW, DeMatteo C. Exploring accelerometer versus self-report sleep assessment in youth with concussion. Glob Pediatr Heal. (2017) 4:2333794X1774597. doi: 10.1177/2333794x17745973
26. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
27. Ruiter KI, Boshra R, Dematteo C, Noseworthy M, John F. Neurophysiological markers of cognitive deficits and recovery in concussed adolescents. Brain Res. (2020) 1746:146998. doi: 10.1016/j.brainres.2020.146998
28. Boshra R, Ruiter KI, DeMatteo C, Reilly JP, Connolly JF. Neurophysiological correlates of concussion: deep learning for clinical assessment. Sci Rep. (2019) 9(1):1–10. doi: 10.1038/s41598-019-53751-9
29. Dona O, Noseworthy MD, DeMatteo C, Connolly JF. Fractal analysis of brain blood oxygenation level dependent (BOLD) signals from children with mild traumatic brain injury (mTBI). PLoS One. (2017) 12(1):e0169647. doi: 10.1371/journal.pone.0169647
30. DeMatteo CA, Randall S, Lin CYA, Claridge EA. What comes first: return to school or return to activity for youth after concussion? Maybe we don’t have to choose. Front Neurol. (2019) 10:792. doi: 10.3389/fneur.2019.00792
31. Ransom DM, Vaughan CG, Pratson L, Sady MD, McGill CA, Gioia GA. Academic effects of concussion in children and adolescents. Pediatrics. (2015) 135(6):1043–50. doi: 10.1542/peds.2014-3434
32. Howell DR, Fazekas M, Grady M, Halstead M, Master C, McLeod T, et al. Quality-of-life outcomes and academic concerns following pediatric concussion: initial findings from the prism concussion rig. Orthop J Sport Med. (2020) 8(4_suppl3):2325967120S0014. doi: 10.1177/2325967120s00146
33. Lowry R, Haarbauer-Krupa JK, Breiding MJ, Thigpen S, Rasberry CN, Lee SM. Concussion and academic impairment among U.S. high school students. Am J Prev Med. (2019) 57(6):733–40. doi: 10.1016/j.amepre.2019.08.016
34. Neelakantan M, Ryali B, Cabral MD, Harris A, McCarroll J, Patel DR. Academic performance following sport-related concussions in children and adolescents: a scoping review. Int J Environ Res Public Health. (2020) 17(20):1–12. doi: 10.3390/ijerph17207602
35. DeMatteo CA, Lin CA, Foster G, Giglia L, Thabane L, Claridge E, et al. Evaluating adherence to return to school and activity protocols in children after concussion. Clin J Sport Med. (2019) 31:e406–13. doi: 10.1097/jsm.0000000000000800
36. Hajek CA, Yeates KO, Taylor HG, Bangert B, Dietrich A, Nuss KE, et al. Agreement between parents and children on ratings of post-concussive symptoms following mild traumatic brain injury. Child Neuropsychol. (2011) 17(1):17–33. doi: 10.1080/09297049.2010.495058
37. Rowhani-Rahbar A, Chrisman SPD, Drescher S, Schiff MA, Rivara FP. Agreement between high school athletes and their parents on reporting athletic events and concussion symptoms. J Neurotrauma. (2016) 33(8):784–91. doi: 10.1089/neu.2015.4100
38. Porter S, Smith-Forrester J, Alhajri N, Kusch C, Sun J, Barrable B, et al. The child sport concussion assessment tool (child SCAT3): normative values and correspondence between child and parent symptom scores in male child athletes. BMJ Open Sport Exerc Med. (2015) 1(1):1–6. doi: 10.1136/bmjsem-2015-000029
39. Jones KM, Starkey NJ, Theadom A, Gheorghe A, Willix-Payne D, Prah P, et al. Parent and child ratings of child behaviour following mild traumatic brain injury. Brain Inj. (2018) 32(11):1397–404. doi: 10.1080/02699052.2018.1496477
40. Liu R, Hicks SD. Discrepancies in child and parent reporting of concussion symptoms. Brain Inj. (2021) 35(6):675–81. doi: 10.1080/02699052.2021.1894483
Keywords: return to school, pediatric concussion, return to activity, brain injury, school performance, children and youth
Citation: DeMatteo CA, Jakubowski J, Randall S, Stazyk K, Lin C and Yakubov R (2022) School performance in youth after a concussion. Front. Sports Act. Living 4:1008551. doi: 10.3389/fspor.2022.1008551
Received: 31 July 2022; Accepted: 16 November 2022;
Published: 22 December 2022.
Edited by:
Elizabeth Teel, Concordia University, CanadaReviewed by:
Nicola Jayne Starkey, University of Waikato, New ZealandVipul Lugade, Binghamton University, United States
© 2022 DeMatteo, Jakubowski, Randall, Stazyk, Lin and Yakubov. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carol A. DeMatteo ZGVtYXR0ZW9AbWNtYXN0ZXIuY2E=
Specialty Section: This article was submitted to Injury Prevention and Rehabilitation, a section of the journal Frontiers in Sports and Active Living
 Carol A. DeMatteo
Carol A. DeMatteo Josephine Jakubowski
Josephine Jakubowski Sarah Randall
Sarah Randall Kathy Stazyk1
Kathy Stazyk1 Chia-Yu Lin
Chia-Yu Lin Rebecca Yakubov
Rebecca Yakubov