- 1Department of Psychiatry, College of Medicine, University of Florida, Gainesville, FL, United States
- 2Department of Clinical and Health Psychology, College of Public Health and Health Professions, University of Florida, Gainesville, FL, United States
- 3UF Center for OCD, Anxiety, and Related Disorders, University of Florida, Gainesville, FL, United States
- 4Evelyn F. and William L. McKnight Brain Institute, University of Florida, Gainesville, FL, United States
- 5Department of Psychiatry, College of Medicine-Jacksonville, University of Florida, Jacksonville, FL, United States
- 6Department of Emergency Medicine, College of Medicine, University of Florida, Gainesville, FL, United States
Past research has shown that healthcare workers (HCWs) experience high levels of psychological distress during epidemics and pandemics, resulting in cascading effects that have led to chronically understaffed hospitals and healthcare centers. Due to the nature of their responsibilities and workplace stress, HCWs are among vulnerable groups especially during global health crises. During COVID-19 many healthcare workers reported greater symptoms of anxiety, depression, and COVID-19 related worries. Furthermore, adverse childhood experiences increase vulnerability for psychological conditions, especially during pandemics. This study sets out to (1) investigate the moderating effects of adverse childhood experiences on healthcare workers’ COVID-19 related stressors and depression/anxiety symptoms, and (2) investigate the moderating effects of adverse childhood experiences on proximity to the COVID-19 virus and depression/anxiety symptoms. Participants included 438 employed HCWs recruited from academic medical centers and smaller healthcare agencies in northcentral Florida between October to December 2020. Mean age of participants was 38.23 (SD = 11.5) with most of the HCWs being white (72.1%), non-Hispanic (86.8%) and female (82%). Healthcare workers completed several online questionnaires, including the Adverse Childhood Experiences scale, Patient Health Questionnaire, Generalized Anxiety Disorder Scale, a COVID-19 specific worries scale, and a Social Proximity to COVID-19 scale. Healthcare workers experiencing specific COVID-19 worries reported experiencing anxiety and depressive symptoms. A significant positive interaction was seen between childhood adverse experiences globally and COVID-19 worries on anxiety symptoms. A significant positive interaction was observed between childhood maltreatment specifically and COVID-19 worries on depressive symptoms. Additionally, a positive interaction effect was seen between childhood adverse experiences and COVID-19 social proximity for both depression symptoms and anxiety symptoms. Findings from the present study indicate that adverse childhood experiences strengthen the relationship between COVID-19 worry/proximity and negative psychological symptoms. Vulnerable populations such as individuals who have experienced ACEs could benefit from targeted and specific interventions to cope with the collective trauma experienced globally due to COVID-19. As COVID-19 becomes endemic, hospital leadership and authorities should continue addressing COVID-19 worries and HCWs’ psychological symptoms through mental health support and organizational interventions.
1. Introduction
The onset of the COVID-19 pandemic caused many individuals to experience specific COVID-19 related worries, such as infecting family members with COVID-19, or becoming seriously ill from COVID-19 (Hidaka et al., 2021). These worries were related to greater anxiety and depressive symptoms more generally (Gupta et al., 2021). The healthcare workforce was particularly at risk for developing COVID-19 related worries as well as mental health symptoms, resulting in cascading effects that have led to chronically understaffed hospitals and healthcare centers (Gupta et al., 2021; Søvold et al., 2021). Understanding the risk factors that make individuals more vulnerable to pandemic related worries and associated mental health symptoms is an important public health concern. Prior to the pandemic, adverse childhood experiences were shown to predict mental health disorders in adulthood (McKay et al., 2022; Tzouvara et al., 2023). However, little is known about the interaction effect between adverse childhood experiences and COVID-19 specific worries on healthcare workers’ (HCWs) psychological symptoms. Similarly, the interaction effect between adverse childhood experiences and COVID-19 social proximity on HCWs’ psychological symptoms has also not been explored. COVID-19 social proximity refers to the impact COVID-19 has had on an individual’s social circle.
In the general population, the COVID-19 pandemic has negatively impacted individuals’ mental well-being and coincided with increased levels of anxiety, depression, and posttraumatic stress symptoms (Prout et al., 2020; Marvaldi et al., 2021). Recent research has shown that these adverse mental health outcomes have been exacerbated in HCWs, potentially due to their proximity to COVID-19 patients, COVID-19 quarantine rules and those rules changing, and work environment (Labrague and Santos, 2020; Dobson et al., 2021; Tiete et al., 2021). Similar trends have been seen in non-clinical staff who work in healthcare settings, such as custodians and technicians (Dobson et al., 2021; Jang et al., 2021). A meta-analysis identified 38 studies that reported an increase in mental health symptoms among doctors, nurses, and allied health workers since the start of the pandemic (Saragih et al., 2021), with a pooled prevalence among these HCWs for anxiety of 40, and 37% for depression.
Psychological symptoms have been seen in the United States in both general and healthcare populations (Amsalem et al., 2021; Guastello et al., 2022). Additionally, studies have shown that nurses in particular are at higher vulnerability for psychological distress during infectious disease outbreaks (Greenberg et al., 2020; Magalhaes et al., 2021). A five-month longitudinal study of HCWs in the United States in the early stages of the COVID-19 pandemic found that anxiety and depression symptoms were related to decreased fulfilment and elevated burnout (Guastello et al., 2022).
The burden of the COVID-19 pandemic has had major impacts on HCWs and the healthcare system. This burden has impacted the physical and mental health of individuals who work in healthcare (Luo et al., 2020). At the onset of COVID-19 certain worries were prevalent such as worrying about the health of family and friends, due to the possibility of bringing the virus home, as well as an individual’s own health (Hidaka et al., 2021). These COVID-19 specific worries can in turn increase other anxiety and depressive symptoms. For example, higher perceived risk has been shown to predict higher depressive symptoms (Kim et al., 2022). In particular, this is seen in HCWs due to their proximity to the illness and the uncertainty involved with medical care and precautions needed. Additionally, pandemics elicit anticipatory anxiety for both real and perceived threats which can create high stress environments in hospitals and burnout in HCWs (Denning et al., 2021). Similarly, Carmassi and colleagues found that HCWs were at a higher risk for PTSD during pandemics due to infection rates, high mortality, and the constant change of guidelines experienced during COVID-19 (Carmassi et al., 2020).
In HCWs, anxiety is commonly seen during pandemics due to the uncertainty and anticipation that comes from an unknown disease (Labrague and Santos, 2020). COVID-19 specific worries in this population can be due to fear of being infected, fear of unknowingly infecting others, lack of personal protective equipment, and lack of access to testing (Mo et al., 2020; Shanafelt et al., 2020).
Kim and colleagues found that higher perceived COVID-19 risk predicted greater depression symptoms among the general population in South Africa (Kim et al., 2022). A U.S. sample of young adults ages 18 to 25 indicated that this population reported up to a 55% increase in COVID-19 related stressors (Ballou et al., 2020). Importantly, past research has shown that among young adults COVID-19 related worry is related to negative mental health outcomes (Rogers et al., 2020; Mayorga et al., 2022). Research has also shown that proximity to an individual with the SARS-COV2 virus that causes COVID-19 can also have a psychological impact on the people around them (Su et al., 2020). Several studies have reported on the connection between social proximity to COVID-19 cases and increased anxiety and depression (Su et al., 2020; Wang et al., 2020; Shabahang et al., 2021; Vigo et al., 2021).
Another factor that can have a negative impact on mental health outcomes is adverse childhood experiences (ACEs). ACEs are identified as experiences that can negatively harm a child (0–17 years old). These experiences can be in the form of childhood maltreatment (emotional, physical, and sexual abuse), neglect (emotional and physical), familial challenges and dysfunction (caregiver separation, poor or impaired caregiver mental health, and caregiver drug abuse) (Felitti et al., 1998; LeMoult et al., 2020). It is estimated that 61% of US adults have experienced at least one ACE, and approximately 16% have experienced four or more categories (Merrick et al., 2019). These experiences are associated with an increase in psychiatric disorders (such as depression and anxiety) in adolescence and adulthood (Felitti et al., 1998; Cicchetti and Toth, 2005; Cicchetti, 2016; Iob et al., 2022). For example, a study of 1,142 participants aged 22–24 in the Chicago Longitudinal Study found that ACEs scores were related to increased depressive symptoms in early adulthood (Mersky et al., 2013). These relationships have also been examined by some research teams during the pandemic. A cross-sectional survey of 1,399 German adults found that ACEs were a significant risk factor for an increase in depression during the first wave of the pandemic (Clemens et al., 2022). ACEs put individuals at a higher vulnerability for psychological conditions, and several studies have examined the relationship between ACEs and negative mental health symptoms during the pandemic (Castellini et al., 2022; Kim et al., 2022; Békés et al., 2023). However, this specific relationship has not been extensively examined with HCWs’ to the others knowledge at the time of the study.
HCWs’ mental health symptoms during pandemic times is well-documented (Labrague and Santos, 2020; Amsalem et al., 2021; Saragih et al., 2021; Guastello et al., 2022). However, less is known about the way past adverse childhood experiences can impact their worries about the pandemic and/or their own proximity to COVID-19 and their mental health and well-being. The current study aims to examine the relationships between these variables in HCWs during an early stage of the COVID-19 pandemic (from October to December 2020). The aims of this study were:
Aim 1: To examine the role that adverse childhood experiences plays in the relationship between COVID-19 specific worries and negative psychological symptoms.
Hypothesis 1.1: We hypothesized an interaction between COVID-19 specific worries and adverse childhood experiences, such that the association between HCWs COVID-19 specific worries and depression/anxiety would be stronger in participants who had more adverse childhood experiences.
Aim 2: To examine the role that adverse childhood experiences plays in the relationship between proximity to COVID-19 and negative psychological symptoms.
Hypothesis 2.1: We hypothesized an interaction between proximity to COVID-19 cases and adverse childhood experiences, such that the association between HCWs proximity to COVID-19 cases and depression/anxiety would be stronger in participants who had more adverse childhood experiences.
2. Methods
2.1. Procedures
All procedures in this study were approved by the University of Florida’s Institutional Review Board. Participants were largely recruited from two academic medical centers in north central Florida. Announcements were posted throughout clinics, hospitals, and nursing homes in Florida via brochures emailed to relevant departments or clinical services from an administrator. Also, flyers were given to smaller medical groups and private practices in two cities near the academic medical centers. Additionally, the study was incorporated into the comprehensive Healthcare Worker Exposure Responses & Outcomes (HERO) registry of studies (heroesrearch.org). In order to maintain anonymity, the exact location of a participant’s workplace was not included in their responses. Using a QR code or link provided on the brochure, participants were directed to Research Electronic Data Capture (REDCap), a secure survey service, where their responses to the survey questions were recorded. This study is part of a larger dataset which had a 5-month longitudinal data collection (Guastello et al., 2022.) Recruitment was on a rolling basis between October and December 2020. The present study focused on solely baseline findings. Lastly, participants were reimbursed with $10 Amazon gift cards for completing the baseline surveys.
2.2. Participants
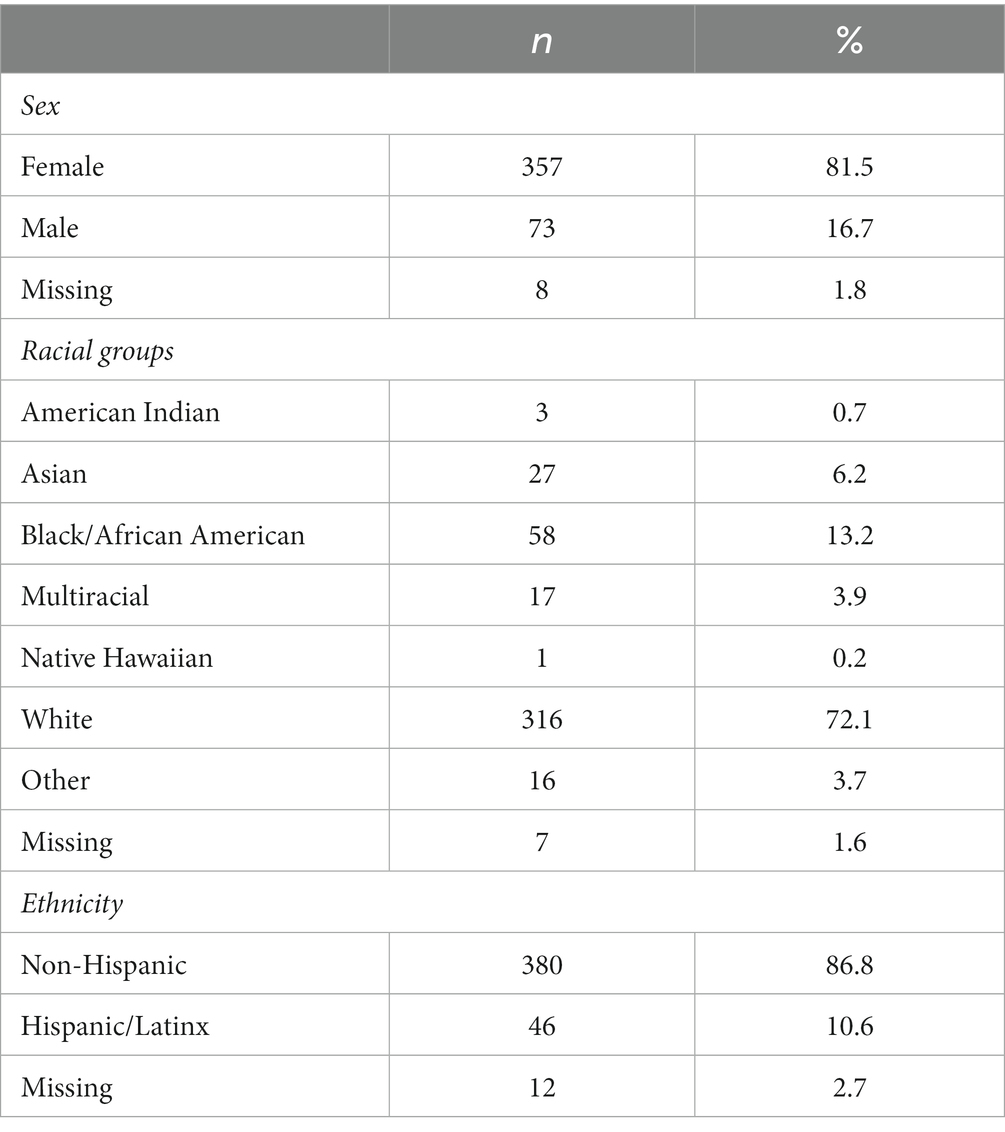
Participants included 438 employed HCWs recruited from academic medical centers and smaller healthcare agencies in north central Florida. Specific workplace location was not collected to protect the participants anonymity, however based on the collection of the zip code data, the majority of the participants resided in Florida (95.3%). Mean age of participants was 38.23 (SD = 11.5) with most of the HCWs being white (72.1%), non-Hispanic (86.8%) and female (82%). See Table 1 for a summary of the sample characteristics.
2.3. Measures
2.3.1. Adverse childhood experiences
The Adverse and Traumatic Experiences Scale (Dale et al., 2020, 2022; Kolacz et al., 2020) was administered to assess adverse childhood experiences (ACEs). This is a 30-question instrument that asks about adversity and traumatic experiences, and covers both childhood and adulthood. This measure is comprised of items from: ACES (Felitti et al., 1998), Trauma History Questionnaire (Hooper et al., 2011), Life Events Checklist for DSM-5 (Weathers et al., 2013), and Brief Trauma Questionnaire (Schnurr et al., 1999). The participants specify the occurrence and impact of each event via a 5-point Likert scale (0 = event did not occur, 1 = occurred and had no impact on my life, 2 = minimal impact on my life, 3 = some impact on my life, and 4 = big impact on my life). The items are grouped to form the following scales: Childhood Adverse Experiences, Childhood Maltreatment, Intimate Partner Maltreatment, Other Person Maltreatment, Life-threatening Situations, Sudden Losses, and Personal Health Situations. For the purpose of examining ACEs, the subscales Childhood Adverse Experiences and Childhood Maltreatment were used in this study. The subscale Childhood Adverse Experiences captures caregiver unavailability, caregiver separation, caregiver drug abuse, caregiver medical or mental illness, caregiver experience of emotional/physical/sexual abuse. The subscale Childhood Maltreatment captures emotional abuse, physical assault, sexual abuse of the participant by the caregiver. In our sample, the internal consistency for Childhood Adverse Experiences was 0.72, and for Childhood Maltreatment it was 0.69.
2.3.2. Depression
The Patient Health Questionnaire (PHQ-8; Kroenke et al., 2001) was administered to assess depression symptoms. On the PHQ-8 the participant is asked to rate over the last two weeks how frequently they have experienced the following symptoms of depression: low mood, anhedonia, hyper/hyposomnia, increased/decreased appetite, difficulty concentrating, self-blame, psychomotor retardation/agitation. Responses are recorded on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The total score of the eight items of the PHQ-8 ranges from 0 to 24, with a cut point of 10 indicating clinically significant symptoms of depression (Kroenke et al., 2009). In our sample, the internal consistency of the PHQ-8 was 0.89.
2.3.3. Anxiety
The Generalized Anxiety Disorder Scale (GAD-7; Spitzer et al., 2006) was administered to assess anxiety symptoms. On the GAD-7 the participant is asked to rate how frequently over the last two weeks they have experienced the following symptoms of anxiety: feeling nervous, anxious or on edge; difficulty controlling worry; psychomotor agitation; trouble relaxing; general worries; fear that something terrible will happen; and irritability. Responses are recorded on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The total score of the 7 items of the GAD-7 ranges from 0 to 21, with scores exceeding 10 representing clinically significant anxiety. In our sample, the internal consistency of the GAD-7 was 0.93.
2.3.4. COVID-19 specific worries
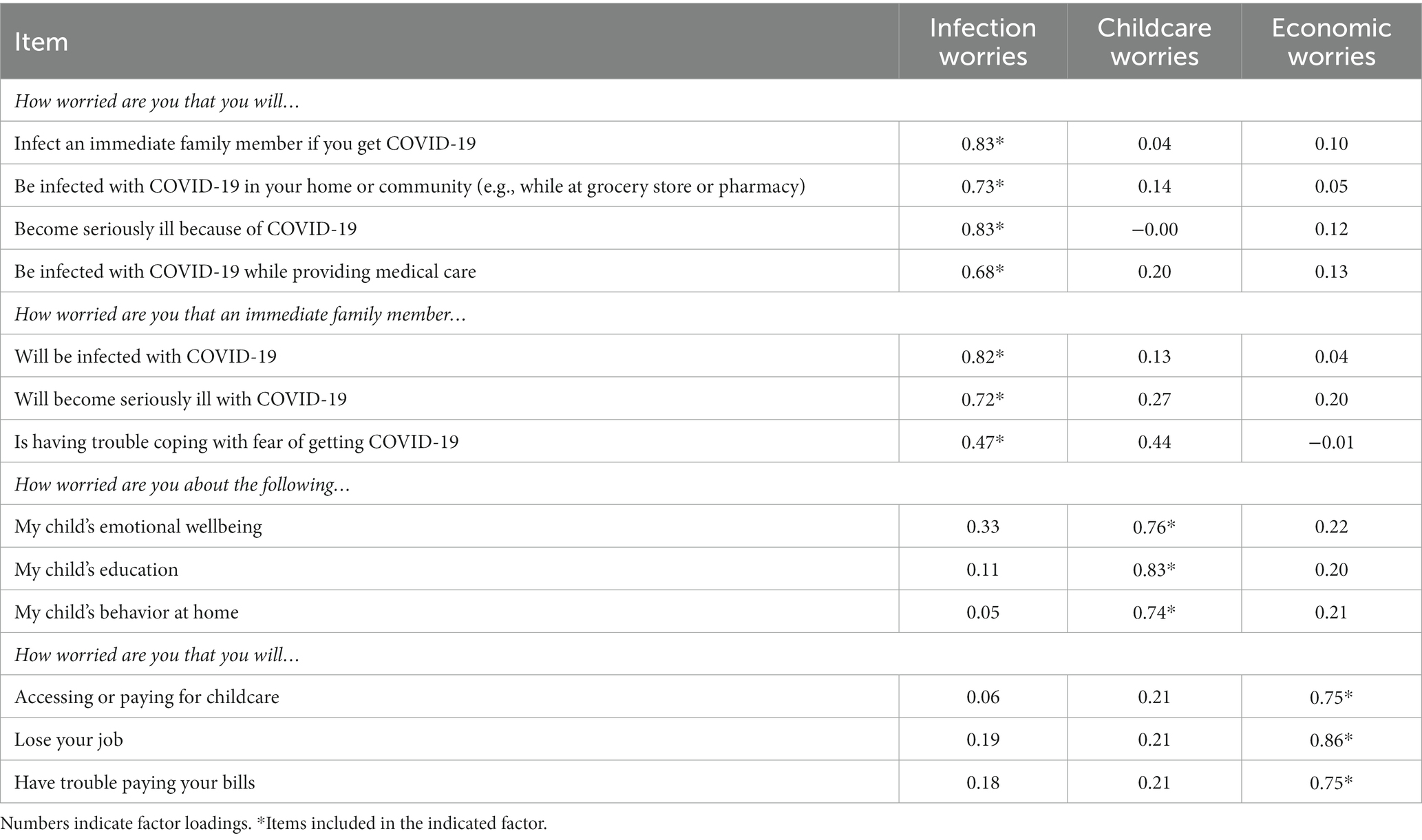
A COVID-19 specific worries and experiences questionnaire was created by the research team which consisted of various HCWs including psychiatrists, psychologists, and emergency medicine physicians. The scale consisted of 13 items, rated on a 0 to 3 scale with the following descriptors: 0 (Not worried), 1 (A little worried), 2 (Somewhat worried), and 3 (Very worried). The principal components analysis produced 3 terms accounting for 68.12% of the variance. The items and their accompanying factor loadings are presented in Table 2, and the derivation of the subscales can be found in the paper (Guastello et al., 2022). The first component, termed Infection Worries, was comprised of seven items regarding worry about self and family members being infected and/or becoming seriously ill from COVID-19; the internal consistency of this factor was 0.89. The second component, termed Childcare Worries, was comprised of three items related to worries about emotional wellbeing, education, and behavior; the internal consistency of this factor was 0.77. Lastly, the third component, termed Economic Worry, was comprised of three items regarding financial concerns such as accessing or paying for childcare, loss of job, and having trouble paying bills; the internal consistency of this factor was 0.86. See Table 2 for full factor analysis. The Infection Worry factor, also referred to as the COVID-19 Worries subscale, was utilized in this study.
2.3.5. Social proximity to COVID-19
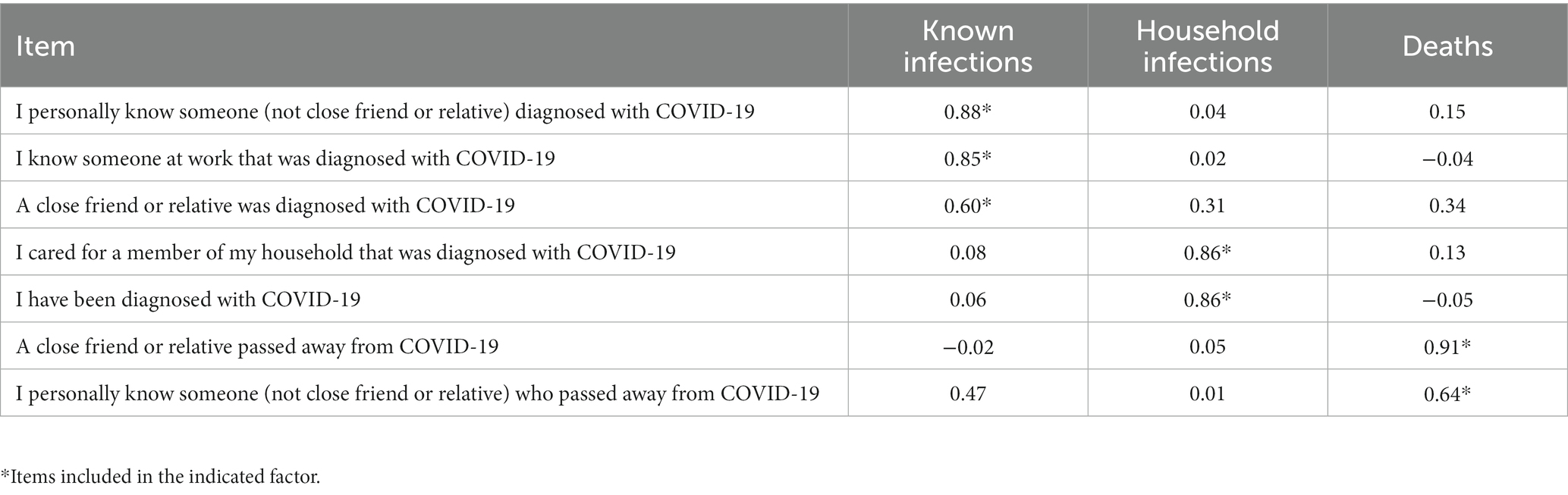
A Social Proximity to COVID-19 scale was created by the research team to measure the degree to which COVID-19 was impacting an individual’s social circle (Table 3). The scale originally consisted of 8 items, though one item (i.e., a member of my household passed away from COVID-19) was removed due to low endorsement. Each item was rated on a 0 to 4 scale with the following descriptors: 0 (Did not occur), 1 (Occurred, and no impact on my life), 2 (Minimal impact on my life), 3 (Some impact on my life), 4 (Big impact on my life). A principal components analysis for the remaining 7 items was conducted using varimax rotation. Items were considered to load on a factor if they had a factor loading of ≥0.50. Items that loaded onto more than one factor were included in all factors. The principal components analysis produced 3 factors that accounted for 72.65% of the variance. The factor loadings are presented in Table 3. The first component, termed Known Infections, contained three items regarding the social proximity to COVID-19 infections; internal consistency was 0.74. The second component, termed Household Infections, contained two items regarding members of the participant’s household and they themselves being infected; internal consistency was 0.69. The third component, termed, Deaths, contained two items regarding social proximity to COVID-19 related deaths; internal consistency 0.53. See Table 3 for full factor analysis.
2.4. Overview of statistical analyses
All analyses were conducted in SPSS Statistics Version 26 [IBM Corp (SPSS Inc.), 2019], using data collected at baseline. Descriptive statistics were first used to assess the distributions, normality, missing data, and any outliers among variables. Out of 438 participants, only 177 had children and answered for the variable Childcare Worries. Therefore, this subscale was dropped due to the significant loss in sample size. Additionally, the subscale Economic worries was not used due to high cross-loading with Childcare Worries subscale. For Aims 1 and 2, four separate hierarchical linear regressions were conducted in order to examine the models with COVID-19 worries, COVID-19 social proximity, childhood adverse experiences and childhood maltreatment as predictors, and depression and anxiety as outcome variables. An interaction variable was computed for the variables of interest and added to the second block of the regression.
3. Results
3.1. Descriptive statistics and preliminary findings
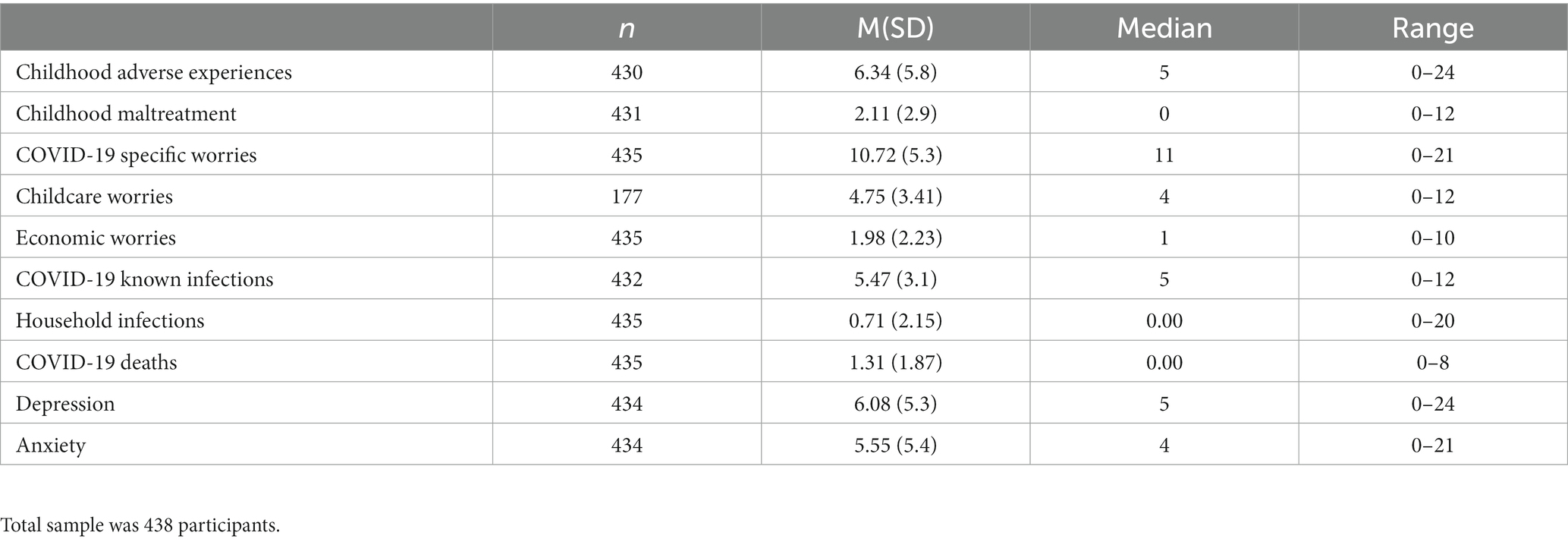
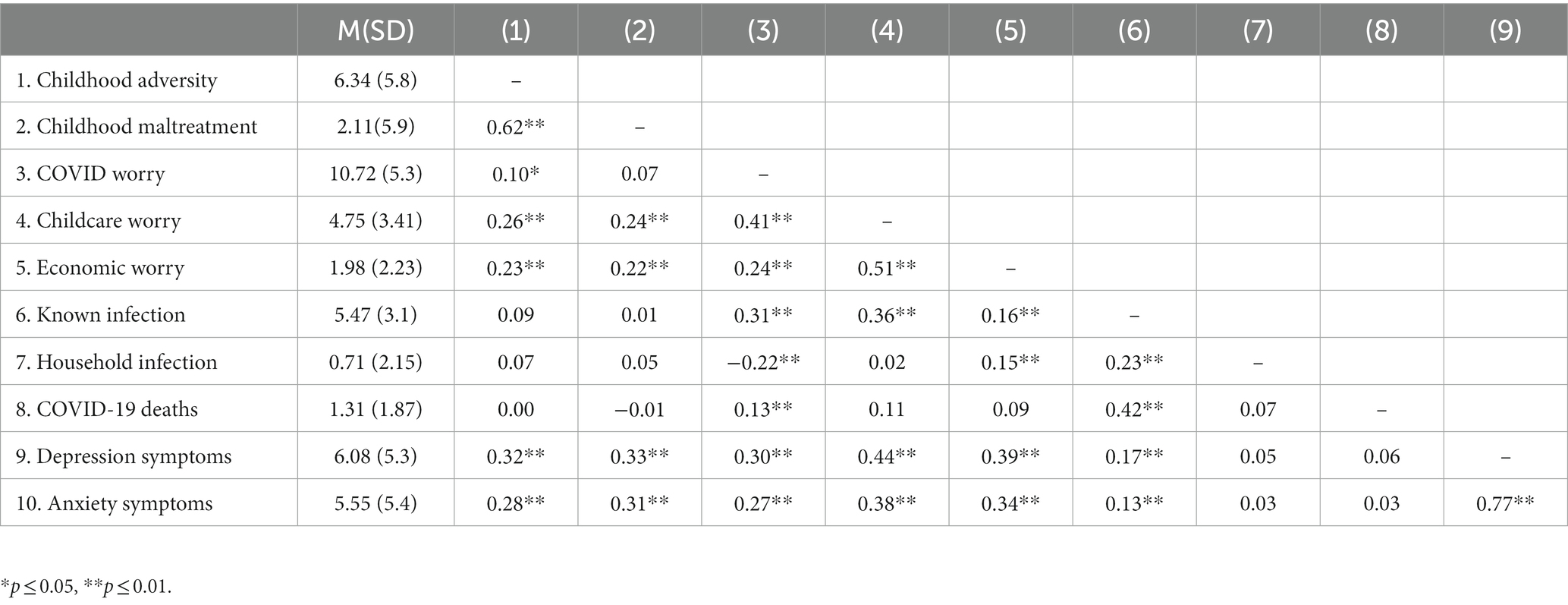
The mean number of childhood adverse experiences reported in the sample was 6.35 (SD = 5.8), and the mean number of childhood maltreatment experiences reported in the sample was 2.11 (SD = 2.9). A floor effect was observed for both scales, with 21.9% of HCWs reporting no childhood adverse experiences, and 54.1% reporting no childhood maltreatment. Variability was seen across all variables. See Table 4 for a summary of the findings. Correlational analyses were used to examine the relationship between the variables of interest. See Table 5 for a summary of the findings.
3.2. Aim 1
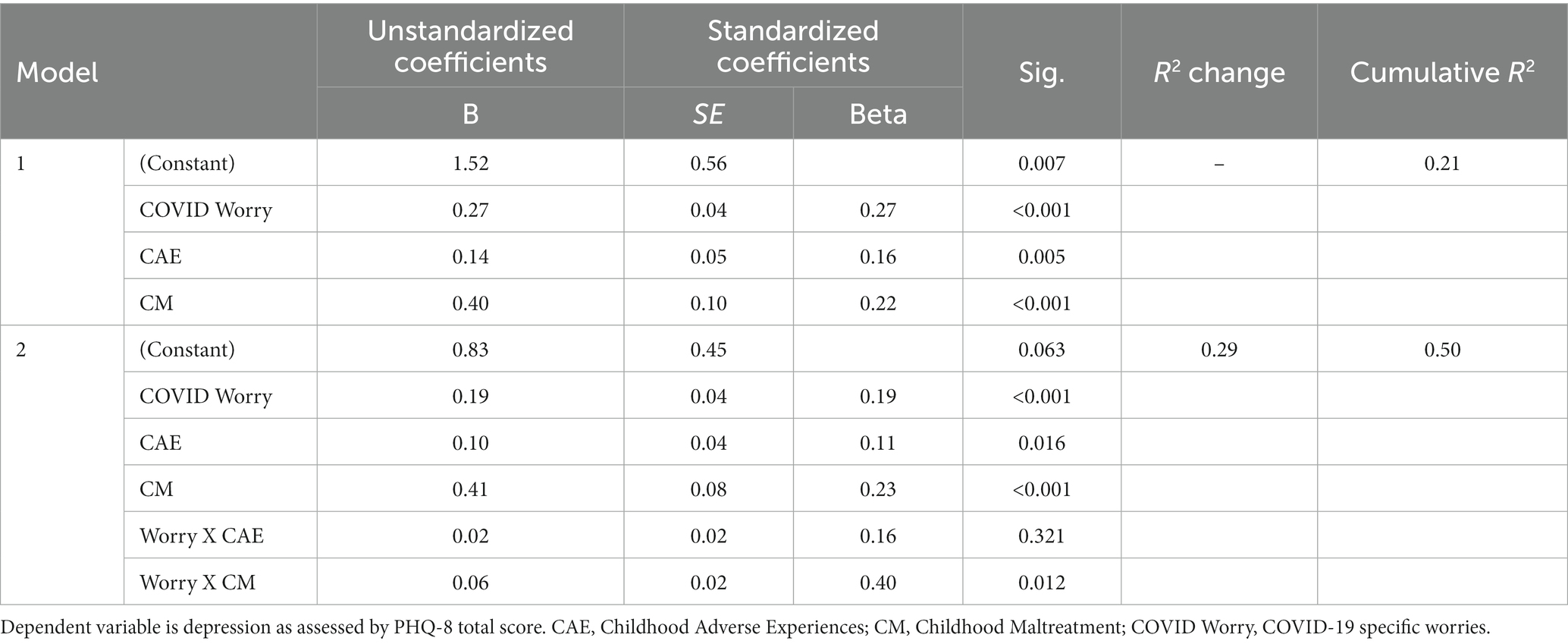
To investigate the effects of childhood adverse experiences and childhood maltreatment on the relationship between COVID-19 related stressors and depression, main effects were examined in step one of the linear regressions. Model 1 included childhood adverse events, childhood maltreatment, and COVID-19 worries as predictors and depression as the outcome, shows that COVID worry significantly predicted depression (B = 0.27, p < 0.001), childhood adverse experiences significantly predicted depression (B = 0.14, p = 0.005), and childhood maltreatment significantly predicted depression (B = 0.40, p < 0.001). Model 2 included all of these predictors and interaction terms between COVID-19 worry and the two childhood experiences variables. The R2 change between model 1 and model 2 was 0.29, with a significant F change (F = 132.01, p < 0.001). Model 1 explained 20% of the variance, whereas model 2 explained 49% of the variance, indicating that the model fit improved when accounting for the interactions between childhood maltreatment and childhood adverse experiences with COVID worry. The relationship between COVID worry and depression was stronger among individuals who scored higher in childhood maltreatment (B = 0.06, p = 0.01). The same interaction was not seen for childhood adverse experiences, suggesting that the level of exposure to childhood adverse experiences did not influence the relationship between COVID worries and depression. See Table 6 for hierarchical linear regression analyses, and Figure 1 for graphical representation of the interaction.
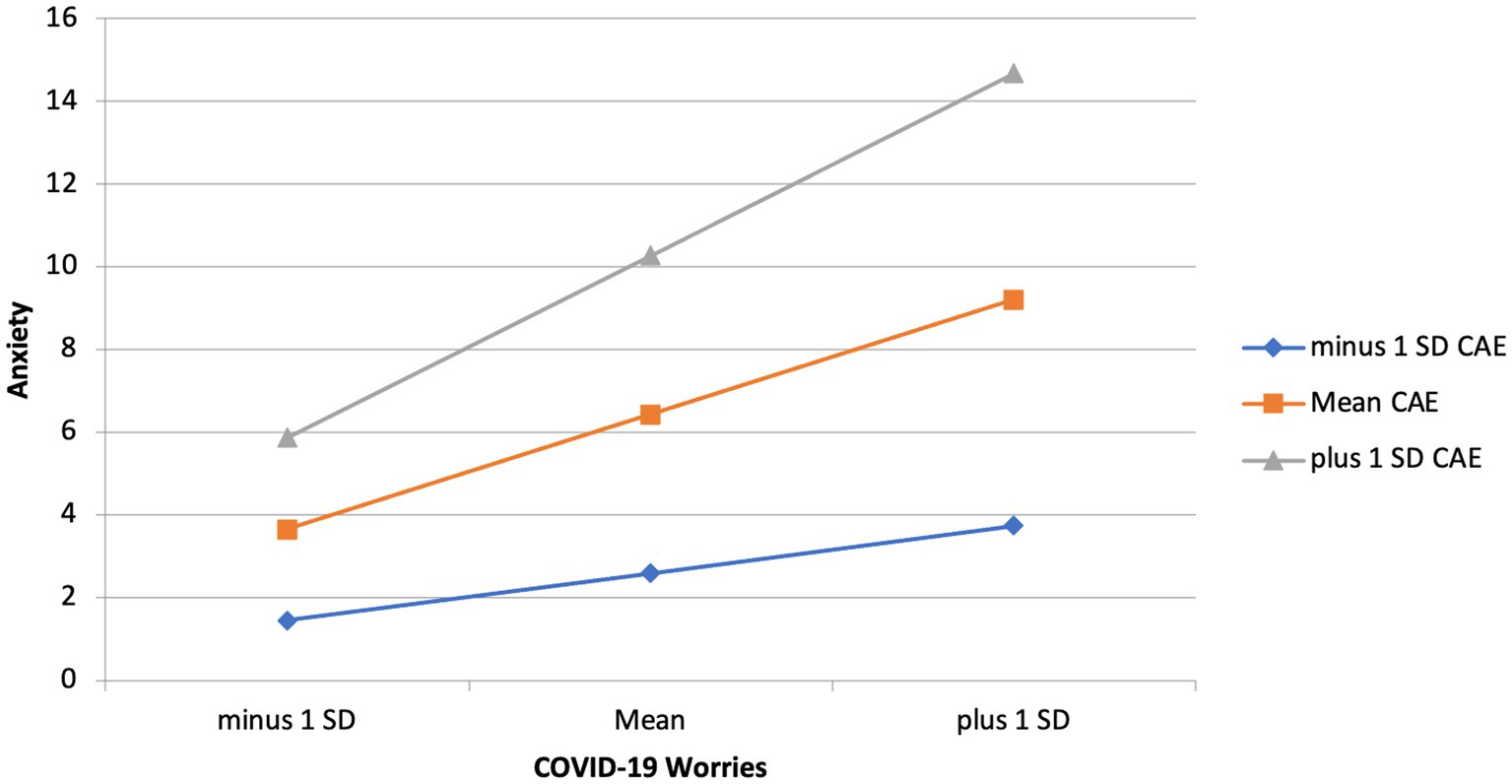
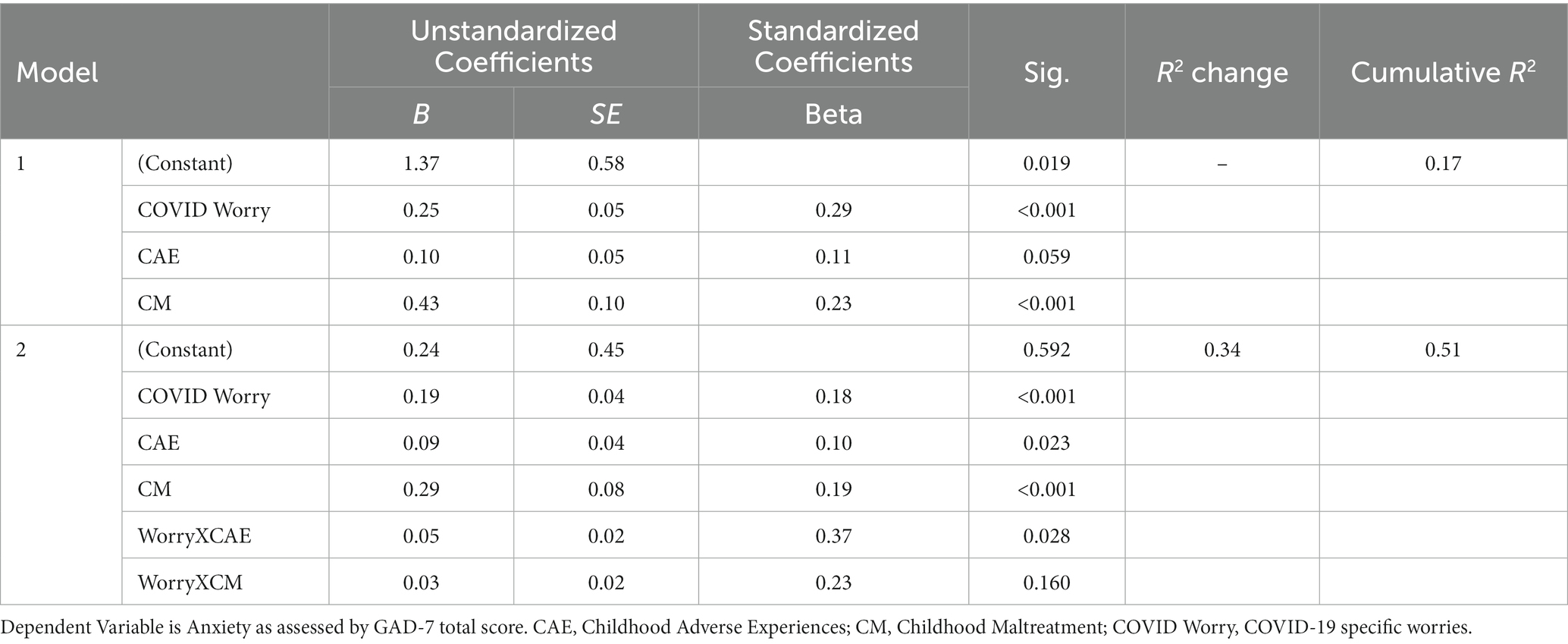
To investigate the effects of childhood adverse experiences and childhood maltreatment on the relationship between COVID-19 related worries and anxiety main effects were examined. Model 1 shows that COVID worry significantly predicts anxiety (B = 0.25, p < 0.001), and childhood maltreatment significantly predicts anxiety (B = 0.43, p < 0.001). The R2 change between model 1 and model 2 was 0.34, with a significant F change (F = 128.01, p < 0.001). Model one consisting of main effects explains 17% of the variance, whereas model 2 with interactions added explains 50% of the variance. This indicates that the regression model improved when accounting for the interactions between childhood maltreatment and childhood adverse experiences with COVID worry. The relationship between COVID worry and anxiety was stronger among individuals who scored higher in childhood adverse experiences (B = 0.05, p = 0.03). The same interaction was not seen for childhood maltreatment, meaning that the level of exposure to childhood maltreatment did not influence the relationship between COVID worries and anxiety. See Tables 3, 4 for hierarchical linear regression analyses, and Figure 2 for graphical representation of the interaction.
3.3. Aim 2
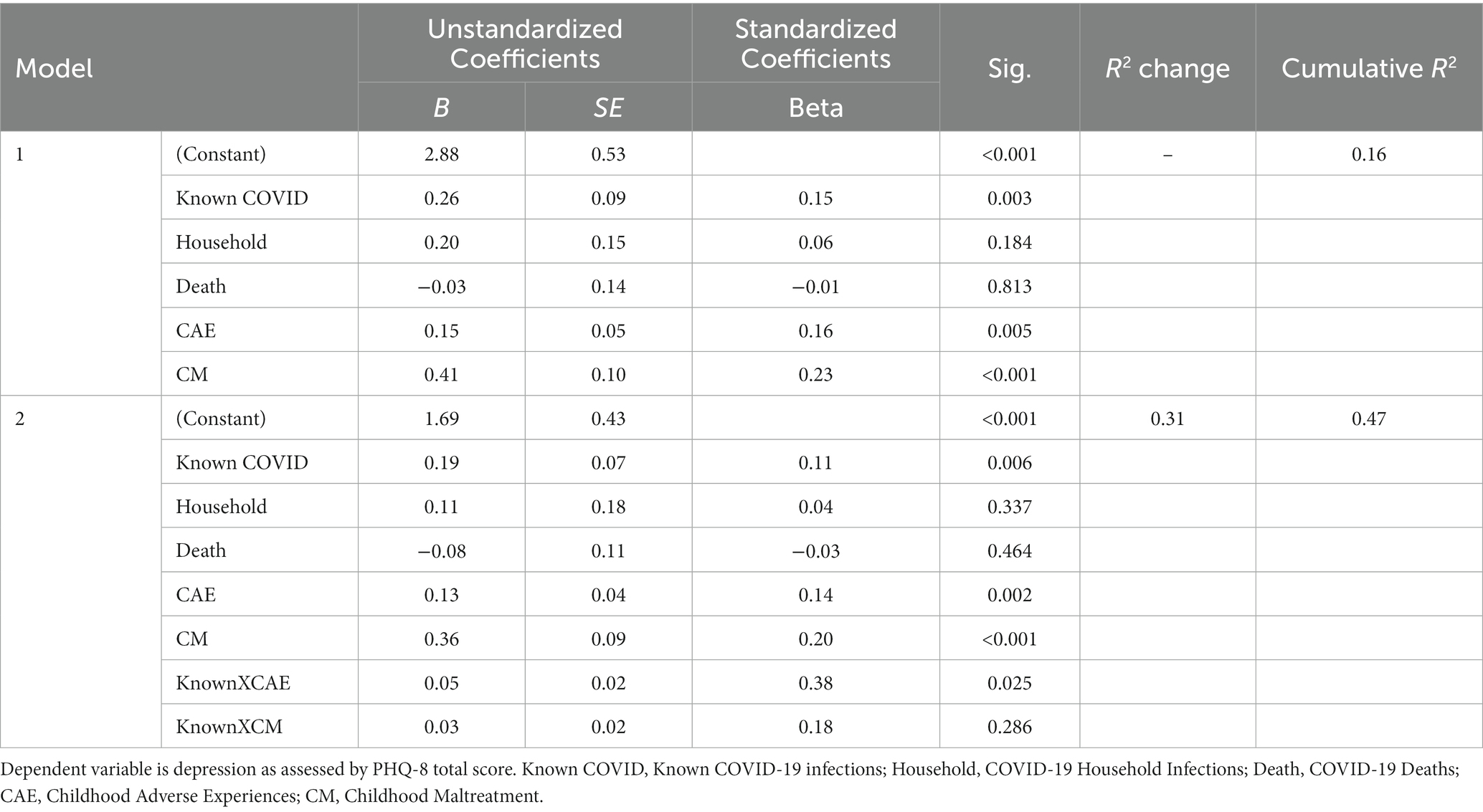
To investigate the effects of childhood adverse experiences and childhood maltreatment on the relationship between Known COVID-19 Infection and depression main effects were examined. Model 1 shows that Known COVID worry significantly predicted depression (B = 0.26, p = 0.003), childhood adverse experiences significantly predicted depression (B = 0.15, p = 0.005) and childhood maltreatment significantly predicted depression (B = 0.41, p < 0.001). Household infections and COVID-19 Deaths did not significantly predict depression and therefore were not included in the subsequent interaction models. The R2 change between model 1 and model 2 was 0.31, with a significant F change (F = 122.00, p < 0.001). Model one consisting of main effects explained 16% of the variance, whereas model 2 with interactions added explained 47% of the variance. This indicates that the regression model improved when accounting for the interactions between childhood maltreatment and childhood adverse experiences with Known COVID-19. The relationship between Known COVID-19 infection and depression was stronger among individuals who scored higher in childhood adverse experiences (B = 0.05, p = 0.03). The same interaction was not seen for childhood maltreatment, meaning that the level of exposure to childhood maltreatment did not influence the relationship between Known COVID-19 infection and depression. See Tables 3–5 for hierarchical linear regression analyses, and Figure 3 for graphical representation of the interaction.
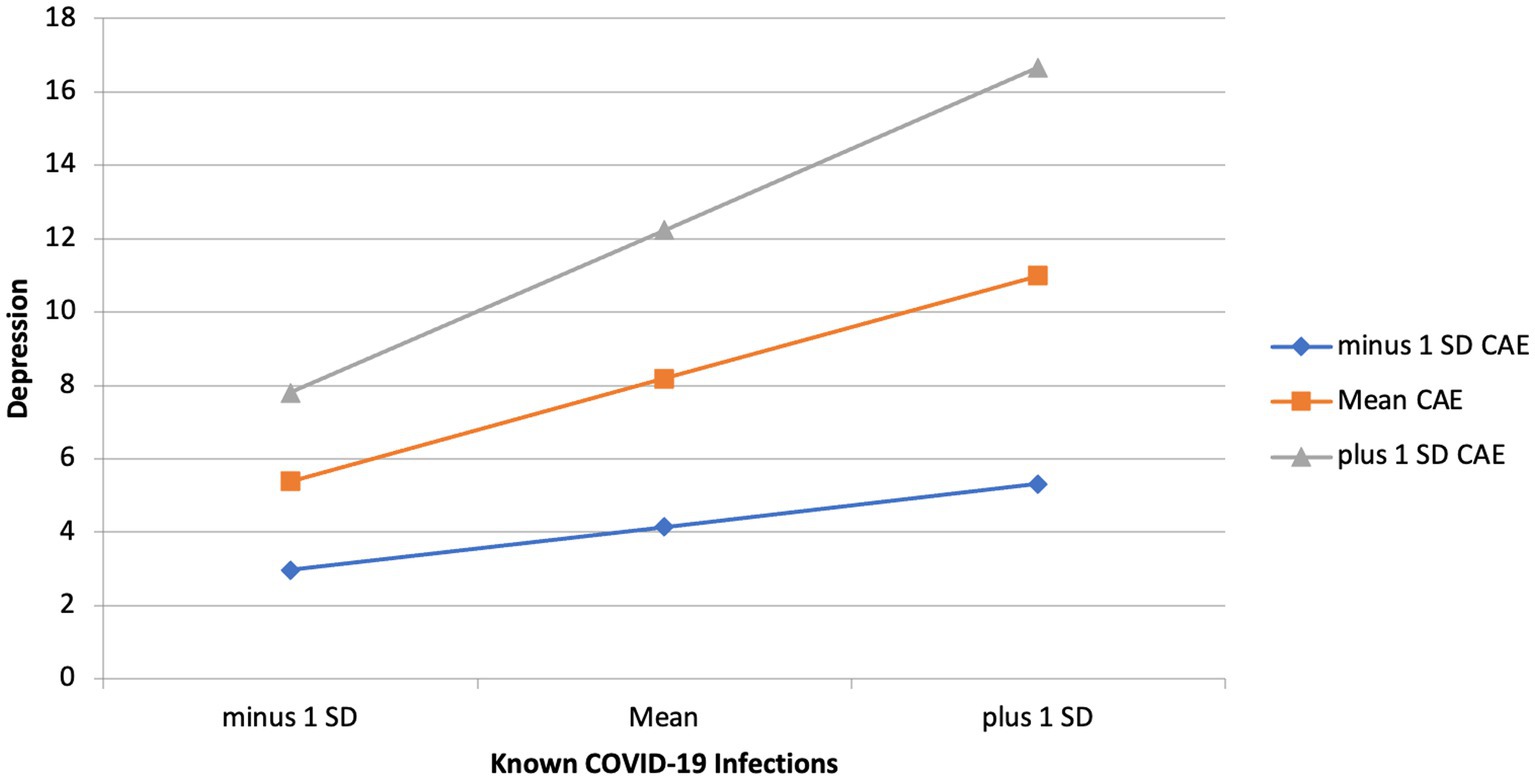
Figure 3. Interaction effect of childhood adverse experiences and known COVID-19 infections on depression.
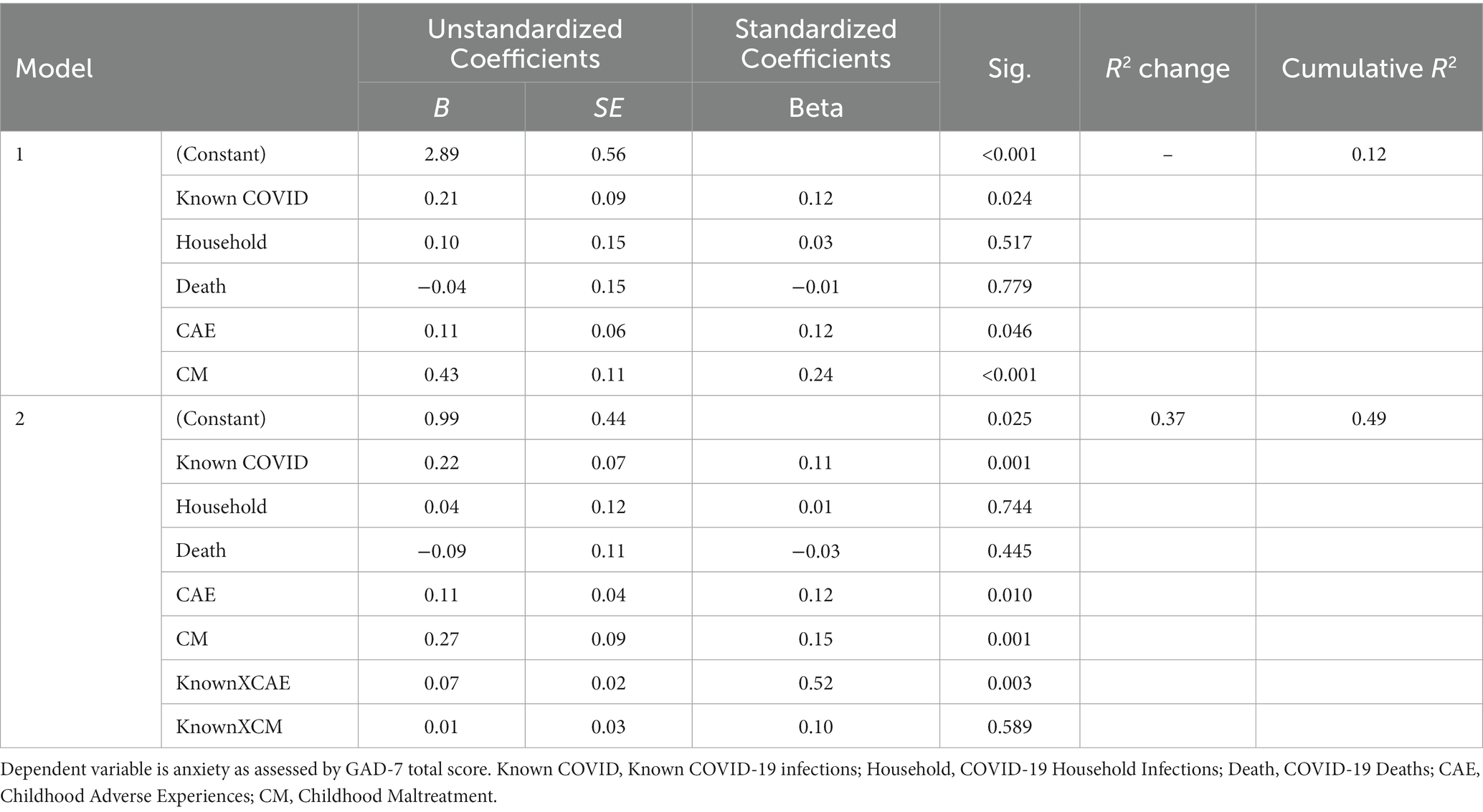
To investigate the effects of childhood adverse experiences and childhood maltreatment on the relationship between Known COVID-19 Infection and anxiety main effects were examined. Model 1 shows that Known COVID Infection significantly predicts anxiety (B = 0.21, p = 0.024), childhood adverse experiences on anxiety is significant (B = 0.11, p = 0.046), and childhood maltreatment on anxiety is significant (B = 0.43, p < 0.001). Household infections and COVID-19 Deaths did not significantly predict depression and therefore were not included in the interactions. The R2 change between model 1 and model 2 was 0.37, with a significant F change (F = 149.04, p < 0.001). Model one consisting of main effects explains 12% of the variance, whereas model 2 with interactions added explains 49% of the variance. This indicates that the regression model improved when accounting for the interactions between childhood maltreatment and childhood adverse experiences with Known COVID. The relationship between Known COVID-19 infection and anxiety was stronger among individuals who scored higher in childhood adverse experiences (B = 0.07, p = 0.003). The same interaction was not seen for childhood maltreatment, meaning that the level of exposure to childhood maltreatment did not influence did not influence the relationship between Known COVID-19 infection and anxiety. See Tables 3–6 for hierarchical linear regression analyses, and Figure 4 for graphical representation of the interaction.

Figure 4. Interaction effect of childhood adverse experiences and known COVID-19 infections on anxiety.
4. Discussion
The current study aimed to examine the relationships between adverse childhood experiences, worries about the COVID-19 pandemic, proximity to COVID-19, and the mental health symptoms of HCWs during the early stage of the pandemic. The findings of this study can provide insights into the complex interplay between these variables and highlight the potential impact of childhood experiences on HCWs’ psychological well-being. Consistent with previous research documenting the mental health challenges faced by HCWs during the pandemic (Labrague and Santos, 2020; Amsalem et al., 2021; Saragih et al., 2021; Guastello et al., 2022), the study findings show a significant association between COVID-19 worries and negative psychological symptoms, including depression and anxiety. These results highlight the substantial burden placed on HCWs due to the pandemic-related concerns they face, emphasizing the importance of addressing these worries to support their well-being (Tables 7–9).
One novel contribution of this study is the exploration of the role of adverse childhood experiences in moderating the relationship between COVID-19 worries and mental health outcomes among HCWs. The study hypotheses proposed that the association between COVID-19 worries, and depression/anxiety would be stronger for HCWs who had experienced more adverse childhood events. The results partially supported these hypotheses, as the interaction between childhood maltreatment and COVID-19 worries was found to significantly predict depression. Specifically, individuals with higher levels of childhood maltreatment demonstrated a stronger relationship between COVID-19 worries and depressive symptoms. Similar results have been seen in a study done in South Africa during the first wave of the COVID-19 pandemic which found that adults with histories of childhood trauma experience higher depressive impacts of perceived COVID-19 infection risk compared to individuals with no or minimal childhood trauma (Kim et al., 2022). These findings could imply that childhood maltreatment may amplify the impact of COVID-19 worries on HCWs’ mental health. Gaining insight into this interaction can inform interventions to support HCWs with a history of childhood maltreatment and alleviate the negative psychological consequences of COVID-19 worries.
Furthermore, the interaction between childhood adverse experiences and COVID-19 worries was found to significantly predict anxiety. This interaction was not seen with childhood maltreatment suggesting that individuals who have experienced childhood maltreatment will report anxiety independent of having COVID-19 specific worries. Similarly, to our findings, Békés and colleagues found that the number of reported adverse childhood experiences positively predicted reported levels of COVID-19 related fears, anxiety, and depression (2022). However, unlike our results, Castellini and colleagues found in a general population sample of 101 Italian women that individuals that experienced childhood trauma, specifically emotional abuse, had increased levels of distress at the onset of the pandemic compared to individuals that did not report emotional abuse (2022).
Moreover, the study examined the role of adverse childhood experiences in the relationship between HCWs’ proximity to COVID-19 cases and negative psychological symptoms. The hypothesis proposed that the association between proximity to COVID-19 cases and depression/anxiety would be stronger for HCWs with more adverse childhood experiences. When we examined the interaction effects, the relationship between Known COVID-19 infection and depression was stronger among individuals who scored higher in childhood adverse experiences and not childhood maltreatment. This finding builds on previous research done by Wang and colleagues which found that having knowledge of COVID-19 cases in relatives and family members was associated with elevated levels of depression symptoms (2020).
Similar interaction was seen when examining this model with anxiety symptoms as the outcome variable, results show that Known COVID-19 infection, childhood adverse experiences, and childhood maltreatments all significantly predicted anxiety symptoms. These results were hypothesized given the previous research on COVID-19 proximity and anxiety symptoms. In a housing compound in Guangzhou, China, the results of 403 participants showed that higher anxiety levels were associated with residents that knew of the presence of individuals with COVID-19 in their building (Su et al., 2020). Similarly, a web-based survey of 398 university students in Iran found that individuals who personally knew of someone with COVID-19 experienced more COVID-19 anxiety than individuals who did not (Shabahang et al., 2021). A study of university students in Vancouver found that knowledge of COVID-19 cases was associated with probability of elevated anxiety symptoms (Vigo et al., 2021). When examining the interaction effects for this model, the relationship between Known COVID-19 infection and anxiety was only stronger among individuals who scored higher in childhood adverse experiences and not childhood maltreatment.
The current study has several implications in line with current literature (Greenberg et al., 2020; Amsalem et al., 2021; Magalhaes et al., 2021), for understanding and addressing the mental health needs of HCWs during pandemic times. Firstly, it emphasizes the importance of recognizing and addressing the specific worries and concerns related to the COVID-19 pandemic that HCWs experience. Interventions and support systems should be implemented to help HCWs manage these worries effectively, providing them with resources and coping strategies to mitigate the negative psychological symptoms associated with the pandemic. Secondly, the study highlights the potential long-lasting impact of childhood maltreatment on HCWs’ mental health during the pandemic. Expanding on past literature, this study demonstrates how the presence of childhood adverse experiences such as caregiver unavailability, caregiver separation, caregiver drug abuse, caregiver medical or mental illness, caregiver experience of emotional/physical/sexual abuse can exacerbate the relationship between COVID-19 specific worries and anxiety, as well as proximity to COVID-19 (Known COVID-19 infection) and depression and anxiety.
Due to the nature of their responsibilities and workplace stress, HCWs are among vulnerable groups especially during global health crises. Considering the prevalence rates of ACEs in the United States, the results of this study emphasize the importance of keeping in mind HCWs who have experienced past aversive childhood experiences as these experiences can experience more psychiatric symptoms. In addition to daily life stressors, HCWs are responding to unknown virus outbreaks and patient crises. For them to provide effective care without experiencing burnout and significant depression and or anxiety, they need to attend to their own mental health well-being first. Seeking mental health care can be intimating and may be accompanied with stigma even in medical settings. Therefore, the sole presence of resources is not enough. Creating an environment where HCWs feel encouraged to seek out mental health services is imperative for hospital leaders, policymakers, and direct supervisors. Trauma-informed approaches and evidence-based interventions for individuals with a history of childhood maltreatment should be considered to enhance their resilience and well-being during these challenging times.
4.1. Strengths and limitations
One of the strengths of this study is the inclusion of non-clinical HCWs in the sample. Many studies on HCWs focus on doctors and nurses, and as prior research has shown non-clinical HCWs face psychological distress given the environment of their work (Dobson et al., 2021; Jang et al., 2021). Another strength of this study is the sample size which allowed for better statistical power to detect relationships. One of the limitations when examining this study is its limited diversity, the majority of the sample were white American women, and the sample was drawn from one health system in Florida. Gender of the participant could impact both adverse childhood experiences and the manifestation of psychological symptoms. Diversifying the data by examining multiple different academic medical centers with different policies will provide a more comprehensive insight to HCWs mental health given that it will provide a larger variance in gender, ethnicity, and socioeconomic status.
This data was collected from October to December 2020, a time where many COVID-19 outcomes were still uncertain. It is worth emphasizing that high-risk medical workers in these health systems gained access to COVID-19 vaccines starting from December 2020. The pandemic could have affected HCWs that participated in the first month of the study differently than HCWs that participated in the last month of the study given the availability of the vaccines and more understanding of the virus. Therefore, due to the rapid change in policies at both state level and hospital level, as well as the unpredictability and unknown nature of COVID-19 at the beginning stages of the pandemic, the generalizability of this data can be a limitation. Nevertheless, this study provides an insight into the impact COVID-19 had on HCWs at the end of the first year of the pandemic. Future research could explore the long-term impact of COVID-19 stress and adverse childhood experiences on HCWs’ mental health throughout different phases of the pandemic.
5. Conclusion
This study expands on previous literature regarding the impact of COVID-19 on HCWs’ mental health. The current study found that adverse childhood experiences strengthen the relationship between HCWs COVID-19 worries and proximity when predicting their psychological symptoms. As COVID-19 becomes endemic, hospital leaderships and authorities need to continue addressing COVID-19 worries and HCWs’ psychological symptoms through mental health support and organizational interventions. More specifically, vulnerable populations such as individuals who have ACEs will benefit from targeted and specific interventions to cope with the collective trauma experienced globally due to COVID-19.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the University of Florida Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
TM conceptualized the manuscript, wrote the majority of the manuscript, and revised the manuscript. AG contributed funding for the parent study, conceptualized the manuscript, assisted with statistical analyses and write up, and revised the manuscript. LD conceptualized the parent study and inclusion of the measures of interest, and edited and revised the manuscript. NS conceptualized and secured funding for the parent study. BA and CM conceptualized the parent study and edited and revised the manuscript. CM contributed funding for the parent study. All authors contributed to the article and approved the final version.
Funding
This work was supported in part by the University of Florida, Clinical and Translational Science Institute (supported in part by the NIH National Center for Advancing Translational Sciences under award number UL1TR001427), and in part by the Evelyn F. and William L. McKnight Brain Institute and the UF Center for OCD, Anxiety, and Related Disorders.
Acknowledgments
The authors would like to acknowledge with gratitude the healthcare workers who took time from their stressful jobs during the pandemic to participate in our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Amsalem, D., Lazarov, A., Markowitz, J. C., Naiman, A., Smith, T. E., Dixon, L. B., et al. (2021). Psychiatric symptoms and moral injury among US healthcare workers in the COVID-19 era. BMC Psychiatry 21:546. doi: 10.1186/s12888-021-03565-9
Ballou, S., Gray, S., and Palsson, O. S. (2020). Validation of the pandemic emotional impact scale. Brain Behav. Immun. Health 9:100161. doi: 10.1016/j.bbih.2020.100161
Békés, V., Starrs, C. J., and Perry, J. C. (2023). The COVID-19 pandemic as traumatic stressor: distress in older adults is predicted by childhood trauma and mitigated by defensive functioning. Psychol. Trauma Theory Res. Pract. Policy 15, 449–457. doi: 10.1037/tra0001253
Carmassi, C., Foghi, C., Dell’Oste, V., Cordone, A., Bertelloni, C. A., Bui, E., et al. (2020). PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 292:113312. doi: 10.1016/j.psychres.2020.113312
Castellini, G., Tarchi, L., Cassioli, E., Rossi, E., Sanfilippo, G., Innocenti, M., et al. (2022). Attachment style and childhood traumatic experiences moderate the impact of initial and prolonged COVID-19 pandemic: mental health longitudinal trajectories in a sample of Italian women. Int. J. Ment. Health Addic. 1–20. Advance online publication. doi: 10.1007/s11469-022-00798-x
Cicchetti, D. (2016). Socioemotional, personality, and biological development: illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annu. Rev. Psychol. 67, 187–211. doi: 10.1146/annurev-psych-122414-033259
Cicchetti, D., and Toth, S. L. (2005). Child maltreatment. Annu. Rev. Clin. Psychol. 1, 409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029
Clemens, V., Köhler-Dauner, F., Keller, F., Ziegenhain, U., and Fegert, J. M. (2022). Adverse childhood experiences are associated with a higher risk for increased depressive symptoms during Covid-19 pandemic – a cross-sectional study in Germany. BMC Psychiatry 22:540. doi: 10.1186/s12888-022-04177-7
Dale, L. P., Davidson, C., and Kolacz, J. (2020). Adverse traumatic experiences scale. Jacksonville, FL.
Dale, L. P., Cuffe, S. P., Kolacz, J., Leon, K. G., Bossemeyer Biernacki, N., Bhullar, A., et al. (2022). Increased autonomic reactivity and mental health difficulties in COVID-19 survivors: implications for medical providers. Front. Psychiatry 13:830926. doi: 10.3389/fpsyt.2022.830926
Denning, M., Goh, E. T., Tan, B., Kanneganti, A., Almonte, M., Scott, A., et al. (2021). Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. PLoS One 16:e0238666. doi: 10.1371/journal.pone.0238666
Dobson, H., Malpas, C. B., Burrell, A. J., Gurvich, C., Chen, L., Kulkarni, J., et al. (2021). Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas. Psychiatry 29, 26–30. doi: 10.1177/1039856220965045
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am. J. Prev. Med. 14, 245–258. doi: 10.1016/s0749-3797(98)00017-8
Greenberg, N., Docherty, M., Gnanapragasam, S., and Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368. doi: 10.1136/bmj.m1211
Guastello, A. D., Brunson, J. C., Sambuco, N., Dale, L. P., Tracy, N. A., Allen, B. R., et al. (2022). Predictors of professional burnout and fulfilment in a longitudinal analysis on nurses and healthcare workers in the COVID-19 pandemic. J. Clin. Nurs. doi: 10.1111/jocn.16463
Gupta, N., Dhamija, S., Patil, J., and Chaudhari, B. (2021). Impact of COVID-19 pandemic on healthcare workers. Ind. Psychiatry J. 30, 282–S284. doi: 10.4103/0972-6748.328830
Hidaka, Y., Sasaki, N., Imamura, K., Tsuno, K., Kuroda, R., and Kawakami, N. (2021). Changes in fears and worries related to COVID-19 during the pandemic among current employees in Japan: a 5-month longitudinal study. Public Health 198, 69–74. doi: 10.1016/j.puhe.2021.06.017
Hooper, L., Stockton, P., Krupnick, J., and Green, B. (2011). Development, use, and psychometric properties of the Trauma History Questionnaire. J. Loss Trauma 16, 258–283. doi: 10.1080/15325024.2011.572035
IBM Corp (SPSS Inc.). (2019). IBM SPSS statistics for windows (version 26.0) [computer software]. Armonk, NY: IBM Corp.
Iob, E., Lacey, R., Giunchiglia, V., and Steptoe, A. (2022). Adverse childhood experiences and severity levels of inflammation and depression from childhood to young adulthood: a longitudinal cohort study. Mol. Psychiatry 27, 2255–2263. doi: 10.1038/s41380-022-01478-x
Jang, Y., You, M., Lee, H., Lee, M., Lee, Y., Han, J.-O., et al. (2021). Burnout and peritraumatic distress of healthcare workers in the COVID-19 pandemic. BMC Public Health 21:2075. doi: 10.1186/s12889-021-11978-0
Kim, A. W., Nyengerai, T., and Mendenhall, E. (2022). Evaluating the mental health impacts of the COVID-19 pandemic: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Psychol. Med. 52, 1587–1599. doi: 10.1017/s0033291720003414
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B., Berry, J. T., and Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 114, 163–173. doi: 10.1016/j.jad.2008.06.026
Kolacz, J., Dale, L. P., Nix, E. J., Roath, O. K., Lewis, G. F., and Porges, S. W. (2020). Adversity history predicts self-reported autonomic reactivity and mental health in US residents during the COVID-19 pandemic. Front. Psychiatry 11:577728. doi: 10.3389/fpsyt.2020.577728
Labrague, L. J., and Santos, J. A. A. (2020). COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 28, 1653–1661. doi: 10.1111/jonm.13121
LeMoult, J., Humphreys, K. L., Tracy, A., Hoffmeister, J.-A., Ip, E., and Gotlib, I. H. (2020). Meta-analysis: exposure to early life stress and risk for depression in childhood and adolescence. J. Am. Acad. Child Adolesc. Psychiatry 59, 842–855. doi: 10.1016/j.jaac.2019.10.011
Luo, M., Guo, L., Yu, M., Jiang, W., and Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. 291:113190. doi: 10.1016/j.psychres.2020.113190
Magalhaes, E., Stoner, A., Palmer, J., Schranze, R., Grandy, S., Amin, S., et al. (2021). An assessment of mental health outcomes during the COVID-19 pandemic. Community Ment. Health J. 57, 1267–1277. doi: 10.1007/s10597-021-00876-9
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R., and Guessoum, S. B. (2021). Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126, 252–264. doi: 10.1016/j.neubiorev.2021.03.024
Mayorga, N. A., Smit, T., Garey, L., Gold, A. K., Otto, M. W., and Zvolensky, M. J. (2022). Evaluating the interactive effect of COVID-19 worry and loneliness on mental health among young adults. Cogn. Ther. Res. 46, 11–19. doi: 10.1007/s10608-021-10252-2
McKay, M. T., Kilmartin, L., Meagher, A., Cannon, M., Healy, C., and Clarke, M. C. (2022). A revised and extended systematic review and meta-analysis of the relationship between childhood adversity and adult psychiatric disorder. J. Psychiatr. Res. 156, 268–283. doi: 10.1016/j.jpsychires.2022.10.015
Merrick, M. T., Ford, D. C., Ports, K. A., Guinn, A. S., Chen, J., Klevens, J., et al. (2019). Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 states, 2015–2017. MMWR Morb. Mortal. Wkly Rep. 68, 999–1005. doi: 10.15585/mmwr.mm6844e1
Mersky, J. P., Topitzes, J., and Reynolds, A. J. (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child abuse & neglect 37, 917–925. doi: 10.1016/j.chiabu.2013.07.011
Mo, Y., Deng, L., Zhang, L., Lang, Q., Liao, C., Wang, N., et al. (2020). Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 28, 1002–1009. doi: 10.1111/jonm.13014
Prout, T. A., Zilcha-Mano, S., Aafjes-van Doorn, K., Békés, V., Christman-Cohen, I., Whistler, K., et al. (2020). Identifying predictors of psychological distress during COVID-19: a machine learning approach. Front. Psychol. 11:586202. doi: 10.3389/fpsyg.2020.586202
Rogers, A. H., Shepherd, J. M., Garey, L., and Zvolensky, M. J. (2020). Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res. 293:113407. doi: 10.1016/j.psychres.2020.113407
Saragih, I. D., Tonapa, S. I., Saragih, I. S., Advani, S., Batubara, S. O., Suarilah, I., et al. (2021). Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int. J. Nurs. Stud. 121:104002. doi: 10.1016/j.ijnurstu.2021.104002
Schnurr, P., Vielhauer, M., Weathers, F., and Findler, M. (1999). Brief Trauma Questionnaire (BTQ) [Database record]. APA PsycTests. doi: 10.1037/t07488-000
Shabahang, R., Aruguete, M. S., Rezaei, S., and McCutcheon, L. E. (2021). Psychological determinants and consequences of COVID-19 anxiety: a web-based study in Iran. Health Psychol. Res. 9:24841. doi: 10.52965/001c.24841
Shanafelt, T., Ripp, J., and Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 323, 2133–2134. doi: 10.1001/jama.2020.5893
Søvold, L. E., Naslund, J. A., Kousoulis, A. A., Saxena, S., Qoronfleh, M. W., Grobler, C., et al. (2021). Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front. Public Health 9:679397. doi: 10.3389/fpubh.2021.679397
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Su, J., Chen, X., Yang, N., Sun, M., and Zhou, L. (2020). Proximity to people with COVID-19 and anxiety among community residents during the epidemic in Guangzhou, China. BJPsych Open 6:e75. doi: 10.1192/bjo.2020.59
Tiete, J., Guatteri, M., Lachaux, A., Matossian, A., Hougardy, J.-M., Loas, G., et al. (2021). Mental health outcomes in healthcare workers in COVID-19 and non-COVID-19 care units: a cross-sectional survey in Belgium. Front. Psychol. 11:612241. doi: 10.3389/fpsyg.2020.612241
Tzouvara, V., Kupdere, P., Wilson, K., Matthews, L., Simpson, A., and Foye, U. (2023). Adverse childhood experiences, mental health, and social functioning: a scoping review of the literature. Child Abuse Negl. 139:106092. doi: 10.1016/j.chiabu.2023.106092
Vigo, D., Jones, L., Munthali, R., Pei, J., Westenberg, J., Munro, L., et al. (2021). Investigating the effect of COVID-19 dissemination on symptoms of anxiety and depression among university students. BJPsych Open 7:e69. doi: 10.1192/bjo.2021.24
Wang, Z.-H., Yang, H.-L., Yang, Y.-Q., Liu, D., Li, Z.-H., Zhang, X.-R., et al. (2020). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 275, 188–193. doi: 10.1016/j.jad.2020.06.034
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., and Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5) - standard. [Measurement instrument]. Available from https://www.ptsd.va.gov/
Keywords: healthcare workers, COVID-19, stress, anxiety, depression, adverse childhood experiences, mental health, cross-sectional study
Citation: Mirhosseini T, Guastello AD, Dale LP, Sambuco N, Allen BR and Mathews CA (2023) Effects of COVID-19 stress, proximity, and adverse childhood experiences on healthcare workers’ mental health. Front. Psychol. 14:1228515. doi: 10.3389/fpsyg.2023.1228515
Edited by:
Vasfiye Bayram Deger, Mardin Artuklu University, TürkiyeReviewed by:
Alessia Renzi, Sapienza University of Rome, ItalyMajed Wadi, Qassim University, Saudi Arabia
Copyright © 2023 Mirhosseini, Guastello, Dale, Sambuco, Allen and Mathews. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tannaz Mirhosseini, dG1pcmhvc3NlaW5pQHVmbC5lZHU=
 Tannaz Mirhosseini
Tannaz Mirhosseini Andrea D. Guastello
Andrea D. Guastello Lourdes P. Dale
Lourdes P. Dale Nicola Sambuco2,3,4
Nicola Sambuco2,3,4 Carol A. Mathews
Carol A. Mathews