Abstract
Introduction:
Perceived stress and depression were indirect effects of the COVID-19 pandemic, especially in square-cabin hospitals. It was paramount to understand their mediating effects, which might detonate factors that led to mental illness.
Materials and methods:
We conducted a cross-sectional study to investigate perceived stress and depressive symptoms among patients with COVID-19 in Shanghai square-cabin hospitals from April 18 to May 19, 2022. The questionnaire included the Perceived Stress Scale 10, Patient Health Questionnaire 9, Perceived Social Support Scale, and the Connor-Davidson Resilience Scale 10.
Results:
This study investigated the chain-mediating roles of perceived social support and resilience in the relationship between perceived stress and depression. Perceived stress positively predicted depression (r = 0.613, p < 0.01), negatively correlated with perceived social support (r = −0.318, p < 0.01) and resilience (r = −0.398, p < 0.01). In the chain mediating model, perceived stress had significant direct predictive effects on depression, and significant indirect predictive effects on depression through perceived social support and/or resilience.
Conclusion:
It showed that higher perceived social support and resilience were associated with lower perceived stress among COVID-19 patients, which might lead to symptoms of mild depression, and highlights the importance of resilience and perceived social support in reducing depressive symptoms.
1 Introduction
Coronavirus disease 2019 (COVID-19) has become a public health threat worldwide. In this situation, a series of objective events triggered by the pandemic have led to different levels of psychological problems in different populations. The COVID-19 patients suffer from anxiety, stress and restlessness (Duan and Zhu, 2020; Matalon et al., 2021; Robinson et al., 2022). In addition to the direct effects of COVID-19, the pandemic has created an environment in which many determinants of mental health are also affected (Damian et al., 2021). The feeling of experiencing stress may also be aggravated by centralized isolation and treatment, dense population, unfamiliar environment, cohabitation of COVID-19 patients, depressing environment of the ward, family members and loved ones suffering from COVID-19 or worsening of the disease or death due to COVID-19 (Awano et al., 2020; Lu et al., 2021). Therefore, they might be considered as one of the most vulnerable people to experience psychological stress and other mental health symptoms (Du et al., 2024).
The COVID-19 patients were reported high stress levels during the COVID-19 epidemics (Vindegaard and Benros, 2020; Matalon et al., 2021; Fu et al., 2022; Malinauskas and Malinauskiene, 2022). Perceived stress is an individual response or experience to a stimulus, threat or event in different circumstances, which is one of the gateways to several mental health disorders, such as anxiety, depression, phobia, post traumatic disorder and even psychotic disorders (Banjongrewadee et al., 2020). Numerous research has suggested a link between perceived stress and depressive symptoms (Spada et al., 2008; Besharart et al., 2020; Yan et al., 2021; Dymecka et al., 2022; Lathabhavan and Vispute, 2022). The fear of disease and the pathological state of the body could aggravate the perceived stress symptoms of COVID-19 patients, which is one of the important reasons for the depression (Li J. et al., 2020; Li Z. et al., 2020; Lu et al., 2021). However, the internal mechanism of the relationship between perceived stress and depression during the COVID-19 pandemic remain largely unexplored (Duan and Zhu, 2020; Damico et al., 2021). Models of the stress-depression relationship emphasized the importance of perceived stress and coping resources (Hewitt et al., 1992; Dulaney et al., 2008). Previous studies have paid more attention to how perceived stress negatively affect patients, and generally ignored the protective or buffering factors on depression (Banjongrewadee et al., 2020; Dymecka et al., 2022; Hu et al., 2022). Therefore, in order to better respond to mental health problems, we need to identify the protective or buffer factors for the COVID-19 patients, focusing on people’s positive psychological strength from a new perspective.
Among several protective factors, social support and psychological resilience have been proven to alleviate the negative effects of stress and depression (Santini et al., 2015; Bloom et al., 2017; Labrague et al., 2018; Chen and Bonanno, 2020). Social support improved mental status possibly in the form of benefits from social relationships and a buffer against stressful situations (Alsubaie et al., 2019). One study has pointed that social support would be a potential determinant for depression during the COVID-19 pandemic (Chan and Lee, 2022). Perceived social support is considered to be one of the important social factors for predicting individual depression (Hyde et al., 2011). There is a direct or indirect relationship between perceived social support and depression (Cohen and Wills, 1985). Previous studies found that higher level of perceived social support is associated with lower level of depression (Grey et al., 2020; Chan and Lee, 2022). Some studies have shown that positive experiences of social support foster resilience to stress and prevent psychopathology (Ozbay et al., 2007). In addition, the predictive effect of social support on mental health can be achieved through resilience (Wilks and Croom, 2008).
As a key psychosocial factor, resilience can help individuals cope with stress more effectively when they experience psychological pain in stressful situations (Richardson, 2002). Studies indicated that resilience was a protective factor for COVID-19 patients and was negatively correlated with depression (Awano et al., 2020), people with high resilience were less likely to suffer from depression (Benedek et al., 2007). Some studies pointed out that resilience worked through interaction with the environment (Luthar et al., 2000). As an external environmental factor, social support enhanced individuals’ adaptability to adverse conditions by endowing and mobilizing their psychological resources, thus improving their mental health status (Chen, 2019).
This study aimed to elucidate the mechanisms underlying the associations between stress, perceived social support, resilience, and depression in patients with COVID-19. Patients with COVID-19 isolated from Shanghai Makeshift Hospitals were enrolled in this study. We not only analyzed the independent mediating effects of perceived social support and mental resilience, but also analyzed the chain mediating effects of perceived social support and mental resilience. This may provide a better understanding of the stressful events experienced by patients and their contribution to the risk of depression. We speculated that the association between stress and depressive symptoms is mediated by perceived social support and mental resilience. Specifically, we hypothesized that individuals in stressful situations have lower levels of perceived social support and mental resilience, which may further lead to more severe depressive symptoms. Furthermore, we predicted that the effect of psychological resilience on depression in stressful situations is influenced by perceived social support, that is, high levels of perceived social support would strengthen the association between stress, resilience, and depressive symptoms.
2 Materials and methods
2.1 Participants
The participants were COVID-19 patients at Shanghai square-cabin hospitals from April 18 to May 19, 2022. Considering data collection and patient isolation, an online method was used. They completed the questionnaires on their mobile phones by scanning a QR code which were provided by an online platform.1 All participants gave their electronic informed consent after understanding the research content and the rights and obligations of the researcher and participants. A total of 1,014 questionnaires were collected, of which 126 invalid questionnaires were excluded. The exclusion criteria were as follows: (1) the time took less than 100 s to complete the survey; (2) selection of the same option for all items; (3) the total score exceeded three standard deviations. The remaining 888 valid questionnaires constituted the data for this study. The effective utilization rate was 87.57%.
2.2 Measures
2.2.1 Perceived stress scale questionnaire (PSS-10)
Perceived stress symptoms were assessed using the Simplified Chinese Perceived Stress Scale (PSS-10) questionnaire (Lee and Crockett, 1994), based on the PSS-10 (Cohen et al., 1983). The PSS-10 includes 10 items, each rated on a 5-point scale from 0 (never) to 4 (very common). Higher scores indicate higher levels of perceived stress. The scale has been demonstrated with strong reliability and validity (Sun et al., 2019; Hu et al., 2023). In the current study, the Cronbach’s α coefficient for the entire scale was 0.861.
2.2.2 Patient health questionnaire (PHQ-9)
Depression was measured using the validated Chinese version of the 9-item self-report Patient Health Questionnaire-9 (PHQ-9) (Yu et al., 2012), based on the nine Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria which was employed to assess the frequency of depressive symptoms over the past 2 weeks (Spitzer, 1999). The Patient Health Questionnaire-9 (PHQ-9) is a widely used self-rated version to ascertain the mental state of COVID-19 patients (Liu C. H. et al., 2020; Liu J. et al., 2020; Cha et al., 2022; Zhao et al., 2022). The score for each item varies from 0 (not at all) to 3 (nearly every day). The sum of the scores ranges from 0 to 27, and a higher total PHQ-9 score indicates more severe depressive symptoms. In this study, the Cronbach’s α coefficient for the entire scale was 0.911.
2.2.3 Perceived social support scale (PSSS)
The Perceived Social Support Scale (PSSS) is a 12-item self-report measure in which participants indicate their perception of support from friends, family, and a significant other on a seven-point Likert scale ranging from 1 (very strongly disagree) to 7 (very strongly agree) (Zimet et al., 1988). The modified Chinese PSSS validated by Wang was used in this study (Wang et al., 1999). The scale has been used with excellent psychometric properties (Wen et al., 2020; Zhao et al., 2023). In this study, the Cronbach’s α coefficient for the entire scale was 0.961.
2.2.4 Connor-Davidson resilience scale (CD-RISC 10)
The 10-item Connor-Davidson Resilience Scale (CD-RISC 10) is a common scale used to assess resilience (Campbell-Sills and Stein, 2007). The translated Chinese version was used in this study (Lyu et al., 2017). The CD-RISC 10 includes 10 items, each rated on a 5-point scale from 0 (never) to 4 (very common). Previous studies have shown that this scale was in excellent reliability and validity (Fu and Wang, 2022; Lu et al., 2024). Higher scores on this scale are interpreted as higher resilience. In this study, the Cronbach’s α coefficient for the entire scale was 0.956.
2.3 Statistical analyses
IBM’s SPSS software (version26.0) was used to analyze the data. The results of common method bias were examined using the Harman one-way test (Podsakoff et al., 2003), which indicates a serious common bias if one factor explains more than 50% of the common variance (the result is 40.98%) (Podsakoff and Management, 1986). Measurement data conforming to a normal distribution were expressed as mean ± SD, and count data were described using frequency and composition ratios. Bivariate relationships between the variables were determined using Pearson’s correlation analysis. The bias-corrected percentile bootstrap method was employed to test the hypothesized chain mediation model. Chain-mediated effect implementation (Model 6, Process Macro) (Hayes, 2015) was performed by repeated sampling 5,000 times. The 95% corrected confidence interval (CI) method-mediated effects were considered statistically significant if the 95% bootstrap CI for the indirect effect did not contain zero (Preacher and Hayes, 2008). The direct effect was considered when the independent variable directly affected the dependent variable, and when the 95% CI of the bootstrap test did not include zero, the effect was valid. An indirect effect was considered when the independent variable had an effect on the dependent variable through the intermediary variable, and when the 95% CI did not include zero via the bootstrap method, the indirect effect was valid. Figure 1 shows the conceptual chained mediation model of the current study.
Figure 1
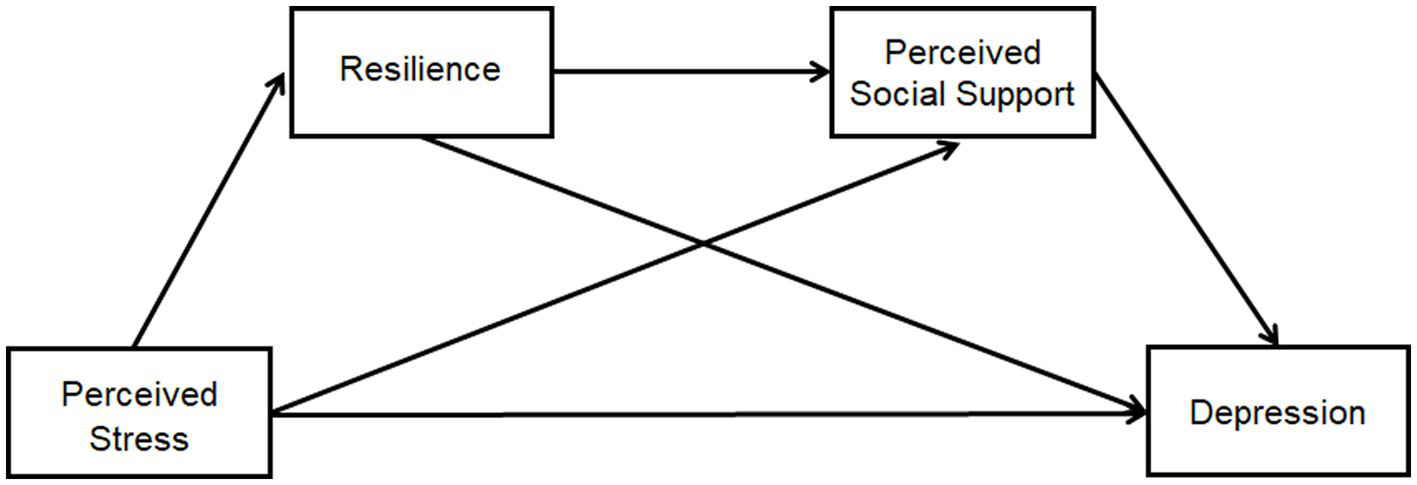
Conceptual chained mediation model. The prediction of a chain mediating model of resilience and perceived social support on the relationship between perceived stress and depression among patients with COVID-19 in Shanghai square-cabin hospitals.
3 Results
3.1 Descriptive analysis
A total of 888 patients with valid questionnaires in square-cabin hospitals in Shanghai were analyzed in this study, of whom there were 517 males (58.22%) and 371 were females (41.78%). All of them had tested positive for COVID-19 and received the corresponding treatment for COVID-19. Means, frequencies and standard deviations (SDs) were used to quantify the data. Patient variables were analyzed using the independent sample t-test for gender characteristic and using analysis of variance for age, education and job characteristics. There were differences in the questionnaire scores of the Perceived Stress Scale 10 (PSS-10), Patient Health Questionnaire 9 (PHQ-9), Perceived Social Support Scale (PSSS), and Connor-Davidson Resilience Scale10 (CD-RISC10) between the sexes. Women demonstrated higher scores in Perceived Stress and Patient Health Questionnaire 9 (Depression) compared to men, yet exhibited lower scores in Perceived Social Support and Resilience questionnaires. The age item showed differences in the Perceived Social Support Scale (PSSS) and the Resilience Scale. Participants aged 50–60 years reported higher scores on Perceived Social Support and Resilience Scales than other age groups. They also exhibited lower scores on Perceived Stress and Depression scales. The different levels of education exhibited differences in their scores on the Perceived Social Support Scale. Participants possessing higher educational attainments showed higher scores on the Perceived Stress Scale. However, the different kinds of job showed no significant differences on the four scales. The descriptive statistics for each variable are presented in Table 1.
Table 1
| Perceived stress | Perceived social support | Resilience | COVID-19 depression | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Categories | Fre | Mean | SD | Test | p | Effect size | Mean | SD | Test | p | Effect size | Mean | SD | Test | p | Effect size | Mean | SD | Test | p | Effect size |
| Gendera | Male | 517 | 14.25 | 7.999 | −3.775 | 0.000*** | 0.257c | 57.57 | 17.201 | 2.131 | 0.033* | 0.145c | 24.56 | 10.492 | 2.86 | 0.004** | 0.195c | 6.3 | 5.606 | −3.1 | 0.002** | 0.211c |
| Female | 371 | 16.28 | 7.835 | 55.04 | 17.716 | 22.54 | 10.271 | 7.5 | 5.769 | |||||||||||||
| Ageb | 18–30 | 302 | 15.18 | 7.252 | 0.503 | 0.734 | 0.002d | 54.66 | 16.934 | 3.363 | 0.010** | 0.015d | 22.63 | 9.933 | 3.184 | 0.013* | 0.014d | 6.87 | 5.596 | 0.485 | 0.747 | 0.002d |
| 31–40 | 238 | 15.56 | 7.934 | 56.42 | 17.21 | 23.44 | 10.423 | 6.95 | 5.392 | |||||||||||||
| 40–50 | 163 | 14.80 | 8.475 | 57.79 | 18.407 | 23.79 | 10.704 | 6.5 | 5.778 | |||||||||||||
| 50–60 | 130 | 14.42 | 8.610 | 60.67 | 16.658 | 26.48 | 10.260 | 6.47 | 6.041 | |||||||||||||
| >60 | 55 | 15.15 | 9.178 | 53.49 | 18.724 | 24.15 | 11.988 | 7.51 | 6.588 | |||||||||||||
| Educationb | Junior high school and below | 350 | 13.46 | 8.727 | 18.316 | 0.000*** | 0.040d | 56.03 | 18.511 | 0.664 | 0.515 | 0.001d | 23.6 | 10.814 | 0.29 | 0.749 | 0.001d | 6.66 | 5.961 | 0.356 | 0.701 | 0.001d |
| High school, technical school | 364 | 15.38 | 7.701 | 56.34 | 16.981 | 24.02 | 10.388 | 6.8 | 5.702 | |||||||||||||
| Bachelor degree or above | 174 | 17.81 | 6.02 | 57.85 | 16.222 | 23.33 | 9.819 | 7.1 | 5.164 | |||||||||||||
| Jobb | Freelance work | 239 | 14.72 | 8.452 | 1.676 | 0.138 | 0.009d | 56.30 | 17.131 | 0.34 | 0.889 | 0.002d | 24.32 | 10.46 | 0.89 | 0.487 | 0.005d | 6.86 | 6.047 | 0.192 | 0.966 | 0.001d |
| farmer | 4 | 15 | 6.218 | 53.75 | 10.308 | 24 | 6.164 | 7.5 | 1.732 | |||||||||||||
| staff | 428 | 14.78 | 7.816 | 56.13 | 17.748 | 23.59 | 9.936 | 6.67 | 5.388 | |||||||||||||
| manager | 86 | 17.2 | 7.877 | 58.55 | 18.538 | 21.74 | 11.558 | 7.29 | 6.056 | |||||||||||||
| student | 51 | 16.29 | 6.392 | 57.59 | 15.954 | 24.67 | 10.539 | 6.86 | 6.177 | |||||||||||||
| retire | 80 | 14.91 | 8.399 | 56.48 | 17.987 | 24.08 | 11.814 | 6.75 | 5.819 | |||||||||||||
The descriptive statistics of perceived stress, perceived social support, resilience, and depression among COVID-19 patients*.
*Fre, Frequency; Test, Test statistic; at test for independent group; bAnalysis of variance; cCohen’s d; deta-squared; p, p value; *p < 0.05, **p < 0.01, ***p < 0.001.
3.2 Pearson correlation analysis
To investigate the relationship between variables, we employed the Pearson correlation analysis. It showed a positive correlation between perceived stress and depression (r = 0.613, p < 0.01), indicating that higher perceived stress is associated with higher levels of depression. In contrast, the data showed that perceived social support and resilience scores were negatively correlated with depression (r = −0.521, p < 0.01; r = −0.527, p < 0.01). It showed that higher levels of perceived social support and resilience are associated with lower levels of depression. Furthermore, there was a negative correlation between perceived stress and perceived social support (r = −0.318, p < 0.01), resilience (r = −0.398, p < 0.01) which suggested that higher perceived stress is associated with lower levels of social support and resilience. Specific data are presented in Table 2.
Table 2
| Scores | Perceived stress | Perceived social support | Resilience | Depression | |
|---|---|---|---|---|---|
| (Mean ± SD) | |||||
| Perceived stress | 15.10 ± 7.99 | – | |||
| Perceived social support | 56.51 ± 17.453 | −0.318** | – | ||
| Resilience | 23.72 ± 10.443 | −0.398** | 0.460** | – | |
| Depression | 6.80 ± 5.702 | 0.613** | −0.521** | −0.527** | – |
Bivariate correlations among main study variables.
**p < 0.01.
3.3 Mediation effects analysis
Model 6 of the SPSS plug-in process provided by Hayes was used (Hayes and Preacher, 2014). Perceived stress symptoms were taken as the independent variable, depression as the dependent variable, resilience and perceived social support as chained mediating variables. The path coefficient results are shown in Figure 2.
Figure 2
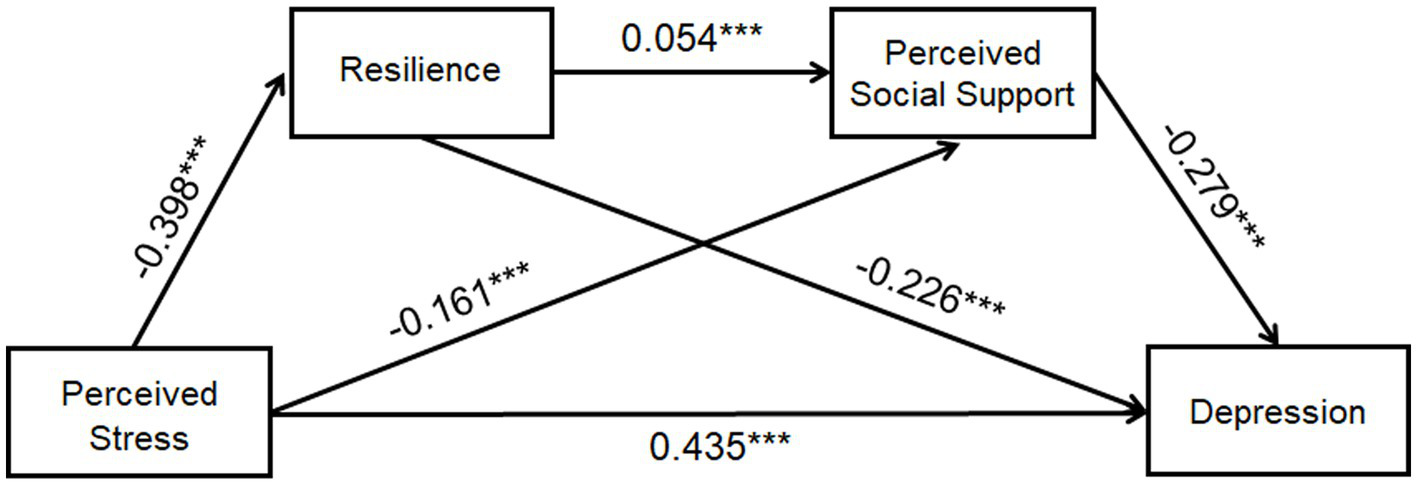
The path coefficient results of the chained mediation model between perceived stress, resilience, perceived social support and depression. Perceived stress can negatively predict resilience (β = −0.398) and perceived social support (β = −0.161), whereas positively predict depression (β = 0.435). Resilience and perceived social support were significant negative predictor of depression (β = −0.226, −0.279). Resilience was thought to be a significant positive predictor of perceived social support (β = 0.054). *p < 0.05, **p < 0.01, ***p < 0.001.
Table 3 lists the results of the multiple linear regression analysis of the major research variables. It also shows that perceived stress can significantly positively predict depression (β = 0.310, p < 0.001) and can significantly negatively predict resilience (β = −0.520, p < 0.001) and perceived social support (β = −0.352, p < 0.001). Resilience was thought to be a significant positive predictor of perceived social support (β = 0.661, p < 0.001) and a significant negative predictor of depression (β = −0.123, p < 0.001), while perceived social support was a significant negative predictor of depression (β = −0.091, p < 0.001).
Table 3
| Items | Regression equation | Integral fitting index | coefficient | Significance of regression coefficient | ||||
|---|---|---|---|---|---|---|---|---|
| Predictive variables | R | R 2 | F | β | standardization β | t | P | |
| Resilience | Perceived Stress | 0.398 | 0.158 | 166.554 | −0.520*** | −0.398 | −12.906 | 0.000 |
| Perceived Social Support | Perceived Stress | 0.483 | 0.233 | 134.475 | −0.352*** | −0.161 | −5.02 | 0.000 |
| Resilience | 0.661*** | 0.054 | 12.327 | 0.000 | ||||
| Depression | Perceived Stress | 0.729 | 0.531 | 333.525 | 0.310*** | 0.435 | 17.078 | 0.000 |
| Resilience | −0.123*** | −0.226 | −8.304 | 0.000 | ||||
| Perceived Social Support | −0.091*** | −0.279 | −10.602 | 0.000 | ||||
The relationship between perceived stress and depression: the chain mediating effect of perceived social support and resilience.
***p < 0.001.
The bootstrap test (Table 4) further showed that the 95% CI of the three paths did not include zero, indicating that the three indirect effects reached significance. Table 4 shows that the total effect of the relationship between perceived stress and depression was significant (effect = 0.4493, 95% CI: 0.0000, 0.4114). Meanwhile, the total indirect effect was significant (effect = 0.1328, 95% CI: 0.1013, 0.1703). The indirect effect was significant (effect = 0.0666, 95% CI: 0.0432, 0.0952) with resilience as the mediating variable. The indirect effect of the pathway with perceived social support as the mediating variable was significant (effect = 0.0354, 95% CI: 0.0163, 0.0603). The indirect effect of the pathway with resilience and perceived social support as mediating variables was also significant (effect = 0.0308, 95% CI: 0.0201, 0.0440).
Table 4
| Item | Effect size | Boot SE | Boot CI | Proportion of indirect effect | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Total effects | 0.4493 | 0.0193 | 0.0000 | 0.4114 | |
| Direct effect | 0.3165 | 0.0187 | 0.0000 | 0.2798 | |
| Total indirect effects | 0.1328 | 0.0176 | 0.1013 | 0.1703 | |
| Indp1: PS → RE → DE | 0.0666 | 0.0132 | 0.0432 | 0.0952 | 14.82% |
| Indp2: PS → PSS → DE | 0.0354 | 0.0111 | 0.0163 | 0.0603 | 7.87% |
| Indp3: PS → RE → PSS → DE | 0.0308 | 0.061 | 0.0201 | 0.0440 | 6.86% |
The mediating effect test of perceived social support and resilience*.
*Indp, indirect path; PS, perceived stress; RE, Resilience; PSS, perceived social support; DE, depression; CI, confidence interval.
4 Discussion
4.1 The chain mediating effects of resilience and perceived social support
The present study used a chained mediation model to investigate the relationship between perceived stress, resilience, perceived social support, and depressive symptoms among patients with COVID-19. This study found that perceived stress had a significant positive predictive effect on depression. Furthermore, the resilience and perceived social support had a chain mediating effect on the relationship between perceived stress and depression. The higher the level of perceived stress in COVID-19 patients, the lower their resilience level, which in turn led to lower perceived social support, thus led to higher depressive status. In the study, we found that perceived stress was a significant positive predictor of depression in COVID-19 patients, indicating that the higher the degree of perceived stress, the higher the level of depression, which is consistent with previous studies (Duan and Zhu, 2020; Damico et al., 2021). The relocation of COVID-19 patients to an isolated environment was a significant stressful event (Rauch et al., 2021), which can easily induce individual depression (Hammen, 2005). A stressor typically triggers a stress reaction if the stressor was perceived as a threat or demand, or the coping resources were perceived as insufficient for handling the given situation (Cohen et al., 1983). For COVID-19 patients, centralized isolation and treatment are required. Thus, they cannot go to work, seek support from loved ones and engage in their communities. Loneliness, fear of infection, suffering and death for oneself and for loved ones, grief after bereavement and financial worries have also all been cited as stressors leading to depression (Cottin et al., 2021). Hewitt and colleagues had highlighted the importance of perceived stress and coping resources in the prediction of stress-related symptoms (Hewitt et al., 1992). Therefore, it is necessary to recognize the negative influence of perceived stress on depression, and clarify the relationship between perceived stress and depression, which facilitates us to identify effective coping strategies to avoid mental health problems.
The results showed that perceived stress negatively predicted resilience, and resilience negatively predicted depression, which is consistent with other research results (Awano et al., 2020; Luceno-Moreno et al., 2020). Resilience had a mediating effect between perceived stress and depression, which verified the mediating path of resilience between perceived stress and depression. Resilience has been considered a personal characteristic that can help individuals preserve mental health in situations of severe stress or trauma (Connor, 2006; Poudel-Tandukar et al., 2019). It indicated better coping results in stressful situations (Burns et al., 2011). According to the stress buffer model of resilience (Richardson, 2002), the researchers found that resilience gradually varied with the way individuals cope with stress under stressful circumstances, and played an important role in the mitigation mechanism. Resilience can bring a positive transformation for individuals in adversity, greater threat, or trauma (Southwick and Charney, 2012). Some researchers have found that resilience minimized and buffered the negative influence of stress on mental health (Arrogante and Aparicio-Zaldivar, 2017). Furthermore, resilience was also considered as an index of mental health (Davydov et al., 2010). As a protective factor, resilience prompted individuals to change their original cognitive mode, mobilized personal resources, and coped with the stress flexibly, thus improving the mental health and reducing their depression level (Kalisch et al., 2017; Zhang et al., 2020; Kinser et al., 2021).
In addition, the results of the mediation analysis showed that perceived stress level significantly negatively predicted perceived social support, and perceived social support significantly negatively predicted depression level, indicating the mediating effect of perceived social support between perceived stress and depression. Perceived social support referred to an individual’s expectations, feelings and evaluation of social support situations (Wang et al., 1999). Social support referred to the support provided by family, friends and others as available to provide overall support (Xu et al., 2024). Research on relationships and health has pointed exclusively on the importance of supportive relationships in the context of stress or adversity (Cohen and Wills, 1985). Close relationships promoted well-being in many ways, not just as a resource in times of adversity. This can be explained by the following aspects. Firstly, when individuals faced stressful events, the perception of social support can produce positive mental states, including a sense of self-worth and a sense of security, which was beneficial to mental health and reduces the level of depression of individuals (Cohen, 2004). Secondly, perceived social support can also affect the regulation of the neuroendocrine response to stress and reduce the level of depression in individuals (Peng et al., 2022). Finally, the perception of social support can increase an individual’s sense of self-worth and self-control, generate positive evaluations of stressful events, and reduce their level of depression (Ozbay et al., 2007).
Moreover, this study found that perceived stress could have a significant influence on depression through the chain mediating effect of resilience and perceived social support, which verified the chain mediating path of resilience and perceived social support. This suggested that resilience not only acted as a single mediator between perceived stress and depression, but also further influenced depression by affecting perceived social support levels. The data showed that perceived social support was positively correlated with resilience, which is basically consistent with existing conclusions (Labrague and Santos, 2020). Feeney and Collins proposed an integrative model of thriving, in which perceived social support and resilience were thriving components (Feeney and Collins, 2015). This model pointed that perceived social support can provide emotional comfort and reassurance, convey understanding and acceptance, shield or defend the close other from negative forces related to the stressor, and benefit an individual’s ability to cope with stress, which is a catalyst for resilience.
Researchers have mostly regarded mental toughness as a process, that is, an individual’s ability to deal with adversity challenges, which has been proven to reduce the impact of traumatic events and the possibility of developing post-traumatic stress disorder (Lee et al., 2014). According to Kumpfer’s (1999) Resilience Framework, the selective perception was an internal mechanism that affected resilience. Some studies have pointed out that perceived social support (as a positive selective perception) was an important factor affecting resilience (Kalisch et al., 2015; Veer et al., 2021), which was based on the assumption that the belief that one can rely on others will make the potential stressors perceived as less threatening. Perceived social support can act as a protective factor against psychological resilience (Masten and Garmezy, 1985; Werner, 2004). Studies have suggested that perceived social support mediated the relationship between mental resilience and burden (Ong et al., 2018). Previous studies showed high levels of social support and resilience were protective factors against alcohol and drug abuse amongst the general public (Studer et al., 2017; Caravaca-Sánchez and García-Jarillo, 2020). According to the study, it is necessary to pay attention to the physical and mental conditions of COVD19 patients during clinical work. At the same time, the perceived social support of patients needs to be evaluated to improve resilience levels, thus reducing depression in COVID-19 patients with stress.
4.2 Limitations and future research
While this study has provided valuable insights, there are some limitations to this study as well. Firstly, the study was confined to a single hospital with a centralized COVID-19 patient management system. This may introduce bias as management systems and work schedules at other hospitals could potentially influence the variables. To validate the findings, future studies should extend their scope to multiple regions and hospitals. Secondly, the research was limited to perceived stress and depression among COVID-19 patients, ignoring other mental health outcomes such as anxiety. Nevertheless, we postulate that the relationships uncovered in this study likely extend to other conditions.
5 Conclusion
Based on the above, the present model shows that perceived stress influences depression through the independent and combined effects of two mediating variables, namely perceived social support and resilience, which further explains the mechanism of the influence of perceived stress on depression, as well as provides new perspectives for the relationship between the perceived stress and depression for COVID-19 patients. In the future, when suffering public health crises such as pandemics, we could attempt to mobilize individuals’ positive psychological traits to improve their mental health in clinical practice. This finding confirms and extends the protective effect of perceived social support and resilience that are being assessed in populations of adults confronted with the epidemic crisis situations.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of the First Affiliated Hospital of the Air Force Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LW: Writing – original draft, Conceptualization, Data curation, Formal analysis, Methodology. JY: Writing – original draft, Formal analysis, Software, Validation. XD: Investigation, Software, Writing – review & editing. YZ: Data curation, Writing – review & editing. YM: Conceptualization, Formal analysis, Funding acquisition, Validation, Writing – review & editing. WH: Funding acquisition, Project administration, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Aviation Medicine Project of Air Force Military Medical University (No.2020ZTE03) and Natural Science Foundation Youth Project of Shaanxi Province (No.2023-JC-QN-0816).
Acknowledgments
We would like to express our gratitude to all the COVID-19 patients who bravely confronted the virus and participated in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1
Alsubaie M. Stain H. J. Webster L. A. D. Wadman R. (2019). The role of sources of social support on depression and quality of life for university students. Int. J. Adolesc. Youth24, 484–496. doi: 10.1080/02673843.2019.1568887
2
Arrogante O. Aparicio-Zaldivar E. (2017). Burnout and health among critical care professionals: the mediational role of resilience. Intensive Crit. Care Nurs.42, 110–115. doi: 10.1016/j.iccn.2017.04.010
3
Awano N. Oyama N. Akiyama K. Inomata M. Kuse N. Tone M. et al . (2020). Anxiety, depression, and resilience of healthcare Workers in Japan during the coronavirus disease 2019 outbreak. Intern. Med.59, 2693–2699. doi: 10.2169/internalmedicine.5694-20
4
Banjongrewadee M. Wongpakaran N. Wongpakaran T. Pipanmekaporn T. Punjasawadwong Y. Mueankwan S. (2020). The role of perceived stress and cognitive function on the relationship between neuroticism and depression among the elderly: a structural equation model approach. BMC Psychiatry20:25. doi: 10.1186/s12888-020-2440-9
5
Benedek D. M. Fullerton C. Ursano R. J. (2007). First responders: mental health consequences of natural and human-made disasters for public health and public safety workers. Annu. Rev. Public Health28, 55–68. doi: 10.1146/annurev.publhealth.28.021406.144037
6
Besharart M. A. Khadem H. Zarei V. Momtaz A. (2020). Mediating role of perceived stress in the relationship between facing existential issues and symptoms of depression and anxiety. Iran. J. Psychiatry15, 80–87.
7
Bloom D. E. Black S. Rappuoli R. (2017). Emerging infectious diseases: a proactive approach. Proc. Natl. Acad. Sci. USA114, 4055–4059. doi: 10.1073/pnas.1701410114
8
Burns R. A. Anstey K. J. Windsor T. D. (2011). Subjective well-being mediates the effects of resilience and mastery on depression and anxiety in a large community sample of young and middle-aged adults. Austr. New Zealand J. Psychiatry45, 240–248. doi: 10.3109/00048674.2010.529604
9
Campbell-Sills L. Stein M. B. (2007). Psychometric analysis and refinement of the Connor-davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J. Trauma. Stress.20, 1019–1028. doi: 10.1002/jts.20271
10
Caravaca-Sánchez F. García-Jarillo M. (2020). Perceived social support, resilience and consumption of psychoactive substances amongst inmates in prisons. Rev. Española Sanidad Penitenciaria22, 75–79. doi: 10.18176/resp.00013
11
Cha E. J. Jeon H. J. Chung S. (2022). Central symptoms of insomnia in relation to depression and COVID-19 anxiety in general population: a network analysis. J. Clin. Med.11:3416. doi: 10.3390/jcm11123416
12
Chan M. H. Lee A. T. C. (2022). Perceived social support and depression among occupational therapists in Hong Kong during COVID-19 pandemic. East Asian Arch. Psychiatr.32, 17–21. doi: 10.12809/eaap2205
13
Chen M. (2019). A study on the relationship between resilience and social support and disease perception among young and middle-aged patients with type2 diabetes. Nanchang: Nanchang University.
14
Chen S. Bonanno G. A. (2020). Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol. Trauma12, S51–s54. doi: 10.1037/tra0000685
15
Cohen S. (2004). Social relationships and health. Am. Psychol.59, 676–684. doi: 10.1037/0003-066X.59.8.676
16
Cohen S. Kamarck T. Mermelstein R. (1983). A global measure of perceived stress. J. Health Soc. Behav.24, 385–396. doi: 10.2307/2136404
17
Cohen S. Wills T. A. (1985). Stress, social support, and the buffering hypothesis. Psychol. Bull.98, 310–357. doi: 10.1037/0033-2909.98.2.310
18
Connor K. M. (2006). Assessment of resilience in the aftermath of trauma. J. Clin. Psychiatry67 Suppl 2, 46–49
19
Cottin M. Hernández C. Núñez C. Labbé N. Quevedo Y. Davanzo A. et al . (2021). “What if we get sick?”: Spanish adaptation and validation of the fear of illness and virus evaluation scale in a non-clinical sample exposed to the COVID-19 pandemic. Front. Psychol.12:590283. doi: 10.3389/fpsyg.2021.590283
20
Damian F. S. Ana M. M. H. Jamileh S. Peng Z. Charlie A. David M. P. et al . (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet398, 1700–1712. doi: 10.1016/S0140-6736(21)02143-7
21
Damico V. Murano L. Teli M. Margosio V. Ripamonti C. Nattino G. (2021). Prevalence of post traumatic stress disorder, anxiety and depression among COVID-19 survivors 1 year after intensive care discharge. Prof. Inferm.74:264. doi: 10.7429/pi.2021.744264a
22
Davydov D. M. Stewart R. Ritchie K. Chaudieu I. (2010). Resilience and mental health. Clin. Psychol. Rev.30, 479–495. doi: 10.1016/j.cpr.2010.03.003
23
Du J. Wu C. Zheng W. K. Cui S. N. Li L. Liu Z. et al . (2024). Insomnia and anxiety among COVID-19 patients in China: the chain mediating effect of psychological capital and self-esteem. BMC Nurs.23:221. doi: 10.1186/s12912-023-01563-8
24
Duan L. Zhu G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry7, 300–302. doi: 10.1016/S2215-0366(20)30073-0
25
Dulaney E. S. Graupmann V. Grant K. E. Adam E. K. Chen E. (2008). Taking on the stress-depression link: meaning as a resource in adolescence. J. Adolesc.65, 39–49. doi: 10.1016/j.adolescence.2018.02.011
26
Dymecka J. Gerymski R. Machnik-Czerwik A. (2022). How does stress affect life satisfaction during the COVID-19 pandemic? Moderated mediation analysis of sense of coherence and fear of coronavirus. Psychol. Health Med.27, 280–288. doi: 10.1080/13548506.2021.1906436
27
Feeney B. C. Collins N. L. (2015). A new look at social support: a theoretical perspective on thriving through relationships. Personal. Soc. Psychol. Rev.19, 113–147. doi: 10.1177/1088868314544222
28
Fu Y. Sun Y. Zhang C. Li Q. (2022). A survey of mental health and influencing factors of COVID-19 patients in fangcang shelter hospitals in Shanghai. J. Tongji Univ.43, 303–309. doi: 10.12289/j.issn.1008-0392.22173
29
Fu H. Wang B. (2022). The effect of risk perception on anxiety in emerging adulthood under the local outbreak of COVID-19: a conditional process analysis. Front. Psychol.13:759510. doi: 10.3389/fpsyg.2022.759510
30
Grey I. Arora T. Thomas J. Saneh A. Tohme P. Abi-Habib R. (2020). The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res.293:113452. doi: 10.1016/j.psychres.2020.113452
31
Hammen C. (2005). Stress and depression. Annu. Rev. Clin. Psychol.1, 293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938
32
Hayes A. F. (2015). An index and test of linear moderated mediation. Multivariate Behav. Res.50, 1–22. doi: 10.1080/00273171.2014.962683
33
Hayes A. F. Preacher K. J. (2014). Statistical mediation analysis with a multi-categorical independent variable. Br J Math Stat Psychol.67, 451–470. doi: 10.1111/bmsp.12028
34
Hewitt P. L. Flett G. L. Mosher S. W. (1992). The perceived stress scale: factor structure and relation to depression symptoms in a psychiatric sample. J. Psychopathol. Behav. Assess.14, 247–257. doi: 10.1007/BF00962631
35
Hu J. Huang Y. Liu J. Zheng Z. Xu X. Zhou Y. et al . (2022). COVID-19 related stress and mental health outcomes 1 year after the peak of the pandemic outbreak in China: the mediating effect of resilience and social support. Front. Psych.13:828379. doi: 10.3389/fpsyt.2022.828379
36
Hu J. Ye B. Yildirim M. Yang Q. (2023). Perceived stress and life satisfaction during COVID-19 pandemic: the mediating role of social adaptation and the moderating role of emotional resilience. Psychol. Health Med.28, 124–130. doi: 10.1080/13548506.2022.2038385
37
Hyde L. W. Gorka A. Manuck S. B. Hariri A. R. (2011). Perceived social support moderates the link between threat-related amygdala reactivity and trait anxiety. Neuropsychologia49, 651–656. doi: 10.1016/j.neuropsychologia.2010.08.025
38
Kalisch R. Baker D. G. Basten U. Boks M. P. Bonanno G. A. Brummelman E. et al . (2017). The resilience framework as a strategy to combat stress-related disorders. Nat Hum Behav.1, 784–790. doi: 10.1038/s41562-017-0200-8
39
Kalisch R. Müller M. B. Tüscher O. (2015). A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci.38:e92. doi: 10.1017/s0140525x1400082x
40
Kinser P. A. Jallo N. Amstadter A. B. Thacker L. R. Jones E. Moyer S. et al . (2021). Depression, anxiety, resilience, and coping: the experience of pregnant and new mothers during the first few months of the covid-19 pandemic. J Womens Health (Larchmt).30, 654–664. doi: 10.1089/jwh.2020.8866
41
Kumpfer K. L. (1999). Factors and processes contributing to resilience: The resilience framework. New York: Kluwer Academic Publishers.
42
Labrague L. J. Hammad K. Gloe D. S. McEnroe-Petitte D. M. Fronda D. C. Obeidat A. A. et al . (2018). Disaster preparedness among nurses: a systematic review of literature. Int. Nurs. Rev.65, 41–53. doi: 10.1111/inr.12369
43
Labrague L. J. Santos J. A. A. (2020). COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J. Nurs. Manag.28, 1653–1661. doi: 10.1111/jonm.13121
44
Lathabhavan R. Vispute S. (2022). Examining the mediating effects of stress on fear of COVID-19 and well-being using structural equation modeling. Int. J. Ment. Heal. Addict.20, 2681–2689. doi: 10.1007/s11469-021-00541-y
45
Lee J. S. Ahn Y. S. Jeong K. S. Chae J. H. Choi K. S. (2014). Resilience buffers the impact of traumatic events on the development of PTSD symptoms in firefighters. J. Affect. Disord.162, 128–133. doi: 10.1016/j.jad.2014.02.031
46
Lee S. Crockett M. S. (1994). Effect of assertiveness training on levels of stress and assertiveness experienced by nurses in Taiwan, republic of China. Issues Ment. Health Nurs.15, 419–432. doi: 10.3109/01612849409006918
47
Li Z. Ge J. Yang M. Feng J. Qiao M. Jiang R. et al . (2020). Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun.88, 916–919. doi: 10.1016/j.bbi.2020.03.007
48
Li J. Liu X. Xu L. Jin Z. (2020). Current status of demoralization and its relationship with medical coping style, self-efficacy and perceived social support in Chinese breast cancer patients. Eur. J. Psychiatry34, 211–218. doi: 10.1016/j.ejpsy.2020.06.007
49
Liu C. H. Zhang E. Wong G. T. F. Hyun S. Hahm H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res.290:113172. doi: 10.1016/j.psychres.2020.113172
50
Liu J. Zhu Q. Fan W. Makamure J. Zheng C. Wang J. (2020). Online mental health survey in a medical College in China during the COVID-19 outbreak. Front. Psych.11:459. doi: 10.3389/fpsyt.2020.00459
51
Lu X. Xie Y. Feng H. Liu Z. Ouyang K. Hou B. et al . (2021). Psychological impact on COVID-19 patients during the outbreak in China: a case-control study. Psychiatry Res.305:114180. doi: 10.1016/j.psychres.2021.114180
52
Lu H. Yang J. Zhao K. Jin Z. Wen X. Hu N. et al . (2024). Perceived risk of COVID-19 hurts mental health: The mediating role of fear of COVID-19 and the moderating role of resilience. BMC Psychiatry.24:58. doi: 10.1186/s12888-024-05511-x
53
Luceno-Moreno L. Talavera-Velasco B. Garcia-Albuerne Y. Martin-Garcia J. (2020). Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health17:5514. doi: 10.3390/ijerph17155514
54
Luthar S. S. Cicchetti D. Becker B. (2000). The construct of resilience: a critical evaluation and guidelines for future work. Child Dev.71, 543–562. doi: 10.1111/1467-8624.00164
55
Lyu M. Xi J. Luo Y. (2017). Daily emotional characteristics in individuals with different resilience levels: supplementary evidence from experience-sampling method (ESM). Acta Psychol. Sin.49:928. doi: 10.3724/SP.J.1041.2017.00928
56
Malinauskas R. Malinauskiene V. (2022). Meta-analysis of psychological interventions for reducing stress, anxiety, and depression among university students during the COVID-19 pandemic. Int. J. Environ. Res. Public Health19:9199. doi: 10.3390/ijerph19159199
57
Masten A. S. Garmezy N. J. S. U. (1985). Risk, vulnerability, and protective factors in developmental psychopathology. Berlin: Springer Group.
58
Matalon N. Dorman-Ilan S. Hasson-Ohayon I. Hertz-Palmor N. Shani S. Basel D. et al . (2021). Trajectories of post-traumatic stress symptoms, anxiety, and depression in hospitalized COVID-19 patients: a one-month follow-up. J. Psychosom. Res.143:110399. doi: 10.1016/j.jpsychores.2021.110399
59
Ong H. L. Vaingankar J. A. Abdin E. Sambasivam R. Fauziana R. Tan M. E. et al . (2018). Resilience and burden in caregivers of older adults: moderating and mediating effects of perceived social support. BMC Psychiatry18:27. doi: 10.1186/s12888-018-1616-z
60
Ozbay F. Johnson D. C. Dimoulas E. Morgan C. A. Charney D. Southwick S. (2007). Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry4, 35–40
61
Peng L. Ye Y. Wang L. Qiu W. Huang S. Wang L. et al . (2022). Chain mediation model of perceived stress, resilience, and social support on coping styles of Chinese patients on hemodialysis during COVID-19 pandemic lockdown. Med. Sci. Monit.28:e935300. doi: 10.12659/MSM.935300
62
Podsakoff P. M. MacKenzie S. B. Lee J. Y. Podsakoff N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol.88, 879–903. doi: 10.1037/0021-9010.88.5.879
63
Podsakoff P. M. Management D. W. (1986). Self-reports in organizational research: problems and prospects. J. Manag.12, 531–544. doi: 10.1177/014920638601200408
64
Poudel-Tandukar K. Chandler G. E. Jacelon C. S. Gautam B. Bertone-Johnson E. R. Hollon S. D. (2019). Resilience and anxiety or depression among resettled Bhutanese adults in the United States. Int. J. Soc. Psychiatry65, 496–506. doi: 10.1177/0020764019862312
65
Preacher K. J. Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods40, 879–891. doi: 10.3758/brm.40.3.879
66
Rauch S. A. M. Simon N. M. Rothbaum B. O. (2021). Rising tide: responding to the mental health impact of the COVID-19 pandemic. Focus19, 243–246. doi: 10.1176/appi.focus.19204
67
Richardson G. E. (2002). The metatheory of resilience and resiliency. J. Clin. Psychol.58, 307–321. doi: 10.1002/jclp.10020
68
Robinson E. Sutin A. R. Daly M. Jones A. (2022). A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord.296, 567–576. doi: 10.1016/j.jad.2021.09.098
69
Santini Z. I. Koyanagi A. Tyrovolas S. Mason C. Haro J. M. (2015). The association between social relationships and depression: a systematic review. J. Affect. Disord.175, 53–65. doi: 10.1016/j.jad.2014.12.049
70
Southwick S. M. Charney D. S. (2012). The science of resilience: implications for the prevention and treatment of depression. Science338, 79–82. doi: 10.1126/science.1222942
71
Spada M. M. Nikcevic A. V. Moneta G. B. Wells A. (2008). Metacognition, perceived stress, and negative emotion. Personal. Individ. Differ.44, 1172–1181. doi: 10.1016/j.paid.2007.11.010
72
Spitzer R. L. (1999). Validation and utility of a self-report version of PRIME-MDThe PHQ primary care study. JAMA282, 1737–1744. doi: 10.1001/jama.282.18.1737
73
Studer J. Baggio S. Dupuis M. Mohler-Kuo M. Daeppen J.-B. Gmel G. (2017). Substance use in young Swiss men: the interplay of perceived social support and dispositional characteristics. Subst. Use Misuse52, 798–810. doi: 10.1080/10826084.2016.1264966
74
Sun Y. Gao L. Kan Y. Shi B-X. (2019). The perceived stress scale-10 (pss-10) is reliable and has construct validity in chinese patients with systemic lupus erythematosus. Lupus.28, 149–155. doi: 10.1177/0961203318815595
75
Veer I. M. Riepenhausen A. Zerban M. Wackerhagen C. Puhlmann L. M. C. Engen H. et al . (2021). Psycho-social factors associated with mental resilience in the Corona lockdown. Transl. Psychiatry11:67. doi: 10.1038/s41398-020-01150-4
76
Vindegaard N. Benros M. E. (2020). COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun.89, 531–542. doi: 10.1016/j.bbi.2020.05.048
77
Wang X. D. Wang X. L. Ma H. (1999). Rating scales for mental health. Beijing: Chinese Mental Health Journal Press.
78
Wen X. Zhao C. Y. Kishimoto T. Qian M. Y. (2020). Effect of perceived social support on the efficacy of online cognitive behavioral therapy for social anxiety disorder. Acta Sci. Nat. Univ. Pekin.56, 571–578. doi: 10.13209/j.0479-8023.2020.025
79
Werner E. E. (2004). Journeys from childhood to midlife: risk, resilience, and recovery. Pediatrics114:492. doi: 10.1542/peds.114.2.492a
80
Wilks S. E. Croom B. (2008). Perceived stress and resilience in Alzheimer's disease caregivers: testing moderation and mediation models of social support. Aging Ment. Health12, 357–365. doi: 10.1080/13607860801933323
81
Xu L. Gao Y. Shi D. Wang Y. Li R. Cai Y. (2024). Social support moderates the relationship between sleep quality and mental health: a Chinese Fangcang shelter hospital-based study in asymptomatic COVID-19 carriers. Heliyon10:e31782. doi: 10.1016/j.heliyon.2024.e31782
82
Yan L. Gan Y. Ding X. Wu J. Duan H. (2021). The relationship between perceived stress and emotional distress during the COVID-19 outbreak: Effects of boredom proneness and coping style. J. Anxiety Disorders.77:102328. doi: 10.1016/j.janxdis.2020.102328
83
Yu X. Tam W. W. S. Wong P. T. K. Lam T. H. Stewart S. M. (2012). The patient health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr. Psychiatry53, 95–102. doi: 10.1016/j.comppsych.2010.11.002
84
Zhang J. Yang Z. Wang X. Li J. Dong L. Wang F. et al . (2020). The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J. Clin. Nurs.29, 4020–4029. doi: 10.1111/jocn.15425
85
Zhao Z. Guo J. Zhou J. Qiao J. Yue S. Ouyang Y. Q. et al . (2023). Perceived social support and professional identity in nursing students during the COVID-19 pandemic era: the mediating effects of self-efficacy and the moderating role of anxiety. BMC Med. Educ.23:117. doi: 10.1186/s12909-022-03968-6
86
Zhao Y. J. Xing X. Tian T. Wang Q. Liang S. Wang Z. et al . (2022). Post COVID-19 mental health symptoms and quality of life among COVID-19 frontline clinicians: a comparative study using propensity score matching approach. Transl. Psychiatry12:376. doi: 10.1038/s41398-022-02089-4
87
Zimet G. D. Dahlem N. W. Zimet S. G. Farley G. K. (1988). The multidimensional scale of perceived social support. J. Pers. Assess.52, 30–41. doi: 10.1207/s15327752jpa5201_2
Summary
Keywords
resilience, depression, perceived social support, perceived stress, COVID-19 patients, chain mediating effect
Citation
Wang L, Yu J, Diao X, Zhang Y, Miao Y and He W (2024) The chain mediating effects of resilience and perceived social support in the relationship between perceived stress and depression in patients with COVID-19. Front. Psychol. 15:1400267. doi: 10.3389/fpsyg.2024.1400267
Received
18 March 2024
Accepted
09 August 2024
Published
29 August 2024
Volume
15 - 2024
Edited by
Satja Mulej Bratec, University of Maribor, Slovenia
Reviewed by
Diana Carolina Oviedo, Catholic University Santa Maria La Antigua, Panama
Huangqi Jiang, Case Western Reserve University, United States
Updates
Copyright
© 2024 Wang, Yu, Diao, Zhang, Miao and He.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei He, afmmuhw@163.comYe Miao, 85913036@qq.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.