- 1Department of Renal Transplant Surgery, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
- 2Institute of Inflammation and Ageing, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
- 3Department of Research and Innovation, Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
- 4Institute of Immunology and Immunotherapy, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
- 5Department of Inflammation and Ageing, NIHR Birmingham Biomedical Research Centre, Birmingham, United Kingdom
Background: Given the increasing age and frailty of kidney transplant candidates, there is an emerging drive to optimise patients before transplantation. Lack of exercise has been linked with poor outcomes at all stages of the transplant pathway. The aim of this study was to evaluate the attitudes and perception to exercise in such patients and assess how these practises vary by demographics.
Methods: A single-centre, prospective, survey-based study was conducted on consecutive adult patients being assessed for activation on the deceased-donor kidney transplant waiting list.
Results: A total of 103 patients (65% male; 56% White ethnicity; mean age: 47.8 years) completed the survey. Of these, 42% were on haemodialysis and 24% on peritoneal dialysis. Most patients agreed/strongly agreed that exercise was important (86%) and that they would be willing to do so to optimise their health (97%). Despite this, only 56% of patients reported exercising on a regular basis. Most patients stated that they would be willing to wear exercise monitoring devices (81%). Younger (Spearman's rho: 0.20, p = 0.047) and Black/Asian ethnicity (p = 0.038) patients reported performing significantly less exercise activity than their older and White counterparts.
Conclusion: Whilst kidney transplant candidates have generally positive attitudes toward exercise, only around half of those surveyed reported exercising regularly. The findings of this study, including differences across age and ethnicity, would be useful to consider when designing patient-centred prehabilitation interventions to encourage exercise in this cohort.
Introduction
Chronic kidney disease (CKD) is a growing public health emergency, due to an ageing and more co-morbid population (1). These factors are contributing to an increasing burden of physical frailty in patients awaiting kidney transplantation, which remains the optimal intervention for end-stage kidney disease (ESKD) (2). Recent UK data has demonstrated that 35%–40% of kidney transplant candidates are either frail or “vulnerable” to frailty (3). Frailty is an age-related, sustained loss in physiological reserve, which is further compounded in kidney transplant candidates by underlying disease progression, associated comorbidities and adverse effects of dialysis (4). At all ages, ESKD patients are more susceptible to developing frailty when compared to the general population (5, 6). The presence of frailty is now well-recognised as impacting on all aspects of kidney transplantation, resulting in a lower likelihood of receiving a kidney transplant, either due to waiting list mortality or being removed from the waiting list, as well as poorer post-transplant patient and graft survival (5, 7).
Studies have shown that frailty and overall health status can be improved through exercise and increased physical activity (8, 9). There is a growing realisation in the transplant community that this form of intervention should be delivered through personalised prehabilitation programs, and this remains an area of active interest (10, 11). The relatively long waiting-list period (averaging two years in the UK) for a suitable kidney graft provides a window of opportunity to deliver prehabilitation (12). An international working group from the European Society for Organ Transplantation (ESOT) recently published a consensus document stating the increasing importance of research into various aspects of prehabilitation programs (13).
Attitudes to, and perceptions of exercise in kidney transplant candidates are poorly understood, particularly in the context of varying demographics such as age and ethnicity. Available evidence is based on the wider population of CKD patients, which is a heterogenous group, with not all being eligible for transplantation (14, 15). Kidney transplant candidates are a select group and an understanding of their unique views and circumstances is paramount in designing future clinical trials, ensuring sustained engagement and achieving positive outcomes. Recruitment, retention, and protocol adherence in exercise trials tend to be poor, suggesting that trial design may not resonate with patients (16). In addition, whilst the use of advanced monitoring and exercise techniques, such as wearable accelerometers and resistance exercises, respectively, have shown some benefit, patient's attitudes to these remain poorly explored.
The aim of this study was to collect data to inform the exercise intervention component of a future prehabilitation trial in patients on the waiting list for a deceased donor kidney transplant. The primary objective was to assess patients' attitudes to three components related to exercise at the time of entry to the kidney transplant waiting list, namely willingness to exercise, current activity levels, and barriers to exercise. The secondary objective was to identify associations between clinical features (e.g., age, ethnicity, gender, and type of dialysis) and both levels of physical activity and willingness to exercise.
Methods
Study overview
A single-centre, prospective, survey-based study was performed on adult patients listed for deceased donor kidney transplantation at a high-volume renal transplant centre. Patients were approached at the time of their assessment for activation on the deceased donor transplant waiting list and provided with a patient information sheet and a survey. The patient information sheet stated that participation was optional, and neither the choice to participate nor the answers given would have any influence on treatment; patients were deemed to give consent by completing the survey. The study was registered as an audit and quality improvement project at our institution (CARMS18907).
Eligibility
All adult patients (age 18 or above) listed for deceased donor kidney transplantation between February and September 2023 were eligible for inclusion in the study. Non-English-speaking patients were assisted to complete the survey by their next of kin, interpreter or the transplant co-ordinator in clinic.
Data collection
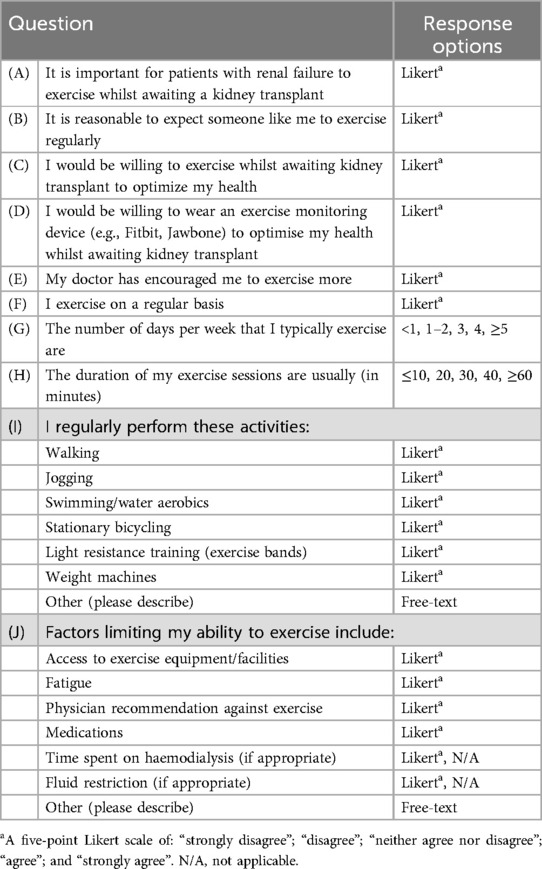
The survey was based on one used in a previous study of patients listed for liver transplantation, and was adapted for use in patients with ESKD (14). It comprised five-point Likert scale questions, to assess patients' attitudes towards exercise; the type and duration of exercise performed; and barriers to performing exercise (see Table 1). The response options for the Likert scale questions relating to agreement were assigned values between 1 = strongly disagree and 5 = strongly agree for analysis, such that higher scores were indicative of greater agreement with the statement.
Patient demographic data [age, body mass index (BMI), gender and ethnicity], comorbidities (hypertension, ischemic heart disease, diabetes mellitus, and smoking status), and the current type of dialysis were obtained from individual patient case notes.
Statistical methods
The Likert scale questions were treated as ordinal for analysis and compared across nominal variables using Mann–Whitney U or Kruskal–Wallis tests for factors with two, or more than two categories, respectively. Associations with ordinal or continuous variables were assessed using Spearman's rank correlation coefficients (rho) and the associated p-values. All analyses were performed using IBM SPSS 24 (IBM Corp. Armonk, NY), with p < 0.05 deemed to be indicative of statistical significance throughout. Cases with missing data, either due to patients not giving a response or where a question was not applicable, were excluded from the analysis of the affected question. Continuous variables were summarised as “mean ± standard deviation” where approximately normally distributed, or as “median (interquartile range)” otherwise.
Results
Patient population
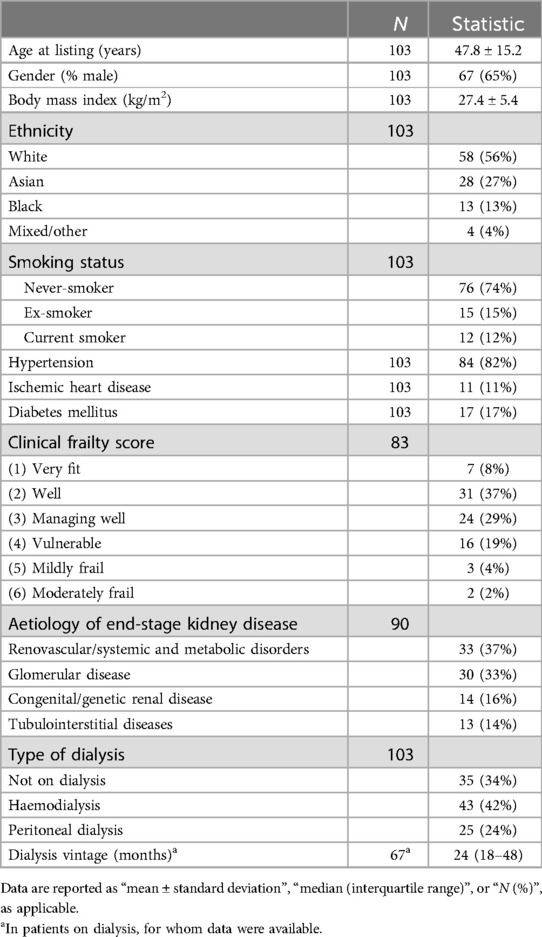
A total of 105 surveys were issued and returned during the study period. Of these, the surveys from two participants were discarded due to lack of completion of the survey, resulting in a total sample size of 103 (98% response rate). The 103 patients who completed the survey had a mean age at listing of 47.8 years, with 65% being male and 56% of White ethnicity. These demographics are in keeping with gender and ethnic variation seen in our regional CKD population (17). The majority had hypertension (82%), with 42% being on haemodialysis and 24% on peritoneal dialysis (PD). The remaining 34% of patients were pre-dialysis, with an estimated glomerular filtration rate (eGFR) < 15 ml/min/1.73 m2, who were pre-emptively listed for a deceased-donor transplantation. Further details of the cohort are reported in Table 2.
Exercise attitudes and behaviour
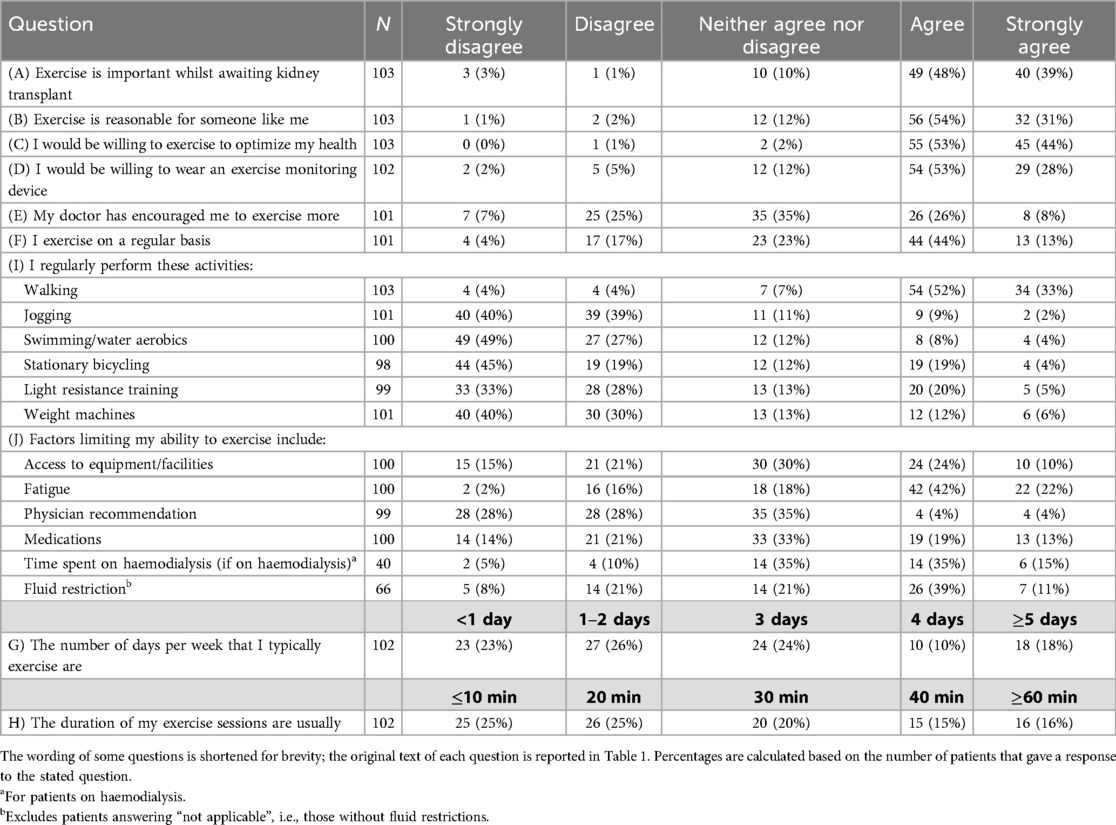
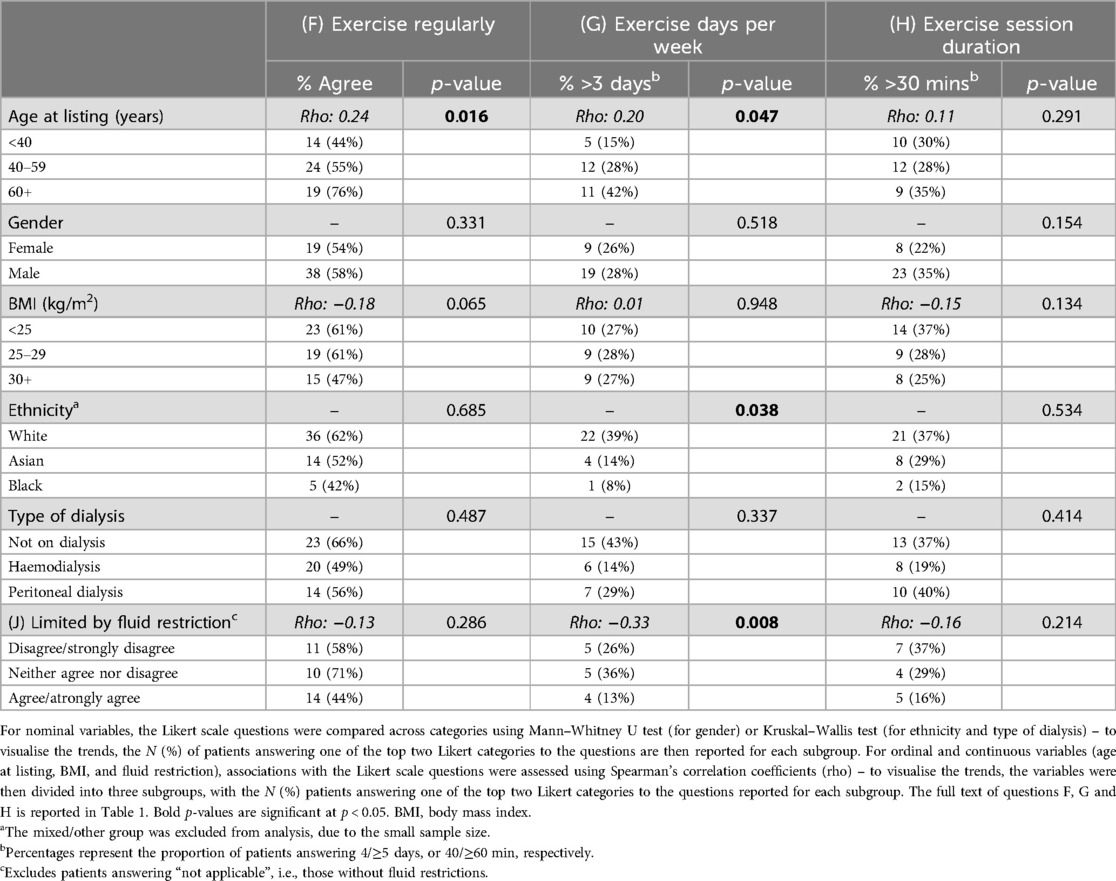
Survey responses are reported in Table 3 and visualised in Figure 1. Most patients agreed/strongly agreed that exercise was important whilst awaiting a kidney transplant (86%); that it would be reasonable to expect them to exercise regularly (85%); and that they would be willing to do so to optimise their health (97%). However, despite this, only 56% of patients agreed/strongly agreed that they currently exercised on a regular basis, with the average amount of exercise being approximately two sessions of 20 min per week.
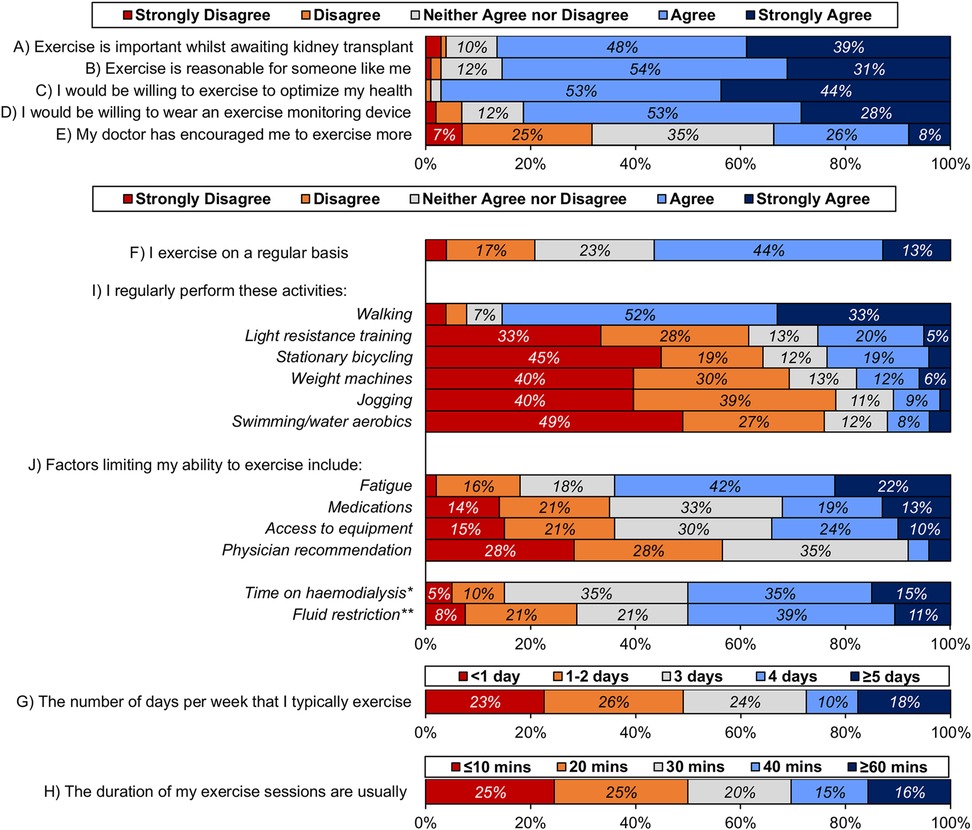
Figure 1. Responses to Likert-scale questions. The wording of some questions is shortened for brevity; the original text of each question is reported in Table 1. Percentages are calculated based on the number of patients that gave a response to the stated question, as reported in Table 3. For questions I) and J), the activities/factors are sorted in descending order, based on the mean response. Unlabelled bars have a frequency of <5%. *For patients on haemodialysis. **Excludes patients answering “not applicable”, i.e., those without fluid restrictions.
By far the most common exercise activity was walking, with 85% of patients agreeing/strongly agreeing that this was performed on a regular basis, this was followed by light resistance training (25%) and stationary bicycling (23%). Free-text responses listing activities not already included in the survey were given by seven patients; these included yoga/Pilates (N = 3) and sports (badminton/cricket; N = 2). Fewer participants engaged in exercises of increasing intensity.
Fatigue was the most common factor limiting patients' ability to exercise (agree/strongly agree: 64%); time spent on haemodialysis (50%) and fluid restriction (50%) were also major barriers to exercise for the subgroups of patients for whom these were applicable. Only 34% of patients reported that they had been encouraged to do more exercise by their doctor. The majority of patients stated that they would be willing to wear exercise monitoring devices (agree/strongly agree: 81%).
Associations between patient factors and exercise attitudes and behaviour
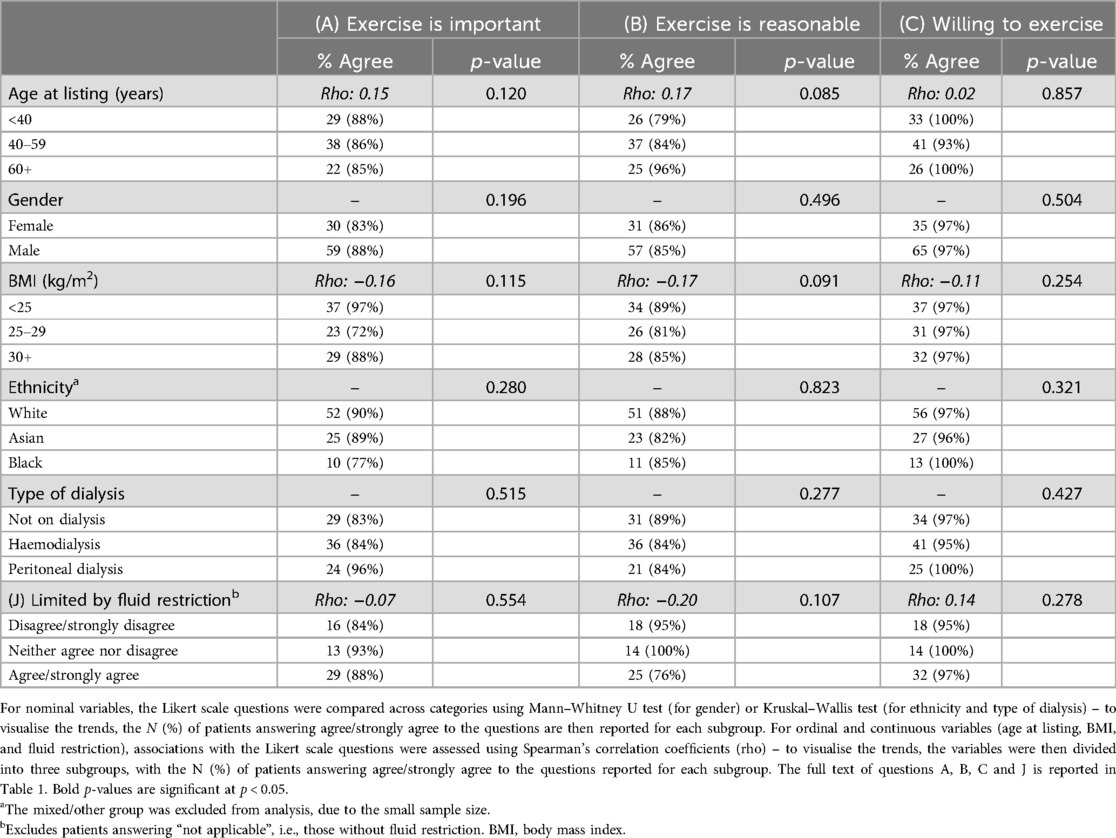
None of the patient characteristics considered were found to be significantly associated with views on the importance or reasonableness of exercise, or with willingness to exercise (Table 4A). However, significant associations with the amount of exercise reported by patients were observed (Table 4B; Figure 2). Specifically, older patients tended to perform greater amounts of exercise, with the proportion of patients reporting that they exercise regularly increasing from 44% in those aged <40 years to 76% in those aged 60+ years (rho: 0.24, p = 0.016) and a corresponding increase in those reporting exercising on more than three days per week (15% vs. 42%, rho: 0.20, p = 0.047). A significant difference across subgroups of ethnicity was also observed, with 39% of White patients exercising on more than three days per week, compared to 14% of Asian and 8% of Black patients (p = 0.038). Neither gender, BMI, nor type of dialysis were found to be significantly associated with the views on exercise, or the amount of exercise performed.
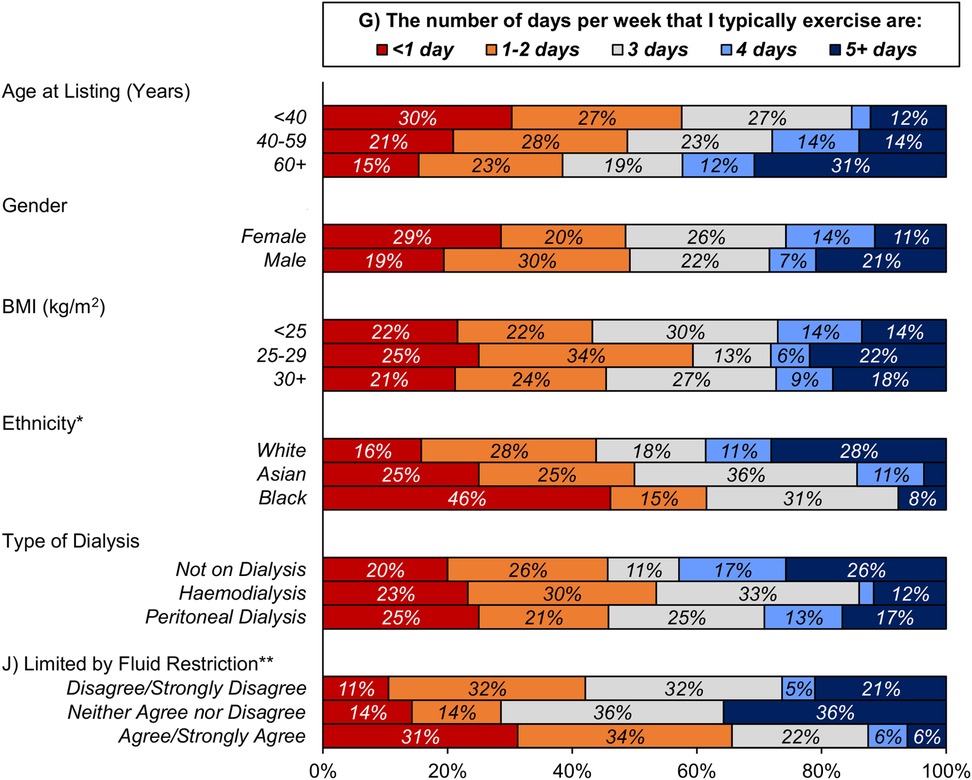
Figure 2. Associations between patient characteristics and exercise frequency. The wording of some questions is shortened for brevity; the original text of each question is reported in Table 1. Percentages are calculated based on the number of patients that gave a response to the stated question, as reported in Table 3. Unlabelled bars have a frequency of <5%. *The mixed/other group was excluded from analysis, due to the small sample size. **Excludes patients answering “not applicable”, i.e., those without fluid restrictions. BMI, body mass index.
Discussion
This survey demonstrates that, whilst ESKD patients who are listed for kidney transplantation have a positive attitude towards exercise, only around half report regularly performing any form of exercise, with fatigue being a major barrier. To our knowledge, this is the first study of attitudes to exercise in kidney transplant candidates and, as intended by the study, provides granular views based on varying demographics, type of dialysis and exercise patterns. Attitudes to exercise varied between different age groups and ethnicities, suggesting the need for personalised interventions. Most patients were willing to consider a wearable device to monitor sedentary behaviour. Only a minority of patients performed any form of resistance exercise.
This study was inspired by Chasca et al., who evaluated patient perspectives regarding exercise in liver transplant candidates (14). They reported similar findings, with around 90% of patients stating that exercise was important and that that they would be willing to exercise, but only around half reporting regularly performing exercise, with walking being the most common. Delgado et al. performed a similar survey on 100 ESKD patients undergoing haemodialysis (18). They also reported findings consistent with our audit, with 54% of patients stating that they did not perform even 30 min of light activity a day. In addition, 8% of patients of their cohort were concerned about the risk of exercise and 24% acknowledged a fear of getting hurt. Whilst we did not specifically ask about concerns relating to exercise, 15% of patients stated that they did not agree that exercise would be reasonable for them, some of which may have reflected similar concerns. Finally, in addition to fatigue, Delgado et al. also noted that “lack of motivation” was a key barrier to exercise – a concept that we did not explore in our study.
Only 34% of our cohort agreed/strongly agreed that their doctor had encouraged them to do more exercise. An international survey of nephrologists by Taryana et al. indicated that most nephrologists viewed exercise counselling as within the scope of their practise and identified exercise prescriptions and programs as an important area of research to further aid counselling (19). However, studies have often found exercise counselling to be poor because of competing interests and fears of harm to the patient (20). MacRae et al. assessed healthcare provider counselling in 108 ESKD patients receiving PD, and found considerable variability in the exercise-related advice provided (15). For example, 76% were told not to lift weights and 44% were told not to swim due to the presence of a PD catheter. This may reflect the lack of clear guidance on exercise in PD patients and requires further evaluation given the discrepancy in patient and clinician views (21).
Less than a quarter of patients in our cohort agreed/strongly agreed to performing resistance or weight training. This is in keeping with the low rate of recruitment seen in trials that have attempted to study resistance training in the CKD population (22). In CKD, skeletal muscle wasting is associated with increased morbidity and mortality, which worsens in ESKD patients who start dialysis. Evidence suggests that resistance training it is well tolerated by CKD patients and confers important clinical benefits (23, 24). However, perceptions of resistance training have only been studied in patients with CKD stage 3 and 4, and not ESKD or kidney transplant candidates (25). Therefore, further work is required to address how to encourage resistance training and how best to deliver programs (e.g., home- vs. hospital-based) whilst waiting for a kidney transplant (26).
We demonstrated a significant difference in physical activity levels between ethnic groups in our cohort, with Black and Asian individuals performing less activity compared to their White counterparts. This was despite there being no significant difference between ethnic groups in the perceptions of, and willingness to exercise. Ethnic minority groups have a greater burden of risk factors for CKD and are 3–5 times more likely to progress to dialysis than White patients. In the UK, over a third of people waiting for a kidney transplant are from ethnic minority communities. Therefore, it is important to reflect on how physical activity interventions can be tailored to these patients (24). Mayes et al. performed a qualitative study exploring the cultural and ethnic influences on physical activity in CKD patients, and concluded that attitudes and beliefs towards exercise vary across ethnic groups (27). For example, in South Asian patients, inter-generational relationships and relatives play an important role in diet and exercise, which needs to be considered when designing exercise interventions.
We did not note any clear differences in either views on exercise or physical activity levels between the subgroups of pre-dialysis, haemodialysis and PD patients. This may reflect heterogeneity in symptom burden that impedes exercise, even amongst end-stage pre-dialysis patients, as they approach dialysis (9). Consequently, dialysis does not appear to have directly impacted physical activity in this cohort. However, half of the patients on haemodialysis reported the time spent on dialysis to be a barrier to exercise, with half of those with fluid restrictions reporting this to be a barrier. As such, these additional challenges may represent indirect impacts on the ability of patients to exercise, which should be considered when designing exercise interventions. For example, programmes of shorter but more frequent sessions may be more convenient for patients who have limited time to dedicate to exercise, whilst lower-intensity exercises could be more appropriate for patients on fluid restrictions.
This study had several strengths, with the main one being that it is unique in the current literature, as it focuses on kidney transplant candidates. Given the wide spectrum of CKD, further studies such as these are required to gain specific understanding of attitudes of CKD patients listed for transplantation, as these may differ from the general CKD population. In addition, unlike most exercise studies that focus predominately on haemodialysis patients alone, this cohort includes pre-dialysis and PD patients making the results more generalisable. The cohort was also diverse, with a large proportion being of non-White ethnicity (44%), an under-represented group in exercise studies; the fact that patients with language barriers were not excluded, and instead supported in completing the survey likely contributed to this diversity. However, our study also has limitations, which need to be considered when interpreting the results. Firstly, the self-reported nature of the study meant that the reliability of the results is dependent on patients answering the questions truthfully and accurately. However, it is possible that social desirability bias may have resulted in some patients giving overly positive responses, particularly in the knowledge that their answers would potentially be seen by their clinician. As such, future studies would ideally use wearable exercise monitoring devices, to validate patients' responses. Secondly, the study had only modest statistical power, resulting from the relatively small sample size. A post-hoc power calculation indicated that the sample size of N = 103 yielded a minimal detectable correlation coefficient of 0.3 at 80% power. As such, whilst the study was sufficiently powered to detect moderate-to-large effects, small effects may have been missed, leading to false-negative errors.
Thirdly, the survey did not formally define “exercise”, which may have resulted in inconsistency of responses if the interpretation of this term varied between patients. This can be seen by the discrepancy between the proportion of patients stating that they regularly exercised, and that reported walking regularly (agree/strongly agree = 56% vs. 85%), implying that some patients classified walking as exercise and others did not. This may also explain why older patients in our cohort appear to engage in greater amounts of exercise, contrary to other reported studies (18). This confusion between what is considered “physical activity” or “exercise” has been documented in many exercise-related studies (28). As such, this provides further justification for the use of wearable exercise monitoring devices in future studies, to allow for a more consistent measurement of the quantity and intensity of physical activity. Finally, our cohort was relatively young (mean age: 47.8 years), compared to the current European demographic (mean age: 50–52 years) (29, 30). This was particularly pertinent, given that some of the responses (e.g., exercise frequency) were found to differ significantly with age. Consequently, the results may not be generalisable to cohorts with a considerably different age distribution.
Conclusion
Whilst the vast majority of kidney transplant candidates have positive attitudes towards exercise, a smaller proportion report regularly performing exercise. With rising levels of frailty, sarcopenia and obesity within the CKD population, the transplant community is waking up to the need for prehabilitation and optimisation of patients on the waiting list. This audit provides granular data with respect to attitudes to exercise, which would be useful in designing prehabilitation programs and future studies in this area.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies involving humans because study registered and approved as an audit of practise by University Hospitals Birmingham Audit Review Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ST: Writing – original draft. KP: Conceptualization, Writing – original draft. JH: Methodology, Writing – review & editing. FM: Data curation, Writing – review & editing. LB: Data curation, Writing – review & editing. FW: Conceptualization, Writing – review & editing. SJ: Supervision, Writing – review & editing. MA: Methodology, Writing – review & editing. AS: Conceptualization, Writing – review & editing. DD: Conceptualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
This study was carried out at a National Institute for Health and Care Research (NIHR) Birmingham Biomedical Research Centre (BRC).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. UK KR. Kidney disease: a UK public health emergency (2023). Available online at: https://www.kidneyresearchuk.org/wp-content/uploads/2023/06/Economics-of-Kidney-Disease-full-report_accessible.pdf (Accessed January 12, 2025).
2. Quint EE, Zogaj D, Banning LBD, Benjamens S, Annema C, Bakker SJL, et al. Frailty and kidney transplantation: a systematic review and meta-analysis. Transplant Direct. (2021) 7(6):e701. doi: 10.1097/TXD.0000000000001156
3. Thind AK, Rule A, Goodall D, Levy S, Brice S, Dor F, et al. Prevalence of frailty and cognitive impairment in older transplant candidates - a preview to the kidney transplantation in older people (KTOP): impact of frailty on outcomes study. BMC Nephrol. (2022) 23(1):283. doi: 10.1186/s12882-022-02900-w
4. Chan GC, Kalantar-Zadeh K, Ng JK, Tian N, Burns A, Chow KM, et al. Frailty in patients on dialysis. Kidney Int. (2024) 106(1):35–49. doi: 10.1016/j.kint.2024.02.026
5. Harhay MN, Rao MK, Woodside KJ, Johansen KL, Lentine KL, Tullius SG, et al. An overview of frailty in kidney transplantation: measurement, management and future considerations. Nephrol Dial Transplant. (2020) 35(7):1099–112. doi: 10.1093/ndt/gfaa016
6. Chu NM, Chen X, Norman SP, Fitzpatrick J, Sozio SM, Jaar BG, et al. Frailty prevalence in younger end-stage kidney disease patients undergoing dialysis and transplantation. Am J Nephrol. (2020) 51(7):501–10. doi: 10.1159/000508576
7. McAdams-DeMarco MA, Chu NM, Segev DL. Frailty and long-term post-kidney transplant outcomes. Curr Transplant Rep. (2019) 6(1):45–51. doi: 10.1007/s40472-019-0231-3
8. Pesce de Souza F, Massierer D, Anand Raje U, Tansey CM, Boruff J, Janaudis-Ferreira T. Exercise interventions in solid organ transplant candidates: a systematic review. Clin Transplant. (2020) 34(9):e13900. doi: 10.1111/ctr.13900
9. Wilkinson TJ, McAdams-DeMarco M, Bennett PN, Wilund K, Global Renal Exercise N. Advances in exercise therapy in predialysis chronic kidney disease, hemodialysis, peritoneal dialysis, and kidney transplantation. Curr Opin Nephrol Hypertens. (2020) 29(5):471–9. doi: 10.1097/MNH.0000000000000627
10. Quint EE, Ferreira M, van Munster BC, Nieuwenhuijs-Moeke G, Te Velde-Keyzer C, Bakker SJL, et al. Prehabilitation in adult solid organ transplant candidates. Curr Transplant Rep. (2023) 10(2):70–82. doi: 10.1007/s40472-023-00395-4
11. Quint EE, Haanstra AJ, van der Veen Y, Maring H, Berger SP, Ranchor A, et al. PREhabilitation of CAndidates for REnal transplantation (PreCareTx) study: protocol for a hybrid type I, mixed method, randomised controlled trial. BMJ Open. (2023) 13(7):e072805. doi: 10.1136/bmjopen-2023-072805
12. NHSBT. UK NHSBT annual kidney transplant activity report (2024). Available online at: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/33795/section-5-kidney-activity.pdf (Accessed January 12, 2025).
13. Annema C, De Smet S, Castle EM, Overloop Y, Klaase JM, Janaudis-Ferreira T, et al. European Society of Organ Transplantation (ESOT) consensus statement on prehabilitation for solid organ transplantation candidates. Transpl Int. (2023) 36:11564. doi: 10.3389/ti.2023.11564
14. Chascsa DM, Lai JC, Dunn MA, Montano-Loza AJ, Kappus MR, Dasarathy S, et al. Patient and caregiver attitudes and practices of exercise in candidates listed for liver transplantation. Dig Dis Sci. (2018) 63(12):3290–6. doi: 10.1007/s10620-018-5271-5
15. MacRae JM, Tam TA, Harrison T, Harasemiw O, Bohm C, Bennett PN, et al. Exercise perceptions and practices of people receiving peritoneal dialysis: an international cross-sectional survey. Perit Dial Int. (2024) 45(2):106–12. doi: 10.1177/08968608241237686
16. Manfredini F, Mallamaci F, D'Arrigo G, Baggetta R, Bolignano D, Torino C, et al. Exercise in patients on dialysis: a multicenter, randomized clinical trial. J Am Soc Nephrol. (2017) 28(4):1259–68. doi: 10.1681/ASN.2016030378
17. Association UK. UK Renal Registry 25 annual report (2021). Available online at: https://ukkidney.org/sites/renal.org/files/publication/file-attachments/25th%20Annual%20Report%20Final%2030.6.23%20-%20Edited%202024.pdf (Accessed January 12, 2025).
18. Delgado C, Johansen KL. Barriers to exercise participation among dialysis patients. Nephrol Dial Transplant. (2012) 27(3):1152–7. doi: 10.1093/ndt/gfr404
19. Taryana AA, Krishnasamy R, Bohm C, Palmer SC, Wiebe N, Boudville N, et al. Physical activity for people with chronic kidney disease: an international survey of nephrologist practice patterns and research priorities. BMJ Open. (2019) 9(12):e032322. doi: 10.1136/bmjopen-2019-032322
20. Delgado C, Johansen KL. Deficient counseling on physical activity among nephrologists. Nephron Clin Pract. (2010) 116(4):c330–6. doi: 10.1159/000319593
21. Lambert K, Lightfoot CJ, Jegatheesan DK, Gabrys I, Bennett PN. Physical activity and exercise recommendations for people receiving dialysis: a scoping review. PLoS One. (2022) 17(4):e0267290. doi: 10.1371/journal.pone.0267290
22. Watson EL, Greening NJ, Viana JL, Aulakh J, Bodicoat DH, Barratt J, et al. Progressive resistance exercise training in CKD: a feasibility study. Am J Kidney Dis. (2015) 66(2):249–57. doi: 10.1053/j.ajkd.2014.10.019
23. Chen CC, Huang YY, Hua Z, Xia L, Li XQ, Long YQ, et al. Impact of resistance exercise on patients with chronic kidney disease. BMC Nephrol. (2024) 25(1):115. doi: 10.1186/s12882-024-03547-5
24. Gollie JM, Harris-Love MO, Patel SS, Argani S. Chronic kidney disease: considerations for monitoring skeletal muscle health and prescribing resistance exercise. Clin Kidney J. (2018) 11(6):822–31. doi: 10.1093/ckj/sfy054
25. Lightfoot CJ, Vadaszy N, Watson EL, Robertson N, Smith AC. Perceptions and experiences of a progressive resistance exercise program in people with chronic kidney disease. Nephrol Nurs J. (2022) 49(1):19–27. doi: 10.37526/1526-744X.2022.49.1.19
26. Noor H, Reid J, Slee A. Resistance exercise and nutritional interventions for augmenting sarcopenia outcomes in chronic kidney disease: a narrative review. J Cachexia Sarcopenia Muscle. (2021) 12(6):1621–40. doi: 10.1002/jcsm.12791
27. Mayes J, Castle EM, Greenwood J, Ormandy P, Howe PD, Greenwood SA. Cultural influences on physical activity and exercise beliefs in patients with chronic kidney disease: ‘the culture-CKD study'-a qualitative study. BMJ Open. (2022) 12(1):e046950. doi: 10.1136/bmjopen-2020-046950
28. Moorman D, Suri R, Hiremath S, Jegatheswaran J, Kumar T, Bugeja A, et al. Benefits and barriers to and desired outcomes with exercise in patients with ESKD. Clin J Am Soc Nephrol. (2019) 14(2):268–76. doi: 10.2215/CJN.09700818
29. Knobbe TJ, Kremer D, Zelle DM, Klaassen G, Dijkema D, van Vliet IMY, et al. Effect of an exercise intervention or combined exercise and diet intervention on health-related quality of life-physical functioning after kidney transplantation: the active care after transplantation (ACT) multicentre randomised controlled trial. Lancet Healthy Longev. (2024) 5(9):100622. doi: 10.1016/j.lanhl.2024.07.005
Keywords: exercise, kidney transplantation, prehabilitation, attitudes, waiting list
Citation: Tasleem S, Patel K, Hodson J, Mazhar F, Bedford L, Williams FR, Jones S, Armstrong MJ, Sharif A and Dabare D (2025) Exercise attitudes and practices among adults listed for kidney transplantation: a survey of a diverse patient cohort. Front. Sports Act. Living 7:1559322. doi: 10.3389/fspor.2025.1559322
Received: 14 March 2025; Accepted: 16 June 2025;
Published: 14 July 2025.
Edited by:
Diogo Vaz Leal, University of Maia, PortugalReviewed by:
Luciano Pereira, University of Porto, PortugalRoseanne Billany, University of Leicester, United Kingdom
Copyright: © 2025 Tasleem, Patel, Hodson, Mazhar, Bedford, Williams, Jones, Armstrong, Sharif and Dabare. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dilan Dabare, ZGlsYW4uZGFiYXJlQHVoYi5uaHMudWs=
 Sadia Tasleem
Sadia Tasleem Kamlesh Patel1
Kamlesh Patel1 James Hodson
James Hodson Farah Mazhar
Farah Mazhar Felicity R. Williams
Felicity R. Williams Simon Jones
Simon Jones Adnan Sharif
Adnan Sharif Dilan Dabare
Dilan Dabare