- 1Department of Psychiatry, Castle Point VA Medical Center, Wappingers Falls, NY, United States
- 2Department of Psychiatry, Garnet Health Medical Center-Catskills, Harris, NY, United States
- 3Department of Psychiatry, Nilux Clinic, Hollywood, CA, United States
- 4Department of Psychiatry, Nilux Clinic, Manhattan, NY, United States
- 5Department of Psychiatry, Hackensack Meridian Health-Hackensack University Medical Center, Hackensack, NJ, United States
- 6Department of Psychiatry, Stony Brook University Hospital, Stony Brook, NY, United States
Aim: When a skill is lost, this can impact a person's career and psychological wellbeing. As this is the case with the yips, preventing, treating, and curing them is important. This study was prompted by the limited information available on the yips, specifically regarding etiologies. The intent of this study was to utilize surveys with both a medical review of systems and psychological questioning to identify commonalities in afflicted players. This could then provide considerations of the causes and guide future research.
Methods: The study recruited experienced golfers for in-person surveys and stroke demonstrations from January 26, 2019 to March 28, 2020. The analyses included statistical methods and discussion. These methods included Yates’ chi-squared test and Fisher's exact test targeted toward smaller sample sizes.
Results: Finding participants was difficult and resulted in a small sample size (n = 14). The study had 4 participants with the yips and 10 controls. Statistical methods for small sample sizes found few associations. However, Fisher's exact test showed negative associations between the yips and sore throats (p = 0.0050), fever (p = 0.0150), and physical trauma (p = 0.0150). Yates' chi-squared test also found significance for fever (p = 0.0328), sore throat (p = 0.0105), and physical trauma (p = 0.0328). Qualitative data were also highlighted in the study, including tabulating the treatments tried and the outcomes of the participants.
Conclusion: The yips cause problems, especially for those who have invested significant time into perfecting a skill. Continued research is warranted to elucidate the causes and effective treatments.
Introduction
The yips are unintended movements that impact accuracy. Their onset is sudden, with no apparent explanation or foreshadowing. In golf, they appear as involuntary movements and/or freezing during a stroke (1–6). These movements have been described as jerking, twisting, and/or a tremor, while freezing is a hesitation prior to executing a swing (1–6).
The yips have been categorized in a variety of ways. They have been described as “physical symptoms (dystonia: type I), psychosocial symptoms (choking: type II), or a combination of both (non-categorized)” (6). One study categorized the yips as dystonic and non-dystonic where dystonic yips had a “jerk, twist, or posturing” (7), and non-dystonic forms appeared as “pushing or steering” the ball while putting (7). Similarly, other research has highlighted a cramping/dystonia perspective (1–3). The prevalence of perceived yips in studies has varied based on sample size. In a 69-question survey provided to 1,050 “professional and amateur golfers,” 42% responded, of which 28% self-reported having the yips (1, 2). In a separate survey sent to 2,630 tournament players, 1,031 (39%) responded and 52% felt they had the yips (5). Furthermore, they have been associated with older age (1, 2). Outside of sports, they afflict musicians, surgeons, and dentists (1, 2, 4, 6).
Regarding the psychological aspects of the yips, the topic of anxiety is frequently addressed. Researchers have found that the yips may be exacerbated by performance anxiety, a fear associated with a specific task, and “choking” (4, 6). Choking has been a focal point of some research and is described as “an extreme manifestation of performance anxiety” and “a suboptimal performance that results from self-focused or distracted attention” (6). One study concluded anxiety is not a sole cause, but “a necessary factor for the manifestation of the yips in a number of golfers, and exacerbates the problem in others” (4).
There have also been neurological studies conducted on the yips, many of which sought to better identify them and liken them to movement disorders. Thus, the topic of dystonia was added to the discussion. In one approach, the yips were delineated into neurological (dystonia) and psychological (choking) categories (6). Dystonia, “a neurological disorder characterized by involuntary movements resulting in spasms, twisting and posturing of a body part,” has described the yips and some suggest they are a “task-specific dystonia” (6). It was postulated for dystonic types that “performance anxiety contributes to and exacerbates the ‘yips’ symptoms” (6). For “chokers,” performance anxiety likely combines “with self-focused attention and over-analysis to cause the ‘yips’” (6). This study implied the unlikeliness of dystonic or choking symptoms occurring in the “absence of performance anxiety” (6).
The yips have destroyed the careers of many professional athletes, causing them to either circumvent their damaged technique using a lesser form or abandon their sport. While there are no FDA-approved medications for the yips, the suspected contributing factors such as anxiety have known protocols. Propranolol and diazepam are two of these that have been prescribed off-label (8). If cramping/dystonia is present, botulinum toxin injections have been prescribed (1–3). Some suggest taking a break, and instructors teach new techniques to change muscle memory.
The task of this pilot study is to further explore potential medical and psychological etiologies of the yips and their treatment in the context of golf.
Methods
Recruitment
Participants were solicited for a telephone prescreening via postings at local golf facilities, classified ads in a local newspaper, emails, and word of mouth in the Hudson Valley region of New York and southeastern Pennsylvania. Emails were also specifically sent to Professional Golfers’ Association of America (PGA) players in an effort to recruit competitive tournament players. If the criteria were met, an in-person survey and stroke demonstration were arranged locally. A witnessed signing of an informed consent form, as required by the Internal Review Board that approved this study, was completed upon meeting.
The inclusion criteria for this study included significant golf experience (i.e., tournament experience and/or 18-hole competition >3 years) and age (18–80 years). This experience was validated in discussions with players and reviewing their competitive histories online. This age range was sought to exclude potential inexperience in younger players, particularly in regard to learning a stroke and recognizing developmental changes in youth (i.e., growth spurts). In addition, confounding medical comorbidities in elderly adults were considered when choosing the age limit.
The exclusion criterion was a current movement disorder diagnosis. We separated participants into two groups: yips and no yips (controls). The inclusion criterion for a yips group participant (YGP) was a “yes” response to all the following screening questions:
1. Have you developed a significant difficulty with a golf swing (putting, driving, chipping, etc.) that was once an asset in your game?
2. Have you noted any form of tremor, involuntary movement, jerking, twisting, and/or freezing (pausing) develop in your stroke (1–7)?
3. Have you found difficulty in recovering that golf swing to its original effectiveness?
Survey
The 156-question survey consisted of medical review of systems (ROS) questions (digestive, immune, respiratory, etc.). The goal was to employ the basics of a medical investigation to discover connections between the yips and a system. Additional categories included psychiatric/psychological, infection/illness, trauma, coaching, treatment, medications, yip description, family history, general health, yip history, and personal opinion. The questions were organized into subcategories based on their medical system. These surveys were conducted in-person and based on the participants’ accounts of their medical and psychological histories. The participants were required to answer all questions in the musculoskeletal, cardiac, neurologic, respiratory, and psychological subcategories; however, if they denied diagnoses in other medical categories, they were not required to answer questions under that system. This helped avoid fatigue, and differences were accounted for in statistical measures.
Observations
Each participant demonstrated a stroke (chipping, putting, or driving) to confirm the presence of the yips or not. Players were asked to demonstrate their golf strokes three times (in person) to ensure they were properly warmed up and appropriately replicated. Observations for the yips movements included jerking, twisting, and/or posturing patterns in comparison to standard stroke accordance.
Data collection
Survey responses were organized and analyzed using Microsoft Excel. The website langsrud.com (9) was used to calculate Fischer's exact test values.
Data analyses
Yates' chi-squared test and Fisher's exact test were the statistical methods used. These were chosen as they are intended to work with smaller sample sizes to identify statistically significant data from them.
In Fischer's exact test, if a one-tailed left test (negative relationship) accompanied a statistically significant “two-tailed test,” this suggested a negative relationship and, conversely, should a one-tailed right test accompany a two-tailed test, this suggests a positive relationship. Yates’ chi-squared test was another statistical assessment utilized to confirm the relationships.
Survey questions on popularized or potentially relevant topics of yips etiologies were chosen for presentation in charts/tables and the discussion.
Results
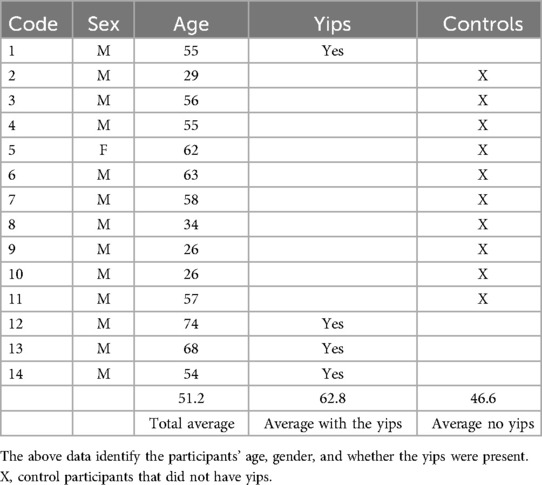
Surveys were administered from January 26, 2019 to March 28, 2020 and 14 participants volunteered. Four were YGPs and 10 were controls. Difficulties finding participants resulted in a small sample size. There were 13 men and 1 woman (control) in the study (Table 1). There were limited responses to outreach attempts, which included flyers in newspapers, postings in private golf clubs, and emails to PGA players.
The majority of the ROS and psychiatric/psychological questions proved statistically insignificant for both Yates’ chi-squared test and Fisher's exact test. However, negative associations existed between the yips and infections involving sore throats (p = 0.0050) and fevers (p = 0.0150) (Table 2). If a one-tailed association (positive or negative) accompanied a two-tailed association, this was significant. The trauma-related question, “Have you endured any physical trauma prior to the development of your yips (i.e., car accident, falling on your arm)?”, was also negatively associated (p = 0.0150) (Table 2). Yates' chi-squared test also helped confirm these relationships involving sore throats (p = 0.0105), fever (p = 0.0328), and any physical trauma (p = 0.0328).
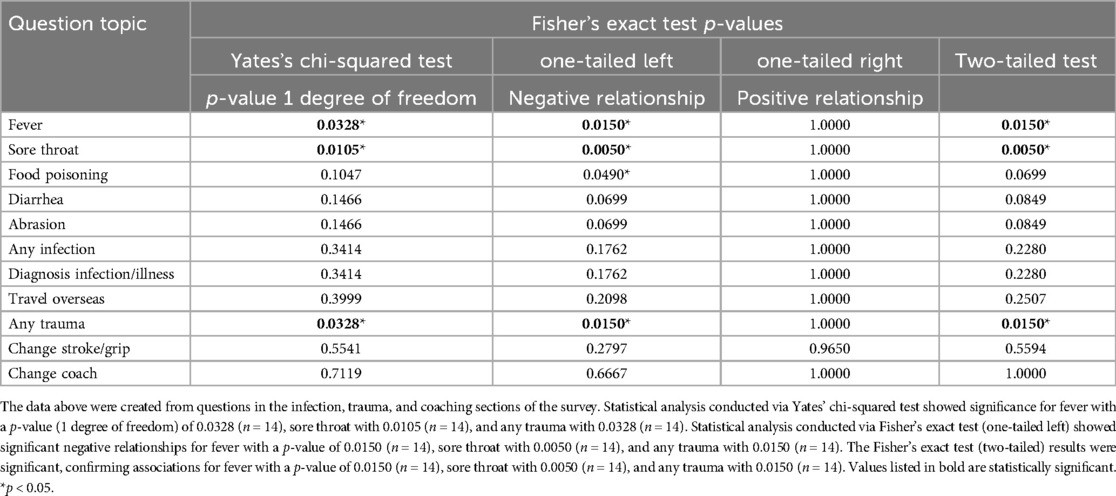
Table 2. Yates' chi-squared test and Fisher's exact test results for the infection, trauma, and coaching questions.
Regarding some specific findings, 3/4 (75%) of the YGPs felt the yips were not preventable. The YGPs thought they were psychological in nature and age-related. Furthermore, 3/4 (75%) of the YGPs sought treatment including but not limited to changing grips, sports psychology videos, playing with their non-dominant hand, and using long putters and/or wedges for sensory distraction purposes. Only 1/4 (25%) thought medication could be related to golfing issues. Half (2/4) of the YGPs and 3/10 of the controls had taken anti-anxiety medication, including diazepam, alprazolam, and beta blockers. Botulinum toxin injections were not mentioned.
Half (2/4) of the YGPs self-medicated using alcohol and found no benefit. In addition, 3/4 (75%) of the YGPs and 5/10 (50%) of the controls had sleep issues. Although prior musculoskeletal trauma was not indicated by the YGPs, 2/4 (50%) had surgery after acquiring the yips. Interestingly, one surgery involved wrist carpel tunnel syndrome, and the other trigger finger release surgery. Concerning coaching, 1/4 (25%) of the YGPs attempted to change their grip/stroke technique as advised prior to developing their yips. All the YGPs indicated decreased performance, but only 2/4 (50%) said someone else noticed their yips, inclusive of golf peers and coaches. A list of strategies attempted by the YGPs to overcome the yips and their outcomes are presented in Table 3.
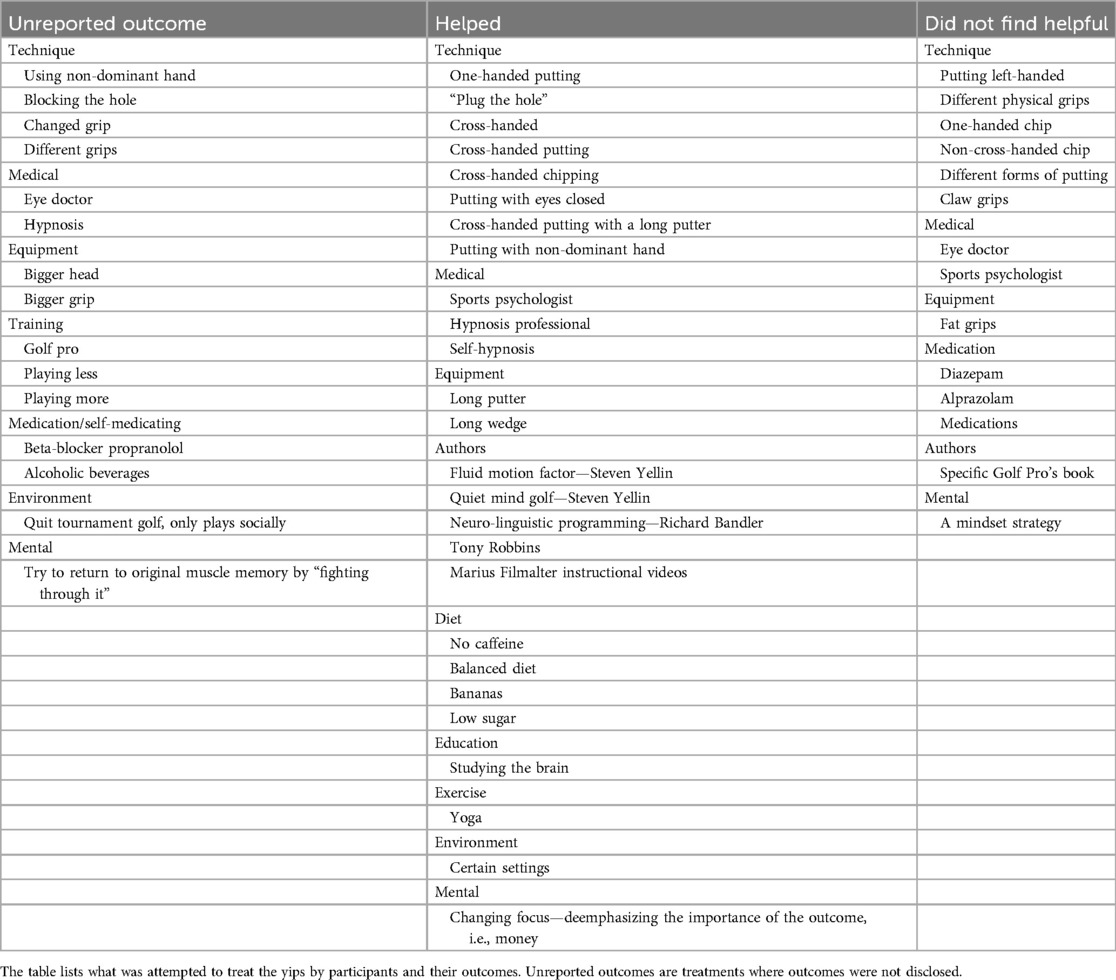
Table 3. Verbal survey responses concerning the techniques and treatments attempted and their outcomes.
Discussion
The lack of participants (1 woman, 13 men) limited the study, especially regarding statistical analyses. Nevertheless, a platform was developed using Microsoft Excel, and statistics were calculated, charted, and tabulated. Therefore, the major outcome of this study was building an initial prototype for future research.
There were limited responses to recruitment attempts. Some players cited concerns with discussing the yips, believing they are psychological in nature and fearing they could acquire them through discussions.
The in-person aspect of this study was important not only for data accuracy and insight but also to confirm the yips. It is not uncommon to blame a bad stroke on the yips.
The average age of yips onset was 34.8 (SD 14.62), and the participants had endured them for 40, 49, 18, and 4 years, respectively. All were seasoned tournament players at the onset. Despite 3/4 (75%) of the YGPs enduring more losses and 2/4 (50%) avoiding their bad strokes, they still enjoy golf.
Standardizing testing remains critical in observation assessment and an ongoing goal of future studies. Recent research has highlighted measuring “external load” across different training modalities (10). This concept should be considered in future analyses to better understand how load difference and exertion can contribute to flawed strokes and yips development (10).
Interestingly, two controls reported previously overcoming the yips. One reported using a 3D simulator to observe and make corrections and the other relaxed using deep breathing techniques. However, their past yips could not be verified. One research study reported a player overcame their yips in a year by changing their grip (4). These accounts suggest the yips are curable.
In conclusion, physicians need to be aware of the yips and be empathetic. These patients need compassion and understanding. There may be a tendency to make light of a bad golf swing, but this should be avoided. Prior to assuming the yips exist, this must be confirmed by ruling out movement disorders including essential tremor or Parkinson's disease and patients must be educated on the prognosis possibly being a lengthy process.
Depression and anxiety also need to be addressed as they could be the most damaging. Furthermore, the patient's support system should be assessed and kept involved. Whenever a patient working in these fields reports losing fine motor skills, the yips should be considered as a possible differential diagnosis (11).
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Garnet Health Medical Center Institutional Review Board (IRB). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KCA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing, Software, Visualization. UV: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing. NP: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The content of this manuscript was presented at the American Association for Geriatric Psychiatry's (AAGP) 2022 Annual Meeting in Orlando, Florida. The abstract was then published in The American Journal of Geriatric Psychiatry (11).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Adler CH, Crews D, Kahol K, Santello M, Noble B, Hentz JG, et al. Are the yips a task-specific dystonia or “golfer’s cramp”? Mov Disord. (2011) 26(11):1993–6. doi: 10.1002/mds.23824
2. McDaniel KD, Cummings JL, Shain S. The “yips”: a focal dystonia of golfers. Neurology. (1989) 39(2):192–5. doi: 10.1212/WNL.39.2.192
3. Howland J. Mayo Clinic Minute: are the yips just nerves or something more? (2018). Available at: https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-are-the-yips-just-nerves-or-something-more/ (Accessed April 7, 2025).
4. Sachdev P. Golfers’ cramp: clinical characteristics and evidence against it being an anxiety disorder. Mov Disord. (1992) 7(4):326–32. doi: 10.1002/mds.870070405
5. Smith AM, Malo SA, Laskowski ER, Sabick M, Cooney WP 3rd, Finnie SB, et al. A multidisciplinary study of the ‘yips’ phenomenon in golf: an exploratory analysis. Sports Med. (2000) 30(6):423–37. doi: 10.2165/00007256-200030060-00004
6. Smith AM, Adler CH, Crews D, Wharen RE, Laskowski ER, Barnes K, et al. The ‘yips’ in golf: a continuum between a focal dystonia and choking. Sports Med. (2003) 33(1):13–31. doi: 10.2165/00007256-200333010-00002
7. Adler CH, Temkit M, Crews D, McDaniel T, Tucker J, Hentz JG, et al. The yips: methods to identify golfers with a dystonic etiology/golfer’s cramp. Med Sci Sports Exerc. (2018) 50(11):2226–30. doi: 10.1249/MSS.0000000000001687
8. Adler CH, Zhang N, Crews D, McDaniel T, Tucker J, Marquardt C, et al. Dystonic golfer’s cramp: pilot study of propranolol and looking at the hole. Parkinsonism Relat Disord. (2020) 80:108–12. doi: 10.1016/j.parkreldis.2020.09.018
9. Langsrud Ø. Fisher’s exact test (2012). Available at: https://langsrud.com/fisher.htm (Accessed May 20, 2020).
10. Dhahbi W, Chaabene H, Pyne D, Chamari K. Standardizing the quantification of external load across different training modalities: a critical need in sport-science research. Int J Sports Physiol Perform. (2024) 19(11):1173–5. doi: 10.1123/ijspp.2024-0366
Keywords: yips, golf, sports, movement, performance
Citation: Afrassiabian KC, Mahato B, Vieux U and Palekar N (2025) The yips: an investigation of the causes and treatments in the context of golf. Front. Sports Act. Living 7:1563370. doi: 10.3389/fspor.2025.1563370
Received: 19 January 2025; Accepted: 31 March 2025;
Published: 17 April 2025.
Edited by:
Wissem Dhahbi, University of Jendouba, TunisiaReviewed by:
Hatem Ghouili, University of Jendouba, TunisiaManar Boujabli, University of Jendouba, Tunisia
Copyright: © 2025 Afrassiabian, Mahato, Vieux and Palekar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kian-Taj Claire Afrassiabian, a3RjYW1lZEBnbWFpbC5jb20=
 Kian-Taj Claire Afrassiabian
Kian-Taj Claire Afrassiabian Bisundev Mahato
Bisundev Mahato Ulrick Vieux5
Ulrick Vieux5