- 1Department of Orthopedic Surgery, New York-Presbyterian/Columbia University Irving Medical Center, New York, NY, United States
- 2Department of Orthopedic Surgery, University of Minnesota Twin Cities, Minneapolis, MN, United States
- 3Department of Pediatric Orthopedic Surgery, Gillette Children's, St. Paul, MN, United States
The preparticipation evaluation (PPE) continues to be a recommended and widely used tool in identifying athletes with health conditions or injury risks that may impact their athletic participation. In the last 10 years, updates to the PPE mirror the increasing impacts of sport specialization, level of competition, importance of mental health in injury risk and recovery, research on cardiovascular and concussive health in youth athletes, and increased awareness of metabolic demands placed on both male and female athletes. The PPE at this snapshot in time exists within an evolving landscape of recommendations. However, it continues to present a vital opportunity for health care providers, preferably within the athlete's “medical home”, to discuss anticipatory guidance, intervene on injury risk, and establish a baseline for future monitoring as the athlete enters competition. As mentioned, there continues to be a need for further research and development, but the orthopedic surgeon should be aware of the purpose the PPE currently serves given the intersectionality of their field with young athletes at the brink or in the midst of injury.
Introduction
It has been 10 years since we published our recommendations for the orthopedic surgeon in the preparticipation evaluation (PPE) of the young athlete (1). Since then, the number of children and adolescents participating in sports in the United States has nearly doubled to 60 million (2). Along with this tremendous rise comes the trend of early sports specialization, with more youth athletes committing to a single sport prior to the age of 14 (3). Sports-related injuries continue to contribute heavily to the overall pediatric injury burden, with 3.5 million injuries per year resulting in time lost from sport (4). As previously outlined, the PPE is a multisystem evaluation of a youth athlete that has three major components intended to (1) detect health or injury risks that should delay their participation in sport, (2) identify previous injury patterns to prevent recurrence, and (3) provide individualized anticipatory guidance and counseling.
Through collaboration between the American Academy of Family Physicians, American Academy of Pediatrics, American College of Sports Medicine (ACSM), American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, and American Osteopathic Academy of Sports Medicine the formal PPE is in its 5th iteration as of 2021. There remains no universal mandate regarding the PPE, but it continues to be required by the National Collegiate Association (NCAA) within 6 months of the start of each season and endorsed by the National Federation of State High School Associations (NFHS) (5).
This article serves to update our previous recommendations for orthopedic surgeons, as well as the multidisciplinary teams, who provide medical coverage spanning from the interscholastic to the collegiate level. These teams include primary care physicians, non-operative sports medicine physicians, athletic trainers, physical therapists, and qualified exercise professionals. By including each of these stakeholders in this conversation, a more universal understanding of what it means to take care of the young competitive athlete may be conveyed. This will result in more comprehensive, seamless care for athletes as they progress through each phase of their sport and require the care expertise of each member of the multidisciplinary team. Key updates include addressing the shift in metabolic and nutritional health associated with the relative energy deficiency in sport syndrome, the number of sport hours per week, joint laxity, jump tests, and psychological evaluation. As our athletes evolve, so to must our evaluations to ensure safe athletic participation in the upcoming season.
Our review will largely focus on the evaluation of young, competitive athletes participating in organized sports. The preparticipation evaluation of the general public prior to participating in physical activity will be explored briefly but will not be discussed at length.
Organization and timing
As previously recommended, the PPE should take place in advance of athletic participation, with the recommendation generally being between 4 and 8 weeks prior. Approximately 3–14 percent of students require additional evaluation and this time frame allows for any additional testing, rehabilitation, or consultation that is required to avoid delaying competition (5). The updated recommendations from the AAP recommend against completing the PPE in a group or team-based setting, but rather within the athlete's “medical home”. Not only does this draw on the trust and continuity of care that exists between an athlete and their primary care practitioner but also allows for routine healthcare topics to be assessed at the same time (2). Conversely, at the collegiate level, the PPE is generally done by a provider local to the university or institution, and it is unrealistic for each athlete to have their individual PCP oversee the PPE. Thus, it is recommended that the same provider complete the entirety of the evaluation for each athlete in an individualized setting in order to provide the most thorough evaluation.
Medical history
A complete medical history continues to be the most important tool in the PPE as it can detect up to 88% of general medical conditions and 67%–75% of musculoskeletal conditions (2). The most recent version of the PPE monograph, Version 5 published in 2019, provides updated, simpler, and shorter history forms and should be completed in concordance with the athlete's parent or guardian if they are a minor (2). In addition to a thorough and complete review of symptoms, specific areas should be focused on as detailed below. While we will focus on the recommendations within the authors' country of practice, the international standards as they relate to the ACSM recommendations will be explored briefly at the end of this section.
Cardiovascular issues
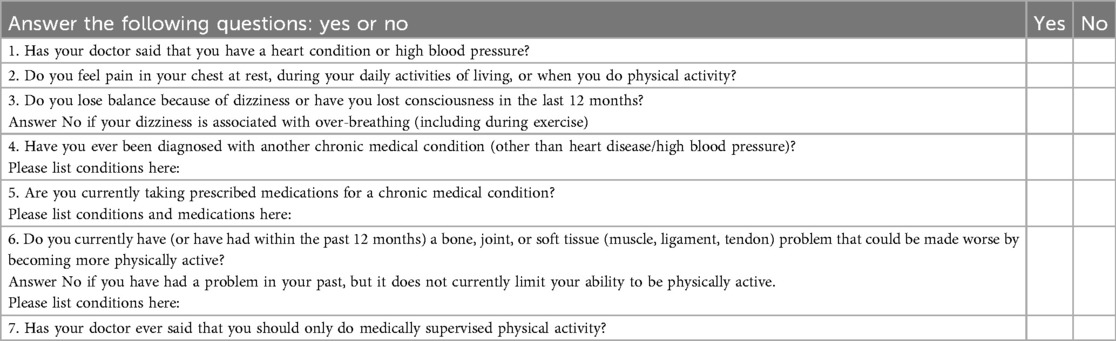
Underlying congenital or acquired cardiac malformation continue to account for the vast majority of sudden deaths in athletes younger than 35 years of age (6). There has been much debate about how best to identify patients who may be at increased risk for sudden cardiac death (SCD). Recommendations from the Choosing Wisely Campaign include not ordering annual electrocardiography or any other cardiac screening test for asymptomatic, low risk patients. Screening is recommended to occur during the PPE at a minimum of every three years. There are four main screening questions, in addition to the formal American Heart Association evaluation that has been updated since our last recommendation to include 14 items consisting of 10 historical factors and four physical examination factors (Table 1) (7). The four main screening questions are as follows (8):
1. Have you ever fainted, passed out, or had an unexplained seizure suddenly and without warning, especially during exercise or in response to sudden loud noises, such as doorbells, alarm clocks, and ringing telephones?
2. Have you ever had exercise-related chest pain or shortness of breath?
3. Has anyone in your immediate family (parents, grandparents, siblings) or other more distant relatives (aunts, uncles, cousins) died of heart problems or had an unexpected sudden death before age 50 years? This would include unexpected drownings, unexplained car accidents in which the relative was driving, or sudden infant death syndrome.
4. Are you related to anyone with HCM or hypertrophic obstructive cardiomyopathy, Marfan syndrome, AC, LQTS, short QT syndrome, Brugada syndrome or CPVT, or a condition requiring implantation of a pacemaker or ICD at younger than 50 years?
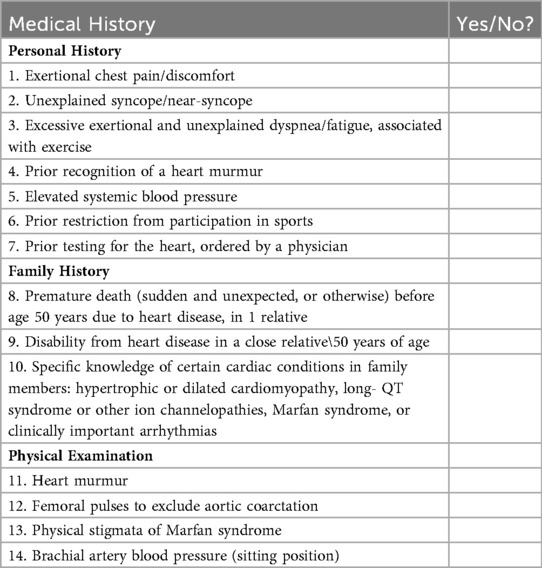
Table 1. The 14-Element American Heart Association Recommendations for Preparticipation Cardiovascular Screening of Competitive Athletes (7).
Pulmonary issues
There are no significant updates to our previously published recommendations for pulmonary issues. Asthma is a chronic inflammatory disorder of the airways characterized by bronchial hyperresponsiveness leading to intermittent dyspnea, coughing, and wheezing. It is among the most frequent chronic diseases among children and adolescents in the United States (9). Exercise-induced bronchoconstriction describes the transient narrowing of the airways after exercise that is common even in athletes without a diagnosis of asthma. The prevalence of asthma and exercise induced bronchoconstriction among athletes has been estimated to be between 30% and 70% among elite athletes depending on the type of sports performed (10). As such, the team physician should be familiar with the management of this condition. Peak flow measurements may be recorded at the beginning of the season to serve as a baseline for future asthma exacerbations. Short-acting bronchodilators are the mainstay of treatment for intermittent asthma. Patients should have short-acting bronchodilators available for use at home and at school, and ideally a bronchodilator should be kept with a trainer or coach. Make a referral to primary care and consider a pulmonology consult for athletes requiring long-acting bronchodilators or corticosteroids for asthma control.
Musculoskeletal health
A full musculoskeletal history includes careful review of prior injuries, including mechanism, severity, treatment, and any resulting disability. Prior injury or surgery is a known risk factor for reinjury of a given body part and should direct detailed physical examination of the affected areas. Several studies have demonstrated that athletes who underwent a knee surgery prior to college require more MRIs and have increased rates of knee injury and knee surgery, with a recent study by Falstrom et al. reported as high as 38% of female soccer players who sustained an ACL injury went on to sustain a second ACL injury (11, 12). Additionally, in a cohort comprised of men's football, women's basketball, soccer, and lacrosse players at the collegiate level, it was found that lower extremity musculoskeletal injuries occurred at a higher rate (50%) in previously concussed athletes compared to those athletes that had no history of concussion (20% <0.01) (13). In recognizing prior injury patterns, practitioners can develop athlete-specific rehabilitation and prevention programs (14).
Medications and supplements
All medications, including over the counter drugs and supplements should be reviewed for possible adverse effects. Additionally, recent changes in the NCAA regulations of banned medications or supplements should be reviewed (Table 2) (15). Most notably, cannabinoids were removed from the banned substances list in 2023. The physician and athlete should be aware of which medications require documentation of medical necessity, such as methylphenidate for attention deficit/hyperactivity disorder. Using the banned substances list provided, the physician has the opportunity to discuss possible elicit use that would disqualify the athlete. Medications that are required for chronic conditions should additionally be documented for exemption, such as diuretics or rate controlling medications for cardiac conditions. These medications can affect fluid status and should be monitored in the setting of athletic exertion.
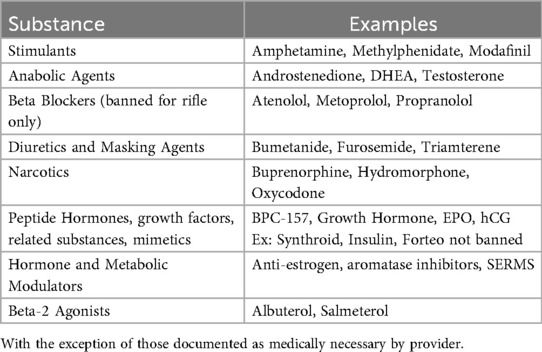
Table 2. Banned drugs and substances according to the National Athletic Association (15).
The last decade has seen a decrease in the prevalence of performance-enhancing drug use, though there has been an increase in blood doping amongst youth athletes (16). Reasons for continued use include getting an edge and improve athletic performance by increasing energy, maintaining health and nutrition, and speeding up recovery. Team physicians covering youth sports should be familiar with common ergogenic drugs and supplements, such as anabolic-androgenic steroids (AASs), human growth hormone (hGH), creatine, amphetamines, and erythropoietin (EPO), thus facilitating an open discussion with athletes about the performance benefits of these agents in contrast with the adverse effects and complications that can occur from their use. The PPE in many cases is an appropriate time to ask about ergogenic drug use. The CRAFFT questionnaire (Table 3) (17) is a validated health screening tool that can be used to evaluate for substance use, related driving risk, and possible substance use disorder for youths age 12–21 (18). An affirmative answer to two or more of questions 4–9 suggest a more serious problem and require further assessment by the primary care provider. The graph included here (Figure 1) should be discussed, with motivational interviewing attempted, prior to a referral to psychiatry or addiction medicine if the risk remains high (18). Our previous publication reviews anabolic-androgenic steroids, human growth hormone, creatine, stimulants, and erythropoietin and blood doping in detail and can be used as a guide for understanding the potential usage and adverse effects associated with each.
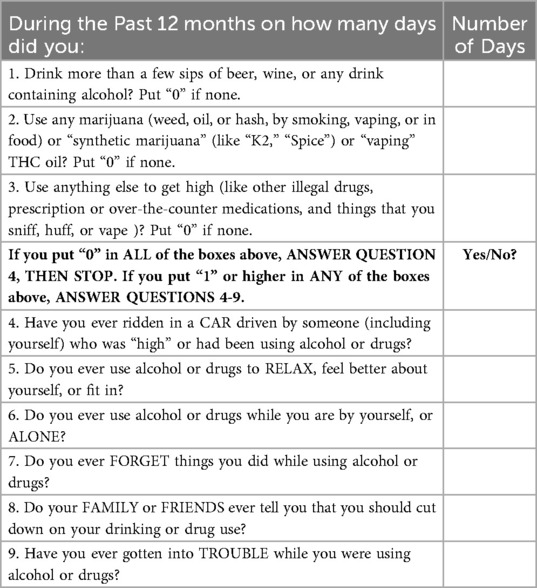
Table 3. CRAFFT Questionnaire (17).
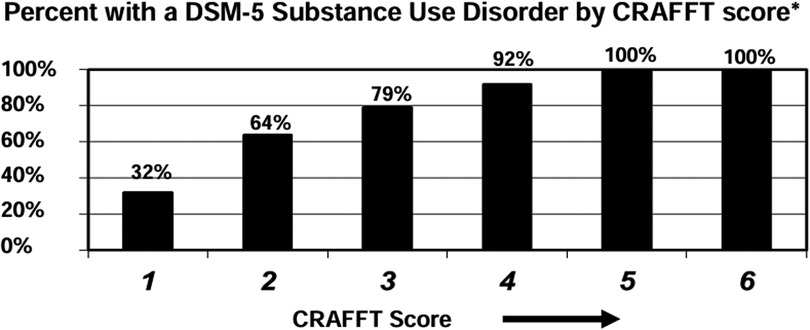
Figure 1. CRAFFT score interpretation: percentage with a DSM-5 substance use disorder by CRAFFT score.
Allergies
A patient's allergens (both medication and environmental) and the nature of the reaction should still be reviewed. A history of anaphylactic reaction may require the presence of self-administered epinephrine (e.g., EpiPen; Mylan LP) at all activities.
Metabolic/nutritional health
Screening for the female athlete triad has expanded and evolved over the last decade. The recommendation is now to screen for relative energy deficiency in sport (RED-S), an all-encompassing syndrome first introduced by the International Olympic Committee in 2014, that occurs when energy expenditure is disproportionately high relative to caloric intake (2, 19). Low energy availability is the underlying issue in both the female athlete triad and RED-S and is associated with poor performance, decreased power, delayed recovery and injury resolution in the short term, but in the long term can lead to multi-organ system dysfunction. While the previous screening focused solely on female athletes, RED-S can be evaluated for in all athletes and is characterized by relative energy deficiency, low bone mineral density, impaired psychological, immune, and cardiovascular health. It is reported that RED-S affects 22%–58% of male and female adolescent athletes (20). As with the endocrinopathy seen in the female athlete triad, menstrual dysfunction is an important contributory aspect of RED-S. The equivalent in male athletes is low testosterone levels and erectile dysfunction. Screening for eating disorders, symptoms of low estrogen or low testosterone, and symptoms of low energy such as fatigue or delayed recovery, should be included for both the female and male athlete. A history of stress fractures or overuse injury should raise suspicion for osteopenia or osteoporosis and may warrant laboratory workup or evaluation by an endocrinologist (19). There are conditions that can mimic or mask RED-S, such as pregnancy or iron deficiency anemia, that should be evaluated for as indicated.
Psychological evaluation
Recently, a cyclical correlation has been described between mental health of the athlete, injury risk, and delayed injury recovery. An AJSM study of NCAA athletes found a significant relationship between anxiety/depressive symptoms during the preseason period and subsequent risk of injury to the athlete, and this has been described in various cohorts from the youth to elite levels (21, 22). The cycle of mental health and injuries extends to post-operative outcomes after sports related injuries with pre-operative mental and physical health scored on the Short-Form Health Survey being predictive of return-to-play after ACL reconstruction and rotator cuff repair (23). This evidence points towards a benefit in being able to identify and potentially intervene with athletes that are at-risk from a mental health perspective. In 2020, the American Medical Society for Sports Medicine released a consensus statement with recommendations for identifying psychological factors as risk factors for poor outcomes after athletic injury (23). Given the correlation between depression/anxiety and risk of injury and/or prolonged recovery, we recommend using two simple screening tools to identify those athletes that are at risk. For depression, the PHQ-9 has been validated in identifying depression (Table 4) (24), while the GAD-7 can be used to screen for anxiety (Table 5) (26). For both scales, a score equal to or greater than 5 is considered mild depression and anxiety respectively, and should trigger the provider to have heightened awareness with these athletes. Additional check-ins and monitoring for worsening of symptoms can be done using the scales provided and a score of 10 or higher on either, indicates the need referral to a mental health professional (27, 28).
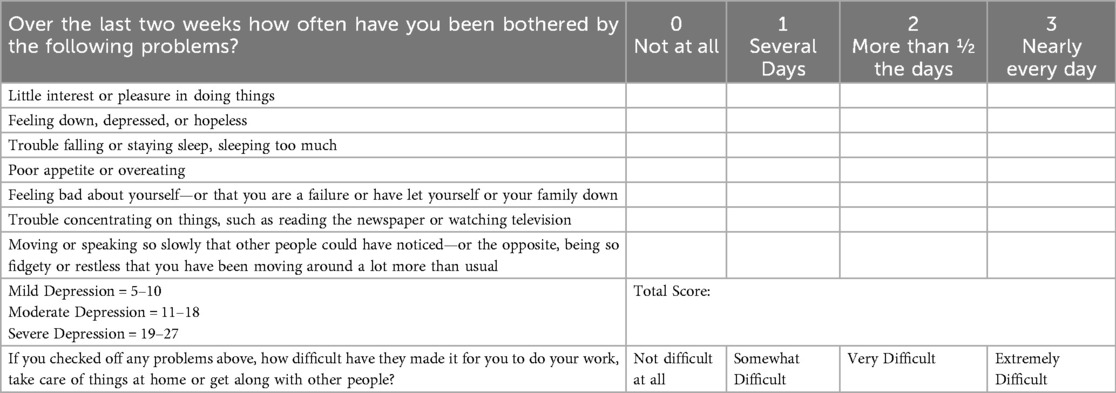
Table 4. PHQ9 (24).
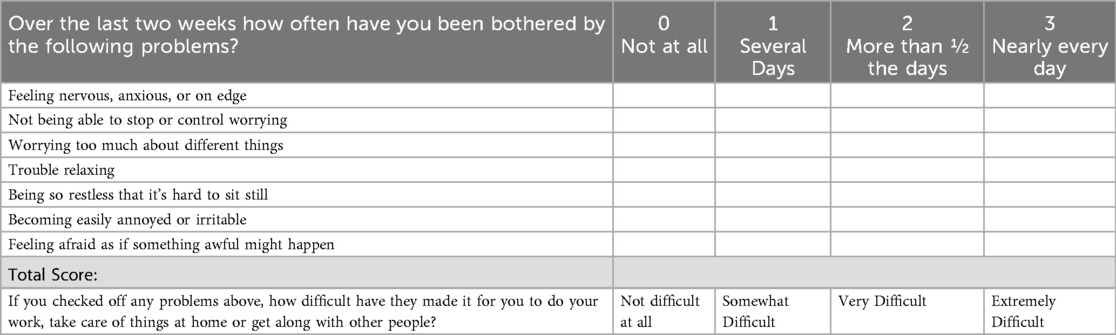
Table 5. GAD7 (25).
Sport hours per week
In the last decade, sport specialization has reached a fever pitch among adolescent athletes. Participation in intensive training, focused on a single sport, has become the new norm in the highly competitive youth sports world (29). Both the American Orthopaedic Society for Sports Medicine and the International Olympic Committee have published consensus statements advising against excessive participation in a single sport, specifically in a prepubertal population given concerning physical and mental health concerns including overuse injuries, burnout, and decreased athletic development (29, 30). Despite these prior warnings, the trend of specialization continues, and recent research has confirmed the correlation between overuse injury risk with higher degrees of sport specialization (31). While sport specialization may be inevitable in the older athlete, especially as they approach the collegiate level, there is still concern regarding the sheer number of hours played; A longitudinal case-control study published in the Orthopaedic Journal of Sports Medicine followed athletes aged 7–18 years and found a higher proportion of injuries in athletes that (1) trained more hours per week than their age and (2) had a ratio of training hours to free play hours that exceeded 2:1 (31). Further studies have provided support for the dose response relationship between hours per week and injury risk, specifically 3–7 h per week carried a significantly lower risk than 12 or more hours per week (32). As such, the number of weekly hours spent on their sport, as well as hours of free play per week, is an important screening question to ask youth athletes to establish their future injury risk profile.
The international perspective
The general medical history that is recommended across international governing bodies in relation to young competitive athletes does not diverge from those previously discussed. For recreational athletes, the 2021 ACSM recommendations reference self-administered Physical Activity Readiness Questionnaire (PAR-Q+), the international standard for risk stratification and screening (33). In response to the call to increase physical activity as a means of managing and preventing chronic disease, the PAR-Q was originally developed in Canada in 1970 and consisted of seven binary questions to evaluate the everyday person prior to engaging in exercise (34). It became widely used as a general screening, but it was only applicable to those ages 15–69 and ultimately had the opposite of the desired effect as it over-screened individuals out of increasing their physical activity (34). Maintaining the initial seven questions, it was revised and expanded with evidence-based consensus to the PAR-Q + in 2010 (Table 6) (34, 35). This instrument has been translated and validated in several difference languages and has allowed a variety of populations to safely start or increase physical activity participation. A recent study out of Brazil highlighted the simple, self-determined clearance pathway that allowed participants to pursue unrestricted activity vs. recommended physician consultation, based on their results (35).
Both the PPE as discussed here, and the PAR-Q + are tools for assessing physical readiness. However, the PPE is a comprehensive and physician-led clinical exam targeted towards athletes, while the PAR-Q + is a simpler self-screening tool intended to provide general recommendations prior to initiating any physical activity (35). Although the PAR-Q + is an internationally recognized screening tool, it is important to note that an international collaboration of organizations did not recommend any more formal preparticipation evaluation for those intending to be physically active at light to moderate intensity (36). The competitive youth athlete stands to benefit from more rigorous screening than just the PAR-Q + .
Physical exam
The majority of our recommendations for physical examination of the young athlete from our prior publication remain relevant, with a focus on ensuring that the athlete can safely participate in a sport without the risk of incurring a new or worsening injury. Athletes should still undergo a comprehensive physical examination with the addition of advanced cardiac examination, concussion management and baseline testing, and laboratory evaluation for sickle cell disease as indicated. We provide key updates to our previously published recommendations below and discuss the key difference in international preparticipation recommendations that largely arise within the cardiac evaluation.
Advanced cardiac evaluation
The cardiovascular physical exam should focus on identifying concerning findings such as pathologic heart murmurs or the clinical findings associated with Marfan syndrome. Our previous recommendations discussed the need for routine advanced cardiac evaluation, exploring the controversies associated with mandated ECG and echocardiography for each athlete (1). While sudden cardiac death (SCD) is relatively rare, with a recent JAMA article citing a nearly 70% decrease in SCD rates between 2002 and 2022 in the NCAA (6), it is still a devastating outcome that must be prevented through thorough screening. As outlined in the medical history, a thorough cardiac history is vital to assessing an athlete's cardiac risk profile, however a recent study published in 2023 by Blank et al. found that, despite 48 states having PPE evaluation forms available online, only 14 included all 14 AHA screening elements (37). The majority of European and international guidelines recommend universal inclusion of ECG while American guidelines, citing high costs and false positive rates, recommend that it be considered only in certain cohorts. Specifically, the 2023 investigation into SCD in NCAA athletes by the American Heart Association found that male athletes carry a 4-fold risk and black athletes a 3-fold risk compared to their counterparts (6). Additionally, a recent four year analysis of all US competitive athletes confirmed trends reported in prior studies that highlighted a significantly higher annual incidence rate of sudden cardiac arrest and sudden cardiac death in male basketball and American football players (38). This highlights the greatest divergence in international recommendations from the American guidelines we focus on in this review and is exemplified by the current recommendations in Italy. A prospective cohort study completed in Veneto (Italy) is the basis for the European Society of Cardiology recommendation that routine, annual screening ECG be done for every athlete (39, 40). The observational study, carried out between 1982 and 2004 reported an 89% decrease in the incidence of SCD in athletes following the implementation of a mandated screening that included an ECG (40). However, the observational nature, lack of multiple control groups, and possible confounding from improved management of athletes across the study period raise concerns about the predictive value of including the ECG routinely (6). While the AHA upholds that ECG should not be included in routine cardiac screening of all athletes, they do point toward possible inclusion for the higher risk athletes previously highlighted and further emphasizes the heightened importance of secondary prevention methods and emergency response protocols within these populations (6). Universally, advanced multimodal imaging such as echocardiography is not recommended. There needs to be close evaluation of the athlete, with referral to cardiology if significant risk is assessed.
Concussion management and baseline testing
The reported incidence of concussions in young athletes has increased over the last decade, in part due to increased awareness, improved diagnostics, and higher likelihood of symptoms reporting. A study found a 2.2-fold increase in the number of concussions reported in high school athletes in the last decade (41). Recent studies published in JAMA indicate that in children aged 5–7, 43% of concussions are sport-related, increasing to 68% in children aged 8–12 (42). American Football continues to be the leading cause of concussions among young athletes, accounting for 45.3% of those reported from 2012 to 2021 and this does not account for the serious concern for underreporting when it comes to concussions in sport (43). This emphasizes the importance of including concussion management and baseline testing in the PPE.
While concussion can be a difficult diagnosis due to the several biomechanical forces and alteration in mental status, there are several different assessment tools that can be used. Currently baseline concussion testing is recommended by the American Academy of Neurology as well as the US Centers for Disease Control and Prevention in order to establish scores that the athlete can be compared to when there is concern for concussion. A recent JBJS Critical Analysis Review outlines the current status of concussion assessment scales and recommends the King-Devick (KD), child Sport Concussion Assessment Tool (cSCAT3), child Immediate Post-Concussion Assessment and Cognitive Testing cImPACT), and the Vestibular Oculomotor Screening (VOMS) tests to evaluate for concussion in the pediatric athlete. The KD serves as a screening test along with the Standardized Assessment of Concussion (SAC) and the Balance Error Scoring System (BESS) (44).
As the vast majority of concussion symptoms are not easily observable, reported symptoms continue to be the most accurate indicator of concussion as established by a recent JAMA case-control study (45). concussion nondisclosure continues to be a barrier to protecting athletes from the potentially catastrophic sequelae of concussive head impacts. The risks of underreporting symptoms in young athletes range from relapse of concussion symptoms with premature return to sport or return to the classroom to the catastrophic possibility of long-term neuropathologic disorders such as chronic traumatic encephalopathy (CTE) (46, 47). A ground-breaking 2023 JAMA Neurology study found that greater than 40% of contact sport athletes younger than 30 years at the time of death had evidence of CTE, with all participants demonstrating behavioral changes prior to their death (47). It has been reported that one in four athletes experiences pressure to continue to play after a head impact, while nearly half of athletes continue playing with symptoms of a possible concussion (48). Thus, educating youth athletes about possible concussion symptoms, and emphasizing the importance of honest symptom reporting if the athlete does incur a head injury is a vital aspect of this portion of the PPE.
Jump tests
Historically, the drop box vertical jump test has been widely used to clinically assess ACL injury risk. The athlete would drop from a 1-ft box and maximally jump upon landing. Visual assessment of the knee separation distance, knee flexion, and landing mechanics were used by examiners to classify athletes as high, medium, or low risk of noncontact anterior cruciate ligament injuries (49). However, more recent prospective and 3-D motion analysis studies have suggested that these tests cannot accurately predict injury risk. Specifically, one prospective cohort study of 880 female athletes found that visual assessment of hip and knee control during the drop box vertical jump test, as well as the single-leg squat test, was not associated with accurately predicting anterior cruciate ligament injury risk (50). In most studies, observers over-predicted who might be at risk of an ACL injury. However, there is an argument that given the simplicity of the test and the global benefits that can be derived from the recommended neuromuscular training after a positive test, there still may be utility in completing the drop box vertical jump test (51). A 2022 scoping review of all screening tests for ACL injury highlighted these controversial aspects of jump tests and recommended 3D kinematics and kinetics to increase the utility of the drop box vertical jump test, a notion supported by a 2023 laboratory study published in the Orthopaedic Journal of Sports Medicine (52, 53). However, we recognize that the inclusion of 3D analysis is not feasible for all providers completing the PPE. The drop box vertical jump test continues to demonstrate good to excellent intra-rater reliability and can still be used as a screening test with emphasis on increased knee valgus being associated with future ACL injury (54). Despite its lack of specificity, a positive test can still identify abnormal landing mechanics and help tailor neuromuscular training programs to eliminate asymmetries. However, further research is needed on feasible, multiplanar field-based tests to better evaluate possible deficiencies that can predict injury.
Laxity
Generalized joint laxity (GJL) is a condition in which synovial joints range beyond normal limits. There has been a lot of discussion regarding the potential risks, and benefits, of GJL in young athletes. GJL allows for greater flexibility, thus potentially benefitting dancers, figure skaters, and gymnasts, with rates of GJH amongst these populations reaching greater than 60% (55). However, several studies have also indicated that GJL increases the risk of musculoskeletal injury and prolongs the recovery time for these athletes (55). Specifically, athletes who participate in contact sports and have GJL are at higher risk for ligamentous injuries (odds ratio 4.7, Pacey et al.) (56, 57). A recent JBJS review highlights the importance of screening patients for GJL using the Beighton and Horan Criteria (Table 7) (55). For young athletes this screening can elucidate a potential risk factor that can be mitigated by joint-stabilizing strength training and injury prevention. We recommend all athletes, both contact and non-contact be screened. A positive Beighton score is ≥6 in pre-pubertal athletes and ≥5 in post-pubertal athletes (58) and should trigger a discussion regarding the risk of injury associated with overtraining joint flexibility rather than stability (59). Physical therapy can be initiated with a focus on joint stability, core strengthening, proper form and biomechanics in proprioceptive and balancing exercises in order to decrease injury risk (60).
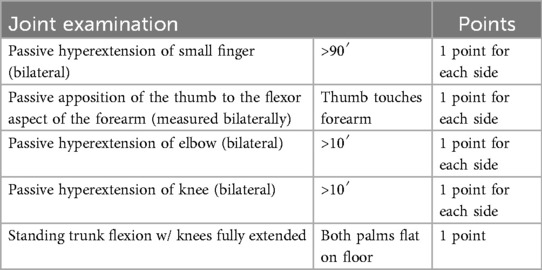
Table 7. Beighton-Horan criteria for generalized hypermobility (total score/9) (58).
Evidence review of the PPE
Despite the evolving landscape of youth sports and the PPE over the last decade, there have been no major advancements in the evidence base for the PPE. Similar to a decade ago, while the importance of the PPE is universally accepted, the lack of standardization and limited evidence of efficacy persists. While it still stands that only a small percentage of athletes are prevented from participating in sport after the PPE, beyond acting as a screening, it has the potential to act more as an optimization for each athlete and allow for quick action if they face unexpected changes in their physical, mental, and musculoskeletal health. It continues to be widely performed and is mandated by The Special Olympics, most state high school athletic associations and the National Collegiate Athletic Association (2). Corrente et al. recently published a study evaluating the current practice with regards to the MSK screening exam within the PPE and found that while 82% were familiar with the AAP PPE Monograph, only 42% felt that it screened for future injury, while 26% did not perform a physical exam at all (61). This highlights the importance of orthopedic surgeons, and the multidisciplinary teams that collaborate in the care of young athletes, being aware and involved in the PPE. Further emphasized is the need for further research and consistent implementation of evidence-based guidelines. Future establishment of the predictive value for injury prevention of the PPE will require a more standardized, algorithmic approach to its evaluation. Randomized controlled trials comparing the inclusion of various pre-participation screening tools and their implementation in diverse, international settings will aid in establishing the validity of various aspects. Only then will mandates be able to be made regarding its universal use in youth athletics.
Summary
A decade has passed since our last recommendations on the PPE for orthopedic surgeons and in that time, we have seen an increase in young athletes participating in sport on the scale of millions. This highlights the importance of the PPE now more than ever, especially as young athletes become more specialized, and potentially more prone to orthopedic injury. The orthopedic surgeon should be aware and capable of completing a thorough and complete PPE in order to aid in the care of these young athletes. This review provides key updates to our previous recommendations while highlighting the controversies that continue to exist. The PPE evolves with our population of athletes and still requires further standardization and high-quality validation. However, we can still come together in helping young athletes pursue sport at their desired level by identifying social, behavioral, medical, and musculoskeletal conditions that may prohibit them from doing so.
Author contributions
GP: Investigation, Writing – review & editing, Methodology, Conceptualization, Data curation, Writing – original draft. DM: Writing – review & editing. RC: Writing – review & editing. DT: Writing – review & editing. LR: Writing – review & editing. WL: Writing – review & editing. CA: Writing – review & editing. CP: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Miller DJ, Blum AB, Levine WN, Ahmad CS, Popkin CA. Preparticipation evaluation of the young athlete: what an orthopaedic surgeon needs to know. Am J Sports Med. (2016) 44(6):1605–15. doi: 10.1177/0363546515598994
2. MacDonald J, Schaefer M, Stumph J. Preparticipation physical evaluation 5th edition. Am Acad Pediatr. (2019):539–46. PMID: 33929170
3. Ahlquist S, Cash BM, Hame SL. Associations of early sport specialization and high training volume with injury rates in national collegiate athletic association division I athletes. Orthop J Sports Med. (2020) 8(3):2325967120906825. doi: 10.1177/2325967120906825
4. Haraldsdottir K, Watson AM. Psychosocial impacts of sports-related injuries in adolescent athletes. Curr Sports Med Rep. (2021) 20(2):104–8. doi: 10.1249/JSR.0000000000000809
5. Ronshaugen N, Moffatt K. Reviewing value, timing of the preparticipation physical evaluation. NFHS.org. (2024). Available online at: https://www.nfhs.org/articles/reviewing-value-timing-of-the-preparticipation-physical-evaluation/
6. Petek BJ, Churchill TW, Moulson N, Kliethermes SA, Baggish AL, Drezner JA, et al. Sudden cardiac death in national collegiate athletic association athletes: a 20-year study. Circulation. (2024) 149(2):80–90. doi: 10.1161/CIRCULATIONAHA.123.065908
7. Maron BJ, Friedman RA, Kligfield P, Levine BD, Viskin S, Chaitman BR, et al. Assessment of the 12-lead ECG as a screening test for detection of cardiovascular disease in healthy general populations of young people (12–25 years of age): a scientific statement from the American Heart Association and the American College of Cardiology. Circulation. (2014) 130(15):1303–34. doi: 10.1161/CIR.0000000000000025
8. Spencer R, Quraishi S. Athlete screening and sudden cardiac death. Pediatr Rev. (2023) 44(12):669–81. doi: 10.1542/pir.2023-005975
9. Cloutier MM, Dixon AE, Krishnan JA, Lemanske RF Jr, Pace W, Schatz M. Managing asthma in adolescents and adults: 2020 asthma guideline update from the national asthma education and prevention program. JAMA. (2020) 324(22):2301–17. doi: 10.1001/jama.2020.21974
10. Louis-Philippe B, O’Byrne Paul M. Asthma and exercise-induced bronchoconstriction in athletes. N Engl J Med. (2015) 372(7):641–8. doi: 10.1056/NEJMra1407552
11. Fältström A, Hägglund M, Kvist J, Mendonça LD. Risk factors for sustaining a second ACL injury after primary ACL reconstruction in female football players: a study investigating the effects of follow-up time and the statistical approach. Sports Med Open. (2023) 9(1):29. doi: 10.1186/s40798-023-00571-x
12. Rugg CM, Wang D, Sulzicki P, Hame SL. Effects of prior knee surgery on subsequent injury, imaging, and surgery in NCAA collegiate athletes. Am J Sports Med. (2014) 42(4):959–64. doi: 10.1177/0363546513519951
13. Herman DC, Jones D, Harrison A, Moser M, Tillman S, Farmer K, et al. Concussion may increase the risk of subsequent lower extremity musculoskeletal injury in collegiate athletes. Sports Med. (2017) 47(5):1003–10. doi: 10.1007/s40279-016-0607-9
14. Brenner JS, Watson A, MEDICINE COS, FITNESS. Overuse injuries, overtraining, and burnout in young athletes. Pediatrics. (2024) 153(2):e2023065129. doi: 10.1542/peds.2023-065129
15. National Collegiate Athletic Association. NCAA banned substances. National Collegiate Athletic Association. (2025–26). Available online at: https://ncaaorg.s3.amazonaws.com/ssi/substance/2025-26/2025-26NCAA_BannedSubstances.pdf
16. Miech RA, Johnston LD, Patrick ME, O’Malley PM. Monitoring the future national survey results on drug use, 1975–2024: overview and detailed results for secondary school students. In: US Department of Health and Human Services, editors. Monitoring the Future Monograph Series Institute for Social Research. Michigan: University of Michigan (2024). p. 53–86.
17. Mitchell SG, Kelly SM, Gryczynski J, Myers CP, O’Grady KE, Kirk AS, et al. The CRAFFT cut-points and DSM-5 criteria for alcohol and other drugs: a reevaluation and reexamination. Subst Abus. (2014) 35(4):376–80. doi: 10.1080/08897077.2014.936992
18. McCarty CA, Levy S, Harris SK. Alcohol use screening and behavioral counseling with adolescents in primary care: a call to action. JAMA Pediatr. (2019) 173(1):12–4. doi: 10.1001/jamapediatrics.2018.4171
19. Heikura IA, Mountjoy ML, Ackerman KE, Bailey DM, Burke LM, Constantini N, et al. International Olympic committee relative energy deficiency in sport clinical assessment tool 2 (IOC REDs CAT2). Br J Sports Med. (2023) 57(17):1068–9. doi: 10.1136/bjsports-2023-107549
20. Biese KM, Winans M, Rudek G, Cadmus-Bertram L, Andreae S, Brooks MA, et al. Sport specialization and sport motivation in middle school-aged athletes. J Athl Train. (2024) 59(3):274–80. doi: 10.4085/1062-6050-0690.22
21. Li H, Moreland JJ, Peek-Asa C, Yang J. Preseason anxiety and depressive symptoms and prospective injury risk in collegiate athletes. Am J Sports Med. (2017) 45(9):2148–55. doi: 10.1177/0363546517702847
22. Timpka T, Jacobsson J, Bargoria V, Périard JD, Racinais S, Ronsen O, et al. Preparticipation predictors for championship injury and illness: cohort study at the Beijing 2015 international association of athletics federations world championships. Br J Sports Med. (2017) 51(4):271–6. doi: 10.1136/bjsports-2016-096580
23. Chang CJ, Putukian M, Aerni G, Diamond AB, Hong ES, Ingram YM, et al. Mental health issues and psychological factors in athletes: detection, management, effect on performance, and prevention: American Medical Society for Sports Medicine Position Statement. Clin J Sport Med. (2020) 30(2):e61–87. doi: 10.1097/JSM.0000000000000817
24. Keenan L, Ingram Y, Green B, Daltry R, Harenberg S. Validation and clinical utility of the patient health questionnaire-9 and center for epidemiologic studies depression scale as depression screening tools in collegiate student-athletes. J Athl Train. (2023) 58(10):821–30. doi: 10.4085/1062-6050-0558.22
25. Perez-Pedrogo C, Sanchez-Cardona I, Castro-Diaz B, Lopez-Torres S. Psychometric properties of the generalized anxiety disorder 7-item scale in adolescents: an effective screening tool for school and community settings. P R Health Sci J. (2022) 41(4):226–32. PMID: 3651620936516209
26. Sanfilippo JL, Haralsdottir K, Watson AM. Anxiety and depression prevalence in incoming division I collegiate athletes from 2017 to 2021. Sports Health. (2024) 16(5):776–82. doi: 10.1177/19417381231198537
27. Fonseca-Pedrero E, Díez-Gómez A, Pérez-Albéniz A, Al-Halabí S, Lucas-Molina B, Debbané M. Youth screening depression: validation of the patient health questionnaire-9 (PHQ-9) in a representative sample of adolescents. Psychiatry Res. (2023) 328:115486. doi: 10.1016/j.psychres.2023.115486
28. Mossman SA, Luft MJ, Schroeder HK, Varney ST, Fleck DE, Barzman DH, et al. The generalized anxiety disorder 7-item scale in adolescents with generalized anxiety disorder: signal detection and validation. Ann Clin Psychiatry. (2017) 29(4):227–34A. doi: 10.1177/104012371702900404
29. LaPrade RF, Agel J, Baker J, Brenner JS, Cordasco FA, Côté J, et al. AOSSM early sport specialization consensus statement. Orthop J Sports Med. (2016) 4(4):2325967116644241. doi: 10.1177/2325967116644241
30. Bergeron MF, Mountjoy M, Armstrong N, Chia M, Côté J, Emery CA, et al. International Olympic committee consensus statement on youth athletic development. Br J Sports Med. (2015) 49(13):843–51. doi: 10.1136/bjsports-2015-094962
31. Jayanthi N, Kleithermes S, Dugas L, Pasulka J, Iqbal S, LaBella C. Risk of injuries associated with sport specialization and intense training patterns in young athletes: a longitudinal clinical case-control study. Orthop J Sports Med. (2020) 8(6):2325967120922764. doi: 10.1177/2325967120922764
32. Shigematsu R, Katoh S, Suzuki K, Nakata Y, Sasai H. Risk factors of sports-related injury in school-aged children and adolescents: a retrospective questionnaire survey. Int J Environ Res Public Health. (2022) 19(14):8662. doi: 10.3390/ijerph19148662
33. Ozemek C, Bonikowske A, Christle J, Gallo P. ACSM’s) Guidelines for Exercise Testing and Prescription. 12th ed. Philadelphia, PA: Lippincott Williams & Wilkins (2025). p. 200–20.
34. Warburton DER, Jamnik VK, Bredin SSD, Gledhill N, PAR-Q+ research collaboration. The physical activity readiness questionnaire (PAR-Q+) and electronic physical activity readiness medical examination (ePARmed-X+). Health Fitness J Can. (2011) 4:3–23. doi: 10.14288/hfjc.v4i2.103
35. Schwartz J, Oh P, Takito MY, Saunders B, Dolan E, Franchini E, et al. Translation, cultural adaptation, and reproducibility of the physical activity readiness questionnaire for everyone (PAR-Q+): the Brazilian Portuguese version. Front Cardiovasc Med. (2021) 8:712696. doi: 10.3389/fcvm.2021.712696
36. Thornton JS, Frémont P, Khan K, Poirier P, Fowles J, Wells GD. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian academy of sport and exercise medicine. Clin J Sport Med. 2016 26(4):259–65.27359294
37. Blank ZJ, Spicer RL, Robinson JA. Preparticipation state cardiac screening forms for athletes. Pediatrics. (2022) 151(1):e2022056798. doi: 10.1542/peds.2022-056798
38. Peterson DF, Kucera K, Thomas LC, Maleszewski J, Siebert D, Lopez-Anderson M, et al. Aetiology and incidence of sudden cardiac arrest and death in young competitive athletes in the USA: a 4-year prospective study. Br J Sports Med. (2021) 55(21):1196–203. doi: 10.1136/bjsports-2020-102666
39. Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. (2006) 296(13):1593–601. doi: 10.1001/jama.296.13.1593
40. Corrado D, Basso C, Schiavon M, Thiene G. Screening for hypertrophic cardiomyopathy in young athletes. N Engl J Med. (1998) 339(6):364–9. doi: 10.1056/NEJM199808063390602
41. Schallmo MS, Weiner JA, Hsu W. Assessing trends in the epidemiology of concussions among high school athletes. Orthop J Sports Med. (2017) 5(7 suppl6). doi: 10.1177/2325967117S00439
42. Ledoux AA, Sicard V, Bijelic V, Barrowman N, van Ierssel J, Beer D, et al. Symptom recovery in children aged 5 to 12 years with sport-related and non–sport-related concussion. JAMA Network Open. (2024) 7(12):e2448797. doi: 10.1001/jamanetworkopen.2024.48797
43. Cassinat JJ, Grise A, Aceto M, Wright V. Pediatric concussions in contact sports: a 10-year retrospective analysis of mechanisms and associated symptoms. Orthop J Sports Med. (2024) 12(8):23259671241262009. doi: 10.1177/23259671241262009
44. Kaufman MW, Su CA, Trivedi NN, Lee MK, Nelson GB, Cupp SA, et al. The current status of concussion assessment scales: a critical analysis review. JBJS Rev. (2021) 9(6):e20.00108. doi: 10.2106/JBJS.RVW.20.00108
45. Harmon KG, Whelan BM, Aukerman DF, Hwang CE, Poddar SK, DeLeo A, et al. Diagnosis of sports-related concussion using symptom report or standardized assessment of concussion. JAMA Netw Open. (2024) 7(6):e2416223. doi: 10.1001/jamanetworkopen.2024.16223
46. Carson JD, Diep D, Baker C, Kraft SA, Kuwahara N, Garel A, et al. Relapse of concussion symptoms in the context of premature return to learn and return to play: comparative analysis of 2006 to 2011 and 2011 to 2016. Can Fam Physician. (2022) 68(3):e87–91. doi: 10.46747/cfp.6803e87
47. McKee AC, Mez J, Abdolmohammadi B, Butler M, Huber BR, Uretsky M, et al. Neuropathologic and clinical findings in young contact sport athletes exposed to repetitive head impacts. JAMA Neurol. (2023) 80(10):1037–50. doi: 10.1001/jamaneurol.2023.2907
48. Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc Sci Med. (2015) 134:66–75. doi: 10.1016/j.socscimed.2015.04.011
49. Hewett TE, Myer GD, Ford KR, Slauterbeck JR. Preparticipation physical examination using a box drop vertical jump test in young athletes: the effects of puberty and sex. Clin J Sport Med. (2006) 16(4):298–304. doi: 10.1097/00042752-200607000-00003
50. Petushek E, Nilstad A, Bahr R, Krosshaug T. Drop jump? Single-leg squat? Not if you aim to predict anterior cruciate ligament injury from real-time clinical assessment: a prospective cohort study involving 880 elite female athletes. J Orthop Sports Phys Ther. (2021) 51(7):372–8. doi: 10.2519/jospt.2021.10170
51. Redler LH, Watling JP, Dennis ER, Swart E, Ahmad CS. Reliability of a field-based drop vertical jump screening test for ACL injury risk assessment. Phys Sportsmed. (2016) 44(1):46–52. doi: 10.1080/00913847.2016.1131107
52. Morooka T, Yoshiya S, Tsukagoshi R, Kawaguchi K, Fujioka H, Onishi S, et al. Evaluation of the anterior cruciate ligament injury risk during a jump-landing task using 3-dimensional kinematic analysis versus the landing error scoring system. Orthop J Sports Med. (2023) 11(11):23259671231211244. doi: 10.1177/23259671231211244
53. Schweizer N, Strutzenberger G, Franchi MV, Farshad M, Scherr J, Spörri J. Screening tests for assessing athletes at risk of ACL injury or reinjury-A scoping review. Int J Environ Res Public Health. (2022) 19(5):2864. doi: 10.3390/ijerph19052864
54. Beyer EB, Hale RF, Hellem AR, Mumbleau AM, Schilaty ND, Hewett TE. Inter and intra-rater reliability of the drop vertical jump (DVJ) assessment. Int J Sports Phys Ther. (2020) 15(5):770–5. doi: 10.26603/ijspt20200770
55. Sacks HA, Prabhakar P, Wessel LE, Hettler J, Strickland SM, Potter HG, et al. Generalized joint laxity in orthopaedic patients: clinical manifestations, radiographic correlates, and management. J Bone Joint Surg Am. (2019) 101(6):558–66. doi: 10.2106/JBJS.18.00458
56. Pacey V, Nicholson LL, Adams RD, Munn J, Munns CF. Generalized joint hypermobility and risk of lower limb joint injury during sport: a systematic review with meta-analysis. Am J Sports Med. (2010) 38(7):1487–97. doi: 10.1177/0363546510364838
57. Rejeb A, Fourchet F, Materne O, Johnson A, Horobeanu C, Farooq A, et al. Beighton scoring of joint laxity and injury incidence in middle eastern male youth athletes: a cohort study. BMJ Open Sport Exerc Med. (2019) 5(1):e000482. doi: 10.1136/bmjsem-2018-000482
58. Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. (1969) 51(3):444–53. doi: 10.1302/0301-620X.51B3.444
59. Mehendale S, Mehendale AM, Gakkhar A. A comprehensive case study of a hyperlaxity dilemma: an injury-prone young athlete. Cureus. (2024) 16(3):e56245. doi: 10.7759/cureus.56245
60. Castori M, Tinkle B, Levy H, Grahame R, Malfait F, Hakim A. A framework for the classification of joint hypermobility and related conditions. Am J Med Genet C Semin Med Genet. (2017) 175(1):148–57. doi: 10.1002/ajmg.c.31539
Keywords: preparticipation evaluation, RED-S, preparticipation athlete screening, orthopedic surgeon, athlete safety, injury prevention
Citation: Plassche GC, Miller DJ, Christian RA, Trofa DP, Redler LH, Levine WN, Ahmad CS and Popkin CA (2025) The preparticipation evaluation of the young athlete—an update to what the orthopedic surgeon needs to know. Front. Sports Act. Living 7:1650463. doi: 10.3389/fspor.2025.1650463
Received: 19 June 2025; Accepted: 30 September 2025;
Published: 21 October 2025.
Edited by:
Gerasimos V. Grivas, Hellenic Naval Academy, GreeceReviewed by:
Colin K. Drummond, Case Western Reserve University, United StatesDarren E. R. Warburton, University of British Columbia, Canada
Copyright: © 2025 Plassche, Miller, Christian, Trofa, Redler, Levine, Ahmad and Popkin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Grace C. Plassche, Z2NwMjEyM0BjdW1jLmNvbHVtYmlhLmVkdQ==; Charles A. Popkin, Y3AyNjU0QGN1bWMuY29sdW1iaWEuZWR1
 Grace C. Plassche
Grace C. Plassche Daniel James Miller2,3
Daniel James Miller2,3 Charles A. Popkin
Charles A. Popkin