- 1Institute of Sport, National Research Institute, Warsaw, Poland
- 2Laboratory of Experimental and Applied Microbiology, Fluminense Federal University, Niterói, Brazil
- 3Department of Clinical and Community Sciences, Faculty of Medicine and Surgery, University of Milan, Milan, Italy
- 4School of Sport, Exercise and Health Sciences, Loughborough University, Loughborough, United Kingdom
- 5School of Education, Childhood, Youth and Sport, Faculty of Wellbeing, Education and Language Studies, The Open University, Milton Keynes, United Kingdom
Since traditional, sport-specific training or exercise programs lack sufficient stimulus to improve the function of the respiratory muscle, the rationale for integrating additional respiratory muscle training (RMT) emerged. RMT has the potential to improve intermittent exercise performance in team sports athletes, as proven in multiple studies. This narrative review aims to provide coaches with tools to select the appropriate form of RMT, tailored to the athletes’ needs, using appropriate diagnostic methods, intervention protocols, and devices. Common protocols may include performing 30 inspiratory maneuvers twice a day, five days a week, with resistance-based trainers or engaging in 20–40 min of vigorous ventilation with isocapnic devices every other day. Most of the interventions that positively influence intermittent exercise performance employed inspiratory pressure threshold loading, lasted 6–8 weeks, and relied on a high frequency of training sessions, progressive overload, and relatively high initial resistance (starting intensity). Less-investigated RMT methods, such as tapered flow resistive loading or voluntary isocapnic hyperpnea, should be analyzed in the context of intermittent exercise performance. Moreover, further research addressing RMT and hypoxia, between-gender differences, and athletes with disabilities seems warranted.
Introduction
Team sports have gained immense popularity worldwide, involving millions of participants who engage in dynamic and physically demanding activities (1). Based on global participation, viewership, and cultural significance, disciplines such as soccer (football), basketball, cricket, rugby, hockey, baseball, volleyball, and various types of football are considered the most popular (2, 3). The performance determinants vary to a certain extent depending on the discipline and players’ specific roles (4). However, team-sports athletes are usually required to execute repeated skillful and high-intensity actions such as accelerations, changes in pace and direction, sprints, jumps, and kicks. These efforts are typically performed in cycles of maximal or near-maximal intensity, interspersed with brief recovery periods that may consist of rest or low- to moderate-intensity activity. Such activities often extend over prolonged periods, ranging from one to two hours, placing considerable demands on the athlete's physical capacities (5, 6). Noteworthy, physiological team-sports requirements are closely intertwined with the execution of specific skills, highlighting the complex and multifaceted nature of team-sport performance (7).
The combination of technical skills and physical demands requires athletes to maintain optimal conditioning tailored to the unique challenges of their sport and athlete's roles (4). The interplay between high-intensity actions and recovery periods underscores the importance of targeted physical preparation, enabling athletes to perform effectively and consistently throughout the game (8). Consequently, one of the most emphasized physical training goals is the ability to repeatedly perform intense exercise, often evaluated with the Yo-Yo Tests (YYT) or Repeated Sprint Ability (RSA) assessments (9, 10). The physiology of such testing is driven by the interplay of energy systems, muscle function, and recovery mechanisms (7, 9). RSA relies primarily on the phosphagen (ATP-PCr) system to supply rapid energy during the initial seconds of each sprint, with anaerobic glycolysis contributing as phosphocreatine (PCr) stores become depleted. These systems enable short bursts of high-intensity effort but are limited by the accumulation of metabolic by-products such as hydrogen ions, contributing to fatigue. Compared to RSA tests, which focus predominantly on anaerobic power and fatigue resistance during repeated sprints, the YYT places greater emphasis on sustained aerobic metabolism and recovery between efforts (11). In both tests, recovery between efforts depends heavily on the aerobic system, which supports PCr resynthesis, lactate clearance, and the restoration of muscle pH (7, 11, 12). Additionally, effective intermittent exercise performance requires well-developed neuromuscular efficiency and the ability to resist fatigue-related reductions in motor unit activity (13–15).
No single type of training can be universally recommended as the most effective for enhancing intermittent exercise performance or addressing all the factors contributing to output declines during repeated effort tasks (16). Typically, two recommended training goals are improved single-sprint performance and improved aerobic fitness to enhance the ability to recover between efforts (16). Noteworthy, respiratory muscle training (RMT) may improve intermittent exercise performance (17, 18). RMT is a specific conditioning method designed to enhance the strength and endurance of the muscles involved in breathing. Nicks et al. (19) and Najafi et al. (20) reported that RMT improved intermittent exercise performance in both male and female soccer players (19, 20). Tong et al. (21) noted enhanced tolerance to intense intermittent exercise after both RMT programs and respiratory muscle warm-ups (21). Romer et al. (22) also observed faster recovery time during high-intensity, intermittent exercise in repetitive-sprint athletes (22). More recently, after RMT interventions a decrease in sprint time and improved exercise tolerance during RSA assessments in professional soccer players, as well as increased distance covered by rugby athletes in YYT were reported (23, 24).
On the physiological side, RMT was reported to attenuate the blood lactate concentration, plasma ammonia, and uric acid responses during high-intensity, intermittent exercise. Moreover, it was associated with improved perceptual responses and breathlessness (21, 22). All the relevant studies included in the systematic review from Lorca-Santiago et al. reported significant decreases in perceived exertion during RSA and YYT, from 8% to 29%, with large effect sizes (18). Moreover, the mechanistic explanation may be associated with attenuated respiratory metaboreflex and improved blood flow to limb muscles during high intensity, as reported in professional women soccer players (25). Although not easy to observe in applied environments, the respiratory metaboreflex is widely associated with performance improvements originating from RMT. The practical implications stem from findings that fatigue and metabolite accumulation in respiratory muscle lead to reduced blood flow to skeletal muscles, redirecting it toward the respiratory muscle (26). This results in vasoconstriction in the active limbs during exercise, contributing to increased local fatigue and performance limitations (27). RMT enhances respiratory muscle function and is anticipated to counteract the negative effects of the metaboreflex, thereby reducing its systemic impact.
Traditional sport-specific training or exercise programs lack sufficient stimulus to improve the function of the respiratory muscles, underscoring the rationale of integrating additional RMT into training regimens (28, 29).
Training methods and equipment
A wide range of RMT methods and devices are available, with three key approaches demonstrating significant benefits in athletic contexts: inspiratory pressure threshold loading (IPTL), tapered flow resistive loading (TFRL), and voluntary isocapnic hyperpnea (VIH). While TFRL and IPTL are primarily linked to enhanced respiratory muscle strength, VIH is more closely associated with improvements in respiratory muscle endurance (29). Specifically, IPTL and TFRL result in larger improvements in maximal inspiratory pressures, and VIH was associated with improved maximal voluntary ventilation, significant flow rates, and high velocities of respiratory muscle contraction (17). Illustrative application of both approaches is presented in Figure 1 (30).
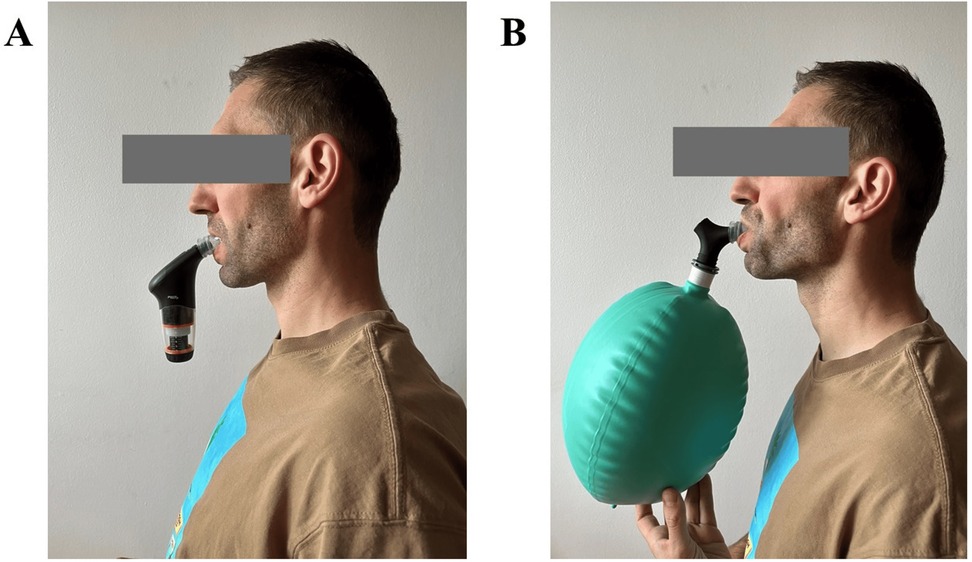
Figure 1. Illustrative application of two training methods. (A) Presentation of respiratory muscle strength training. (B) Presentation of respiratory muscle endurance training. Figure adapted from Kowalski et al. (30).
TFRL and IPTL might be used as inspiratory-only, expiratory-only, or mixed respiratory muscle training. Inspiratory muscle training has consistently demonstrated benefits in improving respiratory muscle strength, endurance, and overall exercise performance in healthy and trained subjects. In contrast, evidence regarding the effectiveness of expiratory or mixed training remains inconsistent, with fewer studies addressing its potential benefits in a well-trained population. Hence, the following section focuses on inspiratory muscle training as the optimal and proven approach. IPTL and TFRL rely on dedicated breathing devices that provide resistance during inspiration and allow for expiration without additional resistance (31). Training protocols typically require individuals to perform vigorous inspirations, starting from the residual volume, against a resistance set at 30%–80% of their maximal inspiratory pressure. Most popular and studied programs require 30 quick and forceful maneuvers from functional residual capacity, twice daily for 5–6 days per week, for at least 4–6 weeks (29). A key distinction between IPTL and TFRL lies in how resistance is applied. In IPTL, the resistance remains constant throughout the breath, resulting in a progressive shift from low pressure and high airflow at smaller lung volumes to high pressure and low airflow as the lungs fill. Due to the pressure–flow dynamics of the respiratory muscle, inspiration at higher lung volumes demands greater muscle strength. Eventually, the resistance can surpass the muscle's capacity to generate sufficient inspiratory pressure, limiting further shortening of respiratory muscle and preventing full lung expansion. In contrast, TFRL features a progressively decreasing external resistance during inspiration, delivering moderate pressure and airflow evenly across the entire vital capacity range (32).
VIH involves devices equipped with partial rebreathing circuits and emphasizes controlled, intense breathing exercises. This method relies on intentional hyperpnea as the primary training stimulus, operating at an intensity of 60%–90% of maximal voluntary ventilation, with minimal or no external resistance applied. The rebreathing circuits help maintain an athlete's homeostasis, as prolonged hyperventilation without specialized equipment is not feasible and, even over short periods, can cause significant disturbances in blood gas levels and negatively impact well-being (29). VIH training programs are usually based on 3–5 sessions per week, from 15 to 40 min each, and should last at least 4–6 weeks.
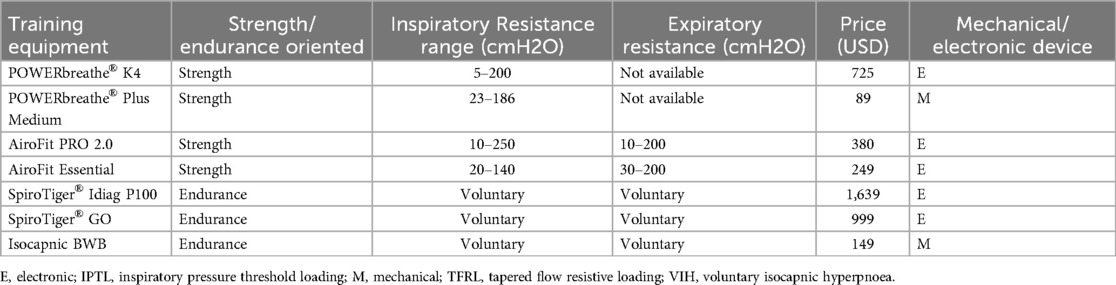
Notably, not all RMT programs are associated with improved performance, as this depends on the intervention design (33, 34). Ineffective interventions may result from an insufficient training stimulus, characterized by inadequate resistance, limited program duration, or failure to implement progressive overload principles (33, 35). Moreover, low motivation and adherence to RMT programs may be significant limiting factors in achieving optimal outcomes. Consequently, providing appropriate supervision is essential to ensure consistent engagement and maximize the effectiveness of the intervention (33). On the other hand, most of the effective interventions addressing intermittent performance share common characteristics and last 6–8 weeks, employ IPTL, rely on a high frequency of training sessions, progressive overload, and relatively high initial resistance (starting intensity). A summary of protocols resulting in a significant, positive influence on intermittent exercise performance from peer-reviewed studies is presented in Table 1. Importantly, the lack of TFRL and VIH studies in Table 1 does not mean they are not effective, but understudied. The available literature that compares different RMT methods does not address intermittent exercise performance. However, studies typically report similar outcomes concerning continuous or sport-specific efforts (30, 36, 37).
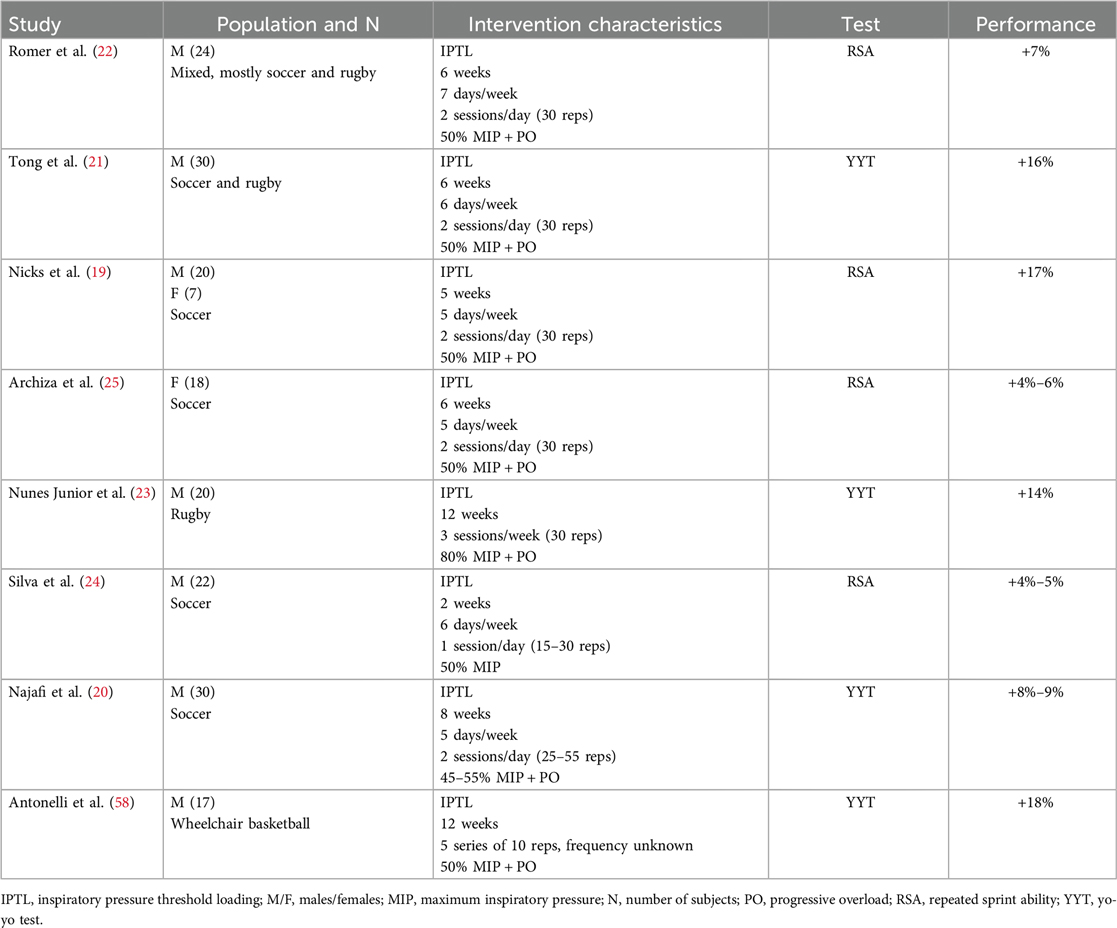
Table 1. Summary of protocols resulting in a significant, positive influence on intermittent exercise performance from peer-reviewed studies.
Products such as POWERbreathe®, Airofit, BreathWayBetter (recently released as Isocapnic), and SpiroTiger® (recently released as Idiag) are commonly used in sports science and remain most popular on the market. Their brief characteristics may be found in Table 2. Airofit devices might be particularly useful for coaches or scientists, as they offer remote supervision options, and staff may track RMT execution and progress via the online platform.
Methodological considerations for optimizing RMT interventions
Training interventions should begin with a well-defined baseline, and RMT is no exception. Such an approach allows for identifying an athlete's needs and measuring adaptation or lack thereof. Therefore, an evaluation of the athlete's respiratory muscle function is recommended before introducing RMT. Noteworthy, it may be performed with easy-to-use and mobile devices, such as the above-mentioned POWERbreathe® K-Series or Airofit (38, 39).
The theory of sport outlines several key principles designed to optimize the training process and athletic performance. While different sources might list slightly different numbers or names for these principles, they are generally consistent across disciplines and also apply to RMT (40). Consequently, progressive overload, periodization, training specificity, and reversibility should be considered when designing RMT programs. To implement progressive overload in RMT, the workload must be gradually increased over time to stimulate adaptation. This can be achieved by progressively adjusting variables such as frequency, intensity, or duration of training sessions. For IPTL and TFRL, it is recommended to increase the resistance and maintain a similar number of training sessions or repetitions. Most of the protocols are based on 30 inspiratory maneuvers per session, and if these 30 maneuvers stop being a challenge, the resistance should be increased (29). For VIH, the progressive overload should be achieved by increased breathing frequency and total training time per week (41). When considering periodization, it is warranted to focus on efficient breathing patterns and proper RMT technique before adding moderate or high training loads. Another important aspect to consider is that RMT typically results in a plateau concerning maximum dynamic inspiratory muscle function after 6–9 weeks of training (40). Hence, to optimize RMT periodization, the training method could be adjusted every six to eight weeks. For example, this might involve transitioning from VIH to IPTL or alternating phases emphasizing lower repetitions with higher resistance and higher repetitions with lower resistance (42). During a detraining period, the respiratory muscle exhibits a decline in force-generation ability similar to that observed in limb muscles with similar practical implications (43). However, short periods without RMT should not result in significant functional gains. Notably, 8–12 weeks after RMT cessation, small yet significant declines in inspiratory muscle function were observed (40). Interestingly, reducing training frequency by 67% allowed for the maintenance of respiratory function during the observed 18 weeks, and even after discontinuing RMT the athletes exhibited improved pulmonary parameters compared with their pre-RMT values (40, 44).
Although employing RMT during exercise caught the attention of researchers and coaches, it is not a recommended combination (45). Additional respiratory loading during aerobic exercise leads to deterioration of performance due to an inadequate ventilatory response, breathing discomfort, anxiety, and intensification of effort (46). Rodrigues and McConnell (45) argued that additional RMT during exercise had the same pitfalls as training at high altitudes (45). Similarly, as the advantages of altitude training could be optimized by adopting the ‘live-high-train-low’ paradigm where benefits of altitude exposure are achieved without compromising training quality, separating RMT sessions and specific exercises is recommended (47).
RMT is generally considered a low-risk, safe activity when performed in accordance with the manufacturers’ guidelines. Some athletes, particularly women, may experience minor acute effects such as headaches or dizziness. The training load associated with RMT is small yet noticeable, therefore should be taken into account during training programming to limit the risk of overtraining or overreaching (41).
Environmental and population factors
Although the presented guidelines are universal and may be applied in multiple settings, environment- and population-specific contexts should be considered. For example, exercising in hypoxia might constitute an additional challenge for the respiratory system and contribute to respiratory muscle fatigue due to increased work of breathing (48, 49). The use of hypoxic conditions in team sports is relatively limited, both in terms of altitude training and in preparation for competition at altitude, compared to the well-established practices in endurance sports (50). However, several team-sports arenas are situated at high altitude, including Mexico City's Estadio Azteca (2,200 m above sea level, ASL) and Estadio Akron in Guadalajara (1,672 m ASL), both of which will host matches during the 2026 FIFA World Cup. A recent review synthesizing findings from seven independent studies (investigating altitudes from 1,400 to 5,500 m ASL) highlighted the advantages of RMT for performance under hypoxic conditions (51). The outcomes revealed that RMT helped reduce fatigue in the respiratory muscle, enhanced the clearance and tolerance of anaerobic byproducts, postponed the activation of the respiratory muscle metaboreflex, and supported oxygen saturation and blood flow to the muscles involved in the movement (51). These multidimensional, positive influences are well-documented. However, the reviewed studies generally focused on incremental tests and performance-related physiological variables, rather than intermittent performance. Consequently, further research could explore how RMT affects RSA and YYT under various oxygen availability conditions.
Available research suggests that the respiratory system may impose greater limitations on athletic performance in women than in men (52). Compared to men of similar anthropometric indices, women generally have smaller lung volumes, reduced diffusion surface area, lower maximal expiratory flow rates, and narrower airways. As a result, they experience a higher work of breathing, greater airway hyperresponsiveness, more pronounced expiratory flow limitations, and an increased likelihood of exercise-induced arterial hypoxemia (53, 54). Consequently, RMT might be more beneficial in women in regular environments and prior to or during altitude exposure (55).
Scientific reporting on RMT and intermittent exercise performance in disabled team-sports athletes is scarce and not conclusive regarding best practices. Contrary to body-abled well-trained athletes, simple sport-specific training might have a significant positive influence on respiratory function (56). Also, it was suggested that combined inspiratory and expiratory training might be the most effective modality in athletes with spinal cord injuries (57). More specifically, studies on well-trained wheelchair basketball players present mixed results depending on the applied protocol. RMT of 12 weeks with progressive overload towards 70% of maximum inspiratory pressure increased YYT performance and maximal inspiratory strength recovery (58), whereas a shorter and lower-dose program (6 weeks and only 50% of maximum inspiratory pressure) did not result in improvement of RSA (59). However, even in the latter study, the athletes reported “less breathlessness” and “less tightness in the chest during the training”, and improved respiratory muscle function was observed (59). The differences may also be associated with the heterogeneity of the sample, which is a natural limitation of studies in Paralympic athletes (60). Overall, studies using cardiopulmonary exercise testing instead of intermittent exercise performance assessment to evaluate performance are prevalent in the disabled. Many report improved respiratory muscle strength (57), but the reports on exercise capacity are mixed (57, 61). The available evidence suggests that although RMT may improve pulmonary function, it should not be considered the primary method for improving the exercise performance of athletes with disabilities.
State-of-the-art research provides guidance regarding environments and populations discussed in this section. However, studies concerning RMT's influence on intermittent exercise performance in hypoxia, between-gender differences, or the disabled are scarce or non-existent. Consequently, any relevant coaching decisions would be an educated guess rather than following well-established, evidence-based protocol. Further research might not only address the abovementioned populations and environments, but also analyze less-investigated RMT methods such as TFRL or VIH.
Conclusions and practical application
• Traditional sport-specific training or exercise programs lack sufficient stimulus to improve the function of the respiratory muscle, underscoring the rationale of integrating additional RMT into training regimens.
• RMT has the potential to improve intermittent exercise performance in team sports athletes, especially in women.
• Most of the interventions resulting in a significant, positive influence on intermittent exercise performance employed inspiratory pressure threshold loading, lasted 6–8 weeks, and relied on a high frequency of training sessions, progressive overload, and relatively high initial resistance (starting intensity).
• The respiratory muscle shares structural and functional similarities with other striated muscles, allowing standard training principles such as progressive overload, periodization, specificity, and reversibility to be applied when creating RMT programs.
• A variety of RMT devices and protocols can be tailored to the athlete's training level, preference, and performance goals. Common protocols may include performing 30 inspiratory maneuvers twice a day, five days a week, with resistance-based trainers or engaging in 20–40 min of vigorous ventilation with isocapnic devices every other day.
• Less-investigated RMT methods, such as TFRL or VIH, should be analyzed in the context of intermittent exercise performance. Moreover, further research addressing RMT and hypoxia, between-gender differences, and athletes with disabilities seems warranted.
Author contributions
TK: Conceptualization, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. GD: Conceptualization, Writing – original draft, Writing – review & editing. MZ: Writing – original draft, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bishop DJ, Girard O. Determinants of team-sport performance: implications for altitude training by team-sport athletes. Br J Sports Med. (2013) 47(Suppl 1):i17–21. doi: 10.1136/bjsports-2013-092950
2. Riess SA. Professional Team Sports in the United States. Routledge: Oxford University Press (2017).
3. Khodaee M, Mathern SA. “Soccer,” in Sports-related Fractures, Dislocations and Trauma. Cham: Springer International Publishing (2020). p. 951–3.
4. Drust B, Atkinson G, Reilly T. Future perspectives in the evaluation of the physiological demands of soccer. Sports Med. (2007) 37:783–805. doi: 10.2165/00007256-200737090-00003
5. Gabbett TJ. Science of rugby league football: a review. J Sports Sci. (2005) 23:961–76. doi: 10.1080/02640410400023381
6. Stojanović E, Stojiljković N, Scanlan AT, Dalbo VJ, Berkelmans DM, Milanović Z. The activity demands and physiological responses encountered during basketball match-play: a systematic review. Sports Med. (2018) 48:111–35. doi: 10.1007/s40279-017-0794-z
7. Spencer M, Bishop D, Dawson B, Goodman C. Physiological and metabolic responses of repeated-sprint activities. Sports Med. (2005) 35:1025–44. doi: 10.2165/00007256-200535120-00003
8. Donskov A. Physical Preparation for Ice Hockey: Biological Principles and Practical Solutions. Bloomington, IN: AuthorHouse (2016).
9. Krustrup P, Mohr M, Amstrup T, Rysgaard T, Johansen J, Steensberg A, et al. The yo-yo intermittent recovery test: physiological response, reliability, and validity. Med Sci Sports Exerc. (2003) 35:697–705. doi: 10.1249/01.MSS.0000058441.94520.32
10. Gharbi Z, Dardouri W, Haj-Sassi R, Chamari K, Souissi N. Aerobic and anaerobic determinants of repeated sprint ability in team sports athletes. Biol Sport. (2015) 32:207–12. doi: 10.5604/20831862.1150302
11. Bangsbo J, Iaia FM, Krustrup P. The yo-yo intermittent recovery test: a useful tool for evaluation of physical performance in intermittent sports. Sports Med. (2008) 38:37–51. doi: 10.2165/00007256-200838010-00004
12. Girard O, Mendez-Villanueva A, Bishop D. Repeated-sprint ability—part I: factors contributing to fatigue. Sports Med. (2011) 41:673–94. doi: 10.2165/11590550-000000000-00000
13. Twist C, Eston R. The effects of exercise-induced muscle damage on maximal intensity intermittent exercise performance. Eur J Appl Physiol. (2005) 94:652–8. doi: 10.1007/s00421-005-1357-9
14. Mendez-Villanueva A, Hamer P, Bishop D. Fatigue in repeated-sprint exercise is related to muscle power factors and reduced neuromuscular activity. Eur J Appl Physiol. (2008) 103:411–9. doi: 10.1007/s00421-008-0723-9
15. Cormack SJ, Mooney MG, Morgan W, McGuigan MR. Influence of neuromuscular fatigue on accelerometer load in elite Australian football players. Int J Sports Physiol Perform. (2013) 8:373–8. doi: 10.1123/ijspp.8.4.373
16. Bishop D, Girard O, Mendez-Villanueva A. Repeated-sprint ability—part II: recommendations for training. Sports Med. (2011) 41:741–56. doi: 10.2165/11590560-000000000-00000
17. HajGhanbari B, Yamabayashi C, Buna TR, Coelho JD, Freedman KD, Morton TA, et al. Effects of respiratory muscle training on performance in athletes: a systematic review with meta-analyses. J Strength Cond Res. (2013) 27:1643–63. doi: 10.1519/JSC.0b013e318269f73f
18. Lorca-Santiago J, Jiménez SL, Pareja-Galeano H, Lorenzo A. Inspiratory muscle training in intermittent sports modalities: a systematic review. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17124448
19. Nicks CR, Morgan DW, Fuller DK, Caputo JL. The influence of respiratory muscle training upon intermittent exercise performance. Int J Sports Med. (2009) 30:16–21. doi: 10.1055/s-2008-1038794
20. Najafi A, Ebrahim K, Ahmadizad S, Jahani Ghaeh Ghashlagh GR, Javidi M, Hackett D. Improvements in soccer-specific fitness and exercise tolerance following 8 weeks of inspiratory muscle training in adolescent males. J Sports Med Phys Fitness. (2019) 59:1975–84.31062540
21. Tong TK, Fu FH, Chung PK, Eston R, Lu K, Quach B, et al. The effect of inspiratory muscle training on high-intensity, intermittent running performance to exhaustion. Appl Physiol Nutr Metab. (2008) 33:671–81. doi: 10.1139/H08-050
22. Romer LM, McConnell AK, Jones DA. Effects of inspiratory muscle training upon recovery time during high intensity, repetitive sprint activity. Int J Sports Med. (2002) 23:353–60. doi: 10.1055/s-2002-33143
23. Nunes Júnior AdO, Donzeli MA, Shimano SGN, Oliveira NMLd, Ruas G, Bertoncello D. Effects of high-intensity inspiratory muscle training in rugby players. Rev Brasil Med Esporte. (2018) 24:216–9. doi: 10.1590/1517-869220182403166216
24. Silva RLC, Hall E, Maior AS. Inspiratory muscle training improves performance of a repeated sprints ability test in professional soccer players. J Bodyw Mov Ther. (2019) 23:452–5. doi: 10.1016/j.jbmt.2019.01.016
25. Archiza B, Andaku DK, Caruso FCR, Bonjorno JC, de Oliveira CR, Ricci PA, et al. Effects of inspiratory muscle training in professional women football players: a randomized sham-controlled trial. J Sports Sci. (2018) 36:771–80. doi: 10.1080/02640414.2017.1340659
26. Sheel AW, Boushel R, Dempsey JA. Competition for blood flow distribution between respiratory and locomotor muscles: implications for muscle fatigue. J Appl Physiol. (2018) 125:820–31. doi: 10.1152/japplphysiol.00189.2018
27. Dempsey JA, Romer L, Rodman J, Miller J, Smith C. Consequences of exercise-induced respiratory muscle work. Respir Physiol Neurobiol. (2006) 151:242–50. doi: 10.1016/j.resp.2005.12.015
28. Coast JR, Clifford PS, Henrich TW, Stray-Gundersen J, Johnson RL Jr. Maximal inspiratory pressure following maximal exercise in trained and untrained subjects. Med. Sci. Sports Exerc. (1990) 22:811–5. doi: 10.1249/00005768-199012000-00013
30. Kowalski T, Klusiewicz A, Rębiś K, Wilk A, Starczewski M. Comparative study of different respiratory muscle training methods: effects on cardiopulmonary indices and athletic performance in elite short-track speedskaters. Life (Basel). (2024) 14:1159. doi: 10.3390/life14091159
31. Van Hollebeke M, Gosselink R, Langer D. Training specificity of inspiratory muscle training methods: a randomized trial. Front Physiol. (2020) 11:576595. doi: 10.3389/fphys.2020.576595
32. Langer D, Charususin N, Jácome C, Hoffman M, McConnell A, Decramer M, et al. Efficacy of a novel method for inspiratory muscle training in people with chronic obstructive pulmonary disease. Phys Ther. (2015) 95:1264–73. doi: 10.2522/ptj.20140245
33. McConnell AK. Crosstalk opposing view: respiratory muscle training does improve exercise tolerance. J Physiol. (2012) 590:3397–8. discussion 3399–400. doi: 10.1113/jphysiol.2012.235572
34. Patel MS, Hart N, Polkey MI. Crosstalk proposal: training the respiratory muscles does not improve exercise tolerance. J Physiol. (2012) 590:3393–5. discussion 3401. doi: 10.1113/jphysiol.2012.235408
35. Shei R-J. Recent advancements in our understanding of the ergogenic effect of respiratory muscle training in healthy humans: a systematic review. J Strength Cond Res. (2018) 32:2665–76. doi: 10.1519/JSC.0000000000002730
36. Illi SK, Held U, Frank I, Spengler CM. Effect of respiratory muscle training on exercise performance in healthy individuals: a systematic review and meta-analysis. Sports Med. (2012) 42:707–24. doi: 10.1007/BF03262290
37. Notter DA, Verges S, Renggli AS, Beltrami FG, Spengler CM. Similar effects on exercise performance following different respiratory muscle training programs in healthy young men. Sci Rep. (2023) 13:16135. doi: 10.1038/s41598-023-41580-w
38. Stavrou VT, Tourlakopoulos KN, Daniil Z, Gourgoulianis KI. Respiratory muscle strength: new technology for easy assessment. Cureus. (2021) 13:e14803. doi: 10.7759/cureus.14803
39. Kowalski T, Klusiewicz A. POWERbreathe® S-index test—guidelines and recommendations for practitioners. Biomed Hum Kinet. (2023) 15:225–8. doi: 10.2478/bhk-2023-0026
40. Romer LM, McConnell AK. Specificity and reversibility of inspiratory muscle training. Med Sci Sports Exerc. (2003) 35:237–44. doi: 10.1249/01.MSS.0000048642.58419.1E
41. Kowalski T, Kasiak P, Rebis K, Klusiewicz A, Granda D, Wiecha S. Respiratory muscle training induces additional stress and training load in well-trained triathletes—randomized controlled trial. Front Physiol. (2023) 14. doi: 10.3389/fphys.2023.1264265
42. Kowalski T, Granda D, Klusiewicz A. Practical application of respiratory muscle training in endurance sports. Strength Cond J. (2024). doi: 10.1519/ssc.0000000000000842
43. Mujika I, Padilla S. Muscular characteristics of detraining in humans. Med Sci Sports Exercise. (2001) 33:1297–303. doi: 10.1097/00005768-200108000-00009
44. Klusiewicz A, Borkowski L, Zdanowicz R, Boros P, Wesołowski S. The inspiratory muscle training in elite rowers. J Sports Med Phys Fitness. (2008) 48:279–84.18974711
45. Rodrigues GD, McConnell AK. The misuse of respiratory resistive loading during aerobic exercises: revisiting mechanisms of “standalone” inspiratory muscle training. Am J Physiol Lung Cell Mol Physiol. (2024) 327:L815–7. doi: 10.1152/ajplung.00396.2023
46. López-Pérez ME, Romero-Arenas S, Giráldez-García MA, Colomer-Poveda D, Márquez G. Acute psychophysiological responses during exercise while using resistive respiratory devices: a systematic review. Physiol Behav. (2022) 256:113968. doi: 10.1016/j.physbeh.2022.113968
47. Bejder J, Nordsborg NB. Specificity of “live high-train low” altitude training on exercise performance. Exerc Sport Sci Rev. (2018) 46:129–36. doi: 10.1249/JES.0000000000000144
48. Amann M, Pegelow DF, Jacques AJ, Dempsey JA. Inspiratory muscle work in acute hypoxia influences locomotor muscle fatigue and exercise performance of healthy humans. Am J Physiol Regul Integr Comp Physiol. (2007) 293:R2036–45. doi: 10.1152/ajpregu.00442.2007
49. Romer LM, Polkey MI. Exercise-induced respiratory muscle fatigue: implications for performance. J Appl Physiol. (2008) 104:879–88. doi: 10.1152/japplphysiol.01157.2007
50. Billaut F, Gore CJ, Aughey RJ. Enhancing team-sport athlete performance: is altitude training relevant? Sports Med. (2012) 42:751–67. doi: 10.1007/BF03262293
51. Álvarez-Herms J, Julià-Sánchez S, Corbi F, Odriozola-Martínez A, Burtscher M. Putative role of respiratory muscle training to improve endurance performance in hypoxia: a review. Front Physiol. (2018) 9:1970. doi: 10.3389/fphys.2018.01970
52. Amann M. Pulmonary system limitations to endurance exercise performance in humans. Exp Physiol. (2012) 97:311–8. doi: 10.1113/expphysiol.2011.058800
53. Sheel AW, Richards JC, Foster GE, Guenette JA. Sex differences in respiratory exercise physiology. Sports Med. (2004) 34:567–79. doi: 10.2165/00007256-200434090-00002
54. Harms CA, Smith JR, Kurti SP. “Sex Differences in Normal Pulmonary Structure and Function at Rest and During Exercise,” in Gender, Sex Hormones and Respiratory Disease. Cham: Springer International Publishing (2016). p. 1–26.
55. Raberin A, Burtscher J, Citherlet T, Manferdelli G, Krumm B, Bourdillon N, et al. Women at altitude: sex-related physiological responses to exercise in hypoxia. Sports Med. (2024) 54:271–87. doi: 10.1007/s40279-023-01954-6
56. Moreno MA, Zamunér AR, Paris JV, Teodori RM, Barros RML. Effects of wheelchair sports on respiratory muscle strength and thoracic mobility of individuals with spinal cord injury. Am J Phys Med Rehabil. (2012) 91:470–7. doi: 10.1097/PHM.0b013e3182adcb0
57. Lemos JR, da Cunha FA, Lopes AJ, Guimarães FS, do Amaral Vasconcellos FV, Dos Santos Vigário P. Respiratory muscle training in non-athletes and athletes with spinal cord injury: a systematic review of the effects on pulmonary function, respiratory muscle strength and endurance, and cardiorespiratory fitness based on the FITT principle of exercise prescription. J Back Musculoskelet Rehabil. (2020) 33:655–67.31594206
58. Antonelli CBB, Hartz CS, Santos SdS, Moreno MA. Effects of inspiratory muscle training with progressive loading on respiratory muscle function and sports performance in high-performance wheelchair basketball athletes: a randomized clinical trial. Int J Sports Physiol Perform. (2020) 15:238–42. doi: 10.1123/ijspp.2018-0979
59. Goosey-Tolfrey V, Foden E, Perret C, Degens H. Effects of inspiratory muscle training on respiratory function and repetitive sprint performance in wheelchair basketball players. Br J Sports Med. (2010) 44:665–8. doi: 10.1136/bjsm.2008.049486
60. Alter M, Krassioukov A. Autonomic nervous system in paralympic athletes with spinal cord injury. Phys Med Rehabil Clin N Am. (2018) 29(2):245–66. doi: 10.1016/j.pmr.2018.01.001
Keywords: respiratory muscle training, repeated sprint ability, yo-yo test, football, rugby, soccer
Citation: Kowalski T, Dias Rodrigues G and Zanini M (2025) Application of respiratory muscle training for improved intermittent exercise performance in team sports: a narrative review. Front. Sports Act. Living 7:1632207. doi: 10.3389/fspor.2025.1632207
Received: 20 May 2025; Accepted: 30 June 2025;
Published: 15 July 2025.
Edited by:
Samuel Verges, Université Grenoble Alpes, FranceReviewed by:
Mehmet Ismail Tosun, Hitit University, TürkiyeŁukasz Tota, Akademia Wychowania Fizycznego im. Bronisława Czecha w Krakowie, Poland
Copyright: © 2025 Kowalski, Dias Rodrigues and Zanini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tomasz Kowalski, dG9tYXN6Lmtvd2Fsc2tpQGluc3AucGw=
 Tomasz Kowalski
Tomasz Kowalski Gabriel Dias Rodrigues
Gabriel Dias Rodrigues Michele Zanini
Michele Zanini