- 1University of Redlands, Redlands, CA, United States
- 2Lawrence D Longo Center for Perinatal Biology, Loma Linda University School of Medicine, Loma Linda, CA, United States
- 3Outride, Morgan Hill, CA, United States
- 4Loma Linda University School of Public Health, Loma Linda, CA, United States
- 5Department of Educational Psychology, University of Oklahoma, Norman, OK, United States
Introduction: The impact of the Riding for Focus (R4F) school-based cycling program and key risk factors on middle school students’ mental health was evaluated following COVID-19 lockdowns. Adolescents face growing mental health challenges that the R4F program aims to address by promoting physical activity and well-being.
Methods: The study surveyed students from 31 U.S. schools, assessing mental health via the WHO-5 Well-Being Index and PSC-17-Y checklist. Non-parametric tests (Mann–Whitney U, Kruskal–Wallis ANOVA with Dunn's test) and effect size calculations (Cohen's d) were used; clinical risk assessments employed Fisher's Exact Test and Koopman scores with established cutoff values. Modifiable risk factors analyzed included physical activity, sleep, screen time, and breakfast habits. Linear regression evaluated dose-response relationships between these factors and wellness scores.
Results: Participation in R4F was linked to a modest 5% boost in WHO-5 well-being scores; however, PSC-17-Y scores also increased slightly, contrary to previous findings, indicating more reported symptoms. Differences in outcomes were seen across gender and race/ethnicity. Notably, modifiable risk factors such as sleep, screen time, and physical activity showed clear dose-response relationships with mental health metrics.
Discussion: Results suggest the R4F program may support adolescent mental health, though outcomes vary by demographic and lifestyle factors, highlighting a need for targeted, individualized interventions in youth populations.
1 Introduction
Mental health research, particularly focusing on adolescents, is of paramount importance to our society. Recent studies investigating the COVID-19 pandemic's impact on adolescent mental health and well-being are yielding new insights into the development of psychological disorders. Following the COVID-19 lockdowns, rates of general anxiety, depression, post-traumatic stress disorder, and social anxiety symptoms increased significantly (1–5) and have yet to return to pre-pandemic levels (6, 7). As of 2021, a staggering 42% of the youth population in the United States reported consistently feeling sad or hopeless, with nearly one-third experiencing poor mental health (8). Major depressive episodes and anxiety are among the most prevalent symptoms of poor mental health, with a substantial number of children and adolescents experiencing these conditions (9). A comprehensive review reveals that by age 14, approximately one-third of young teens already exhibit externalizing, internalizing, and attention behavioral issues, which rises to nearly half of all adolescents by age 18 (10).
Adolescent mental health and psychological well-being are influenced by multiple lifestyle, socioeconomic, and other factors, which interact to affect risk and outcomes. Key determinants include gender, race, socioeconomic status (SES), social interaction and engagement, screentime, sleep duration and physical activity (PA) levels (11, 12). Regular PA is closely linked to improved mental health and psychological well-being in children and adolescents (13–15). Research consistently shows that exercise enhances self-image, quality of life, and happiness, while also reducing psychological distress (16). Numerous studies support the role of exercise as both a preventive and therapeutic strategy for depression and anxiety (17, 18). The positive effects of PA are broad, ranging from the alleviation of negative emotions to neurobiological changes that support emotional regulation (19–21). Cycling as a form of exercise has been shown to promote a healthier physical well-being including, but not limited to, lower risks of a cardiovascular event (22–24), Type 2 Diabetes (25), and obesity (25).
Aerobic as well as resistance based PA, whether performed as a leisure activity or in school, is widely recognized as an effective method to combat poor mental, physical, and cognitive health in children, adolescents, and adults (13–16, 18, 19). Considering that adolescents in U.S. public schools spend an average of 180 days per year in school (26), well-designed school-based physical education (PE) programs present a valuable opportunity to help students meet the 1 h daily PA recommendations outlined in both U.S. Physical Activity Guidelines and WHO global standards (27, 28). Well-designed PE programs not only promote active lifestyle behaviors but also foster emotional intelligence, social skills, and long-term enthusiasm for PA (29, 30). However, these benefits are not always realized due to budget constraints, inconsistent program quality, or lack of accessibility (30–32). The COVID-19 pandemic further complicated the picture, as lockdowns and remote learning disrupted PA routines and contributed to declines in mental health, consistent with the established link between reduced PA and increased risk of mental health disorders (19, 33) Nevertheless, some forms of PA experienced rises in participation during the pandemic. Notably, cycling outdoors in the U.S. experienced a 16% increase between 2019 and 2020 (34), and generally saw an increase in prevalence in 2022 compared to 2020 (35). Unfortunately, participation rates among 10- to 17-year-olds continued to decline, with just under half reporting bicycling within the previous year. Young riders under 17 are most likely to use bicycles for recreation or a combination of recreation and transportation. However, engagement drops as adolescents approach driving age, largely due to increased academic pressures, participation in extracurricular activities, social influences, and persistent safety concerns (36). These and other barriers have contributed to a steady decline in biking frequency and participation over the last decade. For cycling to become a lifestyle choice rather than merely a transitional or recreational activity, systematic improvements including safer infrastructure, supportive social norms, and integration into daily routines are essential to keep riding accessible and appealing for adolescents and beyond (37, 38).
Cycling is particularly valuable because it supports physical endurance, bone and muscle health, mental well-being, and prevention of chronic diseases such as diabetes (39). Cycling has a number of distinctions that set it apart from other physical activities and sports, including that the bicycle can be used for recreation, transportation, as well as competition. Riding bicycles is low impact, which minimizes bone stress, it allows for participation across all ages and fitness levels, and cycling provides additional benefits of balance and lifelong accessibility relative to high impact and skill-based sports. Researchers support cycling as interventions that promote increased physical activity, which is crucial for youth health and combating sedentary lifestyles. School-based cycling programs have demonstrated improvements in moderate-to-vigorous physical activity, cycling skills, and physical fitness among children and adolescents (40–42). Learning to cycle through progressive skill building strategies, such as using balance bikes before learning to pedal, leads to more efficient cycling skill acquisition, reduced sedentary time, and improved leg strength and body composition (43, 44). Beyond physical benefits, cycling fosters prosocial development by providing opportunities for increased responsibility, confidence, leadership, and social connection (45, 46). Given the immense societal and economic burden of mental illness, which is estimated at $282 billion annually in the U.S. alone (47), leveraging structured, evidence-based PE programs, alongside accessible forms of community PA like cycling, may provide scalable and sustainable opportunities to promote health and resilience in youth during both ordinary and extraordinary times.
The purpose of this study was to expand upon our earlier findings, with focus on understanding the impact of the R4F program in a COVID-19 emergent population. Our previous work demonstrated that the Riding for Focus (R4F) scholastic-based cycling program is associated with improved mental health and well-being in adolescents during the COVID-19 pandemic, providing additional support regarding the importance of cycling as a form of PA (39). Our earlier work showed that participating in the R4F program was associated with enhanced psychosocial well-being and a reduced relative risk of developing psychosocial disorders (12). R4F is a 6–8-week curriculum-based PE program designed for middle school students, providing exposure to and education about cycling activities. In this study, we were able to examine associations and dose-response relationships between lifestyle behaviors and mental health outcomes in a cohort of students post-COVID-19. We hypothesized that participation in the R4F program would be associated with improvements in adolescent students' mental health and well-being, and that these benefits would be evident when considering both modifiable (e.g., physical activity, sleep, screen time) and nonmodifiable (e.g., gender, race/ethnicity, socioeconomic status) risk factors.
2 Methods
2.1 Participants and methods
The methods for the current study were largely adapted from our previous research (12). Each school's participation in the R4F program is determined by the individual school. In some schools, every student within a grade level will go through the R4F program. In other schools, the program may be within an elective course. Data on students with physical disabilities and special educational needs is not currently collected, but is an area of future interest. However, many schools do report sourcing adaptive bikes to ensure all students are included, and this is an area of future growth and development of the program. The current study lacked a comparison/control group, like our previous study, and instead relied on before and after program participation measurements (12). The program was part of standard educational practice at the school, and parents and legal guardians were sent home letters outlining school participation in the program and surveys as part of the program. Parents or legal guardians who did not wish for their child to participate in the survey signed a form and returned it to the teacher (passive consent). In addition, each student had the option to opt-out of the survey, even if a parent or legal guardian did not opt them out. At the beginning of the surveys, students were invited to only continue if they would like to participate in the surveys, with no impact to their grades. Data were collected via a voluntary anonymous survey that was provided in English as well as Spanish from participants in the Outride R4F scholastic middle school cycling physical education program, further ensuring participant anonymity and minimizing risk. The study was approved by an Institutional Review Board (Advarra), with secondary analysis approved by Loma Linda University IRB. Participants completed online surveys through a Qualtrics platform on classroom or at-home electronic devices before and after the R4F program, which may introduce variability in the survey environment. We do not have information on how much additional instruction was provided to students at each different school or by their parents in the home environment.
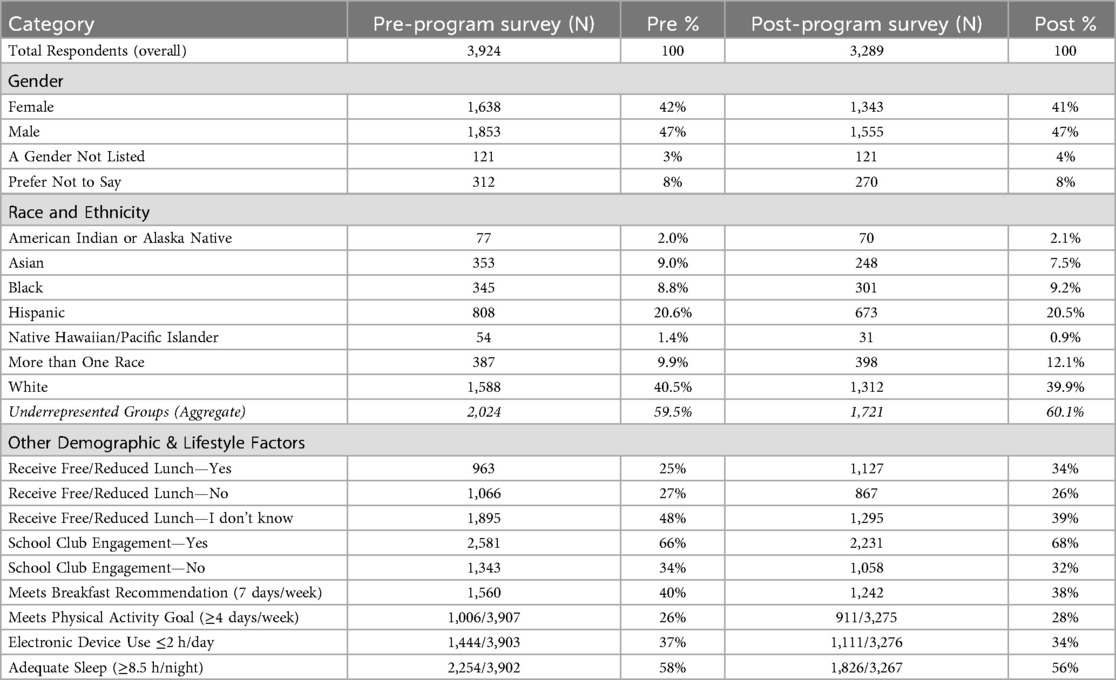
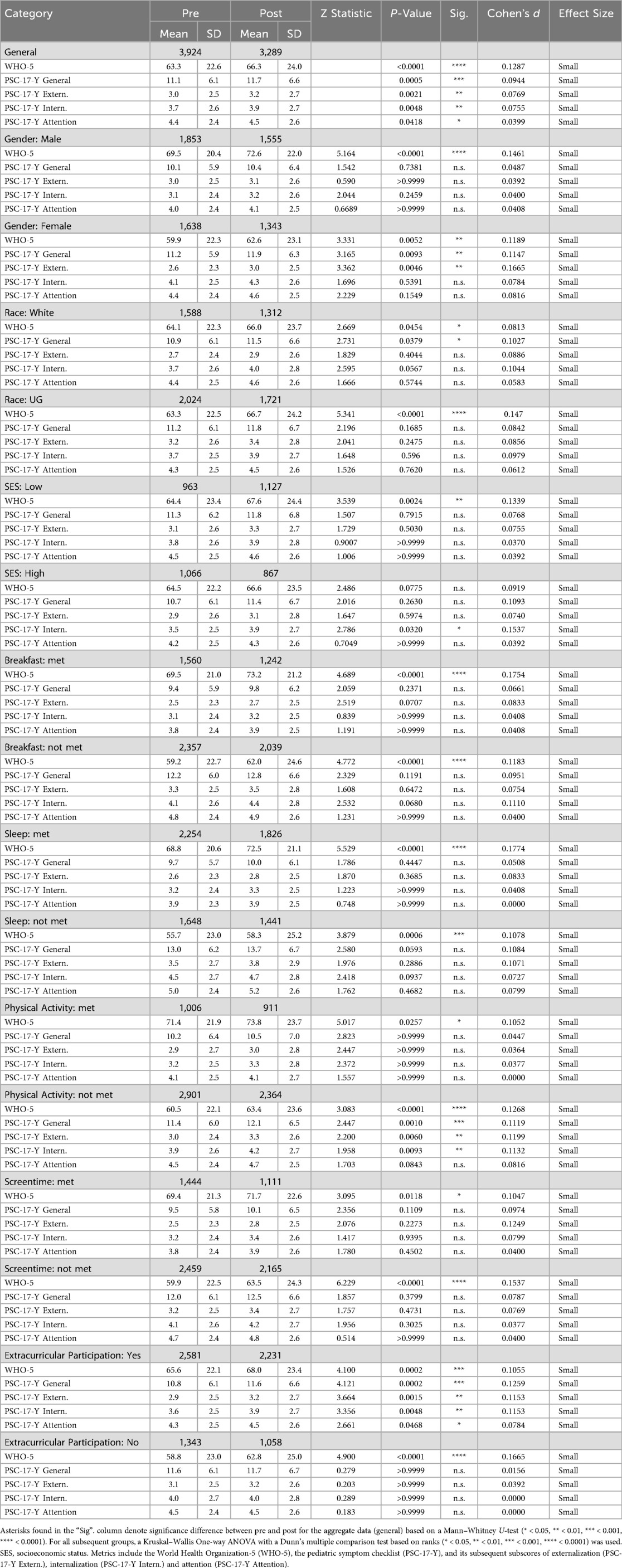
A total of 8,639 student responses (4,820 PRE surveys and 3,819 POST surveys) from 44 schools across the United States who participated in the R4F program during the 2021–2022 school year participated in the surveys, during a period of easing COVID-19 lockdown restrictions (48). As the surveys were conducted anonymously as part of a program evaluation and surveillance process, we were unable to verify that every student completed both a pre- and post-program survey, with analysis being performed using unpaired analysis techniques. To achieve the most balanced and unbiased set of PRE and POST responses across schools a series of filters were applied to the dataset. In an initial screen, 13 schools that only participated in PRE surveys or POST surveys but not consistently both sets of surveys were removed from analysis, resulting in 8,007 remaining responses (92.7%) from 31 participating schools. To ensure only students who actively completed the survey during class time were included, we also filtered survey responses based on response time. The mean time for survey completion was 10.56 min, with a standard deviation (SD) of 10.27 min. Surveys completed in fewer than 3 min or not completed within 31.1 min (2 SD longer than the mean completion time) were removed. This method was used to provide a more unbiased approach to eliminate data where we suspect that the participant did not perform the survey with intent, including answering the questions too rapidly, without properly reading the question or answer set or that the individual allowed the survey to sit open for many minutes without being attentive to the survey. The length of the survey for the current study is shorter than other routine surveys or assessments taken during the school day, many of which far exceed 10–15 min. For example, the full Youth Risk Behavioral Survey takes about 35 min for students to complete (49), while the California School Climate, Health, and Learning core module takes middle school students an average of 17 min (50). In addition, we applied a response quality filtration, including only surveys with complete responses to all sub-items of the youth self-report version of the Pediatric Symptom Checklist (PSC-17-Y) (51) and WHO-5 well-being index (52, 53). This step prevented skewed scores due to non-responses to individual items and resulted in the removal of an additional 794 survey responses. After applying these filters, the final dataset consisted of 3,924 pre-program survey responses and 3,289 post-program survey responses across 31 schools. Unlike our previous study (12), most schools were not subject to COVID-19 related lockdowns during this period (54, 55). The included 31 schools for this study represent 14% of the total number of schools that have been awarded the R4F program since its inception. Students were between the ages of 11 and 14, corresponding to grade levels 6 through 8, and are considered adolescents as defined by WHO and UN criteria (11) and by modern viewpoints regarding the transition to adulthood (56). The schools included in this study were from multiple regions throughout the United States, as depicted in Figure 1. The demographics of self-reported participant gender, race and ethnicity along with lifestyle and other factors are provided in Table 1.
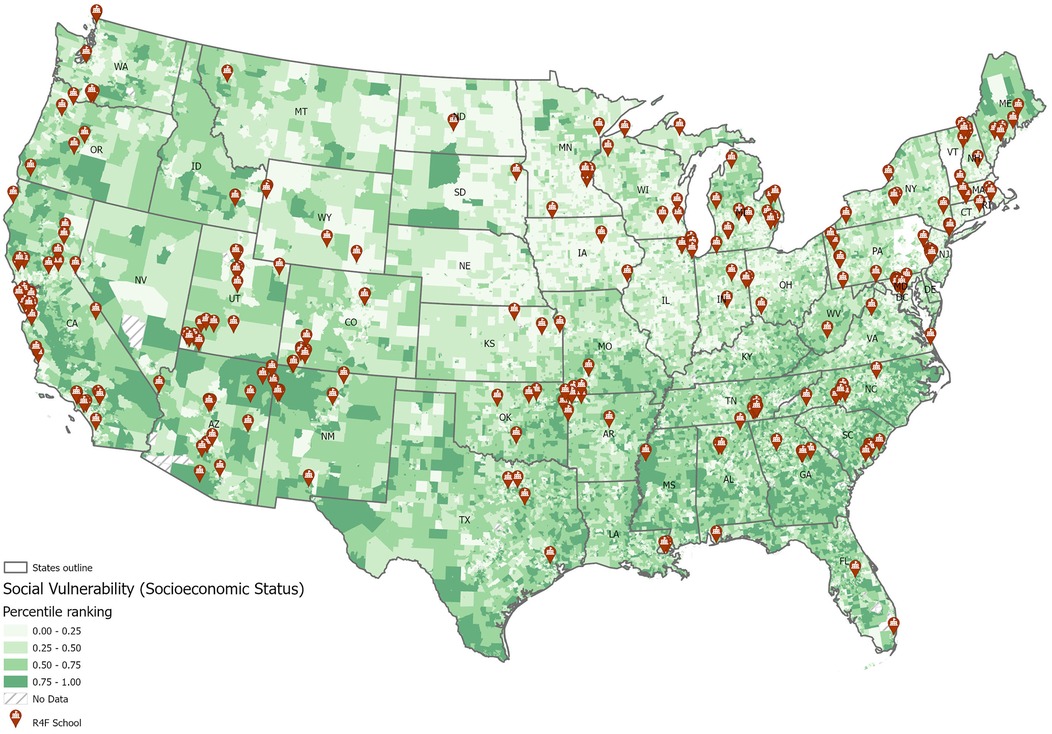
Figure 1. Schools with riding for focus programs are distributed in multiple states and in locations with varied median household incomes.
Students self-reported their gender, race, and ethnicity. For gender, students self-selected between Male, Female, A gender not listed, and Prefer not to say (Table 1). Due to the small sample sizes of participants not selecting Female or Male, only students who selected Female and Male were included in the comparative analyses. For race and ethnicity, students self-reported as American Indian or Alaska Native, Asian, Black, Hispanic or Latino, Native Hawaiian or Pacific Islander, More than One Race, White, or they did not specify (Table 1). As the data are analyzed using many sub-categories (i.e., days per week physically active), the small sample sizes in many of the reported racial and ethnic minority groups become challenging to interpret. As a result, throughout this manuscript, students from racial and ethnic minority groups (American Indian or Alaska Native, Asian, Black, Hispanic or Latino, Native Hawaiian or Pacific Islander, or students who selected More than One Race) will be aggregated for analysis and referred to as underrepresented groups (UG). While these data were aggregated for statistical power, this grouping may mask distinct experiences across racial and ethnic subgroups.
Students also answered questions about sleep duration, screen time, PA levels, and involvement in clubs and sports teams. They also self-reported their previous participation in a R4F program, and whether they received free or reduced-cost school lunches, which served as a proxy for socioeconomic status (SES) (12, 57). To further understand the SES of the study population, we evaluated the social vulnerability index of each school site, which was 0.41 ± 0.23 (mean ± SD) with a range of 0.10 to 0.92 on a 0–1 scale (58). The schools were in the following SVI ranges, including 8 low SVI, 12 moderate, 2 high, and 4 very high.
To measure psychosocial well-being, students completed assessments that were chosen because they are adolescent centered and designed for a middle school level. Questions were chosen from pre-existing validated instruments for this age group and address both positive and negative psychosocial functioning. Many questions were adopted from CDC's Middle School Youth Risk Behavioral Survey (59). Among the number of metrics available including the Strengths and Difficulties Questionnaire (SDQ) (60), KIDSCREEN (61), the WHO-5 Well-Being Index (52, 53) and the youth self-report version of the PSC-17-Y (51, 62, 63), we chose the WHO-5 and PSC-17-Y metrics based on their psychometric strengths, their brevity, and ease of delivery in school settings. Although these are both strong metrics, it is worth noting concerns regarding the psychometric properties of the WHO-5 and PSC-17-Y measures used in this age group. While they are both established instruments, their validity and sensitivity in younger adolescents (11–14 years) may be limited, as this age range presents distinct developmental characteristics that can influence both self-reflection and reporting accuracy (64, 65). Reliance on self-report alone may also overlook important behavioral or contextual factors; complementing these data with proxy-reports from parents or teachers, as supported by instruments such as the SDQ or KIDSCREEN, could provide a more balanced perspective in future work.
The WHO-5 is a 5-item, self-report questionnaire evaluating positive well-being and depression, validated for use with adolescent respondents ages 11 and older with higher scores indicating greater well-being (66, 67). The PSC-17-Y complements the WHO-5, helping to identify and assess emotional and behavioral problems, with lower scores indicating fewer psychosocial challenges (63, 68). The PSC-17-Y is not meant as a diagnostic tool, rather it is meant to help understand what emotional and behavioral challenges a child may be facing. It covers a range of emotional and behavioral problems and assesses psychosocial functioning, including sub-scores reflecting behavioral conduct and disruptive behavior (externalization), anxiety and depressive symptoms (internalization), and attention difficulties (attention). As both the WHO-5 and PSC-17-Y scores may fluctuate slightly over time, it is important to consider what is considered a meaningful change, as opposed to a statistically significant change. Here, we report WHO-5 scores out of 100, with changes of 10% or more reflecting a meaningful change (69). Each of the 5 items was scored 0 (“At no time”) to 5 (“All of the time”), yielding a raw total of 0–25, which was converted to a percentage score by multiplying by 4. For the PSC each of the17 items were scored 0 (“Never”), 1 (“Sometimes”), or 2 (“Often”) for a total score from 0 to 34. While a difference of 6 or greater for the total score, or differences of 2 or more on the subscales are considered a reliable change for the longer 35-item version (51, 63), reliable change benchmarks have not been published for the short-form version. After completing the R4F program, students took the same survey with additional open and closed questions about the program. The survey was designed to be completed in 10–15 min.
2.2 Cycling program curriculum
The Riding for Focus (R4F) program curriculum used in the current study was identical to that employed in our previous research (12). Designed to be integrated into the school day, R4F sessions are run by the physical education teachers at the school and typically take place during students' physical education class time. The program is structured to span 6 to 8 weeks, comprising 12 recommended sessions. Throughout these sessions, students acquire various cycling skills while aiming to achieve at least 20 min of moderate-to-vigorous PA per session. The skills are designed to prepare the participants to be safe while riding on the road. This includes how to start and stop the bike, how to balance and control the bike, along with shifting gears, how to scan and avoid obstacles, and how to conduct themselves as a vehicle on the roadway. Activities are conducted on diverse terrains surrounding the school campus. The R4F program is designed to provide 1 h of PA each day, adhering to the Public Health Strategies (PHS) and WHO guidelines for PA (27, 28). The program also and aligns with the standards set by SHAPE America (70), ensuring a comprehensive and well-rounded approach to physical education and cycling instruction.
2.3 Statistical methods
Data analysis procedures and graph production largely followed the methods outlined in our previous study (12). We used R (71) to create data frames and filter data, streamlining the workflow for the current dataset. GraphPad Prism 10 (La Jolla, CA) was employed for graphing and statistical analyses. Prior to analysis, all datasets were tested for normality, with none showing normal distribution. For comparisons between two groups, we used the Mann–Whitney U-test to identify potential differences in well-being metrics. For analyses involving more than two groups, we performed a Kruskal–Wallis ANOVA with Dunn's multiple comparisons test. Graphs present violin plots showing median, 25th and 75th quartiles, along with minimum and maximum data ranges. Statistical significance was set at P < 0.05, with further distinctions made for P < 0.01, P < 0.001, and P < 0.0001 where appropriate. We calculated Cohen's d test statistic based on Cohen's recommendations (72, 73) to estimate effect size in pre- and post-program comparisons. According to widely accepted benchmarks, a Cohen's d value of 0.2 reflects a small effect size, 0.5 indicates a medium effect, and 0.8 or above signifies a large effect. These thresholds are valuable because they help interpret the real-world significance of observed changes, emphasizing not only whether a difference is statistically significant but also whether it is likely to be meaningful in practice. Consequently, Cohen's d provides additional insight into the practical magnitude of changes in adolescent mental health and well-being scores beyond what traditional p-values alone can offer. To examine the relative clinical risk of developing psychosocial disorders, we used a Fisher Exact Test in combination with Koopman asymptotic scores (74) for PSC-17-Y and WHO-5 metrics, based on established cutoff scores of ≥15 and ≤ 50, respectively (63, 67). Decreases in the PSC-17-Y scores signify reduced anxiety, depression, attention, and behavioral challenges, while increases in the WHO-5 score are reflective of better mental health and well-being. Both of these instruments are used as screening tools, and individuals meeting the established cutoff scores are referred to for professional evaluation and potential treatment for mental health disorders.
We evaluated the impact of various risk factors on WHO-5 and PSC-17-Y scores using specific cutoffs for various risk factors based on current research and recommendations as outlined in our previous work (12). The physical activity cutoff was set at 4 days a week of 60 min of PA, as adolescents who do not meet this threshold have an increased risk of developing psychosocial disorders compared to those who participate in PA more (75). For sleep, we used a cutoff of 8 h each weeknight, considering that adolescents who sleep less than the recommended amount (9 h for 6–12 year olds, 8 h for 13–18 year olds) on school nights are at greater risk of psychosocial disorders (76). Screen time was limited to 2 h a day, in line with the American Academy of Pediatrics' 2016 policy statement on adolescent media use (77). Regarding breakfast consumption, we set the cutoff at 7 days a week, as regular breakfast consumption is associated with maintaining a healthy body weight, greater life satisfaction, and better academic performance (78, 79). For breakfast consumption we only analyzed whether something was eaten, without considering the content or caloric amount of the meal.
We conducted linear regression analyses to examine relationships between psychosocial wellness scores (WHO-5 and PSC-17-Y) and various self-reported factors, including hours of sleep, screen time, the number of days of breakfast consumption, and the number of days of PA that met PHS guidelines. An F-test was used to determine if the slope of each association was significantly different from zero (80). Additionally, we compared the slopes of the pre- and post-program regression analyses using an F-test to assess whether the two datasets shared a common slope or had independent slopes (80). For all slope analyses, a P-value of P < 0.05 was considered statistically significant.
3 Results
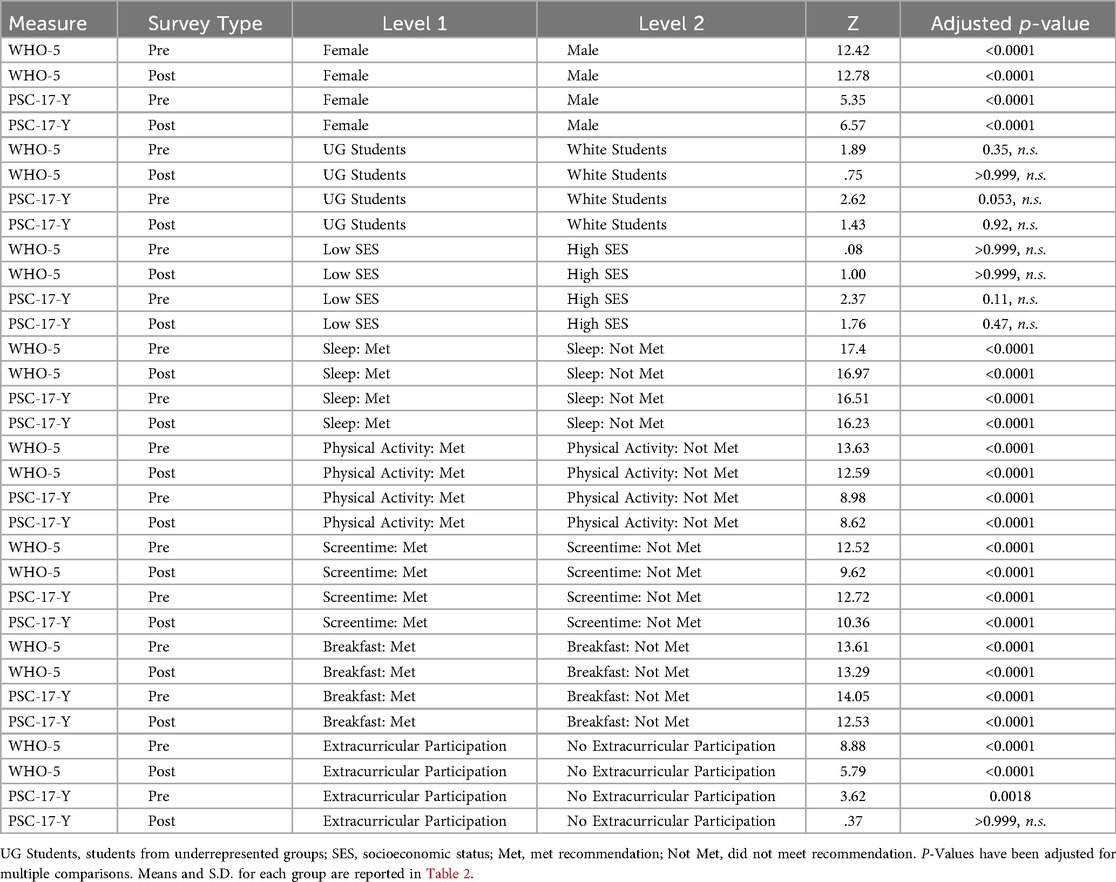
Based on our previous report examining the efficacy of the Riding for Focus (R4F) program on adolescent health and well-being during COVID-19, we aimed to assess whether this effect would be replicated in a cohort of students not subjected to the same restrictions and stresses as our initial study group (3, 12, 16, 19, 20, 54, 55, 81). To evaluate the potential association between the R4F program and mental health and well-being among the student population, we analyzed WHO-5 and PSC-17-Y scores before and after the R4F program. A summary of findings, including statistical test outcomes, can be reviewed in Tables 2, 3. Consistent with our previous findings (12), students' WHO-5 increased by 5% following the R4F program (MPRE = 63.3, MPOST = 66.3; Figure 2A). However, we also observed a 5% increase in PSC-17-Y composite scores (MPRE = 11.1, MPOST = 11.7) departing from previous findings. Each of the PSC-17-Y sub scores also demonstrated small but significant increases after participation in the R4F program (Table 2): externalization increased by 7% (MPRE = 3.0, MPOST = 3.2; Figure 2C), internalization by 5% (MPRE = 3.7, MPOST = 3.9; Figure 2D), and attention by 3% (MPRE = 4.4, MPOST = 4.5; Figure 2E).
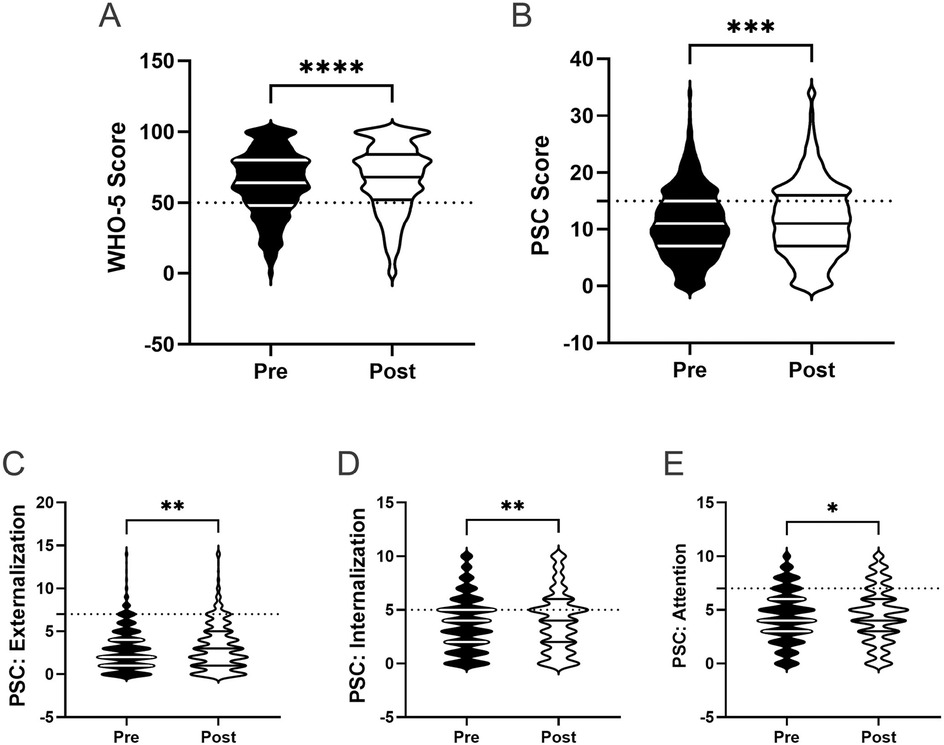
Figure 2. General effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores on the PSC and sub scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Mann–Whitney U-test (* < 0.05, ** < 0.01, *** < 0.001, **** < 0.0001). N = 3,924 for pre-program, N = 3,289 for post-program.
The relative clinical risk for the development of mental health disorders was assessed by examining the number of respondents who either met or did not meet critical clinical cutoff scores for both the WHO-5 (score ≤ 50) and the PSC-17-Y (score ≥ 15) (12, 63, 67). Participation in the R4F program was associated with a reduced relative risk (.91, 95% CI [0.84, 0.99), as measured by the WHO-5 in all study participants. In comparison, the relative risk as determined by the PSC-17-Y was higher post-program (1.17, 95% CI [1.1, 1.26).
3.1 Analysis of specific risk factors and their interplay with the R4F program and daily recommendations
3.1.1 Gender
(12) and others have demonstrated that both psychosocial well-being and responses to PA programs often differ across gender (82–86). In line with this work, we examined whether there were gender differences in mental well-being, as well as whether any potential differences changed after participation in the R4F program. We also assessed whether there were differences in the relative risk of poor mental health across genders.
Prior to the implementation of the R4F program, we observed differences in psychosocial well-being scores across gender. Males demonstrated higher WHO-5 scores (M = 69.5) compared to females (M = 59.9), indicating better overall well-being (Figure 3A). Females also showed higher PSC-17-Y composite scores (M = 11.2) than males (M = 10.1), reporting more psychosocial challenges (Figure 3B). When examining the PSC-17-Y sub scores, males exhibited higher externalization scores (MMale = 3.0, MFemale = 2.6; Figure 3C), while females scored higher in both internalization (MMale = 3.1, MFemale = 4.1) and attention (MMale = 4.0, MFemale = 4.4) domains (Figures 3D,E).
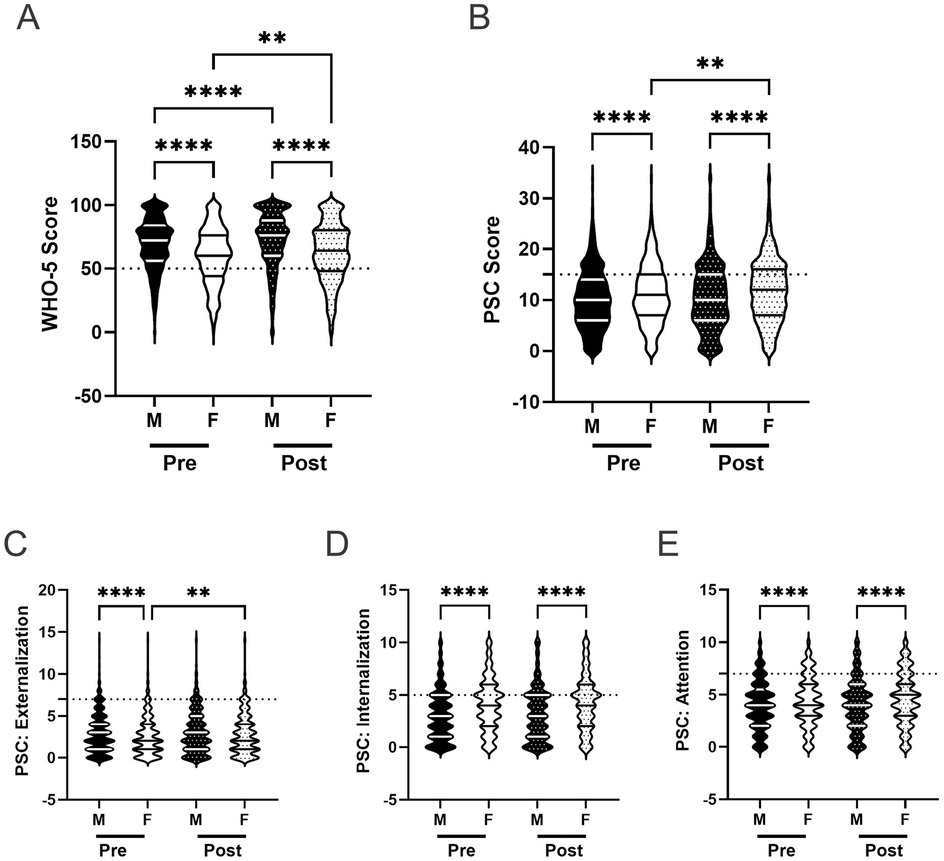
Figure 3. Gender and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (** < 0.01, **** < 0.0001). Pre-program, N = 1,853 for male, N = 1,638 for female. Post-program, N = 1,555 for male, N = 1,343 for female.
After completing the R4F program, both male and female students showed improvements in their WHO-5 scores, with males experiencing a 5% increase (MPRE = 69.5, MPOST = 72.6) and females a 5% increase (MPRE = 59.9, MPOST = 62.6) compared to before the program (Figure 3A). The gap between males and females persisted post-program. Regarding the PSC-17-Y, male students' scores did not change after completing the program, while female students' scores increased by 6% (MPRE = 11.2, MPOST = 11.9; Figure 3B).
Examining the PSC-17-Y sub scores, males showed no changes in any of the three domains following the program (Figures 3C–E). In contrast, females experienced a 15% increase in their externalization scores (MPRE = 2.6, MPOST = 3.0; Figure 3C), resulting in no significant difference between males and females in this domain post-program. Females' internalization and attention sub scores remained unchanged after the R4F program (Figures 3D,E). Notably, females maintained significantly higher internalization and attention sub scores compared to males, regardless of program participation.
We also assessed the relative risk of male and female students developing psychosocial illnesses using both the WHO-5 (Figure 4A) and the PSC-17-Y (Figure 4B). Female students were found to be at a higher relative risk for developing mental health disorders than male students across both metrics before (WHO-5: 1.9, 95% CI [1.7,2.1]; PSC: 1.2, 95% CI [1.1, 1.4) and after (WHO-5: 1.8, 95% CI [1.6,2.1]; PSC: 1.3, 95% CI [1.2, 1.5) the R4F program.
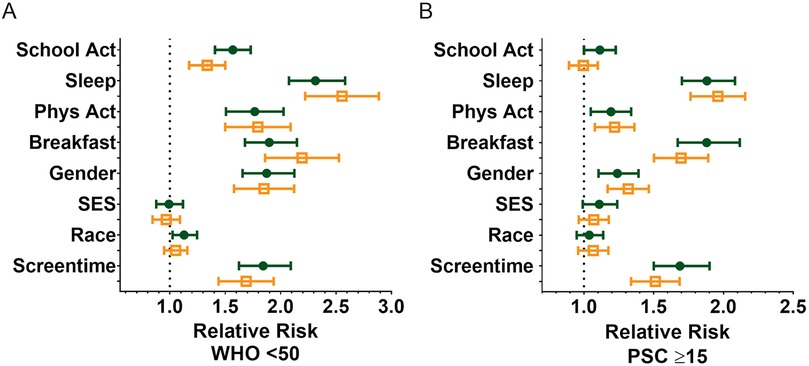
Figure 4. Impact of the R4F program on the relative risk of developing psychosocial disorders. (A) Relative risk based on WHO-5 scores below the critical cutoff of 50. (B) Relative risk based on PSC-17-Y scores 15 and above. Shown are the mean +/− 95CI before (green circles) and after (orange open squares) the program. As indicated on the figure, relative risk was performed for the influence of being involved in school activity (Y) vs. uninvolved in school activity (N) (School Activity), ≥8 h of sleep/night vs. <8 h of sleep/night (Sleep), ≥4 days/week of PA vs. <4 days/week of PA (Physical Activity), eating breakfast 7 days/week <7 days/week (Breakfast), being male vs. female (Gender), low-income vs. medium/high-income (SES), White identifying (W) vs. Underrepresented Groups (UG), ≤2 h/day screen time vs. >2 h/day of screen time (Screen time), and based on performing a Koopman asymptotic score (74).
3.1.2 Race and ethnicity
Previous research has indicated that students from underrepresented groups typically report lower scores of mental well-being, compared to their White peers (12, 87, 88). Here, we assessed whether there are differences in self-reported psychosocial well-being across students from racial and ethnic minority backgrounds and White students. We also examined whether any potential differences were affected by participation in the R4F program.
Before participating in the R4F program, both students from underrepresented groups and White students showed similar scores on most measures of psychosocial well-being, including WHO-5 composite scores (MUG = 63.3, MW = 64.1; Figure 5A), PSC-17-Y composite scores (MUG = 11.2, MW = 10.9; Figure 5B), and PSC-17-Y internalization (MUG = 3.7, MW = 3.7; Figure 5D) and attention sub scores (MUG = 4.3, MW = 4.4; Figure 5E). However, students from underrepresented groups had significantly higher externalization sub scores (M = 3.2) compared to White students (M = 2.7) prior to the program (Figure 5C).
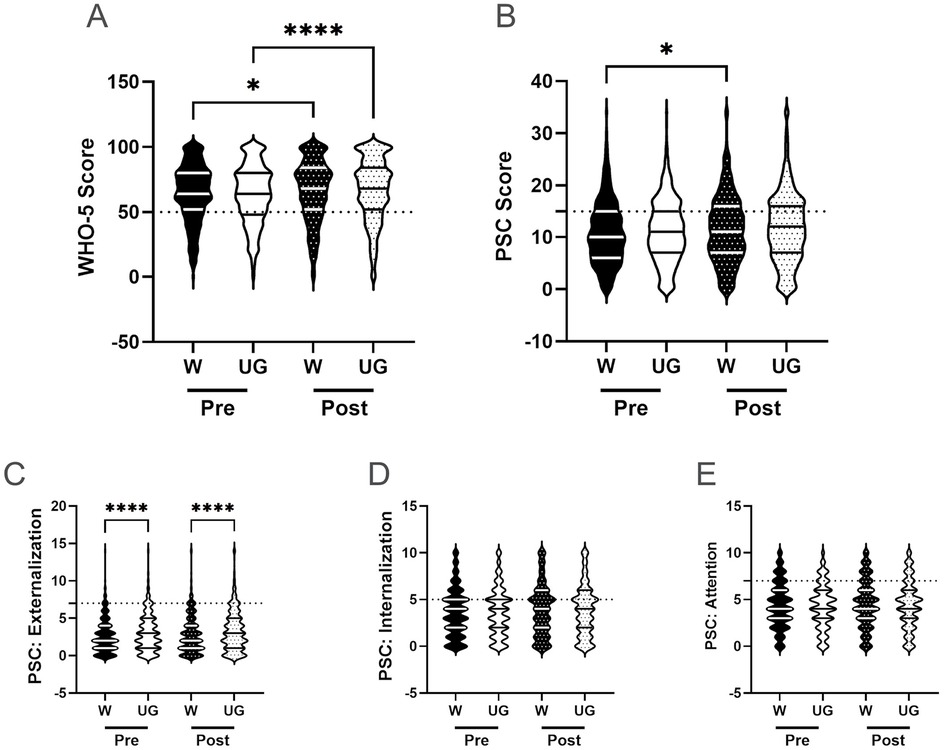
Figure 5. Racial identity and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (* < 0.05, **** < 0.0001). W = White students, UG = Underrepresented Groups. Pre-program, N = 1,588 for white students, N = 2,024 for Underrepresented Groups. Post-program, N = 1,312 for white students, N = 1,721 for Underrepresented Groups.
Upon completion of the R4F program, both groups showed improvements in WHO-5 composite scores, with White students increasing by 3% (MPRE = 64.1, MPOST = 66.0) and students from underrepresented groups by 5% (MPRE = 63.3, MPOST = 66.7; Figure 5A). There were no significant differences between the two groups either before or after the program. White students' PSC-17-Y composite scores increased following the program by 6% (MPRE = 10.9, MPOST = 11.5) while the scores of students from underrepresented groups remained unchanged (Figure 5B). No significant differences were observed between the groups after program participation.
Examining the PSC-17-Y sub scores post-program, both students from underrepresented groups and White students' sub scores showed no significant changes following the program (externalization, internalization, and attention; Figures 5C–E). The externalization sub scores of students from underrepresented groups remained elevated relative to White students after the program (MUG = 3.4, MW = 2.9; Figure 5C).
The relative risk of developing a psychosocial illness was assessed using critical clinical cutoff scores for both the WHO-5 (Figure 4A) and the PSC-17-Y (Figure 4B). Students from underrepresented groups had similar risks of poor mental well-being compared to White students before the R4F program (WHO-5: 1.1, 95% CI [1.0,1.2]; PSC: 1.0, 95% CI [0.95, 1.1) as well as following the program as delineated by the WHO-5 metric (1.0, 95% CI [0.95, 1.2) and PSC-17-Y metric (1.1, 95% CI [0.96, 1.2).
3.1.3 Socioeconomic status
We next examined the role of family socioeconomic status (SES) on adolescents' psychosocial well-being, as numerous studies have reported associations between these factors (84, 89–91). Consistent with our previous methodology, we used students' self-reported qualification for free or reduced lunch as a proxy measure for SES (12). This approach allowed us to investigate potential differences in psychosocial outcomes based on socioeconomic background within the context of the R4F program.
Prior to the R4F program, there were no significant differences between students of different socioeconomic status (SES) on their WHO-5 composite scores (Figure 6A), PSC-17-Y composite scores (Figure 6B), or any of the PSC-17-Y sub scores (externalization, internalization, and attention; Figures 6C–E). Following the R4F program, students who qualified for free or reduced lunch (low SES) showed a significant 5% increase in WHO-5 scores (MPRE = 64.4, MPOST = 67.6), while the difference in high SES students' scores was not significant (MPRE = 64.5, MPOST = 66.6; Figure 6A). There were no significant differences in WHO-5 scores between low and high SES groups, regardless of program participation. PSC-17-Y composite scores remained similar between the two SES groups both before and after the R4F program (Figure 6B).

Figure 6. Socioeconomic status and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (* < 0.05, ** < 0.01). H = intermediate/high SES, L = low SES. Pre-program N = 963 for low SES, N = 1,066 for intermediate/high SES. Post-program, N = 1,127 for low SES, N = 867 for intermediate/high SES.
Examining the PSC-17-Y sub scores, participation in the R4F program was not associated with changes in externalization and attention sub scores for either SES group, which remained similar between groups (Figures 6C,E). Internalization sub scores did not differ from pre to post program for low SES students (MPRE = 3.8, MPOST = 3.9) but increased by 11% for high SES students (MPRE = 3.5, MPOST = 3.9; Figure 6D). Despite this change, internalization sub scores were similar between SES groups both before and after the program.
There were no differences in the relative risk for either the WHO-5 or PSC-17-Y metrics both before (WHO-5: 1.0, 95% CI [.9,1.1]; PSC: 1.1, 95% CI [1.0, 1.2) and after the R4F program (WHO-5: 1.0, 95% CI [.8,1.1]; PSC: 1.1, 95% CI [1.0, 1.2), with low and high SES students having equivalent risk.
3.1.4 Club involvement
Previous research has demonstrated that participation in extracurricular activities can have positive effects on mental health and well-being (12, 92). We therefore investigated how students' involvement in at least one extracurricular activity at school (such as sports or music) may influence student mental health outcomes, and whether that interacts with participation in the R4F program. This allowed us to understand whether the R4F program's impact differed between students who were already engaged in other school activities and those who were not.
Prior to the R4F program, students involved in clubs demonstrated better psychosocial well-being compared to those without club involvement. Club-involved students had 12% higher WHO-5 scores (MEC = 65.6, MNoEC = 58.8; Figure 7A) and 7% lower PSC-17-Y scores (MEC = 10.8, MNoEC = 11.6; Figure 7B) than students who were not involved in extracurricular clubs. They also had significantly lower externalization and internalization sub scores, by 6% (MEC = 2.9, MNoEC = 3.1) and 10% MEC = 3.6, MNoEC = 4.0) respectively (Figures 7C,D). Attention sub scores were similar between the two groups (Figure 7E).
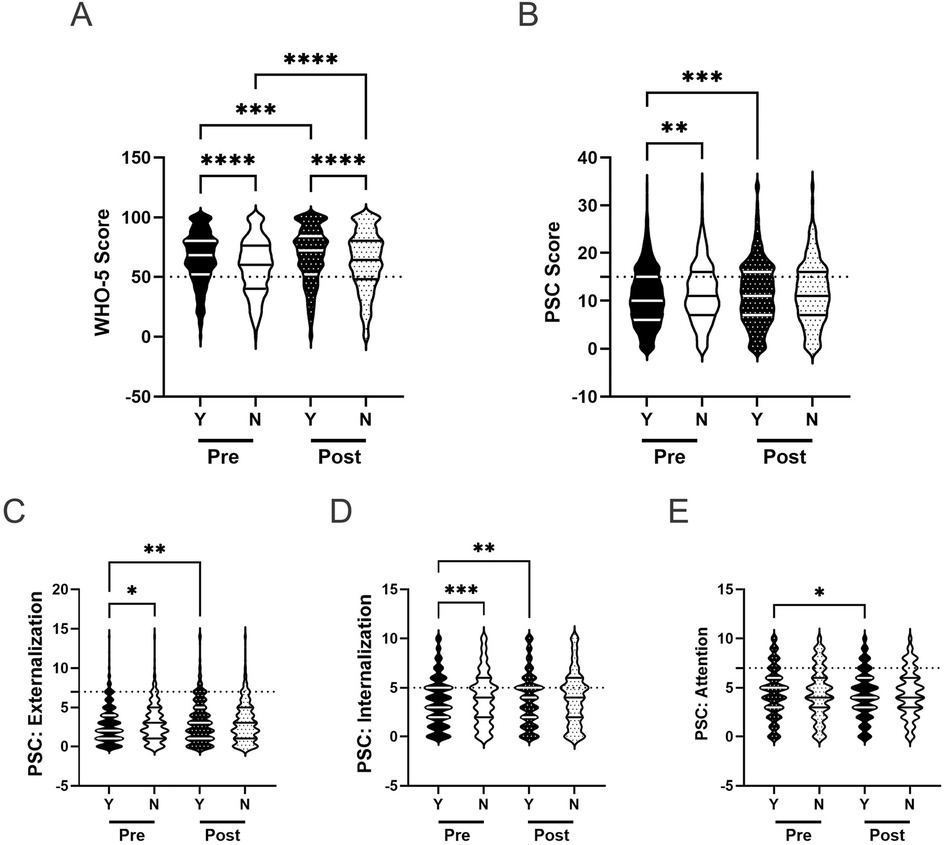
Figure 7. Participation in school activities and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (* < 0.05, ** < 0.01, *** < 0.001, **** < 0.0001). Y = Involved, N = not involved. Pre-program, N = 2,581 for involved, N = 1,343 for uninvolved. Post-program, N = 2,231 for involved, N = 1,058 for uninvolved.
Following the R4F program, both groups showed improvements in WHO-5 scores, with club-involved students increasing by 4% (MPRE = 65.6, MPOST = 68.0) and non-involved students by 7% (MPRE = 58.8, MPOST = 62.8; Figure 7A). Club-involved students maintained higher WHO-5 scores both before (12% higher) and after (8% higher) the program than non-involved students. Club participation was associated with a 7% increase in PSC-17-Y scores (MPRE = 10.8, MPOST = 11.6), while non-involved students' scores remained unchanged (MPRE = 11.6, MPOST = 11.7; Figure 7B). This resulted in similar PSC-17-Y composite scores between the two groups post-program. Examining PSC-17-Y sub scores, club-involved students showed significant increases across all domains: 10% in externalization (MPRE = 2.9, MPOST = 3.2; Figure 7C), 8% in internalization (MPRE = 3.6, MPOST = 3.9; Figure 7D), and 5% in attention (MPRE = 4.3, MPOST = 4.5; Figure 7E). In contrast, non-involved students' sub scores remained unchanged. After the R4F program, there were no significant differences in any sub score measures between the two groups.
With regards to relative risk, before the R4F program, the WHO-5 (1.6, 95% CI [1.4, 1.7), but not PSC-17-Y metric (1.1, 95% CI [1.0, 1.2), indicated that those students not involved in any extracurricular activities were at greater risk of a psychosocial disorder. Following the R4F program, students not involved in an extracurricular activity exhibited reduced relative risk as delineated by the WHO-5 metric (1.3, 95% CI [1.2, 1.5) and were not at-risk as measured by the PSC-17-Y metric (1.0, 95% CI [.9, 1.1).
3.1.5 Breakfast
CDC guidelines recommend that adolescents eat breakfast every day of the week to optimize mental health and well-being (93, 94). To better understand the relationship between breakfast consumption and student mental health, we examined students' self-reported breakfast eating habits before and after program participation. By investigating this factor, we aimed to explore how regular breakfast consumption might interact with the R4F program's effects on students' psychosocial outcomes. In addition, we examined whether there was a dose-response relationship between frequency of eating breakfast and mental well-being.
Before the R4F program, students who met daily breakfast recommendations demonstrated significantly better psychosocial well-being compared to those who did not, illustrated in the WHO-5 and PSC-17-Y metrics (Table 2). They had 17% higher WHO-5 scores (MBK = 69.5, MNoBK = 59.2; Figure 8A) and 23% lower PSC-17-Y scores (MBK = 9.4, MNoBK = 12.2; Figure 8B). Additionally, their PSC-17-Y sub scores were significantly lower: 24% for externalization (MBK = 2.5, MNoBK = 3.3; Figure 8C), 32% for internalization (MBK = 3.1, MNoBK = 4.1; Figure 8D), and 26% for attention (MBK = 3.8, MNoBK = 4.8; Figures 8E).
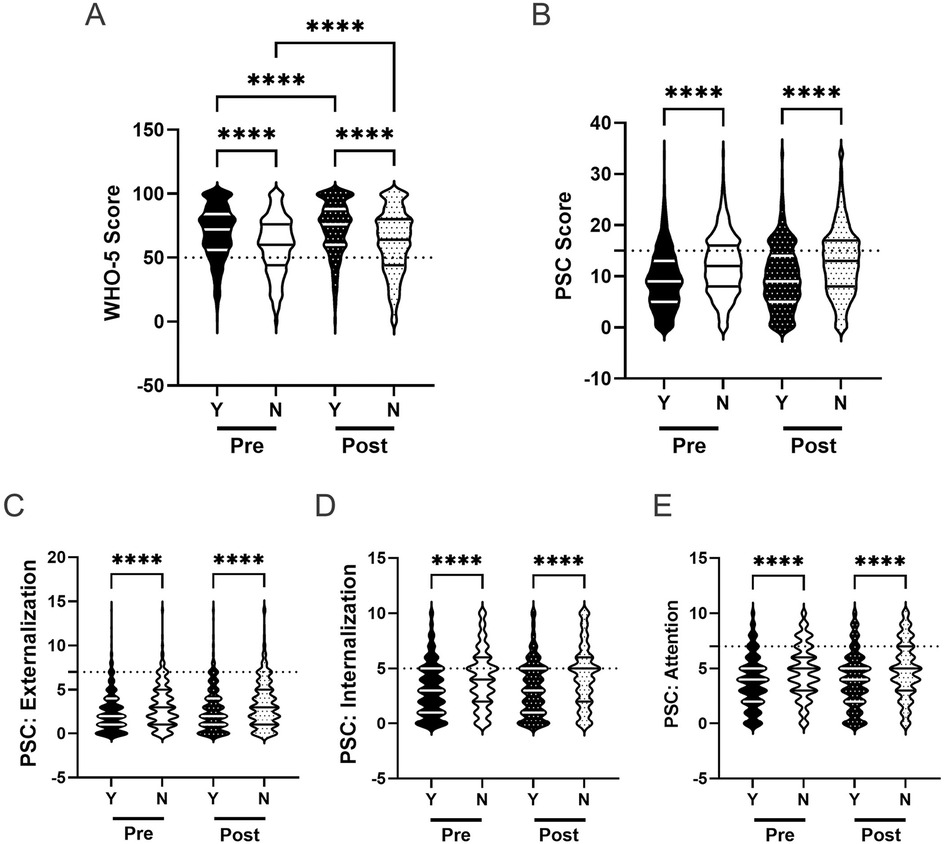
Figure 8. Impact of eating breakfast and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (**** < 0.0001). Pre-program, N = 1,560 for 7 days/week, N = 2,357 for <7 days/week. Post-program, N = 1,242 for 7 days/week, N = 2,039 for <7 days/week.
After completing the R4F program, both groups showed a 5% increase in WHO-5 scores (Figure 8A), with students meeting breakfast recommendations maintaining an 18% higher score (M = 73.2) than those who did not meet recommendations (M = 62.0). PSC-17-Y composite scores did not change for either group (Figure 8B) with the gap between students who met breakfast recommendations (M = 9.8) and those who did not (M = 12.8) persisting. Externalization, internalization, and attention sub scores also remained unchanged for both groups (Figures 8C–E), with students meeting breakfast recommendations continuing to show significantly lower sub scores than those who did not meet recommendations by 25%, 37%, and 26%, respectively.
Relative risk was also influenced by regular breakfast consumption. Across both metrics, before (WHO-5: 1.9, 95% CI [1.7,2.1]; PSC: 1.9, 95% CI [1.7, 2.1) and after R4F participation (WHO-5: 2.2, 95% CI [1.9,2.5]; PSC: 1.7, 95% CI [1.5, 1.9), students who did not meet breakfast recommendations had higher rates of poor mental health and were at a higher relative risk for developing a psychosocial disorder compared to those who met recommendations (Figures 4A,B).
To further understand the role of breakfast consumption on psychosocial well-being, we examined the association between the number of days an adolescent ate breakfast and their psychosocial wellness scores. Figure 9A shows the positive association between WHO-5 scores and the frequency of breakfast consumption. Conversely, Figures 9B–E demonstrate negative associations between breakfast frequency and PSC-17-Y composite and sub scores, indicating better well-being with more frequent breakfast consumption. These associations remained consistent following the R4F program, as the slopes of the relationships were not significantly modified by program participation.
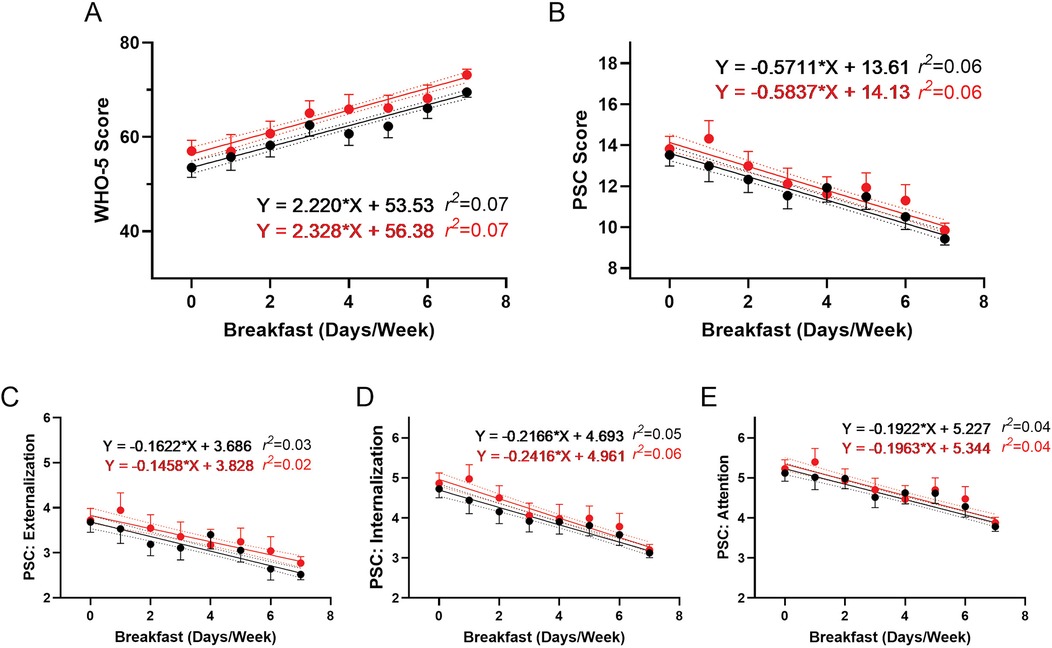
Figure 9. Association of eating breakfast and the effectiveness of the R4F program on psychosocial wellness. (A) WHO-5 well-being scores. (B) PSC-17-Y composite well-being scores. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention. Black dots and lines and for pre-program; Red dots and lines are for post-program. Shown are the mean +/− 95CI, a linear curve fit (solid lines) and 95CI for the linear regression analysis (dotted lines) between the WHO-5 or PSC-17-Y scores and the number of days the participants ate breakfast each week. Also shown are the regression formulae and r2 value for each regression analysis.
3.1.6 Physical activity
The impact of PA on mental health is best established in adult populations, with causality in children and adolescents remaining unresolved (12, 95–97). Towards this end, we examined the role of self-reported students' PA frequency and its effects on psychosocial well-being and whether there was an interrelationship with the R4F program.
Prior to the R4F program, adolescents who participated in PA 4 or more days per week demonstrated 15% higher WHO-5 scores (M = 71.4) compared to those who did not meet this threshold (M = 60.5; Figure 10A). They also showed significantly lower PSC-17-Y composite scores by 12% (MPA = 10.2, MNoPA = 11.4), as well as PSC-17-Y sub scores (externalization, internalization, and attention; Figures 10B–E) by 4% (MPA = 2.9, MNoPA = 3.0), 22% (MPA = 3.2, MNoPA = 3.9), and 9% (MPA = 4.1, MNoPA = 4.5), respectively (Table 2).
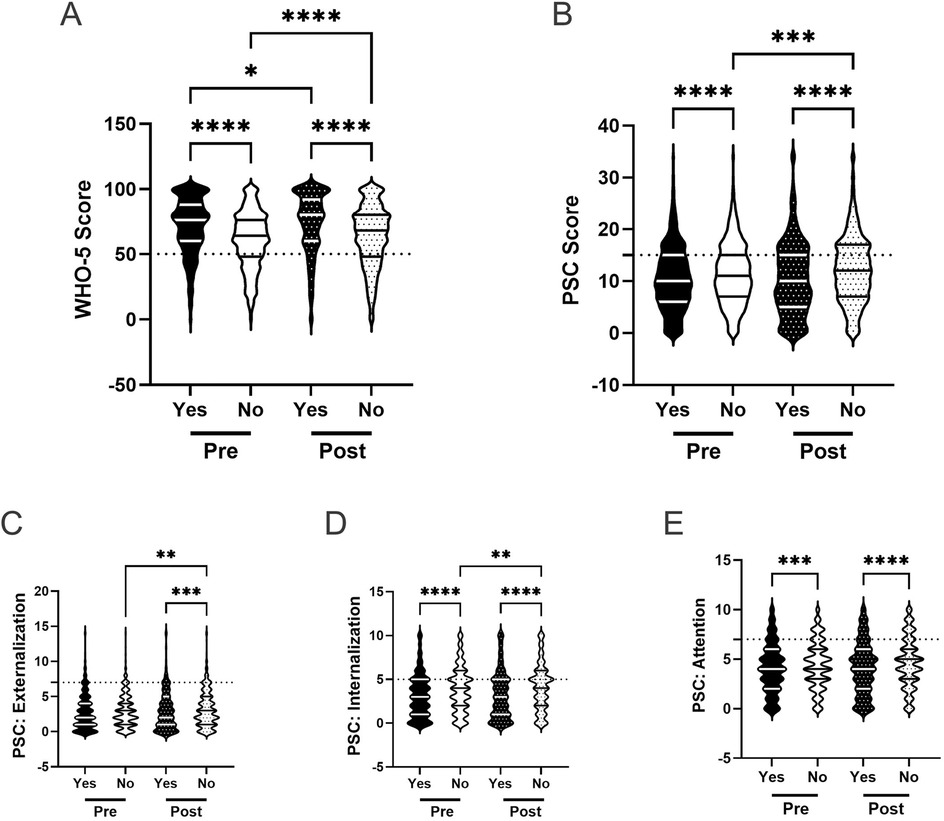
Figure 10. Physical activity and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (* < 0.05, **** < 0.0001). Pre-program, N = 1,006 for ≥4 days/week, N = 2,901 for <4 days/week. Post-program, N = 911 for ≥4 days/week, N = 2,364 for <4 days/week.
Following the R4F program, WHO-5 scores increased for both groups: 3% for students meeting PA recommendations (MPRE = 71.4, MPOST = 73.8) and 5% for those who did not (MPRE = 60.5, MPOST = 63.4; Figure 10A). Post program, students exercising at least 4 days weekly had 14% higher WHO-5 scores than those who did not. PSC-17-Y composite scores increased by 3% for students who met PA recommendations (MPRE = 10.2, MPOST = 10.5) and were increased by 6% for those who did not (MPRE = 11.4, MPOST = 12.1; Figure 10B). Post-program, students meeting activity guidelines had 16% lower PSC-17-Y scores than those who did not. PSC-17-Y sub scores showed no differences after the program compared to before the program for both groups, (Figures 10C–E) with students who met PA recommendations continuing to have lower externalization, internalization, and attention sub scores than those who did not meet recommendations by 9%, 26%, and 13%, respectively (Table 2).
The relative risk of developing a psychosocial illness, assessed using critical clinical cutoff scores for both the WHO-5 (Figure 4A) and PSC-17-Y (Figure 4B), indicated that students not meeting PA recommendations consistently were at higher risk for developing psychosocial disorders, both before (WHO-5: 1.8, 95% CI [1.5,2.0]; PSC: 1.2, 95% CI [1.1, 1.3) and after the R4F program (WHO-5: 1.8, 95% CI [1.5,2.1]; PSC: 1.2, 95% CI [1.1, 1.4).
Further analysis of the association between PA frequency and psychosocial well-being scores revealed a positive correlation with WHO-5 scores (Figure 11A) and negative correlations with PSC-17-Y composite and sub scores (Figure 11B–E), both before and after the R4F program. These relationships indicate that more frequent PA is associated with better psychosocial well-being outcomes.
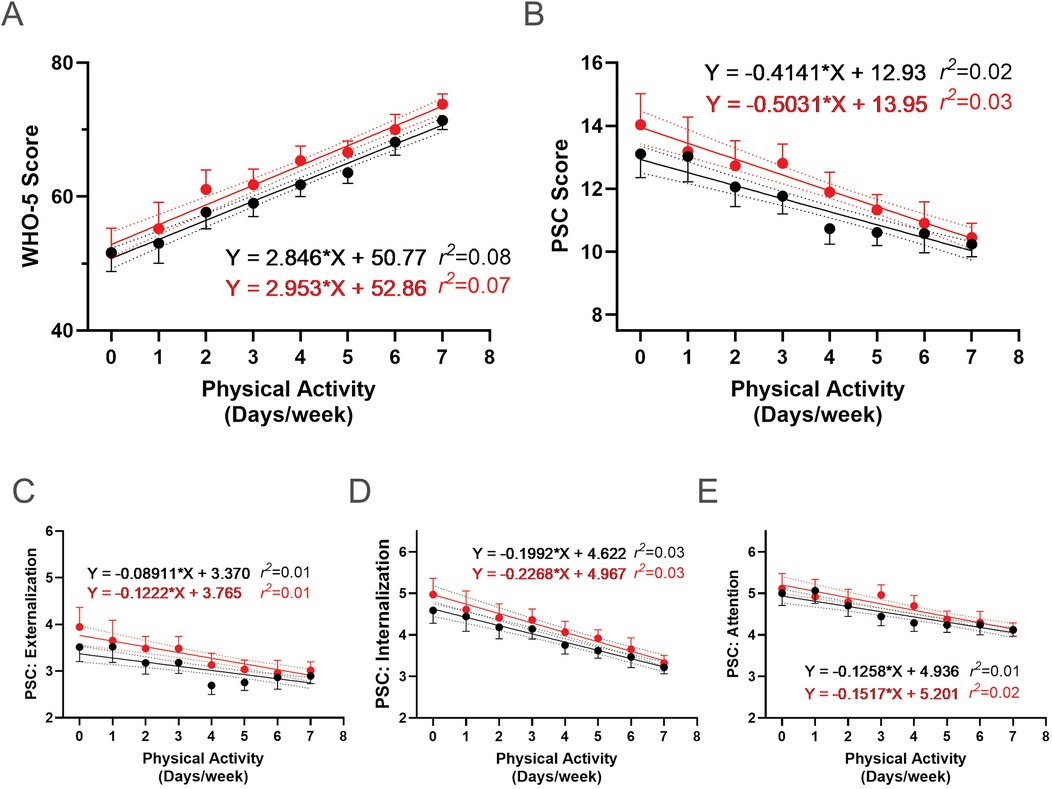
Figure 11. Association between physical activity and the effectiveness of the R4F program on psychosocial wellness. (A) WHO-5 well-being scores. (B) PSC-17-Y composite well-being scores. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention. Black dots and lines and for pre-program; Red dots and lines are for post-program. Shown are the mean +/− 95CI, a linear curve fit (solid lines) and 95CI for the linear regression analysis (dotted lines) between the WHO-5 or PSC-17-Y scores and the number of days participants met physical activity guidelines each week. Also shown are the regression formulae and r2 value for each regression analysis.
3.1.7 Screen time
Current literature suggests that spending more than 2 h a day on electronic devices negatively impacts psychosocial well-being (12, 98). We examined the influence of screen time on student well-being, along with whether this changes after participation in the R4F program. Before the R4F program, students who adhered to the 2 h screen time recommendation demonstrated better psychosocial well-being, with significantly higher WHO-5 scores (MST = 69.4, MNoST = 59.9) and significantly lower PSC-17-Y composite scores (MST = 9.5, MNoST = 12.0) by 13% and 27%, respectively, compared to those exceeding 2 h a day (Figures 12A,B). Students exceeding the screen time recommendation also had significantly higher baseline externalization, internalization, and attention sub scores by 22% (MST = 2.5, MNoST = 3.2), 21% (MST = 3.2, MNoST = 4.1), and 20% (MST = 3.8, MNoST = 4.7), respectively (Figures 12C–E).
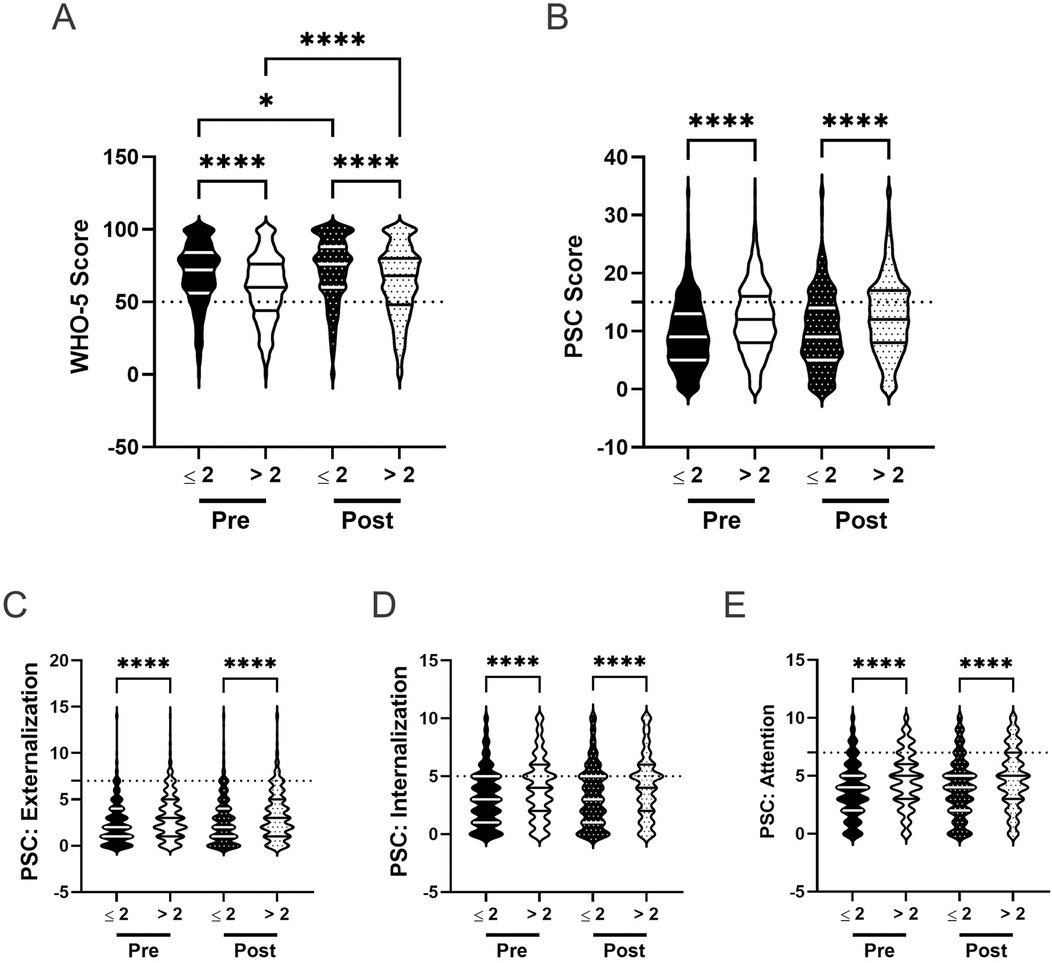
Figure 12. Screen time and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (* < 0.05, **** < 0.0001). Pre-program, N = 1,444 for ≤2 h/day, N = 2,459 for >2 h/day. Post-program, N = 1,111 for ≤2 h/day, N = 2,165 for >2 h/day.
Following the R4F program, both groups showed improvements in WHO-5 scores: a 3% increase for those meeting the screen time recommendation (MPRE = 69.4, MPOST = 71.7) and a 6% increase for those exceeding it (MPRE = 59.9, MPOST = 63.5; Figure 12A). Students adhering to the 2 h limit maintained 11% higher WHO-5 scores than those who did not meet the recommendation after the program. Both groups showed no change in PSC-17-Y scores, with students who adhered to screen time recommendations maintaining significantly lower PSC-17-Y scores (MPRE = 9.5, MPOST = 10.1), by 24%, compared to those that did not (MPRE = 12.0, MPOST = 12.5; Figure 12B). There were no significant changes in externalization, internalization, or attention sub scores for either group following the R4F program (Figures 12C–E), with students exceeding screen time recommendations maintaining significantly higher sub scores after the program by 24%, 26%, and 22%, respectively (Table 2).
The relative risk of developing a psychosocial illness, assessed using critical clinical cutoff scores for both the WHO-5 and PSC-17-Y, indicated that students exceeding screen time recommendations were consistently at higher risk for developing psychosocial disorders, both before (WHO-5: 1.8, 95% CI [1.6,2.1]; PSC: 1.7, 95% CI [1.5, 1.9) and after the R4F program (WHO-5: 1.7, 95% CI [1.4,1.9]; PSC: 1.5, 95% CI [1.3, 1.7).
Further analysis revealed a negative association between screen time use and WHO-5 scores, with fewer hours of screen time correlating with higher WHO-5 scores (Figure 13A). Conversely, there was a positive association between screen time use and PSC-17-Y composite and sub scores (Figures 13B–E), with fewer hours correlating with lower scores. These associations remained consistent following the R4F program, as the slopes of the relationships were not significantly altered by program participation.
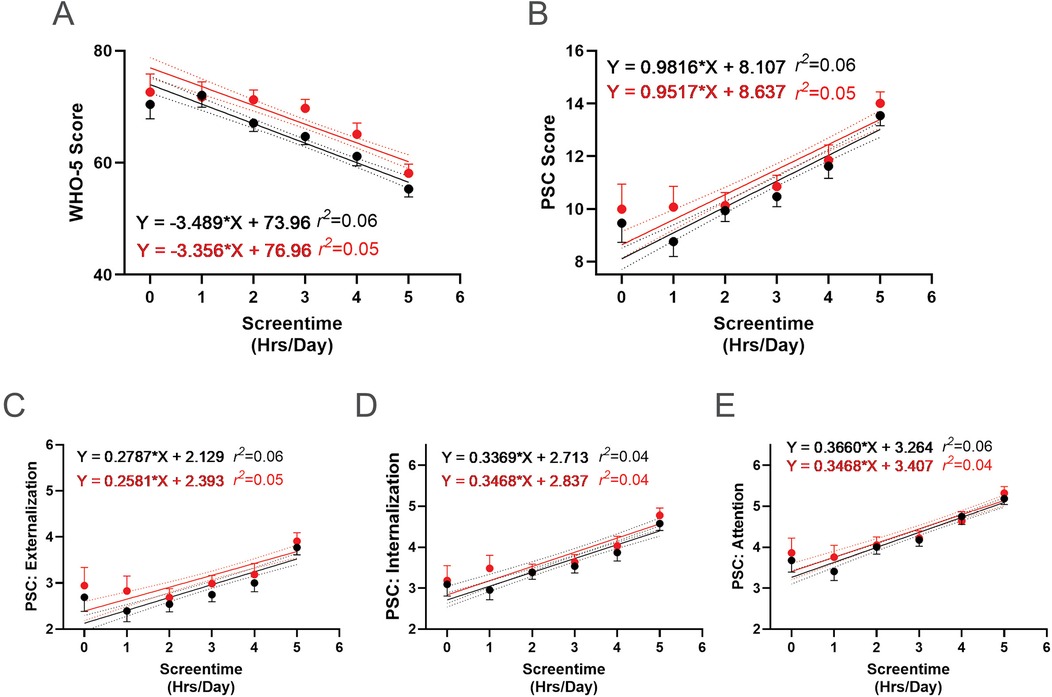
Figure 13. Association between screen time and the effectiveness of the R4F program on psychosocial wellness. (A) WHO-5 well-being scores. (B) PSC-17-Y composite well-being scores. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention. Black dots and lines and for pre-program; Red dots and lines are for post-program. Shown are the mean +/− 95CI, a linear curve fit (solid lines) and 95CI for the linear regression analysis (dotted lines) between the WHO-5 or PSC-17-Y scores and the number of screentime hours participants had each day. Also shown are the regression formulae and r2 value for each regression analysis.
3.1.8 Sleep
Current literature suggests that sleeping 8 or more hours a night positively impacts psychosocial well-being (12, 99, 100). We assessed whether meeting sleep recommendations positively influences students well-being, and whether this is impacted by participating in the R4F program. Before the R4F program, students meeting sleep recommendations demonstrated better psychosocial well-being, with 19% higher WHO-5 scores (MS = 68.8, MNoS = 55.7; Figure 14A) and 34% lower PSC-17-Y scores (MS = 9.7, MNoS = 13.0; Figure 14B) compared to those not meeting recommendations. They also showed significantly lower baseline externalization, internalization, and attention sub scores by 36% (MS = 2.6, MNoS = 3.5), 38% (MS = 3.2, MNoS = 4.5), and 29% (MS = 3.9, MNoS = 5.0), respectively (Figures 14C–E).
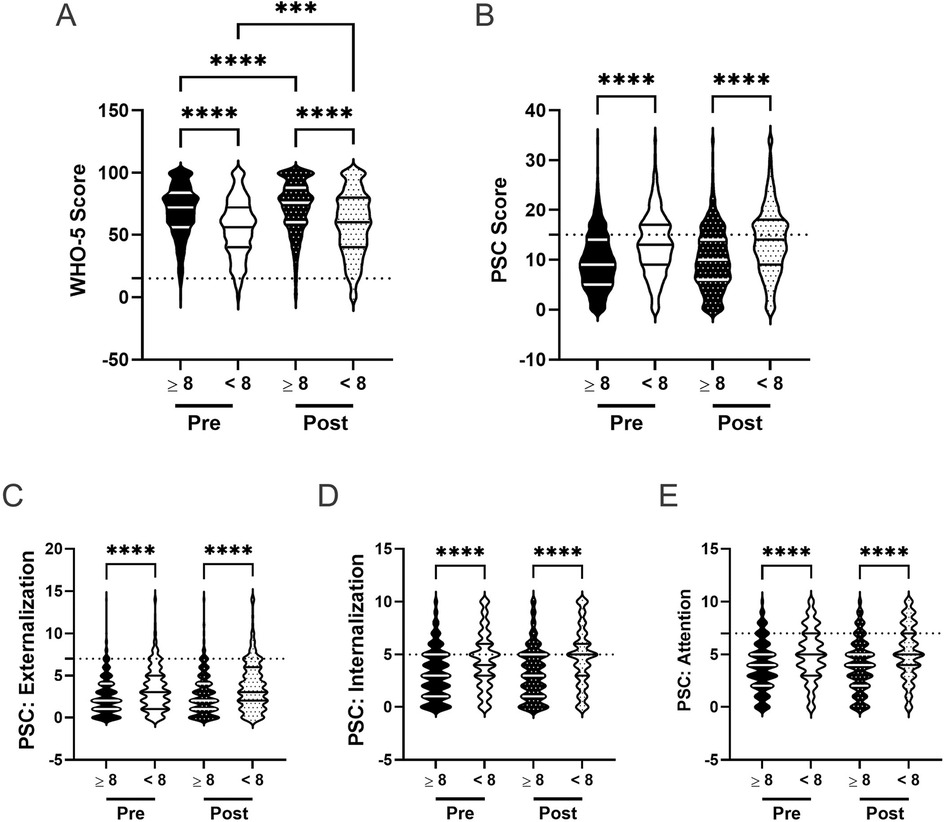
Figure 14. Impact of sleep and the effectiveness of the R4F program on psychosocial wellness. (A) Distribution of WHO-5 well-being scores in a violin plot. Dashed horizontal line shows the critical risk cutoff of 50 points with lower scores indicating lower well-being. (B) Distribution of PSC-17-Y composite well-being scores with a critical risk cutoff of 15 points. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention on violin plots with critical risk cutoffs of 7 points, 5 points, and 7 points, respectively. Higher scores indicate lower well-being. Within each violin plot the median and 25% and 75% quartiles are shown. Asterisks denote significant difference between groups based on a Kruskal–Wallis One-way ANOVA with a Dunn's multiple comparison test based on ranks (*** < 0.001, **** < 0.0001). Pre-program, N = 2,254 for sleeping ≥ 8 h/night, N = 1,648 for sleeping < 8 h/night. Post-program, N = 1,826 for sleeping ≥ 8 h/night, N = 1,441 for sleeping < 8 h/night.
Following the R4F program, both groups experienced a 5% increase in WHO-5 scores (Figure 14A), with students meeting sleep recommendations maintaining 20% higher scores (MPRE = 68.8, MPOST = 72.5) than those who did not meet recommendations (MPRE = 55.7, MPOST = 58.3). PSC-17-Y composite scores remained unchanged for both groups (Figure 14B), with students not meeting sleep recommendations (MPRE = 13.0, MPOST = 13.7) consistently showing significantly lower scores post program than those who met sleep recommendations (MPRE = 9.7, MPOST = 10.0). There were no significant changes in PSC-17-Y sub scores for either group (Figures 14C–E), but these sub scores remained lower in students meeting sleep recommendations, being 37% for externalization, 42% for internalization, and 33% for attention (Table 2).
The relative risk of developing a psychosocial illness, assessed using critical clinical cutoff scores for both the WHO-5 (Figure 4A) and PSC-17-Y (Figure 4B), indicated that students not meeting sleep recommendations were consistently at higher risk for developing psychosocial disorders, both before (WHO-5: 2.3, 95% CI [2.1,2.6]; PSC: 1.9, 95% CI [1.7, 2.1) and after the R4F program (WHO-5: 2.5, 95% CI [2.2,2.9]; PSC: 2.0, 95% CI [1.8, 2.1).
We also examined whether there were dose-response relationships between sleep and student well-being. There was a positive association between sleep duration and WHO-5 scores, with more hours of sleep a night correlating with higher WHO-5 scores (Figure 15A). Conversely, there was a negative association between sleep duration and PSC-17-Y composite and sub scores (Figures 15B–E), with more hours of sleep correlating with lower scores, indicating better well-being. These associations remained consistent following the R4F program, as the slopes of the relationships were not significantly altered by program participation.
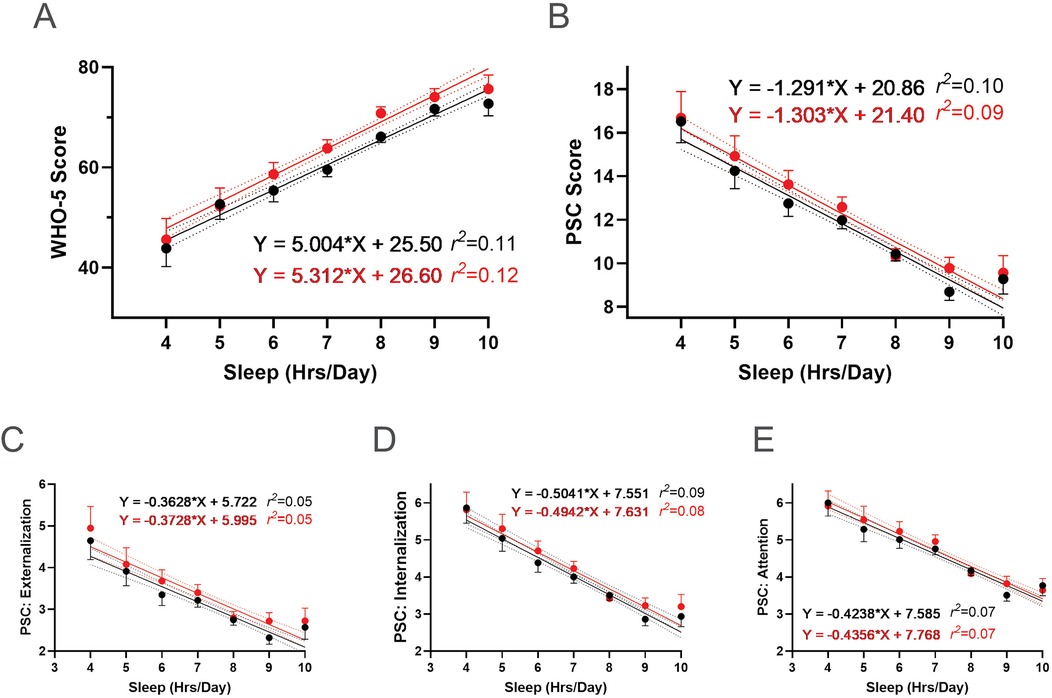
Figure 15. Association between sleep and the effectiveness of the R4F program on psychosocial wellness. (A) WHO-5 well-being scores. (B) PSC-17-Y composite well-being scores. (C–E) PSC-17-Y sub scores of externalization, internalization, or attention. Black dots and lines are for pre-program; Red dots and lines are for post-program. Shown are the mean +/− 95CI, a linear curve fit (solid lines) and 95CI for the linear regression analysis (dotted lines) between the WHO-5 or PSC-17-Y scores and the number of hours of sleep participants had each night. Also shown are the regression formulae and r2 value for each regression analysis.
4 Discussion
The results of our study on the Riding for Focus (R4F) program in a post-COVID cohort of adolescents reveal a complex picture of its impact on mental health and well-being. Our findings both align with and diverge from our previous research, highlighting the multifaceted nature of adolescent mental health interventions. This topic holds great significance as we have seen poor mental health symptoms become more evident post-COVID-19 pandemic (2–5).
The study revealed persistent gender disparities in adolescent mental health outcomes, both before and after the Riding for Focus (R4F) program, highlighting the complex interplay of these factors (12). Additionally, mental health disparities were observed in students who did not meet recommendations for breakfast consumption, PA, sleep duration, and screen time. Further, these modifiable factors had a dose-dependent impact on student mental well-being, with incremental improvements in both WHO-5 and PSC-17-Y scores for each additional day or hour closer to the recommendation. These findings underscore the need for tailored interventions to address diverse student populations effectively, considering multiple lifestyle factors that impact adolescent well-being.
Similar to our earlier study, we observed a modest increase in WHO-5 composite scores following program participation, which is associated with an improvement in overall well-being. However, unlike our previous findings (12), we also observed small increases in PSC-17-Y scores, suggesting that participants may exhibit a potential decline in some aspects of psychosocial functioning. These contrasting results warrant careful interpretation (63, 68). Importantly, although the changes in both the WHO-5 and PSC-17-Y scores from pre- to post-program are statistically significant, their biological or clinical significance remains uncertain due to the modest magnitude of these changes. In comparison to the current studies, we previously observed much larger, dose-dependent improvements when participants met various lifestyle recommendations. This suggests that the modest shifts seen in the current analysis may not be directly attributable to participation in the program. Instead, they could reflect natural variation over time or other unrelated factors. To clarify the true impact of program participation, further research is needed. These future studies should include appropriate comparison groups to help distinguish between changes that occur naturally and those that result specifically from involvement in the program.
There were also differences between the study populations in the current study and our previous work that may have influenced our findings. First, the current sample reflects a broader racial composition than our previous study. In addition, Dementyev et al. (12) was conducted during the 2020–2021 school year at the height of the COVID-19 pandemic, involving a limited cohort from 20 North American schools, most of which were under pandemic restrictions. In comparison, the current study was conducted post-peak COVID-19 during the 2021–2022 school year, included 31 schools, and had more than three times as many responses, with most schools open. Post COVID-19, many adolescents are facing a complex web of social and emotional challenges that are not captured in this study and cannot be expected to be resolved through participation in a cycling program alone. Indeed, the lack of significant change in relative clinical risk for mental health disorders following the R4F program is noteworthy. This stability suggests that the program may influence self-reported well-being and symptom awareness. However, on its own, the R4F program may not substantially alter the underlying risk for clinical mental health disorders in the short term. These findings align with research indicating that mental health interventions often require sustained effort and time to produce clinically significant changes (101–103). Overall, this study provides insights on how numerous factors contribute to the mental health and well-being of a broader sample of American adolescents and explores recovery following pandemic-era restrictions.
4.1 Gender
The current study builds upon our previous research demonstrating that participating in the R4F program is associated with better psychosocial well-being in adolescents, as evidenced by increased WHO-5 scores (12). Our findings regarding gender differences in mental health outcomes align with both our earlier work and the broader literature (29, 95, 104). Consistent with previous studies, our results show that males generally report better psychosocial well-being and a reduced risk of potential mental health issues compared to females (12). This gender disparity in mental health outcomes has been well-documented, particularly in the context of the COVID-19 pandemic (2, 104). Research suggests that females report lower mental well-being and are at greater risk for poor mental health outcomes compared to males (105–109). These differences have been attributed to a combination of biological and non-biological factors. These include gender-specific stressors, societal expectations, differences in mood symptom development, disproportionate hormonal transitions, lower life satisfaction, and higher levels of psychological distress among females (2). Additionally, females tend to participate in PA less frequently compared to their male counterparts (110), which may also contribute to these disparities in mental health outcomes (95, 104). However, it's important to note that the relationship between PA and mental health is complex and understudied, with mental health status potentially influencing PA habits and vice versa (111–113). Promoting PA opportunities that are supportive and tailored to the interests of female students is essential for beginning to close the gender gap in participation (110). Epidemiological evidence consistently demonstrates a pronounced female predominance in the prevalence of depression, with women being approximately twice as likely as men to experience depressive symptoms. Although studies suggest a narrowing of this gender disparity, the divergence typically emerges around age 12, peaks during mid-adolescence (around age 16), and subsequently declines, stabilizing in adulthood (105, 106, 108, 109). Our findings regarding the potential prevalence of psychiatric disorders across genders align with the existing literature, which consistently reports higher rates of mood, anxiety, trauma-related, and depressive disorders in females. Our findings regarding the prevalence of specific types of disorders among genders are also consistent with existing literature such as increased mood, anxiety, trauma-related, and depressive disorders seen in females and (105, 106, 108, 109).
4.2 Race
Studies often show that adolescents from racial and ethnic minority backgrounds report higher rates of experiencing mental and behavioral health (MBH) conditions-including anxiety, depression, ADHD, impulse control disorder, but are also less likely to access treatment services (114). This lack of care often results in more persistent and more severe MBH conditions. Additionally, racial and ethnic minority adolescents are less frequently offered high-quality, evidence-based care and are more likely to face adverse stressors early in life, such as toxic environments, cultural hardships, and macro-societal factors (115, 116). However, in contrast to this previous work, we did not observe consistent differences in mental well-being outcomes between students from underrepresented groups and white students. This is in line with the most recent Youth Risk Behavior Surveillance System (YRBSS) data from the CDC (88), whereby across most mental health measures, there were not significant differences across racial and ethnic groups. Of course, factors contributing to overall mental health are complex, and several factors may have contributed to this change. For example, our earlier study was conducted during the COVID-19 pandemic—a period that disproportionately affected the mental health of UG students compared to their White counterparts (84, 117). In addition, these results highlight potential differences among the schools that chose to implement the R4F program compared to those that do not, as they are offering increased access to additional programming to their students. Such opportunities, including tailored social-emotional learning curricula, targeted teacher and student training programs, and increased access to after-school programming opportunities are all associated with better mental health outcomes among students (118–121). Ultimately, identifying the precise and complex factors underlying these findings is beyond the scope of our current study, but warrants additional investigation given the potential mental health benefits for students.
4.3 Socioeconomic status
We did not observe any significant differences in student well-being across students from low and high SES backgrounds. This result is surprising based on previous research on socioeconomic disparities in adolescent mental health, which typically shows a higher prevalence of externalizing, internalizing, and attention behavior issues among students from low SES households (122–124). Two possible reasons for the lack of difference may be due to the schools that tend to implement the R4F program, as well as reliance on student self-report data. Many students either were not aware of their free or reduced lunch status (39% stated “I don’t know”) or did not want to share it, which could lead to student self-report of free and reduced lunch being less reliable. Secondarily, the wide range of social vulnerability indices among the sampled schools reflects the diversity in socioeconomic context among the sampled participants, which may contribute to the differences in student well-being that could impact study outcomes.
However, students from low SES backgrounds reported higher levels of well-being (WHO-5) after participating in the R4F program compared to before the program. Yet, there was not a statistically significant change in students from high SES backgrounds. These findings contrast with our previous work (12). This difference may reflect the changing influence of COVID-19-related stressors on low SES student mental health, which may have been more prominent in our earlier cohort but less so in this more recent, post-pandemic lockdown group (125).
Lower SES households are likely to have reduced access to sport facilities, related equipment, and other activities known to improve mental health (113, 126), which may have been exacerbated by the pandemic (127, 128). The subsequent school year may have seen a restoration of these opportunities, contributing to the observed improvements (125). This underscores the potential importance of easily accessible, school based, programs for adolescents from low SES backgrounds, such as the R4F program. Schools may be uniquely positioned to intervene in the traditionally bidirectional, positively-reinforcing relationship between low SES and poor mental health by providing such programs (129–131). However, these differences could also be attributed to factors not accounted for in this study, such as geographical and economic barriers, nutritional status, or other variables that interact with socioeconomic status to influence mental health outcomes. Further research is needed to elucidate these potential confounding factors and their impact on the effectiveness of programs like R4F across different socioeconomic groups.
4.4 Club involvement
Students involved in extracurricular clubs exhibited higher levels of psychosocial well-being both before and after participating in the R4F program. Numerous studies support this observation, demonstrating that participation in extracurricular activities predicts positive outcomes among adolescents including improved social belonging, reduced depression, better mental health, increased civic engagement, and higher educational achievement (132–135).
However, participating in the R4F program was associated with better WHO-5 scores for students who were not engaged in clubs. This suggests that structured PA programs offered during the school day in a non-competitive setting can provide positive avenues for social interaction, confidence-building, and improved well-being. This finding aligns with research highlighting the psychological, educational, and social health benefits of participation in club-based or team-based sports (103, 136, 137). While the R4F program may not fully replace the positive aspects of extracurricular club involvement, it appears to offer valuable opportunities for enhancing mental health and well-being, particularly for students with limited access to traditional extracurricular activities.
Examining the common elements between clubs and the R4F program could provide valuable insights for shaping school policies. Both clubs and the R4F program offer opportunities for skill development, social interaction, and a sense of belonging, which are crucial factors in promoting adolescent well-being. The quality of experiences in organized activities, rather than mere participation, may be key to understanding their developmental benefits (138). Integrating structured PA programs like R4F into the school day could complement existing extracurricular offerings and provide more equitable access to the mental health benefits associated with organized activities. Future research should focus on identifying the specific mechanisms through which these programs enhance adolescent well-being and how they can be optimally implemented in diverse school settings.
4.5 Breakfast
Participation in the R4F program was associated with increased WHO-5 scores, regardless of whether students ate breakfast daily or not. However, students who ate breakfast daily had significantly higher baseline and post-program WHO-5 scores than those who did not eat breakfast daily. This aligns with existing evidence suggesting that breakfast consumption is associated with improved mental health and well-being in adolescents (79, 139, 140).
In addition, we observed a dose-dependent relationship between the number of days students reported eating breakfast and their psychosocial well-being, a finding supported by current literature (79, 141). For instance, a nearly linear relationship has been observed between higher frequency of breakfast consumption and greater life satisfaction in children and adolescents (79). To build on these findings, future research should explore not only the frequency of breakfast consumption but also the quality of the breakfast consumed in relation to PA, given their potentially synergistic impact on student psychosocial well-being and associations with better mental health outcomes in adolescence (139, 141). Indeed, as cycling can be a vigorous activity, ensuring students are properly fueled before going for a bicycle ride can ultimately impact their experience with the activity.
4.6 Physical activity
We observed higher WHO-5 scores following participating in the R4F program compared to before participating in the program, regardless of whether the students were regularly active outside of the program. However, both at baseline and after participating in the program, students who were active at least 4 days a week had higher WHO-5 and lower PSC-17-Y scores, aligning with previous work (12, 142). In addition, students who reported being active at least 4 days a week also had lower externalization, internalization, and attention sub scores both pre- and post-program compared to those who were not regularly active. This finding is consistent with existing literature (143, 144), which suggests that PA can be an important tool that helps reduce anxiety, mood disorders, and ADHD symptoms.
We also saw a clear dose-dependent relationship between the number of days of PA reported and the WHO-5 and PSC-17-Y scores. In line with current PA recommendations (27, 88, 95), we observed the highest levels of student well-being, across both measures, in those who reported being active 7 days a week. However, this must be balanced against the observation that those already meeting PA recommendations experienced only modest increases in their mental health and wellness scores. These findings illustrate that further research is needed to resolve the optimal frequency and intensity of PA for maximizing mental health benefits in adolescents (95, 104).
4.7 Screen time
The relationship between PA, screen time, and adolescent mental health is complex and increasingly relevant in our digital era. Our study builds upon previous research and provides new insights into this relationship, particularly regarding the impact of interventions like the R4F program (12). Consistent with existing literature, we found that students adhering to screen time recommendations generally reported better psychosocial well-being (98, 145, 146). In addition, students who exceeded the recommended screen time of 2 h per day also reported significantly higher PSC-17-Y externalization, internalization, and attention sub scores than students who met screen time recommendations. This observation is consistent with studies reporting associations between excessive screen time use and various mental health challenges, including behavioral issues, emotional problems, and attention difficulties (147, 148). However, we also observed that participating in the R4F program was associated with larger changes in mental well-being for students who did not meet screen time recommendations compared to those who met the recommendations. While more research is needed, cycling may be a particularly promising intervention for adolescents with higher screen time use, an important consideration given the increasing time young people spend on electronic devices. However, the persistence of the gap in WHO-5 scores, PSC-17-Y composite scores, and PSC-17-Y sub scores between the two groups indicates that the benefits of limited screen time remain significant even after the intervention.
Our study also identified a dose-response relationship between screen time and mental health outcomes. The negative association between screen time use and WHO-5 scores, coupled with the positive association with both the PSC-17-Y composite and sub scores, suggests that even incremental increases in screen time may have negative impacts on mental health. This relationship persisted after the R4F program, indicating that the impact of screen time on mental health is robust and cannot be fully offset by PA intervention on its own (145, 149–151). Further, while PA interventions like R4F show promise in improving some mental health outcomes (12, 145, 149), they do not comprehensively address all aspects of psychosocial well-being, especially for heavy screen users. The program's limited impact on certain mental health risks associated with excessive screen time warrants further investigation.
4.8 Sleep
The influence of sleep on adolescent psychosocial well-being and the efficacy of the R4F program is a critical area of investigation, given the importance of adequate sleep for mental health (12, 99, 100). Our findings provide compelling evidence for the significant role of sleep in adolescent mental health and its interaction with PA interventions. Both before and after participating in the R4F program, students meeting sleep recommendations demonstrated markedly better psychosocial well-being than those who did not. Additionally, students who slept at least 8 h a night exhibited lower baseline externalization, internalization, and attention sub scores. These results align with existing literature emphasizing the positive impact of adequate sleep on various aspects of mental health and cognitive function in adolescents (152, 153).
Participation in the R4F program was associated with modest improvements in student well-being, regardless of meeting sleep recommendations, consistent with our previous findings (12). However, sleep is an important factor contributing to overall mental well-being, and participating in R4F alone is not enough to overcome poor sleep. Indeed, large gaps in well-being scores persisted between those who did and did not report meeting sleep recommendations.
Our analysis of relative risk for developing psychosocial illness reveals a concerning trend and again supports our earlier work (12). Students not meeting sleep recommendations consistently demonstrated higher rates of poor mental health and an elevated risk for psychosocial disorders, both before and after the R4F program. This finding highlights the critical role of sleep in mental health resilience and suggests that PA interventions alone may not be sufficient to mitigate the risks associated with inadequate sleep.
The observed dose-response relationships between sleep duration and mental health outcomes provide valuable insights into adolescent well-being. Our findings reveal a positive association between sleep duration and WHO-5 scores and a negative association between sleep duration and PSC-17-Y composite and sub scores. Each additional hour of sleep incrementally improved mental health and well-being scores in the adolescents of our study. These results align with current literature (150), which emphasizes the importance of adequate sleep for mental health. Importantly, even modest increases in sleep duration were associated with measurable improvements in mental health outcomes. These findings underscore the independent and enduring role of sleep in adolescent mental health, highlighting the need for sleep-focused interventions alongside PA programs to comprehensively support adolescent well-being.
5 Limitations
Our investigation into the R4F program's effects on adolescent mental health and well-being in a post-pandemic cohort reveals a nuanced landscape of outcomes. The results, while partially consistent with our earlier findings, also demonstrate some departures, underscoring the intricate nature of mental health interventions for adolescents (12). While the anonymous nature of our surveys, the lack of a comparison group, and the pandemic-emergent context influenced our ability to draw causal conclusions, the study nonetheless provides valuable insights into the program's potential impact, and the relationships between important lifestyle factors and overall well-being in adolescents. Although we observed many meaningful relationships between lifestyle factors and well-being outcomes, the absence of a control group limits our ability to attribute changes in WHO-5 and PSC-17-Y scores to the program itself rather than to other developmental, social, or environmental influences adolescents may be experiencing. This limitation persists despite additional qualitative data, which we are currently analyzing for potential efficacy-related insights suggesting program effectiveness. The lack of congruence between WHO-5 and PSC-17-Y outcomes observed across the various subgroups following the R4F program may also reflect the differential sensitivity of each instrument to mood, behavioral, and attentional domains (51, 53, 63, 66, 68). This could also arise because the PSC-17-Y has not been fully validated, and thus it is unclear if the observed score changes reflect true shifts in symptoms or are within the range of expected measurement variation. This divergence between the two assessments could signal selective program benefits or increased student awareness of psychosocial symptoms, effects which are possibly enhanced by engagement with the R4F program. Such patterns highlight the complexity of adolescent mental health and the necessity of multimodal, longitudinal, and context-sensitive assessment strategies in future research.
To strengthen future research, comparison groups must be included, and longitudinal tracking of individual students is recommended. Future research may also consider incorporating physiological or behavioral measurements such as heart rate monitoring, accelerometry, cardiorespiratory fitness, or sleep assessments to better understand the activity levels and student responses to the program (154–157). These enhancements will provide a more robust evaluation of how cycling programs influence adolescent mental health, allowing us to better understand and optimize their effectiveness in supporting student well-being.
We opted to prioritize a more exploratory approach in this preliminary phase of the study due to its simplicity and interpretability whereas future studies would benefit from statistical sophistication. In this case, single-level analyses were easier to conduct, interpret, and communicate findings for non-technical stakeholders. While preliminary results from our study yield promising information, these results should be interpreted with caution as a result of the study analysis. Our current approach sought to treat participant observations independently, which could potentially underestimate standard errors and produce overly narrow confidence intervals, likely increasing a Type I error rate. Given the hierarchical nature of our data, students nested within schools, future analysis would benefit from a multilevel modeling approach to provide effect estimates of school-level variation in program effectiveness. Further, our use of listwise deletion for missing data may have introduced bias, whereas a multilevel modeling approach can handle missing data through techniques like maximum likelihood estimation.
6 Perspectives
This study underscores the importance of in-school cycling programs and their potential to impact adolescents' mental health. Building on our previous pandemic-era research, our work demonstrates a modest association between participation in the program and overall mental health and well-being among participants in the COVID-emergent R4F program. These findings highlight the potential benefits of in-school cycling initiatives for enhancing the mental health and wellness of middle school students in the United States. Beyond the R4F program, our research highlighted how various factors, including race, gender, socioeconomic status, club involvement, breakfast consumption, PA levels, screen time, and sleep duration, can also play a role in understanding student well-being. These intricate relationships emphasize the need for tailored interventions that address the diverse needs of student populations, as well as further research to better understand and effectively target these multifaceted influences on adolescent mental health. By acknowledging these complexities, we can work towards developing more comprehensive and effective strategies to support the mental well-being of middle school students through cycling programs and other targeted interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by an Institutional Review Board (Advarra), with secondary analysis approved by Loma Linda University IRB. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
SM: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. AP: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. FD: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. BB-S: Data curation, Formal analysis, Writing – review & editing. EB: Writing – review & editing, Data curation, Formal analysis, Methodology. HW: Conceptualization, Methodology, Writing – review & editing. KM: Data curation, Formal analysis, Writing – review & editing. LS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing. SAW: Conceptualization, Methodology, Visualization, Writing – review & editing. CB: Conceptualization, Writing – review & editing. EW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. SMW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded in part by Specialized Bicycle Components, who provides funding and equipment support for the Riding for Focus program and Outride staff and by the Loma Linda University School of Medicine. BBS was an Apprenticeship Bridge To College (ABC) while FD was an Undergraduate Training Program (UTP) Summer Research Fellow supported by P20MD006988 (M. DeLeon) (“LLU Center for Health Disparities Research”) from the National Institute of Health Disparities and Minority Health of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: EW and LS are employed by Outride, which is funded in part by Specialized Bicycle Components. To address and mitigate potential biases arising from the critical involvement of EW and LS in survey design, implementation, and initial data cleaning, several safeguards were incorporated. All study procedures were approved by an independent Institutional Review Board (IRB), including secondary data analysis conducted at Loma Linda University. Data collection was strictly anonymous, with student responses gathered via secure online platforms (Qualtrics) to ensure participant confidentiality and reduce the potential for reporting and observer bias. After initial data cleaning by EW and LS, all subsequent statistical analysis and interpretation were performed independently by research investigators at Loma Linda University, helping preserve objectivity in result reporting. The data cleaning script was also made available to the investigators at Loma Linda University to ensure they were aware of the entire data cleaning process. Furthermore, prior to the rollout of each survey cycle, external academic collaborators, including members of the Loma Linda University research team, were invited to contribute to the development and refinement of survey questions, ensuring diverse perspectives and reducing the influence of program staff on instrument content. These steps, combined with transparent disclosure of authors’ roles and organizational affiliations, offer a robust framework for minimizing bias and enhancing the credibility of the outcomes presented from these studies. Future research will benefit from continuing these collaborative and blinded approaches to reinforce research integrity in program evaluations.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. To check the grammar of the text and to generate consistency in style between sections written by different co-authors. In order to guarantee accuracy, scientific integrity, and adherence to journal policies, all authors examined and approved AI-assisted edits.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
2. Kerekes N, Bador K, Sfendla A, Belaatar M, Mzadi AE, Jovic V, et al. Changes in Adolescents’ psychosocial functioning and well-being as a consequence of long-term COVID-19 restrictions. Int J Environ Res Public Health. (2021) 18:8755. doi: 10.3390/ijerph18168755
3. Cao C, Wang L, Fang R, Liu P, Bi Y, Luo S, et al. Anxiety, depression, and PTSD symptoms among high school students in China in response to the COVID-19 pandemic and lockdown. J Affect Disord. (2022) 296:126–9. doi: 10.1016/j.jad.2021.09.052
4. Marcotullio C, Attanasi M, Porreca A, Di Filippo P, Matricardi S, Venanzi A, et al. Neuropsychological symptoms and quality of life during the COVID-19 pandemic in children: a survey in a pediatric population in the Abruzzo region, Italy. Children. (2024) 11:532. doi: 10.3390/children11050532
5. Reiss F, Cosma A, Bersia M, Erhart M, Dalmasso P, Devine J, et al. Adolescents perception of the COVID-19 pandemic restrictions and associated mental health and well-being: gender, age and socioeconomic differences in 22 countries. Child Adolesc Psychiatry Ment Health. (2024) 18:86. doi: 10.1186/s13034-024-00779-z
6. Shah AD, Laternser C, Tatachar P, Duong P. The COVID-19 pandemic and its effects on mental health-A before, during, and after comparison using the U.S. census bureau’s household pulse survey. Int J Environ Res Public Health. (2024) 21:1306. doi: 10.3390/ijerph21101306
7. Wright N, Hill J, Sharp H, Refberg-Brown M, Crook D, Kehl S, et al. COVID-19 pandemic impact on adolescent mental health: a reassessment accounting for development. Eur Child Adolesc Psychiatry. (2024) 33:2615–27. doi: 10.1007/s00787-023-02337-y
8. Mpofu JJ, Underwood JM, Thornton JE, Brener ND, Rico A, Kilmer G, et al. Overview and methods for the youth risk behavior surveillance system—united States, 2021. MMWR Suppl. (2023) 72:1–12. doi: 10.15585/mmwr.su7201a1
9. Reinert M, Nguyen T. The State Mental Health America 2024. Alexandria, VA: Mental Health America (2024).
10. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2022) 27:281–95. doi: 10.1038/s41380-021-01161-7
11. Newby H, Marsh AD, Moller A-B, Adebayo E, Azzopardi PS, Carvajal L, et al. A scoping review of adolescent health indicators. J Adolesc Health. (2021) 69:365–74. doi: 10.1016/j.jadohealth.2021.04.026
12. Dementyev F, Fish B, Sakyi Opoku NY, Tesfaye L, Chan J, Ortiz L, et al. Middle school cycling program is associated with improved mental health and wellbeing in adolescents during COVID-19. Front Sports Act Living. (2023) 5:1255514. doi: 10.3389/fspor.2023.1255514
13. Fu Q, Li L, Li Q, Wang J. The effects of physical activity on the mental health of typically developing children and adolescents: a systematic review and meta-analysis. BMC Public Health. (2025) 25:1514. doi: 10.1186/s12889-025-22690-8
14. Ruiz-Ranz E, Asín-Izquierdo I. Physical activity, exercise, and mental health of healthy adolescents: a review of the last 5 years. Sports Med Health Sci. (2025) 7:161–72. doi: 10.1016/j.smhs.2024.10.003
15. Song H, Ge S, Wang Y, Ran L, Zhang H. Aerobic exercise strategies for anxiety and depression among children and adolescents: a systematic review and meta-analysis. Front Public Health. (2025) 13:1555029. doi: 10.3389/fpubh.2025.1555029
16. Chen P, Wang D, Shen H, Yu L, Gao Q, Mao L, et al. Physical activity and health in Chinese children and adolescents: expert consensus statement. Br J Sports Med. (2020) 54:1321–31. doi: 10.1136/bjsports-2020-102261
17. Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. (2011) 41:15–28. doi: 10.2190/PM.41.1.c
18. Philippot A, Dubois V, Lambrechts K, Grogna D, Robert A, Jonckheer U, et al. Impact of physical exercise on depression and anxiety in adolescent inpatients: a randomized controlled trial. J Affect Disord. (2022) 301:145–53. doi: 10.1016/j.jad.2022.01.011
19. Mandolesi L, Polverino A, Montuori S, Foti F, Ferraioli G, Sorrentino P, et al. Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits. Front Psychol. (2018) 9:509. doi: 10.3389/fpsyg.2018.00509
20. Wang X, Cai Z-D, Jiang W-T, Fang Y-Y, Sun W-X, Wang X. Systematic review and meta-analysis of the effects of exercise on depression in adolescents. Child Adolesc Psychiatry Ment Health. (2022) 16:16. doi: 10.1186/s13034-022-00453-2
21. Wu J, Zhao X, Shao Y, Zang W, Jun H, Yu W. The impact of physical exercise on internalizing and externalizing problem behaviors among middle school students: correlation and regression prediction analysis. Child Adolesc Psychiatry Ment Health. (2025) 19:45. doi: 10.1186/s13034-025-00903-7
22. Hoevenaar-Blom MP, Wendel-Vos GCW, Spijkerman AMW, Kromhout D, Verschuren WMM. Cycling and sports, but not walking, are associated with 10-year cardiovascular disease incidence: the MORGEN study. Eur J Cardiovasc Prev Rehabil. (2011) 18:41–7. doi: 10.1097/HJR.0b013e32833bfc87
23. Celis-Morales CA, Lyall DM, Welsh P, Anderson J, Steell L, Guo Y, et al. Association between active commuting and incident cardiovascular disease, cancer, and mortality: prospective cohort study. Br Med J. (2017) 357:j1456. doi: 10.1136/bmj.j1456
24. Kubesch NJ, Therming Jørgensen J, Hoffmann B, Loft S, Nieuwenhuijsen MJ, Raaschou-Nielsen O, et al. Effects of leisure-time and transport-related physical activities on the risk of incident and recurrent myocardial infarction and interaction with traffic-related air pollution: a cohort study. J Am Heart Assoc. (2018) 7:e009554. doi: 10.1161/JAHA.118.009554
25. Millett C, Agrawal S, Sullivan R, Vaz M, Kurpad A, Bharathi AV, et al. Associations between active travel to work and overweight, hypertension, and diabetes in India: a cross-sectional study. PLoS Med. (2013) 10:e1001459. doi: 10.1371/journal.pmed.1001459
26. State Education Practices (SEP). (2025). Available online at: https://nces.ed.gov/programs/statereform/index.asp (Accessed August 18, 2024).
27. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
29. Barr-Anderson DJ, Neumark-Sztainer D, Schmitz KH, Ward DS, Conway TL, Pratt C, et al. But I like PE: factors associated with enjoyment of physical education class in middle school girls: factors associated with enjoyment of physical education class in middle school girls. Res Q Exerc Sport. (2008) 79(1):18–27. doi: 10.1080/02701367.2008.10599456
30. Lewallen TC, Hunt H, Potts-Datema W, Zaza S, Giles W. The whole school, whole community, whole child model: a new approach for improving educational attainment and healthy development for students. J Sch Health. (2015) 85:729–39. doi: 10.1111/josh.12310
31. Packham A, Street B. The effects of physical education on student fitness, achievement, and behavior. Econ Educ Rev. (2019) 72:1–18. doi: 10.1016/j.econedurev.2019.04.003
32. Ferguson MC, Bartsch SM, O’Shea KJ, Thomas DM, Moran TH, Solano Gonzales M, et al. The potential epidemiologic, clinical, and economic impact of requiring schools to offer physical education (PE) classes in Mexico City. PLoS One. (2022) 17:e0268118. doi: 10.1371/journal.pone.0268118
33. Rossi L, Behme N, Breuer C. Physical activity of children and adolescents during the COVID-19 pandemic-A scoping review. Int J Environ Res Public Health. (2021) 18:11440. doi: 10.3390/ijerph182111440
34. Barbour N, Mannering F. Intended cycling frequency and the role of happiness and environmental friendliness after COVID-19. Sci Rep. (2023) 13:636. doi: 10.1038/s41598-023-27681-6
35. People for bikes. (2023). Bicycle Participation Study 2022 Survey of U.S. Residents. Available online at: https://24hournation.com/wp-content/uploads/2022-PeopleForBikes-US-Bicycling-Participation-Study.pdf (Accessed September 11, 2025).
36. Younes H, Noland RB, Von Hagen LA, Sinclair J. Cycling during and after COVID: has there been a boom in activity? Transp Res Part F Traffic Psychol Behav. (2023) 99:71–82. doi: 10.1016/j.trf.2023.09.017
37. Pucher J, Buehler R. Safer cycling through improved infrastructure. Am J Public Health. (2016) 106:2089–91. doi: 10.2105/AJPH.2016.303507
39. Ding P, Ding C, Feng S. The health benefits of bicycling to school among adolescents in China: a propensity score matching study. Front Public Health. (2023) 11:1049254. doi: 10.3389/fpubh.2023.1049254
40. Schönbach DMI, Altenburg TM, Marques A, Chinapaw MJM, Demetriou Y. Strategies and effects of school-based interventions to promote active school transportation by bicycle among children and adolescents: a systematic review. Int J Behav Nutr Phys Act. (2020) 17:138. doi: 10.1186/s12966-020-01035-1
41. Aranda-Balboa MJ, Huertas-Delgado FJ, Gálvez-Fernández P, Saucedo-Araujo R, Molina-Soberanes D, Campos-Garzón P, et al. The effect of a school-based intervention on children’s cycling knowledge, mode of commuting and perceived barriers: a randomized controlled trial. Int J Environ Res Public Health. (2022) 19:9626. doi: 10.3390/ijerph19159626
42. van Hoef T, Kerr S, Roth R, Brenni C, Endes K. Effects of a cycling intervention on adolescents cycling skills. J Transp Health. (2022) 25:101345. doi: 10.1016/j.jth.2022.101345
43. Mercê C, Pereira JV, Branco M, Catela D, Cordovil R. Training programmes to learn how to ride a bicycle independently for children and youths: a systematic review. Phys Educ Sport Pedagogy. (2023) 28:530–45. doi: 10.1080/17408989.2021.2005014
44. Mercê C, Davids K, Catela D, Branco M, Correia V, Cordovil R. Learning to cycle: a constraint-led intervention programme using different cycling task constraints. Phys Educ Sport Pedagogy. (2025) 30:78–91. doi: 10.1080/17408989.2023.2185599
45. Clanton T, Chancellor HC, Pinckney HVIV, Balidemaj V, Hadiandehkordi P. Bicycling as a positive youth development mechanism. J Park Recreat Adm. (2022) 40:88–103. doi: 10.18666/JPRA-2021-10589
46. Brown CL, Christian DD, Crowson HM. Effects of an adventure therapy mountain bike program on middle school students’ resiliency. J Child Adolesc Couns. (2023) 9:222–41. doi: 10.1080/23727810.2023.2229084
47. Abramson B, Boerma J, Tsyvinski A. Macroeconomics of Mental Health. Cambridge, MA: National Bureau of Economic Research (2024). doi: 10.3386/w32354
48. Li D, Nyhan K, Zhou X, Zhu Y, Castro D, Vermund SH, et al. School closures and reopenings during the COVID-19 pandemic: a scoping review protocol. BMJ Open. (2022) 12:e054292. doi: 10.1136/bmjopen-2021-054292
49. YRBSS. (2018). Available online at: https://archive.cdc.gov/www_cdc_gov/healthyschools/yrbs_archive/faq.htm (Accessed September 21, 2025).
50. Sample Module Time. (n.d.). Estimated survey completion time on select CalSCHLS survey modules. Available online at: https://calschls.org/docs/completiontime_202425survey_selectmodules.pdf (Accessed September 21, 2025).
51. Bergmann P, Lucke C, Nguyen T, Jellinek M, Murphy JM. Identification and utility of a short form of the pediatric symptom checklist-youth self-report (PSC-17-Y). Eur J Psychol Assess. (2020) 36:56–64. doi: 10.1027/1015-5759/a000486
52. Johansen S. The use of Well-being measures in Primary Health Care—the DepCare Project; in World Health Organization, Regional Office for Europe: Well-Being Measures in Primary Health Care—the DepCare Project. Geneva: World Health Organization (1998) 12.
53. Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. (2015) 84:167–76. doi: 10.1159/000376585
54. Map: Where were schools required to be open for the 2020-21 school year? (2020). Educ Week. Available online at: https://www.edweek.org/ew/section/multimedia/map-covid-19-schools-open-closed.html (Accessed August 18, 2024).
55. Grimes A, Lightner JS, Eighmy K, Steel C, Shook RP, Carlson J. Decreased physical activity among youth resulting from COVID-19 pandemic-related school closures: natural experimental study. JMIR Form Res. (2022) 6:e35854. doi: 10.2196/35854
56. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. (2018) 2:223–8. doi: 10.1016/S2352-4642(18)30022-1
57. Verification toolkit. (2024). Available online at: https://www.fns.usda.gov/cn/verification-toolkit (Accessed August 18, 2024).
58. Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homel Secur Emerg Manag. (2011) 8:3. doi: 10.2202/1547-7355.1792
59. Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the youth risk behavior survey questionnaire. Am J Epidemiol. (1995) 141:575–80. doi: 10.1093/oxfordjournals.aje.a117473
60. Van Roy B, Veenstra M, Clench-Aas J. Construct validity of the five-factor strengths and difficulties questionnaire (SDQ) in pre-, early, and late adolescence. J Child Psychol Psychiatry. (2008) 49:1304–12. doi: 10.1111/j.1469-7610.2008.01942.x
61. Ravens-Sieberer U, Schmidt S, Gosch A, Erhart M, Petersen C, Bullinger M. Measuring subjective health in children and adolescents: results of the European KIDSCREEN/DISABKIDS project. Psychosoc Med. (2007) 4:Doc08. PMID: 19742297; PMCID: PMC2736532.19742297
62. Gardner W, Murphy M, Childs G, Kelleher K, Pagano M, Jellinek M, et al. The PSC-17: a brief pediatric symptom checklist with psychosocial problem subscales. A report from PROS and ASPN. Ambulatory Child Health. (1999) 5:225–36.
63. Murphy JM, Bergmann P, Chiang C, Sturner R, Howard B, Abel MR, et al. The PSC-17: subscale scores, reliability, and factor structure in a new national sample. Pediatrics. (2016) 138:e20160038. doi: 10.1542/peds.2016-0038
64. Cosma A, Költő A, Chzhen Y, Kleszczewska D, Kalman M, Martin G. Measurement invariance of the WHO-5 well-being index: evidence from 15 European countries. Int J Environ Res Public Health. (2022) 19:9798. doi: 10.3390/ijerph19169798
65. Sischka PE, Martin G, Residori C, Hammami N, Page N, Schnohr C, et al. Cross-national validation of the WHO-5 well-being Index within adolescent populations: findings from 43 countries. Assessment. (2025) doi: 10.1177/10731911241309452
66. Allgaier A-K, Pietsch K, Frühe B, Prast E, Sigl-Glöckner J, Schulte-Körne G. Depression in pediatric care: is the WHO-five well-being Index a valid screening instrument for children and adolescents? Gen Hosp Psychiatry. (2012) 34:234–41. doi: 10.1016/j.genhosppsych.2012.01.007
67. Sischka PE, Costa AP, Steffgen G, Schmidt AF. The WHO-5 well-being index–validation based on item response theory and the analysis of measurement invariance across 35 countries. J Affect Disord. (2020) 1:100020. doi: 10.1016/j.jadr.2020.10002
68. Gall G, Pagano ME, Desmond MS, Perrin JM, Murphy JM. Utility of psychosocial screening at a school-based health center. J Sch Health. (2000) 70:292–8. doi: 10.1111/j.1746-1561.2000.tb07254.x
69. Ware JE. The status of health assessment 1994. Annu Rev Public Health. (1995) 16:327–54. doi: 10.1146/annurev.pu.16.050195.001551
70. SHAPE America—Society of Health and Physical Educators. National Standards & Grade-level outcomes for K-12 Physical Education. Champaign, IL: Human Kinetics (2014).
71. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing (2021). Available online at: https://www.R-project.org/
72. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Elsevier Science (2013).
73. Social Science Statistics. (2025). Cohen’s d. Social Science Statistics Effect Size Calculator. Available online at: https://www.socscistatistics.com/effectsize/default3.aspx#google_vignette (Accessed May 4, 2025).
74. Koopman PAR. Confidence intervals for the ratio of two binomial proportions. Biometrics. (1984) 40:513–7. doi: 10.2307/2531405
75. Fossati C, Torre G, Vasta S, Giombini A, Quaranta F, Papalia R, et al. Physical exercise and mental health: the routes of a reciprocal relation. Int J Environ Res Public Health. (2021) 18:12364. doi: 10.3390/ijerph182312364
76. Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. (2010) 10:831–41. doi: 10.1037/a0020138
77. Council on Communications and Media. Media use in school-aged children and adolescents. Pediatrics. (2016) 138:e20162592. doi: 10.1542/peds.2016-2592
78. Adolphus K, Hoyland A, Walton J, Quadt F, Lawton CL, Dye L. Ready-to-eat cereal and milk for breakfast compared with no breakfast has a positive acute effect on cognitive function and subjective state in 11–13-year-olds: a school-based, randomised, controlled, parallel groups trial. Eur J Nutr. (2021) 60:3325–42. doi: 10.1007/s00394-021-02506-2
79. López-Gil JF, Tully MA, Cristi-Montero C, Brazo-Sayavera J, Gaya AR, Calatayud J, et al. Is the frequency of breakfast consumption associated with life satisfaction in children and adolescents? A cross-sectional study with 154,151 participants from 42 countries. Nutr J. (2024) 23:78. doi: 10.1186/s12937-024-00979-5
80. Rawlings JO, Pantula SG, Dickey DA. Applied Regression Analysis: A Research Tool. New York, NY: Springer Science & Business Media (2001).
81. Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiatry. (2022) 79:550–9. doi: 10.1001/jamapsychiatry.2022.0609
82. Campbell OLK, Bann D, Patalay P. The gender gap in adolescent mental health: a cross-national investigation of 566,829 adolescents across 73 countries. SSM Popul Health. (2021) 13:100742. doi: 10.1016/j.ssmph.2021.100742
83. McGuine TA, Biese KM, Petrovska L, Hetzel SJ, Reardon C, Kliethermes S, et al. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19-related school closures and sport cancellations: a study of 13 000 athletes. J Athl Train. (2021) 56:11–9. doi: 10.4085/1062-6050-0478.20
84. Delfin D, Eke R, Gray H, Kerr ZY, Wallace JS. Associations between Major depressive episodes and school- or community-based activity participation among adolescents using nationwide representative data. J Sch Health. (2022) 92:692–701. doi: 10.1111/josh.13172
85. Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, et al. Review: mental health impacts of the COVID-19 pandemic on children and youth—a systematic review. Child Adolesc Ment Health. (2022) 27:173–89. doi: 10.1111/camh.12501
86. Yoon Y, Eisenstadt M, Lereya ST, Deighton J. Gender difference in the change of adolescents’ mental health and subjective wellbeing trajectories. Eur Child Adolesc Psychiatry. (2023) 32:1569–78. doi: 10.1007/s00787-022-01961-4
87. Lu W. Child and adolescent mental disorders and health care disparities: results from the national survey of Children’s health, 2011–2012. hpu. (2017) 28:988–1011. doi: 10.1353/hpu.2017.0092
88. Centers for Disease Control and Prevention. Youth Risk Behavior Survey Data Summary & Trends Report: 2013–2023. Washington, DC: U.S. Department of Health and Human Services (2024). Available online at: https://www.cdc.gov/yrbs/dstr/pdf/YRBS-2023-Data-Summary-Trend-Report.pdf (Accessed April 23, 2025).
89. Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. (2020) 370:eaay0214. doi: 10.1126/science.aay0214
90. Elsayed NM, Luby JL, Barch DM. Contributions of socioeconomic status and cognition to emotion processes and internalizing psychopathology in childhood and adolescence: a systematic review. Neurosci Biobehav Rev. (2023) 152:105303. doi: 10.1016/j.neubiorev.2023.105303
91. Erratum for the Review “Poverty, depression, and anxiety: Causal evidence and mechanisms” by M. Ridley et al. Science. (2024) 383:eadp1916. doi: 10.1126/science.adp1916
92. Opstoel K, Chapelle L, Prins FJ, De Meester A, Haerens L, van Tartwijk J, et al. Personal and social development in physical education and sports: a review study. Eur Phys Educ Rev. (2020) 26:797–813. doi: 10.1177/1356336X19882054
93. Lyerly JE. The Relationship Between Breakfast Skipping and Physical Activity Among Adolescents Aged 12–19. Charlotte, NC: University of North Carolina at Charlotte (2012).
94. Sawa S, Hashizume K, Abe T, Kusaka Y, Fukazawa Y, Hiraku Y, et al. Pathway linking physical activity, sleep duration, and breakfast consumption with the physical/psychosocial health of schoolchildren. J Child Health Care. (2021) 25:5–17. doi: 10.1177/1367493519891019
95. Chekroud SR, Gueorguieva R, Zheutlin AB, Paulus M, Krumholz HM, Krystal JH, et al. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. (2018) 5:739–46. doi: 10.1016/S2215-0366(18)30227-X
96. Pascoe M, Bailey AP, Craike M, Carter T, Patten R, Stepto N, et al. Physical activity and exercise in youth mental health promotion: a scoping review. BMJ Open Sport Exerc Med. (2020) 6:e000677. doi: 10.1136/bmjsem-2019-000677
97. Puccinelli PJ, da Costa TS, Seffrin A, de Lira CAB, Vancini RL, Nikolaidis PT, et al. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health. (2021) 21:425. doi: 10.1186/s12889-021-10470-z
98. Priftis N, Panagiotakos D. Screen time and its health consequences in children and adolescents. Children. (2023) 10:1665. doi: 10.3390/children10101665
99. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1:40–3. doi: 10.1016/j.sleh.2014.12.010
100. Marciano L, Camerini AL. Recommendations on screen time, sleep and physical activity: associations with academic achievement in Swiss adolescents. Public Health. (2021) 198:211–7. doi: 10.1016/j.puhe.2021.07.027
101. Anderson N, Ozakinci G. Effectiveness of psychological interventions to improve quality of life in people with long-term conditions: rapid systematic review of randomised controlled trials. BMC Psychol. (2018) 6:11. doi: 10.1186/s40359-018-0225-4
102. Gan DZQ, McGillivray L, Han J, Christensen H, Torok M. Effect of engagement with digital interventions on mental health outcomes: a systematic review and meta-analysis. Front Digit Health. (2021) 3:764079. doi: 10.3389/fdgth.2021.764079
103. Eather N, Wade L, Pankowiak A, Eime R. The impact of sports participation on mental health and social outcomes in adults: a systematic review and the “Mental Health through Sport” conceptual model. Syst Rev. (2023) 12:102. doi: 10.1186/s13643-023-02264-8
104. Kim YS, Park YS, Allegrante JP, Marks R, Ok H, Ok Cho K, et al. Relationship between physical activity and general mental health. Prev Med. (2012) 55:458–63. doi: 10.1016/j.ypmed.2012.08.021
105. Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. (2017) 4:8–9. doi: 10.1016/S2215-0366(16)30348-0
106. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
107. Yu S. Uncovering the hidden impacts of inequality on mental health: a global study. Transl Psychiatry. (2018) 8:98. doi: 10.1038/s41398-018-0148-0
108. Walton CC, Rice S, Gao CX, Butterworth M, Clements M, Purcell R. Gender differences in mental health symptoms and risk factors in Australian elite athletes. BMJ Open Sport Exerc Med. (2021) 7:e000984. doi: 10.1136/bmjsem-2020-000984
109. Farhane-Medina NZ, Luque B, Tabernero C, Castillo-Mayén R. Factors associated with gender and sex differences in anxiety prevalence and comorbidity: a systematic review. Sci Prog. (2022) 105:368504221135469. doi: 10.1177/00368504221135469
110. Kretschmer L, Salali GD, Andersen LB, Hallal PC, Northstone K, Sardinha LB, et al. Gender differences in the distribution of children’s physical activity: evidence from nine countries. Int J Behav Nutr Phys Act. (2023) 20:103. doi: 10.1186/s12966-023-01496-0
111. Jerstad SJ, Boutelle KN, Ness KK, Stice E. Prospective reciprocal relations between physical activity and depression in female adolescents. J Consult Clin Psychol. (2010) 78:268–72. doi: 10.1037/a0018793
112. Omorou AY, Langlois J, Lecomte E, Briançon S, Vuillemin A. Cumulative and bidirectional association of physical activity and sedentary behaviour with health-related quality of life in adolescents. Qual Life Res. (2016) 25:1169–78. doi: 10.1007/s11136-015-1172-7
113. Kopp PM, Möhler E, Gröpel P. Physical activity and mental health in school-aged children: a prospective two-wave study during the easing of the COVID-19 restrictions. Child Adolesc Psychiatry Ment Health. (2024) 18:4. doi: 10.1186/s13034-023-00695-8
114. Fan Q, DuPont-Reyes MJ, Hossain MM, Chen L-S, Lueck J, Ma P. Racial and ethnic differences in major depressive episode, severe role impairment, and mental health service utilization in U.S. adolescents. J Affect Disord. (2022) 306:190–9. doi: 10.1016/j.jad.2022.03.015
115. Hoffmann JA, Alegría M, Alvarez K, Anosike A, Shah PP, Simon KM, et al. Disparities in pediatric mental and behavioral health conditions. Pediatrics. (2022) 150:e2022058227. doi: 10.1542/peds.2022-058227
116. Martin R, Banaag A, Riggs DS, Koehlmoos TP. Minority adolescent mental health diagnosis differences in a national sample. Mil Med. (2022) 187:e969–77. doi: 10.1093/milmed/usab326
117. Eboigbe LI, Simon CB, Wang YS, Tyrell FA. The compounded effect of the dual pandemic on ethnic-racial minority adolescents’ mental health and psychosocial well-being. Curr Opin Psychol. (2023) 52:101626. doi: 10.1016/j.copsyc.2023.101626
118. McLaughlin KA, Hilt LM, Nolen-Hoeksema S. Racial/ethnic differences in internalizing and externalizing symptoms in adolescents. J Abnorm Child Psychol. (2007) 35:801–16. doi: 10.1007/s10802-007-9128-1
119. Hanlon TE, Simon BD, O’Grady KE, Carswell SB, Callaman JM. The effectiveness of an after-school program targeting urban African American youth. Educ Urban Soc. (2009) 42:96–118. doi: 10.1177/0013124509343144
120. Raposa EB, Rhodes J, Stams GJJM, Card N, Burton S, Schwartz S, et al. The effects of youth mentoring programs: a meta-analysis of outcome studies. J Youth Adolesc. (2019) 48:423–43. doi: 10.1007/s10964-019-00982-8
121. Blewitt C, O’Connor A, Morris H, Mousa A, Bergmeier H, Nolan A, et al. Do curriculum-based social and emotional learning programs in early childhood education and care strengthen teacher outcomes? A systematic literature review. Int J Environ Res Public Health. (2020) 17:1049. doi: 10.3390/ijerph17031049
122. Conger RD, Conger KJ, Martin MJ. Socioeconomic status, family processes, and individual development. J Marriage Fam. (2010) 72:685–704. doi: 10.1111/j.1741-3737.2010.00725.x
123. Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. (2016) 16:115. doi: 10.1186/s12889-016-2720-y
124. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
125. Blackwell CK, Wu G, Chandran A, Arizaga J, Bosquet Enlow M, Brennan PA, et al. Longitudinal changes in youth mental health from before to during the COVID-19 pandemic. JAMA Netw Open. (2024) 7:e2430198. doi: 10.1001/jamanetworkopen.2024.30198
126. Abu-Omar K, Rütten A, Burlacu I, Schätzlein V, Messing S, Suhrcke M. The cost-effectiveness of physical activity interventions: a systematic review of reviews. Prev Med Rep. (2017) 8:72–8. doi: 10.1016/j.pmedr.2017.08.006
127. Bann D, Scholes S, Fluharty M, Shure N. Adolescents’ physical activity: cross-national comparisons of levels, distributions and disparities across 52 countries. Int J Behav Nutr Phys Act. (2019) 16:141. doi: 10.1186/s12966-019-0897-z
128. Lee S, Lee C, Xu M, Li W, Ory M. People living in disadvantaged areas faced greater challenges in staying active and using recreational facilities during the COVID-19 pandemic. Health Place. (2022) 75:102805. doi: 10.1016/j.healthplace.2022.102805
129. Santos L, Ramos Miguel R, do Rosário Pinheiro M, Rijo D. Fostering emotional and mental health in residential youth care facilities: a systematic review of programs targeted to care workers. Child Youth Serv Rev. (2023) 147:106839. doi: 10.1016/j.childyouth.2023.106839
130. Shidhaye R. Global priorities for improving access to mental health services for adolescents in the post-pandemic world. Curr Opin Psychol. (2023) 53:101661. doi: 10.1016/j.copsyc.2023.101661
131. Cohen A. Stuck between a rock and a hard place: an investigation into a youth-serving community-based organization, philanthropy, and urban public schools. Child Sch. (2024) 46:183–93. doi: 10.1093/cs/cdae012
132. Mahoney JL, Vest AE. The over-scheduling hypothesis revisited: intensity of organized activity participation during adolescence and young adult outcomes. J Res Adolesc. (2012) 22:409–18. doi: 10.1111/j.1532-7795.2012.00808.x
133. Oberle E, Ji XR, Guhn M, Schonert-Reichl KA, Gadermann AM. Benefits of extracurricular participation in early adolescence: associations with peer belonging and mental health. J Youth Adolesc. (2019) 48:2255–70. doi: 10.1007/s10964-019-01110-2
134. Oberle E, Ji XR, Magee C, Guhn M, Schonert-Reichl KA, Gadermann AM. Extracurricular activity profiles and wellbeing in middle childhood: a population-level study. PLoS One. (2019) 14:e0218488. doi: 10.1371/journal.pone.0218488
135. Knifsend CA, Juvonen J. Type and breadth of high school extracurricular activity involvement and postsecondary psychosocial well-being among diverse youth. J Youth Adolesc. (2023) 52:319–30. doi: 10.1007/s10964-022-01695-1
136. Eccles JS, Barber BL. Student council, volunteering, basketball, or marching band. J Adolesc Res. (1999) 14:10–43. doi: 10.1177/0743558499141003
137. Eime R, Harvey J, Thompson H, Feely P. Sport and recreation spatial: development of a national geographical information system for the sport and recreation sector. J Sci Med Sport. (2013) 16:e10–1. doi: 10.1016/j.jsams.2013.10.026
138. Fredricks JA, Eccles JS. Extracurricular involvement and adolescent adjustment: impact of duration, number of activities, and breadth of participation. Appl Dev Sci. (2006) 10:132–46. doi: 10.1207/s1532480xads1003_3
139. O’Sullivan TA, Robinson M, Kendall GE, Miller M, Jacoby P, Silburn SR, et al. A good-quality breakfast is associated with better mental health in adolescence. Public Health Nutr. (2009) 12:249–58. doi: 10.1017/S1368980008003935
140. Zahedi H, Djalalinia S, Sadeghi O, Zare Garizi F, Asayesh H, Payab M, et al. Breakfast consumption and mental health: a systematic review and meta-analysis of observational studies. Nutr Neurosci. (2022) 25:1250–64. doi: 10.1080/1028415X.2020.1853411
141. Liu L, Guo C, Lang F, Yan Y. Association of breakfast, total diet quality, and mental health in adolescents: a cross-sectional study of HBSC in Greece. Eur J Pediatr. (2023) 182:5385–97. doi: 10.1007/s00431-023-05180-0
142. Chaput J-P, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. (2016) 41:S266–82. doi: 10.1139/apnm-2015-0627
143. Zang Y. Impact of physical exercise on children with attention deficit hyperactivity disorders: evidence through a meta-analysis. Medicine. (2019) 98:e17980. doi: 10.1097/MD.0000000000017980
144. Xie Y, Gao X, Song Y, Zhu X, Chen M, Yang L, et al. Effectiveness of physical activity intervention on ADHD symptoms: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:706625. doi: 10.3389/fpsyt.2021.706625
145. Hrafnkelsdottir SM, Brychta RJ, Rognvaldsdottir V, Gestsdottir S, Chen KY, Johannsson E, et al. Less screen time and more frequent vigorous physical activity is associated with lower risk of reporting negative mental health symptoms among Icelandic adolescents. PLoS One. (2018) 13:e0196286. doi: 10.1371/journal.pone.0196286
146. Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. (2019) 9:e023191. doi: 10.1136/bmjopen-2018-023191
147. Descarpentry A, Melchior M, Galera C, Hazo J-B, Falissard B, Warszawski J, et al. High screen time and internalizing and externalizing behaviours among children aged 3 to 14 years during the COVID-19 pandemic in France. Eur Child Adolesc Psychiatry. (2024) 33:1151–61. doi: 10.1007/s00787-023-02241-5
148. Sârbu EA, Iovu M-B, Lazăr F, Ghețău C. Screen time exposure and the development of internalizing and externalizing problems in a sample of Romanian urban highschoolers. Brain. (2024) 15:59–73. doi: 10.18662/brain/15.1/536
149. Nagata JM, Cortez CA, Dooley EE, Iyer P, Ganson KT, Bibbins-Domingo K, et al. 10. Screen time and moderate-to-vigorous intensity physical activity among adolescents during the COVID-19 pandemic: findings from the adolescent brain cognitive development study. J Adolesc Health. (2022) 70:S6. doi: 10.1016/j.jadohealth.2022.01.014
150. Nagata JM, Cortez CA, Cattle CJ, Ganson KT, Iyer P, Bibbins-Domingo K, et al. Screen time use among US adolescents during the COVID-19 pandemic: findings from the adolescent brain cognitive development (ABCD) study. JAMA Pediatr. (2022) 176:94–6. doi: 10.1001/jamapediatrics.2021.4334
151. Nagata JM, Al-Shoaibi AAA, Leong AW, Zamora G, Testa A, Ganson KT, et al. Screen time and mental health: a prospective analysis of the adolescent brain cognitive development (ABCD) study. BMC Public Health. (2024) 24:2686. doi: 10.1186/s12889-024-20102-x
152. Dimakos J, Gauthier-Gagné G, Lin L, Scholes S, Gruber R. The associations between sleep and externalizing and internalizing problems in children and adolescents with attention-deficit/hyperactivity disorder: empirical findings, clinical implications, and future research directions. Child Adolesc Psychiatr Clin N Am. (2021) 30:175–93. doi: 10.1016/j.chc.2020.08.001
153. Qiu J, Morales-Muñoz I. Associations between sleep and mental health in adolescents: results from the UK Millennium cohort study. Int J Environ Res Public Health. (2022) 19:1868. doi: 10.3390/ijerph19031868
154. Dyrstad SM, Hansen BH, Holme IM, Anderssen SA. Comparison of self-reported versus accelerometer-measured physical activity. Med Sci Sports Exerc. (2014) 46:99–106. doi: 10.1249/MSS.0b013e3182a0595f
155. di Fronso S, Tamburro G, Robazza C, Bortoli L, Comani S, Bertollo M. Focusing attention on muscle exertion increases EEG coherence in an endurance cycling task. Front Psychol. (2018) 9:1249. doi: 10.3389/fpsyg.2018.01249
156. Thompson MA, Toner J, Perry JL, Burke R, Nicholls AR. Stress appraisals influence athletic performance and psychophysiological response during 16.1 km cycling time trials. Psychol Sport Exerc. (2020) 49:101682. doi: 10.1016/j.psychsport.2020.101682
Keywords: WHO-5, PSC-17-Y, adolescent mental health and well-being, school-based physical activity programmes, cycling intervention, post-pandemic well-being, modifiable lifestyle factors
Citation: Murillo S, Philipsheck A, Dementyev F, Bello-Sotto B, Bhatt E, Wilson H, Madison K, Schuck L, Wiafe SA, Brown CL, Walker EJ and Wilson SM (2025) Psychosocial well-being in middle schoolers: effects of a school cycling program in the wake of COVID-19. Front. Sports Act. Living 7:1646805. doi: 10.3389/fspor.2025.1646805
Received: 14 June 2025; Accepted: 14 October 2025;
Published: 7 November 2025.
Edited by:
Pedro Forte, Higher Institute of Educational Sciences of the Douro, PortugalReviewed by:
Soukaina Hattabi, University of Jendouba, TunisiaTiago Ferrão Venâncio, Polytechnic Institute of Portalegre, Portugal
Philipp Kopp, Technical University of Munich, Germany
Copyright: © 2025 Murillo, Philipsheck, Dementyev, Bello-Sotto, Bhatt, Wilson, Madison, Schuck, Wiafe, Brown, Walker and Wilson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sean M. Wilson, c2VhbndpbHNvbkBsbHUuZWR1
 Starla Murillo
Starla Murillo Ashtyn Philipsheck
Ashtyn Philipsheck Fletcher Dementyev
Fletcher Dementyev Benjamin Bello-Sotto
Benjamin Bello-Sotto Eshan Bhatt
Eshan Bhatt Hunter Wilson2
Hunter Wilson2 Lauren Schuck
Lauren Schuck Cian L. Brown
Cian L. Brown Esther J. Walker
Esther J. Walker Sean M. Wilson
Sean M. Wilson