- 1Department of Population Health, NYU Grossman School of Medicine, New York, NY, United States
- 2Institute for Excellence in Health Equity, NYU Grossman School of Medicine, New York, NY, United States
- 3Harlem Congregations for Community Improvement, New York, NY, United States
- 4Henry Street Settlement, New York, NY, United States
- 5Department of Public Health Policy and Management, NYU School of Global Public Health, New York, NY, United States
Background: As part of an initiative to increase COVID-19 testing uptake among underserved populations, we conducted focus groups to explore experiences and attitudes related to testing in two understudied groups—young adults and socially-isolated older adults—recruited from residents living in New York City Housing Authority (NYCHA) public housing developments.
Materials and methods: In June through November 2022, we conducted eight virtual focus groups with 21 young adults and 11 older adults living in NYCHA (n = 32 total). To identify themes, we conducted a rapid qualitative analysis approach.
Results: Residents discussed four overarching themes: (1) trusted COVID-19 information sources; (2) reasons for testing; (3) barriers to testing, and (4) strategies to increase testing uptake. Findings were similar across the two age groups; both cited multiple sources of information, including major media outlets, government or public health officials, and doctors. Young adults were more likely to access information from social media despite concerns about misinformation. Participants identified several barriers to testing, such as long lines, insurance coverage, and cost. Young adults reported that at-home COVID testing was more convenient, while older adults expressed concern about accuracy and administering the tests themselves. Recommendations for improving testing emphasized easier access via a central well-known location, in-home visits, free or low-cost tests, and increased outreach.
Conclusion: Mainstream media, doctors and public agencies remain the most trusted sources of information among younger and older residents alike. Many resident recommendations involved leveraging NYCHA infrastructure, highlighting the continuing role public housing authorities can play in COVID-19 and other health initiatives.
1 Introduction
To mitigate the effects of COVID-19, diagnostic testing is an essential tool to rapidly identify cases, isolate and treat infected individuals when indicated, and quarantine those who may have been exposed (1, 2). For diagnostic testing to be effective, tests must be widely available, easy to access, and trusted (3). Moreover, testing and access to other public health resources should be prioritized for communities facing increased vulnerability to the effects of the pandemic.
Within the United States, Black and Latinx populations have been disproportionately impacted by COVID-19 infections, illness, and death—in part, due to fewer resources to help prevent the spread of the virus (4–7). Additional upstream drivers of these disparities include lower household incomes, higher propensity for working in essential services, as well as residing in high-poverty neighborhoods and overcrowded housing (8–11).
As part of the National Institutes of Health’s Rapid Acceleration of Diagnostics – Underserved Populations (RADx-UP) initiative, NYU’s Grossman School of Medicine and Global School of Public Health, in partnership with community-based organizations (CBOs), received funding to study strategies to improve COVID-19 testing among residents of public housing. New York City Public Housing Authority (NYCHA) is the largest public housing authority in the nation. Home to approximately 400,000 people, or roughly 5% of the city’s population, residents of NYCHA have an average household income of just under $25,000 and approximately 90% identify as Black or Latinx (12–14). With respect to transmission risk, residents are disproportionately employed in essential service sectors that were associated with higher COVID incidence and mortality rates, including healthcare, retail and food services, transportation, warehousing, and manufacturing (15–17). In addition, NYCHA developments have a population density that far surpasses that of the city as a whole (18–20).
Nested within NYCHA communities are two subgroups with distinct risk profiles: young adults and older adults. Young adults, though at a lower risk for COVID-19 morbidity and mortality, consistently experience the highest rates of transmission, and are disproportionately responsible for COVID resurgences and hotspots, making them a key group to target for preventative efforts (7, 21). Older adults, in contrast, are far more susceptible to the effects of COVID-19. The risks are compounded for older residents of NYCHA, who have poorer self-reported health as well as higher rates of chronic conditions and limitations on activities of daily living when compared to older residents living in New York City (NYC) (22). Moreover, the proportion of older adults who live alone is far higher in NYCHA, making this a particularly hard-to-reach group for health promotion and disease prevention services (22).
This paper presents findings from focus groups conducted in 2022, after the introduction of at-home testing. We focused on young adults (ages 16 to 29 years) and older adults (ages 60 years and older) because previous research has not focused on comparing these two groups’ knowledge and attitudes about COVID-19 testing options, potential barriers and facilitators to getting tested, reasons for testing oneself, and sources of information about testing. Though both groups are disproportionately impacted by COVID-19, they are distinct populations with distinct experiences, beliefs and needs. By highlighting where the two populations overlap versus where they may require separate, targeted interventions, these findings can be used to guide policies and programs that optimize reach across risk groups.
2 Materials and methods
2.1 Study setting and recruitment
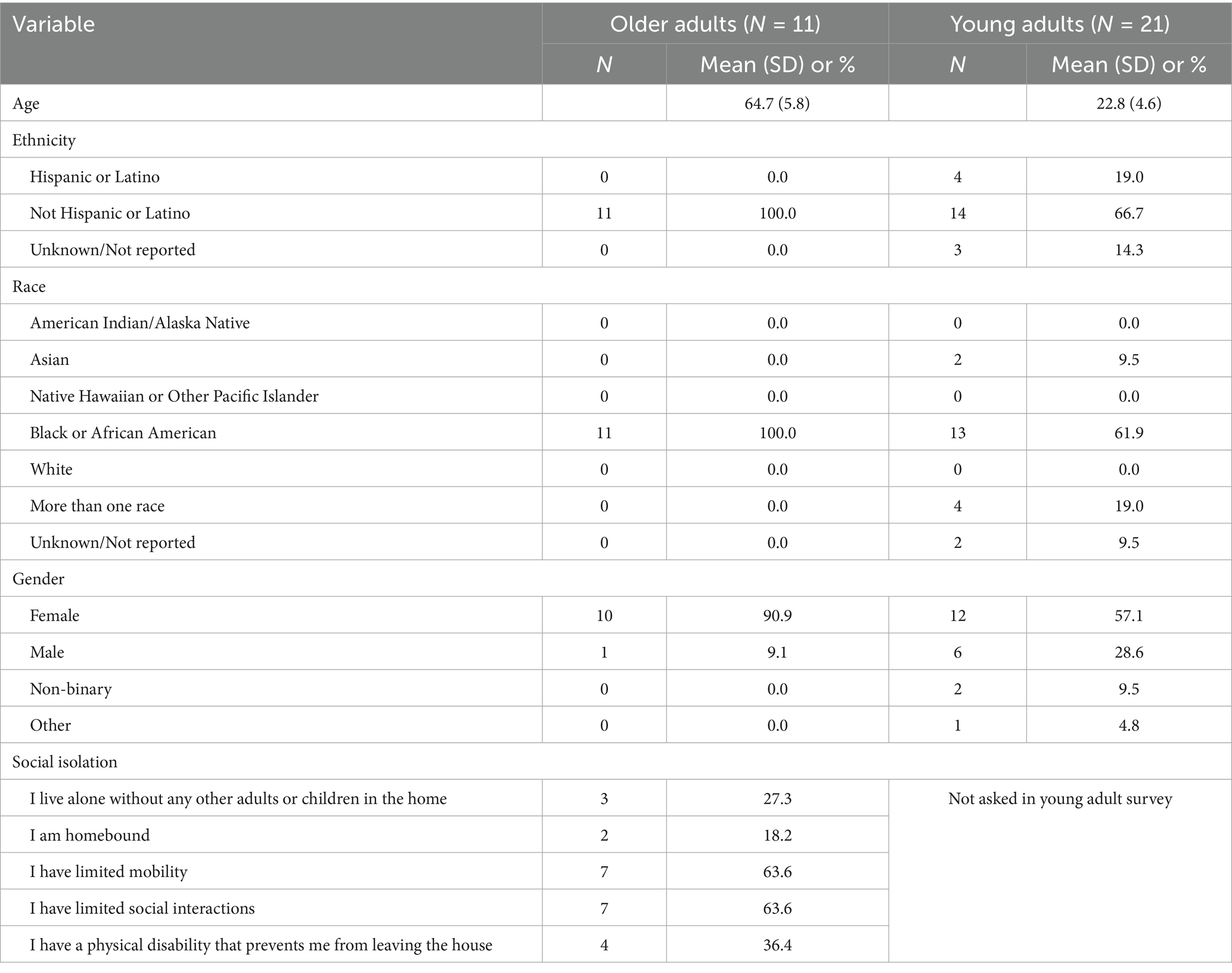
From June through November 2022, we conducted eight virtual focus groups (via HIPAA Zoom) with 32 individuals. All focus groups were conducted in English. We focused recruitment efforts on NYCHA developments across three neighborhoods (Central Harlem, Lower East Side and East New York) in NYC, each chosen for their high public housing density and persistently high levels of COVID-19 infections. Individuals were eligible for study participation if they were residents of NYCHA who were either young adults (those 16–29 years old), or socially isolated older adults (those 60 years and older who met one or more of our pre-determined social isolation criteria, as seen in Table 1). Participants were referred to the study through community partners, who recruited individuals using flyers, social media, and one-on-one conversations with people who might have more limited access to virtual forms of communication. Community partners also conducted home visits to reach residents with limited mobility. Additional information on this academic-community partnership can be found in a previous publication (23). Once an individual was referred to the study team, they were screened, consented, and given the necessary information to join the focus group. Each focus group lasted approximately 1 h, and participants were compensated $30 for their time. The study protocol was approved by the Institutional Review Board of NYU Grossman School of Medicine (i20-01636).
2.2 Semi-structured interview guides
The interview guide was informed by the Integrated Behavioral Model (IBM), which integrates two earlier social science theories—the Theory of Planned Behavior and the Theory of Reasoned Action (24). Following this framework, interview questions assessed residents’ general experience of the pandemic, their knowledge of and overall attitudes toward COVID-19 testing, who they trusted for COVID related information (normative referents), as well as barriers to testing and suggestions as to how the process can be improved (personal agency) (24). We also explored residents’ attitudes toward municipal agencies (e.g., NYCHA; NYC Department of Health and Hygiene) with the rationale being twofold. First, municipal agencies played a significant role in developing and maintaining the infrastructure for COVID-19 testing. Second, based on our earlier work, it may be difficult for agencies to establish and maintain trust among community members they serve (25).
2.3 Data analysis
Study team members reviewed responses after each focus group to preliminarily discuss findings and assess if new data were emerging. In total, five focus groups were conducted with young adults, and three with older adults, at which point no novel responses were generated and thematic saturation was declared. Once data collection was complete, we analyzed focus group data using rapid qualitative analysis methods (26, 27). Five study team members (1) developing a mix of deductive and inductive codes, (2) independently coding all transcripts after they were de-identified, and (3) comparing emerging themes, including some not detailed previously in the interview guide. After successive iterations, two members merged codes and generated themes about residents’ experiences with testing and other preventative behaviors. Where conflicts arose, coders reviewed transcripts together until consensus was achieved. We then used this template to create a matrix of themes, subthemes, and illustrative quotes.
3 Results
3.1 Participant characteristics
Participant characteristics are summarized in Table 1. Thirty-two adults participated across 8 focus groups. The mean age for a participant in the young adult age group was 22.8 years (SD = 4.6). Within this group of 21 adults, 62% identified as Black or African American, 19% identified as Hispanic or Latino, 10% identified as Asian, and 19% identified as more than one race. More than half (57%) of participants were female. The older adult age group was comprised of 11 participants, all of whom identified as Black or African American. The mean age of this group was 64.7 years (SD = 5.8), and almost all (91%) participants were female.
3.2 Overarching themes
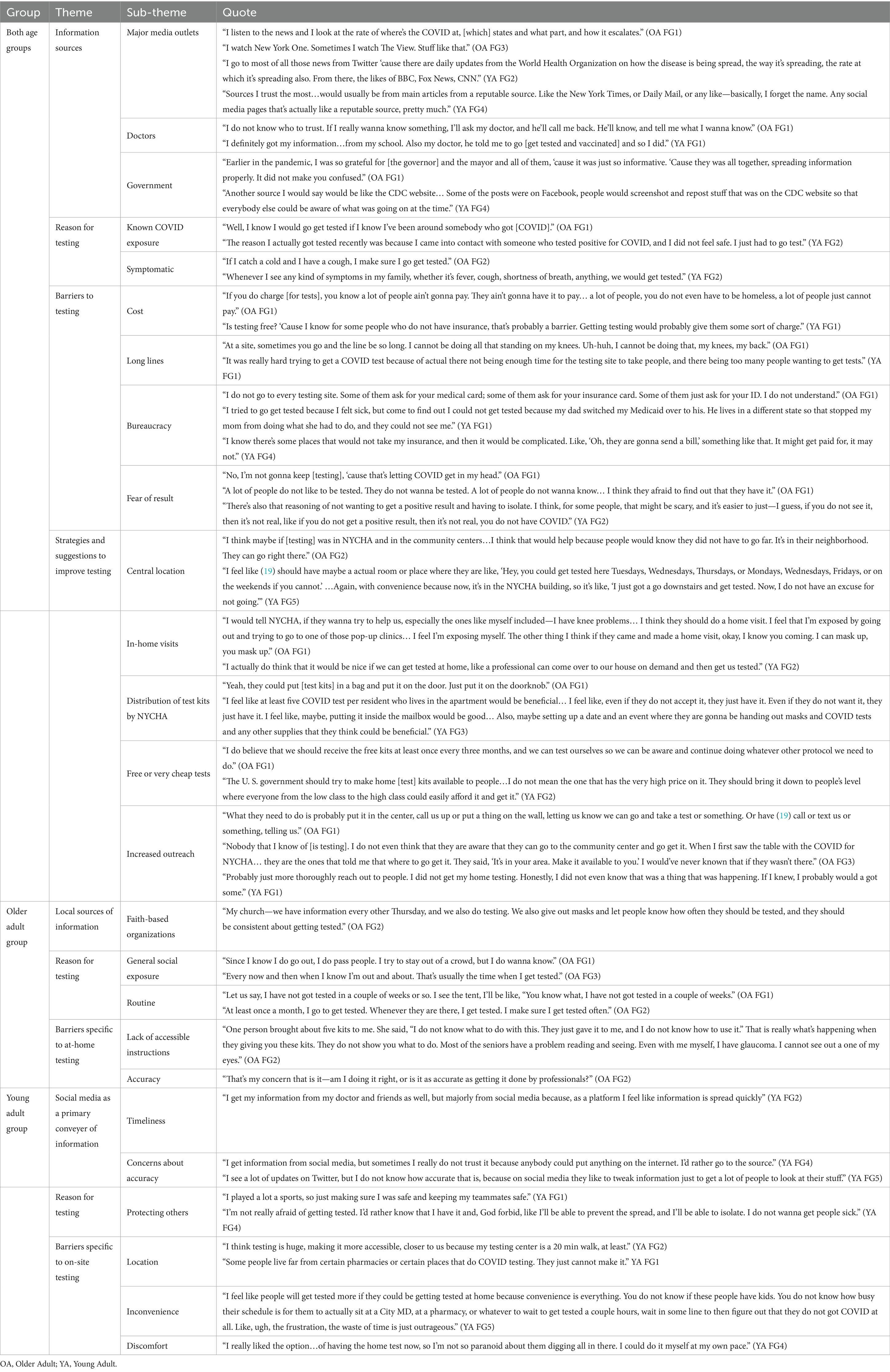
Residents discussed four primary themes: (1) trusted COVID-19 information sources; (2) reasons for testing; (3) barriers to testing, and (4) strategies to increase testing uptake. To facilitate comparisons between the two study populations we organized results to highlight areas in which older adults and younger adults reported similar responses and ways in which they differed. Illustrative quotes can be found in Table 2.
3.2.1 Sources of information
Participants from both age groups cited major media outlets, doctors, and government agencies as trusted information sources. Regarding the differences in themes between the two groups, younger adults mainly accessed this information using social media, including Twitter, Facebook, and TikTok, though they noted a risk of misinformation on these sites and made efforts to identify the original source to verify the information. In contrast, older adults reported receiving information mainly from television news, and described local government sources (e.g., governor and mayor) as important. Only the older adults cited faith-based organizations as a source of information and materials related to COVID-19. Both groups included doctors as an important source of information and guidance. Participants mentioned major media outlets as useful for monitoring the spread and general risk level of COVID-19, though none mentioned using these outlets as a resource for receiving the most up-to-date recommended public health practices. Of note, some participants referenced government as also being a source of confusion, stating that communication was better in the earlier stages of the pandemic, because information was “coming from one office at one time” (OA FG1). Moreover, some participants cited the government as propagating the norm that COVID-19 precautions were no longer necessary (YA FG5).
3.2.2 Reasons for testing
Having a recent confirmed COVID-19 exposure and experiencing COVID-19 symptoms were the two main reasons both groups cited as to why they would decide to get tested or have been tested previously. However, only older adults indicated that they intended to test because of general exposure to others, regardless of (known or unknown) COVID-19 status of the people they interacted with. Young adults frequently cited the safety of others as motivation for testing themselves (YA FG2). Additionally, some participants in the older adult group indicated they were testing themselves routinely, often within a defined window of time they deemed appropriate, which could range from 2 weeks to 4 months (OA FG2-3).
3.2.3 Barriers to testing
Participants across focus groups cited cost, bureaucracy (e.g., being unsure of insurance requirements or coverage), long lines, and fear of a positive test result as barriers to COVID-19 testing. Most participants indicated that requiring any payment for tests would significantly decrease the likelihood that they would get tested (YA FG4). Participants also described multiple reasons why long lines and wait times were barriers, including mobility issues (e.g., pain or difficulty with standing), having to take time off from work, fear of exposure while waiting in line, logistical difficulties for those with children, and general negative feelings that arise from long wait times, including anxiety. Both groups indicated that fear of a positive test was also a barrier. Many people preferred not to know their COVID-19 status (in some cases even when individuals were symptomatic) because receiving a positive result meant lost wages, the need to notify others, possible medical care, and the potential mental and emotional toll of having to isolate from others. As for the older adult group, some expressed the opinion that at-home testing presented more barriers than on-site testing. Among these concerns were a lack of confidence in their ability to self-administer a COVID-19 test and a lack of confidence in the accuracy of the result (OA FG1). Conversely, considering the barriers they cited regarding on-site testing, the young adult groups expressed a preference for at-home testing. A specific concern with on-site testing in this age group was inconvenience, citing the time spent traveling and waiting in line as barriers, as well as the pain and discomfort that can come from having another person swab your nasal cavity. To them, at-home testing allowed for autonomy over both issues.
3.2.4 Suggestions and strategies to increase testing uptake
Despite age differences and some divergence in testing motivation and preferences, there was considerable consensus on strategies and suggestions to improve testing. Both groups suggested opening test sites in central locations to minimize inconvenience. Location suggestions included NYCHA-affiliated management offices and community centers, as well as high-traffic non-NYCHA areas outside of major business or grocery stores. Participants expressed support for maintaining or restoring the placement of pop-up and mobile testing sites. Older adults proposed in-home testing administered by a professional, as a solution to address both mobility issues experienced by older adults and their concerns about self-administering the tests. Participants in the young adult focus groups were also supportive of this idea, though they expressed some concerns about feasibility, given the volume of individuals needing tests and risk of infection for any health officials entering the residents’ homes. Additionally, residents suggested that NYCHA offer test kits at no-cost, either by delivery or pick-up within the building. Universally, participants believed that providing free or affordable test kits was the role of governmental or municipal agencies. Finally, participants proposed greater outreach as a strategy to increase testing. Often participants noted that they or others would be willing to test but aren’t aware of their options. Flyers placed in common areas and under apartment doors, text messages, phone calls, social media and in-person events held at NYCHA community centers were some ideas for expanding reach.
4 Discussion
To our knowledge, this is the first study to identify barriers specific to at-home testing for older adults, and to draw comparisons between the attitudes of older adults and younger adults toward COVID-19 testing. We found that mainstream media, doctors and government agencies remain the most trusted sources of information among younger and older residents alike. Residents offered viable strategies to improve testing, including suggestions to leverage the infrastructure of public housing for testing services, and for public housing authorities to continue distributing tests to all residents.
Among the young adults and older adults who participated in age-specific focus groups, multiple themes emerged that spanned both groups. Both groups reported several trusted sources of information, including major media outlets, doctors, and public health officials or government employees. While this is consistent with previous literature (28–32), it is notable these remained the named trusted sources well into the pandemic, despite widespread concerns about erosion of trust in public health authorities and the medical establishment, and of the proliferation of fake news (28, 30, 33–35). One of the main differences between the groups was that young adults were more likely to access information from social media, despite being aware that these sources may contain misinformation, a concern noted in prior COVID-19 studies (25, 30, 32). Conversely, older adults preferred people with whom they can actually discuss their health, as opposed to the Internet (36). This included healthcare providers, friends and family, and community or faith-based organizations.
Both groups cited a COVID-19 exposure or exhibiting symptoms as the main reason for getting tested. Separately, older adults emphasized awareness of their own vulnerability to the virus in high-risk settings (e.g., social events) as a reason for testing. This is consistent with other studies examining the relationship between older age and COVID-related behaviors (37, 38). Feeling more susceptible, older adults are more likely to test, get vaccinated, and more likely to perceive preventative behaviors—such as social distancing and avoiding crowds—as effective (37, 39, 40). In contrast, young adults in the study were motivated to test to protect older or more vulnerable people in their social circle. Younger adults, though they see themselves as less susceptible, recognized the increased risk to older groups, and often cited “protecting others” as a primary motivation for testing and vaccination (31, 41).
Participants identified a number of barriers to testing, including some of which have been identified in prior studies, such as long lines, difficulty navigating questions about insurance coverage and how to access tests, and cost (28, 30, 42–44). While at-home COVID testing was seen as a more convenient and accessible alternative to in-person testing by younger participants, older adults expressed concern about making an error during self-testing. As other population groups have identified, both young adult and older adult participants emphasized the benefits of easier access via a central well known location, in-home visits, free or low-cost tests, and increased outreach (28, 42, 45, 46). Notably, all groups recommended the housing authority as a venue for testing service provision.
Participants in this study provided recommendations that could be utilized and expanded on, many of which were specific to NYCHA. For example, participants proposed that building management could distribute PPE or test kits, and a number of participants reported a higher level of cleanliness in communal areas of their buildings (e.g., lobbies; stairwells), which supported their ability to reduce transmission of COVID-19 through safe hygiene practices. Though underexplored in research literature, there are examples of the critical role of public housing programs in addressing the spread and effects of COVID-19. One paper examining the impact of the U. S. Housing and Urban Development sponsored service coordinators found that throughout the pandemic these coordinators were crucial in several areas, including resident needs assessment, benefits and program applications, dissemination of public health recommendations, addressing loneliness/isolation, and coordination between organizations (47). In the face the of rapidly changing nature of the pandemic, as well as lapses in typical benefits and services, these coordinators were able to leverage their knowledge of residents’ needs, property resources and staff, and public and community service programs to great effect (47).
In NYC specifically, NYCHA was a key partner to government agencies and CBOs. Test & Trace – the city’s interagency initiative to provide testing, contact tracing, and aftercare support – implemented a mobile testing program to address testing inequities in neighborhoods disproportionately affected by COVID-19. Between June 2020 and December 2021, Test & Trace was the largest provider of COVID testing services in NYC, operating 586 testing sites throughout the city (48). Many of these testing sites were set up on or near NYCHA property, including on-site senior and community centers (48, 49). Moreover, 90% of NYCHA service coordinators surveyed indicated that their properties had offered on-site vaccination at least once (47). Our participants repeatedly referenced these on-site centers, stating that they were crucial in making testing and vaccination accessible, and should continue to serve as a site for COVID-19 related resources and services. One analysis of housing and COVID-19 found that living in NYCHA may have a protective effect (9). One possible explanation could be that as a public entity, NYCHA—and therefore the residents—can more easily be connected to public services and initiatives (49, 50). This was demonstrated in another study, whereby public housing residence was associated with lower rates of uninsurance and unmet medical need. The authors posited that housing stability and reduced housing costs may give residents the opportunity and resources needed to access care (51). Presumably, this holistic approach could also contribute to COVID-19 awareness.
Our study has some limitations, including the small sample size of 32 focus group participants. Focus groups were only conducted in English due to time and staffing constraints, which limited our reach to other populations, particularly Spanish-only speaking older adults who may have been linguistically isolated (51). Additionally, using a virtual platform for the focus groups may have been a barrier to participation for some older adults, possibly hindering their enrollment. The confluence of these two factors may explain why our older adult group was both smaller and more homogenous than that of young adults. However, our sample can still be considered representative with regards to other characteristics: all participants were residents of public housing, and there was a high degree of similarity for certain socioeconomic factors (income, percent employment, educational attainment) that remained consistent across race/ethnicity (12, 52). Moreover, though women were overrepresented in our participant pool, this is also reflective of NYCHA’s overall population, including older residents (12). The timing of the study may also present a limitation – focus groups were conducted from June through November of 2022, when the level of public concern for COVID-19 was declining (52). Some of our focus group questions asked participants to recall how they felt during the early stages of the pandemic, which may have introduced some recall bias (53).
Despite these limitations, our findings are still a major contribution to the literature due to our populations of interest. A focus on residents of public housing is important given the particular vulnerabilities of this group, as well as the potential for public housing infrastructure to provide resources to improve COVID-19-related information sharing and testing. Equally important is our focus on two high-risk, understudied age profiles. To adequately target these distinct populations, a comparative understanding of their needs, beliefs and behaviors will be required, and our findings can be used to inform interventions in the event of future COVID surges or similar epidemics. Though it has been several years since the acute phase of the COVID-19 pandemic, there remains a potential for COVID-19 resurgences due to new variants, waning immunity, low vaccination rates, and the relaxation of social distancing and other protective behaviors. As such, mitigation strategies specific to COVID-19 may still be needed in the future (54–56). Moreover, our results are also broadly applicable to other infectious diseases, in particular respiratory viruses such as influenza, RSV, streptococcus, and other coronaviruses, which, like COVID-19, are seasonally epidemic, disproportionately affect the same populations, and have multiple means of diagnostic testing (clinical and at-home) that can be leveraged to reduce spread and burden of disease (57–60).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of NYU Grossman School of Medicine (i20-01636). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EG: Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. ZH: Formal analysis, Investigation, Visualization, Writing – review & editing. LT: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. NW: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. EA: Writing – review & editing. SB: Writing – review & editing. MP: Conceptualization, Methodology, Writing – review & editing. JR: Conceptualization, Methodology, Writing – review & editing. DS: Conceptualization, Funding acquisition, Investigation, Methodology, Writing – review & editing. MB: Conceptualization, Formal analysis, Investigation, Methodology, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by National Institutes of Health (Grant No: 3R01CA220591-03S1).
Acknowledgments
We would like to thank our colleagues at the New York City Housing Authority and partnering community-based organizations (Harlem Congregations for Community Improvement, Inc. and Henry Street Settlement) for their assistance in conducting this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1484473/full#supplementary-material
Abbreviations
RADx-UP, Rapid Diagnostics of Underserved Populations; CBO, Community based Organization; NYCHA, New York City Housing Authority; NYC, New York City; IBM, Integrated Behavioral Model; OA, Older Adults; YA, Younger Adults.
References
1. Kuniya, T, and Inaba, H. Possible effects of mixed prevention strategy for COVID-19 epidemic: massive testing, quarantine and social distancing. AIMS Public Health. (2020) 7:490–503. doi: 10.3934/publichealth.2020040
2. Binnicker, MJ. Emergence of a novel coronavirus disease (COVID-19) and the importance of diagnostic testing: why partnership between clinical laboratories, public health agencies, and industry is essential to control the outbreak. Clin Chem. (2020) 66:664–6. doi: 10.1093/clinchem/hvaa071
3. Salathé, M, Althaus, CL, Neher, R, Stringhini, S, Hodcroft, E, Fellay, J, et al. COVID-19 epidemic in Switzerland: on the importance of testing, contact tracing and isolation. Swiss Med Wkly. (2020) 150:w20225. doi: 10.4414/smw.2020.20225
4. Shortreed, SM, Gray, R, Akosile, MA, Walker, RL, Fuller, S, Temposky, L, et al. Increased COVID-19 infection risk drives racial and ethnic disparities in severe COVID-19 outcomes. J Racial Ethn Health Disparities. (2023) 10:149–59. doi: 10.1007/s40615-021-01205-2
5. Holtgrave, DR, Barranco, MA, Tesoriero, JM, Blog, DS, and Rosenberg, ES. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York state. Ann Epidemiol. (2020) 48:9–14. doi: 10.1016/j.annepidem.2020.06.010
6. Raine, S, Liu, A, Mintz, J, Wahood, W, Huntley, K, and Haffizulla, F. Racial and ethnic disparities in COVID-19 outcomes: social determination of health. Int J Environ Res Public Health. (2020) 17:8115. doi: 10.3390/ijerph17218115
7. CDC COVID-19 Response Team. Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:343–6. doi: 10.15585/mmwr.mm6912e2
8. Snowden, LR, and Graaf, G. COVID-19, social determinants past, present, and future, and African Americans’ health. J Racial Ethn Health Disparities. (2021) 8:12–20. doi: 10.1007/s40615-020-00923-3
9. Gouse, I, Walters, S, Miller-Archie, S, Singh, T, and Lim, S. The role of housing characteristics in racial and ethnic disparities in SARS-CoV-2 antibody seropositivity among new York City adults: a population representative study. Prev Med. (2022) 164:107287. doi: 10.1016/j.ypmed.2022.107287
10. Gu, T, Mack, JA, Salvatore, M, Prabhu Sankar, S, Valley, TS, Singh, K, et al. Characteristics associated with racial/ethnic disparities in COVID-19 outcomes in an academic health care system. JAMA Netw Open. (2020) 3:e2025197. doi: 10.1001/jamanetworkopen.2020.25197
11. Varshney, K, Glodjo, T, and Adalbert, J. Overcrowded housing increases risk for COVID-19 mortality: an ecological study. BMC Res Notes. (2022) 15:126. doi: 10.1186/s13104-022-06015-1
13. Schwartz, B. Monitor's first quarterly report for the New York City housing authority. New York: NYCHA (2019).
15. Chen, Y-H, Glymour, M, Riley, A, Balmes, J, Duchowny, K, Harrison, R, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: march through November 2020. PLoS One. (2021) 16:e0252454. doi: 10.1371/journal.pone.0252454
16. Hawkins, D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am J Ind Med. (2021) 63:817–20. doi: 10.1002/ajim.23145
17. Gates, MJC, Sen, M, Mandeville, C, Calvin, E, Nicholas, M, and Uribe, M. NYCHA’S crisis: a matter for all New Yorkers. New York: Regional Plan Association (2018).
18. CDC. (2021). COVID-19 vaccination and case trends by age group, United States. Available online at: https://data.cdc.gov/Vaccinations/Archive-COVID-19-Vaccination-and-Case-Trends-by-Ag/gxj9-t96f. (Accessed November 15, 2022).
20. U.S. Census Bureau. Total population and persons per acre, 2000 and 2010 New York City and boroughs. U.S. Census Bureau (2010).
21. Monod, M, Blenkinsop, A, Xi, X, Hebert, D, Bershan, S, Tietze, S, et al. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. (2021) 371:eabe8372. doi: 10.1126/science.abe8372
22. Parton, HB, Flatley, AM, Viswanathan, N, Wilensky, L, Berman, J, Ralph, N, et al. Health of older adults in new york city public housing: part 1, findings from the new york city housing authority senior survey. Care Mgt J. (2012) 13:134–47.
23. Williams, NJ, Gill, E, Punter, MA, Reiss, J, Goodman, M, Shelley, D, et al. Rapid community engagement in response to SARS-CoV-2 funding opportunities: new York City, 2020–2021. Am J Public Health. (2022) 112:S904–8. doi: 10.2105/AJPH.2022.307072
24. Glanz, K. Health behavior: theory, research, and practice. Newark, United States: John Wiley & Sons (2015).
25. Izeogu, C, Gill, E, Van Allen, K, Williams, N, Thorpe, LE, and Shelley, D. Attitudes, perceptions, and preferences towards SARS CoV-2 testing and vaccination among African American and Hispanic public housing residents, new York City: 2020–2021. PLoS One. (2023) 18:e0280460. doi: 10.1371/journal.pone.0280460
26. Gale, RC, Wu, J, Erhardt, T, Bounthavong, M, Reardon, CM, Damschroder, LJ, et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the veterans health administration. Implement Sci. (2019) 14:11. doi: 10.1186/s13012-019-0853-y
27. Singh, H, Tang, T, Thombs, R, Armas, A, Nie, JX, Nelson, MLA, et al. Methodological insights from a virtual, team-based rapid qualitative method applied to a study of providers' perspectives of the COVID-19 pandemic impact on hospital-to-home transitions. Int J Qual Methods. (2022) 21:16094069221107144. doi: 10.1177/16094069221107144
28. Bateman, LB, Hall, AG, Anderson, WA, Cherrington, AL, Helova, A, Judd, S, et al. Exploring COVID-19 vaccine hesitancy among stakeholders in African American and Latinx communities in the deep south through the Lens of the health belief model. Am J Health Promot. (2022) 36:288–95. doi: 10.1177/08901171211045038
29. Gin, JL, Balut, MD, and Dobalian, A. COVID-19 vaccine hesitancy among U.S. veterans experiencing homelessness in transitional housing. Int J Environ Res Public Health. (2022) 19:5863. doi: 10.3390/ijerph192315863
30. Balhotra, K, Chahal, K, Silver, M, Atallah, F, Narayanamoorthy, S, and Minkoff, H. COVID-19 vaccine hesitancy in an underrepresented minority community. J Community Health. (2023) 48:489–95. doi: 10.1007/s10900-022-01184-3
31. Brandt, EJ, Rosenberg, J, Waselewski, ME, Amaro, X, Wasag, J, and Chang, T. National Study of youth opinions on vaccination for COVID-19 in the U.S. J Adolesc Health. (2021) 68:869–72. doi: 10.1016/j.jadohealth.2021.02.013
32. Gentsch, AT, Butler, J, O'Laughlin, K, Eucker, SA, Chang, A, Duber, H, et al. Perspectives of COVID-19 vaccine–hesitant emergency department patients to inform messaging platforms to promote vaccine uptake. Acad Emerg Med. (2023) 30:32–9. doi: 10.1111/acem.14620
33. Carllee, S, Willis, DE, Andersen, JA, Gurel-Headley, M, Kraleti, SS, Selig, JP, et al. Healthcare access and experiences of racial discrimination as predictors of general vaccine hesitancy. Vaccine. (2023) 11:409. doi: 10.3390/vaccines11020409
34. Bardosh, K, de Figueiredo, A, Gur-Arie, R, Jamrozik, E, Doidge, J, Lemmens, T, et al. The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good. BMJ glob. Health. (2022) 7:8684. doi: 10.1136/bmjgh-2022-008684
35. Bok, S, Martin, DE, Acosta, E, Lee, M, and Shum, J. Validation of the COVID-19 transmission misinformation scale and conditional indirect negative effects on wearing a mask in public. Int J Environ Res Public Health. (2021) 18:1319. doi: 10.3390/ijerph182111319
36. Chaudhuri, S, Le, T, White, C, Thompson, H, and Demiris, G. Examining health information-seeking behaviors of older adults. Comput Inform Nurs. (2013) 31:547–53. doi: 10.1097/01.NCN.0000432131.92020.42
37. Sun, N, Hua, CL, Qiu, X, and Brown, JS. Determinants of COVID-19 testing among late middle-aged and older adults: applying the health belief model. Aging Health Res. (2022) 2:100066. doi: 10.1016/j.ahr.2022.100066
38. Niño, M, Harris, C, Drawve, G, and Fitzpatrick, KM. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: evidence from two national data sources. SSM Popul Health. (2021) 13:100717. doi: 10.1016/j.ssmph.2020.100717
39. Bechard, LE, Bergelt, M, Neudorf, B, DeSouza, TC, and Middleton, LE. Using the health belief model to understand age differences in perceptions and responses to the COVID-19 pandemic. Front Psychol. (2021) 12:609893. doi: 10.3389/fpsyg.2021.609893
40. McElfish, PA, Willis, DE, Shah, SK, Bryant-Moore, K, Rojo, MO, and Selig, JP. Sociodemographic determinants of COVID-19 vaccine hesitancy, fear of infection, and protection self-efficacy. J Prim Care Community Health. (2021) 12:21501327211040746. doi: 10.1177/21501327211040746
41. Ravert, RD, Fu, LY, and Zimet, GD. Young adults' COVID-19 testing intentions: the role of health beliefs and anticipated regret. J Adolesc Health. (2021) 68:460–3. doi: 10.1016/j.jadohealth.2020.12.001
42. Embrett, M, Sim, SM, Caldwell, HAT, Boulos, L, Yu, Z, Agarwal, G, et al. Barriers to and strategies to address COVID-19 testing hesitancy: a rapid scoping review. BMC Public Health. (2022) 22:750. doi: 10.1186/s12889-022-13127-7
43. Garcini, LM, Pham, TT, Ambriz, AM, Lill, S, and Tsevat, J. COVID-19 diagnostic testing among underserved Latino communities: barriers and facilitators. Health Soc Care Community. (2022) 30:e1907–16. doi: 10.1111/hsc.13621
44. Carson, SL, Casillas, A, Castellon-Lopez, Y, Mansfield, LN, Morris, D, Barron, J, et al. COVID-19 vaccine decision-making factors in racial and ethnic minority communities in Los Angeles, California. JAMA Netw Open. (2021) 4:e2127582. doi: 10.1001/jamanetworkopen.2021.27582
45. Leal, DU. Communication and health in Brazil during the Covid-19 pandemic. J Qual Healthc Econ. (2023) 6:1–3. doi: 10.23880/jqhe-16000322
46. Chen, WC, and Huang, AS-E. COVID-19 public health surveillance and response in Taiwan: from containment to mitigation. J Formos Med Assoc. (2023) 123:S17–26. doi: 10.1016/j.jfma.2023.08.016
47. Scheckler, S, and Molinsky, J. Service coordination in HUD housing during the COVID-19 pandemic: bridging the gap. J Gerontol Soc Work. (2023) 66:152–76. doi: 10.1080/01634372.2022.2139320
48. Thorpe, LC, Bendik, S, Berry, C, Islam, N, Massar, R, and Wallach, A. Scale up of COVID-19 testing services in NYC, 2020-2021:lessons learned to maximize reach, equity and timeliness. J Urban Health. (2024) 101:913–22. doi: 10.1007/s11524-024-00918-z
49. Jiménez, J, Parra, YJ, Murphy, K, Chen, AN, Cook, A, Watkins, J, et al. Community-informed Mobile COVID-19 testing model to addressing health inequities. J Public Health Manag Pract. (2022) 28:S101–10. doi: 10.1097/PHH.0000000000001445
50. Lane, K, Smalls-Mantey, L, Hernández, D, Watson, S, Jessel, S, Jack, D, et al. Extreme heat and COVID-19 in new York City: an evaluation of a large air conditioner distribution program to address compounded public health risks in summer 2020. J Urban Health. (2023) 100:290–302. doi: 10.1007/s11524-022-00704-9
51. Simon, AE, Fenelon, A, Helms, V, Lloyd, PC, and Rossen, LM. HUD housing assistance associated with lower Uninsurance rates and unmet medical need. Health Aff. (2017) 36:1016–23. doi: 10.1377/hlthaff.2016.1152
52. Jones, J. Americans less optimistic about COVID-19 situation. (2022). Available online at: https://news.gallup.com/poll/396134/americans-less-optimistic-covid-situation.aspx (Accessed October 5, 2023).
53. Talari, K, and Goyal, M. Retrospective studies - utility and caveats. J R Coll Physicians Edinb. (2020) 50:398–402. doi: 10.4997/jrcpe.2020.409
54. COVIDVaxView C-. COVID-19 Vaccination Coverage and Intent for Vaccination, Adults 18 Years and Older, United States. (2025) Available online at: https://www.cdc.gov/covidvaxview/weekly-dashboard/adult-vaccination-coverage.html (Accessed May 23, 2025).
55. Zhou, W, Tang, B, Bai, Y, Shao, Y, Xiao, Y, and Tang, S. The resurgence risk of COVID-19 in China in the presence of immunity waning and ADE: a mathematical modelling study. Vaccine. (2022) 40:7141–50. doi: 10.1016/j.vaccine.2022.10.043
56. Truelove, S, Smith, CP, Qin, M, Mullany, LC, Borchering, RK, Lessler, J, et al. Projected resurgence of COVID-19 in the United States in July-December 2021 resulting from the increased transmissibility of the Delta variant and faltering vaccination. eLife. (2022) 11:e73584. doi: 10.7554/eLife.73584
57. Zhao, C, Zhang, T, Guo, L, Sun, S, Miao, Y, Yung, CF, et al. Characterising the asynchronous resurgence of common respiratory viruses following the COVID-19 pandemic. Nat Commun. (2025) 16:1610. doi: 10.1038/s41467-025-56776-z
58. Black, CL, O'Halloran, A, Hung, MC, Srivastav, A, Lu, PJ, Garg, S, et al. Vital signs: influenza hospitalizations and vaccination coverage by race and ethnicity-United States, 2009-10 through 2021-22 influenza seasons. MMWR Morb Mortal Wkly Rep. (2022) 71:1366–73. doi: 10.15585/mmwr.mm7143e1
59. Kondo, KK, Williams, BE, Ayers, CK, Kansagara, D, Smith, M, Advani, SM, et al. Factors associated with health inequalities in infectious disease pandemics predating COVID-19 in the United States: a systematic review. Health Equity. (2022) 6:254–69. doi: 10.1089/heq.2021.0049
Keywords: COVID-19, public housing, testing intentions, information sources, health belief model
Citation: Gill E, Hall Z, Thorpe LE, Williams NJ, Anastasiou E, Bendik S, Punter M, Reiss J, Shelley D and Bragg M (2025) COVID-19 testing experiences and attitudes among young adults and socially isolated older adults living in public housing, New York City (2022). Front. Public Health. 13:1484473. doi: 10.3389/fpubh.2025.1484473
Edited by:
Jeff Bolles, Francis Marion University, United StatesReviewed by:
Maria Francesca Piazza, University of Genoa, ItalyNichole Sams, University of Washington, United States
Copyright © 2025 Gill, Hall, Thorpe, Williams, Anastasiou, Bendik, Punter, Reiss, Shelley and Bragg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emily Gill, ZW1pbHkuZ2lsbEBueXVsYW5nb25lLm9yZw==
 Emily Gill
Emily Gill Zora Hall1
Zora Hall1 Lorna E. Thorpe
Lorna E. Thorpe Natasha J. Williams
Natasha J. Williams Malcolm Punter
Malcolm Punter