- 1School of Sport Science, Beijing Sport University, Beijing, China
- 2School of Physical Education, Xihua University, Chengdu, China
- 3Shanxi Sports Vocational School, Taiyuan, Shanxi, China
- 4Department of Kinesiology, Recreation, and Sport Studies, The University of Tennessee, Knoxville, TN, United States
Background: Childhood obesity is a growing public health concern, with preschool obesity rates in China reaching 10.4%. Physical activity (PA) is crucial for childhood obesity prevention, yet many children fail to meet recommended PA levels. Existing research primarily examines BMI rather than a detailed analysis of body composition, with sex differences remaining uncertain. This study explores the effects of different 8-week PA interventions (LPA vs. MVPA) on body composition in Chinese preschoolers, offering valuable insights for early obesity prevention.
Methods: This study utilized a two-arm experimental design with repeated measures, involving 86 preschool children from Beijing, China. Participants were randomly assigned to either the LPA or MVPA group and participated in an 8-week intervention, consisting of three 30-min sessions per week. Body composition was assessed pre- and post-intervention using bioelectrical impedance analysis (BIA), while dietary intake was evaluated through 24-h dietary recalls. Data analysis mainly included repeated-measures MANCOVA, with dietary intake controlled as a covariate.
Results: There were no significant interaction effects of Group × Time, and Group × Time × Sex for any variables. A small but significant Sex × Time interaction for BMI was detected (F (1,71) = 4.41, p = 0.04,
Conclusion: PA showed a positive effect in preventing excessive BMI growth in boys, with MVPA potentially preventing the rapid accumulation of body fat. Compared to LPA, MVPA appears to yield greater benefits in increasing TBW, SMM, and FFM, while also being more effective in preventing rapid increases in BFM and PBF among preschool children. For girls, engaging in vigorous PA may be crucial for effectively enhancing body composition development.
1 Introduction
The World Health Organization (WHO) identifies childhood obesity as a critical global public health issue (1). The prevalence of childhood overweight and obesity is expected to rise by 60% worldwide, with projections indicating that approximately 250 million children will be affected by 2030 (2, 3). Recent data show that the prevalence of obesity among preschool children in China has sharply increased to 10.4% (4). This is particularly concerning as childhood obesity often continues into adulthood (5) and is strongly linked to a higher risk of premature mortality, diabetes, and cardiovascular disease later in life (6, 7). Additionally, Children who have not yet reached the body mass index (BMI) threshold for being overweight or obese may still be at a higher risk of developing obesity (1). Regular participation in physical activity (PA) is one of the most crucial interventions to combat childhood obesity and maintain a healthy body composition in children (8, 9). The WHO guidelines on physical activity, sedentary behavior, and sleep for children under 5 years of age recommend that children aged 3–4 years engage in at least 180 min of total physical activity (TPA) per day, including a minimum of 60 min of moderate-to-vigorous physical activity (MVPA) (10). The Exercise Guidelines for Children (3–6 years old), issued by the Chinese government in 2018, recommend that preschool-aged children participate in over 180 min of various PA daily, including at least 60 min of MVPA (11). However, many children still fail to meet the recommended amounts of TPA (12–15) and MVPA (16–19). Notably, only a small proportion of Chinese children and adolescents met the recommendations outlined in the Canadian 24-Hour Movement Guidelines (20, 21). For example, Yin et al. found that only 14.6% of Chinese preschoolers met the integrated guidelines for PA, sleep duration, and screen time (22). Furthermore, a comparative study across 11 countries from five major geographical regions revealed that Chinese children had the lowest average daily engagement in MVPA (23). Therefore, there is an urgent need to develop and implement effective and novel PA programs for Chinese preschoolers to prevent and curb childhood obesity.
Many studies have examined the impacts of PA on childhood overweight and obesity (24–26), and the finding among preschool children have been inconsistent (27, 28). Numerous studies have demonstrated the benefits of PA in preventing childhood overweight and obesity, showing that increased PA can help lower BMI or reduce obesity risk in preschool children (29–34). However, research findings yielded mixed results. Some studies suggested no significant differences in BMI between intervention and control groups after PA interventions (35–37). One study even suggested a positive association between PA and BMI-z scores, providing evidence that higher PA levels may even increase the likelihood of overweight or obesity in children (38). A systematic review examining the relationships between combinations of movement behaviors and health indicators reported that, the most ideal combinations of sedentary behavior and PA were both favorably and not associated with adiposity among toddlers and preschool-aged children (27). Similar studies conducted in China often adopt comprehensive policy-based intervention measures, primarily including dietary modifications, PA, health education, family involvement, and kindergarten-based initiatives (39–41). However, these studies typically consider PA, diet, health education, and other factors as an integrated whole, making it difficult to isolate and analyze the specific relationships between obesity and any single component of the multi-component intervention, such as the association between obesity and PA.
Notably, it is evident that research in this field has primarily relied on BMI and similar simple metrics, such as BMI-z scores, while more accurate and comprehensive measures of body composition have been less frequently utilized (42). Most studies investigating the associations between PA and body composition in preschool children used cross-sectional designs (43, 44). As a result, these studies can only identify correlations rather than confirm causation. A few longitudinal studies conducted in this area have produced inconsistent findings. In brief, Bürgi et al. and Metcalf et al. reported no association between PA and adiposity among preschool-aged children (45, 46). In contrast, Leppänen and associates identified a positive correlation between MVPA and vigorous VPA with the fat-free mass (FFM) index (47). The impact of PA intensity on preschool children’s body composition remains inconclusive. Fu and colleagues found that, as MVPA time increased in overweight preschool children, the reduction in percent body fat (PBF) occurred at a faster rate compared to light PA (LPA) (48). Conversely, Bürgi et al. found no longitudinal relationship between baseline MVPA and changes in body fat or BMI (45). Jimenez-Pavon suggested that while higher PA levels may contribute to obesity prevention, further research is needed, particularly in younger children (49). Thus, although an increasing number of studies (9, 48, 50) have begun to emphasize the importance of early childhood body composition development—rather than focusing solely on BMI and its derived indicators, as was the case in earlier research—findings regarding the effects of PA, particularly at different intensities, on body composition in preschool children remain inconsistent. In China, empirical research on the impact of PA interventions on body composition in preschool children remains unexplored, highlighting the urgent need for further studies to fill this literature gap. Furthermore, while existing literature has extensively documented the health benefits of MVPA, limited evidence exists regarding the impact of LPA on preschool children’s body composition. In a longitudinal study with 6,059 children, Agbaje et al. examined the effects of accelerometer-measured sedentary time and physical activity on DEXA- measured fat mass, which demonstrated that cumulative LPA was associated with decreased total fat mass and trunk fat mass from childhood through young adulthood. Although this association may be partially mediated by increased insulin levels, the pediatric population especially those with chronic diseases or mobility challenges could benefit from LPA (51). The researchers also emphasized that their findings require further validation across diverse ethnic populations. Additionally, further research is warranted to explore potential associations between LPA and other important body composition indicators in preschool-aged children.
Body composition, including the distribution of materials and tissues, varies significantly based on age and sex (52). Throughout most of childhood, boys and girls exhibit similar growth rates. However, on average, boys tend to have slightly greater height, body mass, BMI, total body water (TBW), skeletal muscle mass (SMM) and fat-free mass (FFM) compared to girls, whereas while girls generally have higher body fat mass (BFM) and percent body fat (PBF) (53–59). Studies conducted in China and other countries have also reported sex differences in PA (19, 60, 61). Societal norms and expectations often lead to boys receiving greater encouragement and more opportunities to engage in PA, contributing to higher PA levels among boys compared to girls (62). As a result, boys are more likely to engage in greater amounts of PA, particularly MVPA, in their daily lives (63–66). Chen et al., in their large-scale study, further confirmed that preschool boys accumulate significantly more daily MVPA than girls (67). Additionally, participate in higher levels of MVPA across various activity types on both weekdays and weekends than their female counterparts (68). Moreover, the impact of PA on body composition may also differ by sex (49, 69, 70). Previous studies have found associations between MVPA and body composition parameters, such as BMI and PBF, particularly in boys (49, 70). Specifically, Basterfield et al. reported a significant correlation between MVPA and fat mass index (FMI) as well as BMI z-scores in boys, while no such relationship was observed in girls (70). Jiménez-Pavón et al., in their systematic review, concluded that the link between MVPA and body composition variables was more consistent in boys than in girls. However, the underlying reasons for boys’ greater sensitivity to MVPA variations remain unclear (49). Ferrari and colleagues found that in boys, moderate PA (MPA), VPA, MVPA, and step counts were all associated with body composition variables, whereas in girls, only VPA showed a significant correlation, independent of sedentary behavior (69). Meanwhile, studies have shown that the PBF of girls was more influenced by LPA and sleep (71, 72). However, most existing studies are cross-sectional, limiting the ability to determine causal relationships. It remains unclear whether PA directly influences body composition or if it serves as an indicator of other lifestyle factors, such as dietary habits, that may contribute to body composition changes. Furthermore, sex differences in how PA affects body composition in Chinese preschool children remain largely unanswered. Therefore, further research is needed to examine these sex-specific associations in this population.
Additionally, most research has focused on the overall growth and development of body composition in children, with limited attention to regional balance. However, fat mass (FM) and FFM may be distributed unevenly across the body, such as between the arms and legs or between the limbs and trunk, influenced by factors like sex, age, and physical activity (73). Santarém et al. found that total and segmental FFM were linked to walking capacity, with upper and lower limb FFM in women and trunk FFM in men correlating with functional performance (74). Therefore, assessing both total and segmental FFM in early childhood is essential.
This study aims to explore how PA affects the body composition of Chinese preschool children. We created a curriculum for both LPA and MVPA, followed by an 8-week intervention. We hypothesized that, compared to LPA, MVPA has a more significant impact on body composition in preschool children and that the impact of PA on body composition varies by sex. This research aims to provide valuable insights that can inform the creation of early intervention strategies to combat overweight and obesity in children. By understanding the impact of PA on body composition, these findings will help shape targeted interventions in preschool children. Ultimately, the goal is to promote healthier lifestyles among preschool children in China, ensuring they develop habits that support long-term wellbeing.
2 Materials and methods
2.1 Research design and participants
This study employed a 2-arm experimental design with repeated measures. A total of 86 preschool children (50 girls; mean age: 5.62 ± 0.26 years) were recruited from a kindergarten in Beijing, China. The inclusion criteria were that children: (1) were 5–6 years of age, (2) had no cognitive, developmental, mental or motor impairments, and no fractures or other injuries, and (3) had parental consent and child verbal assent. The exclusion criterion was defined as attendance absences exceeding 20% of the total intervention sessions.
Cluster randomization was implemented at the classroom level to avoid contamination between intervention conditions, as the PA programs were delivered during scheduled physical education classes. The randomization procedure was conducted as follows: (1) Eligibility Screening: All four senior kindergarten classes met the inclusion criteria (e.g., similar class sizes, baseline body composition indicators). (2) Random Allocation: An independent statistician generated a randomization sequence using a computer-based random number generator (block randomization with a 1:1 ratio). Class identifiers (e.g., Class A, B, C, D) were concealed in opaque envelopes labeled with unique codes. After baseline assessments, the envelopes were opened sequentially by a research assistant uninvolved in recruitment or intervention delivery, revealing the group assignment (i.e., LPA or MVPA). (3) Implementation: Teachers and researchers were blinded to the allocation sequence until interventions began. Participants attended kindergarten for approximately 8 h per day, Monday through Friday. The intervention took place over an 8-week intervention period for 30 min per session (including 20 min of exercise intervention games and 10 min of warm-up and cool-down) 3 days per week. Children’s body composition indicators were measured before and after the intervention, while dietary intake was measured at baseline. This study was approved by the Sports Science Experiment Ethics Committee of Beijing Sport University.
2.2 Procedures
Participants were recruited from kindergarten classes with the help of classroom teachers. The teachers distributed flyers describing the study to parents when they picked up their children after school. Preschool children who returned signed consent forms were then screened by the researchers. Body composition was measured at both baseline and post-intervention using the same testing procedures. To minimize data loss, any child absent on a scheduled measurement day was assessed on an alternate day. A detailed body composition analysis report and exercise recommendations was given to each child’s parents as an incentive for successfully completing all data collection sessions.
2.3 Intervention conditions
Prior to the formal intervention, we pre-designed both LPA and MVPA sessions. The development of these sessions drew upon the guidelines provided in the “Guidelines for the Learning and Development of Children Aged 3–6” (75) and the “Exercise Guidelines for Children (3–6 years old)” (11). This approach ensured that the intervention content was aligned with the physical and psychological developmental characteristics of preschool children. PA games, which combine physical exercise with engaging activities, are an effective approach to promoting the growth and development of preschool-aged children (76, 77). Therefore, both the LPA and MVPA sessions in this study were designed in the form of PA games. Polar H10 heart rate monitors (Polar Electro Oy, Kempele, Finland) and ActiGraph GT3X + Link accelerometers (ActiGraph Corp., Pensacola, FL, USA) were used to validate the intensity of each intervention session. Any session in which more than 60% of the activity time met the prescribed intensity requirements for each group was considered to fulfill the criteria for formal intervention. The accelerometer sampling frequency was set at 100 Hz, with data aggregated into 15-s epochs. Intensity thresholds were defined using the Buttle cut-points (78): sedentary (0–60 counts/15 s), light (60–530 counts/15 s), moderate (530–1,112.5 counts/15 s), and vigorous (≥1,112.5 counts/15 s). A threshold of 60% of the maximum heart rate (HRmax) was used, with light intensity defined as < 60% HRmax and moderate-to-vigorous intensity defined as > 60% HRmax (79). The maximum heart rate was calculated as HRmax = 208–0.7 × age. All intensity validations of the sessions were conducted on children not included in the main study sample.
A total of 30 structured sessions (15 for LPA and 15 for MVPA) were developed, each comprising a 5-min warm-up (e.g., dynamic stretching and low-intensity games), a 20-min core phase, and a 5-min cool-down (guided breathing and stretching). While both groups shared identical frequency (3 sessions/week), duration (30 min/session), and 8-week timeline, the only variation in intensity between the two groups was achieved by modifying game density (i.e., number of games per session), movement complexity (e.g., walking versus running while carrying a basketball), and contextual roles (e.g., children acting as pandas [slow-paced] versus monkeys [rapid-paced] in games) to regulate the intensity of PA. All sessions underwent intensity validation before being included in the formal intervention to ensure compliance with research requirements.
The primary researcher worked closely with school administrators and teachers to integrate the intervention into the kindergarten curriculum. Intervention fidelity was continuously monitored across all components. PA interventionists underwent extensive training and were actively involved in session design, modification, and validation. All PA interventionists actively participated in the implementation of the formal 8-week intervention program throughout its duration. Weekly meetings between the lead researcher and interventionists ensured program consistency. The research team conducted weekly monitoring to ensure adherence to pre-established protocols. Regular assessments evaluated protocol compliance, content fidelity, activity intensity, and children’s engagement. Attendance for each session was documented by interventionists, and researchers subsequently compiled the records to calculate attendance rates. 87% of participants completed ≥19/24 sessions (e.g., LPA: 86%; MVPA: 88%).
2.4 Measures
2.4.1 Body composition
Height and weight were measured according to the early childhood section of the China National Physical Fitness Determination Standard Manual, formulated by the State General Administration of Sports (80). Body mass index (BMI) was calculated from BMI = BM [kg] ÷ Height2 [m2].
In children, BMI assessment is usually interpreted using percentile charts. However, BMI alone does not offer detailed information about body fat mass (BFM). Overweight and obesity not only affect BFM and percent body fat (PBF) but can also lead to changes in other components of body composition. Dual-energy X-ray absorptiometry (DXA) is considered the” gold standard” for body composition assessment due to its safety, non-invasiveness, rapid scanning capability, and high precision (81). However, its widespread use among preschool-aged children is limited by the challenges of conducting on-site testing in kindergarten settings and the generally low acceptance rate among parents. Consequently, bioelectrical impedance analysis (BIA) has become one of the most widely used methods for estimating body composition, given its high accuracy, reproducibility, and suitability for field-based research outside laboratory settings (50, 82). Body composition was measured using an octapolar multifrequency bioelectrical impedance analyzer (Inbody models J30, Inbody, Seoul, Korea) at both baseline and post-intervention. The analysis allowed for the estimation of total body water (TBW), skeletal muscle mass (SMM), body fat mass (BFM), percent body fat (PBF), fat-free mass (FFM), free-fat mass of arm, leg and trunk. The tests were conducted after the children’s midday nap while standing, following the measurement guidelines (83).
2.4.2 Dietary intake
Daily energy intake was estimated using validated 24-h dietary recalls (84), conducted on three weekdays and one weekend day. These recalls were performed at the beginning of the training program with assistance from parents and/or investigators. The dietary records were then analyzed using Boohee health software (Boohee Info Technology Co., Shanghai, China) to calculate energy intake. Participants were asked to maintain their current diet throughout the duration of the study.
2.5 Statistical analyses
Data were imported from Excel into an SPSS Version 29.0 (IBM Corp., Armonk, NY, USA) dataset for descriptive and inferential statistical analyses. Screening for outliers and non-normality was conducted before the main analysis. First, a descriptive analysis was conducted to describe the sample characteristics, including frequencies of sex and all variables’ means and standard deviations. Second, independent samples t-tests were used to determine if there were differences in body composition indicators between the LPA group and MVPA group at baseline. Last, a multivariate analysis of co-variance with repeated measures was used to examine changes in preschool children’s body composition indicators across time. Group (LPA group vs. MVPA group) and sex (boys vs. girls) were included as between-subject factors, time was treated as a within-subject factor, and dietary intake was included as a covariate. The significance level was set at 0.05 for all statistical analyses, with effect sizes reported for each comparison. Specifically, partial eta-squared ( ) was used as an index of effect size, for which small, medium, and large effect sizes were designated as 0.10, 0.25, and 0.40, respectively (85).
3 Results
A priori power analysis was performed using G*Power 3.1. Based on a repeated-measures MANCOVA design with two between-subject factors (Group and Sex), two time points (pre-test and post-test), and dietary intake as a covariate. With α = 0.05 and β = 0.20 (80% power), the analysis indicated a required sample of 64 participants (16 per Group × Sex cell) to detect significant Time × Group interactions. While sample size calculations were performed at the individual level, we recognize that the cluster randomization design (with classes as the unit of randomization) may have introduced intra-class correlations. This design effect could potentially reduce the effective sample size and statistical power.
To account for potential attrition, 86 children were recruited. A total of 11 participants were excluded from the analysis due to missing data or insufficient attendance rates. The final sample comprised 75 preschool children (44 girls; 5.60 ± 0.27 years, mean ± SD), which is deemed as appropriate to yield meaningful results. Detailed demographic characteristics and pre-test body composition indicators between LPA and MVPA group is displayed in Table 1.
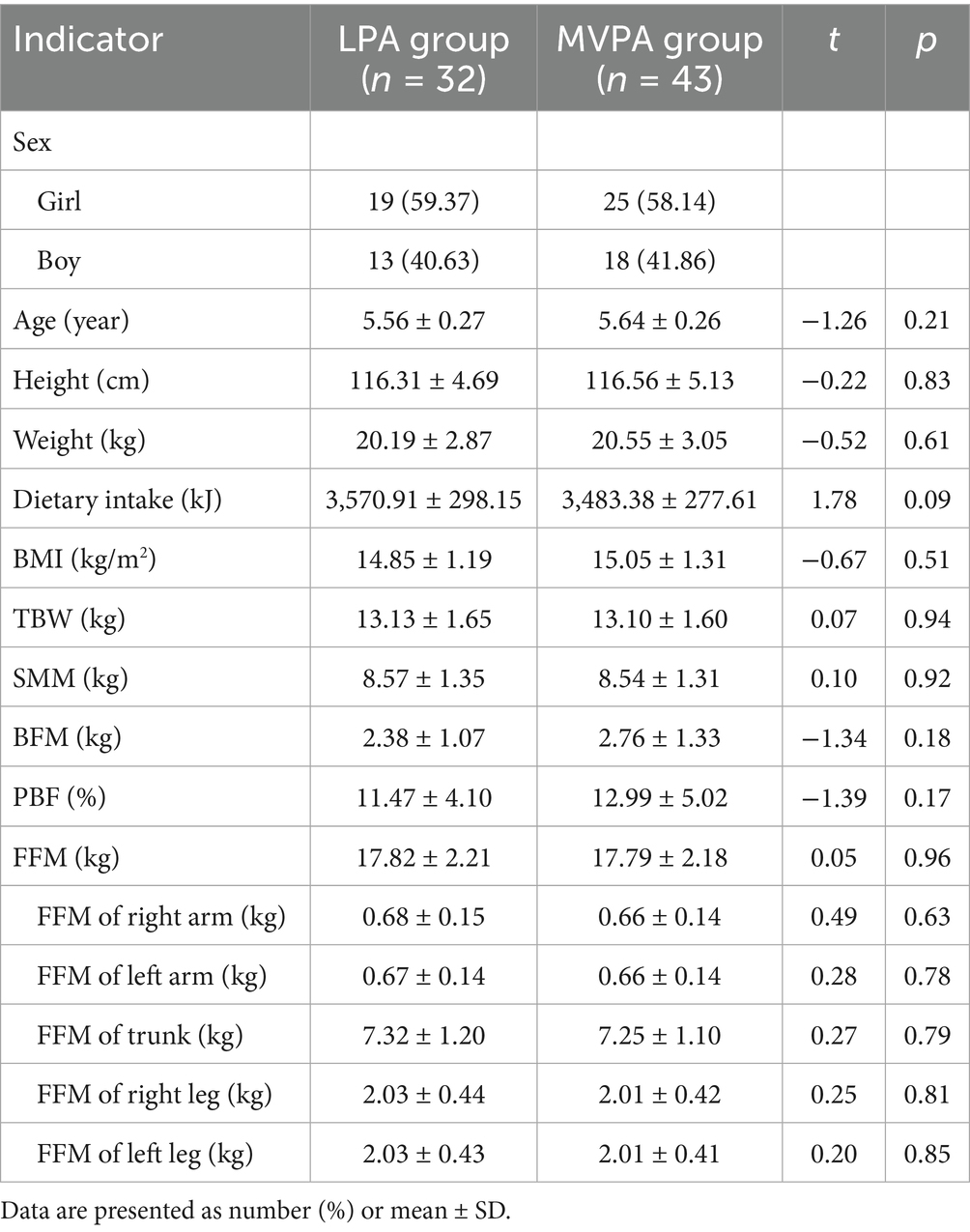
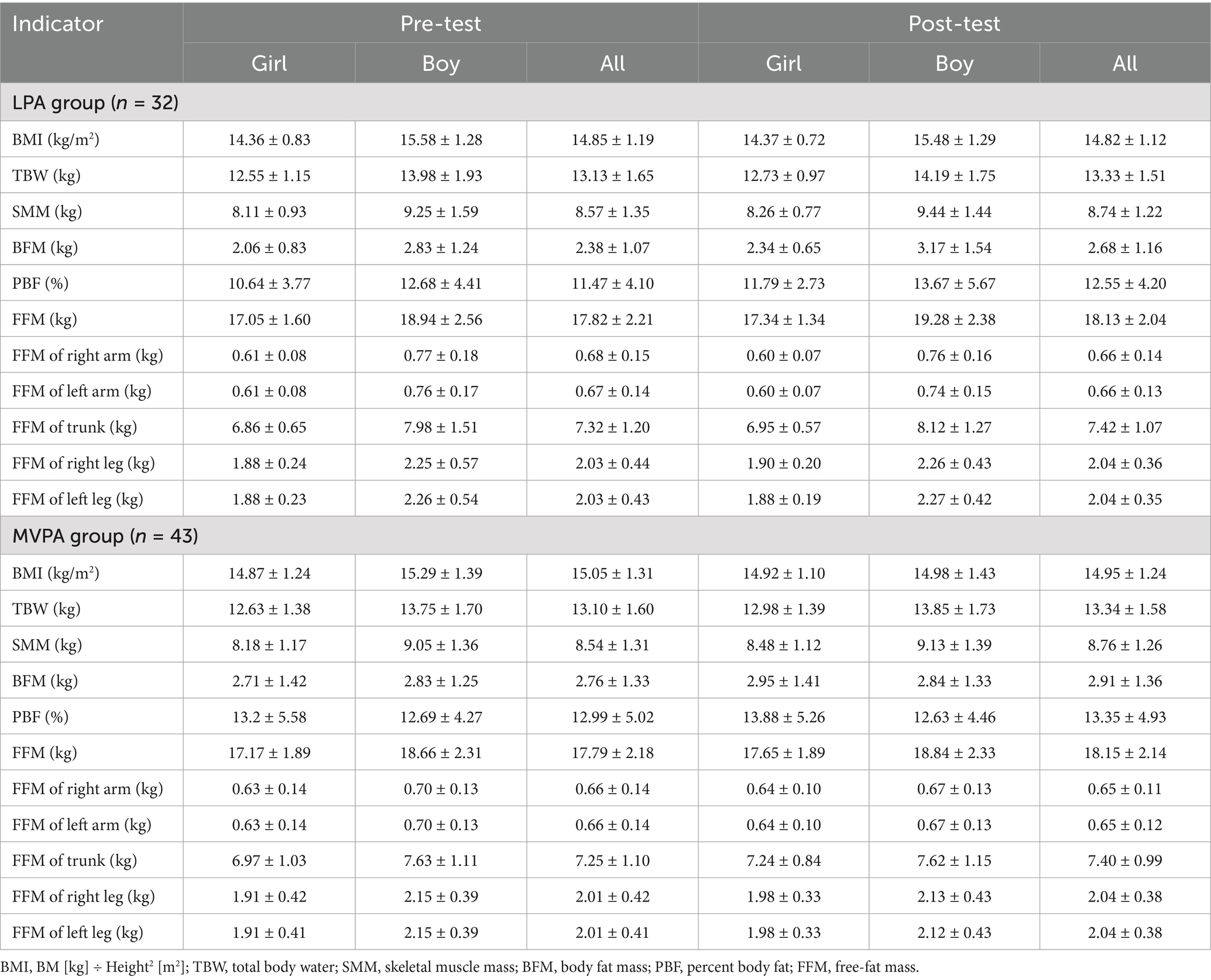
Table 1. Demographic characteristics and pre-test body composition indicators between LPA and MVPA group.
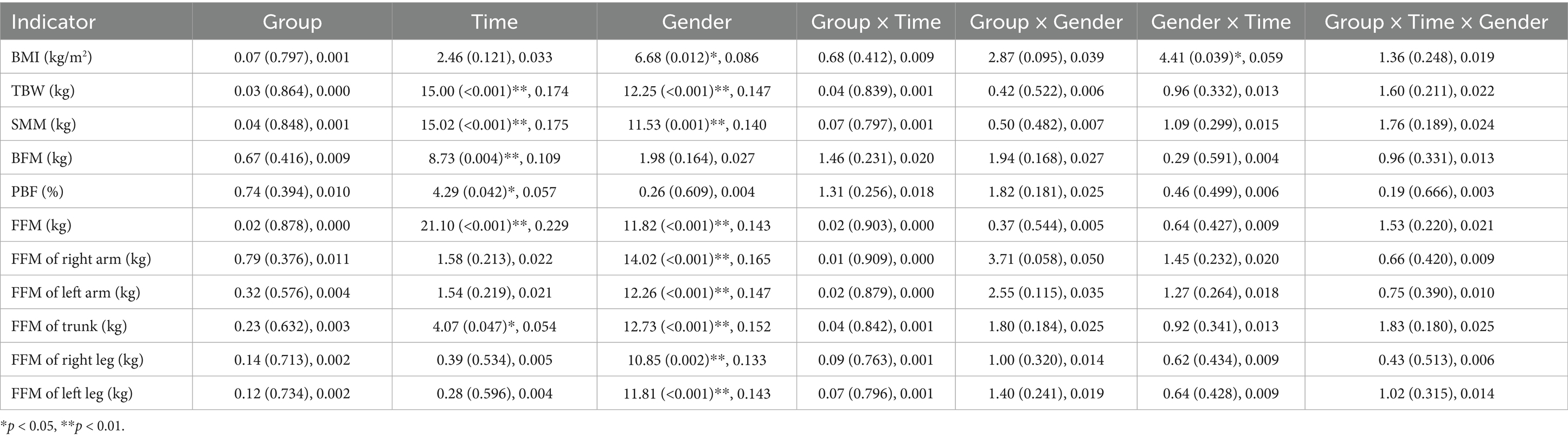
Pre-test data for children in the LPA group were comparable to those in the MVPA group with respect to age, height, weight, dietary intake, and body composition indicators (Table 1). Table 2 shows the descriptive results for the preschool children’s body composition indicators between intervention/sex groups and across time. Table 3 shows the results of the main effects and interaction effects analysis. Covariates appearing in the model are evaluated at the following values: Dietary intake = 3,533.57 (kJ).
There were no significant interaction effects of Group × Time for any variables. The Group × Sex interaction effect on FFM of the Right Arm was marginally significant (F (1,71) = 3.71, p = 0.06, = 0.05), suggesting a potential moderating role of sex in the observed effect. A small but significant Sex × Time interaction for BMI was detected (F (1,71) = 4.41, p = 0.04, = 0.06), while no significant interaction effects were found for other variables. Specifically, girls exhibited a significantly greater increase in BMI compared to boys, with a small effect size (Table 2). Moreover, there were no significant interaction effects of Group × Time × Sex for any variables (Table 3).
There was no significant group effect for any variable. Significant time effects were observed for TBW (F (1,71) = 15.00, p < 0.01, = 0.18) (Table 3; Figure 1A), SMM (F (1,71) = 15.02, p < 0.01, = 0.18) (Table 3; Figure 2A), BFM (F (1,71) = 8.73, p < 0.01, = 0.11) (Table 3; Figure 3A), PBF (F (1,71) = 4.29, p = 0.04, = 0.06) (Table 3; Figure 4A), FFM (F (1,71) = 21.10, p < 0.01, = 0.23) (Table 3; Figure 5A), and FFM of Trunk (F (1,71) = 4.07, p = 0.05, = 0.05) (Table 3; Figures 6A, 7A).
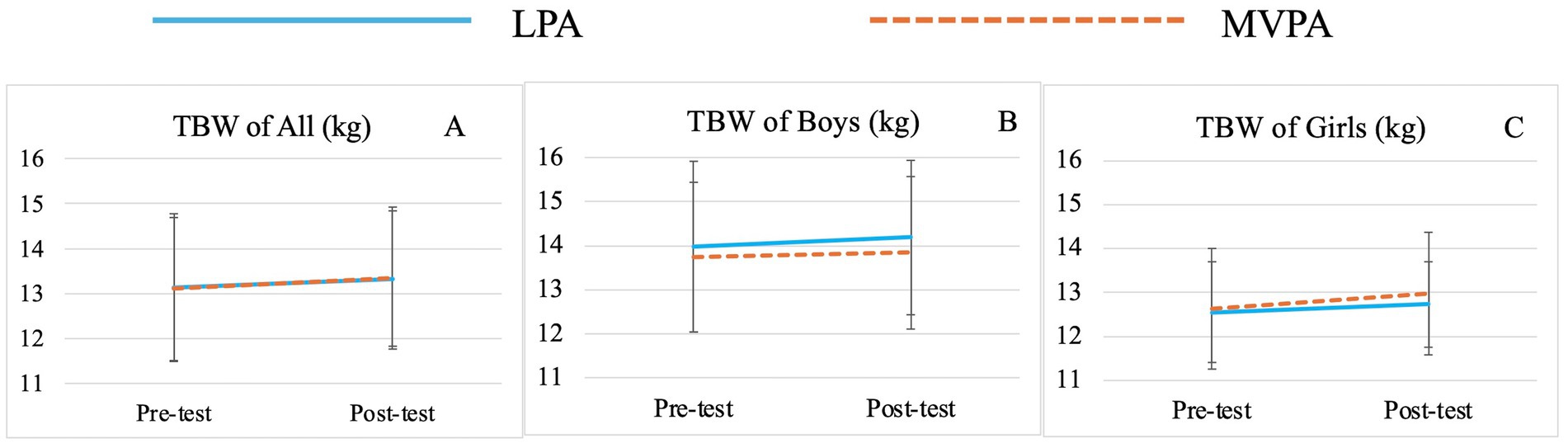
Figure 1. Changes of preschooler’s total body water (TBW) over time for the whole sample (A) and by genders (B for boys, C for girls).
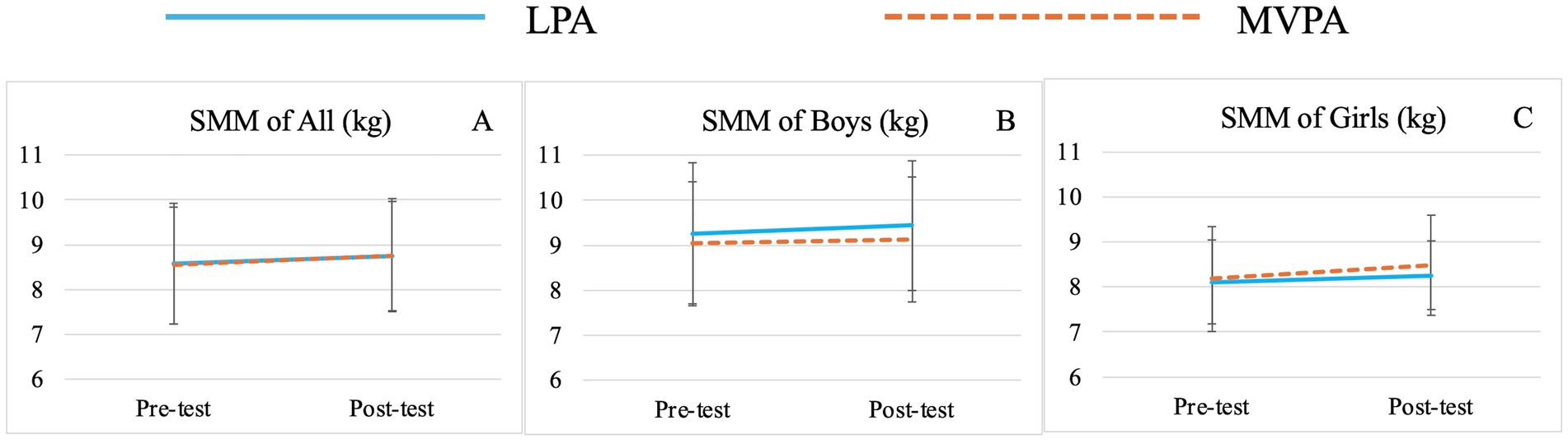
Figure 2. Changes of preschooler’s skeletal muscle mass (SMM) over time for the whole sample (A) and by genders (B for boys, C for girls).
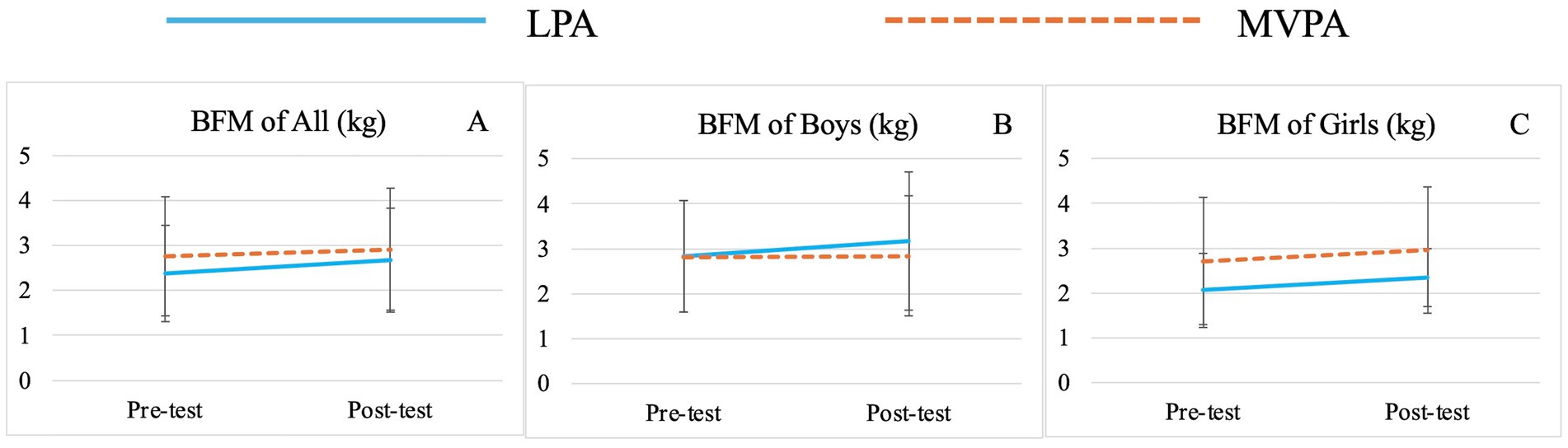
Figure 3. Changes of preschooler’s body fat mass (BFM) over time for the whole sample (A) and by genders (B for boys, C for girls).
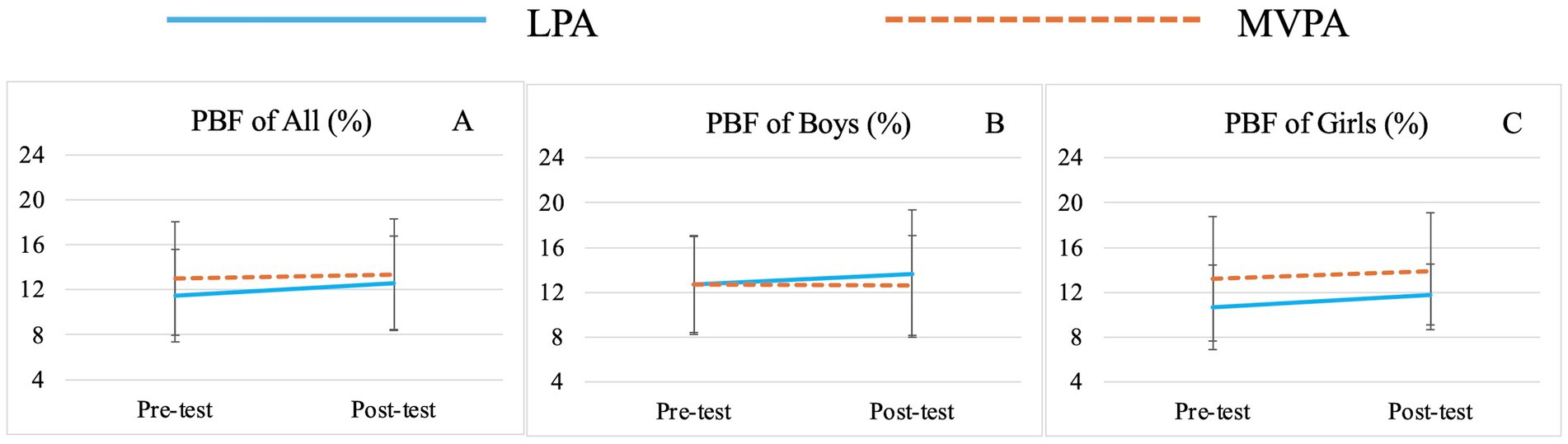
Figure 4. Changes of preschooler’s percent body fat (PBF) over time for the whole sample (A) and by genders (B for boys, C for girls).
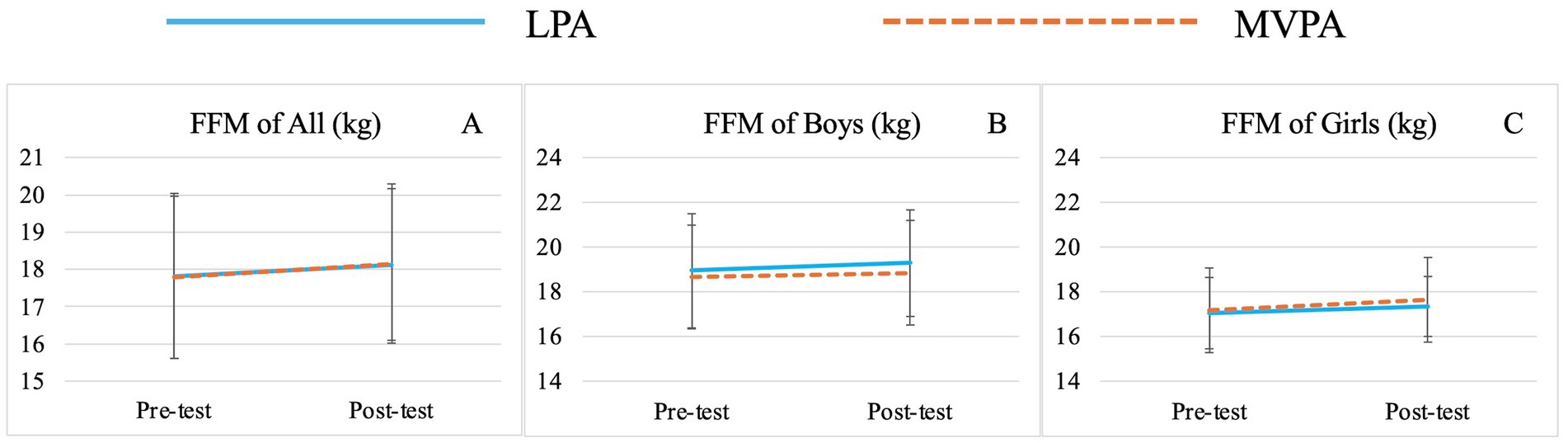
Figure 5. Changes of preschooler’s free-fat mass (FFM) over time for the whole sample (A) and by genders (B for boys, C for girls).
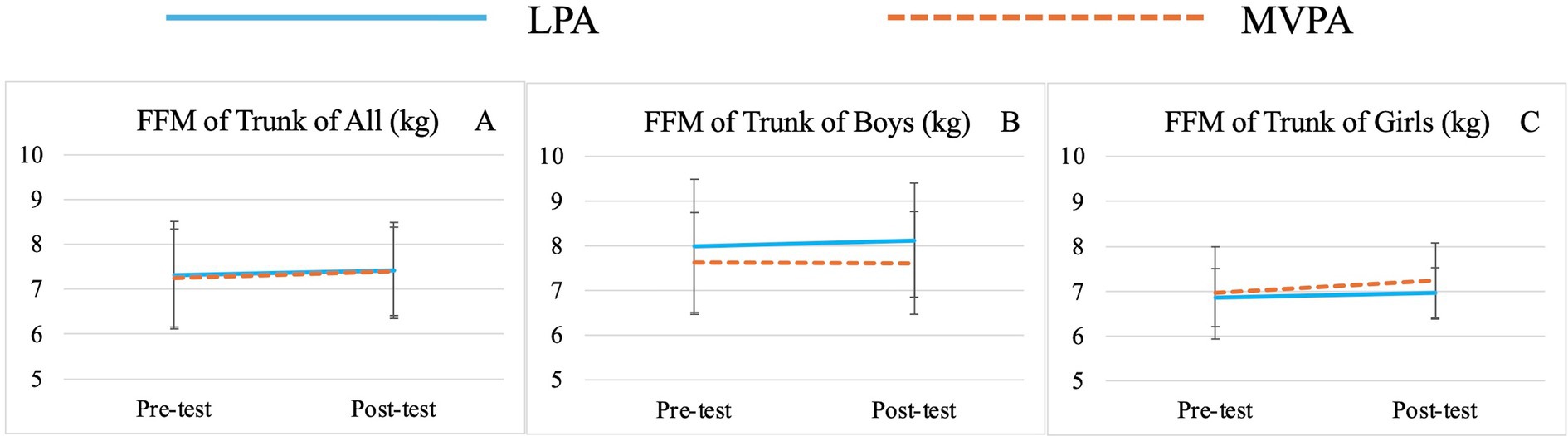
Figure 6. Changes of preschooler’s free-fat mass (FFM) of Trunk over time for the whole sample (A) and by genders (B for boys, C for girls).
Significant sex effects were observed for BMI (F (1,71) = 6.68, p = 0.01, = 0.09) (Table 3; Figures 7B,C), TBW (F (1,71) = 12.25, p < 0.01, = 0.15) (Table 3; Figures 1B,C), SMM (F (1,71) = 11.53, p < 0.01, = 0.14) (Table 3; Figures 2B,C), FFM (F (1,71) = 11.82, p < 0.01, = 0.14) (Table 3; Figures 5B,C), FFM of Right Arm (F (1,71) = 14.02, p < 0.01, = 0.17) (Table 3; Figure 8), FFM of Left Arm (F (1,71) = 12.26, p < 0.01, = 0.15) (Table 3; Figure 8), FFM of Trunk (F (1,71) = 12.73, p < 0.01, = 0.15) (Table 3; Figures 6B,C, 9), FFM of Right Leg (F (1,71) = 10.85, p < 0.01, = 0.13) (Table 3; Figure 10), and FFM of Left Leg (F (1,71) = 11.81, p < 0.01, = 0.14) (Table 3; Figure 10). Specifically, boys demonstrated higher BMI, TBW, SMM, FFM, FFM of Right Arm, FFM of Left Arm, FFM of Trunk, FFM of Right Leg, and FFM of Left Leg than girls at both time points (Table 2).
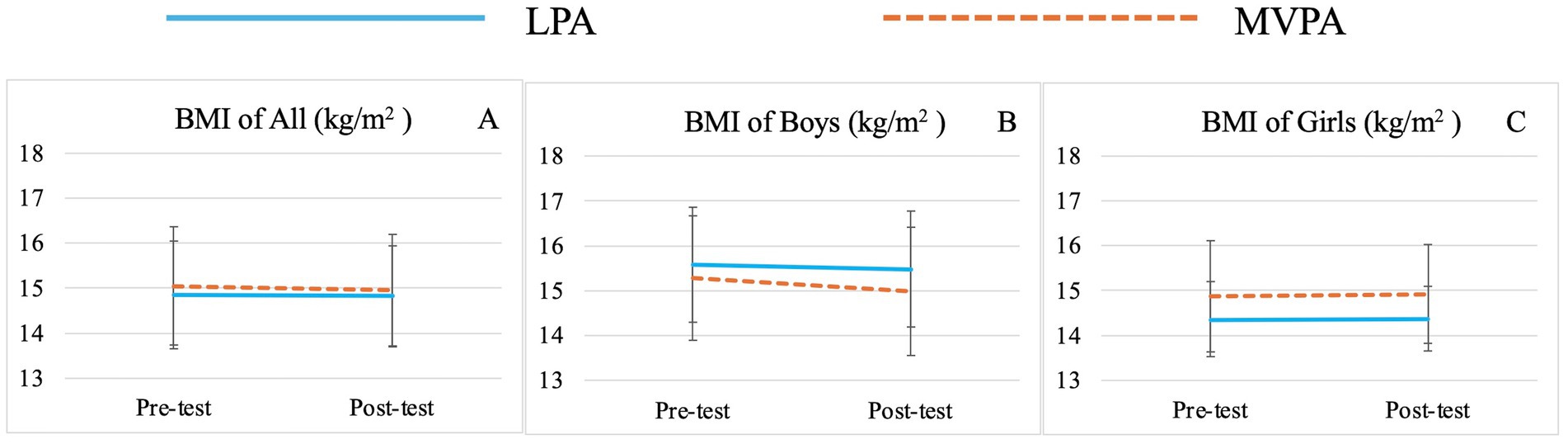
Figure 7. Changes of preschooler’s body mass index (BMI) over time for the whole sample (A) and by genders (B for boys, C for girls).
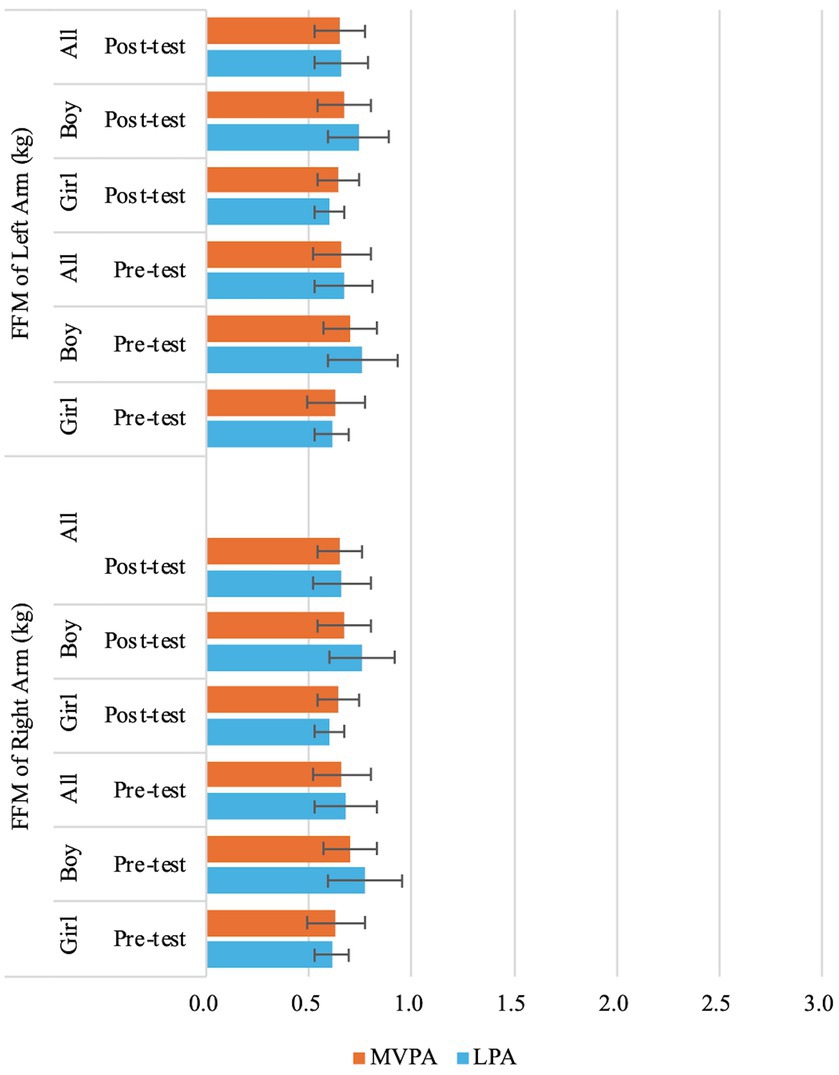
Figure 8. Changes of preschooler’s free-fat mass (FFM) of left arm and right arm over time for the whole sample and by genders.
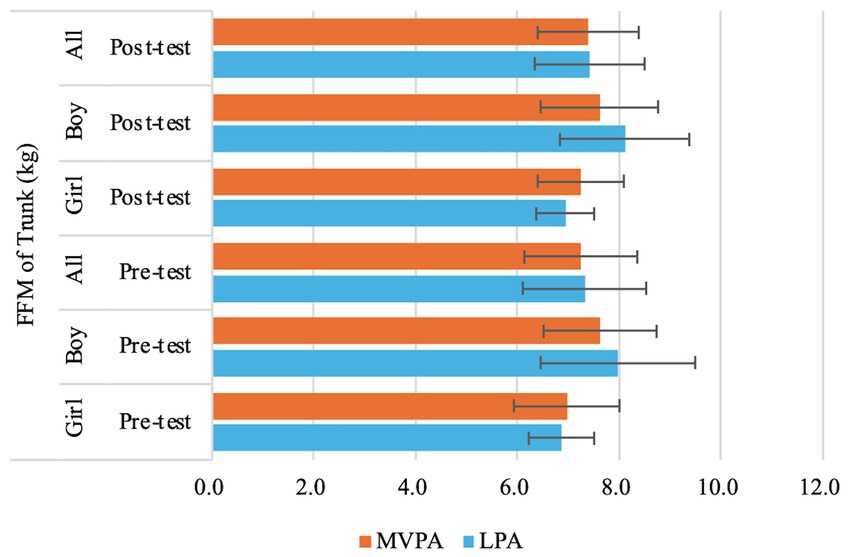
Figure 9. Changes of preschooler’s free-fat mass (FFM) of trunk over time for the whole sample and by genders.
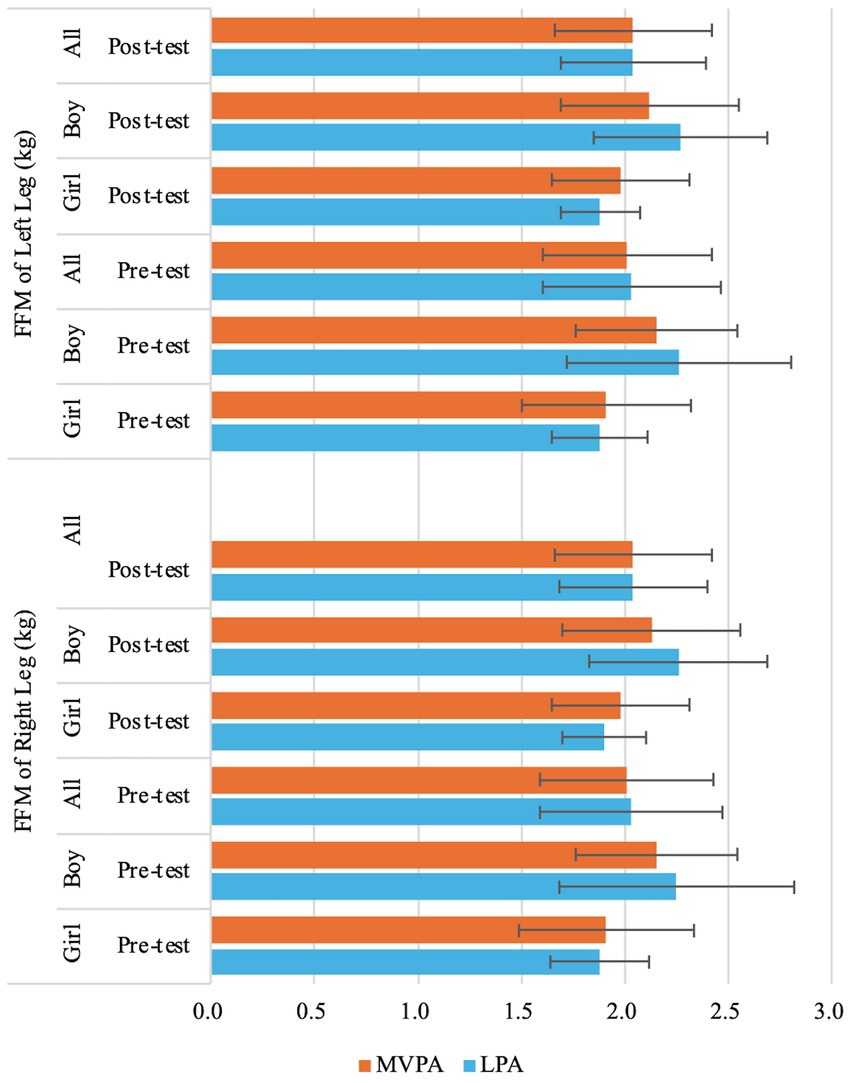
Figure 10. Changes of preschooler’s free-fat mass (FFM) of left leg and right leg over time for the whole sample and by genders.
4 Discussion
The healthy development of body composition during early childhood is vital for subsequent growth and development (86). PA games, which blend physical exercise with playful activities, are particularly important for the growth of preschool-aged children (76, 77). In this study, both types of PA interventions were delivered through PA games. Individual-level randomization was deemed impractical because the intervention required modifying structured physical education sessions at the classroom level. Cluster randomization minimized logistical conflicts (e.g., differing activity protocols within the same class) and ensured fidelity to the intervention design. This study assesses the effects of a school-based intervention on the body composition of Chinese preschool children by examining changes in body composition indicators before and after an 8-week PA game intervention, conducted at equal doses but differing in intensity (LPA vs. MVPA).
In this study, we found no significant interaction effects of Group × Time for body composition indicators. Our finding of no significant change at the 8-week follow-up is consistent with previous obesity prevention studies in both younger (87) and older children (88, 89). This may primarily be attributed to the fact that the majority of preschool children included in this study were within the healthy weight range. Yavuz et al. found that interventions focusing solely on overweight and obese children were more effective than those including children with a healthy weight (90). Had this study exclusively targeted overweight and obese children, the intervention effects might have been more pronounced. However, this study intentionally included healthy-weight children, emphasizing the importance of prevention in combating childhood obesity. Encouraging the early adoption of healthy behaviors and supporting long-term weight maintenance is essential for all children (91). Additionally, it is plausible that the 8-week intervention might be too short to yield positive effects on most study variables. Thus, a longer intervention period may be necessary to detect significant differences in body composition changes between groups.
Among the remaining interaction effects, this study only identified a significant Sex × Time interaction. It is observed that the changes in BMI differed between boys and girls over the 8-week PA intervention. In detail, girls had significantly greater increase in BMI than those in boys. During childhood, developmental trajectories of growth are largely comparable between sexes. Nevertheless, sex-specific differences in body composition emerge, with boys demonstrating moderately higher values in anthropometric indices (height, body mass, BMI) (53–59). The findings indicate that, compared to girls, boys’ BMI is more sensitive to PA. From the perspective of growth and development, research suggests that BMI in preschool-aged children typically displays a pattern of initial increase, followed by a decline—most notably between ages 4 and 5—before gradually rising again (104). In this study, the preschool children had a mean age of 5.6 years at baseline, a stage when BMI is expected to begin increasing. This further illustrates that, compared to girls, the PA intervention was more effective in moderating excessive BMI increases among boys.
Similarly, no significant group effects on body composition indicators were observed in this study. As previously mentioned, research on obesity or body composition interventions targeting preschool children remains limited (36), and the findings of existing studies have been mixed (27, 28). In brief, Waters and colleagues in their review identified only eight obesity prevention intervention studies focused on children under 5 years old. When examining the combined results, researchers found that BMI change from pre- to post-intervention was 0.26 units lower in the intervention group compared to the control group, though this difference was not statistically significant (92). Another systematic review of obesity intervention programs targeting Hispanic preschool children included eight studies, all incorporating nutrition and PA components, with some also addressing parenting guidance and social networking. However, only four of these studies reported significant reductions in children’s weight, BMI, or BMI-z scores (93). Overall, obesity prevention interventions in preschool children have shown differential effects on weight change and adiposity, highlighting the challenges of addressing obesity in this population (36). Interestingly, studies incorporating multiple intervention components have demonstrated limited effectiveness in improving BMI and body composition outcomes. Although the intervention was implemented rigorously in the present study, no significant main group effect on body composition was observed. However, this study still adds valuable insights to the evidence base for childhood obesity prevention. Previous research suggests that interventions targeting one or two specific behaviors (e.g., PA, diet) tend to yield the most effective outcomes (94, 95). This rationale underscores our study’s approach of controlling for dietary intake variables and focusing solely on changes in PA.
Although group effects on various body composition indicators were not observed in this study, preschoolers’ TBW, SMM, BFM, PBF, FFM and FFM of Trunk significantly improved from baseline to post-intervention regardless of group and sex affiliations. It should be acknowledged that this may be attributed to the natural growth and development of young children. However, greater increases in TBW, SMM, FFM and FFM of Trunk were still observed in the MVPA group over time, while greater increases in BFM and PBF were noted in the LPA group. The lack of statistical significance may be attributed to the relatively short intervention duration of 8 weeks and relatively small sample size. Nevertheless, these findings still provide valuable insights, to some extent, MVPA offers superior advantages in promoting the growth of TBW, SMM and FFM, while also being more effective in preventing the rapid increase in BFM and PBF in preschool children. This observation is consistent with those of previous studies (47, 69, 96–100). For example, Leppänen et al. found that higher levels of vigorous PA (VPA) and moderate-to-vigorous PA (MVPA) at age 4.5 were significantly linked to greater fat-free mass (FFM) after 12 months, suggesting that promoting high-intensity PA at an early age may have lasting benefits for body composition (47). Wyszyńska and colleagues, in their cross-sectional study with preschoolers, reported that boys engaging in less than 60 min of MVPA per day had twice the risk of obesity compared to peers who met the 60-min threshold (101). Similar trends have been observed in school-aged children and adolescents. A study on Brazilian children found that MVPA and daily step counts, particularly VPA, were associated with body composition independent of sedentary behavior (69). Research on adolescents further supports these findings, showing that VPA more effectively reduces subcutaneous fat and increases muscle mass (96–99). Adolescents engaging in VPA tend to have better body composition indicators, reflecting a higher proportion of metabolically active lean mass (102).
Significant sex effects were observed for BMI, TBW, SMM and FFM, with boys consistently showing higher values across time, aligning with previous research (53–59). Studies indicate that sex differences in body composition emerge early, with boys exhibiting greater BMI (53, 56, 59), TBW (58, 59), SMM (58, 59), FFM (53, 54, 59) than girls. However, prior research has also found that while boys generally have higher body composition indicators, girls tend to have greater BFM (53, 58, 59) and PBF (53–55, 57–59, 103). This study did not find significant sex differences in BFM or PBF. Within the MVPA group, boys initially had higher BFM than girls, despite having lower PBF, suggesting that their greater body weight contributed to more fat mass without an elevated body fat percentage. Notably, after the intervention, boys’ BFM decreased below that of girls, reinforcing the idea that MVPA may be particularly effective in reducing excess fat accumulation and controlling BMI growth in boys. Previous studies have highlighted sex differences in how PA impacts body composition. Among boys, MVPA was significantly associated with reductions in body fat indicators, while for girls, only VPA showed similar effects, independent of sedentary behavior (69). These findings suggest that for girls, VPA may be necessary to achieve meaningful improvements in body composition.
In addition to analyzing the overall changes in whole-body composition, this study also examined changes in FFM across specific body regions, an approach rarely seen in previous research (73, 74). The findings indicated significant sex effects in FFM of Right Arm, FFM of Left Arm, FFM of Trunk, FFM of Right Leg, and FFM of Left Leg, with boys exhibiting higher values for these indicators than girls across time. Moreover, differences in FFM between boys and girls were most pronounced in the trunks, followed by the legs, and least noticeable in the arms. After the intervention, although overall fat-free mass (FFM) increased in both boys and girls, FFM in the right and left arms decreased post-intervention, particularly among boys and girls in the LPA group and boys in the MVPA group. This suggests that body composition development in early childhood may not occur uniformly across different body regions. The results may be influenced by the nature of the PA programs, which primarily focused on running and jumping games, leading to limited upper limb engagement. This highlights an important consideration: designing PA programs for young children should incorporate exercises that target all body regions to support balanced body composition development.
This study had the following strengths: (1) It was one of the few known studies to integrate same dose but two different intensity of PA games into the school curriculum for preschool-aged children; (2) It considered the impact of food intake on body composition. After baseline dietary intake assessments, participants were instructed to maintain their usual dietary habits throughout the intervention period, minimizing potential confounding effects from dietary intake; and (3) It included a comprehensive range of objective body composition indicators, such as TBW, SMM, BFM, PBF, FFM, FFM of the arm, leg, and trunk. By examining the effects of different PA programs on these indicators, the study provides valuable and up-to-date information for parents, teachers, and researchers about the impact of PA on overall body composition and the composition of different body regions in young children. It provides theoretical support for enhancing awareness among parents and professionals in the field about early childhood growth and development, highlighting the critical importance of early attention to body composition development.
However, this study has several limitations. First, an important limitation is that our study included only four classes, which may have constrained our ability to detect small effect sizes. The cluster randomization design, while appropriate for our intervention, means that the effective sample size may be smaller than the nominal number of individual participants due to potential intra-class correlations. Future studies with larger numbers of clusters would help address this limitation. Second, while the study employed a quasi-experimental design, the absence of a true no-intervention control group precludes definitive causal inferences regarding intervention effects versus natural developmental changes. Third, despite the rigorous training for the researchers involved, the intervention duration was relatively short. Longer intervention periods are recommended for future studies. Fourth, due to class schedule constraints, it was not possible to randomly assign children to different classrooms, which resulted in the absence of individual-level randomization. Future studies should implement cluster randomized controlled trials across multiple kindergartens to minimize threats to the internal validity of the experiment. Additionally, the PA programs implemented in this study primarily focused on locomotor skills (e.g., running, and jumping), which may have resulted in limited upper limb engagement. Future research should incorporate upper-body-dominant activities (e.g., ladder climbing, and beanbag throwing) to investigate the region-specific effects of PA interventions on body composition. Lastly, while our current analysis accounted for clustering through appropriate methods, we acknowledge that employing hierarchical linear modeling (HLM) or generalized estimating equations (GEE) could provide additional robustness by more fully accounting for intra-cluster correlations. Future studies incorporating these advanced analytical approaches may yield further insights into these relationships.
5 Conclusion
The findings of this study provide new insights into the impact of PA programs of same dose but varying intensities on body composition in Chinese preschool children. PA showed a positive effect in preventing excessive BMI growth in boys, with MVPA potentially preventing the rapid accumulation of body fat. Compared to LPA, MVPA appears to have greater benefits in increasing TBW, SMM, and FFM, while also being more effective in preventing rapid increases in BFM and PBF among preschool-aged children. For girls, engaging in vigorous PA may be crucial for effectively enhancing body composition development. Future studies should identify different segments on children’s PA behaviors both at school and outside of school (105). High-quality intervention studies incorporating health education control groups and extended durations (e.g., ≥12 weeks) are needed to explore the role of PA at varying intensities in improving body composition and other health indicators among preschool children, and to systematically investigate the mechanisms underlying sex-specific responses to PA.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Sports Science Experiment Ethics Committee of Beijing Sport University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SQ: Writing – original draft, Writing – review & editing. YF: Investigation, Writing – original draft. WS: Methodology, Writing – original draft. ZW: Investigation, Writing – original draft. ZG: Methodology, Writing – review & editing. XZ: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by a grant from the National Social Science Foundation of China General Education Project: “Scientific Development of Body Composition and Mechanisms of Precision Exercise Promotion in Preschool Children Based on Accelerated Tracking Design” (grant number BLA220235).
Acknowledgments
The authors would like to thank the staff and faculty at the Enjili BSU Kindergarten and at the School of Sport Science at Beijing Sport University, one of which offers the study place and the other offers experimental equipment.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Report of the commission on ending childhood obesity. Geneva: World Health Organization (2016). 50 p.
2. World Health Organization. World obesity day 2022 – Accelerating action to stop obesity. Available online at: https://www.who.int/news/item/04-03-2022-world-obesity-day-2022-accelerating-action-to-stop-obesity (Accessed February 3, 2025).
3. Changing Systems Healthier Lives. Obesity fact sheet 2022. Available online at: https://www.worldobesityday.org/assets/downloads/Factsheet_2022_-_English_-_1pg_1.pdf (Accessed February 3, 2025).
4. The National Health Commission (NHC) of China. The launch of the report on nutrition and chronic diseases of Chinese residents. (2020). Available online at: http://www.scio.gov.cn/xwfbh/xwbfbh/wqfbh/42311/44583/index.htm (Accessed January 1, 2025).
5. Simmonds, M, Burch, J, Llewellyn, A, Griffiths, C, Yang, H, Owen, C, et al. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: a systematic review and meta-analysis. Health Technol Assess. (2015) 19:1–336. doi: 10.3310/hta19430
6. August, GP, Caprio, S, Fennoy, I, Freemark, M, Kaufman, FR, Lustig, RH, et al. Prevention and treatment of pediatric obesity: an endocrine society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab. (2008) 93:4576–99. doi: 10.1210/jc.2007-2458
7. Lakshman, R, Elks, CE, and Ong, KK. Childhood obesity. Circulation. (2012) 126:1770–9. doi: 10.1161/CIRCULATIONAHA.111.047738
8. Tremblay, MS, Duncan, MJ, Kuzik, N, Silva, DAS, and Carson, V. Towards precision 24-hour movement behavior recommendations—the next new paradigm? J Sport Health Sci. (2024) 13:743–8. doi: 10.1016/j.jshs.2024.05.003
9. Su, X, Hassan, MA, Kim, H, and Gao, Z. Comparative effectiveness of lifestyle interventions on children’s body composition management: a systematic review and network meta-analysis. J Sport Health Sci. (2025) 14:101008. doi: 10.1016/j.jshs.2024.101008
10. World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Available online at: https://www.who.int/publications/i/item/9789241550536 (Accessed December 30, 2024).
11. Guan, H, Zhao, X, Qu, S, Wu, J, Yang, Y, Guo, J, et al. Exercise guide for preschool children (3–6 years old). Chin J Child Health Care. (2020) 28:714–20.
12. Hinkley, T, Salmon, J, Okely, AD, Crawford, D, and Hesketh, K. Preschoolers’ physical activity, screen time, and compliance with recommendations. Med Sci Sports Exerc. (2012) 44:458–65. doi: 10.1249/MSS.0b013e318233763b
13. Chaput, J-P, Colley, RC, Aubert, S, Carson, V, Janssen, I, Roberts, KC, et al. Proportion of preschool-aged children meeting the Canadian 24-hour movement guidelines and associations with adiposity: results from the Canadian health measures survey. BMC Public Health. (2017) 17:829. doi: 10.1186/s12889-017-4854-y
14. Gabel, L, Proudfoot, NA, Obeid, J, MacDonald, MJ, Bray, SR, Cairney, J, et al. Step count targets corresponding to new physical activity guidelines for the early years. Med Sci Sports Exerc. (2013) 45:314–8. doi: 10.1249/MSS.0b013e318271765a
15. FitzGerald, TL, Cameron, KL, Albesher, RA, Mentiplay, BF, Lee, KJ, Clark, RA, et al. Strength, motor skills, and physical activity in preschool-aged children born either at less than 30 weeks of gestation or at term. Phys Ther. (2021) 101:pzab–037. doi: 10.1093/ptj/pzab037
16. Chen, B, Bernard, JY, Padmapriya, N, Yao, J, Goh, C, Tan, KH, et al. Socio-demographic and maternal predictors of adherence to 24-hour movement guidelines in Singaporean children. Int J Behav Nutr Phys Act. (2019) 16:70. doi: 10.1186/s12966-019-0834-1
17. Hall, CJS, Eyre, ELJ, Oxford, SW, and Duncan, MJ. Relationships between motor competence, physical activity, and obesity in British preschool aged children. J Funct Morphol Kinesiol. (2018) 3:57. doi: 10.3390/jfmk3040057
18. Slaton, A, Kowalski, AJ, Zemanick, A, Pulling Kuhn, A, Hager, ER, and Black, MM. Motor competence and attainment of global physical activity guidelines among a statewide sample of preschoolers. Int J Environ Res Public Health. (2020) 17:8546. doi: 10.3390/ijerph17228546
19. Ishii, K, Shibata, A, Adachi, M, Nonoue, K, and Oka, K. Gender and grade differences in objectively measured physical activity and sedentary behavior patterns among Japanese children and adolescents: a cross-sectional study. BMC Public Health. (2015) 15:1254. doi: 10.1186/s12889-015-2607-3
20. Chen, S, Liu, Y, Tremblay, MS, Hong, J, Tang, Y, Cao, Z, et al. Meeting 24-h movement guidelines: prevalence, correlates, and the relationships with overweight and obesity among Chinese children and adolescents. J Sport Health Sci. (2021) 10:349–59. doi: 10.1016/j.jshs.2020.07.002
21. Li, F, Yin, L, Sun, M, and Gao, Z. Examining relationships among Chinese preschool children’s meeting 24-hour movement guidelines and fundamental movement skills. J Clin Med. (2022) 11:5623. doi: 10.3390/jcm11195623
22. Yin, L, Li, F, Liu, P, Yin, Z, Yang, Z, Pi, L, et al. Examining the relationship between meeting 24-hour movement behaviour guidelines and mental health in Chinese preschool children. Front Pediatr. (2024) 12:1337158. doi: 10.3389/fped.2024.1337158
23. Sampasa-Kanyinga, H, Standage, M, Tremblay, MS, Katzmarzyk, PT, Hu, G, Kuriyan, R, et al. Associations between meeting combinations of 24-h movement guidelines and health-related quality of life in children from 12 countries. Public Health. (2017) 153:16–24. doi: 10.1016/j.puhe.2017.07.010
24. Saunders, TJ, Gray, CE, Poitras, VJ, Chaput, J-P, Janssen, I, Katzmarzyk, PT, et al. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. (2016) 41:S283–93. doi: 10.1139/apnm-2015-0626
25. Burns, RD, Brusseau, TA, Bai, Y, and Byun, W. Segmented school physical activity and weight status in children: application of compositional data analysis. Int J Environ Res Public Health. (2021) 18:3243. doi: 10.3390/ijerph18063243
26. Gába, A, Pedišić, Ž, Štefelová, N, Dygrýn, J, Hron, K, Dumuid, D, et al. Sedentary behavior patterns and adiposity in children: a study based on compositional data analysis. BMC Pediatr. (2020) 20:147. doi: 10.1186/s12887-020-02036-6
27. Kuzik, N, Poitras, VJ, Tremblay, MS, Lee, E-Y, Hunter, S, and Carson, V. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0-4 years). BMC Public Health. (2017) 17:849. doi: 10.1186/s12889-017-4851-1
28. Taylor, RW, Haszard, JJ, Meredith-Jones, KA, Galland, BC, Heath, A-LM, Lawrence, J, et al. 24-h movement behaviors from infancy to preschool: cross-sectional and longitudinal relationships with body composition and bone health. Int J Behav Nutr Phys Act. (2018) 15:118. doi: 10.1186/s12966-018-0753-6
29. Tan, S, Chen, C, Sui, M, Xue, L, and Wang, J. Exercise training improved body composition, cardiovascular function, and physical fitness of 5-year-old children with obesity or normal body mass. Pediatr Exerc Sci. (2017) 29:245–53. doi: 10.1123/pes.2016-0107
30. Alkon, A, Crowley, AA, Neelon, SEB, Hill, S, Pan, Y, Nguyen, V, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. (2014) 14:215. doi: 10.1186/1471-2458-14-215
31. Annesi, JJ, Smith, AE, and Tennant, GA. Reducing high BMI in African American preschoolers: effects of a behavior-based physical activity intervention on caloric expenditure. South Med J. (2013) 106:456–9. doi: 10.1097/smj.0b013e3182a05bef
32. Llargues, E, Franco, R, Recasens, A, Nadal, A, Vila, M, Pérez, MJ, et al. Assessment of a school-based intervention in eating habits and physical activity in school children: the AVall study. J Epidemiol Community Health. (2011) 65:896–901. doi: 10.1136/jech.2009.102319
33. Eliakim, A, Nemet, D, Balakirski, Y, and Epstein, Y. The effects of nutritional-physical activity school-based intervention on fatness and fitness in preschool children. J Pediatr Endocrinol Metab. (2007) 20:711–8. doi: 10.1515/JPEM.2007.20.6.711
34. Goldfield, GS, Harvey, ALJ, Grattan, KP, Temple, V, Naylor, P-J, Alberga, AS, et al. Effects of child care intervention on physical activity and body composition. Am J Prev Med. (2016) 51:225–31. doi: 10.1016/j.amepre.2016.03.024
35. Reilly, JJ, Kelly, L, Montgomery, C, Williamson, A, Fisher, A, McColl, JH, et al. Physical activity to prevent obesity in young children: cluster randomised controlled trial. BMJ. (2006) 333:1041. doi: 10.1136/bmj.38979.623773.55
36. Davis, SM, Myers, OB, Cruz, TH, Morshed, AB, Canaca, GF, Keane, PC, et al. Chile: outcomes of a group randomized controlled trial of an intervention to prevent obesity in preschool Hispanic and American Indian children. Prev Med. (2016) 89:162–8. doi: 10.1016/j.ypmed.2016.05.018
37. Martínez-Vizcaíno, V, Pozuelo-Carrascosa, DP, García-Prieto, JC, Cavero-Redondo, I, Solera-Martínez, M, Garrido-Miguel, M, et al. Effectiveness of a school-based physical activity intervention on adiposity, fitness and blood pressure: MOVI-KIDS study. Br J Sports Med. (2020) 54:279–85. doi: 10.1136/bjsports-2018-099655
38. Er, V, Dias, KI, Papadaki, A, White, J, Wells, S, Ward, DS, et al. Association of diet in nurseries and physical activity with zBMI in 2–4-year olds in England: a cross-sectional study. BMC Public Health. (2018) 18:1262. doi: 10.1186/s12889-018-6138-6
39. Zhou, Z, Ren, H, Yin, Z, Wang, L, and Wang, K. A policy-driven multifaceted approach for early childhood physical fitness promotion: impacts on body composition and physical fitness in young Chinese children. BMC Pediatr. (2014) 14:118. doi: 10.1186/1471-2431-14-118
40. Ma, L, Zhang, Y, Yang, H, and Jiang, Y. Research on comprehensive intervention approaches and methods for simple obesity in children. Chin J Child Health Care. (2007) 15:183–5. doi: 10.3969/j.issn.1008-6579.2007.02.031
41. Ma, Z, Zhang, Y, Yu, H, and Xu, X. Comparative analysis of obesity intervention methods in school-age children. Contemp Sports Technol. (2012) 2:15–6.
42. Wang, L. 24-hour movement of children and adolescents aged 5–18: current situation, influencing factors, and healthy impact. China Sport Sci Technol. (2022) 58:46–56.
43. Mielke, GI, Ding, D, Keating, SE, Nunes, BP, Brady, R, and Brown, WJ. Physical activity volume, frequency, and intensity: associations with hypertension and obesity over 21 years in Australian women. J Sport Health Sci. (2024) 13:631–41. doi: 10.1016/j.jshs.2024.05.004
44. Bennie, JA, Ding, D, and De Cocker, K. Dose-dependent associations of joint aerobic and muscle-strengthening exercise with obesity: a cross-sectional study of 280, 605 adults. J Sport Health Sci. (2023) 12:186–93. doi: 10.1016/j.jshs.2021.01.002
45. Bürgi, F, Meyer, U, Granacher, U, Schindler, C, Marques-Vidal, P, Kriemler, S, et al. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross-sectional and longitudinal study (Ballabeina). Int J Obes. (2005) 35:937–44. doi: 10.1038/ijo.2011.54
46. Metcalf, BS, Voss, LD, Hosking, J, Jeffery, AN, and Wilkin, TJ. Physical activity at the government-recommended level and obesity-related health outcomes: a longitudinal study (early bird 37). Arch Dis Child. (2008) 93:772–7. doi: 10.1136/adc.2007.135012
47. Leppänen, MH, Henriksson, P, Delisle Nyström, C, Henriksson, H, Ortega, FB, Pomeroy, J, et al. Longitudinal physical activity, body composition, and physical fitness in preschoolers. Med Sci Sports Exerc. (2017) 49:2078–85. doi: 10.1249/MSS.0000000000001313
48. Fu, J, Sun, S, Zhu, S, Wang, R, Chen, D, Chen, R, et al. Relationship between 24-h activity behavior and body fat percentage in preschool children: based on compositional data and isotemporal substitution analysis. BMC Public Health. (2024) 24:1063. doi: 10.1186/s12889-024-18570-2
49. Jiménez-Pavón, D, Kelly, J, and Reilly, JJ. Associations between objectively measured habitual physical activity and adiposity in children and adolescents: systematic review. Int J Pediatr Obes. (2010) 5:3–18. doi: 10.3109/17477160903067601
50. Brener, A, Waksman, Y, Rosenfeld, T, Levy, S, Peleg, I, Raviv, A, et al. The heritability of body composition. BMC Pediatr. (2021) 21:225. doi: 10.1186/s12887-021-02695-z
51. Agbaje, AO, Perng, W, and Tuomainen, T-P. Effects of accelerometer-based sedentary time and physical activity on DEXA-measured fat mass in 6059 children. Nat Commun. (2023) 14:8232. doi: 10.1038/s41467-023-43316-w
52. Pezoa-Fuentes, P, Cossio-Bolaños, M, Urra-Albornoz, C, Alvear-Vasquez, F, Lazari, E, Urzua-Alul, L, et al. Fat-free mass and maturity status are determinants of physical fitness performance in schoolchildren and adolescents. J Pediatr. (2023) 99:38–44. doi: 10.1016/j.jped.2022.03.007
53. Zhao, Y, Gong, J, Ji, Y, Zhao, X, He, L, Cai, S, et al. Cross-sectional study of characteristics of body composition of 24, 845 children and adolescents aged 3–17 years in Suzhou. BMC Pediatr. (2023) 23:358. doi: 10.1186/s12887-023-04134-7
54. Chen, F, Liu, J, Huang, G, and Mi, J. Developmental characteristics on body composition in Chinese urban children and adolescents aged 3-17 years old. Chin J Epidemiol. (2020) 41:213–9. doi: 10.3760/cma.j.issn.0254-6450.2020.02.014
55. Ji, C. Body composition analysis of preschool children. Chin J Women Child Health. (2015) 30:4989–91.
56. Wang, Z, Heshka, S, Pietrobelli, A, Chen, Z, Silva, AM, Sardinha, LB, et al. A new total body potassium method to estimate total body skeletal muscle mass in children. J Nutr. (2007) 137:1988–91. doi: 10.1093/jn/137.8.1988
57. Kamruzzaman, M, Rahman, SA, Akter, S, Shushmita, H, Ali, MY, Billah, MA, et al. The anthropometric assessment of body composition and nutritional status in children aged 2–15 years: a cross-sectional study from three districts in Bangladesh. PLoS One. (2021) 16:e0257055. doi: 10.1371/journal.pone.0257055
58. Wang, W, Tu, C, Han, X, Qin, P, Xia, Y, Zheng, Y, et al. Body composition analysis of preschool children in Hangzhou. Chin J Women Child Health. (2019) 34:4921–3. doi: 10.7620/zgfybj.j.issn.1001-4411.2019.21.26
59. Fan, B, Wang, J, Dong, J, Yang, L, Huang, F, Qian, J, et al. Body composition analysis of preschool children aged 3-6 in Nanjing. Chin J Child Health Care. (2023) 31:1081–1084+1090.
60. Zou, R, Wang, K, Li, D, Liu, Y, Zhang, T, and Wei, X. Study on the relationship and related factors between physical fitness and health behavior of preschool children in Southwest China. BMC Public Health. (2024) 24:1759. doi: 10.1186/s12889-024-19269-0
61. Gao, Z, Zeng, N, Pope, ZC, Wang, R, and Yu, F. Effects of exergaming on motor skill competence, perceived competence, and physical activity in preschool children. J Sport Health Sci. (2019) 8:106–13. doi: 10.1016/j.jshs.2018.12.001
62. Velija, P, and Allen, G. ‘Every day we’d have an arranged activity, so she’d have football, swimming, dance, gymnastics’: a sociological analysis of parenting and sports-based enrichment activities for the under-fives. Int Rev Sociol Sport. (2024) 59:903–20. doi: 10.1177/10126902241238236
63. Bonis, M, Loftin, M, Ward, D, Tseng, TS, Clesi, A, and Sothern, M. Improving physical activity in daycare interventions. Child Obes. (2014) 10:334–41. doi: 10.1089/chi.2014.0040
64. Gao, Z, Chen, S, Pasco, D, and Pope, Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes Rev. (2015) 16:783–94. doi: 10.1111/obr.12287
65. Gao, Z. Growth trajectories of young children’s objectively determined physical activity, sedentary behavior, and body mass index. Child Obes. (2018) 14:259–64. doi: 10.1089/chi.2018.0042
66. Cooper, AR, Goodman, A, Page, AS, Sherar, LB, Esliger, DW, van Sluijs, EM, et al. Objectively measured physical activity and sedentary time in youth: the international children’s accelerometry database (ICAD). Int J Behav Nutr Phys Act. (2015) 12:113. doi: 10.1186/s12966-015-0274-5
67. Chen, H, Liu, J, and Bai, Y. Global accelerometer-derived physical activity levels from preschoolers to adolescents: a multilevel meta-analysis and meta-regression. Ann Behav Med. (2023) 57:511–29. doi: 10.1093/abm/kaac030
68. Deng, P, Ozaki, H, Natsume, T, Ishihara, Y, Ke, D, Suzuki, K, et al. Relationship between skeletal muscle thickness and physical activity in 4- to 6-year-olds in Japan. Children. (2023) 10:455. doi: 10.3390/children10030455
69. Ferrari, GLM, Oliveira, LC, Araujo, TL, Matsudo, V, Barreira, TV, Tudor-Locke, C, et al. Moderate-to-vigorous physical activity and sedentary behavior: independent associations with body composition variables in Brazilian children. Pediatr Exerc Sci. (2015) 27:380–9. doi: 10.1123/pes.2014-0150
70. Basterfield, L, Pearce, MS, Adamson, AJ, Frary, JK, Parkinson, KN, Wright, CM, et al. Physical activity, sedentary behavior, and adiposity in English children. Am J Prev Med. (2012) 42:445–51. doi: 10.1016/j.amepre.2012.01.007
71. Webster, EK, Martin, CK, and Staiano, AE. Fundamental motor skills, screen-time, and physical activity in preschoolers. J Sport Health Sci. (2019) 8:114–21. doi: 10.1016/j.jshs.2018.11.006
72. Zhao, G, Wang, R, Quan, M, Cao, Z, Zhang, H, Zhang, J, et al. Effects of physical activity on physical growth of preschool children. J Shanghai Univ Sport. (2017) 41:65–9. doi: 10.16099/j.sus.2017.04.011
73. Jung, S, Park, J, and Seo, Y-G. Relationship between arm-to-leg and limbs-to-trunk body composition ratio and cardiovascular disease risk factors. Sci Rep. (2021) 11:17414. doi: 10.1038/s41598-021-96874-8
74. Santarém, GC d F, de Cleva, R, Santo, MA, Bernhard, AB, Gadducci, AV, Greve, JMD, et al. Correlation between body composition and walking capacity in severe obesity. PLoS One. (2015) 10:e0130268. doi: 10.1371/journal.pone.0130268
75. Ministry of Education of the People’s Republic of China. Guidelines for the learning and development of children aged 3–6. Beijing: Capital Normal University Press (2012).
76. Aadland, E, Tjomsland, HE, Johannessen, K, Nilsen, AKO, Resaland, GK, Glosvik, Ø, et al. Active learning Norwegian preschool (er) s (ACTNOW) – design of a cluster randomized controlled trial of staff professional development to promote physical activity, motor skills, and cognition in preschoolers. Front Psychol. (2020) 11:1382. doi: 10.3389/fpsyg.2020.01382
77. Best, JR. Exergaming immediately enhances children’s executive function. Dev Psychol. (2012) 48:1501–10. doi: 10.1037/a0026648
78. Butte, NF, Wong, WW, Lee, JS, Adolph, AL, Puyau, MR, and Zakeri, IF. Prediction of energy expenditure and physical activity in preschoolers. Med Sci Sports Exerc. (2014) 46:1216–26. doi: 10.1249/MSS.0000000000000209
79. Gai, X, Xu, J, Yan, Y, Wang, Y, and Xie, X. Exergame can improve children’s executive function: the role of physical intensity and cognitive engagement. Acta Psychol Sin. (2021) 53:505. doi: 10.3724/SP.J.1041.2021.00505
80. Zhang, Y, He, Z, and Xu, J. National physical fitness surveillance and evaluation. Beijing: Science Press (2017). 378 p.
81. Laskey, MA. Dual-energy X-ray absorptiometry and body composition. Nutrition. (1996) 12:45–51. doi: 10.1016/0899-9007(95)00017-8
82. Verney, J, Metz, L, Chaplais, E, Cardenoux, C, Pereira, B, and Thivel, D. Bioelectrical impedance is an accurate method to assess body composition in obese but not severely obese adolescents. Nutr Res. (2016) 36:663–70. doi: 10.1016/j.nutres.2016.04.003
83. InBody Co., Ltd. Inbody J30 user’s manual. Available online at: https://ekp.inbody.com/en/technology/contents/inbodytest (Accessed January 1, 2025).
84. Wong, JE, Parnell, WR, Black, KE, and Skidmore, PML. Reliability and relative validity of a food frequency questionnaire to assess food group intakes in New Zealand adolescents. Nutr J. (2012) 11:65. doi: 10.1186/1475-2891-11-65
85. Richardson, JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev. (2011) 6:135–47. doi: 10.1016/j.edurev.2010.12.001
86. Druet, C, and Ong, KK. Early childhood predictors of adult body composition. Best Pract Res Clin Endocrinol Metab. (2008) 22:489–502. doi: 10.1016/j.beem.2008.02.002
87. Wald, ER, Ewing, LJ, Moyer, SCL, and Eickhoff, JC. An interactive web-based intervention to achieve healthy weight in young children. Clin Pediatr (Phila). (2018) 57:547–57. doi: 10.1177/0009922817733703
88. Hammersley, ML, Okely, AD, Batterham, MJ, and Jones, RA. An internet-based childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged children: randomized controlled trial. J Med Internet Res. (2019) 21:e11964. doi: 10.2196/11964
89. Paineau, DL, Beaufils, F, Boulier, A, Cassuto, D-A, Chwalow, J, Combris, P, et al. Family dietary coaching to improve nutritional intakes and body weight control: a randomized controlled trial. Arch Pediatr Adolesc Med. (2008) 162:34–43. doi: 10.1001/archpediatrics.2007.2
90. Yavuz, HM, van Ijzendoorn, MH, Mesman, J, and van der Veek, S. Interventions aimed at reducing obesity in early childhood: a meta-analysis of programs that involve parents. J Child Psychol Psychiatry. (2015) 56:677–92. doi: 10.1111/jcpp.12330
91. Gruber, KJ, and Haldeman, LA. Using the family to combat childhood and adult obesity. Prev Chronic Dis. (2009) 6:A106.
92. Waters, E, de Silva-Sanigorski, A, Burford, BJ, Brown, T, Campbell, KJ, Gao, Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. (2011) 12:CD001871. doi: 10.1002/14651858.CD001871.pub3
93. Tovar, A, Renzaho, AMN, Guerrero, AD, Mena, N, and Ayala, GX. A systematic review of obesity prevention intervention studies among immigrant populations in the US. Curr Obes Rep. (2014) 3:206–22. doi: 10.1007/s13679-014-0101-3
94. Reilly, JJ, and McDowell, ZC. Physical activity interventions in the prevention and treatment of paediatric obesity: systematic review and critical appraisal. Proc Nutr Soc. (2003) 62:611–9. doi: 10.1079/PNS2003276
95. Reilly, JJ, Wilson, ML, Summerbell, CD, and Wilson, DC. Obesity: diagnosis, prevention, and treatment; evidence based answers to common questions. Arch Dis Child. (2002) 86:392–4. doi: 10.1136/adc.86.6.392
96. Wang, J, Han, H, and Zhang, H. Effects of high-intensity interval training on abdominal fat content in young obese women. Chin J Sports Med. (2015) 34:15–20,30.
97. Hernández-Reyes, A, Cámara-Martos, F, Molina-Luque, R, Romero-Saldaña, M, Molina-Recio, G, and Moreno-Rojas, R. Changes in body composition with a hypocaloric diet combined with sedentary, moderate and high-intense physical activity: a randomized controlled trial. BMC Womens Health. (2019) 19:167. doi: 10.1186/s12905-019-0864-5
98. Logan, GRM, Harris, N, Duncan, S, Plank, LD, Merien, F, and Schofield, G. Low-active male adolescents: a dose response to high-intensity interval training. Med Sci Sports Exerc. (2016) 48:481–90. doi: 10.1249/MSS.0000000000000799
99. Feng, Y. Dose-response effects of treadmill training at different intensities on body composition intervention in male college students. Chin Sch Phys Educ High Educ. (2018) 5:82–6.
100. Herrmann, D, Buck, C, Sioen, I, Kouride, Y, Marild, S, Molnár, D, et al. Impact of physical activity, sedentary behaviour and muscle strength on bone stiffness in 2-10-year-old children-cross-sectional results from the IDEFICS study. Int J Behav Nutr Phys Act. (2015) 12:112. doi: 10.1186/s12966-015-0273-6
101. Wyszyńska, J, Matłosz, P, Szybisty, A, Lenik, P, Dereń, K, Mazur, A, et al. Obesity and body composition in preschool children with different levels of Actigraphy-derived physical activity-a cross-sectional study. J Clin Med. (2020) 9:1210. doi: 10.3390/jcm9041210
102. Morelli, C, Avolio, E, Galluccio, A, Caparello, G, Manes, E, Ferraro, S, et al. Impact of vigorous-intensity physical activity on body composition parameters, lipid profile markers, and Irisin levels in adolescents: a cross-sectional study. Nutrients. (2020) 12:742. doi: 10.3390/nu12030742
103. Costa-Urrutia, P, Vizuet-Gámez, A, Ramirez-Alcántara, M, Guillen-González, MÁ, Medina-Contreras, O, Valdes-Moreno, M, et al. Obesity measured as percent body fat, relationship with body mass index, and percentile curves for Mexican pediatric population. PLoS One. (2019) 14:e0212792. doi: 10.1371/journal.pone.0212792
104. Tu, C, Zhang, Y, Wu, D, Zhang, S, and Jiang, C. Construction BMI percentile standard curve and cut-off points for overweight and obesity of 3~6 years children based on GAMLSS model in China. China Sport Sci. (2021) 41:63–73. doi: 10.16469/j.css.202103008
Keywords: body mass index, childhood obesity, sex differences, light physical activity, moderate-to-vigorous physical activity
Citation: Qu S, Feng Y, Song W, Wang Z, Gao Z and Zhao X (2025) Effects of different game-based physical activity programs on body composition in Chinese preschool children. Front. Public Health. 13:1592084. doi: 10.3389/fpubh.2025.1592084
Edited by:
Maurizio Delvecchio, University of L’Aquila, ItalyCopyright © 2025 Qu, Feng, Song, Wang, Gao and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sha Qu, cXVzaGFAYnN1LmVkdS5jbg==; Xing Zhao, emhhb3hpbmdAYnN1LmVkdS5jbg==
 Sha Qu
Sha Qu Yueyu Feng1
Yueyu Feng1 Zan Gao
Zan Gao Xing Zhao
Xing Zhao